User login
Unhealthy drug use: How to screen, when to intervene
› Implement screening and brief intervention (SBI) for unhealthy drug use among adults in primary care. C
› Consult the National Institute on Drug Abuse’s Screening for Drug Use in General Medical Settings Resource Guide for step-by-step recommendations for implementing a drug SBI. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Joe M, age 54, comes to your office for his annual physical examination. As part of your routine screening, you ask him, “In the past year, how often have you used alcohol, tobacco, prescription drugs for nonmedical reasons, or illegal drugs?” Mr. M replies that he does not use tobacco and has not used prescription drugs for nonmedical reasons, but drinks alcohol weekly and uses cannabis and cocaine monthly.
If Mr. M were your patient, what would your next steps be?
One promising approach to alleviate substance use problems is screening and brief intervention (SBI), and—when appropriate—referral to an addiction treatment program. With strong evidence of efficacy, alcohol and tobacco SBIs have become recommended “usual” care for adults in primary care settings.1,2 Strategies for applying SBI to unhealthy drug use (“drug” SBI) in primary care have been a natural extension of the evidence that supports alcohol and tobacco SBIs.
Screening for unhealthy drug use consists of a quick risk appraisal, typically via a brief questionnaire.3-5 Patients with a positive screen then receive a more detailed assessment to estimate the extent of their substance use and severity of its consequences. If appropriate, this is followed with a brief intervention (BI), which is a time-limited, patient-centered counseling session designed to reduce substance use and/or related harm.4-6
So how can you make use of a drug SBI in your office setting?
Drug screening: What the evidence says
Currently, evidence on drug SBI is limited. The US Preventive Services Task Force (USPSTF) found insufficient evidence to recommend for or against universal drug SBI.4,7,8 The scarcity of validated screening and assessment tools that are brief enough to be used in primary care, patients’ use of multiple drugs, and confidentiality concerns likely contribute to the relative lack of research in this area.3,6,9
To our knowledge, results of only 5 randomized controlled trials (RCTs) of drug SBI that included universal screening have been published in English. Here is what these researchers found:
Bernstein et al10 investigated the efficacy of SBI for cocaine and heroin use among 23,699 adults in urgent care, women’s health, and homeless clinic settings. They randomized 1175 patients who screened positive on the Drug Abuse Screening Test11 to receive a single BI session or a handout. At 6 months, patients in the BI group were 1.5 times more likely than controls to be abstinent from cocaine (22% vs 17%; P=.045) and heroin (40% vs 31%; P=.050).
Zahradnik et al12 examined the efficacy of SBI in reducing the use of potentially addictive prescription drugs by hospitalized patients. After researchers screened 6000 inpatients, 126 patients who used, abused, or were dependent on prescription medications were randomized to receive 2 BI sessions or an information booklet. At 3 months, 52% of patients in the BI group had a ≥25% reduction in their daily doses of prescription drugs, compared to 30% in the control group (P=.017),12 However, this difference was not maintained at 12 months.13
Humeniuk et al14 evaluated the efficacy of SBI among primary care patients ages 16 to 62 years in Australia, Brazil, India, and the United States who used cannabis, cocaine, amphetamines, or opioids. Patients were screened and assessed using the World Health Organization Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).15 Patients whose scores indicated they had a moderate risk for problem use (N=731) were randomly assigned to receive a BI or usual care. At 3 months, patients in the BI group reported a reduction in total score for “illicit substance involvement” compared to controls (P<.001). However, country-specific analyses found that BI did not have a statistically significant effect on drug use by those in the United States (N=218), possibly due to protocol differences and a greater exposure to previous substance use treatment among US patients.14
Saitz et al16 investigated the efficacy of drug SBI among primary care patients (N=528) who had been screened using the ASSIST. The most commonly used drugs were marijuana (63% of patients), cocaine (19%), and opioids (17%). Patients were randomly assigned to a 10- to 15-minute BI, a 30- to 45-minute intervention, or no intervention. BI did not show efficacy for decreasing drug use at 6-month follow-up.
Roy-Byrne et al17 screened 10,337 primary care patients of “safety net” clinics serving low-income populations. Of 1621 patients who screened positive for problem drug use, 868 were enrolled and randomly assigned to either a BI group (one-time BI using motivational interviewing, a telephone booster session, and a handout, which included relevant drug-use related information and a list of substance abuse resources) or enhanced care as usual (usual care plus a handout). Over 12 months of follow-up, there were no differences between groups in drug use or related consequences. However, a subgroup analysis suggested that compared to enhanced usual care, BI may help reduce emergency department use and increase admissions to specialized drug treatment programs among those with severe drug problems.
In addition to these 5 RCTs, a large, prospective, uncontrolled trial looked at the efficacy of drug BI among 459,599 patients from various medical settings, including primary care.18 Twenty-three percent of patients screened positive for illicit drug use and were recommended BI (16%), brief treatment (3%) or specialty treatment (4%). At a 6-month follow-up, drug use among these patients decreased by 68% and heavy alcohol use decreased by 39% (P<.001). In addition, general health, mental health, employment, housing status, and criminal behavior improved among patients recommended for brief or specialty treatments (P<.001). Although this trial lent support for the efficacy of drug SBI in primary care, it was limited by the lack of a control group and low follow-up rates at some sites.
A step-by-step approach to drug screening
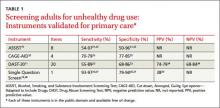
Although a variety of instruments can be used to screen and assess patients for unhealthy drug use, few have been validated in primary care (TABLE 1).11,15,19-27 Despite limited evidence, multiple professional organizations, including the American Academy of Family Physicians28 and the American Psychiatric Association,26 support routine implementation of drug SBI in primary care.
The National Institute on Drug Abuse (NIDA)’s Screening for Drug Use in General Medical Settings Resource Guide19 provides a step-by-step approach to drug SBI in primary care and other general medical settings. Primarily focused on drug SBI in adults, the NIDA guide details the use of the NIDA Quick Screen and the NIDA-Modified ASSIST (NM ASSIST). These tools are available as a PDF that you can print out and complete manually (http://www.drugabuse.gov/sites/default/ files/pdf/nmassist.pdf) or as a series of forms you can complete online (http://www.drugabuse.gov/nmassist). The NIDA guide also conveniently incorporates links to alcohol and tobacco SBI recommendations.
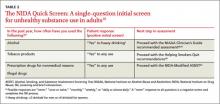
What to ask first. Following the NIDA algorithm, first screen patients with the Quick Screen, which consists of a single question about substance use: “In the past year, how often have you used alcohol, tobacco products, prescription drugs for nonmedical reasons, or illegal drugs?" (TABLE 2).19,29-32
A negative Quick Screen (a “never” response for all substances) completes the process. Patients with a negative screen should be praised and encouraged to continue their healthy lifestyle, then rescreened annually.
For patients who respond “Yes” to heavy drinking or any tobacco use, the NIDA guide recommends proceeding with an alcohol29 or tobacco30 SBI, respectively, and provides links to appropriate resources (TABLE 2).19,29-32 Those who screen positive for drugs (“Yes” to any drug use in the past year) should receive a detailed assessment using the NM ASSIST32 to determine their risk level for developing a substance use disorder. The NM ASSIST includes 8 questions about the patient’s desire for, use of, and problems related to the use of a wide range of drugs, including cannabis, cocaine, methamphetamine, hallucinogens, and other substances (eg, “In the past 3 months, how often have you used the following substances?” “How often have you had a strong desire or urge to use this substance?” “How often has your use of this substance led to health, social, legal or financial problems?”). The score on the NM ASSIST is used to calculate the patient’s risk level as low, moderate, or high.
For patients who use more than one drug, this risk level is scored separately for each drug and may differ from drug to drug. Multi-drug assessment can become time-consuming and may not be appropriate in some patients, especially if time is an issue (eg, the patient would like to focus on other concerns) or the patient is not interested in addressing certain drugs. In general, the decision about which substances to address should be clinically-driven, tailored to the needs of an individual patient. Focusing on the substance with the highest risk score or associated with the patient’s expressed greatest motivation to change may produce the best results.
CASE › Based on Mr. M’s response to your Quick Screen indicating he drinks alcohol and uses illicit drugs, you administer the NM ASSIST to perform a detailed assessment. His answer to a screening question for problematic alcohol use is negative (In the past year, he has not had >4 drinks in a day). Next, you calculate his NM ASSIST-based risk scores for cannabis and cocaine, and determine he is at moderate risk for developing problems due to cannabis use and at high risk for developing problems based on his use of cocaine. You also note Mr. M’s blood pressure (BP) is elevated (155/90 mm hg).
Conducting a brief intervention
Depending on the patient’s risk level for developing a substance use disorder, he or she should receive either brief advice (for those at low risk) or a BI (for those at moderate or high risk) and, if needed, a referral to treatment. Two popular approaches are FRAMES (Feedback, Responsibility, Advice, Menu of Strategies, Empathy, Self-efficacy) and the NIDA-recommended 5 As intervention. The latter approach entails Asking the patient about his drug use (via the Quick Screen); Advising the patient about his drug use by providing specific medical advice on why he should stop or cut down, and how; Assessing the patient’s readiness to quit or reduce use; Assisting the patient in making a change by creating a plan with specific goals; and Arranging a follow-up visit or specialty assessment and treatment by making referrals as appropriate.19
What about children and adolescents? Implementing a drug SBI in young patients often entails overcoming unique challenges and ethical dilemmas. Although the American Academy of Pediatrics recommends SBI for unhealthy drug and alcohol use among children and adolescents,33,34 the USPSTF did not find sufficient evidence to recommend the practice.1,8,35 Screening for drug use in minors often is complicated by questions about the age at which to start routine screening and issues related to confidentiality and parental involvement. The Center for Adolescent Health and the Law and the National Institute on Alcohol Abuse and Alcoholism provide useful resources related to youth SBI, including guidance on when to consider breeching a child’s confidentiality by engaging parents or guardians (TABLE 3).
TABLE 3
Resources
NIDA Resource Guide NIDA-Modified ASSIST Coding for SBI reimbursement SAMHSA’s Treatment Services Locator NIDA’s List of Community Treatment Programs SAMHSA Opioid Overdose Toolkit Buprenorphine training program Center for Adolescent Health and the Law NIAAA Alcohol Screening and Brief Intervention for Youth |
Help is available for securing treatment, reimbursement
In addition to NIDA, many other organizations offer resources to assist clinicians in using drug SBI and helping patients obtain treatment (TABLE 3). For reimbursement, the Centers for Medicare and Medicaid Services has adopted billing codes for SBI services.36,37 The Substance Abuse and Mental Health Services Administration (SAMHSA)’s Behavioral Health Treatment Services Locator and NIDA’s National Drug Abuse Treatment Clinical Trials Network List of Associated Community Treatment Programs can assist clinicians and patients in finding specialty treatment programs. Self-help groups such as Narcotics Anonymous, Alcoholic Anonymous, or Self-Managment and Recovery Training may help alleviate problems related to insurance coverage, location, and/or timing of services.
SAMHSA’s Opioid Overdose Toolkit provides guidance to clinicians and patients on ways to reduce the risk of overdose. Physicians also can complete a short training program in office-based buprenorphine maintenance therapy to provide evidence-based care to patients with opioid dependence; more details about this program are available from http://www.buppractice.com.
CASE › You decide to use the 5 as intervention with Mr. M. You explain to him that he is at high risk of developing a substance use disorder. You also discuss his elevated BP and the possible negative effects of drug use, especially cocaine, on BP. You advise him that medically it is in his best interest to stop using cocaine and stop or reduce using cannabis. When you ask Mr. M about his readiness to change his drug use, he expresses moderate interest in stopping cocaine but is not willing to reduce his cannabis use. At this time, he is not willing to discuss these issues further (“I’ll think about that”) or create a specific plan. You assure him of your ongoing support, provide him with resources on specialty treatment programs should he wish to consider those, and schedule a follow-up visit in 2 weeks to address BP and, if the patient agrees, drug use.
CORRESPONDENCE
Aleksandra Zgierska, MD, Phd, Department of Family Medicine, University of Wisconsin School of Medicine and Public Health, 1100 Delaplaine Court, Madison, WI 53715-1896; [email protected]
1. US Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/ uspsdrin.htm. Accessed March 4, 2013.
2. US Preventive Services Task Force. Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstbac2.htm. Accessed March 4, 2014.
3. Saitz R, Alford DP, Bernstein J, et al. Screening and brief intervention for unhealthy drug use in primary care settings: randomized clinical trials are needed. J Addict Med. 2010;4: 123-130.
4. Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst Abuse Rehabil. 2012;3:25-34.
5. Substance Abuse and Mental Health Services Administration. Screening, Brief Intervention, and Referral to Treatment (SBIRT). Substance Abuse and Mental Health Services Administration Web site. Available at: http://www.samhsa.gov/ prevention/sbirt/. Accessed March 4, 2014.
6. Squires LE, Alford DP, Bernstein J, et al. Clinical case discussion: screening and brief intervention for drug use in primary care. J Addict Med. 2010;4:131-136.
7. Krupski A, Joesch JM, Dunn C, et al. Testing the effects of brief intervention in primary care for problem drug use in a randomized controlled trial: rationale, design, and methods. Addict Sci Clin Pract. 2012;7:27.
8. US Preventive Services Task Force. Screening for illicit drug use. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrug.htm. Accessed March 4, 2014.
9. Lanier D, Ko S. Screening in Primary Care Settings for Illicit Drug Use: Assessment of Screening Instruments—A Supplemental Evidence Update for the U.S. Preventive Services Task Force. AHRQ Publication No. 08-05108-EF-2. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
10. Bernstein J, Bernstein E, Tassiopoulos K, et al. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug Alcohol Depend. 2005;77:49-59.
11. Skinner HA. The drug abuse screening test. Addict Behav. 1982;7:363-371.
12. Zahradnik A, Otto C, Crackau B, et al. Randomized controlled trial of a brief intervention for problematic prescription drug use in non-treatment-seeking patients. Addiction. 2009;104:109-117.
13. Otto C, Crackau B, Löhrmann I, et al. Brief intervention in general hospital for problematic prescription drug use: 12-month outcome. Drug Alcohol Depend. 2009;105:221-226.
14. Humeniuk R, Ali R, Babor T, et al. A randomized controlled trial of a brief intervention for illicit drugs linked to the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in clients recruited from primary health-care settings in four countries. Addiction. 2012;107:957-966.
15. WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97:1183-1194.
16. Saitz R, Palfai TP, Cheng DM, et al. Screening and brief intervention for drug use in primary care: the Assessing Screening Plus brief Intervention’s Resulting Efficacy to stop drug use (ASPIRE) randomized trial. Addict Sci Clin Pract. 2013;8(suppl 1):A61.
17. Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. JAMA. 2014;312(5):492-501.
18. Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99:280-295.
19. National Institute on Drug Abuse. Resource guide: Screening for drug use in general medical settings. National Institute on Drug Abuse Web site. Available at: http://www.drugabuse. gov/publications/resource-guide. Accessed March 8, 2014.
20. Saitz R, Cheng DM, Allensworth-Davies D, et al. The ability of single screening questions for unhealthy alcohol and other drug use to identify substance dependence in primary care. J Stud Alcohol Drugs. 2014;75:153-157.
21. Newcombe DA, Humeniuk RE, Ali R. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev. 2005;24:217-226.
22. Humeniuk R, Ali R, Babor TF, et al. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST). Addiction. 2008;103:1039-1047.
23. Mdege ND, Lang J. Screening instruments for detecting illicit drug use/abuse that could be useful in general hospital wards: a systematic review. Addict Behav. 2011;36:1111-1119.
24. Cassidy CM, Schmitz N, Malla A. Validation of the alcohol use disorders identification test and the drug abuse screening test in first episode psychosis. Can J Psychiatry. 2008;53:26-33.
25. Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 1995;94:135-140.
26. American Psychiatric Association. Position statement on substance use disorders. American Psychiatric Association Web site. Available at: http://www.psychiatry.org/File%20Library/Advocacy%20and%20Newsroom/Position%20Statements/ps2012_Substance.pdf. Accessed March 4, 2014.
27. Smith PC, Schmidt SM, Allensworth-Davies D, et al. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170:1155-1160.
28. American Academy of Family Physicians. Substance abuse and addiction. American Academy of Family Physicians Web site. Available at: http://www.aafp.org/about/policies/all/substance-abuse.html. Accessed March 4, 2014.
29. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide. National Institute on Alcohol Abuse and Alcoholism Web site. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed March 4, 2014.
30. US Department of Health and Human Services Public Health Service. Helping smokers quit: A guide for clinicians. US Department of Health and Human Services Public Health Service Web site. Available at: http://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/tobacco/clinicians//clinhlpsmkqt/. Accessed March 4, 2014.
31. National Institute on Alcohol Abuse and Alcoholism. A Pocket Guide for Alcohol Screening and Brief Intervention. National Institute on Alcohol Abuse and Alcoholism Web site. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/pocketguide/pocket_guide.htm. Accessed July 30, 2014.
32. National Institute on Drug Abuse. NIDA-Quick Screen V1.0. National Institute on Drug Abuse Web site. Available at: http://www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf. Accessed March 4, 2014.
33. Committee on Substance Abuse, Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128:e1330-e1340.
34. Kulig JW; American Academy of Pediatrics Committee on Substance Abuse. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics. 2005;115:816-821.
35. US Preventive Services Task Force. Primary care behavioral interventions to reduce the nonmedical use of drugs in children and adolescents. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsnonmed.htm. Accessed March 4, 2014.
36. Centers for Medicare & Medicaid Services. Screening, Brief Intervention, and Referral to Treatment (SBIRT) services. Centers for Medicare & Medicaid Services Web site. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/sbirt_factsheet_icn904084.pdf. Accessed March 4, 2014.
37. Substance Abuse and Mental Health Services Administration. Coding for screening and brief intervention reimbursement. Substance Abuse and Mental Health Services Administration Web site. Available at: http://beta.samhsa.gov/sbirt/coding-reimbursement. Accessed August 4, 2014.
› Implement screening and brief intervention (SBI) for unhealthy drug use among adults in primary care. C
› Consult the National Institute on Drug Abuse’s Screening for Drug Use in General Medical Settings Resource Guide for step-by-step recommendations for implementing a drug SBI. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Joe M, age 54, comes to your office for his annual physical examination. As part of your routine screening, you ask him, “In the past year, how often have you used alcohol, tobacco, prescription drugs for nonmedical reasons, or illegal drugs?” Mr. M replies that he does not use tobacco and has not used prescription drugs for nonmedical reasons, but drinks alcohol weekly and uses cannabis and cocaine monthly.
If Mr. M were your patient, what would your next steps be?
One promising approach to alleviate substance use problems is screening and brief intervention (SBI), and—when appropriate—referral to an addiction treatment program. With strong evidence of efficacy, alcohol and tobacco SBIs have become recommended “usual” care for adults in primary care settings.1,2 Strategies for applying SBI to unhealthy drug use (“drug” SBI) in primary care have been a natural extension of the evidence that supports alcohol and tobacco SBIs.
Screening for unhealthy drug use consists of a quick risk appraisal, typically via a brief questionnaire.3-5 Patients with a positive screen then receive a more detailed assessment to estimate the extent of their substance use and severity of its consequences. If appropriate, this is followed with a brief intervention (BI), which is a time-limited, patient-centered counseling session designed to reduce substance use and/or related harm.4-6
So how can you make use of a drug SBI in your office setting?
Drug screening: What the evidence says
Currently, evidence on drug SBI is limited. The US Preventive Services Task Force (USPSTF) found insufficient evidence to recommend for or against universal drug SBI.4,7,8 The scarcity of validated screening and assessment tools that are brief enough to be used in primary care, patients’ use of multiple drugs, and confidentiality concerns likely contribute to the relative lack of research in this area.3,6,9
To our knowledge, results of only 5 randomized controlled trials (RCTs) of drug SBI that included universal screening have been published in English. Here is what these researchers found:
Bernstein et al10 investigated the efficacy of SBI for cocaine and heroin use among 23,699 adults in urgent care, women’s health, and homeless clinic settings. They randomized 1175 patients who screened positive on the Drug Abuse Screening Test11 to receive a single BI session or a handout. At 6 months, patients in the BI group were 1.5 times more likely than controls to be abstinent from cocaine (22% vs 17%; P=.045) and heroin (40% vs 31%; P=.050).
Zahradnik et al12 examined the efficacy of SBI in reducing the use of potentially addictive prescription drugs by hospitalized patients. After researchers screened 6000 inpatients, 126 patients who used, abused, or were dependent on prescription medications were randomized to receive 2 BI sessions or an information booklet. At 3 months, 52% of patients in the BI group had a ≥25% reduction in their daily doses of prescription drugs, compared to 30% in the control group (P=.017),12 However, this difference was not maintained at 12 months.13
Humeniuk et al14 evaluated the efficacy of SBI among primary care patients ages 16 to 62 years in Australia, Brazil, India, and the United States who used cannabis, cocaine, amphetamines, or opioids. Patients were screened and assessed using the World Health Organization Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).15 Patients whose scores indicated they had a moderate risk for problem use (N=731) were randomly assigned to receive a BI or usual care. At 3 months, patients in the BI group reported a reduction in total score for “illicit substance involvement” compared to controls (P<.001). However, country-specific analyses found that BI did not have a statistically significant effect on drug use by those in the United States (N=218), possibly due to protocol differences and a greater exposure to previous substance use treatment among US patients.14
Saitz et al16 investigated the efficacy of drug SBI among primary care patients (N=528) who had been screened using the ASSIST. The most commonly used drugs were marijuana (63% of patients), cocaine (19%), and opioids (17%). Patients were randomly assigned to a 10- to 15-minute BI, a 30- to 45-minute intervention, or no intervention. BI did not show efficacy for decreasing drug use at 6-month follow-up.
Roy-Byrne et al17 screened 10,337 primary care patients of “safety net” clinics serving low-income populations. Of 1621 patients who screened positive for problem drug use, 868 were enrolled and randomly assigned to either a BI group (one-time BI using motivational interviewing, a telephone booster session, and a handout, which included relevant drug-use related information and a list of substance abuse resources) or enhanced care as usual (usual care plus a handout). Over 12 months of follow-up, there were no differences between groups in drug use or related consequences. However, a subgroup analysis suggested that compared to enhanced usual care, BI may help reduce emergency department use and increase admissions to specialized drug treatment programs among those with severe drug problems.
In addition to these 5 RCTs, a large, prospective, uncontrolled trial looked at the efficacy of drug BI among 459,599 patients from various medical settings, including primary care.18 Twenty-three percent of patients screened positive for illicit drug use and were recommended BI (16%), brief treatment (3%) or specialty treatment (4%). At a 6-month follow-up, drug use among these patients decreased by 68% and heavy alcohol use decreased by 39% (P<.001). In addition, general health, mental health, employment, housing status, and criminal behavior improved among patients recommended for brief or specialty treatments (P<.001). Although this trial lent support for the efficacy of drug SBI in primary care, it was limited by the lack of a control group and low follow-up rates at some sites.
A step-by-step approach to drug screening
Although a variety of instruments can be used to screen and assess patients for unhealthy drug use, few have been validated in primary care (TABLE 1).11,15,19-27 Despite limited evidence, multiple professional organizations, including the American Academy of Family Physicians28 and the American Psychiatric Association,26 support routine implementation of drug SBI in primary care.
The National Institute on Drug Abuse (NIDA)’s Screening for Drug Use in General Medical Settings Resource Guide19 provides a step-by-step approach to drug SBI in primary care and other general medical settings. Primarily focused on drug SBI in adults, the NIDA guide details the use of the NIDA Quick Screen and the NIDA-Modified ASSIST (NM ASSIST). These tools are available as a PDF that you can print out and complete manually (http://www.drugabuse.gov/sites/default/ files/pdf/nmassist.pdf) or as a series of forms you can complete online (http://www.drugabuse.gov/nmassist). The NIDA guide also conveniently incorporates links to alcohol and tobacco SBI recommendations.
What to ask first. Following the NIDA algorithm, first screen patients with the Quick Screen, which consists of a single question about substance use: “In the past year, how often have you used alcohol, tobacco products, prescription drugs for nonmedical reasons, or illegal drugs?" (TABLE 2).19,29-32
A negative Quick Screen (a “never” response for all substances) completes the process. Patients with a negative screen should be praised and encouraged to continue their healthy lifestyle, then rescreened annually.
For patients who respond “Yes” to heavy drinking or any tobacco use, the NIDA guide recommends proceeding with an alcohol29 or tobacco30 SBI, respectively, and provides links to appropriate resources (TABLE 2).19,29-32 Those who screen positive for drugs (“Yes” to any drug use in the past year) should receive a detailed assessment using the NM ASSIST32 to determine their risk level for developing a substance use disorder. The NM ASSIST includes 8 questions about the patient’s desire for, use of, and problems related to the use of a wide range of drugs, including cannabis, cocaine, methamphetamine, hallucinogens, and other substances (eg, “In the past 3 months, how often have you used the following substances?” “How often have you had a strong desire or urge to use this substance?” “How often has your use of this substance led to health, social, legal or financial problems?”). The score on the NM ASSIST is used to calculate the patient’s risk level as low, moderate, or high.
For patients who use more than one drug, this risk level is scored separately for each drug and may differ from drug to drug. Multi-drug assessment can become time-consuming and may not be appropriate in some patients, especially if time is an issue (eg, the patient would like to focus on other concerns) or the patient is not interested in addressing certain drugs. In general, the decision about which substances to address should be clinically-driven, tailored to the needs of an individual patient. Focusing on the substance with the highest risk score or associated with the patient’s expressed greatest motivation to change may produce the best results.
CASE › Based on Mr. M’s response to your Quick Screen indicating he drinks alcohol and uses illicit drugs, you administer the NM ASSIST to perform a detailed assessment. His answer to a screening question for problematic alcohol use is negative (In the past year, he has not had >4 drinks in a day). Next, you calculate his NM ASSIST-based risk scores for cannabis and cocaine, and determine he is at moderate risk for developing problems due to cannabis use and at high risk for developing problems based on his use of cocaine. You also note Mr. M’s blood pressure (BP) is elevated (155/90 mm hg).
Conducting a brief intervention
Depending on the patient’s risk level for developing a substance use disorder, he or she should receive either brief advice (for those at low risk) or a BI (for those at moderate or high risk) and, if needed, a referral to treatment. Two popular approaches are FRAMES (Feedback, Responsibility, Advice, Menu of Strategies, Empathy, Self-efficacy) and the NIDA-recommended 5 As intervention. The latter approach entails Asking the patient about his drug use (via the Quick Screen); Advising the patient about his drug use by providing specific medical advice on why he should stop or cut down, and how; Assessing the patient’s readiness to quit or reduce use; Assisting the patient in making a change by creating a plan with specific goals; and Arranging a follow-up visit or specialty assessment and treatment by making referrals as appropriate.19
What about children and adolescents? Implementing a drug SBI in young patients often entails overcoming unique challenges and ethical dilemmas. Although the American Academy of Pediatrics recommends SBI for unhealthy drug and alcohol use among children and adolescents,33,34 the USPSTF did not find sufficient evidence to recommend the practice.1,8,35 Screening for drug use in minors often is complicated by questions about the age at which to start routine screening and issues related to confidentiality and parental involvement. The Center for Adolescent Health and the Law and the National Institute on Alcohol Abuse and Alcoholism provide useful resources related to youth SBI, including guidance on when to consider breeching a child’s confidentiality by engaging parents or guardians (TABLE 3).
TABLE 3
Resources
NIDA Resource Guide NIDA-Modified ASSIST Coding for SBI reimbursement SAMHSA’s Treatment Services Locator NIDA’s List of Community Treatment Programs SAMHSA Opioid Overdose Toolkit Buprenorphine training program Center for Adolescent Health and the Law NIAAA Alcohol Screening and Brief Intervention for Youth |
Help is available for securing treatment, reimbursement
In addition to NIDA, many other organizations offer resources to assist clinicians in using drug SBI and helping patients obtain treatment (TABLE 3). For reimbursement, the Centers for Medicare and Medicaid Services has adopted billing codes for SBI services.36,37 The Substance Abuse and Mental Health Services Administration (SAMHSA)’s Behavioral Health Treatment Services Locator and NIDA’s National Drug Abuse Treatment Clinical Trials Network List of Associated Community Treatment Programs can assist clinicians and patients in finding specialty treatment programs. Self-help groups such as Narcotics Anonymous, Alcoholic Anonymous, or Self-Managment and Recovery Training may help alleviate problems related to insurance coverage, location, and/or timing of services.
SAMHSA’s Opioid Overdose Toolkit provides guidance to clinicians and patients on ways to reduce the risk of overdose. Physicians also can complete a short training program in office-based buprenorphine maintenance therapy to provide evidence-based care to patients with opioid dependence; more details about this program are available from http://www.buppractice.com.
CASE › You decide to use the 5 as intervention with Mr. M. You explain to him that he is at high risk of developing a substance use disorder. You also discuss his elevated BP and the possible negative effects of drug use, especially cocaine, on BP. You advise him that medically it is in his best interest to stop using cocaine and stop or reduce using cannabis. When you ask Mr. M about his readiness to change his drug use, he expresses moderate interest in stopping cocaine but is not willing to reduce his cannabis use. At this time, he is not willing to discuss these issues further (“I’ll think about that”) or create a specific plan. You assure him of your ongoing support, provide him with resources on specialty treatment programs should he wish to consider those, and schedule a follow-up visit in 2 weeks to address BP and, if the patient agrees, drug use.
CORRESPONDENCE
Aleksandra Zgierska, MD, Phd, Department of Family Medicine, University of Wisconsin School of Medicine and Public Health, 1100 Delaplaine Court, Madison, WI 53715-1896; [email protected]
› Implement screening and brief intervention (SBI) for unhealthy drug use among adults in primary care. C
› Consult the National Institute on Drug Abuse’s Screening for Drug Use in General Medical Settings Resource Guide for step-by-step recommendations for implementing a drug SBI. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Joe M, age 54, comes to your office for his annual physical examination. As part of your routine screening, you ask him, “In the past year, how often have you used alcohol, tobacco, prescription drugs for nonmedical reasons, or illegal drugs?” Mr. M replies that he does not use tobacco and has not used prescription drugs for nonmedical reasons, but drinks alcohol weekly and uses cannabis and cocaine monthly.
If Mr. M were your patient, what would your next steps be?
One promising approach to alleviate substance use problems is screening and brief intervention (SBI), and—when appropriate—referral to an addiction treatment program. With strong evidence of efficacy, alcohol and tobacco SBIs have become recommended “usual” care for adults in primary care settings.1,2 Strategies for applying SBI to unhealthy drug use (“drug” SBI) in primary care have been a natural extension of the evidence that supports alcohol and tobacco SBIs.
Screening for unhealthy drug use consists of a quick risk appraisal, typically via a brief questionnaire.3-5 Patients with a positive screen then receive a more detailed assessment to estimate the extent of their substance use and severity of its consequences. If appropriate, this is followed with a brief intervention (BI), which is a time-limited, patient-centered counseling session designed to reduce substance use and/or related harm.4-6
So how can you make use of a drug SBI in your office setting?
Drug screening: What the evidence says
Currently, evidence on drug SBI is limited. The US Preventive Services Task Force (USPSTF) found insufficient evidence to recommend for or against universal drug SBI.4,7,8 The scarcity of validated screening and assessment tools that are brief enough to be used in primary care, patients’ use of multiple drugs, and confidentiality concerns likely contribute to the relative lack of research in this area.3,6,9
To our knowledge, results of only 5 randomized controlled trials (RCTs) of drug SBI that included universal screening have been published in English. Here is what these researchers found:
Bernstein et al10 investigated the efficacy of SBI for cocaine and heroin use among 23,699 adults in urgent care, women’s health, and homeless clinic settings. They randomized 1175 patients who screened positive on the Drug Abuse Screening Test11 to receive a single BI session or a handout. At 6 months, patients in the BI group were 1.5 times more likely than controls to be abstinent from cocaine (22% vs 17%; P=.045) and heroin (40% vs 31%; P=.050).
Zahradnik et al12 examined the efficacy of SBI in reducing the use of potentially addictive prescription drugs by hospitalized patients. After researchers screened 6000 inpatients, 126 patients who used, abused, or were dependent on prescription medications were randomized to receive 2 BI sessions or an information booklet. At 3 months, 52% of patients in the BI group had a ≥25% reduction in their daily doses of prescription drugs, compared to 30% in the control group (P=.017),12 However, this difference was not maintained at 12 months.13
Humeniuk et al14 evaluated the efficacy of SBI among primary care patients ages 16 to 62 years in Australia, Brazil, India, and the United States who used cannabis, cocaine, amphetamines, or opioids. Patients were screened and assessed using the World Health Organization Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).15 Patients whose scores indicated they had a moderate risk for problem use (N=731) were randomly assigned to receive a BI or usual care. At 3 months, patients in the BI group reported a reduction in total score for “illicit substance involvement” compared to controls (P<.001). However, country-specific analyses found that BI did not have a statistically significant effect on drug use by those in the United States (N=218), possibly due to protocol differences and a greater exposure to previous substance use treatment among US patients.14
Saitz et al16 investigated the efficacy of drug SBI among primary care patients (N=528) who had been screened using the ASSIST. The most commonly used drugs were marijuana (63% of patients), cocaine (19%), and opioids (17%). Patients were randomly assigned to a 10- to 15-minute BI, a 30- to 45-minute intervention, or no intervention. BI did not show efficacy for decreasing drug use at 6-month follow-up.
Roy-Byrne et al17 screened 10,337 primary care patients of “safety net” clinics serving low-income populations. Of 1621 patients who screened positive for problem drug use, 868 were enrolled and randomly assigned to either a BI group (one-time BI using motivational interviewing, a telephone booster session, and a handout, which included relevant drug-use related information and a list of substance abuse resources) or enhanced care as usual (usual care plus a handout). Over 12 months of follow-up, there were no differences between groups in drug use or related consequences. However, a subgroup analysis suggested that compared to enhanced usual care, BI may help reduce emergency department use and increase admissions to specialized drug treatment programs among those with severe drug problems.
In addition to these 5 RCTs, a large, prospective, uncontrolled trial looked at the efficacy of drug BI among 459,599 patients from various medical settings, including primary care.18 Twenty-three percent of patients screened positive for illicit drug use and were recommended BI (16%), brief treatment (3%) or specialty treatment (4%). At a 6-month follow-up, drug use among these patients decreased by 68% and heavy alcohol use decreased by 39% (P<.001). In addition, general health, mental health, employment, housing status, and criminal behavior improved among patients recommended for brief or specialty treatments (P<.001). Although this trial lent support for the efficacy of drug SBI in primary care, it was limited by the lack of a control group and low follow-up rates at some sites.
A step-by-step approach to drug screening
Although a variety of instruments can be used to screen and assess patients for unhealthy drug use, few have been validated in primary care (TABLE 1).11,15,19-27 Despite limited evidence, multiple professional organizations, including the American Academy of Family Physicians28 and the American Psychiatric Association,26 support routine implementation of drug SBI in primary care.
The National Institute on Drug Abuse (NIDA)’s Screening for Drug Use in General Medical Settings Resource Guide19 provides a step-by-step approach to drug SBI in primary care and other general medical settings. Primarily focused on drug SBI in adults, the NIDA guide details the use of the NIDA Quick Screen and the NIDA-Modified ASSIST (NM ASSIST). These tools are available as a PDF that you can print out and complete manually (http://www.drugabuse.gov/sites/default/ files/pdf/nmassist.pdf) or as a series of forms you can complete online (http://www.drugabuse.gov/nmassist). The NIDA guide also conveniently incorporates links to alcohol and tobacco SBI recommendations.
What to ask first. Following the NIDA algorithm, first screen patients with the Quick Screen, which consists of a single question about substance use: “In the past year, how often have you used alcohol, tobacco products, prescription drugs for nonmedical reasons, or illegal drugs?" (TABLE 2).19,29-32
A negative Quick Screen (a “never” response for all substances) completes the process. Patients with a negative screen should be praised and encouraged to continue their healthy lifestyle, then rescreened annually.
For patients who respond “Yes” to heavy drinking or any tobacco use, the NIDA guide recommends proceeding with an alcohol29 or tobacco30 SBI, respectively, and provides links to appropriate resources (TABLE 2).19,29-32 Those who screen positive for drugs (“Yes” to any drug use in the past year) should receive a detailed assessment using the NM ASSIST32 to determine their risk level for developing a substance use disorder. The NM ASSIST includes 8 questions about the patient’s desire for, use of, and problems related to the use of a wide range of drugs, including cannabis, cocaine, methamphetamine, hallucinogens, and other substances (eg, “In the past 3 months, how often have you used the following substances?” “How often have you had a strong desire or urge to use this substance?” “How often has your use of this substance led to health, social, legal or financial problems?”). The score on the NM ASSIST is used to calculate the patient’s risk level as low, moderate, or high.
For patients who use more than one drug, this risk level is scored separately for each drug and may differ from drug to drug. Multi-drug assessment can become time-consuming and may not be appropriate in some patients, especially if time is an issue (eg, the patient would like to focus on other concerns) or the patient is not interested in addressing certain drugs. In general, the decision about which substances to address should be clinically-driven, tailored to the needs of an individual patient. Focusing on the substance with the highest risk score or associated with the patient’s expressed greatest motivation to change may produce the best results.
CASE › Based on Mr. M’s response to your Quick Screen indicating he drinks alcohol and uses illicit drugs, you administer the NM ASSIST to perform a detailed assessment. His answer to a screening question for problematic alcohol use is negative (In the past year, he has not had >4 drinks in a day). Next, you calculate his NM ASSIST-based risk scores for cannabis and cocaine, and determine he is at moderate risk for developing problems due to cannabis use and at high risk for developing problems based on his use of cocaine. You also note Mr. M’s blood pressure (BP) is elevated (155/90 mm hg).
Conducting a brief intervention
Depending on the patient’s risk level for developing a substance use disorder, he or she should receive either brief advice (for those at low risk) or a BI (for those at moderate or high risk) and, if needed, a referral to treatment. Two popular approaches are FRAMES (Feedback, Responsibility, Advice, Menu of Strategies, Empathy, Self-efficacy) and the NIDA-recommended 5 As intervention. The latter approach entails Asking the patient about his drug use (via the Quick Screen); Advising the patient about his drug use by providing specific medical advice on why he should stop or cut down, and how; Assessing the patient’s readiness to quit or reduce use; Assisting the patient in making a change by creating a plan with specific goals; and Arranging a follow-up visit or specialty assessment and treatment by making referrals as appropriate.19
What about children and adolescents? Implementing a drug SBI in young patients often entails overcoming unique challenges and ethical dilemmas. Although the American Academy of Pediatrics recommends SBI for unhealthy drug and alcohol use among children and adolescents,33,34 the USPSTF did not find sufficient evidence to recommend the practice.1,8,35 Screening for drug use in minors often is complicated by questions about the age at which to start routine screening and issues related to confidentiality and parental involvement. The Center for Adolescent Health and the Law and the National Institute on Alcohol Abuse and Alcoholism provide useful resources related to youth SBI, including guidance on when to consider breeching a child’s confidentiality by engaging parents or guardians (TABLE 3).
TABLE 3
Resources
NIDA Resource Guide NIDA-Modified ASSIST Coding for SBI reimbursement SAMHSA’s Treatment Services Locator NIDA’s List of Community Treatment Programs SAMHSA Opioid Overdose Toolkit Buprenorphine training program Center for Adolescent Health and the Law NIAAA Alcohol Screening and Brief Intervention for Youth |
Help is available for securing treatment, reimbursement
In addition to NIDA, many other organizations offer resources to assist clinicians in using drug SBI and helping patients obtain treatment (TABLE 3). For reimbursement, the Centers for Medicare and Medicaid Services has adopted billing codes for SBI services.36,37 The Substance Abuse and Mental Health Services Administration (SAMHSA)’s Behavioral Health Treatment Services Locator and NIDA’s National Drug Abuse Treatment Clinical Trials Network List of Associated Community Treatment Programs can assist clinicians and patients in finding specialty treatment programs. Self-help groups such as Narcotics Anonymous, Alcoholic Anonymous, or Self-Managment and Recovery Training may help alleviate problems related to insurance coverage, location, and/or timing of services.
SAMHSA’s Opioid Overdose Toolkit provides guidance to clinicians and patients on ways to reduce the risk of overdose. Physicians also can complete a short training program in office-based buprenorphine maintenance therapy to provide evidence-based care to patients with opioid dependence; more details about this program are available from http://www.buppractice.com.
CASE › You decide to use the 5 as intervention with Mr. M. You explain to him that he is at high risk of developing a substance use disorder. You also discuss his elevated BP and the possible negative effects of drug use, especially cocaine, on BP. You advise him that medically it is in his best interest to stop using cocaine and stop or reduce using cannabis. When you ask Mr. M about his readiness to change his drug use, he expresses moderate interest in stopping cocaine but is not willing to reduce his cannabis use. At this time, he is not willing to discuss these issues further (“I’ll think about that”) or create a specific plan. You assure him of your ongoing support, provide him with resources on specialty treatment programs should he wish to consider those, and schedule a follow-up visit in 2 weeks to address BP and, if the patient agrees, drug use.
CORRESPONDENCE
Aleksandra Zgierska, MD, Phd, Department of Family Medicine, University of Wisconsin School of Medicine and Public Health, 1100 Delaplaine Court, Madison, WI 53715-1896; [email protected]
1. US Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/ uspsdrin.htm. Accessed March 4, 2013.
2. US Preventive Services Task Force. Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstbac2.htm. Accessed March 4, 2014.
3. Saitz R, Alford DP, Bernstein J, et al. Screening and brief intervention for unhealthy drug use in primary care settings: randomized clinical trials are needed. J Addict Med. 2010;4: 123-130.
4. Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst Abuse Rehabil. 2012;3:25-34.
5. Substance Abuse and Mental Health Services Administration. Screening, Brief Intervention, and Referral to Treatment (SBIRT). Substance Abuse and Mental Health Services Administration Web site. Available at: http://www.samhsa.gov/ prevention/sbirt/. Accessed March 4, 2014.
6. Squires LE, Alford DP, Bernstein J, et al. Clinical case discussion: screening and brief intervention for drug use in primary care. J Addict Med. 2010;4:131-136.
7. Krupski A, Joesch JM, Dunn C, et al. Testing the effects of brief intervention in primary care for problem drug use in a randomized controlled trial: rationale, design, and methods. Addict Sci Clin Pract. 2012;7:27.
8. US Preventive Services Task Force. Screening for illicit drug use. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrug.htm. Accessed March 4, 2014.
9. Lanier D, Ko S. Screening in Primary Care Settings for Illicit Drug Use: Assessment of Screening Instruments—A Supplemental Evidence Update for the U.S. Preventive Services Task Force. AHRQ Publication No. 08-05108-EF-2. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
10. Bernstein J, Bernstein E, Tassiopoulos K, et al. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug Alcohol Depend. 2005;77:49-59.
11. Skinner HA. The drug abuse screening test. Addict Behav. 1982;7:363-371.
12. Zahradnik A, Otto C, Crackau B, et al. Randomized controlled trial of a brief intervention for problematic prescription drug use in non-treatment-seeking patients. Addiction. 2009;104:109-117.
13. Otto C, Crackau B, Löhrmann I, et al. Brief intervention in general hospital for problematic prescription drug use: 12-month outcome. Drug Alcohol Depend. 2009;105:221-226.
14. Humeniuk R, Ali R, Babor T, et al. A randomized controlled trial of a brief intervention for illicit drugs linked to the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in clients recruited from primary health-care settings in four countries. Addiction. 2012;107:957-966.
15. WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97:1183-1194.
16. Saitz R, Palfai TP, Cheng DM, et al. Screening and brief intervention for drug use in primary care: the Assessing Screening Plus brief Intervention’s Resulting Efficacy to stop drug use (ASPIRE) randomized trial. Addict Sci Clin Pract. 2013;8(suppl 1):A61.
17. Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. JAMA. 2014;312(5):492-501.
18. Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99:280-295.
19. National Institute on Drug Abuse. Resource guide: Screening for drug use in general medical settings. National Institute on Drug Abuse Web site. Available at: http://www.drugabuse. gov/publications/resource-guide. Accessed March 8, 2014.
20. Saitz R, Cheng DM, Allensworth-Davies D, et al. The ability of single screening questions for unhealthy alcohol and other drug use to identify substance dependence in primary care. J Stud Alcohol Drugs. 2014;75:153-157.
21. Newcombe DA, Humeniuk RE, Ali R. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev. 2005;24:217-226.
22. Humeniuk R, Ali R, Babor TF, et al. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST). Addiction. 2008;103:1039-1047.
23. Mdege ND, Lang J. Screening instruments for detecting illicit drug use/abuse that could be useful in general hospital wards: a systematic review. Addict Behav. 2011;36:1111-1119.
24. Cassidy CM, Schmitz N, Malla A. Validation of the alcohol use disorders identification test and the drug abuse screening test in first episode psychosis. Can J Psychiatry. 2008;53:26-33.
25. Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 1995;94:135-140.
26. American Psychiatric Association. Position statement on substance use disorders. American Psychiatric Association Web site. Available at: http://www.psychiatry.org/File%20Library/Advocacy%20and%20Newsroom/Position%20Statements/ps2012_Substance.pdf. Accessed March 4, 2014.
27. Smith PC, Schmidt SM, Allensworth-Davies D, et al. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170:1155-1160.
28. American Academy of Family Physicians. Substance abuse and addiction. American Academy of Family Physicians Web site. Available at: http://www.aafp.org/about/policies/all/substance-abuse.html. Accessed March 4, 2014.
29. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide. National Institute on Alcohol Abuse and Alcoholism Web site. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed March 4, 2014.
30. US Department of Health and Human Services Public Health Service. Helping smokers quit: A guide for clinicians. US Department of Health and Human Services Public Health Service Web site. Available at: http://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/tobacco/clinicians//clinhlpsmkqt/. Accessed March 4, 2014.
31. National Institute on Alcohol Abuse and Alcoholism. A Pocket Guide for Alcohol Screening and Brief Intervention. National Institute on Alcohol Abuse and Alcoholism Web site. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/pocketguide/pocket_guide.htm. Accessed July 30, 2014.
32. National Institute on Drug Abuse. NIDA-Quick Screen V1.0. National Institute on Drug Abuse Web site. Available at: http://www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf. Accessed March 4, 2014.
33. Committee on Substance Abuse, Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128:e1330-e1340.
34. Kulig JW; American Academy of Pediatrics Committee on Substance Abuse. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics. 2005;115:816-821.
35. US Preventive Services Task Force. Primary care behavioral interventions to reduce the nonmedical use of drugs in children and adolescents. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsnonmed.htm. Accessed March 4, 2014.
36. Centers for Medicare & Medicaid Services. Screening, Brief Intervention, and Referral to Treatment (SBIRT) services. Centers for Medicare & Medicaid Services Web site. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/sbirt_factsheet_icn904084.pdf. Accessed March 4, 2014.
37. Substance Abuse and Mental Health Services Administration. Coding for screening and brief intervention reimbursement. Substance Abuse and Mental Health Services Administration Web site. Available at: http://beta.samhsa.gov/sbirt/coding-reimbursement. Accessed August 4, 2014.
1. US Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/ uspsdrin.htm. Accessed March 4, 2013.
2. US Preventive Services Task Force. Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstbac2.htm. Accessed March 4, 2014.
3. Saitz R, Alford DP, Bernstein J, et al. Screening and brief intervention for unhealthy drug use in primary care settings: randomized clinical trials are needed. J Addict Med. 2010;4: 123-130.
4. Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst Abuse Rehabil. 2012;3:25-34.
5. Substance Abuse and Mental Health Services Administration. Screening, Brief Intervention, and Referral to Treatment (SBIRT). Substance Abuse and Mental Health Services Administration Web site. Available at: http://www.samhsa.gov/ prevention/sbirt/. Accessed March 4, 2014.
6. Squires LE, Alford DP, Bernstein J, et al. Clinical case discussion: screening and brief intervention for drug use in primary care. J Addict Med. 2010;4:131-136.
7. Krupski A, Joesch JM, Dunn C, et al. Testing the effects of brief intervention in primary care for problem drug use in a randomized controlled trial: rationale, design, and methods. Addict Sci Clin Pract. 2012;7:27.
8. US Preventive Services Task Force. Screening for illicit drug use. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrug.htm. Accessed March 4, 2014.
9. Lanier D, Ko S. Screening in Primary Care Settings for Illicit Drug Use: Assessment of Screening Instruments—A Supplemental Evidence Update for the U.S. Preventive Services Task Force. AHRQ Publication No. 08-05108-EF-2. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
10. Bernstein J, Bernstein E, Tassiopoulos K, et al. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug Alcohol Depend. 2005;77:49-59.
11. Skinner HA. The drug abuse screening test. Addict Behav. 1982;7:363-371.
12. Zahradnik A, Otto C, Crackau B, et al. Randomized controlled trial of a brief intervention for problematic prescription drug use in non-treatment-seeking patients. Addiction. 2009;104:109-117.
13. Otto C, Crackau B, Löhrmann I, et al. Brief intervention in general hospital for problematic prescription drug use: 12-month outcome. Drug Alcohol Depend. 2009;105:221-226.
14. Humeniuk R, Ali R, Babor T, et al. A randomized controlled trial of a brief intervention for illicit drugs linked to the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in clients recruited from primary health-care settings in four countries. Addiction. 2012;107:957-966.
15. WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97:1183-1194.
16. Saitz R, Palfai TP, Cheng DM, et al. Screening and brief intervention for drug use in primary care: the Assessing Screening Plus brief Intervention’s Resulting Efficacy to stop drug use (ASPIRE) randomized trial. Addict Sci Clin Pract. 2013;8(suppl 1):A61.
17. Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. JAMA. 2014;312(5):492-501.
18. Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99:280-295.
19. National Institute on Drug Abuse. Resource guide: Screening for drug use in general medical settings. National Institute on Drug Abuse Web site. Available at: http://www.drugabuse. gov/publications/resource-guide. Accessed March 8, 2014.
20. Saitz R, Cheng DM, Allensworth-Davies D, et al. The ability of single screening questions for unhealthy alcohol and other drug use to identify substance dependence in primary care. J Stud Alcohol Drugs. 2014;75:153-157.
21. Newcombe DA, Humeniuk RE, Ali R. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev. 2005;24:217-226.
22. Humeniuk R, Ali R, Babor TF, et al. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST). Addiction. 2008;103:1039-1047.
23. Mdege ND, Lang J. Screening instruments for detecting illicit drug use/abuse that could be useful in general hospital wards: a systematic review. Addict Behav. 2011;36:1111-1119.
24. Cassidy CM, Schmitz N, Malla A. Validation of the alcohol use disorders identification test and the drug abuse screening test in first episode psychosis. Can J Psychiatry. 2008;53:26-33.
25. Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 1995;94:135-140.
26. American Psychiatric Association. Position statement on substance use disorders. American Psychiatric Association Web site. Available at: http://www.psychiatry.org/File%20Library/Advocacy%20and%20Newsroom/Position%20Statements/ps2012_Substance.pdf. Accessed March 4, 2014.
27. Smith PC, Schmidt SM, Allensworth-Davies D, et al. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170:1155-1160.
28. American Academy of Family Physicians. Substance abuse and addiction. American Academy of Family Physicians Web site. Available at: http://www.aafp.org/about/policies/all/substance-abuse.html. Accessed March 4, 2014.
29. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide. National Institute on Alcohol Abuse and Alcoholism Web site. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed March 4, 2014.
30. US Department of Health and Human Services Public Health Service. Helping smokers quit: A guide for clinicians. US Department of Health and Human Services Public Health Service Web site. Available at: http://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/tobacco/clinicians//clinhlpsmkqt/. Accessed March 4, 2014.
31. National Institute on Alcohol Abuse and Alcoholism. A Pocket Guide for Alcohol Screening and Brief Intervention. National Institute on Alcohol Abuse and Alcoholism Web site. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/pocketguide/pocket_guide.htm. Accessed July 30, 2014.
32. National Institute on Drug Abuse. NIDA-Quick Screen V1.0. National Institute on Drug Abuse Web site. Available at: http://www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf. Accessed March 4, 2014.
33. Committee on Substance Abuse, Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128:e1330-e1340.
34. Kulig JW; American Academy of Pediatrics Committee on Substance Abuse. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics. 2005;115:816-821.
35. US Preventive Services Task Force. Primary care behavioral interventions to reduce the nonmedical use of drugs in children and adolescents. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsnonmed.htm. Accessed March 4, 2014.
36. Centers for Medicare & Medicaid Services. Screening, Brief Intervention, and Referral to Treatment (SBIRT) services. Centers for Medicare & Medicaid Services Web site. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/sbirt_factsheet_icn904084.pdf. Accessed March 4, 2014.
37. Substance Abuse and Mental Health Services Administration. Coding for screening and brief intervention reimbursement. Substance Abuse and Mental Health Services Administration Web site. Available at: http://beta.samhsa.gov/sbirt/coding-reimbursement. Accessed August 4, 2014.
Remission Of Alcohol Disorders In Primary Care Patients
METHODS: A total of 119 eligible and randomly selected primary care patients with alcohol abuse or dependence in remission (as defined in Diagnostic and Statistical Manual of Mental Disorders, third edition, revised) participated in a semistructured telephone interview.
RESULTS: Of the subjects, 59.7% were women; 50.4% had been alcohol dependent; 66.3% made a conscious decision to modify their drinking; and 62.1%, including 54.2% of the alcohol-dependent subjects, moderated their drinking without abstaining. Family, emotional, and medical issues most often prompted reduced drinking. Nearly one third of the subjects found specific strategies and rules helpful in reducing their drinking, and many cited circumstances that helped or hindered their efforts. Only 10.9% had formal alcohol treatment.
CONCLUSIONS: A significant proportion of patients with AUDs remitted without formal treatment. Abstinence may not be necessary for a subset of dependent patients. When counseling patients with active AUDs, primary care clinicians are advised to counsel patients about the psychosocial and medical reasons to control drinking, promote rule-setting about drinking, help patients avoid circumstances that trigger drinking, and support patients’ attempts at moderating drinking rather than abstaining. Motivational interviewing (motivational enhancement therapy) may provide a useful framework for such counseling.
Alcohol use disorders (AUDs) are prevalent in primary care settings.1,2 Research has shown that appropriately trained primary care clinicians can use screening and brief intervention to identify and assist many patients with risky and problematic drinking.3,4 Clinicians are advised to refer all alcohol-dependent patients for formal specialized treatment. The traditional teaching is that alcohol-dependent patients must receive formal treatment and must abstain.
Recent studies have suggested that some alcohol-dependent patients remit spontaneously.5-12 The generalizability of these findings to general populations is unknown, since most of the studies used convenience sampling. Also, the applicability of these findings is unclear with regard to specific AUDs, since many of these studies used screening questionnaires rather than diagnostic assessments to classify subjects.
Our goal was to describe the phenomenology of remission for a randomly selected sample of primary care patients who had been diagnosed with alcohol abuse or had alcohol dependence in remission for at least 1 year. Specifically, we assessed patients’ decisions and reasons for modifying their drinking, their decisions regarding whether to cut down or abstain from drinking, the strategies and circumstances that helped or hindered their efforts, and the roles played by professionals in their process of change. Our results are intended to guide the treatment of AUDs in primary care settings.
Methods
Subjects
A total of 702 English-speaking primary care patients aged 18 to 59 years who were not pregnant were randomly selected from 3 family practice clinics to participate in a previous study.13 For the earlier study, all participants responded to the Composite International Diagnostic Interview-Substance Abuse Module, which assesses current and lifetime alcohol and other drug disorders with excellent reliability and validity.14-17 The response rate was 90.4%.
Subjects were eligible to participate in our study if they met the Diagnostic and Statistical Manual of Mental Disorders, third edition, revised (DSM-III-R) criteria for alcohol abuse or alcohol dependence in remission. In the previous study, 217 (30.9%) of the 702 participants had these DSM-III-R diagnoses. Of those patients, 196 expressed a willingness to participate in further studies, and 179 could be reached. Of those 179, 3 were pregnant, 1 had died, 14 had relapsed, and 6 could not respond to many of the questions because they did not remember reducing their alcohol consumption. Of the 155 remaining eligible individuals, 119 (76.8%) agreed to participate. Demographic information is presented in Table 1.
Eligible subjects were invited to participate with a letter and a follow-up telephone call. Participants received $10 after completing a 30-minute telephone interview. The protocol was approved by the University of Wisconsin Center for Health Sciences human subjects committee.
Data Collection
Four research assistants were trained to administer semistructured telephone interviews. To enhance interrater reliability, the interviewers were trained together and frequently monitored; they also often listened to each other’s interviews. The interview protocol consisted of a sequence of closed-ended and open-ended questions. Initial questions assessed the subjects’ current quantity and frequency of alcohol use and alcohol-related diagnoses. They were asked whether they consciously decided to either quit or cut down on their drinking or if their level of drinking decreased without intention. Subjects were asked open-ended, somewhat redundant questions designed to elicit their reasons for quitting or cutting down. The remainder of the questions focused on how the subjects moderated their alcohol use Table 2.
Analysis
We entered and analyzed data using custom programs written in Microsoft Access (Microsoft, Redmond, Washington), a relational database which enabled us to classify the content of open-ended responses and to determine the frequency of common themes across questions. Microsoft Excel was used to calculate chi-square values according to Siegel’s formula.18
Results
The subjects were well distributed among the third through sixth decades of life Table 1. Women outnumbered men 3 to 2. Most subjects had private insurance, were well educated, and were married or remarried. The demographic attributes of the study subjects and the nonresponders were similar (chi-square tests, P >.05).
The subjects’ AUDs had been active for an average of 11.3 years (standard deviation [SD] =9.0 years, range=1-40 years). The disorders were in remission for an average of 11.1 years (SD=7.8 years, range=0-32 years). Subjects experienced their first alcohol-related symptoms at an average age of 19.3 (SD=5.4, range=10-50 years). The average age for their first attempt at quitting or cutting down was 27.5 years (SD=8.5 years, range=16-53 years). The average age for their most recent attempt at quitting or cutting down was 31.8 years (SD=10 years, range=16-56 years). The majority of subjects (57.9%; N=69) made only one attempt to quit or cut down; 32.7% (39) made 2 to 5 attempts; and 4.2% (11) made 6 or more attempts. One subject reported 20 attempts at quitting or cutting down; another reported 100 attempts. More than two thirds (N=81) of the subjects drank in the past month, and 79.8% (95) drank in the past year. Subjects who continued to drink did so on an average of 3.0 days in the past month (SD=4.4 days, range=0-30 days). Nearly half of the subjects (N=54) drank on 1 to 4 occasions in the last 30 days, and 31.9% (38) did not drink at all. Approximately half of the subjects (N=60) had alcohol dependence in remission, and half (59) had alcohol abuse in remission.
Table 2 shows subjects’ responses to many of the closed-ended questions of the study. Approximately two thirds (N=79) made a conscious decision to quit or cut down; for the remainder, the reduction in drinking occurred without intent.
Table 3 shows the subjects’ specific answers grouped by the major themes that emerged from our analysis of their responses. Within each theme, there were responses reflecting both positive and negative reasons to modify drinking. For example, one subject mentioned that he changed his drinking pattern to be a better role model to children; another stated that she changed because of family disapproval.
Thirty-six subjects initially planned to cut down on their drinking; the others attempted abstinence. A total of 10.9% (13) of the subjects underwent formal alcohol treatment, and an additional 1.7% (2) received help from other professionals. A total of 15.1% (18) attended self-help groups, such as Alcoholics Anonymous.
Thirty-six subjects identified at least one specific strategy that helped them modify their drinking. Thirteen mentioned that it was helpful to avoid bars and people who drink. Others mentioned that it was helpful to change their social activities (N=9), follow the rules of Alcoholics Anonymous (7), keep busy (6), and keep no alcohol at home (5). A total of 12.6% (N=15) tried strategies that did not prove helpful, such as limiting the occasions they went out (5), quitting “cold turkey” (3), avoiding peer pressure (2), and going to Alcoholics Anonymous meetings (2).
Nearly one third (N=39) of the subjects made rules for themselves about their drinking. The most frequently mentioned rules involved limitation. Examples were limits on the amount of alcohol permissible to consume on a particular occasion and limits on the number of days per week or times of the day in which drinking was allowed. Three of those who made rules failed at attempts to quit “cold turkey” by using will power or by “taking control.” Two subjects felt that the 12 steps and other rules of Alcoholics Anonymous were not helpful, and 2 felt that avoiding drinkers was not helpful.
A total of 16.8% (N=20) of the subjects stated that certain circumstances in their lives prompted them to modify their drinking. The most frequently mentioned circumstances were medical conditions and medications that were not compatible with alcohol (N=4). Others mentioned a religious experience (N=3) or the death or injury of a friend or family member (3). Ten of the subjects cited circumstances that hindered their efforts to modify their drinking. Such unfavorable circumstances included obligated exposures to others who drink and peer pressure (N=7), divorce and other family stress (4), and depression (1).
There were several significant (P <.05) differences in responses between the subjects with alcohol abuse in remission and those with dependence in remission. Those with dependence in remission more frequently made conscious decisions to modify their drinking. The previously dependent subjects more frequently reported discrete events that precipitated attempts to modify their drinking, cited emotional concerns as an impetus to modify their drinking, wanted to change their lives, found helpful strategies for modifying their drinking, and experienced circumstances that helped them to quit or cut down. They more frequently had help from nonprofessionals, professionals, formal alcohol treatment programs, and self-help groups, such as Alcoholics Anonymous. Although the dependent subjects were more likely than the abusing subjects to make rules about their drinking (23 of 59, 38.9% vs 16 of 60, 26.6%) and aim for abstinence (27 of 59, 45.7% vs 18 of 60, 30.0%), the differences between the dependent and abusing subjects were not statistically significant. More than half (32 of 59, 54.2%) of the subjects with alcohol dependence in remission did not attempt abstinence.
There were some statistically significant differences between the 16 previously dependent subjects who had received formal treatment and the 43 who had not. Those who had received treatment more frequently attempted abstinence, attempted strategies that were not helpful, found others helpful in modifying their drinking, and attended self-help groups. Those who had received treatment more frequently cited family and emotional issues, but not medical, legal, financial, work, or social issues as contributing to their desire to modify their drinking. There were no statistically significant differences in the frequency with which the subjects in these 2 groups made conscious decisions to modify their drinking, made rules about their drinking, experienced discrete events that precipitated efforts to modify drinking, wanted their lives to go differently, found helpful strategies to modify their drinking, found circumstances that helped or hindered modification of drinking, or returned to previous levels of drinking. Similar comparisons could not be made for the subjects with alcohol abuse in remission, because only 3 of those 60 subjects had received formal treatment.
Discussion
We found a high prevalence (30.9%) of alcohol problems in remission. Other studies have shown that the prevalence of current alcohol dependence, alcohol abuse, and risky but not problematic drinking is also substantial.4,13 Although patients with alcohol issues may not seek or may avoid specialized treatment, they frequently return to primary care settings for a variety of medical issues. Thus, as others have concluded,1,19-22 primary care settings offer clinicians opportunities to intervene for patients with AUDs or risky drinking behaviors.
Strengths and limitations
There are some potential limitations to our study. The 76.8% response rate raises concern about whether the subjects were representative of the entire target population. Although the participants and the nonresponders were similar in demographic attributes and in alcohol-related diagnoses, they might have provided different responses to the more substantive questions of the interview. There is also the possibility that the self-reports were not always accurate. Although the interviewers were trained to project neutrality and general support, a socially desirable response set might have been operative. For some subjects, the long period of time between the onset of their remission and the interview might have reduced the accuracy of their responses. Also, we only sampled individuals who were currently in remission, elucidating factors that may have facilitated remission. We did not explore the impact of such factors on individuals who were not in remission.
The generalizability of the prevalence of AUDs in remission may be limited, because our study was conducted in Wisconsin, a state with particularly high levels of alcohol consumption. The generalizability of other findings may be limited, because the study sample was fairly affluent and well educated and because there were 2 eligibility screenings-one for the original screening study and another for our study.
The strengths of our study include subjects sampled from a general primary care population; other studies used mass media recruiting or convenience sampling.5-12 Also, we used a standard validated instrument to assess alcohol problems, while others used less accurate screening tools.5,6,11,12
Nevertheless, our results agreed with previous studies that many patients with alcohol abuse or dependence can remit without formal alcohol treatment. The potential for spontaneous remission appears to be particularly strong for young adults who experience growth in their families and career demands. However, other research suggests that many middle-aged alcohol-dependent men may experience remission without treatment.23 A substantial number of dependent patients in the sample attained remission despite continued moderate drinking, with remission defined as cessation of the negative consequences of drinking. This result stands in stark contrast to the opinion, espoused by Alcoholics Anonymous and held by many substance abuse treatment professionals, that the vast majority of alcohol-dependent patients can never drink safely again. One possible explanation for this discrepancy may be a difference in case-mix of alcohol-dependent patients in specialized alcohol treatment settings and primary care settings. If predisposition for alcohol dependence is truly polygenic as is suspected,3 one would expect alcohol dependence to occur with varying severity. In primary care settings, alcohol dependence may be less severe and more amenable to self-treatment than in specialized alcohol treatment settings. Thus, in primary care settings, attempts to reduce drinking to safer levels, rather than insistence on abstinence, may be an appropriate initial therapeutic approach for alcohol-dependent patients who do not have serious alcohol-related medical problems. At follow-up, those dependent patients who cannot moderate their drinking or remain free of alcohol-related problems would then be advised to abstain.
Another possibility is that the current definitions of AUDs are flawed and that individuals who can actually control their drinking are misclassified as dependent. Under the current definitions of AUDs, if the same initial therapeutic approach is appropriate for patients with alcohol abuse or dependence, it may not be important for primary care clinicians to ascertain precise alcohol-related diagnoses for problem drinkers. A practical point, however, is that patients should be assessed for potential alcohol withdrawal before they are advised to cut down or stop their drinking.
There were some notable differences between those dependent subjects who did receive treatment for their drinking and those who did not. The higher frequency of attempts at strategies that proved unhelpful by those who received treatment may indicate that some dependent patients seek treatment only after attempts at self-treatment fail. The higher frequency of family and emotional problems among those who received treatment is compatible with the notion that more severely affected individuals receive treatment more often than those with milder disorders. These findings support the notion that dependent patients need not be referred immediately for treatment.
Suggested Strategies
For some of the subjects, medical disorders and medical contraindications to drinking were influential in their remissions. Therefore, clinicians are advised to educate patients about any special medical risks of continued excessive drinking. We also found that family and emotional issues were often more important than biomedical factors in eliciting reduced drinking. Thus, a narrow counseling focus on the biomedical consequences and risks of drinking may miss opportunities with many patients. Primary care clinicians may enhance the effectiveness of their alcohol counseling by reflecting back the more personal psychosocial consequences or risks of drinking.
When helping patients devise strategies to modify their drinking, primary care clinicians should consider helping patients to set rules of limitation and avoidance for themselves, since such rules were helpful for many of the subjects in this study. Clinicians should also assess patients’ barriers to reducing their drinking. Exposure to others who drink and family dysfunction may be key barriers. Simple brainstorming and problem-solving techniques may help patients realize how they can minimize their contact with others who drink. Family dysfunction that interferes with a patient’s attempts to reduce drinking could be addressed with similar brief techniques, and referrals for individual psychotherapy or family therapy might be useful.
These suggestions adhere to an approach for counseling problem drinkers called “motivational interviewing” or “motivational enhancement therapy.” This approach stems partly from Carl Rogers’s theory that behavioral change is fostered by unconditional positive regard, nonpossessive warmth, and genuine concern.24 Applying diagnostic labels, such as “alcohol abuse” and “alcoholism” and issuing directives, such as mandating abstinence, are avoided. Instead, for patients who have not committed themselves to modifying their drinking, clinicians help them recognize and weigh the advantages and disadvantages of drinking in the context of their goals and values. For those who have committed themselves to modifying their drinking, clinicians can help them construct, implement, evaluate, and refine their plans for change. The results of Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity) suggest that motivational interviewing is as effective, and perhaps more efficient, than cognitive-behavioral coping skills therapy and 12-step facilitation therapy.25
Brief interventions that adhere to the principles of motivational interviewing are effective in reducing drinking by alcohol abusers.3,4 Since it is apparent that many alcohol-dependent primary care patients can remit without specialized treatment, a brief intervention may be sufficient to prompt remission in others who do not remit independently. Randomized controlled trials are needed to assess the effectiveness of brief interventions for alcohol-dependent primary care patients.
Conclusions
Our study suggests that AUDs in remission are common in primary care, that many patients with AUDs will remit without formal treatment, that some patients improve spontaneously without intention, and that many dependent patients can remain free of alcohol-related problems with moderate drinking. Many primary care clinicians may be unduly pessimistic about AUDs. Primary care clinicians who understand the factors that promote remission and can apply appropriate counseling techniques may be able to help primary care patients remit from AUDs without formal treatment.
Acknowledgments
Our study was supported by a grant from the National Institute on Drug Abuse (DA-07334) and the Department of Family Medicine, University of Wisconsin Medical School. The authors acknowledge Dr Kym Erbes, Sabrina Holmquist, and Scott Klein for their dedication and perseverance in data collection.
1. D. The role of the generalist in the care of the substance-abusing patient. Med Clin North Am 1997;81:831-43.
2. of Medicine. Broadening the base of treatment for alcohol problems. Washington, DC: National Academy Press; 1990.
3. Institute on Alcohol Abuse and Alcoholism. Eighth special report to the US Congress on alcohol and health 1993. Rockville, Md: NIAAA; 1994. Publication no. 94-3699.
4. M, Barry K, Manwell L, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA 1997;277:1039-80.
5. B. Spontaneous remission in alcoholics: empirical observations and theoretical implications. J Stud Alcohol 1981;42:626-41.
6. A. Cognitive processes associated with “spontaneous” recovery from alcoholism. J Stud Alcohol 1985;46:53-8.
7. H. Coping and maintenance strategies of spontaneous remitters from problem use of alcohol and heroin in Switzerland. Int J Addict 1992;27:1359-88.
8. L, Sobell M, Toneatto T, Leo G. What triggers the resolution of alcohol problems without treatment? Alcohol Clin Exp Res 1993;17:217-24.
9. J, Vuchinich R, Akiko-Gladsjo J. Environmental events surrounding natural recovery from alcohol-related problems. J Stud Alcohol 1994;55:401-11.
10. DL. Resolution of drinking problems without formal treatment: perspectives in Psychiatric Care 1997;33:14-23.
11. JA, Gladsjo JA. Help-seeking and recovery by problem drinkers: characteristics of drinkers who attended Alcoholics Anonymous or formal treatment or who recover without assistance. Addict Behav 1993;18:529-42.
12. JA, Sobell LC, Sobell MB, Kapur G. Resolution from alcohol problems with and without treatment: reasons for change. J Subst Abuse 1995;7:365-72.
13. RL, Leonard T, Rounds LA, Papasouliotis O. A two-item screen for alcohol and other drug problems. J Fam Pract 1997;44:151-60.
14. L, Robins L, Helzer J. The reliability of the CIDI-SAM: a comprehensive substance abuse interview. Br J Addict 1989;84:801-14.
15. A, Robins LN, Bucholz KK, Early TS, Shakya JJ. Comparison of composite international diagnostic interview and clinical DSM-II-R criteria checklist diagnoses. Acta Psyciatr Scand 1992a;85:440-43.
16. A, Robins LN, Cottler LB, Early TS. Clinical observation of assessment using the composite international diagnostic interview (CIDI). Br J Psychiatry 1992b;160:815-18.
17. HU, Robins LB, Cottler LB, et al. Cross-cultural feasibility, reliability and sources of variance of the composite international diagnostic interview (CIDI). Br J Psychiatry 1991;159:645-53.
18. S. Non parametric statistics for the behavioral sciences. New York, NY: McGraw-Hill; 1956;104-10.
19. W. Prevention in practice. Primary Care 1995;22:543-54.
20. for Substance Abuse Prevention. Substance abuse prevention in healthcare: how can you help? In: Macro International Inc; 1997.
21. JL, Zettleer-Segal M, Block M, McClelland M, Schulberg HC. Recognition of alcoholism and substance abuse in primary care patients. Arch Intern Med 1987;147:349-52.
22. H, Stein M. Identifying substance abuse in primary care. Am Fam Physician 1995;52:2029-35.
23. GE. The natural history of alcoholism. Cambridge, Mass: Harvard University Press; 1983.
24. WR, Rollnick S. Motivational Interviewing. New York, NY: Guilford Press; 1991.
25. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol 1997;58:7-29.
METHODS: A total of 119 eligible and randomly selected primary care patients with alcohol abuse or dependence in remission (as defined in Diagnostic and Statistical Manual of Mental Disorders, third edition, revised) participated in a semistructured telephone interview.
RESULTS: Of the subjects, 59.7% were women; 50.4% had been alcohol dependent; 66.3% made a conscious decision to modify their drinking; and 62.1%, including 54.2% of the alcohol-dependent subjects, moderated their drinking without abstaining. Family, emotional, and medical issues most often prompted reduced drinking. Nearly one third of the subjects found specific strategies and rules helpful in reducing their drinking, and many cited circumstances that helped or hindered their efforts. Only 10.9% had formal alcohol treatment.
CONCLUSIONS: A significant proportion of patients with AUDs remitted without formal treatment. Abstinence may not be necessary for a subset of dependent patients. When counseling patients with active AUDs, primary care clinicians are advised to counsel patients about the psychosocial and medical reasons to control drinking, promote rule-setting about drinking, help patients avoid circumstances that trigger drinking, and support patients’ attempts at moderating drinking rather than abstaining. Motivational interviewing (motivational enhancement therapy) may provide a useful framework for such counseling.
Alcohol use disorders (AUDs) are prevalent in primary care settings.1,2 Research has shown that appropriately trained primary care clinicians can use screening and brief intervention to identify and assist many patients with risky and problematic drinking.3,4 Clinicians are advised to refer all alcohol-dependent patients for formal specialized treatment. The traditional teaching is that alcohol-dependent patients must receive formal treatment and must abstain.
Recent studies have suggested that some alcohol-dependent patients remit spontaneously.5-12 The generalizability of these findings to general populations is unknown, since most of the studies used convenience sampling. Also, the applicability of these findings is unclear with regard to specific AUDs, since many of these studies used screening questionnaires rather than diagnostic assessments to classify subjects.
Our goal was to describe the phenomenology of remission for a randomly selected sample of primary care patients who had been diagnosed with alcohol abuse or had alcohol dependence in remission for at least 1 year. Specifically, we assessed patients’ decisions and reasons for modifying their drinking, their decisions regarding whether to cut down or abstain from drinking, the strategies and circumstances that helped or hindered their efforts, and the roles played by professionals in their process of change. Our results are intended to guide the treatment of AUDs in primary care settings.
Methods
Subjects
A total of 702 English-speaking primary care patients aged 18 to 59 years who were not pregnant were randomly selected from 3 family practice clinics to participate in a previous study.13 For the earlier study, all participants responded to the Composite International Diagnostic Interview-Substance Abuse Module, which assesses current and lifetime alcohol and other drug disorders with excellent reliability and validity.14-17 The response rate was 90.4%.
Subjects were eligible to participate in our study if they met the Diagnostic and Statistical Manual of Mental Disorders, third edition, revised (DSM-III-R) criteria for alcohol abuse or alcohol dependence in remission. In the previous study, 217 (30.9%) of the 702 participants had these DSM-III-R diagnoses. Of those patients, 196 expressed a willingness to participate in further studies, and 179 could be reached. Of those 179, 3 were pregnant, 1 had died, 14 had relapsed, and 6 could not respond to many of the questions because they did not remember reducing their alcohol consumption. Of the 155 remaining eligible individuals, 119 (76.8%) agreed to participate. Demographic information is presented in Table 1.
Eligible subjects were invited to participate with a letter and a follow-up telephone call. Participants received $10 after completing a 30-minute telephone interview. The protocol was approved by the University of Wisconsin Center for Health Sciences human subjects committee.
Data Collection
Four research assistants were trained to administer semistructured telephone interviews. To enhance interrater reliability, the interviewers were trained together and frequently monitored; they also often listened to each other’s interviews. The interview protocol consisted of a sequence of closed-ended and open-ended questions. Initial questions assessed the subjects’ current quantity and frequency of alcohol use and alcohol-related diagnoses. They were asked whether they consciously decided to either quit or cut down on their drinking or if their level of drinking decreased without intention. Subjects were asked open-ended, somewhat redundant questions designed to elicit their reasons for quitting or cutting down. The remainder of the questions focused on how the subjects moderated their alcohol use Table 2.
Analysis
We entered and analyzed data using custom programs written in Microsoft Access (Microsoft, Redmond, Washington), a relational database which enabled us to classify the content of open-ended responses and to determine the frequency of common themes across questions. Microsoft Excel was used to calculate chi-square values according to Siegel’s formula.18
Results
The subjects were well distributed among the third through sixth decades of life Table 1. Women outnumbered men 3 to 2. Most subjects had private insurance, were well educated, and were married or remarried. The demographic attributes of the study subjects and the nonresponders were similar (chi-square tests, P >.05).
The subjects’ AUDs had been active for an average of 11.3 years (standard deviation [SD] =9.0 years, range=1-40 years). The disorders were in remission for an average of 11.1 years (SD=7.8 years, range=0-32 years). Subjects experienced their first alcohol-related symptoms at an average age of 19.3 (SD=5.4, range=10-50 years). The average age for their first attempt at quitting or cutting down was 27.5 years (SD=8.5 years, range=16-53 years). The average age for their most recent attempt at quitting or cutting down was 31.8 years (SD=10 years, range=16-56 years). The majority of subjects (57.9%; N=69) made only one attempt to quit or cut down; 32.7% (39) made 2 to 5 attempts; and 4.2% (11) made 6 or more attempts. One subject reported 20 attempts at quitting or cutting down; another reported 100 attempts. More than two thirds (N=81) of the subjects drank in the past month, and 79.8% (95) drank in the past year. Subjects who continued to drink did so on an average of 3.0 days in the past month (SD=4.4 days, range=0-30 days). Nearly half of the subjects (N=54) drank on 1 to 4 occasions in the last 30 days, and 31.9% (38) did not drink at all. Approximately half of the subjects (N=60) had alcohol dependence in remission, and half (59) had alcohol abuse in remission.
Table 2 shows subjects’ responses to many of the closed-ended questions of the study. Approximately two thirds (N=79) made a conscious decision to quit or cut down; for the remainder, the reduction in drinking occurred without intent.
Table 3 shows the subjects’ specific answers grouped by the major themes that emerged from our analysis of their responses. Within each theme, there were responses reflecting both positive and negative reasons to modify drinking. For example, one subject mentioned that he changed his drinking pattern to be a better role model to children; another stated that she changed because of family disapproval.
Thirty-six subjects initially planned to cut down on their drinking; the others attempted abstinence. A total of 10.9% (13) of the subjects underwent formal alcohol treatment, and an additional 1.7% (2) received help from other professionals. A total of 15.1% (18) attended self-help groups, such as Alcoholics Anonymous.
Thirty-six subjects identified at least one specific strategy that helped them modify their drinking. Thirteen mentioned that it was helpful to avoid bars and people who drink. Others mentioned that it was helpful to change their social activities (N=9), follow the rules of Alcoholics Anonymous (7), keep busy (6), and keep no alcohol at home (5). A total of 12.6% (N=15) tried strategies that did not prove helpful, such as limiting the occasions they went out (5), quitting “cold turkey” (3), avoiding peer pressure (2), and going to Alcoholics Anonymous meetings (2).
Nearly one third (N=39) of the subjects made rules for themselves about their drinking. The most frequently mentioned rules involved limitation. Examples were limits on the amount of alcohol permissible to consume on a particular occasion and limits on the number of days per week or times of the day in which drinking was allowed. Three of those who made rules failed at attempts to quit “cold turkey” by using will power or by “taking control.” Two subjects felt that the 12 steps and other rules of Alcoholics Anonymous were not helpful, and 2 felt that avoiding drinkers was not helpful.
A total of 16.8% (N=20) of the subjects stated that certain circumstances in their lives prompted them to modify their drinking. The most frequently mentioned circumstances were medical conditions and medications that were not compatible with alcohol (N=4). Others mentioned a religious experience (N=3) or the death or injury of a friend or family member (3). Ten of the subjects cited circumstances that hindered their efforts to modify their drinking. Such unfavorable circumstances included obligated exposures to others who drink and peer pressure (N=7), divorce and other family stress (4), and depression (1).
There were several significant (P <.05) differences in responses between the subjects with alcohol abuse in remission and those with dependence in remission. Those with dependence in remission more frequently made conscious decisions to modify their drinking. The previously dependent subjects more frequently reported discrete events that precipitated attempts to modify their drinking, cited emotional concerns as an impetus to modify their drinking, wanted to change their lives, found helpful strategies for modifying their drinking, and experienced circumstances that helped them to quit or cut down. They more frequently had help from nonprofessionals, professionals, formal alcohol treatment programs, and self-help groups, such as Alcoholics Anonymous. Although the dependent subjects were more likely than the abusing subjects to make rules about their drinking (23 of 59, 38.9% vs 16 of 60, 26.6%) and aim for abstinence (27 of 59, 45.7% vs 18 of 60, 30.0%), the differences between the dependent and abusing subjects were not statistically significant. More than half (32 of 59, 54.2%) of the subjects with alcohol dependence in remission did not attempt abstinence.
There were some statistically significant differences between the 16 previously dependent subjects who had received formal treatment and the 43 who had not. Those who had received treatment more frequently attempted abstinence, attempted strategies that were not helpful, found others helpful in modifying their drinking, and attended self-help groups. Those who had received treatment more frequently cited family and emotional issues, but not medical, legal, financial, work, or social issues as contributing to their desire to modify their drinking. There were no statistically significant differences in the frequency with which the subjects in these 2 groups made conscious decisions to modify their drinking, made rules about their drinking, experienced discrete events that precipitated efforts to modify drinking, wanted their lives to go differently, found helpful strategies to modify their drinking, found circumstances that helped or hindered modification of drinking, or returned to previous levels of drinking. Similar comparisons could not be made for the subjects with alcohol abuse in remission, because only 3 of those 60 subjects had received formal treatment.
Discussion
We found a high prevalence (30.9%) of alcohol problems in remission. Other studies have shown that the prevalence of current alcohol dependence, alcohol abuse, and risky but not problematic drinking is also substantial.4,13 Although patients with alcohol issues may not seek or may avoid specialized treatment, they frequently return to primary care settings for a variety of medical issues. Thus, as others have concluded,1,19-22 primary care settings offer clinicians opportunities to intervene for patients with AUDs or risky drinking behaviors.
Strengths and limitations
There are some potential limitations to our study. The 76.8% response rate raises concern about whether the subjects were representative of the entire target population. Although the participants and the nonresponders were similar in demographic attributes and in alcohol-related diagnoses, they might have provided different responses to the more substantive questions of the interview. There is also the possibility that the self-reports were not always accurate. Although the interviewers were trained to project neutrality and general support, a socially desirable response set might have been operative. For some subjects, the long period of time between the onset of their remission and the interview might have reduced the accuracy of their responses. Also, we only sampled individuals who were currently in remission, elucidating factors that may have facilitated remission. We did not explore the impact of such factors on individuals who were not in remission.
The generalizability of the prevalence of AUDs in remission may be limited, because our study was conducted in Wisconsin, a state with particularly high levels of alcohol consumption. The generalizability of other findings may be limited, because the study sample was fairly affluent and well educated and because there were 2 eligibility screenings-one for the original screening study and another for our study.
The strengths of our study include subjects sampled from a general primary care population; other studies used mass media recruiting or convenience sampling.5-12 Also, we used a standard validated instrument to assess alcohol problems, while others used less accurate screening tools.5,6,11,12
Nevertheless, our results agreed with previous studies that many patients with alcohol abuse or dependence can remit without formal alcohol treatment. The potential for spontaneous remission appears to be particularly strong for young adults who experience growth in their families and career demands. However, other research suggests that many middle-aged alcohol-dependent men may experience remission without treatment.23 A substantial number of dependent patients in the sample attained remission despite continued moderate drinking, with remission defined as cessation of the negative consequences of drinking. This result stands in stark contrast to the opinion, espoused by Alcoholics Anonymous and held by many substance abuse treatment professionals, that the vast majority of alcohol-dependent patients can never drink safely again. One possible explanation for this discrepancy may be a difference in case-mix of alcohol-dependent patients in specialized alcohol treatment settings and primary care settings. If predisposition for alcohol dependence is truly polygenic as is suspected,3 one would expect alcohol dependence to occur with varying severity. In primary care settings, alcohol dependence may be less severe and more amenable to self-treatment than in specialized alcohol treatment settings. Thus, in primary care settings, attempts to reduce drinking to safer levels, rather than insistence on abstinence, may be an appropriate initial therapeutic approach for alcohol-dependent patients who do not have serious alcohol-related medical problems. At follow-up, those dependent patients who cannot moderate their drinking or remain free of alcohol-related problems would then be advised to abstain.
Another possibility is that the current definitions of AUDs are flawed and that individuals who can actually control their drinking are misclassified as dependent. Under the current definitions of AUDs, if the same initial therapeutic approach is appropriate for patients with alcohol abuse or dependence, it may not be important for primary care clinicians to ascertain precise alcohol-related diagnoses for problem drinkers. A practical point, however, is that patients should be assessed for potential alcohol withdrawal before they are advised to cut down or stop their drinking.
There were some notable differences between those dependent subjects who did receive treatment for their drinking and those who did not. The higher frequency of attempts at strategies that proved unhelpful by those who received treatment may indicate that some dependent patients seek treatment only after attempts at self-treatment fail. The higher frequency of family and emotional problems among those who received treatment is compatible with the notion that more severely affected individuals receive treatment more often than those with milder disorders. These findings support the notion that dependent patients need not be referred immediately for treatment.
Suggested Strategies
For some of the subjects, medical disorders and medical contraindications to drinking were influential in their remissions. Therefore, clinicians are advised to educate patients about any special medical risks of continued excessive drinking. We also found that family and emotional issues were often more important than biomedical factors in eliciting reduced drinking. Thus, a narrow counseling focus on the biomedical consequences and risks of drinking may miss opportunities with many patients. Primary care clinicians may enhance the effectiveness of their alcohol counseling by reflecting back the more personal psychosocial consequences or risks of drinking.
When helping patients devise strategies to modify their drinking, primary care clinicians should consider helping patients to set rules of limitation and avoidance for themselves, since such rules were helpful for many of the subjects in this study. Clinicians should also assess patients’ barriers to reducing their drinking. Exposure to others who drink and family dysfunction may be key barriers. Simple brainstorming and problem-solving techniques may help patients realize how they can minimize their contact with others who drink. Family dysfunction that interferes with a patient’s attempts to reduce drinking could be addressed with similar brief techniques, and referrals for individual psychotherapy or family therapy might be useful.
These suggestions adhere to an approach for counseling problem drinkers called “motivational interviewing” or “motivational enhancement therapy.” This approach stems partly from Carl Rogers’s theory that behavioral change is fostered by unconditional positive regard, nonpossessive warmth, and genuine concern.24 Applying diagnostic labels, such as “alcohol abuse” and “alcoholism” and issuing directives, such as mandating abstinence, are avoided. Instead, for patients who have not committed themselves to modifying their drinking, clinicians help them recognize and weigh the advantages and disadvantages of drinking in the context of their goals and values. For those who have committed themselves to modifying their drinking, clinicians can help them construct, implement, evaluate, and refine their plans for change. The results of Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity) suggest that motivational interviewing is as effective, and perhaps more efficient, than cognitive-behavioral coping skills therapy and 12-step facilitation therapy.25
Brief interventions that adhere to the principles of motivational interviewing are effective in reducing drinking by alcohol abusers.3,4 Since it is apparent that many alcohol-dependent primary care patients can remit without specialized treatment, a brief intervention may be sufficient to prompt remission in others who do not remit independently. Randomized controlled trials are needed to assess the effectiveness of brief interventions for alcohol-dependent primary care patients.
Conclusions
Our study suggests that AUDs in remission are common in primary care, that many patients with AUDs will remit without formal treatment, that some patients improve spontaneously without intention, and that many dependent patients can remain free of alcohol-related problems with moderate drinking. Many primary care clinicians may be unduly pessimistic about AUDs. Primary care clinicians who understand the factors that promote remission and can apply appropriate counseling techniques may be able to help primary care patients remit from AUDs without formal treatment.
Acknowledgments
Our study was supported by a grant from the National Institute on Drug Abuse (DA-07334) and the Department of Family Medicine, University of Wisconsin Medical School. The authors acknowledge Dr Kym Erbes, Sabrina Holmquist, and Scott Klein for their dedication and perseverance in data collection.
METHODS: A total of 119 eligible and randomly selected primary care patients with alcohol abuse or dependence in remission (as defined in Diagnostic and Statistical Manual of Mental Disorders, third edition, revised) participated in a semistructured telephone interview.
RESULTS: Of the subjects, 59.7% were women; 50.4% had been alcohol dependent; 66.3% made a conscious decision to modify their drinking; and 62.1%, including 54.2% of the alcohol-dependent subjects, moderated their drinking without abstaining. Family, emotional, and medical issues most often prompted reduced drinking. Nearly one third of the subjects found specific strategies and rules helpful in reducing their drinking, and many cited circumstances that helped or hindered their efforts. Only 10.9% had formal alcohol treatment.
CONCLUSIONS: A significant proportion of patients with AUDs remitted without formal treatment. Abstinence may not be necessary for a subset of dependent patients. When counseling patients with active AUDs, primary care clinicians are advised to counsel patients about the psychosocial and medical reasons to control drinking, promote rule-setting about drinking, help patients avoid circumstances that trigger drinking, and support patients’ attempts at moderating drinking rather than abstaining. Motivational interviewing (motivational enhancement therapy) may provide a useful framework for such counseling.
Alcohol use disorders (AUDs) are prevalent in primary care settings.1,2 Research has shown that appropriately trained primary care clinicians can use screening and brief intervention to identify and assist many patients with risky and problematic drinking.3,4 Clinicians are advised to refer all alcohol-dependent patients for formal specialized treatment. The traditional teaching is that alcohol-dependent patients must receive formal treatment and must abstain.
Recent studies have suggested that some alcohol-dependent patients remit spontaneously.5-12 The generalizability of these findings to general populations is unknown, since most of the studies used convenience sampling. Also, the applicability of these findings is unclear with regard to specific AUDs, since many of these studies used screening questionnaires rather than diagnostic assessments to classify subjects.
Our goal was to describe the phenomenology of remission for a randomly selected sample of primary care patients who had been diagnosed with alcohol abuse or had alcohol dependence in remission for at least 1 year. Specifically, we assessed patients’ decisions and reasons for modifying their drinking, their decisions regarding whether to cut down or abstain from drinking, the strategies and circumstances that helped or hindered their efforts, and the roles played by professionals in their process of change. Our results are intended to guide the treatment of AUDs in primary care settings.
Methods
Subjects
A total of 702 English-speaking primary care patients aged 18 to 59 years who were not pregnant were randomly selected from 3 family practice clinics to participate in a previous study.13 For the earlier study, all participants responded to the Composite International Diagnostic Interview-Substance Abuse Module, which assesses current and lifetime alcohol and other drug disorders with excellent reliability and validity.14-17 The response rate was 90.4%.
Subjects were eligible to participate in our study if they met the Diagnostic and Statistical Manual of Mental Disorders, third edition, revised (DSM-III-R) criteria for alcohol abuse or alcohol dependence in remission. In the previous study, 217 (30.9%) of the 702 participants had these DSM-III-R diagnoses. Of those patients, 196 expressed a willingness to participate in further studies, and 179 could be reached. Of those 179, 3 were pregnant, 1 had died, 14 had relapsed, and 6 could not respond to many of the questions because they did not remember reducing their alcohol consumption. Of the 155 remaining eligible individuals, 119 (76.8%) agreed to participate. Demographic information is presented in Table 1.
Eligible subjects were invited to participate with a letter and a follow-up telephone call. Participants received $10 after completing a 30-minute telephone interview. The protocol was approved by the University of Wisconsin Center for Health Sciences human subjects committee.
Data Collection
Four research assistants were trained to administer semistructured telephone interviews. To enhance interrater reliability, the interviewers were trained together and frequently monitored; they also often listened to each other’s interviews. The interview protocol consisted of a sequence of closed-ended and open-ended questions. Initial questions assessed the subjects’ current quantity and frequency of alcohol use and alcohol-related diagnoses. They were asked whether they consciously decided to either quit or cut down on their drinking or if their level of drinking decreased without intention. Subjects were asked open-ended, somewhat redundant questions designed to elicit their reasons for quitting or cutting down. The remainder of the questions focused on how the subjects moderated their alcohol use Table 2.
Analysis
We entered and analyzed data using custom programs written in Microsoft Access (Microsoft, Redmond, Washington), a relational database which enabled us to classify the content of open-ended responses and to determine the frequency of common themes across questions. Microsoft Excel was used to calculate chi-square values according to Siegel’s formula.18
Results
The subjects were well distributed among the third through sixth decades of life Table 1. Women outnumbered men 3 to 2. Most subjects had private insurance, were well educated, and were married or remarried. The demographic attributes of the study subjects and the nonresponders were similar (chi-square tests, P >.05).
The subjects’ AUDs had been active for an average of 11.3 years (standard deviation [SD] =9.0 years, range=1-40 years). The disorders were in remission for an average of 11.1 years (SD=7.8 years, range=0-32 years). Subjects experienced their first alcohol-related symptoms at an average age of 19.3 (SD=5.4, range=10-50 years). The average age for their first attempt at quitting or cutting down was 27.5 years (SD=8.5 years, range=16-53 years). The average age for their most recent attempt at quitting or cutting down was 31.8 years (SD=10 years, range=16-56 years). The majority of subjects (57.9%; N=69) made only one attempt to quit or cut down; 32.7% (39) made 2 to 5 attempts; and 4.2% (11) made 6 or more attempts. One subject reported 20 attempts at quitting or cutting down; another reported 100 attempts. More than two thirds (N=81) of the subjects drank in the past month, and 79.8% (95) drank in the past year. Subjects who continued to drink did so on an average of 3.0 days in the past month (SD=4.4 days, range=0-30 days). Nearly half of the subjects (N=54) drank on 1 to 4 occasions in the last 30 days, and 31.9% (38) did not drink at all. Approximately half of the subjects (N=60) had alcohol dependence in remission, and half (59) had alcohol abuse in remission.
Table 2 shows subjects’ responses to many of the closed-ended questions of the study. Approximately two thirds (N=79) made a conscious decision to quit or cut down; for the remainder, the reduction in drinking occurred without intent.
Table 3 shows the subjects’ specific answers grouped by the major themes that emerged from our analysis of their responses. Within each theme, there were responses reflecting both positive and negative reasons to modify drinking. For example, one subject mentioned that he changed his drinking pattern to be a better role model to children; another stated that she changed because of family disapproval.
Thirty-six subjects initially planned to cut down on their drinking; the others attempted abstinence. A total of 10.9% (13) of the subjects underwent formal alcohol treatment, and an additional 1.7% (2) received help from other professionals. A total of 15.1% (18) attended self-help groups, such as Alcoholics Anonymous.
Thirty-six subjects identified at least one specific strategy that helped them modify their drinking. Thirteen mentioned that it was helpful to avoid bars and people who drink. Others mentioned that it was helpful to change their social activities (N=9), follow the rules of Alcoholics Anonymous (7), keep busy (6), and keep no alcohol at home (5). A total of 12.6% (N=15) tried strategies that did not prove helpful, such as limiting the occasions they went out (5), quitting “cold turkey” (3), avoiding peer pressure (2), and going to Alcoholics Anonymous meetings (2).
Nearly one third (N=39) of the subjects made rules for themselves about their drinking. The most frequently mentioned rules involved limitation. Examples were limits on the amount of alcohol permissible to consume on a particular occasion and limits on the number of days per week or times of the day in which drinking was allowed. Three of those who made rules failed at attempts to quit “cold turkey” by using will power or by “taking control.” Two subjects felt that the 12 steps and other rules of Alcoholics Anonymous were not helpful, and 2 felt that avoiding drinkers was not helpful.
A total of 16.8% (N=20) of the subjects stated that certain circumstances in their lives prompted them to modify their drinking. The most frequently mentioned circumstances were medical conditions and medications that were not compatible with alcohol (N=4). Others mentioned a religious experience (N=3) or the death or injury of a friend or family member (3). Ten of the subjects cited circumstances that hindered their efforts to modify their drinking. Such unfavorable circumstances included obligated exposures to others who drink and peer pressure (N=7), divorce and other family stress (4), and depression (1).
There were several significant (P <.05) differences in responses between the subjects with alcohol abuse in remission and those with dependence in remission. Those with dependence in remission more frequently made conscious decisions to modify their drinking. The previously dependent subjects more frequently reported discrete events that precipitated attempts to modify their drinking, cited emotional concerns as an impetus to modify their drinking, wanted to change their lives, found helpful strategies for modifying their drinking, and experienced circumstances that helped them to quit or cut down. They more frequently had help from nonprofessionals, professionals, formal alcohol treatment programs, and self-help groups, such as Alcoholics Anonymous. Although the dependent subjects were more likely than the abusing subjects to make rules about their drinking (23 of 59, 38.9% vs 16 of 60, 26.6%) and aim for abstinence (27 of 59, 45.7% vs 18 of 60, 30.0%), the differences between the dependent and abusing subjects were not statistically significant. More than half (32 of 59, 54.2%) of the subjects with alcohol dependence in remission did not attempt abstinence.
There were some statistically significant differences between the 16 previously dependent subjects who had received formal treatment and the 43 who had not. Those who had received treatment more frequently attempted abstinence, attempted strategies that were not helpful, found others helpful in modifying their drinking, and attended self-help groups. Those who had received treatment more frequently cited family and emotional issues, but not medical, legal, financial, work, or social issues as contributing to their desire to modify their drinking. There were no statistically significant differences in the frequency with which the subjects in these 2 groups made conscious decisions to modify their drinking, made rules about their drinking, experienced discrete events that precipitated efforts to modify drinking, wanted their lives to go differently, found helpful strategies to modify their drinking, found circumstances that helped or hindered modification of drinking, or returned to previous levels of drinking. Similar comparisons could not be made for the subjects with alcohol abuse in remission, because only 3 of those 60 subjects had received formal treatment.
Discussion
We found a high prevalence (30.9%) of alcohol problems in remission. Other studies have shown that the prevalence of current alcohol dependence, alcohol abuse, and risky but not problematic drinking is also substantial.4,13 Although patients with alcohol issues may not seek or may avoid specialized treatment, they frequently return to primary care settings for a variety of medical issues. Thus, as others have concluded,1,19-22 primary care settings offer clinicians opportunities to intervene for patients with AUDs or risky drinking behaviors.
Strengths and limitations
There are some potential limitations to our study. The 76.8% response rate raises concern about whether the subjects were representative of the entire target population. Although the participants and the nonresponders were similar in demographic attributes and in alcohol-related diagnoses, they might have provided different responses to the more substantive questions of the interview. There is also the possibility that the self-reports were not always accurate. Although the interviewers were trained to project neutrality and general support, a socially desirable response set might have been operative. For some subjects, the long period of time between the onset of their remission and the interview might have reduced the accuracy of their responses. Also, we only sampled individuals who were currently in remission, elucidating factors that may have facilitated remission. We did not explore the impact of such factors on individuals who were not in remission.
The generalizability of the prevalence of AUDs in remission may be limited, because our study was conducted in Wisconsin, a state with particularly high levels of alcohol consumption. The generalizability of other findings may be limited, because the study sample was fairly affluent and well educated and because there were 2 eligibility screenings-one for the original screening study and another for our study.
The strengths of our study include subjects sampled from a general primary care population; other studies used mass media recruiting or convenience sampling.5-12 Also, we used a standard validated instrument to assess alcohol problems, while others used less accurate screening tools.5,6,11,12
Nevertheless, our results agreed with previous studies that many patients with alcohol abuse or dependence can remit without formal alcohol treatment. The potential for spontaneous remission appears to be particularly strong for young adults who experience growth in their families and career demands. However, other research suggests that many middle-aged alcohol-dependent men may experience remission without treatment.23 A substantial number of dependent patients in the sample attained remission despite continued moderate drinking, with remission defined as cessation of the negative consequences of drinking. This result stands in stark contrast to the opinion, espoused by Alcoholics Anonymous and held by many substance abuse treatment professionals, that the vast majority of alcohol-dependent patients can never drink safely again. One possible explanation for this discrepancy may be a difference in case-mix of alcohol-dependent patients in specialized alcohol treatment settings and primary care settings. If predisposition for alcohol dependence is truly polygenic as is suspected,3 one would expect alcohol dependence to occur with varying severity. In primary care settings, alcohol dependence may be less severe and more amenable to self-treatment than in specialized alcohol treatment settings. Thus, in primary care settings, attempts to reduce drinking to safer levels, rather than insistence on abstinence, may be an appropriate initial therapeutic approach for alcohol-dependent patients who do not have serious alcohol-related medical problems. At follow-up, those dependent patients who cannot moderate their drinking or remain free of alcohol-related problems would then be advised to abstain.
Another possibility is that the current definitions of AUDs are flawed and that individuals who can actually control their drinking are misclassified as dependent. Under the current definitions of AUDs, if the same initial therapeutic approach is appropriate for patients with alcohol abuse or dependence, it may not be important for primary care clinicians to ascertain precise alcohol-related diagnoses for problem drinkers. A practical point, however, is that patients should be assessed for potential alcohol withdrawal before they are advised to cut down or stop their drinking.
There were some notable differences between those dependent subjects who did receive treatment for their drinking and those who did not. The higher frequency of attempts at strategies that proved unhelpful by those who received treatment may indicate that some dependent patients seek treatment only after attempts at self-treatment fail. The higher frequency of family and emotional problems among those who received treatment is compatible with the notion that more severely affected individuals receive treatment more often than those with milder disorders. These findings support the notion that dependent patients need not be referred immediately for treatment.
Suggested Strategies
For some of the subjects, medical disorders and medical contraindications to drinking were influential in their remissions. Therefore, clinicians are advised to educate patients about any special medical risks of continued excessive drinking. We also found that family and emotional issues were often more important than biomedical factors in eliciting reduced drinking. Thus, a narrow counseling focus on the biomedical consequences and risks of drinking may miss opportunities with many patients. Primary care clinicians may enhance the effectiveness of their alcohol counseling by reflecting back the more personal psychosocial consequences or risks of drinking.
When helping patients devise strategies to modify their drinking, primary care clinicians should consider helping patients to set rules of limitation and avoidance for themselves, since such rules were helpful for many of the subjects in this study. Clinicians should also assess patients’ barriers to reducing their drinking. Exposure to others who drink and family dysfunction may be key barriers. Simple brainstorming and problem-solving techniques may help patients realize how they can minimize their contact with others who drink. Family dysfunction that interferes with a patient’s attempts to reduce drinking could be addressed with similar brief techniques, and referrals for individual psychotherapy or family therapy might be useful.
These suggestions adhere to an approach for counseling problem drinkers called “motivational interviewing” or “motivational enhancement therapy.” This approach stems partly from Carl Rogers’s theory that behavioral change is fostered by unconditional positive regard, nonpossessive warmth, and genuine concern.24 Applying diagnostic labels, such as “alcohol abuse” and “alcoholism” and issuing directives, such as mandating abstinence, are avoided. Instead, for patients who have not committed themselves to modifying their drinking, clinicians help them recognize and weigh the advantages and disadvantages of drinking in the context of their goals and values. For those who have committed themselves to modifying their drinking, clinicians can help them construct, implement, evaluate, and refine their plans for change. The results of Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity) suggest that motivational interviewing is as effective, and perhaps more efficient, than cognitive-behavioral coping skills therapy and 12-step facilitation therapy.25
Brief interventions that adhere to the principles of motivational interviewing are effective in reducing drinking by alcohol abusers.3,4 Since it is apparent that many alcohol-dependent primary care patients can remit without specialized treatment, a brief intervention may be sufficient to prompt remission in others who do not remit independently. Randomized controlled trials are needed to assess the effectiveness of brief interventions for alcohol-dependent primary care patients.
Conclusions
Our study suggests that AUDs in remission are common in primary care, that many patients with AUDs will remit without formal treatment, that some patients improve spontaneously without intention, and that many dependent patients can remain free of alcohol-related problems with moderate drinking. Many primary care clinicians may be unduly pessimistic about AUDs. Primary care clinicians who understand the factors that promote remission and can apply appropriate counseling techniques may be able to help primary care patients remit from AUDs without formal treatment.
Acknowledgments
Our study was supported by a grant from the National Institute on Drug Abuse (DA-07334) and the Department of Family Medicine, University of Wisconsin Medical School. The authors acknowledge Dr Kym Erbes, Sabrina Holmquist, and Scott Klein for their dedication and perseverance in data collection.
1. D. The role of the generalist in the care of the substance-abusing patient. Med Clin North Am 1997;81:831-43.
2. of Medicine. Broadening the base of treatment for alcohol problems. Washington, DC: National Academy Press; 1990.
3. Institute on Alcohol Abuse and Alcoholism. Eighth special report to the US Congress on alcohol and health 1993. Rockville, Md: NIAAA; 1994. Publication no. 94-3699.
4. M, Barry K, Manwell L, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA 1997;277:1039-80.
5. B. Spontaneous remission in alcoholics: empirical observations and theoretical implications. J Stud Alcohol 1981;42:626-41.
6. A. Cognitive processes associated with “spontaneous” recovery from alcoholism. J Stud Alcohol 1985;46:53-8.
7. H. Coping and maintenance strategies of spontaneous remitters from problem use of alcohol and heroin in Switzerland. Int J Addict 1992;27:1359-88.
8. L, Sobell M, Toneatto T, Leo G. What triggers the resolution of alcohol problems without treatment? Alcohol Clin Exp Res 1993;17:217-24.
9. J, Vuchinich R, Akiko-Gladsjo J. Environmental events surrounding natural recovery from alcohol-related problems. J Stud Alcohol 1994;55:401-11.
10. DL. Resolution of drinking problems without formal treatment: perspectives in Psychiatric Care 1997;33:14-23.
11. JA, Gladsjo JA. Help-seeking and recovery by problem drinkers: characteristics of drinkers who attended Alcoholics Anonymous or formal treatment or who recover without assistance. Addict Behav 1993;18:529-42.
12. JA, Sobell LC, Sobell MB, Kapur G. Resolution from alcohol problems with and without treatment: reasons for change. J Subst Abuse 1995;7:365-72.
13. RL, Leonard T, Rounds LA, Papasouliotis O. A two-item screen for alcohol and other drug problems. J Fam Pract 1997;44:151-60.
14. L, Robins L, Helzer J. The reliability of the CIDI-SAM: a comprehensive substance abuse interview. Br J Addict 1989;84:801-14.
15. A, Robins LN, Bucholz KK, Early TS, Shakya JJ. Comparison of composite international diagnostic interview and clinical DSM-II-R criteria checklist diagnoses. Acta Psyciatr Scand 1992a;85:440-43.
16. A, Robins LN, Cottler LB, Early TS. Clinical observation of assessment using the composite international diagnostic interview (CIDI). Br J Psychiatry 1992b;160:815-18.
17. HU, Robins LB, Cottler LB, et al. Cross-cultural feasibility, reliability and sources of variance of the composite international diagnostic interview (CIDI). Br J Psychiatry 1991;159:645-53.
18. S. Non parametric statistics for the behavioral sciences. New York, NY: McGraw-Hill; 1956;104-10.
19. W. Prevention in practice. Primary Care 1995;22:543-54.
20. for Substance Abuse Prevention. Substance abuse prevention in healthcare: how can you help? In: Macro International Inc; 1997.
21. JL, Zettleer-Segal M, Block M, McClelland M, Schulberg HC. Recognition of alcoholism and substance abuse in primary care patients. Arch Intern Med 1987;147:349-52.
22. H, Stein M. Identifying substance abuse in primary care. Am Fam Physician 1995;52:2029-35.
23. GE. The natural history of alcoholism. Cambridge, Mass: Harvard University Press; 1983.
24. WR, Rollnick S. Motivational Interviewing. New York, NY: Guilford Press; 1991.
25. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol 1997;58:7-29.
1. D. The role of the generalist in the care of the substance-abusing patient. Med Clin North Am 1997;81:831-43.
2. of Medicine. Broadening the base of treatment for alcohol problems. Washington, DC: National Academy Press; 1990.
3. Institute on Alcohol Abuse and Alcoholism. Eighth special report to the US Congress on alcohol and health 1993. Rockville, Md: NIAAA; 1994. Publication no. 94-3699.
4. M, Barry K, Manwell L, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA 1997;277:1039-80.
5. B. Spontaneous remission in alcoholics: empirical observations and theoretical implications. J Stud Alcohol 1981;42:626-41.
6. A. Cognitive processes associated with “spontaneous” recovery from alcoholism. J Stud Alcohol 1985;46:53-8.
7. H. Coping and maintenance strategies of spontaneous remitters from problem use of alcohol and heroin in Switzerland. Int J Addict 1992;27:1359-88.
8. L, Sobell M, Toneatto T, Leo G. What triggers the resolution of alcohol problems without treatment? Alcohol Clin Exp Res 1993;17:217-24.
9. J, Vuchinich R, Akiko-Gladsjo J. Environmental events surrounding natural recovery from alcohol-related problems. J Stud Alcohol 1994;55:401-11.
10. DL. Resolution of drinking problems without formal treatment: perspectives in Psychiatric Care 1997;33:14-23.
11. JA, Gladsjo JA. Help-seeking and recovery by problem drinkers: characteristics of drinkers who attended Alcoholics Anonymous or formal treatment or who recover without assistance. Addict Behav 1993;18:529-42.
12. JA, Sobell LC, Sobell MB, Kapur G. Resolution from alcohol problems with and without treatment: reasons for change. J Subst Abuse 1995;7:365-72.
13. RL, Leonard T, Rounds LA, Papasouliotis O. A two-item screen for alcohol and other drug problems. J Fam Pract 1997;44:151-60.
14. L, Robins L, Helzer J. The reliability of the CIDI-SAM: a comprehensive substance abuse interview. Br J Addict 1989;84:801-14.
15. A, Robins LN, Bucholz KK, Early TS, Shakya JJ. Comparison of composite international diagnostic interview and clinical DSM-II-R criteria checklist diagnoses. Acta Psyciatr Scand 1992a;85:440-43.
16. A, Robins LN, Cottler LB, Early TS. Clinical observation of assessment using the composite international diagnostic interview (CIDI). Br J Psychiatry 1992b;160:815-18.
17. HU, Robins LB, Cottler LB, et al. Cross-cultural feasibility, reliability and sources of variance of the composite international diagnostic interview (CIDI). Br J Psychiatry 1991;159:645-53.
18. S. Non parametric statistics for the behavioral sciences. New York, NY: McGraw-Hill; 1956;104-10.
19. W. Prevention in practice. Primary Care 1995;22:543-54.
20. for Substance Abuse Prevention. Substance abuse prevention in healthcare: how can you help? In: Macro International Inc; 1997.
21. JL, Zettleer-Segal M, Block M, McClelland M, Schulberg HC. Recognition of alcoholism and substance abuse in primary care patients. Arch Intern Med 1987;147:349-52.
22. H, Stein M. Identifying substance abuse in primary care. Am Fam Physician 1995;52:2029-35.
23. GE. The natural history of alcoholism. Cambridge, Mass: Harvard University Press; 1983.
24. WR, Rollnick S. Motivational Interviewing. New York, NY: Guilford Press; 1991.
25. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol 1997;58:7-29.