User login
Opportunities and Challenges for Improving the Patient Experience in the Acute and Post–Acute Care Setting Using Patient Portals: The Patient’s Perspective
To realize the vision of patient-centered care, efforts are focusing on engaging patients and “care partners,” often a family caregiver, by using patient-facing technologies.1-4 Web-based patient portals linked to the electronic health record (EHR) provide patients and care partners with the ability to access personal health information online and to communicate with clinicians. In recent years, institutions have been increasing patient portal offerings to improve the patient experience, promote safety, and optimize healthcare delivery.5-7
DRIVERS OF ADOPTION
The adoption of patient portals has been driven by federal incentive programs (Meaningful Use), efforts by the Center for Medicare and Medicaid Services, and the Office of the National Coordinator for Health Information Technology to improve patient outcomes and the transition toward value-based reimbursement.2,8,9 The vast majority of use has been in ambulatory settings; use for acute care is nascent at best.10 Among hospitalized patients, few bring an internet-enabled computer or mobile device to access personal health records online.11 However, evidence suggests that care partners will use portals on behalf of acutely ill patients.4 As the Caregiver Advise, Record, Enable Act is implemented, hospitals will be required to identify patients’ care partners during hospitalization, inform them when the patient is ready for discharge, and provide self-management instructions during the transition home.12 In this context, understanding how best to leverage acute care patient portals will be important to institutions, clinicians, and vendors.
CURRENT KNOWLEDGE
The literature regarding acute care patient portals is rapidly growing.4,10 Hospitalized patients have unmet information and communication needs, and hospital-based clinicians struggle to meet these needs in a timely manner.13-15 In general, patients feel that using a mobile device to access personal health records has the potential to improve their experience.11 Early studies suggest that acute care patient portals can promote patient-centered communication and collaboration during hospitalization, including in intensive care settings.4,16,17 Furthermore, the use of acute care patient portals can improve perception of safety and quality, decrease anxiety, and increase understanding of health conditions.3,14 Although early evidence is promising, considerable knowledge gaps exist regarding patient outcomes over the acute episode of care.10,18
OUTSTANDING QUESTIONS
A clear area of interest is accessing acute care patient portals via mobile technology to engage patients during recovery from hospitalization.4,11 Although we do not yet know whether use during care transitions will favorably impact outcomes, given the high rate of harm after discharge, this seems likely.19 The few studies evaluating the effect on validated measures of engagement (Patient Activation Measure) and hospital readmissions have not shown demonstrable improvement to date.20,21 Clearly, optimizing acute care patient portals with regard to patient-clinician communication, as well as the type, timing, and format of information delivered, will be necessary to maximize value.4,22
From the patient’s perspective, there is much we can learn.23 Is the information that is presented pertinent, timely, and easy to understand? Will the use of portals detract from face-to-face interactions? Does greater transparency foster more accountability? Achieving an appropriate balance of digital health-information sharing for hospitalized patients is challenging given the sensitivity of patient data when diagnoses are uncertain and treatments are in flux.4,24 These questions must be answered as hospitals implement acute care patient portals.
ACUTE CARE PATIENT PORTAL TASK FORCE
To start addressing knowledge gaps, we established a task force of 21 leading researchers, informatics and policy experts, and clinical leaders. The Acute Care Patient Portal Task Force was a subgroup of the Libretto Consortium, a collaboration of 4 academic medical centers established by the Gordon and Betty Moore Foundation to design, develop, and implement technologies to engage patients, care partners, and providers in preventing harm in hospital settings. Initially, we were challenged with assessing stakeholders’ perspectives from early adopter institutions. We learned that acute care patient portals must offer an integrated experience across care settings, humanize the patient-clinician relationship, enable equitable access, and align with institutional strategy to promote sustainability.19
Cognitive Support
The opportunities identified include acclimatizing and assimilating to the hospital environment (reviewing policies and patient rights) and facilitating self-education and preparation by linking to personal health information and providing structured guidance at transitions.4 For example, a care partner of an incapacitated patient may watch a video to orient to the intensive care unit, navigate educational content linked to the patient’s admission diagnosis (pneumonia) entered in the EHR, view the timing of an upcoming imaging study (chest computed tomography scan), and complete a standardized checklist prior to discharge.
The main challenges we identified include ensuring accuracy of hospital-, unit-, and patient-level information, addressing information overload, configuring notification and display settings to optimize the user experience, presenting information at an appropriate health literacy level,4,21 and addressing security and privacy concerns when expanding access to family members.24
Respect and Boundaries
Opportunities identified include supporting individual learning styles by using interactive features of mobile devices to improve comprehension for visual, auditory, and tactile learners and reinforcing learning through the use of various types of digital media.25-27 For example, a visual learner may view a video tutorial for a newly prescribed medication. A tactile learner may prefer to use interactive graphical displays that exploit multidimensional touch capabilities of mobile devices to learn about active conditions or an upcoming procedure. An auditory learner may choose to use intelligent personal assistants to navigate their plan of care (“Hey Siri, what is my schedule for today?”). By addressing the learning preferences of patients and time constraints of clinicians, institutions can use acute care patient portals to promote more respectful interactions and collaborative decision-making during important care processes, such as obtaining surgical consent.28,29
We also identified opportunities to facilitate personalization by tailoring educational content and by enabling the use of patient-generated health data collected from wearable devices. For example, patients may prefer to interact with a virtual advocate to review discharge instructions (“Louis” in Project Re-Engineered Discharge) when personalized to their demographics and health literacy level.30-32 Patients may choose to upload step counts from wearable devices so that clinicians can monitor activity goals in preparation for discharge and while recovering afterwards. When supported in these ways, acute care patient portals allow patients to have more meaningful interactions with clinicians about diagnoses, treatments, prognosis, and goals for recovery.
The main challenges we identified include balancing interactions with technology and clinicians, ensuring clinicians understand how patients from different socioeconomic backgrounds use existing and newer technology to enhance self-management, assessing health and technology literacy, and understanding individual preferences for sharing patient-generated health data. Importantly, we must remain vigilant that patients will express concern about overdependence on technology, especially if it detracts from in-person interaction; our panelists emphasized that technology should never replace “human touch.”
Patient and Family Empowerment
The opportunities identified include promoting patient-centered communication by supporting a real-time and asynchronous dialogue among patients, care partners, and care team members (including ambulatory clinicians) while minimizing conversational silos4,33; displaying names, roles, and pictures of all care team members4,34; fostering transparency by sharing clinician documentation in progress notes and sign-outs35; ensuring accountability for a single plan of care spanning shift changes and handoffs, and providing a mechanism to enable real-time feedback.
Hospitalization can be a vulnerable and isolating experience, perpetuated by a lack of timely and coordinated communication with the care team. We identified opportunities to mitigate anxiety by promoting shared understanding when questions require input from multiple clinicians, when team members change, or when patients wish to communicate with their longitudinal ambulatory providers.4,34 For example, inviting patients to review clinicians’ progress notes should stimulate more open and meaningful communication.35 Furthermore, requesting that patients state their wishes, preferences, and goals could improve overall concordance with care team members.36,37 Empowering patients and care partners to voice their concerns, particularly those related to miscommunication, may mitigate harm propagated by handoffs, shift work, and weekend coverage.38,39 While reporting safety concerns represents a novel mechanism to augment medical-error reporting by clinicians alone,23,40 this strategy will be most effective when aligned with standardized communication initiatives (I-PASS) that have been proven to reduce medical errors and preventable adverse events and are being implemented nationally.41 Finally, by leveraging tools that facilitate instantaneous feedback, patients can be empowered to react to their plan (ranking skilled nursing facility options) as it is developed.
The main challenges we identified include managing expectations regarding the use of communication tools, accurately and reliably identifying care team members in the EHR,34 acknowledging patients as equal partners, ensuring patients receive a consistent message about diagnoses and therapies during handoffs and when multiple consultants have conflicting opinions about the plan,37 and addressing patient concerns fairly and respectfully.
RECOMMENDATIONS AND CONCLUSIONS
In summary, the patient-centered themes we identified serve as guiding principles for institutions, clinicians, and vendors who wish to use patient portals to improve the acute and postacute care patient experience. One central message resonates: Patients do not simply want access to their health information and the ability to communicate with the clinicians who furnish this information; they want to feel supported, respected, and empowered when doing so. It is only through partnership with patients and their advocates that we can fully realize the impact of digital technologies when patients are in their most vulnerable state.
Acknowledgments
The authors thank their colleagues and the patient and family advocates who contributed to this body of work as part of the Acute Care Patient Portal Task Force and conference: Brittany Couture; Ronen Rozenblum, PhD, MPH; Jennifer Prey, MPhil, MS, PhD; Kristin O’Reilly, RN, BSN, MPH; Patricia Q. Bourie, RN, MS, Cindy Dwyer, RN, BSN,S; Ryan Greysen, MD, MHS, MA; Jeffery Smith, MPP; Michael Gropper, MD, PhD; Patricia Dykes, RN, PhD; Martha B. Carnie; Jeffrey W. Mello; and Jane Webster.
Disclosure
Anuj K. Dalal, MD, David W. Bates, MD, MSc, and Sarah Collins, RN, PhD, are responsible for the conception or design of the work; acquisition, analysis, or interpretation of data; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published. The authors agree to be accountable for all aspects of the work and to ensure that questions related to the accuracy or integrity of the work are appropriately investigated and resolved. This work was supported by a grant from the Gordon and Betty Moore Foundation ([GBMF] #4993). GBMF had no role in the design or conduct of the study; the collection, analysis, or interpretation of data; or preparation or review of the manuscript. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of GBMF. The authors report no conflicts of interest.
1. Sarkar U, Bates DW. Care partners and online patient portals. JAMA. 2014;311(4):357-358. PubMed
2. Grando MA, Rozenblum R, Bates DW, eds. Information Technology for Patient Empowerment in Healthcare, 1st Edition. Berlin: Walter de Gruyter Inc.; 2015.
3. Kelly MM, Hoonakker PLT, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Inform Assoc. 2016;24(1):153-161. PubMed
4. Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: A preliminary evaluation. J Am Med Inform Assoc. 2016;23(1):80-87. PubMed
5. Prey JE, Restaino S, Vawdrey DK. Providing hospital patients with access to their medical records. AMIA Annu Symp Proc. 2014;2014:1884-1893. PubMed
6. Herrin J, Harris KG, Kenward K, Hines S, Joshi MS, Frosch DL. Patient and family engagement: A survey of US hospital practices. BMJ Qual Saf. 2016;25(3):182-189. PubMed
7. Tom JO, Mangione-Smith R, Solomon C, Grossman DC. Integrated personal health record use: Association with parent-reported care experiences. Pediatrics. 2012;130(1):e183-e190. PubMed
8. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare and Medicaid Programs; Electronic Health Record Incentive Program-Stage 2. Federal Register Final Rule. Sect. 170; 2012. https://www.federalregister.gov/documents/2012/03/07/2012-4443/medicare-and-medicaid-programs-electronic-health-record-incentive-program-stage-2. Accessed March 1, 2017.
9. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; merit-based incentive payment system (MIPS) and alternative payment model (APM) incentive under the physician fee schedule, and criteria for physician-focused payment models. Final rule with comment period. Fed Regist. 2016;81(214):77008-77831. PubMed
10. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: A systematic review. J Am Med Informat Assoc. 2014;21(4):742-750. PubMed
11. Ludwin S, Greysen SR. Use of smartphones and mobile devices in hospitalized patients: Untapped opportunities for inpatient engagement. J Hosp Med. 2015;10(7):459-461. PubMed
12. Coleman EA. Family caregivers as partners in care transitions: The caregiver advise record and enable act. J Hosp Med. 2016;11(12):883-885. PubMed
13. Kaziunas E, Hanauer DA, Ackerman MS, Choi SW. Identifying unmet informational needs in the inpatient setting to increase patient and caregiver engagement in the context of pediatric hematopoietic stem cell transplantation. J Am Med Inform Assoc. 2016;23(1):94-104. PubMed
14. Woollen J, Prey J, Wilcox L, et al. Patient experiences using an inpatient personal health record. Appl Clin Inform. 2016;7(2):446-460. PubMed
15. Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: A state of the science review. J Med Internet Res. 2015;17(6):e148. doi:10.2196/jmir.4255. PubMed
16. Vawdrey DK, Wilcox LG, Collins SA, et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428-1435. PubMed
17. Collins SA, Rozenblum R, Leung WY, et al. Acute care patient portals: A qualitative study of stakeholder perspectives on current practices. J Am Med Inform Assoc. 2016;24(e1):e9-e17. PubMed
18. Berger Z, Flickinger TE, Pfoh E, Martinez KA, Dy SM. Promoting engagement by patients and families to reduce adverse events in acute care settings: A systematic review. BMJ Qual Saf. 2014;23(7):548-555. PubMed
19. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167. PubMed
20. Griffin A, Skinner A, Thornhill J, Weinberger M. Patient Portals: Who uses them? What features do they use? And do they reduce hospital readmissions? Appl Clin Inform. 2016;7(2):489-501. PubMed
21. O’Leary KJ, Lohman ME, Culver E, Killarney A, Randy Smith G Jr, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Inform Assoc. 2016;23(1):159-165. PubMed
22. O’Leary KJ, Sharma RK, Killarney A, et al. Patients’ and Healthcare Providers’ Perceptions of a Mobile Portal Application for Hospitalized Patients. BMC Med Inform Decis Mak. 2016;16(1):123. PubMed
23. Pell JM, Mancuso M, Limon S, Oman K, Lin CT. Patient access to electronic health records during hospitalization. JAMA Intern Med. 2015;175(5):856-858. PubMed
24. Brown SM, Aboumatar HJ, Francis L, et al. Balancing digital information-sharing and patient privacy when engaging families in the intensive care unit. J Am Med Inform Assoc. 2016;23(5):995-1000. PubMed
25. Krishna S, Francisco BD, Balas EA, et al. Internet-enabled interactive multimedia asthma education program: A randomized trial. Pediatrics. 2003;111(3):503-510. PubMed
26. Fox MP. A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Educ Couns. 2009;77(1):6-13. PubMed
27. Morgan ER, Laing K, McCarthy J, McCrate F, Seal MD. Using tablet-based technology in patient education about systemic therapy options for early-stage breast cancer: A pilot study. Curr Oncol. 2015;22(5):e364-e369. PubMed
28. Nehme J, El-Khani U, Chow A, Hakky S, Ahmed AR, Purkayastha S. The use of multimedia consent programs for surgical procedures: A systematic review. Surg Innov. 2013;20(1):13-23. PubMed
29. Waller A, Forshaw K, Carey M, et al. Optimizing patient preparation and surgical experience using eHealth technology. JMIR Med Inform. 2015;3(3):e29. PubMed
30. Abbott MB, Shaw P. Virtual nursing avatars: Nurse roles and evolving concepts of care. Online J Issues Nurs. 2016;21(3):7. PubMed
31. Cawthon C, Walia S, Osborn CY, Niesner KJ, Schnipper JL, Kripalani S. Improving care transitions: The patient perspective. J Health Commun. 2012;17 Suppl 3:312-324. PubMed
32. Bickmore TW, Pfeifer LM, Byron D, et al. Usability of conversational agents by patients with inadequate health literacy: Evidence from two clinical trials. J Health Commun. 2010;15 Suppl 2:197-210. PubMed
33. 2017;376(20):1905-1907. N Engl J Med.42. Mandl KD, Kohane IS. A 21st-century health IT system—creating a real-world information economy. PubMed
34. 2014;371(19):1803-1812.N Engl J Med41. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. PubMed
35. 2016;24(1):153-161.J Am Med Inform Assoc.40. Kelly MM, Hoonakker PLT, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. PubMed
36. 2017;171(4):372-381.JAMA Pediatr.39. Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. PubMed
37. 2017;17(4):389-402.Acad Pediatr.38. Khan A, Baird J, Rogers JE, et al. Parent and provider experience and shared understanding after a family-centered nighttime communication intervention. PubMed
38. 2016;6(6):319-329.Hosp Pediatr. 37. Khan A, Rogers JE, Forster CS, Furtak SL, Schuster MA, Landrigan CP. Communication and shared understanding between parents and resident-physicians at night. PubMed
39. 2016;11(9):615-619.J Hosp Med36. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient’s primary recovery goal for hospitalization? PubMed
40. 2013;8(7):414-417.J Hosp Med.35. Feldman HJ, Walker J, Li J, Delbanco T. OpenNotes: Hospitalists’ challenge and opportunity. PubMed
41. 2016;11(5):381-385.J Hosp Med.34. Dalal AK, Schnipper JL. Care team identification in the electronic health record: A critical first step for patient-centered communication.PubMed
42. 2016;24(e1):e178-e184.J Am Med Inform Assoc.33. Dalal AK, Schnipper J, Massaro A, et al. A web-based and mobile patient-centered “microblog” messaging platform to improve care team communication in acute care. PubMed
To realize the vision of patient-centered care, efforts are focusing on engaging patients and “care partners,” often a family caregiver, by using patient-facing technologies.1-4 Web-based patient portals linked to the electronic health record (EHR) provide patients and care partners with the ability to access personal health information online and to communicate with clinicians. In recent years, institutions have been increasing patient portal offerings to improve the patient experience, promote safety, and optimize healthcare delivery.5-7
DRIVERS OF ADOPTION
The adoption of patient portals has been driven by federal incentive programs (Meaningful Use), efforts by the Center for Medicare and Medicaid Services, and the Office of the National Coordinator for Health Information Technology to improve patient outcomes and the transition toward value-based reimbursement.2,8,9 The vast majority of use has been in ambulatory settings; use for acute care is nascent at best.10 Among hospitalized patients, few bring an internet-enabled computer or mobile device to access personal health records online.11 However, evidence suggests that care partners will use portals on behalf of acutely ill patients.4 As the Caregiver Advise, Record, Enable Act is implemented, hospitals will be required to identify patients’ care partners during hospitalization, inform them when the patient is ready for discharge, and provide self-management instructions during the transition home.12 In this context, understanding how best to leverage acute care patient portals will be important to institutions, clinicians, and vendors.
CURRENT KNOWLEDGE
The literature regarding acute care patient portals is rapidly growing.4,10 Hospitalized patients have unmet information and communication needs, and hospital-based clinicians struggle to meet these needs in a timely manner.13-15 In general, patients feel that using a mobile device to access personal health records has the potential to improve their experience.11 Early studies suggest that acute care patient portals can promote patient-centered communication and collaboration during hospitalization, including in intensive care settings.4,16,17 Furthermore, the use of acute care patient portals can improve perception of safety and quality, decrease anxiety, and increase understanding of health conditions.3,14 Although early evidence is promising, considerable knowledge gaps exist regarding patient outcomes over the acute episode of care.10,18
OUTSTANDING QUESTIONS
A clear area of interest is accessing acute care patient portals via mobile technology to engage patients during recovery from hospitalization.4,11 Although we do not yet know whether use during care transitions will favorably impact outcomes, given the high rate of harm after discharge, this seems likely.19 The few studies evaluating the effect on validated measures of engagement (Patient Activation Measure) and hospital readmissions have not shown demonstrable improvement to date.20,21 Clearly, optimizing acute care patient portals with regard to patient-clinician communication, as well as the type, timing, and format of information delivered, will be necessary to maximize value.4,22
From the patient’s perspective, there is much we can learn.23 Is the information that is presented pertinent, timely, and easy to understand? Will the use of portals detract from face-to-face interactions? Does greater transparency foster more accountability? Achieving an appropriate balance of digital health-information sharing for hospitalized patients is challenging given the sensitivity of patient data when diagnoses are uncertain and treatments are in flux.4,24 These questions must be answered as hospitals implement acute care patient portals.
ACUTE CARE PATIENT PORTAL TASK FORCE
To start addressing knowledge gaps, we established a task force of 21 leading researchers, informatics and policy experts, and clinical leaders. The Acute Care Patient Portal Task Force was a subgroup of the Libretto Consortium, a collaboration of 4 academic medical centers established by the Gordon and Betty Moore Foundation to design, develop, and implement technologies to engage patients, care partners, and providers in preventing harm in hospital settings. Initially, we were challenged with assessing stakeholders’ perspectives from early adopter institutions. We learned that acute care patient portals must offer an integrated experience across care settings, humanize the patient-clinician relationship, enable equitable access, and align with institutional strategy to promote sustainability.19
Cognitive Support
The opportunities identified include acclimatizing and assimilating to the hospital environment (reviewing policies and patient rights) and facilitating self-education and preparation by linking to personal health information and providing structured guidance at transitions.4 For example, a care partner of an incapacitated patient may watch a video to orient to the intensive care unit, navigate educational content linked to the patient’s admission diagnosis (pneumonia) entered in the EHR, view the timing of an upcoming imaging study (chest computed tomography scan), and complete a standardized checklist prior to discharge.
The main challenges we identified include ensuring accuracy of hospital-, unit-, and patient-level information, addressing information overload, configuring notification and display settings to optimize the user experience, presenting information at an appropriate health literacy level,4,21 and addressing security and privacy concerns when expanding access to family members.24
Respect and Boundaries
Opportunities identified include supporting individual learning styles by using interactive features of mobile devices to improve comprehension for visual, auditory, and tactile learners and reinforcing learning through the use of various types of digital media.25-27 For example, a visual learner may view a video tutorial for a newly prescribed medication. A tactile learner may prefer to use interactive graphical displays that exploit multidimensional touch capabilities of mobile devices to learn about active conditions or an upcoming procedure. An auditory learner may choose to use intelligent personal assistants to navigate their plan of care (“Hey Siri, what is my schedule for today?”). By addressing the learning preferences of patients and time constraints of clinicians, institutions can use acute care patient portals to promote more respectful interactions and collaborative decision-making during important care processes, such as obtaining surgical consent.28,29
We also identified opportunities to facilitate personalization by tailoring educational content and by enabling the use of patient-generated health data collected from wearable devices. For example, patients may prefer to interact with a virtual advocate to review discharge instructions (“Louis” in Project Re-Engineered Discharge) when personalized to their demographics and health literacy level.30-32 Patients may choose to upload step counts from wearable devices so that clinicians can monitor activity goals in preparation for discharge and while recovering afterwards. When supported in these ways, acute care patient portals allow patients to have more meaningful interactions with clinicians about diagnoses, treatments, prognosis, and goals for recovery.
The main challenges we identified include balancing interactions with technology and clinicians, ensuring clinicians understand how patients from different socioeconomic backgrounds use existing and newer technology to enhance self-management, assessing health and technology literacy, and understanding individual preferences for sharing patient-generated health data. Importantly, we must remain vigilant that patients will express concern about overdependence on technology, especially if it detracts from in-person interaction; our panelists emphasized that technology should never replace “human touch.”
Patient and Family Empowerment
The opportunities identified include promoting patient-centered communication by supporting a real-time and asynchronous dialogue among patients, care partners, and care team members (including ambulatory clinicians) while minimizing conversational silos4,33; displaying names, roles, and pictures of all care team members4,34; fostering transparency by sharing clinician documentation in progress notes and sign-outs35; ensuring accountability for a single plan of care spanning shift changes and handoffs, and providing a mechanism to enable real-time feedback.
Hospitalization can be a vulnerable and isolating experience, perpetuated by a lack of timely and coordinated communication with the care team. We identified opportunities to mitigate anxiety by promoting shared understanding when questions require input from multiple clinicians, when team members change, or when patients wish to communicate with their longitudinal ambulatory providers.4,34 For example, inviting patients to review clinicians’ progress notes should stimulate more open and meaningful communication.35 Furthermore, requesting that patients state their wishes, preferences, and goals could improve overall concordance with care team members.36,37 Empowering patients and care partners to voice their concerns, particularly those related to miscommunication, may mitigate harm propagated by handoffs, shift work, and weekend coverage.38,39 While reporting safety concerns represents a novel mechanism to augment medical-error reporting by clinicians alone,23,40 this strategy will be most effective when aligned with standardized communication initiatives (I-PASS) that have been proven to reduce medical errors and preventable adverse events and are being implemented nationally.41 Finally, by leveraging tools that facilitate instantaneous feedback, patients can be empowered to react to their plan (ranking skilled nursing facility options) as it is developed.
The main challenges we identified include managing expectations regarding the use of communication tools, accurately and reliably identifying care team members in the EHR,34 acknowledging patients as equal partners, ensuring patients receive a consistent message about diagnoses and therapies during handoffs and when multiple consultants have conflicting opinions about the plan,37 and addressing patient concerns fairly and respectfully.
RECOMMENDATIONS AND CONCLUSIONS
In summary, the patient-centered themes we identified serve as guiding principles for institutions, clinicians, and vendors who wish to use patient portals to improve the acute and postacute care patient experience. One central message resonates: Patients do not simply want access to their health information and the ability to communicate with the clinicians who furnish this information; they want to feel supported, respected, and empowered when doing so. It is only through partnership with patients and their advocates that we can fully realize the impact of digital technologies when patients are in their most vulnerable state.
Acknowledgments
The authors thank their colleagues and the patient and family advocates who contributed to this body of work as part of the Acute Care Patient Portal Task Force and conference: Brittany Couture; Ronen Rozenblum, PhD, MPH; Jennifer Prey, MPhil, MS, PhD; Kristin O’Reilly, RN, BSN, MPH; Patricia Q. Bourie, RN, MS, Cindy Dwyer, RN, BSN,S; Ryan Greysen, MD, MHS, MA; Jeffery Smith, MPP; Michael Gropper, MD, PhD; Patricia Dykes, RN, PhD; Martha B. Carnie; Jeffrey W. Mello; and Jane Webster.
Disclosure
Anuj K. Dalal, MD, David W. Bates, MD, MSc, and Sarah Collins, RN, PhD, are responsible for the conception or design of the work; acquisition, analysis, or interpretation of data; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published. The authors agree to be accountable for all aspects of the work and to ensure that questions related to the accuracy or integrity of the work are appropriately investigated and resolved. This work was supported by a grant from the Gordon and Betty Moore Foundation ([GBMF] #4993). GBMF had no role in the design or conduct of the study; the collection, analysis, or interpretation of data; or preparation or review of the manuscript. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of GBMF. The authors report no conflicts of interest.
To realize the vision of patient-centered care, efforts are focusing on engaging patients and “care partners,” often a family caregiver, by using patient-facing technologies.1-4 Web-based patient portals linked to the electronic health record (EHR) provide patients and care partners with the ability to access personal health information online and to communicate with clinicians. In recent years, institutions have been increasing patient portal offerings to improve the patient experience, promote safety, and optimize healthcare delivery.5-7
DRIVERS OF ADOPTION
The adoption of patient portals has been driven by federal incentive programs (Meaningful Use), efforts by the Center for Medicare and Medicaid Services, and the Office of the National Coordinator for Health Information Technology to improve patient outcomes and the transition toward value-based reimbursement.2,8,9 The vast majority of use has been in ambulatory settings; use for acute care is nascent at best.10 Among hospitalized patients, few bring an internet-enabled computer or mobile device to access personal health records online.11 However, evidence suggests that care partners will use portals on behalf of acutely ill patients.4 As the Caregiver Advise, Record, Enable Act is implemented, hospitals will be required to identify patients’ care partners during hospitalization, inform them when the patient is ready for discharge, and provide self-management instructions during the transition home.12 In this context, understanding how best to leverage acute care patient portals will be important to institutions, clinicians, and vendors.
CURRENT KNOWLEDGE
The literature regarding acute care patient portals is rapidly growing.4,10 Hospitalized patients have unmet information and communication needs, and hospital-based clinicians struggle to meet these needs in a timely manner.13-15 In general, patients feel that using a mobile device to access personal health records has the potential to improve their experience.11 Early studies suggest that acute care patient portals can promote patient-centered communication and collaboration during hospitalization, including in intensive care settings.4,16,17 Furthermore, the use of acute care patient portals can improve perception of safety and quality, decrease anxiety, and increase understanding of health conditions.3,14 Although early evidence is promising, considerable knowledge gaps exist regarding patient outcomes over the acute episode of care.10,18
OUTSTANDING QUESTIONS
A clear area of interest is accessing acute care patient portals via mobile technology to engage patients during recovery from hospitalization.4,11 Although we do not yet know whether use during care transitions will favorably impact outcomes, given the high rate of harm after discharge, this seems likely.19 The few studies evaluating the effect on validated measures of engagement (Patient Activation Measure) and hospital readmissions have not shown demonstrable improvement to date.20,21 Clearly, optimizing acute care patient portals with regard to patient-clinician communication, as well as the type, timing, and format of information delivered, will be necessary to maximize value.4,22
From the patient’s perspective, there is much we can learn.23 Is the information that is presented pertinent, timely, and easy to understand? Will the use of portals detract from face-to-face interactions? Does greater transparency foster more accountability? Achieving an appropriate balance of digital health-information sharing for hospitalized patients is challenging given the sensitivity of patient data when diagnoses are uncertain and treatments are in flux.4,24 These questions must be answered as hospitals implement acute care patient portals.
ACUTE CARE PATIENT PORTAL TASK FORCE
To start addressing knowledge gaps, we established a task force of 21 leading researchers, informatics and policy experts, and clinical leaders. The Acute Care Patient Portal Task Force was a subgroup of the Libretto Consortium, a collaboration of 4 academic medical centers established by the Gordon and Betty Moore Foundation to design, develop, and implement technologies to engage patients, care partners, and providers in preventing harm in hospital settings. Initially, we were challenged with assessing stakeholders’ perspectives from early adopter institutions. We learned that acute care patient portals must offer an integrated experience across care settings, humanize the patient-clinician relationship, enable equitable access, and align with institutional strategy to promote sustainability.19
Cognitive Support
The opportunities identified include acclimatizing and assimilating to the hospital environment (reviewing policies and patient rights) and facilitating self-education and preparation by linking to personal health information and providing structured guidance at transitions.4 For example, a care partner of an incapacitated patient may watch a video to orient to the intensive care unit, navigate educational content linked to the patient’s admission diagnosis (pneumonia) entered in the EHR, view the timing of an upcoming imaging study (chest computed tomography scan), and complete a standardized checklist prior to discharge.
The main challenges we identified include ensuring accuracy of hospital-, unit-, and patient-level information, addressing information overload, configuring notification and display settings to optimize the user experience, presenting information at an appropriate health literacy level,4,21 and addressing security and privacy concerns when expanding access to family members.24
Respect and Boundaries
Opportunities identified include supporting individual learning styles by using interactive features of mobile devices to improve comprehension for visual, auditory, and tactile learners and reinforcing learning through the use of various types of digital media.25-27 For example, a visual learner may view a video tutorial for a newly prescribed medication. A tactile learner may prefer to use interactive graphical displays that exploit multidimensional touch capabilities of mobile devices to learn about active conditions or an upcoming procedure. An auditory learner may choose to use intelligent personal assistants to navigate their plan of care (“Hey Siri, what is my schedule for today?”). By addressing the learning preferences of patients and time constraints of clinicians, institutions can use acute care patient portals to promote more respectful interactions and collaborative decision-making during important care processes, such as obtaining surgical consent.28,29
We also identified opportunities to facilitate personalization by tailoring educational content and by enabling the use of patient-generated health data collected from wearable devices. For example, patients may prefer to interact with a virtual advocate to review discharge instructions (“Louis” in Project Re-Engineered Discharge) when personalized to their demographics and health literacy level.30-32 Patients may choose to upload step counts from wearable devices so that clinicians can monitor activity goals in preparation for discharge and while recovering afterwards. When supported in these ways, acute care patient portals allow patients to have more meaningful interactions with clinicians about diagnoses, treatments, prognosis, and goals for recovery.
The main challenges we identified include balancing interactions with technology and clinicians, ensuring clinicians understand how patients from different socioeconomic backgrounds use existing and newer technology to enhance self-management, assessing health and technology literacy, and understanding individual preferences for sharing patient-generated health data. Importantly, we must remain vigilant that patients will express concern about overdependence on technology, especially if it detracts from in-person interaction; our panelists emphasized that technology should never replace “human touch.”
Patient and Family Empowerment
The opportunities identified include promoting patient-centered communication by supporting a real-time and asynchronous dialogue among patients, care partners, and care team members (including ambulatory clinicians) while minimizing conversational silos4,33; displaying names, roles, and pictures of all care team members4,34; fostering transparency by sharing clinician documentation in progress notes and sign-outs35; ensuring accountability for a single plan of care spanning shift changes and handoffs, and providing a mechanism to enable real-time feedback.
Hospitalization can be a vulnerable and isolating experience, perpetuated by a lack of timely and coordinated communication with the care team. We identified opportunities to mitigate anxiety by promoting shared understanding when questions require input from multiple clinicians, when team members change, or when patients wish to communicate with their longitudinal ambulatory providers.4,34 For example, inviting patients to review clinicians’ progress notes should stimulate more open and meaningful communication.35 Furthermore, requesting that patients state their wishes, preferences, and goals could improve overall concordance with care team members.36,37 Empowering patients and care partners to voice their concerns, particularly those related to miscommunication, may mitigate harm propagated by handoffs, shift work, and weekend coverage.38,39 While reporting safety concerns represents a novel mechanism to augment medical-error reporting by clinicians alone,23,40 this strategy will be most effective when aligned with standardized communication initiatives (I-PASS) that have been proven to reduce medical errors and preventable adverse events and are being implemented nationally.41 Finally, by leveraging tools that facilitate instantaneous feedback, patients can be empowered to react to their plan (ranking skilled nursing facility options) as it is developed.
The main challenges we identified include managing expectations regarding the use of communication tools, accurately and reliably identifying care team members in the EHR,34 acknowledging patients as equal partners, ensuring patients receive a consistent message about diagnoses and therapies during handoffs and when multiple consultants have conflicting opinions about the plan,37 and addressing patient concerns fairly and respectfully.
RECOMMENDATIONS AND CONCLUSIONS
In summary, the patient-centered themes we identified serve as guiding principles for institutions, clinicians, and vendors who wish to use patient portals to improve the acute and postacute care patient experience. One central message resonates: Patients do not simply want access to their health information and the ability to communicate with the clinicians who furnish this information; they want to feel supported, respected, and empowered when doing so. It is only through partnership with patients and their advocates that we can fully realize the impact of digital technologies when patients are in their most vulnerable state.
Acknowledgments
The authors thank their colleagues and the patient and family advocates who contributed to this body of work as part of the Acute Care Patient Portal Task Force and conference: Brittany Couture; Ronen Rozenblum, PhD, MPH; Jennifer Prey, MPhil, MS, PhD; Kristin O’Reilly, RN, BSN, MPH; Patricia Q. Bourie, RN, MS, Cindy Dwyer, RN, BSN,S; Ryan Greysen, MD, MHS, MA; Jeffery Smith, MPP; Michael Gropper, MD, PhD; Patricia Dykes, RN, PhD; Martha B. Carnie; Jeffrey W. Mello; and Jane Webster.
Disclosure
Anuj K. Dalal, MD, David W. Bates, MD, MSc, and Sarah Collins, RN, PhD, are responsible for the conception or design of the work; acquisition, analysis, or interpretation of data; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published. The authors agree to be accountable for all aspects of the work and to ensure that questions related to the accuracy or integrity of the work are appropriately investigated and resolved. This work was supported by a grant from the Gordon and Betty Moore Foundation ([GBMF] #4993). GBMF had no role in the design or conduct of the study; the collection, analysis, or interpretation of data; or preparation or review of the manuscript. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of GBMF. The authors report no conflicts of interest.
1. Sarkar U, Bates DW. Care partners and online patient portals. JAMA. 2014;311(4):357-358. PubMed
2. Grando MA, Rozenblum R, Bates DW, eds. Information Technology for Patient Empowerment in Healthcare, 1st Edition. Berlin: Walter de Gruyter Inc.; 2015.
3. Kelly MM, Hoonakker PLT, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Inform Assoc. 2016;24(1):153-161. PubMed
4. Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: A preliminary evaluation. J Am Med Inform Assoc. 2016;23(1):80-87. PubMed
5. Prey JE, Restaino S, Vawdrey DK. Providing hospital patients with access to their medical records. AMIA Annu Symp Proc. 2014;2014:1884-1893. PubMed
6. Herrin J, Harris KG, Kenward K, Hines S, Joshi MS, Frosch DL. Patient and family engagement: A survey of US hospital practices. BMJ Qual Saf. 2016;25(3):182-189. PubMed
7. Tom JO, Mangione-Smith R, Solomon C, Grossman DC. Integrated personal health record use: Association with parent-reported care experiences. Pediatrics. 2012;130(1):e183-e190. PubMed
8. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare and Medicaid Programs; Electronic Health Record Incentive Program-Stage 2. Federal Register Final Rule. Sect. 170; 2012. https://www.federalregister.gov/documents/2012/03/07/2012-4443/medicare-and-medicaid-programs-electronic-health-record-incentive-program-stage-2. Accessed March 1, 2017.
9. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; merit-based incentive payment system (MIPS) and alternative payment model (APM) incentive under the physician fee schedule, and criteria for physician-focused payment models. Final rule with comment period. Fed Regist. 2016;81(214):77008-77831. PubMed
10. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: A systematic review. J Am Med Informat Assoc. 2014;21(4):742-750. PubMed
11. Ludwin S, Greysen SR. Use of smartphones and mobile devices in hospitalized patients: Untapped opportunities for inpatient engagement. J Hosp Med. 2015;10(7):459-461. PubMed
12. Coleman EA. Family caregivers as partners in care transitions: The caregiver advise record and enable act. J Hosp Med. 2016;11(12):883-885. PubMed
13. Kaziunas E, Hanauer DA, Ackerman MS, Choi SW. Identifying unmet informational needs in the inpatient setting to increase patient and caregiver engagement in the context of pediatric hematopoietic stem cell transplantation. J Am Med Inform Assoc. 2016;23(1):94-104. PubMed
14. Woollen J, Prey J, Wilcox L, et al. Patient experiences using an inpatient personal health record. Appl Clin Inform. 2016;7(2):446-460. PubMed
15. Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: A state of the science review. J Med Internet Res. 2015;17(6):e148. doi:10.2196/jmir.4255. PubMed
16. Vawdrey DK, Wilcox LG, Collins SA, et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428-1435. PubMed
17. Collins SA, Rozenblum R, Leung WY, et al. Acute care patient portals: A qualitative study of stakeholder perspectives on current practices. J Am Med Inform Assoc. 2016;24(e1):e9-e17. PubMed
18. Berger Z, Flickinger TE, Pfoh E, Martinez KA, Dy SM. Promoting engagement by patients and families to reduce adverse events in acute care settings: A systematic review. BMJ Qual Saf. 2014;23(7):548-555. PubMed
19. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167. PubMed
20. Griffin A, Skinner A, Thornhill J, Weinberger M. Patient Portals: Who uses them? What features do they use? And do they reduce hospital readmissions? Appl Clin Inform. 2016;7(2):489-501. PubMed
21. O’Leary KJ, Lohman ME, Culver E, Killarney A, Randy Smith G Jr, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Inform Assoc. 2016;23(1):159-165. PubMed
22. O’Leary KJ, Sharma RK, Killarney A, et al. Patients’ and Healthcare Providers’ Perceptions of a Mobile Portal Application for Hospitalized Patients. BMC Med Inform Decis Mak. 2016;16(1):123. PubMed
23. Pell JM, Mancuso M, Limon S, Oman K, Lin CT. Patient access to electronic health records during hospitalization. JAMA Intern Med. 2015;175(5):856-858. PubMed
24. Brown SM, Aboumatar HJ, Francis L, et al. Balancing digital information-sharing and patient privacy when engaging families in the intensive care unit. J Am Med Inform Assoc. 2016;23(5):995-1000. PubMed
25. Krishna S, Francisco BD, Balas EA, et al. Internet-enabled interactive multimedia asthma education program: A randomized trial. Pediatrics. 2003;111(3):503-510. PubMed
26. Fox MP. A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Educ Couns. 2009;77(1):6-13. PubMed
27. Morgan ER, Laing K, McCarthy J, McCrate F, Seal MD. Using tablet-based technology in patient education about systemic therapy options for early-stage breast cancer: A pilot study. Curr Oncol. 2015;22(5):e364-e369. PubMed
28. Nehme J, El-Khani U, Chow A, Hakky S, Ahmed AR, Purkayastha S. The use of multimedia consent programs for surgical procedures: A systematic review. Surg Innov. 2013;20(1):13-23. PubMed
29. Waller A, Forshaw K, Carey M, et al. Optimizing patient preparation and surgical experience using eHealth technology. JMIR Med Inform. 2015;3(3):e29. PubMed
30. Abbott MB, Shaw P. Virtual nursing avatars: Nurse roles and evolving concepts of care. Online J Issues Nurs. 2016;21(3):7. PubMed
31. Cawthon C, Walia S, Osborn CY, Niesner KJ, Schnipper JL, Kripalani S. Improving care transitions: The patient perspective. J Health Commun. 2012;17 Suppl 3:312-324. PubMed
32. Bickmore TW, Pfeifer LM, Byron D, et al. Usability of conversational agents by patients with inadequate health literacy: Evidence from two clinical trials. J Health Commun. 2010;15 Suppl 2:197-210. PubMed
33. 2017;376(20):1905-1907. N Engl J Med.42. Mandl KD, Kohane IS. A 21st-century health IT system—creating a real-world information economy. PubMed
34. 2014;371(19):1803-1812.N Engl J Med41. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. PubMed
35. 2016;24(1):153-161.J Am Med Inform Assoc.40. Kelly MM, Hoonakker PLT, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. PubMed
36. 2017;171(4):372-381.JAMA Pediatr.39. Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. PubMed
37. 2017;17(4):389-402.Acad Pediatr.38. Khan A, Baird J, Rogers JE, et al. Parent and provider experience and shared understanding after a family-centered nighttime communication intervention. PubMed
38. 2016;6(6):319-329.Hosp Pediatr. 37. Khan A, Rogers JE, Forster CS, Furtak SL, Schuster MA, Landrigan CP. Communication and shared understanding between parents and resident-physicians at night. PubMed
39. 2016;11(9):615-619.J Hosp Med36. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient’s primary recovery goal for hospitalization? PubMed
40. 2013;8(7):414-417.J Hosp Med.35. Feldman HJ, Walker J, Li J, Delbanco T. OpenNotes: Hospitalists’ challenge and opportunity. PubMed
41. 2016;11(5):381-385.J Hosp Med.34. Dalal AK, Schnipper JL. Care team identification in the electronic health record: A critical first step for patient-centered communication.PubMed
42. 2016;24(e1):e178-e184.J Am Med Inform Assoc.33. Dalal AK, Schnipper J, Massaro A, et al. A web-based and mobile patient-centered “microblog” messaging platform to improve care team communication in acute care. PubMed
1. Sarkar U, Bates DW. Care partners and online patient portals. JAMA. 2014;311(4):357-358. PubMed
2. Grando MA, Rozenblum R, Bates DW, eds. Information Technology for Patient Empowerment in Healthcare, 1st Edition. Berlin: Walter de Gruyter Inc.; 2015.
3. Kelly MM, Hoonakker PLT, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Inform Assoc. 2016;24(1):153-161. PubMed
4. Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: A preliminary evaluation. J Am Med Inform Assoc. 2016;23(1):80-87. PubMed
5. Prey JE, Restaino S, Vawdrey DK. Providing hospital patients with access to their medical records. AMIA Annu Symp Proc. 2014;2014:1884-1893. PubMed
6. Herrin J, Harris KG, Kenward K, Hines S, Joshi MS, Frosch DL. Patient and family engagement: A survey of US hospital practices. BMJ Qual Saf. 2016;25(3):182-189. PubMed
7. Tom JO, Mangione-Smith R, Solomon C, Grossman DC. Integrated personal health record use: Association with parent-reported care experiences. Pediatrics. 2012;130(1):e183-e190. PubMed
8. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare and Medicaid Programs; Electronic Health Record Incentive Program-Stage 2. Federal Register Final Rule. Sect. 170; 2012. https://www.federalregister.gov/documents/2012/03/07/2012-4443/medicare-and-medicaid-programs-electronic-health-record-incentive-program-stage-2. Accessed March 1, 2017.
9. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; merit-based incentive payment system (MIPS) and alternative payment model (APM) incentive under the physician fee schedule, and criteria for physician-focused payment models. Final rule with comment period. Fed Regist. 2016;81(214):77008-77831. PubMed
10. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: A systematic review. J Am Med Informat Assoc. 2014;21(4):742-750. PubMed
11. Ludwin S, Greysen SR. Use of smartphones and mobile devices in hospitalized patients: Untapped opportunities for inpatient engagement. J Hosp Med. 2015;10(7):459-461. PubMed
12. Coleman EA. Family caregivers as partners in care transitions: The caregiver advise record and enable act. J Hosp Med. 2016;11(12):883-885. PubMed
13. Kaziunas E, Hanauer DA, Ackerman MS, Choi SW. Identifying unmet informational needs in the inpatient setting to increase patient and caregiver engagement in the context of pediatric hematopoietic stem cell transplantation. J Am Med Inform Assoc. 2016;23(1):94-104. PubMed
14. Woollen J, Prey J, Wilcox L, et al. Patient experiences using an inpatient personal health record. Appl Clin Inform. 2016;7(2):446-460. PubMed
15. Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: A state of the science review. J Med Internet Res. 2015;17(6):e148. doi:10.2196/jmir.4255. PubMed
16. Vawdrey DK, Wilcox LG, Collins SA, et al. A tablet computer application for patients to participate in their hospital care. AMIA Annu Symp Proc. 2011;2011:1428-1435. PubMed
17. Collins SA, Rozenblum R, Leung WY, et al. Acute care patient portals: A qualitative study of stakeholder perspectives on current practices. J Am Med Inform Assoc. 2016;24(e1):e9-e17. PubMed
18. Berger Z, Flickinger TE, Pfoh E, Martinez KA, Dy SM. Promoting engagement by patients and families to reduce adverse events in acute care settings: A systematic review. BMJ Qual Saf. 2014;23(7):548-555. PubMed
19. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167. PubMed
20. Griffin A, Skinner A, Thornhill J, Weinberger M. Patient Portals: Who uses them? What features do they use? And do they reduce hospital readmissions? Appl Clin Inform. 2016;7(2):489-501. PubMed
21. O’Leary KJ, Lohman ME, Culver E, Killarney A, Randy Smith G Jr, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Inform Assoc. 2016;23(1):159-165. PubMed
22. O’Leary KJ, Sharma RK, Killarney A, et al. Patients’ and Healthcare Providers’ Perceptions of a Mobile Portal Application for Hospitalized Patients. BMC Med Inform Decis Mak. 2016;16(1):123. PubMed
23. Pell JM, Mancuso M, Limon S, Oman K, Lin CT. Patient access to electronic health records during hospitalization. JAMA Intern Med. 2015;175(5):856-858. PubMed
24. Brown SM, Aboumatar HJ, Francis L, et al. Balancing digital information-sharing and patient privacy when engaging families in the intensive care unit. J Am Med Inform Assoc. 2016;23(5):995-1000. PubMed
25. Krishna S, Francisco BD, Balas EA, et al. Internet-enabled interactive multimedia asthma education program: A randomized trial. Pediatrics. 2003;111(3):503-510. PubMed
26. Fox MP. A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Educ Couns. 2009;77(1):6-13. PubMed
27. Morgan ER, Laing K, McCarthy J, McCrate F, Seal MD. Using tablet-based technology in patient education about systemic therapy options for early-stage breast cancer: A pilot study. Curr Oncol. 2015;22(5):e364-e369. PubMed
28. Nehme J, El-Khani U, Chow A, Hakky S, Ahmed AR, Purkayastha S. The use of multimedia consent programs for surgical procedures: A systematic review. Surg Innov. 2013;20(1):13-23. PubMed
29. Waller A, Forshaw K, Carey M, et al. Optimizing patient preparation and surgical experience using eHealth technology. JMIR Med Inform. 2015;3(3):e29. PubMed
30. Abbott MB, Shaw P. Virtual nursing avatars: Nurse roles and evolving concepts of care. Online J Issues Nurs. 2016;21(3):7. PubMed
31. Cawthon C, Walia S, Osborn CY, Niesner KJ, Schnipper JL, Kripalani S. Improving care transitions: The patient perspective. J Health Commun. 2012;17 Suppl 3:312-324. PubMed
32. Bickmore TW, Pfeifer LM, Byron D, et al. Usability of conversational agents by patients with inadequate health literacy: Evidence from two clinical trials. J Health Commun. 2010;15 Suppl 2:197-210. PubMed
33. 2017;376(20):1905-1907. N Engl J Med.42. Mandl KD, Kohane IS. A 21st-century health IT system—creating a real-world information economy. PubMed
34. 2014;371(19):1803-1812.N Engl J Med41. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. PubMed
35. 2016;24(1):153-161.J Am Med Inform Assoc.40. Kelly MM, Hoonakker PLT, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. PubMed
36. 2017;171(4):372-381.JAMA Pediatr.39. Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. PubMed
37. 2017;17(4):389-402.Acad Pediatr.38. Khan A, Baird J, Rogers JE, et al. Parent and provider experience and shared understanding after a family-centered nighttime communication intervention. PubMed
38. 2016;6(6):319-329.Hosp Pediatr. 37. Khan A, Rogers JE, Forster CS, Furtak SL, Schuster MA, Landrigan CP. Communication and shared understanding between parents and resident-physicians at night. PubMed
39. 2016;11(9):615-619.J Hosp Med36. Figueroa JF, Schnipper JL, McNally K, Stade D, Lipsitz SR, Dalal AK. How often are hospitalized patients and providers on the same page with regard to the patient’s primary recovery goal for hospitalization? PubMed
40. 2013;8(7):414-417.J Hosp Med.35. Feldman HJ, Walker J, Li J, Delbanco T. OpenNotes: Hospitalists’ challenge and opportunity. PubMed
41. 2016;11(5):381-385.J Hosp Med.34. Dalal AK, Schnipper JL. Care team identification in the electronic health record: A critical first step for patient-centered communication.PubMed
42. 2016;24(e1):e178-e184.J Am Med Inform Assoc.33. Dalal AK, Schnipper J, Massaro A, et al. A web-based and mobile patient-centered “microblog” messaging platform to improve care team communication in acute care. PubMed
© 2017 Society of Hospital Medicine
Electronic Communication
INTRODUCTION
Coordination of care within a practice, during transitions of care, and between primary and specialty care teams requires more than data exchange; it requires effective communication among healthcare providers.[1, 2, 3] In clinical terms, data exchange, communication, and care coordination are related, but they represent distinct concepts.[4] Data exchange refers to transfer of information between settings, independent of the individuals involved, whereas communication is the multistep process that enables information exchange between two people.[5] Care coordination, as defined by O'Malley, is integration of care in consultation with patients, their families and caregivers across all of a patient's conditions, needs, clinicians and settings.[3]
Strong collaboration among providers has been associated with improved patient outcomes.[2, 6] Yet, despite the significant role of communication in healthcare, communication may not take place at all, even at high‐stakes events like transitions of care,[7, 8] or it may be done poorly at the risk of substantial clinical morbidity and mortality.[9, 10, 11, 12, 13, 14, 15, 16]
Proof of the global effectiveness of health information technology (HIT) to improve patient care is lacking, but data from some studies demonstrate real improvements in quality and safety in specific areas,[17, 18, 19] especially with computerized physician order entry[20] and electronic prescribing.[21]
The limited information about the effect of HIT on communication focuses largely on the anticipated improvements in patient‐physician communication[22, 23, 24, 25, 26, 27]; provider‐to‐provider communication within the electronic domain is not as well understood. A recent review of interventions involving communication devices such as pagers and mobile phones found limited high‐quality evidence in the literature.[28] Clinicians have described what they consider to be key characteristics of clinical electronic communications systems such as security/reliability, cross coverage, overall convenience, and message prioritization.[29] Although the electronic health record (EHR) is expected to assist with this communication,[30] it also has the potential to impede effective communication, leading physicians to resort to more traditional workarounds.[31, 32, 33]
Measuring and improving the use of EHRs nationally were driving forces behind the creation of the Meaningful Use incentive program in the United States.[34] To receive the incentive payments, providers must meet and report on a series of measures set in three stages over the course of five years.[35] In the current state, Meaningful Use does not reward provider‐to‐provider communication within the EHR.[36, 37] The main communication objectives for stages 1 and 2 concentrate on patient‐to‐provider communication, such as patient portals and patient‐to‐provider messaging.[36, 37]
Understanding the current evidence for provider‐to‐provider communication within EHRs, its reported effectiveness, and its shortcomings may help to develop a roadmap for identifying next‐generation solutions to support coordination of care.[38, 39] This review assesses the literature regarding provider‐to‐provider electronic communication tools (as supported within or external to an EHR). It is intended as a comprehensive view of studies reporting quantitative measures of the impact of electronic communication on providers and patients.
METHODS
Definitions and Conceptual Model of Provider‐to‐Provider Communication
We conducted a systematic review of studies of provider‐to‐provider electronic communication. This review included only formal clinical communication between providers and was informed by the Coiera communications paradigm.[5] This paradigm consists of four steps: (1) task identification, when a task is identified and associated with the appropriate individual; (2) connection, when an attempt is made to contact that person; (3) communication, when task‐specific information is exchanged between the parties; and (4) disconnection, when the task reaches some stage of completion.
Literature Review
We examined written electronic communication between providers including e‐mail, text messaging, and instant messaging. We did not review provider‐to‐provider telephone or telehealth communication, as these are not generally supported within EHR systems. Communication in all clinical contexts was included among providers within an individual clinic or hospital and among providers across specialties or practice settings.[40] We excluded physician handoff communication because it has been extensively reviewed elsewhere and because handoff occurs largely through verbal exchange not recorded in the EHR.[41, 42] Communication from clinical information systems to providers, such as automated notification of unacknowledged orders, was also excluded, as it is not within the scope of provider‐to‐provider interaction.
Data Sources and Searches
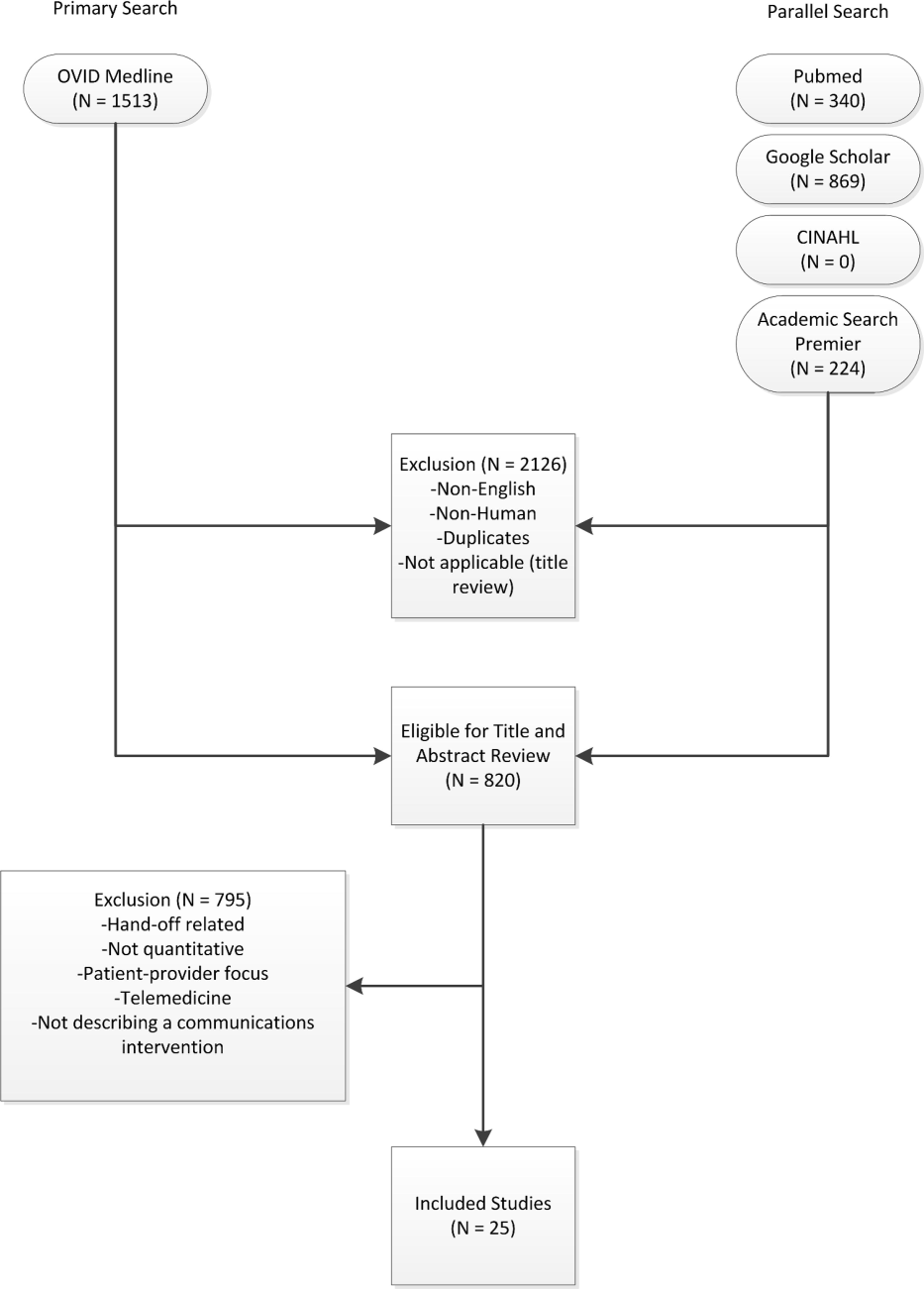
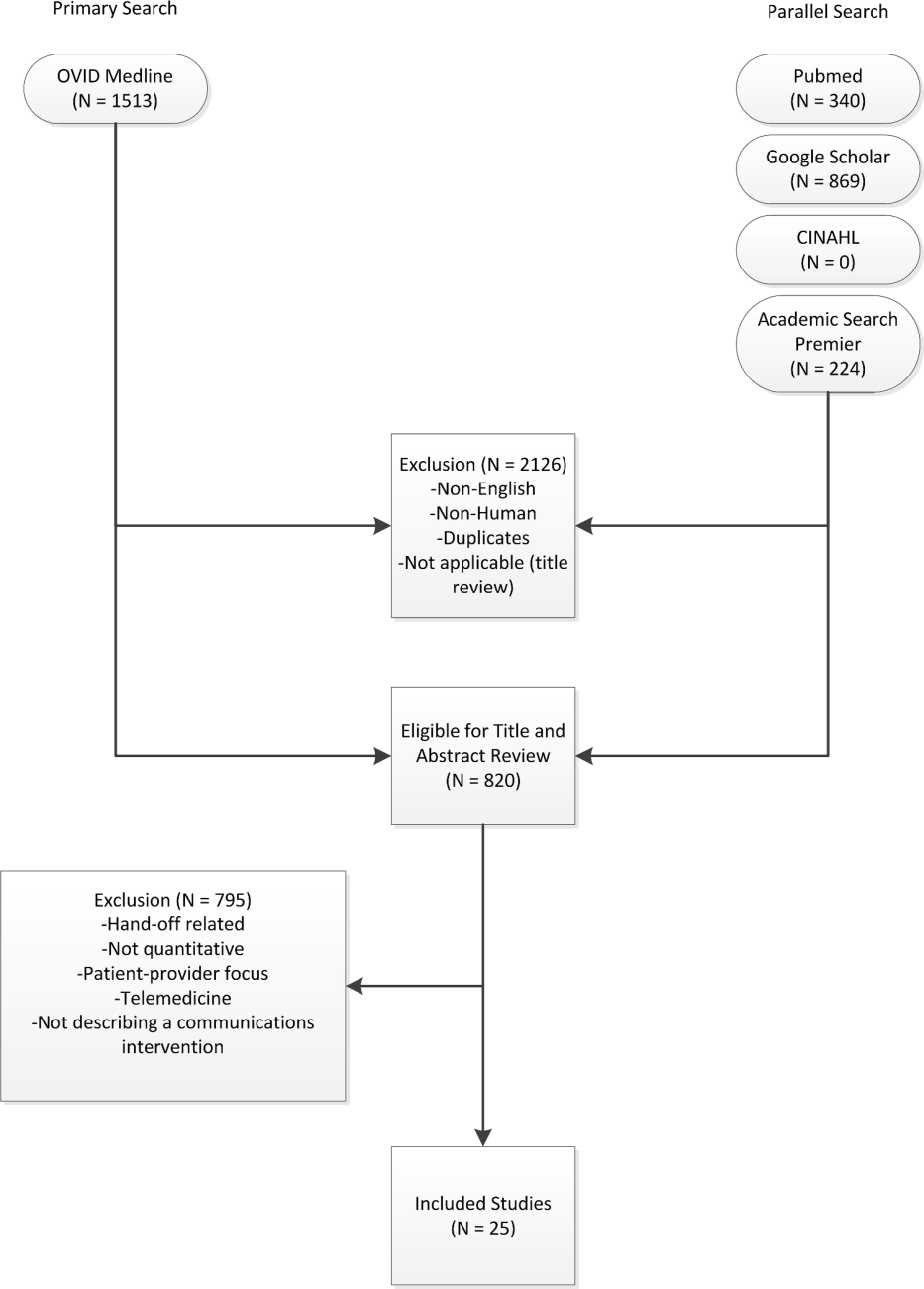
A comprehensive literature search was conducted in Ovid MEDLINE with the input of a medical librarian, and a parallel search was performed using PubMed. The Ovid MEDLINE query and parallel database search terms are documented in Table 1. Subsearches were conducted in Google Scholar, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Academic Search Premier for peer‐reviewed journals. Subsequent studies citing the initially detected articles were found through citation maps.
| Database | Strategy | Items Reviewed |
|---|---|---|
| ||
| Ovid MEDLINE | Query terms: exp medicine/ or physicians or exp outpatient clinics/ or exp hospitals/ AND *communication/ or *computer communication networks/ or *interprofessional relations/ or *continuity of patient care/ AND electronic mail or referral and consultation or text messaging/ or reminder systems. | 1513 |
| PubMed | Healthcare, provider, communication, messaging, e‐mail, texting, text messaging, instant messaging, paging, coordination, referral, EHR, EMR, electronic health record, electronic medical record, electronic, and physician. Excluding patient‐provider and patient‐physician | 340 |
| Google Scholar | Physician‐physician electronic communication excluding physician‐patient | 940 |
| CINAHL | Medical records and communication; or computerized patient records and communication | None |
| Academic Search Premier (peer‐reviewed journals) | Electronic health record and communication | 54 |
| Communication and electronic health record | 80 | |
| Physician‐physician communication | 2 | |
| Physicians and electronic health records | 88 | |
Study Selection
Paper Inclusion Criteria
Requirements included publication in English‐language peer‐reviewed journals. Included studies provided quantitative provider‐to‐provider communication data, provider satisfaction statistics, or EHR communication data. Provider‐to‐staff communication was also included if it fell within the scope of studies of communication between providers.
Paper Exclusion Criteria
Studies excluded in this review were articles that reviewed EHR systems without any focus on communication between providers and those that discussed EHR models and strategies but did not include actual testing and quantitative results. Results that included nontraditional online documents or that were found on nonpeer‐reviewed websites were also discarded. Duplicate records or publications that covered the same study were also removed. The most common reason for exclusion was the lack of quantitative evaluation.
Data Extraction and Quality Assessment
Three authors (Walsh, Siegler, Stetson) reviewed titles and abstracts of resultant studies against inclusion and exclusion criteria (Figure 1). Studies were evaluated qualitatively and findings summarized. Given the heterogeneous nature of data reported, statistical analysis was not possible.
RESULTS
The primary and parallel searches produced 2946 results that were weaned through title review and exclusion of duplicates, nonEnglish‐language, and nonhuman studies to 820 articles for title and abstract review (Figure 1). After careful review of the articles' titles, abstracts, or full content (where appropriate), twenty‐five articles met inclusion criteria and presented data about provider‐to‐provider electronic communication, either within an EHR or through a system designed to promote provider‐to‐provider communication. All of the studies that met inclusion criteria focused on physicians as providers. Five studies (20%) described trial design, three (12%) were pilot studies, and seventeen (68%) were observational studies. Thirteen of twenty‐five articles (52%) described studies conducted in the United States and twelve in Europe.
Most of the studies (56%) focused on electronic referrals between primary care and subspecialty providers. The clinical need was to communicate information on a specific patient with a specialist who shared responsibility for the overall plan of care. Only two studies evaluated curbside consultation, where providers ask for clinical recommendations without formally engaging a specialist in the plan of care for a particular patient. Table 2 summarizes included studies and has been organized with respect to clinical need under evaluation. The major themes that emerged from this review included: studies of penetration of communication tools either within the EHR system (intra‐EHR IT) or external to the EHR (extra‐EHR IT); electronic referrals; curbside consultations; and test results reporting (results notification).
| Primary Author, Year | Design | Intervention | Measurement | Results |
|---|---|---|---|---|
| ||||
| Need: Communicate care across clinical settings (inpatient‐outpatient) | ||||
| Branger, 1992[4, 6] | Observational study | Introduction of electronic messaging system in the Netherlands between hospital and PCPs. | Satisfaction survey data using Likert scale of usefulness. | Free text messaging to exchange patient data was rated very useful or useful by 20 of 27 PCP respondents. |
| Reponen, 2004[66] | Observational study | Finnish study of electronic referrals XML messages between EHRs or secure web links. | User questionnaire. No description of respondents was provided. | Internists surveyed estimated that electronic referrals accelerate the referral process by 1 week. |
| Need: Communicate care across specialties (primary care physicians‐specialists) | ||||
| Kooijman, 1998[67] | Observational study | Survey of 45 PCPs who received notes from specialists via Electronic Data Interchange. | User questionnaire with 5‐point Likert scale of satisfaction, from 1 (much better) to 5 (much worse). | Highest satisfaction scores for speed (1.51.8) and efficiency (1.51.7) for electronic messages, with lower scores for reliability (2.52.7) and clarity (2.5). |
| Harno, 2000[4][8] | Nonrandomized trial | Eight‐month prospective comparative study in Finland of outpatient clinics in hospitals with and without intranet referral systems. | Comparison of numbers of electronic referrals, clinic visits, costs. | There were 43% of electronic referrals and 79% of outpatient referrals that resulted in outpatient visits. A 3‐fold increase in productivity overall and 7‐fold reduction in visit costs per patient using e‐mail consultation. |
| Moorman, 2001[4][7] | Observational study | Supersedes Branger, 1999.[68] Analyzes intra‐EHR communications between PCPs and consultant in Netherlands re: diabetes management of patients (19941998). | Descriptive statistics of number of messages, content, whether message had been copied into EMR; survey of PCPs (12 of 15 responded). | Decline in integration by PCPs of messages in the EHR from 75% to 51% over first 3 years. Despite this, most PCPs wanted to extend messaging to other patient groups. |
| Bergus, 2006[69] | Observational study | Follow‐up of Bergus, 1998[54]; evaluated formulation of clinical referrals to specialists at the University of Iowa by retrospective review of e‐mail transcripts. | Analyzed taxonomy of clinical questions; assessed need for clinical consultation of 1618 clinical questions. | Specialists less likely to recommend clinic consultation if referral specified the clinical task (OR: 0.36, P0.001), intervention (OR: 0.62, P=0.004), or outcome (OR: 0.49, P0.001). This effect was independent of clinical content (P>0.05). |
| Dennison, 2006[70] | Pilot study | Construction of an electronic referral pro forma to facilitate referral of patients to colorectal surgeons. | Descriptive statistics. Comparisons of patient attendance rate, delays to booking and to actual appointment between 54 electronic referrals and 189 paper referrals. | Compared to paper referrals, electronic referrals were booked more quickly (same day vs 1 week later on average) and patients had lower nonattendance rates (8.5% vs 22.5%). Both results stated as statistically significant, but P values were not provided. |
| Shaw, 2007[49] | Observational study | Dermatology electronic referral in England. | Content of 131 electronic vs 139 paper referrals to dermatologists(NHS Choose and Book).[71] | Paper superior to electronic for clinical data such as current treatments (included in 68% of paper vs 39% of electronic referrals, P0.001); electronic superior for demographic data. |
| Gandhi, 2008[50] | Nonrandomized trial | Electronic referral tool in the Partners Healthcare System in Massachusetts that included a structured referral‐letter generator and referral status tracker. Assigned to 1 intervention site and 1 control site. | Survey assessment. Fifty‐four of 117 PCPs responded (46%), 235 of 430 specialists responded (55%), 143 out of 210 patients responded (69%). | Intervention group showed high voluntary adoption (99%), higher information transfer rates prior to subspecialty visit (62% vs 12%), and lower rates of conflicting information being given to patients (6% vs 20%). |
| John, 2008[72] | Pilot study | Validation study of the Lower Gastrointestinal e‐RP (through the Choose and Book System in the United Kingdom) intended to improve yield of colon cancers diagnosed and to reduce delays in diagnosis. | Comparison of actual to simulated referral patterns through e‐RP for 300 patients divided into colorectal cancer, 2‐week wait suspected cancer, and routine referral groups. | e‐RP was more accurate than traditional referral at upgrading patients who had cancer to the appropriate suspected cancer referral group (85% vs 43%, P=0.002). |
| Kim, 2009[73] | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Included reply functionality and ability to forward messaging to a scheduler for calendaring. | Impact of electronic referral system as measured by questionnaire to referring providers. A total of 298/368 participated (24 clinics); 53.5% attending physicians. | Electronic referrals improved overall quality of care (reported by 72%), guidance of presubspecialty visit (73%), and the ability to track referrals (89%). Small change in access for urgent issues (35% better, 49% reported no change). |
| Scott, 2009[74] | Pilot study | Pilot of urgent electronic referral system from PCPs to oncologists at South West Wales Cancer Centre. | Satisfaction statistics (10‐point Likert scale) collected from PCPs via interview. | Over 6 months, 99 referrals submitted; 81% were processed within 1 hour with high satisfaction scores. |
| Were, 2009[75] | Nonrandomized trial | Geriatrics consultants were provided system to make electronic recommendations (consultant‐recommended orders) in the native CPOE system along with consult notes in the intervention vs consult notes alone in the control. | Rates of implementation of consultant recommendations. Qualitative survey of users of the new system. | Higher total number of recommendations (247 vs 192, P0.05) and higher implementation rates of consultant‐recommended orders in the intervention group vs control (78% vs 59%, P=0.01). High satisfaction scores on 5‐point Likert scale for the intervention system with good survey response rate (83%). |
| Dixon, 2010[52] | Observational study | Comparison of 2 extra‐EHR systems (NHS Choose and Book, Dutch ZorgDomein) for booking referrals. Patients choose doctor or hospital and the system transfers demographic and clinical information between PCP and specialist. | National data, patient and provider surveys, focus groups, observational studies. Focus was on patient choice, but evaluations included all aspects of the systems. | Resistance from PCPs during implementation; 78% of ZorgDomein PCPs felt referrals took more time; general displeasure on the part of specialists re: quality of referrals, although not quantified. |
| Patterson, 2010[51] | Observational study | E‐mail referral system to a neurologist in Northern Ireland. Referrals were template based and recorded as clinical episode in the patient administration system. Comparison of this system to conventional referrals to another neurologist. | Evaluated effectiveness, cost, safety for period 20022007. | Decreased referral wait times (4 vs 13 weeks) and 35% cost reduction per patient for the e‐mail referral vs conventional referrals. |
| No diminution in safety. Limitation: single neurologist participated. | ||||
| Singh, 2011[76] | Observational study | Chart review of electronic referrals to specialist practices in a Veterans Affairs outpatient system. | Follow‐up actions taken by subspecialists within 30 days of receiving referral. | An intra‐EHR referral system was still affected by communication breakdowns. Of 61,931 referrals, 36.4% were discontinued for inappropriate or incomplete referral requests. |
| Kim‐Hwang, 2010[77] | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Follow‐up to Kim, 2009.[73] | Survey of medical and surgical subspecialty consultants. | Statistically significant differences in clarity of consult request in both medical and surgical clinics, in decreased inappropriate referrals in surgical clinics, in decreased use of follow‐up appointments by surgical specialists, and in decreased avoidable follow‐up surgical visits. |
| Warren, 2011[53] | Observational study | Electronic referrals from general medical practices to public referral network of Hutt Hospital in New Zealand (20072010). | Retrospective analysis of transactional data from messaging system and from general inpatient tracking system. Qualitative data collection via interviews. | Estimated 71% of 10,367 referrals were electronic referrals over 3 years. Statistically significant improvement in referral latency without change in staffing. Clinicians appreciate shared transparency of referrals but cite usability issues as barriers. |
| Need: Curbside consults (primary care physicians‐specialists) | ||||
| Bergus, 1998[54] | Observational study | Evaluation of the ECS for curbside consultations between family physicians and subspecialists. | Descriptive statistics of usage data; survey of users. | Median response time 16.1 hours; 92% of questions answered; almost 90% concerned specific patients. Both groups expressed satisfaction. |
| Abbott, 2002[55] | Observational study | Evaluation of Department of Defense Ask a Doc physician‐to‐physicians e‐mail consultation system over network of 21 states (19982000). | Descriptive statistics; qualitative assessment. | There were 3121 consultations. Average response time 12 hours. Minimal cost and effort to initiate and sustain. Felt to mirror clinical practice. Barriers were security and assignation of credit for consultation. |
| Need: Communication of results (primary care physicians ‐specialists) | ||||
| Singh, 2007[5][6] | Nonrandomized trial | Concurrent prospective evaluation of responses to 1017 critical imaging alert notifications in a Veterans Affairs outpatient system (2006). Radiologists generated alerts. Included receipt system. | Measured percentage of unacknowledged alerts and imaging lost to follow‐up. | There were 368 of 1017 transmitted alerts unacknowledged (36%); 45 were completely lost to follow‐up. There were 0.2% outpatient imaging results lost to follow‐up overall. |
| Singh, 2009[5][7] | Nonrandomized trial | Concurrent evaluation of responses to 1196 critical imaging alert notifications in a Veterans Affairs outpatient system (20072008). Similar coding system to Singh, 2007.[56] | Measured percentage of alerts acknowledged, timely follow‐up; compared electronic alerts alone to combination of alerts and phone calls or admission. | Percentage of alerts acknowledged did not differ by type of communication; combination of electronic alerts with phone follow‐up (OR: 0.12, P0.001) or admission (OR: 0.22, P0.001) decreased likelihood of delayed follow‐up. Alerts to 2 providers increased the likelihood of delayed follow‐up (OR: 1.99, P=0.03). |
| Abujudeh, 2009[5][8] | Observational study | Retrospective review of e‐mailbased alert system for abnormal imaging results at Massachusetts General Hospital 20052007. E‐mail alerting by radiologist to ordering physician of nonurgent findings. | Descriptive statistics; survey of referring physicians (12/26). | There were 56,691 out of 1,540,254 reports for important but not urgent findings; 93.3% generated e‐mail message (6.7% failure rate); 80% of alerts were viewed. Higher satisfaction for e‐mail alerts over conventional methods (eg, facsimile) for nonurgent but important findings. |
| Need: Communicate within 1 care setting (primary care physicians) | ||||
| Lanham, 2012[78] | Observational study | Comparison of practice‐level EHR use with communication patterns among physicians, nurses, medical assistants, practice managers, and nonclinical staff within individual practices in Texas. | Observation and semistructured interviews. Within‐practice communication patterns were categorized as fragmented or cohesive. Practice‐level EHR use was categorized as homogeneous or heterogeneous. | Clinical practices with cohesive within‐practice communication patterns were associated with homogeneous patterns of practice‐level EHR use. |
| Murphy, 2012[79] | Observational study | Review of note‐based messaging within the EHR in outpatient clinics of large tertiary Veterans Affairs facility. Clinic staff send additional signature request alerts linked to parent notes in the EHR to primary care physicians. | Reason for and origin of alerts. Parent note linked to alert was also reviewed for 3 value attributes: urgency; potential harm if alert was missed; subjective value to PCP of the alert. | Of the alerts reviewed, 53.7% of 525 were deemed of high value but required PCPs to review significant amounts of extraneous text (80.3% of words in parent notes) to get relevant information. Most alerts (40%) were medication, prescription, or refill related. |
Extra‐EHR IT
A review of electronic communication in 2000 examined electronic communication among primary care physicians but notably did not distinguish between communication and data exchange.[43] Of the thirty included publications in that review, seventeen publications dealt with electronically communicated information in general; the remaining studies focused on notifications of test results or transitions of care, reports from specialists, or electronic communication as replacement of traditional referral.[43] Although many studies of electronic communication described positive benefits, few included objective data, and most did not analyze provider‐to‐provider communication specifically. A survey of IT use outside of the EHR in 2006 documented that approximately 30% of clinicians used e‐mail to communicate with other clinicians, fewer than those who consulted on‐line journals (40.8%), but many more than those who communicated with patients by e‐mail at that time (3.6%).[44]
Intra‐EHR IT
A comparison of two physician surveys of EHR use in Massachusetts (the first in 2005 and the second in 2007) documented an increase in the percentage of practices with an EHR, from 23% to 35%; in those practices with EHRs, only the use of electronic prescribing increased over time. Use of secure electronic referrals or messaging including secure e‐mail remained unchanged; of note, referrals and messaging were considered a singular clinical function in that study. Between 2005 and 2007, referrals or clinical messaging were available in 62% and 63% of EHR systems, respectively, and they were used most or all of the time by 29% to 33% of the physicians who had an EHR.[45]
Electronic Referrals
Fourteen articles focused on electronic referrals. Two had a prepost or longitudinal study design,[46, 47] and five included a control group.[48, 49, 50, 51] The rest were descriptive. In most cases, electronic referral improved the transfer of information, especially when standardized message templates were created. Use of electronic referral appeared to result in reduced waiting time for appointments and enabled more efficient triage.
Barriers to integration of electronic referral in the EHR were also assessed. An intra‐EHR communication system requiring a primary care physician to integrate information e‐mailed by the consultant into the record showed the percentage of integrated notes decreasing over time.[47] Practitioners had mixed feelings about the system; although the majority (92% of respondents) felt that the system improved patient care and wanted to extend messaging to other patient groups, they also felt that electronic messaging decreased the ease of reviewing data (83%) and confused tasks and responsibilities (59%). A study of British and Dutch electronic referral systems described significant resistance on the part of practitioners to electronic referrals and concern on the part of specialists about the quality of referrals.[52] Another study demonstrated improvement in quality of demographic data but degradation in quality of clinical information when referrals were submitted electronically.[49] A recent transactional analysis of electronic referrals in New Zealand showed high uptake and reduced referral latency compared to conventional referral; clinicians cited usability concerns as the major barrier to use.[53]
Curbside Consultations via E‐mail
Two studies evaluated curbside consultations via e‐mail and documented high provider satisfaction and rapid turnaround.[54, 55] The preliminary nature of these studies raises questions of sustainability and long‐term implementation.
Results Notification
Three studies focused on test‐result reporting from radiologists. In these studies, a radiologist could designate a result as high priority and have an e‐mail notification sent to the ordering physicians.[56, 57, 58] Urgent results were relayed by telephone. Lack of acknowledgement of alerts impacted the results of every study, and in one of these studies, alerting two physicians, rather than just one, decreased the likelihood that the results would be followed up.[57] Providers did prefer e‐mail to fax notification.[58]
DISCUSSION
The principal findings of the literature review demonstrate the paucity of quantitative data surrounding provider‐to‐provider communication. The majority of studies focused on physicians as providers without emphasis on other provider types on the care team. Most of the quantitative studies investigated electronic referrals. Data collected largely represented measures of provider satisfaction and process measures. Few quantitative studies used established models or measures of team coordination or communication.
This study extends the work of others by compiling a comprehensive view of electronic provider‐to‐provider communication. A recent review of devices for clinical communication tells a part of the story,[28] and our review adds a comprehensive, device‐agnostic look at the systems physicians and other providers use every day.
Limitations of this review include the small number of eligible studies and a homogenous provider type (physicians). The latter is both an important finding and a limitation to generalizability of our results. Reviewed studies were in English only. The literature review by its nature is subject to publication bias.
Intra‐EHR communication cannot serve all purposes, and is it not a panacea for effective care coordination. One recent qualitative study warns about the pitfalls of electronic communication. Interviews with physicians from twenty‐six practices elicited some concerns about the resulting decrease in face‐to‐face communication that has resulted from the adoption of electronic communication tools.[32] This finding brings implications: (1) a false sense of security may reduce verbal communications when they are needed mostduring emergencies or when caring for complex patients who require detailed, nuanced discussion; and (2) fewer conversations within a practice can reduce both knowledge sharing and basic social interactions necessary for the maintenance of a collaboration. Last, privacy and confidentiality are top priorities. Common electronic communication tools are susceptible to security breaches,[47, 59] and innovations within this domain must conform to Health Insurance Portability and Accountability Act of 1996 and Health Information Technology for Economic and Clinical Health Act regulations.[60]
Although electronic communication is not a complete solution for clinical collaboration, it is difficult to use face‐to‐face communication and telephone communication to convey large amounts of patient information while simultaneously generating a record of the transaction. Moreover, paging functions, telephone calls, and face‐to‐face encounters can be highly interruptive, increasing cognitive load, burdening working memory, and shifting attention from the task at hand.[14] Interruptions contribute to inefficiency and to the potential for errors.[61]
Effective coordination of care for the chronically ill is one of the essential goals of the health system; it is an ongoing process that depends on constant, effective communication. Bates and Bitton have recognized this and described the crucial role that HIT will play in creating an effective medical home by enumerating seven domains of HIT especially in need of research.[62] In particular, they note that effective team care and care transitions will depend on an EHR that promotes both implicit and real‐time communication: it will be essential to develop communication tools that allow practices to record goals shared by providers and patients alike, and to track medical interventions and progress.[62]
Future research could investigate a number of open questions. Overall, an emphasis should be placed on rigorous qualitative and quantitative evaluation of electronic communication. Process measures, such as length of stay, hospital readmission rates, and measures of care coordination, should be framed ultimately with respect to patient health outcomes. Such data are beginning to be reported.[63]
It is unclear which types of communications would be best served within the EHR and which should remain external to it. Instant communication or chat has not been studied sufficiently to show a demonstrable impact on patient care. Cross‐coverage and team identification within the EHR can be further studied with respect to workflows and best practices. Studies using structured observation or time‐and‐motion analysis could provide insight into use cases and workflows that providers implement to discuss patients. Future research should incorporate established models of communication[5] and coordination.[64] Data on unintended consequences or harms of provider‐to‐provider electronic communication have been limited, and this area should be considered in subsequent work. Finally, although the scope of this review focused on communication between providers, transformative electronic communication systems should bridge communication gaps between providers and patients as well.
As adoption of EHRs in US hospitals has increased from 15.1% of US hospitals in 2010 to 26.6% in 2011 for any type of EHR and 3.6% to 8.7% for comprehensive EHRs,[65] it is worth noting that Meaningful Use, as it stands, incentivizes patient‐provider communication, but not communication between providers. Inclusion of certification criteria focused on provider‐to‐provider communication may spur additional innovation.
CONCLUSIONS
The optimal features to support electronic communication between providers remain under‐assessed, although there is preliminary evidence for the acceptability of electronic referrals. Without better understanding of electronic communication on workflow, provider satisfaction, and patient outcomes, the impact of such tools on coordination of complex medical care will be an open question, and it remains an important one to answer.
Acknowledgments
The authors would like to express their gratitude to Dr. Thomas Payne, Medical Director of IT Services at the University of Washington, for sharing his expertise, and to Marina Chilov, medical librarian at Columbia University, for her assistance with the literature search. The authors would like to thank Paul Sun, MA, for his assistance with the literature review.
Disclosures: This work was funded by 5K22LM8805 (PDS) and T15 LM007079 (CW, SC) grants. Dr. Stetson serves on the advisory board of the Allscripts Enterprise EHR.
- , . Physician‐physician communication: what's the hang‐up? J Gen Intern Med. 2009;24:437–439.
- , , , et al. Meta‐analysis: effect of interactive communication between collaborating primary care physicians and specialists. Ann Intern Med. 2010;152(4):247–258.
- , , , , . Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2009;25:177–185.
- , , , , , . Development of an ontology to model medical errors, information needs, and the clinical communication space. Proc AMIA Symp. 2001:672–676.
- . Clinical communication: a new informatics paradigm. Proc AMIA Annu Fall Symp. 1996:17–21.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):CD000072.
- , , , . Primary care physician attitudes regarding communication with hospitalists. Dis Mon. 2002;48(4):218–229.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280(15):1311–1316.
- , , , . Analysing potential harm in Australian general practice: an incident‐monitoring study. J Am Med Inform Assoc. 1998;169:73–76.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , , . Communication loads on clinical staff in the emergency department. J Am Med Inform Assoc. 2002;176(9):415–418.
- , , , , , . Deficit in communicaiton and information transfer between hospital‐based and primary care physicians. JAMA. 2007;297:831–841.
- , . Improving clinical communication: a view from psychology. J Am Med Inform Assoc. 2000;7(5):453–461.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , , , , . The Quality in Australian Health Care Study. Med J Aust. 1995;163:458–471.
- , , , et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752.
- , , . Costs and benefits of health information technology. Evid Rep Technol Assess. 2006;132:1–71.
- , , , et al. Relationship between use of electronic health record features and health care quality: results of a statewide survey. Med Care. 2010;48:203–209.
- , , , et al. Decrease in hospital‐wide mortality rate after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2010;126:e1–e8.
- , , , , . Electronic prescribing improves medication safety in community‐based office practices. J Gen Intern Med. 2010;25:530–536.
- . Patient‐centered Care. Radiol Technol. 2009;81(2):133–147.
- , . The missing link: bridging the patient‐provider health information gap. Health Aff (Millwood). 2005;24(5):1290–1295.
- , , , , . Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126.
- , . Web messaging: a new tool for patient‐physician communication. J Am Med Inform Assoc. 2003;10(3):260–270.
- , , , . Expanding the guidelines for electronic communication with patients. J Am Med Inform Assoc. 2001;8(4):344–348.
- , , , . The utility of electronic mail as a medium for patient‐physician communication. Arch Fam Med. 1994;3(3):268–271.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , . Desiderata for personal electronic communication in clinical systems. J Am Med Inform Assoc. 2002;9(3):209–216.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7:277–286.
- . Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25:174–176.
- , , . Electronic medical records and communication with patients and other clinicians: are we talking less? Issue Brief Cent Stud Health Syst Change. 2010;(131):1–4.
- , . Referral and consultation communication between primary care and specialist physicians: finding common ground. Arch Intern Med. 2011;171(1):56–65.
- , . The "meaningful use" regulation for electronic health records. N Engl J Med. 2010;363(6):501–504.
- Centers for Medicare 25(3):177–185.
- . Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25(3):174–176.
- , , , . A framework for clinical communication supporting healthcare delivery. AMIA Annu Symp Proc. 2005:375–379.
- Understanding and improving patient handoffs. Jt Comm J Qual Improv. 2010:49–96.
- , , , . Signout: a collaborative document with implications for the future of clinical information systems. AMIA Annu Symp Proc. 2007:696–700.
- , , . Effects of electronic communication in general practice. Int J Med Inform. 2000;60(1):59–70.
- , , , , . Prevalence of basic information technology use by U.S. physicians. J Gen Intern Med. 2006;21:1150–1155.
- , , , et al. Physicians' use of key functions in electronic health records from 2005 to 2007: a statewide survey. J Am Med Inform Assoc. 2009;16:465–470.
- , , , et al. Electronic communication between providers of primary and secondary care. BMJ. 1992;305(6861):1068–1070.
- , , , . Electronic messaging between primary and secondary care: a four‐year case report. J Am Med Inform Assoc. 2001;8(4):372–378.
- , , , . Patient referral by telemedicine: effectiveness and cost anslysis of an intranet system. J Telemed Telecare. 2000;6(6):320–329.
- , . Strengths and weaknesses of electronic referral: comparison of data content and clinical value of electronic and paper referrals in dermatology. Br J Gen Pract. 2007;57(536):223–224.
- , , , et al. Improving referral communication using a referral tool within an electronic medical record. In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches. Vol. 3. Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality; 2008:63–74.
- , , , . Email triage is an effective, efficient, and safe way of managing new referrals to a neurologist. Qual Safety Health Care. 2010;19(5):e51.
- , , . The experience of implementing choice at point of referral: a comparison of the Netherlands and England. Health Econ Policy Law. 2010;13:1–23.
- , , , , . Introduction of electronic referral from community associated with more timely review by secondary services. Appl Clin Inform. 2011;2(4):546–564.
- , , , . Use of an e‐mail curbside consultation service by family physicians. J Fam Pract. 1998;47:357–360.
- , , , , , . Physician‐to‐physician consultation via electronic mail: the Walter Reed Army Medical Center Ask a Doc system. Mil Med. 2002;167:200–204.
- , , , , , . Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459–466.
- , , , et al. Timely follow‐up of abnormal diagnostic imaging test results in an outpatient setting: are electronic medical records achieving their potential? Arch of Intern Med. 2009;169(17):1578–1586.
- , , , , . Important imaging finding e‐mail alert system: experience after 3 years of implementation. Radiology. 2009;252:747–753.
- . Instant insecurity: security issues of instant messaging. Symantec website. Available at: http://www.symantec.com/connect/articles/instant‐insecurity‐security‐issues‐instant‐messaging.
- . Secure messaging in healthcare. Tech solutions for HIPAA‐compliant messaging. J AHIMA. 2008;79(6):50–51.
- , , , , . Association of interruptions with an increased risk and severity of medication administration errors. Arch Intern Med. 2010;170(8):683–690.
- , . The future of health information technology in the patient‐centered medical home. Health Aff (Millwood). 2010;29(4):614–621.
- , , . eReferral—a new model for integrated care. N Engl J Med. 2013;368(26):2450–2453.
- , , , et al. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. Vol 7. Care Coordination. Rockville, MD; 2007.
- , , , , . Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff (Millwood). 2012;31(5):1092–1099.
- , , , . Extending a multimedia medical record to a regional service with electronic referral and discharge letters. J Telemed Telecare. 2004;10S:81–83.
- , . Sending specialist reports to GPs using EDI. Stud Health Tech Inform. 1998;52(pt 1):408–411.
- , , , , . Shared care for diabetes: supporting communication between primary and secondary care. Int J Med Inform. 1999;53(2-3):133–142.
- , , , . Email teleconsultations: well formulated clinical referrals reduce the need for clinic consultation. J Telemed Telecare. 2006;12(1):33–38.
- , , , . An effective electronic surgical referral system. Ann R Coll Surg Engl. 2006;88(6):554–556.
- . Choose and book. Clin Med. 2006;6(5):473–476.
- , , , . Validation of the lower gastrointestinal electronic referral protocol. Brit J Surg. 2008;95:506–514.
- , , , , . Not perfect, but better: primary care providers' experiences with electronic referrals in a safety net health system. J Gen Intern Med. 2009;24:614–619.
- . The Swansea electronic referrals project. J Telemed Telecare. 2009;15:156–158.
- , , , , . Using computerized provider order entry and clinical decision support to improve referring physicians' implementation of consultants' medical recommendations. J Am Med Inform Assoc. 2009;16(2):196–202.
- , , , et al. Follow‐up actions on electronic referral communication in a multispecialty outpatient setting. J Gen Intern Med. 2011;26(1):64–69.
- , , , , , . Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med. 2010;25(10):1123–11028.
- , , . Same organization, same electronic health records (EHRs) system, different use: exploring the linkage between practice member communication patterns and EHR use patterns in an ambulatory care setting. J Am Med Inform Assoc. 2012;19(3):382–391.
- , , , et al. Electronic health record‐based messages to primary care providers: valuable information or just noise? Arch Intern Med. 2012;172(3):283–285.
INTRODUCTION
Coordination of care within a practice, during transitions of care, and between primary and specialty care teams requires more than data exchange; it requires effective communication among healthcare providers.[1, 2, 3] In clinical terms, data exchange, communication, and care coordination are related, but they represent distinct concepts.[4] Data exchange refers to transfer of information between settings, independent of the individuals involved, whereas communication is the multistep process that enables information exchange between two people.[5] Care coordination, as defined by O'Malley, is integration of care in consultation with patients, their families and caregivers across all of a patient's conditions, needs, clinicians and settings.[3]
Strong collaboration among providers has been associated with improved patient outcomes.[2, 6] Yet, despite the significant role of communication in healthcare, communication may not take place at all, even at high‐stakes events like transitions of care,[7, 8] or it may be done poorly at the risk of substantial clinical morbidity and mortality.[9, 10, 11, 12, 13, 14, 15, 16]
Proof of the global effectiveness of health information technology (HIT) to improve patient care is lacking, but data from some studies demonstrate real improvements in quality and safety in specific areas,[17, 18, 19] especially with computerized physician order entry[20] and electronic prescribing.[21]
The limited information about the effect of HIT on communication focuses largely on the anticipated improvements in patient‐physician communication[22, 23, 24, 25, 26, 27]; provider‐to‐provider communication within the electronic domain is not as well understood. A recent review of interventions involving communication devices such as pagers and mobile phones found limited high‐quality evidence in the literature.[28] Clinicians have described what they consider to be key characteristics of clinical electronic communications systems such as security/reliability, cross coverage, overall convenience, and message prioritization.[29] Although the electronic health record (EHR) is expected to assist with this communication,[30] it also has the potential to impede effective communication, leading physicians to resort to more traditional workarounds.[31, 32, 33]
Measuring and improving the use of EHRs nationally were driving forces behind the creation of the Meaningful Use incentive program in the United States.[34] To receive the incentive payments, providers must meet and report on a series of measures set in three stages over the course of five years.[35] In the current state, Meaningful Use does not reward provider‐to‐provider communication within the EHR.[36, 37] The main communication objectives for stages 1 and 2 concentrate on patient‐to‐provider communication, such as patient portals and patient‐to‐provider messaging.[36, 37]
Understanding the current evidence for provider‐to‐provider communication within EHRs, its reported effectiveness, and its shortcomings may help to develop a roadmap for identifying next‐generation solutions to support coordination of care.[38, 39] This review assesses the literature regarding provider‐to‐provider electronic communication tools (as supported within or external to an EHR). It is intended as a comprehensive view of studies reporting quantitative measures of the impact of electronic communication on providers and patients.
METHODS
Definitions and Conceptual Model of Provider‐to‐Provider Communication
We conducted a systematic review of studies of provider‐to‐provider electronic communication. This review included only formal clinical communication between providers and was informed by the Coiera communications paradigm.[5] This paradigm consists of four steps: (1) task identification, when a task is identified and associated with the appropriate individual; (2) connection, when an attempt is made to contact that person; (3) communication, when task‐specific information is exchanged between the parties; and (4) disconnection, when the task reaches some stage of completion.
Literature Review
We examined written electronic communication between providers including e‐mail, text messaging, and instant messaging. We did not review provider‐to‐provider telephone or telehealth communication, as these are not generally supported within EHR systems. Communication in all clinical contexts was included among providers within an individual clinic or hospital and among providers across specialties or practice settings.[40] We excluded physician handoff communication because it has been extensively reviewed elsewhere and because handoff occurs largely through verbal exchange not recorded in the EHR.[41, 42] Communication from clinical information systems to providers, such as automated notification of unacknowledged orders, was also excluded, as it is not within the scope of provider‐to‐provider interaction.
Data Sources and Searches
A comprehensive literature search was conducted in Ovid MEDLINE with the input of a medical librarian, and a parallel search was performed using PubMed. The Ovid MEDLINE query and parallel database search terms are documented in Table 1. Subsearches were conducted in Google Scholar, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Academic Search Premier for peer‐reviewed journals. Subsequent studies citing the initially detected articles were found through citation maps.
| Database | Strategy | Items Reviewed |
|---|---|---|
| ||
| Ovid MEDLINE | Query terms: exp medicine/ or physicians or exp outpatient clinics/ or exp hospitals/ AND *communication/ or *computer communication networks/ or *interprofessional relations/ or *continuity of patient care/ AND electronic mail or referral and consultation or text messaging/ or reminder systems. | 1513 |
| PubMed | Healthcare, provider, communication, messaging, e‐mail, texting, text messaging, instant messaging, paging, coordination, referral, EHR, EMR, electronic health record, electronic medical record, electronic, and physician. Excluding patient‐provider and patient‐physician | 340 |
| Google Scholar | Physician‐physician electronic communication excluding physician‐patient | 940 |
| CINAHL | Medical records and communication; or computerized patient records and communication | None |
| Academic Search Premier (peer‐reviewed journals) | Electronic health record and communication | 54 |
| Communication and electronic health record | 80 | |
| Physician‐physician communication | 2 | |
| Physicians and electronic health records | 88 | |
Study Selection
Paper Inclusion Criteria
Requirements included publication in English‐language peer‐reviewed journals. Included studies provided quantitative provider‐to‐provider communication data, provider satisfaction statistics, or EHR communication data. Provider‐to‐staff communication was also included if it fell within the scope of studies of communication between providers.
Paper Exclusion Criteria
Studies excluded in this review were articles that reviewed EHR systems without any focus on communication between providers and those that discussed EHR models and strategies but did not include actual testing and quantitative results. Results that included nontraditional online documents or that were found on nonpeer‐reviewed websites were also discarded. Duplicate records or publications that covered the same study were also removed. The most common reason for exclusion was the lack of quantitative evaluation.
Data Extraction and Quality Assessment
Three authors (Walsh, Siegler, Stetson) reviewed titles and abstracts of resultant studies against inclusion and exclusion criteria (Figure 1). Studies were evaluated qualitatively and findings summarized. Given the heterogeneous nature of data reported, statistical analysis was not possible.
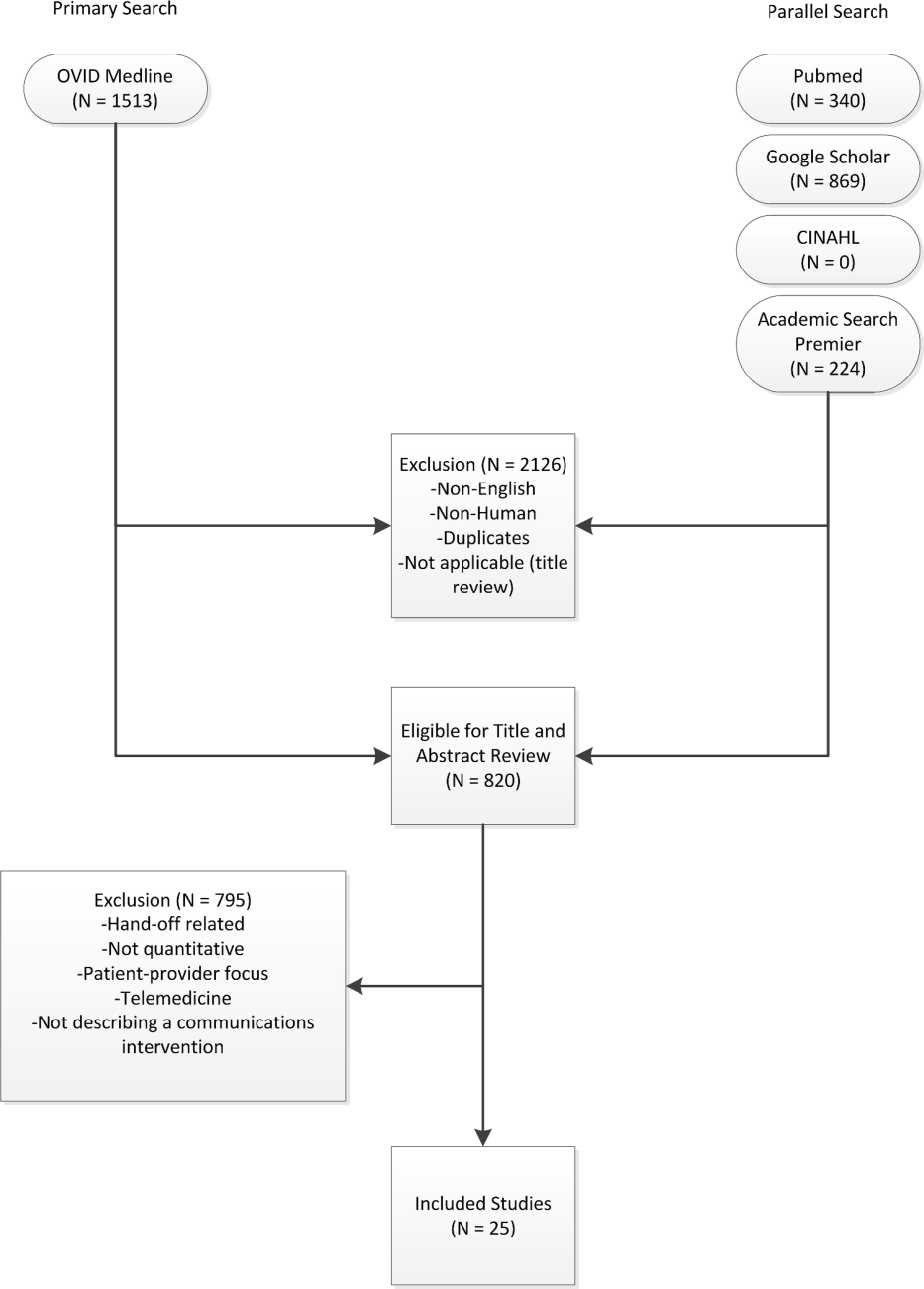
RESULTS
The primary and parallel searches produced 2946 results that were weaned through title review and exclusion of duplicates, nonEnglish‐language, and nonhuman studies to 820 articles for title and abstract review (Figure 1). After careful review of the articles' titles, abstracts, or full content (where appropriate), twenty‐five articles met inclusion criteria and presented data about provider‐to‐provider electronic communication, either within an EHR or through a system designed to promote provider‐to‐provider communication. All of the studies that met inclusion criteria focused on physicians as providers. Five studies (20%) described trial design, three (12%) were pilot studies, and seventeen (68%) were observational studies. Thirteen of twenty‐five articles (52%) described studies conducted in the United States and twelve in Europe.
Most of the studies (56%) focused on electronic referrals between primary care and subspecialty providers. The clinical need was to communicate information on a specific patient with a specialist who shared responsibility for the overall plan of care. Only two studies evaluated curbside consultation, where providers ask for clinical recommendations without formally engaging a specialist in the plan of care for a particular patient. Table 2 summarizes included studies and has been organized with respect to clinical need under evaluation. The major themes that emerged from this review included: studies of penetration of communication tools either within the EHR system (intra‐EHR IT) or external to the EHR (extra‐EHR IT); electronic referrals; curbside consultations; and test results reporting (results notification).
| Primary Author, Year | Design | Intervention | Measurement | Results |
|---|---|---|---|---|
| ||||
| Need: Communicate care across clinical settings (inpatient‐outpatient) | ||||
| Branger, 1992[4, 6] | Observational study | Introduction of electronic messaging system in the Netherlands between hospital and PCPs. | Satisfaction survey data using Likert scale of usefulness. | Free text messaging to exchange patient data was rated very useful or useful by 20 of 27 PCP respondents. |
| Reponen, 2004[66] | Observational study | Finnish study of electronic referrals XML messages between EHRs or secure web links. | User questionnaire. No description of respondents was provided. | Internists surveyed estimated that electronic referrals accelerate the referral process by 1 week. |
| Need: Communicate care across specialties (primary care physicians‐specialists) | ||||
| Kooijman, 1998[67] | Observational study | Survey of 45 PCPs who received notes from specialists via Electronic Data Interchange. | User questionnaire with 5‐point Likert scale of satisfaction, from 1 (much better) to 5 (much worse). | Highest satisfaction scores for speed (1.51.8) and efficiency (1.51.7) for electronic messages, with lower scores for reliability (2.52.7) and clarity (2.5). |
| Harno, 2000[4][8] | Nonrandomized trial | Eight‐month prospective comparative study in Finland of outpatient clinics in hospitals with and without intranet referral systems. | Comparison of numbers of electronic referrals, clinic visits, costs. | There were 43% of electronic referrals and 79% of outpatient referrals that resulted in outpatient visits. A 3‐fold increase in productivity overall and 7‐fold reduction in visit costs per patient using e‐mail consultation. |
| Moorman, 2001[4][7] | Observational study | Supersedes Branger, 1999.[68] Analyzes intra‐EHR communications between PCPs and consultant in Netherlands re: diabetes management of patients (19941998). | Descriptive statistics of number of messages, content, whether message had been copied into EMR; survey of PCPs (12 of 15 responded). | Decline in integration by PCPs of messages in the EHR from 75% to 51% over first 3 years. Despite this, most PCPs wanted to extend messaging to other patient groups. |
| Bergus, 2006[69] | Observational study | Follow‐up of Bergus, 1998[54]; evaluated formulation of clinical referrals to specialists at the University of Iowa by retrospective review of e‐mail transcripts. | Analyzed taxonomy of clinical questions; assessed need for clinical consultation of 1618 clinical questions. | Specialists less likely to recommend clinic consultation if referral specified the clinical task (OR: 0.36, P0.001), intervention (OR: 0.62, P=0.004), or outcome (OR: 0.49, P0.001). This effect was independent of clinical content (P>0.05). |
| Dennison, 2006[70] | Pilot study | Construction of an electronic referral pro forma to facilitate referral of patients to colorectal surgeons. | Descriptive statistics. Comparisons of patient attendance rate, delays to booking and to actual appointment between 54 electronic referrals and 189 paper referrals. | Compared to paper referrals, electronic referrals were booked more quickly (same day vs 1 week later on average) and patients had lower nonattendance rates (8.5% vs 22.5%). Both results stated as statistically significant, but P values were not provided. |
| Shaw, 2007[49] | Observational study | Dermatology electronic referral in England. | Content of 131 electronic vs 139 paper referrals to dermatologists(NHS Choose and Book).[71] | Paper superior to electronic for clinical data such as current treatments (included in 68% of paper vs 39% of electronic referrals, P0.001); electronic superior for demographic data. |
| Gandhi, 2008[50] | Nonrandomized trial | Electronic referral tool in the Partners Healthcare System in Massachusetts that included a structured referral‐letter generator and referral status tracker. Assigned to 1 intervention site and 1 control site. | Survey assessment. Fifty‐four of 117 PCPs responded (46%), 235 of 430 specialists responded (55%), 143 out of 210 patients responded (69%). | Intervention group showed high voluntary adoption (99%), higher information transfer rates prior to subspecialty visit (62% vs 12%), and lower rates of conflicting information being given to patients (6% vs 20%). |
| John, 2008[72] | Pilot study | Validation study of the Lower Gastrointestinal e‐RP (through the Choose and Book System in the United Kingdom) intended to improve yield of colon cancers diagnosed and to reduce delays in diagnosis. | Comparison of actual to simulated referral patterns through e‐RP for 300 patients divided into colorectal cancer, 2‐week wait suspected cancer, and routine referral groups. | e‐RP was more accurate than traditional referral at upgrading patients who had cancer to the appropriate suspected cancer referral group (85% vs 43%, P=0.002). |
| Kim, 2009[73] | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Included reply functionality and ability to forward messaging to a scheduler for calendaring. | Impact of electronic referral system as measured by questionnaire to referring providers. A total of 298/368 participated (24 clinics); 53.5% attending physicians. | Electronic referrals improved overall quality of care (reported by 72%), guidance of presubspecialty visit (73%), and the ability to track referrals (89%). Small change in access for urgent issues (35% better, 49% reported no change). |
| Scott, 2009[74] | Pilot study | Pilot of urgent electronic referral system from PCPs to oncologists at South West Wales Cancer Centre. | Satisfaction statistics (10‐point Likert scale) collected from PCPs via interview. | Over 6 months, 99 referrals submitted; 81% were processed within 1 hour with high satisfaction scores. |
| Were, 2009[75] | Nonrandomized trial | Geriatrics consultants were provided system to make electronic recommendations (consultant‐recommended orders) in the native CPOE system along with consult notes in the intervention vs consult notes alone in the control. | Rates of implementation of consultant recommendations. Qualitative survey of users of the new system. | Higher total number of recommendations (247 vs 192, P0.05) and higher implementation rates of consultant‐recommended orders in the intervention group vs control (78% vs 59%, P=0.01). High satisfaction scores on 5‐point Likert scale for the intervention system with good survey response rate (83%). |
| Dixon, 2010[52] | Observational study | Comparison of 2 extra‐EHR systems (NHS Choose and Book, Dutch ZorgDomein) for booking referrals. Patients choose doctor or hospital and the system transfers demographic and clinical information between PCP and specialist. | National data, patient and provider surveys, focus groups, observational studies. Focus was on patient choice, but evaluations included all aspects of the systems. | Resistance from PCPs during implementation; 78% of ZorgDomein PCPs felt referrals took more time; general displeasure on the part of specialists re: quality of referrals, although not quantified. |
| Patterson, 2010[51] | Observational study | E‐mail referral system to a neurologist in Northern Ireland. Referrals were template based and recorded as clinical episode in the patient administration system. Comparison of this system to conventional referrals to another neurologist. | Evaluated effectiveness, cost, safety for period 20022007. | Decreased referral wait times (4 vs 13 weeks) and 35% cost reduction per patient for the e‐mail referral vs conventional referrals. |
| No diminution in safety. Limitation: single neurologist participated. | ||||
| Singh, 2011[76] | Observational study | Chart review of electronic referrals to specialist practices in a Veterans Affairs outpatient system. | Follow‐up actions taken by subspecialists within 30 days of receiving referral. | An intra‐EHR referral system was still affected by communication breakdowns. Of 61,931 referrals, 36.4% were discontinued for inappropriate or incomplete referral requests. |
| Kim‐Hwang, 2010[77] | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Follow‐up to Kim, 2009.[73] | Survey of medical and surgical subspecialty consultants. | Statistically significant differences in clarity of consult request in both medical and surgical clinics, in decreased inappropriate referrals in surgical clinics, in decreased use of follow‐up appointments by surgical specialists, and in decreased avoidable follow‐up surgical visits. |
| Warren, 2011[53] | Observational study | Electronic referrals from general medical practices to public referral network of Hutt Hospital in New Zealand (20072010). | Retrospective analysis of transactional data from messaging system and from general inpatient tracking system. Qualitative data collection via interviews. | Estimated 71% of 10,367 referrals were electronic referrals over 3 years. Statistically significant improvement in referral latency without change in staffing. Clinicians appreciate shared transparency of referrals but cite usability issues as barriers. |
| Need: Curbside consults (primary care physicians‐specialists) | ||||
| Bergus, 1998[54] | Observational study | Evaluation of the ECS for curbside consultations between family physicians and subspecialists. | Descriptive statistics of usage data; survey of users. | Median response time 16.1 hours; 92% of questions answered; almost 90% concerned specific patients. Both groups expressed satisfaction. |
| Abbott, 2002[55] | Observational study | Evaluation of Department of Defense Ask a Doc physician‐to‐physicians e‐mail consultation system over network of 21 states (19982000). | Descriptive statistics; qualitative assessment. | There were 3121 consultations. Average response time 12 hours. Minimal cost and effort to initiate and sustain. Felt to mirror clinical practice. Barriers were security and assignation of credit for consultation. |
| Need: Communication of results (primary care physicians ‐specialists) | ||||
| Singh, 2007[5][6] | Nonrandomized trial | Concurrent prospective evaluation of responses to 1017 critical imaging alert notifications in a Veterans Affairs outpatient system (2006). Radiologists generated alerts. Included receipt system. | Measured percentage of unacknowledged alerts and imaging lost to follow‐up. | There were 368 of 1017 transmitted alerts unacknowledged (36%); 45 were completely lost to follow‐up. There were 0.2% outpatient imaging results lost to follow‐up overall. |
| Singh, 2009[5][7] | Nonrandomized trial | Concurrent evaluation of responses to 1196 critical imaging alert notifications in a Veterans Affairs outpatient system (20072008). Similar coding system to Singh, 2007.[56] | Measured percentage of alerts acknowledged, timely follow‐up; compared electronic alerts alone to combination of alerts and phone calls or admission. | Percentage of alerts acknowledged did not differ by type of communication; combination of electronic alerts with phone follow‐up (OR: 0.12, P0.001) or admission (OR: 0.22, P0.001) decreased likelihood of delayed follow‐up. Alerts to 2 providers increased the likelihood of delayed follow‐up (OR: 1.99, P=0.03). |
| Abujudeh, 2009[5][8] | Observational study | Retrospective review of e‐mailbased alert system for abnormal imaging results at Massachusetts General Hospital 20052007. E‐mail alerting by radiologist to ordering physician of nonurgent findings. | Descriptive statistics; survey of referring physicians (12/26). | There were 56,691 out of 1,540,254 reports for important but not urgent findings; 93.3% generated e‐mail message (6.7% failure rate); 80% of alerts were viewed. Higher satisfaction for e‐mail alerts over conventional methods (eg, facsimile) for nonurgent but important findings. |
| Need: Communicate within 1 care setting (primary care physicians) | ||||
| Lanham, 2012[78] | Observational study | Comparison of practice‐level EHR use with communication patterns among physicians, nurses, medical assistants, practice managers, and nonclinical staff within individual practices in Texas. | Observation and semistructured interviews. Within‐practice communication patterns were categorized as fragmented or cohesive. Practice‐level EHR use was categorized as homogeneous or heterogeneous. | Clinical practices with cohesive within‐practice communication patterns were associated with homogeneous patterns of practice‐level EHR use. |
| Murphy, 2012[79] | Observational study | Review of note‐based messaging within the EHR in outpatient clinics of large tertiary Veterans Affairs facility. Clinic staff send additional signature request alerts linked to parent notes in the EHR to primary care physicians. | Reason for and origin of alerts. Parent note linked to alert was also reviewed for 3 value attributes: urgency; potential harm if alert was missed; subjective value to PCP of the alert. | Of the alerts reviewed, 53.7% of 525 were deemed of high value but required PCPs to review significant amounts of extraneous text (80.3% of words in parent notes) to get relevant information. Most alerts (40%) were medication, prescription, or refill related. |
Extra‐EHR IT
A review of electronic communication in 2000 examined electronic communication among primary care physicians but notably did not distinguish between communication and data exchange.[43] Of the thirty included publications in that review, seventeen publications dealt with electronically communicated information in general; the remaining studies focused on notifications of test results or transitions of care, reports from specialists, or electronic communication as replacement of traditional referral.[43] Although many studies of electronic communication described positive benefits, few included objective data, and most did not analyze provider‐to‐provider communication specifically. A survey of IT use outside of the EHR in 2006 documented that approximately 30% of clinicians used e‐mail to communicate with other clinicians, fewer than those who consulted on‐line journals (40.8%), but many more than those who communicated with patients by e‐mail at that time (3.6%).[44]
Intra‐EHR IT
A comparison of two physician surveys of EHR use in Massachusetts (the first in 2005 and the second in 2007) documented an increase in the percentage of practices with an EHR, from 23% to 35%; in those practices with EHRs, only the use of electronic prescribing increased over time. Use of secure electronic referrals or messaging including secure e‐mail remained unchanged; of note, referrals and messaging were considered a singular clinical function in that study. Between 2005 and 2007, referrals or clinical messaging were available in 62% and 63% of EHR systems, respectively, and they were used most or all of the time by 29% to 33% of the physicians who had an EHR.[45]
Electronic Referrals
Fourteen articles focused on electronic referrals. Two had a prepost or longitudinal study design,[46, 47] and five included a control group.[48, 49, 50, 51] The rest were descriptive. In most cases, electronic referral improved the transfer of information, especially when standardized message templates were created. Use of electronic referral appeared to result in reduced waiting time for appointments and enabled more efficient triage.
Barriers to integration of electronic referral in the EHR were also assessed. An intra‐EHR communication system requiring a primary care physician to integrate information e‐mailed by the consultant into the record showed the percentage of integrated notes decreasing over time.[47] Practitioners had mixed feelings about the system; although the majority (92% of respondents) felt that the system improved patient care and wanted to extend messaging to other patient groups, they also felt that electronic messaging decreased the ease of reviewing data (83%) and confused tasks and responsibilities (59%). A study of British and Dutch electronic referral systems described significant resistance on the part of practitioners to electronic referrals and concern on the part of specialists about the quality of referrals.[52] Another study demonstrated improvement in quality of demographic data but degradation in quality of clinical information when referrals were submitted electronically.[49] A recent transactional analysis of electronic referrals in New Zealand showed high uptake and reduced referral latency compared to conventional referral; clinicians cited usability concerns as the major barrier to use.[53]
Curbside Consultations via E‐mail
Two studies evaluated curbside consultations via e‐mail and documented high provider satisfaction and rapid turnaround.[54, 55] The preliminary nature of these studies raises questions of sustainability and long‐term implementation.
Results Notification
Three studies focused on test‐result reporting from radiologists. In these studies, a radiologist could designate a result as high priority and have an e‐mail notification sent to the ordering physicians.[56, 57, 58] Urgent results were relayed by telephone. Lack of acknowledgement of alerts impacted the results of every study, and in one of these studies, alerting two physicians, rather than just one, decreased the likelihood that the results would be followed up.[57] Providers did prefer e‐mail to fax notification.[58]
DISCUSSION
The principal findings of the literature review demonstrate the paucity of quantitative data surrounding provider‐to‐provider communication. The majority of studies focused on physicians as providers without emphasis on other provider types on the care team. Most of the quantitative studies investigated electronic referrals. Data collected largely represented measures of provider satisfaction and process measures. Few quantitative studies used established models or measures of team coordination or communication.
This study extends the work of others by compiling a comprehensive view of electronic provider‐to‐provider communication. A recent review of devices for clinical communication tells a part of the story,[28] and our review adds a comprehensive, device‐agnostic look at the systems physicians and other providers use every day.
Limitations of this review include the small number of eligible studies and a homogenous provider type (physicians). The latter is both an important finding and a limitation to generalizability of our results. Reviewed studies were in English only. The literature review by its nature is subject to publication bias.
Intra‐EHR communication cannot serve all purposes, and is it not a panacea for effective care coordination. One recent qualitative study warns about the pitfalls of electronic communication. Interviews with physicians from twenty‐six practices elicited some concerns about the resulting decrease in face‐to‐face communication that has resulted from the adoption of electronic communication tools.[32] This finding brings implications: (1) a false sense of security may reduce verbal communications when they are needed mostduring emergencies or when caring for complex patients who require detailed, nuanced discussion; and (2) fewer conversations within a practice can reduce both knowledge sharing and basic social interactions necessary for the maintenance of a collaboration. Last, privacy and confidentiality are top priorities. Common electronic communication tools are susceptible to security breaches,[47, 59] and innovations within this domain must conform to Health Insurance Portability and Accountability Act of 1996 and Health Information Technology for Economic and Clinical Health Act regulations.[60]
Although electronic communication is not a complete solution for clinical collaboration, it is difficult to use face‐to‐face communication and telephone communication to convey large amounts of patient information while simultaneously generating a record of the transaction. Moreover, paging functions, telephone calls, and face‐to‐face encounters can be highly interruptive, increasing cognitive load, burdening working memory, and shifting attention from the task at hand.[14] Interruptions contribute to inefficiency and to the potential for errors.[61]
Effective coordination of care for the chronically ill is one of the essential goals of the health system; it is an ongoing process that depends on constant, effective communication. Bates and Bitton have recognized this and described the crucial role that HIT will play in creating an effective medical home by enumerating seven domains of HIT especially in need of research.[62] In particular, they note that effective team care and care transitions will depend on an EHR that promotes both implicit and real‐time communication: it will be essential to develop communication tools that allow practices to record goals shared by providers and patients alike, and to track medical interventions and progress.[62]
Future research could investigate a number of open questions. Overall, an emphasis should be placed on rigorous qualitative and quantitative evaluation of electronic communication. Process measures, such as length of stay, hospital readmission rates, and measures of care coordination, should be framed ultimately with respect to patient health outcomes. Such data are beginning to be reported.[63]
It is unclear which types of communications would be best served within the EHR and which should remain external to it. Instant communication or chat has not been studied sufficiently to show a demonstrable impact on patient care. Cross‐coverage and team identification within the EHR can be further studied with respect to workflows and best practices. Studies using structured observation or time‐and‐motion analysis could provide insight into use cases and workflows that providers implement to discuss patients. Future research should incorporate established models of communication[5] and coordination.[64] Data on unintended consequences or harms of provider‐to‐provider electronic communication have been limited, and this area should be considered in subsequent work. Finally, although the scope of this review focused on communication between providers, transformative electronic communication systems should bridge communication gaps between providers and patients as well.
As adoption of EHRs in US hospitals has increased from 15.1% of US hospitals in 2010 to 26.6% in 2011 for any type of EHR and 3.6% to 8.7% for comprehensive EHRs,[65] it is worth noting that Meaningful Use, as it stands, incentivizes patient‐provider communication, but not communication between providers. Inclusion of certification criteria focused on provider‐to‐provider communication may spur additional innovation.
CONCLUSIONS
The optimal features to support electronic communication between providers remain under‐assessed, although there is preliminary evidence for the acceptability of electronic referrals. Without better understanding of electronic communication on workflow, provider satisfaction, and patient outcomes, the impact of such tools on coordination of complex medical care will be an open question, and it remains an important one to answer.
Acknowledgments
The authors would like to express their gratitude to Dr. Thomas Payne, Medical Director of IT Services at the University of Washington, for sharing his expertise, and to Marina Chilov, medical librarian at Columbia University, for her assistance with the literature search. The authors would like to thank Paul Sun, MA, for his assistance with the literature review.
Disclosures: This work was funded by 5K22LM8805 (PDS) and T15 LM007079 (CW, SC) grants. Dr. Stetson serves on the advisory board of the Allscripts Enterprise EHR.
INTRODUCTION
Coordination of care within a practice, during transitions of care, and between primary and specialty care teams requires more than data exchange; it requires effective communication among healthcare providers.[1, 2, 3] In clinical terms, data exchange, communication, and care coordination are related, but they represent distinct concepts.[4] Data exchange refers to transfer of information between settings, independent of the individuals involved, whereas communication is the multistep process that enables information exchange between two people.[5] Care coordination, as defined by O'Malley, is integration of care in consultation with patients, their families and caregivers across all of a patient's conditions, needs, clinicians and settings.[3]
Strong collaboration among providers has been associated with improved patient outcomes.[2, 6] Yet, despite the significant role of communication in healthcare, communication may not take place at all, even at high‐stakes events like transitions of care,[7, 8] or it may be done poorly at the risk of substantial clinical morbidity and mortality.[9, 10, 11, 12, 13, 14, 15, 16]
Proof of the global effectiveness of health information technology (HIT) to improve patient care is lacking, but data from some studies demonstrate real improvements in quality and safety in specific areas,[17, 18, 19] especially with computerized physician order entry[20] and electronic prescribing.[21]
The limited information about the effect of HIT on communication focuses largely on the anticipated improvements in patient‐physician communication[22, 23, 24, 25, 26, 27]; provider‐to‐provider communication within the electronic domain is not as well understood. A recent review of interventions involving communication devices such as pagers and mobile phones found limited high‐quality evidence in the literature.[28] Clinicians have described what they consider to be key characteristics of clinical electronic communications systems such as security/reliability, cross coverage, overall convenience, and message prioritization.[29] Although the electronic health record (EHR) is expected to assist with this communication,[30] it also has the potential to impede effective communication, leading physicians to resort to more traditional workarounds.[31, 32, 33]
Measuring and improving the use of EHRs nationally were driving forces behind the creation of the Meaningful Use incentive program in the United States.[34] To receive the incentive payments, providers must meet and report on a series of measures set in three stages over the course of five years.[35] In the current state, Meaningful Use does not reward provider‐to‐provider communication within the EHR.[36, 37] The main communication objectives for stages 1 and 2 concentrate on patient‐to‐provider communication, such as patient portals and patient‐to‐provider messaging.[36, 37]
Understanding the current evidence for provider‐to‐provider communication within EHRs, its reported effectiveness, and its shortcomings may help to develop a roadmap for identifying next‐generation solutions to support coordination of care.[38, 39] This review assesses the literature regarding provider‐to‐provider electronic communication tools (as supported within or external to an EHR). It is intended as a comprehensive view of studies reporting quantitative measures of the impact of electronic communication on providers and patients.
METHODS
Definitions and Conceptual Model of Provider‐to‐Provider Communication
We conducted a systematic review of studies of provider‐to‐provider electronic communication. This review included only formal clinical communication between providers and was informed by the Coiera communications paradigm.[5] This paradigm consists of four steps: (1) task identification, when a task is identified and associated with the appropriate individual; (2) connection, when an attempt is made to contact that person; (3) communication, when task‐specific information is exchanged between the parties; and (4) disconnection, when the task reaches some stage of completion.
Literature Review
We examined written electronic communication between providers including e‐mail, text messaging, and instant messaging. We did not review provider‐to‐provider telephone or telehealth communication, as these are not generally supported within EHR systems. Communication in all clinical contexts was included among providers within an individual clinic or hospital and among providers across specialties or practice settings.[40] We excluded physician handoff communication because it has been extensively reviewed elsewhere and because handoff occurs largely through verbal exchange not recorded in the EHR.[41, 42] Communication from clinical information systems to providers, such as automated notification of unacknowledged orders, was also excluded, as it is not within the scope of provider‐to‐provider interaction.
Data Sources and Searches
A comprehensive literature search was conducted in Ovid MEDLINE with the input of a medical librarian, and a parallel search was performed using PubMed. The Ovid MEDLINE query and parallel database search terms are documented in Table 1. Subsearches were conducted in Google Scholar, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Academic Search Premier for peer‐reviewed journals. Subsequent studies citing the initially detected articles were found through citation maps.
| Database | Strategy | Items Reviewed |
|---|---|---|
| ||
| Ovid MEDLINE | Query terms: exp medicine/ or physicians or exp outpatient clinics/ or exp hospitals/ AND *communication/ or *computer communication networks/ or *interprofessional relations/ or *continuity of patient care/ AND electronic mail or referral and consultation or text messaging/ or reminder systems. | 1513 |
| PubMed | Healthcare, provider, communication, messaging, e‐mail, texting, text messaging, instant messaging, paging, coordination, referral, EHR, EMR, electronic health record, electronic medical record, electronic, and physician. Excluding patient‐provider and patient‐physician | 340 |
| Google Scholar | Physician‐physician electronic communication excluding physician‐patient | 940 |
| CINAHL | Medical records and communication; or computerized patient records and communication | None |
| Academic Search Premier (peer‐reviewed journals) | Electronic health record and communication | 54 |
| Communication and electronic health record | 80 | |
| Physician‐physician communication | 2 | |
| Physicians and electronic health records | 88 | |
Study Selection
Paper Inclusion Criteria
Requirements included publication in English‐language peer‐reviewed journals. Included studies provided quantitative provider‐to‐provider communication data, provider satisfaction statistics, or EHR communication data. Provider‐to‐staff communication was also included if it fell within the scope of studies of communication between providers.
Paper Exclusion Criteria
Studies excluded in this review were articles that reviewed EHR systems without any focus on communication between providers and those that discussed EHR models and strategies but did not include actual testing and quantitative results. Results that included nontraditional online documents or that were found on nonpeer‐reviewed websites were also discarded. Duplicate records or publications that covered the same study were also removed. The most common reason for exclusion was the lack of quantitative evaluation.
Data Extraction and Quality Assessment
Three authors (Walsh, Siegler, Stetson) reviewed titles and abstracts of resultant studies against inclusion and exclusion criteria (Figure 1). Studies were evaluated qualitatively and findings summarized. Given the heterogeneous nature of data reported, statistical analysis was not possible.
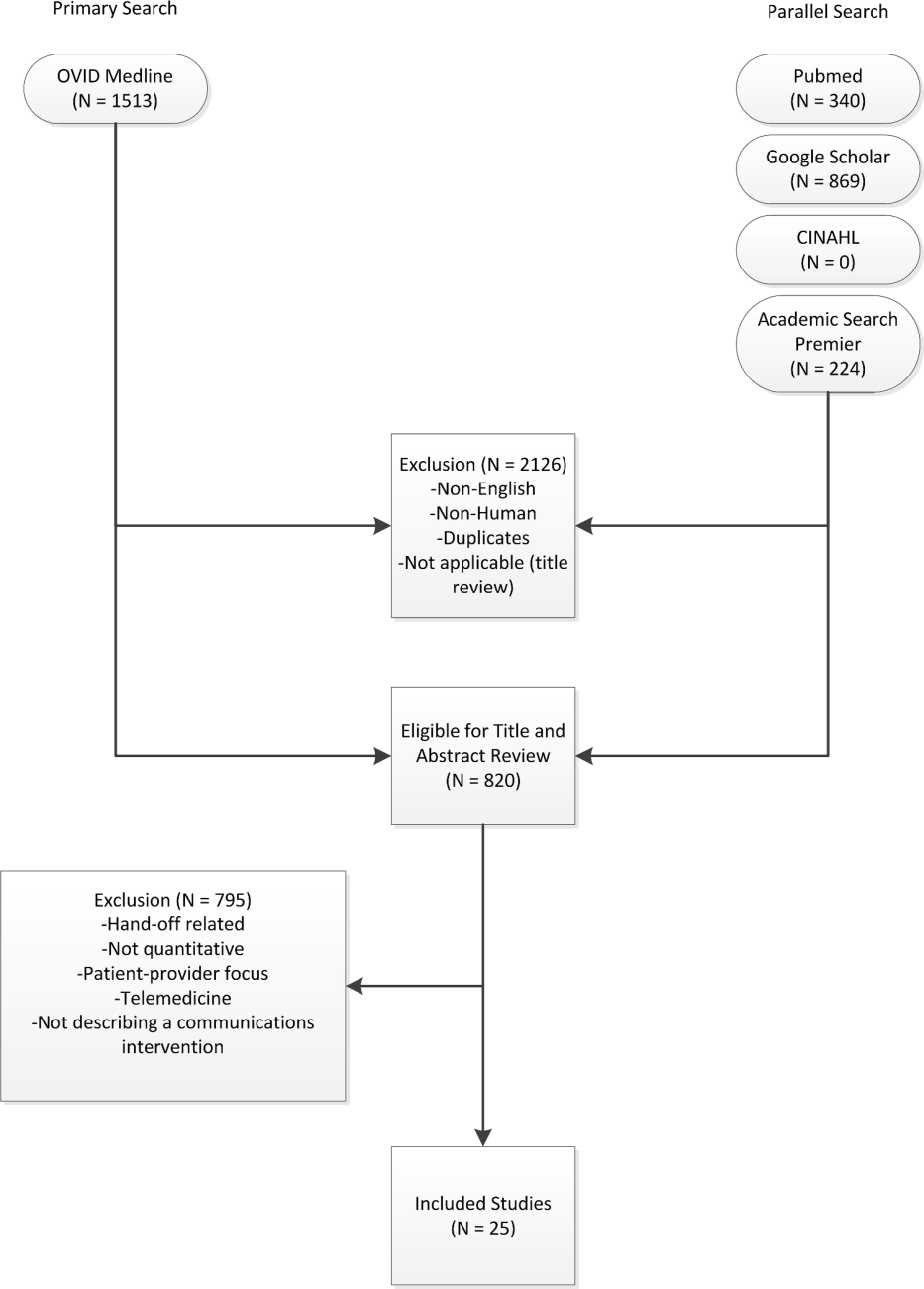
RESULTS
The primary and parallel searches produced 2946 results that were weaned through title review and exclusion of duplicates, nonEnglish‐language, and nonhuman studies to 820 articles for title and abstract review (Figure 1). After careful review of the articles' titles, abstracts, or full content (where appropriate), twenty‐five articles met inclusion criteria and presented data about provider‐to‐provider electronic communication, either within an EHR or through a system designed to promote provider‐to‐provider communication. All of the studies that met inclusion criteria focused on physicians as providers. Five studies (20%) described trial design, three (12%) were pilot studies, and seventeen (68%) were observational studies. Thirteen of twenty‐five articles (52%) described studies conducted in the United States and twelve in Europe.
Most of the studies (56%) focused on electronic referrals between primary care and subspecialty providers. The clinical need was to communicate information on a specific patient with a specialist who shared responsibility for the overall plan of care. Only two studies evaluated curbside consultation, where providers ask for clinical recommendations without formally engaging a specialist in the plan of care for a particular patient. Table 2 summarizes included studies and has been organized with respect to clinical need under evaluation. The major themes that emerged from this review included: studies of penetration of communication tools either within the EHR system (intra‐EHR IT) or external to the EHR (extra‐EHR IT); electronic referrals; curbside consultations; and test results reporting (results notification).
| Primary Author, Year | Design | Intervention | Measurement | Results |
|---|---|---|---|---|
| ||||
| Need: Communicate care across clinical settings (inpatient‐outpatient) | ||||
| Branger, 1992[4, 6] | Observational study | Introduction of electronic messaging system in the Netherlands between hospital and PCPs. | Satisfaction survey data using Likert scale of usefulness. | Free text messaging to exchange patient data was rated very useful or useful by 20 of 27 PCP respondents. |
| Reponen, 2004[66] | Observational study | Finnish study of electronic referrals XML messages between EHRs or secure web links. | User questionnaire. No description of respondents was provided. | Internists surveyed estimated that electronic referrals accelerate the referral process by 1 week. |
| Need: Communicate care across specialties (primary care physicians‐specialists) | ||||
| Kooijman, 1998[67] | Observational study | Survey of 45 PCPs who received notes from specialists via Electronic Data Interchange. | User questionnaire with 5‐point Likert scale of satisfaction, from 1 (much better) to 5 (much worse). | Highest satisfaction scores for speed (1.51.8) and efficiency (1.51.7) for electronic messages, with lower scores for reliability (2.52.7) and clarity (2.5). |
| Harno, 2000[4][8] | Nonrandomized trial | Eight‐month prospective comparative study in Finland of outpatient clinics in hospitals with and without intranet referral systems. | Comparison of numbers of electronic referrals, clinic visits, costs. | There were 43% of electronic referrals and 79% of outpatient referrals that resulted in outpatient visits. A 3‐fold increase in productivity overall and 7‐fold reduction in visit costs per patient using e‐mail consultation. |
| Moorman, 2001[4][7] | Observational study | Supersedes Branger, 1999.[68] Analyzes intra‐EHR communications between PCPs and consultant in Netherlands re: diabetes management of patients (19941998). | Descriptive statistics of number of messages, content, whether message had been copied into EMR; survey of PCPs (12 of 15 responded). | Decline in integration by PCPs of messages in the EHR from 75% to 51% over first 3 years. Despite this, most PCPs wanted to extend messaging to other patient groups. |
| Bergus, 2006[69] | Observational study | Follow‐up of Bergus, 1998[54]; evaluated formulation of clinical referrals to specialists at the University of Iowa by retrospective review of e‐mail transcripts. | Analyzed taxonomy of clinical questions; assessed need for clinical consultation of 1618 clinical questions. | Specialists less likely to recommend clinic consultation if referral specified the clinical task (OR: 0.36, P0.001), intervention (OR: 0.62, P=0.004), or outcome (OR: 0.49, P0.001). This effect was independent of clinical content (P>0.05). |
| Dennison, 2006[70] | Pilot study | Construction of an electronic referral pro forma to facilitate referral of patients to colorectal surgeons. | Descriptive statistics. Comparisons of patient attendance rate, delays to booking and to actual appointment between 54 electronic referrals and 189 paper referrals. | Compared to paper referrals, electronic referrals were booked more quickly (same day vs 1 week later on average) and patients had lower nonattendance rates (8.5% vs 22.5%). Both results stated as statistically significant, but P values were not provided. |
| Shaw, 2007[49] | Observational study | Dermatology electronic referral in England. | Content of 131 electronic vs 139 paper referrals to dermatologists(NHS Choose and Book).[71] | Paper superior to electronic for clinical data such as current treatments (included in 68% of paper vs 39% of electronic referrals, P0.001); electronic superior for demographic data. |
| Gandhi, 2008[50] | Nonrandomized trial | Electronic referral tool in the Partners Healthcare System in Massachusetts that included a structured referral‐letter generator and referral status tracker. Assigned to 1 intervention site and 1 control site. | Survey assessment. Fifty‐four of 117 PCPs responded (46%), 235 of 430 specialists responded (55%), 143 out of 210 patients responded (69%). | Intervention group showed high voluntary adoption (99%), higher information transfer rates prior to subspecialty visit (62% vs 12%), and lower rates of conflicting information being given to patients (6% vs 20%). |
| John, 2008[72] | Pilot study | Validation study of the Lower Gastrointestinal e‐RP (through the Choose and Book System in the United Kingdom) intended to improve yield of colon cancers diagnosed and to reduce delays in diagnosis. | Comparison of actual to simulated referral patterns through e‐RP for 300 patients divided into colorectal cancer, 2‐week wait suspected cancer, and routine referral groups. | e‐RP was more accurate than traditional referral at upgrading patients who had cancer to the appropriate suspected cancer referral group (85% vs 43%, P=0.002). |
| Kim, 2009[73] | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Included reply functionality and ability to forward messaging to a scheduler for calendaring. | Impact of electronic referral system as measured by questionnaire to referring providers. A total of 298/368 participated (24 clinics); 53.5% attending physicians. | Electronic referrals improved overall quality of care (reported by 72%), guidance of presubspecialty visit (73%), and the ability to track referrals (89%). Small change in access for urgent issues (35% better, 49% reported no change). |
| Scott, 2009[74] | Pilot study | Pilot of urgent electronic referral system from PCPs to oncologists at South West Wales Cancer Centre. | Satisfaction statistics (10‐point Likert scale) collected from PCPs via interview. | Over 6 months, 99 referrals submitted; 81% were processed within 1 hour with high satisfaction scores. |
| Were, 2009[75] | Nonrandomized trial | Geriatrics consultants were provided system to make electronic recommendations (consultant‐recommended orders) in the native CPOE system along with consult notes in the intervention vs consult notes alone in the control. | Rates of implementation of consultant recommendations. Qualitative survey of users of the new system. | Higher total number of recommendations (247 vs 192, P0.05) and higher implementation rates of consultant‐recommended orders in the intervention group vs control (78% vs 59%, P=0.01). High satisfaction scores on 5‐point Likert scale for the intervention system with good survey response rate (83%). |
| Dixon, 2010[52] | Observational study | Comparison of 2 extra‐EHR systems (NHS Choose and Book, Dutch ZorgDomein) for booking referrals. Patients choose doctor or hospital and the system transfers demographic and clinical information between PCP and specialist. | National data, patient and provider surveys, focus groups, observational studies. Focus was on patient choice, but evaluations included all aspects of the systems. | Resistance from PCPs during implementation; 78% of ZorgDomein PCPs felt referrals took more time; general displeasure on the part of specialists re: quality of referrals, although not quantified. |
| Patterson, 2010[51] | Observational study | E‐mail referral system to a neurologist in Northern Ireland. Referrals were template based and recorded as clinical episode in the patient administration system. Comparison of this system to conventional referrals to another neurologist. | Evaluated effectiveness, cost, safety for period 20022007. | Decreased referral wait times (4 vs 13 weeks) and 35% cost reduction per patient for the e‐mail referral vs conventional referrals. |
| No diminution in safety. Limitation: single neurologist participated. | ||||
| Singh, 2011[76] | Observational study | Chart review of electronic referrals to specialist practices in a Veterans Affairs outpatient system. | Follow‐up actions taken by subspecialists within 30 days of receiving referral. | An intra‐EHR referral system was still affected by communication breakdowns. Of 61,931 referrals, 36.4% were discontinued for inappropriate or incomplete referral requests. |
| Kim‐Hwang, 2010[77] | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Follow‐up to Kim, 2009.[73] | Survey of medical and surgical subspecialty consultants. | Statistically significant differences in clarity of consult request in both medical and surgical clinics, in decreased inappropriate referrals in surgical clinics, in decreased use of follow‐up appointments by surgical specialists, and in decreased avoidable follow‐up surgical visits. |
| Warren, 2011[53] | Observational study | Electronic referrals from general medical practices to public referral network of Hutt Hospital in New Zealand (20072010). | Retrospective analysis of transactional data from messaging system and from general inpatient tracking system. Qualitative data collection via interviews. | Estimated 71% of 10,367 referrals were electronic referrals over 3 years. Statistically significant improvement in referral latency without change in staffing. Clinicians appreciate shared transparency of referrals but cite usability issues as barriers. |
| Need: Curbside consults (primary care physicians‐specialists) | ||||
| Bergus, 1998[54] | Observational study | Evaluation of the ECS for curbside consultations between family physicians and subspecialists. | Descriptive statistics of usage data; survey of users. | Median response time 16.1 hours; 92% of questions answered; almost 90% concerned specific patients. Both groups expressed satisfaction. |
| Abbott, 2002[55] | Observational study | Evaluation of Department of Defense Ask a Doc physician‐to‐physicians e‐mail consultation system over network of 21 states (19982000). | Descriptive statistics; qualitative assessment. | There were 3121 consultations. Average response time 12 hours. Minimal cost and effort to initiate and sustain. Felt to mirror clinical practice. Barriers were security and assignation of credit for consultation. |
| Need: Communication of results (primary care physicians ‐specialists) | ||||
| Singh, 2007[5][6] | Nonrandomized trial | Concurrent prospective evaluation of responses to 1017 critical imaging alert notifications in a Veterans Affairs outpatient system (2006). Radiologists generated alerts. Included receipt system. | Measured percentage of unacknowledged alerts and imaging lost to follow‐up. | There were 368 of 1017 transmitted alerts unacknowledged (36%); 45 were completely lost to follow‐up. There were 0.2% outpatient imaging results lost to follow‐up overall. |
| Singh, 2009[5][7] | Nonrandomized trial | Concurrent evaluation of responses to 1196 critical imaging alert notifications in a Veterans Affairs outpatient system (20072008). Similar coding system to Singh, 2007.[56] | Measured percentage of alerts acknowledged, timely follow‐up; compared electronic alerts alone to combination of alerts and phone calls or admission. | Percentage of alerts acknowledged did not differ by type of communication; combination of electronic alerts with phone follow‐up (OR: 0.12, P0.001) or admission (OR: 0.22, P0.001) decreased likelihood of delayed follow‐up. Alerts to 2 providers increased the likelihood of delayed follow‐up (OR: 1.99, P=0.03). |
| Abujudeh, 2009[5][8] | Observational study | Retrospective review of e‐mailbased alert system for abnormal imaging results at Massachusetts General Hospital 20052007. E‐mail alerting by radiologist to ordering physician of nonurgent findings. | Descriptive statistics; survey of referring physicians (12/26). | There were 56,691 out of 1,540,254 reports for important but not urgent findings; 93.3% generated e‐mail message (6.7% failure rate); 80% of alerts were viewed. Higher satisfaction for e‐mail alerts over conventional methods (eg, facsimile) for nonurgent but important findings. |
| Need: Communicate within 1 care setting (primary care physicians) | ||||
| Lanham, 2012[78] | Observational study | Comparison of practice‐level EHR use with communication patterns among physicians, nurses, medical assistants, practice managers, and nonclinical staff within individual practices in Texas. | Observation and semistructured interviews. Within‐practice communication patterns were categorized as fragmented or cohesive. Practice‐level EHR use was categorized as homogeneous or heterogeneous. | Clinical practices with cohesive within‐practice communication patterns were associated with homogeneous patterns of practice‐level EHR use. |
| Murphy, 2012[79] | Observational study | Review of note‐based messaging within the EHR in outpatient clinics of large tertiary Veterans Affairs facility. Clinic staff send additional signature request alerts linked to parent notes in the EHR to primary care physicians. | Reason for and origin of alerts. Parent note linked to alert was also reviewed for 3 value attributes: urgency; potential harm if alert was missed; subjective value to PCP of the alert. | Of the alerts reviewed, 53.7% of 525 were deemed of high value but required PCPs to review significant amounts of extraneous text (80.3% of words in parent notes) to get relevant information. Most alerts (40%) were medication, prescription, or refill related. |
Extra‐EHR IT
A review of electronic communication in 2000 examined electronic communication among primary care physicians but notably did not distinguish between communication and data exchange.[43] Of the thirty included publications in that review, seventeen publications dealt with electronically communicated information in general; the remaining studies focused on notifications of test results or transitions of care, reports from specialists, or electronic communication as replacement of traditional referral.[43] Although many studies of electronic communication described positive benefits, few included objective data, and most did not analyze provider‐to‐provider communication specifically. A survey of IT use outside of the EHR in 2006 documented that approximately 30% of clinicians used e‐mail to communicate with other clinicians, fewer than those who consulted on‐line journals (40.8%), but many more than those who communicated with patients by e‐mail at that time (3.6%).[44]
Intra‐EHR IT
A comparison of two physician surveys of EHR use in Massachusetts (the first in 2005 and the second in 2007) documented an increase in the percentage of practices with an EHR, from 23% to 35%; in those practices with EHRs, only the use of electronic prescribing increased over time. Use of secure electronic referrals or messaging including secure e‐mail remained unchanged; of note, referrals and messaging were considered a singular clinical function in that study. Between 2005 and 2007, referrals or clinical messaging were available in 62% and 63% of EHR systems, respectively, and they were used most or all of the time by 29% to 33% of the physicians who had an EHR.[45]
Electronic Referrals
Fourteen articles focused on electronic referrals. Two had a prepost or longitudinal study design,[46, 47] and five included a control group.[48, 49, 50, 51] The rest were descriptive. In most cases, electronic referral improved the transfer of information, especially when standardized message templates were created. Use of electronic referral appeared to result in reduced waiting time for appointments and enabled more efficient triage.
Barriers to integration of electronic referral in the EHR were also assessed. An intra‐EHR communication system requiring a primary care physician to integrate information e‐mailed by the consultant into the record showed the percentage of integrated notes decreasing over time.[47] Practitioners had mixed feelings about the system; although the majority (92% of respondents) felt that the system improved patient care and wanted to extend messaging to other patient groups, they also felt that electronic messaging decreased the ease of reviewing data (83%) and confused tasks and responsibilities (59%). A study of British and Dutch electronic referral systems described significant resistance on the part of practitioners to electronic referrals and concern on the part of specialists about the quality of referrals.[52] Another study demonstrated improvement in quality of demographic data but degradation in quality of clinical information when referrals were submitted electronically.[49] A recent transactional analysis of electronic referrals in New Zealand showed high uptake and reduced referral latency compared to conventional referral; clinicians cited usability concerns as the major barrier to use.[53]
Curbside Consultations via E‐mail
Two studies evaluated curbside consultations via e‐mail and documented high provider satisfaction and rapid turnaround.[54, 55] The preliminary nature of these studies raises questions of sustainability and long‐term implementation.
Results Notification
Three studies focused on test‐result reporting from radiologists. In these studies, a radiologist could designate a result as high priority and have an e‐mail notification sent to the ordering physicians.[56, 57, 58] Urgent results were relayed by telephone. Lack of acknowledgement of alerts impacted the results of every study, and in one of these studies, alerting two physicians, rather than just one, decreased the likelihood that the results would be followed up.[57] Providers did prefer e‐mail to fax notification.[58]
DISCUSSION
The principal findings of the literature review demonstrate the paucity of quantitative data surrounding provider‐to‐provider communication. The majority of studies focused on physicians as providers without emphasis on other provider types on the care team. Most of the quantitative studies investigated electronic referrals. Data collected largely represented measures of provider satisfaction and process measures. Few quantitative studies used established models or measures of team coordination or communication.
This study extends the work of others by compiling a comprehensive view of electronic provider‐to‐provider communication. A recent review of devices for clinical communication tells a part of the story,[28] and our review adds a comprehensive, device‐agnostic look at the systems physicians and other providers use every day.
Limitations of this review include the small number of eligible studies and a homogenous provider type (physicians). The latter is both an important finding and a limitation to generalizability of our results. Reviewed studies were in English only. The literature review by its nature is subject to publication bias.
Intra‐EHR communication cannot serve all purposes, and is it not a panacea for effective care coordination. One recent qualitative study warns about the pitfalls of electronic communication. Interviews with physicians from twenty‐six practices elicited some concerns about the resulting decrease in face‐to‐face communication that has resulted from the adoption of electronic communication tools.[32] This finding brings implications: (1) a false sense of security may reduce verbal communications when they are needed mostduring emergencies or when caring for complex patients who require detailed, nuanced discussion; and (2) fewer conversations within a practice can reduce both knowledge sharing and basic social interactions necessary for the maintenance of a collaboration. Last, privacy and confidentiality are top priorities. Common electronic communication tools are susceptible to security breaches,[47, 59] and innovations within this domain must conform to Health Insurance Portability and Accountability Act of 1996 and Health Information Technology for Economic and Clinical Health Act regulations.[60]
Although electronic communication is not a complete solution for clinical collaboration, it is difficult to use face‐to‐face communication and telephone communication to convey large amounts of patient information while simultaneously generating a record of the transaction. Moreover, paging functions, telephone calls, and face‐to‐face encounters can be highly interruptive, increasing cognitive load, burdening working memory, and shifting attention from the task at hand.[14] Interruptions contribute to inefficiency and to the potential for errors.[61]
Effective coordination of care for the chronically ill is one of the essential goals of the health system; it is an ongoing process that depends on constant, effective communication. Bates and Bitton have recognized this and described the crucial role that HIT will play in creating an effective medical home by enumerating seven domains of HIT especially in need of research.[62] In particular, they note that effective team care and care transitions will depend on an EHR that promotes both implicit and real‐time communication: it will be essential to develop communication tools that allow practices to record goals shared by providers and patients alike, and to track medical interventions and progress.[62]
Future research could investigate a number of open questions. Overall, an emphasis should be placed on rigorous qualitative and quantitative evaluation of electronic communication. Process measures, such as length of stay, hospital readmission rates, and measures of care coordination, should be framed ultimately with respect to patient health outcomes. Such data are beginning to be reported.[63]
It is unclear which types of communications would be best served within the EHR and which should remain external to it. Instant communication or chat has not been studied sufficiently to show a demonstrable impact on patient care. Cross‐coverage and team identification within the EHR can be further studied with respect to workflows and best practices. Studies using structured observation or time‐and‐motion analysis could provide insight into use cases and workflows that providers implement to discuss patients. Future research should incorporate established models of communication[5] and coordination.[64] Data on unintended consequences or harms of provider‐to‐provider electronic communication have been limited, and this area should be considered in subsequent work. Finally, although the scope of this review focused on communication between providers, transformative electronic communication systems should bridge communication gaps between providers and patients as well.
As adoption of EHRs in US hospitals has increased from 15.1% of US hospitals in 2010 to 26.6% in 2011 for any type of EHR and 3.6% to 8.7% for comprehensive EHRs,[65] it is worth noting that Meaningful Use, as it stands, incentivizes patient‐provider communication, but not communication between providers. Inclusion of certification criteria focused on provider‐to‐provider communication may spur additional innovation.
CONCLUSIONS
The optimal features to support electronic communication between providers remain under‐assessed, although there is preliminary evidence for the acceptability of electronic referrals. Without better understanding of electronic communication on workflow, provider satisfaction, and patient outcomes, the impact of such tools on coordination of complex medical care will be an open question, and it remains an important one to answer.
Acknowledgments
The authors would like to express their gratitude to Dr. Thomas Payne, Medical Director of IT Services at the University of Washington, for sharing his expertise, and to Marina Chilov, medical librarian at Columbia University, for her assistance with the literature search. The authors would like to thank Paul Sun, MA, for his assistance with the literature review.
Disclosures: This work was funded by 5K22LM8805 (PDS) and T15 LM007079 (CW, SC) grants. Dr. Stetson serves on the advisory board of the Allscripts Enterprise EHR.
- , . Physician‐physician communication: what's the hang‐up? J Gen Intern Med. 2009;24:437–439.
- , , , et al. Meta‐analysis: effect of interactive communication between collaborating primary care physicians and specialists. Ann Intern Med. 2010;152(4):247–258.
- , , , , . Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2009;25:177–185.
- , , , , , . Development of an ontology to model medical errors, information needs, and the clinical communication space. Proc AMIA Symp. 2001:672–676.
- . Clinical communication: a new informatics paradigm. Proc AMIA Annu Fall Symp. 1996:17–21.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):CD000072.
- , , , . Primary care physician attitudes regarding communication with hospitalists. Dis Mon. 2002;48(4):218–229.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280(15):1311–1316.
- , , , . Analysing potential harm in Australian general practice: an incident‐monitoring study. J Am Med Inform Assoc. 1998;169:73–76.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , , . Communication loads on clinical staff in the emergency department. J Am Med Inform Assoc. 2002;176(9):415–418.
- , , , , , . Deficit in communicaiton and information transfer between hospital‐based and primary care physicians. JAMA. 2007;297:831–841.
- , . Improving clinical communication: a view from psychology. J Am Med Inform Assoc. 2000;7(5):453–461.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , , , , . The Quality in Australian Health Care Study. Med J Aust. 1995;163:458–471.
- , , , et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752.
- , , . Costs and benefits of health information technology. Evid Rep Technol Assess. 2006;132:1–71.
- , , , et al. Relationship between use of electronic health record features and health care quality: results of a statewide survey. Med Care. 2010;48:203–209.
- , , , et al. Decrease in hospital‐wide mortality rate after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2010;126:e1–e8.
- , , , , . Electronic prescribing improves medication safety in community‐based office practices. J Gen Intern Med. 2010;25:530–536.
- . Patient‐centered Care. Radiol Technol. 2009;81(2):133–147.
- , . The missing link: bridging the patient‐provider health information gap. Health Aff (Millwood). 2005;24(5):1290–1295.
- , , , , . Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126.
- , . Web messaging: a new tool for patient‐physician communication. J Am Med Inform Assoc. 2003;10(3):260–270.
- , , , . Expanding the guidelines for electronic communication with patients. J Am Med Inform Assoc. 2001;8(4):344–348.
- , , , . The utility of electronic mail as a medium for patient‐physician communication. Arch Fam Med. 1994;3(3):268–271.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , . Desiderata for personal electronic communication in clinical systems. J Am Med Inform Assoc. 2002;9(3):209–216.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7:277–286.
- . Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25:174–176.
- , , . Electronic medical records and communication with patients and other clinicians: are we talking less? Issue Brief Cent Stud Health Syst Change. 2010;(131):1–4.
- , . Referral and consultation communication between primary care and specialist physicians: finding common ground. Arch Intern Med. 2011;171(1):56–65.
- , . The "meaningful use" regulation for electronic health records. N Engl J Med. 2010;363(6):501–504.
- Centers for Medicare 25(3):177–185.
- . Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25(3):174–176.
- , , , . A framework for clinical communication supporting healthcare delivery. AMIA Annu Symp Proc. 2005:375–379.
- Understanding and improving patient handoffs. Jt Comm J Qual Improv. 2010:49–96.
- , , , . Signout: a collaborative document with implications for the future of clinical information systems. AMIA Annu Symp Proc. 2007:696–700.
- , , . Effects of electronic communication in general practice. Int J Med Inform. 2000;60(1):59–70.
- , , , , . Prevalence of basic information technology use by U.S. physicians. J Gen Intern Med. 2006;21:1150–1155.
- , , , et al. Physicians' use of key functions in electronic health records from 2005 to 2007: a statewide survey. J Am Med Inform Assoc. 2009;16:465–470.
- , , , et al. Electronic communication between providers of primary and secondary care. BMJ. 1992;305(6861):1068–1070.
- , , , . Electronic messaging between primary and secondary care: a four‐year case report. J Am Med Inform Assoc. 2001;8(4):372–378.
- , , , . Patient referral by telemedicine: effectiveness and cost anslysis of an intranet system. J Telemed Telecare. 2000;6(6):320–329.
- , . Strengths and weaknesses of electronic referral: comparison of data content and clinical value of electronic and paper referrals in dermatology. Br J Gen Pract. 2007;57(536):223–224.
- , , , et al. Improving referral communication using a referral tool within an electronic medical record. In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches. Vol. 3. Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality; 2008:63–74.
- , , , . Email triage is an effective, efficient, and safe way of managing new referrals to a neurologist. Qual Safety Health Care. 2010;19(5):e51.
- , , . The experience of implementing choice at point of referral: a comparison of the Netherlands and England. Health Econ Policy Law. 2010;13:1–23.
- , , , , . Introduction of electronic referral from community associated with more timely review by secondary services. Appl Clin Inform. 2011;2(4):546–564.
- , , , . Use of an e‐mail curbside consultation service by family physicians. J Fam Pract. 1998;47:357–360.
- , , , , , . Physician‐to‐physician consultation via electronic mail: the Walter Reed Army Medical Center Ask a Doc system. Mil Med. 2002;167:200–204.
- , , , , , . Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459–466.
- , , , et al. Timely follow‐up of abnormal diagnostic imaging test results in an outpatient setting: are electronic medical records achieving their potential? Arch of Intern Med. 2009;169(17):1578–1586.
- , , , , . Important imaging finding e‐mail alert system: experience after 3 years of implementation. Radiology. 2009;252:747–753.
- . Instant insecurity: security issues of instant messaging. Symantec website. Available at: http://www.symantec.com/connect/articles/instant‐insecurity‐security‐issues‐instant‐messaging.
- . Secure messaging in healthcare. Tech solutions for HIPAA‐compliant messaging. J AHIMA. 2008;79(6):50–51.
- , , , , . Association of interruptions with an increased risk and severity of medication administration errors. Arch Intern Med. 2010;170(8):683–690.
- , . The future of health information technology in the patient‐centered medical home. Health Aff (Millwood). 2010;29(4):614–621.
- , , . eReferral—a new model for integrated care. N Engl J Med. 2013;368(26):2450–2453.
- , , , et al. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. Vol 7. Care Coordination. Rockville, MD; 2007.
- , , , , . Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff (Millwood). 2012;31(5):1092–1099.
- , , , . Extending a multimedia medical record to a regional service with electronic referral and discharge letters. J Telemed Telecare. 2004;10S:81–83.
- , . Sending specialist reports to GPs using EDI. Stud Health Tech Inform. 1998;52(pt 1):408–411.
- , , , , . Shared care for diabetes: supporting communication between primary and secondary care. Int J Med Inform. 1999;53(2-3):133–142.
- , , , . Email teleconsultations: well formulated clinical referrals reduce the need for clinic consultation. J Telemed Telecare. 2006;12(1):33–38.
- , , , . An effective electronic surgical referral system. Ann R Coll Surg Engl. 2006;88(6):554–556.
- . Choose and book. Clin Med. 2006;6(5):473–476.
- , , , . Validation of the lower gastrointestinal electronic referral protocol. Brit J Surg. 2008;95:506–514.
- , , , , . Not perfect, but better: primary care providers' experiences with electronic referrals in a safety net health system. J Gen Intern Med. 2009;24:614–619.
- . The Swansea electronic referrals project. J Telemed Telecare. 2009;15:156–158.
- , , , , . Using computerized provider order entry and clinical decision support to improve referring physicians' implementation of consultants' medical recommendations. J Am Med Inform Assoc. 2009;16(2):196–202.
- , , , et al. Follow‐up actions on electronic referral communication in a multispecialty outpatient setting. J Gen Intern Med. 2011;26(1):64–69.
- , , , , , . Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med. 2010;25(10):1123–11028.
- , , . Same organization, same electronic health records (EHRs) system, different use: exploring the linkage between practice member communication patterns and EHR use patterns in an ambulatory care setting. J Am Med Inform Assoc. 2012;19(3):382–391.
- , , , et al. Electronic health record‐based messages to primary care providers: valuable information or just noise? Arch Intern Med. 2012;172(3):283–285.
- , . Physician‐physician communication: what's the hang‐up? J Gen Intern Med. 2009;24:437–439.
- , , , et al. Meta‐analysis: effect of interactive communication between collaborating primary care physicians and specialists. Ann Intern Med. 2010;152(4):247–258.
- , , , , . Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2009;25:177–185.
- , , , , , . Development of an ontology to model medical errors, information needs, and the clinical communication space. Proc AMIA Symp. 2001:672–676.
- . Clinical communication: a new informatics paradigm. Proc AMIA Annu Fall Symp. 1996:17–21.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):CD000072.
- , , , . Primary care physician attitudes regarding communication with hospitalists. Dis Mon. 2002;48(4):218–229.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280(15):1311–1316.
- , , , . Analysing potential harm in Australian general practice: an incident‐monitoring study. J Am Med Inform Assoc. 1998;169:73–76.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , , . Communication loads on clinical staff in the emergency department. J Am Med Inform Assoc. 2002;176(9):415–418.
- , , , , , . Deficit in communicaiton and information transfer between hospital‐based and primary care physicians. JAMA. 2007;297:831–841.
- , . Improving clinical communication: a view from psychology. J Am Med Inform Assoc. 2000;7(5):453–461.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , , , , . The Quality in Australian Health Care Study. Med J Aust. 1995;163:458–471.
- , , , et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752.
- , , . Costs and benefits of health information technology. Evid Rep Technol Assess. 2006;132:1–71.
- , , , et al. Relationship between use of electronic health record features and health care quality: results of a statewide survey. Med Care. 2010;48:203–209.
- , , , et al. Decrease in hospital‐wide mortality rate after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2010;126:e1–e8.
- , , , , . Electronic prescribing improves medication safety in community‐based office practices. J Gen Intern Med. 2010;25:530–536.
- . Patient‐centered Care. Radiol Technol. 2009;81(2):133–147.
- , . The missing link: bridging the patient‐provider health information gap. Health Aff (Millwood). 2005;24(5):1290–1295.
- , , , , . Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126.
- , . Web messaging: a new tool for patient‐physician communication. J Am Med Inform Assoc. 2003;10(3):260–270.
- , , , . Expanding the guidelines for electronic communication with patients. J Am Med Inform Assoc. 2001;8(4):344–348.
- , , , . The utility of electronic mail as a medium for patient‐physician communication. Arch Fam Med. 1994;3(3):268–271.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , . Desiderata for personal electronic communication in clinical systems. J Am Med Inform Assoc. 2002;9(3):209–216.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7:277–286.
- . Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25:174–176.
- , , . Electronic medical records and communication with patients and other clinicians: are we talking less? Issue Brief Cent Stud Health Syst Change. 2010;(131):1–4.
- , . Referral and consultation communication between primary care and specialist physicians: finding common ground. Arch Intern Med. 2011;171(1):56–65.
- , . The "meaningful use" regulation for electronic health records. N Engl J Med. 2010;363(6):501–504.
- Centers for Medicare 25(3):177–185.
- . Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25(3):174–176.
- , , , . A framework for clinical communication supporting healthcare delivery. AMIA Annu Symp Proc. 2005:375–379.
- Understanding and improving patient handoffs. Jt Comm J Qual Improv. 2010:49–96.
- , , , . Signout: a collaborative document with implications for the future of clinical information systems. AMIA Annu Symp Proc. 2007:696–700.
- , , . Effects of electronic communication in general practice. Int J Med Inform. 2000;60(1):59–70.
- , , , , . Prevalence of basic information technology use by U.S. physicians. J Gen Intern Med. 2006;21:1150–1155.
- , , , et al. Physicians' use of key functions in electronic health records from 2005 to 2007: a statewide survey. J Am Med Inform Assoc. 2009;16:465–470.
- , , , et al. Electronic communication between providers of primary and secondary care. BMJ. 1992;305(6861):1068–1070.
- , , , . Electronic messaging between primary and secondary care: a four‐year case report. J Am Med Inform Assoc. 2001;8(4):372–378.
- , , , . Patient referral by telemedicine: effectiveness and cost anslysis of an intranet system. J Telemed Telecare. 2000;6(6):320–329.
- , . Strengths and weaknesses of electronic referral: comparison of data content and clinical value of electronic and paper referrals in dermatology. Br J Gen Pract. 2007;57(536):223–224.
- , , , et al. Improving referral communication using a referral tool within an electronic medical record. In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches. Vol. 3. Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality; 2008:63–74.
- , , , . Email triage is an effective, efficient, and safe way of managing new referrals to a neurologist. Qual Safety Health Care. 2010;19(5):e51.
- , , . The experience of implementing choice at point of referral: a comparison of the Netherlands and England. Health Econ Policy Law. 2010;13:1–23.
- , , , , . Introduction of electronic referral from community associated with more timely review by secondary services. Appl Clin Inform. 2011;2(4):546–564.
- , , , . Use of an e‐mail curbside consultation service by family physicians. J Fam Pract. 1998;47:357–360.
- , , , , , . Physician‐to‐physician consultation via electronic mail: the Walter Reed Army Medical Center Ask a Doc system. Mil Med. 2002;167:200–204.
- , , , , , . Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459–466.
- , , , et al. Timely follow‐up of abnormal diagnostic imaging test results in an outpatient setting: are electronic medical records achieving their potential? Arch of Intern Med. 2009;169(17):1578–1586.
- , , , , . Important imaging finding e‐mail alert system: experience after 3 years of implementation. Radiology. 2009;252:747–753.
- . Instant insecurity: security issues of instant messaging. Symantec website. Available at: http://www.symantec.com/connect/articles/instant‐insecurity‐security‐issues‐instant‐messaging.
- . Secure messaging in healthcare. Tech solutions for HIPAA‐compliant messaging. J AHIMA. 2008;79(6):50–51.
- , , , , . Association of interruptions with an increased risk and severity of medication administration errors. Arch Intern Med. 2010;170(8):683–690.
- , . The future of health information technology in the patient‐centered medical home. Health Aff (Millwood). 2010;29(4):614–621.
- , , . eReferral—a new model for integrated care. N Engl J Med. 2013;368(26):2450–2453.
- , , , et al. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. Vol 7. Care Coordination. Rockville, MD; 2007.
- , , , , . Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff (Millwood). 2012;31(5):1092–1099.
- , , , . Extending a multimedia medical record to a regional service with electronic referral and discharge letters. J Telemed Telecare. 2004;10S:81–83.
- , . Sending specialist reports to GPs using EDI. Stud Health Tech Inform. 1998;52(pt 1):408–411.
- , , , , . Shared care for diabetes: supporting communication between primary and secondary care. Int J Med Inform. 1999;53(2-3):133–142.
- , , , . Email teleconsultations: well formulated clinical referrals reduce the need for clinic consultation. J Telemed Telecare. 2006;12(1):33–38.
- , , , . An effective electronic surgical referral system. Ann R Coll Surg Engl. 2006;88(6):554–556.
- . Choose and book. Clin Med. 2006;6(5):473–476.
- , , , . Validation of the lower gastrointestinal electronic referral protocol. Brit J Surg. 2008;95:506–514.
- , , , , . Not perfect, but better: primary care providers' experiences with electronic referrals in a safety net health system. J Gen Intern Med. 2009;24:614–619.
- . The Swansea electronic referrals project. J Telemed Telecare. 2009;15:156–158.
- , , , , . Using computerized provider order entry and clinical decision support to improve referring physicians' implementation of consultants' medical recommendations. J Am Med Inform Assoc. 2009;16(2):196–202.
- , , , et al. Follow‐up actions on electronic referral communication in a multispecialty outpatient setting. J Gen Intern Med. 2011;26(1):64–69.
- , , , , , . Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med. 2010;25(10):1123–11028.
- , , . Same organization, same electronic health records (EHRs) system, different use: exploring the linkage between practice member communication patterns and EHR use patterns in an ambulatory care setting. J Am Med Inform Assoc. 2012;19(3):382–391.
- , , , et al. Electronic health record‐based messages to primary care providers: valuable information or just noise? Arch Intern Med. 2012;172(3):283–285.