User login
Health Care Use Among Iraq and Afghanistan Veterans With Infectious Diseases
In 2010, the VA gave presumptive status to 9 infectious diseases that are endemic to southwest Asia and Afghanistan. This classification relieves the veteran of having to prove that an illness was connected to exposure during service in a specific region. The purpose of this secondary analysis is to determine the impact of the presumptive infectious disease (PID) ruling by the VHA by assessing the pre- and postruling health care use of veterans diagnosed with one of the infectious diseases.
Background
As of December 2012, 1.6 million veterans who served in Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) were eligible to receive VHA care. The number of combat related injuries is commonly released to the public, but figures related to noncombat illnesses, such as infectious diseases, are reported less frequently. Sixteen percent of the 899,752 OEF/OIF/OND veterans who received VHA care through December 2012 were diagnosed with an infectious disease.1
Long-term disability stemming from any type of illness, disease, or injury is potentially compensable through VA disability compensation programs. The disability must be service-connected for a veteran to receive compensation; that is, it must be determined to be a likely by-product of “an illness, disease or injury incurred or aggravated while the soldier was on active military service.”2 The benefit application process takes time, because service connection must be established prior to determining entitlement to disability benefits.2
Congress mandated that the VA determine the illnesses that justified a presumption of service-connection based on exposure to hazards of Iraq and Afghanistan service. In response, the VA requested that the Institute of Medicine (IOM) conduct a review of the scientific and medical literature to determine the diseases related to hazards of service in southwest Asia and Afghanistan.
In a 2006 report, the IOM identified several diseases that were relevant to and known to have been diagnosed among military personnel during and after deployment in these regions. On September 29, 2010, responding to the report, VA added brucellosis, Campylobacter jejuni, Coxiella burnetti (Q fever), malaria, Mycobacterium tuberculosis (TB), nontyphoid Salmonella, Shigella, visceral leishmaniasis, and West Nile virus to the list of presumptive illnesses.3 The final rule was published in the Federal Register and is codified in 38 C.F.R. § 3.317(c).4
Classifying an illness as presumptive relieves the veteran of having to prove that their illness was connected to exposure during service in a specific region, “…[shifting] the burden of proof concerning whether a disease or disability was caused or aggravated due to service from the Veteran to the VA.”5 Based on latency periods, 7 of the 9 diseases must manifest to a > 10% degree of disability within a year of separation from a qualifying period of service. No date boundary was set on the period of presumption for TB or visceral leishmaniasis.6
Methods
Veterans are eligible for VHA care when they separate from active-duty service, or they are deactivated at the completion of their reserve or guard tour. Veterans eligible for health care were identified using a roster file from the DoD Defense Manpower Data Center (DMDC). This file also contained demographic (eg, sex, race) and service (eg, branch, rank) information. Inpatient and outpatient health care data were extracted from the VHA Office of Public Health’s quarterly files.
Study Population
OEF/OIF/OND veterans whose roster file records indicated a deployment to Iraq, Kuwait, Saudi Arabia, the neutral zone (between Iraq and Saudi Arabia), Bahrain, Qatar, The United Arab Emirates, Oman, Gulf of Aden, Gulf of Oman, waters of the Persian Gulf, the Arabian Sea, the Red Sea, and Afghanistan were eligible for the study. These veterans had to have separated from service between June 28, 2009, and December 29, 2011, and sought VHA care within a year of separation. Veterans with a human immunodeficiency virus diagnosis, an illness that is highly correlated with TB, were excluded from the study, as were deceased and Coast Guard veterans.
The final study population of 107,030 OEF/OIF/OND veterans was further divided into 2 mutually exclusive study groups by assessing the ICD-9-CM code in the first diagnostic position. The first group, the PID group, was given priority. To be included in this group, a veteran must have been diagnosed with ≥ 1 of the following presumptive diseases within a year of separation (ICD-9-CM codes): Brucellosis (023), Campylobacter jejuni (008.43), Coxiella burnetti/Q fever (083.0), malaria (084), nontyphoid Salmonella (003), Shigella (004), or West Nile virus (066.4). For TB (010-018) and visceral leishmaniasis (085.0), a diagnosis could occur any time after separation.
Related: DoD Healthy Base Initiative
The second infectious disease group included veterans diagnosed with any infectious disease (ICD-9-CM codes 001-139) that was not a PID. To be considered for inclusion in the other infectious disease group, a veteran must have been diagnosed with the illness at any point after separation. This group was created as a control group for comparing differences in health care use of the veterans diagnosed with a PID both before and after the rule change. The illnesses within each study group were distinct, thus no direct comparisons were made between the groups. Instead, the magnitude of the difference in use before and after the presumptive disease ruling was compared.
Statistical Analysis
It is possible to have multiple services performed during a single outpatient visit, services that will generate separate bills, thus appearing to be different visits. For the purposes of this study, only 1 visit per day was counted when constructing the monthly health care counts for the 12 months before and after the date of diagnosis of a PID or another infectious disease. A general linear model was created to assess differences in the number of outpatient visits pre- and postruling, adjusting for the number of unique illnesses a veteran had. To adjust for normality in the model, the inverse log of the count of outpatient visits was used in the procedure. P values were compared with an á level of 0.05 to determine significance.
Results
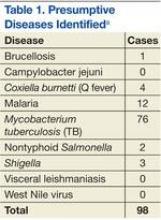
Among the 107,030 veterans receiving VHA care between June 28, 2009, and December 29, 2011, < 0.1% (n = 98) were in the PID group, and 7% (n = 7,603) were in the other infectious disease group (Tables 1 and 2). A significantly smaller proportion of active-duty (“regular”) veterans was in the PID group (50.0%) compared with the other infectious disease group (63.9%). Conversely, a significantly larger proportion of reserve or guard veterans werein the PID group (51.0%) compared with the other infectious disease group (36.1%) (P = .0089). The PID group included a higher proportion of Hispanic veterans (16.3%) and a lower proportion of black veterans (7.1%) than did the other infectious disease group.
The opposite was observed in the other infectious disease group: There was a lower proportion of Hispanic veterans (12.6%) and a higher proportion of black veterans (17.0%). Veterans whose military occupation status indicated combat experience were highly represented in each of the disease groups, as were males. Army veterans were disproportionately represented in the PID group (76.5%) compared with the other infectious disease group (65.4%), whereas the opposite was true for Marine Corps veterans (13.3% and 18.9%, respectively)(Table 2).
To assess the impact of the ruling on the health care-seeking behaviors of veterans, each group was further divided by the timing of diagnosis, specifically, before or after the PID ruling on September 29, 2010. Forty-five percent of the study population received a diagnosis prior to the ruling. Thirty-six percent of the PID group and 30% of the other infectious disease study groups were diagnosed before the ruling (Table 3).
Veterans in the other infectious disease group who were diagnosed after the PID ruling had a significantly higher total number of outpatient visits than did those diagnosed before the ruling (P < .05). A small increase was observed in the median number of outpatient visits among veterans diagnosed with a PID preruling (median = 7) compared with those diagnosed postruling (median = 8), but the difference was not statistically significant. Veterans in the preruling PID group received a diagnosis < 117 days (median value) after separation from service, whereas those in the postruling group received a diagnosis < 291 days (median value) after separation from service (Table 3).
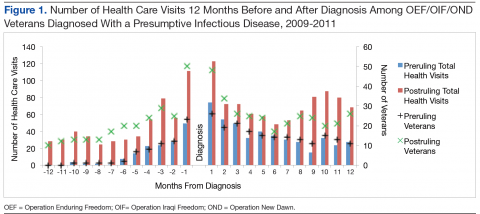
There was an increase in health care visits in the months directly before and after diagnosis, regardless of whether a veteran was diagnosed before or after the ruling. Figure 1 shows the total number of health care visits (visits for any condition) in the 12 months before and 12 months after a PID diagnosis, as well as the number of patients receiving care in those same months. In the months prior to receiving a diagnosis, the number of veterans receiving health care services followed the same trajectory as the total number of health care visits, regardless of the timing of the diagnosis. In the months after receiving a diagnosis, the trajectory for the total number of health care visits and the number of veterans generally followed the same path within the preruling group. In contrast, within the postruling group, the total number of visits was higher than the number of veterans, especially in the latter months, indicating that veterans were receiving services multiple times in a month.
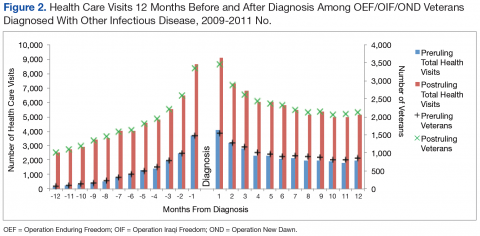
The patterns of health care use in the other infectious disease group were similar to those of the PID group, though the trajectories were more symmetrical for the other infectious disease pre- and postruling groups. There is a distinct increase in the total number of health care visits until diagnosis and a steady decrease in the 12 months after diagnosis with a leveling off of health care use toward the end of the observation period (Figure 2).
Discussion
The rate of PIDs in the U.S. was different from the observed rate in the study population, albeit a limited comparison. In the U.S. in 2010, the reported incidence per 100,000 persons was 0.04 for brucellosis, 13.52 for Campylobacter jejuni, 17.73 for nontyphoid Salmonella, and 0.2 for West Nile virus, vs no cases reported in the study.7,8 In contrast, the 2010-reported U.S. incidence rates per 100,000 persons with Q fever (0.04), malaria (0.58), and TB (3.64) were lower than those reported in the study population (3.32, 8.30, and 41.50 per 100,000 patients, respectively).7
Of the 107,030 OEF/OIF/OND veterans who received care during the study period, < 0.1% were diagnosed with a PIDs and 7% were diagnosed with a different infectious disease. Analysis indicated that 88 of the 98 PID were either TB or malaria cases. Thirty-six percent of the PID cases and 30% of the other infectious disease cases were diagnosed prior to the PID ruling. Veterans in the preruling PID and other infectious disease groups received a diagnosis within 4 or 5 months of becoming eligible for VHA services, whereas those in the postruling groups received a diagnosis within 10 months of eligibility, an observation that may have been caused by outliers and amplified by the small number of cases in the preruling PID group. However, this difference in time to diagnosis between the pre- and postruling groups does not seem to be a reflection of a delay in health care-seeking behavior in general: Veterans in both study groups sought VA services within 73 days of separating from active-duty service.
No significant difference in health care use was found between the pre- and postruling PID groups. When looking at the number of veterans receiving care each month and the total number of health care encounters, the ratio of encounters to veterans was less stable in the PID group than that of the other infectious disease group. Veterans with a PID received multiple outpatient services per month, especially in the postruling PID group. This may be a reflection of follow-up care needed for specific diseases.
Limitations
There are several limitations to note in the study. First, service members could have been diagnosed while still receiving health care services in the military health system, resulting in a low diagnosis rate within the VA. Second, the cases were identified solely based on ICD-9-CM codes; these are not confirmed diagnoses, and misclassification may occur. Future studies should consider incorporating laboratory results and other confirmatory methods of identification for case capture. A third limitation was the lack of availability of health care records outside of VHA. A large proportion of the study population was composed of the reserve/guard component. These veterans return to civilian jobs after separation and often have access to health care outside of VHA. Combined, these limitations affect the ability to identify the prevalence of infectious diseases among veterans.
Related: Women Using VA Health Care
Several findings could not be explored due to methodological limitations but warrant further exploration. First, the longer time period between eligibility and diagnosis post- vs preruling may be an indication that the ruling affected a veteran’s health care-seeking behavior. Second, it was possible that veterans presented with symptoms similar to one of the PIDs but were subsequently diagnosed with another infectious disease, which would affect the disease and use figures. Finally, studies should consider using confirmatory methods of diagnosis to assess the true prevalence of presumptive infectious diseases in the veteran population.
Conclusions
Very few PID cases were identified in the study population. This may be due to the limitation of the available data. However, some interesting findings such as a greater number of encounters for the infectious disease group post- vs preruling and differences in time between eligibility and diagnosis pre- and postruling were found and should be investigated further.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration, Department of Veterans Affairs. Analysis of VA Health Care Utilization Among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OED) Veterans: Cumulative from 1st Qtr FY 2002 through 1st Qtr FY 2013 (October 1, 2001—December 31, 2012). Washington, DC: Department of Veterans Affairs; 2013.
2. Bilmes L. Soldiers returning from Iraq and Afghanistan: The long-term costs of providing veterans medical care and disability benefits. KSG Faculty Research Working Paper Series RWP07-001, January 2007.
3. Institute of Medicine. Gulf War and Health, Volume 5: Infectious Diseases. Washington, DC: National Academies Press; 2007.
4. Department of Veterans Affairs. Presumption of service connection for Persian Gulf service. Fed Regist. 2010;75(188):59968-59972.
5. Panangala SV, Scott C; Congressional Research Service. CRS Report for Congress: Veterans Affairs: Presumptive Service Connection and Disability Compensation: September 13, 2010–R41405. Washington, DC: BiblioGov, 2013.
6. Fact Sheet 64-022-0312: Presumptive Disability for Nine Infectious Diseases Related to Military Service in Southwest Asia (1990-Present): Potential for Long-term Outcomes. U.S. Army Public Health Command. http://phc.amedd.army.mil/PHC%20Resource%20Library/PresumptiveDisability_NineDiseases.pdf
7. Centers for Disease Control and Prevention. Foodborne Diseases Active Surveillance Network (FoodNet): FoodNet Surveillance Report for 2010 (Final Report). Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011.
8. Centers for Disease Control and Prevention. Summary of notifiable diseases—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;59(53):1-111.
In 2010, the VA gave presumptive status to 9 infectious diseases that are endemic to southwest Asia and Afghanistan. This classification relieves the veteran of having to prove that an illness was connected to exposure during service in a specific region. The purpose of this secondary analysis is to determine the impact of the presumptive infectious disease (PID) ruling by the VHA by assessing the pre- and postruling health care use of veterans diagnosed with one of the infectious diseases.
Background
As of December 2012, 1.6 million veterans who served in Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) were eligible to receive VHA care. The number of combat related injuries is commonly released to the public, but figures related to noncombat illnesses, such as infectious diseases, are reported less frequently. Sixteen percent of the 899,752 OEF/OIF/OND veterans who received VHA care through December 2012 were diagnosed with an infectious disease.1
Long-term disability stemming from any type of illness, disease, or injury is potentially compensable through VA disability compensation programs. The disability must be service-connected for a veteran to receive compensation; that is, it must be determined to be a likely by-product of “an illness, disease or injury incurred or aggravated while the soldier was on active military service.”2 The benefit application process takes time, because service connection must be established prior to determining entitlement to disability benefits.2
Congress mandated that the VA determine the illnesses that justified a presumption of service-connection based on exposure to hazards of Iraq and Afghanistan service. In response, the VA requested that the Institute of Medicine (IOM) conduct a review of the scientific and medical literature to determine the diseases related to hazards of service in southwest Asia and Afghanistan.
In a 2006 report, the IOM identified several diseases that were relevant to and known to have been diagnosed among military personnel during and after deployment in these regions. On September 29, 2010, responding to the report, VA added brucellosis, Campylobacter jejuni, Coxiella burnetti (Q fever), malaria, Mycobacterium tuberculosis (TB), nontyphoid Salmonella, Shigella, visceral leishmaniasis, and West Nile virus to the list of presumptive illnesses.3 The final rule was published in the Federal Register and is codified in 38 C.F.R. § 3.317(c).4
Classifying an illness as presumptive relieves the veteran of having to prove that their illness was connected to exposure during service in a specific region, “…[shifting] the burden of proof concerning whether a disease or disability was caused or aggravated due to service from the Veteran to the VA.”5 Based on latency periods, 7 of the 9 diseases must manifest to a > 10% degree of disability within a year of separation from a qualifying period of service. No date boundary was set on the period of presumption for TB or visceral leishmaniasis.6
Methods
Veterans are eligible for VHA care when they separate from active-duty service, or they are deactivated at the completion of their reserve or guard tour. Veterans eligible for health care were identified using a roster file from the DoD Defense Manpower Data Center (DMDC). This file also contained demographic (eg, sex, race) and service (eg, branch, rank) information. Inpatient and outpatient health care data were extracted from the VHA Office of Public Health’s quarterly files.
Study Population
OEF/OIF/OND veterans whose roster file records indicated a deployment to Iraq, Kuwait, Saudi Arabia, the neutral zone (between Iraq and Saudi Arabia), Bahrain, Qatar, The United Arab Emirates, Oman, Gulf of Aden, Gulf of Oman, waters of the Persian Gulf, the Arabian Sea, the Red Sea, and Afghanistan were eligible for the study. These veterans had to have separated from service between June 28, 2009, and December 29, 2011, and sought VHA care within a year of separation. Veterans with a human immunodeficiency virus diagnosis, an illness that is highly correlated with TB, were excluded from the study, as were deceased and Coast Guard veterans.
The final study population of 107,030 OEF/OIF/OND veterans was further divided into 2 mutually exclusive study groups by assessing the ICD-9-CM code in the first diagnostic position. The first group, the PID group, was given priority. To be included in this group, a veteran must have been diagnosed with ≥ 1 of the following presumptive diseases within a year of separation (ICD-9-CM codes): Brucellosis (023), Campylobacter jejuni (008.43), Coxiella burnetti/Q fever (083.0), malaria (084), nontyphoid Salmonella (003), Shigella (004), or West Nile virus (066.4). For TB (010-018) and visceral leishmaniasis (085.0), a diagnosis could occur any time after separation.
Related: DoD Healthy Base Initiative
The second infectious disease group included veterans diagnosed with any infectious disease (ICD-9-CM codes 001-139) that was not a PID. To be considered for inclusion in the other infectious disease group, a veteran must have been diagnosed with the illness at any point after separation. This group was created as a control group for comparing differences in health care use of the veterans diagnosed with a PID both before and after the rule change. The illnesses within each study group were distinct, thus no direct comparisons were made between the groups. Instead, the magnitude of the difference in use before and after the presumptive disease ruling was compared.
Statistical Analysis
It is possible to have multiple services performed during a single outpatient visit, services that will generate separate bills, thus appearing to be different visits. For the purposes of this study, only 1 visit per day was counted when constructing the monthly health care counts for the 12 months before and after the date of diagnosis of a PID or another infectious disease. A general linear model was created to assess differences in the number of outpatient visits pre- and postruling, adjusting for the number of unique illnesses a veteran had. To adjust for normality in the model, the inverse log of the count of outpatient visits was used in the procedure. P values were compared with an á level of 0.05 to determine significance.
Results
Among the 107,030 veterans receiving VHA care between June 28, 2009, and December 29, 2011, < 0.1% (n = 98) were in the PID group, and 7% (n = 7,603) were in the other infectious disease group (Tables 1 and 2). A significantly smaller proportion of active-duty (“regular”) veterans was in the PID group (50.0%) compared with the other infectious disease group (63.9%). Conversely, a significantly larger proportion of reserve or guard veterans werein the PID group (51.0%) compared with the other infectious disease group (36.1%) (P = .0089). The PID group included a higher proportion of Hispanic veterans (16.3%) and a lower proportion of black veterans (7.1%) than did the other infectious disease group.
The opposite was observed in the other infectious disease group: There was a lower proportion of Hispanic veterans (12.6%) and a higher proportion of black veterans (17.0%). Veterans whose military occupation status indicated combat experience were highly represented in each of the disease groups, as were males. Army veterans were disproportionately represented in the PID group (76.5%) compared with the other infectious disease group (65.4%), whereas the opposite was true for Marine Corps veterans (13.3% and 18.9%, respectively)(Table 2).
To assess the impact of the ruling on the health care-seeking behaviors of veterans, each group was further divided by the timing of diagnosis, specifically, before or after the PID ruling on September 29, 2010. Forty-five percent of the study population received a diagnosis prior to the ruling. Thirty-six percent of the PID group and 30% of the other infectious disease study groups were diagnosed before the ruling (Table 3).
Veterans in the other infectious disease group who were diagnosed after the PID ruling had a significantly higher total number of outpatient visits than did those diagnosed before the ruling (P < .05). A small increase was observed in the median number of outpatient visits among veterans diagnosed with a PID preruling (median = 7) compared with those diagnosed postruling (median = 8), but the difference was not statistically significant. Veterans in the preruling PID group received a diagnosis < 117 days (median value) after separation from service, whereas those in the postruling group received a diagnosis < 291 days (median value) after separation from service (Table 3).
There was an increase in health care visits in the months directly before and after diagnosis, regardless of whether a veteran was diagnosed before or after the ruling. Figure 1 shows the total number of health care visits (visits for any condition) in the 12 months before and 12 months after a PID diagnosis, as well as the number of patients receiving care in those same months. In the months prior to receiving a diagnosis, the number of veterans receiving health care services followed the same trajectory as the total number of health care visits, regardless of the timing of the diagnosis. In the months after receiving a diagnosis, the trajectory for the total number of health care visits and the number of veterans generally followed the same path within the preruling group. In contrast, within the postruling group, the total number of visits was higher than the number of veterans, especially in the latter months, indicating that veterans were receiving services multiple times in a month.
The patterns of health care use in the other infectious disease group were similar to those of the PID group, though the trajectories were more symmetrical for the other infectious disease pre- and postruling groups. There is a distinct increase in the total number of health care visits until diagnosis and a steady decrease in the 12 months after diagnosis with a leveling off of health care use toward the end of the observation period (Figure 2).
Discussion
The rate of PIDs in the U.S. was different from the observed rate in the study population, albeit a limited comparison. In the U.S. in 2010, the reported incidence per 100,000 persons was 0.04 for brucellosis, 13.52 for Campylobacter jejuni, 17.73 for nontyphoid Salmonella, and 0.2 for West Nile virus, vs no cases reported in the study.7,8 In contrast, the 2010-reported U.S. incidence rates per 100,000 persons with Q fever (0.04), malaria (0.58), and TB (3.64) were lower than those reported in the study population (3.32, 8.30, and 41.50 per 100,000 patients, respectively).7
Of the 107,030 OEF/OIF/OND veterans who received care during the study period, < 0.1% were diagnosed with a PIDs and 7% were diagnosed with a different infectious disease. Analysis indicated that 88 of the 98 PID were either TB or malaria cases. Thirty-six percent of the PID cases and 30% of the other infectious disease cases were diagnosed prior to the PID ruling. Veterans in the preruling PID and other infectious disease groups received a diagnosis within 4 or 5 months of becoming eligible for VHA services, whereas those in the postruling groups received a diagnosis within 10 months of eligibility, an observation that may have been caused by outliers and amplified by the small number of cases in the preruling PID group. However, this difference in time to diagnosis between the pre- and postruling groups does not seem to be a reflection of a delay in health care-seeking behavior in general: Veterans in both study groups sought VA services within 73 days of separating from active-duty service.
No significant difference in health care use was found between the pre- and postruling PID groups. When looking at the number of veterans receiving care each month and the total number of health care encounters, the ratio of encounters to veterans was less stable in the PID group than that of the other infectious disease group. Veterans with a PID received multiple outpatient services per month, especially in the postruling PID group. This may be a reflection of follow-up care needed for specific diseases.
Limitations
There are several limitations to note in the study. First, service members could have been diagnosed while still receiving health care services in the military health system, resulting in a low diagnosis rate within the VA. Second, the cases were identified solely based on ICD-9-CM codes; these are not confirmed diagnoses, and misclassification may occur. Future studies should consider incorporating laboratory results and other confirmatory methods of identification for case capture. A third limitation was the lack of availability of health care records outside of VHA. A large proportion of the study population was composed of the reserve/guard component. These veterans return to civilian jobs after separation and often have access to health care outside of VHA. Combined, these limitations affect the ability to identify the prevalence of infectious diseases among veterans.
Related: Women Using VA Health Care
Several findings could not be explored due to methodological limitations but warrant further exploration. First, the longer time period between eligibility and diagnosis post- vs preruling may be an indication that the ruling affected a veteran’s health care-seeking behavior. Second, it was possible that veterans presented with symptoms similar to one of the PIDs but were subsequently diagnosed with another infectious disease, which would affect the disease and use figures. Finally, studies should consider using confirmatory methods of diagnosis to assess the true prevalence of presumptive infectious diseases in the veteran population.
Conclusions
Very few PID cases were identified in the study population. This may be due to the limitation of the available data. However, some interesting findings such as a greater number of encounters for the infectious disease group post- vs preruling and differences in time between eligibility and diagnosis pre- and postruling were found and should be investigated further.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
In 2010, the VA gave presumptive status to 9 infectious diseases that are endemic to southwest Asia and Afghanistan. This classification relieves the veteran of having to prove that an illness was connected to exposure during service in a specific region. The purpose of this secondary analysis is to determine the impact of the presumptive infectious disease (PID) ruling by the VHA by assessing the pre- and postruling health care use of veterans diagnosed with one of the infectious diseases.
Background
As of December 2012, 1.6 million veterans who served in Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) were eligible to receive VHA care. The number of combat related injuries is commonly released to the public, but figures related to noncombat illnesses, such as infectious diseases, are reported less frequently. Sixteen percent of the 899,752 OEF/OIF/OND veterans who received VHA care through December 2012 were diagnosed with an infectious disease.1
Long-term disability stemming from any type of illness, disease, or injury is potentially compensable through VA disability compensation programs. The disability must be service-connected for a veteran to receive compensation; that is, it must be determined to be a likely by-product of “an illness, disease or injury incurred or aggravated while the soldier was on active military service.”2 The benefit application process takes time, because service connection must be established prior to determining entitlement to disability benefits.2
Congress mandated that the VA determine the illnesses that justified a presumption of service-connection based on exposure to hazards of Iraq and Afghanistan service. In response, the VA requested that the Institute of Medicine (IOM) conduct a review of the scientific and medical literature to determine the diseases related to hazards of service in southwest Asia and Afghanistan.
In a 2006 report, the IOM identified several diseases that were relevant to and known to have been diagnosed among military personnel during and after deployment in these regions. On September 29, 2010, responding to the report, VA added brucellosis, Campylobacter jejuni, Coxiella burnetti (Q fever), malaria, Mycobacterium tuberculosis (TB), nontyphoid Salmonella, Shigella, visceral leishmaniasis, and West Nile virus to the list of presumptive illnesses.3 The final rule was published in the Federal Register and is codified in 38 C.F.R. § 3.317(c).4
Classifying an illness as presumptive relieves the veteran of having to prove that their illness was connected to exposure during service in a specific region, “…[shifting] the burden of proof concerning whether a disease or disability was caused or aggravated due to service from the Veteran to the VA.”5 Based on latency periods, 7 of the 9 diseases must manifest to a > 10% degree of disability within a year of separation from a qualifying period of service. No date boundary was set on the period of presumption for TB or visceral leishmaniasis.6
Methods
Veterans are eligible for VHA care when they separate from active-duty service, or they are deactivated at the completion of their reserve or guard tour. Veterans eligible for health care were identified using a roster file from the DoD Defense Manpower Data Center (DMDC). This file also contained demographic (eg, sex, race) and service (eg, branch, rank) information. Inpatient and outpatient health care data were extracted from the VHA Office of Public Health’s quarterly files.
Study Population
OEF/OIF/OND veterans whose roster file records indicated a deployment to Iraq, Kuwait, Saudi Arabia, the neutral zone (between Iraq and Saudi Arabia), Bahrain, Qatar, The United Arab Emirates, Oman, Gulf of Aden, Gulf of Oman, waters of the Persian Gulf, the Arabian Sea, the Red Sea, and Afghanistan were eligible for the study. These veterans had to have separated from service between June 28, 2009, and December 29, 2011, and sought VHA care within a year of separation. Veterans with a human immunodeficiency virus diagnosis, an illness that is highly correlated with TB, were excluded from the study, as were deceased and Coast Guard veterans.
The final study population of 107,030 OEF/OIF/OND veterans was further divided into 2 mutually exclusive study groups by assessing the ICD-9-CM code in the first diagnostic position. The first group, the PID group, was given priority. To be included in this group, a veteran must have been diagnosed with ≥ 1 of the following presumptive diseases within a year of separation (ICD-9-CM codes): Brucellosis (023), Campylobacter jejuni (008.43), Coxiella burnetti/Q fever (083.0), malaria (084), nontyphoid Salmonella (003), Shigella (004), or West Nile virus (066.4). For TB (010-018) and visceral leishmaniasis (085.0), a diagnosis could occur any time after separation.
Related: DoD Healthy Base Initiative
The second infectious disease group included veterans diagnosed with any infectious disease (ICD-9-CM codes 001-139) that was not a PID. To be considered for inclusion in the other infectious disease group, a veteran must have been diagnosed with the illness at any point after separation. This group was created as a control group for comparing differences in health care use of the veterans diagnosed with a PID both before and after the rule change. The illnesses within each study group were distinct, thus no direct comparisons were made between the groups. Instead, the magnitude of the difference in use before and after the presumptive disease ruling was compared.
Statistical Analysis
It is possible to have multiple services performed during a single outpatient visit, services that will generate separate bills, thus appearing to be different visits. For the purposes of this study, only 1 visit per day was counted when constructing the monthly health care counts for the 12 months before and after the date of diagnosis of a PID or another infectious disease. A general linear model was created to assess differences in the number of outpatient visits pre- and postruling, adjusting for the number of unique illnesses a veteran had. To adjust for normality in the model, the inverse log of the count of outpatient visits was used in the procedure. P values were compared with an á level of 0.05 to determine significance.
Results
Among the 107,030 veterans receiving VHA care between June 28, 2009, and December 29, 2011, < 0.1% (n = 98) were in the PID group, and 7% (n = 7,603) were in the other infectious disease group (Tables 1 and 2). A significantly smaller proportion of active-duty (“regular”) veterans was in the PID group (50.0%) compared with the other infectious disease group (63.9%). Conversely, a significantly larger proportion of reserve or guard veterans werein the PID group (51.0%) compared with the other infectious disease group (36.1%) (P = .0089). The PID group included a higher proportion of Hispanic veterans (16.3%) and a lower proportion of black veterans (7.1%) than did the other infectious disease group.
The opposite was observed in the other infectious disease group: There was a lower proportion of Hispanic veterans (12.6%) and a higher proportion of black veterans (17.0%). Veterans whose military occupation status indicated combat experience were highly represented in each of the disease groups, as were males. Army veterans were disproportionately represented in the PID group (76.5%) compared with the other infectious disease group (65.4%), whereas the opposite was true for Marine Corps veterans (13.3% and 18.9%, respectively)(Table 2).
To assess the impact of the ruling on the health care-seeking behaviors of veterans, each group was further divided by the timing of diagnosis, specifically, before or after the PID ruling on September 29, 2010. Forty-five percent of the study population received a diagnosis prior to the ruling. Thirty-six percent of the PID group and 30% of the other infectious disease study groups were diagnosed before the ruling (Table 3).
Veterans in the other infectious disease group who were diagnosed after the PID ruling had a significantly higher total number of outpatient visits than did those diagnosed before the ruling (P < .05). A small increase was observed in the median number of outpatient visits among veterans diagnosed with a PID preruling (median = 7) compared with those diagnosed postruling (median = 8), but the difference was not statistically significant. Veterans in the preruling PID group received a diagnosis < 117 days (median value) after separation from service, whereas those in the postruling group received a diagnosis < 291 days (median value) after separation from service (Table 3).
There was an increase in health care visits in the months directly before and after diagnosis, regardless of whether a veteran was diagnosed before or after the ruling. Figure 1 shows the total number of health care visits (visits for any condition) in the 12 months before and 12 months after a PID diagnosis, as well as the number of patients receiving care in those same months. In the months prior to receiving a diagnosis, the number of veterans receiving health care services followed the same trajectory as the total number of health care visits, regardless of the timing of the diagnosis. In the months after receiving a diagnosis, the trajectory for the total number of health care visits and the number of veterans generally followed the same path within the preruling group. In contrast, within the postruling group, the total number of visits was higher than the number of veterans, especially in the latter months, indicating that veterans were receiving services multiple times in a month.
The patterns of health care use in the other infectious disease group were similar to those of the PID group, though the trajectories were more symmetrical for the other infectious disease pre- and postruling groups. There is a distinct increase in the total number of health care visits until diagnosis and a steady decrease in the 12 months after diagnosis with a leveling off of health care use toward the end of the observation period (Figure 2).
Discussion
The rate of PIDs in the U.S. was different from the observed rate in the study population, albeit a limited comparison. In the U.S. in 2010, the reported incidence per 100,000 persons was 0.04 for brucellosis, 13.52 for Campylobacter jejuni, 17.73 for nontyphoid Salmonella, and 0.2 for West Nile virus, vs no cases reported in the study.7,8 In contrast, the 2010-reported U.S. incidence rates per 100,000 persons with Q fever (0.04), malaria (0.58), and TB (3.64) were lower than those reported in the study population (3.32, 8.30, and 41.50 per 100,000 patients, respectively).7
Of the 107,030 OEF/OIF/OND veterans who received care during the study period, < 0.1% were diagnosed with a PIDs and 7% were diagnosed with a different infectious disease. Analysis indicated that 88 of the 98 PID were either TB or malaria cases. Thirty-six percent of the PID cases and 30% of the other infectious disease cases were diagnosed prior to the PID ruling. Veterans in the preruling PID and other infectious disease groups received a diagnosis within 4 or 5 months of becoming eligible for VHA services, whereas those in the postruling groups received a diagnosis within 10 months of eligibility, an observation that may have been caused by outliers and amplified by the small number of cases in the preruling PID group. However, this difference in time to diagnosis between the pre- and postruling groups does not seem to be a reflection of a delay in health care-seeking behavior in general: Veterans in both study groups sought VA services within 73 days of separating from active-duty service.
No significant difference in health care use was found between the pre- and postruling PID groups. When looking at the number of veterans receiving care each month and the total number of health care encounters, the ratio of encounters to veterans was less stable in the PID group than that of the other infectious disease group. Veterans with a PID received multiple outpatient services per month, especially in the postruling PID group. This may be a reflection of follow-up care needed for specific diseases.
Limitations
There are several limitations to note in the study. First, service members could have been diagnosed while still receiving health care services in the military health system, resulting in a low diagnosis rate within the VA. Second, the cases were identified solely based on ICD-9-CM codes; these are not confirmed diagnoses, and misclassification may occur. Future studies should consider incorporating laboratory results and other confirmatory methods of identification for case capture. A third limitation was the lack of availability of health care records outside of VHA. A large proportion of the study population was composed of the reserve/guard component. These veterans return to civilian jobs after separation and often have access to health care outside of VHA. Combined, these limitations affect the ability to identify the prevalence of infectious diseases among veterans.
Related: Women Using VA Health Care
Several findings could not be explored due to methodological limitations but warrant further exploration. First, the longer time period between eligibility and diagnosis post- vs preruling may be an indication that the ruling affected a veteran’s health care-seeking behavior. Second, it was possible that veterans presented with symptoms similar to one of the PIDs but were subsequently diagnosed with another infectious disease, which would affect the disease and use figures. Finally, studies should consider using confirmatory methods of diagnosis to assess the true prevalence of presumptive infectious diseases in the veteran population.
Conclusions
Very few PID cases were identified in the study population. This may be due to the limitation of the available data. However, some interesting findings such as a greater number of encounters for the infectious disease group post- vs preruling and differences in time between eligibility and diagnosis pre- and postruling were found and should be investigated further.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration, Department of Veterans Affairs. Analysis of VA Health Care Utilization Among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OED) Veterans: Cumulative from 1st Qtr FY 2002 through 1st Qtr FY 2013 (October 1, 2001—December 31, 2012). Washington, DC: Department of Veterans Affairs; 2013.
2. Bilmes L. Soldiers returning from Iraq and Afghanistan: The long-term costs of providing veterans medical care and disability benefits. KSG Faculty Research Working Paper Series RWP07-001, January 2007.
3. Institute of Medicine. Gulf War and Health, Volume 5: Infectious Diseases. Washington, DC: National Academies Press; 2007.
4. Department of Veterans Affairs. Presumption of service connection for Persian Gulf service. Fed Regist. 2010;75(188):59968-59972.
5. Panangala SV, Scott C; Congressional Research Service. CRS Report for Congress: Veterans Affairs: Presumptive Service Connection and Disability Compensation: September 13, 2010–R41405. Washington, DC: BiblioGov, 2013.
6. Fact Sheet 64-022-0312: Presumptive Disability for Nine Infectious Diseases Related to Military Service in Southwest Asia (1990-Present): Potential for Long-term Outcomes. U.S. Army Public Health Command. http://phc.amedd.army.mil/PHC%20Resource%20Library/PresumptiveDisability_NineDiseases.pdf
7. Centers for Disease Control and Prevention. Foodborne Diseases Active Surveillance Network (FoodNet): FoodNet Surveillance Report for 2010 (Final Report). Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011.
8. Centers for Disease Control and Prevention. Summary of notifiable diseases—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;59(53):1-111.
1. Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration, Department of Veterans Affairs. Analysis of VA Health Care Utilization Among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OED) Veterans: Cumulative from 1st Qtr FY 2002 through 1st Qtr FY 2013 (October 1, 2001—December 31, 2012). Washington, DC: Department of Veterans Affairs; 2013.
2. Bilmes L. Soldiers returning from Iraq and Afghanistan: The long-term costs of providing veterans medical care and disability benefits. KSG Faculty Research Working Paper Series RWP07-001, January 2007.
3. Institute of Medicine. Gulf War and Health, Volume 5: Infectious Diseases. Washington, DC: National Academies Press; 2007.
4. Department of Veterans Affairs. Presumption of service connection for Persian Gulf service. Fed Regist. 2010;75(188):59968-59972.
5. Panangala SV, Scott C; Congressional Research Service. CRS Report for Congress: Veterans Affairs: Presumptive Service Connection and Disability Compensation: September 13, 2010–R41405. Washington, DC: BiblioGov, 2013.
6. Fact Sheet 64-022-0312: Presumptive Disability for Nine Infectious Diseases Related to Military Service in Southwest Asia (1990-Present): Potential for Long-term Outcomes. U.S. Army Public Health Command. http://phc.amedd.army.mil/PHC%20Resource%20Library/PresumptiveDisability_NineDiseases.pdf
7. Centers for Disease Control and Prevention. Foodborne Diseases Active Surveillance Network (FoodNet): FoodNet Surveillance Report for 2010 (Final Report). Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011.
8. Centers for Disease Control and Prevention. Summary of notifiable diseases—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;59(53):1-111.