User login
Repositionable aortic valve meets performance goals
SAN FRANCISCO – A mean aortic valve pressure gradient of 11.5 mm Hg 30 days after transcatheter aortic valve replacement with the investigational repositionable Lotus valve in 120 patients was significantly better than the performance goal of 18 mm Hg, a study showed.
Approximately 4% of patients in the prospective registry study died within the 30 days and 2% had a disabling stroke, both of which could be considered low rates, Dr. Ian T. Meredith said at the Transcatheter Cardiovascular Therapeutics annual meeting. Another 4% of patients developed nondisabling strokes by the 30-day follow-up in an intent-to-treat analysis.
Aortic regurgitation rates were "negligible" after the procedure, said Dr. Meredith of Monash Medical Centre, Clayton, Australia, and professor of cardiology at Monash University, Melbourne.
Before valve replacement, 15% of patients had moderate or severe aortic regurgitation. Thirty days later, none had severe and 1% had moderate aortic regurgitation in the REPRISE II study (Repositionable Percutaneous Replacement of Stenotic Aortic Valve Through Implantation of Lotus Valve System – Evaluation of Safety and Performance).
Mild aortic regurgitation rates went from 44% at baseline to 17% at 30 days. Trace regurgitation was seen in 21% at baseline and at 30 days of follow-up.
The primary endpoints in the study were mean aortic valve pressure gradient at 30 days and 30-day all-cause mortality. The mean aortic gradient decreased from 46 mm Hg at baseline to 12.1 mm Hg at discharge and 11.5 mm Hg at 30 days. The mean effective orifice area increased from 0.7 cm2 at baseline to 1.6 cm2 at discharge and 1.7 cm2 at 30 days. Clinical event rates were similar to those reported in other valve trials, he said.
The 14-center study enrolled patients between October 2012 and April 2013 who were aged at least 70 years and rated New York Heart Association class II or greater. They had an aortic valve area less than 1 cm2, an aortic annulus measuring 19-27 mm, and a mean pressure gradient greater than 40 mm Hg or a jet velocity greater than 4 m/sec. Patients also had a Society of Thoracic Surgeons score of at least 8% and/or high surgical risk due to frailty or comorbidities.
The Lotus valve can be assessed in position before release, shortened or expanded mechanically, and, if desired, repositioned or fully resheathed and retrieved. It includes patented adaptive seal technology on the outside surfaces of the valve to fill up irregular surfaces of the fractured native aortic valve and reduce paravalvular leakage, Dr. Meredith said. The study used two valve sizes, 23 mm and 27 mm.
All 120 Lotus valves were successfully placed. Repositionings of 31 valves were all successful, and attempted retrievals of 6 valves were all successful. "As a consequence of this, there was no valve migration, no embolization, no ectopic valve deployment, and absolutely no need to put a second valve inside a valve for incorrect positioning or aortic regurgitation," he said at the meeting, cosponsored by the American College of Cardiology.
New pacemakers were needed in 29% (34 patients), mainly for third-degree atrioventricular block in 30 patients. "Perhaps the most important determinant of new pacemaker insertion was oversizing of the left ventricular outflow tract or the annulus due to the fact that only two valve sizes were available for this study," Dr. Meredith said. He predicted that this high rate of pacemaker implantation could be halved when more Lotus valve sizes and a more flexible catheter are available for future trials.
"We use the Lotus valve. The beauty of the valve is it can be repositioned and retrieved," Dr. A. Pieter Kappetein said at a press briefing. "You can plant the valve with a lot of confidence for the operator. At every stage of the procedure, you can control. I think that is the beauty of this valve," said Dr. Kappetein, professor of thoracic surgery at Erasmus University, Rotterdam, the Netherlands.
The Lotus valve system is available at selected centers in Europe and is not yet approved in the United States or Japan. The investigators plan to conduct a 130-patient extension of REPRISE II and a 1,000-patient pivotal trial (REPRISE III) to seek Food and Drug Administration approval.
Boston Scientific, which makes the Lotus valve system, funded the study. Dr. Meredith reported financial associations with Boston Scientific and Medtronic.
On Twitter @sherryboschert
SAN FRANCISCO – A mean aortic valve pressure gradient of 11.5 mm Hg 30 days after transcatheter aortic valve replacement with the investigational repositionable Lotus valve in 120 patients was significantly better than the performance goal of 18 mm Hg, a study showed.
Approximately 4% of patients in the prospective registry study died within the 30 days and 2% had a disabling stroke, both of which could be considered low rates, Dr. Ian T. Meredith said at the Transcatheter Cardiovascular Therapeutics annual meeting. Another 4% of patients developed nondisabling strokes by the 30-day follow-up in an intent-to-treat analysis.
Aortic regurgitation rates were "negligible" after the procedure, said Dr. Meredith of Monash Medical Centre, Clayton, Australia, and professor of cardiology at Monash University, Melbourne.
Before valve replacement, 15% of patients had moderate or severe aortic regurgitation. Thirty days later, none had severe and 1% had moderate aortic regurgitation in the REPRISE II study (Repositionable Percutaneous Replacement of Stenotic Aortic Valve Through Implantation of Lotus Valve System – Evaluation of Safety and Performance).
Mild aortic regurgitation rates went from 44% at baseline to 17% at 30 days. Trace regurgitation was seen in 21% at baseline and at 30 days of follow-up.
The primary endpoints in the study were mean aortic valve pressure gradient at 30 days and 30-day all-cause mortality. The mean aortic gradient decreased from 46 mm Hg at baseline to 12.1 mm Hg at discharge and 11.5 mm Hg at 30 days. The mean effective orifice area increased from 0.7 cm2 at baseline to 1.6 cm2 at discharge and 1.7 cm2 at 30 days. Clinical event rates were similar to those reported in other valve trials, he said.
The 14-center study enrolled patients between October 2012 and April 2013 who were aged at least 70 years and rated New York Heart Association class II or greater. They had an aortic valve area less than 1 cm2, an aortic annulus measuring 19-27 mm, and a mean pressure gradient greater than 40 mm Hg or a jet velocity greater than 4 m/sec. Patients also had a Society of Thoracic Surgeons score of at least 8% and/or high surgical risk due to frailty or comorbidities.
The Lotus valve can be assessed in position before release, shortened or expanded mechanically, and, if desired, repositioned or fully resheathed and retrieved. It includes patented adaptive seal technology on the outside surfaces of the valve to fill up irregular surfaces of the fractured native aortic valve and reduce paravalvular leakage, Dr. Meredith said. The study used two valve sizes, 23 mm and 27 mm.
All 120 Lotus valves were successfully placed. Repositionings of 31 valves were all successful, and attempted retrievals of 6 valves were all successful. "As a consequence of this, there was no valve migration, no embolization, no ectopic valve deployment, and absolutely no need to put a second valve inside a valve for incorrect positioning or aortic regurgitation," he said at the meeting, cosponsored by the American College of Cardiology.
New pacemakers were needed in 29% (34 patients), mainly for third-degree atrioventricular block in 30 patients. "Perhaps the most important determinant of new pacemaker insertion was oversizing of the left ventricular outflow tract or the annulus due to the fact that only two valve sizes were available for this study," Dr. Meredith said. He predicted that this high rate of pacemaker implantation could be halved when more Lotus valve sizes and a more flexible catheter are available for future trials.
"We use the Lotus valve. The beauty of the valve is it can be repositioned and retrieved," Dr. A. Pieter Kappetein said at a press briefing. "You can plant the valve with a lot of confidence for the operator. At every stage of the procedure, you can control. I think that is the beauty of this valve," said Dr. Kappetein, professor of thoracic surgery at Erasmus University, Rotterdam, the Netherlands.
The Lotus valve system is available at selected centers in Europe and is not yet approved in the United States or Japan. The investigators plan to conduct a 130-patient extension of REPRISE II and a 1,000-patient pivotal trial (REPRISE III) to seek Food and Drug Administration approval.
Boston Scientific, which makes the Lotus valve system, funded the study. Dr. Meredith reported financial associations with Boston Scientific and Medtronic.
On Twitter @sherryboschert
SAN FRANCISCO – A mean aortic valve pressure gradient of 11.5 mm Hg 30 days after transcatheter aortic valve replacement with the investigational repositionable Lotus valve in 120 patients was significantly better than the performance goal of 18 mm Hg, a study showed.
Approximately 4% of patients in the prospective registry study died within the 30 days and 2% had a disabling stroke, both of which could be considered low rates, Dr. Ian T. Meredith said at the Transcatheter Cardiovascular Therapeutics annual meeting. Another 4% of patients developed nondisabling strokes by the 30-day follow-up in an intent-to-treat analysis.
Aortic regurgitation rates were "negligible" after the procedure, said Dr. Meredith of Monash Medical Centre, Clayton, Australia, and professor of cardiology at Monash University, Melbourne.
Before valve replacement, 15% of patients had moderate or severe aortic regurgitation. Thirty days later, none had severe and 1% had moderate aortic regurgitation in the REPRISE II study (Repositionable Percutaneous Replacement of Stenotic Aortic Valve Through Implantation of Lotus Valve System – Evaluation of Safety and Performance).
Mild aortic regurgitation rates went from 44% at baseline to 17% at 30 days. Trace regurgitation was seen in 21% at baseline and at 30 days of follow-up.
The primary endpoints in the study were mean aortic valve pressure gradient at 30 days and 30-day all-cause mortality. The mean aortic gradient decreased from 46 mm Hg at baseline to 12.1 mm Hg at discharge and 11.5 mm Hg at 30 days. The mean effective orifice area increased from 0.7 cm2 at baseline to 1.6 cm2 at discharge and 1.7 cm2 at 30 days. Clinical event rates were similar to those reported in other valve trials, he said.
The 14-center study enrolled patients between October 2012 and April 2013 who were aged at least 70 years and rated New York Heart Association class II or greater. They had an aortic valve area less than 1 cm2, an aortic annulus measuring 19-27 mm, and a mean pressure gradient greater than 40 mm Hg or a jet velocity greater than 4 m/sec. Patients also had a Society of Thoracic Surgeons score of at least 8% and/or high surgical risk due to frailty or comorbidities.
The Lotus valve can be assessed in position before release, shortened or expanded mechanically, and, if desired, repositioned or fully resheathed and retrieved. It includes patented adaptive seal technology on the outside surfaces of the valve to fill up irregular surfaces of the fractured native aortic valve and reduce paravalvular leakage, Dr. Meredith said. The study used two valve sizes, 23 mm and 27 mm.
All 120 Lotus valves were successfully placed. Repositionings of 31 valves were all successful, and attempted retrievals of 6 valves were all successful. "As a consequence of this, there was no valve migration, no embolization, no ectopic valve deployment, and absolutely no need to put a second valve inside a valve for incorrect positioning or aortic regurgitation," he said at the meeting, cosponsored by the American College of Cardiology.
New pacemakers were needed in 29% (34 patients), mainly for third-degree atrioventricular block in 30 patients. "Perhaps the most important determinant of new pacemaker insertion was oversizing of the left ventricular outflow tract or the annulus due to the fact that only two valve sizes were available for this study," Dr. Meredith said. He predicted that this high rate of pacemaker implantation could be halved when more Lotus valve sizes and a more flexible catheter are available for future trials.
"We use the Lotus valve. The beauty of the valve is it can be repositioned and retrieved," Dr. A. Pieter Kappetein said at a press briefing. "You can plant the valve with a lot of confidence for the operator. At every stage of the procedure, you can control. I think that is the beauty of this valve," said Dr. Kappetein, professor of thoracic surgery at Erasmus University, Rotterdam, the Netherlands.
The Lotus valve system is available at selected centers in Europe and is not yet approved in the United States or Japan. The investigators plan to conduct a 130-patient extension of REPRISE II and a 1,000-patient pivotal trial (REPRISE III) to seek Food and Drug Administration approval.
Boston Scientific, which makes the Lotus valve system, funded the study. Dr. Meredith reported financial associations with Boston Scientific and Medtronic.
On Twitter @sherryboschert
AT TCT 2013
Major finding: The 30-day mean aortic valve pressure gradient was 11.5 mm Hg, and 4% of patients died within 30 days.
Data source: A prospective registry study of 120 patients with aortic stenosis and high surgery risk who underwent transcatheter aortic valve replacement with the Lotus valve system.
Disclosures: Boston Scientific, which makes the Lotus valve system, funded the study. Dr. Meredith reported financial associations with Boston Scientific and Medtronic.
Comfort care informs critical care societies’ Choosing Wisely list
SAN FRANCISCO – Four critical care societies released a list of the top five things that intensivists should avoid doing, part of the larger Choosing Wisely campaign to reduce unnecessary and costly medical practices. The list includes a potentially difficult issue: offering patients' families the option of comfort care in lieu of continuing life support.
Fifth on the list, the life-support item may be the most controversial and is also the one that the representatives felt the most strongly about including, whether or not it saves many resources, according to Dr. Hannah Wunsch, who served on the collaborative task force. "Many ... patients receive aggressive life-sustaining therapies, in part due to clinicians’ failures to elicit patients’ values and goals, and to provide patient-centered recommendations," the task force wrote.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Discussion of the list, which was announced at the Critical Care Congress, quickly turned to how to implement the recommendations, including how to empower families to challenge physicians or nurses when they see these steps being taken in the care of a loved one.
The Society for Critical Care Medicine, which sponsored the Congress, collaborated with the American College of Chest Physicians, the American Thoracic Society, and the American Association of Critical Care Nurses to create the list. It’s the first Choosing Wisely list to include collaboration with a nursing organization and only the second that’s a product of collaboration instead of being issued by a sole medical society, said Dr. Scott D. Halpern of the University of Pennsylvania, Philadelphia, chair of the collaborative group.
The four groups – the Critical Care Societies Collaborative – started with a list of 58 medical practices that they found objectionable, which they trimmed to 9 items based on the strength of evidence and their prevalence, relevance, and cost, explained Dr. Wunsch of the department of anesthesiology at Columbia University Medical Center, N.Y. Discussion winnowed that to the Top 5, an arbitrary number selected by the Choosing Wisely campaign that everyone should recognize as "a starting point," she said.
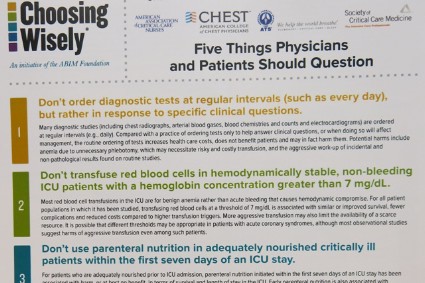
A two-page document of the critical care list can be downloaded from the Choosing Wisely website. It includes some of the sources for the recommendations and these top five "don’ts" displayed on the front:
1. Don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions. Ordering diagnostic studies such as x-rays, arterial blood gases, blood counts, blood chemistries, or ECGs daily or at routine intervals drives up costs, doesn’t benefit patients, and may harm them through radiation exposure, inducing anemia, or triggering aggressive follow-up of incidental results. "I think this has become more prevalent with electronic medical records," where one click can order x-rays for the next 5 days, she said.
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 mg/dL. Blood is a scarce resource, and studies show that limiting red blood cell transfusions to thresholds of 7 mg/dL or higher does not worsen survival, complications, or costs, and causes fewer complications. Different thresholds may be appropriate for patients with acute coronary syndrome, but even in this subgroup aggressive transfusion is harmful, most observational studies suggest.
3. Don’t use parenteral nutrition in adequately nourished critically ill patients within the first 7 days of an ICU stay. Early parenteral nutrition is harmful, even in patients who cannot tolerate enteral nutrition, if they were adequately nourished prior to ICU admission. The evidence is less clear for patients with nosocomial infections, and early parenteral nutrition may benefit patients who were severely malnourished right before ICU admission.
A study to be published soon shows that 90% of parenteral nutrition in the United States starts within 7 days of admission, usually within the first 2 days, Dr. Wunsch said. "It’s definitely more prevalent than I think many of us realize," she said.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Deep sedation of patients on mechanical ventilation prolongs the duration of ventilation and hospitalization. Several protocols for limiting sedation have been shown to improve patient outcomes.
5. Don’t continue life support for patients at high risk of death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. When an audience member expressed concern about discontinuation of life support possibly increasing premature deaths, Dr. Wunsch stressed that the second part of the statement is key – giving the family the choice of comfort care or continuing life support.
The simplicity of the Choosing Wisely list and its focus on overuse and costs make it possible to pursue unconventional ways of making it widely adopted, such as empowering families to question care, said Dr. Jeremy M. Kahn of the University of Pittsburgh. The 5 recommendations are far fewer than the 85 recommendations in the 2002 Surviving Sepsis campaign, for example, and the Choosing Wisely campaign has partnered with Consumer Reports and engaged the lay press to help spread the word, he said.
Dr. Kahn described a recent uncomfortable experience in which he had to question some of the medical care being offered to a hospitalized family member. It wasn’t easy to speak up, even though he’s a physician, and it must be even harder for lay people, he said. Hanging a sign in every ICU with the Choosing Wisely list might help empower families to speak up, one physician suggested during the discussion.
Incorporating decision-support prompts in electronic health records also could help physicians adhere to the Choosing Wisely recommendations, Dr. Kahn said.
Beyond the five items that made the Choosing Wisely list, the four runners-up were issues of antimicrobial duration; CT or MRI scanning for altered level of consciousness; vascular catheter indications; and ICU admission criteria for patients with poor prognosis, Dr. Wunsch said.
The Critical Care Societies Collaborative represents approximately 150,000 critical care providers, according to Dr. Curtis Sessler, president-designate of the American College of Chest Physicians.
The Choosing Wisely campaign, a project of the ABIM Foundation, released lists of "Five Things Physicians and Patients Should Question" by 9 medical societies in April 2012 and 17 more in February 2013, with the development of more lists ongoing.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Four critical care societies released a list of the top five things that intensivists should avoid doing, part of the larger Choosing Wisely campaign to reduce unnecessary and costly medical practices. The list includes a potentially difficult issue: offering patients' families the option of comfort care in lieu of continuing life support.
Fifth on the list, the life-support item may be the most controversial and is also the one that the representatives felt the most strongly about including, whether or not it saves many resources, according to Dr. Hannah Wunsch, who served on the collaborative task force. "Many ... patients receive aggressive life-sustaining therapies, in part due to clinicians’ failures to elicit patients’ values and goals, and to provide patient-centered recommendations," the task force wrote.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Discussion of the list, which was announced at the Critical Care Congress, quickly turned to how to implement the recommendations, including how to empower families to challenge physicians or nurses when they see these steps being taken in the care of a loved one.
The Society for Critical Care Medicine, which sponsored the Congress, collaborated with the American College of Chest Physicians, the American Thoracic Society, and the American Association of Critical Care Nurses to create the list. It’s the first Choosing Wisely list to include collaboration with a nursing organization and only the second that’s a product of collaboration instead of being issued by a sole medical society, said Dr. Scott D. Halpern of the University of Pennsylvania, Philadelphia, chair of the collaborative group.
The four groups – the Critical Care Societies Collaborative – started with a list of 58 medical practices that they found objectionable, which they trimmed to 9 items based on the strength of evidence and their prevalence, relevance, and cost, explained Dr. Wunsch of the department of anesthesiology at Columbia University Medical Center, N.Y. Discussion winnowed that to the Top 5, an arbitrary number selected by the Choosing Wisely campaign that everyone should recognize as "a starting point," she said.
A two-page document of the critical care list can be downloaded from the Choosing Wisely website. It includes some of the sources for the recommendations and these top five "don’ts" displayed on the front:
1. Don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions. Ordering diagnostic studies such as x-rays, arterial blood gases, blood counts, blood chemistries, or ECGs daily or at routine intervals drives up costs, doesn’t benefit patients, and may harm them through radiation exposure, inducing anemia, or triggering aggressive follow-up of incidental results. "I think this has become more prevalent with electronic medical records," where one click can order x-rays for the next 5 days, she said.
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 mg/dL. Blood is a scarce resource, and studies show that limiting red blood cell transfusions to thresholds of 7 mg/dL or higher does not worsen survival, complications, or costs, and causes fewer complications. Different thresholds may be appropriate for patients with acute coronary syndrome, but even in this subgroup aggressive transfusion is harmful, most observational studies suggest.
3. Don’t use parenteral nutrition in adequately nourished critically ill patients within the first 7 days of an ICU stay. Early parenteral nutrition is harmful, even in patients who cannot tolerate enteral nutrition, if they were adequately nourished prior to ICU admission. The evidence is less clear for patients with nosocomial infections, and early parenteral nutrition may benefit patients who were severely malnourished right before ICU admission.
A study to be published soon shows that 90% of parenteral nutrition in the United States starts within 7 days of admission, usually within the first 2 days, Dr. Wunsch said. "It’s definitely more prevalent than I think many of us realize," she said.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Deep sedation of patients on mechanical ventilation prolongs the duration of ventilation and hospitalization. Several protocols for limiting sedation have been shown to improve patient outcomes.
5. Don’t continue life support for patients at high risk of death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. When an audience member expressed concern about discontinuation of life support possibly increasing premature deaths, Dr. Wunsch stressed that the second part of the statement is key – giving the family the choice of comfort care or continuing life support.
The simplicity of the Choosing Wisely list and its focus on overuse and costs make it possible to pursue unconventional ways of making it widely adopted, such as empowering families to question care, said Dr. Jeremy M. Kahn of the University of Pittsburgh. The 5 recommendations are far fewer than the 85 recommendations in the 2002 Surviving Sepsis campaign, for example, and the Choosing Wisely campaign has partnered with Consumer Reports and engaged the lay press to help spread the word, he said.
Dr. Kahn described a recent uncomfortable experience in which he had to question some of the medical care being offered to a hospitalized family member. It wasn’t easy to speak up, even though he’s a physician, and it must be even harder for lay people, he said. Hanging a sign in every ICU with the Choosing Wisely list might help empower families to speak up, one physician suggested during the discussion.
Incorporating decision-support prompts in electronic health records also could help physicians adhere to the Choosing Wisely recommendations, Dr. Kahn said.
Beyond the five items that made the Choosing Wisely list, the four runners-up were issues of antimicrobial duration; CT or MRI scanning for altered level of consciousness; vascular catheter indications; and ICU admission criteria for patients with poor prognosis, Dr. Wunsch said.
The Critical Care Societies Collaborative represents approximately 150,000 critical care providers, according to Dr. Curtis Sessler, president-designate of the American College of Chest Physicians.
The Choosing Wisely campaign, a project of the ABIM Foundation, released lists of "Five Things Physicians and Patients Should Question" by 9 medical societies in April 2012 and 17 more in February 2013, with the development of more lists ongoing.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Four critical care societies released a list of the top five things that intensivists should avoid doing, part of the larger Choosing Wisely campaign to reduce unnecessary and costly medical practices. The list includes a potentially difficult issue: offering patients' families the option of comfort care in lieu of continuing life support.
Fifth on the list, the life-support item may be the most controversial and is also the one that the representatives felt the most strongly about including, whether or not it saves many resources, according to Dr. Hannah Wunsch, who served on the collaborative task force. "Many ... patients receive aggressive life-sustaining therapies, in part due to clinicians’ failures to elicit patients’ values and goals, and to provide patient-centered recommendations," the task force wrote.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Discussion of the list, which was announced at the Critical Care Congress, quickly turned to how to implement the recommendations, including how to empower families to challenge physicians or nurses when they see these steps being taken in the care of a loved one.
The Society for Critical Care Medicine, which sponsored the Congress, collaborated with the American College of Chest Physicians, the American Thoracic Society, and the American Association of Critical Care Nurses to create the list. It’s the first Choosing Wisely list to include collaboration with a nursing organization and only the second that’s a product of collaboration instead of being issued by a sole medical society, said Dr. Scott D. Halpern of the University of Pennsylvania, Philadelphia, chair of the collaborative group.
The four groups – the Critical Care Societies Collaborative – started with a list of 58 medical practices that they found objectionable, which they trimmed to 9 items based on the strength of evidence and their prevalence, relevance, and cost, explained Dr. Wunsch of the department of anesthesiology at Columbia University Medical Center, N.Y. Discussion winnowed that to the Top 5, an arbitrary number selected by the Choosing Wisely campaign that everyone should recognize as "a starting point," she said.
A two-page document of the critical care list can be downloaded from the Choosing Wisely website. It includes some of the sources for the recommendations and these top five "don’ts" displayed on the front:
1. Don’t order diagnostic tests at regular intervals (such as every day), but rather in response to specific clinical questions. Ordering diagnostic studies such as x-rays, arterial blood gases, blood counts, blood chemistries, or ECGs daily or at routine intervals drives up costs, doesn’t benefit patients, and may harm them through radiation exposure, inducing anemia, or triggering aggressive follow-up of incidental results. "I think this has become more prevalent with electronic medical records," where one click can order x-rays for the next 5 days, she said.
2. Don’t transfuse red blood cells in hemodynamically stable, non-bleeding ICU patients with a hemoglobin concentration greater than 7 mg/dL. Blood is a scarce resource, and studies show that limiting red blood cell transfusions to thresholds of 7 mg/dL or higher does not worsen survival, complications, or costs, and causes fewer complications. Different thresholds may be appropriate for patients with acute coronary syndrome, but even in this subgroup aggressive transfusion is harmful, most observational studies suggest.
3. Don’t use parenteral nutrition in adequately nourished critically ill patients within the first 7 days of an ICU stay. Early parenteral nutrition is harmful, even in patients who cannot tolerate enteral nutrition, if they were adequately nourished prior to ICU admission. The evidence is less clear for patients with nosocomial infections, and early parenteral nutrition may benefit patients who were severely malnourished right before ICU admission.
A study to be published soon shows that 90% of parenteral nutrition in the United States starts within 7 days of admission, usually within the first 2 days, Dr. Wunsch said. "It’s definitely more prevalent than I think many of us realize," she said.
4. Don’t deeply sedate mechanically ventilated patients without a specific indication and without daily attempts to lighten sedation. Deep sedation of patients on mechanical ventilation prolongs the duration of ventilation and hospitalization. Several protocols for limiting sedation have been shown to improve patient outcomes.
5. Don’t continue life support for patients at high risk of death or severely impaired functional recovery without offering patients and their families the alternative of care focused entirely on comfort. When an audience member expressed concern about discontinuation of life support possibly increasing premature deaths, Dr. Wunsch stressed that the second part of the statement is key – giving the family the choice of comfort care or continuing life support.
The simplicity of the Choosing Wisely list and its focus on overuse and costs make it possible to pursue unconventional ways of making it widely adopted, such as empowering families to question care, said Dr. Jeremy M. Kahn of the University of Pittsburgh. The 5 recommendations are far fewer than the 85 recommendations in the 2002 Surviving Sepsis campaign, for example, and the Choosing Wisely campaign has partnered with Consumer Reports and engaged the lay press to help spread the word, he said.
Dr. Kahn described a recent uncomfortable experience in which he had to question some of the medical care being offered to a hospitalized family member. It wasn’t easy to speak up, even though he’s a physician, and it must be even harder for lay people, he said. Hanging a sign in every ICU with the Choosing Wisely list might help empower families to speak up, one physician suggested during the discussion.
Incorporating decision-support prompts in electronic health records also could help physicians adhere to the Choosing Wisely recommendations, Dr. Kahn said.
Beyond the five items that made the Choosing Wisely list, the four runners-up were issues of antimicrobial duration; CT or MRI scanning for altered level of consciousness; vascular catheter indications; and ICU admission criteria for patients with poor prognosis, Dr. Wunsch said.
The Critical Care Societies Collaborative represents approximately 150,000 critical care providers, according to Dr. Curtis Sessler, president-designate of the American College of Chest Physicians.
The Choosing Wisely campaign, a project of the ABIM Foundation, released lists of "Five Things Physicians and Patients Should Question" by 9 medical societies in April 2012 and 17 more in February 2013, with the development of more lists ongoing.
The speakers reported having no financial disclosures.
On Twitter @sherryboschert
AT THE CRITICAL CARE CONGRESS
Luteal-phase antidepressant an option in recalcitrant PMS, PMDD
SAN FRANCISCO – Selective serotonin reuptake inhibitor antidepressants can alleviate symptoms of premenstrual syndrome or premenstrual dysphoric disorder, but are far from first-line therapies for either disorder, according to Dr. Ellen Haller.
The first steps in treating PMS and PMDD are basic wellness strategies such as a healthy diet, smoking cessation, exercise, adequate sleep, and stress management, Dr. Haller said at a conference on women’s health sponsored by the University of California, San Francisco.
Calcium supplementation also has been shown to reduce total emotional and physical symptom scores by 48% in women with PMS compared with a 30% reduction from placebo in a multicenter, randomized placebo-controlled study of 497 patients. That study used 600 mg, twice daily, of calcium carbonate or placebo for three menstrual cycles, said Dr. Haller, professor of clinical psychiatry at the university.
The results of that study (Am. J. Obstet.Gynecol. 1998;179:444-52) have not been replicated, she added.
If wellness treatments and calcium supplementation don’t work, the next step for treating women with PMS may be an SSRI. A Cochrane review of 31 randomized controlled trials found that SSRIs are more effective than placebo in treating PMS (Cochrane Database Syst. Rev. 2013;6:CD001396). Treatment should be an SSRI antidepressant, Dr. Haller emphasized. Bupropion, which is a norepinephrine dopamine reuptake inhibitor, is not effective for these women.
Low-dose SSRIs may be taken daily or can be effective against emotional and physical symptoms if taken only during the luteal phase of menstruation, starting on day 14 of the cycle and stopping on day 1, the first day of menses, Dr. Haller said. Patients with PMS tend to respond more quickly and at lower doses than patients with depression, and usually don’t get withdrawal symptoms when stopping the SSRI on the luteal-phase dosing regimen.
In women with PMDD, there is a preliminary suggestion that an SSRI may be more effective than calcium supplements. A pilot study of 39 women with PMDD found that the SSRI fluoxetine was more effective than calcium or placebo for PMDD, though scores were significantly better than calcium only on just two of five symptom scales. The study compared fluoxetine 10 mg b.i.d., calcium carbonate 600 mg b.i.d., and placebo (J. Clin. Psychopharmacol. 2013;33:614-20).
Dr. Haller also advised avoiding progesterone-only or other combination oral contraceptives, most of which can worsen PMDD symptoms. The oral contraceptive Yaz (drospirenone 3 mg plus ethinyl estradiol 20 mcg) is an evidence-based option that is approved to treat PMDD.
In a double-blind, randomized placebo-controlled trial, 450 women with rigorously diagnosed PMDD spent 24 days on Yaz or placebo and 4 days on an inert pill per cycle for three menstrual cycles. The Yaz group had a significant 47% decrease in total symptom scores compared with a 38% decrease in the placebo group. Side effects, most commonly nausea and intermenstrual bleeding, prompted 15% on Yaz and 4% on placebo to drop out of the study (Obstet. Gynecol. 2005;106:492-501).
Significant PMS symptoms affect approximately 30% of women, but PMDD affects perhaps 3%-8%. PMDD typically starts in a woman’s 3rd decade (in her 20s) and worsens over time, Dr. Haller said. PMDD is a formal diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V). The illness reduces quality of life and level of functioning during the late luteal phase of the menstrual cycle, affecting relationships, work, or school.
"We miss this diagnosis a lot of the time," she said. Missed diagnosis rates for PMDD are estimated to be as high as 90%.
Conversely, approximately 40% of patients who think they have PMDD actually experience premenstrual exacerbations of bipolar disorder, major depression, anxiety, or other psychiatric disorders with symptoms that can get worse during the late luteal phase.
To diagnose PMDD, first rule out other psychiatric disorders and other medical disorders such as hypothyroidism, Dr. Haller advised. Then, have patients prospectively record their symptoms on a daily symptom diary to track associations with the menstrual cycle.
Dr. Haller reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Selective serotonin reuptake inhibitor antidepressants can alleviate symptoms of premenstrual syndrome or premenstrual dysphoric disorder, but are far from first-line therapies for either disorder, according to Dr. Ellen Haller.
The first steps in treating PMS and PMDD are basic wellness strategies such as a healthy diet, smoking cessation, exercise, adequate sleep, and stress management, Dr. Haller said at a conference on women’s health sponsored by the University of California, San Francisco.
Calcium supplementation also has been shown to reduce total emotional and physical symptom scores by 48% in women with PMS compared with a 30% reduction from placebo in a multicenter, randomized placebo-controlled study of 497 patients. That study used 600 mg, twice daily, of calcium carbonate or placebo for three menstrual cycles, said Dr. Haller, professor of clinical psychiatry at the university.
The results of that study (Am. J. Obstet.Gynecol. 1998;179:444-52) have not been replicated, she added.
If wellness treatments and calcium supplementation don’t work, the next step for treating women with PMS may be an SSRI. A Cochrane review of 31 randomized controlled trials found that SSRIs are more effective than placebo in treating PMS (Cochrane Database Syst. Rev. 2013;6:CD001396). Treatment should be an SSRI antidepressant, Dr. Haller emphasized. Bupropion, which is a norepinephrine dopamine reuptake inhibitor, is not effective for these women.
Low-dose SSRIs may be taken daily or can be effective against emotional and physical symptoms if taken only during the luteal phase of menstruation, starting on day 14 of the cycle and stopping on day 1, the first day of menses, Dr. Haller said. Patients with PMS tend to respond more quickly and at lower doses than patients with depression, and usually don’t get withdrawal symptoms when stopping the SSRI on the luteal-phase dosing regimen.
In women with PMDD, there is a preliminary suggestion that an SSRI may be more effective than calcium supplements. A pilot study of 39 women with PMDD found that the SSRI fluoxetine was more effective than calcium or placebo for PMDD, though scores were significantly better than calcium only on just two of five symptom scales. The study compared fluoxetine 10 mg b.i.d., calcium carbonate 600 mg b.i.d., and placebo (J. Clin. Psychopharmacol. 2013;33:614-20).
Dr. Haller also advised avoiding progesterone-only or other combination oral contraceptives, most of which can worsen PMDD symptoms. The oral contraceptive Yaz (drospirenone 3 mg plus ethinyl estradiol 20 mcg) is an evidence-based option that is approved to treat PMDD.
In a double-blind, randomized placebo-controlled trial, 450 women with rigorously diagnosed PMDD spent 24 days on Yaz or placebo and 4 days on an inert pill per cycle for three menstrual cycles. The Yaz group had a significant 47% decrease in total symptom scores compared with a 38% decrease in the placebo group. Side effects, most commonly nausea and intermenstrual bleeding, prompted 15% on Yaz and 4% on placebo to drop out of the study (Obstet. Gynecol. 2005;106:492-501).
Significant PMS symptoms affect approximately 30% of women, but PMDD affects perhaps 3%-8%. PMDD typically starts in a woman’s 3rd decade (in her 20s) and worsens over time, Dr. Haller said. PMDD is a formal diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V). The illness reduces quality of life and level of functioning during the late luteal phase of the menstrual cycle, affecting relationships, work, or school.
"We miss this diagnosis a lot of the time," she said. Missed diagnosis rates for PMDD are estimated to be as high as 90%.
Conversely, approximately 40% of patients who think they have PMDD actually experience premenstrual exacerbations of bipolar disorder, major depression, anxiety, or other psychiatric disorders with symptoms that can get worse during the late luteal phase.
To diagnose PMDD, first rule out other psychiatric disorders and other medical disorders such as hypothyroidism, Dr. Haller advised. Then, have patients prospectively record their symptoms on a daily symptom diary to track associations with the menstrual cycle.
Dr. Haller reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Selective serotonin reuptake inhibitor antidepressants can alleviate symptoms of premenstrual syndrome or premenstrual dysphoric disorder, but are far from first-line therapies for either disorder, according to Dr. Ellen Haller.
The first steps in treating PMS and PMDD are basic wellness strategies such as a healthy diet, smoking cessation, exercise, adequate sleep, and stress management, Dr. Haller said at a conference on women’s health sponsored by the University of California, San Francisco.
Calcium supplementation also has been shown to reduce total emotional and physical symptom scores by 48% in women with PMS compared with a 30% reduction from placebo in a multicenter, randomized placebo-controlled study of 497 patients. That study used 600 mg, twice daily, of calcium carbonate or placebo for three menstrual cycles, said Dr. Haller, professor of clinical psychiatry at the university.
The results of that study (Am. J. Obstet.Gynecol. 1998;179:444-52) have not been replicated, she added.
If wellness treatments and calcium supplementation don’t work, the next step for treating women with PMS may be an SSRI. A Cochrane review of 31 randomized controlled trials found that SSRIs are more effective than placebo in treating PMS (Cochrane Database Syst. Rev. 2013;6:CD001396). Treatment should be an SSRI antidepressant, Dr. Haller emphasized. Bupropion, which is a norepinephrine dopamine reuptake inhibitor, is not effective for these women.
Low-dose SSRIs may be taken daily or can be effective against emotional and physical symptoms if taken only during the luteal phase of menstruation, starting on day 14 of the cycle and stopping on day 1, the first day of menses, Dr. Haller said. Patients with PMS tend to respond more quickly and at lower doses than patients with depression, and usually don’t get withdrawal symptoms when stopping the SSRI on the luteal-phase dosing regimen.
In women with PMDD, there is a preliminary suggestion that an SSRI may be more effective than calcium supplements. A pilot study of 39 women with PMDD found that the SSRI fluoxetine was more effective than calcium or placebo for PMDD, though scores were significantly better than calcium only on just two of five symptom scales. The study compared fluoxetine 10 mg b.i.d., calcium carbonate 600 mg b.i.d., and placebo (J. Clin. Psychopharmacol. 2013;33:614-20).
Dr. Haller also advised avoiding progesterone-only or other combination oral contraceptives, most of which can worsen PMDD symptoms. The oral contraceptive Yaz (drospirenone 3 mg plus ethinyl estradiol 20 mcg) is an evidence-based option that is approved to treat PMDD.
In a double-blind, randomized placebo-controlled trial, 450 women with rigorously diagnosed PMDD spent 24 days on Yaz or placebo and 4 days on an inert pill per cycle for three menstrual cycles. The Yaz group had a significant 47% decrease in total symptom scores compared with a 38% decrease in the placebo group. Side effects, most commonly nausea and intermenstrual bleeding, prompted 15% on Yaz and 4% on placebo to drop out of the study (Obstet. Gynecol. 2005;106:492-501).
Significant PMS symptoms affect approximately 30% of women, but PMDD affects perhaps 3%-8%. PMDD typically starts in a woman’s 3rd decade (in her 20s) and worsens over time, Dr. Haller said. PMDD is a formal diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V). The illness reduces quality of life and level of functioning during the late luteal phase of the menstrual cycle, affecting relationships, work, or school.
"We miss this diagnosis a lot of the time," she said. Missed diagnosis rates for PMDD are estimated to be as high as 90%.
Conversely, approximately 40% of patients who think they have PMDD actually experience premenstrual exacerbations of bipolar disorder, major depression, anxiety, or other psychiatric disorders with symptoms that can get worse during the late luteal phase.
To diagnose PMDD, first rule out other psychiatric disorders and other medical disorders such as hypothyroidism, Dr. Haller advised. Then, have patients prospectively record their symptoms on a daily symptom diary to track associations with the menstrual cycle.
Dr. Haller reported having no relevant financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A CONFERENCE ON WOMEN’S HEALTH
Wide variation found in early pregnancy beta-HCG values
SAN FRANCISCO – Beta-HCG values can vary widely in early pregnancy, and should not be used in isolation to declare a pregnancy to be abnormal, according to Dr. Jody Steinauer.
In 366 women with vaginal bleeding or pain who went on to have a normal intrauterine pregnancy, the lowest level of beta-HCG at which an intrauterine pregnancy could be seen was 390 mIU/mL. The same study reported that women with beta-HCG levels as high as 3,510 mIU/mL in whom no gestational sac can be seen may still have normal pregnancies (Obstet. Gynecol. 2013;121:65-70).
The widely accepted upper cutoff value is 1,500-2,000 mIU/mL, Dr. Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco. Yet "it’s not a hard-and-fast rule. We have all heard of patients who had even higher beta-HCG levels and went on to have normal singleton pregnancies." On the lower end of beta-HCG values, the attitude may be "her beta-HCG is only 700 mIU/mL, so I’m not expecting to see a gestational sac" on ultrasound. Dr. Steinauer said.
In the current study, using a beta-HCG cutoff of 1,500 mIU/mL when no gestational sac can be seen would identify 80% of normal intrauterine pregnancies. A 2,000-mIU/mL cutoff would identify 91% of normal pregnancies. With either cutoff value, "there would have been a high proportion of normal pregnancies that were called abnormal," said Dr. Steinauer of the university.
New criteria released by the Society of Radiologists in Ultrasound for diagnosing a nonviable pregnancy early in the first trimester also address beta-HCG levels. If no gestational sac is visible at a beta-HCG level greater than 2,000 mIU/mL, an ectopic pregnancy is 19 times more likely than a viable pregnancy, but a nonviable intrauterine pregnancy still is twice as likely as an ectopic pregnancy (N. Engl. J. Med. 2013;369:1443-51).
Those estimates apply to the general U.S. population, Dr. Steinauer said, and may vary depending on patient population.
In women with beta-HCG levels of 2,000-3,000 mIU/mL, there will be 19 ectopic pregnancies and 38 nonviable pregnancies for every viable pregnancy. Yet as many as 2% of women with values this high can have viable pregnancies, according to the society’s criteria. Once the beta-HCG level climbs higher than 3,000 mIU/mL and no gestational sac is visible, an ectopic pregnancy is 70 times more likely than a viable pregnancy.
Ultrasound measurements of the yolk sac or fetal pole also can help diagnose early pregnancy loss, but these are more variable and thus less helpful than gestational sac measurements.
Studies have shown that when no embryo is seen with a mean gestational sac diameter of 2 mm, a diagnosis of early pregnancy loss will be false in 0.5% of cases in which no yolk sac is seen and in 0.4% of cases with a yolk sac. The false-positive rate approaches 0, however, with a mean gestational sac diameter of 21 mm, she said.
Several studies have shown that an inability to find cardiac activity when the fetal pole measures 5 mm does not confirm a diagnosis of early pregnancy loss because 8.3% of cases will be false positives under those criteria. A fetal pole measuring at least 5.3 mm with no cardiac activity, however, eliminates the possibility of a false-positive diagnosis.
The criteria released by the Society of Radiologists in Ultrasound express concern about the difficulty for an average ultrasonographer to detect fractions of millimeters in differences, so they allow a margin of error. The cutoff for a diagnosis of early pregnancy loss is extended to a mean gestational sac diameter of 25 mm with no embryo, or a fetal pole measuring 7 mm with no cardiac activity.
Dr. Steinauer reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Beta-HCG values can vary widely in early pregnancy, and should not be used in isolation to declare a pregnancy to be abnormal, according to Dr. Jody Steinauer.
In 366 women with vaginal bleeding or pain who went on to have a normal intrauterine pregnancy, the lowest level of beta-HCG at which an intrauterine pregnancy could be seen was 390 mIU/mL. The same study reported that women with beta-HCG levels as high as 3,510 mIU/mL in whom no gestational sac can be seen may still have normal pregnancies (Obstet. Gynecol. 2013;121:65-70).
The widely accepted upper cutoff value is 1,500-2,000 mIU/mL, Dr. Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco. Yet "it’s not a hard-and-fast rule. We have all heard of patients who had even higher beta-HCG levels and went on to have normal singleton pregnancies." On the lower end of beta-HCG values, the attitude may be "her beta-HCG is only 700 mIU/mL, so I’m not expecting to see a gestational sac" on ultrasound. Dr. Steinauer said.
In the current study, using a beta-HCG cutoff of 1,500 mIU/mL when no gestational sac can be seen would identify 80% of normal intrauterine pregnancies. A 2,000-mIU/mL cutoff would identify 91% of normal pregnancies. With either cutoff value, "there would have been a high proportion of normal pregnancies that were called abnormal," said Dr. Steinauer of the university.
New criteria released by the Society of Radiologists in Ultrasound for diagnosing a nonviable pregnancy early in the first trimester also address beta-HCG levels. If no gestational sac is visible at a beta-HCG level greater than 2,000 mIU/mL, an ectopic pregnancy is 19 times more likely than a viable pregnancy, but a nonviable intrauterine pregnancy still is twice as likely as an ectopic pregnancy (N. Engl. J. Med. 2013;369:1443-51).
Those estimates apply to the general U.S. population, Dr. Steinauer said, and may vary depending on patient population.
In women with beta-HCG levels of 2,000-3,000 mIU/mL, there will be 19 ectopic pregnancies and 38 nonviable pregnancies for every viable pregnancy. Yet as many as 2% of women with values this high can have viable pregnancies, according to the society’s criteria. Once the beta-HCG level climbs higher than 3,000 mIU/mL and no gestational sac is visible, an ectopic pregnancy is 70 times more likely than a viable pregnancy.
Ultrasound measurements of the yolk sac or fetal pole also can help diagnose early pregnancy loss, but these are more variable and thus less helpful than gestational sac measurements.
Studies have shown that when no embryo is seen with a mean gestational sac diameter of 2 mm, a diagnosis of early pregnancy loss will be false in 0.5% of cases in which no yolk sac is seen and in 0.4% of cases with a yolk sac. The false-positive rate approaches 0, however, with a mean gestational sac diameter of 21 mm, she said.
Several studies have shown that an inability to find cardiac activity when the fetal pole measures 5 mm does not confirm a diagnosis of early pregnancy loss because 8.3% of cases will be false positives under those criteria. A fetal pole measuring at least 5.3 mm with no cardiac activity, however, eliminates the possibility of a false-positive diagnosis.
The criteria released by the Society of Radiologists in Ultrasound express concern about the difficulty for an average ultrasonographer to detect fractions of millimeters in differences, so they allow a margin of error. The cutoff for a diagnosis of early pregnancy loss is extended to a mean gestational sac diameter of 25 mm with no embryo, or a fetal pole measuring 7 mm with no cardiac activity.
Dr. Steinauer reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Beta-HCG values can vary widely in early pregnancy, and should not be used in isolation to declare a pregnancy to be abnormal, according to Dr. Jody Steinauer.
In 366 women with vaginal bleeding or pain who went on to have a normal intrauterine pregnancy, the lowest level of beta-HCG at which an intrauterine pregnancy could be seen was 390 mIU/mL. The same study reported that women with beta-HCG levels as high as 3,510 mIU/mL in whom no gestational sac can be seen may still have normal pregnancies (Obstet. Gynecol. 2013;121:65-70).
The widely accepted upper cutoff value is 1,500-2,000 mIU/mL, Dr. Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco. Yet "it’s not a hard-and-fast rule. We have all heard of patients who had even higher beta-HCG levels and went on to have normal singleton pregnancies." On the lower end of beta-HCG values, the attitude may be "her beta-HCG is only 700 mIU/mL, so I’m not expecting to see a gestational sac" on ultrasound. Dr. Steinauer said.
In the current study, using a beta-HCG cutoff of 1,500 mIU/mL when no gestational sac can be seen would identify 80% of normal intrauterine pregnancies. A 2,000-mIU/mL cutoff would identify 91% of normal pregnancies. With either cutoff value, "there would have been a high proportion of normal pregnancies that were called abnormal," said Dr. Steinauer of the university.
New criteria released by the Society of Radiologists in Ultrasound for diagnosing a nonviable pregnancy early in the first trimester also address beta-HCG levels. If no gestational sac is visible at a beta-HCG level greater than 2,000 mIU/mL, an ectopic pregnancy is 19 times more likely than a viable pregnancy, but a nonviable intrauterine pregnancy still is twice as likely as an ectopic pregnancy (N. Engl. J. Med. 2013;369:1443-51).
Those estimates apply to the general U.S. population, Dr. Steinauer said, and may vary depending on patient population.
In women with beta-HCG levels of 2,000-3,000 mIU/mL, there will be 19 ectopic pregnancies and 38 nonviable pregnancies for every viable pregnancy. Yet as many as 2% of women with values this high can have viable pregnancies, according to the society’s criteria. Once the beta-HCG level climbs higher than 3,000 mIU/mL and no gestational sac is visible, an ectopic pregnancy is 70 times more likely than a viable pregnancy.
Ultrasound measurements of the yolk sac or fetal pole also can help diagnose early pregnancy loss, but these are more variable and thus less helpful than gestational sac measurements.
Studies have shown that when no embryo is seen with a mean gestational sac diameter of 2 mm, a diagnosis of early pregnancy loss will be false in 0.5% of cases in which no yolk sac is seen and in 0.4% of cases with a yolk sac. The false-positive rate approaches 0, however, with a mean gestational sac diameter of 21 mm, she said.
Several studies have shown that an inability to find cardiac activity when the fetal pole measures 5 mm does not confirm a diagnosis of early pregnancy loss because 8.3% of cases will be false positives under those criteria. A fetal pole measuring at least 5.3 mm with no cardiac activity, however, eliminates the possibility of a false-positive diagnosis.
The criteria released by the Society of Radiologists in Ultrasound express concern about the difficulty for an average ultrasonographer to detect fractions of millimeters in differences, so they allow a margin of error. The cutoff for a diagnosis of early pregnancy loss is extended to a mean gestational sac diameter of 25 mm with no embryo, or a fetal pole measuring 7 mm with no cardiac activity.
Dr. Steinauer reported having no relevant financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A CONFERENCE ON WOMEN’S HEALTH
CDC Resources Aid Contraceptive Selection
SAN FRANCISCO – Pop quiz: Do you know which contraceptive methods are safe for women who are postpartum or who smoke? How about for women who have diabetic nephropathy or migraine with aura?
Handy online tools and smart-phone apps from the Centers for Disease Control and Prevention now offer recommendations for contraceptive choices. The U.S. Medical Eligibility Criteria for Contraception, or MEC (MMWR 2010;59:1-6), now has a newer companion document, the U.S. Selected Practice Recommendations for Contraception, released by the U.S. Centers for Disease Control and Prevention (MMWR 2013;62:1-46), Dr. Jody Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco.
The U.S. version of the MEC features four color-coded tables that compare contraceptive methods and more than 60 medical conditions or characteristics. Each pair of method and condition is scored for safety on a scale of 1-4.
A score of 1 (color-coded dark green) means there are no concerns about the method to be used in that scenario. A score of 2 (light green) means that generally the advantages outweigh the risks of the method, said Dr. Steinauer, of the university.
A score of 3 (pink) suggests there is a "relative contraindication" in which there are some concerns, but the advantages of using that contraceptive method outweigh the risks for that patient. "You might talk with the woman about using a different method and if she decides to use the method with a 3 score, you would counsel her about the risks but would still prescribe it," she said. A score of 4 (red) means there’s an absolute contraindication to the method for that condition.
The MEC is available in an app for iPhone or iPad. The app lists choices by condition or by method; the online tables can be printed out and the options viewed all at once, she said.
"We have these hanging around at our clinic, and all of the residents carry them on their iPhones as well," she said. "It’s a really useful document."
The companion Selected Practice Recommendations for Contraception provide advice on how to use contraceptive methods in clinical practice. For example, there are recommendations on how long to use a backup contraceptive method once it has been started, special considerations for each method, and what to do when there are missed or late doses.
Dr. Steinauer reported having no financial disclosures,
On Twitter @sherryboschert
SAN FRANCISCO – Pop quiz: Do you know which contraceptive methods are safe for women who are postpartum or who smoke? How about for women who have diabetic nephropathy or migraine with aura?
Handy online tools and smart-phone apps from the Centers for Disease Control and Prevention now offer recommendations for contraceptive choices. The U.S. Medical Eligibility Criteria for Contraception, or MEC (MMWR 2010;59:1-6), now has a newer companion document, the U.S. Selected Practice Recommendations for Contraception, released by the U.S. Centers for Disease Control and Prevention (MMWR 2013;62:1-46), Dr. Jody Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco.
The U.S. version of the MEC features four color-coded tables that compare contraceptive methods and more than 60 medical conditions or characteristics. Each pair of method and condition is scored for safety on a scale of 1-4.
A score of 1 (color-coded dark green) means there are no concerns about the method to be used in that scenario. A score of 2 (light green) means that generally the advantages outweigh the risks of the method, said Dr. Steinauer, of the university.
A score of 3 (pink) suggests there is a "relative contraindication" in which there are some concerns, but the advantages of using that contraceptive method outweigh the risks for that patient. "You might talk with the woman about using a different method and if she decides to use the method with a 3 score, you would counsel her about the risks but would still prescribe it," she said. A score of 4 (red) means there’s an absolute contraindication to the method for that condition.
The MEC is available in an app for iPhone or iPad. The app lists choices by condition or by method; the online tables can be printed out and the options viewed all at once, she said.
"We have these hanging around at our clinic, and all of the residents carry them on their iPhones as well," she said. "It’s a really useful document."
The companion Selected Practice Recommendations for Contraception provide advice on how to use contraceptive methods in clinical practice. For example, there are recommendations on how long to use a backup contraceptive method once it has been started, special considerations for each method, and what to do when there are missed or late doses.
Dr. Steinauer reported having no financial disclosures,
On Twitter @sherryboschert
SAN FRANCISCO – Pop quiz: Do you know which contraceptive methods are safe for women who are postpartum or who smoke? How about for women who have diabetic nephropathy or migraine with aura?
Handy online tools and smart-phone apps from the Centers for Disease Control and Prevention now offer recommendations for contraceptive choices. The U.S. Medical Eligibility Criteria for Contraception, or MEC (MMWR 2010;59:1-6), now has a newer companion document, the U.S. Selected Practice Recommendations for Contraception, released by the U.S. Centers for Disease Control and Prevention (MMWR 2013;62:1-46), Dr. Jody Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco.
The U.S. version of the MEC features four color-coded tables that compare contraceptive methods and more than 60 medical conditions or characteristics. Each pair of method and condition is scored for safety on a scale of 1-4.
A score of 1 (color-coded dark green) means there are no concerns about the method to be used in that scenario. A score of 2 (light green) means that generally the advantages outweigh the risks of the method, said Dr. Steinauer, of the university.
A score of 3 (pink) suggests there is a "relative contraindication" in which there are some concerns, but the advantages of using that contraceptive method outweigh the risks for that patient. "You might talk with the woman about using a different method and if she decides to use the method with a 3 score, you would counsel her about the risks but would still prescribe it," she said. A score of 4 (red) means there’s an absolute contraindication to the method for that condition.
The MEC is available in an app for iPhone or iPad. The app lists choices by condition or by method; the online tables can be printed out and the options viewed all at once, she said.
"We have these hanging around at our clinic, and all of the residents carry them on their iPhones as well," she said. "It’s a really useful document."
The companion Selected Practice Recommendations for Contraception provide advice on how to use contraceptive methods in clinical practice. For example, there are recommendations on how long to use a backup contraceptive method once it has been started, special considerations for each method, and what to do when there are missed or late doses.
Dr. Steinauer reported having no financial disclosures,
On Twitter @sherryboschert
EXPERT ANALYSIS AT A CONFERENCE ON WOMEN’S HEALTH
CDC resources aid contraceptive selection
SAN FRANCISCO – Pop quiz: Do you know which contraceptive methods are safe for women who are postpartum or who smoke? How about for women who have diabetic nephropathy or migraine with aura?
Handy online tools and smart-phone apps from the Centers for Disease Control and Prevention now offer recommendations for contraceptive choices. The U.S. Medical Eligibility Criteria for Contraception, or MEC (MMWR 2010;59:1-6), now has a newer companion document, the U.S. Selected Practice Recommendations for Contraception, released by the U.S. Centers for Disease Control and Prevention (MMWR 2013;62:1-46), Dr. Jody Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco.
The U.S. version of the MEC features four color-coded tables that compare contraceptive methods and more than 60 medical conditions or characteristics. Each pair of method and condition is scored for safety on a scale of 1-4.
A score of 1 (color-coded dark green) means there are no concerns about the method to be used in that scenario. A score of 2 (light green) means that generally the advantages outweigh the risks of the method, said Dr. Steinauer, of the university.
A score of 3 (pink) suggests there is a "relative contraindication" in which there are some concerns, but the advantages of using that contraceptive method outweigh the risks for that patient. "You might talk with the woman about using a different method and if she decides to use the method with a 3 score, you would counsel her about the risks but would still prescribe it," she said. A score of 4 (red) means there’s an absolute contraindication to the method for that condition.
The MEC is available in an app for iPhone or iPad. The app lists choices by condition or by method; the online tables can be printed out and the options viewed all at once, she said.
"We have these hanging around at our clinic, and all of the residents carry them on their iPhones as well," she said. "It’s a really useful document."
The companion Selected Practice Recommendations for Contraception provide advice on how to use contraceptive methods in clinical practice. For example, there are recommendations on how long to use a backup contraceptive method once it has been started, special considerations for each method, and what to do when there are missed or late doses.
Dr. Steinauer reported having no financial disclosures,
On Twitter @sherryboschert
SAN FRANCISCO – Pop quiz: Do you know which contraceptive methods are safe for women who are postpartum or who smoke? How about for women who have diabetic nephropathy or migraine with aura?
Handy online tools and smart-phone apps from the Centers for Disease Control and Prevention now offer recommendations for contraceptive choices. The U.S. Medical Eligibility Criteria for Contraception, or MEC (MMWR 2010;59:1-6), now has a newer companion document, the U.S. Selected Practice Recommendations for Contraception, released by the U.S. Centers for Disease Control and Prevention (MMWR 2013;62:1-46), Dr. Jody Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco.
The U.S. version of the MEC features four color-coded tables that compare contraceptive methods and more than 60 medical conditions or characteristics. Each pair of method and condition is scored for safety on a scale of 1-4.
A score of 1 (color-coded dark green) means there are no concerns about the method to be used in that scenario. A score of 2 (light green) means that generally the advantages outweigh the risks of the method, said Dr. Steinauer, of the university.
A score of 3 (pink) suggests there is a "relative contraindication" in which there are some concerns, but the advantages of using that contraceptive method outweigh the risks for that patient. "You might talk with the woman about using a different method and if she decides to use the method with a 3 score, you would counsel her about the risks but would still prescribe it," she said. A score of 4 (red) means there’s an absolute contraindication to the method for that condition.
The MEC is available in an app for iPhone or iPad. The app lists choices by condition or by method; the online tables can be printed out and the options viewed all at once, she said.
"We have these hanging around at our clinic, and all of the residents carry them on their iPhones as well," she said. "It’s a really useful document."
The companion Selected Practice Recommendations for Contraception provide advice on how to use contraceptive methods in clinical practice. For example, there are recommendations on how long to use a backup contraceptive method once it has been started, special considerations for each method, and what to do when there are missed or late doses.
Dr. Steinauer reported having no financial disclosures,
On Twitter @sherryboschert
SAN FRANCISCO – Pop quiz: Do you know which contraceptive methods are safe for women who are postpartum or who smoke? How about for women who have diabetic nephropathy or migraine with aura?
Handy online tools and smart-phone apps from the Centers for Disease Control and Prevention now offer recommendations for contraceptive choices. The U.S. Medical Eligibility Criteria for Contraception, or MEC (MMWR 2010;59:1-6), now has a newer companion document, the U.S. Selected Practice Recommendations for Contraception, released by the U.S. Centers for Disease Control and Prevention (MMWR 2013;62:1-46), Dr. Jody Steinauer said at a conference on women’s health sponsored by the University of California, San Francisco.
The U.S. version of the MEC features four color-coded tables that compare contraceptive methods and more than 60 medical conditions or characteristics. Each pair of method and condition is scored for safety on a scale of 1-4.
A score of 1 (color-coded dark green) means there are no concerns about the method to be used in that scenario. A score of 2 (light green) means that generally the advantages outweigh the risks of the method, said Dr. Steinauer, of the university.
A score of 3 (pink) suggests there is a "relative contraindication" in which there are some concerns, but the advantages of using that contraceptive method outweigh the risks for that patient. "You might talk with the woman about using a different method and if she decides to use the method with a 3 score, you would counsel her about the risks but would still prescribe it," she said. A score of 4 (red) means there’s an absolute contraindication to the method for that condition.
The MEC is available in an app for iPhone or iPad. The app lists choices by condition or by method; the online tables can be printed out and the options viewed all at once, she said.
"We have these hanging around at our clinic, and all of the residents carry them on their iPhones as well," she said. "It’s a really useful document."
The companion Selected Practice Recommendations for Contraception provide advice on how to use contraceptive methods in clinical practice. For example, there are recommendations on how long to use a backup contraceptive method once it has been started, special considerations for each method, and what to do when there are missed or late doses.
Dr. Steinauer reported having no financial disclosures,
On Twitter @sherryboschert
EXPERT ANALYSIS AT A CONFERENCE ON WOMEN’S HEALTH
Outcomes at 1 year similar for Resolute Integrity and BioMatrix Flex stents
SAN FRANCISCO – Major adverse cardiac events were comparable at 5.3% of 1,502 patients who received a zotarolimus-eluting stent with a permanent polymer coating and 5.1% of 1,497 patients who received a biolimus-eluting stent with a biodegradable polymer coating in a population-based randomized trial.
The 1-year outcomes in the Scandinavian study, known as the SORT-OUT VI trial, showed that the Resolute Integrity zotarolimus-eluting stent is noninferior to the BioMatrix Flex Biolimus A9-eluting stent. The trial results represent the first large comparison study of the two systems that included all comers, Dr. Bent Raungaard said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The primary outcome measure was a composite of cardiac death, myocardial infarction (not clearly attributable to a nontarget lesion), or target lesion revascularization within a year of stent implantation. The study enrolled adults with chronic stable coronary artery disease or acute coronary syndromes who had at least one coronary lesion with more than 50% diameter stenosis in a vessel with a reference diameter of 2.25-4 mm and who were undergoing percutaneous coronary intervention (PCI).
At the 1-year follow-up, cardiac death rates were 1.5% with the Resolute Integrity stent and 1.7% with the BioMatrix Flex stent, and the rates of MI were 1.3% and 0.9%, respectively, reported Dr. Raungaard of Aalborg (Denmark) University Hospital and his associates. Rates of target lesion revascularization were 3.5% with the Resolute Integrity stent and 3.1% with the BioMatrix Flex stent.
Rates were similar between groups at 1 year for target vessel revascularization (4.5% with Resolute Integrity and 4.7% with BioMatrix Flex), definite stent thrombosis (0.6% and 0.4%, respectively), and definite or probable stent thrombosis (0.8% and 0.5%, respectively).
"Both the zotarolimus-eluting stents and the biolimus-eluting stents were associated with low rates of major adverse cardiac events," Dr. Raungaard said.
Dr. Gregg W. Stone, moderator of the session for Dr. Raungaard’s presentation, noted that the major cardiac event rates were about what investigators had predicted for the zotarolimus-eluting stent and lower than predicted for the biolimus-eluting stent. "The take-home message here is that event rates were very low," said Dr. Stone, director of cardiovascular research and education at the Center for Interventional Vascular Therapy at New York-Presbyterian Hospital/Columbia University Medical Center. "I guess this begs the fact that we may need to start looking at higher-risk populations to bring out the differences between the devices," he said.
Baseline characteristics of patients were similar between groups, except that a significantly higher proportion of patients in the BioMatrix Flex group had undergone prior PCI (22%) compared with the Resolute Integrity group (19%), he said at the meeting, cosponsored by the American College of Cardiology. A higher proportion of patients in the Resolute Integrity group had more than one coronary lesion (25%) compared with the BioMatrix Flex group (22%). Total stent length per patient was significantly longer in the Resolute Integrity group (21 mm) than in the BioMatrix Flex group (18 mm).
The trial excluded patients who were expected to die within a year, who could not provide written informed consent, or who were deemed to be at unacceptable risk if put on 12 months of dual antiplatelet treatment. It also excluded patients who were allergic to aspirin, clopidogrel, prasugrel, ticagrelor, zotarolimus, or biolimus.
The study was funded by Biosensors Interventional Technologies, which makes the biolimus-eluting biodegradable stent, and by Medtronic CardioVascular, which makes the zotarolimus-eluting permanent polymer stent. Dr. Raungaard reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – Major adverse cardiac events were comparable at 5.3% of 1,502 patients who received a zotarolimus-eluting stent with a permanent polymer coating and 5.1% of 1,497 patients who received a biolimus-eluting stent with a biodegradable polymer coating in a population-based randomized trial.
The 1-year outcomes in the Scandinavian study, known as the SORT-OUT VI trial, showed that the Resolute Integrity zotarolimus-eluting stent is noninferior to the BioMatrix Flex Biolimus A9-eluting stent. The trial results represent the first large comparison study of the two systems that included all comers, Dr. Bent Raungaard said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The primary outcome measure was a composite of cardiac death, myocardial infarction (not clearly attributable to a nontarget lesion), or target lesion revascularization within a year of stent implantation. The study enrolled adults with chronic stable coronary artery disease or acute coronary syndromes who had at least one coronary lesion with more than 50% diameter stenosis in a vessel with a reference diameter of 2.25-4 mm and who were undergoing percutaneous coronary intervention (PCI).
At the 1-year follow-up, cardiac death rates were 1.5% with the Resolute Integrity stent and 1.7% with the BioMatrix Flex stent, and the rates of MI were 1.3% and 0.9%, respectively, reported Dr. Raungaard of Aalborg (Denmark) University Hospital and his associates. Rates of target lesion revascularization were 3.5% with the Resolute Integrity stent and 3.1% with the BioMatrix Flex stent.
Rates were similar between groups at 1 year for target vessel revascularization (4.5% with Resolute Integrity and 4.7% with BioMatrix Flex), definite stent thrombosis (0.6% and 0.4%, respectively), and definite or probable stent thrombosis (0.8% and 0.5%, respectively).
"Both the zotarolimus-eluting stents and the biolimus-eluting stents were associated with low rates of major adverse cardiac events," Dr. Raungaard said.
Dr. Gregg W. Stone, moderator of the session for Dr. Raungaard’s presentation, noted that the major cardiac event rates were about what investigators had predicted for the zotarolimus-eluting stent and lower than predicted for the biolimus-eluting stent. "The take-home message here is that event rates were very low," said Dr. Stone, director of cardiovascular research and education at the Center for Interventional Vascular Therapy at New York-Presbyterian Hospital/Columbia University Medical Center. "I guess this begs the fact that we may need to start looking at higher-risk populations to bring out the differences between the devices," he said.
Baseline characteristics of patients were similar between groups, except that a significantly higher proportion of patients in the BioMatrix Flex group had undergone prior PCI (22%) compared with the Resolute Integrity group (19%), he said at the meeting, cosponsored by the American College of Cardiology. A higher proportion of patients in the Resolute Integrity group had more than one coronary lesion (25%) compared with the BioMatrix Flex group (22%). Total stent length per patient was significantly longer in the Resolute Integrity group (21 mm) than in the BioMatrix Flex group (18 mm).
The trial excluded patients who were expected to die within a year, who could not provide written informed consent, or who were deemed to be at unacceptable risk if put on 12 months of dual antiplatelet treatment. It also excluded patients who were allergic to aspirin, clopidogrel, prasugrel, ticagrelor, zotarolimus, or biolimus.
The study was funded by Biosensors Interventional Technologies, which makes the biolimus-eluting biodegradable stent, and by Medtronic CardioVascular, which makes the zotarolimus-eluting permanent polymer stent. Dr. Raungaard reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – Major adverse cardiac events were comparable at 5.3% of 1,502 patients who received a zotarolimus-eluting stent with a permanent polymer coating and 5.1% of 1,497 patients who received a biolimus-eluting stent with a biodegradable polymer coating in a population-based randomized trial.
The 1-year outcomes in the Scandinavian study, known as the SORT-OUT VI trial, showed that the Resolute Integrity zotarolimus-eluting stent is noninferior to the BioMatrix Flex Biolimus A9-eluting stent. The trial results represent the first large comparison study of the two systems that included all comers, Dr. Bent Raungaard said at the Transcatheter Cardiovascular Therapeutics annual meeting.
The primary outcome measure was a composite of cardiac death, myocardial infarction (not clearly attributable to a nontarget lesion), or target lesion revascularization within a year of stent implantation. The study enrolled adults with chronic stable coronary artery disease or acute coronary syndromes who had at least one coronary lesion with more than 50% diameter stenosis in a vessel with a reference diameter of 2.25-4 mm and who were undergoing percutaneous coronary intervention (PCI).
At the 1-year follow-up, cardiac death rates were 1.5% with the Resolute Integrity stent and 1.7% with the BioMatrix Flex stent, and the rates of MI were 1.3% and 0.9%, respectively, reported Dr. Raungaard of Aalborg (Denmark) University Hospital and his associates. Rates of target lesion revascularization were 3.5% with the Resolute Integrity stent and 3.1% with the BioMatrix Flex stent.
Rates were similar between groups at 1 year for target vessel revascularization (4.5% with Resolute Integrity and 4.7% with BioMatrix Flex), definite stent thrombosis (0.6% and 0.4%, respectively), and definite or probable stent thrombosis (0.8% and 0.5%, respectively).
"Both the zotarolimus-eluting stents and the biolimus-eluting stents were associated with low rates of major adverse cardiac events," Dr. Raungaard said.
Dr. Gregg W. Stone, moderator of the session for Dr. Raungaard’s presentation, noted that the major cardiac event rates were about what investigators had predicted for the zotarolimus-eluting stent and lower than predicted for the biolimus-eluting stent. "The take-home message here is that event rates were very low," said Dr. Stone, director of cardiovascular research and education at the Center for Interventional Vascular Therapy at New York-Presbyterian Hospital/Columbia University Medical Center. "I guess this begs the fact that we may need to start looking at higher-risk populations to bring out the differences between the devices," he said.
Baseline characteristics of patients were similar between groups, except that a significantly higher proportion of patients in the BioMatrix Flex group had undergone prior PCI (22%) compared with the Resolute Integrity group (19%), he said at the meeting, cosponsored by the American College of Cardiology. A higher proportion of patients in the Resolute Integrity group had more than one coronary lesion (25%) compared with the BioMatrix Flex group (22%). Total stent length per patient was significantly longer in the Resolute Integrity group (21 mm) than in the BioMatrix Flex group (18 mm).
The trial excluded patients who were expected to die within a year, who could not provide written informed consent, or who were deemed to be at unacceptable risk if put on 12 months of dual antiplatelet treatment. It also excluded patients who were allergic to aspirin, clopidogrel, prasugrel, ticagrelor, zotarolimus, or biolimus.
The study was funded by Biosensors Interventional Technologies, which makes the biolimus-eluting biodegradable stent, and by Medtronic CardioVascular, which makes the zotarolimus-eluting permanent polymer stent. Dr. Raungaard reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
AT TCT 2013
Major finding: Rates of major adverse cardiac events at 1 year were 5.3% with the Resolute Integrity stent and 5.1% with the BioMatrix Flex stent.
Data source: A randomized, population-based, multicenter, noninferiority study of 2,999 patients with stable coronary artery disease or acute coronary syndrome undergoing PCI.
Disclosures: The study was funded by Biosensors Interventional Technologies, which makes the biolimus-eluting biodegradable stent, and by Medtronic CardioVascular, which makes the zotarolimus-eluting permanent polymer stent. Dr. Raungaard reported having no financial disclosures.
Expert prefers questionnaire for diagnosing fibromyalgia
SAN FRANCISCO – A two-page questionnaire is more helpful than a tender-point exam for diagnosing fibromyalgia in clinical practice, according to Dr. Andrew Gross.
Tender point exams – pressing on the 18 tender points of the body as advised in the American College of Rheumatology’s fibromyalgia classification criteria – can make even healthy people flinch in pain. The exam may be useful when enrolling patients in studies, but "for the most part, I find this a complete waste of time," he said at a conference on women’s health sponsored by the University of California, San Francisco.
*Instead, Dr. Gross hands patients with suspected fibromyalgia a brief questionnaire based on the ACR’s modified Diagnostic Criteria for Fibromyalgia (J. Rheumatol. 2001;38:1113-22) and steps out of the room while the patient completes the form."I use this in clinical practice all the time," said Dr. Gross, director of the Rheumatology Clinic at the university.
Patients fill out the questionnaire by checking off areas of the body in which they’ve experienced pain in the past week (the Widespread Pain Index). Dr. Gross also asks patients to provide information about the severity of their symptoms using a scale of 0-3 (none to severe) to quantify their degree of fatigue, extent of waking from sleep feeling unrefreshed, and cognitive symptoms, giving a symptom severity score. He then reviews the questionnaire with patients to understand the extent and severity of symptoms, and often diagnoses fibromyalgia when he determines there is a widespread pain score of 7 or more areas of the body plus a symptom severity score of at least 5.
Dr. Gross gives the questionnaire to patients who have the three hallmarks of fibromyalgia – widespread pain present for longer than 3 months, fatigue, and poor sleep. "If someone has pain in multiple areas, right away I’m thinking about fibromyalgia," he said.
Other tip-offs to fibromyalgia include cognitive problems, pain unrelieved by changing the body’s position, or the complaint that a specific activity had consequences. For example, "I helped my sister move the other day and I was in bed for a week." Odd complaints are another tip-off. One patient recently told him, "My body feels like it has tinnitus."
Before diagnosing fibromyalgia, Dr. Gross evaluates the patient for other medical conditions that can cause pain and/or fatigue. In addition to a comprehensive patient interview and physical examination, he orders a limited panel of blood tests to evaluate for other conditions. These include tests for erythrocyte sedimentation rate and C-reactive protein tests, a CBC, a comprehensive metabolic panel, a fasting glucose test, thyroid hormone tests, hepatitis B and C tests, and in some populations an HIV test. He checks vitamin D levels because vitamin D deficiency can aggravate pain, though it doesn’t cause it. If the patient is having weakness, he’ll check the creatinine phosphokinase level. In rare cases he’ll test for antinuclear antibodies. He’ll sometimes order x-rays of affected areas to look for joint damage, and he biopsies skin lesions that are concerning, particularly rashes. If there are many persistent neurologic symptoms, he may order an electromyogram.
Multiple studies have shown that the number of medical tests and costs increase over time for patients with undiagnosed fibromyalgia but level off or decrease once the diagnosis is made. "People stop looking for Lyme disease or multiple sclerosis or whatever," he said.
Dr. Gross reported having no relevant financial disclosures.
*CLARIFICATION: This story was revised on 1/15/2014 to include new information provided by Dr. Gross after publication.
On Twitter @sherryboschert
SAN FRANCISCO – A two-page questionnaire is more helpful than a tender-point exam for diagnosing fibromyalgia in clinical practice, according to Dr. Andrew Gross.
Tender point exams – pressing on the 18 tender points of the body as advised in the American College of Rheumatology’s fibromyalgia classification criteria – can make even healthy people flinch in pain. The exam may be useful when enrolling patients in studies, but "for the most part, I find this a complete waste of time," he said at a conference on women’s health sponsored by the University of California, San Francisco.
*Instead, Dr. Gross hands patients with suspected fibromyalgia a brief questionnaire based on the ACR’s modified Diagnostic Criteria for Fibromyalgia (J. Rheumatol. 2001;38:1113-22) and steps out of the room while the patient completes the form."I use this in clinical practice all the time," said Dr. Gross, director of the Rheumatology Clinic at the university.
Patients fill out the questionnaire by checking off areas of the body in which they’ve experienced pain in the past week (the Widespread Pain Index). Dr. Gross also asks patients to provide information about the severity of their symptoms using a scale of 0-3 (none to severe) to quantify their degree of fatigue, extent of waking from sleep feeling unrefreshed, and cognitive symptoms, giving a symptom severity score. He then reviews the questionnaire with patients to understand the extent and severity of symptoms, and often diagnoses fibromyalgia when he determines there is a widespread pain score of 7 or more areas of the body plus a symptom severity score of at least 5.
Dr. Gross gives the questionnaire to patients who have the three hallmarks of fibromyalgia – widespread pain present for longer than 3 months, fatigue, and poor sleep. "If someone has pain in multiple areas, right away I’m thinking about fibromyalgia," he said.
Other tip-offs to fibromyalgia include cognitive problems, pain unrelieved by changing the body’s position, or the complaint that a specific activity had consequences. For example, "I helped my sister move the other day and I was in bed for a week." Odd complaints are another tip-off. One patient recently told him, "My body feels like it has tinnitus."
Before diagnosing fibromyalgia, Dr. Gross evaluates the patient for other medical conditions that can cause pain and/or fatigue. In addition to a comprehensive patient interview and physical examination, he orders a limited panel of blood tests to evaluate for other conditions. These include tests for erythrocyte sedimentation rate and C-reactive protein tests, a CBC, a comprehensive metabolic panel, a fasting glucose test, thyroid hormone tests, hepatitis B and C tests, and in some populations an HIV test. He checks vitamin D levels because vitamin D deficiency can aggravate pain, though it doesn’t cause it. If the patient is having weakness, he’ll check the creatinine phosphokinase level. In rare cases he’ll test for antinuclear antibodies. He’ll sometimes order x-rays of affected areas to look for joint damage, and he biopsies skin lesions that are concerning, particularly rashes. If there are many persistent neurologic symptoms, he may order an electromyogram.
Multiple studies have shown that the number of medical tests and costs increase over time for patients with undiagnosed fibromyalgia but level off or decrease once the diagnosis is made. "People stop looking for Lyme disease or multiple sclerosis or whatever," he said.
Dr. Gross reported having no relevant financial disclosures.
*CLARIFICATION: This story was revised on 1/15/2014 to include new information provided by Dr. Gross after publication.
On Twitter @sherryboschert
SAN FRANCISCO – A two-page questionnaire is more helpful than a tender-point exam for diagnosing fibromyalgia in clinical practice, according to Dr. Andrew Gross.
Tender point exams – pressing on the 18 tender points of the body as advised in the American College of Rheumatology’s fibromyalgia classification criteria – can make even healthy people flinch in pain. The exam may be useful when enrolling patients in studies, but "for the most part, I find this a complete waste of time," he said at a conference on women’s health sponsored by the University of California, San Francisco.
*Instead, Dr. Gross hands patients with suspected fibromyalgia a brief questionnaire based on the ACR’s modified Diagnostic Criteria for Fibromyalgia (J. Rheumatol. 2001;38:1113-22) and steps out of the room while the patient completes the form."I use this in clinical practice all the time," said Dr. Gross, director of the Rheumatology Clinic at the university.
Patients fill out the questionnaire by checking off areas of the body in which they’ve experienced pain in the past week (the Widespread Pain Index). Dr. Gross also asks patients to provide information about the severity of their symptoms using a scale of 0-3 (none to severe) to quantify their degree of fatigue, extent of waking from sleep feeling unrefreshed, and cognitive symptoms, giving a symptom severity score. He then reviews the questionnaire with patients to understand the extent and severity of symptoms, and often diagnoses fibromyalgia when he determines there is a widespread pain score of 7 or more areas of the body plus a symptom severity score of at least 5.
Dr. Gross gives the questionnaire to patients who have the three hallmarks of fibromyalgia – widespread pain present for longer than 3 months, fatigue, and poor sleep. "If someone has pain in multiple areas, right away I’m thinking about fibromyalgia," he said.
Other tip-offs to fibromyalgia include cognitive problems, pain unrelieved by changing the body’s position, or the complaint that a specific activity had consequences. For example, "I helped my sister move the other day and I was in bed for a week." Odd complaints are another tip-off. One patient recently told him, "My body feels like it has tinnitus."
Before diagnosing fibromyalgia, Dr. Gross evaluates the patient for other medical conditions that can cause pain and/or fatigue. In addition to a comprehensive patient interview and physical examination, he orders a limited panel of blood tests to evaluate for other conditions. These include tests for erythrocyte sedimentation rate and C-reactive protein tests, a CBC, a comprehensive metabolic panel, a fasting glucose test, thyroid hormone tests, hepatitis B and C tests, and in some populations an HIV test. He checks vitamin D levels because vitamin D deficiency can aggravate pain, though it doesn’t cause it. If the patient is having weakness, he’ll check the creatinine phosphokinase level. In rare cases he’ll test for antinuclear antibodies. He’ll sometimes order x-rays of affected areas to look for joint damage, and he biopsies skin lesions that are concerning, particularly rashes. If there are many persistent neurologic symptoms, he may order an electromyogram.
Multiple studies have shown that the number of medical tests and costs increase over time for patients with undiagnosed fibromyalgia but level off or decrease once the diagnosis is made. "People stop looking for Lyme disease or multiple sclerosis or whatever," he said.
Dr. Gross reported having no relevant financial disclosures.
*CLARIFICATION: This story was revised on 1/15/2014 to include new information provided by Dr. Gross after publication.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A CONFERENCE ON WOMEN’S HEALTH
Transradial PCI seems feasible in women
SAN FRANCISCO – Rates of bleeding or vascular complications in women undergoing percutaneous coronary intervention were 59% lower using radial access, compared with femoral access, a difference that did not reach statistical significance in a randomized study of 1,787 patients.
Bleeding or vascular complications within 72 hours or at hospital discharge were seen in 1.2% of 345 women who had transradial percutaneous coronary intervention (PCI) and 2.9% of 345 women who had transfemoral PCI, Dr. Sunil V. Rao reported at the Trans-catheter Cardiovascular Therapeutics annual meeting.
Although that difference was not statistically significant in this prespecified analysis of patients who actually underwent PCI, the rate of bleeding and vascular complications was significantly lower for the group randomized to radial access in an analysis of the whole cohort, regardless of whether they had PCI or just diagnostic catheterization. Bleeding and vascular complication rates were 0.6% in those randomized to radial access and 1.7% in those randomized to femoral access.
In both the PCI cohort and the total cohort, significantly more women in the radial group needed to cross over to femoral access for PCI compared with the crossover rate in the femoral group. In the PCI cohort, 6.1% of the radial group crossed over, as did 1.7% of the femoral group. In the total cohort, crossover was needed in 6.7% of the radial group and 1.9% of the femoral group, said Dr. Rao of Duke University, Durham, N.C. The main reason for crossover from radial to femoral access was radial artery spasm, in 43% of cases.
The Study of Access Site for Enhancement of PCI for Women (SAFE-PCI) leveraged data from the National Cardiovascular Data Registry’s CathPCI Registry from 60 institutions on adult women undergoing elective or urgent PCI or undergoing diagnostic angiography to evaluate ischemic symptoms with the possibility of PCI. The primary outcome measure was Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding events and vascular complications requiring intervention.
The investigators had planned to randomize 3,000 women to obtain 1,800 who underwent PCI, but a routine review after randomizing 1,120 patients suggested that the trial would be too small to show a difference because of lower-than-expected bleeding rates. Because no harm was noted in either the radial or femoral group, the investigators continued until they had enough patients for a quality-of-life substudy, then prematurely discontinued the trial.
The reduction in bleeding with the radial approach was similar to reductions seen in previous studies, Dr. Rao said at the meeting, cosponsored by the American College of Cardiology. The conversion rate from radial to femoral access was similar to the 7.6% rate reported in a prior trial (Lancet 2011;377:1409-20).
Compared with men, women have an increased risk for bleeding from antithrombotic therapy and from femoral access for PCI. Radial access can decrease bleeding risk, but trans-radial PCI has been less common in women, in part because they have smaller radial arteries.
The current trial’s results suggest that "an initial strategy of radial access is reasonable and may be preferred by some operators for women undergoing cardiac catheterization or PCI, with the recognition that a proportion of patients will require conversion to femoral access," he said.
Women preferred the radial approach over femoral access in the study, he added.
The results could be looked at as a glass half empty or half full, Dr. Roxana Mehran said as the discussant of the study at the meeting. She served on the executive committee of the SAFE-PCI trial.
In the eyes of a purist statistician, the results show no significant evidence that radial access prevents bleeding or vascular complications, the primary endpoint, said Dr. Mehran, professor of medicine and director of interventional cardiovascular research at Mount Sinai School of Medicine, New York.
From a clinician’s viewpoint, however, the estimates of benefit from radial access in the overall cohort and the PCI cohort were similar, yielding approximately a 60% reduction in bleeding with radial access, she noted. "The study provides evidence, albeit not conclusive, for greater efficacy with radial access in women," she said.
The crossover rates suggest that for every bleeding event or vascular complication prevented in the radial access group, three patients would cross over. "While there’s a higher crossover from [the] radial to the femoral approach, it’s reasonable and intuitive to begin with the radial approach in women," she said, "especially in those women at high risk for bleeding."
Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
I don’t think we have the data to say that this is a positive study or that we should change our practice because of these results. It’s an incomplete study, so we really don’t have the data. We need to think about why we didn’t have the anticipated enrollment and why the bleeding rate was lower than expected in the femoral access group. Those are the things that I think led to the futility. But it’s not really a negative trial. We simply don’t know whether radial access will be better in high-risk women undergoing PCI. It’s promising, and it makes all the sense in the world because of the bleeding risk in women.
Dr. Alice K. Jacobs is a professor of medicine and director of the cardiac catheterization laboratory and interventional cardiology at Boston University. She gave these remarks at a press briefing. Dr. Jacobs reported having no relevant financial disclosures.
I don’t think we have the data to say that this is a positive study or that we should change our practice because of these results. It’s an incomplete study, so we really don’t have the data. We need to think about why we didn’t have the anticipated enrollment and why the bleeding rate was lower than expected in the femoral access group. Those are the things that I think led to the futility. But it’s not really a negative trial. We simply don’t know whether radial access will be better in high-risk women undergoing PCI. It’s promising, and it makes all the sense in the world because of the bleeding risk in women.
Dr. Alice K. Jacobs is a professor of medicine and director of the cardiac catheterization laboratory and interventional cardiology at Boston University. She gave these remarks at a press briefing. Dr. Jacobs reported having no relevant financial disclosures.
I don’t think we have the data to say that this is a positive study or that we should change our practice because of these results. It’s an incomplete study, so we really don’t have the data. We need to think about why we didn’t have the anticipated enrollment and why the bleeding rate was lower than expected in the femoral access group. Those are the things that I think led to the futility. But it’s not really a negative trial. We simply don’t know whether radial access will be better in high-risk women undergoing PCI. It’s promising, and it makes all the sense in the world because of the bleeding risk in women.
Dr. Alice K. Jacobs is a professor of medicine and director of the cardiac catheterization laboratory and interventional cardiology at Boston University. She gave these remarks at a press briefing. Dr. Jacobs reported having no relevant financial disclosures.
SAN FRANCISCO – Rates of bleeding or vascular complications in women undergoing percutaneous coronary intervention were 59% lower using radial access, compared with femoral access, a difference that did not reach statistical significance in a randomized study of 1,787 patients.
Bleeding or vascular complications within 72 hours or at hospital discharge were seen in 1.2% of 345 women who had transradial percutaneous coronary intervention (PCI) and 2.9% of 345 women who had transfemoral PCI, Dr. Sunil V. Rao reported at the Trans-catheter Cardiovascular Therapeutics annual meeting.
Although that difference was not statistically significant in this prespecified analysis of patients who actually underwent PCI, the rate of bleeding and vascular complications was significantly lower for the group randomized to radial access in an analysis of the whole cohort, regardless of whether they had PCI or just diagnostic catheterization. Bleeding and vascular complication rates were 0.6% in those randomized to radial access and 1.7% in those randomized to femoral access.
In both the PCI cohort and the total cohort, significantly more women in the radial group needed to cross over to femoral access for PCI compared with the crossover rate in the femoral group. In the PCI cohort, 6.1% of the radial group crossed over, as did 1.7% of the femoral group. In the total cohort, crossover was needed in 6.7% of the radial group and 1.9% of the femoral group, said Dr. Rao of Duke University, Durham, N.C. The main reason for crossover from radial to femoral access was radial artery spasm, in 43% of cases.
The Study of Access Site for Enhancement of PCI for Women (SAFE-PCI) leveraged data from the National Cardiovascular Data Registry’s CathPCI Registry from 60 institutions on adult women undergoing elective or urgent PCI or undergoing diagnostic angiography to evaluate ischemic symptoms with the possibility of PCI. The primary outcome measure was Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding events and vascular complications requiring intervention.
The investigators had planned to randomize 3,000 women to obtain 1,800 who underwent PCI, but a routine review after randomizing 1,120 patients suggested that the trial would be too small to show a difference because of lower-than-expected bleeding rates. Because no harm was noted in either the radial or femoral group, the investigators continued until they had enough patients for a quality-of-life substudy, then prematurely discontinued the trial.
The reduction in bleeding with the radial approach was similar to reductions seen in previous studies, Dr. Rao said at the meeting, cosponsored by the American College of Cardiology. The conversion rate from radial to femoral access was similar to the 7.6% rate reported in a prior trial (Lancet 2011;377:1409-20).
Compared with men, women have an increased risk for bleeding from antithrombotic therapy and from femoral access for PCI. Radial access can decrease bleeding risk, but trans-radial PCI has been less common in women, in part because they have smaller radial arteries.
The current trial’s results suggest that "an initial strategy of radial access is reasonable and may be preferred by some operators for women undergoing cardiac catheterization or PCI, with the recognition that a proportion of patients will require conversion to femoral access," he said.
Women preferred the radial approach over femoral access in the study, he added.
The results could be looked at as a glass half empty or half full, Dr. Roxana Mehran said as the discussant of the study at the meeting. She served on the executive committee of the SAFE-PCI trial.
In the eyes of a purist statistician, the results show no significant evidence that radial access prevents bleeding or vascular complications, the primary endpoint, said Dr. Mehran, professor of medicine and director of interventional cardiovascular research at Mount Sinai School of Medicine, New York.
From a clinician’s viewpoint, however, the estimates of benefit from radial access in the overall cohort and the PCI cohort were similar, yielding approximately a 60% reduction in bleeding with radial access, she noted. "The study provides evidence, albeit not conclusive, for greater efficacy with radial access in women," she said.
The crossover rates suggest that for every bleeding event or vascular complication prevented in the radial access group, three patients would cross over. "While there’s a higher crossover from [the] radial to the femoral approach, it’s reasonable and intuitive to begin with the radial approach in women," she said, "especially in those women at high risk for bleeding."
Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
SAN FRANCISCO – Rates of bleeding or vascular complications in women undergoing percutaneous coronary intervention were 59% lower using radial access, compared with femoral access, a difference that did not reach statistical significance in a randomized study of 1,787 patients.
Bleeding or vascular complications within 72 hours or at hospital discharge were seen in 1.2% of 345 women who had transradial percutaneous coronary intervention (PCI) and 2.9% of 345 women who had transfemoral PCI, Dr. Sunil V. Rao reported at the Trans-catheter Cardiovascular Therapeutics annual meeting.
Although that difference was not statistically significant in this prespecified analysis of patients who actually underwent PCI, the rate of bleeding and vascular complications was significantly lower for the group randomized to radial access in an analysis of the whole cohort, regardless of whether they had PCI or just diagnostic catheterization. Bleeding and vascular complication rates were 0.6% in those randomized to radial access and 1.7% in those randomized to femoral access.
In both the PCI cohort and the total cohort, significantly more women in the radial group needed to cross over to femoral access for PCI compared with the crossover rate in the femoral group. In the PCI cohort, 6.1% of the radial group crossed over, as did 1.7% of the femoral group. In the total cohort, crossover was needed in 6.7% of the radial group and 1.9% of the femoral group, said Dr. Rao of Duke University, Durham, N.C. The main reason for crossover from radial to femoral access was radial artery spasm, in 43% of cases.
The Study of Access Site for Enhancement of PCI for Women (SAFE-PCI) leveraged data from the National Cardiovascular Data Registry’s CathPCI Registry from 60 institutions on adult women undergoing elective or urgent PCI or undergoing diagnostic angiography to evaluate ischemic symptoms with the possibility of PCI. The primary outcome measure was Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding events and vascular complications requiring intervention.
The investigators had planned to randomize 3,000 women to obtain 1,800 who underwent PCI, but a routine review after randomizing 1,120 patients suggested that the trial would be too small to show a difference because of lower-than-expected bleeding rates. Because no harm was noted in either the radial or femoral group, the investigators continued until they had enough patients for a quality-of-life substudy, then prematurely discontinued the trial.
The reduction in bleeding with the radial approach was similar to reductions seen in previous studies, Dr. Rao said at the meeting, cosponsored by the American College of Cardiology. The conversion rate from radial to femoral access was similar to the 7.6% rate reported in a prior trial (Lancet 2011;377:1409-20).
Compared with men, women have an increased risk for bleeding from antithrombotic therapy and from femoral access for PCI. Radial access can decrease bleeding risk, but trans-radial PCI has been less common in women, in part because they have smaller radial arteries.
The current trial’s results suggest that "an initial strategy of radial access is reasonable and may be preferred by some operators for women undergoing cardiac catheterization or PCI, with the recognition that a proportion of patients will require conversion to femoral access," he said.
Women preferred the radial approach over femoral access in the study, he added.
The results could be looked at as a glass half empty or half full, Dr. Roxana Mehran said as the discussant of the study at the meeting. She served on the executive committee of the SAFE-PCI trial.
In the eyes of a purist statistician, the results show no significant evidence that radial access prevents bleeding or vascular complications, the primary endpoint, said Dr. Mehran, professor of medicine and director of interventional cardiovascular research at Mount Sinai School of Medicine, New York.
From a clinician’s viewpoint, however, the estimates of benefit from radial access in the overall cohort and the PCI cohort were similar, yielding approximately a 60% reduction in bleeding with radial access, she noted. "The study provides evidence, albeit not conclusive, for greater efficacy with radial access in women," she said.
The crossover rates suggest that for every bleeding event or vascular complication prevented in the radial access group, three patients would cross over. "While there’s a higher crossover from [the] radial to the femoral approach, it’s reasonable and intuitive to begin with the radial approach in women," she said, "especially in those women at high risk for bleeding."
Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
Major finding: Rates of bleeding or vascular complications were 1.2% using radial access and 2.9% using femoral access in the PCI subgroup and 6.7% and 1.9%, respectively, in the entire cohort.
Data source: A randomized study of 1,787 women undergoing definite or possible PCI at 60 institutions.
Disclosures: Dr. Rao has been a consultant for the Medicines Co., which helped fund the trial, and for AstraZeneca. Dr. Mehran reported financial associations with these companies and with Abbott Vascular and Daiichi-Sankyo/Eli Lilly & Co., which also funded the trial. Other funders of the study included Abbott Vascular, Daiichi-Sankyo/Eli Lilly & Co., Terumo Medical, Medtronic, ACIST Medical Systems, and Guerbet. Dr. Mehran also reported financial associations with nine other medical companies.
Fistula risk quadrupled with hyperthermia during pancreaticoduodenectomy
SAN FRANCISCO – A patient body temperature higher than 99.5° F (37.5° C) at the end of elective pancreaticoduodenectomy predicted a fourfold increased risk of postoperative pancreatic fistula in a retrospective study of 123 patients.
Two factors independently predicted a significantly increased risk for postoperative pancreatic fistula in a multivariate logistic regression analysis – body temperature at the end of surgery and a soft pancreatic texture (which conferred a 34-fold increase in risk), Dr. Tadashi Tanioku and his associates.
It wasn’t clear whether pancreatic fistula caused the intraoperative elevated body temperature or the hyperthermia contributed to postoperative development of fistula, but the findings suggest that body temperature at the conclusion of surgery may provide a clue to a patient’s risk of postoperative pancreatic fistula, said Dr. Tanioku of Wakayama (Japan) Medical University.
The study included all patients who underwent pancreaticoduodenectomy for benign or malignant diseases in the pancreatic head and the periampullary region during a 2-year period at his hospital. Thirty-six percent developed postoperative pancreatic fistulas, the investigators reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
In a univariate logistic regression analysis, significant predictors for postoperative pancreatic fistula included a body temperature higher than 99.5 degrees Fahrenheit in 45% of patients, soft pancreatic texture in 52%, and a pancreatic duct diameter less than 3 mm in 43% of patients. Having a body mass index greater than 25 kg/m2 (in 17% of patients) was not a significant predictor).
Previous studies have reported an association between hyperthermia on postoperative day 3 after pancreaticoduodenectomy and the development of postoperative pancreatic fistula. Other data have shown an association between intraoperative hyperthermia during colorectal surgery and increased risk of postoperative anastomotic leakage.
In general, operative mortality after pancreaticoduodenectomy had declined to less than 5% but postoperative morality rates are still 40%-50%, mainly from postoperative pancreatic fistula, Dr. Tanioku said.
Patients who developed pancreatic fistula were significantly younger than those who didn’t (a mean of 68 vs. 72 years, respectively) and were significantly more likely to have a main pancreatic duct diameter less than 3 mm (59% vs. 30%, respectively). Fifty-nine percent of patients who developed postoperative fistulas and 37% of those who didn’t had a body temperature higher than 99.5° F at the end of surgery. Eighty-six percent of patients who went on to develop fistulas and 29% of those who didn’t had a soft pancreatic texture.
Dr. Tanioku reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A patient body temperature higher than 99.5° F (37.5° C) at the end of elective pancreaticoduodenectomy predicted a fourfold increased risk of postoperative pancreatic fistula in a retrospective study of 123 patients.
Two factors independently predicted a significantly increased risk for postoperative pancreatic fistula in a multivariate logistic regression analysis – body temperature at the end of surgery and a soft pancreatic texture (which conferred a 34-fold increase in risk), Dr. Tadashi Tanioku and his associates.
It wasn’t clear whether pancreatic fistula caused the intraoperative elevated body temperature or the hyperthermia contributed to postoperative development of fistula, but the findings suggest that body temperature at the conclusion of surgery may provide a clue to a patient’s risk of postoperative pancreatic fistula, said Dr. Tanioku of Wakayama (Japan) Medical University.
The study included all patients who underwent pancreaticoduodenectomy for benign or malignant diseases in the pancreatic head and the periampullary region during a 2-year period at his hospital. Thirty-six percent developed postoperative pancreatic fistulas, the investigators reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
In a univariate logistic regression analysis, significant predictors for postoperative pancreatic fistula included a body temperature higher than 99.5 degrees Fahrenheit in 45% of patients, soft pancreatic texture in 52%, and a pancreatic duct diameter less than 3 mm in 43% of patients. Having a body mass index greater than 25 kg/m2 (in 17% of patients) was not a significant predictor).
Previous studies have reported an association between hyperthermia on postoperative day 3 after pancreaticoduodenectomy and the development of postoperative pancreatic fistula. Other data have shown an association between intraoperative hyperthermia during colorectal surgery and increased risk of postoperative anastomotic leakage.
In general, operative mortality after pancreaticoduodenectomy had declined to less than 5% but postoperative morality rates are still 40%-50%, mainly from postoperative pancreatic fistula, Dr. Tanioku said.
Patients who developed pancreatic fistula were significantly younger than those who didn’t (a mean of 68 vs. 72 years, respectively) and were significantly more likely to have a main pancreatic duct diameter less than 3 mm (59% vs. 30%, respectively). Fifty-nine percent of patients who developed postoperative fistulas and 37% of those who didn’t had a body temperature higher than 99.5° F at the end of surgery. Eighty-six percent of patients who went on to develop fistulas and 29% of those who didn’t had a soft pancreatic texture.
Dr. Tanioku reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – A patient body temperature higher than 99.5° F (37.5° C) at the end of elective pancreaticoduodenectomy predicted a fourfold increased risk of postoperative pancreatic fistula in a retrospective study of 123 patients.
Two factors independently predicted a significantly increased risk for postoperative pancreatic fistula in a multivariate logistic regression analysis – body temperature at the end of surgery and a soft pancreatic texture (which conferred a 34-fold increase in risk), Dr. Tadashi Tanioku and his associates.
It wasn’t clear whether pancreatic fistula caused the intraoperative elevated body temperature or the hyperthermia contributed to postoperative development of fistula, but the findings suggest that body temperature at the conclusion of surgery may provide a clue to a patient’s risk of postoperative pancreatic fistula, said Dr. Tanioku of Wakayama (Japan) Medical University.
The study included all patients who underwent pancreaticoduodenectomy for benign or malignant diseases in the pancreatic head and the periampullary region during a 2-year period at his hospital. Thirty-six percent developed postoperative pancreatic fistulas, the investigators reported in a poster presentation at the annual meeting of the American Society of Anesthesiologists.
In a univariate logistic regression analysis, significant predictors for postoperative pancreatic fistula included a body temperature higher than 99.5 degrees Fahrenheit in 45% of patients, soft pancreatic texture in 52%, and a pancreatic duct diameter less than 3 mm in 43% of patients. Having a body mass index greater than 25 kg/m2 (in 17% of patients) was not a significant predictor).
Previous studies have reported an association between hyperthermia on postoperative day 3 after pancreaticoduodenectomy and the development of postoperative pancreatic fistula. Other data have shown an association between intraoperative hyperthermia during colorectal surgery and increased risk of postoperative anastomotic leakage.
In general, operative mortality after pancreaticoduodenectomy had declined to less than 5% but postoperative morality rates are still 40%-50%, mainly from postoperative pancreatic fistula, Dr. Tanioku said.
Patients who developed pancreatic fistula were significantly younger than those who didn’t (a mean of 68 vs. 72 years, respectively) and were significantly more likely to have a main pancreatic duct diameter less than 3 mm (59% vs. 30%, respectively). Fifty-nine percent of patients who developed postoperative fistulas and 37% of those who didn’t had a body temperature higher than 99.5° F at the end of surgery. Eighty-six percent of patients who went on to develop fistulas and 29% of those who didn’t had a soft pancreatic texture.
Dr. Tanioku reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ASA ANNUAL MEETING
Major finding: The likelihood of postoperative pancreatic fistula quadrupled in patients with a body temperature higher than 99.5 degrees F at the end of pancreaticoduodenectomy.
Data source: Retrospective study of 123 patients undergoing elective pancreaticoduodenectomy at one hospital.
Disclosures: Dr. Tanioku reported having no financial disclosures.