User login
European research team to study drug resistance in psychiatry
Having secured 11 million euros in funding from the European Union’s Horizon Health program, an international team of pharmacology, pharmacogenetics, and psychiatry experts has set to work in hopes of helping patients with severe mental illnesses.
On this team is a group of researchers from the University of Cagliari in Sardinia, Italy. They are part of a network of international experts from 26 universities, research centers, and European associations, all of whom have vast experience in the fields of psychiatry, pharmacology, genetics, and statistics. Coordinating the project is Bernhard T. Baune, MD, PhD, professor of psychiatry at the University of Münster, Germany.
The problem of drug resistance is of great relevance to psychiatrists. About one-third of patients do not respond to pharmacologic therapies; as a result, their illness becomes more and more severe. This development has a major impact on these patients’ quality of life. In addition, health care and social services face a rise in the costs associated with managing the illnesses.
The research team from the University of Cagliari has two members from the department of biomedical sciences – Alessio Squassina, PhD, head of the pharmacogenetics laboratory, and Claudia Pisanu, MD, PhD – and two translational clinical researchers from the department of medical sciences and public health – Bernardo Carpiniello, MD, head of the psychiatry division, and Mirko Manchia, MD, PhD. They will be in charge of recruiting and collecting biological material from one set of patients with mental illnesses, collecting DNA and performing genetic screenings for all of the patients recruited by the network’s members in the various European countries, and conducting and coordinating clinical trials in which the pharmacologic therapies will be guided based on the molecular results.
“The process of figuring out whether someone has drug resistance is complex,” explained Dr. Squassina. “It may require very long periods of treatment and observation which, in the end, severely impact the patient’s chances of seeing a significant improvement in their symptoms and of being able to reintegrate themselves into society in the shortest possible time frame.” The goal of the Psych-STRATA project is to come up with a predictive algorithm – consisting of molecular markers and clinical data – that, before a specific antidepressant is even given, will be able to identify the patients who have a greater probability of responding and those who have a greater probability of not responding. Psych-STRATA’s findings could have a meaningful positive effect on the lives of patients with mental illnesses, as they would provide psychiatrists with guidance for managing pharmacologic therapies more precisely and in a way that is based on patients’ biological characteristics. This, in turn, would increase the efficacy of drugs, lower the risks of adverse effects, and significantly contribute to achieving quick remission of symptoms.
A version of this article appeared on Medscape.com. This article was translated from Univadis Italy.
Having secured 11 million euros in funding from the European Union’s Horizon Health program, an international team of pharmacology, pharmacogenetics, and psychiatry experts has set to work in hopes of helping patients with severe mental illnesses.
On this team is a group of researchers from the University of Cagliari in Sardinia, Italy. They are part of a network of international experts from 26 universities, research centers, and European associations, all of whom have vast experience in the fields of psychiatry, pharmacology, genetics, and statistics. Coordinating the project is Bernhard T. Baune, MD, PhD, professor of psychiatry at the University of Münster, Germany.
The problem of drug resistance is of great relevance to psychiatrists. About one-third of patients do not respond to pharmacologic therapies; as a result, their illness becomes more and more severe. This development has a major impact on these patients’ quality of life. In addition, health care and social services face a rise in the costs associated with managing the illnesses.
The research team from the University of Cagliari has two members from the department of biomedical sciences – Alessio Squassina, PhD, head of the pharmacogenetics laboratory, and Claudia Pisanu, MD, PhD – and two translational clinical researchers from the department of medical sciences and public health – Bernardo Carpiniello, MD, head of the psychiatry division, and Mirko Manchia, MD, PhD. They will be in charge of recruiting and collecting biological material from one set of patients with mental illnesses, collecting DNA and performing genetic screenings for all of the patients recruited by the network’s members in the various European countries, and conducting and coordinating clinical trials in which the pharmacologic therapies will be guided based on the molecular results.
“The process of figuring out whether someone has drug resistance is complex,” explained Dr. Squassina. “It may require very long periods of treatment and observation which, in the end, severely impact the patient’s chances of seeing a significant improvement in their symptoms and of being able to reintegrate themselves into society in the shortest possible time frame.” The goal of the Psych-STRATA project is to come up with a predictive algorithm – consisting of molecular markers and clinical data – that, before a specific antidepressant is even given, will be able to identify the patients who have a greater probability of responding and those who have a greater probability of not responding. Psych-STRATA’s findings could have a meaningful positive effect on the lives of patients with mental illnesses, as they would provide psychiatrists with guidance for managing pharmacologic therapies more precisely and in a way that is based on patients’ biological characteristics. This, in turn, would increase the efficacy of drugs, lower the risks of adverse effects, and significantly contribute to achieving quick remission of symptoms.
A version of this article appeared on Medscape.com. This article was translated from Univadis Italy.
Having secured 11 million euros in funding from the European Union’s Horizon Health program, an international team of pharmacology, pharmacogenetics, and psychiatry experts has set to work in hopes of helping patients with severe mental illnesses.
On this team is a group of researchers from the University of Cagliari in Sardinia, Italy. They are part of a network of international experts from 26 universities, research centers, and European associations, all of whom have vast experience in the fields of psychiatry, pharmacology, genetics, and statistics. Coordinating the project is Bernhard T. Baune, MD, PhD, professor of psychiatry at the University of Münster, Germany.
The problem of drug resistance is of great relevance to psychiatrists. About one-third of patients do not respond to pharmacologic therapies; as a result, their illness becomes more and more severe. This development has a major impact on these patients’ quality of life. In addition, health care and social services face a rise in the costs associated with managing the illnesses.
The research team from the University of Cagliari has two members from the department of biomedical sciences – Alessio Squassina, PhD, head of the pharmacogenetics laboratory, and Claudia Pisanu, MD, PhD – and two translational clinical researchers from the department of medical sciences and public health – Bernardo Carpiniello, MD, head of the psychiatry division, and Mirko Manchia, MD, PhD. They will be in charge of recruiting and collecting biological material from one set of patients with mental illnesses, collecting DNA and performing genetic screenings for all of the patients recruited by the network’s members in the various European countries, and conducting and coordinating clinical trials in which the pharmacologic therapies will be guided based on the molecular results.
“The process of figuring out whether someone has drug resistance is complex,” explained Dr. Squassina. “It may require very long periods of treatment and observation which, in the end, severely impact the patient’s chances of seeing a significant improvement in their symptoms and of being able to reintegrate themselves into society in the shortest possible time frame.” The goal of the Psych-STRATA project is to come up with a predictive algorithm – consisting of molecular markers and clinical data – that, before a specific antidepressant is even given, will be able to identify the patients who have a greater probability of responding and those who have a greater probability of not responding. Psych-STRATA’s findings could have a meaningful positive effect on the lives of patients with mental illnesses, as they would provide psychiatrists with guidance for managing pharmacologic therapies more precisely and in a way that is based on patients’ biological characteristics. This, in turn, would increase the efficacy of drugs, lower the risks of adverse effects, and significantly contribute to achieving quick remission of symptoms.
A version of this article appeared on Medscape.com. This article was translated from Univadis Italy.
Multiple myeloma patients with t(11;14) respond best to venetoclax monotherapy
Phase 1 data on venetoclax monotherapy for relapsed/refractory multiple myeloma, initially presented at the 2016 annual meeting of the American Society of Hematology, have been published in Blood.
Of 66 patients enrolled in the study (NCT01794520), 61% were bortezomib and lenalidomide double refractory, and 46% had t(11;14), said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minn, and his colleagues.
The overall response rate was 21% (14/66), and 15% achieved very good or better partial responses; 12 of the 14 responses occurred in patients with t(11;14).
(Click here to read the initial report and to view a video of Dr. Kumar discussing the study results at ASH 2016.)
Venetoclax is a selective, orally bioavailable BCL-2 inhibitor that is particularly effective against MM cells harboring t(11;14). Biomarker analysis confirmed that response to venetoclax correlated with higher BCL2:BCL2L1 and BCL2:MCL1 mRNA expression ratios.
The study is sponsored by Abbvie, and Dr. Kumar receives research support from Abbvie.
Phase 1 data on venetoclax monotherapy for relapsed/refractory multiple myeloma, initially presented at the 2016 annual meeting of the American Society of Hematology, have been published in Blood.
Of 66 patients enrolled in the study (NCT01794520), 61% were bortezomib and lenalidomide double refractory, and 46% had t(11;14), said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minn, and his colleagues.
The overall response rate was 21% (14/66), and 15% achieved very good or better partial responses; 12 of the 14 responses occurred in patients with t(11;14).
(Click here to read the initial report and to view a video of Dr. Kumar discussing the study results at ASH 2016.)
Venetoclax is a selective, orally bioavailable BCL-2 inhibitor that is particularly effective against MM cells harboring t(11;14). Biomarker analysis confirmed that response to venetoclax correlated with higher BCL2:BCL2L1 and BCL2:MCL1 mRNA expression ratios.
The study is sponsored by Abbvie, and Dr. Kumar receives research support from Abbvie.
Phase 1 data on venetoclax monotherapy for relapsed/refractory multiple myeloma, initially presented at the 2016 annual meeting of the American Society of Hematology, have been published in Blood.
Of 66 patients enrolled in the study (NCT01794520), 61% were bortezomib and lenalidomide double refractory, and 46% had t(11;14), said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minn, and his colleagues.
The overall response rate was 21% (14/66), and 15% achieved very good or better partial responses; 12 of the 14 responses occurred in patients with t(11;14).
(Click here to read the initial report and to view a video of Dr. Kumar discussing the study results at ASH 2016.)
Venetoclax is a selective, orally bioavailable BCL-2 inhibitor that is particularly effective against MM cells harboring t(11;14). Biomarker analysis confirmed that response to venetoclax correlated with higher BCL2:BCL2L1 and BCL2:MCL1 mRNA expression ratios.
The study is sponsored by Abbvie, and Dr. Kumar receives research support from Abbvie.
from blood
AML capsules
Detecting hereditary MDS/AML
Unexplained cytopenias or failure to mobilize stem cells in related donors of patients with myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML) – important clues for the detection of a hereditary MDS/AML syndrome – should prompt efforts to obtain germ line tissue sources for collaborative research, Jane E. Churpek, MD, of the Hereditary Hematologic Malignancies Program at The University of Chicago Medicine, wrote.
Partnering with families to obtain germ line tissue sources uncontaminated by tumor cells from large numbers of patients with MDS/AML, and international collaboration to determine the mechanisms and multi-step processes from the carrier state to overt disease, have enormous potential to improve the outcomes of patients with both familial and sporadic forms of MDS/AML. Incorporating collection of ideal germ line tissue along with family histories to the already robust international MDS/AML registries and data sharing are all essential to future progress in this field, she wrote in a recent article published onlne in Best Practice & Research Clinical Haematology.
Prophylactic granulocyte transfusions
Giving prophylactic granulocyte transfusions to AML patients during the induction phase of therapy is feasible and safe, but assuring an adequate donor pool and patient continuation of the transfusions are another matter.
In a phase 2 trial of 45 neutropenic patients with AML or high-risk myelodysplastic syndrome undergoing induction or first-salvage therapy, non-irradiated allogeneic granulocyte transfusions were to be given every 3-4 days until sustained ANC recovery, initiation of new therapy, or completion of 6 weeks on study. But logistical problems limited the success of the protocol: 5 patients never received a granulocyte transfusion due to donor screening failure or donor unavailability and the other 40 received a median of 3 (range 1-9) granulocyte transfusions.
“We anticipated approximately 8 GTs per patient ... only 11 received 6 or more GTs,” Fleur M. Aung, MD, and colleagues at The MD Anderson Cancer Center, Houston, wrote in the Journal of Blood Disorders and Transfusion (DOI 10.4172/2155-9864.1000376).
The authors concluded that while the process is feasible, ex vivo expanded neutrophils, produced from multiple donors and cryopreserved to provide an “off the shelf” myeloid progenitor product, will likely prove more reliable for treating patients with prolonged neutropenia.
From ONC201 to ONC212
Oncoceutics has expanded its research collaboration agreement with The University of Texas MD Anderson Cancer Center, Houston, to include the clinical development of a second novel imipridone called ONC212.
Oncoceutics and MD Anderson are already collaborating on the clinical development of another imipridone, ONC201. Both drugs have the same chemical core that interacts with G-Protein Coupled Receptors (GPCRs). ONC212 targets GPR132, which influences the growth of acute leukemias and has not previously been successfully targeted by a small molecule.
This alliance between MD Anderson and Oncoceutics will support Phase I and Phase II clinical trials of ONC212 in patients with refractory acute myeloid leukemia (AML), according to Oncoceutics. The alliance provides for a sharing of risk and rewards from potential commercialization of ONC212.
Top risk factor miRNA
The miRNA hsa-mir-425 was identified as the top risk factor miRNA of AML survival and CD44 was identified as one of the top three risk factor target-genes associated with AML survival, based on a miRNA-mRNA interaction network.
Chunmei Zhang, MD, of the department of hematology at Taian City Central Hospital, Taian, Shandong, China, and colleagues used The Cancer Genome Atlas database to obtain miRNA and mRNA expression profiles from AML patients. Of 14 miRNAs associated with AML survival, 3 were associated with risk – hsa-mir-425, hsa-mir-1201, and hsa-mir-1978. GTSF1, RTN4R, and CD44 were the top risk factor target-genes associated with AML survival. Med Sci Monit 2017; 23:4705-14 (DOI: 10.12659/MSM.903989)
Detecting hereditary MDS/AML
Unexplained cytopenias or failure to mobilize stem cells in related donors of patients with myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML) – important clues for the detection of a hereditary MDS/AML syndrome – should prompt efforts to obtain germ line tissue sources for collaborative research, Jane E. Churpek, MD, of the Hereditary Hematologic Malignancies Program at The University of Chicago Medicine, wrote.
Partnering with families to obtain germ line tissue sources uncontaminated by tumor cells from large numbers of patients with MDS/AML, and international collaboration to determine the mechanisms and multi-step processes from the carrier state to overt disease, have enormous potential to improve the outcomes of patients with both familial and sporadic forms of MDS/AML. Incorporating collection of ideal germ line tissue along with family histories to the already robust international MDS/AML registries and data sharing are all essential to future progress in this field, she wrote in a recent article published onlne in Best Practice & Research Clinical Haematology.
Prophylactic granulocyte transfusions
Giving prophylactic granulocyte transfusions to AML patients during the induction phase of therapy is feasible and safe, but assuring an adequate donor pool and patient continuation of the transfusions are another matter.
In a phase 2 trial of 45 neutropenic patients with AML or high-risk myelodysplastic syndrome undergoing induction or first-salvage therapy, non-irradiated allogeneic granulocyte transfusions were to be given every 3-4 days until sustained ANC recovery, initiation of new therapy, or completion of 6 weeks on study. But logistical problems limited the success of the protocol: 5 patients never received a granulocyte transfusion due to donor screening failure or donor unavailability and the other 40 received a median of 3 (range 1-9) granulocyte transfusions.
“We anticipated approximately 8 GTs per patient ... only 11 received 6 or more GTs,” Fleur M. Aung, MD, and colleagues at The MD Anderson Cancer Center, Houston, wrote in the Journal of Blood Disorders and Transfusion (DOI 10.4172/2155-9864.1000376).
The authors concluded that while the process is feasible, ex vivo expanded neutrophils, produced from multiple donors and cryopreserved to provide an “off the shelf” myeloid progenitor product, will likely prove more reliable for treating patients with prolonged neutropenia.
From ONC201 to ONC212
Oncoceutics has expanded its research collaboration agreement with The University of Texas MD Anderson Cancer Center, Houston, to include the clinical development of a second novel imipridone called ONC212.
Oncoceutics and MD Anderson are already collaborating on the clinical development of another imipridone, ONC201. Both drugs have the same chemical core that interacts with G-Protein Coupled Receptors (GPCRs). ONC212 targets GPR132, which influences the growth of acute leukemias and has not previously been successfully targeted by a small molecule.
This alliance between MD Anderson and Oncoceutics will support Phase I and Phase II clinical trials of ONC212 in patients with refractory acute myeloid leukemia (AML), according to Oncoceutics. The alliance provides for a sharing of risk and rewards from potential commercialization of ONC212.
Top risk factor miRNA
The miRNA hsa-mir-425 was identified as the top risk factor miRNA of AML survival and CD44 was identified as one of the top three risk factor target-genes associated with AML survival, based on a miRNA-mRNA interaction network.
Chunmei Zhang, MD, of the department of hematology at Taian City Central Hospital, Taian, Shandong, China, and colleagues used The Cancer Genome Atlas database to obtain miRNA and mRNA expression profiles from AML patients. Of 14 miRNAs associated with AML survival, 3 were associated with risk – hsa-mir-425, hsa-mir-1201, and hsa-mir-1978. GTSF1, RTN4R, and CD44 were the top risk factor target-genes associated with AML survival. Med Sci Monit 2017; 23:4705-14 (DOI: 10.12659/MSM.903989)
Detecting hereditary MDS/AML
Unexplained cytopenias or failure to mobilize stem cells in related donors of patients with myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML) – important clues for the detection of a hereditary MDS/AML syndrome – should prompt efforts to obtain germ line tissue sources for collaborative research, Jane E. Churpek, MD, of the Hereditary Hematologic Malignancies Program at The University of Chicago Medicine, wrote.
Partnering with families to obtain germ line tissue sources uncontaminated by tumor cells from large numbers of patients with MDS/AML, and international collaboration to determine the mechanisms and multi-step processes from the carrier state to overt disease, have enormous potential to improve the outcomes of patients with both familial and sporadic forms of MDS/AML. Incorporating collection of ideal germ line tissue along with family histories to the already robust international MDS/AML registries and data sharing are all essential to future progress in this field, she wrote in a recent article published onlne in Best Practice & Research Clinical Haematology.
Prophylactic granulocyte transfusions
Giving prophylactic granulocyte transfusions to AML patients during the induction phase of therapy is feasible and safe, but assuring an adequate donor pool and patient continuation of the transfusions are another matter.
In a phase 2 trial of 45 neutropenic patients with AML or high-risk myelodysplastic syndrome undergoing induction or first-salvage therapy, non-irradiated allogeneic granulocyte transfusions were to be given every 3-4 days until sustained ANC recovery, initiation of new therapy, or completion of 6 weeks on study. But logistical problems limited the success of the protocol: 5 patients never received a granulocyte transfusion due to donor screening failure or donor unavailability and the other 40 received a median of 3 (range 1-9) granulocyte transfusions.
“We anticipated approximately 8 GTs per patient ... only 11 received 6 or more GTs,” Fleur M. Aung, MD, and colleagues at The MD Anderson Cancer Center, Houston, wrote in the Journal of Blood Disorders and Transfusion (DOI 10.4172/2155-9864.1000376).
The authors concluded that while the process is feasible, ex vivo expanded neutrophils, produced from multiple donors and cryopreserved to provide an “off the shelf” myeloid progenitor product, will likely prove more reliable for treating patients with prolonged neutropenia.
From ONC201 to ONC212
Oncoceutics has expanded its research collaboration agreement with The University of Texas MD Anderson Cancer Center, Houston, to include the clinical development of a second novel imipridone called ONC212.
Oncoceutics and MD Anderson are already collaborating on the clinical development of another imipridone, ONC201. Both drugs have the same chemical core that interacts with G-Protein Coupled Receptors (GPCRs). ONC212 targets GPR132, which influences the growth of acute leukemias and has not previously been successfully targeted by a small molecule.
This alliance between MD Anderson and Oncoceutics will support Phase I and Phase II clinical trials of ONC212 in patients with refractory acute myeloid leukemia (AML), according to Oncoceutics. The alliance provides for a sharing of risk and rewards from potential commercialization of ONC212.
Top risk factor miRNA
The miRNA hsa-mir-425 was identified as the top risk factor miRNA of AML survival and CD44 was identified as one of the top three risk factor target-genes associated with AML survival, based on a miRNA-mRNA interaction network.
Chunmei Zhang, MD, of the department of hematology at Taian City Central Hospital, Taian, Shandong, China, and colleagues used The Cancer Genome Atlas database to obtain miRNA and mRNA expression profiles from AML patients. Of 14 miRNAs associated with AML survival, 3 were associated with risk – hsa-mir-425, hsa-mir-1201, and hsa-mir-1978. GTSF1, RTN4R, and CD44 were the top risk factor target-genes associated with AML survival. Med Sci Monit 2017; 23:4705-14 (DOI: 10.12659/MSM.903989)
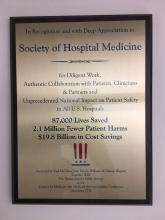
CMS recognizes Society of Hospital Medicine’s Center for Quality Improvement
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
PHILADELPHIA – The Society of Hospital Medicine (SHM)’s Center for Quality Improvement (QI) has been distinguished by the Centers for Medicare & Medicaid Services for maintaining an ongoing collaborative partnership with CMS to enhance patient safety.
The letter of recognition from Paul McGann, MD, Jean Moody-Williams, RN, MPP, and Dennis Wagner, MPA, of the CMS, to Jenna Goldstein, MA, director of SHM’s Center for QI, and Kevin Vuernick, MPA, senior project manager, noted: “Over the last several years, our team has been privileged to partner with you and the Society of Hospital Medicine on the work of quality improvement and patient safety. Without relationships like these, the results in the reduction of patient harm we have seen at a national scale, saving 87,000 lives and nearly $20 billion in cost savings, would never have been possible.”
In August 2016, CMS’ Hospital Improvement Innovation Networks contacted SHM to participate in their weekly Partnership for Patients (PfP) Pacing Event webinar to present strategies for reducing opioid use and preventing adverse drug events, including SHM’s Mentored Implementation pilot program on Reducing Adverse Drug Events Related to Opioids (RADEO). SHM’s contribution to this webinar was twofold: Thomas W. Frederickson, MD, the lead author of the RADEO guide and one of two program mentors, spoke about the development of the RADEO program and its importance in the acute care setting. Matthew Jared, MD, a hospitalist at St. Anthony Hospital in Oklahoma City, one of the five pilot RADEO sites, discussed his experience implementing specific RADEO interventions as well as the mentoring provided by Dr. Frederickson of the department of hospital medicine at CHI Health in Omaha, Neb.
As a result of this successful partnership, SHM was contacted in January to provide its perspective on best practices in managing inpatients receiving opioids and adverse drug event data collection. At that time, Mr. Vuernick discussed the lessons learned between RADEO’s pilot program and the second iteration of RADEO, which launched in November 2016.
For more information about SHM’s Center for QI, please visit www.hospitalmedicine.org/QI. For more information about SHM and hospital medicine, visit www.hospitalmedicine.org and follow SHM on Twitter at @SHMLive.
2016 Humanitarian Award
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
The Patient Safety Movement Foundation presented pediatric hospitalist Patrick Conway, MD, MSc, SFHM, with one of its 2016 Humanitarian Awards. The honor recognizes “life-saving achievement” in patient safety and efforts to “improve quality, affordability, access, and health outcomes,” according to a press release.
SHM welcomes its newest members - January 2017
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Cardiothoracic Clinical Trails Move Forward
The Cardiothoracic Surgical Trials Network is a major collaborative effort focusing on surgical approaches for cardiac disease. Two of their trials recently reached enrollment milestones, according to the CTSN.
In August the University of Pennsylvania randomized the 200th patient in the severe ischemic mitral regurgitation (SMR) trial. As of the end of the month, the Network randomized 205 patients in the trial designed to evaluate the efficacy and safety of mitral valve repair and replacement for severe MR patients.
There is a companion trial, the moderate MR (MMR) trial, to evaluate the safety and efficacy of mitral valve repair and coronary artery bypass grafting (CABG) vs. CABG alone.
The goal of these trials is to determine the optimal approach to treatment of patients with ischemic MR, a controversial subject involving significant variations in surgical practice. Investigators expect to complete enrollment in the SMR trial (n=250) in the fall of 2011, and in the MMR trial (n=300) by summer of 202.
Also in August, the University of Virginia randomized the 100th patient in the atrial fibrillation (AF) trial. The Network designed a comparative effectiveness randomized trial of surgical ablation with left atrial appendage (LAA) closure versus LAA closure alone in patients with (longstanding) persistent AF undergoing MVS. According to CTSN, nested within this trial, is a further randomized comparison of 2 different lesions sets (pulmonary vein isolation only and Maze lesion set).
The FDA recently approved expansion from 13 to 23 clinical centers and these new sites are now being launched to enable completion of enrollment in 2012.
Two new CTSN-sponsored cell therapy trials are also in the works.
Left ventricular assist device (LVAD) therapy has become widely used and outcomes have improved over time. However, adverse events are still noted and could be minimized. In addition, quality of life could be improved if the duration of support could be limited. One potential way to do this is by inducing myocardial recovery through cell therapy, according to the CTSN.
In collaboration with the Cardiovascular Cell Therapy Research Network, CTSN has developed a translational trial that is intended to evaluate the safety, and explore the efficacy, of direct myocardial injection of off-the-shelf mesenchymal precursor cells in LVAD recipients. The FDA recently approved the protocol, and start-up activities are underway. The ttraining of site coordinators is scheduled to begin in mid-fall 2011.
The second cell therapy trial planned involves the use of intracoronary injections of autologous cardiac stem cells to be performed following cardiac transplantation. According to the CSTN, this trial will be designed to provide "important exploratory information regarding safety and the ability of stem cells to engraft and differentiate within the scaffold of the transplanted heart."
The rationale for this research is to modulate tolerance of the transplanted heart in order to reduce the incidence of allograft rejection. A pre-IND meeting to discuss the protocol was initiated with the FDA.
In the important area of drug support for cardiac surgery patients, CTSN is collaborating with the VA Cooperative Clinical Studies Program, to design what is intended to be a large, simple trial evaluating the effect of adding ticagrelor to aspirin after coronary artery bypass grafting.
The primary efficacy endpoint in the trial will be MACCE and the primary safety endpoint will be severe bleeding. The sample size will be close to 5,000 patients, and the trial is designed to detect a 20% reduction in the primary efficacy endpoint.
Further information on these and other upcoming and ongoing trials can be found on the CSTN website: www.ctsurgerynet.org along with access to their monthly newsletter.n
The Cardiothoracic Surgical Trials Network is a major collaborative effort focusing on surgical approaches for cardiac disease. Two of their trials recently reached enrollment milestones, according to the CTSN.
In August the University of Pennsylvania randomized the 200th patient in the severe ischemic mitral regurgitation (SMR) trial. As of the end of the month, the Network randomized 205 patients in the trial designed to evaluate the efficacy and safety of mitral valve repair and replacement for severe MR patients.
There is a companion trial, the moderate MR (MMR) trial, to evaluate the safety and efficacy of mitral valve repair and coronary artery bypass grafting (CABG) vs. CABG alone.
The goal of these trials is to determine the optimal approach to treatment of patients with ischemic MR, a controversial subject involving significant variations in surgical practice. Investigators expect to complete enrollment in the SMR trial (n=250) in the fall of 2011, and in the MMR trial (n=300) by summer of 202.
Also in August, the University of Virginia randomized the 100th patient in the atrial fibrillation (AF) trial. The Network designed a comparative effectiveness randomized trial of surgical ablation with left atrial appendage (LAA) closure versus LAA closure alone in patients with (longstanding) persistent AF undergoing MVS. According to CTSN, nested within this trial, is a further randomized comparison of 2 different lesions sets (pulmonary vein isolation only and Maze lesion set).
The FDA recently approved expansion from 13 to 23 clinical centers and these new sites are now being launched to enable completion of enrollment in 2012.
Two new CTSN-sponsored cell therapy trials are also in the works.
Left ventricular assist device (LVAD) therapy has become widely used and outcomes have improved over time. However, adverse events are still noted and could be minimized. In addition, quality of life could be improved if the duration of support could be limited. One potential way to do this is by inducing myocardial recovery through cell therapy, according to the CTSN.
In collaboration with the Cardiovascular Cell Therapy Research Network, CTSN has developed a translational trial that is intended to evaluate the safety, and explore the efficacy, of direct myocardial injection of off-the-shelf mesenchymal precursor cells in LVAD recipients. The FDA recently approved the protocol, and start-up activities are underway. The ttraining of site coordinators is scheduled to begin in mid-fall 2011.
The second cell therapy trial planned involves the use of intracoronary injections of autologous cardiac stem cells to be performed following cardiac transplantation. According to the CSTN, this trial will be designed to provide "important exploratory information regarding safety and the ability of stem cells to engraft and differentiate within the scaffold of the transplanted heart."
The rationale for this research is to modulate tolerance of the transplanted heart in order to reduce the incidence of allograft rejection. A pre-IND meeting to discuss the protocol was initiated with the FDA.
In the important area of drug support for cardiac surgery patients, CTSN is collaborating with the VA Cooperative Clinical Studies Program, to design what is intended to be a large, simple trial evaluating the effect of adding ticagrelor to aspirin after coronary artery bypass grafting.
The primary efficacy endpoint in the trial will be MACCE and the primary safety endpoint will be severe bleeding. The sample size will be close to 5,000 patients, and the trial is designed to detect a 20% reduction in the primary efficacy endpoint.
Further information on these and other upcoming and ongoing trials can be found on the CSTN website: www.ctsurgerynet.org along with access to their monthly newsletter.n
The Cardiothoracic Surgical Trials Network is a major collaborative effort focusing on surgical approaches for cardiac disease. Two of their trials recently reached enrollment milestones, according to the CTSN.
In August the University of Pennsylvania randomized the 200th patient in the severe ischemic mitral regurgitation (SMR) trial. As of the end of the month, the Network randomized 205 patients in the trial designed to evaluate the efficacy and safety of mitral valve repair and replacement for severe MR patients.
There is a companion trial, the moderate MR (MMR) trial, to evaluate the safety and efficacy of mitral valve repair and coronary artery bypass grafting (CABG) vs. CABG alone.
The goal of these trials is to determine the optimal approach to treatment of patients with ischemic MR, a controversial subject involving significant variations in surgical practice. Investigators expect to complete enrollment in the SMR trial (n=250) in the fall of 2011, and in the MMR trial (n=300) by summer of 202.
Also in August, the University of Virginia randomized the 100th patient in the atrial fibrillation (AF) trial. The Network designed a comparative effectiveness randomized trial of surgical ablation with left atrial appendage (LAA) closure versus LAA closure alone in patients with (longstanding) persistent AF undergoing MVS. According to CTSN, nested within this trial, is a further randomized comparison of 2 different lesions sets (pulmonary vein isolation only and Maze lesion set).
The FDA recently approved expansion from 13 to 23 clinical centers and these new sites are now being launched to enable completion of enrollment in 2012.
Two new CTSN-sponsored cell therapy trials are also in the works.
Left ventricular assist device (LVAD) therapy has become widely used and outcomes have improved over time. However, adverse events are still noted and could be minimized. In addition, quality of life could be improved if the duration of support could be limited. One potential way to do this is by inducing myocardial recovery through cell therapy, according to the CTSN.
In collaboration with the Cardiovascular Cell Therapy Research Network, CTSN has developed a translational trial that is intended to evaluate the safety, and explore the efficacy, of direct myocardial injection of off-the-shelf mesenchymal precursor cells in LVAD recipients. The FDA recently approved the protocol, and start-up activities are underway. The ttraining of site coordinators is scheduled to begin in mid-fall 2011.
The second cell therapy trial planned involves the use of intracoronary injections of autologous cardiac stem cells to be performed following cardiac transplantation. According to the CSTN, this trial will be designed to provide "important exploratory information regarding safety and the ability of stem cells to engraft and differentiate within the scaffold of the transplanted heart."
The rationale for this research is to modulate tolerance of the transplanted heart in order to reduce the incidence of allograft rejection. A pre-IND meeting to discuss the protocol was initiated with the FDA.
In the important area of drug support for cardiac surgery patients, CTSN is collaborating with the VA Cooperative Clinical Studies Program, to design what is intended to be a large, simple trial evaluating the effect of adding ticagrelor to aspirin after coronary artery bypass grafting.
The primary efficacy endpoint in the trial will be MACCE and the primary safety endpoint will be severe bleeding. The sample size will be close to 5,000 patients, and the trial is designed to detect a 20% reduction in the primary efficacy endpoint.
Further information on these and other upcoming and ongoing trials can be found on the CSTN website: www.ctsurgerynet.org along with access to their monthly newsletter.n
News From the FDA
Liver Injury With Dronedarone
The Food and Drug Administration issued a safety announcement about reports of rare but severe liver injury in patients taking dronedarone, including two patients who had acute liver failure that required transplantation.
Dronedarone (Multaq) is used to treat abnormal heart rhythm in patients who have those symptoms for the past 6 months, according to FDA.
The announcement warned physicians and patients to be alert for signs and symptoms of liver injury or toxicity, including anorexia, nausea, vomiting, fever, malaise, fatigue, right upper quadrant pain, jaundice, dark urine, or itching. Physicians are encouraged to consider ordering periodic hepatic serum enzymes, particularly during the initial 6 months of treatment with dronedarone.
The label's adverse reactions and warnings and precautions sections are being updated to include information about the potential risk of liver injury.
Lower Acetaminophen Doses Sought
The FDA has asked manufacturers of prescription pain products containing acetaminophen to include no more than 325 mg of the drug in each capsule, tablet, or other dosage unit.
According to a safety announcement by the agency, the action was taken to address the ongoing problem of acetaminophen overdose, a leading cause of severe liver injury in the United States.
The FDA requests that manufacturers of these combination products – including Vicodin and Percocet – add a boxed warning to product labels about the potential risk of severe liver injury if acetaminophen is taken in excessive doses or with alcohol.
Manufacturers have until January 2014 to comply with the recommendations, so a shortage of these medications is not anticipated, according to the agency.
The FDA is also asking clinicians to educate their patients about the dangers of acetaminophen overdose and to advise patients to take no more than the maximum daily dose of acetaminophen (4,000 mg).
“For physicians and other health care providers, we want to emphasize that it's important to talk to patients and make sure that they are aware of the risks of using prescription pain medicines with acetaminophen,” Dr. Sandra Kweder said during a press briefing.
Currently, prescription acetaminophen products contain up to 750 mg of acetaminophen per dosage unit, but there are no data indicating that more than 325 mg of acetaminophen per unit provides greater pain relief, according to the FDA.
The agency's request does not apply to over-the-counter products, which can contain as much as 500 mg per tablet or capsule in the products marketed as extra strength.
Almost half of acetaminophen-related cases of liver failure in the United States are caused by overdoses from prescription opioid-acetaminophen products, which are among the most commonly prescribed products in the United States, accounting for almost 200 million prescriptions dispensed per year.
Rules on Tobacco Tightened
Certain tobacco products – including cigarettes, roll-your-own, and smokeless varieties – that were introduced or changed in the United States after Feb. 15, 2007, must be reviewed by the FDA to show that they are “substantially equivalent” to existing products, Dr. Lawrence Deyton, director of the agency's Center for Tobacco Products, said in a press briefing.
The FDA action is driven by the Family Smoking Prevention and Tobacco Control Act, which became law in June 2009. The law allows the FDA to regulate tobacco products with the goal of protecting public health.
The substantial equivalence provisions are “meant to ensure that new tobacco products or changes to existing products are evaluated by the FDA before they enter the marketplace and are consumed by millions of people,” Dr. Deyton said. “Up to now, tobacco products have been the only mass-consumed products for which users do not know what they are consuming,” he said.
The Tobacco Control Act allows tobacco companies to market products that were available after Feb. 15, 2007, if the companies submit at least a preliminary report to the FDA by March 22, 2011, to show that these products are not significantly different from pre-existing products. Products in existence before Feb. 15, 2007, are not subject to the new FDA review, said Ann Simoneau, director of the Center for Tobacco Products' Office of Compliance and Enforcement.
New products introduced after March 22 will follow a different regulatory pathway, Dr. Deyton said.
Physicians should know that the FDA is now examining certain tobacco products and that manufacturers are required to submit information to the FDA about the products and changes to them, “particularly if those changes might raise new questions about public health,” Dr. Deyton said.
Liver Injury With Dronedarone
The Food and Drug Administration issued a safety announcement about reports of rare but severe liver injury in patients taking dronedarone, including two patients who had acute liver failure that required transplantation.
Dronedarone (Multaq) is used to treat abnormal heart rhythm in patients who have those symptoms for the past 6 months, according to FDA.
The announcement warned physicians and patients to be alert for signs and symptoms of liver injury or toxicity, including anorexia, nausea, vomiting, fever, malaise, fatigue, right upper quadrant pain, jaundice, dark urine, or itching. Physicians are encouraged to consider ordering periodic hepatic serum enzymes, particularly during the initial 6 months of treatment with dronedarone.
The label's adverse reactions and warnings and precautions sections are being updated to include information about the potential risk of liver injury.
Lower Acetaminophen Doses Sought
The FDA has asked manufacturers of prescription pain products containing acetaminophen to include no more than 325 mg of the drug in each capsule, tablet, or other dosage unit.
According to a safety announcement by the agency, the action was taken to address the ongoing problem of acetaminophen overdose, a leading cause of severe liver injury in the United States.
The FDA requests that manufacturers of these combination products – including Vicodin and Percocet – add a boxed warning to product labels about the potential risk of severe liver injury if acetaminophen is taken in excessive doses or with alcohol.
Manufacturers have until January 2014 to comply with the recommendations, so a shortage of these medications is not anticipated, according to the agency.
The FDA is also asking clinicians to educate their patients about the dangers of acetaminophen overdose and to advise patients to take no more than the maximum daily dose of acetaminophen (4,000 mg).
“For physicians and other health care providers, we want to emphasize that it's important to talk to patients and make sure that they are aware of the risks of using prescription pain medicines with acetaminophen,” Dr. Sandra Kweder said during a press briefing.
Currently, prescription acetaminophen products contain up to 750 mg of acetaminophen per dosage unit, but there are no data indicating that more than 325 mg of acetaminophen per unit provides greater pain relief, according to the FDA.
The agency's request does not apply to over-the-counter products, which can contain as much as 500 mg per tablet or capsule in the products marketed as extra strength.
Almost half of acetaminophen-related cases of liver failure in the United States are caused by overdoses from prescription opioid-acetaminophen products, which are among the most commonly prescribed products in the United States, accounting for almost 200 million prescriptions dispensed per year.
Rules on Tobacco Tightened
Certain tobacco products – including cigarettes, roll-your-own, and smokeless varieties – that were introduced or changed in the United States after Feb. 15, 2007, must be reviewed by the FDA to show that they are “substantially equivalent” to existing products, Dr. Lawrence Deyton, director of the agency's Center for Tobacco Products, said in a press briefing.
The FDA action is driven by the Family Smoking Prevention and Tobacco Control Act, which became law in June 2009. The law allows the FDA to regulate tobacco products with the goal of protecting public health.
The substantial equivalence provisions are “meant to ensure that new tobacco products or changes to existing products are evaluated by the FDA before they enter the marketplace and are consumed by millions of people,” Dr. Deyton said. “Up to now, tobacco products have been the only mass-consumed products for which users do not know what they are consuming,” he said.
The Tobacco Control Act allows tobacco companies to market products that were available after Feb. 15, 2007, if the companies submit at least a preliminary report to the FDA by March 22, 2011, to show that these products are not significantly different from pre-existing products. Products in existence before Feb. 15, 2007, are not subject to the new FDA review, said Ann Simoneau, director of the Center for Tobacco Products' Office of Compliance and Enforcement.
New products introduced after March 22 will follow a different regulatory pathway, Dr. Deyton said.
Physicians should know that the FDA is now examining certain tobacco products and that manufacturers are required to submit information to the FDA about the products and changes to them, “particularly if those changes might raise new questions about public health,” Dr. Deyton said.
Liver Injury With Dronedarone
The Food and Drug Administration issued a safety announcement about reports of rare but severe liver injury in patients taking dronedarone, including two patients who had acute liver failure that required transplantation.
Dronedarone (Multaq) is used to treat abnormal heart rhythm in patients who have those symptoms for the past 6 months, according to FDA.
The announcement warned physicians and patients to be alert for signs and symptoms of liver injury or toxicity, including anorexia, nausea, vomiting, fever, malaise, fatigue, right upper quadrant pain, jaundice, dark urine, or itching. Physicians are encouraged to consider ordering periodic hepatic serum enzymes, particularly during the initial 6 months of treatment with dronedarone.
The label's adverse reactions and warnings and precautions sections are being updated to include information about the potential risk of liver injury.
Lower Acetaminophen Doses Sought
The FDA has asked manufacturers of prescription pain products containing acetaminophen to include no more than 325 mg of the drug in each capsule, tablet, or other dosage unit.
According to a safety announcement by the agency, the action was taken to address the ongoing problem of acetaminophen overdose, a leading cause of severe liver injury in the United States.
The FDA requests that manufacturers of these combination products – including Vicodin and Percocet – add a boxed warning to product labels about the potential risk of severe liver injury if acetaminophen is taken in excessive doses or with alcohol.
Manufacturers have until January 2014 to comply with the recommendations, so a shortage of these medications is not anticipated, according to the agency.
The FDA is also asking clinicians to educate their patients about the dangers of acetaminophen overdose and to advise patients to take no more than the maximum daily dose of acetaminophen (4,000 mg).
“For physicians and other health care providers, we want to emphasize that it's important to talk to patients and make sure that they are aware of the risks of using prescription pain medicines with acetaminophen,” Dr. Sandra Kweder said during a press briefing.
Currently, prescription acetaminophen products contain up to 750 mg of acetaminophen per dosage unit, but there are no data indicating that more than 325 mg of acetaminophen per unit provides greater pain relief, according to the FDA.
The agency's request does not apply to over-the-counter products, which can contain as much as 500 mg per tablet or capsule in the products marketed as extra strength.
Almost half of acetaminophen-related cases of liver failure in the United States are caused by overdoses from prescription opioid-acetaminophen products, which are among the most commonly prescribed products in the United States, accounting for almost 200 million prescriptions dispensed per year.
Rules on Tobacco Tightened
Certain tobacco products – including cigarettes, roll-your-own, and smokeless varieties – that were introduced or changed in the United States after Feb. 15, 2007, must be reviewed by the FDA to show that they are “substantially equivalent” to existing products, Dr. Lawrence Deyton, director of the agency's Center for Tobacco Products, said in a press briefing.
The FDA action is driven by the Family Smoking Prevention and Tobacco Control Act, which became law in June 2009. The law allows the FDA to regulate tobacco products with the goal of protecting public health.
The substantial equivalence provisions are “meant to ensure that new tobacco products or changes to existing products are evaluated by the FDA before they enter the marketplace and are consumed by millions of people,” Dr. Deyton said. “Up to now, tobacco products have been the only mass-consumed products for which users do not know what they are consuming,” he said.
The Tobacco Control Act allows tobacco companies to market products that were available after Feb. 15, 2007, if the companies submit at least a preliminary report to the FDA by March 22, 2011, to show that these products are not significantly different from pre-existing products. Products in existence before Feb. 15, 2007, are not subject to the new FDA review, said Ann Simoneau, director of the Center for Tobacco Products' Office of Compliance and Enforcement.
New products introduced after March 22 will follow a different regulatory pathway, Dr. Deyton said.
Physicians should know that the FDA is now examining certain tobacco products and that manufacturers are required to submit information to the FDA about the products and changes to them, “particularly if those changes might raise new questions about public health,” Dr. Deyton said.
FROM THE FOOD AND DRUG ADMINISTRATION
Policy & Practice
DSM-5 Field Trials Begin
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is getting its first real-world trial at 11 large medical centers and among nearly 4,000 mental health professionals, the American Psychiatric Association has announced. The field trials will test whether proposed diagnostic criteria are understandable and easy for practitioners to use, accurately describe psychiatric problems, and yield consistent diagnoses. Psychiatrists, psychologists, social workers, and psychiatric/mental health nurses will test the new criteria by using them repeatedly to evaluate new and existing patients. After this testing phase, the manual will undergo a second round of public comment, editing, and more field trials lasting into 2012. “It is important that the proposed diagnostic criteria are subjected to rigorous and empirically sound field trials before DSM-5 is published in 2013,” Dr. David Kupfer, DSM-5 Task Force chair, said in a statement.
Grants Fund Lupus Research
The Lupus Foundation of America has made six new grants for studies into what it considers neglected areas of lupus research: pediatric lupus, reproductive health issues in lupus, lupus nephritis, and neuropsychiatric lupus. “The research funded this year tackles some of the most complex and challenging areas of lupus research,” said Sandra C. Raymond, president and CEO of the Washington-based foundation. “These areas of research have suffered from a lack of resources, and in some cases have seen little advancement.” With the new grants, Dr. Bruce C. Richardson of the University of Michigan in Ann Arbor will study the genetics of male lupus; Dr. Richard K. Burt of Northwestern University in Chicago will look at hematopoietic stem cell transplantation in lupus; Dr. Richard J. Quigg of the University of Chicago will study complement manipulation in lupus nephritis; Dr. Martin G. Pomper of the Johns Hopkins School of Medicine in Baltimore will assess imaging microglial activation in neuropsychiatric lupus; Dr. Michelle A. Petri of Johns Hopkins will study the use of levothyroxine in pregnant systemic lupus erythematosus (SLE) patients; and Dr. Kathleen M. O'Neil of the University of Oklahoma in Oklahoma City will look at the effect of puberty on SLE.
Giving Back to the DEA
Americans turned in more than 242,000 pounds of unused or unwanted prescription drugs for disposal as part of the first national prescription drug “Take-Back” campaign, the Drug Enforcement Administration reports. The agency reported a huge turnout of people turning in large quantities of old drugs at more than 4,000 disposal sites being run by law enforcement personnel across the country. For example, at one site a woman turned in nearly 50 years' worth of medications for disposal, while at another site, a man dumped a kitchen drawer full of medications, a DEA announcement said. “The Take-Back campaign was a stunning nationwide success [and] a crucial step toward reducing the epidemic of prescription drug abuse that is plaguing this nation,” said DEA Acting Administrator Michele Leonhart in the announcement.
IOM Backs Nursing Expansion
The roles and responsibilities of nurses should change significantly to meet the increased demand for care created by health care reform, according to an Institute of Medicine report that immediately drew criticism from the American Medical Association. The report urged removal of regulatory and institutional obstacles that prevent nurses from taking on additional patient-care duties. To handle these new responsibilities, nurses should receive higher levels of training through an improved educational system, including a new residency program and additional opportunities for lifelong learning, the institute report said. The AMA took issue with the report's call to expand nurses' scope of practice, saying that nurses do not have nearly the amount of training and clinical experience that doctors do. “With a shortage of both nurses and physicians, increasing the responsibility of nurses is not the answer to the physician shortage,” AMA board member Rebecca J. Patchin said in a statement.
New Rules Target Fraud
The Department of Health and Human Services has proposed new rules aimed at fighting waste, fraud, and abuse in Medicare, Medicaid, and the Children's Health Insurance Program (CHIP). The rules are authorized by the Affordable Care Act and would tighten screening of providers wishing to bill government programs for services, for example, by using broader criminal background checks and even fingerprinting. The rules also require states to terminate from their Medicaid and CHIP programs any provider who has been thrown out of Medicare or another state's health programs. The proposed rule asked for advice on how best to ensure provider compliance.
DSM-5 Field Trials Begin
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is getting its first real-world trial at 11 large medical centers and among nearly 4,000 mental health professionals, the American Psychiatric Association has announced. The field trials will test whether proposed diagnostic criteria are understandable and easy for practitioners to use, accurately describe psychiatric problems, and yield consistent diagnoses. Psychiatrists, psychologists, social workers, and psychiatric/mental health nurses will test the new criteria by using them repeatedly to evaluate new and existing patients. After this testing phase, the manual will undergo a second round of public comment, editing, and more field trials lasting into 2012. “It is important that the proposed diagnostic criteria are subjected to rigorous and empirically sound field trials before DSM-5 is published in 2013,” Dr. David Kupfer, DSM-5 Task Force chair, said in a statement.
Grants Fund Lupus Research
The Lupus Foundation of America has made six new grants for studies into what it considers neglected areas of lupus research: pediatric lupus, reproductive health issues in lupus, lupus nephritis, and neuropsychiatric lupus. “The research funded this year tackles some of the most complex and challenging areas of lupus research,” said Sandra C. Raymond, president and CEO of the Washington-based foundation. “These areas of research have suffered from a lack of resources, and in some cases have seen little advancement.” With the new grants, Dr. Bruce C. Richardson of the University of Michigan in Ann Arbor will study the genetics of male lupus; Dr. Richard K. Burt of Northwestern University in Chicago will look at hematopoietic stem cell transplantation in lupus; Dr. Richard J. Quigg of the University of Chicago will study complement manipulation in lupus nephritis; Dr. Martin G. Pomper of the Johns Hopkins School of Medicine in Baltimore will assess imaging microglial activation in neuropsychiatric lupus; Dr. Michelle A. Petri of Johns Hopkins will study the use of levothyroxine in pregnant systemic lupus erythematosus (SLE) patients; and Dr. Kathleen M. O'Neil of the University of Oklahoma in Oklahoma City will look at the effect of puberty on SLE.
Giving Back to the DEA
Americans turned in more than 242,000 pounds of unused or unwanted prescription drugs for disposal as part of the first national prescription drug “Take-Back” campaign, the Drug Enforcement Administration reports. The agency reported a huge turnout of people turning in large quantities of old drugs at more than 4,000 disposal sites being run by law enforcement personnel across the country. For example, at one site a woman turned in nearly 50 years' worth of medications for disposal, while at another site, a man dumped a kitchen drawer full of medications, a DEA announcement said. “The Take-Back campaign was a stunning nationwide success [and] a crucial step toward reducing the epidemic of prescription drug abuse that is plaguing this nation,” said DEA Acting Administrator Michele Leonhart in the announcement.
IOM Backs Nursing Expansion
The roles and responsibilities of nurses should change significantly to meet the increased demand for care created by health care reform, according to an Institute of Medicine report that immediately drew criticism from the American Medical Association. The report urged removal of regulatory and institutional obstacles that prevent nurses from taking on additional patient-care duties. To handle these new responsibilities, nurses should receive higher levels of training through an improved educational system, including a new residency program and additional opportunities for lifelong learning, the institute report said. The AMA took issue with the report's call to expand nurses' scope of practice, saying that nurses do not have nearly the amount of training and clinical experience that doctors do. “With a shortage of both nurses and physicians, increasing the responsibility of nurses is not the answer to the physician shortage,” AMA board member Rebecca J. Patchin said in a statement.
New Rules Target Fraud
The Department of Health and Human Services has proposed new rules aimed at fighting waste, fraud, and abuse in Medicare, Medicaid, and the Children's Health Insurance Program (CHIP). The rules are authorized by the Affordable Care Act and would tighten screening of providers wishing to bill government programs for services, for example, by using broader criminal background checks and even fingerprinting. The rules also require states to terminate from their Medicaid and CHIP programs any provider who has been thrown out of Medicare or another state's health programs. The proposed rule asked for advice on how best to ensure provider compliance.
DSM-5 Field Trials Begin
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is getting its first real-world trial at 11 large medical centers and among nearly 4,000 mental health professionals, the American Psychiatric Association has announced. The field trials will test whether proposed diagnostic criteria are understandable and easy for practitioners to use, accurately describe psychiatric problems, and yield consistent diagnoses. Psychiatrists, psychologists, social workers, and psychiatric/mental health nurses will test the new criteria by using them repeatedly to evaluate new and existing patients. After this testing phase, the manual will undergo a second round of public comment, editing, and more field trials lasting into 2012. “It is important that the proposed diagnostic criteria are subjected to rigorous and empirically sound field trials before DSM-5 is published in 2013,” Dr. David Kupfer, DSM-5 Task Force chair, said in a statement.
Grants Fund Lupus Research
The Lupus Foundation of America has made six new grants for studies into what it considers neglected areas of lupus research: pediatric lupus, reproductive health issues in lupus, lupus nephritis, and neuropsychiatric lupus. “The research funded this year tackles some of the most complex and challenging areas of lupus research,” said Sandra C. Raymond, president and CEO of the Washington-based foundation. “These areas of research have suffered from a lack of resources, and in some cases have seen little advancement.” With the new grants, Dr. Bruce C. Richardson of the University of Michigan in Ann Arbor will study the genetics of male lupus; Dr. Richard K. Burt of Northwestern University in Chicago will look at hematopoietic stem cell transplantation in lupus; Dr. Richard J. Quigg of the University of Chicago will study complement manipulation in lupus nephritis; Dr. Martin G. Pomper of the Johns Hopkins School of Medicine in Baltimore will assess imaging microglial activation in neuropsychiatric lupus; Dr. Michelle A. Petri of Johns Hopkins will study the use of levothyroxine in pregnant systemic lupus erythematosus (SLE) patients; and Dr. Kathleen M. O'Neil of the University of Oklahoma in Oklahoma City will look at the effect of puberty on SLE.
Giving Back to the DEA
Americans turned in more than 242,000 pounds of unused or unwanted prescription drugs for disposal as part of the first national prescription drug “Take-Back” campaign, the Drug Enforcement Administration reports. The agency reported a huge turnout of people turning in large quantities of old drugs at more than 4,000 disposal sites being run by law enforcement personnel across the country. For example, at one site a woman turned in nearly 50 years' worth of medications for disposal, while at another site, a man dumped a kitchen drawer full of medications, a DEA announcement said. “The Take-Back campaign was a stunning nationwide success [and] a crucial step toward reducing the epidemic of prescription drug abuse that is plaguing this nation,” said DEA Acting Administrator Michele Leonhart in the announcement.
IOM Backs Nursing Expansion
The roles and responsibilities of nurses should change significantly to meet the increased demand for care created by health care reform, according to an Institute of Medicine report that immediately drew criticism from the American Medical Association. The report urged removal of regulatory and institutional obstacles that prevent nurses from taking on additional patient-care duties. To handle these new responsibilities, nurses should receive higher levels of training through an improved educational system, including a new residency program and additional opportunities for lifelong learning, the institute report said. The AMA took issue with the report's call to expand nurses' scope of practice, saying that nurses do not have nearly the amount of training and clinical experience that doctors do. “With a shortage of both nurses and physicians, increasing the responsibility of nurses is not the answer to the physician shortage,” AMA board member Rebecca J. Patchin said in a statement.
New Rules Target Fraud
The Department of Health and Human Services has proposed new rules aimed at fighting waste, fraud, and abuse in Medicare, Medicaid, and the Children's Health Insurance Program (CHIP). The rules are authorized by the Affordable Care Act and would tighten screening of providers wishing to bill government programs for services, for example, by using broader criminal background checks and even fingerprinting. The rules also require states to terminate from their Medicaid and CHIP programs any provider who has been thrown out of Medicare or another state's health programs. The proposed rule asked for advice on how best to ensure provider compliance.
Business Briefs
FDA Clears Glucose Monitoring Strip
Abbott has received Food and Drug Administration clearance to market its FreeStyle Lite blood glucose monitoring strip. First shipments will go out in July; widespread availability is expected by the end of August. The test trips use a glucose dehydrogenase flavin adenine dinucleotide, which is unaffected by common nonglucose sugars such as maltose and galactose, and which minimizes the potential for other interference, according to a company statement. The new strips are designed to ensure faster blood application and a reduction in the number of error messages and wasted strips. These features provide a “better testing experience … especially for people who use insulin to manage their diabetes,” said Heather L. Mason, senior vice president of Abbott Diabetes Care. The FDA clearance follows Abbott's announcement of the product's European availability.
GSK Inks Deal With Dong-A Pharmaceutical
In an alliance designed to help GlaxoSmithKline gain a share in the rapidly growing Korean pharmaceutical market, GSK is paying 142.9 billion South Korean won ($128.7 million) to acquire a 9.9% stake in Dong-A Pharmaceutical, South Korea's leading prescription and over-the-counter drug company. The deal will make GSK Dong-A's second largest shareholder after Kang Shin-Ho, Dong-A's chairman, who holds a 10.6% share. According to GSK, the initial focus of the collaboration will be to copromote products from both firms in Korea's primary care market. A new business unit will be established within Seoul-based Dong-A to capture additional synergies. These could include partnerships on select Dong-A chemical entities leveraging GSK's global commercial infrastructure and expertise, as well as codevelopment of branded generics, the company added. “It's an innovative partnership to support GSK's growth and diversification strategy,” said Kim Jin-Ho, general manager of GSK Korea. The partnership could serve as a cushion for GSK's pending loss of patent protection on some of its drugs, said Bae Ki-Dal of Shinhan Investment Corp. “It's fair to say that GSK and Dong-A are forming a united front against potential setbacks,” he said.
Takeda Cuts Jobs, Boosts R&D
Citing patent loss on key products sold in North America along with the strong yen against the U.S. dollar and other currencies, the Japanese pharmaceutical company Takeda reported revenue decreases of 4.7% in fiscal 2009, its first sales decline in 19 years. The type 2 diabetes drug Actos (pioglitazone), one of Takeda's core products, will lose its U.S. patent in 2011. The company's settlement of patent infringement lawsuits with six of eight generic firms for Actos and Actoplus Met (pioglitazone/metformin) will delay the generics' penetration until August 2012. Anticipating a 5% reduction revenues and a 26% loss in operating income for fiscal 2010, Takeda will boost research and development expenditures to accelerate pipeline development. The company plans to launch alogliptin, which it positions as a key post-Actos product, in 2012. Basen (voglibose), a type 2 diabetes treatment, and several other company products also are facing expirations. In light of patent expiries and revenue loss, Takeda announced that it will let go 10% of its employees—about 2,000 people. Most of the cuts are expected in the company's U.S. subsidiary, Takeda Pharmaceuticals North America.
Pfizer, Washington U. in 5-Year Deal
Pfizer has announced a 5-year deal with Washington University in St. Louis, during which time the university will receive $22.5 million and its researchers will have access to a searchable, proprietary database of Pfizer compounds and related information. It will be a “truly collaborative partnership,” said Don Frail, chief scientific officer of Pfizer's Indications Discovery Unit. The arrangement enables the pharmaceutical company to take advantage of external research and development capabilities at a nominal price. Pfizer's history of partnerships with Washington University, which goes back nearly 30 years, has shown that the school's Center for Genome Sciences has significant expertise in a broad range of diseases, including diabetes and related metabolic disorders, asthma, chronic obstructive pulmonary disease, and Alzheimer's, Mr. Frail said.
Reporters and editors from Elsevier's “The Pink Sheet” contributed to this column.
FDA Clears Glucose Monitoring Strip
Abbott has received Food and Drug Administration clearance to market its FreeStyle Lite blood glucose monitoring strip. First shipments will go out in July; widespread availability is expected by the end of August. The test trips use a glucose dehydrogenase flavin adenine dinucleotide, which is unaffected by common nonglucose sugars such as maltose and galactose, and which minimizes the potential for other interference, according to a company statement. The new strips are designed to ensure faster blood application and a reduction in the number of error messages and wasted strips. These features provide a “better testing experience … especially for people who use insulin to manage their diabetes,” said Heather L. Mason, senior vice president of Abbott Diabetes Care. The FDA clearance follows Abbott's announcement of the product's European availability.
GSK Inks Deal With Dong-A Pharmaceutical
In an alliance designed to help GlaxoSmithKline gain a share in the rapidly growing Korean pharmaceutical market, GSK is paying 142.9 billion South Korean won ($128.7 million) to acquire a 9.9% stake in Dong-A Pharmaceutical, South Korea's leading prescription and over-the-counter drug company. The deal will make GSK Dong-A's second largest shareholder after Kang Shin-Ho, Dong-A's chairman, who holds a 10.6% share. According to GSK, the initial focus of the collaboration will be to copromote products from both firms in Korea's primary care market. A new business unit will be established within Seoul-based Dong-A to capture additional synergies. These could include partnerships on select Dong-A chemical entities leveraging GSK's global commercial infrastructure and expertise, as well as codevelopment of branded generics, the company added. “It's an innovative partnership to support GSK's growth and diversification strategy,” said Kim Jin-Ho, general manager of GSK Korea. The partnership could serve as a cushion for GSK's pending loss of patent protection on some of its drugs, said Bae Ki-Dal of Shinhan Investment Corp. “It's fair to say that GSK and Dong-A are forming a united front against potential setbacks,” he said.
Takeda Cuts Jobs, Boosts R&D
Citing patent loss on key products sold in North America along with the strong yen against the U.S. dollar and other currencies, the Japanese pharmaceutical company Takeda reported revenue decreases of 4.7% in fiscal 2009, its first sales decline in 19 years. The type 2 diabetes drug Actos (pioglitazone), one of Takeda's core products, will lose its U.S. patent in 2011. The company's settlement of patent infringement lawsuits with six of eight generic firms for Actos and Actoplus Met (pioglitazone/metformin) will delay the generics' penetration until August 2012. Anticipating a 5% reduction revenues and a 26% loss in operating income for fiscal 2010, Takeda will boost research and development expenditures to accelerate pipeline development. The company plans to launch alogliptin, which it positions as a key post-Actos product, in 2012. Basen (voglibose), a type 2 diabetes treatment, and several other company products also are facing expirations. In light of patent expiries and revenue loss, Takeda announced that it will let go 10% of its employees—about 2,000 people. Most of the cuts are expected in the company's U.S. subsidiary, Takeda Pharmaceuticals North America.
Pfizer, Washington U. in 5-Year Deal
Pfizer has announced a 5-year deal with Washington University in St. Louis, during which time the university will receive $22.5 million and its researchers will have access to a searchable, proprietary database of Pfizer compounds and related information. It will be a “truly collaborative partnership,” said Don Frail, chief scientific officer of Pfizer's Indications Discovery Unit. The arrangement enables the pharmaceutical company to take advantage of external research and development capabilities at a nominal price. Pfizer's history of partnerships with Washington University, which goes back nearly 30 years, has shown that the school's Center for Genome Sciences has significant expertise in a broad range of diseases, including diabetes and related metabolic disorders, asthma, chronic obstructive pulmonary disease, and Alzheimer's, Mr. Frail said.
Reporters and editors from Elsevier's “The Pink Sheet” contributed to this column.
FDA Clears Glucose Monitoring Strip
Abbott has received Food and Drug Administration clearance to market its FreeStyle Lite blood glucose monitoring strip. First shipments will go out in July; widespread availability is expected by the end of August. The test trips use a glucose dehydrogenase flavin adenine dinucleotide, which is unaffected by common nonglucose sugars such as maltose and galactose, and which minimizes the potential for other interference, according to a company statement. The new strips are designed to ensure faster blood application and a reduction in the number of error messages and wasted strips. These features provide a “better testing experience … especially for people who use insulin to manage their diabetes,” said Heather L. Mason, senior vice president of Abbott Diabetes Care. The FDA clearance follows Abbott's announcement of the product's European availability.
GSK Inks Deal With Dong-A Pharmaceutical
In an alliance designed to help GlaxoSmithKline gain a share in the rapidly growing Korean pharmaceutical market, GSK is paying 142.9 billion South Korean won ($128.7 million) to acquire a 9.9% stake in Dong-A Pharmaceutical, South Korea's leading prescription and over-the-counter drug company. The deal will make GSK Dong-A's second largest shareholder after Kang Shin-Ho, Dong-A's chairman, who holds a 10.6% share. According to GSK, the initial focus of the collaboration will be to copromote products from both firms in Korea's primary care market. A new business unit will be established within Seoul-based Dong-A to capture additional synergies. These could include partnerships on select Dong-A chemical entities leveraging GSK's global commercial infrastructure and expertise, as well as codevelopment of branded generics, the company added. “It's an innovative partnership to support GSK's growth and diversification strategy,” said Kim Jin-Ho, general manager of GSK Korea. The partnership could serve as a cushion for GSK's pending loss of patent protection on some of its drugs, said Bae Ki-Dal of Shinhan Investment Corp. “It's fair to say that GSK and Dong-A are forming a united front against potential setbacks,” he said.
Takeda Cuts Jobs, Boosts R&D
Citing patent loss on key products sold in North America along with the strong yen against the U.S. dollar and other currencies, the Japanese pharmaceutical company Takeda reported revenue decreases of 4.7% in fiscal 2009, its first sales decline in 19 years. The type 2 diabetes drug Actos (pioglitazone), one of Takeda's core products, will lose its U.S. patent in 2011. The company's settlement of patent infringement lawsuits with six of eight generic firms for Actos and Actoplus Met (pioglitazone/metformin) will delay the generics' penetration until August 2012. Anticipating a 5% reduction revenues and a 26% loss in operating income for fiscal 2010, Takeda will boost research and development expenditures to accelerate pipeline development. The company plans to launch alogliptin, which it positions as a key post-Actos product, in 2012. Basen (voglibose), a type 2 diabetes treatment, and several other company products also are facing expirations. In light of patent expiries and revenue loss, Takeda announced that it will let go 10% of its employees—about 2,000 people. Most of the cuts are expected in the company's U.S. subsidiary, Takeda Pharmaceuticals North America.
Pfizer, Washington U. in 5-Year Deal
Pfizer has announced a 5-year deal with Washington University in St. Louis, during which time the university will receive $22.5 million and its researchers will have access to a searchable, proprietary database of Pfizer compounds and related information. It will be a “truly collaborative partnership,” said Don Frail, chief scientific officer of Pfizer's Indications Discovery Unit. The arrangement enables the pharmaceutical company to take advantage of external research and development capabilities at a nominal price. Pfizer's history of partnerships with Washington University, which goes back nearly 30 years, has shown that the school's Center for Genome Sciences has significant expertise in a broad range of diseases, including diabetes and related metabolic disorders, asthma, chronic obstructive pulmonary disease, and Alzheimer's, Mr. Frail said.
Reporters and editors from Elsevier's “The Pink Sheet” contributed to this column.