User login
Screening for Alcoholism in the Primary Care Setting
BACKGROUND: This study assessed which demographic groups were most likely to consume alcohol excessively, and which groups had received inquiries and discussion about alcohol use from their physicians compared with discussions about other health risks.
STUDY DESIGN: This was a cross-sectional study using data from the Centers for Disease Control Behavioral Risk Factors Surveillance System 1997 data set that represents a stratified random sample in the United States.
POPULATION: We selected 23,349 adults who reported a routine physical examination within the last 3 years.
OUTCOMES MEASURED: The main variables involved responses to questions about alcohol intake and whether the respondent’s physician had initiated discussions about drinking.
RESULTS: Physicians spoke to patients about alcohol use much less frequently than about other health-related behaviors. Discussions were roughly targeted to groups with the largest intake. However, physicians were least likely to speak with white patients, women, and widows who drank significantly.
CONCLUSIONS: Regularly asking patients about alcohol use could substantially reduce the under-recognition of alcoholism. Since brief counseling is effective, negative consequences of excessive alcohol intake may be avoided.
- Alcohol screening occurs less frequently than screening about other health-related behaviors.
- There were no demographic groups in which the prevalence of excessive drinking was so low that general screening was not appropriate.
- Physicians frequently miss the opportunity to discuss alcohol use with patients in certain groups, such as white patients and women (widows, in particular).
Physicians and related health care workers are well positioned to detect possible alcohol-related problems during routine patient visits, provided the appropriate screening procedures are implemented.2-4 Ideally, the primary care clinician should be the most prominent source of alcohol abuse screening and referrals, rather than the provider of treatment after an alcohol-related incident.
Although screening for alcoholism adds another step to an already over-worked health care system, it can result in substantial benefits by reducing the burden of overall health care costs. According to recent information, alcohol abuse costs our society $184.6 billion.5 In 1997, an estimated 1.3 million hospital discharges reported an alcohol-related diagnosis.6 And an estimated 12,870 alcohol-related traffic fatalities accounted for nearly one third of all traffic deaths in that same year.7 Even when individuals reamin socially functional and do not meet the formal criteria for an alcohol-related disorder, excessive use of alcohol is associated with a variety of medical problems. Although cardioprotective effects have been reported with moderate use (ie, 1 to 2 drinks per day), the list of medical complications associated with longstanding alcoholism (hypertension, cardiomyopathy, cirrhosis, erosive gastris, pancreatitis, and esophageal varices, for example) account for considerable morbidity and mortality.8,9 Increased alcohol consumption over a 1-year period is also associated with accidents and injuries necessitating emergency services.10
Because the primary care physician is in a unique position to influence the preventive care of the community they serve, our study examined alcohol screening in the primary care setting. The following 2 questions were asked: (1) Which patients were assessed for excessive alcohol use, and what patient characteristics predicted the assessment? and (2) How often did discussions about alcohol occur compared with other health risk discussions (eg, eating habits or smoking)?
Methods
Subjects
This is a secondary analysis of data from an epidemiologic telephone interview conducted by the Behavioral Risk Factors Surveillance System (BRFSS)1 involving a random stratified sample of people living within the United States. In the 1997 interviews, all state interviews included questions about alcohol consumption. Alaska, Colorado, Idaho, Louisiana, Missouri, New York, North Carolina, Oklahoma, Pennsylvania, Virginia, and Wyoming included a counseling module that asked, “Has a doctor or other health professional ever talked with you about alcohol use?”
The 1997 BRFSS data set represents 135,582 interviews. The sample reported here includes only respondents who reported a routine physical examination within the last 3 years and who were asked questions from the counseling module (n = 23,349), as well as questions about other health habits. There were 9106 men (mean age = 45.82 years; SD = 16.86) and 14,203 women (mean age = 46.90; SD = 17.44) who responded.
Excessive drinking was defined as consuming 60 alcoholic beverages per month or 5 on a single occasion (binge drinking) in the month prior to the interview (n = 2772). The 60 beverages per month threshold follows recommendations by the National Institute for Alcohol Abuse and Alcoholism and the US Department of Health and Human Services’ Dietary Guidelines for Americans.11,12
Statistical analysis
Analysis used the sampling weights provided by the Centers for Disease Control. The data were weighted so that the summary statistics, standard errors, and test statistics took into account the sampling design and represented estimates in the total US. population. We used the procedures described by Levy and Lemeshow,13 and implemented them using STATA.14 These included simple chi-square tests, logistic regression with F- or t-approximations. The F- and t-approximations for the logistic regression were necessary to adjust for the complex survey design.13 Hierarchical (protected) testing procedures helped correct for multiple comparisons. We used omnibus tests for variables with multiple options (eg, marital status), and only considered follow-up tests when the overall test result was significant. Furthermore, a conservative threshold for significance (P < .01) was a compromise to the Bonferroni correction for multiple comparisons.
Results
Approximately 1 in 6 patients (16.1%; 95% confidence interval [CI], 15.4 - 16.8) reported that a physician or other health care worker had initiated a discussion about alcohol use. Table W1* compares patients who reported such a discussion with those who did not. Physicians talked to male patients about alcohol use most frequently. This corresponds to men reporting nearly 3 times more drinks consumed (12.9 drinks/month) than women (4.7 drinks/month; t = 16.26, df = 18,323, P < .001).
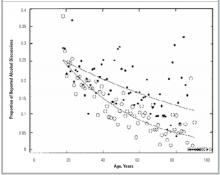
In general, physicians spoke about alcohol more often to younger people. There was a significant interaction, however, between sex and age, as shown in Figure 1. Discussions with women demonstrated a clear decrease in frequency with age; discussions with men decreased with age more slowly.
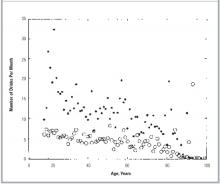
The amount of drinking in our sample, indexed by the number of drinks per month, is shown in Figure 2. Both the frequency of discussions and amount of alcohol consumed declined with advancing age. Women drank less alcohol than men overall and showed a moderate decline in use with age.
Nonwhite respondents reported more physician discussions about alcohol than did whites. However, white patients reported greater consumption (8.9 drinks/month) than nonwhites (6.8 drinks; t = 2.79, df = 18253, P < .005).
The lowest income group reported being advised about alcohol most frequently. Interestingly, the highest income respondents tended to drink more than those with less income. Marital status also predicted alcohol discussions. Physicians discussed alcohol more often with patients who were unmarried. While divorced patients reported discussions about alcohol use frequently, widowed patients reported them least often.
Discussions about alcohol occurred more often with respondents who had consumed alcohol within the month prior to the interview. Respondents who reported having these discussions also consumed more (14.6 drinks/month) than those who did not report a discussion (7.3 drinks/month, t = 7.20, df = 17985, P < .001). People who binge drank were more than twice as likely (OR = 2.25; 95% CI, 1.94 - 2.60) to report such a discussion (27.5%).
All of these predictors of a discussion about alcohol use were entered into a multivariate logistic regression. Backward elimination removed items that failed to provide independent information. The final model appears in the Table. Factors other than drinking behaviors that uniquely increased the chance of such a discussion about alcohol were being young, male, nonwhite, and of lower income.
More than 1 in 9 people (12.3%; n = 2768) in the sample met criteria for excessive drinking (ie, consuming 60 drinks per month or drinking 5 or more drinks on a single occasion in the last month). Within this group, 11.9% engaged in binge drinking and 3.5% consumed 60 drinks a month. Most were men (71.3%) with a mean age of 35 years, and they averaged 39.7 (95% CI, 36.74 - 42.74) drinks per month. They binged an average of 3.44 (95% CI, 3.18 - 3.70) times during the last month.
Slightly more than 1 in 4 excessive drinkers (28%; 95% CI, 25.41 - 30.69) reported a discussion about alcohol with a physician. While none of the demographic factors met our stringent criteria for significance (P < .01), many would have met the more usual threshold of P < .05. For example, among the respondents with excessive alcohol use, 23.9% of the women had been screened by their physicians compared with 29.9% of the men (P < .013). This suggests that these women may receive less preventive discussions and screening than they require. While the percent of nonwhite respondents who drank excessively and were successfully screened was above the mean rate overall (35.6%), the percent of white patients was lower than the mean (26.4%; P < .012). Compared with married patients, excessive drinkers who were divorced (35.2%; P < .019) or separated (38.1%; P < .091) reported a higher frequency of screening. Widowed patients with excessive alcohol use rarely reported screening (13%; P < .032).
TABLE
FINAL LOGISTIC REGRESSION PREDICTING A DISCUSSION ABOUT ALCOHOL
| Predictor | Beta | OR(95% CI) |
|---|---|---|
| Sex | -0.48 | 0.62 (0.44 - 0.87)* |
| Age | -0.028 | 0.97 (0.97 - 0.98)† |
| Age, by sex interaction | 0.02 | 1.02 (1.01 - 1.03)† |
| Did not drink ‡ | -0.57 | 0.57 (0.44 - 0.73)† |
| Drinks per month § | 0.28 | 1.33 (1.24 - 1.43)† |
| Income | -0.08 | 0.93 (0.90 - 0.96)† |
| Race ¶ | 0.34 | 1.41 (1.22 - 1.63)† |
| Constant | -0.24 | |
| OR denotes odds ratio from univariate logistic regression; CI, confidence interval. | ||
| *P< .01 | ||
| †P< .001 | ||
| Respondent reported not drinking any alcohol in the last month. | ||
| § Log transform of the number of drinks per month. | ||
| ¶ Race coded as white versus nonwhite. | ||
FIGURE 1
LOGISTIC REGRESSION PREDICTING THE OCCURRENCE OF PHYSICIAN DISCUSSION ABOUT ALCOHOL FROM THE PATIENTS’ AGE AND SEX (WOMEN =o MEN =●).
FIGURE 2
MEAN NUMBERS OF ALCOHOLIC DRINKS CONSUMED BY AGE AND SEX (WOMEN = o MEN = ● ).
Other preventive services
We also assessed the rate of talks about healthy eating as a comparison for the alcohol discussions. A total of 44.6% of patients reported having a conversation about healthy eating compared with 16.1% having an alcohol discussion. On the chance that people who drank excessively might differentially remember conversations with their physicians, we assessed the association between alcohol use and reports of experiencing counseling on healthy eating. No significant associations were found between reported conversations about eating and any variable related to alcohol consumption even after controlling for sex, age, sex-by-age interaction, race, income, and education. Similar results were obtained for discussions about exercise, AIDS, and illegal drugs. Discussions about illegal drug use occurred less frequently than discussions about alcohol use (12.5%). Discussions about AIDS were reported by 26.1% of the respondents, exercise-related conversations were reported 47.4% of the time, and smoking was mentioned by 49.2% of the respondents. Considering any preventive health discussions (smoking, drinking, drug abuse, exercise, healthy eating, or AIDS), 97.4% of the respondents reported a discussion of at least 1 topic.
Discussion
Physicians currently incorporate preventive counseling about behavioral health risks as part of standard clinical care. In a recent survey of general practitioners, 97% of those surveyed thought that members of their profession should inquire about drinking behaviors.15 Moreover, brief office visit screening followed by physician advice has been documented as effective in reducing alcohol consumption.16,17 Despite the general positive opinion of alcohol screening, however, discussions about AIDS and other health-related behaviors were discussed much more frequently than alcohol-related behaviors.
Our analysis identified patients who consume a significant amount of alcohol, yet did not report being screened or counseled by their physicians. We gathered information about the magnitude of use, as well as about the presence or absence of a discussion regarding alcohol. This allowed us to examine 2 important aspects of alcohol screening: (1) the demographic features that predicted it, and (2) whether these demographic features represented patients who actually consumed large amounts of alcohol and could therefore benefit from counseling.
Although the BRFSS did not assess alcohol dependence or abuse directly, the goal of the study was to designate which patients might be appropriate candidates for screening or preventive counseling. Assessments of alcohol abuse or dependence using strict Diagnostic and Statistical Manual of Mental Disorders – 4th Edition (DSM-IV) criteria require insight, as well as a willingness to share this information with the interviewer. Kosten and Rounsaville18 found that DSM-based diagnostic interviews for alcoholism and substance abuse showed the lowest sensitivity relative to other psychiatric diagnoses. Therefore, more recent surveys of alcohol abuse assess the quantity of consumption before applying strict DSM-IV criteria.19,20 Although participants may also minimize actual consumption, the screening for quantity requires less insight than a formal diagnosis and may more effectively identify candidates for counseling. However, our findings suggest that physicians do not routinely attempt to ascertain alcohol use quantitatively.21,22 Implementing alcohol screening as a routine preventive health care practice would allow physicians to detect problems without relying on insightful spontaneous reporting from patients.
The most successful strategy to identify more candidates for treatment involves simply screening a larger number of patients, especially high-risk patients. Our data suggest that physicians do target discussions somewhat toward people who report excessive alcohol consumption. Approximately 16% of the general patient population reported such a discussion, but this rate was greater (27.8%) among heavy or binge drinkers. Unfortunately, these data also suggest that the majority of patients who might benefit from such counseling, did not report a discussion about alcohol use. Individuals who are likely to be appropriate candidates but who were not counseled include white patients and women (widows, in particular).
The frequency of discussions about alcohol for women and widows who drank excessively was low. This finding is consistent with current research demonstrating that alcohol problems among women, and widowed women in particular, are under-recognized. Physiologically, the lower body water volume in women, especially in elderly women, increases the detrimental effects of alcohol.23 Physicians also appear to have more difficulty recognizing alcohol problems among the elderly.24 Alcohol-related symptoms among elderly women may be misinterpreted as caused by depression, anxiety, or other psychiatric problems.25 Elderly women taking psychoactive medications or medications with sedative effects may be even more difficult to assess. Moreover, our analysis categorized excessive drinking using a single criterion for all respondents. Evidence is mounting that indicates that women26 and the elderly23 are more at risk from lower levels of drinking. Had we lowered our criterion for these patients, the magnitude of problem drinking would have appeared even greater.
Limitations
There are several limitations to our study. A number of reasons, including forgetfulness or inattention, may account for under-reporting. An overall problem with memory is unlikely, since almost all respondents remembered at least one discussion about some kind of health risk. Nonetheless, patients may be selectively less likely to recall a discussion about alcohol because of emotional associations with the topic. However, it is unclear why memory would be less reliable about alcohol use than memory about another potentially emotionally-charged topic, such as AIDS.
Additionally, our information was self-reported through a telephone interview. There have been positive study results published that validate the BRFSS survey data on alcohol consumption.27,28 Nevertheless, the potential remains that respondents underestimate their alcohol use, and this might lead to false-negatives. Furthermore, the nature of the BRFSS question for alcohol discussions is somewhat ambiguous since we do not know if the discussion was a screening for excessive drinking or simply educational counseling.
Conclusions
Ideally, alcohol screening should occur in all primary care office visits, but given the extreme time constraints in the clinic setting, identification of under-recognized groups for targeted screening may enhance the recognition of alcohol abuse in a most time-effective manner.
1. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Atlanta: National Center for Chronic Disease Prevention and Health Promotion, US Department of Health and Human Services, 1997.
2. The National Center on Addiction and Substance Abuse at Columbia University. Missed Opportunity: National Survey of Primary Care Physicians and Patients on Substance Abuse. New York: The National Center on Addiction and Substance Abuse at Columbia University, 2000.
3. Leshner AI. Science-based views of drug addiction and its treatment. JAMA 1999;282:1314-16.
4. Weisner C, Schmidt LA. Expanding the frame of health services research in the drug abuse field. Health Serv Res 1995;30:707-26.
5. Department of Health and Human Services, National Institutes of Health. Disease-Specific Estimates of Direct and Indirect Costs of Illness and NIH Support: Fiscal Year 2000 Update. Washington, DC: Department of Health and Human Services, National Institutes of Health, 2000.
6. Whitmore CC, Stinson FS, Dufour MC. Surveillance Report #50. Trends in Alcohol-Related Morbidity Among Short-Stay Community Hospital Discharges, United States, 1979-97. Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1999.
7. National Institute of Alcohol Abuse and Alcoholism. Traffic crashes, traffic crash fatalities, and alcohol-related traffic crash fatalities, United States, 1977-97. Washington, DC: National Institute of Alcohol Abuse and Alcoholism, 1999.
8. Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly US adults. New Eng J Med 1997;337:1705-14.
9. Gorelick PB, Erkinjuntti T, Hofman A, Rocca WA, Skoog I, Winblad B. Prevention of vascular dementia. Alzheimer Dis Assoc Disord 1999;3:S131-39
10. Borges G, Cherpitel CJ, Medina-Mora ME, Mondragon L, Casanova L. Alcohol consumption in emergency room patients and the general population: a population based study. Alcohol Clin Exp Res 1998;22:1986-91.
11. National Institute on Alcohol Abuse and Alcoholism. Physicians’ guide to helping patients with alcohol problems. Washington, DC: US Department of Health and Human Services, 1995.
12. US Department of Health and Human Services. Nutrition and your health: dietary guidelines for Americans. 3rd edition. Washington, DC: Supt of Docs, US Govt Print Office, 1990.
13. Levy PS, Lemeshow S. Sampling of populations. New York: John Wiley & Sons, 1999.
14. Stata Corporation. Stata 6.0. College Station, TX: Stata Corporation, 2000.
15. Herbert C, Bass F. Early at-risk alcohol intake. Definitions and physicians’ role in modifying behavior. Can Fam Phys 1997;43:639-44.
16. Fleming MG, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice from problem alcohol drinkers. J Am Med Assoc 1997;277:1039-45.
17. Wallace P, Cutler S, Haines A. Randomized controlled trial of general practitioner intervention in patients with excessive alcohol consumption. Br Med J 1988;297:663-68.
18. Kosten TA, Rounsaville BJ. Sensitivity of psychiatric diagnosis based on the best estimate procedure. Am J Psych 1992;149:1225-27.
19. First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV axis I disorders—clinician version. New York: Biometrics Research Department, New York State Psychiatric Institute, 1997.
20. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Study. Arch Gen Psych 1994;51:8-19.
21. Brown RL, Leonard T, Saunders LA, Papasouliotis O. A 2-item conjoint screen for alcohol and other drug problems. J Am Board Fam Pract 2001;14:95-106.
22. Hays RD, Ellickson PL. Comparison of the Rost and the CAGE alcohol screening instruments in young adults. Subst Use Misuse 2001;36:639-51.
23. National Institute on Alcohol Abuse and Alcoholism. Alcohol alert #40: alcohol and aging. Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1998.
24. Curtis JR, Geller G, Stokes EJ, Levine DM, Moore RD. Characteristics, diagnosis, and treatment of alcoholism in elderly patients. J Am Geriatrics Soc 1989;37:310-16.
25. The National Center on Addiction and Substance Abuse at Columbia University. Under the rug: substance abuse and the mature woman. New York: The National Center on Addiction and Substance Abuse at Columbia University, 1998.
26. National Institute on Alcohol Abuse and Alcoholism. Alcohol alert #46: are women more vulnerable to alcohol’s effects? Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1999.
27. Smith PF, Remington PL, Williamson DF, Anda RF. A comparison of alcohol sales data with survey data on self-reported alcohol use in 21 states. Am J Public Health 1990;0:309-12.
28. Anda RF, Williamson DF, Dodson D, Remington PL. Telephone versus in-person reporting of smoking and alcohol use: a comparison of 2 statewide surveys. Am J Health Promotion 1989;4:32-36.
BACKGROUND: This study assessed which demographic groups were most likely to consume alcohol excessively, and which groups had received inquiries and discussion about alcohol use from their physicians compared with discussions about other health risks.
STUDY DESIGN: This was a cross-sectional study using data from the Centers for Disease Control Behavioral Risk Factors Surveillance System 1997 data set that represents a stratified random sample in the United States.
POPULATION: We selected 23,349 adults who reported a routine physical examination within the last 3 years.
OUTCOMES MEASURED: The main variables involved responses to questions about alcohol intake and whether the respondent’s physician had initiated discussions about drinking.
RESULTS: Physicians spoke to patients about alcohol use much less frequently than about other health-related behaviors. Discussions were roughly targeted to groups with the largest intake. However, physicians were least likely to speak with white patients, women, and widows who drank significantly.
CONCLUSIONS: Regularly asking patients about alcohol use could substantially reduce the under-recognition of alcoholism. Since brief counseling is effective, negative consequences of excessive alcohol intake may be avoided.
- Alcohol screening occurs less frequently than screening about other health-related behaviors.
- There were no demographic groups in which the prevalence of excessive drinking was so low that general screening was not appropriate.
- Physicians frequently miss the opportunity to discuss alcohol use with patients in certain groups, such as white patients and women (widows, in particular).
Physicians and related health care workers are well positioned to detect possible alcohol-related problems during routine patient visits, provided the appropriate screening procedures are implemented.2-4 Ideally, the primary care clinician should be the most prominent source of alcohol abuse screening and referrals, rather than the provider of treatment after an alcohol-related incident.
Although screening for alcoholism adds another step to an already over-worked health care system, it can result in substantial benefits by reducing the burden of overall health care costs. According to recent information, alcohol abuse costs our society $184.6 billion.5 In 1997, an estimated 1.3 million hospital discharges reported an alcohol-related diagnosis.6 And an estimated 12,870 alcohol-related traffic fatalities accounted for nearly one third of all traffic deaths in that same year.7 Even when individuals reamin socially functional and do not meet the formal criteria for an alcohol-related disorder, excessive use of alcohol is associated with a variety of medical problems. Although cardioprotective effects have been reported with moderate use (ie, 1 to 2 drinks per day), the list of medical complications associated with longstanding alcoholism (hypertension, cardiomyopathy, cirrhosis, erosive gastris, pancreatitis, and esophageal varices, for example) account for considerable morbidity and mortality.8,9 Increased alcohol consumption over a 1-year period is also associated with accidents and injuries necessitating emergency services.10
Because the primary care physician is in a unique position to influence the preventive care of the community they serve, our study examined alcohol screening in the primary care setting. The following 2 questions were asked: (1) Which patients were assessed for excessive alcohol use, and what patient characteristics predicted the assessment? and (2) How often did discussions about alcohol occur compared with other health risk discussions (eg, eating habits or smoking)?
Methods
Subjects
This is a secondary analysis of data from an epidemiologic telephone interview conducted by the Behavioral Risk Factors Surveillance System (BRFSS)1 involving a random stratified sample of people living within the United States. In the 1997 interviews, all state interviews included questions about alcohol consumption. Alaska, Colorado, Idaho, Louisiana, Missouri, New York, North Carolina, Oklahoma, Pennsylvania, Virginia, and Wyoming included a counseling module that asked, “Has a doctor or other health professional ever talked with you about alcohol use?”
The 1997 BRFSS data set represents 135,582 interviews. The sample reported here includes only respondents who reported a routine physical examination within the last 3 years and who were asked questions from the counseling module (n = 23,349), as well as questions about other health habits. There were 9106 men (mean age = 45.82 years; SD = 16.86) and 14,203 women (mean age = 46.90; SD = 17.44) who responded.
Excessive drinking was defined as consuming 60 alcoholic beverages per month or 5 on a single occasion (binge drinking) in the month prior to the interview (n = 2772). The 60 beverages per month threshold follows recommendations by the National Institute for Alcohol Abuse and Alcoholism and the US Department of Health and Human Services’ Dietary Guidelines for Americans.11,12
Statistical analysis
Analysis used the sampling weights provided by the Centers for Disease Control. The data were weighted so that the summary statistics, standard errors, and test statistics took into account the sampling design and represented estimates in the total US. population. We used the procedures described by Levy and Lemeshow,13 and implemented them using STATA.14 These included simple chi-square tests, logistic regression with F- or t-approximations. The F- and t-approximations for the logistic regression were necessary to adjust for the complex survey design.13 Hierarchical (protected) testing procedures helped correct for multiple comparisons. We used omnibus tests for variables with multiple options (eg, marital status), and only considered follow-up tests when the overall test result was significant. Furthermore, a conservative threshold for significance (P < .01) was a compromise to the Bonferroni correction for multiple comparisons.
Results
Approximately 1 in 6 patients (16.1%; 95% confidence interval [CI], 15.4 - 16.8) reported that a physician or other health care worker had initiated a discussion about alcohol use. Table W1* compares patients who reported such a discussion with those who did not. Physicians talked to male patients about alcohol use most frequently. This corresponds to men reporting nearly 3 times more drinks consumed (12.9 drinks/month) than women (4.7 drinks/month; t = 16.26, df = 18,323, P < .001).
In general, physicians spoke about alcohol more often to younger people. There was a significant interaction, however, between sex and age, as shown in Figure 1. Discussions with women demonstrated a clear decrease in frequency with age; discussions with men decreased with age more slowly.
The amount of drinking in our sample, indexed by the number of drinks per month, is shown in Figure 2. Both the frequency of discussions and amount of alcohol consumed declined with advancing age. Women drank less alcohol than men overall and showed a moderate decline in use with age.
Nonwhite respondents reported more physician discussions about alcohol than did whites. However, white patients reported greater consumption (8.9 drinks/month) than nonwhites (6.8 drinks; t = 2.79, df = 18253, P < .005).
The lowest income group reported being advised about alcohol most frequently. Interestingly, the highest income respondents tended to drink more than those with less income. Marital status also predicted alcohol discussions. Physicians discussed alcohol more often with patients who were unmarried. While divorced patients reported discussions about alcohol use frequently, widowed patients reported them least often.
Discussions about alcohol occurred more often with respondents who had consumed alcohol within the month prior to the interview. Respondents who reported having these discussions also consumed more (14.6 drinks/month) than those who did not report a discussion (7.3 drinks/month, t = 7.20, df = 17985, P < .001). People who binge drank were more than twice as likely (OR = 2.25; 95% CI, 1.94 - 2.60) to report such a discussion (27.5%).
All of these predictors of a discussion about alcohol use were entered into a multivariate logistic regression. Backward elimination removed items that failed to provide independent information. The final model appears in the Table. Factors other than drinking behaviors that uniquely increased the chance of such a discussion about alcohol were being young, male, nonwhite, and of lower income.
More than 1 in 9 people (12.3%; n = 2768) in the sample met criteria for excessive drinking (ie, consuming 60 drinks per month or drinking 5 or more drinks on a single occasion in the last month). Within this group, 11.9% engaged in binge drinking and 3.5% consumed 60 drinks a month. Most were men (71.3%) with a mean age of 35 years, and they averaged 39.7 (95% CI, 36.74 - 42.74) drinks per month. They binged an average of 3.44 (95% CI, 3.18 - 3.70) times during the last month.
Slightly more than 1 in 4 excessive drinkers (28%; 95% CI, 25.41 - 30.69) reported a discussion about alcohol with a physician. While none of the demographic factors met our stringent criteria for significance (P < .01), many would have met the more usual threshold of P < .05. For example, among the respondents with excessive alcohol use, 23.9% of the women had been screened by their physicians compared with 29.9% of the men (P < .013). This suggests that these women may receive less preventive discussions and screening than they require. While the percent of nonwhite respondents who drank excessively and were successfully screened was above the mean rate overall (35.6%), the percent of white patients was lower than the mean (26.4%; P < .012). Compared with married patients, excessive drinkers who were divorced (35.2%; P < .019) or separated (38.1%; P < .091) reported a higher frequency of screening. Widowed patients with excessive alcohol use rarely reported screening (13%; P < .032).
TABLE
FINAL LOGISTIC REGRESSION PREDICTING A DISCUSSION ABOUT ALCOHOL
| Predictor | Beta | OR(95% CI) |
|---|---|---|
| Sex | -0.48 | 0.62 (0.44 - 0.87)* |
| Age | -0.028 | 0.97 (0.97 - 0.98)† |
| Age, by sex interaction | 0.02 | 1.02 (1.01 - 1.03)† |
| Did not drink ‡ | -0.57 | 0.57 (0.44 - 0.73)† |
| Drinks per month § | 0.28 | 1.33 (1.24 - 1.43)† |
| Income | -0.08 | 0.93 (0.90 - 0.96)† |
| Race ¶ | 0.34 | 1.41 (1.22 - 1.63)† |
| Constant | -0.24 | |
| OR denotes odds ratio from univariate logistic regression; CI, confidence interval. | ||
| *P< .01 | ||
| †P< .001 | ||
| Respondent reported not drinking any alcohol in the last month. | ||
| § Log transform of the number of drinks per month. | ||
| ¶ Race coded as white versus nonwhite. | ||
FIGURE 1
LOGISTIC REGRESSION PREDICTING THE OCCURRENCE OF PHYSICIAN DISCUSSION ABOUT ALCOHOL FROM THE PATIENTS’ AGE AND SEX (WOMEN =o MEN =●).
FIGURE 2
MEAN NUMBERS OF ALCOHOLIC DRINKS CONSUMED BY AGE AND SEX (WOMEN = o MEN = ● ).
Other preventive services
We also assessed the rate of talks about healthy eating as a comparison for the alcohol discussions. A total of 44.6% of patients reported having a conversation about healthy eating compared with 16.1% having an alcohol discussion. On the chance that people who drank excessively might differentially remember conversations with their physicians, we assessed the association between alcohol use and reports of experiencing counseling on healthy eating. No significant associations were found between reported conversations about eating and any variable related to alcohol consumption even after controlling for sex, age, sex-by-age interaction, race, income, and education. Similar results were obtained for discussions about exercise, AIDS, and illegal drugs. Discussions about illegal drug use occurred less frequently than discussions about alcohol use (12.5%). Discussions about AIDS were reported by 26.1% of the respondents, exercise-related conversations were reported 47.4% of the time, and smoking was mentioned by 49.2% of the respondents. Considering any preventive health discussions (smoking, drinking, drug abuse, exercise, healthy eating, or AIDS), 97.4% of the respondents reported a discussion of at least 1 topic.
Discussion
Physicians currently incorporate preventive counseling about behavioral health risks as part of standard clinical care. In a recent survey of general practitioners, 97% of those surveyed thought that members of their profession should inquire about drinking behaviors.15 Moreover, brief office visit screening followed by physician advice has been documented as effective in reducing alcohol consumption.16,17 Despite the general positive opinion of alcohol screening, however, discussions about AIDS and other health-related behaviors were discussed much more frequently than alcohol-related behaviors.
Our analysis identified patients who consume a significant amount of alcohol, yet did not report being screened or counseled by their physicians. We gathered information about the magnitude of use, as well as about the presence or absence of a discussion regarding alcohol. This allowed us to examine 2 important aspects of alcohol screening: (1) the demographic features that predicted it, and (2) whether these demographic features represented patients who actually consumed large amounts of alcohol and could therefore benefit from counseling.
Although the BRFSS did not assess alcohol dependence or abuse directly, the goal of the study was to designate which patients might be appropriate candidates for screening or preventive counseling. Assessments of alcohol abuse or dependence using strict Diagnostic and Statistical Manual of Mental Disorders – 4th Edition (DSM-IV) criteria require insight, as well as a willingness to share this information with the interviewer. Kosten and Rounsaville18 found that DSM-based diagnostic interviews for alcoholism and substance abuse showed the lowest sensitivity relative to other psychiatric diagnoses. Therefore, more recent surveys of alcohol abuse assess the quantity of consumption before applying strict DSM-IV criteria.19,20 Although participants may also minimize actual consumption, the screening for quantity requires less insight than a formal diagnosis and may more effectively identify candidates for counseling. However, our findings suggest that physicians do not routinely attempt to ascertain alcohol use quantitatively.21,22 Implementing alcohol screening as a routine preventive health care practice would allow physicians to detect problems without relying on insightful spontaneous reporting from patients.
The most successful strategy to identify more candidates for treatment involves simply screening a larger number of patients, especially high-risk patients. Our data suggest that physicians do target discussions somewhat toward people who report excessive alcohol consumption. Approximately 16% of the general patient population reported such a discussion, but this rate was greater (27.8%) among heavy or binge drinkers. Unfortunately, these data also suggest that the majority of patients who might benefit from such counseling, did not report a discussion about alcohol use. Individuals who are likely to be appropriate candidates but who were not counseled include white patients and women (widows, in particular).
The frequency of discussions about alcohol for women and widows who drank excessively was low. This finding is consistent with current research demonstrating that alcohol problems among women, and widowed women in particular, are under-recognized. Physiologically, the lower body water volume in women, especially in elderly women, increases the detrimental effects of alcohol.23 Physicians also appear to have more difficulty recognizing alcohol problems among the elderly.24 Alcohol-related symptoms among elderly women may be misinterpreted as caused by depression, anxiety, or other psychiatric problems.25 Elderly women taking psychoactive medications or medications with sedative effects may be even more difficult to assess. Moreover, our analysis categorized excessive drinking using a single criterion for all respondents. Evidence is mounting that indicates that women26 and the elderly23 are more at risk from lower levels of drinking. Had we lowered our criterion for these patients, the magnitude of problem drinking would have appeared even greater.
Limitations
There are several limitations to our study. A number of reasons, including forgetfulness or inattention, may account for under-reporting. An overall problem with memory is unlikely, since almost all respondents remembered at least one discussion about some kind of health risk. Nonetheless, patients may be selectively less likely to recall a discussion about alcohol because of emotional associations with the topic. However, it is unclear why memory would be less reliable about alcohol use than memory about another potentially emotionally-charged topic, such as AIDS.
Additionally, our information was self-reported through a telephone interview. There have been positive study results published that validate the BRFSS survey data on alcohol consumption.27,28 Nevertheless, the potential remains that respondents underestimate their alcohol use, and this might lead to false-negatives. Furthermore, the nature of the BRFSS question for alcohol discussions is somewhat ambiguous since we do not know if the discussion was a screening for excessive drinking or simply educational counseling.
Conclusions
Ideally, alcohol screening should occur in all primary care office visits, but given the extreme time constraints in the clinic setting, identification of under-recognized groups for targeted screening may enhance the recognition of alcohol abuse in a most time-effective manner.
BACKGROUND: This study assessed which demographic groups were most likely to consume alcohol excessively, and which groups had received inquiries and discussion about alcohol use from their physicians compared with discussions about other health risks.
STUDY DESIGN: This was a cross-sectional study using data from the Centers for Disease Control Behavioral Risk Factors Surveillance System 1997 data set that represents a stratified random sample in the United States.
POPULATION: We selected 23,349 adults who reported a routine physical examination within the last 3 years.
OUTCOMES MEASURED: The main variables involved responses to questions about alcohol intake and whether the respondent’s physician had initiated discussions about drinking.
RESULTS: Physicians spoke to patients about alcohol use much less frequently than about other health-related behaviors. Discussions were roughly targeted to groups with the largest intake. However, physicians were least likely to speak with white patients, women, and widows who drank significantly.
CONCLUSIONS: Regularly asking patients about alcohol use could substantially reduce the under-recognition of alcoholism. Since brief counseling is effective, negative consequences of excessive alcohol intake may be avoided.
- Alcohol screening occurs less frequently than screening about other health-related behaviors.
- There were no demographic groups in which the prevalence of excessive drinking was so low that general screening was not appropriate.
- Physicians frequently miss the opportunity to discuss alcohol use with patients in certain groups, such as white patients and women (widows, in particular).
Physicians and related health care workers are well positioned to detect possible alcohol-related problems during routine patient visits, provided the appropriate screening procedures are implemented.2-4 Ideally, the primary care clinician should be the most prominent source of alcohol abuse screening and referrals, rather than the provider of treatment after an alcohol-related incident.
Although screening for alcoholism adds another step to an already over-worked health care system, it can result in substantial benefits by reducing the burden of overall health care costs. According to recent information, alcohol abuse costs our society $184.6 billion.5 In 1997, an estimated 1.3 million hospital discharges reported an alcohol-related diagnosis.6 And an estimated 12,870 alcohol-related traffic fatalities accounted for nearly one third of all traffic deaths in that same year.7 Even when individuals reamin socially functional and do not meet the formal criteria for an alcohol-related disorder, excessive use of alcohol is associated with a variety of medical problems. Although cardioprotective effects have been reported with moderate use (ie, 1 to 2 drinks per day), the list of medical complications associated with longstanding alcoholism (hypertension, cardiomyopathy, cirrhosis, erosive gastris, pancreatitis, and esophageal varices, for example) account for considerable morbidity and mortality.8,9 Increased alcohol consumption over a 1-year period is also associated with accidents and injuries necessitating emergency services.10
Because the primary care physician is in a unique position to influence the preventive care of the community they serve, our study examined alcohol screening in the primary care setting. The following 2 questions were asked: (1) Which patients were assessed for excessive alcohol use, and what patient characteristics predicted the assessment? and (2) How often did discussions about alcohol occur compared with other health risk discussions (eg, eating habits or smoking)?
Methods
Subjects
This is a secondary analysis of data from an epidemiologic telephone interview conducted by the Behavioral Risk Factors Surveillance System (BRFSS)1 involving a random stratified sample of people living within the United States. In the 1997 interviews, all state interviews included questions about alcohol consumption. Alaska, Colorado, Idaho, Louisiana, Missouri, New York, North Carolina, Oklahoma, Pennsylvania, Virginia, and Wyoming included a counseling module that asked, “Has a doctor or other health professional ever talked with you about alcohol use?”
The 1997 BRFSS data set represents 135,582 interviews. The sample reported here includes only respondents who reported a routine physical examination within the last 3 years and who were asked questions from the counseling module (n = 23,349), as well as questions about other health habits. There were 9106 men (mean age = 45.82 years; SD = 16.86) and 14,203 women (mean age = 46.90; SD = 17.44) who responded.
Excessive drinking was defined as consuming 60 alcoholic beverages per month or 5 on a single occasion (binge drinking) in the month prior to the interview (n = 2772). The 60 beverages per month threshold follows recommendations by the National Institute for Alcohol Abuse and Alcoholism and the US Department of Health and Human Services’ Dietary Guidelines for Americans.11,12
Statistical analysis
Analysis used the sampling weights provided by the Centers for Disease Control. The data were weighted so that the summary statistics, standard errors, and test statistics took into account the sampling design and represented estimates in the total US. population. We used the procedures described by Levy and Lemeshow,13 and implemented them using STATA.14 These included simple chi-square tests, logistic regression with F- or t-approximations. The F- and t-approximations for the logistic regression were necessary to adjust for the complex survey design.13 Hierarchical (protected) testing procedures helped correct for multiple comparisons. We used omnibus tests for variables with multiple options (eg, marital status), and only considered follow-up tests when the overall test result was significant. Furthermore, a conservative threshold for significance (P < .01) was a compromise to the Bonferroni correction for multiple comparisons.
Results
Approximately 1 in 6 patients (16.1%; 95% confidence interval [CI], 15.4 - 16.8) reported that a physician or other health care worker had initiated a discussion about alcohol use. Table W1* compares patients who reported such a discussion with those who did not. Physicians talked to male patients about alcohol use most frequently. This corresponds to men reporting nearly 3 times more drinks consumed (12.9 drinks/month) than women (4.7 drinks/month; t = 16.26, df = 18,323, P < .001).
In general, physicians spoke about alcohol more often to younger people. There was a significant interaction, however, between sex and age, as shown in Figure 1. Discussions with women demonstrated a clear decrease in frequency with age; discussions with men decreased with age more slowly.
The amount of drinking in our sample, indexed by the number of drinks per month, is shown in Figure 2. Both the frequency of discussions and amount of alcohol consumed declined with advancing age. Women drank less alcohol than men overall and showed a moderate decline in use with age.
Nonwhite respondents reported more physician discussions about alcohol than did whites. However, white patients reported greater consumption (8.9 drinks/month) than nonwhites (6.8 drinks; t = 2.79, df = 18253, P < .005).
The lowest income group reported being advised about alcohol most frequently. Interestingly, the highest income respondents tended to drink more than those with less income. Marital status also predicted alcohol discussions. Physicians discussed alcohol more often with patients who were unmarried. While divorced patients reported discussions about alcohol use frequently, widowed patients reported them least often.
Discussions about alcohol occurred more often with respondents who had consumed alcohol within the month prior to the interview. Respondents who reported having these discussions also consumed more (14.6 drinks/month) than those who did not report a discussion (7.3 drinks/month, t = 7.20, df = 17985, P < .001). People who binge drank were more than twice as likely (OR = 2.25; 95% CI, 1.94 - 2.60) to report such a discussion (27.5%).
All of these predictors of a discussion about alcohol use were entered into a multivariate logistic regression. Backward elimination removed items that failed to provide independent information. The final model appears in the Table. Factors other than drinking behaviors that uniquely increased the chance of such a discussion about alcohol were being young, male, nonwhite, and of lower income.
More than 1 in 9 people (12.3%; n = 2768) in the sample met criteria for excessive drinking (ie, consuming 60 drinks per month or drinking 5 or more drinks on a single occasion in the last month). Within this group, 11.9% engaged in binge drinking and 3.5% consumed 60 drinks a month. Most were men (71.3%) with a mean age of 35 years, and they averaged 39.7 (95% CI, 36.74 - 42.74) drinks per month. They binged an average of 3.44 (95% CI, 3.18 - 3.70) times during the last month.
Slightly more than 1 in 4 excessive drinkers (28%; 95% CI, 25.41 - 30.69) reported a discussion about alcohol with a physician. While none of the demographic factors met our stringent criteria for significance (P < .01), many would have met the more usual threshold of P < .05. For example, among the respondents with excessive alcohol use, 23.9% of the women had been screened by their physicians compared with 29.9% of the men (P < .013). This suggests that these women may receive less preventive discussions and screening than they require. While the percent of nonwhite respondents who drank excessively and were successfully screened was above the mean rate overall (35.6%), the percent of white patients was lower than the mean (26.4%; P < .012). Compared with married patients, excessive drinkers who were divorced (35.2%; P < .019) or separated (38.1%; P < .091) reported a higher frequency of screening. Widowed patients with excessive alcohol use rarely reported screening (13%; P < .032).
TABLE
FINAL LOGISTIC REGRESSION PREDICTING A DISCUSSION ABOUT ALCOHOL
| Predictor | Beta | OR(95% CI) |
|---|---|---|
| Sex | -0.48 | 0.62 (0.44 - 0.87)* |
| Age | -0.028 | 0.97 (0.97 - 0.98)† |
| Age, by sex interaction | 0.02 | 1.02 (1.01 - 1.03)† |
| Did not drink ‡ | -0.57 | 0.57 (0.44 - 0.73)† |
| Drinks per month § | 0.28 | 1.33 (1.24 - 1.43)† |
| Income | -0.08 | 0.93 (0.90 - 0.96)† |
| Race ¶ | 0.34 | 1.41 (1.22 - 1.63)† |
| Constant | -0.24 | |
| OR denotes odds ratio from univariate logistic regression; CI, confidence interval. | ||
| *P< .01 | ||
| †P< .001 | ||
| Respondent reported not drinking any alcohol in the last month. | ||
| § Log transform of the number of drinks per month. | ||
| ¶ Race coded as white versus nonwhite. | ||
FIGURE 1
LOGISTIC REGRESSION PREDICTING THE OCCURRENCE OF PHYSICIAN DISCUSSION ABOUT ALCOHOL FROM THE PATIENTS’ AGE AND SEX (WOMEN =o MEN =●).
FIGURE 2
MEAN NUMBERS OF ALCOHOLIC DRINKS CONSUMED BY AGE AND SEX (WOMEN = o MEN = ● ).
Other preventive services
We also assessed the rate of talks about healthy eating as a comparison for the alcohol discussions. A total of 44.6% of patients reported having a conversation about healthy eating compared with 16.1% having an alcohol discussion. On the chance that people who drank excessively might differentially remember conversations with their physicians, we assessed the association between alcohol use and reports of experiencing counseling on healthy eating. No significant associations were found between reported conversations about eating and any variable related to alcohol consumption even after controlling for sex, age, sex-by-age interaction, race, income, and education. Similar results were obtained for discussions about exercise, AIDS, and illegal drugs. Discussions about illegal drug use occurred less frequently than discussions about alcohol use (12.5%). Discussions about AIDS were reported by 26.1% of the respondents, exercise-related conversations were reported 47.4% of the time, and smoking was mentioned by 49.2% of the respondents. Considering any preventive health discussions (smoking, drinking, drug abuse, exercise, healthy eating, or AIDS), 97.4% of the respondents reported a discussion of at least 1 topic.
Discussion
Physicians currently incorporate preventive counseling about behavioral health risks as part of standard clinical care. In a recent survey of general practitioners, 97% of those surveyed thought that members of their profession should inquire about drinking behaviors.15 Moreover, brief office visit screening followed by physician advice has been documented as effective in reducing alcohol consumption.16,17 Despite the general positive opinion of alcohol screening, however, discussions about AIDS and other health-related behaviors were discussed much more frequently than alcohol-related behaviors.
Our analysis identified patients who consume a significant amount of alcohol, yet did not report being screened or counseled by their physicians. We gathered information about the magnitude of use, as well as about the presence or absence of a discussion regarding alcohol. This allowed us to examine 2 important aspects of alcohol screening: (1) the demographic features that predicted it, and (2) whether these demographic features represented patients who actually consumed large amounts of alcohol and could therefore benefit from counseling.
Although the BRFSS did not assess alcohol dependence or abuse directly, the goal of the study was to designate which patients might be appropriate candidates for screening or preventive counseling. Assessments of alcohol abuse or dependence using strict Diagnostic and Statistical Manual of Mental Disorders – 4th Edition (DSM-IV) criteria require insight, as well as a willingness to share this information with the interviewer. Kosten and Rounsaville18 found that DSM-based diagnostic interviews for alcoholism and substance abuse showed the lowest sensitivity relative to other psychiatric diagnoses. Therefore, more recent surveys of alcohol abuse assess the quantity of consumption before applying strict DSM-IV criteria.19,20 Although participants may also minimize actual consumption, the screening for quantity requires less insight than a formal diagnosis and may more effectively identify candidates for counseling. However, our findings suggest that physicians do not routinely attempt to ascertain alcohol use quantitatively.21,22 Implementing alcohol screening as a routine preventive health care practice would allow physicians to detect problems without relying on insightful spontaneous reporting from patients.
The most successful strategy to identify more candidates for treatment involves simply screening a larger number of patients, especially high-risk patients. Our data suggest that physicians do target discussions somewhat toward people who report excessive alcohol consumption. Approximately 16% of the general patient population reported such a discussion, but this rate was greater (27.8%) among heavy or binge drinkers. Unfortunately, these data also suggest that the majority of patients who might benefit from such counseling, did not report a discussion about alcohol use. Individuals who are likely to be appropriate candidates but who were not counseled include white patients and women (widows, in particular).
The frequency of discussions about alcohol for women and widows who drank excessively was low. This finding is consistent with current research demonstrating that alcohol problems among women, and widowed women in particular, are under-recognized. Physiologically, the lower body water volume in women, especially in elderly women, increases the detrimental effects of alcohol.23 Physicians also appear to have more difficulty recognizing alcohol problems among the elderly.24 Alcohol-related symptoms among elderly women may be misinterpreted as caused by depression, anxiety, or other psychiatric problems.25 Elderly women taking psychoactive medications or medications with sedative effects may be even more difficult to assess. Moreover, our analysis categorized excessive drinking using a single criterion for all respondents. Evidence is mounting that indicates that women26 and the elderly23 are more at risk from lower levels of drinking. Had we lowered our criterion for these patients, the magnitude of problem drinking would have appeared even greater.
Limitations
There are several limitations to our study. A number of reasons, including forgetfulness or inattention, may account for under-reporting. An overall problem with memory is unlikely, since almost all respondents remembered at least one discussion about some kind of health risk. Nonetheless, patients may be selectively less likely to recall a discussion about alcohol because of emotional associations with the topic. However, it is unclear why memory would be less reliable about alcohol use than memory about another potentially emotionally-charged topic, such as AIDS.
Additionally, our information was self-reported through a telephone interview. There have been positive study results published that validate the BRFSS survey data on alcohol consumption.27,28 Nevertheless, the potential remains that respondents underestimate their alcohol use, and this might lead to false-negatives. Furthermore, the nature of the BRFSS question for alcohol discussions is somewhat ambiguous since we do not know if the discussion was a screening for excessive drinking or simply educational counseling.
Conclusions
Ideally, alcohol screening should occur in all primary care office visits, but given the extreme time constraints in the clinic setting, identification of under-recognized groups for targeted screening may enhance the recognition of alcohol abuse in a most time-effective manner.
1. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Atlanta: National Center for Chronic Disease Prevention and Health Promotion, US Department of Health and Human Services, 1997.
2. The National Center on Addiction and Substance Abuse at Columbia University. Missed Opportunity: National Survey of Primary Care Physicians and Patients on Substance Abuse. New York: The National Center on Addiction and Substance Abuse at Columbia University, 2000.
3. Leshner AI. Science-based views of drug addiction and its treatment. JAMA 1999;282:1314-16.
4. Weisner C, Schmidt LA. Expanding the frame of health services research in the drug abuse field. Health Serv Res 1995;30:707-26.
5. Department of Health and Human Services, National Institutes of Health. Disease-Specific Estimates of Direct and Indirect Costs of Illness and NIH Support: Fiscal Year 2000 Update. Washington, DC: Department of Health and Human Services, National Institutes of Health, 2000.
6. Whitmore CC, Stinson FS, Dufour MC. Surveillance Report #50. Trends in Alcohol-Related Morbidity Among Short-Stay Community Hospital Discharges, United States, 1979-97. Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1999.
7. National Institute of Alcohol Abuse and Alcoholism. Traffic crashes, traffic crash fatalities, and alcohol-related traffic crash fatalities, United States, 1977-97. Washington, DC: National Institute of Alcohol Abuse and Alcoholism, 1999.
8. Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly US adults. New Eng J Med 1997;337:1705-14.
9. Gorelick PB, Erkinjuntti T, Hofman A, Rocca WA, Skoog I, Winblad B. Prevention of vascular dementia. Alzheimer Dis Assoc Disord 1999;3:S131-39
10. Borges G, Cherpitel CJ, Medina-Mora ME, Mondragon L, Casanova L. Alcohol consumption in emergency room patients and the general population: a population based study. Alcohol Clin Exp Res 1998;22:1986-91.
11. National Institute on Alcohol Abuse and Alcoholism. Physicians’ guide to helping patients with alcohol problems. Washington, DC: US Department of Health and Human Services, 1995.
12. US Department of Health and Human Services. Nutrition and your health: dietary guidelines for Americans. 3rd edition. Washington, DC: Supt of Docs, US Govt Print Office, 1990.
13. Levy PS, Lemeshow S. Sampling of populations. New York: John Wiley & Sons, 1999.
14. Stata Corporation. Stata 6.0. College Station, TX: Stata Corporation, 2000.
15. Herbert C, Bass F. Early at-risk alcohol intake. Definitions and physicians’ role in modifying behavior. Can Fam Phys 1997;43:639-44.
16. Fleming MG, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice from problem alcohol drinkers. J Am Med Assoc 1997;277:1039-45.
17. Wallace P, Cutler S, Haines A. Randomized controlled trial of general practitioner intervention in patients with excessive alcohol consumption. Br Med J 1988;297:663-68.
18. Kosten TA, Rounsaville BJ. Sensitivity of psychiatric diagnosis based on the best estimate procedure. Am J Psych 1992;149:1225-27.
19. First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV axis I disorders—clinician version. New York: Biometrics Research Department, New York State Psychiatric Institute, 1997.
20. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Study. Arch Gen Psych 1994;51:8-19.
21. Brown RL, Leonard T, Saunders LA, Papasouliotis O. A 2-item conjoint screen for alcohol and other drug problems. J Am Board Fam Pract 2001;14:95-106.
22. Hays RD, Ellickson PL. Comparison of the Rost and the CAGE alcohol screening instruments in young adults. Subst Use Misuse 2001;36:639-51.
23. National Institute on Alcohol Abuse and Alcoholism. Alcohol alert #40: alcohol and aging. Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1998.
24. Curtis JR, Geller G, Stokes EJ, Levine DM, Moore RD. Characteristics, diagnosis, and treatment of alcoholism in elderly patients. J Am Geriatrics Soc 1989;37:310-16.
25. The National Center on Addiction and Substance Abuse at Columbia University. Under the rug: substance abuse and the mature woman. New York: The National Center on Addiction and Substance Abuse at Columbia University, 1998.
26. National Institute on Alcohol Abuse and Alcoholism. Alcohol alert #46: are women more vulnerable to alcohol’s effects? Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1999.
27. Smith PF, Remington PL, Williamson DF, Anda RF. A comparison of alcohol sales data with survey data on self-reported alcohol use in 21 states. Am J Public Health 1990;0:309-12.
28. Anda RF, Williamson DF, Dodson D, Remington PL. Telephone versus in-person reporting of smoking and alcohol use: a comparison of 2 statewide surveys. Am J Health Promotion 1989;4:32-36.
1. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Atlanta: National Center for Chronic Disease Prevention and Health Promotion, US Department of Health and Human Services, 1997.
2. The National Center on Addiction and Substance Abuse at Columbia University. Missed Opportunity: National Survey of Primary Care Physicians and Patients on Substance Abuse. New York: The National Center on Addiction and Substance Abuse at Columbia University, 2000.
3. Leshner AI. Science-based views of drug addiction and its treatment. JAMA 1999;282:1314-16.
4. Weisner C, Schmidt LA. Expanding the frame of health services research in the drug abuse field. Health Serv Res 1995;30:707-26.
5. Department of Health and Human Services, National Institutes of Health. Disease-Specific Estimates of Direct and Indirect Costs of Illness and NIH Support: Fiscal Year 2000 Update. Washington, DC: Department of Health and Human Services, National Institutes of Health, 2000.
6. Whitmore CC, Stinson FS, Dufour MC. Surveillance Report #50. Trends in Alcohol-Related Morbidity Among Short-Stay Community Hospital Discharges, United States, 1979-97. Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1999.
7. National Institute of Alcohol Abuse and Alcoholism. Traffic crashes, traffic crash fatalities, and alcohol-related traffic crash fatalities, United States, 1977-97. Washington, DC: National Institute of Alcohol Abuse and Alcoholism, 1999.
8. Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly US adults. New Eng J Med 1997;337:1705-14.
9. Gorelick PB, Erkinjuntti T, Hofman A, Rocca WA, Skoog I, Winblad B. Prevention of vascular dementia. Alzheimer Dis Assoc Disord 1999;3:S131-39
10. Borges G, Cherpitel CJ, Medina-Mora ME, Mondragon L, Casanova L. Alcohol consumption in emergency room patients and the general population: a population based study. Alcohol Clin Exp Res 1998;22:1986-91.
11. National Institute on Alcohol Abuse and Alcoholism. Physicians’ guide to helping patients with alcohol problems. Washington, DC: US Department of Health and Human Services, 1995.
12. US Department of Health and Human Services. Nutrition and your health: dietary guidelines for Americans. 3rd edition. Washington, DC: Supt of Docs, US Govt Print Office, 1990.
13. Levy PS, Lemeshow S. Sampling of populations. New York: John Wiley & Sons, 1999.
14. Stata Corporation. Stata 6.0. College Station, TX: Stata Corporation, 2000.
15. Herbert C, Bass F. Early at-risk alcohol intake. Definitions and physicians’ role in modifying behavior. Can Fam Phys 1997;43:639-44.
16. Fleming MG, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice from problem alcohol drinkers. J Am Med Assoc 1997;277:1039-45.
17. Wallace P, Cutler S, Haines A. Randomized controlled trial of general practitioner intervention in patients with excessive alcohol consumption. Br Med J 1988;297:663-68.
18. Kosten TA, Rounsaville BJ. Sensitivity of psychiatric diagnosis based on the best estimate procedure. Am J Psych 1992;149:1225-27.
19. First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV axis I disorders—clinician version. New York: Biometrics Research Department, New York State Psychiatric Institute, 1997.
20. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Study. Arch Gen Psych 1994;51:8-19.
21. Brown RL, Leonard T, Saunders LA, Papasouliotis O. A 2-item conjoint screen for alcohol and other drug problems. J Am Board Fam Pract 2001;14:95-106.
22. Hays RD, Ellickson PL. Comparison of the Rost and the CAGE alcohol screening instruments in young adults. Subst Use Misuse 2001;36:639-51.
23. National Institute on Alcohol Abuse and Alcoholism. Alcohol alert #40: alcohol and aging. Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1998.
24. Curtis JR, Geller G, Stokes EJ, Levine DM, Moore RD. Characteristics, diagnosis, and treatment of alcoholism in elderly patients. J Am Geriatrics Soc 1989;37:310-16.
25. The National Center on Addiction and Substance Abuse at Columbia University. Under the rug: substance abuse and the mature woman. New York: The National Center on Addiction and Substance Abuse at Columbia University, 1998.
26. National Institute on Alcohol Abuse and Alcoholism. Alcohol alert #46: are women more vulnerable to alcohol’s effects? Washington, DC: National Institute on Alcohol Abuse and Alcoholism, 1999.
27. Smith PF, Remington PL, Williamson DF, Anda RF. A comparison of alcohol sales data with survey data on self-reported alcohol use in 21 states. Am J Public Health 1990;0:309-12.
28. Anda RF, Williamson DF, Dodson D, Remington PL. Telephone versus in-person reporting of smoking and alcohol use: a comparison of 2 statewide surveys. Am J Health Promotion 1989;4:32-36.