User login
An incidental finding
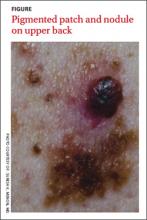
A 37-year-old Caucasian man sought care at our clinic for the pruritic patches on his trunk and extremities that had developed 3 days earlier. The patient said that the lesions started on his right arm but had spread to his left arm, posterior legs, and trunk. He reported that the trunk lesions had resolved, but the extremity lesions persisted. He’d had no specific contact exposures.
Upon further questioning, the patient indicated that he had noted the pigmented patch for at least 4 years, but was not sure how long the nodular area had been there. He thought it was a birthmark. He grew up spending a lot of time at the beach in the sun and recalled at least one blistering sunburn on his back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Melanoma
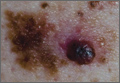
The patient underwent elliptical excisional biopsy of the primary lesion after no palpable lymphadenopathy was noted. The lateral and deep margins were negative for melanoma; the mitotic rate was <1/mm2. Aggregates of lymphocytes were associated with the lesion, but did not infiltrate it. There was no tumor regression or ulceration of the lesion. The Breslow depth was 1.25 mm.
A histopathologic evaluation revealed a superficial spreading melanoma (inferior lesion in the FIGURE) and a nodular lesion (the superior reddish-black lesion in the FIGURE). (For more on these and other forms of melanoma, see “The 4 main types of melanoma”1-4 see below.) It was unclear from the patient’s history whether this represented 2 types of melanoma (superficial spreading and nodular) in the same field of skin or the development of a nodular component in a superficial spreading lesion. Important clinical information was also missing, including the evolution of the lesions and how quickly the nodule had grown.
Who’s affected most? More than 45,000 cases of melanoma occurred in 45 states and the District of Columbia annually between 2004 and 2006, according to a 2011 report from the Centers for Disease Control and Prevention.5 White, non-Hispanics have a far higher incidence of melanoma than any other race or ethnicity.6 Women are more likely than men to be diagnosed with melanoma early in life, while men are twice as likely as women to be diagnosed after age 60.6 The etiology for the malignant transformation of melanocytes has not been fully clarified, but it is likely multifactorial, including genetic susceptibility and ultraviolet (UV) radiation damage.4
The ABCDE mnemonic is widely taught to aid in the detection of melanomas: A = asymmetry of the lesion; B = border irregularities; C = color variegation; D = diameter >6 mm; and E = evolution. The evolution of the lesion has been shown in some studies to be the most specific finding for detecting melanomas.4
Regional lymph nodes should also be carefully examined for evidence of clinical spread prior to biopsy of a suspicious lesion. This is important because biopsy may cause regional lymphadenopathy, which could confound later examinations and staging of the disease.1
The differential: Is it a worrisome lesion—or not?
The differential diagnosis of melanoma includes both benign and malignant lesions. Malignant and potentially malignant diagnoses to consider include pigmented basal cell carcinoma, pigmented squamous cell carcinoma, carcinoma metastatic to the skin, and dysplastic nevi.2,3
Benign diagnoses to consider include pigmented seborrheic keratoses, lentigo, pyogenic granuloma, Kaposi sarcoma, cherry angioma, subungual traumatic hematoma, dermatofibroma, and nevi (including blue nevi).2,3
The biopsy is paramount
A diagnosis is established based on the microscopic evaluation of suspicious lesions. Studies suggest that one-third to one-half of melanomas arise from existing nevi, with the remainder developing from previously normal-appearing skin.1,2 Patients with increased numbers of either common or dysplastic nevi are at increased risk of melanoma compared with the general population.4 Historical clues include changes in a lesion’s size, color, or symmetry; new growths; personal or family history of melanoma; and bleeding.
A biopsy for histopathologic evaluation is mandatory when a lesion is suspicious for melanoma. Dermoscopy, which involves a device that magnifies skin lesions, may reveal highly specific dermoscopic features for melanoma that can help in determining the need for biopsy.4
The preferred method for biopsy is complete elliptical excision with 2- to 3-mm margins of normal skin.2,3 However, a deep shave biopsy may also be appropriate, depending upon the clinical situation and physician experience with the technique.4
A deep shave biopsy is less time consuming than elliptical excision, making it easier to perform at the time the lesion is first evaluated. Deep shave biopsy may provide several benefits, including reducing the amount of normal tissue that is removed (especially if pathology is benign) as well as, the cost, scarring, and likelihood of wound infections. Deep shave biopsy also can avoid the need for a second elliptical excision.7,8
Determine margins, proceed with surgical excision
Early surgical excision is the primary treatment for malignant melanoma. After the diagnosis is confirmed by initial biopsy, the depth of the lesion dictates the surgical recommendations. Recommended surgical margins based on depth are: 5 mm with a layer of subcutaneous fat for melanoma in situ, 1 cm down to the fascia for lesions with a Breslow depth ≤2 mm, and 2 cm down to the fascia for lesions with a depth >2 mm.1,4
The surgical treatment of lentigo maligna melanoma can be challenging due to indistinct borders and large size. Mohs micrographic surgery can be helpful to fully remove the lesion with sparing of healthy surrounding tissue.4 When surgical excision of large lentigo maligna is technically difficult, radiation therapy is another option.3
Subungual melanoma may necessitate amputation or grafting of the digit. Mohs micrographic surgery can be useful in these situations for tissue sparing.2 (To learn more, see “When to consider Mohs surgery,” J Fam Pract. 2013;558-564.)
Is a sentinel lymph node biopsy needed?
Sentinel lymph node biopsy is often recommended for melanomas >1 mm in depth.2-4 It provides guidance on who may benefit from regional lymphadenectomy and adjuvant immunotherapy.1,3
Adjuvant therapy for patients without evidence of distant metastases can be considered in patients with positive nodes or node-negative melanoma that is 4 mm thick or Clark Level IV or V. Adjuvant high-dose interferon alpha-2b is the most commonly used agent in these situations.2 Some studies suggest an increase in median overall survival of up to 11 months with high-dose interferon as compared to no treatment.3 Limitations include toxicity from these high-dose regimens.3 Treatment with interferon does not represent a cure; rather, it should be considered a palliative intervention with marginal benefit.1
When there are distant metastases…
Once distant metastases are identified, the goal of therapy should be palliative care as this condition is generally incurable. Chemotherapy, radiation, and excision of solitary metastases are all interventions that have traditionally been employed.1 The primary site for metastasis is the skin, but all organs are potential sites of spread. Central nervous system metastasis is the most common cause of the death.2
Novel therapies include inhibition of BRAF, an enzyme of the mitogen-activated protein kinase pathway (MAPK), and blocking of cytotoxic T lymphocyte-associated antigen-4 (CTLA-4).
BRAF-enzyme inhibitor. Mutated BRAF contributes to uncontrolled cell growth and resistance to programmed cell death (apoptosis).9,10 In August 2011, vemurafenib (Zelboraf ), a BRAF-enzyme inhibitor, was approved by the US Food and Drug Administration (FDA) for the treatment of late-stage melanoma. It works only in patients with the BRAFV600E mutation, which is found in approximately 60% of melanomas.11,12 One phase 1 study showed partial to complete regression in 80% of patients treated, but this regression lasted only 2 to 18 months.13
Anti-CTLA-4 monoclonal antibody. Cytotoxic T-lymphocytes can recognize and potentially destroy cancer cells.14 However, CTLA-4, which is expressed on the surface of cytotoxic T-lymphocytes, has a suppressive effect on the T-lymphocyte response after interaction with the antigen-presenting cell. Researchers deduced that blocking CTLA-4 would allow the immune system to remain responsive to abnormal antigens, including those from melanoma.9
Ipilimumab (Yervoy), an anti-CTLA-4 monoclonal antibody, was approved by the FDA in March 2011 for the treatment of late-stage melanoma.11 Partial and complete responses have been shown in trials of ipilimumab as monotherapy and in combination with vaccines, chemotherapy, and interleukin-2, but these responses have not been sustained.9
Although these novel therapies represent significant advancements in the understanding of the pathogenesis of melanoma, the short duration of efficacy highlights the cancer’s ability to develop resistance to these treatments. This ability to adapt suggests that melanoma harbors multiple oncogenes and several pathways for carcinogenesis. Combination targeted therapies may be required to improve clinical results; research is ongoing.9 Toxicities associated with these medications are also a limiting factor.
What about vaccines? Vaccine studies are also ongoing. Although some have shown promising results, no clearly effective therapy has been produced to date.2
Factors that affect prognosis
The prognosis for melanoma is related to tumor thickness, presence or absence of melanoma in regional lymph nodes, and extent of metastases.1-4 The TNM classification system takes these factors into account in staging melanoma.4 Based on this staging, a 5- and 10-year survival estimate can be discussed with the patient.
Survival estimates based on depth of invasion alone are also used. As an example, one study cited a 5-year survival rate of 95% for a tumor thickness <.75 mm; 85% (.75-1.4 mm); 66% (1.5-3.9 mm); and 46% (≥4 mm).1
Other variables that affect prognosis include lymphocytic infiltrate (more brisk and tumor infiltrating is better prognostically), mitotic rate (less is better; >6/mm2 is worse), ulceration (worse prognostically), and regression of the tumor.2 Regression will appear as areas of depigmentation in a previously completely pigmented lesion; it is associated with a poorer prognosis.1
Follow-up with patients is key
Regular skin, lymph node, and general follow-up exams are recommended to detect metastatic disease or new primary lesions. It has been estimated that approximately 5% of patients with a history of melanoma will develop a new primary lesion.3 Lab and imaging studies should be used when prompted by clinical findings.2
Some protocols recommend routine use of labs, including lactate dehydrogenase, complete blood count, and chemistries, as well as imaging such as chest x-ray, positron emission tomography (PET), or computed tomography (CT) based on the stage of the disease.4 No evidence has shown that routine laboratory or imaging studies affect prognosis.2
Close surveillance for my patient
My patient underwent re-excision of the tumor site with wide margins. Sentinel lymph nodes excised from the bilateral axilla were negative for melanoma. He was seen by colleagues in the oncology department, and his lab work and chest x-ray were normal. PET/CT revealed no evidence of fluorodeoxyglucose avid metastatic disease.
Based on staging, my patient’s 5-year survival was estimated at 81% and his 10-year survival at 67%. No further oncology follow-up was planned and the patient was instructed to be seen by a dermatologist for close clinical surveillance.
CORRESPONDENCE
Suresh K. Menon, MD, Hahn Medical Practices, 5078 Williamsport Pike, Martinsburg, WV 25404; [email protected]
1. Fleischer AB, Feldman SR, Clayton E, et al. Melanoma. In: Hefta J, Noujaim SR, Edmonson KG, eds. 20 Common Problems in Dermatology. 1st ed. New York, NY: McGraw-Hill; 2000:201-217.
2. James WD, Berger TG, Elston DM. Melanoma (malignant melanoma). In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Philadelphia, Pa: Saunders Elsevier; 2006:694-699.
3. Marks JG, Miller JJ. Malignant melanoma. In: Marks JG, Miller JJ, Lookingbill DP, eds. Principles of Dermatology. 4th ed. Philadelphia, Pa: Saunders Elsevier; 2006:78-81.
4. Shenenberger DW. Cutaneous malignant melanoma: a primary care perspective. Am Fam Physician. 2012;85:161-168.
5. Melanoma surveillance in the United States. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/cancer/skin/what_cdc_is_doing/melanoma_supplement.htm. Accessed October 11, 2013.
6. Bleyer A, O’Leary M, Barr R, et al, eds. Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. Bethesda, MD: National Cancer Institute, NIH Pub. No. 06-5767; 2006.
7. Usatine RP, Pfenninger JL, Stulberg DL, et al. Choosing the biopsy type. In: Usatine RP, Pfenninger, JL, Stulberg DL, et al, eds. Dermatologic and Cosmetic Procedures in Office Practice. 1st ed. Philadelphia, Pa: Elsevier; 2011: 75.
8. Usatine RP, Pfenninger JL, Stulberg DL, et al. The shave biopsy. In: Usatine RP, Pfenninger, JL, Stulberg DL, et al, eds. Dermatologic and Cosmetic Procedures in Office Practice. 1st ed. Philadelphia, Pa: Elsevier; 2011: 88.
9. Weber, JS. A New Era Approaches: Anti-CTLA-4 Monoclonal Antibodies for the Treatment of Malignant Melanoma. Medscape Education Web site. Available at: http://www.medscape.org/viewprogram/17800. Accessed July 7, 2012.
10. Shao Y, Aplin AE. Akt3-mediated resistance to apoptosis in B-RAF-targeted melanoma cells. Cancer Res. 2010;70:6670-6681.
11. Hatzivassiliou G, Song K, Yen I, et al. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature. 2010;464:431-435.
12. Halaban R, Zhang W, Bacchiocchi A, et al. PLX4032, a selective BRAF(V600E) kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAF melanoma cells. Pigment Cell Melanoma Res. 2010;23:190-200.
13. Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363:809-819.
14. Ribas A. Tumor immunotherapy directed at PD-1. N Engl J Med. 2012;366:2517-2519.
A 37-year-old Caucasian man sought care at our clinic for the pruritic patches on his trunk and extremities that had developed 3 days earlier. The patient said that the lesions started on his right arm but had spread to his left arm, posterior legs, and trunk. He reported that the trunk lesions had resolved, but the extremity lesions persisted. He’d had no specific contact exposures.
Upon further questioning, the patient indicated that he had noted the pigmented patch for at least 4 years, but was not sure how long the nodular area had been there. He thought it was a birthmark. He grew up spending a lot of time at the beach in the sun and recalled at least one blistering sunburn on his back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Melanoma
The patient underwent elliptical excisional biopsy of the primary lesion after no palpable lymphadenopathy was noted. The lateral and deep margins were negative for melanoma; the mitotic rate was <1/mm2. Aggregates of lymphocytes were associated with the lesion, but did not infiltrate it. There was no tumor regression or ulceration of the lesion. The Breslow depth was 1.25 mm.
A histopathologic evaluation revealed a superficial spreading melanoma (inferior lesion in the FIGURE) and a nodular lesion (the superior reddish-black lesion in the FIGURE). (For more on these and other forms of melanoma, see “The 4 main types of melanoma”1-4 see below.) It was unclear from the patient’s history whether this represented 2 types of melanoma (superficial spreading and nodular) in the same field of skin or the development of a nodular component in a superficial spreading lesion. Important clinical information was also missing, including the evolution of the lesions and how quickly the nodule had grown.
Who’s affected most? More than 45,000 cases of melanoma occurred in 45 states and the District of Columbia annually between 2004 and 2006, according to a 2011 report from the Centers for Disease Control and Prevention.5 White, non-Hispanics have a far higher incidence of melanoma than any other race or ethnicity.6 Women are more likely than men to be diagnosed with melanoma early in life, while men are twice as likely as women to be diagnosed after age 60.6 The etiology for the malignant transformation of melanocytes has not been fully clarified, but it is likely multifactorial, including genetic susceptibility and ultraviolet (UV) radiation damage.4
The ABCDE mnemonic is widely taught to aid in the detection of melanomas: A = asymmetry of the lesion; B = border irregularities; C = color variegation; D = diameter >6 mm; and E = evolution. The evolution of the lesion has been shown in some studies to be the most specific finding for detecting melanomas.4
Regional lymph nodes should also be carefully examined for evidence of clinical spread prior to biopsy of a suspicious lesion. This is important because biopsy may cause regional lymphadenopathy, which could confound later examinations and staging of the disease.1
The differential: Is it a worrisome lesion—or not?
The differential diagnosis of melanoma includes both benign and malignant lesions. Malignant and potentially malignant diagnoses to consider include pigmented basal cell carcinoma, pigmented squamous cell carcinoma, carcinoma metastatic to the skin, and dysplastic nevi.2,3
Benign diagnoses to consider include pigmented seborrheic keratoses, lentigo, pyogenic granuloma, Kaposi sarcoma, cherry angioma, subungual traumatic hematoma, dermatofibroma, and nevi (including blue nevi).2,3
The biopsy is paramount
A diagnosis is established based on the microscopic evaluation of suspicious lesions. Studies suggest that one-third to one-half of melanomas arise from existing nevi, with the remainder developing from previously normal-appearing skin.1,2 Patients with increased numbers of either common or dysplastic nevi are at increased risk of melanoma compared with the general population.4 Historical clues include changes in a lesion’s size, color, or symmetry; new growths; personal or family history of melanoma; and bleeding.
A biopsy for histopathologic evaluation is mandatory when a lesion is suspicious for melanoma. Dermoscopy, which involves a device that magnifies skin lesions, may reveal highly specific dermoscopic features for melanoma that can help in determining the need for biopsy.4
The preferred method for biopsy is complete elliptical excision with 2- to 3-mm margins of normal skin.2,3 However, a deep shave biopsy may also be appropriate, depending upon the clinical situation and physician experience with the technique.4
A deep shave biopsy is less time consuming than elliptical excision, making it easier to perform at the time the lesion is first evaluated. Deep shave biopsy may provide several benefits, including reducing the amount of normal tissue that is removed (especially if pathology is benign) as well as, the cost, scarring, and likelihood of wound infections. Deep shave biopsy also can avoid the need for a second elliptical excision.7,8
Determine margins, proceed with surgical excision
Early surgical excision is the primary treatment for malignant melanoma. After the diagnosis is confirmed by initial biopsy, the depth of the lesion dictates the surgical recommendations. Recommended surgical margins based on depth are: 5 mm with a layer of subcutaneous fat for melanoma in situ, 1 cm down to the fascia for lesions with a Breslow depth ≤2 mm, and 2 cm down to the fascia for lesions with a depth >2 mm.1,4
The surgical treatment of lentigo maligna melanoma can be challenging due to indistinct borders and large size. Mohs micrographic surgery can be helpful to fully remove the lesion with sparing of healthy surrounding tissue.4 When surgical excision of large lentigo maligna is technically difficult, radiation therapy is another option.3
Subungual melanoma may necessitate amputation or grafting of the digit. Mohs micrographic surgery can be useful in these situations for tissue sparing.2 (To learn more, see “When to consider Mohs surgery,” J Fam Pract. 2013;558-564.)
Is a sentinel lymph node biopsy needed?
Sentinel lymph node biopsy is often recommended for melanomas >1 mm in depth.2-4 It provides guidance on who may benefit from regional lymphadenectomy and adjuvant immunotherapy.1,3
Adjuvant therapy for patients without evidence of distant metastases can be considered in patients with positive nodes or node-negative melanoma that is 4 mm thick or Clark Level IV or V. Adjuvant high-dose interferon alpha-2b is the most commonly used agent in these situations.2 Some studies suggest an increase in median overall survival of up to 11 months with high-dose interferon as compared to no treatment.3 Limitations include toxicity from these high-dose regimens.3 Treatment with interferon does not represent a cure; rather, it should be considered a palliative intervention with marginal benefit.1
When there are distant metastases…
Once distant metastases are identified, the goal of therapy should be palliative care as this condition is generally incurable. Chemotherapy, radiation, and excision of solitary metastases are all interventions that have traditionally been employed.1 The primary site for metastasis is the skin, but all organs are potential sites of spread. Central nervous system metastasis is the most common cause of the death.2
Novel therapies include inhibition of BRAF, an enzyme of the mitogen-activated protein kinase pathway (MAPK), and blocking of cytotoxic T lymphocyte-associated antigen-4 (CTLA-4).
BRAF-enzyme inhibitor. Mutated BRAF contributes to uncontrolled cell growth and resistance to programmed cell death (apoptosis).9,10 In August 2011, vemurafenib (Zelboraf ), a BRAF-enzyme inhibitor, was approved by the US Food and Drug Administration (FDA) for the treatment of late-stage melanoma. It works only in patients with the BRAFV600E mutation, which is found in approximately 60% of melanomas.11,12 One phase 1 study showed partial to complete regression in 80% of patients treated, but this regression lasted only 2 to 18 months.13
Anti-CTLA-4 monoclonal antibody. Cytotoxic T-lymphocytes can recognize and potentially destroy cancer cells.14 However, CTLA-4, which is expressed on the surface of cytotoxic T-lymphocytes, has a suppressive effect on the T-lymphocyte response after interaction with the antigen-presenting cell. Researchers deduced that blocking CTLA-4 would allow the immune system to remain responsive to abnormal antigens, including those from melanoma.9
Ipilimumab (Yervoy), an anti-CTLA-4 monoclonal antibody, was approved by the FDA in March 2011 for the treatment of late-stage melanoma.11 Partial and complete responses have been shown in trials of ipilimumab as monotherapy and in combination with vaccines, chemotherapy, and interleukin-2, but these responses have not been sustained.9
Although these novel therapies represent significant advancements in the understanding of the pathogenesis of melanoma, the short duration of efficacy highlights the cancer’s ability to develop resistance to these treatments. This ability to adapt suggests that melanoma harbors multiple oncogenes and several pathways for carcinogenesis. Combination targeted therapies may be required to improve clinical results; research is ongoing.9 Toxicities associated with these medications are also a limiting factor.
What about vaccines? Vaccine studies are also ongoing. Although some have shown promising results, no clearly effective therapy has been produced to date.2
Factors that affect prognosis
The prognosis for melanoma is related to tumor thickness, presence or absence of melanoma in regional lymph nodes, and extent of metastases.1-4 The TNM classification system takes these factors into account in staging melanoma.4 Based on this staging, a 5- and 10-year survival estimate can be discussed with the patient.
Survival estimates based on depth of invasion alone are also used. As an example, one study cited a 5-year survival rate of 95% for a tumor thickness <.75 mm; 85% (.75-1.4 mm); 66% (1.5-3.9 mm); and 46% (≥4 mm).1
Other variables that affect prognosis include lymphocytic infiltrate (more brisk and tumor infiltrating is better prognostically), mitotic rate (less is better; >6/mm2 is worse), ulceration (worse prognostically), and regression of the tumor.2 Regression will appear as areas of depigmentation in a previously completely pigmented lesion; it is associated with a poorer prognosis.1
Follow-up with patients is key
Regular skin, lymph node, and general follow-up exams are recommended to detect metastatic disease or new primary lesions. It has been estimated that approximately 5% of patients with a history of melanoma will develop a new primary lesion.3 Lab and imaging studies should be used when prompted by clinical findings.2
Some protocols recommend routine use of labs, including lactate dehydrogenase, complete blood count, and chemistries, as well as imaging such as chest x-ray, positron emission tomography (PET), or computed tomography (CT) based on the stage of the disease.4 No evidence has shown that routine laboratory or imaging studies affect prognosis.2
Close surveillance for my patient
My patient underwent re-excision of the tumor site with wide margins. Sentinel lymph nodes excised from the bilateral axilla were negative for melanoma. He was seen by colleagues in the oncology department, and his lab work and chest x-ray were normal. PET/CT revealed no evidence of fluorodeoxyglucose avid metastatic disease.
Based on staging, my patient’s 5-year survival was estimated at 81% and his 10-year survival at 67%. No further oncology follow-up was planned and the patient was instructed to be seen by a dermatologist for close clinical surveillance.
CORRESPONDENCE
Suresh K. Menon, MD, Hahn Medical Practices, 5078 Williamsport Pike, Martinsburg, WV 25404; [email protected]
A 37-year-old Caucasian man sought care at our clinic for the pruritic patches on his trunk and extremities that had developed 3 days earlier. The patient said that the lesions started on his right arm but had spread to his left arm, posterior legs, and trunk. He reported that the trunk lesions had resolved, but the extremity lesions persisted. He’d had no specific contact exposures.
Upon further questioning, the patient indicated that he had noted the pigmented patch for at least 4 years, but was not sure how long the nodular area had been there. He thought it was a birthmark. He grew up spending a lot of time at the beach in the sun and recalled at least one blistering sunburn on his back.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Melanoma
The patient underwent elliptical excisional biopsy of the primary lesion after no palpable lymphadenopathy was noted. The lateral and deep margins were negative for melanoma; the mitotic rate was <1/mm2. Aggregates of lymphocytes were associated with the lesion, but did not infiltrate it. There was no tumor regression or ulceration of the lesion. The Breslow depth was 1.25 mm.
A histopathologic evaluation revealed a superficial spreading melanoma (inferior lesion in the FIGURE) and a nodular lesion (the superior reddish-black lesion in the FIGURE). (For more on these and other forms of melanoma, see “The 4 main types of melanoma”1-4 see below.) It was unclear from the patient’s history whether this represented 2 types of melanoma (superficial spreading and nodular) in the same field of skin or the development of a nodular component in a superficial spreading lesion. Important clinical information was also missing, including the evolution of the lesions and how quickly the nodule had grown.
Who’s affected most? More than 45,000 cases of melanoma occurred in 45 states and the District of Columbia annually between 2004 and 2006, according to a 2011 report from the Centers for Disease Control and Prevention.5 White, non-Hispanics have a far higher incidence of melanoma than any other race or ethnicity.6 Women are more likely than men to be diagnosed with melanoma early in life, while men are twice as likely as women to be diagnosed after age 60.6 The etiology for the malignant transformation of melanocytes has not been fully clarified, but it is likely multifactorial, including genetic susceptibility and ultraviolet (UV) radiation damage.4
The ABCDE mnemonic is widely taught to aid in the detection of melanomas: A = asymmetry of the lesion; B = border irregularities; C = color variegation; D = diameter >6 mm; and E = evolution. The evolution of the lesion has been shown in some studies to be the most specific finding for detecting melanomas.4
Regional lymph nodes should also be carefully examined for evidence of clinical spread prior to biopsy of a suspicious lesion. This is important because biopsy may cause regional lymphadenopathy, which could confound later examinations and staging of the disease.1
The differential: Is it a worrisome lesion—or not?
The differential diagnosis of melanoma includes both benign and malignant lesions. Malignant and potentially malignant diagnoses to consider include pigmented basal cell carcinoma, pigmented squamous cell carcinoma, carcinoma metastatic to the skin, and dysplastic nevi.2,3
Benign diagnoses to consider include pigmented seborrheic keratoses, lentigo, pyogenic granuloma, Kaposi sarcoma, cherry angioma, subungual traumatic hematoma, dermatofibroma, and nevi (including blue nevi).2,3
The biopsy is paramount
A diagnosis is established based on the microscopic evaluation of suspicious lesions. Studies suggest that one-third to one-half of melanomas arise from existing nevi, with the remainder developing from previously normal-appearing skin.1,2 Patients with increased numbers of either common or dysplastic nevi are at increased risk of melanoma compared with the general population.4 Historical clues include changes in a lesion’s size, color, or symmetry; new growths; personal or family history of melanoma; and bleeding.
A biopsy for histopathologic evaluation is mandatory when a lesion is suspicious for melanoma. Dermoscopy, which involves a device that magnifies skin lesions, may reveal highly specific dermoscopic features for melanoma that can help in determining the need for biopsy.4
The preferred method for biopsy is complete elliptical excision with 2- to 3-mm margins of normal skin.2,3 However, a deep shave biopsy may also be appropriate, depending upon the clinical situation and physician experience with the technique.4
A deep shave biopsy is less time consuming than elliptical excision, making it easier to perform at the time the lesion is first evaluated. Deep shave biopsy may provide several benefits, including reducing the amount of normal tissue that is removed (especially if pathology is benign) as well as, the cost, scarring, and likelihood of wound infections. Deep shave biopsy also can avoid the need for a second elliptical excision.7,8
Determine margins, proceed with surgical excision
Early surgical excision is the primary treatment for malignant melanoma. After the diagnosis is confirmed by initial biopsy, the depth of the lesion dictates the surgical recommendations. Recommended surgical margins based on depth are: 5 mm with a layer of subcutaneous fat for melanoma in situ, 1 cm down to the fascia for lesions with a Breslow depth ≤2 mm, and 2 cm down to the fascia for lesions with a depth >2 mm.1,4
The surgical treatment of lentigo maligna melanoma can be challenging due to indistinct borders and large size. Mohs micrographic surgery can be helpful to fully remove the lesion with sparing of healthy surrounding tissue.4 When surgical excision of large lentigo maligna is technically difficult, radiation therapy is another option.3
Subungual melanoma may necessitate amputation or grafting of the digit. Mohs micrographic surgery can be useful in these situations for tissue sparing.2 (To learn more, see “When to consider Mohs surgery,” J Fam Pract. 2013;558-564.)
Is a sentinel lymph node biopsy needed?
Sentinel lymph node biopsy is often recommended for melanomas >1 mm in depth.2-4 It provides guidance on who may benefit from regional lymphadenectomy and adjuvant immunotherapy.1,3
Adjuvant therapy for patients without evidence of distant metastases can be considered in patients with positive nodes or node-negative melanoma that is 4 mm thick or Clark Level IV or V. Adjuvant high-dose interferon alpha-2b is the most commonly used agent in these situations.2 Some studies suggest an increase in median overall survival of up to 11 months with high-dose interferon as compared to no treatment.3 Limitations include toxicity from these high-dose regimens.3 Treatment with interferon does not represent a cure; rather, it should be considered a palliative intervention with marginal benefit.1
When there are distant metastases…
Once distant metastases are identified, the goal of therapy should be palliative care as this condition is generally incurable. Chemotherapy, radiation, and excision of solitary metastases are all interventions that have traditionally been employed.1 The primary site for metastasis is the skin, but all organs are potential sites of spread. Central nervous system metastasis is the most common cause of the death.2
Novel therapies include inhibition of BRAF, an enzyme of the mitogen-activated protein kinase pathway (MAPK), and blocking of cytotoxic T lymphocyte-associated antigen-4 (CTLA-4).
BRAF-enzyme inhibitor. Mutated BRAF contributes to uncontrolled cell growth and resistance to programmed cell death (apoptosis).9,10 In August 2011, vemurafenib (Zelboraf ), a BRAF-enzyme inhibitor, was approved by the US Food and Drug Administration (FDA) for the treatment of late-stage melanoma. It works only in patients with the BRAFV600E mutation, which is found in approximately 60% of melanomas.11,12 One phase 1 study showed partial to complete regression in 80% of patients treated, but this regression lasted only 2 to 18 months.13
Anti-CTLA-4 monoclonal antibody. Cytotoxic T-lymphocytes can recognize and potentially destroy cancer cells.14 However, CTLA-4, which is expressed on the surface of cytotoxic T-lymphocytes, has a suppressive effect on the T-lymphocyte response after interaction with the antigen-presenting cell. Researchers deduced that blocking CTLA-4 would allow the immune system to remain responsive to abnormal antigens, including those from melanoma.9
Ipilimumab (Yervoy), an anti-CTLA-4 monoclonal antibody, was approved by the FDA in March 2011 for the treatment of late-stage melanoma.11 Partial and complete responses have been shown in trials of ipilimumab as monotherapy and in combination with vaccines, chemotherapy, and interleukin-2, but these responses have not been sustained.9
Although these novel therapies represent significant advancements in the understanding of the pathogenesis of melanoma, the short duration of efficacy highlights the cancer’s ability to develop resistance to these treatments. This ability to adapt suggests that melanoma harbors multiple oncogenes and several pathways for carcinogenesis. Combination targeted therapies may be required to improve clinical results; research is ongoing.9 Toxicities associated with these medications are also a limiting factor.
What about vaccines? Vaccine studies are also ongoing. Although some have shown promising results, no clearly effective therapy has been produced to date.2
Factors that affect prognosis
The prognosis for melanoma is related to tumor thickness, presence or absence of melanoma in regional lymph nodes, and extent of metastases.1-4 The TNM classification system takes these factors into account in staging melanoma.4 Based on this staging, a 5- and 10-year survival estimate can be discussed with the patient.
Survival estimates based on depth of invasion alone are also used. As an example, one study cited a 5-year survival rate of 95% for a tumor thickness <.75 mm; 85% (.75-1.4 mm); 66% (1.5-3.9 mm); and 46% (≥4 mm).1
Other variables that affect prognosis include lymphocytic infiltrate (more brisk and tumor infiltrating is better prognostically), mitotic rate (less is better; >6/mm2 is worse), ulceration (worse prognostically), and regression of the tumor.2 Regression will appear as areas of depigmentation in a previously completely pigmented lesion; it is associated with a poorer prognosis.1
Follow-up with patients is key
Regular skin, lymph node, and general follow-up exams are recommended to detect metastatic disease or new primary lesions. It has been estimated that approximately 5% of patients with a history of melanoma will develop a new primary lesion.3 Lab and imaging studies should be used when prompted by clinical findings.2
Some protocols recommend routine use of labs, including lactate dehydrogenase, complete blood count, and chemistries, as well as imaging such as chest x-ray, positron emission tomography (PET), or computed tomography (CT) based on the stage of the disease.4 No evidence has shown that routine laboratory or imaging studies affect prognosis.2
Close surveillance for my patient
My patient underwent re-excision of the tumor site with wide margins. Sentinel lymph nodes excised from the bilateral axilla were negative for melanoma. He was seen by colleagues in the oncology department, and his lab work and chest x-ray were normal. PET/CT revealed no evidence of fluorodeoxyglucose avid metastatic disease.
Based on staging, my patient’s 5-year survival was estimated at 81% and his 10-year survival at 67%. No further oncology follow-up was planned and the patient was instructed to be seen by a dermatologist for close clinical surveillance.
CORRESPONDENCE
Suresh K. Menon, MD, Hahn Medical Practices, 5078 Williamsport Pike, Martinsburg, WV 25404; [email protected]
1. Fleischer AB, Feldman SR, Clayton E, et al. Melanoma. In: Hefta J, Noujaim SR, Edmonson KG, eds. 20 Common Problems in Dermatology. 1st ed. New York, NY: McGraw-Hill; 2000:201-217.
2. James WD, Berger TG, Elston DM. Melanoma (malignant melanoma). In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Philadelphia, Pa: Saunders Elsevier; 2006:694-699.
3. Marks JG, Miller JJ. Malignant melanoma. In: Marks JG, Miller JJ, Lookingbill DP, eds. Principles of Dermatology. 4th ed. Philadelphia, Pa: Saunders Elsevier; 2006:78-81.
4. Shenenberger DW. Cutaneous malignant melanoma: a primary care perspective. Am Fam Physician. 2012;85:161-168.
5. Melanoma surveillance in the United States. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/cancer/skin/what_cdc_is_doing/melanoma_supplement.htm. Accessed October 11, 2013.
6. Bleyer A, O’Leary M, Barr R, et al, eds. Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. Bethesda, MD: National Cancer Institute, NIH Pub. No. 06-5767; 2006.
7. Usatine RP, Pfenninger JL, Stulberg DL, et al. Choosing the biopsy type. In: Usatine RP, Pfenninger, JL, Stulberg DL, et al, eds. Dermatologic and Cosmetic Procedures in Office Practice. 1st ed. Philadelphia, Pa: Elsevier; 2011: 75.
8. Usatine RP, Pfenninger JL, Stulberg DL, et al. The shave biopsy. In: Usatine RP, Pfenninger, JL, Stulberg DL, et al, eds. Dermatologic and Cosmetic Procedures in Office Practice. 1st ed. Philadelphia, Pa: Elsevier; 2011: 88.
9. Weber, JS. A New Era Approaches: Anti-CTLA-4 Monoclonal Antibodies for the Treatment of Malignant Melanoma. Medscape Education Web site. Available at: http://www.medscape.org/viewprogram/17800. Accessed July 7, 2012.
10. Shao Y, Aplin AE. Akt3-mediated resistance to apoptosis in B-RAF-targeted melanoma cells. Cancer Res. 2010;70:6670-6681.
11. Hatzivassiliou G, Song K, Yen I, et al. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature. 2010;464:431-435.
12. Halaban R, Zhang W, Bacchiocchi A, et al. PLX4032, a selective BRAF(V600E) kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAF melanoma cells. Pigment Cell Melanoma Res. 2010;23:190-200.
13. Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363:809-819.
14. Ribas A. Tumor immunotherapy directed at PD-1. N Engl J Med. 2012;366:2517-2519.
1. Fleischer AB, Feldman SR, Clayton E, et al. Melanoma. In: Hefta J, Noujaim SR, Edmonson KG, eds. 20 Common Problems in Dermatology. 1st ed. New York, NY: McGraw-Hill; 2000:201-217.
2. James WD, Berger TG, Elston DM. Melanoma (malignant melanoma). In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin: Clinical Dermatology. 10th ed. Philadelphia, Pa: Saunders Elsevier; 2006:694-699.
3. Marks JG, Miller JJ. Malignant melanoma. In: Marks JG, Miller JJ, Lookingbill DP, eds. Principles of Dermatology. 4th ed. Philadelphia, Pa: Saunders Elsevier; 2006:78-81.
4. Shenenberger DW. Cutaneous malignant melanoma: a primary care perspective. Am Fam Physician. 2012;85:161-168.
5. Melanoma surveillance in the United States. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/cancer/skin/what_cdc_is_doing/melanoma_supplement.htm. Accessed October 11, 2013.
6. Bleyer A, O’Leary M, Barr R, et al, eds. Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. Bethesda, MD: National Cancer Institute, NIH Pub. No. 06-5767; 2006.
7. Usatine RP, Pfenninger JL, Stulberg DL, et al. Choosing the biopsy type. In: Usatine RP, Pfenninger, JL, Stulberg DL, et al, eds. Dermatologic and Cosmetic Procedures in Office Practice. 1st ed. Philadelphia, Pa: Elsevier; 2011: 75.
8. Usatine RP, Pfenninger JL, Stulberg DL, et al. The shave biopsy. In: Usatine RP, Pfenninger, JL, Stulberg DL, et al, eds. Dermatologic and Cosmetic Procedures in Office Practice. 1st ed. Philadelphia, Pa: Elsevier; 2011: 88.
9. Weber, JS. A New Era Approaches: Anti-CTLA-4 Monoclonal Antibodies for the Treatment of Malignant Melanoma. Medscape Education Web site. Available at: http://www.medscape.org/viewprogram/17800. Accessed July 7, 2012.
10. Shao Y, Aplin AE. Akt3-mediated resistance to apoptosis in B-RAF-targeted melanoma cells. Cancer Res. 2010;70:6670-6681.
11. Hatzivassiliou G, Song K, Yen I, et al. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature. 2010;464:431-435.
12. Halaban R, Zhang W, Bacchiocchi A, et al. PLX4032, a selective BRAF(V600E) kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAF melanoma cells. Pigment Cell Melanoma Res. 2010;23:190-200.
13. Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363:809-819.
14. Ribas A. Tumor immunotherapy directed at PD-1. N Engl J Med. 2012;366:2517-2519.