User login
Providing Quality Epilepsy Care for Veterans
Epilepsy is a common and complex neurologic condition marked by recurrent seizures. It has been diagnosed in more than 87,000 veterans enrolled in the VA health care system, 16% of whom have comorbid traumatic brain injury (TBI), and nearly 25% also have posttraumatic stress disorder (PTSD).1 These comorbidities were even more common in Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans: TBI in 52.6% and PTSD in 70.4%. With 25 drugs for seizures and 2 approved devices, treatment of epilepsy can prove challenging to providers whose goal is to balance seizure control and adverse effects (AEs).
Despite the therapeutic armamentarium, about one-third of people with epilepsy have poorly controlled seizures, and an untold number may experience delays in referral to higher levels of epilepsy care or undergo troubling antiepileptic medication AEs and comorbid psychiatric disorders that have profound impacts on quality of life (QOL).
Quality generally has been defined as “providing the right care to the right patient at the right time and in the right way to achieve the best possible results.”2 Much work has been done over the past 2 decades to identify “the right care” for epilepsy patients.3
The American Academy of Neurology (AAN) has developed evidence-based, clinically focused guidelines on numerous topics, including antiepileptic drugs and women’s health, and has developed quality measure sets.4,5 More broadly, the Institute of Medicine (IOM) proposed 13 recommendations, including improving quality of care, establishing epilepsy centers and an epilepsy care network, educating health professionals about epilepsy, and providing education for people with epilepsy and their families.6
Within the VA, health care for veterans with epilepsy is changing in part by the Epilepsy Centers of Excellence (ECoC), established by federal law. The ECoE’s primary missions are to improve quality of and access to epilepsy specialty care to improve the health and well-being of veteran patients with epilepsy and other seizure disorders through integration of clinical care, outreach, research, and education to VA providers and patients.7
The goal of this article is to outline the key elements of quality epilepsy care and make recommendations for providing quality care in the VA health care system.
Diagnosis and Seizure Types
Quality care for veterans with epilepsy begins with the provider reviewing pertinent history and establishing the clinical characteristics of the patient’s seizures and epilepsy. The provider should ask about the first signs of the seizure or warning (aura), the seizure (ictal period), and the period after the seizure (postictal period). Seizure histories from the patient and observers are critical.
The first step is to define whether the patient’s seizures are generalized, that is, start all over the brain at once, or focal, starting in one area of the brain. The patient’s initial sensation at the onset of a seizure (aura) may help localize onset and define focal seizures. For example, déjà vu sensations often point to seizure onset in the mesial temporal lobe and hippocampus. Focal seizures can spread and cause cognitive dysfunction, including aphasia and amnesia, or evolve into a generalized convulsion (tonic-clonic seizure). Many patients present with a generalized tonic-clonic seizure and have had brief focal seizures that were not considered seizures by the patient or by other providers. This seizure type should be clarified by asking specifically about paroxysmal symptoms. For example, brief periods of confusion that are episodic may be focal seizures. In general, focal seizures are stereotyped and may have a feature that helps in establishing the diagnosis. Many temporal lobe seizures are associated with lip smacking behaviors (oral buccal automatisms).
Tonic-clonic seizures may begin without an aura and are generalized from onset. Patients with this type of seizure may have electroencephalogram (EEG) findings that define a generalized abnormality, which consist of frontocentral spike and wave discharges in the EEG. In the VA population, the first generalized tonic-clonic seizure may occur while in the military. Some of these patients have juvenile myoclonic epilepsy, and a history of brief jerks on waking (myoclonus) may have been occurring but not recognized as seizures. The treatment of seizures, in part, depends on whether they begin focally or are generalized at onset.
Often people with epilepsy have multiple seizure types. The types of seizures should be documented and, if possible, corroborated by a witness. Epileptic seizures tend to be stereotyped and of relatively brief duration, usually < 2 minutes. The period after a seizure may be followed by a more prolonged period of neurologic dysfunction that includes confusion and fatigue. These symptoms may be the only indication that the patient has had a seizure.
At each clinic visit, the characteristics of the patient’s seizures should be reviewed and the frequency of seizures documented. A calendar to track seizure frequency is helpful to understand precipitating factors and response to treatment.
The health care provider (HCP) should look for the cause of a patient’s epilepsy. It is important to ask the patient about family history, age of first seizure, occurrence of febrile seizures, developmental history, past history of meningitis or encephalitis, history of childhood seizures or spells, and history of brain lesions, including tumors, strokes, or TBI. Most patients with epilepsy do not have a clear cause for their epilepsy, but the cause may be clarified with EEG and magnetic resonance imaging (MRI) testing.
EEG and Brain Imaging
All patients with epilepsy should be evaluated with an EEG, and for those with focal epilepsy or undefined epilepsy, with an imaging study of the brain, preferably an MRI. These results should be reviewed at each visit. The EEG may show focal features that are related to neurophysiologic dysfunction, such as slowing that is not definitely epileptiform in character, or show focal spike or sharp waves that are epileptiform in character. Generalized abnormalities may include generalized slowing that is not an epileptiform feature or frontocentral spike wave patterns that are epileptiform in character. The EEG cannot rule out epilepsy, but can rule in the likelihood of epilepsy when definite epileptiform features are present.
Brain imaging can define many conditions that can cause focal epilepsy, and an MRI is more sensitive for defining a number of these conditions (cavernous angiomas, hippocampal sclerosis, developmental migration disorders, and low-grade neoplasms). Significant trauma with signal abnormalities to suggest prior bleeding predispose to epilepsy. When patients are refractory to medical therapy and have imaging findings concordant with EEG onset of seizures, then surgery can be a better treatment.
Adverse Effects
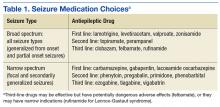
Broad-spectrum drug treatments are efficacious for either generalized or focal seizures, whereas narrow-spectrum treatments are most efficacious for focal seizures (Table 1). The choice of a seizure medication is based on the patient’s seizure type(s) and other comorbid conditions.7 For example, a patient with epilepsy and migraines may do better with a seizure medication that also is used for migraine prophylaxis (valproate or topiramate). In general, seizure control is unlikely to be achieved if patients fail the first 2 medications tried.8 Treating with > 1 medication may improve seizure control but may increase AEs. A review of current seizure medications and their AEs can be found on the ECoE website (http://www.epilepsy.va.gov/Provider_Education.asp).
In VA cooperative studies that evaluated seizure medications, the most common reason for discontinuing a drug was the combination of ineffectiveness and AEs.9-11 Addressing AEs is a quality measure for the care of patients with epilepsy. Adverse effects may be dose dependent or idiosyncratic (rashes). Drug levels may help in determining dose-dependent AEs; for example, diplopia with carbamazepine levels above 10 μg/mL. Each patient may have susceptibility to medication AEs that do not exactly match therapeutic levels. When patients have AEs, a reduction in dose or trial of an alternative medication is advised.
Uncontrollable Epilepsy
About one-third of people with epilepsy have uncontrolled seizures, known as medically intractable epilepsy, which may be identified early in their clinical course by failure of the first 2 tolerated medications.8 Patients should be referred to an epilepsy center so their epilepsy can be defined by video EEG monitoring to capture seizures. Unfortunately, in the VA system, this route is often delayed, and patients may not be diagnosed appropriately for years.12 Some of these patients may be considered treatment failures because the right medications were not tried (eg, generalized epilepsy that is treated with narrow-spectrum seizure medications). Juvenile myoclonic epilepsy often may not be controlled by phenytoin or carbamazepine, but valproate, lamotrigine, levetiracetam, and zonisamide may be more effective.
Other patients may not have epilepsy but have psychogenic nonepileptic seizures (PNES). These behavioral seizures do not have an EEG epileptiform correlate. About 25% of patients who undergo prolonged video EEG monitoring have PNES, and seizure medications do not treat these events.12 A smaller percentage of patients have both epileptic and nonepileptic seizures (5%-15%). Psychogenic nonepileptic seizures often occur within the context of traumatic exposure(s) or previous physical or sexual abuse.
In the VA population, PNES is more often associated with PTSD or head trauma history than in patients with epilepsy.13,14 To confirm the diagnosis of PNES, video-EEG capture of the patient’s seizures is required. Because of the increased number of combat veterans with TBI and PTSD, the diagnosis of epilepsy may be difficult without video-EEG monitoring. Management consists of addressing the underlying conversion disorder and recognition and treatment of comorbidities, such as mood, anxiety, personality, or PTSD. Recently, cognitive behavioral-informed psychotherapy (CB-ip) has been shown to be effective in patients with PNES and is available through the VA national telemental health center and at some ECoE sites.15
If a patient with uncontrolled epilepsy has focal seizures, surgical therapy is more likely to result in seizure control than will medical therapy.16,17 This is especially true when other testing, including MRI, positron emission tomography, and neuropsychiatric evaluation, point to a concordance of localization. These patients should be evaluated in a center that can provide surgical therapy and if necessary also record seizures with invasive techniques using electrodes placed directly over the cortex or into the brain to sample deeper structures like the hippocampus or amygdala. Patients who are refractory should be considered for reevaluation every 2 years by a comprehensive epilepsy center.
Unfortunately, some patients have seizures that begin in eloquent cortex, which if removed, leads to undesirable neurologic loss or multifocal seizure onset. In these patients, seizure frequency can be reduced by vagus nerve stimulation or intracranial responsive neurostimulation.18,19
Safety
Epilepsy has inherent risks for injury. Patients and their families often need to be informed about risks and risky behaviors to avoid. A frank discussion about safety is prudent. What to do for the patient during a seizure should be addressed. For convulsive seizures: Protect the patient from injury by placing something soft between the patient’s head and the floor, keep the patient on his or her side; do not restrain the patient or put anything in the mouth; stay calm and time the seizure; as the patient gains consciousness, talk to the patient and be reassuring. For nonconvulsive seizures: Stay with the patient; time the seizure; gently guide the patient away from dangerous situations like streets or stairs; stay with the patient until he or she is back to normal, and reassure the patient.
Driving
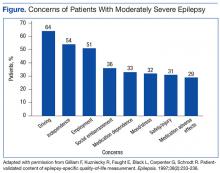
People with epilepsy identify driving as one of their major concerns; therefore, it is important for HCPs to properly counsel patients with seizure disorders and their families about driving (Figure).20 In general people with controlled seizures are permitted to drive in every state in the U.S., but people with uncontrolled seizures are restricted from licensure. Despite the desire and necessity to drive for many individuals with epilepsy, seizures while driving pose risks for crashes, which may result in property damage, injuries, and death.21 Factors, such as duration of seizure freedom, help predict the risk for crashes. The legal rules for determining control and administering restrictions are a complex mix of federal and state laws, regulations, and local practices, which vary widely across the country.21,22 The standards also change over time; updated information is available from local state authorities and on good informational sites, such as those of the Epilepsy Foundation.
The key standard for determining accident risks is the seizure free interval, which is the duration of time a person with epilepsy has been seizure-free.21-23 In the U.S., the accepted period for seizure freedom varies from about 3 months to 12 months, depending on individual state rules.24
California, Delaware, Nevada, New Jersey, Oregon, and Pennsylvania require mandatory reporting. Generally physician groups in the U.S. and elsewhere oppose such mandatory reporting, because of the concern that their patients will not report their seizures, and thus may not receive appropriate treatment. Indeed, patients with epilepsy often do not tell physicians about their seizures, fearing loss of driving privileges and other social consequences.21,23 Providers should make an effort to determine seizure frequency and whether the patient is being truthful. This information then provides a background for the provider to discuss driving issues.
Injury
People with epilepsy are susceptible to injury during a seizure and need to be counseled regarding safety, particularly when seizures are not well controlled. Hazardous situations include being near stoves or cooking, bathing alone, swimming alone, working at heights without a safety harness, and using power tools.26
Sudden Unexplained Death
Patients with recurrent seizures have an increased risk for accidental fatality and for sudden unexplained death in epilepsy (SUDEP), which accounts for up to 17% of all deaths in people with epilepsy. The risk for sudden death from recurrent seizures increases 2.3 times compared with the risk in the general population.25 A SUDEP is an unexpected death in a person who has epilepsy with no other obvious cause of death.26 Because increased seizure frequency, the presence of tonic-clonic seizures, and other accidental risks of seizures are associated with SUDEP, the subject should be discussed with patients and their families, to encourage adherence to treatment. Epileptologists also discuss these risks with patients and their families when surgical interventions are being considered. The potential risks for injury or SUDEP may offset the surgical risks when pursuing a potentially curative epilepsy procedure.
Women of Childbearing Age
In January 2015, the ECoE started a women veterans epilepsy workgroup with the goal of improving clinical care within the VAHCS to provide education to patients, family members, and VA health care providers about the care of women with epilepsy.
Providers need to be aware that seizure medications that induce certain hepatic enzymes can lead to hormonal contraceptive failure (Table 2).27 Preconception folic acid supplementation (with at least 0.4 mg) should be considered, because it may reduce the risk of major congenital malformations.28 The goal of epilepsy management prior to conception is to maximize seizure control with the optimal seizure medication to avoid the need to make changes during the pregnancy.
During pregnancy, the volume of distribution increases and seizure medication metabolism may change requiring dose adjustment. The best predictor of seizure frequency during pregnancy is a woman’s epilepsy pattern prior to conception. Seizure freedom for 9 months prior to conception is associated with a 84% to 92% likelihood of seizure freedom throughout the pregnancy.29
International seizure medication pregnancy registries have provided valuable information regarding the risk of major congenital malformation (MCM) of development, which seems to be a consequence of seizure medication therapy and not epilepsy itself. The risk of MCM associated with seizure medication therapy is about 4% to 5% compared with 1.5% to 3% in the general population.30,31 A seizure medication table that supplements the existing VA ECoE information specifically addresses women’s issues with the recognition that recent revisions to the teratogenicity classification have been made by the FDA (Table 2).32 If possible, valproate should be avoided during pregnancy due to its higher rate of MCM and impact on neurocognitive function.33 Obstetrical input is essential in arranging routine prenatal fetal testing. Although women with epilepsy do not have a substantially increased risk of undergoing a cesarean section, delivery in a hospital obstetric unit is advised.
Postpartum women veterans with epilepsy should be encouraged to breast feed since the potential benefits seem to outweigh any established risk of seizure medication exposure to the infant. No relative impact on cognition was found in breastfed infants exposed to a variety of seizure medications.34 Following delivery, vigilance is needed to monitor for sleep deprivation, postpartum depression, and the safe care of the infant.35 Care of women with epilepsy does not end with pregnancy planning, additional important topics include psychiatric comorbidities, catamenial epilepsy, and bone health, which are unique to women veterans with epilepsy.
Identifying Psychiatric Conditions
People with epilepsy have a number of psychiatric comorbidities. Suicide and suicide attempts are 6 to 25 times more common in patients with temporal lobe epilepsy compared with those in the general population.36-38 Although the FDA identified all seizure medications as potential contributors to suicide risk, a recent longitudinal study of suicidal ideation and attempt found that those who received seizure medications were more likely to have suicidal ideation and attempt than those who did not received seizure medications, suggesting that medication may relate to baseline depression or suicidal ideation.39 When seeing patients with epilepsy, screening for suicidal ideation is good practice.
Depression and anxiety disorders are the most common psychiatric comorbidities in people with epilepsy.40,41 About half of people with epilepsy have symptoms of depression, and 40% have anxiety.42 Depression often precedes the diagnosis of epilepsy, and anxiety often is present and related to the fear of having seizures and of social embarrassment.43 People with epilepsy may not self-report these symptoms if not asked directly. Identification of comorbid depression and anxiety should lead to appropriate treatment. The CB-ip being used for PNES also is being used for treatment of epilepsy and its comorbidities.44
Mild traumatic brain injury (mTBI) has a small increased risk of epilepsy.45 Veterans with mTBI that occurs in the context of blasts are set up for the development of PTSD. These veterans may have other mild cognitive symptoms that can be confused with seizures. Furthermore, mTBI and PNES often occur together, more so than do mTBI and epileptic seizures.14 Video-EEG monitoring may be warranted for these patients.
Education and Self-Management
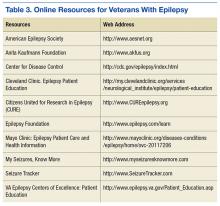
The IOM report on epilepsy identified patient and family education as essential for better epilepsy care.6 Providers should help educate patients about their epilepsy and refer them to resources available online (Table 3). A continuing exchange about their condition and treatment with seizure medications should occur with each visit. People with epilepsy should also receive guidance regarding how to manage their epilepsy and day-to-day issues. Referring, patients to social workers, psychologists, vocational rehabilitation services, and support groups can enhance a patient’s QOL.3,6 The stigma of epilepsy is another burden that can be diminished by attending support groups. Recently, being a part of an online patient community of veterans was found to improve self-management.46
Conclusion
People with epilepsy have many issues that are unique to the condition and, in part, are related to the unpredictable occurrence of seizures and loss of function. Ideally, seizure control provides a normal lifestyle; however, some mood and anxiety comorbidities may persist despite seizure control. Care in the VA system includes access to 16 sites that have programs dedicated to treating veterans with epilepsy and many more consortium sites that interact with the ECoE to provide high-quality patient care (http:\\www.epilepsy.va.gov). The ECoE also provides a readily available resource to optimally manage veterans with epilepsy. Attention to the issues addressed in this article will promote quality care for veterans with epilepsy.
1. Rehman R, Kelly P, Husain AM, Tran TT. Characteristics of veterans diagnosed with seizures within Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762.
2. National Committee for Quality Assurance (NCQA). The essential guide to health care quality. https://www.ncqa.org/Portals/0/Publications/Resource%20Library/NCQA_Primer_web.pdf. Accessed August 9, 2016.
3. Pugh MJ, Berlowitz DR, Montouris GB, et al. What constitutes high quality of care for adults with epilepsy? Neurology. 2007;69(21):2020-2027.
4. Fountain NB, Van Ness PC, Swain-Eng R, Tonn S, Bever CT Jr; American Academy of Neurology Epilepsy Measure Development Panel and the American Medical Association-Convened Physician Consortium for Performance Improvement Independent Measure Development Process. Quality improvement in neurology: AAN epilepsy quality measures: report of the Quality Measurement and Reporting Subcommittee of the American Academy of Neurology. Neurology. 2011;76(1):94-99.
5. Fountain NB, Van Ness PC, Bennett A, et al. Quality improvement in neurology: epilepsy update quality measurement set. Neurology. 2015;84(14):1483-1487.
6. England MJ, Liverman CT, Schultz AM, Strawbridge LM, eds; Committee on the Public Health Dimensions of the Epilepsies, Board on Health Sciences Policy, Institute of Medicine. Epilepsy Across the Spectrum: Promoting Health and Understanding. Washington, DC: The National Academies Press; 2012.
7. Tortorice K, Rutecki P. Principles of Treatment. In: Hussain, AM, Tran TT, eds. Department of Veterans Affairs Epilepsy Manual. San Francisco, CA: Epilepsy Centers of Excellence, Department of Veteran Affairs; 2014:120-127.
8. Kwan P, Brodie MJ. Early Identification of refractory epilepsy. N Engl J Med. 2000;342(5):314-319.
9. Mattson RH, Cramer JA, Collins JF, et al. Comparison of carbamazepine, phenobarbital, phenytoin, and primidone in partial and secondarily generalized tonic-clonic seizures. N Eng J Med. 1985;313(3):145-151.
10. Mattson RH, Cramer JA, Collins JF. A comparison of valproate with carbamazepine for the treatment of complex partial seizures and secondarily generalized tonic-clonic seizures in adults. The Department of Veterans Affairs Epilepsy Cooperative Study No. 264 Group. N Eng J Med. 1992;327(11):765-771.
11. Rowan AJ, Ramsay RE, Collins JF, et al; VA Cooperative Study 428 Group. New onset geriatric epilepsy: a randomized study of gabapentin, lamotrigine, and carbamazepine. Neurology. 2005;64(11):1868-1873.
12. Salinsky M, Spencer D, Boudreau E, Ferguson F. Psychogenic nonepileptic seizures in US veterans. Neurology. 2011;77(10):945-950.
13. Salinsky M, Evrard C, Storzbach D, Pugh MJ. Psychiatric comorbidity in veterans with psychogenic seizures. Epilepsy Behav. 2012;25(3):345-349.
14. Salinsky M, Storzbach D, Goy E, Evrard C. Traumatic brain injury and psychogenic seizures in veterans. J Head Trauma Rehabil. 2015;30(1):E65-E70.
15. LaFrance WC Jr, Baird GL, Barry JJ, et al; NES Treatment Trial (NEST-T) Consortium. Multicenter pilot treatment trial for psychogenic nonepileptic seizures: a randomized clinical trial. JAMA Psychiatry. 2014;71(9):997-1005.
16. Wiebe S, Blume WT, Girvin JP, Eliasziw M; Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, control trial for temporal-lobe epilepsy. N Engl J Med. 2001;345(5):311-318.
17. Engel J Jr, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy. Epilepsia. 2003;44(6):741-751.
18. Morris GL III, Gloss D, Buchhalter J, Mack KJ, Nickels K, Harden C. Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy. report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;81(16):1453-1459.
19. Morrell M; RNS System in Epilepsy Study Group. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology. 2011;77(13):1295-1304.
20. Gilliam F, Kuzniecky R, Faught E, Black L, Carpenter G, Schrodt R. Patient-validated content of epilepsy-specific quality-of-life measurement. Epilepsia. 1997;38(2):233-236.
21. Krumholz A. Driving issues in epilepsy: past, present, and future. Epilepsy Curr. 2009;9(2):31-35.
22. Krauss GL, Ampaw L, Krumholz A. Individual state driving restrictions for people with epilepsy in the US. Neurology. 2001;57(10):1780-1785.
23. Krauss GL, Krumholz A, Carter RC, Kaplan P. Risk factors for seizure-related motor vehicle crashes in patients with epilepsy. Neurology. 1999;52(7):1324-1329.
24. Consensus statements, sample statutory provisions, and model regulations regarding driver licensing and epilepsy. American Academy of Neurology. American Epilepsy Society, Epilepsy Foundation of America. Epilepsia. 1994:35(3):696-705.
25. Cavazos, JE. SUDEP and Other Risks of Seizures. In: Husain AM, Tran, TT, eds. VA Epilepsy Manual. San Francisco, CA: Epilepsy Centers of Excellence, Department of Veteran Affairs; 2014:206-209.
26. Tolstykh GP, Cavazos JE. Potential mechanisms of sudden unexpected death in epilepsy. Epilepsy Behav. 2013;26(3):410-414.
27. Gaffield ME, Culwell KR, Lee CR. The use of hormonal contraception among women taking anticonvulsant therapy. Contraception. 2011;83(1):16-29.
28. Harden CL, Pennell PB, Koppel BS, et al; American Academy of Neurology; American Epilepsy Society. Practice parameter update: management issues for women with epilepsy—focus on pregnancy (an evidence-based review): vitamin K, folic acid, blood levels, and breast-feeding: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2009;73(2):142-149.
29. Harden CL, Hopp J, Ting TY, et al; American Academy of Neurology; American Epilepsy Society. Management issues for women with epilepsy-focus on pregnancy (an evidence-based review): 1. Obstetrical complications and change in seizure frequency: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia. 2009;50(5):1229-1236.
30. Artama M, Auvinen A, Raudaskoski T, Isojärvi I, Isojärvi J. Antiepileptic drug use of women with epilepsy and congenital malformations in offspring. Neurology. 2005;64(11):1874-1878.
31. Morrow J, Russell A, Guthrie E, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry. 2006;77(2):193-198.
32. U.S. Food and Drug Administration. Pregnancy and lactation labeling (drugs) final rule. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Published December 3, 2014. Accessed June 27, 2016.
33. Meador KJ, Baker GA, Browning N, et al; NEAD Study Group. Cognitive function at 3 years of age after fetal exposure to antiepileptic drugs. N Engl J Med. 2009;360(16):1597-1605.
34. Meador KH, Baker GA, Browning N, et al; NEAD Study Group. Effects of breastfeeding in children of women taking antiepileptic drugs. Neurology. 2010;75(22):1954-1960.
35. Klein A. The postpartum period in women with epilepsy. Neurol Clin. 2012;30(3):867-875.
36. Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205-228.
37. Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2013;4(suppl 3):S31-S38.
38. Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol. 2007;6(8):693-698.
39. Pugh MJ, Hesdorffer D, Wang CP, et al. Temporal trends in new exposure to antiepileptic drug monotherapy and suicide-related behavior. Neurology. 2013;81(22):1900-1906.
40. Barry JJ, Ettinger AB, Friel P, et al; Advisory Group of the Epilepsy Foundation as part of its Mood Disorder. Consensus statement: the evaluation and treatment of people with epilepsy and affective disorders. Epilepsy Behav. 2008;13(suppl 1):S1-S29.
41. Ottman R, Lipton RB, Ettinger AB, et al. Comorbidities of epilepsy: results from the Epilepsy Comorbidities and Health (EPIC) survey. Epilepsia. 2011;52(2):308-315.
42. Kanner AM. Depression in epilepsy: prevalence, clinical semiology, pathogenic mechanism, and treatment. Biol Psychiatry. 2003;54(3):388-398.
43. Kanner AM. The treatment of depressive disorders in epilepsy: what all neurologists should know. Epilepsia. 2013;54(suppl 1):3-12.
44. Reiter JM, Andrews DJ. A neurobehavioral approach for treatment of complex partial epilepsy: efficacy. Seizure. 2000;9(3):198-203.
45. Pugh MJ, Orman JA, Jaramillo CA, et al. The prevalence of epilepsy and association with traumatic brain Injury in Veterans of the Afghanistan and Iraq Wars. J Head Trauma Rehabil. 2015;30(1):29-37.
46. Hixson JD, Barnes D, Parko K, et al. Patients optimizing epilepsy management via an online community: the POEM Study. Neurology. 2015;85(2):129-136.
47. Winterfeld U, Merlob P, Baud D, et al. Pregnancy outcome following maternal exposure to pregabalin may call for concern. Neurology. 2016;86(24):2251-2257.
Epilepsy is a common and complex neurologic condition marked by recurrent seizures. It has been diagnosed in more than 87,000 veterans enrolled in the VA health care system, 16% of whom have comorbid traumatic brain injury (TBI), and nearly 25% also have posttraumatic stress disorder (PTSD).1 These comorbidities were even more common in Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans: TBI in 52.6% and PTSD in 70.4%. With 25 drugs for seizures and 2 approved devices, treatment of epilepsy can prove challenging to providers whose goal is to balance seizure control and adverse effects (AEs).
Despite the therapeutic armamentarium, about one-third of people with epilepsy have poorly controlled seizures, and an untold number may experience delays in referral to higher levels of epilepsy care or undergo troubling antiepileptic medication AEs and comorbid psychiatric disorders that have profound impacts on quality of life (QOL).
Quality generally has been defined as “providing the right care to the right patient at the right time and in the right way to achieve the best possible results.”2 Much work has been done over the past 2 decades to identify “the right care” for epilepsy patients.3
The American Academy of Neurology (AAN) has developed evidence-based, clinically focused guidelines on numerous topics, including antiepileptic drugs and women’s health, and has developed quality measure sets.4,5 More broadly, the Institute of Medicine (IOM) proposed 13 recommendations, including improving quality of care, establishing epilepsy centers and an epilepsy care network, educating health professionals about epilepsy, and providing education for people with epilepsy and their families.6
Within the VA, health care for veterans with epilepsy is changing in part by the Epilepsy Centers of Excellence (ECoC), established by federal law. The ECoE’s primary missions are to improve quality of and access to epilepsy specialty care to improve the health and well-being of veteran patients with epilepsy and other seizure disorders through integration of clinical care, outreach, research, and education to VA providers and patients.7
The goal of this article is to outline the key elements of quality epilepsy care and make recommendations for providing quality care in the VA health care system.
Diagnosis and Seizure Types
Quality care for veterans with epilepsy begins with the provider reviewing pertinent history and establishing the clinical characteristics of the patient’s seizures and epilepsy. The provider should ask about the first signs of the seizure or warning (aura), the seizure (ictal period), and the period after the seizure (postictal period). Seizure histories from the patient and observers are critical.
The first step is to define whether the patient’s seizures are generalized, that is, start all over the brain at once, or focal, starting in one area of the brain. The patient’s initial sensation at the onset of a seizure (aura) may help localize onset and define focal seizures. For example, déjà vu sensations often point to seizure onset in the mesial temporal lobe and hippocampus. Focal seizures can spread and cause cognitive dysfunction, including aphasia and amnesia, or evolve into a generalized convulsion (tonic-clonic seizure). Many patients present with a generalized tonic-clonic seizure and have had brief focal seizures that were not considered seizures by the patient or by other providers. This seizure type should be clarified by asking specifically about paroxysmal symptoms. For example, brief periods of confusion that are episodic may be focal seizures. In general, focal seizures are stereotyped and may have a feature that helps in establishing the diagnosis. Many temporal lobe seizures are associated with lip smacking behaviors (oral buccal automatisms).
Tonic-clonic seizures may begin without an aura and are generalized from onset. Patients with this type of seizure may have electroencephalogram (EEG) findings that define a generalized abnormality, which consist of frontocentral spike and wave discharges in the EEG. In the VA population, the first generalized tonic-clonic seizure may occur while in the military. Some of these patients have juvenile myoclonic epilepsy, and a history of brief jerks on waking (myoclonus) may have been occurring but not recognized as seizures. The treatment of seizures, in part, depends on whether they begin focally or are generalized at onset.
Often people with epilepsy have multiple seizure types. The types of seizures should be documented and, if possible, corroborated by a witness. Epileptic seizures tend to be stereotyped and of relatively brief duration, usually < 2 minutes. The period after a seizure may be followed by a more prolonged period of neurologic dysfunction that includes confusion and fatigue. These symptoms may be the only indication that the patient has had a seizure.
At each clinic visit, the characteristics of the patient’s seizures should be reviewed and the frequency of seizures documented. A calendar to track seizure frequency is helpful to understand precipitating factors and response to treatment.
The health care provider (HCP) should look for the cause of a patient’s epilepsy. It is important to ask the patient about family history, age of first seizure, occurrence of febrile seizures, developmental history, past history of meningitis or encephalitis, history of childhood seizures or spells, and history of brain lesions, including tumors, strokes, or TBI. Most patients with epilepsy do not have a clear cause for their epilepsy, but the cause may be clarified with EEG and magnetic resonance imaging (MRI) testing.
EEG and Brain Imaging
All patients with epilepsy should be evaluated with an EEG, and for those with focal epilepsy or undefined epilepsy, with an imaging study of the brain, preferably an MRI. These results should be reviewed at each visit. The EEG may show focal features that are related to neurophysiologic dysfunction, such as slowing that is not definitely epileptiform in character, or show focal spike or sharp waves that are epileptiform in character. Generalized abnormalities may include generalized slowing that is not an epileptiform feature or frontocentral spike wave patterns that are epileptiform in character. The EEG cannot rule out epilepsy, but can rule in the likelihood of epilepsy when definite epileptiform features are present.
Brain imaging can define many conditions that can cause focal epilepsy, and an MRI is more sensitive for defining a number of these conditions (cavernous angiomas, hippocampal sclerosis, developmental migration disorders, and low-grade neoplasms). Significant trauma with signal abnormalities to suggest prior bleeding predispose to epilepsy. When patients are refractory to medical therapy and have imaging findings concordant with EEG onset of seizures, then surgery can be a better treatment.
Adverse Effects
Broad-spectrum drug treatments are efficacious for either generalized or focal seizures, whereas narrow-spectrum treatments are most efficacious for focal seizures (Table 1). The choice of a seizure medication is based on the patient’s seizure type(s) and other comorbid conditions.7 For example, a patient with epilepsy and migraines may do better with a seizure medication that also is used for migraine prophylaxis (valproate or topiramate). In general, seizure control is unlikely to be achieved if patients fail the first 2 medications tried.8 Treating with > 1 medication may improve seizure control but may increase AEs. A review of current seizure medications and their AEs can be found on the ECoE website (http://www.epilepsy.va.gov/Provider_Education.asp).
In VA cooperative studies that evaluated seizure medications, the most common reason for discontinuing a drug was the combination of ineffectiveness and AEs.9-11 Addressing AEs is a quality measure for the care of patients with epilepsy. Adverse effects may be dose dependent or idiosyncratic (rashes). Drug levels may help in determining dose-dependent AEs; for example, diplopia with carbamazepine levels above 10 μg/mL. Each patient may have susceptibility to medication AEs that do not exactly match therapeutic levels. When patients have AEs, a reduction in dose or trial of an alternative medication is advised.
Uncontrollable Epilepsy
About one-third of people with epilepsy have uncontrolled seizures, known as medically intractable epilepsy, which may be identified early in their clinical course by failure of the first 2 tolerated medications.8 Patients should be referred to an epilepsy center so their epilepsy can be defined by video EEG monitoring to capture seizures. Unfortunately, in the VA system, this route is often delayed, and patients may not be diagnosed appropriately for years.12 Some of these patients may be considered treatment failures because the right medications were not tried (eg, generalized epilepsy that is treated with narrow-spectrum seizure medications). Juvenile myoclonic epilepsy often may not be controlled by phenytoin or carbamazepine, but valproate, lamotrigine, levetiracetam, and zonisamide may be more effective.
Other patients may not have epilepsy but have psychogenic nonepileptic seizures (PNES). These behavioral seizures do not have an EEG epileptiform correlate. About 25% of patients who undergo prolonged video EEG monitoring have PNES, and seizure medications do not treat these events.12 A smaller percentage of patients have both epileptic and nonepileptic seizures (5%-15%). Psychogenic nonepileptic seizures often occur within the context of traumatic exposure(s) or previous physical or sexual abuse.
In the VA population, PNES is more often associated with PTSD or head trauma history than in patients with epilepsy.13,14 To confirm the diagnosis of PNES, video-EEG capture of the patient’s seizures is required. Because of the increased number of combat veterans with TBI and PTSD, the diagnosis of epilepsy may be difficult without video-EEG monitoring. Management consists of addressing the underlying conversion disorder and recognition and treatment of comorbidities, such as mood, anxiety, personality, or PTSD. Recently, cognitive behavioral-informed psychotherapy (CB-ip) has been shown to be effective in patients with PNES and is available through the VA national telemental health center and at some ECoE sites.15
If a patient with uncontrolled epilepsy has focal seizures, surgical therapy is more likely to result in seizure control than will medical therapy.16,17 This is especially true when other testing, including MRI, positron emission tomography, and neuropsychiatric evaluation, point to a concordance of localization. These patients should be evaluated in a center that can provide surgical therapy and if necessary also record seizures with invasive techniques using electrodes placed directly over the cortex or into the brain to sample deeper structures like the hippocampus or amygdala. Patients who are refractory should be considered for reevaluation every 2 years by a comprehensive epilepsy center.
Unfortunately, some patients have seizures that begin in eloquent cortex, which if removed, leads to undesirable neurologic loss or multifocal seizure onset. In these patients, seizure frequency can be reduced by vagus nerve stimulation or intracranial responsive neurostimulation.18,19
Safety
Epilepsy has inherent risks for injury. Patients and their families often need to be informed about risks and risky behaviors to avoid. A frank discussion about safety is prudent. What to do for the patient during a seizure should be addressed. For convulsive seizures: Protect the patient from injury by placing something soft between the patient’s head and the floor, keep the patient on his or her side; do not restrain the patient or put anything in the mouth; stay calm and time the seizure; as the patient gains consciousness, talk to the patient and be reassuring. For nonconvulsive seizures: Stay with the patient; time the seizure; gently guide the patient away from dangerous situations like streets or stairs; stay with the patient until he or she is back to normal, and reassure the patient.
Driving
People with epilepsy identify driving as one of their major concerns; therefore, it is important for HCPs to properly counsel patients with seizure disorders and their families about driving (Figure).20 In general people with controlled seizures are permitted to drive in every state in the U.S., but people with uncontrolled seizures are restricted from licensure. Despite the desire and necessity to drive for many individuals with epilepsy, seizures while driving pose risks for crashes, which may result in property damage, injuries, and death.21 Factors, such as duration of seizure freedom, help predict the risk for crashes. The legal rules for determining control and administering restrictions are a complex mix of federal and state laws, regulations, and local practices, which vary widely across the country.21,22 The standards also change over time; updated information is available from local state authorities and on good informational sites, such as those of the Epilepsy Foundation.
The key standard for determining accident risks is the seizure free interval, which is the duration of time a person with epilepsy has been seizure-free.21-23 In the U.S., the accepted period for seizure freedom varies from about 3 months to 12 months, depending on individual state rules.24
California, Delaware, Nevada, New Jersey, Oregon, and Pennsylvania require mandatory reporting. Generally physician groups in the U.S. and elsewhere oppose such mandatory reporting, because of the concern that their patients will not report their seizures, and thus may not receive appropriate treatment. Indeed, patients with epilepsy often do not tell physicians about their seizures, fearing loss of driving privileges and other social consequences.21,23 Providers should make an effort to determine seizure frequency and whether the patient is being truthful. This information then provides a background for the provider to discuss driving issues.
Injury
People with epilepsy are susceptible to injury during a seizure and need to be counseled regarding safety, particularly when seizures are not well controlled. Hazardous situations include being near stoves or cooking, bathing alone, swimming alone, working at heights without a safety harness, and using power tools.26
Sudden Unexplained Death
Patients with recurrent seizures have an increased risk for accidental fatality and for sudden unexplained death in epilepsy (SUDEP), which accounts for up to 17% of all deaths in people with epilepsy. The risk for sudden death from recurrent seizures increases 2.3 times compared with the risk in the general population.25 A SUDEP is an unexpected death in a person who has epilepsy with no other obvious cause of death.26 Because increased seizure frequency, the presence of tonic-clonic seizures, and other accidental risks of seizures are associated with SUDEP, the subject should be discussed with patients and their families, to encourage adherence to treatment. Epileptologists also discuss these risks with patients and their families when surgical interventions are being considered. The potential risks for injury or SUDEP may offset the surgical risks when pursuing a potentially curative epilepsy procedure.
Women of Childbearing Age
In January 2015, the ECoE started a women veterans epilepsy workgroup with the goal of improving clinical care within the VAHCS to provide education to patients, family members, and VA health care providers about the care of women with epilepsy.
Providers need to be aware that seizure medications that induce certain hepatic enzymes can lead to hormonal contraceptive failure (Table 2).27 Preconception folic acid supplementation (with at least 0.4 mg) should be considered, because it may reduce the risk of major congenital malformations.28 The goal of epilepsy management prior to conception is to maximize seizure control with the optimal seizure medication to avoid the need to make changes during the pregnancy.
During pregnancy, the volume of distribution increases and seizure medication metabolism may change requiring dose adjustment. The best predictor of seizure frequency during pregnancy is a woman’s epilepsy pattern prior to conception. Seizure freedom for 9 months prior to conception is associated with a 84% to 92% likelihood of seizure freedom throughout the pregnancy.29
International seizure medication pregnancy registries have provided valuable information regarding the risk of major congenital malformation (MCM) of development, which seems to be a consequence of seizure medication therapy and not epilepsy itself. The risk of MCM associated with seizure medication therapy is about 4% to 5% compared with 1.5% to 3% in the general population.30,31 A seizure medication table that supplements the existing VA ECoE information specifically addresses women’s issues with the recognition that recent revisions to the teratogenicity classification have been made by the FDA (Table 2).32 If possible, valproate should be avoided during pregnancy due to its higher rate of MCM and impact on neurocognitive function.33 Obstetrical input is essential in arranging routine prenatal fetal testing. Although women with epilepsy do not have a substantially increased risk of undergoing a cesarean section, delivery in a hospital obstetric unit is advised.
Postpartum women veterans with epilepsy should be encouraged to breast feed since the potential benefits seem to outweigh any established risk of seizure medication exposure to the infant. No relative impact on cognition was found in breastfed infants exposed to a variety of seizure medications.34 Following delivery, vigilance is needed to monitor for sleep deprivation, postpartum depression, and the safe care of the infant.35 Care of women with epilepsy does not end with pregnancy planning, additional important topics include psychiatric comorbidities, catamenial epilepsy, and bone health, which are unique to women veterans with epilepsy.
Identifying Psychiatric Conditions
People with epilepsy have a number of psychiatric comorbidities. Suicide and suicide attempts are 6 to 25 times more common in patients with temporal lobe epilepsy compared with those in the general population.36-38 Although the FDA identified all seizure medications as potential contributors to suicide risk, a recent longitudinal study of suicidal ideation and attempt found that those who received seizure medications were more likely to have suicidal ideation and attempt than those who did not received seizure medications, suggesting that medication may relate to baseline depression or suicidal ideation.39 When seeing patients with epilepsy, screening for suicidal ideation is good practice.
Depression and anxiety disorders are the most common psychiatric comorbidities in people with epilepsy.40,41 About half of people with epilepsy have symptoms of depression, and 40% have anxiety.42 Depression often precedes the diagnosis of epilepsy, and anxiety often is present and related to the fear of having seizures and of social embarrassment.43 People with epilepsy may not self-report these symptoms if not asked directly. Identification of comorbid depression and anxiety should lead to appropriate treatment. The CB-ip being used for PNES also is being used for treatment of epilepsy and its comorbidities.44
Mild traumatic brain injury (mTBI) has a small increased risk of epilepsy.45 Veterans with mTBI that occurs in the context of blasts are set up for the development of PTSD. These veterans may have other mild cognitive symptoms that can be confused with seizures. Furthermore, mTBI and PNES often occur together, more so than do mTBI and epileptic seizures.14 Video-EEG monitoring may be warranted for these patients.
Education and Self-Management
The IOM report on epilepsy identified patient and family education as essential for better epilepsy care.6 Providers should help educate patients about their epilepsy and refer them to resources available online (Table 3). A continuing exchange about their condition and treatment with seizure medications should occur with each visit. People with epilepsy should also receive guidance regarding how to manage their epilepsy and day-to-day issues. Referring, patients to social workers, psychologists, vocational rehabilitation services, and support groups can enhance a patient’s QOL.3,6 The stigma of epilepsy is another burden that can be diminished by attending support groups. Recently, being a part of an online patient community of veterans was found to improve self-management.46
Conclusion
People with epilepsy have many issues that are unique to the condition and, in part, are related to the unpredictable occurrence of seizures and loss of function. Ideally, seizure control provides a normal lifestyle; however, some mood and anxiety comorbidities may persist despite seizure control. Care in the VA system includes access to 16 sites that have programs dedicated to treating veterans with epilepsy and many more consortium sites that interact with the ECoE to provide high-quality patient care (http:\\www.epilepsy.va.gov). The ECoE also provides a readily available resource to optimally manage veterans with epilepsy. Attention to the issues addressed in this article will promote quality care for veterans with epilepsy.
Epilepsy is a common and complex neurologic condition marked by recurrent seizures. It has been diagnosed in more than 87,000 veterans enrolled in the VA health care system, 16% of whom have comorbid traumatic brain injury (TBI), and nearly 25% also have posttraumatic stress disorder (PTSD).1 These comorbidities were even more common in Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans: TBI in 52.6% and PTSD in 70.4%. With 25 drugs for seizures and 2 approved devices, treatment of epilepsy can prove challenging to providers whose goal is to balance seizure control and adverse effects (AEs).
Despite the therapeutic armamentarium, about one-third of people with epilepsy have poorly controlled seizures, and an untold number may experience delays in referral to higher levels of epilepsy care or undergo troubling antiepileptic medication AEs and comorbid psychiatric disorders that have profound impacts on quality of life (QOL).
Quality generally has been defined as “providing the right care to the right patient at the right time and in the right way to achieve the best possible results.”2 Much work has been done over the past 2 decades to identify “the right care” for epilepsy patients.3
The American Academy of Neurology (AAN) has developed evidence-based, clinically focused guidelines on numerous topics, including antiepileptic drugs and women’s health, and has developed quality measure sets.4,5 More broadly, the Institute of Medicine (IOM) proposed 13 recommendations, including improving quality of care, establishing epilepsy centers and an epilepsy care network, educating health professionals about epilepsy, and providing education for people with epilepsy and their families.6
Within the VA, health care for veterans with epilepsy is changing in part by the Epilepsy Centers of Excellence (ECoC), established by federal law. The ECoE’s primary missions are to improve quality of and access to epilepsy specialty care to improve the health and well-being of veteran patients with epilepsy and other seizure disorders through integration of clinical care, outreach, research, and education to VA providers and patients.7
The goal of this article is to outline the key elements of quality epilepsy care and make recommendations for providing quality care in the VA health care system.
Diagnosis and Seizure Types
Quality care for veterans with epilepsy begins with the provider reviewing pertinent history and establishing the clinical characteristics of the patient’s seizures and epilepsy. The provider should ask about the first signs of the seizure or warning (aura), the seizure (ictal period), and the period after the seizure (postictal period). Seizure histories from the patient and observers are critical.
The first step is to define whether the patient’s seizures are generalized, that is, start all over the brain at once, or focal, starting in one area of the brain. The patient’s initial sensation at the onset of a seizure (aura) may help localize onset and define focal seizures. For example, déjà vu sensations often point to seizure onset in the mesial temporal lobe and hippocampus. Focal seizures can spread and cause cognitive dysfunction, including aphasia and amnesia, or evolve into a generalized convulsion (tonic-clonic seizure). Many patients present with a generalized tonic-clonic seizure and have had brief focal seizures that were not considered seizures by the patient or by other providers. This seizure type should be clarified by asking specifically about paroxysmal symptoms. For example, brief periods of confusion that are episodic may be focal seizures. In general, focal seizures are stereotyped and may have a feature that helps in establishing the diagnosis. Many temporal lobe seizures are associated with lip smacking behaviors (oral buccal automatisms).
Tonic-clonic seizures may begin without an aura and are generalized from onset. Patients with this type of seizure may have electroencephalogram (EEG) findings that define a generalized abnormality, which consist of frontocentral spike and wave discharges in the EEG. In the VA population, the first generalized tonic-clonic seizure may occur while in the military. Some of these patients have juvenile myoclonic epilepsy, and a history of brief jerks on waking (myoclonus) may have been occurring but not recognized as seizures. The treatment of seizures, in part, depends on whether they begin focally or are generalized at onset.
Often people with epilepsy have multiple seizure types. The types of seizures should be documented and, if possible, corroborated by a witness. Epileptic seizures tend to be stereotyped and of relatively brief duration, usually < 2 minutes. The period after a seizure may be followed by a more prolonged period of neurologic dysfunction that includes confusion and fatigue. These symptoms may be the only indication that the patient has had a seizure.
At each clinic visit, the characteristics of the patient’s seizures should be reviewed and the frequency of seizures documented. A calendar to track seizure frequency is helpful to understand precipitating factors and response to treatment.
The health care provider (HCP) should look for the cause of a patient’s epilepsy. It is important to ask the patient about family history, age of first seizure, occurrence of febrile seizures, developmental history, past history of meningitis or encephalitis, history of childhood seizures or spells, and history of brain lesions, including tumors, strokes, or TBI. Most patients with epilepsy do not have a clear cause for their epilepsy, but the cause may be clarified with EEG and magnetic resonance imaging (MRI) testing.
EEG and Brain Imaging
All patients with epilepsy should be evaluated with an EEG, and for those with focal epilepsy or undefined epilepsy, with an imaging study of the brain, preferably an MRI. These results should be reviewed at each visit. The EEG may show focal features that are related to neurophysiologic dysfunction, such as slowing that is not definitely epileptiform in character, or show focal spike or sharp waves that are epileptiform in character. Generalized abnormalities may include generalized slowing that is not an epileptiform feature or frontocentral spike wave patterns that are epileptiform in character. The EEG cannot rule out epilepsy, but can rule in the likelihood of epilepsy when definite epileptiform features are present.
Brain imaging can define many conditions that can cause focal epilepsy, and an MRI is more sensitive for defining a number of these conditions (cavernous angiomas, hippocampal sclerosis, developmental migration disorders, and low-grade neoplasms). Significant trauma with signal abnormalities to suggest prior bleeding predispose to epilepsy. When patients are refractory to medical therapy and have imaging findings concordant with EEG onset of seizures, then surgery can be a better treatment.
Adverse Effects
Broad-spectrum drug treatments are efficacious for either generalized or focal seizures, whereas narrow-spectrum treatments are most efficacious for focal seizures (Table 1). The choice of a seizure medication is based on the patient’s seizure type(s) and other comorbid conditions.7 For example, a patient with epilepsy and migraines may do better with a seizure medication that also is used for migraine prophylaxis (valproate or topiramate). In general, seizure control is unlikely to be achieved if patients fail the first 2 medications tried.8 Treating with > 1 medication may improve seizure control but may increase AEs. A review of current seizure medications and their AEs can be found on the ECoE website (http://www.epilepsy.va.gov/Provider_Education.asp).
In VA cooperative studies that evaluated seizure medications, the most common reason for discontinuing a drug was the combination of ineffectiveness and AEs.9-11 Addressing AEs is a quality measure for the care of patients with epilepsy. Adverse effects may be dose dependent or idiosyncratic (rashes). Drug levels may help in determining dose-dependent AEs; for example, diplopia with carbamazepine levels above 10 μg/mL. Each patient may have susceptibility to medication AEs that do not exactly match therapeutic levels. When patients have AEs, a reduction in dose or trial of an alternative medication is advised.
Uncontrollable Epilepsy
About one-third of people with epilepsy have uncontrolled seizures, known as medically intractable epilepsy, which may be identified early in their clinical course by failure of the first 2 tolerated medications.8 Patients should be referred to an epilepsy center so their epilepsy can be defined by video EEG monitoring to capture seizures. Unfortunately, in the VA system, this route is often delayed, and patients may not be diagnosed appropriately for years.12 Some of these patients may be considered treatment failures because the right medications were not tried (eg, generalized epilepsy that is treated with narrow-spectrum seizure medications). Juvenile myoclonic epilepsy often may not be controlled by phenytoin or carbamazepine, but valproate, lamotrigine, levetiracetam, and zonisamide may be more effective.
Other patients may not have epilepsy but have psychogenic nonepileptic seizures (PNES). These behavioral seizures do not have an EEG epileptiform correlate. About 25% of patients who undergo prolonged video EEG monitoring have PNES, and seizure medications do not treat these events.12 A smaller percentage of patients have both epileptic and nonepileptic seizures (5%-15%). Psychogenic nonepileptic seizures often occur within the context of traumatic exposure(s) or previous physical or sexual abuse.
In the VA population, PNES is more often associated with PTSD or head trauma history than in patients with epilepsy.13,14 To confirm the diagnosis of PNES, video-EEG capture of the patient’s seizures is required. Because of the increased number of combat veterans with TBI and PTSD, the diagnosis of epilepsy may be difficult without video-EEG monitoring. Management consists of addressing the underlying conversion disorder and recognition and treatment of comorbidities, such as mood, anxiety, personality, or PTSD. Recently, cognitive behavioral-informed psychotherapy (CB-ip) has been shown to be effective in patients with PNES and is available through the VA national telemental health center and at some ECoE sites.15
If a patient with uncontrolled epilepsy has focal seizures, surgical therapy is more likely to result in seizure control than will medical therapy.16,17 This is especially true when other testing, including MRI, positron emission tomography, and neuropsychiatric evaluation, point to a concordance of localization. These patients should be evaluated in a center that can provide surgical therapy and if necessary also record seizures with invasive techniques using electrodes placed directly over the cortex or into the brain to sample deeper structures like the hippocampus or amygdala. Patients who are refractory should be considered for reevaluation every 2 years by a comprehensive epilepsy center.
Unfortunately, some patients have seizures that begin in eloquent cortex, which if removed, leads to undesirable neurologic loss or multifocal seizure onset. In these patients, seizure frequency can be reduced by vagus nerve stimulation or intracranial responsive neurostimulation.18,19
Safety
Epilepsy has inherent risks for injury. Patients and their families often need to be informed about risks and risky behaviors to avoid. A frank discussion about safety is prudent. What to do for the patient during a seizure should be addressed. For convulsive seizures: Protect the patient from injury by placing something soft between the patient’s head and the floor, keep the patient on his or her side; do not restrain the patient or put anything in the mouth; stay calm and time the seizure; as the patient gains consciousness, talk to the patient and be reassuring. For nonconvulsive seizures: Stay with the patient; time the seizure; gently guide the patient away from dangerous situations like streets or stairs; stay with the patient until he or she is back to normal, and reassure the patient.
Driving
People with epilepsy identify driving as one of their major concerns; therefore, it is important for HCPs to properly counsel patients with seizure disorders and their families about driving (Figure).20 In general people with controlled seizures are permitted to drive in every state in the U.S., but people with uncontrolled seizures are restricted from licensure. Despite the desire and necessity to drive for many individuals with epilepsy, seizures while driving pose risks for crashes, which may result in property damage, injuries, and death.21 Factors, such as duration of seizure freedom, help predict the risk for crashes. The legal rules for determining control and administering restrictions are a complex mix of federal and state laws, regulations, and local practices, which vary widely across the country.21,22 The standards also change over time; updated information is available from local state authorities and on good informational sites, such as those of the Epilepsy Foundation.
The key standard for determining accident risks is the seizure free interval, which is the duration of time a person with epilepsy has been seizure-free.21-23 In the U.S., the accepted period for seizure freedom varies from about 3 months to 12 months, depending on individual state rules.24
California, Delaware, Nevada, New Jersey, Oregon, and Pennsylvania require mandatory reporting. Generally physician groups in the U.S. and elsewhere oppose such mandatory reporting, because of the concern that their patients will not report their seizures, and thus may not receive appropriate treatment. Indeed, patients with epilepsy often do not tell physicians about their seizures, fearing loss of driving privileges and other social consequences.21,23 Providers should make an effort to determine seizure frequency and whether the patient is being truthful. This information then provides a background for the provider to discuss driving issues.
Injury
People with epilepsy are susceptible to injury during a seizure and need to be counseled regarding safety, particularly when seizures are not well controlled. Hazardous situations include being near stoves or cooking, bathing alone, swimming alone, working at heights without a safety harness, and using power tools.26
Sudden Unexplained Death
Patients with recurrent seizures have an increased risk for accidental fatality and for sudden unexplained death in epilepsy (SUDEP), which accounts for up to 17% of all deaths in people with epilepsy. The risk for sudden death from recurrent seizures increases 2.3 times compared with the risk in the general population.25 A SUDEP is an unexpected death in a person who has epilepsy with no other obvious cause of death.26 Because increased seizure frequency, the presence of tonic-clonic seizures, and other accidental risks of seizures are associated with SUDEP, the subject should be discussed with patients and their families, to encourage adherence to treatment. Epileptologists also discuss these risks with patients and their families when surgical interventions are being considered. The potential risks for injury or SUDEP may offset the surgical risks when pursuing a potentially curative epilepsy procedure.
Women of Childbearing Age
In January 2015, the ECoE started a women veterans epilepsy workgroup with the goal of improving clinical care within the VAHCS to provide education to patients, family members, and VA health care providers about the care of women with epilepsy.
Providers need to be aware that seizure medications that induce certain hepatic enzymes can lead to hormonal contraceptive failure (Table 2).27 Preconception folic acid supplementation (with at least 0.4 mg) should be considered, because it may reduce the risk of major congenital malformations.28 The goal of epilepsy management prior to conception is to maximize seizure control with the optimal seizure medication to avoid the need to make changes during the pregnancy.
During pregnancy, the volume of distribution increases and seizure medication metabolism may change requiring dose adjustment. The best predictor of seizure frequency during pregnancy is a woman’s epilepsy pattern prior to conception. Seizure freedom for 9 months prior to conception is associated with a 84% to 92% likelihood of seizure freedom throughout the pregnancy.29
International seizure medication pregnancy registries have provided valuable information regarding the risk of major congenital malformation (MCM) of development, which seems to be a consequence of seizure medication therapy and not epilepsy itself. The risk of MCM associated with seizure medication therapy is about 4% to 5% compared with 1.5% to 3% in the general population.30,31 A seizure medication table that supplements the existing VA ECoE information specifically addresses women’s issues with the recognition that recent revisions to the teratogenicity classification have been made by the FDA (Table 2).32 If possible, valproate should be avoided during pregnancy due to its higher rate of MCM and impact on neurocognitive function.33 Obstetrical input is essential in arranging routine prenatal fetal testing. Although women with epilepsy do not have a substantially increased risk of undergoing a cesarean section, delivery in a hospital obstetric unit is advised.
Postpartum women veterans with epilepsy should be encouraged to breast feed since the potential benefits seem to outweigh any established risk of seizure medication exposure to the infant. No relative impact on cognition was found in breastfed infants exposed to a variety of seizure medications.34 Following delivery, vigilance is needed to monitor for sleep deprivation, postpartum depression, and the safe care of the infant.35 Care of women with epilepsy does not end with pregnancy planning, additional important topics include psychiatric comorbidities, catamenial epilepsy, and bone health, which are unique to women veterans with epilepsy.
Identifying Psychiatric Conditions
People with epilepsy have a number of psychiatric comorbidities. Suicide and suicide attempts are 6 to 25 times more common in patients with temporal lobe epilepsy compared with those in the general population.36-38 Although the FDA identified all seizure medications as potential contributors to suicide risk, a recent longitudinal study of suicidal ideation and attempt found that those who received seizure medications were more likely to have suicidal ideation and attempt than those who did not received seizure medications, suggesting that medication may relate to baseline depression or suicidal ideation.39 When seeing patients with epilepsy, screening for suicidal ideation is good practice.
Depression and anxiety disorders are the most common psychiatric comorbidities in people with epilepsy.40,41 About half of people with epilepsy have symptoms of depression, and 40% have anxiety.42 Depression often precedes the diagnosis of epilepsy, and anxiety often is present and related to the fear of having seizures and of social embarrassment.43 People with epilepsy may not self-report these symptoms if not asked directly. Identification of comorbid depression and anxiety should lead to appropriate treatment. The CB-ip being used for PNES also is being used for treatment of epilepsy and its comorbidities.44
Mild traumatic brain injury (mTBI) has a small increased risk of epilepsy.45 Veterans with mTBI that occurs in the context of blasts are set up for the development of PTSD. These veterans may have other mild cognitive symptoms that can be confused with seizures. Furthermore, mTBI and PNES often occur together, more so than do mTBI and epileptic seizures.14 Video-EEG monitoring may be warranted for these patients.
Education and Self-Management
The IOM report on epilepsy identified patient and family education as essential for better epilepsy care.6 Providers should help educate patients about their epilepsy and refer them to resources available online (Table 3). A continuing exchange about their condition and treatment with seizure medications should occur with each visit. People with epilepsy should also receive guidance regarding how to manage their epilepsy and day-to-day issues. Referring, patients to social workers, psychologists, vocational rehabilitation services, and support groups can enhance a patient’s QOL.3,6 The stigma of epilepsy is another burden that can be diminished by attending support groups. Recently, being a part of an online patient community of veterans was found to improve self-management.46
Conclusion
People with epilepsy have many issues that are unique to the condition and, in part, are related to the unpredictable occurrence of seizures and loss of function. Ideally, seizure control provides a normal lifestyle; however, some mood and anxiety comorbidities may persist despite seizure control. Care in the VA system includes access to 16 sites that have programs dedicated to treating veterans with epilepsy and many more consortium sites that interact with the ECoE to provide high-quality patient care (http:\\www.epilepsy.va.gov). The ECoE also provides a readily available resource to optimally manage veterans with epilepsy. Attention to the issues addressed in this article will promote quality care for veterans with epilepsy.
1. Rehman R, Kelly P, Husain AM, Tran TT. Characteristics of veterans diagnosed with seizures within Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762.
2. National Committee for Quality Assurance (NCQA). The essential guide to health care quality. https://www.ncqa.org/Portals/0/Publications/Resource%20Library/NCQA_Primer_web.pdf. Accessed August 9, 2016.
3. Pugh MJ, Berlowitz DR, Montouris GB, et al. What constitutes high quality of care for adults with epilepsy? Neurology. 2007;69(21):2020-2027.
4. Fountain NB, Van Ness PC, Swain-Eng R, Tonn S, Bever CT Jr; American Academy of Neurology Epilepsy Measure Development Panel and the American Medical Association-Convened Physician Consortium for Performance Improvement Independent Measure Development Process. Quality improvement in neurology: AAN epilepsy quality measures: report of the Quality Measurement and Reporting Subcommittee of the American Academy of Neurology. Neurology. 2011;76(1):94-99.
5. Fountain NB, Van Ness PC, Bennett A, et al. Quality improvement in neurology: epilepsy update quality measurement set. Neurology. 2015;84(14):1483-1487.
6. England MJ, Liverman CT, Schultz AM, Strawbridge LM, eds; Committee on the Public Health Dimensions of the Epilepsies, Board on Health Sciences Policy, Institute of Medicine. Epilepsy Across the Spectrum: Promoting Health and Understanding. Washington, DC: The National Academies Press; 2012.
7. Tortorice K, Rutecki P. Principles of Treatment. In: Hussain, AM, Tran TT, eds. Department of Veterans Affairs Epilepsy Manual. San Francisco, CA: Epilepsy Centers of Excellence, Department of Veteran Affairs; 2014:120-127.
8. Kwan P, Brodie MJ. Early Identification of refractory epilepsy. N Engl J Med. 2000;342(5):314-319.
9. Mattson RH, Cramer JA, Collins JF, et al. Comparison of carbamazepine, phenobarbital, phenytoin, and primidone in partial and secondarily generalized tonic-clonic seizures. N Eng J Med. 1985;313(3):145-151.
10. Mattson RH, Cramer JA, Collins JF. A comparison of valproate with carbamazepine for the treatment of complex partial seizures and secondarily generalized tonic-clonic seizures in adults. The Department of Veterans Affairs Epilepsy Cooperative Study No. 264 Group. N Eng J Med. 1992;327(11):765-771.
11. Rowan AJ, Ramsay RE, Collins JF, et al; VA Cooperative Study 428 Group. New onset geriatric epilepsy: a randomized study of gabapentin, lamotrigine, and carbamazepine. Neurology. 2005;64(11):1868-1873.
12. Salinsky M, Spencer D, Boudreau E, Ferguson F. Psychogenic nonepileptic seizures in US veterans. Neurology. 2011;77(10):945-950.
13. Salinsky M, Evrard C, Storzbach D, Pugh MJ. Psychiatric comorbidity in veterans with psychogenic seizures. Epilepsy Behav. 2012;25(3):345-349.
14. Salinsky M, Storzbach D, Goy E, Evrard C. Traumatic brain injury and psychogenic seizures in veterans. J Head Trauma Rehabil. 2015;30(1):E65-E70.
15. LaFrance WC Jr, Baird GL, Barry JJ, et al; NES Treatment Trial (NEST-T) Consortium. Multicenter pilot treatment trial for psychogenic nonepileptic seizures: a randomized clinical trial. JAMA Psychiatry. 2014;71(9):997-1005.
16. Wiebe S, Blume WT, Girvin JP, Eliasziw M; Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, control trial for temporal-lobe epilepsy. N Engl J Med. 2001;345(5):311-318.
17. Engel J Jr, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy. Epilepsia. 2003;44(6):741-751.
18. Morris GL III, Gloss D, Buchhalter J, Mack KJ, Nickels K, Harden C. Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy. report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;81(16):1453-1459.
19. Morrell M; RNS System in Epilepsy Study Group. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology. 2011;77(13):1295-1304.
20. Gilliam F, Kuzniecky R, Faught E, Black L, Carpenter G, Schrodt R. Patient-validated content of epilepsy-specific quality-of-life measurement. Epilepsia. 1997;38(2):233-236.
21. Krumholz A. Driving issues in epilepsy: past, present, and future. Epilepsy Curr. 2009;9(2):31-35.
22. Krauss GL, Ampaw L, Krumholz A. Individual state driving restrictions for people with epilepsy in the US. Neurology. 2001;57(10):1780-1785.
23. Krauss GL, Krumholz A, Carter RC, Kaplan P. Risk factors for seizure-related motor vehicle crashes in patients with epilepsy. Neurology. 1999;52(7):1324-1329.
24. Consensus statements, sample statutory provisions, and model regulations regarding driver licensing and epilepsy. American Academy of Neurology. American Epilepsy Society, Epilepsy Foundation of America. Epilepsia. 1994:35(3):696-705.
25. Cavazos, JE. SUDEP and Other Risks of Seizures. In: Husain AM, Tran, TT, eds. VA Epilepsy Manual. San Francisco, CA: Epilepsy Centers of Excellence, Department of Veteran Affairs; 2014:206-209.
26. Tolstykh GP, Cavazos JE. Potential mechanisms of sudden unexpected death in epilepsy. Epilepsy Behav. 2013;26(3):410-414.
27. Gaffield ME, Culwell KR, Lee CR. The use of hormonal contraception among women taking anticonvulsant therapy. Contraception. 2011;83(1):16-29.
28. Harden CL, Pennell PB, Koppel BS, et al; American Academy of Neurology; American Epilepsy Society. Practice parameter update: management issues for women with epilepsy—focus on pregnancy (an evidence-based review): vitamin K, folic acid, blood levels, and breast-feeding: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2009;73(2):142-149.
29. Harden CL, Hopp J, Ting TY, et al; American Academy of Neurology; American Epilepsy Society. Management issues for women with epilepsy-focus on pregnancy (an evidence-based review): 1. Obstetrical complications and change in seizure frequency: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia. 2009;50(5):1229-1236.
30. Artama M, Auvinen A, Raudaskoski T, Isojärvi I, Isojärvi J. Antiepileptic drug use of women with epilepsy and congenital malformations in offspring. Neurology. 2005;64(11):1874-1878.
31. Morrow J, Russell A, Guthrie E, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry. 2006;77(2):193-198.
32. U.S. Food and Drug Administration. Pregnancy and lactation labeling (drugs) final rule. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Published December 3, 2014. Accessed June 27, 2016.
33. Meador KJ, Baker GA, Browning N, et al; NEAD Study Group. Cognitive function at 3 years of age after fetal exposure to antiepileptic drugs. N Engl J Med. 2009;360(16):1597-1605.
34. Meador KH, Baker GA, Browning N, et al; NEAD Study Group. Effects of breastfeeding in children of women taking antiepileptic drugs. Neurology. 2010;75(22):1954-1960.
35. Klein A. The postpartum period in women with epilepsy. Neurol Clin. 2012;30(3):867-875.
36. Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205-228.
37. Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2013;4(suppl 3):S31-S38.
38. Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol. 2007;6(8):693-698.
39. Pugh MJ, Hesdorffer D, Wang CP, et al. Temporal trends in new exposure to antiepileptic drug monotherapy and suicide-related behavior. Neurology. 2013;81(22):1900-1906.
40. Barry JJ, Ettinger AB, Friel P, et al; Advisory Group of the Epilepsy Foundation as part of its Mood Disorder. Consensus statement: the evaluation and treatment of people with epilepsy and affective disorders. Epilepsy Behav. 2008;13(suppl 1):S1-S29.
41. Ottman R, Lipton RB, Ettinger AB, et al. Comorbidities of epilepsy: results from the Epilepsy Comorbidities and Health (EPIC) survey. Epilepsia. 2011;52(2):308-315.
42. Kanner AM. Depression in epilepsy: prevalence, clinical semiology, pathogenic mechanism, and treatment. Biol Psychiatry. 2003;54(3):388-398.
43. Kanner AM. The treatment of depressive disorders in epilepsy: what all neurologists should know. Epilepsia. 2013;54(suppl 1):3-12.
44. Reiter JM, Andrews DJ. A neurobehavioral approach for treatment of complex partial epilepsy: efficacy. Seizure. 2000;9(3):198-203.
45. Pugh MJ, Orman JA, Jaramillo CA, et al. The prevalence of epilepsy and association with traumatic brain Injury in Veterans of the Afghanistan and Iraq Wars. J Head Trauma Rehabil. 2015;30(1):29-37.
46. Hixson JD, Barnes D, Parko K, et al. Patients optimizing epilepsy management via an online community: the POEM Study. Neurology. 2015;85(2):129-136.
47. Winterfeld U, Merlob P, Baud D, et al. Pregnancy outcome following maternal exposure to pregabalin may call for concern. Neurology. 2016;86(24):2251-2257.
1. Rehman R, Kelly P, Husain AM, Tran TT. Characteristics of veterans diagnosed with seizures within Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762.
2. National Committee for Quality Assurance (NCQA). The essential guide to health care quality. https://www.ncqa.org/Portals/0/Publications/Resource%20Library/NCQA_Primer_web.pdf. Accessed August 9, 2016.
3. Pugh MJ, Berlowitz DR, Montouris GB, et al. What constitutes high quality of care for adults with epilepsy? Neurology. 2007;69(21):2020-2027.
4. Fountain NB, Van Ness PC, Swain-Eng R, Tonn S, Bever CT Jr; American Academy of Neurology Epilepsy Measure Development Panel and the American Medical Association-Convened Physician Consortium for Performance Improvement Independent Measure Development Process. Quality improvement in neurology: AAN epilepsy quality measures: report of the Quality Measurement and Reporting Subcommittee of the American Academy of Neurology. Neurology. 2011;76(1):94-99.
5. Fountain NB, Van Ness PC, Bennett A, et al. Quality improvement in neurology: epilepsy update quality measurement set. Neurology. 2015;84(14):1483-1487.
6. England MJ, Liverman CT, Schultz AM, Strawbridge LM, eds; Committee on the Public Health Dimensions of the Epilepsies, Board on Health Sciences Policy, Institute of Medicine. Epilepsy Across the Spectrum: Promoting Health and Understanding. Washington, DC: The National Academies Press; 2012.
7. Tortorice K, Rutecki P. Principles of Treatment. In: Hussain, AM, Tran TT, eds. Department of Veterans Affairs Epilepsy Manual. San Francisco, CA: Epilepsy Centers of Excellence, Department of Veteran Affairs; 2014:120-127.
8. Kwan P, Brodie MJ. Early Identification of refractory epilepsy. N Engl J Med. 2000;342(5):314-319.
9. Mattson RH, Cramer JA, Collins JF, et al. Comparison of carbamazepine, phenobarbital, phenytoin, and primidone in partial and secondarily generalized tonic-clonic seizures. N Eng J Med. 1985;313(3):145-151.
10. Mattson RH, Cramer JA, Collins JF. A comparison of valproate with carbamazepine for the treatment of complex partial seizures and secondarily generalized tonic-clonic seizures in adults. The Department of Veterans Affairs Epilepsy Cooperative Study No. 264 Group. N Eng J Med. 1992;327(11):765-771.
11. Rowan AJ, Ramsay RE, Collins JF, et al; VA Cooperative Study 428 Group. New onset geriatric epilepsy: a randomized study of gabapentin, lamotrigine, and carbamazepine. Neurology. 2005;64(11):1868-1873.
12. Salinsky M, Spencer D, Boudreau E, Ferguson F. Psychogenic nonepileptic seizures in US veterans. Neurology. 2011;77(10):945-950.
13. Salinsky M, Evrard C, Storzbach D, Pugh MJ. Psychiatric comorbidity in veterans with psychogenic seizures. Epilepsy Behav. 2012;25(3):345-349.
14. Salinsky M, Storzbach D, Goy E, Evrard C. Traumatic brain injury and psychogenic seizures in veterans. J Head Trauma Rehabil. 2015;30(1):E65-E70.
15. LaFrance WC Jr, Baird GL, Barry JJ, et al; NES Treatment Trial (NEST-T) Consortium. Multicenter pilot treatment trial for psychogenic nonepileptic seizures: a randomized clinical trial. JAMA Psychiatry. 2014;71(9):997-1005.
16. Wiebe S, Blume WT, Girvin JP, Eliasziw M; Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, control trial for temporal-lobe epilepsy. N Engl J Med. 2001;345(5):311-318.
17. Engel J Jr, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy. Epilepsia. 2003;44(6):741-751.
18. Morris GL III, Gloss D, Buchhalter J, Mack KJ, Nickels K, Harden C. Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy. report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;81(16):1453-1459.
19. Morrell M; RNS System in Epilepsy Study Group. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology. 2011;77(13):1295-1304.
20. Gilliam F, Kuzniecky R, Faught E, Black L, Carpenter G, Schrodt R. Patient-validated content of epilepsy-specific quality-of-life measurement. Epilepsia. 1997;38(2):233-236.
21. Krumholz A. Driving issues in epilepsy: past, present, and future. Epilepsy Curr. 2009;9(2):31-35.
22. Krauss GL, Ampaw L, Krumholz A. Individual state driving restrictions for people with epilepsy in the US. Neurology. 2001;57(10):1780-1785.
23. Krauss GL, Krumholz A, Carter RC, Kaplan P. Risk factors for seizure-related motor vehicle crashes in patients with epilepsy. Neurology. 1999;52(7):1324-1329.
24. Consensus statements, sample statutory provisions, and model regulations regarding driver licensing and epilepsy. American Academy of Neurology. American Epilepsy Society, Epilepsy Foundation of America. Epilepsia. 1994:35(3):696-705.
25. Cavazos, JE. SUDEP and Other Risks of Seizures. In: Husain AM, Tran, TT, eds. VA Epilepsy Manual. San Francisco, CA: Epilepsy Centers of Excellence, Department of Veteran Affairs; 2014:206-209.
26. Tolstykh GP, Cavazos JE. Potential mechanisms of sudden unexpected death in epilepsy. Epilepsy Behav. 2013;26(3):410-414.
27. Gaffield ME, Culwell KR, Lee CR. The use of hormonal contraception among women taking anticonvulsant therapy. Contraception. 2011;83(1):16-29.
28. Harden CL, Pennell PB, Koppel BS, et al; American Academy of Neurology; American Epilepsy Society. Practice parameter update: management issues for women with epilepsy—focus on pregnancy (an evidence-based review): vitamin K, folic acid, blood levels, and breast-feeding: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2009;73(2):142-149.
29. Harden CL, Hopp J, Ting TY, et al; American Academy of Neurology; American Epilepsy Society. Management issues for women with epilepsy-focus on pregnancy (an evidence-based review): 1. Obstetrical complications and change in seizure frequency: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia. 2009;50(5):1229-1236.
30. Artama M, Auvinen A, Raudaskoski T, Isojärvi I, Isojärvi J. Antiepileptic drug use of women with epilepsy and congenital malformations in offspring. Neurology. 2005;64(11):1874-1878.
31. Morrow J, Russell A, Guthrie E, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry. 2006;77(2):193-198.
32. U.S. Food and Drug Administration. Pregnancy and lactation labeling (drugs) final rule. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Published December 3, 2014. Accessed June 27, 2016.
33. Meador KJ, Baker GA, Browning N, et al; NEAD Study Group. Cognitive function at 3 years of age after fetal exposure to antiepileptic drugs. N Engl J Med. 2009;360(16):1597-1605.
34. Meador KH, Baker GA, Browning N, et al; NEAD Study Group. Effects of breastfeeding in children of women taking antiepileptic drugs. Neurology. 2010;75(22):1954-1960.
35. Klein A. The postpartum period in women with epilepsy. Neurol Clin. 2012;30(3):867-875.
36. Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205-228.
37. Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2013;4(suppl 3):S31-S38.
38. Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol. 2007;6(8):693-698.
39. Pugh MJ, Hesdorffer D, Wang CP, et al. Temporal trends in new exposure to antiepileptic drug monotherapy and suicide-related behavior. Neurology. 2013;81(22):1900-1906.
40. Barry JJ, Ettinger AB, Friel P, et al; Advisory Group of the Epilepsy Foundation as part of its Mood Disorder. Consensus statement: the evaluation and treatment of people with epilepsy and affective disorders. Epilepsy Behav. 2008;13(suppl 1):S1-S29.
41. Ottman R, Lipton RB, Ettinger AB, et al. Comorbidities of epilepsy: results from the Epilepsy Comorbidities and Health (EPIC) survey. Epilepsia. 2011;52(2):308-315.
42. Kanner AM. Depression in epilepsy: prevalence, clinical semiology, pathogenic mechanism, and treatment. Biol Psychiatry. 2003;54(3):388-398.
43. Kanner AM. The treatment of depressive disorders in epilepsy: what all neurologists should know. Epilepsia. 2013;54(suppl 1):3-12.
44. Reiter JM, Andrews DJ. A neurobehavioral approach for treatment of complex partial epilepsy: efficacy. Seizure. 2000;9(3):198-203.
45. Pugh MJ, Orman JA, Jaramillo CA, et al. The prevalence of epilepsy and association with traumatic brain Injury in Veterans of the Afghanistan and Iraq Wars. J Head Trauma Rehabil. 2015;30(1):29-37.
46. Hixson JD, Barnes D, Parko K, et al. Patients optimizing epilepsy management via an online community: the POEM Study. Neurology. 2015;85(2):129-136.
47. Winterfeld U, Merlob P, Baud D, et al. Pregnancy outcome following maternal exposure to pregabalin may call for concern. Neurology. 2016;86(24):2251-2257.