User login
1.04 Common Clinical Diagnoses and Conditions: Altered Mental Status
Introduction
Altered mental status (AMS) is a descriptive term that encompasses a wide spectrum of signs and symptoms, ranging from vague complaints of atypical behavior and irritability, to more specific concerns related to both hyperactive states (such as agitation) and hypoactive states (such as lethargy, depressed levels of responsiveness, and loss of consciousness). AMS may be particularly difficult to recognize in very young children and children with medical complexity. Pediatric hospitalists frequently encounter children with AMS, either as a primary cause for admission or a secondary finding during hospitalization, and therefore they must be knowledgeable about the differential diagnosis and various organ system manifestations that may be involved. Pediatric hospitalists must be able to accurately recognize early signs of AMS, triage acuity, and provide prompt stabilization, which is critical to effective management of patients with this condition.
Knowledge
Pediatric Hospitalists should be able to:
- Compare and contrast the different presentations of AMS, and describe the differential diagnosis associated with each for varying chronological or developmental ages.
- Identify the elements of the Glasgow Coma Scale and discuss the implications of the score or a change in score on management of a child with AMS.
- Discuss the features of the medical history and physical examination that prompt specific diagnostic evaluation, including signs and symptoms that warrant urgent management.
- Compare and contrast different features of toxidromes that may present with AMS.
- Discuss approaches to stabilization of a child with AMS, including evaluation of airway, breathing, circulation, disability, exposure, and intracranial perfusion.
- Define the indications to activate a rapid response, code blue, or other local emergency system for children with AMS.
- Explain indications for hospitalization of children with AMS.
- Summarize the initial approach to management of common conditions presenting with AMS, including but not limited to: seizures, increased intracranial pressure, intracranial hemorrhage, infectious or inflammatory encephalitis, sepsis, shock, hypoglycemia, diabetic ketoacidosis, renal or liver failure, neoplastic syndromes, suspected toxic ingestion, medication overdose, and adverse drug reaction.
- Discuss specific considerations for children with medical complexity presenting with AMS, including those with intellectual disability, impaired communication, epilepsy, dystonia, ventricular shunts, ventilator dependence, enteral feeding tubes, and multiple medications.
- Discuss the mechanisms of action of common medications used for delirium or agitation.
- Discuss the mechanisms of action of medications used for increased intracranial pressure (such as mannitol, 3% hypertonic saline, and others).
- List medications commonly used in the inpatient setting that may cause AMS as a side effect of use or withdrawal of use, such as seizure medications, opioids, benzodiazepines, anti-cholinergic medications, barbiturates, cannabinoids, and others.
- Explain the indications for chemical versus physical restraints, one-to-one supervision, and involvement of hospital security to ensure safety of the patient, family, and staff.
- Describe indications for urgent subspecialist consultation for children with AMS (such as toxicology, rheumatology, neurology, neurosurgery, and others).
- Discuss reasons for transfer to higher level of care, within the institution or elsewhere if pediatric-specific or psychiatric services are not available at the local facility.
- Describe the reasons for ancillary service involvement (such as physical, occupational, speech, feeding, behavioral therapies, and others) and durable medical equipment procurement for children with AMS.
- List criteria for inpatient rehabilitation.
- Discuss indications for involvement of social work, child protective services, or law enforcement for children with AMS.
Skills
Pediatric Hospitalists should be able to:
- Elicit a thorough medical history, attending to a detailed care provider history, past medical history, exposures, medications, and medications in the home.
- Perform a physical exam to elicit signs of AMS, including evaluation of airway, breathing, circulation, psychiatric status, and the central and autonomic nervous system.
- Assign an accurate Glasgow Coma Scale score.
- Identify children with potentially reversible, life-threatening conditions, and promptly provide stabilizing measures, activating code or rapid response teams as indicated.
- Review medication list and note any potentially relevant interactions or adverse effects.
- Direct an appropriate, cost-effective evaluation to identify the cause of AMS and correctly interpret results, including performance of a lumbar puncture as indicated.
- Perform careful reassessments (such as serial neurological exams, Glasgow Coma Scale scoring, and others), identifying indications for adjustment to the plan of care, frequency of monitoring, and type of monitoring indicated.
- Identify and manage children who present with altered mental status secondary to common conditions, such as seizures, increased intracranial pressure, intracranial hemorrhage, infectious or inflammatory encephalitis, sepsis, shock, hypoglycemia, diabetic ketoacidosis, renal or liver failure, neoplastic syndromes, suspected toxic ingestion, medication overdose, and adverse drug reaction.
- Engage consultants, including neurologists, neurosurgeons, neuroradiologists, toxicologists, psychiatrists, and psychologists efficiently and appropriately.
- Coordinate care and communicate effectively with caregivers, primary care providers, and consultants about the mental status at the time of discharge and the transition plan, referring to ancillary or rehabilitation services as appropriate.
Attitudes
Pediatric Hospitalists should be able to:
- Realize responsibility for reporting of iatrogenic etiologies as appropriate.
- Acknowledge the need for effective communication with subspecialty providers, primary care providers, and the patients and the family/caregivers to ensure ongoing support and coordinated care.
- Realize responsibility for effective and compassionate communication with patients/caregivers regarding findings, prognosis, and treatments, accounting for the stresses of hospitalization.
- Collaborate with social work, child protective services, and law enforcement when indicated.
Systems Organization and Improvement
In order to improve efficiency and quality within their organizations, pediatric hospitalists should:
- Work with hospital administration and staff to develop, implement, and assess outcomes of intervention strategies for hospitalized patients with deterioration of mental status to prevent adverse outcomes (such as rapid response, code blue, stroke teams, and others).
- Coordinate educational programs for front-line providers to promote early recognition of AMS.
- Lead, coordinate, or participate in institutional efforts to report and reduce cases of AMS due to iatrogenic causes or adverse effects of medications.
1. Lehman RK, Mink J. Altered mental status. Clin Pediatr Emerg Med. 2008; 9:68-75.
2. Avner JR. Altered states of consciousness. Pediatr Rev. 2006; 27:331-338. https://doi.org/10.1542/pir.27-9-331.
3. Malas N, Brahmbhatt K, McDermott C, Smith A. Ortiz-Aguayo R, Turkel S. Pediatric delirium: Evaluation, management, and special considerations. Curr Psychiatry Rep. 2017;19(9):65. https://doi.org/10.1007/s11920-017-0817-3.
1. Lehman RK, Mink J. Altered mental status. Clin Pediatr Emerg Med. 2008; 9:68-75.
2. Avner JR. Altered states of consciousness. Pediatr Rev. 2006; 27:331-338. https://doi.org/10.1542/pir.27-9-331.
3. Malas N, Brahmbhatt K, McDermott C, Smith A. Ortiz-Aguayo R, Turkel S. Pediatric delirium: Evaluation, management, and special considerations. Curr Psychiatry Rep. 2017;19(9):65. https://doi.org/10.1007/s11920-017-0817-3.
Introduction
Altered mental status (AMS) is a descriptive term that encompasses a wide spectrum of signs and symptoms, ranging from vague complaints of atypical behavior and irritability, to more specific concerns related to both hyperactive states (such as agitation) and hypoactive states (such as lethargy, depressed levels of responsiveness, and loss of consciousness). AMS may be particularly difficult to recognize in very young children and children with medical complexity. Pediatric hospitalists frequently encounter children with AMS, either as a primary cause for admission or a secondary finding during hospitalization, and therefore they must be knowledgeable about the differential diagnosis and various organ system manifestations that may be involved. Pediatric hospitalists must be able to accurately recognize early signs of AMS, triage acuity, and provide prompt stabilization, which is critical to effective management of patients with this condition.
Knowledge
Pediatric Hospitalists should be able to:
- Compare and contrast the different presentations of AMS, and describe the differential diagnosis associated with each for varying chronological or developmental ages.
- Identify the elements of the Glasgow Coma Scale and discuss the implications of the score or a change in score on management of a child with AMS.
- Discuss the features of the medical history and physical examination that prompt specific diagnostic evaluation, including signs and symptoms that warrant urgent management.
- Compare and contrast different features of toxidromes that may present with AMS.
- Discuss approaches to stabilization of a child with AMS, including evaluation of airway, breathing, circulation, disability, exposure, and intracranial perfusion.
- Define the indications to activate a rapid response, code blue, or other local emergency system for children with AMS.
- Explain indications for hospitalization of children with AMS.
- Summarize the initial approach to management of common conditions presenting with AMS, including but not limited to: seizures, increased intracranial pressure, intracranial hemorrhage, infectious or inflammatory encephalitis, sepsis, shock, hypoglycemia, diabetic ketoacidosis, renal or liver failure, neoplastic syndromes, suspected toxic ingestion, medication overdose, and adverse drug reaction.
- Discuss specific considerations for children with medical complexity presenting with AMS, including those with intellectual disability, impaired communication, epilepsy, dystonia, ventricular shunts, ventilator dependence, enteral feeding tubes, and multiple medications.
- Discuss the mechanisms of action of common medications used for delirium or agitation.
- Discuss the mechanisms of action of medications used for increased intracranial pressure (such as mannitol, 3% hypertonic saline, and others).
- List medications commonly used in the inpatient setting that may cause AMS as a side effect of use or withdrawal of use, such as seizure medications, opioids, benzodiazepines, anti-cholinergic medications, barbiturates, cannabinoids, and others.
- Explain the indications for chemical versus physical restraints, one-to-one supervision, and involvement of hospital security to ensure safety of the patient, family, and staff.
- Describe indications for urgent subspecialist consultation for children with AMS (such as toxicology, rheumatology, neurology, neurosurgery, and others).
- Discuss reasons for transfer to higher level of care, within the institution or elsewhere if pediatric-specific or psychiatric services are not available at the local facility.
- Describe the reasons for ancillary service involvement (such as physical, occupational, speech, feeding, behavioral therapies, and others) and durable medical equipment procurement for children with AMS.
- List criteria for inpatient rehabilitation.
- Discuss indications for involvement of social work, child protective services, or law enforcement for children with AMS.
Skills
Pediatric Hospitalists should be able to:
- Elicit a thorough medical history, attending to a detailed care provider history, past medical history, exposures, medications, and medications in the home.
- Perform a physical exam to elicit signs of AMS, including evaluation of airway, breathing, circulation, psychiatric status, and the central and autonomic nervous system.
- Assign an accurate Glasgow Coma Scale score.
- Identify children with potentially reversible, life-threatening conditions, and promptly provide stabilizing measures, activating code or rapid response teams as indicated.
- Review medication list and note any potentially relevant interactions or adverse effects.
- Direct an appropriate, cost-effective evaluation to identify the cause of AMS and correctly interpret results, including performance of a lumbar puncture as indicated.
- Perform careful reassessments (such as serial neurological exams, Glasgow Coma Scale scoring, and others), identifying indications for adjustment to the plan of care, frequency of monitoring, and type of monitoring indicated.
- Identify and manage children who present with altered mental status secondary to common conditions, such as seizures, increased intracranial pressure, intracranial hemorrhage, infectious or inflammatory encephalitis, sepsis, shock, hypoglycemia, diabetic ketoacidosis, renal or liver failure, neoplastic syndromes, suspected toxic ingestion, medication overdose, and adverse drug reaction.
- Engage consultants, including neurologists, neurosurgeons, neuroradiologists, toxicologists, psychiatrists, and psychologists efficiently and appropriately.
- Coordinate care and communicate effectively with caregivers, primary care providers, and consultants about the mental status at the time of discharge and the transition plan, referring to ancillary or rehabilitation services as appropriate.
Attitudes
Pediatric Hospitalists should be able to:
- Realize responsibility for reporting of iatrogenic etiologies as appropriate.
- Acknowledge the need for effective communication with subspecialty providers, primary care providers, and the patients and the family/caregivers to ensure ongoing support and coordinated care.
- Realize responsibility for effective and compassionate communication with patients/caregivers regarding findings, prognosis, and treatments, accounting for the stresses of hospitalization.
- Collaborate with social work, child protective services, and law enforcement when indicated.
Systems Organization and Improvement
In order to improve efficiency and quality within their organizations, pediatric hospitalists should:
- Work with hospital administration and staff to develop, implement, and assess outcomes of intervention strategies for hospitalized patients with deterioration of mental status to prevent adverse outcomes (such as rapid response, code blue, stroke teams, and others).
- Coordinate educational programs for front-line providers to promote early recognition of AMS.
- Lead, coordinate, or participate in institutional efforts to report and reduce cases of AMS due to iatrogenic causes or adverse effects of medications.
1. Lehman RK, Mink J. Altered mental status. Clin Pediatr Emerg Med. 2008; 9:68-75.
2. Avner JR. Altered states of consciousness. Pediatr Rev. 2006; 27:331-338. https://doi.org/10.1542/pir.27-9-331.
3. Malas N, Brahmbhatt K, McDermott C, Smith A. Ortiz-Aguayo R, Turkel S. Pediatric delirium: Evaluation, management, and special considerations. Curr Psychiatry Rep. 2017;19(9):65. https://doi.org/10.1007/s11920-017-0817-3.
Introduction
Altered mental status (AMS) is a descriptive term that encompasses a wide spectrum of signs and symptoms, ranging from vague complaints of atypical behavior and irritability, to more specific concerns related to both hyperactive states (such as agitation) and hypoactive states (such as lethargy, depressed levels of responsiveness, and loss of consciousness). AMS may be particularly difficult to recognize in very young children and children with medical complexity. Pediatric hospitalists frequently encounter children with AMS, either as a primary cause for admission or a secondary finding during hospitalization, and therefore they must be knowledgeable about the differential diagnosis and various organ system manifestations that may be involved. Pediatric hospitalists must be able to accurately recognize early signs of AMS, triage acuity, and provide prompt stabilization, which is critical to effective management of patients with this condition.
Knowledge
Pediatric Hospitalists should be able to:
- Compare and contrast the different presentations of AMS, and describe the differential diagnosis associated with each for varying chronological or developmental ages.
- Identify the elements of the Glasgow Coma Scale and discuss the implications of the score or a change in score on management of a child with AMS.
- Discuss the features of the medical history and physical examination that prompt specific diagnostic evaluation, including signs and symptoms that warrant urgent management.
- Compare and contrast different features of toxidromes that may present with AMS.
- Discuss approaches to stabilization of a child with AMS, including evaluation of airway, breathing, circulation, disability, exposure, and intracranial perfusion.
- Define the indications to activate a rapid response, code blue, or other local emergency system for children with AMS.
- Explain indications for hospitalization of children with AMS.
- Summarize the initial approach to management of common conditions presenting with AMS, including but not limited to: seizures, increased intracranial pressure, intracranial hemorrhage, infectious or inflammatory encephalitis, sepsis, shock, hypoglycemia, diabetic ketoacidosis, renal or liver failure, neoplastic syndromes, suspected toxic ingestion, medication overdose, and adverse drug reaction.
- Discuss specific considerations for children with medical complexity presenting with AMS, including those with intellectual disability, impaired communication, epilepsy, dystonia, ventricular shunts, ventilator dependence, enteral feeding tubes, and multiple medications.
- Discuss the mechanisms of action of common medications used for delirium or agitation.
- Discuss the mechanisms of action of medications used for increased intracranial pressure (such as mannitol, 3% hypertonic saline, and others).
- List medications commonly used in the inpatient setting that may cause AMS as a side effect of use or withdrawal of use, such as seizure medications, opioids, benzodiazepines, anti-cholinergic medications, barbiturates, cannabinoids, and others.
- Explain the indications for chemical versus physical restraints, one-to-one supervision, and involvement of hospital security to ensure safety of the patient, family, and staff.
- Describe indications for urgent subspecialist consultation for children with AMS (such as toxicology, rheumatology, neurology, neurosurgery, and others).
- Discuss reasons for transfer to higher level of care, within the institution or elsewhere if pediatric-specific or psychiatric services are not available at the local facility.
- Describe the reasons for ancillary service involvement (such as physical, occupational, speech, feeding, behavioral therapies, and others) and durable medical equipment procurement for children with AMS.
- List criteria for inpatient rehabilitation.
- Discuss indications for involvement of social work, child protective services, or law enforcement for children with AMS.
Skills
Pediatric Hospitalists should be able to:
- Elicit a thorough medical history, attending to a detailed care provider history, past medical history, exposures, medications, and medications in the home.
- Perform a physical exam to elicit signs of AMS, including evaluation of airway, breathing, circulation, psychiatric status, and the central and autonomic nervous system.
- Assign an accurate Glasgow Coma Scale score.
- Identify children with potentially reversible, life-threatening conditions, and promptly provide stabilizing measures, activating code or rapid response teams as indicated.
- Review medication list and note any potentially relevant interactions or adverse effects.
- Direct an appropriate, cost-effective evaluation to identify the cause of AMS and correctly interpret results, including performance of a lumbar puncture as indicated.
- Perform careful reassessments (such as serial neurological exams, Glasgow Coma Scale scoring, and others), identifying indications for adjustment to the plan of care, frequency of monitoring, and type of monitoring indicated.
- Identify and manage children who present with altered mental status secondary to common conditions, such as seizures, increased intracranial pressure, intracranial hemorrhage, infectious or inflammatory encephalitis, sepsis, shock, hypoglycemia, diabetic ketoacidosis, renal or liver failure, neoplastic syndromes, suspected toxic ingestion, medication overdose, and adverse drug reaction.
- Engage consultants, including neurologists, neurosurgeons, neuroradiologists, toxicologists, psychiatrists, and psychologists efficiently and appropriately.
- Coordinate care and communicate effectively with caregivers, primary care providers, and consultants about the mental status at the time of discharge and the transition plan, referring to ancillary or rehabilitation services as appropriate.
Attitudes
Pediatric Hospitalists should be able to:
- Realize responsibility for reporting of iatrogenic etiologies as appropriate.
- Acknowledge the need for effective communication with subspecialty providers, primary care providers, and the patients and the family/caregivers to ensure ongoing support and coordinated care.
- Realize responsibility for effective and compassionate communication with patients/caregivers regarding findings, prognosis, and treatments, accounting for the stresses of hospitalization.
- Collaborate with social work, child protective services, and law enforcement when indicated.
Systems Organization and Improvement
In order to improve efficiency and quality within their organizations, pediatric hospitalists should:
- Work with hospital administration and staff to develop, implement, and assess outcomes of intervention strategies for hospitalized patients with deterioration of mental status to prevent adverse outcomes (such as rapid response, code blue, stroke teams, and others).
- Coordinate educational programs for front-line providers to promote early recognition of AMS.
- Lead, coordinate, or participate in institutional efforts to report and reduce cases of AMS due to iatrogenic causes or adverse effects of medications.
1. Lehman RK, Mink J. Altered mental status. Clin Pediatr Emerg Med. 2008; 9:68-75.
2. Avner JR. Altered states of consciousness. Pediatr Rev. 2006; 27:331-338. https://doi.org/10.1542/pir.27-9-331.
3. Malas N, Brahmbhatt K, McDermott C, Smith A. Ortiz-Aguayo R, Turkel S. Pediatric delirium: Evaluation, management, and special considerations. Curr Psychiatry Rep. 2017;19(9):65. https://doi.org/10.1007/s11920-017-0817-3.
1. Lehman RK, Mink J. Altered mental status. Clin Pediatr Emerg Med. 2008; 9:68-75.
2. Avner JR. Altered states of consciousness. Pediatr Rev. 2006; 27:331-338. https://doi.org/10.1542/pir.27-9-331.
3. Malas N, Brahmbhatt K, McDermott C, Smith A. Ortiz-Aguayo R, Turkel S. Pediatric delirium: Evaluation, management, and special considerations. Curr Psychiatry Rep. 2017;19(9):65. https://doi.org/10.1007/s11920-017-0817-3.
1. Lehman RK, Mink J. Altered mental status. Clin Pediatr Emerg Med. 2008; 9:68-75.
2. Avner JR. Altered states of consciousness. Pediatr Rev. 2006; 27:331-338. https://doi.org/10.1542/pir.27-9-331.
3. Malas N, Brahmbhatt K, McDermott C, Smith A. Ortiz-Aguayo R, Turkel S. Pediatric delirium: Evaluation, management, and special considerations. Curr Psychiatry Rep. 2017;19(9):65. https://doi.org/10.1007/s11920-017-0817-3.
Things We Do For No Reason: Routine Blood Culture Acquisition for Children Hospitalized with Community-Acquired Pneumonia
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 4-year-old previously healthy, fully immunized boy presented to the emergency department (ED) with three days of worsening cough, fever to 103oF, dyspnea, and decreased oral intake. In the ED, he was febrile, temperature 102.7oF, heart rate 115 beats/min, respiratory rate 30 breaths/min, and O2 saturation 86%. Pertinent findings identified on examination included tachypnea, dry mucous membranes, and decreased breath sounds in the posterior right lung fields. Chest radiograph revealed a right lower lobe opacification concerning for community-acquired pneumonia (CAP). He was admitted to the hospital due to hypoxemia and dehydration. A blood culture was obtained, and treatment with ampicillin was initiated. The following morning, he was afebrile, clinically improved, and no longer hypoxemic, but the blood culture grew Gram-positive cocci. Another blood culture was performed, and he was switched to vancomycin. The next day, penicillin-susceptible Streptococcus pneumoniae was confirmed from the original culture, and he was discharged home on high-dose amoxicillin.
WHY YOU MIGHT THINK A BLOOD CULTURE IS HELPFUL
CAP is a prominent cause of childhood morbidity and among the most common causes for acute childhood hospitalizations in the United States, with 124,900 hospital stays documented in 2012.1 In 2011, the Infectious Diseases Society of America (IDSA) released recommendations for pediatric CAP in immunocompetent children aged >3 months without chronic medical conditions. The recommendations clearly discourage blood cultures in the outpatient setting but are less direct in the inpatient setting. The recommendations state that providers should obtain blood cultures “in children requiring hospitalization for presumed bacterial CAP that is moderate to severe, particularly those with complicated pneumonia.”2 The recommendation is graded as “strong”, though the IDSA acknowledged the “low” quality of supporting evidence. Although the organization provides a classification for “complicated pneumonia,” it does not define what constitutes mild versus moderate or severe pneumonia.
Without clear recommendations, decisions to obtain blood cultures for hospitalized children with CAP vary among providers and institutions, with the reported hospital-to-hospital variation being as large as 0%-78.7%.3 Some believe that any child hospitalized with CAP meets the definition of moderate to severe pneumonia and have implemented projects to increase blood culture acquisition for this population.4 The decision to err on the side of routinely obtaining a blood culture may come from providers’ prevalent worry of “missing” a diagnosis, desire to target antibacterial therapy, and assumption that it will provide additional information for patients lacking improvement.
WHY A ROUTINE BLOOD CULTURE ON PEDIATRIC CAP ADMISSIONS IS NOT HELPFUL
Since the publication of the 2011 IDSA guidelines, new evidence has revealed a decreasing incidence of bacteremia in pediatric populations.5 Moreover, viruses were the most frequently identified pathogens in children hospitalized with CAP in a large study, which were isolated in 66% of patients, whereas typical bacteria (either alone or in combination with a virus) were identified in only 7% of cases.6 When blood cultures are obtained for pediatric CAP, the incidence of a true bacterial bloodstream pathogen is 1.4%-7% of patients in the United States in the conjugate vaccine era.7-11 Given that the practice of obtaining blood cultures varies widely among hospitalized patients and that cultures are often obtained based on perceived severity of presentation,8,9,12 the true incidence of bacteremia in children with CAP would likely be lower if blood cultures were performed in all patients.
Since the introduction of the first conjugated pneumococcal vaccine, the prevalence of penicillin resistance among pneumococcal isolates dramatically declined,13 though with geographic variability.14 Therefore, when we isolate pneumococcus strains, resistance prevalence requires that we alter treatment much less frequently in the majority of patients with CAP receiving IDSA-recommended ampicillin/amoxicillin.2 In a large six-center, geographically dispersed retrospective cohort study, Neuman et al. reported a rate of true bacteremia of 2.53%; 82% of all pathogens and 92% of pneumococcal isolates were susceptible to penicillin. Therefore, the authors estimated that 667 children hospitalized with CAP would need blood cultures to identify one child requiring an antibiotic other than an aminopenicillin.9 Staphylococcus aureus was identified only in 1% (23/2,138) of patients in the EPIC cohort; the pathogen was identified via blood culture in only 26% (6/23) of these patients.15 Therefore, the concern about the possibility of S. aureus may be a common reason for physicians straying from IDSA-recommended therapy, but it is an uncommon cause of CAP and infrequently identified via blood culture.
Blood culture contaminants have been reported to approach the rate of true pathogens in some studies8,9,11 and be equal or exceed the rates in others.7,16 While awaiting bacterial speciation, antibiotic coverage is often broadened, even for contaminants,8 which can result in unnecessary exposure to nephrotoxic agents such as vancomycin, cause rare adverse events such as Stevens-Johnson syndrome, contribute to antibiotic resistance and unnecessary costs, and increase the length of stay and laboratory utilization.17-19
WHEN MIGHT A BLOOD CULTURE BE HELPFUL
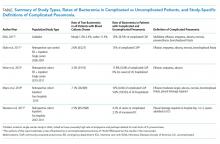
Given the low penicillin resistance prevalence among pneumococcal isolates in several parts of the United States, blood cultures should be used to identify patients with nonpneumococcal CAP as these patients are more likely to require antibiotics other than penicillin or aminopenicillin. Children with complicated pneumonia are more likely to have nonpneumococcal etiologies than children with uncomplicated pneumonia.2 Moreover, literature published since the IDSA guidelines continues to indicate that the incidence of bacteremia in complicated pneumonia is significantly higher than that in uncomplicated pneumonia (Table). This further supports the IDSA guideline recommendation for blood culture acquisition in children with complicated pneumonia.2
One difficulty in interpreting these data is that each publication used a different definition of “complicated” pneumonia, probably due to differences in data sources. Neuman et al. incorporated the narrowest definition of severe and complicated pneumonia as patients who were either admitted to an intensive care unit (ICU) or who underwent a pleural drainage procedure.9 Myers’ and Shah’s definitions were similar to each other but much broader than that of Neuman et al. Shah et al. included lung abscess/necrosis, parapneumonic effusion/empyema, or bronchopleural fistula.11 Myers et al. included the same indications but qualified their pleural fluid effusions as “moderate-to-large” and any effusion that required pleural drainage procedure.8 Myers et al. also reported bacteremia in 75% of patients with metastatic complications, including osteomyelitis.8 These definitions of complicated pneumonia may at least partially explain the differences noted in the rates of bacteremia in complicated pneumonia, with the patients in the study of Myers et al. potentially representing the most severe cohort and with the highest rate of bacteremia8,9 (Table).
These studies not only support the definition of complicated pneumonia put forward by the IDSA but also provide further information, though imperfect, on how to define “moderate to severe.” All the patients with bacteremia in the report of Heine et al. had complicated pneumonia and were described on chart review as either toxic-appearing or requiring ICU care.7 This, in addition to the inclusion of ICU care in the definition of complicated pneumonia of Neuman et al.,9 indicates that children with CAP requiring ICU care may be at higher risk of bacteremia. In fact, the British Thoracic Society guidelines do not recommend microbiological investigations of children with CAP, including blood culture, unless a child requires ICU care.20
WHAT YOU SHOULD DO INSTEAD
Given the low rate of bacteremia in CAP, the risk of blood culture contaminants, and the small likelihood that isolation of a pathogen alters treatment for children, we recommend not using hospital admission as the determining factor for blood culture acquisition. Instead, we recommend a more targeted approach. To achieve a higher rate of true-positive bacteremia in immunocompetent children with up-to-date vaccinations, we recommend acquiring a blood culture in children with complicated pneumonia, metastatic complications, or with ICU needs. By initiating the IDSA-recommended ampicillin/amoxicillin in the remaining hospitalized patients and acquiring blood cultures for the minority of patients who do not improve, we can increase the likelihood of isolating penicillin-resistant bacteria.
Attempting to balance the importance of identifying clinically important bacteremia for children hospitalized with CAP and the inherent risks of obtaining blood cultures for all hospitalized patients, Andrews et al. created and analyzed a cost-effectiveness model. The authors compared universal acquisition of blood cultures for hospitalized children with CAP versus a targeted approach with blood cultures obtained in patients with effusion or empyema, requiring ICU care, or who are immunosuppressed. Based on this model, a targeted approach could save more than $187 million annually, reduce the number of cultures needed to result in a meaningful change in antibiotic therapy for one patient from 122 to 42, and would “miss” only approximately one case of bacteremia resulting in treatment failure per 1,400 patients.17
RECOMMENDATIONS
- Do not obtain blood culture routinely for children aged >3 months hospitalized for uncomplicated CAP.
- Obtain a blood culture for the following hospitalized patients with CAP:
a. Patients with complicated CAP as defined by the IDSA, particularly those with empyema, abscess, or fistula, or metastatic complications of pneumonia (Table); or
b. Patients with CAP requiring ICU care20 for the management of shock and/or advanced respiratory support.
c. Patients with CAP judged to need antibiotic treatment with an agent other than the IDSA-recommended ampicillin/penicillin (concern for pathogens other than penicillin-sensitive S. pneumonia, immunocompromised or under-immunized status, or inadequate clinical response to empiric ampicillin therapy).
CONCLUSION
Implementing a more targeted approach to blood culture acquisition for hospitalized children with CAP will hopefully increase the yield of true bacterial pathogens that alter management decisions. A targeted approach for the child in the opening vignette would have saved him from the pain of unnecessary phlebotomy (repeat culture), exposure to vancomycin as a nephrotoxic agent, and an additional hospital day.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?™” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by e-mailing [email protected].
1. Whitney P, Whitt AJW, Elixhauser A. Overview of hospital stays for children in the United States, 2012. Statistical Brief 187. 2014;187. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb187-Hospital-Stays-Children-2012.jsp. Accessed December 21, 2017.
2. Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-e76. https://doi.org/10.1093/cid/cir531.
3. Brogan TV, Hall M, Williams DJ, et al. Variability in processes of care and outcomes among children hospitalized with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036-1041. https://doi.org/10.1097/INF.0b013e31825f2b10.
4. Murtagh Kurowski E, Shah SS, Thomson J, et al. Improvement methodology increases guideline recommended blood cultures in children with pneumonia. Pediatrics. 2015;135(4):e1052-e1059. https://doi.org/10.1542/peds.2014-2077.
5. Greenhow TL, Hung YY, Herz A. Bacteremia in children 3 to 36 months old after introduction of conjugated pneumococcal vaccines. Pediatrics. 2017;139(4):e20162098. https://doi.org/10.1542/peds.2016-2098.
6. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835-845. https://doi.org/10.1056/NEJMoa1405870.
7. Heine D, Cochran C, Moore M, Titus MO, Andrews AL. The prevalence of bacteremia in pediatric patients with community-acquired pneumonia: guidelines to reduce the frequency of obtaining blood cultures. Hosp Pediatr. 2013;3(2):92-96. https://doi.org/10.1542/hpeds.2012-0050.
8. Myers AL, Hall M, Williams DJ, et al. Prevalence of bacteremia in hospitalized pediatric patients with community-acquired pneumonia. Pediatr Infect Dis J. 2013;32(7):736-740. https://doi.org/10.1097/INF.0b013e318290bf63.
9. Neuman MI, Hall M, Lipsett SC, et al. Utility of blood culture among children hospitalized with community-acquired pneumonia. Pediatrics. 2017;140(3). https://doi.org/10.1542/peds.2017-1013.
10. Sandora TJ, Desai R, Miko BA, Harper MB. Assessing quality indicators for pediatric community-acquired pneumonia. Am J Med Qual. 2009;24(5):419-427. https://doi.org/10.1177/1062860609337900.
11. Shah SS, Dugan MH, Bell LM, et al. Blood cultures in the emergency department evaluation of childhood pneumonia. Pediatr Infect Dis J. 2011;30(6):475-479. https://doi.org/10.1097/INF.0b013e31820a5adb.
12. Davis TR, Evans HR, Murtas J et al. Utility of blood cultures in children admitted to hospital with community-acquired pneumonia. J Paediatr Child Health. 2017;53(3):232-236. https://doi.org/10.1111/jpc.13376.
13. Williams DJ, Shah SS. Community-acquired pneumonia in the conjugate vaccine era. J Pediatr Infect Dis Soc. 2012;1(4):314-328. https://doi.org/10.1093/jpids/pis101.
14. Kyaw MH, Lynfield R, Schaffner W, et al. Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae. N Engl J Med. 2006;354(14):1455-1463. https://doi.org/10.1056/NEJMoa051642.
15. Frush JM, Zhu Y, Edwards KM, et al. Prevalence of Staphylococcus aureus and use of antistaphylococcal therapy in children hospitalized with pneumonia. J Hosp Med. 2018;13(12):848-852. https://doi.org/10.12788/jhm.3093.
16. Mendoza-Paredes A, Bastos J, Leber M, Erickson E, Waseem M. Utility of blood culture in uncomplicated pneumonia in children. Clin Med Insights Pediatr. 2013;7:1-5. https://doi.org/10.4137/CMPed.S8051.
17. Andrews AL, Simpson AN, Heine D, Teufel II RJ. A cost-effectiveness analysis of obtaining blood cultures in children hospitalized for community-acquired pneumonia. J Pediatr. 2015;167(6):1280-1286. https://doi.org/10.1016/j.jpeds.2015.09.025.
18. Leyenaar JK, Lagu T, Shieh MS, Pekow PS, Lindenauer PK. Variation in resource utilization for the management of uncomplicated community-acquired pneumonia across community and children’s hospitals. J Pediatr. 2014;165(3):585-591. https://doi.org/10.1016/j.jpeds.2014.04.062.
19. McCulloh RJ, Koster MP, Yin DE, et al. Evaluating the use of blood cultures in the management of children hospitalized for community-acquired pneumonia. PloS One. 2015;10(2):e0117462. https://doi.org/10.1371/journal.pone.0117462.
20. Harris M, Clark J, Coote N, et al. British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66(2):ii1-ii23. https://doi.org/10.1136/thoraxjnl-2011-200598.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 4-year-old previously healthy, fully immunized boy presented to the emergency department (ED) with three days of worsening cough, fever to 103oF, dyspnea, and decreased oral intake. In the ED, he was febrile, temperature 102.7oF, heart rate 115 beats/min, respiratory rate 30 breaths/min, and O2 saturation 86%. Pertinent findings identified on examination included tachypnea, dry mucous membranes, and decreased breath sounds in the posterior right lung fields. Chest radiograph revealed a right lower lobe opacification concerning for community-acquired pneumonia (CAP). He was admitted to the hospital due to hypoxemia and dehydration. A blood culture was obtained, and treatment with ampicillin was initiated. The following morning, he was afebrile, clinically improved, and no longer hypoxemic, but the blood culture grew Gram-positive cocci. Another blood culture was performed, and he was switched to vancomycin. The next day, penicillin-susceptible Streptococcus pneumoniae was confirmed from the original culture, and he was discharged home on high-dose amoxicillin.
WHY YOU MIGHT THINK A BLOOD CULTURE IS HELPFUL
CAP is a prominent cause of childhood morbidity and among the most common causes for acute childhood hospitalizations in the United States, with 124,900 hospital stays documented in 2012.1 In 2011, the Infectious Diseases Society of America (IDSA) released recommendations for pediatric CAP in immunocompetent children aged >3 months without chronic medical conditions. The recommendations clearly discourage blood cultures in the outpatient setting but are less direct in the inpatient setting. The recommendations state that providers should obtain blood cultures “in children requiring hospitalization for presumed bacterial CAP that is moderate to severe, particularly those with complicated pneumonia.”2 The recommendation is graded as “strong”, though the IDSA acknowledged the “low” quality of supporting evidence. Although the organization provides a classification for “complicated pneumonia,” it does not define what constitutes mild versus moderate or severe pneumonia.
Without clear recommendations, decisions to obtain blood cultures for hospitalized children with CAP vary among providers and institutions, with the reported hospital-to-hospital variation being as large as 0%-78.7%.3 Some believe that any child hospitalized with CAP meets the definition of moderate to severe pneumonia and have implemented projects to increase blood culture acquisition for this population.4 The decision to err on the side of routinely obtaining a blood culture may come from providers’ prevalent worry of “missing” a diagnosis, desire to target antibacterial therapy, and assumption that it will provide additional information for patients lacking improvement.
WHY A ROUTINE BLOOD CULTURE ON PEDIATRIC CAP ADMISSIONS IS NOT HELPFUL
Since the publication of the 2011 IDSA guidelines, new evidence has revealed a decreasing incidence of bacteremia in pediatric populations.5 Moreover, viruses were the most frequently identified pathogens in children hospitalized with CAP in a large study, which were isolated in 66% of patients, whereas typical bacteria (either alone or in combination with a virus) were identified in only 7% of cases.6 When blood cultures are obtained for pediatric CAP, the incidence of a true bacterial bloodstream pathogen is 1.4%-7% of patients in the United States in the conjugate vaccine era.7-11 Given that the practice of obtaining blood cultures varies widely among hospitalized patients and that cultures are often obtained based on perceived severity of presentation,8,9,12 the true incidence of bacteremia in children with CAP would likely be lower if blood cultures were performed in all patients.
Since the introduction of the first conjugated pneumococcal vaccine, the prevalence of penicillin resistance among pneumococcal isolates dramatically declined,13 though with geographic variability.14 Therefore, when we isolate pneumococcus strains, resistance prevalence requires that we alter treatment much less frequently in the majority of patients with CAP receiving IDSA-recommended ampicillin/amoxicillin.2 In a large six-center, geographically dispersed retrospective cohort study, Neuman et al. reported a rate of true bacteremia of 2.53%; 82% of all pathogens and 92% of pneumococcal isolates were susceptible to penicillin. Therefore, the authors estimated that 667 children hospitalized with CAP would need blood cultures to identify one child requiring an antibiotic other than an aminopenicillin.9 Staphylococcus aureus was identified only in 1% (23/2,138) of patients in the EPIC cohort; the pathogen was identified via blood culture in only 26% (6/23) of these patients.15 Therefore, the concern about the possibility of S. aureus may be a common reason for physicians straying from IDSA-recommended therapy, but it is an uncommon cause of CAP and infrequently identified via blood culture.
Blood culture contaminants have been reported to approach the rate of true pathogens in some studies8,9,11 and be equal or exceed the rates in others.7,16 While awaiting bacterial speciation, antibiotic coverage is often broadened, even for contaminants,8 which can result in unnecessary exposure to nephrotoxic agents such as vancomycin, cause rare adverse events such as Stevens-Johnson syndrome, contribute to antibiotic resistance and unnecessary costs, and increase the length of stay and laboratory utilization.17-19
WHEN MIGHT A BLOOD CULTURE BE HELPFUL
Given the low penicillin resistance prevalence among pneumococcal isolates in several parts of the United States, blood cultures should be used to identify patients with nonpneumococcal CAP as these patients are more likely to require antibiotics other than penicillin or aminopenicillin. Children with complicated pneumonia are more likely to have nonpneumococcal etiologies than children with uncomplicated pneumonia.2 Moreover, literature published since the IDSA guidelines continues to indicate that the incidence of bacteremia in complicated pneumonia is significantly higher than that in uncomplicated pneumonia (Table). This further supports the IDSA guideline recommendation for blood culture acquisition in children with complicated pneumonia.2
One difficulty in interpreting these data is that each publication used a different definition of “complicated” pneumonia, probably due to differences in data sources. Neuman et al. incorporated the narrowest definition of severe and complicated pneumonia as patients who were either admitted to an intensive care unit (ICU) or who underwent a pleural drainage procedure.9 Myers’ and Shah’s definitions were similar to each other but much broader than that of Neuman et al. Shah et al. included lung abscess/necrosis, parapneumonic effusion/empyema, or bronchopleural fistula.11 Myers et al. included the same indications but qualified their pleural fluid effusions as “moderate-to-large” and any effusion that required pleural drainage procedure.8 Myers et al. also reported bacteremia in 75% of patients with metastatic complications, including osteomyelitis.8 These definitions of complicated pneumonia may at least partially explain the differences noted in the rates of bacteremia in complicated pneumonia, with the patients in the study of Myers et al. potentially representing the most severe cohort and with the highest rate of bacteremia8,9 (Table).
These studies not only support the definition of complicated pneumonia put forward by the IDSA but also provide further information, though imperfect, on how to define “moderate to severe.” All the patients with bacteremia in the report of Heine et al. had complicated pneumonia and were described on chart review as either toxic-appearing or requiring ICU care.7 This, in addition to the inclusion of ICU care in the definition of complicated pneumonia of Neuman et al.,9 indicates that children with CAP requiring ICU care may be at higher risk of bacteremia. In fact, the British Thoracic Society guidelines do not recommend microbiological investigations of children with CAP, including blood culture, unless a child requires ICU care.20
WHAT YOU SHOULD DO INSTEAD
Given the low rate of bacteremia in CAP, the risk of blood culture contaminants, and the small likelihood that isolation of a pathogen alters treatment for children, we recommend not using hospital admission as the determining factor for blood culture acquisition. Instead, we recommend a more targeted approach. To achieve a higher rate of true-positive bacteremia in immunocompetent children with up-to-date vaccinations, we recommend acquiring a blood culture in children with complicated pneumonia, metastatic complications, or with ICU needs. By initiating the IDSA-recommended ampicillin/amoxicillin in the remaining hospitalized patients and acquiring blood cultures for the minority of patients who do not improve, we can increase the likelihood of isolating penicillin-resistant bacteria.
Attempting to balance the importance of identifying clinically important bacteremia for children hospitalized with CAP and the inherent risks of obtaining blood cultures for all hospitalized patients, Andrews et al. created and analyzed a cost-effectiveness model. The authors compared universal acquisition of blood cultures for hospitalized children with CAP versus a targeted approach with blood cultures obtained in patients with effusion or empyema, requiring ICU care, or who are immunosuppressed. Based on this model, a targeted approach could save more than $187 million annually, reduce the number of cultures needed to result in a meaningful change in antibiotic therapy for one patient from 122 to 42, and would “miss” only approximately one case of bacteremia resulting in treatment failure per 1,400 patients.17
RECOMMENDATIONS
- Do not obtain blood culture routinely for children aged >3 months hospitalized for uncomplicated CAP.
- Obtain a blood culture for the following hospitalized patients with CAP:
a. Patients with complicated CAP as defined by the IDSA, particularly those with empyema, abscess, or fistula, or metastatic complications of pneumonia (Table); or
b. Patients with CAP requiring ICU care20 for the management of shock and/or advanced respiratory support.
c. Patients with CAP judged to need antibiotic treatment with an agent other than the IDSA-recommended ampicillin/penicillin (concern for pathogens other than penicillin-sensitive S. pneumonia, immunocompromised or under-immunized status, or inadequate clinical response to empiric ampicillin therapy).
CONCLUSION
Implementing a more targeted approach to blood culture acquisition for hospitalized children with CAP will hopefully increase the yield of true bacterial pathogens that alter management decisions. A targeted approach for the child in the opening vignette would have saved him from the pain of unnecessary phlebotomy (repeat culture), exposure to vancomycin as a nephrotoxic agent, and an additional hospital day.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?™” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by e-mailing [email protected].
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 4-year-old previously healthy, fully immunized boy presented to the emergency department (ED) with three days of worsening cough, fever to 103oF, dyspnea, and decreased oral intake. In the ED, he was febrile, temperature 102.7oF, heart rate 115 beats/min, respiratory rate 30 breaths/min, and O2 saturation 86%. Pertinent findings identified on examination included tachypnea, dry mucous membranes, and decreased breath sounds in the posterior right lung fields. Chest radiograph revealed a right lower lobe opacification concerning for community-acquired pneumonia (CAP). He was admitted to the hospital due to hypoxemia and dehydration. A blood culture was obtained, and treatment with ampicillin was initiated. The following morning, he was afebrile, clinically improved, and no longer hypoxemic, but the blood culture grew Gram-positive cocci. Another blood culture was performed, and he was switched to vancomycin. The next day, penicillin-susceptible Streptococcus pneumoniae was confirmed from the original culture, and he was discharged home on high-dose amoxicillin.
WHY YOU MIGHT THINK A BLOOD CULTURE IS HELPFUL
CAP is a prominent cause of childhood morbidity and among the most common causes for acute childhood hospitalizations in the United States, with 124,900 hospital stays documented in 2012.1 In 2011, the Infectious Diseases Society of America (IDSA) released recommendations for pediatric CAP in immunocompetent children aged >3 months without chronic medical conditions. The recommendations clearly discourage blood cultures in the outpatient setting but are less direct in the inpatient setting. The recommendations state that providers should obtain blood cultures “in children requiring hospitalization for presumed bacterial CAP that is moderate to severe, particularly those with complicated pneumonia.”2 The recommendation is graded as “strong”, though the IDSA acknowledged the “low” quality of supporting evidence. Although the organization provides a classification for “complicated pneumonia,” it does not define what constitutes mild versus moderate or severe pneumonia.
Without clear recommendations, decisions to obtain blood cultures for hospitalized children with CAP vary among providers and institutions, with the reported hospital-to-hospital variation being as large as 0%-78.7%.3 Some believe that any child hospitalized with CAP meets the definition of moderate to severe pneumonia and have implemented projects to increase blood culture acquisition for this population.4 The decision to err on the side of routinely obtaining a blood culture may come from providers’ prevalent worry of “missing” a diagnosis, desire to target antibacterial therapy, and assumption that it will provide additional information for patients lacking improvement.
WHY A ROUTINE BLOOD CULTURE ON PEDIATRIC CAP ADMISSIONS IS NOT HELPFUL
Since the publication of the 2011 IDSA guidelines, new evidence has revealed a decreasing incidence of bacteremia in pediatric populations.5 Moreover, viruses were the most frequently identified pathogens in children hospitalized with CAP in a large study, which were isolated in 66% of patients, whereas typical bacteria (either alone or in combination with a virus) were identified in only 7% of cases.6 When blood cultures are obtained for pediatric CAP, the incidence of a true bacterial bloodstream pathogen is 1.4%-7% of patients in the United States in the conjugate vaccine era.7-11 Given that the practice of obtaining blood cultures varies widely among hospitalized patients and that cultures are often obtained based on perceived severity of presentation,8,9,12 the true incidence of bacteremia in children with CAP would likely be lower if blood cultures were performed in all patients.
Since the introduction of the first conjugated pneumococcal vaccine, the prevalence of penicillin resistance among pneumococcal isolates dramatically declined,13 though with geographic variability.14 Therefore, when we isolate pneumococcus strains, resistance prevalence requires that we alter treatment much less frequently in the majority of patients with CAP receiving IDSA-recommended ampicillin/amoxicillin.2 In a large six-center, geographically dispersed retrospective cohort study, Neuman et al. reported a rate of true bacteremia of 2.53%; 82% of all pathogens and 92% of pneumococcal isolates were susceptible to penicillin. Therefore, the authors estimated that 667 children hospitalized with CAP would need blood cultures to identify one child requiring an antibiotic other than an aminopenicillin.9 Staphylococcus aureus was identified only in 1% (23/2,138) of patients in the EPIC cohort; the pathogen was identified via blood culture in only 26% (6/23) of these patients.15 Therefore, the concern about the possibility of S. aureus may be a common reason for physicians straying from IDSA-recommended therapy, but it is an uncommon cause of CAP and infrequently identified via blood culture.
Blood culture contaminants have been reported to approach the rate of true pathogens in some studies8,9,11 and be equal or exceed the rates in others.7,16 While awaiting bacterial speciation, antibiotic coverage is often broadened, even for contaminants,8 which can result in unnecessary exposure to nephrotoxic agents such as vancomycin, cause rare adverse events such as Stevens-Johnson syndrome, contribute to antibiotic resistance and unnecessary costs, and increase the length of stay and laboratory utilization.17-19
WHEN MIGHT A BLOOD CULTURE BE HELPFUL
Given the low penicillin resistance prevalence among pneumococcal isolates in several parts of the United States, blood cultures should be used to identify patients with nonpneumococcal CAP as these patients are more likely to require antibiotics other than penicillin or aminopenicillin. Children with complicated pneumonia are more likely to have nonpneumococcal etiologies than children with uncomplicated pneumonia.2 Moreover, literature published since the IDSA guidelines continues to indicate that the incidence of bacteremia in complicated pneumonia is significantly higher than that in uncomplicated pneumonia (Table). This further supports the IDSA guideline recommendation for blood culture acquisition in children with complicated pneumonia.2
One difficulty in interpreting these data is that each publication used a different definition of “complicated” pneumonia, probably due to differences in data sources. Neuman et al. incorporated the narrowest definition of severe and complicated pneumonia as patients who were either admitted to an intensive care unit (ICU) or who underwent a pleural drainage procedure.9 Myers’ and Shah’s definitions were similar to each other but much broader than that of Neuman et al. Shah et al. included lung abscess/necrosis, parapneumonic effusion/empyema, or bronchopleural fistula.11 Myers et al. included the same indications but qualified their pleural fluid effusions as “moderate-to-large” and any effusion that required pleural drainage procedure.8 Myers et al. also reported bacteremia in 75% of patients with metastatic complications, including osteomyelitis.8 These definitions of complicated pneumonia may at least partially explain the differences noted in the rates of bacteremia in complicated pneumonia, with the patients in the study of Myers et al. potentially representing the most severe cohort and with the highest rate of bacteremia8,9 (Table).
These studies not only support the definition of complicated pneumonia put forward by the IDSA but also provide further information, though imperfect, on how to define “moderate to severe.” All the patients with bacteremia in the report of Heine et al. had complicated pneumonia and were described on chart review as either toxic-appearing or requiring ICU care.7 This, in addition to the inclusion of ICU care in the definition of complicated pneumonia of Neuman et al.,9 indicates that children with CAP requiring ICU care may be at higher risk of bacteremia. In fact, the British Thoracic Society guidelines do not recommend microbiological investigations of children with CAP, including blood culture, unless a child requires ICU care.20
WHAT YOU SHOULD DO INSTEAD
Given the low rate of bacteremia in CAP, the risk of blood culture contaminants, and the small likelihood that isolation of a pathogen alters treatment for children, we recommend not using hospital admission as the determining factor for blood culture acquisition. Instead, we recommend a more targeted approach. To achieve a higher rate of true-positive bacteremia in immunocompetent children with up-to-date vaccinations, we recommend acquiring a blood culture in children with complicated pneumonia, metastatic complications, or with ICU needs. By initiating the IDSA-recommended ampicillin/amoxicillin in the remaining hospitalized patients and acquiring blood cultures for the minority of patients who do not improve, we can increase the likelihood of isolating penicillin-resistant bacteria.
Attempting to balance the importance of identifying clinically important bacteremia for children hospitalized with CAP and the inherent risks of obtaining blood cultures for all hospitalized patients, Andrews et al. created and analyzed a cost-effectiveness model. The authors compared universal acquisition of blood cultures for hospitalized children with CAP versus a targeted approach with blood cultures obtained in patients with effusion or empyema, requiring ICU care, or who are immunosuppressed. Based on this model, a targeted approach could save more than $187 million annually, reduce the number of cultures needed to result in a meaningful change in antibiotic therapy for one patient from 122 to 42, and would “miss” only approximately one case of bacteremia resulting in treatment failure per 1,400 patients.17
RECOMMENDATIONS
- Do not obtain blood culture routinely for children aged >3 months hospitalized for uncomplicated CAP.
- Obtain a blood culture for the following hospitalized patients with CAP:
a. Patients with complicated CAP as defined by the IDSA, particularly those with empyema, abscess, or fistula, or metastatic complications of pneumonia (Table); or
b. Patients with CAP requiring ICU care20 for the management of shock and/or advanced respiratory support.
c. Patients with CAP judged to need antibiotic treatment with an agent other than the IDSA-recommended ampicillin/penicillin (concern for pathogens other than penicillin-sensitive S. pneumonia, immunocompromised or under-immunized status, or inadequate clinical response to empiric ampicillin therapy).
CONCLUSION
Implementing a more targeted approach to blood culture acquisition for hospitalized children with CAP will hopefully increase the yield of true bacterial pathogens that alter management decisions. A targeted approach for the child in the opening vignette would have saved him from the pain of unnecessary phlebotomy (repeat culture), exposure to vancomycin as a nephrotoxic agent, and an additional hospital day.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?™” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by e-mailing [email protected].
1. Whitney P, Whitt AJW, Elixhauser A. Overview of hospital stays for children in the United States, 2012. Statistical Brief 187. 2014;187. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb187-Hospital-Stays-Children-2012.jsp. Accessed December 21, 2017.
2. Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-e76. https://doi.org/10.1093/cid/cir531.
3. Brogan TV, Hall M, Williams DJ, et al. Variability in processes of care and outcomes among children hospitalized with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036-1041. https://doi.org/10.1097/INF.0b013e31825f2b10.
4. Murtagh Kurowski E, Shah SS, Thomson J, et al. Improvement methodology increases guideline recommended blood cultures in children with pneumonia. Pediatrics. 2015;135(4):e1052-e1059. https://doi.org/10.1542/peds.2014-2077.
5. Greenhow TL, Hung YY, Herz A. Bacteremia in children 3 to 36 months old after introduction of conjugated pneumococcal vaccines. Pediatrics. 2017;139(4):e20162098. https://doi.org/10.1542/peds.2016-2098.
6. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835-845. https://doi.org/10.1056/NEJMoa1405870.
7. Heine D, Cochran C, Moore M, Titus MO, Andrews AL. The prevalence of bacteremia in pediatric patients with community-acquired pneumonia: guidelines to reduce the frequency of obtaining blood cultures. Hosp Pediatr. 2013;3(2):92-96. https://doi.org/10.1542/hpeds.2012-0050.
8. Myers AL, Hall M, Williams DJ, et al. Prevalence of bacteremia in hospitalized pediatric patients with community-acquired pneumonia. Pediatr Infect Dis J. 2013;32(7):736-740. https://doi.org/10.1097/INF.0b013e318290bf63.
9. Neuman MI, Hall M, Lipsett SC, et al. Utility of blood culture among children hospitalized with community-acquired pneumonia. Pediatrics. 2017;140(3). https://doi.org/10.1542/peds.2017-1013.
10. Sandora TJ, Desai R, Miko BA, Harper MB. Assessing quality indicators for pediatric community-acquired pneumonia. Am J Med Qual. 2009;24(5):419-427. https://doi.org/10.1177/1062860609337900.
11. Shah SS, Dugan MH, Bell LM, et al. Blood cultures in the emergency department evaluation of childhood pneumonia. Pediatr Infect Dis J. 2011;30(6):475-479. https://doi.org/10.1097/INF.0b013e31820a5adb.
12. Davis TR, Evans HR, Murtas J et al. Utility of blood cultures in children admitted to hospital with community-acquired pneumonia. J Paediatr Child Health. 2017;53(3):232-236. https://doi.org/10.1111/jpc.13376.
13. Williams DJ, Shah SS. Community-acquired pneumonia in the conjugate vaccine era. J Pediatr Infect Dis Soc. 2012;1(4):314-328. https://doi.org/10.1093/jpids/pis101.
14. Kyaw MH, Lynfield R, Schaffner W, et al. Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae. N Engl J Med. 2006;354(14):1455-1463. https://doi.org/10.1056/NEJMoa051642.
15. Frush JM, Zhu Y, Edwards KM, et al. Prevalence of Staphylococcus aureus and use of antistaphylococcal therapy in children hospitalized with pneumonia. J Hosp Med. 2018;13(12):848-852. https://doi.org/10.12788/jhm.3093.
16. Mendoza-Paredes A, Bastos J, Leber M, Erickson E, Waseem M. Utility of blood culture in uncomplicated pneumonia in children. Clin Med Insights Pediatr. 2013;7:1-5. https://doi.org/10.4137/CMPed.S8051.
17. Andrews AL, Simpson AN, Heine D, Teufel II RJ. A cost-effectiveness analysis of obtaining blood cultures in children hospitalized for community-acquired pneumonia. J Pediatr. 2015;167(6):1280-1286. https://doi.org/10.1016/j.jpeds.2015.09.025.
18. Leyenaar JK, Lagu T, Shieh MS, Pekow PS, Lindenauer PK. Variation in resource utilization for the management of uncomplicated community-acquired pneumonia across community and children’s hospitals. J Pediatr. 2014;165(3):585-591. https://doi.org/10.1016/j.jpeds.2014.04.062.
19. McCulloh RJ, Koster MP, Yin DE, et al. Evaluating the use of blood cultures in the management of children hospitalized for community-acquired pneumonia. PloS One. 2015;10(2):e0117462. https://doi.org/10.1371/journal.pone.0117462.
20. Harris M, Clark J, Coote N, et al. British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66(2):ii1-ii23. https://doi.org/10.1136/thoraxjnl-2011-200598.
1. Whitney P, Whitt AJW, Elixhauser A. Overview of hospital stays for children in the United States, 2012. Statistical Brief 187. 2014;187. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb187-Hospital-Stays-Children-2012.jsp. Accessed December 21, 2017.
2. Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-e76. https://doi.org/10.1093/cid/cir531.
3. Brogan TV, Hall M, Williams DJ, et al. Variability in processes of care and outcomes among children hospitalized with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036-1041. https://doi.org/10.1097/INF.0b013e31825f2b10.
4. Murtagh Kurowski E, Shah SS, Thomson J, et al. Improvement methodology increases guideline recommended blood cultures in children with pneumonia. Pediatrics. 2015;135(4):e1052-e1059. https://doi.org/10.1542/peds.2014-2077.
5. Greenhow TL, Hung YY, Herz A. Bacteremia in children 3 to 36 months old after introduction of conjugated pneumococcal vaccines. Pediatrics. 2017;139(4):e20162098. https://doi.org/10.1542/peds.2016-2098.
6. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835-845. https://doi.org/10.1056/NEJMoa1405870.
7. Heine D, Cochran C, Moore M, Titus MO, Andrews AL. The prevalence of bacteremia in pediatric patients with community-acquired pneumonia: guidelines to reduce the frequency of obtaining blood cultures. Hosp Pediatr. 2013;3(2):92-96. https://doi.org/10.1542/hpeds.2012-0050.
8. Myers AL, Hall M, Williams DJ, et al. Prevalence of bacteremia in hospitalized pediatric patients with community-acquired pneumonia. Pediatr Infect Dis J. 2013;32(7):736-740. https://doi.org/10.1097/INF.0b013e318290bf63.
9. Neuman MI, Hall M, Lipsett SC, et al. Utility of blood culture among children hospitalized with community-acquired pneumonia. Pediatrics. 2017;140(3). https://doi.org/10.1542/peds.2017-1013.
10. Sandora TJ, Desai R, Miko BA, Harper MB. Assessing quality indicators for pediatric community-acquired pneumonia. Am J Med Qual. 2009;24(5):419-427. https://doi.org/10.1177/1062860609337900.
11. Shah SS, Dugan MH, Bell LM, et al. Blood cultures in the emergency department evaluation of childhood pneumonia. Pediatr Infect Dis J. 2011;30(6):475-479. https://doi.org/10.1097/INF.0b013e31820a5adb.
12. Davis TR, Evans HR, Murtas J et al. Utility of blood cultures in children admitted to hospital with community-acquired pneumonia. J Paediatr Child Health. 2017;53(3):232-236. https://doi.org/10.1111/jpc.13376.
13. Williams DJ, Shah SS. Community-acquired pneumonia in the conjugate vaccine era. J Pediatr Infect Dis Soc. 2012;1(4):314-328. https://doi.org/10.1093/jpids/pis101.
14. Kyaw MH, Lynfield R, Schaffner W, et al. Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae. N Engl J Med. 2006;354(14):1455-1463. https://doi.org/10.1056/NEJMoa051642.
15. Frush JM, Zhu Y, Edwards KM, et al. Prevalence of Staphylococcus aureus and use of antistaphylococcal therapy in children hospitalized with pneumonia. J Hosp Med. 2018;13(12):848-852. https://doi.org/10.12788/jhm.3093.
16. Mendoza-Paredes A, Bastos J, Leber M, Erickson E, Waseem M. Utility of blood culture in uncomplicated pneumonia in children. Clin Med Insights Pediatr. 2013;7:1-5. https://doi.org/10.4137/CMPed.S8051.
17. Andrews AL, Simpson AN, Heine D, Teufel II RJ. A cost-effectiveness analysis of obtaining blood cultures in children hospitalized for community-acquired pneumonia. J Pediatr. 2015;167(6):1280-1286. https://doi.org/10.1016/j.jpeds.2015.09.025.
18. Leyenaar JK, Lagu T, Shieh MS, Pekow PS, Lindenauer PK. Variation in resource utilization for the management of uncomplicated community-acquired pneumonia across community and children’s hospitals. J Pediatr. 2014;165(3):585-591. https://doi.org/10.1016/j.jpeds.2014.04.062.
19. McCulloh RJ, Koster MP, Yin DE, et al. Evaluating the use of blood cultures in the management of children hospitalized for community-acquired pneumonia. PloS One. 2015;10(2):e0117462. https://doi.org/10.1371/journal.pone.0117462.
20. Harris M, Clark J, Coote N, et al. British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66(2):ii1-ii23. https://doi.org/10.1136/thoraxjnl-2011-200598.
© 2020 Society of Hospital Medicine