User login
Visual Management Board Implementation to Enhance High Reliability at a Large VA Health Care System
Health care organizations began implementing Lean management and high reliability organization (HRO) principles in the 1990s to improve quality and efficiency by aligning leaders and staff to a shared vision, fostering a culture of continuous improvement, identifying the root causes of complex problems, and engaging frontline staff as drivers of improvement efforts.1 There are 4 components for establishing a Lean management system: (1) leader standard work; (2) visual management; (3) daily accountability; and (4) discipline to institute the first 3 components.2 Leader standard work promotes continuous improvement by setting a standard routine of behaviors, actions, and tools consistently performed by leadership. These include routine and frequent frontline check-ins (ie, Gemba walks) as well as standardization of employee onboarding, training, and evaluations. Visual management refers to the process of making problems and abnormal conditions readily apparent to staff and leadership.3
The US Department of Veterans Affairs (VA) is committed to implementing similar principles of HROs, which focus on error analysis and process improvement to foster a culture of safety, leadership commitment, and staff engagement.4,5 Visual management is an important tool for HROs; it reflects the mindset of promoting transparency, teamwork, and openness.6,7
Visual management boards (VMBs), such as huddle boards, Gemba boards, or visibility walls, are critical tools that can promote daily accountability and the core principles of Lean thinking and HROs.1,6,8,9 Accountability is enhanced through frequent real-time, data-driven feedback between staff and leadership. This is often facilitated with a huddle, a structured and disciplined team meeting that provides bidirectional information.1 Frequently, a VMB is incorporated into the structure and flow of the huddle.
In a literature review of 20 years of implementation of Lean management systems in health care, Winner and colleagues report that while the frequency and duration of huddles vary, they are often united by several characteristics, including the involvement of the unit team, focus on feedback, problem identification and solutions, and central location around a visual board.1 VMBs most often take the form of a magnetic, dry-erase board located in a hall or conference room central to the work area.1 In addition to identifying and tracking problems in the place of work, VMBs can also provide a representation of key performance indicators and metrics, disseminate essential unit information, and acknowledge the work and successes of staff and leaders.6,8-12
This article outlines the commitment of the Lieutenant Colonel Charles S. Kettles VA Medical Center (VAMC) within the VA Ann Arbor Healthcare System (VAAAHS) to the HRO principle of visual management. We describe the incorporation of VMBs throughout VAAAHS and provide a detailed report of the development and use at a large outpatient subspecialty clinic.
Implementation
The goal of implementing visual management tools at VAAAHS was to empower staff members to identify problems and process improvements, enhance teamwork, and improve communication between staff and section leadership. The Systems Redesign and Improvement Program (SR), which supports Veteran Health Administration high reliability initiatives, helped implement VMBs in VAAAHS departments. Each board was designed to meet the specialized needs of each respective team and could be a physical board, virtual board, or combination. However, all boards sought to create standardized work and identify department needs.
The VAAAHS outpatient cardiology section VMB complemented an existing daily huddle framework. The cardiology section is large and diverse, with 6 subspecialty clinics, and team members who work in multiple locations. The clinic team includes 19 faculty physicians, 14 cardiology fellow physicians,9 nurse care managers, 13 nurse practitioners, 2 licensed practical nurses, and 5 medical support assistants at both the Lieutenant Colonel Charles S. Kettles VAMC and Toledo, Ohio, community based outpatient clinic. Prior to VMB implementation, a morning huddle with clinic team members led by a cardiology manager was an unstructured group discussion about clinic operations for the day. While the daily huddle had a positive impact on staff orientation to daily goals, it did not fully meet the aims of staff empowerment, problem identification and tracking, and knowledge distribution. The VMB was codeveloped with cardiology and the SR program with these goals in mind.
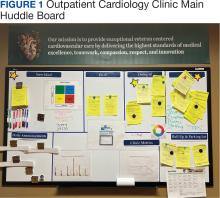
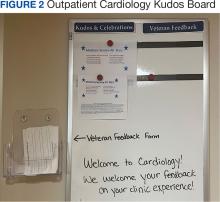
Cardiology was the first VAAAHS outpatient subspecialty clinic to institute a VMB. Two boards were created: a large standard VMB (Figure 1) and a smaller kudos board (Figure 2), which were placed in a central hallway in which staff members and patients pass frequently throughout the day. This location was chosen to promote engagement and promote the VAAAHS commitment to continuous improvement. The VMB focused on identifying and tracking problems, information sharing, and metric monitoring. The goal of the smaller kudos board was to highlight staff achievements and provide an opportunity for patient feedback.
The SR program required that the board incorporate problem identification and a uniform VAAAHS ticket tracking system. Each department could customize the VMB to fit its needs. Staff members are asked to define a problem, complete a ticket describing the issue, consider possible root causes, and suggest solutions. This approach empowers staff to take ownership, make a problem visible, and identify a solution. The problem is then discussed in group huddles using an Impact and Effort Matrix, a tool focused on categorizing and prioritizing those interventions that require low effort and lead to high impact.13
Tickets move along the board as they are addressed using a Plan-Do-Study-Act problem-solving model.14 Plan involves identifying and assigning leadership for the problem and understanding its root causes. Do involves implementing an action plan. Study involves evaluating the results. Finally, Act involves determining whether the plan was successful, and if so, standardizing the improvement and using it regularly.14 Complicated projects that require higher effort or additional resources are moved to the roll-up and parking lot, so they may be addressed by leadership at an appropriate time. Roll up is the escalation of process improvement tickets that frontline staff are unable to resolve with their current resources. The parking lot is for tickets that staff want to address later based on priority determined using an impact vs effort matrix. This allows for enhanced bidirectional communication between the department and high-level leadership, showing a commitment to HRO principles at all levels. The cardiology department customized its board to include essential clinic information, such as faculty staffing for the clinic that day and clinic metric information (eg, patient satisfaction scores, and appointment wait times). The kudos board, a space for patient feedback and to celebrate staff accomplishments, was located across the hall closest to the waiting area.
After the VMB was implemented as a new component to the daily team huddle, the group discussion physically moved to just in front of the board; pertinent clinic information is discussed daily, and the ticketing system is discussed 1 to 3 times per week, depending on ticket progress. Open and unresolved tickets are reviewed for updates on the status by the responsible team member, who receives ongoing feedback and assistance.
Program Impact
A total of 55 improvement opportunity tickets were submitted by staff members during the initial 23 months after the implementation of the outpatient cardiology clinic VMB. Most were submitted by nurse practitioners, although there were contributions from all faculty and staff. The high percentage of ticket submissions by nurse practitioners may be related to their full-time daily presence in the clinic, whereas some other staff members are part-time (most physicians are present 1 day each week). Improvement opportunities were noted within a variety of areas, including clinic facilities (eg, clinic equipment), communication between the clinic and patients (eg, telephone calls from patients or appointment letters), and patient care (eg, medication reconciliation and laboratory requisition).
In an improvement opportunity ticket, a staff member identified that the low seating in the patient waiting area was a fall risk and not diversified for varying body types. They posted a ticket, and the issue was discussed as a group. This staff member assumed ownership of the problem and placed an interior design request for taller chairs and bariatric options. The ticket was resolved when the waiting area was upgraded to include safer and more inclusive seating options for patients. Of 55 tickets submitted by staff as of June 2024, 45 have identified solutions, 4 are in process, and 6 have been placed in the parking lot. On average, the morning huddle spends about 5 to 10 minutes addressing tickets, but on occasion, more complex topics require additional time. The kudos board receives feedback from patients who express their gratitude, and serves as a space to celebrate awards received by staff members.
Implementing a VMB into daily huddles within the cardiology clinic led to increased staff engagement and ownership of challenges, as well as improved communication between frontline workers and leadership. VMBs have proven to be useful for annual staff performance evaluations because staff members who engaged in the board and volunteered to take accountability for ticket resolution could use those accomplishments in their assessments. Finally, VMBs made quality improvement and safety work accessible by normalizing frequent conversations. This empowered staff to engage in improvement projects and even led some members to enroll in formal Lean training.
The outpatient cardiology clinic VMB at the VAAAHS was identified as a best practice during a site visit by the Promising Practice Team in the Veterans Health Administration Office of Integrated Veteran Care. The outpatient cardiology clinic leadership team, including the authors of this article, was invited to present our visual management work as a main topic at the January 2024 Office of Integrated Veteran Care collaborative meeting.
Further Implementation
The SR program has collaborated with additional VAAAHS teams to implement VMBs. Forty-four physical VMBs and 20 virtual VMBs are currently in use throughout the VAAAHS. Virtual VMB content is similar to a physical board and can be modified by each team to meet its particular needs. Several virtual VMBs have been implemented at the VAAAHS and can achieve the same goals of staff teamwork, empowerment, and engagement. Each team can choose the format of the VMB that best fits their needs, which may be partially influenced by the team’s overall interaction style (on-site teams may function better with a physical VMB, and off-site teams may find a virtual VMB works best). VMBs have been implemented in various work areas, including laboratories, inpatient wards, subspecialty outpatient clinics, procedural areas, and the engineering department. In fiscal year 2024, 180 tickets were electronically submitted by teams across the VAAAHS, of which 170 identified solutions and were marked completed. Ticket counts may be underestimated since not all physical board tickets are reported in the electronic system. The SR program periodically attends morning huddles of various teams and obtains feedback on their VMBs, a practice that highlights its contribution to staff engagement, transparency, teamwork, and continuous improvement (Table). A goal of the SR program is to identify areas of the VAAAHS in which VMBs would add value to the team and implement them as necessary.
Discussion
VMBs are common in health care and are implemented to promote the core principlesof Lean thinking and HROs, including visual management and daily accountability. The goals of a visual management tool are to make problems visible and document their management. A VMB can serve as a focal point for team discussion and a physical space to track each problem through its initial identification, understanding of root causes, consideration of potential solutions, and recording of intervention results.
A VMB can foster a culture of safety, leadership commitment, and continuous process improvement when designed and implemented to reflect team needs. VMBs can empower staff members to share work concerns and openly promote engagement. As a central place for discussion between staff and leaders, VMBs can also foster teamwork and communication. The daily huddle provides a safe, productive working environment by ensuring that lines of communication are open among all team members, regardless of role or leadership designation.
Limitations
This article focused on the implementation of 1 type of visual management tool. It provides an in-depth discussion of the development, implementation, and experience with a VMB at multiple clinics of a single section in 1 health care system. These reported experiences may not represent other VA facilities. Perceptions of the impact and usefulness of the VMB were mostly anecdotal. Further evaluation of the VMB implementation experience and utility at other VA health care systems would provide additional insight into the optimal implementation of VMBs.
Conclusions
Through increased transparency, empowerment, and communication, VMBs are an important tool in the visual management tool belt for organizations committed to HROs and Lean management. Given the successful institution of VMBs at the VAAAHS, the description of our experience may aid other VA systems for the incorporation of visual management into the daily culture of their respective health care teams.
1. Winner LE, Reinhardt E, Benishek L, Marsteller JA. Lean management systems in health care: a review of the literature. Qual Manag Health Care. 2022;31(4):221-230. doi:10.1097/QMH.0000000000000353
2. Mann D. Creating a Lean Culture: Tools to Sustain Lean Conversions. Productivity Press; 2005.
3. Graban M. Lean Hospitals: Improving Quality, Patient Safety, and Employee Engagement. 3rd ed. Productivity Press; 2016.
4. Veazie S, Peterson K, Bourne D. Evidence Brief: Implementation of High Reliability Organization Principles. US Dept of Veterans Affairs; 2019. https://www.ncbi.nlm.nih.gov/books/NBK542883/
5. Stone RA, Lieberman SL. VHA’s Vision for a High Reliability Organization. US Dept of Veterans Affairs. Summer 2020. Accessed June 11, 2024. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-1
6. Bourgault AM, Upvall MJ, Graham A. Using Gemba boards to facilitate evidence-based practice in critical care. Crit Care Nurse. 2018;38(3):e1-e7. doi:10.4037/ccn2018714
7. Ferro J, Gouveia R. How to create an effective daily management system. Planet Lean. July 7, 2015. Accessed June 11, 2024. https://www.planet-lean.com/articles/lean-transformation-daily-management
8. Creating a cardiovascular OR huddle board. AORN J. 2020;111(6):687-690. Published 28 May 2020. doi:10.1002/aorn.13057
9. Rakover J, Little K, Scoville R, Holder B. Implementing daily management systems to support sustained quality improvement in ambulatory surgery centers. AORN J. 2020;111(4):415-422. doi:10.1002/aorn.12988
10. Loesche AH. Using huddles to improve communication and teamwork in an instrument-processing department. Nurs Manag (Harrow). 2020;27(6):34-42. doi:10.7748/nm.2020.e1958
11. Zarbo RJ, Varney RC, Copeland JR, D’Angelo R, Sharma G. Daily management system of the Henry Ford production system: QTIPS to focus continuous improvements at the level of the work. Am J Clin Pathol. 2015;144(1):122-136. doi:1309/AJCPLQYMOFWU31CK
12. Hung D, Martinez M, Yakir M, Gray C. Implementing a lean management system in primary care: facilitators and barriers from the front lines. Qual Manag Health Care. 2015;24(3):103-108. doi:10.1097/QMH.0000000000000062
13. Croft D. Guide: Impact and Effort Matrix. Learn Lean 6 Sigma. Accessed June 11, 2024. https://www.learnleansigma.com/guides/impact-effort-matrix/
14. Leis JA, Shojania KG. A primer on PDSA: executing plan-do-study-act cycles in practice, not just in name. BMJ Qual Saf. 2017;26(7):572-577. doi:10.1136/bmjqs-2016-006245
Health care organizations began implementing Lean management and high reliability organization (HRO) principles in the 1990s to improve quality and efficiency by aligning leaders and staff to a shared vision, fostering a culture of continuous improvement, identifying the root causes of complex problems, and engaging frontline staff as drivers of improvement efforts.1 There are 4 components for establishing a Lean management system: (1) leader standard work; (2) visual management; (3) daily accountability; and (4) discipline to institute the first 3 components.2 Leader standard work promotes continuous improvement by setting a standard routine of behaviors, actions, and tools consistently performed by leadership. These include routine and frequent frontline check-ins (ie, Gemba walks) as well as standardization of employee onboarding, training, and evaluations. Visual management refers to the process of making problems and abnormal conditions readily apparent to staff and leadership.3
The US Department of Veterans Affairs (VA) is committed to implementing similar principles of HROs, which focus on error analysis and process improvement to foster a culture of safety, leadership commitment, and staff engagement.4,5 Visual management is an important tool for HROs; it reflects the mindset of promoting transparency, teamwork, and openness.6,7
Visual management boards (VMBs), such as huddle boards, Gemba boards, or visibility walls, are critical tools that can promote daily accountability and the core principles of Lean thinking and HROs.1,6,8,9 Accountability is enhanced through frequent real-time, data-driven feedback between staff and leadership. This is often facilitated with a huddle, a structured and disciplined team meeting that provides bidirectional information.1 Frequently, a VMB is incorporated into the structure and flow of the huddle.
In a literature review of 20 years of implementation of Lean management systems in health care, Winner and colleagues report that while the frequency and duration of huddles vary, they are often united by several characteristics, including the involvement of the unit team, focus on feedback, problem identification and solutions, and central location around a visual board.1 VMBs most often take the form of a magnetic, dry-erase board located in a hall or conference room central to the work area.1 In addition to identifying and tracking problems in the place of work, VMBs can also provide a representation of key performance indicators and metrics, disseminate essential unit information, and acknowledge the work and successes of staff and leaders.6,8-12
This article outlines the commitment of the Lieutenant Colonel Charles S. Kettles VA Medical Center (VAMC) within the VA Ann Arbor Healthcare System (VAAAHS) to the HRO principle of visual management. We describe the incorporation of VMBs throughout VAAAHS and provide a detailed report of the development and use at a large outpatient subspecialty clinic.
Implementation
The goal of implementing visual management tools at VAAAHS was to empower staff members to identify problems and process improvements, enhance teamwork, and improve communication between staff and section leadership. The Systems Redesign and Improvement Program (SR), which supports Veteran Health Administration high reliability initiatives, helped implement VMBs in VAAAHS departments. Each board was designed to meet the specialized needs of each respective team and could be a physical board, virtual board, or combination. However, all boards sought to create standardized work and identify department needs.
The VAAAHS outpatient cardiology section VMB complemented an existing daily huddle framework. The cardiology section is large and diverse, with 6 subspecialty clinics, and team members who work in multiple locations. The clinic team includes 19 faculty physicians, 14 cardiology fellow physicians,9 nurse care managers, 13 nurse practitioners, 2 licensed practical nurses, and 5 medical support assistants at both the Lieutenant Colonel Charles S. Kettles VAMC and Toledo, Ohio, community based outpatient clinic. Prior to VMB implementation, a morning huddle with clinic team members led by a cardiology manager was an unstructured group discussion about clinic operations for the day. While the daily huddle had a positive impact on staff orientation to daily goals, it did not fully meet the aims of staff empowerment, problem identification and tracking, and knowledge distribution. The VMB was codeveloped with cardiology and the SR program with these goals in mind.
Cardiology was the first VAAAHS outpatient subspecialty clinic to institute a VMB. Two boards were created: a large standard VMB (Figure 1) and a smaller kudos board (Figure 2), which were placed in a central hallway in which staff members and patients pass frequently throughout the day. This location was chosen to promote engagement and promote the VAAAHS commitment to continuous improvement. The VMB focused on identifying and tracking problems, information sharing, and metric monitoring. The goal of the smaller kudos board was to highlight staff achievements and provide an opportunity for patient feedback.
The SR program required that the board incorporate problem identification and a uniform VAAAHS ticket tracking system. Each department could customize the VMB to fit its needs. Staff members are asked to define a problem, complete a ticket describing the issue, consider possible root causes, and suggest solutions. This approach empowers staff to take ownership, make a problem visible, and identify a solution. The problem is then discussed in group huddles using an Impact and Effort Matrix, a tool focused on categorizing and prioritizing those interventions that require low effort and lead to high impact.13
Tickets move along the board as they are addressed using a Plan-Do-Study-Act problem-solving model.14 Plan involves identifying and assigning leadership for the problem and understanding its root causes. Do involves implementing an action plan. Study involves evaluating the results. Finally, Act involves determining whether the plan was successful, and if so, standardizing the improvement and using it regularly.14 Complicated projects that require higher effort or additional resources are moved to the roll-up and parking lot, so they may be addressed by leadership at an appropriate time. Roll up is the escalation of process improvement tickets that frontline staff are unable to resolve with their current resources. The parking lot is for tickets that staff want to address later based on priority determined using an impact vs effort matrix. This allows for enhanced bidirectional communication between the department and high-level leadership, showing a commitment to HRO principles at all levels. The cardiology department customized its board to include essential clinic information, such as faculty staffing for the clinic that day and clinic metric information (eg, patient satisfaction scores, and appointment wait times). The kudos board, a space for patient feedback and to celebrate staff accomplishments, was located across the hall closest to the waiting area.
After the VMB was implemented as a new component to the daily team huddle, the group discussion physically moved to just in front of the board; pertinent clinic information is discussed daily, and the ticketing system is discussed 1 to 3 times per week, depending on ticket progress. Open and unresolved tickets are reviewed for updates on the status by the responsible team member, who receives ongoing feedback and assistance.
Program Impact
A total of 55 improvement opportunity tickets were submitted by staff members during the initial 23 months after the implementation of the outpatient cardiology clinic VMB. Most were submitted by nurse practitioners, although there were contributions from all faculty and staff. The high percentage of ticket submissions by nurse practitioners may be related to their full-time daily presence in the clinic, whereas some other staff members are part-time (most physicians are present 1 day each week). Improvement opportunities were noted within a variety of areas, including clinic facilities (eg, clinic equipment), communication between the clinic and patients (eg, telephone calls from patients or appointment letters), and patient care (eg, medication reconciliation and laboratory requisition).
In an improvement opportunity ticket, a staff member identified that the low seating in the patient waiting area was a fall risk and not diversified for varying body types. They posted a ticket, and the issue was discussed as a group. This staff member assumed ownership of the problem and placed an interior design request for taller chairs and bariatric options. The ticket was resolved when the waiting area was upgraded to include safer and more inclusive seating options for patients. Of 55 tickets submitted by staff as of June 2024, 45 have identified solutions, 4 are in process, and 6 have been placed in the parking lot. On average, the morning huddle spends about 5 to 10 minutes addressing tickets, but on occasion, more complex topics require additional time. The kudos board receives feedback from patients who express their gratitude, and serves as a space to celebrate awards received by staff members.
Implementing a VMB into daily huddles within the cardiology clinic led to increased staff engagement and ownership of challenges, as well as improved communication between frontline workers and leadership. VMBs have proven to be useful for annual staff performance evaluations because staff members who engaged in the board and volunteered to take accountability for ticket resolution could use those accomplishments in their assessments. Finally, VMBs made quality improvement and safety work accessible by normalizing frequent conversations. This empowered staff to engage in improvement projects and even led some members to enroll in formal Lean training.
The outpatient cardiology clinic VMB at the VAAAHS was identified as a best practice during a site visit by the Promising Practice Team in the Veterans Health Administration Office of Integrated Veteran Care. The outpatient cardiology clinic leadership team, including the authors of this article, was invited to present our visual management work as a main topic at the January 2024 Office of Integrated Veteran Care collaborative meeting.
Further Implementation
The SR program has collaborated with additional VAAAHS teams to implement VMBs. Forty-four physical VMBs and 20 virtual VMBs are currently in use throughout the VAAAHS. Virtual VMB content is similar to a physical board and can be modified by each team to meet its particular needs. Several virtual VMBs have been implemented at the VAAAHS and can achieve the same goals of staff teamwork, empowerment, and engagement. Each team can choose the format of the VMB that best fits their needs, which may be partially influenced by the team’s overall interaction style (on-site teams may function better with a physical VMB, and off-site teams may find a virtual VMB works best). VMBs have been implemented in various work areas, including laboratories, inpatient wards, subspecialty outpatient clinics, procedural areas, and the engineering department. In fiscal year 2024, 180 tickets were electronically submitted by teams across the VAAAHS, of which 170 identified solutions and were marked completed. Ticket counts may be underestimated since not all physical board tickets are reported in the electronic system. The SR program periodically attends morning huddles of various teams and obtains feedback on their VMBs, a practice that highlights its contribution to staff engagement, transparency, teamwork, and continuous improvement (Table). A goal of the SR program is to identify areas of the VAAAHS in which VMBs would add value to the team and implement them as necessary.
Discussion
VMBs are common in health care and are implemented to promote the core principlesof Lean thinking and HROs, including visual management and daily accountability. The goals of a visual management tool are to make problems visible and document their management. A VMB can serve as a focal point for team discussion and a physical space to track each problem through its initial identification, understanding of root causes, consideration of potential solutions, and recording of intervention results.
A VMB can foster a culture of safety, leadership commitment, and continuous process improvement when designed and implemented to reflect team needs. VMBs can empower staff members to share work concerns and openly promote engagement. As a central place for discussion between staff and leaders, VMBs can also foster teamwork and communication. The daily huddle provides a safe, productive working environment by ensuring that lines of communication are open among all team members, regardless of role or leadership designation.
Limitations
This article focused on the implementation of 1 type of visual management tool. It provides an in-depth discussion of the development, implementation, and experience with a VMB at multiple clinics of a single section in 1 health care system. These reported experiences may not represent other VA facilities. Perceptions of the impact and usefulness of the VMB were mostly anecdotal. Further evaluation of the VMB implementation experience and utility at other VA health care systems would provide additional insight into the optimal implementation of VMBs.
Conclusions
Through increased transparency, empowerment, and communication, VMBs are an important tool in the visual management tool belt for organizations committed to HROs and Lean management. Given the successful institution of VMBs at the VAAAHS, the description of our experience may aid other VA systems for the incorporation of visual management into the daily culture of their respective health care teams.
Health care organizations began implementing Lean management and high reliability organization (HRO) principles in the 1990s to improve quality and efficiency by aligning leaders and staff to a shared vision, fostering a culture of continuous improvement, identifying the root causes of complex problems, and engaging frontline staff as drivers of improvement efforts.1 There are 4 components for establishing a Lean management system: (1) leader standard work; (2) visual management; (3) daily accountability; and (4) discipline to institute the first 3 components.2 Leader standard work promotes continuous improvement by setting a standard routine of behaviors, actions, and tools consistently performed by leadership. These include routine and frequent frontline check-ins (ie, Gemba walks) as well as standardization of employee onboarding, training, and evaluations. Visual management refers to the process of making problems and abnormal conditions readily apparent to staff and leadership.3
The US Department of Veterans Affairs (VA) is committed to implementing similar principles of HROs, which focus on error analysis and process improvement to foster a culture of safety, leadership commitment, and staff engagement.4,5 Visual management is an important tool for HROs; it reflects the mindset of promoting transparency, teamwork, and openness.6,7
Visual management boards (VMBs), such as huddle boards, Gemba boards, or visibility walls, are critical tools that can promote daily accountability and the core principles of Lean thinking and HROs.1,6,8,9 Accountability is enhanced through frequent real-time, data-driven feedback between staff and leadership. This is often facilitated with a huddle, a structured and disciplined team meeting that provides bidirectional information.1 Frequently, a VMB is incorporated into the structure and flow of the huddle.
In a literature review of 20 years of implementation of Lean management systems in health care, Winner and colleagues report that while the frequency and duration of huddles vary, they are often united by several characteristics, including the involvement of the unit team, focus on feedback, problem identification and solutions, and central location around a visual board.1 VMBs most often take the form of a magnetic, dry-erase board located in a hall or conference room central to the work area.1 In addition to identifying and tracking problems in the place of work, VMBs can also provide a representation of key performance indicators and metrics, disseminate essential unit information, and acknowledge the work and successes of staff and leaders.6,8-12
This article outlines the commitment of the Lieutenant Colonel Charles S. Kettles VA Medical Center (VAMC) within the VA Ann Arbor Healthcare System (VAAAHS) to the HRO principle of visual management. We describe the incorporation of VMBs throughout VAAAHS and provide a detailed report of the development and use at a large outpatient subspecialty clinic.
Implementation
The goal of implementing visual management tools at VAAAHS was to empower staff members to identify problems and process improvements, enhance teamwork, and improve communication between staff and section leadership. The Systems Redesign and Improvement Program (SR), which supports Veteran Health Administration high reliability initiatives, helped implement VMBs in VAAAHS departments. Each board was designed to meet the specialized needs of each respective team and could be a physical board, virtual board, or combination. However, all boards sought to create standardized work and identify department needs.
The VAAAHS outpatient cardiology section VMB complemented an existing daily huddle framework. The cardiology section is large and diverse, with 6 subspecialty clinics, and team members who work in multiple locations. The clinic team includes 19 faculty physicians, 14 cardiology fellow physicians,9 nurse care managers, 13 nurse practitioners, 2 licensed practical nurses, and 5 medical support assistants at both the Lieutenant Colonel Charles S. Kettles VAMC and Toledo, Ohio, community based outpatient clinic. Prior to VMB implementation, a morning huddle with clinic team members led by a cardiology manager was an unstructured group discussion about clinic operations for the day. While the daily huddle had a positive impact on staff orientation to daily goals, it did not fully meet the aims of staff empowerment, problem identification and tracking, and knowledge distribution. The VMB was codeveloped with cardiology and the SR program with these goals in mind.
Cardiology was the first VAAAHS outpatient subspecialty clinic to institute a VMB. Two boards were created: a large standard VMB (Figure 1) and a smaller kudos board (Figure 2), which were placed in a central hallway in which staff members and patients pass frequently throughout the day. This location was chosen to promote engagement and promote the VAAAHS commitment to continuous improvement. The VMB focused on identifying and tracking problems, information sharing, and metric monitoring. The goal of the smaller kudos board was to highlight staff achievements and provide an opportunity for patient feedback.
The SR program required that the board incorporate problem identification and a uniform VAAAHS ticket tracking system. Each department could customize the VMB to fit its needs. Staff members are asked to define a problem, complete a ticket describing the issue, consider possible root causes, and suggest solutions. This approach empowers staff to take ownership, make a problem visible, and identify a solution. The problem is then discussed in group huddles using an Impact and Effort Matrix, a tool focused on categorizing and prioritizing those interventions that require low effort and lead to high impact.13
Tickets move along the board as they are addressed using a Plan-Do-Study-Act problem-solving model.14 Plan involves identifying and assigning leadership for the problem and understanding its root causes. Do involves implementing an action plan. Study involves evaluating the results. Finally, Act involves determining whether the plan was successful, and if so, standardizing the improvement and using it regularly.14 Complicated projects that require higher effort or additional resources are moved to the roll-up and parking lot, so they may be addressed by leadership at an appropriate time. Roll up is the escalation of process improvement tickets that frontline staff are unable to resolve with their current resources. The parking lot is for tickets that staff want to address later based on priority determined using an impact vs effort matrix. This allows for enhanced bidirectional communication between the department and high-level leadership, showing a commitment to HRO principles at all levels. The cardiology department customized its board to include essential clinic information, such as faculty staffing for the clinic that day and clinic metric information (eg, patient satisfaction scores, and appointment wait times). The kudos board, a space for patient feedback and to celebrate staff accomplishments, was located across the hall closest to the waiting area.
After the VMB was implemented as a new component to the daily team huddle, the group discussion physically moved to just in front of the board; pertinent clinic information is discussed daily, and the ticketing system is discussed 1 to 3 times per week, depending on ticket progress. Open and unresolved tickets are reviewed for updates on the status by the responsible team member, who receives ongoing feedback and assistance.
Program Impact
A total of 55 improvement opportunity tickets were submitted by staff members during the initial 23 months after the implementation of the outpatient cardiology clinic VMB. Most were submitted by nurse practitioners, although there were contributions from all faculty and staff. The high percentage of ticket submissions by nurse practitioners may be related to their full-time daily presence in the clinic, whereas some other staff members are part-time (most physicians are present 1 day each week). Improvement opportunities were noted within a variety of areas, including clinic facilities (eg, clinic equipment), communication between the clinic and patients (eg, telephone calls from patients or appointment letters), and patient care (eg, medication reconciliation and laboratory requisition).
In an improvement opportunity ticket, a staff member identified that the low seating in the patient waiting area was a fall risk and not diversified for varying body types. They posted a ticket, and the issue was discussed as a group. This staff member assumed ownership of the problem and placed an interior design request for taller chairs and bariatric options. The ticket was resolved when the waiting area was upgraded to include safer and more inclusive seating options for patients. Of 55 tickets submitted by staff as of June 2024, 45 have identified solutions, 4 are in process, and 6 have been placed in the parking lot. On average, the morning huddle spends about 5 to 10 minutes addressing tickets, but on occasion, more complex topics require additional time. The kudos board receives feedback from patients who express their gratitude, and serves as a space to celebrate awards received by staff members.
Implementing a VMB into daily huddles within the cardiology clinic led to increased staff engagement and ownership of challenges, as well as improved communication between frontline workers and leadership. VMBs have proven to be useful for annual staff performance evaluations because staff members who engaged in the board and volunteered to take accountability for ticket resolution could use those accomplishments in their assessments. Finally, VMBs made quality improvement and safety work accessible by normalizing frequent conversations. This empowered staff to engage in improvement projects and even led some members to enroll in formal Lean training.
The outpatient cardiology clinic VMB at the VAAAHS was identified as a best practice during a site visit by the Promising Practice Team in the Veterans Health Administration Office of Integrated Veteran Care. The outpatient cardiology clinic leadership team, including the authors of this article, was invited to present our visual management work as a main topic at the January 2024 Office of Integrated Veteran Care collaborative meeting.
Further Implementation
The SR program has collaborated with additional VAAAHS teams to implement VMBs. Forty-four physical VMBs and 20 virtual VMBs are currently in use throughout the VAAAHS. Virtual VMB content is similar to a physical board and can be modified by each team to meet its particular needs. Several virtual VMBs have been implemented at the VAAAHS and can achieve the same goals of staff teamwork, empowerment, and engagement. Each team can choose the format of the VMB that best fits their needs, which may be partially influenced by the team’s overall interaction style (on-site teams may function better with a physical VMB, and off-site teams may find a virtual VMB works best). VMBs have been implemented in various work areas, including laboratories, inpatient wards, subspecialty outpatient clinics, procedural areas, and the engineering department. In fiscal year 2024, 180 tickets were electronically submitted by teams across the VAAAHS, of which 170 identified solutions and were marked completed. Ticket counts may be underestimated since not all physical board tickets are reported in the electronic system. The SR program periodically attends morning huddles of various teams and obtains feedback on their VMBs, a practice that highlights its contribution to staff engagement, transparency, teamwork, and continuous improvement (Table). A goal of the SR program is to identify areas of the VAAAHS in which VMBs would add value to the team and implement them as necessary.
Discussion
VMBs are common in health care and are implemented to promote the core principlesof Lean thinking and HROs, including visual management and daily accountability. The goals of a visual management tool are to make problems visible and document their management. A VMB can serve as a focal point for team discussion and a physical space to track each problem through its initial identification, understanding of root causes, consideration of potential solutions, and recording of intervention results.
A VMB can foster a culture of safety, leadership commitment, and continuous process improvement when designed and implemented to reflect team needs. VMBs can empower staff members to share work concerns and openly promote engagement. As a central place for discussion between staff and leaders, VMBs can also foster teamwork and communication. The daily huddle provides a safe, productive working environment by ensuring that lines of communication are open among all team members, regardless of role or leadership designation.
Limitations
This article focused on the implementation of 1 type of visual management tool. It provides an in-depth discussion of the development, implementation, and experience with a VMB at multiple clinics of a single section in 1 health care system. These reported experiences may not represent other VA facilities. Perceptions of the impact and usefulness of the VMB were mostly anecdotal. Further evaluation of the VMB implementation experience and utility at other VA health care systems would provide additional insight into the optimal implementation of VMBs.
Conclusions
Through increased transparency, empowerment, and communication, VMBs are an important tool in the visual management tool belt for organizations committed to HROs and Lean management. Given the successful institution of VMBs at the VAAAHS, the description of our experience may aid other VA systems for the incorporation of visual management into the daily culture of their respective health care teams.
1. Winner LE, Reinhardt E, Benishek L, Marsteller JA. Lean management systems in health care: a review of the literature. Qual Manag Health Care. 2022;31(4):221-230. doi:10.1097/QMH.0000000000000353
2. Mann D. Creating a Lean Culture: Tools to Sustain Lean Conversions. Productivity Press; 2005.
3. Graban M. Lean Hospitals: Improving Quality, Patient Safety, and Employee Engagement. 3rd ed. Productivity Press; 2016.
4. Veazie S, Peterson K, Bourne D. Evidence Brief: Implementation of High Reliability Organization Principles. US Dept of Veterans Affairs; 2019. https://www.ncbi.nlm.nih.gov/books/NBK542883/
5. Stone RA, Lieberman SL. VHA’s Vision for a High Reliability Organization. US Dept of Veterans Affairs. Summer 2020. Accessed June 11, 2024. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-1
6. Bourgault AM, Upvall MJ, Graham A. Using Gemba boards to facilitate evidence-based practice in critical care. Crit Care Nurse. 2018;38(3):e1-e7. doi:10.4037/ccn2018714
7. Ferro J, Gouveia R. How to create an effective daily management system. Planet Lean. July 7, 2015. Accessed June 11, 2024. https://www.planet-lean.com/articles/lean-transformation-daily-management
8. Creating a cardiovascular OR huddle board. AORN J. 2020;111(6):687-690. Published 28 May 2020. doi:10.1002/aorn.13057
9. Rakover J, Little K, Scoville R, Holder B. Implementing daily management systems to support sustained quality improvement in ambulatory surgery centers. AORN J. 2020;111(4):415-422. doi:10.1002/aorn.12988
10. Loesche AH. Using huddles to improve communication and teamwork in an instrument-processing department. Nurs Manag (Harrow). 2020;27(6):34-42. doi:10.7748/nm.2020.e1958
11. Zarbo RJ, Varney RC, Copeland JR, D’Angelo R, Sharma G. Daily management system of the Henry Ford production system: QTIPS to focus continuous improvements at the level of the work. Am J Clin Pathol. 2015;144(1):122-136. doi:1309/AJCPLQYMOFWU31CK
12. Hung D, Martinez M, Yakir M, Gray C. Implementing a lean management system in primary care: facilitators and barriers from the front lines. Qual Manag Health Care. 2015;24(3):103-108. doi:10.1097/QMH.0000000000000062
13. Croft D. Guide: Impact and Effort Matrix. Learn Lean 6 Sigma. Accessed June 11, 2024. https://www.learnleansigma.com/guides/impact-effort-matrix/
14. Leis JA, Shojania KG. A primer on PDSA: executing plan-do-study-act cycles in practice, not just in name. BMJ Qual Saf. 2017;26(7):572-577. doi:10.1136/bmjqs-2016-006245
1. Winner LE, Reinhardt E, Benishek L, Marsteller JA. Lean management systems in health care: a review of the literature. Qual Manag Health Care. 2022;31(4):221-230. doi:10.1097/QMH.0000000000000353
2. Mann D. Creating a Lean Culture: Tools to Sustain Lean Conversions. Productivity Press; 2005.
3. Graban M. Lean Hospitals: Improving Quality, Patient Safety, and Employee Engagement. 3rd ed. Productivity Press; 2016.
4. Veazie S, Peterson K, Bourne D. Evidence Brief: Implementation of High Reliability Organization Principles. US Dept of Veterans Affairs; 2019. https://www.ncbi.nlm.nih.gov/books/NBK542883/
5. Stone RA, Lieberman SL. VHA’s Vision for a High Reliability Organization. US Dept of Veterans Affairs. Summer 2020. Accessed June 11, 2024. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-1
6. Bourgault AM, Upvall MJ, Graham A. Using Gemba boards to facilitate evidence-based practice in critical care. Crit Care Nurse. 2018;38(3):e1-e7. doi:10.4037/ccn2018714
7. Ferro J, Gouveia R. How to create an effective daily management system. Planet Lean. July 7, 2015. Accessed June 11, 2024. https://www.planet-lean.com/articles/lean-transformation-daily-management
8. Creating a cardiovascular OR huddle board. AORN J. 2020;111(6):687-690. Published 28 May 2020. doi:10.1002/aorn.13057
9. Rakover J, Little K, Scoville R, Holder B. Implementing daily management systems to support sustained quality improvement in ambulatory surgery centers. AORN J. 2020;111(4):415-422. doi:10.1002/aorn.12988
10. Loesche AH. Using huddles to improve communication and teamwork in an instrument-processing department. Nurs Manag (Harrow). 2020;27(6):34-42. doi:10.7748/nm.2020.e1958
11. Zarbo RJ, Varney RC, Copeland JR, D’Angelo R, Sharma G. Daily management system of the Henry Ford production system: QTIPS to focus continuous improvements at the level of the work. Am J Clin Pathol. 2015;144(1):122-136. doi:1309/AJCPLQYMOFWU31CK
12. Hung D, Martinez M, Yakir M, Gray C. Implementing a lean management system in primary care: facilitators and barriers from the front lines. Qual Manag Health Care. 2015;24(3):103-108. doi:10.1097/QMH.0000000000000062
13. Croft D. Guide: Impact and Effort Matrix. Learn Lean 6 Sigma. Accessed June 11, 2024. https://www.learnleansigma.com/guides/impact-effort-matrix/
14. Leis JA, Shojania KG. A primer on PDSA: executing plan-do-study-act cycles in practice, not just in name. BMJ Qual Saf. 2017;26(7):572-577. doi:10.1136/bmjqs-2016-006245