User login
Dr. Whitcomb is chief medical officer of Remedy Partners. He is co-founder and past president of SHM. E-mail him at [email protected].
Much Ado about Hospital Quality
I have reported previously on major incentive programs under Medicare and the Affordable Care Act that affect hospitals and, by extension, their affiliated hospitalists. I’d like to provide you with an update on these programs. The bad news is that hospitals have more revenue than ever that is at risk based on performance. The good news is that such risk, and its mitigation, centers on performance measures in the sweet spot of hospitalists and the teams they work with to improve patient care.
Hospital-Acquired Conditions
On Dec. 17, 2014, the Centers for Medicare and Medicaid Services (CMS) announced that 724 U.S. hospitals—the lowest quartile—will have 1% of their reimbursement docked effective Oct. 1, 2014, as part of the Hospital-Acquired Condition Reduction Program (HACRP). The HACRP is divided into the following domains:
- 35%, Agency for Healthcare Research and Quality Patient Safety Indicators (PSI-90). This is a composite of eight claims-based harm measures.
- 65%, CDC National Health Safety Network measures. These are clinically derived metrics, currently central line-associated blood stream infection (CLABSI) and catheter-associated urinary tract infection (CAUTI).
The HACRP program, which debuted in October 2014, will continue at least through 2020. The 65% weight domain will change in FY16 with the addition of surgical site infections (colon, hysterectomy) and in FY17 with the addition of MRSA and Clostridium difficile infections.
The full list of U.S. hospitals and their performance in the HACRP and the Hospital Value-Based Purchasing (VBP) program is available at www.modernhealthcare.com/article/20141108/INFO/141109959.
Just two weeks prior to the CMS announcement, AHRQ announced some major accomplishments in efforts to address patient safety at U.S. hospitals. The agency reported that the number of hospital-acquired conditions in the Partnership for Patients (PfP) program in the U.S. declined 9% over a one-year period (2012 to 2013) and 17% over a three-year period (2010 to 2013). Hospital-acquired conditions are defined somewhat differently in the PfP than in the HACRP, with PfP targeting certain hospital-acquired infections, pressure ulcers, falls, and adverse drug effects.
The report noted that reductions in adverse drug events and pressure ulcers were the largest contributors to a reported 50,000 fewer in-hospital deaths over the 2010-2013 period.
Hospital Value-Based Purchasing
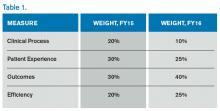
The Hospital VBP program continues to evolve. See Table 1 for a breakdown of the program for the next two years.
Unlike the HACRP and the Hospital Readmissions Reduction Program, which are pure penalty programs, VBP has hospitals at risk for 1.5% (for 2015) of Medicare payments, but they may earn back some, all, or an amount in excess of the 1.5% based on performance. For the years noted above, the VBP program metrics are as follows:
- Clinical Process: selected heart failure (HF), pneumonia (PN), myocardial infarction (MI), and surgical care measures.
- Patient Experience: a subset of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey questions.
- Outcomes: HF, PN, MI, 30-day mortality, CLABSI, and PSI-90.
- Efficiency: Medicare spending per beneficiary (spending from three days prior to an inpatient hospital admission through 30 days after discharge)
Readmission Penalties
CMS announced that in the latest round of the Hospital Readmissions Reduction Program, 2,610 hospitals were penalized in total, while 39 hospitals will receive the largest penalty allowed. For FY15, the program added chronic obstructive pulmonary disease and hip and knee arthroplasty to HF, PN, and MI as the conditions counting toward excess readmissions.
For FY15, the number of hospitals penalized and the amount of the penalty are expected to increase. In addition, 1% of hospitals are anticipated to receive the maximum penalty, while 77% are expected to have some penalty, and 22% will likely have no penalty. The maximum penalty has topped out at 3% of Medicare inpatient payments.
HCAHPS Star Ratings
The CMS Hospital Compare website will debut ‘star ratings’ in April 2015 to make it easier for consumers to decipher the site’s information. In a format similar to the one used by Nursing Home Compare, the website will use a five-star rating system based on the 11 publicly reported HCAHPS measures. The initial ratings will be based on discharges during the period ranging from July 2013 through June 2014.
What’s a Hospitalist to Do?
The latest version of CMS incentive programs should serve to reinforce your hospital medicine group’s strategy to be agents of collaboration and change. Link up with your quality department to align priorities, and make sure you have hospitalist representatives on key patient safety, patient experience, and quality improvement committees.
Because dollars are at stake for your hospital, have a clear understanding of the value your hospitalist group brings to the table, so you can secure the appropriate financial support for the time and work expended on these initiatives.
And don’t forget to keep the patient at the center of your efforts.

I have reported previously on major incentive programs under Medicare and the Affordable Care Act that affect hospitals and, by extension, their affiliated hospitalists. I’d like to provide you with an update on these programs. The bad news is that hospitals have more revenue than ever that is at risk based on performance. The good news is that such risk, and its mitigation, centers on performance measures in the sweet spot of hospitalists and the teams they work with to improve patient care.
Hospital-Acquired Conditions
On Dec. 17, 2014, the Centers for Medicare and Medicaid Services (CMS) announced that 724 U.S. hospitals—the lowest quartile—will have 1% of their reimbursement docked effective Oct. 1, 2014, as part of the Hospital-Acquired Condition Reduction Program (HACRP). The HACRP is divided into the following domains:
- 35%, Agency for Healthcare Research and Quality Patient Safety Indicators (PSI-90). This is a composite of eight claims-based harm measures.
- 65%, CDC National Health Safety Network measures. These are clinically derived metrics, currently central line-associated blood stream infection (CLABSI) and catheter-associated urinary tract infection (CAUTI).
The HACRP program, which debuted in October 2014, will continue at least through 2020. The 65% weight domain will change in FY16 with the addition of surgical site infections (colon, hysterectomy) and in FY17 with the addition of MRSA and Clostridium difficile infections.
The full list of U.S. hospitals and their performance in the HACRP and the Hospital Value-Based Purchasing (VBP) program is available at www.modernhealthcare.com/article/20141108/INFO/141109959.
Just two weeks prior to the CMS announcement, AHRQ announced some major accomplishments in efforts to address patient safety at U.S. hospitals. The agency reported that the number of hospital-acquired conditions in the Partnership for Patients (PfP) program in the U.S. declined 9% over a one-year period (2012 to 2013) and 17% over a three-year period (2010 to 2013). Hospital-acquired conditions are defined somewhat differently in the PfP than in the HACRP, with PfP targeting certain hospital-acquired infections, pressure ulcers, falls, and adverse drug effects.
The report noted that reductions in adverse drug events and pressure ulcers were the largest contributors to a reported 50,000 fewer in-hospital deaths over the 2010-2013 period.
Hospital Value-Based Purchasing
The Hospital VBP program continues to evolve. See Table 1 for a breakdown of the program for the next two years.
Unlike the HACRP and the Hospital Readmissions Reduction Program, which are pure penalty programs, VBP has hospitals at risk for 1.5% (for 2015) of Medicare payments, but they may earn back some, all, or an amount in excess of the 1.5% based on performance. For the years noted above, the VBP program metrics are as follows:
- Clinical Process: selected heart failure (HF), pneumonia (PN), myocardial infarction (MI), and surgical care measures.
- Patient Experience: a subset of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey questions.
- Outcomes: HF, PN, MI, 30-day mortality, CLABSI, and PSI-90.
- Efficiency: Medicare spending per beneficiary (spending from three days prior to an inpatient hospital admission through 30 days after discharge)
Readmission Penalties
CMS announced that in the latest round of the Hospital Readmissions Reduction Program, 2,610 hospitals were penalized in total, while 39 hospitals will receive the largest penalty allowed. For FY15, the program added chronic obstructive pulmonary disease and hip and knee arthroplasty to HF, PN, and MI as the conditions counting toward excess readmissions.
For FY15, the number of hospitals penalized and the amount of the penalty are expected to increase. In addition, 1% of hospitals are anticipated to receive the maximum penalty, while 77% are expected to have some penalty, and 22% will likely have no penalty. The maximum penalty has topped out at 3% of Medicare inpatient payments.
HCAHPS Star Ratings
The CMS Hospital Compare website will debut ‘star ratings’ in April 2015 to make it easier for consumers to decipher the site’s information. In a format similar to the one used by Nursing Home Compare, the website will use a five-star rating system based on the 11 publicly reported HCAHPS measures. The initial ratings will be based on discharges during the period ranging from July 2013 through June 2014.
What’s a Hospitalist to Do?
The latest version of CMS incentive programs should serve to reinforce your hospital medicine group’s strategy to be agents of collaboration and change. Link up with your quality department to align priorities, and make sure you have hospitalist representatives on key patient safety, patient experience, and quality improvement committees.
Because dollars are at stake for your hospital, have a clear understanding of the value your hospitalist group brings to the table, so you can secure the appropriate financial support for the time and work expended on these initiatives.
And don’t forget to keep the patient at the center of your efforts.

I have reported previously on major incentive programs under Medicare and the Affordable Care Act that affect hospitals and, by extension, their affiliated hospitalists. I’d like to provide you with an update on these programs. The bad news is that hospitals have more revenue than ever that is at risk based on performance. The good news is that such risk, and its mitigation, centers on performance measures in the sweet spot of hospitalists and the teams they work with to improve patient care.
Hospital-Acquired Conditions
On Dec. 17, 2014, the Centers for Medicare and Medicaid Services (CMS) announced that 724 U.S. hospitals—the lowest quartile—will have 1% of their reimbursement docked effective Oct. 1, 2014, as part of the Hospital-Acquired Condition Reduction Program (HACRP). The HACRP is divided into the following domains:
- 35%, Agency for Healthcare Research and Quality Patient Safety Indicators (PSI-90). This is a composite of eight claims-based harm measures.
- 65%, CDC National Health Safety Network measures. These are clinically derived metrics, currently central line-associated blood stream infection (CLABSI) and catheter-associated urinary tract infection (CAUTI).
The HACRP program, which debuted in October 2014, will continue at least through 2020. The 65% weight domain will change in FY16 with the addition of surgical site infections (colon, hysterectomy) and in FY17 with the addition of MRSA and Clostridium difficile infections.
The full list of U.S. hospitals and their performance in the HACRP and the Hospital Value-Based Purchasing (VBP) program is available at www.modernhealthcare.com/article/20141108/INFO/141109959.
Just two weeks prior to the CMS announcement, AHRQ announced some major accomplishments in efforts to address patient safety at U.S. hospitals. The agency reported that the number of hospital-acquired conditions in the Partnership for Patients (PfP) program in the U.S. declined 9% over a one-year period (2012 to 2013) and 17% over a three-year period (2010 to 2013). Hospital-acquired conditions are defined somewhat differently in the PfP than in the HACRP, with PfP targeting certain hospital-acquired infections, pressure ulcers, falls, and adverse drug effects.
The report noted that reductions in adverse drug events and pressure ulcers were the largest contributors to a reported 50,000 fewer in-hospital deaths over the 2010-2013 period.
Hospital Value-Based Purchasing
The Hospital VBP program continues to evolve. See Table 1 for a breakdown of the program for the next two years.
Unlike the HACRP and the Hospital Readmissions Reduction Program, which are pure penalty programs, VBP has hospitals at risk for 1.5% (for 2015) of Medicare payments, but they may earn back some, all, or an amount in excess of the 1.5% based on performance. For the years noted above, the VBP program metrics are as follows:
- Clinical Process: selected heart failure (HF), pneumonia (PN), myocardial infarction (MI), and surgical care measures.
- Patient Experience: a subset of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey questions.
- Outcomes: HF, PN, MI, 30-day mortality, CLABSI, and PSI-90.
- Efficiency: Medicare spending per beneficiary (spending from three days prior to an inpatient hospital admission through 30 days after discharge)
Readmission Penalties
CMS announced that in the latest round of the Hospital Readmissions Reduction Program, 2,610 hospitals were penalized in total, while 39 hospitals will receive the largest penalty allowed. For FY15, the program added chronic obstructive pulmonary disease and hip and knee arthroplasty to HF, PN, and MI as the conditions counting toward excess readmissions.
For FY15, the number of hospitals penalized and the amount of the penalty are expected to increase. In addition, 1% of hospitals are anticipated to receive the maximum penalty, while 77% are expected to have some penalty, and 22% will likely have no penalty. The maximum penalty has topped out at 3% of Medicare inpatient payments.
HCAHPS Star Ratings
The CMS Hospital Compare website will debut ‘star ratings’ in April 2015 to make it easier for consumers to decipher the site’s information. In a format similar to the one used by Nursing Home Compare, the website will use a five-star rating system based on the 11 publicly reported HCAHPS measures. The initial ratings will be based on discharges during the period ranging from July 2013 through June 2014.
What’s a Hospitalist to Do?
The latest version of CMS incentive programs should serve to reinforce your hospital medicine group’s strategy to be agents of collaboration and change. Link up with your quality department to align priorities, and make sure you have hospitalist representatives on key patient safety, patient experience, and quality improvement committees.
Because dollars are at stake for your hospital, have a clear understanding of the value your hospitalist group brings to the table, so you can secure the appropriate financial support for the time and work expended on these initiatives.
And don’t forget to keep the patient at the center of your efforts.

A Practice Resolution
In the heart of the holiday season’s gluttony (and the challenges of staffing the holidays), we need something to get us excited for 2015. Let me suggest that you resolve to use “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” to trim those holiday pounds and make your hospitalist group (HMG) fitter than ever.1
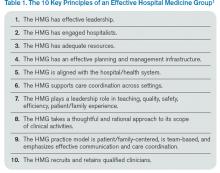
When we published the “Key Principles and Characteristics” in the Journal of Hospital Medicine in February, we intended it to be “aspirational, helping to raise the bar for the specialty of hospital medicine.”1 The author group’s intent was to provide a framework for quality improvement at the HMG level. One can use the 10 principles and 47 characteristics as a basis for self-assessment within the cycle of quality improvement. I will provide an illustration of how a group might utilize the guide to improve its performance using an example and W. Edward Deming’s classic plan-do-study-act (PDSA) cycle.
Principle 6: The HMG supports care coordination across settings.
Characteristic 6.1: The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care provider and/or other providers involved in the patient’s care in the nonacute care setting.
Plan
This phase involves identifying a goal, setting success metrics, and putting a plan into action.
Example: 90% of primary care providers (PCPs) will receive a discharge summary within 24 hours of discharge.
Do
Here the key components of the plan are implemented.
Example: All referring PCPs’ preferred methods of communication and contact information are documented. The HMG has the ability to utilize such communication, e.g. electronic health record (EHR) e-mail or electronic fax. All hospitalists prepare a discharge summary in real time.
Study
In this phase, outcomes are assessed for success and barriers.
Example: Although 97% of discharge summaries are transmitted according to the PCPs’ preferred communication, PCPs state that they received it only 78% of the time.
Act
This is where the lessons learned throughout the process are integrated to adjust the methods, the goal, or the approach in general. Then the entire cycle is repeated.
Example: Even though most PCPs are on the same EHR system as the hospitalists, they don’t check their EHR e-mail (even though during the Plan phase they said they did). Their office staff uses electronic fax, so that will be the method of communication for the PCPs who do not check their EHR e-mail inbox.
In this example, the next time the PDSA cycle is completed, the new approach—using electronic fax for PCPs who don’t check their EHR e-mail while using e-mail for those who check it—will be employed, measured, and further improved in iterative cycles.
Gap Analysis
Another way you can use the “Key Principles and Characteristics” is to do a gap analysis of your HMG. You can assess the current state of your HMG against the “Key Principles and Characteristics,” which can be viewed as an ideal state. The gap between the current and the ideal state can be a roadmap to improvement for your HMG.
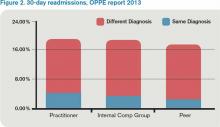
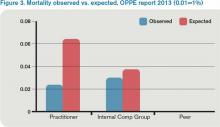
For an example of a large HMG’s gap analysis, see “TeamHealth Hospital Medicine Shares Performance Stats” in the August 2014 issue of The Hospitalist.
Strategic Planning
You may be thinking about taking a block of time to devote to your group’s strategic planning. The “Key Principles and Characteristics” is the ideal framework for such planning. You can use the document as a backdrop to your SWOT (strengths, weaknesses, opportunities, and threats) analysis, which forms the basis of your HMG strategic planning activities.
Keep Your Resolution
One of the best ways to maintain your new habit in the New Year is to let others know of your resolution. In the case of your “Key Principles and Characteristics” resolution, announce your plans at the next monthly meeting of your HMG, and find a way to involve other group members in the project. You might assign a single principle or characteristic to each group member, who is tasked with doing a QI project and reporting on the results at a future date. Or, group members can engage in a portion of a gap analysis or SWOT analysis.
No matter how you use the “Key Principles and Characteristics,” I hope they will guide your HMG to a happy, healthy, and effective 2015!

Reference
In the heart of the holiday season’s gluttony (and the challenges of staffing the holidays), we need something to get us excited for 2015. Let me suggest that you resolve to use “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” to trim those holiday pounds and make your hospitalist group (HMG) fitter than ever.1
When we published the “Key Principles and Characteristics” in the Journal of Hospital Medicine in February, we intended it to be “aspirational, helping to raise the bar for the specialty of hospital medicine.”1 The author group’s intent was to provide a framework for quality improvement at the HMG level. One can use the 10 principles and 47 characteristics as a basis for self-assessment within the cycle of quality improvement. I will provide an illustration of how a group might utilize the guide to improve its performance using an example and W. Edward Deming’s classic plan-do-study-act (PDSA) cycle.
Principle 6: The HMG supports care coordination across settings.
Characteristic 6.1: The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care provider and/or other providers involved in the patient’s care in the nonacute care setting.
Plan
This phase involves identifying a goal, setting success metrics, and putting a plan into action.
Example: 90% of primary care providers (PCPs) will receive a discharge summary within 24 hours of discharge.
Do
Here the key components of the plan are implemented.
Example: All referring PCPs’ preferred methods of communication and contact information are documented. The HMG has the ability to utilize such communication, e.g. electronic health record (EHR) e-mail or electronic fax. All hospitalists prepare a discharge summary in real time.
Study
In this phase, outcomes are assessed for success and barriers.
Example: Although 97% of discharge summaries are transmitted according to the PCPs’ preferred communication, PCPs state that they received it only 78% of the time.
Act
This is where the lessons learned throughout the process are integrated to adjust the methods, the goal, or the approach in general. Then the entire cycle is repeated.
Example: Even though most PCPs are on the same EHR system as the hospitalists, they don’t check their EHR e-mail (even though during the Plan phase they said they did). Their office staff uses electronic fax, so that will be the method of communication for the PCPs who do not check their EHR e-mail inbox.
In this example, the next time the PDSA cycle is completed, the new approach—using electronic fax for PCPs who don’t check their EHR e-mail while using e-mail for those who check it—will be employed, measured, and further improved in iterative cycles.
Gap Analysis
Another way you can use the “Key Principles and Characteristics” is to do a gap analysis of your HMG. You can assess the current state of your HMG against the “Key Principles and Characteristics,” which can be viewed as an ideal state. The gap between the current and the ideal state can be a roadmap to improvement for your HMG.
For an example of a large HMG’s gap analysis, see “TeamHealth Hospital Medicine Shares Performance Stats” in the August 2014 issue of The Hospitalist.
Strategic Planning
You may be thinking about taking a block of time to devote to your group’s strategic planning. The “Key Principles and Characteristics” is the ideal framework for such planning. You can use the document as a backdrop to your SWOT (strengths, weaknesses, opportunities, and threats) analysis, which forms the basis of your HMG strategic planning activities.
Keep Your Resolution
One of the best ways to maintain your new habit in the New Year is to let others know of your resolution. In the case of your “Key Principles and Characteristics” resolution, announce your plans at the next monthly meeting of your HMG, and find a way to involve other group members in the project. You might assign a single principle or characteristic to each group member, who is tasked with doing a QI project and reporting on the results at a future date. Or, group members can engage in a portion of a gap analysis or SWOT analysis.
No matter how you use the “Key Principles and Characteristics,” I hope they will guide your HMG to a happy, healthy, and effective 2015!

Reference
In the heart of the holiday season’s gluttony (and the challenges of staffing the holidays), we need something to get us excited for 2015. Let me suggest that you resolve to use “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” to trim those holiday pounds and make your hospitalist group (HMG) fitter than ever.1
When we published the “Key Principles and Characteristics” in the Journal of Hospital Medicine in February, we intended it to be “aspirational, helping to raise the bar for the specialty of hospital medicine.”1 The author group’s intent was to provide a framework for quality improvement at the HMG level. One can use the 10 principles and 47 characteristics as a basis for self-assessment within the cycle of quality improvement. I will provide an illustration of how a group might utilize the guide to improve its performance using an example and W. Edward Deming’s classic plan-do-study-act (PDSA) cycle.
Principle 6: The HMG supports care coordination across settings.
Characteristic 6.1: The HMG has systems in place to ensure effective and reliable communication with the patient’s primary care provider and/or other providers involved in the patient’s care in the nonacute care setting.
Plan
This phase involves identifying a goal, setting success metrics, and putting a plan into action.
Example: 90% of primary care providers (PCPs) will receive a discharge summary within 24 hours of discharge.
Do
Here the key components of the plan are implemented.
Example: All referring PCPs’ preferred methods of communication and contact information are documented. The HMG has the ability to utilize such communication, e.g. electronic health record (EHR) e-mail or electronic fax. All hospitalists prepare a discharge summary in real time.
Study
In this phase, outcomes are assessed for success and barriers.
Example: Although 97% of discharge summaries are transmitted according to the PCPs’ preferred communication, PCPs state that they received it only 78% of the time.
Act
This is where the lessons learned throughout the process are integrated to adjust the methods, the goal, or the approach in general. Then the entire cycle is repeated.
Example: Even though most PCPs are on the same EHR system as the hospitalists, they don’t check their EHR e-mail (even though during the Plan phase they said they did). Their office staff uses electronic fax, so that will be the method of communication for the PCPs who do not check their EHR e-mail inbox.
In this example, the next time the PDSA cycle is completed, the new approach—using electronic fax for PCPs who don’t check their EHR e-mail while using e-mail for those who check it—will be employed, measured, and further improved in iterative cycles.
Gap Analysis
Another way you can use the “Key Principles and Characteristics” is to do a gap analysis of your HMG. You can assess the current state of your HMG against the “Key Principles and Characteristics,” which can be viewed as an ideal state. The gap between the current and the ideal state can be a roadmap to improvement for your HMG.
For an example of a large HMG’s gap analysis, see “TeamHealth Hospital Medicine Shares Performance Stats” in the August 2014 issue of The Hospitalist.
Strategic Planning
You may be thinking about taking a block of time to devote to your group’s strategic planning. The “Key Principles and Characteristics” is the ideal framework for such planning. You can use the document as a backdrop to your SWOT (strengths, weaknesses, opportunities, and threats) analysis, which forms the basis of your HMG strategic planning activities.
Keep Your Resolution
One of the best ways to maintain your new habit in the New Year is to let others know of your resolution. In the case of your “Key Principles and Characteristics” resolution, announce your plans at the next monthly meeting of your HMG, and find a way to involve other group members in the project. You might assign a single principle or characteristic to each group member, who is tasked with doing a QI project and reporting on the results at a future date. Or, group members can engage in a portion of a gap analysis or SWOT analysis.
No matter how you use the “Key Principles and Characteristics,” I hope they will guide your HMG to a happy, healthy, and effective 2015!

Reference
Homecare Will Help You Achieve the Triple Aim
Where there is variation, there is room for improvement. The Institute of Medicine’s report on geographic variation in Medicare spending concluded that the largest contributor to overall spending variation is spending for post-acute care services.1 Furthermore, we know that a significant amount of overall spending is devoted to post-acute care. For example, for patients hospitalized with a flare-up of a chronic condition like COPD or heart failure, Medicare spends nearly as much on post-acute care and readmissions in the first 30 days after discharge as it does on the initial admission.1
What does this mean for hospitalists?
Numerous research articles and quality improvement projects have focused on what makes a good hospital discharge or hand off to the ‘next provider of care’; however, hospitalists are increasingly participating in value-based payment programs like accountable care organizations (ACOs), risk contracts, and bundled payments. This means they must begin to pay attention to the cost side of the value equation (quality divided by cost) as it relates to hospital discharge.
A day of home care represents a more cost-effective alternative than a day of care in a skilled nursing facility (SNF). Hospitalists who can identify those patients who are appropriate to send home with home health services—and who otherwise would have gone to a SNF—will serve the dual goals of improving patient experience and decreasing costs.
Hospitalists will need to develop a decision-making process that determines the appropriate level of care for the patient after discharge. The decision-making process should address questions like:
- What skilled services lead a patient to go to a SNF instead of home with home health?
- Which patients go to a SNF instead of home simply because they don’t have family or a caregiver to help them with activities of daily living?
- Are there services requiring a nurse or a therapist that can’t be delivered in the home?
Hospitalists also will need to develop a more intimate understanding of the following levels of care:
- Skilled nursing includes management of a nursing care plan, assessment of a patient’s changing condition, and services like wound care, infusion therapy, and management of medications, feeding or drainage tubes, and pain.
- Skilled rehabilitation refers to the array of services provided by physical, occupational, speech, and respiratory therapists.
- Custodial care, usually supplied by a home health aid or family member, includes help with activities of daily living (feeding, dressing, bathing, grooming, personal hygiene, and toileting).
It should be noted that most skilled nursing or therapy services can be delivered in the home setting if the patient’s custodial care needs are met—a big ‘if’ in some cases. Some patients go to a SNF because they require three or more skilled nursing or therapy services, and it is therefore impractical for them to go home.
Here are my suggestions to hospitalists seeking to reengineer the discharge process with the goals of “right-sizing” the number of patients who go to SNFs and optimizing the utilization of home healthcare services:
- Become familiar with the range of post-acute care providers and care coordination services in your community.
- Refer any patient who wishes to go home, either directly or after a SNF stay, for a home care evaluation. Home care agencies are experts in determining if and how patients can return home.
- If a need for help with activities of daily living is the major barrier to having a patient discharged to home, create a system in which case management develops a custodial care plan with the patient and caregivers during the inpatient stay. Currently, this step is delayed until well into the SNF stay and may prolong that stay. Such a plan includes a financial analysis, screening for Medicaid eligibility, and evaluating whether a family member can assume some or all of the custodial care needs.
- If a patient is being discharged to a SNF, review the list of needed services leading to the SNF transfer. Ask the case manager if these services can be provided in the home. If not, then why?
- Bed capacity permitting, consider keeping patients who are functionally improving in the hospital an extra day so they can be discharged directly home instead of to a SNF.2
In his seminal work, The Innovator’s Dilemma, Clayton Christensen describes “disruptive innovation” as that which gives rise to products or services that are cheaper, simpler, and more convenient to use. Even though home care has been around for a while, there is a sizeable group of patients, especially in geographic areas of high SNF spending, who might be better served in the home environment. As we create better systems under value-based payment, we should see an increase in the use of home healthcare as a disruptive innovation when applied to appropriate patients transitioning out of the hospital or a SNF.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
Where there is variation, there is room for improvement. The Institute of Medicine’s report on geographic variation in Medicare spending concluded that the largest contributor to overall spending variation is spending for post-acute care services.1 Furthermore, we know that a significant amount of overall spending is devoted to post-acute care. For example, for patients hospitalized with a flare-up of a chronic condition like COPD or heart failure, Medicare spends nearly as much on post-acute care and readmissions in the first 30 days after discharge as it does on the initial admission.1
What does this mean for hospitalists?
Numerous research articles and quality improvement projects have focused on what makes a good hospital discharge or hand off to the ‘next provider of care’; however, hospitalists are increasingly participating in value-based payment programs like accountable care organizations (ACOs), risk contracts, and bundled payments. This means they must begin to pay attention to the cost side of the value equation (quality divided by cost) as it relates to hospital discharge.
A day of home care represents a more cost-effective alternative than a day of care in a skilled nursing facility (SNF). Hospitalists who can identify those patients who are appropriate to send home with home health services—and who otherwise would have gone to a SNF—will serve the dual goals of improving patient experience and decreasing costs.
Hospitalists will need to develop a decision-making process that determines the appropriate level of care for the patient after discharge. The decision-making process should address questions like:
- What skilled services lead a patient to go to a SNF instead of home with home health?
- Which patients go to a SNF instead of home simply because they don’t have family or a caregiver to help them with activities of daily living?
- Are there services requiring a nurse or a therapist that can’t be delivered in the home?
Hospitalists also will need to develop a more intimate understanding of the following levels of care:
- Skilled nursing includes management of a nursing care plan, assessment of a patient’s changing condition, and services like wound care, infusion therapy, and management of medications, feeding or drainage tubes, and pain.
- Skilled rehabilitation refers to the array of services provided by physical, occupational, speech, and respiratory therapists.
- Custodial care, usually supplied by a home health aid or family member, includes help with activities of daily living (feeding, dressing, bathing, grooming, personal hygiene, and toileting).
It should be noted that most skilled nursing or therapy services can be delivered in the home setting if the patient’s custodial care needs are met—a big ‘if’ in some cases. Some patients go to a SNF because they require three or more skilled nursing or therapy services, and it is therefore impractical for them to go home.
Here are my suggestions to hospitalists seeking to reengineer the discharge process with the goals of “right-sizing” the number of patients who go to SNFs and optimizing the utilization of home healthcare services:
- Become familiar with the range of post-acute care providers and care coordination services in your community.
- Refer any patient who wishes to go home, either directly or after a SNF stay, for a home care evaluation. Home care agencies are experts in determining if and how patients can return home.
- If a need for help with activities of daily living is the major barrier to having a patient discharged to home, create a system in which case management develops a custodial care plan with the patient and caregivers during the inpatient stay. Currently, this step is delayed until well into the SNF stay and may prolong that stay. Such a plan includes a financial analysis, screening for Medicaid eligibility, and evaluating whether a family member can assume some or all of the custodial care needs.
- If a patient is being discharged to a SNF, review the list of needed services leading to the SNF transfer. Ask the case manager if these services can be provided in the home. If not, then why?
- Bed capacity permitting, consider keeping patients who are functionally improving in the hospital an extra day so they can be discharged directly home instead of to a SNF.2
In his seminal work, The Innovator’s Dilemma, Clayton Christensen describes “disruptive innovation” as that which gives rise to products or services that are cheaper, simpler, and more convenient to use. Even though home care has been around for a while, there is a sizeable group of patients, especially in geographic areas of high SNF spending, who might be better served in the home environment. As we create better systems under value-based payment, we should see an increase in the use of home healthcare as a disruptive innovation when applied to appropriate patients transitioning out of the hospital or a SNF.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
Where there is variation, there is room for improvement. The Institute of Medicine’s report on geographic variation in Medicare spending concluded that the largest contributor to overall spending variation is spending for post-acute care services.1 Furthermore, we know that a significant amount of overall spending is devoted to post-acute care. For example, for patients hospitalized with a flare-up of a chronic condition like COPD or heart failure, Medicare spends nearly as much on post-acute care and readmissions in the first 30 days after discharge as it does on the initial admission.1
What does this mean for hospitalists?
Numerous research articles and quality improvement projects have focused on what makes a good hospital discharge or hand off to the ‘next provider of care’; however, hospitalists are increasingly participating in value-based payment programs like accountable care organizations (ACOs), risk contracts, and bundled payments. This means they must begin to pay attention to the cost side of the value equation (quality divided by cost) as it relates to hospital discharge.
A day of home care represents a more cost-effective alternative than a day of care in a skilled nursing facility (SNF). Hospitalists who can identify those patients who are appropriate to send home with home health services—and who otherwise would have gone to a SNF—will serve the dual goals of improving patient experience and decreasing costs.
Hospitalists will need to develop a decision-making process that determines the appropriate level of care for the patient after discharge. The decision-making process should address questions like:
- What skilled services lead a patient to go to a SNF instead of home with home health?
- Which patients go to a SNF instead of home simply because they don’t have family or a caregiver to help them with activities of daily living?
- Are there services requiring a nurse or a therapist that can’t be delivered in the home?
Hospitalists also will need to develop a more intimate understanding of the following levels of care:
- Skilled nursing includes management of a nursing care plan, assessment of a patient’s changing condition, and services like wound care, infusion therapy, and management of medications, feeding or drainage tubes, and pain.
- Skilled rehabilitation refers to the array of services provided by physical, occupational, speech, and respiratory therapists.
- Custodial care, usually supplied by a home health aid or family member, includes help with activities of daily living (feeding, dressing, bathing, grooming, personal hygiene, and toileting).
It should be noted that most skilled nursing or therapy services can be delivered in the home setting if the patient’s custodial care needs are met—a big ‘if’ in some cases. Some patients go to a SNF because they require three or more skilled nursing or therapy services, and it is therefore impractical for them to go home.
Here are my suggestions to hospitalists seeking to reengineer the discharge process with the goals of “right-sizing” the number of patients who go to SNFs and optimizing the utilization of home healthcare services:
- Become familiar with the range of post-acute care providers and care coordination services in your community.
- Refer any patient who wishes to go home, either directly or after a SNF stay, for a home care evaluation. Home care agencies are experts in determining if and how patients can return home.
- If a need for help with activities of daily living is the major barrier to having a patient discharged to home, create a system in which case management develops a custodial care plan with the patient and caregivers during the inpatient stay. Currently, this step is delayed until well into the SNF stay and may prolong that stay. Such a plan includes a financial analysis, screening for Medicaid eligibility, and evaluating whether a family member can assume some or all of the custodial care needs.
- If a patient is being discharged to a SNF, review the list of needed services leading to the SNF transfer. Ask the case manager if these services can be provided in the home. If not, then why?
- Bed capacity permitting, consider keeping patients who are functionally improving in the hospital an extra day so they can be discharged directly home instead of to a SNF.2
In his seminal work, The Innovator’s Dilemma, Clayton Christensen describes “disruptive innovation” as that which gives rise to products or services that are cheaper, simpler, and more convenient to use. Even though home care has been around for a while, there is a sizeable group of patients, especially in geographic areas of high SNF spending, who might be better served in the home environment. As we create better systems under value-based payment, we should see an increase in the use of home healthcare as a disruptive innovation when applied to appropriate patients transitioning out of the hospital or a SNF.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
State of the Art
It has been a couple of years since Jason Stein, MD, SFHM, a hospitalist at Emory University School of Medicine in Atlanta, first reported on his experience with accountable care units (ACUs) and structured interdisciplinary bedside rounds (SIBR). With ACUs, Jason and his team undertook an “extreme makeover” of care on the hospital ward. Because most hospitalist groups are endeavoring to address team-based care, I took the opportunity to catch up with and learn from Jason, who has created an exciting and compelling approach to multidisciplinary, collaborative care in the hospital.
In 2012, Jason’s team won SHM’s Excellence in Teamwork in Quality Improvement Award, and Jason was selected as an innovation advisor to the Center for Medicare and Medicaid Innovation. Since then, ACUs and SIBR have been implemented at a number of sites in the U.S. and abroad, and the work has been referenced by the Agency for Healthcare Research and Quality and the Harvard Business Review. Jason has created Centripital, a nonprofit that trains members of the hospital team to collaborate optimally around the patient and family, the central focus of care.
Here are some excerpts from my interview with Jason:
Question: What is an accountable care unit (ACU)?
Answer: We defined an ACU as a geographic inpatient care area consistently responsible for the clinical, service, and cost outcomes it produces. There are four essential design features of ACUs: 1) unit-based physician teams; 2) structured interdisciplinary bedside rounds, or SIBR; 3) unit-level performance reports; and 4) unit co-management by nurse and physician directors.
Q: What were you observing in the care of the hospitalized patient that led you to create ACUs?
A: We saw fragmentation. We saw weak cohesiveness and poor communication among doctors, nurses, and allied health professionals. HM physicians who travel all over the hospital seeing patients are living with an illusion of teamwork. In reality, to be a high-functioning team, physicians have to share time, space, and a standard way to work together with nurses, patients, and families. When we embraced this way of thinking, we realized we could be so much better than we were. The key was to re-engineer a way to really work together.
Q: What makes an ACU successful?
A: In a word, control. An ACU creates new control levers for all of the key players to have greater influence on other members of the team—nurses with doctors, doctors with nurses, patients with everyone, and vice versa. It’s actually quite simple how this happens. The ACU clinical team spends the day together, caring for the same group of patients. Everyone communicates face to face, rather than by page, text, or phone. Stronger relationships are built, and clinicians are more respectful of one another. A different level of responsiveness and accountability is created. The feeling that every person is accountable to the patient and to the other team members allows the team to gain greater control over what happens on the unit. That’s a very powerful dynamic.
SIBR further reinforces the mutual accountability on an ACU. During SIBR, each person has a chance to hear and be heard, to share their perspective, and to contribute to the care plan. Day after day, SIBR creates a positive, collaborative culture of patient care. Once clinicians realize how much control and how much self-actualization they gain on an ACU, it seems impossible to go back to the old way.

—Jason Stein, MD, SFHM
Q: What is the biggest challenge in implementing and sustaining an ACU?
A: The first challenge, of course, is that this is change. And up front—before they realize they will actually gain greater control from the ACU-SIBR model—nurses and, particularly, doctors can perceive this change as a loss of control. “You’re telling me I have to SIBR every morning? At what time? And I have to do all my primary data gathering, including a patient interview and physical exam, before SIBR? Let me stop you right there. I’m way too busy for that.”
Naturally, not everyone immediately sees that they can gain rather than lose efficiency.
Another challenge is the logistics of implementing and then maintaining unit-based physician teams. There are multiple forces that can make geographic units a challenge to create and sustain, but all the logistics are manageable.
Q: How have you helped hospitals transition from a physician-centric model to the geographic-based model?
A: The most important factor in transitioning to an ACU model is for physicians to come to terms with the reality that geography must be the primary driver of physician assignments to patients. Nurses figured this out a long time ago. Do any of us know, bedside nurses who care for patients on multiple different units? As physicians, we’re due for the same realization.
But this means sacrificing long-practiced physician-centric methods of assigning ourselves to patients: call schedules, load balancing across practice partners—even the cherished concept of continuity is a force that can be at odds with geography as the driver. The way to approach the transition to unit-based teams is to have an honest dialogue. Why do we come to work in the hospital every day? If it’s to serve physician needs first, the old model deserves our loyalty. But if the needs of our patients and families are our focus, then we should embrace models that enable us to work effectively together, to become a great team.
Q: How have ACUs performed so far?
A: In the highest-acuity ACUs, we’ve seen mortality reductions of nearly 50%. In addition, there is a wide range of anecdotal outcomes reported. Most ACUs appear to be seeing reductions in length of stay and improvements in patient satisfaction and employee engagement. One ACU reports significant reductions in average cost per patient per day. Another ACU in a geriatric unit has seen dramatic reductions in falls. Some ACUs have seen improvements in glycemic control and VTE prophylaxis, and reductions in catheter utilization.
The benefits of the model seem to be many and probably depend on the patient population, severity of illness, baseline level of performance, and the focus and ability of the unit leadership team to get the most out of the model.
Q: Will ACUs or ACU features become de rigueur in a transformed healthcare landscape?
A: It’s hard to imagine a reality where features of ACUs do not become the standard of care. Once patients and professionals experience the impact of the ACU model, there’ll be no going back. It feels like exactly what we should be doing together. Several ACU design features are reinforced pretty cogently by Richard Bohmer in a New England Journal of Medicine perspective called “The Four Habits of High-Value Health Care Organizations.”1
Q: Any final thoughts?
A: I did not imagine my career as a QI practitioner at Emory becoming so immersed in social and industrial engineering. Of course, it’s obvious to me now that it’s happened, but six years ago when I first started directing SHM’s quality course, I thought the future in HM was health IT and real-time dashboards. Now I know those things will be important, but only if we first figure out how to get our frontline interdisciplinary clinicians to work as an effective team.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
Reference
It has been a couple of years since Jason Stein, MD, SFHM, a hospitalist at Emory University School of Medicine in Atlanta, first reported on his experience with accountable care units (ACUs) and structured interdisciplinary bedside rounds (SIBR). With ACUs, Jason and his team undertook an “extreme makeover” of care on the hospital ward. Because most hospitalist groups are endeavoring to address team-based care, I took the opportunity to catch up with and learn from Jason, who has created an exciting and compelling approach to multidisciplinary, collaborative care in the hospital.
In 2012, Jason’s team won SHM’s Excellence in Teamwork in Quality Improvement Award, and Jason was selected as an innovation advisor to the Center for Medicare and Medicaid Innovation. Since then, ACUs and SIBR have been implemented at a number of sites in the U.S. and abroad, and the work has been referenced by the Agency for Healthcare Research and Quality and the Harvard Business Review. Jason has created Centripital, a nonprofit that trains members of the hospital team to collaborate optimally around the patient and family, the central focus of care.
Here are some excerpts from my interview with Jason:
Question: What is an accountable care unit (ACU)?
Answer: We defined an ACU as a geographic inpatient care area consistently responsible for the clinical, service, and cost outcomes it produces. There are four essential design features of ACUs: 1) unit-based physician teams; 2) structured interdisciplinary bedside rounds, or SIBR; 3) unit-level performance reports; and 4) unit co-management by nurse and physician directors.
Q: What were you observing in the care of the hospitalized patient that led you to create ACUs?
A: We saw fragmentation. We saw weak cohesiveness and poor communication among doctors, nurses, and allied health professionals. HM physicians who travel all over the hospital seeing patients are living with an illusion of teamwork. In reality, to be a high-functioning team, physicians have to share time, space, and a standard way to work together with nurses, patients, and families. When we embraced this way of thinking, we realized we could be so much better than we were. The key was to re-engineer a way to really work together.
Q: What makes an ACU successful?
A: In a word, control. An ACU creates new control levers for all of the key players to have greater influence on other members of the team—nurses with doctors, doctors with nurses, patients with everyone, and vice versa. It’s actually quite simple how this happens. The ACU clinical team spends the day together, caring for the same group of patients. Everyone communicates face to face, rather than by page, text, or phone. Stronger relationships are built, and clinicians are more respectful of one another. A different level of responsiveness and accountability is created. The feeling that every person is accountable to the patient and to the other team members allows the team to gain greater control over what happens on the unit. That’s a very powerful dynamic.
SIBR further reinforces the mutual accountability on an ACU. During SIBR, each person has a chance to hear and be heard, to share their perspective, and to contribute to the care plan. Day after day, SIBR creates a positive, collaborative culture of patient care. Once clinicians realize how much control and how much self-actualization they gain on an ACU, it seems impossible to go back to the old way.

—Jason Stein, MD, SFHM
Q: What is the biggest challenge in implementing and sustaining an ACU?
A: The first challenge, of course, is that this is change. And up front—before they realize they will actually gain greater control from the ACU-SIBR model—nurses and, particularly, doctors can perceive this change as a loss of control. “You’re telling me I have to SIBR every morning? At what time? And I have to do all my primary data gathering, including a patient interview and physical exam, before SIBR? Let me stop you right there. I’m way too busy for that.”
Naturally, not everyone immediately sees that they can gain rather than lose efficiency.
Another challenge is the logistics of implementing and then maintaining unit-based physician teams. There are multiple forces that can make geographic units a challenge to create and sustain, but all the logistics are manageable.
Q: How have you helped hospitals transition from a physician-centric model to the geographic-based model?
A: The most important factor in transitioning to an ACU model is for physicians to come to terms with the reality that geography must be the primary driver of physician assignments to patients. Nurses figured this out a long time ago. Do any of us know, bedside nurses who care for patients on multiple different units? As physicians, we’re due for the same realization.
But this means sacrificing long-practiced physician-centric methods of assigning ourselves to patients: call schedules, load balancing across practice partners—even the cherished concept of continuity is a force that can be at odds with geography as the driver. The way to approach the transition to unit-based teams is to have an honest dialogue. Why do we come to work in the hospital every day? If it’s to serve physician needs first, the old model deserves our loyalty. But if the needs of our patients and families are our focus, then we should embrace models that enable us to work effectively together, to become a great team.
Q: How have ACUs performed so far?
A: In the highest-acuity ACUs, we’ve seen mortality reductions of nearly 50%. In addition, there is a wide range of anecdotal outcomes reported. Most ACUs appear to be seeing reductions in length of stay and improvements in patient satisfaction and employee engagement. One ACU reports significant reductions in average cost per patient per day. Another ACU in a geriatric unit has seen dramatic reductions in falls. Some ACUs have seen improvements in glycemic control and VTE prophylaxis, and reductions in catheter utilization.
The benefits of the model seem to be many and probably depend on the patient population, severity of illness, baseline level of performance, and the focus and ability of the unit leadership team to get the most out of the model.
Q: Will ACUs or ACU features become de rigueur in a transformed healthcare landscape?
A: It’s hard to imagine a reality where features of ACUs do not become the standard of care. Once patients and professionals experience the impact of the ACU model, there’ll be no going back. It feels like exactly what we should be doing together. Several ACU design features are reinforced pretty cogently by Richard Bohmer in a New England Journal of Medicine perspective called “The Four Habits of High-Value Health Care Organizations.”1
Q: Any final thoughts?
A: I did not imagine my career as a QI practitioner at Emory becoming so immersed in social and industrial engineering. Of course, it’s obvious to me now that it’s happened, but six years ago when I first started directing SHM’s quality course, I thought the future in HM was health IT and real-time dashboards. Now I know those things will be important, but only if we first figure out how to get our frontline interdisciplinary clinicians to work as an effective team.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
Reference
It has been a couple of years since Jason Stein, MD, SFHM, a hospitalist at Emory University School of Medicine in Atlanta, first reported on his experience with accountable care units (ACUs) and structured interdisciplinary bedside rounds (SIBR). With ACUs, Jason and his team undertook an “extreme makeover” of care on the hospital ward. Because most hospitalist groups are endeavoring to address team-based care, I took the opportunity to catch up with and learn from Jason, who has created an exciting and compelling approach to multidisciplinary, collaborative care in the hospital.
In 2012, Jason’s team won SHM’s Excellence in Teamwork in Quality Improvement Award, and Jason was selected as an innovation advisor to the Center for Medicare and Medicaid Innovation. Since then, ACUs and SIBR have been implemented at a number of sites in the U.S. and abroad, and the work has been referenced by the Agency for Healthcare Research and Quality and the Harvard Business Review. Jason has created Centripital, a nonprofit that trains members of the hospital team to collaborate optimally around the patient and family, the central focus of care.
Here are some excerpts from my interview with Jason:
Question: What is an accountable care unit (ACU)?
Answer: We defined an ACU as a geographic inpatient care area consistently responsible for the clinical, service, and cost outcomes it produces. There are four essential design features of ACUs: 1) unit-based physician teams; 2) structured interdisciplinary bedside rounds, or SIBR; 3) unit-level performance reports; and 4) unit co-management by nurse and physician directors.
Q: What were you observing in the care of the hospitalized patient that led you to create ACUs?
A: We saw fragmentation. We saw weak cohesiveness and poor communication among doctors, nurses, and allied health professionals. HM physicians who travel all over the hospital seeing patients are living with an illusion of teamwork. In reality, to be a high-functioning team, physicians have to share time, space, and a standard way to work together with nurses, patients, and families. When we embraced this way of thinking, we realized we could be so much better than we were. The key was to re-engineer a way to really work together.
Q: What makes an ACU successful?
A: In a word, control. An ACU creates new control levers for all of the key players to have greater influence on other members of the team—nurses with doctors, doctors with nurses, patients with everyone, and vice versa. It’s actually quite simple how this happens. The ACU clinical team spends the day together, caring for the same group of patients. Everyone communicates face to face, rather than by page, text, or phone. Stronger relationships are built, and clinicians are more respectful of one another. A different level of responsiveness and accountability is created. The feeling that every person is accountable to the patient and to the other team members allows the team to gain greater control over what happens on the unit. That’s a very powerful dynamic.
SIBR further reinforces the mutual accountability on an ACU. During SIBR, each person has a chance to hear and be heard, to share their perspective, and to contribute to the care plan. Day after day, SIBR creates a positive, collaborative culture of patient care. Once clinicians realize how much control and how much self-actualization they gain on an ACU, it seems impossible to go back to the old way.

—Jason Stein, MD, SFHM
Q: What is the biggest challenge in implementing and sustaining an ACU?
A: The first challenge, of course, is that this is change. And up front—before they realize they will actually gain greater control from the ACU-SIBR model—nurses and, particularly, doctors can perceive this change as a loss of control. “You’re telling me I have to SIBR every morning? At what time? And I have to do all my primary data gathering, including a patient interview and physical exam, before SIBR? Let me stop you right there. I’m way too busy for that.”
Naturally, not everyone immediately sees that they can gain rather than lose efficiency.
Another challenge is the logistics of implementing and then maintaining unit-based physician teams. There are multiple forces that can make geographic units a challenge to create and sustain, but all the logistics are manageable.
Q: How have you helped hospitals transition from a physician-centric model to the geographic-based model?
A: The most important factor in transitioning to an ACU model is for physicians to come to terms with the reality that geography must be the primary driver of physician assignments to patients. Nurses figured this out a long time ago. Do any of us know, bedside nurses who care for patients on multiple different units? As physicians, we’re due for the same realization.
But this means sacrificing long-practiced physician-centric methods of assigning ourselves to patients: call schedules, load balancing across practice partners—even the cherished concept of continuity is a force that can be at odds with geography as the driver. The way to approach the transition to unit-based teams is to have an honest dialogue. Why do we come to work in the hospital every day? If it’s to serve physician needs first, the old model deserves our loyalty. But if the needs of our patients and families are our focus, then we should embrace models that enable us to work effectively together, to become a great team.
Q: How have ACUs performed so far?
A: In the highest-acuity ACUs, we’ve seen mortality reductions of nearly 50%. In addition, there is a wide range of anecdotal outcomes reported. Most ACUs appear to be seeing reductions in length of stay and improvements in patient satisfaction and employee engagement. One ACU reports significant reductions in average cost per patient per day. Another ACU in a geriatric unit has seen dramatic reductions in falls. Some ACUs have seen improvements in glycemic control and VTE prophylaxis, and reductions in catheter utilization.
The benefits of the model seem to be many and probably depend on the patient population, severity of illness, baseline level of performance, and the focus and ability of the unit leadership team to get the most out of the model.
Q: Will ACUs or ACU features become de rigueur in a transformed healthcare landscape?
A: It’s hard to imagine a reality where features of ACUs do not become the standard of care. Once patients and professionals experience the impact of the ACU model, there’ll be no going back. It feels like exactly what we should be doing together. Several ACU design features are reinforced pretty cogently by Richard Bohmer in a New England Journal of Medicine perspective called “The Four Habits of High-Value Health Care Organizations.”1
Q: Any final thoughts?
A: I did not imagine my career as a QI practitioner at Emory becoming so immersed in social and industrial engineering. Of course, it’s obvious to me now that it’s happened, but six years ago when I first started directing SHM’s quality course, I thought the future in HM was health IT and real-time dashboards. Now I know those things will be important, but only if we first figure out how to get our frontline interdisciplinary clinicians to work as an effective team.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
Reference
Hospitalist Pay Shifts from Volume to Value with Global Payment System
The move to paying hospitals and physicians based on value instead of volume is well underway. As programs ultimately designed to offer a global payment for a population (ACOs) or an episode of care (bundled payment) expand, we are left with this paradox: How do we reward physicians for working harder and seeing more patients under a global payment system that encourages physicians and hospitals to do less?
It appears that the existing fee-for-service payment system will need to form the scaffolding of any new, value-based system. Physicians must document the services they provide, leaving a “footprint” that can be recognized and rewarded. Without a record of the volume of services, physicians will have no incentive to see more patients during times of increased demand. This is what we often experience with straight-salary arrangements—physicians question why they should work harder for no additional compensation.
Through the ACO lens, Bruce Landon, professor of health care policy at Harvard Medical School, states the challenge in a different way: “The fundamental questions become how ACOs will divide their global budgets and how their physicians and service providers will be reimbursed. Thus, this system for determining who has earned what portion of payments—keeping score—is likely to be crucially important to the success of these new models of care.”1
In another article addressing value-based payment for physicians, Eric Stecker, MD, MPH, and Steve Schroeder, MD, argue that, due to their longevity and resilience, relative value units (RVUs), instead of physician-level capitation, straight salary, or salary with pay for performance incentives, should be the preferred mechanism to reimburse physicians based on value.2
I’d like to further develop the idea of an RVU-centric approach to value-based physician reimbursement, specifically discussing the case of hospitalists.
In Table 1, I provide examples of “value-based elements” to be added to an RVU reimbursement system. I chose measures related to three hospital-based quality programs: readmission reduction, hospital-acquired conditions, and value-based purchasing; however, one could choose hospitalist-relevant quality measures from other programs, such as ACOs, meaningful use, outpatient quality reporting (for observation patients), bundled payments, or a broad range of other domains. I selected only process measures, because outcome measures such as mortality or readmission rates suffer from sample size that is too small and risk adjustment too inadequate to be applied to individual physician payment.
Drs. Stecker and Schroeder offer an observation that is especially important to hospitalists: “Although RVUs are traditionally used for episodes of care provided by individual clinicians for individual patients, activities linked to RVUs could be more broadly defined to include team-based and supervisory clinical activities as well.”2 In the table, I include “multidisciplinary discharge planning rounds” as a potential measure. One can envision other team-based or supervisory activities involving hospitalists collaborating with nurses, pharmacists, or case managers working on a catheter-UTI bundle, high-risk medication counseling, or readmission risk assessment—with each activity linked to RVUs.
The implementation of an RVU system incorporating quality measures would be aided by documentation templates in the electronic medical record, similar to templates emerging for care bundles like central line blood stream infection. Value-based RVUs would have challenges, such as the need to change the measures over time and the system gaming inherent in any incentive design. Details of implementing the program would need to be worked out, such as attributing measures to individual physicians/providers or limiting to one the number of times certain measures are fulfilled per hospitalization.
Once established, a value-based RVU system could replace the complex and variable physician compensation landscape that exists today. As has always been the case, an RVU system could form the basis of a production incentive. Such a system could be implemented on existing billing software systems, would not require additional resources to administer, and is likely to find acceptance among hospitalists, because it is something most are already accustomed to.
Current efforts to pay physicians based on value are facing substantial headwinds. The Value-Based Payment Modifier has been criticized for being too complex, while the Physician Quality Reporting System, in place since 2007, has been plagued by a “dismal” adoption rate by physicians and has been noted to “reflect a vanishingly small part of professional activities in most clinical specialties.”3 The time may be right to rethink physician value-based payment and integrate it into the existing, time-honored RVU payment system.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
- Landon BE. Keeping score under a global payment system. N Engl J Med. 2012;366(5):393-395.
- Stecker EC, Schroeder SA. Adding value to relative-value units. N Engl J Med. 2013;369(23):2176-2179.
- Berenson RA, Kaye DR. Grading a physician’s value — the misapplication of performance measurement. N Engl J Med. 2013;369(22):2079-2078.
The move to paying hospitals and physicians based on value instead of volume is well underway. As programs ultimately designed to offer a global payment for a population (ACOs) or an episode of care (bundled payment) expand, we are left with this paradox: How do we reward physicians for working harder and seeing more patients under a global payment system that encourages physicians and hospitals to do less?
It appears that the existing fee-for-service payment system will need to form the scaffolding of any new, value-based system. Physicians must document the services they provide, leaving a “footprint” that can be recognized and rewarded. Without a record of the volume of services, physicians will have no incentive to see more patients during times of increased demand. This is what we often experience with straight-salary arrangements—physicians question why they should work harder for no additional compensation.
Through the ACO lens, Bruce Landon, professor of health care policy at Harvard Medical School, states the challenge in a different way: “The fundamental questions become how ACOs will divide their global budgets and how their physicians and service providers will be reimbursed. Thus, this system for determining who has earned what portion of payments—keeping score—is likely to be crucially important to the success of these new models of care.”1
In another article addressing value-based payment for physicians, Eric Stecker, MD, MPH, and Steve Schroeder, MD, argue that, due to their longevity and resilience, relative value units (RVUs), instead of physician-level capitation, straight salary, or salary with pay for performance incentives, should be the preferred mechanism to reimburse physicians based on value.2
I’d like to further develop the idea of an RVU-centric approach to value-based physician reimbursement, specifically discussing the case of hospitalists.
In Table 1, I provide examples of “value-based elements” to be added to an RVU reimbursement system. I chose measures related to three hospital-based quality programs: readmission reduction, hospital-acquired conditions, and value-based purchasing; however, one could choose hospitalist-relevant quality measures from other programs, such as ACOs, meaningful use, outpatient quality reporting (for observation patients), bundled payments, or a broad range of other domains. I selected only process measures, because outcome measures such as mortality or readmission rates suffer from sample size that is too small and risk adjustment too inadequate to be applied to individual physician payment.
Drs. Stecker and Schroeder offer an observation that is especially important to hospitalists: “Although RVUs are traditionally used for episodes of care provided by individual clinicians for individual patients, activities linked to RVUs could be more broadly defined to include team-based and supervisory clinical activities as well.”2 In the table, I include “multidisciplinary discharge planning rounds” as a potential measure. One can envision other team-based or supervisory activities involving hospitalists collaborating with nurses, pharmacists, or case managers working on a catheter-UTI bundle, high-risk medication counseling, or readmission risk assessment—with each activity linked to RVUs.
The implementation of an RVU system incorporating quality measures would be aided by documentation templates in the electronic medical record, similar to templates emerging for care bundles like central line blood stream infection. Value-based RVUs would have challenges, such as the need to change the measures over time and the system gaming inherent in any incentive design. Details of implementing the program would need to be worked out, such as attributing measures to individual physicians/providers or limiting to one the number of times certain measures are fulfilled per hospitalization.
Once established, a value-based RVU system could replace the complex and variable physician compensation landscape that exists today. As has always been the case, an RVU system could form the basis of a production incentive. Such a system could be implemented on existing billing software systems, would not require additional resources to administer, and is likely to find acceptance among hospitalists, because it is something most are already accustomed to.
Current efforts to pay physicians based on value are facing substantial headwinds. The Value-Based Payment Modifier has been criticized for being too complex, while the Physician Quality Reporting System, in place since 2007, has been plagued by a “dismal” adoption rate by physicians and has been noted to “reflect a vanishingly small part of professional activities in most clinical specialties.”3 The time may be right to rethink physician value-based payment and integrate it into the existing, time-honored RVU payment system.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
- Landon BE. Keeping score under a global payment system. N Engl J Med. 2012;366(5):393-395.
- Stecker EC, Schroeder SA. Adding value to relative-value units. N Engl J Med. 2013;369(23):2176-2179.
- Berenson RA, Kaye DR. Grading a physician’s value — the misapplication of performance measurement. N Engl J Med. 2013;369(22):2079-2078.
The move to paying hospitals and physicians based on value instead of volume is well underway. As programs ultimately designed to offer a global payment for a population (ACOs) or an episode of care (bundled payment) expand, we are left with this paradox: How do we reward physicians for working harder and seeing more patients under a global payment system that encourages physicians and hospitals to do less?
It appears that the existing fee-for-service payment system will need to form the scaffolding of any new, value-based system. Physicians must document the services they provide, leaving a “footprint” that can be recognized and rewarded. Without a record of the volume of services, physicians will have no incentive to see more patients during times of increased demand. This is what we often experience with straight-salary arrangements—physicians question why they should work harder for no additional compensation.
Through the ACO lens, Bruce Landon, professor of health care policy at Harvard Medical School, states the challenge in a different way: “The fundamental questions become how ACOs will divide their global budgets and how their physicians and service providers will be reimbursed. Thus, this system for determining who has earned what portion of payments—keeping score—is likely to be crucially important to the success of these new models of care.”1
In another article addressing value-based payment for physicians, Eric Stecker, MD, MPH, and Steve Schroeder, MD, argue that, due to their longevity and resilience, relative value units (RVUs), instead of physician-level capitation, straight salary, or salary with pay for performance incentives, should be the preferred mechanism to reimburse physicians based on value.2
I’d like to further develop the idea of an RVU-centric approach to value-based physician reimbursement, specifically discussing the case of hospitalists.
In Table 1, I provide examples of “value-based elements” to be added to an RVU reimbursement system. I chose measures related to three hospital-based quality programs: readmission reduction, hospital-acquired conditions, and value-based purchasing; however, one could choose hospitalist-relevant quality measures from other programs, such as ACOs, meaningful use, outpatient quality reporting (for observation patients), bundled payments, or a broad range of other domains. I selected only process measures, because outcome measures such as mortality or readmission rates suffer from sample size that is too small and risk adjustment too inadequate to be applied to individual physician payment.
Drs. Stecker and Schroeder offer an observation that is especially important to hospitalists: “Although RVUs are traditionally used for episodes of care provided by individual clinicians for individual patients, activities linked to RVUs could be more broadly defined to include team-based and supervisory clinical activities as well.”2 In the table, I include “multidisciplinary discharge planning rounds” as a potential measure. One can envision other team-based or supervisory activities involving hospitalists collaborating with nurses, pharmacists, or case managers working on a catheter-UTI bundle, high-risk medication counseling, or readmission risk assessment—with each activity linked to RVUs.
The implementation of an RVU system incorporating quality measures would be aided by documentation templates in the electronic medical record, similar to templates emerging for care bundles like central line blood stream infection. Value-based RVUs would have challenges, such as the need to change the measures over time and the system gaming inherent in any incentive design. Details of implementing the program would need to be worked out, such as attributing measures to individual physicians/providers or limiting to one the number of times certain measures are fulfilled per hospitalization.
Once established, a value-based RVU system could replace the complex and variable physician compensation landscape that exists today. As has always been the case, an RVU system could form the basis of a production incentive. Such a system could be implemented on existing billing software systems, would not require additional resources to administer, and is likely to find acceptance among hospitalists, because it is something most are already accustomed to.
Current efforts to pay physicians based on value are facing substantial headwinds. The Value-Based Payment Modifier has been criticized for being too complex, while the Physician Quality Reporting System, in place since 2007, has been plagued by a “dismal” adoption rate by physicians and has been noted to “reflect a vanishingly small part of professional activities in most clinical specialties.”3 The time may be right to rethink physician value-based payment and integrate it into the existing, time-honored RVU payment system.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
- Landon BE. Keeping score under a global payment system. N Engl J Med. 2012;366(5):393-395.
- Stecker EC, Schroeder SA. Adding value to relative-value units. N Engl J Med. 2013;369(23):2176-2179.
- Berenson RA, Kaye DR. Grading a physician’s value — the misapplication of performance measurement. N Engl J Med. 2013;369(22):2079-2078.
Beware Mid-Career
Middle age is typically a difficult passage for many professionals. It is a developmental phase involving the mourning of lost opportunities and the acceptance of one’s limits. One also reflects on his or her identity, takes note of regrets, and reevaluates how one will apportion time in the future.—Glen Gabbard, MD1
Hospital medicine is a relatively young specialty, but we are growing up, with many hospitalists now firmly in the middle phase of their careers. In 1999, 15% of our peers had been hospitalists for more than five years; by 2010, that number had grown to 50%.2 As the ranks of hospitalists grow older, we are faced with questions reflecting a life station marked by a little more wisdom, a few more gray hairs, and an occasional reflection on the legacy we will leave.
Drybye and colleagues recently released further analysis on a survey that had been previously reported, shedding new light on mid-career physician satisfaction and burnout and revealing important implications for hospital medicine.3 The study looked at responses to the Maslach Burnout Inventory for physicians from a range of specialties who had been in practice 10 years or less (early career), 11 to 20 years (mid-career), and 21 years or more (late career).
The study demonstrated that while early and late career have their challenges, middle career is a particularly difficult time for physicians. Mid-career physicians had the lowest satisfaction with their specialty choice and their work-life balance and the highest rates of emotional exhaustion and burnout. Strikingly, mid-career physicians were more than twice as likely as those in early and late career to plan to leave the practice of medicine for reasons other than retirement in the next 24 months.
What does this mean for hospital medicine? Because the survey findings are drawn from multiple specialties, we must use caution in extrapolating the results to hospitalists; however, if hospitalists are leaving the specialty mid-career, a more pressing problem may exist for hospital medicine than for other specialties. Why? First, the specialty has grown so rapidly over the last 15 years that it has been difficult to generate a sufficient supply of physicians to meet the demand. If a large number of mid-career hospitalists leave the specialty, our field may be stuck in a state of “arrested development” without the sufficient presence of mature clinicians. Second, effective hospitalists possess “system” skills that are learned on the job, so seasoned hospitalists often play an integrative and problem-solving role within the hospital. Third, there could be a downward spiral of career satisfaction in the specialty if onlookers like trainees and stakeholders in the healthcare ecosystem see hospitalists as dissatisfied and disengaged. Will the promise of hospital medicine be fulfilled?
In an accompanying editorial, Spinelli suggests three principles for physician well-being, which hospitalist programs would do well to consider:4
- Elevate well-being metrics to the same level of importance as financial, quality, and patient satisfaction metrics. (Place such metrics on the organizational dashboard.)
- Design system and care processes that include intentional plans for physician and staff wellness. (Redesign of care models and workflows should consider physician and staff wellness.)
- Adopt a robust set of self-care strategies for those experiencing burnout.
SHM’s Role
SHM has taken up the issue of hospitalist career satisfaction on a number of occasions over the years, initially engendered by field observations of the stressful nature of hospitalist work and a 2001 study reporting that 25% of hospitalists were “at risk” of burnout and 13% were “burned out.”5 Subsequently, SHM released a white paper with a number of specific recommendations organized around a career satisfaction framework consisting of autonomy, reward/recognition, occupational solidarity, and connection with one’s professional and broader community.6
Recently, the SHM Practice Management Committee has once again taken up the issue of “physician engagement.” Over the next few months, the committee plans to:
- Create a repository of related resources on the SHM website, including physician engagement profiles for some hospitalist practices;
- Initiate a dialogue on the topic of physician engagement on HMX (connect.hospitalmedicine.org), SHM’s social networking platform; and
- Publish a “public domain” survey questionnaire that hospitalist practices can use. This is a crucial matter that remains a central concern for our specialty and for the safety and well-being of our patients.
Conclusion
The Institute for Healthcare Improvement advanced the idea of the Triple Aim (better care, better health, lower costs) several years ago as a guiding principle in the transformation of healthcare. More recently, a growing number of voices suggest that physician satisfaction is a crucial foundation of the Triple Aim.4 I submit that for hospitalists to fulfill their potential as healthcare change agents, we will need to build a professional experience that enables them to traverse mid-career challenges and make it to the professional finish line as engaged and well-adjusted members of the healthcare community.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
- Gabbard GO. Medicine and its discontents. Mayo Clin Proc. 2013;88(12):1347-1349.
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: Toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Drybye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358-1367.
- Spinelli WM. The phantom limb of the triple aim. Mayo Clin Proc. 2013;88(12):1356-1357.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- Society of Hospital Medicine. A challenge for a new specialty: a white paper on hospitalist career satisfaction. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Publications/WhitePapers/White_Papers.htm. Accessed January 4, 2014.
Middle age is typically a difficult passage for many professionals. It is a developmental phase involving the mourning of lost opportunities and the acceptance of one’s limits. One also reflects on his or her identity, takes note of regrets, and reevaluates how one will apportion time in the future.—Glen Gabbard, MD1
Hospital medicine is a relatively young specialty, but we are growing up, with many hospitalists now firmly in the middle phase of their careers. In 1999, 15% of our peers had been hospitalists for more than five years; by 2010, that number had grown to 50%.2 As the ranks of hospitalists grow older, we are faced with questions reflecting a life station marked by a little more wisdom, a few more gray hairs, and an occasional reflection on the legacy we will leave.
Drybye and colleagues recently released further analysis on a survey that had been previously reported, shedding new light on mid-career physician satisfaction and burnout and revealing important implications for hospital medicine.3 The study looked at responses to the Maslach Burnout Inventory for physicians from a range of specialties who had been in practice 10 years or less (early career), 11 to 20 years (mid-career), and 21 years or more (late career).
The study demonstrated that while early and late career have their challenges, middle career is a particularly difficult time for physicians. Mid-career physicians had the lowest satisfaction with their specialty choice and their work-life balance and the highest rates of emotional exhaustion and burnout. Strikingly, mid-career physicians were more than twice as likely as those in early and late career to plan to leave the practice of medicine for reasons other than retirement in the next 24 months.
What does this mean for hospital medicine? Because the survey findings are drawn from multiple specialties, we must use caution in extrapolating the results to hospitalists; however, if hospitalists are leaving the specialty mid-career, a more pressing problem may exist for hospital medicine than for other specialties. Why? First, the specialty has grown so rapidly over the last 15 years that it has been difficult to generate a sufficient supply of physicians to meet the demand. If a large number of mid-career hospitalists leave the specialty, our field may be stuck in a state of “arrested development” without the sufficient presence of mature clinicians. Second, effective hospitalists possess “system” skills that are learned on the job, so seasoned hospitalists often play an integrative and problem-solving role within the hospital. Third, there could be a downward spiral of career satisfaction in the specialty if onlookers like trainees and stakeholders in the healthcare ecosystem see hospitalists as dissatisfied and disengaged. Will the promise of hospital medicine be fulfilled?
In an accompanying editorial, Spinelli suggests three principles for physician well-being, which hospitalist programs would do well to consider:4
- Elevate well-being metrics to the same level of importance as financial, quality, and patient satisfaction metrics. (Place such metrics on the organizational dashboard.)
- Design system and care processes that include intentional plans for physician and staff wellness. (Redesign of care models and workflows should consider physician and staff wellness.)
- Adopt a robust set of self-care strategies for those experiencing burnout.
SHM’s Role
SHM has taken up the issue of hospitalist career satisfaction on a number of occasions over the years, initially engendered by field observations of the stressful nature of hospitalist work and a 2001 study reporting that 25% of hospitalists were “at risk” of burnout and 13% were “burned out.”5 Subsequently, SHM released a white paper with a number of specific recommendations organized around a career satisfaction framework consisting of autonomy, reward/recognition, occupational solidarity, and connection with one’s professional and broader community.6
Recently, the SHM Practice Management Committee has once again taken up the issue of “physician engagement.” Over the next few months, the committee plans to:
- Create a repository of related resources on the SHM website, including physician engagement profiles for some hospitalist practices;
- Initiate a dialogue on the topic of physician engagement on HMX (connect.hospitalmedicine.org), SHM’s social networking platform; and
- Publish a “public domain” survey questionnaire that hospitalist practices can use. This is a crucial matter that remains a central concern for our specialty and for the safety and well-being of our patients.
Conclusion
The Institute for Healthcare Improvement advanced the idea of the Triple Aim (better care, better health, lower costs) several years ago as a guiding principle in the transformation of healthcare. More recently, a growing number of voices suggest that physician satisfaction is a crucial foundation of the Triple Aim.4 I submit that for hospitalists to fulfill their potential as healthcare change agents, we will need to build a professional experience that enables them to traverse mid-career challenges and make it to the professional finish line as engaged and well-adjusted members of the healthcare community.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
- Gabbard GO. Medicine and its discontents. Mayo Clin Proc. 2013;88(12):1347-1349.
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: Toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Drybye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358-1367.
- Spinelli WM. The phantom limb of the triple aim. Mayo Clin Proc. 2013;88(12):1356-1357.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- Society of Hospital Medicine. A challenge for a new specialty: a white paper on hospitalist career satisfaction. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Publications/WhitePapers/White_Papers.htm. Accessed January 4, 2014.
Middle age is typically a difficult passage for many professionals. It is a developmental phase involving the mourning of lost opportunities and the acceptance of one’s limits. One also reflects on his or her identity, takes note of regrets, and reevaluates how one will apportion time in the future.—Glen Gabbard, MD1
Hospital medicine is a relatively young specialty, but we are growing up, with many hospitalists now firmly in the middle phase of their careers. In 1999, 15% of our peers had been hospitalists for more than five years; by 2010, that number had grown to 50%.2 As the ranks of hospitalists grow older, we are faced with questions reflecting a life station marked by a little more wisdom, a few more gray hairs, and an occasional reflection on the legacy we will leave.
Drybye and colleagues recently released further analysis on a survey that had been previously reported, shedding new light on mid-career physician satisfaction and burnout and revealing important implications for hospital medicine.3 The study looked at responses to the Maslach Burnout Inventory for physicians from a range of specialties who had been in practice 10 years or less (early career), 11 to 20 years (mid-career), and 21 years or more (late career).
The study demonstrated that while early and late career have their challenges, middle career is a particularly difficult time for physicians. Mid-career physicians had the lowest satisfaction with their specialty choice and their work-life balance and the highest rates of emotional exhaustion and burnout. Strikingly, mid-career physicians were more than twice as likely as those in early and late career to plan to leave the practice of medicine for reasons other than retirement in the next 24 months.
What does this mean for hospital medicine? Because the survey findings are drawn from multiple specialties, we must use caution in extrapolating the results to hospitalists; however, if hospitalists are leaving the specialty mid-career, a more pressing problem may exist for hospital medicine than for other specialties. Why? First, the specialty has grown so rapidly over the last 15 years that it has been difficult to generate a sufficient supply of physicians to meet the demand. If a large number of mid-career hospitalists leave the specialty, our field may be stuck in a state of “arrested development” without the sufficient presence of mature clinicians. Second, effective hospitalists possess “system” skills that are learned on the job, so seasoned hospitalists often play an integrative and problem-solving role within the hospital. Third, there could be a downward spiral of career satisfaction in the specialty if onlookers like trainees and stakeholders in the healthcare ecosystem see hospitalists as dissatisfied and disengaged. Will the promise of hospital medicine be fulfilled?
In an accompanying editorial, Spinelli suggests three principles for physician well-being, which hospitalist programs would do well to consider:4
- Elevate well-being metrics to the same level of importance as financial, quality, and patient satisfaction metrics. (Place such metrics on the organizational dashboard.)
- Design system and care processes that include intentional plans for physician and staff wellness. (Redesign of care models and workflows should consider physician and staff wellness.)
- Adopt a robust set of self-care strategies for those experiencing burnout.
SHM’s Role
SHM has taken up the issue of hospitalist career satisfaction on a number of occasions over the years, initially engendered by field observations of the stressful nature of hospitalist work and a 2001 study reporting that 25% of hospitalists were “at risk” of burnout and 13% were “burned out.”5 Subsequently, SHM released a white paper with a number of specific recommendations organized around a career satisfaction framework consisting of autonomy, reward/recognition, occupational solidarity, and connection with one’s professional and broader community.6
Recently, the SHM Practice Management Committee has once again taken up the issue of “physician engagement.” Over the next few months, the committee plans to:
- Create a repository of related resources on the SHM website, including physician engagement profiles for some hospitalist practices;
- Initiate a dialogue on the topic of physician engagement on HMX (connect.hospitalmedicine.org), SHM’s social networking platform; and
- Publish a “public domain” survey questionnaire that hospitalist practices can use. This is a crucial matter that remains a central concern for our specialty and for the safety and well-being of our patients.
Conclusion
The Institute for Healthcare Improvement advanced the idea of the Triple Aim (better care, better health, lower costs) several years ago as a guiding principle in the transformation of healthcare. More recently, a growing number of voices suggest that physician satisfaction is a crucial foundation of the Triple Aim.4 I submit that for hospitalists to fulfill their potential as healthcare change agents, we will need to build a professional experience that enables them to traverse mid-career challenges and make it to the professional finish line as engaged and well-adjusted members of the healthcare community.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
- Gabbard GO. Medicine and its discontents. Mayo Clin Proc. 2013;88(12):1347-1349.
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: Toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Drybye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358-1367.
- Spinelli WM. The phantom limb of the triple aim. Mayo Clin Proc. 2013;88(12):1356-1357.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- Society of Hospital Medicine. A challenge for a new specialty: a white paper on hospitalist career satisfaction. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Publications/WhitePapers/White_Papers.htm. Accessed January 4, 2014.
Performance Evaluation Program for Individual Physicians Directional at Best
What makes a great doctor? Heck if I know. Maybe it’s like pornography. A great physician, well, “You know one when you see one.” That approach worked from the time of Hippocrates until the recent past, when the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and others embarked on programs to measure and report physician quality. Of course, bodies like the American Board of Internal Medicine have been certifying physicians for a long time.
Ongoing Professional Practice Evaluation (OPPE) is one such measurement program, now over four years old, with standards put forth by the Joint Commission in an effort to monitor individual physician—and non-physician provider—performance across a number of domains. The program requires accredited hospitals to monitor and report performance to the physician/provider at least every 11 months, and to use such information in the credentialing process.
This year, I received two OPPE reports, causing me to reflect on how helpful these reports are in judging and improving the quality of my practice. Before I discuss some of the “grades” I received, let me start with my conclusion: Physician quality measurement is in its infancy, and the measures are at best “directional” for most physicians, including hospitalists. Some measurement is better than none at all, however, and selected measures, such as surgical site infection and other measures of harm, may be grounds for closer monitoring, or even corrective action, of a physician’s practice. Unfortunately, my stance that OPPE quality measures are “directional” might not help a physician whose privileges are on the line.
Attribution
For hospitalists, the first concern in measuring and reporting quality is, “How can I attribute quality to an individual hospitalist, when several different hospitalists see the patient?” My perspective is that unless a quality measure can be attributed to an individual hospitalist (e.g. discharge medication reconciliation), it should be attributed at the group level.
However, the OPPE program is specifically intended to address the individual physician/provider for purposes of credentialing, and group attribution is a non-starter. In my performance examples below, I believe that attributing outcomes like mortality, readmissions, or resource utilization to individual hospitalists does not make sense—and is probably unfair.
Resource Utilization
The report lists my performance (Practitioner) compared to an Internal Comparison Group for a specified time period (see Figure 1). The comparison group is described as “practitioners in your specialty...from within your health system.” My data were generated based on only 45 cases (I see patients only part time), while the comparison group was based on 4,530 cases. What I take home from this is that, for cost/resource, I look favorable in “supplies” and “pharmacy”; for most of the others, I’m expensive in comparison.
Will this change my practice? Maybe I will think twice about incurring laboratory or pharmacy costs, but I can’t say I am going to fundamentally rethink how or what I order. And I take all these data with a grain of salt, because I share responsibility for patients with several other hospitalists.
Readmissions
My 30-day readmissions performance (see Figure 2) is weak compared to the Internal Comp Group, which I defined above, and the Peer group, which in my report is defined as derived from practitioners at facilities with 501 beds or more (my facility has 700-plus beds). I accept the “directional” nature of the data, meaning that it provides a general idea but not a precise measurement, and vow to reflect on the processes underlying my approach to hospital discharge (teach back, medication reconciliation, PCP communication, and so on).
Mortality
For this category (see Figure 3), I’m looking better. The blue bar is “observed,” while the red bar is “expected.” Although my patients are sicker (higher “expected” mortality), my “observed” mortality is lower than the comparison group. I’m not sure why my observed mortality is lower, but I’m convinced that part of the reason for a higher expected mortality is that my documentation is better than the comparison group.
Will OPPE Change My Practice?
There are other data in my report, including process (core) measures, length of stay, hospital-acquired conditions, and patient flow measures. The OPPE report is but one of a growing number of physician report cards: The Massachusetts Board of Medicine, Physician Compare (CMS), and Health Grades are just a few of the organizations that have public websites reporting my performance. Perhaps at this stage, the primary impact of these reports is through the oft-invoked “Hawthorne Effect,” where subjects modify behavior simply because they are being observed, as opposed to any particular piece of feedback.
My sense is that hospitalists are particularly open to the type of feedback offered in OPPE and similar reports, as long as the data are credible, even if reflecting group level performance. The 2012 SHM State of Hospital Medicine survey shows that the percent of hospitalist compensation based on performance (other than production/billings) increased to 7% from 4% in 2011. It seems that performance measurement with consequences, be it for credentialing or compensation, is here to stay.
Dr. Whitcombis Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
What makes a great doctor? Heck if I know. Maybe it’s like pornography. A great physician, well, “You know one when you see one.” That approach worked from the time of Hippocrates until the recent past, when the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and others embarked on programs to measure and report physician quality. Of course, bodies like the American Board of Internal Medicine have been certifying physicians for a long time.
Ongoing Professional Practice Evaluation (OPPE) is one such measurement program, now over four years old, with standards put forth by the Joint Commission in an effort to monitor individual physician—and non-physician provider—performance across a number of domains. The program requires accredited hospitals to monitor and report performance to the physician/provider at least every 11 months, and to use such information in the credentialing process.
This year, I received two OPPE reports, causing me to reflect on how helpful these reports are in judging and improving the quality of my practice. Before I discuss some of the “grades” I received, let me start with my conclusion: Physician quality measurement is in its infancy, and the measures are at best “directional” for most physicians, including hospitalists. Some measurement is better than none at all, however, and selected measures, such as surgical site infection and other measures of harm, may be grounds for closer monitoring, or even corrective action, of a physician’s practice. Unfortunately, my stance that OPPE quality measures are “directional” might not help a physician whose privileges are on the line.
Attribution
For hospitalists, the first concern in measuring and reporting quality is, “How can I attribute quality to an individual hospitalist, when several different hospitalists see the patient?” My perspective is that unless a quality measure can be attributed to an individual hospitalist (e.g. discharge medication reconciliation), it should be attributed at the group level.
However, the OPPE program is specifically intended to address the individual physician/provider for purposes of credentialing, and group attribution is a non-starter. In my performance examples below, I believe that attributing outcomes like mortality, readmissions, or resource utilization to individual hospitalists does not make sense—and is probably unfair.
Resource Utilization
The report lists my performance (Practitioner) compared to an Internal Comparison Group for a specified time period (see Figure 1). The comparison group is described as “practitioners in your specialty...from within your health system.” My data were generated based on only 45 cases (I see patients only part time), while the comparison group was based on 4,530 cases. What I take home from this is that, for cost/resource, I look favorable in “supplies” and “pharmacy”; for most of the others, I’m expensive in comparison.
Will this change my practice? Maybe I will think twice about incurring laboratory or pharmacy costs, but I can’t say I am going to fundamentally rethink how or what I order. And I take all these data with a grain of salt, because I share responsibility for patients with several other hospitalists.
Readmissions
My 30-day readmissions performance (see Figure 2) is weak compared to the Internal Comp Group, which I defined above, and the Peer group, which in my report is defined as derived from practitioners at facilities with 501 beds or more (my facility has 700-plus beds). I accept the “directional” nature of the data, meaning that it provides a general idea but not a precise measurement, and vow to reflect on the processes underlying my approach to hospital discharge (teach back, medication reconciliation, PCP communication, and so on).
Mortality
For this category (see Figure 3), I’m looking better. The blue bar is “observed,” while the red bar is “expected.” Although my patients are sicker (higher “expected” mortality), my “observed” mortality is lower than the comparison group. I’m not sure why my observed mortality is lower, but I’m convinced that part of the reason for a higher expected mortality is that my documentation is better than the comparison group.
Will OPPE Change My Practice?
There are other data in my report, including process (core) measures, length of stay, hospital-acquired conditions, and patient flow measures. The OPPE report is but one of a growing number of physician report cards: The Massachusetts Board of Medicine, Physician Compare (CMS), and Health Grades are just a few of the organizations that have public websites reporting my performance. Perhaps at this stage, the primary impact of these reports is through the oft-invoked “Hawthorne Effect,” where subjects modify behavior simply because they are being observed, as opposed to any particular piece of feedback.
My sense is that hospitalists are particularly open to the type of feedback offered in OPPE and similar reports, as long as the data are credible, even if reflecting group level performance. The 2012 SHM State of Hospital Medicine survey shows that the percent of hospitalist compensation based on performance (other than production/billings) increased to 7% from 4% in 2011. It seems that performance measurement with consequences, be it for credentialing or compensation, is here to stay.
Dr. Whitcombis Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
What makes a great doctor? Heck if I know. Maybe it’s like pornography. A great physician, well, “You know one when you see one.” That approach worked from the time of Hippocrates until the recent past, when the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and others embarked on programs to measure and report physician quality. Of course, bodies like the American Board of Internal Medicine have been certifying physicians for a long time.
Ongoing Professional Practice Evaluation (OPPE) is one such measurement program, now over four years old, with standards put forth by the Joint Commission in an effort to monitor individual physician—and non-physician provider—performance across a number of domains. The program requires accredited hospitals to monitor and report performance to the physician/provider at least every 11 months, and to use such information in the credentialing process.
This year, I received two OPPE reports, causing me to reflect on how helpful these reports are in judging and improving the quality of my practice. Before I discuss some of the “grades” I received, let me start with my conclusion: Physician quality measurement is in its infancy, and the measures are at best “directional” for most physicians, including hospitalists. Some measurement is better than none at all, however, and selected measures, such as surgical site infection and other measures of harm, may be grounds for closer monitoring, or even corrective action, of a physician’s practice. Unfortunately, my stance that OPPE quality measures are “directional” might not help a physician whose privileges are on the line.
Attribution
For hospitalists, the first concern in measuring and reporting quality is, “How can I attribute quality to an individual hospitalist, when several different hospitalists see the patient?” My perspective is that unless a quality measure can be attributed to an individual hospitalist (e.g. discharge medication reconciliation), it should be attributed at the group level.
However, the OPPE program is specifically intended to address the individual physician/provider for purposes of credentialing, and group attribution is a non-starter. In my performance examples below, I believe that attributing outcomes like mortality, readmissions, or resource utilization to individual hospitalists does not make sense—and is probably unfair.
Resource Utilization
The report lists my performance (Practitioner) compared to an Internal Comparison Group for a specified time period (see Figure 1). The comparison group is described as “practitioners in your specialty...from within your health system.” My data were generated based on only 45 cases (I see patients only part time), while the comparison group was based on 4,530 cases. What I take home from this is that, for cost/resource, I look favorable in “supplies” and “pharmacy”; for most of the others, I’m expensive in comparison.
Will this change my practice? Maybe I will think twice about incurring laboratory or pharmacy costs, but I can’t say I am going to fundamentally rethink how or what I order. And I take all these data with a grain of salt, because I share responsibility for patients with several other hospitalists.
Readmissions
My 30-day readmissions performance (see Figure 2) is weak compared to the Internal Comp Group, which I defined above, and the Peer group, which in my report is defined as derived from practitioners at facilities with 501 beds or more (my facility has 700-plus beds). I accept the “directional” nature of the data, meaning that it provides a general idea but not a precise measurement, and vow to reflect on the processes underlying my approach to hospital discharge (teach back, medication reconciliation, PCP communication, and so on).
Mortality
For this category (see Figure 3), I’m looking better. The blue bar is “observed,” while the red bar is “expected.” Although my patients are sicker (higher “expected” mortality), my “observed” mortality is lower than the comparison group. I’m not sure why my observed mortality is lower, but I’m convinced that part of the reason for a higher expected mortality is that my documentation is better than the comparison group.
Will OPPE Change My Practice?
There are other data in my report, including process (core) measures, length of stay, hospital-acquired conditions, and patient flow measures. The OPPE report is but one of a growing number of physician report cards: The Massachusetts Board of Medicine, Physician Compare (CMS), and Health Grades are just a few of the organizations that have public websites reporting my performance. Perhaps at this stage, the primary impact of these reports is through the oft-invoked “Hawthorne Effect,” where subjects modify behavior simply because they are being observed, as opposed to any particular piece of feedback.
My sense is that hospitalists are particularly open to the type of feedback offered in OPPE and similar reports, as long as the data are credible, even if reflecting group level performance. The 2012 SHM State of Hospital Medicine survey shows that the percent of hospitalist compensation based on performance (other than production/billings) increased to 7% from 4% in 2011. It seems that performance measurement with consequences, be it for credentialing or compensation, is here to stay.
Dr. Whitcombis Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
Workflow Interruptions Threaten Patient Safety, Hospitalists' Job Satisfaction
When I visit hospitalist programs, one of the things I am most interested in learning about is the degree to which the hospitalists enjoy their work and why. On a recent visit, in my usual meeting with the hospitalist group, we talked a lot about what it is like to be a hospitalist. When I asked them what the greatest threat to their job satisfaction was, there was a chorus of consistency in their answers: interruptions. The hospitalists were deeply frustrated by minute-to-minute intrusions into their workflow. The emergency department, nurses, pharmacy, the admitting department, the lab, radiology—you name it, everyone wants a piece of them.
Constant interruptions are a career satisfaction issue for hospitalists. But for patients, the interruptions represent a safety and quality of care issue. Why?
The Myth of Multi-tasking
Some of us take pride in our ability to multi-task. Others freely admit they aren’t very good at it. In any case, we know through cognitive psychology that the brain cannot multi-task, at least in the realm of conscious work. (The brain, of course, carries out basic, life-sustaining functions while we are doing other work cognitively.) The brain is actually a “sequential processor,” and multi-tasking actually is “task-switching.” Those of us who “multi-task” well are able to switch tasks easily and effectively.
But, task switching comes at a cost. When we switch tasks, we are prone to errors in the performance of those tasks. Two psychologists, Rogers and Monsell, demonstrated this in a study that looked at error rates when subjects performed tasks involving numerical or letter manipulations.1 The tasks involved classifying either the digit member of a pair of characters as even/odd or the letter member as consonant/vowel. When subjects performed the tasks while switching among multiple tasks, the error rate was fourfold the rate with no task switching (see Figure 1).1 These findings have been replicated since the original study. Further, there is now well-developed literature devoted to interruptions and patient safety.
It Takes Time
We also know that switching between tasks takes time. Why? Because changing one’s attention from one subject to another involves neurologic processes that are not instantaneous. In a simulated driving study comparing mean reaction times between intoxicated subjects (blood alcohol 0.08%) and those talking on a cell phone, Strayer and Drews found the mean time to brake onset was significantly slower in the cell phone group than in the drunk driving group, presumably because cell phone users had to switch tasks.2
How Can We Tame Interruptions?
I submit that we need to be realistic about our ability to control the number of interruptions hospitalists experience in a given workday. One approach is to identify “high stakes moments” that are protected from excessive interruptions. Taking an example from aviation, airplane takeoffs and landings are “no interruption” zones, meaning that no needless talking or tasking is allowed in the cockpit during these tasks. Potential “no interruption” zones in hospital medicine might include times when hospitalists are developing an assessment and plan, engaged in complex decision-making, or performing medication reconciliation.
But is it realistic to think that we can cordon off hospitalists during these tasks?
Another approach is to establish practices that may decrease interruptions. Interruptions likely are reduced by:
- Having unit-based hospitalist staffing;
- Holding multidisciplinary rounds;
- Training nurses to batch pages;
- Conducting structured evening and night rounds on all nursing units for non-urgent matters; and
- Developing paging “levels” so that a receiving physician knows if a call back is needed and, if so, if it is urgent or not.
In talking to hospitalists who cite interruptions as job dissatisfiers, it occurs to me that anything that erodes career engagement also threatens patient safety. If we could figure out how to control interruptions, we would kill two birds with one stone.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
When I visit hospitalist programs, one of the things I am most interested in learning about is the degree to which the hospitalists enjoy their work and why. On a recent visit, in my usual meeting with the hospitalist group, we talked a lot about what it is like to be a hospitalist. When I asked them what the greatest threat to their job satisfaction was, there was a chorus of consistency in their answers: interruptions. The hospitalists were deeply frustrated by minute-to-minute intrusions into their workflow. The emergency department, nurses, pharmacy, the admitting department, the lab, radiology—you name it, everyone wants a piece of them.
Constant interruptions are a career satisfaction issue for hospitalists. But for patients, the interruptions represent a safety and quality of care issue. Why?
The Myth of Multi-tasking
Some of us take pride in our ability to multi-task. Others freely admit they aren’t very good at it. In any case, we know through cognitive psychology that the brain cannot multi-task, at least in the realm of conscious work. (The brain, of course, carries out basic, life-sustaining functions while we are doing other work cognitively.) The brain is actually a “sequential processor,” and multi-tasking actually is “task-switching.” Those of us who “multi-task” well are able to switch tasks easily and effectively.
But, task switching comes at a cost. When we switch tasks, we are prone to errors in the performance of those tasks. Two psychologists, Rogers and Monsell, demonstrated this in a study that looked at error rates when subjects performed tasks involving numerical or letter manipulations.1 The tasks involved classifying either the digit member of a pair of characters as even/odd or the letter member as consonant/vowel. When subjects performed the tasks while switching among multiple tasks, the error rate was fourfold the rate with no task switching (see Figure 1).1 These findings have been replicated since the original study. Further, there is now well-developed literature devoted to interruptions and patient safety.
It Takes Time
We also know that switching between tasks takes time. Why? Because changing one’s attention from one subject to another involves neurologic processes that are not instantaneous. In a simulated driving study comparing mean reaction times between intoxicated subjects (blood alcohol 0.08%) and those talking on a cell phone, Strayer and Drews found the mean time to brake onset was significantly slower in the cell phone group than in the drunk driving group, presumably because cell phone users had to switch tasks.2
How Can We Tame Interruptions?
I submit that we need to be realistic about our ability to control the number of interruptions hospitalists experience in a given workday. One approach is to identify “high stakes moments” that are protected from excessive interruptions. Taking an example from aviation, airplane takeoffs and landings are “no interruption” zones, meaning that no needless talking or tasking is allowed in the cockpit during these tasks. Potential “no interruption” zones in hospital medicine might include times when hospitalists are developing an assessment and plan, engaged in complex decision-making, or performing medication reconciliation.
But is it realistic to think that we can cordon off hospitalists during these tasks?
Another approach is to establish practices that may decrease interruptions. Interruptions likely are reduced by:
- Having unit-based hospitalist staffing;
- Holding multidisciplinary rounds;
- Training nurses to batch pages;
- Conducting structured evening and night rounds on all nursing units for non-urgent matters; and
- Developing paging “levels” so that a receiving physician knows if a call back is needed and, if so, if it is urgent or not.
In talking to hospitalists who cite interruptions as job dissatisfiers, it occurs to me that anything that erodes career engagement also threatens patient safety. If we could figure out how to control interruptions, we would kill two birds with one stone.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
When I visit hospitalist programs, one of the things I am most interested in learning about is the degree to which the hospitalists enjoy their work and why. On a recent visit, in my usual meeting with the hospitalist group, we talked a lot about what it is like to be a hospitalist. When I asked them what the greatest threat to their job satisfaction was, there was a chorus of consistency in their answers: interruptions. The hospitalists were deeply frustrated by minute-to-minute intrusions into their workflow. The emergency department, nurses, pharmacy, the admitting department, the lab, radiology—you name it, everyone wants a piece of them.
Constant interruptions are a career satisfaction issue for hospitalists. But for patients, the interruptions represent a safety and quality of care issue. Why?
The Myth of Multi-tasking
Some of us take pride in our ability to multi-task. Others freely admit they aren’t very good at it. In any case, we know through cognitive psychology that the brain cannot multi-task, at least in the realm of conscious work. (The brain, of course, carries out basic, life-sustaining functions while we are doing other work cognitively.) The brain is actually a “sequential processor,” and multi-tasking actually is “task-switching.” Those of us who “multi-task” well are able to switch tasks easily and effectively.
But, task switching comes at a cost. When we switch tasks, we are prone to errors in the performance of those tasks. Two psychologists, Rogers and Monsell, demonstrated this in a study that looked at error rates when subjects performed tasks involving numerical or letter manipulations.1 The tasks involved classifying either the digit member of a pair of characters as even/odd or the letter member as consonant/vowel. When subjects performed the tasks while switching among multiple tasks, the error rate was fourfold the rate with no task switching (see Figure 1).1 These findings have been replicated since the original study. Further, there is now well-developed literature devoted to interruptions and patient safety.
It Takes Time
We also know that switching between tasks takes time. Why? Because changing one’s attention from one subject to another involves neurologic processes that are not instantaneous. In a simulated driving study comparing mean reaction times between intoxicated subjects (blood alcohol 0.08%) and those talking on a cell phone, Strayer and Drews found the mean time to brake onset was significantly slower in the cell phone group than in the drunk driving group, presumably because cell phone users had to switch tasks.2
How Can We Tame Interruptions?
I submit that we need to be realistic about our ability to control the number of interruptions hospitalists experience in a given workday. One approach is to identify “high stakes moments” that are protected from excessive interruptions. Taking an example from aviation, airplane takeoffs and landings are “no interruption” zones, meaning that no needless talking or tasking is allowed in the cockpit during these tasks. Potential “no interruption” zones in hospital medicine might include times when hospitalists are developing an assessment and plan, engaged in complex decision-making, or performing medication reconciliation.
But is it realistic to think that we can cordon off hospitalists during these tasks?
Another approach is to establish practices that may decrease interruptions. Interruptions likely are reduced by:
- Having unit-based hospitalist staffing;
- Holding multidisciplinary rounds;
- Training nurses to batch pages;
- Conducting structured evening and night rounds on all nursing units for non-urgent matters; and
- Developing paging “levels” so that a receiving physician knows if a call back is needed and, if so, if it is urgent or not.
In talking to hospitalists who cite interruptions as job dissatisfiers, it occurs to me that anything that erodes career engagement also threatens patient safety. If we could figure out how to control interruptions, we would kill two birds with one stone.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
Massachusetts Hospitalists Experiment with Unit-Based Rounding
Today marks the end of the second week of a three-month experiment we are embarking on to improve team-based care. The main elements of our experiment are two early career hospitalists dedicated to a single nursing unit who are present on the unit throughout the day, structured multidisciplinary rounds, pharmacists doing medication histories to help with medical reconciliation, and a veteran hospitalist serving as a coach, broadly overseeing care coordination and throughput on the unit. (I’m going to focus on multidisciplinary care and leave the coaching part for another day.)
Many have written about and many more have tried to establish unit-based hospitalist models, where a hospitalist is assigned to a single nursing unit. These models often incorporate multidisciplinary rounds, where the hospitalist, case management, social services, physical therapy, and perhaps pharmacy meet each day and review each patient’s progress through the hospitalization. The underlying premise for establishing a unit-based model is that all, or nearly all, of the hospitalist’s patients are located on the nursing unit.
It Can’t Be That Hard
Dedicated units and multidisciplinary rounds are designed to achieve better coordination between the hospitalists and the other members of the hospital team. Most healthcare professionals intuitively support this model; however, many hospitalists have concerns.
To provide the best care for their patients while maintaining career satisfaction, these hospitalists may feel the need for flexibility—the ability to be independent and roam unrestricted through the hallways and departments of the hospital. This goal can be at odds with being limited to a single nursing unit.
For these hospitalists to support the unit-based model, there had better be good reasons for doing so.
Measuring the Effects of Teamwork
Jody Hoffer Gittell, PhD, a professor of management at Brandeis University in Waltham, Mass., has studied relational coordination extensively in healthcare and other service industries. Relational coordination can be defined as “coordinating work through relationships of shared goals, shared knowledge and mutual respect, supported by frequent, timely, accurate, problem-solving communication.”1
Dr. Gittell has developed a validated questionnaire to be completed by each member of the healthcare team, quantifying their perspective on these dimensions for others on the team. I think of relational coordination as a rigorous way of quantifying teamwork.
In 2008, Dr. Gittell published an observational study with SHM senior vice president Joe Miller and hospitalist leader Adrienne L. Bennett, MD, PhD, conducted at a suburban Boston hospital.2 The study looked at relational coordination between members of the hospital team under hospitalist care compared to traditional, PCP-based hospital care. They measured relational coordination by asking the attending physician (hospitalist or PCP providing hospital care), medical resident, floor nurse, case manager, social worker, and therapist (occupational, physical, respiratory, speech) to complete questionnaires about the other team members for a cohort of patients.
The study concluded that relational coordination between other members of the team and the physician was significantly higher for patients treated by hospitalists than for patients treated by traditional PCPs. Further, they found that as relational coordination increased, for patients treated either by hospitalists or PCPs, length of stay, cost, and 30-day readmission rates decreased. I will add that the hospitalists were not unit-based in this study, but were assumed to be more available to the care team than traditional PCPs.
Subsequent studies of multidisciplinary rounds on a “hospitalist unit” conducted by Kevin O’Leary, MD, and colleagues at Northwestern University in Chicago have demonstrated a favorable effect on nurses’ ratings of teamwork and collaboration, as well as the rate of adverse events.3,4 The former study did not, however, find decreased costs or length of stay.
Keys to Success
Before our current experiment, I’ve had the privilege to witness, both at my home institution and at a number of outside ones, many permutations of multidisciplinary rounds and unit-based hospitalists. I’ve seen failures, some mixed results, and occasional success stories. In all cases, participants seem to agree that it takes extra effort to execute on this model, especially once the initial enthusiasm wanes. So, for these arrangements to succeed over time, including our current experiment, I see the following four factors as critical:
- Multidisciplinary rounds must be tightly organized, with case manager, nurse, and hospitalist providing input concisely. Average time per patient should not exceed about three minutes. The total time for rounds, no matter how many patients are under discussion, should not exceed one hour.
- Each team member must be prepared to provide critical information for rounds. For example, hospitalists and nurses should have seen/reviewed their patients, case managers should know expected length of stay and key disposition information, and pharmacists should know medical histories and other pertinent information.
- The fundamental concern of multidisciplinary rounds—that someone’s time is being wasted (when not talking about that team member’s patient at that moment)—must be mitigated one way or another. Solutions include rotating nurses or hospitalists in and out of rounds, and allowing hospitalists to enter orders and do other discreet multitasking during rounds. Careful attention to showing up for the rounds on time and on cue is crucial.
- Hospitalist autonomy and need to roam has to be programmed in by allowing them time to get off the unit, see the broader world, and interact with colleagues.
At the conclusion of three months, as a QI project (as opposed to rigorous research), we will measure a number of things, including cost, throughput, patient satisfaction, and team member satisfaction with the model. If you have predictions, please e-mail me. I’ll report our results in a subsequent column.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. E-mail him at [email protected].
References
- Relational Coordination Research Collaborative. Brandeis University website. Available at: http://rcrc.brandeis.edu/about-rc/What%20is%20Relational%20Coordination.html. Accessed September 23, 2013.
- Gittell JH, Weinberg DB, Bennett AL, Miller JA. Is the doctor in? A relational approach to job design and the coordination of work. Hum Resource Manag J. 2008;47(4):729-755.
- O’Leary KJ, Haviley C, Slade ME, Shah HM, Lee J, Williams MV. Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88-93.
- O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678-684.
Today marks the end of the second week of a three-month experiment we are embarking on to improve team-based care. The main elements of our experiment are two early career hospitalists dedicated to a single nursing unit who are present on the unit throughout the day, structured multidisciplinary rounds, pharmacists doing medication histories to help with medical reconciliation, and a veteran hospitalist serving as a coach, broadly overseeing care coordination and throughput on the unit. (I’m going to focus on multidisciplinary care and leave the coaching part for another day.)
Many have written about and many more have tried to establish unit-based hospitalist models, where a hospitalist is assigned to a single nursing unit. These models often incorporate multidisciplinary rounds, where the hospitalist, case management, social services, physical therapy, and perhaps pharmacy meet each day and review each patient’s progress through the hospitalization. The underlying premise for establishing a unit-based model is that all, or nearly all, of the hospitalist’s patients are located on the nursing unit.
It Can’t Be That Hard
Dedicated units and multidisciplinary rounds are designed to achieve better coordination between the hospitalists and the other members of the hospital team. Most healthcare professionals intuitively support this model; however, many hospitalists have concerns.
To provide the best care for their patients while maintaining career satisfaction, these hospitalists may feel the need for flexibility—the ability to be independent and roam unrestricted through the hallways and departments of the hospital. This goal can be at odds with being limited to a single nursing unit.
For these hospitalists to support the unit-based model, there had better be good reasons for doing so.
Measuring the Effects of Teamwork
Jody Hoffer Gittell, PhD, a professor of management at Brandeis University in Waltham, Mass., has studied relational coordination extensively in healthcare and other service industries. Relational coordination can be defined as “coordinating work through relationships of shared goals, shared knowledge and mutual respect, supported by frequent, timely, accurate, problem-solving communication.”1
Dr. Gittell has developed a validated questionnaire to be completed by each member of the healthcare team, quantifying their perspective on these dimensions for others on the team. I think of relational coordination as a rigorous way of quantifying teamwork.
In 2008, Dr. Gittell published an observational study with SHM senior vice president Joe Miller and hospitalist leader Adrienne L. Bennett, MD, PhD, conducted at a suburban Boston hospital.2 The study looked at relational coordination between members of the hospital team under hospitalist care compared to traditional, PCP-based hospital care. They measured relational coordination by asking the attending physician (hospitalist or PCP providing hospital care), medical resident, floor nurse, case manager, social worker, and therapist (occupational, physical, respiratory, speech) to complete questionnaires about the other team members for a cohort of patients.
The study concluded that relational coordination between other members of the team and the physician was significantly higher for patients treated by hospitalists than for patients treated by traditional PCPs. Further, they found that as relational coordination increased, for patients treated either by hospitalists or PCPs, length of stay, cost, and 30-day readmission rates decreased. I will add that the hospitalists were not unit-based in this study, but were assumed to be more available to the care team than traditional PCPs.
Subsequent studies of multidisciplinary rounds on a “hospitalist unit” conducted by Kevin O’Leary, MD, and colleagues at Northwestern University in Chicago have demonstrated a favorable effect on nurses’ ratings of teamwork and collaboration, as well as the rate of adverse events.3,4 The former study did not, however, find decreased costs or length of stay.
Keys to Success
Before our current experiment, I’ve had the privilege to witness, both at my home institution and at a number of outside ones, many permutations of multidisciplinary rounds and unit-based hospitalists. I’ve seen failures, some mixed results, and occasional success stories. In all cases, participants seem to agree that it takes extra effort to execute on this model, especially once the initial enthusiasm wanes. So, for these arrangements to succeed over time, including our current experiment, I see the following four factors as critical:
- Multidisciplinary rounds must be tightly organized, with case manager, nurse, and hospitalist providing input concisely. Average time per patient should not exceed about three minutes. The total time for rounds, no matter how many patients are under discussion, should not exceed one hour.
- Each team member must be prepared to provide critical information for rounds. For example, hospitalists and nurses should have seen/reviewed their patients, case managers should know expected length of stay and key disposition information, and pharmacists should know medical histories and other pertinent information.
- The fundamental concern of multidisciplinary rounds—that someone’s time is being wasted (when not talking about that team member’s patient at that moment)—must be mitigated one way or another. Solutions include rotating nurses or hospitalists in and out of rounds, and allowing hospitalists to enter orders and do other discreet multitasking during rounds. Careful attention to showing up for the rounds on time and on cue is crucial.
- Hospitalist autonomy and need to roam has to be programmed in by allowing them time to get off the unit, see the broader world, and interact with colleagues.
At the conclusion of three months, as a QI project (as opposed to rigorous research), we will measure a number of things, including cost, throughput, patient satisfaction, and team member satisfaction with the model. If you have predictions, please e-mail me. I’ll report our results in a subsequent column.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. E-mail him at [email protected].
References
- Relational Coordination Research Collaborative. Brandeis University website. Available at: http://rcrc.brandeis.edu/about-rc/What%20is%20Relational%20Coordination.html. Accessed September 23, 2013.
- Gittell JH, Weinberg DB, Bennett AL, Miller JA. Is the doctor in? A relational approach to job design and the coordination of work. Hum Resource Manag J. 2008;47(4):729-755.
- O’Leary KJ, Haviley C, Slade ME, Shah HM, Lee J, Williams MV. Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88-93.
- O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678-684.
Today marks the end of the second week of a three-month experiment we are embarking on to improve team-based care. The main elements of our experiment are two early career hospitalists dedicated to a single nursing unit who are present on the unit throughout the day, structured multidisciplinary rounds, pharmacists doing medication histories to help with medical reconciliation, and a veteran hospitalist serving as a coach, broadly overseeing care coordination and throughput on the unit. (I’m going to focus on multidisciplinary care and leave the coaching part for another day.)
Many have written about and many more have tried to establish unit-based hospitalist models, where a hospitalist is assigned to a single nursing unit. These models often incorporate multidisciplinary rounds, where the hospitalist, case management, social services, physical therapy, and perhaps pharmacy meet each day and review each patient’s progress through the hospitalization. The underlying premise for establishing a unit-based model is that all, or nearly all, of the hospitalist’s patients are located on the nursing unit.
It Can’t Be That Hard
Dedicated units and multidisciplinary rounds are designed to achieve better coordination between the hospitalists and the other members of the hospital team. Most healthcare professionals intuitively support this model; however, many hospitalists have concerns.
To provide the best care for their patients while maintaining career satisfaction, these hospitalists may feel the need for flexibility—the ability to be independent and roam unrestricted through the hallways and departments of the hospital. This goal can be at odds with being limited to a single nursing unit.
For these hospitalists to support the unit-based model, there had better be good reasons for doing so.
Measuring the Effects of Teamwork
Jody Hoffer Gittell, PhD, a professor of management at Brandeis University in Waltham, Mass., has studied relational coordination extensively in healthcare and other service industries. Relational coordination can be defined as “coordinating work through relationships of shared goals, shared knowledge and mutual respect, supported by frequent, timely, accurate, problem-solving communication.”1
Dr. Gittell has developed a validated questionnaire to be completed by each member of the healthcare team, quantifying their perspective on these dimensions for others on the team. I think of relational coordination as a rigorous way of quantifying teamwork.
In 2008, Dr. Gittell published an observational study with SHM senior vice president Joe Miller and hospitalist leader Adrienne L. Bennett, MD, PhD, conducted at a suburban Boston hospital.2 The study looked at relational coordination between members of the hospital team under hospitalist care compared to traditional, PCP-based hospital care. They measured relational coordination by asking the attending physician (hospitalist or PCP providing hospital care), medical resident, floor nurse, case manager, social worker, and therapist (occupational, physical, respiratory, speech) to complete questionnaires about the other team members for a cohort of patients.
The study concluded that relational coordination between other members of the team and the physician was significantly higher for patients treated by hospitalists than for patients treated by traditional PCPs. Further, they found that as relational coordination increased, for patients treated either by hospitalists or PCPs, length of stay, cost, and 30-day readmission rates decreased. I will add that the hospitalists were not unit-based in this study, but were assumed to be more available to the care team than traditional PCPs.
Subsequent studies of multidisciplinary rounds on a “hospitalist unit” conducted by Kevin O’Leary, MD, and colleagues at Northwestern University in Chicago have demonstrated a favorable effect on nurses’ ratings of teamwork and collaboration, as well as the rate of adverse events.3,4 The former study did not, however, find decreased costs or length of stay.
Keys to Success
Before our current experiment, I’ve had the privilege to witness, both at my home institution and at a number of outside ones, many permutations of multidisciplinary rounds and unit-based hospitalists. I’ve seen failures, some mixed results, and occasional success stories. In all cases, participants seem to agree that it takes extra effort to execute on this model, especially once the initial enthusiasm wanes. So, for these arrangements to succeed over time, including our current experiment, I see the following four factors as critical:
- Multidisciplinary rounds must be tightly organized, with case manager, nurse, and hospitalist providing input concisely. Average time per patient should not exceed about three minutes. The total time for rounds, no matter how many patients are under discussion, should not exceed one hour.
- Each team member must be prepared to provide critical information for rounds. For example, hospitalists and nurses should have seen/reviewed their patients, case managers should know expected length of stay and key disposition information, and pharmacists should know medical histories and other pertinent information.
- The fundamental concern of multidisciplinary rounds—that someone’s time is being wasted (when not talking about that team member’s patient at that moment)—must be mitigated one way or another. Solutions include rotating nurses or hospitalists in and out of rounds, and allowing hospitalists to enter orders and do other discreet multitasking during rounds. Careful attention to showing up for the rounds on time and on cue is crucial.
- Hospitalist autonomy and need to roam has to be programmed in by allowing them time to get off the unit, see the broader world, and interact with colleagues.
At the conclusion of three months, as a QI project (as opposed to rigorous research), we will measure a number of things, including cost, throughput, patient satisfaction, and team member satisfaction with the model. If you have predictions, please e-mail me. I’ll report our results in a subsequent column.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. E-mail him at [email protected].
References
- Relational Coordination Research Collaborative. Brandeis University website. Available at: http://rcrc.brandeis.edu/about-rc/What%20is%20Relational%20Coordination.html. Accessed September 23, 2013.
- Gittell JH, Weinberg DB, Bennett AL, Miller JA. Is the doctor in? A relational approach to job design and the coordination of work. Hum Resource Manag J. 2008;47(4):729-755.
- O’Leary KJ, Haviley C, Slade ME, Shah HM, Lee J, Williams MV. Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88-93.
- O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678-684.
New Rules for Value-Based Purchasing, Readmission Penalties, Admissions
October is the beginning of a new year—in this case, fiscal-year 2014 for the Centers for Medicare & Medicaid Services (CMS). It’s a time when the new rules kick in. This month, we’ll look at some highlights, focusing on the new developments affecting your practice. Because you are held accountable for hospital-side performance on programs such as hospital value-based purchasing (HVBP) and the Readmissions Reduction Program, a working knowledge of the 2014 edition of the programs is crucial.
Close the Loop on HVBP
How will your hospital get paid under the 2014 version of HVBP? This past July, your hospital received a report outlining how its Medicare payments will be affected based on your hospital’s performance on process of care (heart failure, pneumonia, myocardial infarction, and surgery), patient experience (HCAHPS), and outcomes (30-day mortality for heart failure, pneumonia, and myocardial infarction).
Here are two hypothetical hospitals and how their performance in the program affects their 2014 payment. As background, in 2014, all hospitals have their base diagnosis related group (DRG) payments reduced by 1.25% for HVBP. They can earn back some, all, or an amount in excess of the 1.25% based on their performance. Payment is based on performance during the April 1 to Dec. 31, 2012, period. Under HVBP, CMS incentive payments occur at the level of individual patients, each of which is assigned a DRG.
Let’s look at two examples:
Hospital 1
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.48%.
- Net change in base DRG payment: +0.23%.
Hospital 2
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.08%.
- Net change in base DRG payment: -0.17%.
Hospital 1 performed relatively well, getting a bump of 0.23% in its base DRG rate. Hospital 2 did not perform so well, so it took a 0.17% hit on its base DRG rate.
In order to determine total dollars made or lost for your hospital, one multiplies the total number of eligible Medicare inpatients for 2014 times the base DRG payment times the percent change in base DRG payment. If Hospital 1 has 10,000 eligible patients in 2014 and a base DRG payment of $5,000, the value is 10,000 x $5,000 x 0.0023 (0.23%) = $115,000 gained. Hospital 2, with the same number of patients and base DRG payment, loses (10,000 x $5,000 x 0.0017 = $85,000).
Readmissions and Penalties
For 2014, CMS is adding 30-day readmissions for COPD to readmissions for heart failure, pneumonia, and myocardial infarction for its penalty program. CMS added COPD because it is the fourth-leading cause of readmissions, according to a recent Medicare Payment Advisory Commission report, and because there is wide variation in the rates (from 18% to 25%) of COPD hospital readmissions.
For 2014, CMS raises the ceiling on readmission penalties to a maximum of 2% of reimbursement for all of a hospital’s Medicare inpatients. (The maximum hit during the first round of readmission penalties, which began in October 2012, was 1%.) More than 2,200 U.S. hospitals will face some financial penalty for excess 30-day readmissions.
Disappointingly, CMS did not add a risk adjustment for socioeconomic status despite being under pressure to do so. There is growing evidence that these factors have a major impact on readmission rates.1,2
New Definition of an Admission
Amidst confusion from many and major blowback from beneficiaries saddled with large out-of-pocket expenses for observation stays and subsequent skilled-nursing-facility stays, CMS is clarifying the definition of an inpatient admission. The agency will define an admission as a hospital stay that spans at least two midnights. If a patient is in the hospital for a shorter period of time, CMS will deem the patient to be on observation status, unless medical record documentation supports a physician’s expectation “that the beneficiary would need care spanning at least two midnights” but unanticipated events led to a shorter stay.
Plan of Attack
For HVBP, make contact with your director of quality to understand your hospital’s performance and payment for 2014. If you have incentive compensation riding on HVBP, make sure you understand how your employer or contracted hospital is calculating the payout (because, for example, the performance period was in 2012!) and that your hospitalist group understands the payout calculation.
For COPD readmissions prevention, ensure patients have a home management plan; appropriate specialist follow-up and that they understand medication use, including inhalers and supplemental oxygen; and that you consider early referral for pulmonary rehabilitation for eligible patients.
For the new definition of inpatient admission, work with your hospital’s physician advisor and case management to ensure your group is getting appropriate guidance on documentation requirements. You are probably being held accountable for your hospital’s total number of observation hours, so remember to track these metrics following implementation of the new rule, as they (hopefully) should decrease. If they do, take some of the credit!
References
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681.
- Lindenauer PK, Lagu T, Rothberg MB, et al. Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ. 2013;346:f521.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
October is the beginning of a new year—in this case, fiscal-year 2014 for the Centers for Medicare & Medicaid Services (CMS). It’s a time when the new rules kick in. This month, we’ll look at some highlights, focusing on the new developments affecting your practice. Because you are held accountable for hospital-side performance on programs such as hospital value-based purchasing (HVBP) and the Readmissions Reduction Program, a working knowledge of the 2014 edition of the programs is crucial.
Close the Loop on HVBP
How will your hospital get paid under the 2014 version of HVBP? This past July, your hospital received a report outlining how its Medicare payments will be affected based on your hospital’s performance on process of care (heart failure, pneumonia, myocardial infarction, and surgery), patient experience (HCAHPS), and outcomes (30-day mortality for heart failure, pneumonia, and myocardial infarction).
Here are two hypothetical hospitals and how their performance in the program affects their 2014 payment. As background, in 2014, all hospitals have their base diagnosis related group (DRG) payments reduced by 1.25% for HVBP. They can earn back some, all, or an amount in excess of the 1.25% based on their performance. Payment is based on performance during the April 1 to Dec. 31, 2012, period. Under HVBP, CMS incentive payments occur at the level of individual patients, each of which is assigned a DRG.
Let’s look at two examples:
Hospital 1
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.48%.
- Net change in base DRG payment: +0.23%.
Hospital 2
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.08%.
- Net change in base DRG payment: -0.17%.
Hospital 1 performed relatively well, getting a bump of 0.23% in its base DRG rate. Hospital 2 did not perform so well, so it took a 0.17% hit on its base DRG rate.
In order to determine total dollars made or lost for your hospital, one multiplies the total number of eligible Medicare inpatients for 2014 times the base DRG payment times the percent change in base DRG payment. If Hospital 1 has 10,000 eligible patients in 2014 and a base DRG payment of $5,000, the value is 10,000 x $5,000 x 0.0023 (0.23%) = $115,000 gained. Hospital 2, with the same number of patients and base DRG payment, loses (10,000 x $5,000 x 0.0017 = $85,000).
Readmissions and Penalties
For 2014, CMS is adding 30-day readmissions for COPD to readmissions for heart failure, pneumonia, and myocardial infarction for its penalty program. CMS added COPD because it is the fourth-leading cause of readmissions, according to a recent Medicare Payment Advisory Commission report, and because there is wide variation in the rates (from 18% to 25%) of COPD hospital readmissions.
For 2014, CMS raises the ceiling on readmission penalties to a maximum of 2% of reimbursement for all of a hospital’s Medicare inpatients. (The maximum hit during the first round of readmission penalties, which began in October 2012, was 1%.) More than 2,200 U.S. hospitals will face some financial penalty for excess 30-day readmissions.
Disappointingly, CMS did not add a risk adjustment for socioeconomic status despite being under pressure to do so. There is growing evidence that these factors have a major impact on readmission rates.1,2
New Definition of an Admission
Amidst confusion from many and major blowback from beneficiaries saddled with large out-of-pocket expenses for observation stays and subsequent skilled-nursing-facility stays, CMS is clarifying the definition of an inpatient admission. The agency will define an admission as a hospital stay that spans at least two midnights. If a patient is in the hospital for a shorter period of time, CMS will deem the patient to be on observation status, unless medical record documentation supports a physician’s expectation “that the beneficiary would need care spanning at least two midnights” but unanticipated events led to a shorter stay.
Plan of Attack
For HVBP, make contact with your director of quality to understand your hospital’s performance and payment for 2014. If you have incentive compensation riding on HVBP, make sure you understand how your employer or contracted hospital is calculating the payout (because, for example, the performance period was in 2012!) and that your hospitalist group understands the payout calculation.
For COPD readmissions prevention, ensure patients have a home management plan; appropriate specialist follow-up and that they understand medication use, including inhalers and supplemental oxygen; and that you consider early referral for pulmonary rehabilitation for eligible patients.
For the new definition of inpatient admission, work with your hospital’s physician advisor and case management to ensure your group is getting appropriate guidance on documentation requirements. You are probably being held accountable for your hospital’s total number of observation hours, so remember to track these metrics following implementation of the new rule, as they (hopefully) should decrease. If they do, take some of the credit!
References
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681.
- Lindenauer PK, Lagu T, Rothberg MB, et al. Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ. 2013;346:f521.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
October is the beginning of a new year—in this case, fiscal-year 2014 for the Centers for Medicare & Medicaid Services (CMS). It’s a time when the new rules kick in. This month, we’ll look at some highlights, focusing on the new developments affecting your practice. Because you are held accountable for hospital-side performance on programs such as hospital value-based purchasing (HVBP) and the Readmissions Reduction Program, a working knowledge of the 2014 edition of the programs is crucial.
Close the Loop on HVBP
How will your hospital get paid under the 2014 version of HVBP? This past July, your hospital received a report outlining how its Medicare payments will be affected based on your hospital’s performance on process of care (heart failure, pneumonia, myocardial infarction, and surgery), patient experience (HCAHPS), and outcomes (30-day mortality for heart failure, pneumonia, and myocardial infarction).
Here are two hypothetical hospitals and how their performance in the program affects their 2014 payment. As background, in 2014, all hospitals have their base diagnosis related group (DRG) payments reduced by 1.25% for HVBP. They can earn back some, all, or an amount in excess of the 1.25% based on their performance. Payment is based on performance during the April 1 to Dec. 31, 2012, period. Under HVBP, CMS incentive payments occur at the level of individual patients, each of which is assigned a DRG.
Let’s look at two examples:
Hospital 1
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.48%.
- Net change in base DRG payment: +0.23%.
Hospital 2
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.08%.
- Net change in base DRG payment: -0.17%.
Hospital 1 performed relatively well, getting a bump of 0.23% in its base DRG rate. Hospital 2 did not perform so well, so it took a 0.17% hit on its base DRG rate.
In order to determine total dollars made or lost for your hospital, one multiplies the total number of eligible Medicare inpatients for 2014 times the base DRG payment times the percent change in base DRG payment. If Hospital 1 has 10,000 eligible patients in 2014 and a base DRG payment of $5,000, the value is 10,000 x $5,000 x 0.0023 (0.23%) = $115,000 gained. Hospital 2, with the same number of patients and base DRG payment, loses (10,000 x $5,000 x 0.0017 = $85,000).
Readmissions and Penalties
For 2014, CMS is adding 30-day readmissions for COPD to readmissions for heart failure, pneumonia, and myocardial infarction for its penalty program. CMS added COPD because it is the fourth-leading cause of readmissions, according to a recent Medicare Payment Advisory Commission report, and because there is wide variation in the rates (from 18% to 25%) of COPD hospital readmissions.
For 2014, CMS raises the ceiling on readmission penalties to a maximum of 2% of reimbursement for all of a hospital’s Medicare inpatients. (The maximum hit during the first round of readmission penalties, which began in October 2012, was 1%.) More than 2,200 U.S. hospitals will face some financial penalty for excess 30-day readmissions.
Disappointingly, CMS did not add a risk adjustment for socioeconomic status despite being under pressure to do so. There is growing evidence that these factors have a major impact on readmission rates.1,2
New Definition of an Admission
Amidst confusion from many and major blowback from beneficiaries saddled with large out-of-pocket expenses for observation stays and subsequent skilled-nursing-facility stays, CMS is clarifying the definition of an inpatient admission. The agency will define an admission as a hospital stay that spans at least two midnights. If a patient is in the hospital for a shorter period of time, CMS will deem the patient to be on observation status, unless medical record documentation supports a physician’s expectation “that the beneficiary would need care spanning at least two midnights” but unanticipated events led to a shorter stay.
Plan of Attack
For HVBP, make contact with your director of quality to understand your hospital’s performance and payment for 2014. If you have incentive compensation riding on HVBP, make sure you understand how your employer or contracted hospital is calculating the payout (because, for example, the performance period was in 2012!) and that your hospitalist group understands the payout calculation.
For COPD readmissions prevention, ensure patients have a home management plan; appropriate specialist follow-up and that they understand medication use, including inhalers and supplemental oxygen; and that you consider early referral for pulmonary rehabilitation for eligible patients.
For the new definition of inpatient admission, work with your hospital’s physician advisor and case management to ensure your group is getting appropriate guidance on documentation requirements. You are probably being held accountable for your hospital’s total number of observation hours, so remember to track these metrics following implementation of the new rule, as they (hopefully) should decrease. If they do, take some of the credit!
References
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681.
- Lindenauer PK, Lagu T, Rothberg MB, et al. Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ. 2013;346:f521.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].