User login
IN THIS ARTICLE
- Complications of acute bacterial sinusitis
- What are the medical options?
- AAP 2013 recommendations for initial antimicrobial treatment
Acute bacterial sinusitis (ABS) is a common diagnosis in pediatric patients. Of children who are evaluated for respiratory complaints, 6% to 7% meet clinical criteria for ABS.1 In addition to being a frequent complication of upper respiratory infection (URI), ABS in children has a significant financial impact. Direct health care expenditures attributed to sinusitis in children ages 12 or younger is $1.8 billion annually.2
Differentiating between viral URI and ABS is a diagnostic challenge for health care providers. In recent years, the American Academy of Pediatrics (AAP) and the Infectious Diseases Society of America (IDSA) have released clinical practice guidelines on the clinical diagnosis and management of ABS in children.3,4
URI AND ABS MANIFESTATIONS
URIs manifest with a predictable pattern of symptoms. Children may experience one to two days of fever, accompanied by constitutional symptoms, such as fatigue, headache, decreased appetite, and myalgia. Nasal discharge typically begins clear and becomes mucopurulent over the next few days; subsequently, it either resolves or becomes serous again at the end of the URI. Cough, hoarseness, malodorous breath, and pharyngitis may be present.3,5 Symptoms typically resolve over five to 10 days, with respiratory symptoms peaking at days 3 to 5. Importantly, in viral URIs, nasal congestion and cough improve toward the end of the illness.1,3
Persistent illness. Patients with ABS may experience persistent illness with nasal discharge (of any quality) and/or daytime cough that persists more than 10 days without improvement.3,4 These patients are differentiated from those with a viral URI by a lack of improvement in congestion and/or cough after 10 days of symptoms.3 While some children with viral illnesses may have persistant upper respiratory symptoms, these should be gradually resolving. Clinicians must take a thorough history to identify children who may have multiple consecutive URIs rather than one persistent illness that is not resolving.
Other diagnoses, such as allergic rhinitis, nasal foreign body, pertussis, influenza, and bacterial pharyngitis, must also be excluded. Children who present with persistent nasal congestion, with or without cough, after 10 days of illness without signs of improvement meet the criteria for ABS.3
Severe symptom onset. Children with ABS may experience severe onset of symptoms.3,4 These children have purulent nasal discharge for at least three consecutive days at onset of illness and concurrent fever (temperature, ≥ 102.2°F). In contrast, a viral URI typically presents with fever for less than 48 hours and clear nasal discharge that becomes purulent after the first few days of symptoms.
“Double sickening.” Finally, children with ABS may have a worsening course of symptoms or a “double sickening.”3,4 These patients experience typical URI symptoms that initially begin to improve, then worsen on day 6 or 7 of illness with increasing or new onset of considerable nasal drainage, daytime cough, or fever.
Continue for physical findings >>
PHYSICAL FINDINGS
Physical exam findings are not sufficient to distinguish between viral URI and ABS.1,3,5 Typical findings on examination may include nasal congestion, postnasal drip, erythematous turbinates, and/or injected posterior oropharynx. Malodorous breath may be present but is not diagnostic.3,5 The tympanic membranes should be examined for signs of concomitant acute otitis media (AOM) or otitis media with effusion. Swelling of the eyelids may be present. Facial pain may also be noted on physical exam.3
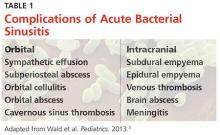
Clinicians should be mindful of the complications of sinusitis when performing the physical examination (see Table 1). The most common complications of ABS are orbital and may manifest with eyelid swelling, proptosis, or decreased extraocular movements. Patients with intracranial complications may present with headache, photophobia, seizure, meningeal signs, or focal neurologic signs.3
Continue to making the diagnosis >>
MAKING THE DIAGNOSIS
The diagnosis of ABS is a clinical one. Clinical guidelines from the AAP and IDSA for the diagnosis of ABS in children are very similar; both describe clinical presentations of persistent, severe, or worsening symptoms.3,4 This display of expert consensus allows clinicians to confidently distinguish between viral URIs and ABS by adhering to the strict diagnostic criteria already discussed.
Imaging
Radiographs and CT scans are not necessary to confirm the diagnosis of ABS. Imaging studies may reveal current or recent upper respiratory symptoms, including mucosal inflammation, opacities, and air-fluid levels6,7; however, no imaging study is available that can distinguish among mucosal inflammation and viral or bacterial infections. CT scans or MRI may be useful if clinicians suspect a complication of sinusitis.3,7
Microbiology
Historically, the microbiology of ABS has been determined by maxillary sinus aspiration. The most recent studies of this method, published in the 1980s, identified Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis as the most common bacterial pathogens.3,6,9 More recently, the microbiology of ABS has been linked with causative pathogens in AOM. The pathogenesis of ABS and AOM are similar, therefore allowing data from tympanocentesis in children with AOM to be used to determine the microbiology of children with ABS.10 Although S pneumoniae, H influenzae, and M catarrhalis remain common causative pathogens in ABS, the introduction of the 7- and 13-valent pneumococcal vaccines has altered the microbiology of AOM, and presumably ABS.11
Importantly, numbers of cases of AOM attributed to S pneumoniae have decreased while those attributed to H influenzae have increased.3,11 In addition, antimicrobial susceptibility of S pneumoniae and the prevalence of β-lactamase–positive H influenzae are important considerations when choosing appropriate antibiotics and can vary significantly by geographic region. Therefore, it is important that clinicians be aware of susceptibility patterns in the communities in which they practice.
Continue for the medical options >>
WHAT ARE THE MEDICAL OPTIONS?
Initial management of ABS in children is contingent on the symptom profile at presentation (persistent, worsening, or severe) and consideration of causative pathogens. While the consensus among experts is that children presenting with severe or worsening symptoms be treated initially with antibiotics,3,4 children who present with mild symptoms consistent with persistent illness may initially be treated with antibiotics or observed for an additional three days. This decision should be made thoughtfully and in collaboration with the patient’s parents or guardians. Any child with ABS who presents with persistent symptoms of illness and is managed initially by observation alone should be reassessed or treated with an antibiotic if symptoms worsen, if new symptoms appear, or if the child fails to improve within 72 hours.
Amoxicillin with or without clavulanate is the antibiotic of choice when ABS has been diagnosed and antibiotic treatment is indicated.1,3 AAP recommendations for antimicrobial treatment of ABS in children are stratified on the basis of age, severity of illness, day care attendance, and history of treatment with amoxicillin in the previous 30 days (see Table 2). Clinicians should rely on their knowledge of drug resistance in their community and judgment regarding severity of illness when choosing between amoxicillin and amoxicillin/clavulanate as initial treatment for ABS.3
Recommendations for duration of antimicrobial treatment for ABS vary considerably. A reasonable suggestion is to continue to treat patients until they are symptom-free for seven days. For many patients, this will mean a 10-day treatment course, with flexibility to increase the duration as needed.3
Children with ABS should be reassessed if there are worsening signs or symptoms or lack of clinical improvement within 72 hours of initial management. Clinicians should evaluate whether the patient has been appropriately diagnosed and assessed for complications of ABS. If the diagnosis is confirmed and ABS complications are not suspected, the clinician may change antibiotics or initiate antibiotic therapy if the child was previously managed by observation only.3,4
A child who is vomiting or unable to tolerate PO medications may benefit from a single 50-gm/kg dose of ceftriaxone IV or IM with follow-up in 24 hours.3 Oral antibiotics may be started at the follow-up visit if the patient demonstrates clinical improvement.
When considering a change in antibiotic, the clinician should consider the possibility of drug resistance. If the child was initially treated with amoxicillin, high-dose amoxicillin/clavulanate may be prescribed. If high-dose amoxicillin/clavulanate was initially prescribed and the patient has not improved or is experiencing worsening symptoms, clindamycin with cefixime, linezolid with cefixime, or levofloxacin may be considered.3,4
Penicillin allergy
Patients with a history of a non–type 1 hypersensitivity reaction to amoxicillin may be treated with cefdinir, cefuroxime, cefpodoxime, or combination therapy with clindamycin plus a third-generation oral cephalosporin. Allergist referral for penicillin or cephalosporin skin testing may be considered before initiation of therapy.3,4,13
Adjuvant therapy
Decongestants, antihistamines, and nasal irrigation are frequently recommended in the management of ABS in children; however, the authors of a 2012 Cochrane review found no properly designed studies to evaluate the effectiveness of these treatments.13 Furthermore, there is insufficient evidence to clearly recommend the use of intranasal steroids as an adjuvant therapy in the treatment of ABS in children (although several randomized controlled studies demonstrate their effectiveness in adolescents and adults).3
Continue for the conclusion >>
CONCLUSION
ABS in children is diagnosed clinically by following a strict set of clinical criteria. Patients commonly present with one of three types of symptoms: persistent URI; severe purulent nasal discharge and fever for at least three consecutive days; or a double sickening. Physical examination findings vary and will not differentiate viral URI symptoms from a diagnosis of ABS. Imaging is not recommended for diagnosis but may be helpful if an orbital or intracranial complication of ABS is suspected.
S pneumoniae, H influenzae, and M catarrhalis continue to be the most common pathogens associated with ABS. However, since the introduction of the 7-valent pneumococcal vaccine, prevalence of H influenzae and β-lactamase–positive H influenzae has increased.
Treatment recommendations vary, based on suspected causative pathogens and presenting symptoms. Amoxicillin or amoxicillin-clavulanate is recommended as firstline antimicrobial treatment for ABS, with alternate antibiotic choices for patients with worsening symptoms or lack of improvement within 72 hours. An awareness of the community’s susceptibility patterns is essential for the clinician who cares for children at risk for ABS.
REFERENCES
1. Wald ER, Nash D, Eickhoff J. Effectiveness of amoxicillin/clavulanate potassium in the treatment of acute bacterial sinusitis in children. Pediatrics. 2009;124(1):9-15.
2. Ray NF, Baraniuk JN, Thamer M, et al. Healthcare expenditures for sinusitis in 1996: contributions of asthma, rhinitis, and other airway disorders. J Allergy Clin Immunol. 1999;103(3 pt 1):408-414.
3. Wald ER, Applegate KE, Bordley C, et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013;132(1):e262-e280.
4. Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):1041-1045.
5. Shaikh N, Hoberman A, Kearney DH, et al. Signs and symptoms that differentiate acute sinusitis from viral upper respiratory tract infection. Pediatr Infect Dis J. 2013;32(10):1061-1065.
6. Kovatch AL, Wald ER, Ledesma-Medina J, et al. Maxillary sinus radiographs in children with nonrespiratory complaints. Pediatrics. 1984; 73(3):306-308.
7. Triulzi F, Zirpoli S. Imaging techniques in the diagnosis and management of rhinosinusitis in children. Pediatr Allergy Immunol. 2007;18(suppl 18):46-49.
8. Wald ER, Milmoe GJ, Bowen A, et al. Acute maxillary sinusitis in children. N Engl J Med. 1981;304(13):749-754.
9. Wald ER, Reilly JS, Casselbrant M, et al. Treatment of acute maxillary sinusitis in childhood: a comparative study of amoxicillin and cefaclor. J Pediatr. 1984;104(2):297-302.
10. Wald ER. Acute otitis media and acute bacterial sinusitis. Clin Infect Dis. 2011;52(suppl 4):S277-S283.
11. Casey JR, Adlowitz DG, Pichichero ME. New patterns in the otopathogens causing acute otitis media six to eight years after introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2010;29(4):304-309.
12. Pichichero ME. A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients. Pediatrics. 2004;115(4):1048-1057.
13. Shaikh N, Wald ER, Pi M. Decongestants, antihistamines and nasal irrigation for acute sinusitis in children. Cochrane Database Syst Rev. 2012;9:CD007909.
IN THIS ARTICLE
- Complications of acute bacterial sinusitis
- What are the medical options?
- AAP 2013 recommendations for initial antimicrobial treatment
Acute bacterial sinusitis (ABS) is a common diagnosis in pediatric patients. Of children who are evaluated for respiratory complaints, 6% to 7% meet clinical criteria for ABS.1 In addition to being a frequent complication of upper respiratory infection (URI), ABS in children has a significant financial impact. Direct health care expenditures attributed to sinusitis in children ages 12 or younger is $1.8 billion annually.2
Differentiating between viral URI and ABS is a diagnostic challenge for health care providers. In recent years, the American Academy of Pediatrics (AAP) and the Infectious Diseases Society of America (IDSA) have released clinical practice guidelines on the clinical diagnosis and management of ABS in children.3,4
URI AND ABS MANIFESTATIONS
URIs manifest with a predictable pattern of symptoms. Children may experience one to two days of fever, accompanied by constitutional symptoms, such as fatigue, headache, decreased appetite, and myalgia. Nasal discharge typically begins clear and becomes mucopurulent over the next few days; subsequently, it either resolves or becomes serous again at the end of the URI. Cough, hoarseness, malodorous breath, and pharyngitis may be present.3,5 Symptoms typically resolve over five to 10 days, with respiratory symptoms peaking at days 3 to 5. Importantly, in viral URIs, nasal congestion and cough improve toward the end of the illness.1,3
Persistent illness. Patients with ABS may experience persistent illness with nasal discharge (of any quality) and/or daytime cough that persists more than 10 days without improvement.3,4 These patients are differentiated from those with a viral URI by a lack of improvement in congestion and/or cough after 10 days of symptoms.3 While some children with viral illnesses may have persistant upper respiratory symptoms, these should be gradually resolving. Clinicians must take a thorough history to identify children who may have multiple consecutive URIs rather than one persistent illness that is not resolving.
Other diagnoses, such as allergic rhinitis, nasal foreign body, pertussis, influenza, and bacterial pharyngitis, must also be excluded. Children who present with persistent nasal congestion, with or without cough, after 10 days of illness without signs of improvement meet the criteria for ABS.3
Severe symptom onset. Children with ABS may experience severe onset of symptoms.3,4 These children have purulent nasal discharge for at least three consecutive days at onset of illness and concurrent fever (temperature, ≥ 102.2°F). In contrast, a viral URI typically presents with fever for less than 48 hours and clear nasal discharge that becomes purulent after the first few days of symptoms.
“Double sickening.” Finally, children with ABS may have a worsening course of symptoms or a “double sickening.”3,4 These patients experience typical URI symptoms that initially begin to improve, then worsen on day 6 or 7 of illness with increasing or new onset of considerable nasal drainage, daytime cough, or fever.
Continue for physical findings >>
PHYSICAL FINDINGS
Physical exam findings are not sufficient to distinguish between viral URI and ABS.1,3,5 Typical findings on examination may include nasal congestion, postnasal drip, erythematous turbinates, and/or injected posterior oropharynx. Malodorous breath may be present but is not diagnostic.3,5 The tympanic membranes should be examined for signs of concomitant acute otitis media (AOM) or otitis media with effusion. Swelling of the eyelids may be present. Facial pain may also be noted on physical exam.3
Clinicians should be mindful of the complications of sinusitis when performing the physical examination (see Table 1). The most common complications of ABS are orbital and may manifest with eyelid swelling, proptosis, or decreased extraocular movements. Patients with intracranial complications may present with headache, photophobia, seizure, meningeal signs, or focal neurologic signs.3
Continue to making the diagnosis >>
MAKING THE DIAGNOSIS
The diagnosis of ABS is a clinical one. Clinical guidelines from the AAP and IDSA for the diagnosis of ABS in children are very similar; both describe clinical presentations of persistent, severe, or worsening symptoms.3,4 This display of expert consensus allows clinicians to confidently distinguish between viral URIs and ABS by adhering to the strict diagnostic criteria already discussed.
Imaging
Radiographs and CT scans are not necessary to confirm the diagnosis of ABS. Imaging studies may reveal current or recent upper respiratory symptoms, including mucosal inflammation, opacities, and air-fluid levels6,7; however, no imaging study is available that can distinguish among mucosal inflammation and viral or bacterial infections. CT scans or MRI may be useful if clinicians suspect a complication of sinusitis.3,7
Microbiology
Historically, the microbiology of ABS has been determined by maxillary sinus aspiration. The most recent studies of this method, published in the 1980s, identified Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis as the most common bacterial pathogens.3,6,9 More recently, the microbiology of ABS has been linked with causative pathogens in AOM. The pathogenesis of ABS and AOM are similar, therefore allowing data from tympanocentesis in children with AOM to be used to determine the microbiology of children with ABS.10 Although S pneumoniae, H influenzae, and M catarrhalis remain common causative pathogens in ABS, the introduction of the 7- and 13-valent pneumococcal vaccines has altered the microbiology of AOM, and presumably ABS.11
Importantly, numbers of cases of AOM attributed to S pneumoniae have decreased while those attributed to H influenzae have increased.3,11 In addition, antimicrobial susceptibility of S pneumoniae and the prevalence of β-lactamase–positive H influenzae are important considerations when choosing appropriate antibiotics and can vary significantly by geographic region. Therefore, it is important that clinicians be aware of susceptibility patterns in the communities in which they practice.
Continue for the medical options >>
WHAT ARE THE MEDICAL OPTIONS?
Initial management of ABS in children is contingent on the symptom profile at presentation (persistent, worsening, or severe) and consideration of causative pathogens. While the consensus among experts is that children presenting with severe or worsening symptoms be treated initially with antibiotics,3,4 children who present with mild symptoms consistent with persistent illness may initially be treated with antibiotics or observed for an additional three days. This decision should be made thoughtfully and in collaboration with the patient’s parents or guardians. Any child with ABS who presents with persistent symptoms of illness and is managed initially by observation alone should be reassessed or treated with an antibiotic if symptoms worsen, if new symptoms appear, or if the child fails to improve within 72 hours.
Amoxicillin with or without clavulanate is the antibiotic of choice when ABS has been diagnosed and antibiotic treatment is indicated.1,3 AAP recommendations for antimicrobial treatment of ABS in children are stratified on the basis of age, severity of illness, day care attendance, and history of treatment with amoxicillin in the previous 30 days (see Table 2). Clinicians should rely on their knowledge of drug resistance in their community and judgment regarding severity of illness when choosing between amoxicillin and amoxicillin/clavulanate as initial treatment for ABS.3
Recommendations for duration of antimicrobial treatment for ABS vary considerably. A reasonable suggestion is to continue to treat patients until they are symptom-free for seven days. For many patients, this will mean a 10-day treatment course, with flexibility to increase the duration as needed.3
Children with ABS should be reassessed if there are worsening signs or symptoms or lack of clinical improvement within 72 hours of initial management. Clinicians should evaluate whether the patient has been appropriately diagnosed and assessed for complications of ABS. If the diagnosis is confirmed and ABS complications are not suspected, the clinician may change antibiotics or initiate antibiotic therapy if the child was previously managed by observation only.3,4
A child who is vomiting or unable to tolerate PO medications may benefit from a single 50-gm/kg dose of ceftriaxone IV or IM with follow-up in 24 hours.3 Oral antibiotics may be started at the follow-up visit if the patient demonstrates clinical improvement.
When considering a change in antibiotic, the clinician should consider the possibility of drug resistance. If the child was initially treated with amoxicillin, high-dose amoxicillin/clavulanate may be prescribed. If high-dose amoxicillin/clavulanate was initially prescribed and the patient has not improved or is experiencing worsening symptoms, clindamycin with cefixime, linezolid with cefixime, or levofloxacin may be considered.3,4
Penicillin allergy
Patients with a history of a non–type 1 hypersensitivity reaction to amoxicillin may be treated with cefdinir, cefuroxime, cefpodoxime, or combination therapy with clindamycin plus a third-generation oral cephalosporin. Allergist referral for penicillin or cephalosporin skin testing may be considered before initiation of therapy.3,4,13
Adjuvant therapy
Decongestants, antihistamines, and nasal irrigation are frequently recommended in the management of ABS in children; however, the authors of a 2012 Cochrane review found no properly designed studies to evaluate the effectiveness of these treatments.13 Furthermore, there is insufficient evidence to clearly recommend the use of intranasal steroids as an adjuvant therapy in the treatment of ABS in children (although several randomized controlled studies demonstrate their effectiveness in adolescents and adults).3
Continue for the conclusion >>
CONCLUSION
ABS in children is diagnosed clinically by following a strict set of clinical criteria. Patients commonly present with one of three types of symptoms: persistent URI; severe purulent nasal discharge and fever for at least three consecutive days; or a double sickening. Physical examination findings vary and will not differentiate viral URI symptoms from a diagnosis of ABS. Imaging is not recommended for diagnosis but may be helpful if an orbital or intracranial complication of ABS is suspected.
S pneumoniae, H influenzae, and M catarrhalis continue to be the most common pathogens associated with ABS. However, since the introduction of the 7-valent pneumococcal vaccine, prevalence of H influenzae and β-lactamase–positive H influenzae has increased.
Treatment recommendations vary, based on suspected causative pathogens and presenting symptoms. Amoxicillin or amoxicillin-clavulanate is recommended as firstline antimicrobial treatment for ABS, with alternate antibiotic choices for patients with worsening symptoms or lack of improvement within 72 hours. An awareness of the community’s susceptibility patterns is essential for the clinician who cares for children at risk for ABS.
REFERENCES
1. Wald ER, Nash D, Eickhoff J. Effectiveness of amoxicillin/clavulanate potassium in the treatment of acute bacterial sinusitis in children. Pediatrics. 2009;124(1):9-15.
2. Ray NF, Baraniuk JN, Thamer M, et al. Healthcare expenditures for sinusitis in 1996: contributions of asthma, rhinitis, and other airway disorders. J Allergy Clin Immunol. 1999;103(3 pt 1):408-414.
3. Wald ER, Applegate KE, Bordley C, et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013;132(1):e262-e280.
4. Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):1041-1045.
5. Shaikh N, Hoberman A, Kearney DH, et al. Signs and symptoms that differentiate acute sinusitis from viral upper respiratory tract infection. Pediatr Infect Dis J. 2013;32(10):1061-1065.
6. Kovatch AL, Wald ER, Ledesma-Medina J, et al. Maxillary sinus radiographs in children with nonrespiratory complaints. Pediatrics. 1984; 73(3):306-308.
7. Triulzi F, Zirpoli S. Imaging techniques in the diagnosis and management of rhinosinusitis in children. Pediatr Allergy Immunol. 2007;18(suppl 18):46-49.
8. Wald ER, Milmoe GJ, Bowen A, et al. Acute maxillary sinusitis in children. N Engl J Med. 1981;304(13):749-754.
9. Wald ER, Reilly JS, Casselbrant M, et al. Treatment of acute maxillary sinusitis in childhood: a comparative study of amoxicillin and cefaclor. J Pediatr. 1984;104(2):297-302.
10. Wald ER. Acute otitis media and acute bacterial sinusitis. Clin Infect Dis. 2011;52(suppl 4):S277-S283.
11. Casey JR, Adlowitz DG, Pichichero ME. New patterns in the otopathogens causing acute otitis media six to eight years after introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2010;29(4):304-309.
12. Pichichero ME. A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients. Pediatrics. 2004;115(4):1048-1057.
13. Shaikh N, Wald ER, Pi M. Decongestants, antihistamines and nasal irrigation for acute sinusitis in children. Cochrane Database Syst Rev. 2012;9:CD007909.
IN THIS ARTICLE
- Complications of acute bacterial sinusitis
- What are the medical options?
- AAP 2013 recommendations for initial antimicrobial treatment
Acute bacterial sinusitis (ABS) is a common diagnosis in pediatric patients. Of children who are evaluated for respiratory complaints, 6% to 7% meet clinical criteria for ABS.1 In addition to being a frequent complication of upper respiratory infection (URI), ABS in children has a significant financial impact. Direct health care expenditures attributed to sinusitis in children ages 12 or younger is $1.8 billion annually.2
Differentiating between viral URI and ABS is a diagnostic challenge for health care providers. In recent years, the American Academy of Pediatrics (AAP) and the Infectious Diseases Society of America (IDSA) have released clinical practice guidelines on the clinical diagnosis and management of ABS in children.3,4
URI AND ABS MANIFESTATIONS
URIs manifest with a predictable pattern of symptoms. Children may experience one to two days of fever, accompanied by constitutional symptoms, such as fatigue, headache, decreased appetite, and myalgia. Nasal discharge typically begins clear and becomes mucopurulent over the next few days; subsequently, it either resolves or becomes serous again at the end of the URI. Cough, hoarseness, malodorous breath, and pharyngitis may be present.3,5 Symptoms typically resolve over five to 10 days, with respiratory symptoms peaking at days 3 to 5. Importantly, in viral URIs, nasal congestion and cough improve toward the end of the illness.1,3
Persistent illness. Patients with ABS may experience persistent illness with nasal discharge (of any quality) and/or daytime cough that persists more than 10 days without improvement.3,4 These patients are differentiated from those with a viral URI by a lack of improvement in congestion and/or cough after 10 days of symptoms.3 While some children with viral illnesses may have persistant upper respiratory symptoms, these should be gradually resolving. Clinicians must take a thorough history to identify children who may have multiple consecutive URIs rather than one persistent illness that is not resolving.
Other diagnoses, such as allergic rhinitis, nasal foreign body, pertussis, influenza, and bacterial pharyngitis, must also be excluded. Children who present with persistent nasal congestion, with or without cough, after 10 days of illness without signs of improvement meet the criteria for ABS.3
Severe symptom onset. Children with ABS may experience severe onset of symptoms.3,4 These children have purulent nasal discharge for at least three consecutive days at onset of illness and concurrent fever (temperature, ≥ 102.2°F). In contrast, a viral URI typically presents with fever for less than 48 hours and clear nasal discharge that becomes purulent after the first few days of symptoms.
“Double sickening.” Finally, children with ABS may have a worsening course of symptoms or a “double sickening.”3,4 These patients experience typical URI symptoms that initially begin to improve, then worsen on day 6 or 7 of illness with increasing or new onset of considerable nasal drainage, daytime cough, or fever.
Continue for physical findings >>
PHYSICAL FINDINGS
Physical exam findings are not sufficient to distinguish between viral URI and ABS.1,3,5 Typical findings on examination may include nasal congestion, postnasal drip, erythematous turbinates, and/or injected posterior oropharynx. Malodorous breath may be present but is not diagnostic.3,5 The tympanic membranes should be examined for signs of concomitant acute otitis media (AOM) or otitis media with effusion. Swelling of the eyelids may be present. Facial pain may also be noted on physical exam.3
Clinicians should be mindful of the complications of sinusitis when performing the physical examination (see Table 1). The most common complications of ABS are orbital and may manifest with eyelid swelling, proptosis, or decreased extraocular movements. Patients with intracranial complications may present with headache, photophobia, seizure, meningeal signs, or focal neurologic signs.3
Continue to making the diagnosis >>
MAKING THE DIAGNOSIS
The diagnosis of ABS is a clinical one. Clinical guidelines from the AAP and IDSA for the diagnosis of ABS in children are very similar; both describe clinical presentations of persistent, severe, or worsening symptoms.3,4 This display of expert consensus allows clinicians to confidently distinguish between viral URIs and ABS by adhering to the strict diagnostic criteria already discussed.
Imaging
Radiographs and CT scans are not necessary to confirm the diagnosis of ABS. Imaging studies may reveal current or recent upper respiratory symptoms, including mucosal inflammation, opacities, and air-fluid levels6,7; however, no imaging study is available that can distinguish among mucosal inflammation and viral or bacterial infections. CT scans or MRI may be useful if clinicians suspect a complication of sinusitis.3,7
Microbiology
Historically, the microbiology of ABS has been determined by maxillary sinus aspiration. The most recent studies of this method, published in the 1980s, identified Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis as the most common bacterial pathogens.3,6,9 More recently, the microbiology of ABS has been linked with causative pathogens in AOM. The pathogenesis of ABS and AOM are similar, therefore allowing data from tympanocentesis in children with AOM to be used to determine the microbiology of children with ABS.10 Although S pneumoniae, H influenzae, and M catarrhalis remain common causative pathogens in ABS, the introduction of the 7- and 13-valent pneumococcal vaccines has altered the microbiology of AOM, and presumably ABS.11
Importantly, numbers of cases of AOM attributed to S pneumoniae have decreased while those attributed to H influenzae have increased.3,11 In addition, antimicrobial susceptibility of S pneumoniae and the prevalence of β-lactamase–positive H influenzae are important considerations when choosing appropriate antibiotics and can vary significantly by geographic region. Therefore, it is important that clinicians be aware of susceptibility patterns in the communities in which they practice.
Continue for the medical options >>
WHAT ARE THE MEDICAL OPTIONS?
Initial management of ABS in children is contingent on the symptom profile at presentation (persistent, worsening, or severe) and consideration of causative pathogens. While the consensus among experts is that children presenting with severe or worsening symptoms be treated initially with antibiotics,3,4 children who present with mild symptoms consistent with persistent illness may initially be treated with antibiotics or observed for an additional three days. This decision should be made thoughtfully and in collaboration with the patient’s parents or guardians. Any child with ABS who presents with persistent symptoms of illness and is managed initially by observation alone should be reassessed or treated with an antibiotic if symptoms worsen, if new symptoms appear, or if the child fails to improve within 72 hours.
Amoxicillin with or without clavulanate is the antibiotic of choice when ABS has been diagnosed and antibiotic treatment is indicated.1,3 AAP recommendations for antimicrobial treatment of ABS in children are stratified on the basis of age, severity of illness, day care attendance, and history of treatment with amoxicillin in the previous 30 days (see Table 2). Clinicians should rely on their knowledge of drug resistance in their community and judgment regarding severity of illness when choosing between amoxicillin and amoxicillin/clavulanate as initial treatment for ABS.3
Recommendations for duration of antimicrobial treatment for ABS vary considerably. A reasonable suggestion is to continue to treat patients until they are symptom-free for seven days. For many patients, this will mean a 10-day treatment course, with flexibility to increase the duration as needed.3
Children with ABS should be reassessed if there are worsening signs or symptoms or lack of clinical improvement within 72 hours of initial management. Clinicians should evaluate whether the patient has been appropriately diagnosed and assessed for complications of ABS. If the diagnosis is confirmed and ABS complications are not suspected, the clinician may change antibiotics or initiate antibiotic therapy if the child was previously managed by observation only.3,4
A child who is vomiting or unable to tolerate PO medications may benefit from a single 50-gm/kg dose of ceftriaxone IV or IM with follow-up in 24 hours.3 Oral antibiotics may be started at the follow-up visit if the patient demonstrates clinical improvement.
When considering a change in antibiotic, the clinician should consider the possibility of drug resistance. If the child was initially treated with amoxicillin, high-dose amoxicillin/clavulanate may be prescribed. If high-dose amoxicillin/clavulanate was initially prescribed and the patient has not improved or is experiencing worsening symptoms, clindamycin with cefixime, linezolid with cefixime, or levofloxacin may be considered.3,4
Penicillin allergy
Patients with a history of a non–type 1 hypersensitivity reaction to amoxicillin may be treated with cefdinir, cefuroxime, cefpodoxime, or combination therapy with clindamycin plus a third-generation oral cephalosporin. Allergist referral for penicillin or cephalosporin skin testing may be considered before initiation of therapy.3,4,13
Adjuvant therapy
Decongestants, antihistamines, and nasal irrigation are frequently recommended in the management of ABS in children; however, the authors of a 2012 Cochrane review found no properly designed studies to evaluate the effectiveness of these treatments.13 Furthermore, there is insufficient evidence to clearly recommend the use of intranasal steroids as an adjuvant therapy in the treatment of ABS in children (although several randomized controlled studies demonstrate their effectiveness in adolescents and adults).3
Continue for the conclusion >>
CONCLUSION
ABS in children is diagnosed clinically by following a strict set of clinical criteria. Patients commonly present with one of three types of symptoms: persistent URI; severe purulent nasal discharge and fever for at least three consecutive days; or a double sickening. Physical examination findings vary and will not differentiate viral URI symptoms from a diagnosis of ABS. Imaging is not recommended for diagnosis but may be helpful if an orbital or intracranial complication of ABS is suspected.
S pneumoniae, H influenzae, and M catarrhalis continue to be the most common pathogens associated with ABS. However, since the introduction of the 7-valent pneumococcal vaccine, prevalence of H influenzae and β-lactamase–positive H influenzae has increased.
Treatment recommendations vary, based on suspected causative pathogens and presenting symptoms. Amoxicillin or amoxicillin-clavulanate is recommended as firstline antimicrobial treatment for ABS, with alternate antibiotic choices for patients with worsening symptoms or lack of improvement within 72 hours. An awareness of the community’s susceptibility patterns is essential for the clinician who cares for children at risk for ABS.
REFERENCES
1. Wald ER, Nash D, Eickhoff J. Effectiveness of amoxicillin/clavulanate potassium in the treatment of acute bacterial sinusitis in children. Pediatrics. 2009;124(1):9-15.
2. Ray NF, Baraniuk JN, Thamer M, et al. Healthcare expenditures for sinusitis in 1996: contributions of asthma, rhinitis, and other airway disorders. J Allergy Clin Immunol. 1999;103(3 pt 1):408-414.
3. Wald ER, Applegate KE, Bordley C, et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013;132(1):e262-e280.
4. Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):1041-1045.
5. Shaikh N, Hoberman A, Kearney DH, et al. Signs and symptoms that differentiate acute sinusitis from viral upper respiratory tract infection. Pediatr Infect Dis J. 2013;32(10):1061-1065.
6. Kovatch AL, Wald ER, Ledesma-Medina J, et al. Maxillary sinus radiographs in children with nonrespiratory complaints. Pediatrics. 1984; 73(3):306-308.
7. Triulzi F, Zirpoli S. Imaging techniques in the diagnosis and management of rhinosinusitis in children. Pediatr Allergy Immunol. 2007;18(suppl 18):46-49.
8. Wald ER, Milmoe GJ, Bowen A, et al. Acute maxillary sinusitis in children. N Engl J Med. 1981;304(13):749-754.
9. Wald ER, Reilly JS, Casselbrant M, et al. Treatment of acute maxillary sinusitis in childhood: a comparative study of amoxicillin and cefaclor. J Pediatr. 1984;104(2):297-302.
10. Wald ER. Acute otitis media and acute bacterial sinusitis. Clin Infect Dis. 2011;52(suppl 4):S277-S283.
11. Casey JR, Adlowitz DG, Pichichero ME. New patterns in the otopathogens causing acute otitis media six to eight years after introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2010;29(4):304-309.
12. Pichichero ME. A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients. Pediatrics. 2004;115(4):1048-1057.
13. Shaikh N, Wald ER, Pi M. Decongestants, antihistamines and nasal irrigation for acute sinusitis in children. Cochrane Database Syst Rev. 2012;9:CD007909.