User login
PHILADELPHIA – Women with epilepsy often reported having an increased number of seizures when taking a hormonal contraceptive, according to data collected from 1,144 women with epilepsy who completed an online survey.
The data showed that women who used hormonal contraception reported having an increased number of seizures while on the contraceptive about 4.5-fold more often than did women who used nonhormonal contraception. The risk for an increased number of seizures with hormonal contraception seemed greatest for women treated with valproate.
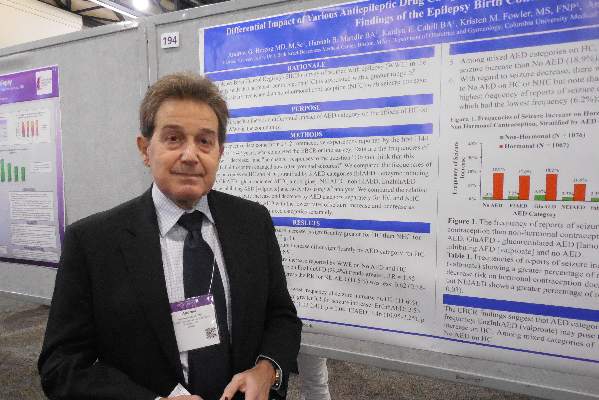
Until now, “valproate was generally accepted as okay to use” by women also taking a hormonal contraceptive, but the new findings suggest that if a woman of childbearing age with epilepsy needs valproate for seizure control she would be better off using a nonhormonal form of contraception such as an intrauterine device, Dr. Andrew G. Herzog said while presenting a poster at the annual meeting of the American Epilepsy Society.
Dr. Herzog highlighted the need for some form of contraception for most younger women on valproate because of the drug’s potential teratogenic effects, but he also stressed that the risk for increased seizures does not appear to affect a majority of women. The survey results showed that overall only 28% of women with epilepsy reported an increased seizure frequency when using a hormonal contraceptive.
“The first goal of a neurologist is to get seizures under control, and you go with the [antiepileptic drugs] that work,” Dr. Herzog said in an interview. Once an effective regimen is found, the physician can then deal with other issues, such as adverse effects as well as the potential for an adverse interaction with a hormonal contraceptive. Valproate can be the antiepileptic drug of choice as it is one of the most effective agents for controlling seizures in patients with primary generalized epilepsy, said Dr. Herzog, professor of neurology at Harvard Medical School, Boston, and director of the neuroendocrine unit of Beth Israel Deaconess Medical Center in Wellesley, Mass.
The new data come from an Internet-based survey, which is subject to biases and appeared to attract a preponderance of responses from women who were better educated and had higher incomes than did the general population. In addition, the researchers collected the data retrospectively. Despite these limitations, the results are notable because they represent the only data set yet reported from a community-based source large enough to allow analysis of the many clinical variables that play into the potential interactions between various contraceptive types, various antiepileptic drug classes, and the diverse number of epilepsy subtypes, he said. Dr. Herzog and his associates are planning a study to collect similar data prospectively, but the results would likely not be available for at least about 5 years, he noted.
The Epilepsy Birth Control Registry enrolled women with epilepsy aged 18-47 years who had a history of using at least one form of contraception while on antiepileptic treatment, and the 1,144 women who completed the survey reported a total of 2,712 contraceptive experiences. The survey asked women, “Do you think this method of birth control changed how often you had seizures?” with the option to reply that their contraceptive method seemed to increase, decrease, or not change their seizure number.
One of the analyses done by Dr. Herzog and his associates compared the responses by women on any form of hormonal contraceptive (combined or progestin pill, hormonal patch, vaginal ring, depot medroxyprogesterone acetate, or implanted hormone) with women on any form of nonhormonal contraception (withdrawal, male or female condom, copper or progestin intrauterine device, or tubal ligation).
The results showed that 72% of women on any hormonal contraceptive and 91% of women on any form of nonhormonal contraceptive reported no change in their seizure frequency. The rates of reporting an increased number of seizures were 19% with hormonal contraceptives and 4% with nonhormonal contraceptives, which computed to a relative risk of about 4.5-fold for an increased number of seizures while on hormonal contraception, compared with nonhormonal contraception, the researchers reported.
Barrier contraception (male or female condoms) had the lowest rate of seizure increase among any of the nonhormonal methods. The risk for greater seizure frequency on hormonal contraceptives of all types was 6.75-fold higher when compared specifically with barrier contraception.
In analyses of specific types of hormonal contraceptives, women using a hormonal patch reported a 68% greater incidence of seizure increases, compared with women using combined oral contraceptive pills (the hormonal method that produced the fewest episodes of seizure increases). Those using a progestin-only pill had a 62% higher rate of seizure increases.
More women on hormonal contraceptives also reported having a decrease in seizures after starting contraception, compared with those starting on a nonhormonal method (9.5% vs. 5.2%, respectively), which calculated to a 85% relative rate increase for decreased seizures. Depot medroxyprogesterone acetate was the only specific hormonal contraceptive that linked with a higher rate of seizure decreases, compared with combined oral pills, a 95% higher rate.
A second analysis of the results by Dr. Herzog and his associates examined the frequencies of seizure outcomes on hormonal and nonhormonal contraceptives stratifying by type of antiepileptic drug women used when starting a particular contraceptive method. This analysis broke down antiepileptic drugs into four types: enzyme inducing (29%), glucuronidated (such as lamotrigine; 27%), nonenzyme inducing (such as levetiracetam; 22%), enzyme inhibiting (valproate; 8%), and a fifth category that included women who were not on any antiepileptic drug (14%).
This analysis showed that the frequency of seizure increases was significantly greater with hormonal contraceptive use, compared with nonhormonal methods, across all five subgroups of antiepileptic drug type. In addition, the frequency of seizure increases with hormonal contraceptives differed significantly, depending on which antiepileptic drug type women used, but these significant differences among the antiepileptic drug types also occurred among women using nonhormonal contraception.
Women receiving a nonenzyme-inducing drug when starting a hormonal contraceptive reported the lowest frequency of seizure increases, a 12% rate. In contrast, women on an enzyme-inhibiting drug, valproate, had the highest rate of increased seizures when starting a hormonal contraceptive, 29%. This calculated out to about a 2.5-fold relative risk increase for having more seizures when starting hormonal contraception while on valproate, compared with women on a nonenzyme-inducing drug, Dr. Herzog reported.
Physicians “need to be on the lookout for the possibility that seizures could increase when women start a hormonal contraceptive,” he concluded.
On Twitter @mitchelzoler
PHILADELPHIA – Women with epilepsy often reported having an increased number of seizures when taking a hormonal contraceptive, according to data collected from 1,144 women with epilepsy who completed an online survey.
The data showed that women who used hormonal contraception reported having an increased number of seizures while on the contraceptive about 4.5-fold more often than did women who used nonhormonal contraception. The risk for an increased number of seizures with hormonal contraception seemed greatest for women treated with valproate.
Until now, “valproate was generally accepted as okay to use” by women also taking a hormonal contraceptive, but the new findings suggest that if a woman of childbearing age with epilepsy needs valproate for seizure control she would be better off using a nonhormonal form of contraception such as an intrauterine device, Dr. Andrew G. Herzog said while presenting a poster at the annual meeting of the American Epilepsy Society.
Dr. Herzog highlighted the need for some form of contraception for most younger women on valproate because of the drug’s potential teratogenic effects, but he also stressed that the risk for increased seizures does not appear to affect a majority of women. The survey results showed that overall only 28% of women with epilepsy reported an increased seizure frequency when using a hormonal contraceptive.
“The first goal of a neurologist is to get seizures under control, and you go with the [antiepileptic drugs] that work,” Dr. Herzog said in an interview. Once an effective regimen is found, the physician can then deal with other issues, such as adverse effects as well as the potential for an adverse interaction with a hormonal contraceptive. Valproate can be the antiepileptic drug of choice as it is one of the most effective agents for controlling seizures in patients with primary generalized epilepsy, said Dr. Herzog, professor of neurology at Harvard Medical School, Boston, and director of the neuroendocrine unit of Beth Israel Deaconess Medical Center in Wellesley, Mass.
The new data come from an Internet-based survey, which is subject to biases and appeared to attract a preponderance of responses from women who were better educated and had higher incomes than did the general population. In addition, the researchers collected the data retrospectively. Despite these limitations, the results are notable because they represent the only data set yet reported from a community-based source large enough to allow analysis of the many clinical variables that play into the potential interactions between various contraceptive types, various antiepileptic drug classes, and the diverse number of epilepsy subtypes, he said. Dr. Herzog and his associates are planning a study to collect similar data prospectively, but the results would likely not be available for at least about 5 years, he noted.
The Epilepsy Birth Control Registry enrolled women with epilepsy aged 18-47 years who had a history of using at least one form of contraception while on antiepileptic treatment, and the 1,144 women who completed the survey reported a total of 2,712 contraceptive experiences. The survey asked women, “Do you think this method of birth control changed how often you had seizures?” with the option to reply that their contraceptive method seemed to increase, decrease, or not change their seizure number.
One of the analyses done by Dr. Herzog and his associates compared the responses by women on any form of hormonal contraceptive (combined or progestin pill, hormonal patch, vaginal ring, depot medroxyprogesterone acetate, or implanted hormone) with women on any form of nonhormonal contraception (withdrawal, male or female condom, copper or progestin intrauterine device, or tubal ligation).
The results showed that 72% of women on any hormonal contraceptive and 91% of women on any form of nonhormonal contraceptive reported no change in their seizure frequency. The rates of reporting an increased number of seizures were 19% with hormonal contraceptives and 4% with nonhormonal contraceptives, which computed to a relative risk of about 4.5-fold for an increased number of seizures while on hormonal contraception, compared with nonhormonal contraception, the researchers reported.
Barrier contraception (male or female condoms) had the lowest rate of seizure increase among any of the nonhormonal methods. The risk for greater seizure frequency on hormonal contraceptives of all types was 6.75-fold higher when compared specifically with barrier contraception.
In analyses of specific types of hormonal contraceptives, women using a hormonal patch reported a 68% greater incidence of seizure increases, compared with women using combined oral contraceptive pills (the hormonal method that produced the fewest episodes of seizure increases). Those using a progestin-only pill had a 62% higher rate of seizure increases.
More women on hormonal contraceptives also reported having a decrease in seizures after starting contraception, compared with those starting on a nonhormonal method (9.5% vs. 5.2%, respectively), which calculated to a 85% relative rate increase for decreased seizures. Depot medroxyprogesterone acetate was the only specific hormonal contraceptive that linked with a higher rate of seizure decreases, compared with combined oral pills, a 95% higher rate.
A second analysis of the results by Dr. Herzog and his associates examined the frequencies of seizure outcomes on hormonal and nonhormonal contraceptives stratifying by type of antiepileptic drug women used when starting a particular contraceptive method. This analysis broke down antiepileptic drugs into four types: enzyme inducing (29%), glucuronidated (such as lamotrigine; 27%), nonenzyme inducing (such as levetiracetam; 22%), enzyme inhibiting (valproate; 8%), and a fifth category that included women who were not on any antiepileptic drug (14%).
This analysis showed that the frequency of seizure increases was significantly greater with hormonal contraceptive use, compared with nonhormonal methods, across all five subgroups of antiepileptic drug type. In addition, the frequency of seizure increases with hormonal contraceptives differed significantly, depending on which antiepileptic drug type women used, but these significant differences among the antiepileptic drug types also occurred among women using nonhormonal contraception.
Women receiving a nonenzyme-inducing drug when starting a hormonal contraceptive reported the lowest frequency of seizure increases, a 12% rate. In contrast, women on an enzyme-inhibiting drug, valproate, had the highest rate of increased seizures when starting a hormonal contraceptive, 29%. This calculated out to about a 2.5-fold relative risk increase for having more seizures when starting hormonal contraception while on valproate, compared with women on a nonenzyme-inducing drug, Dr. Herzog reported.
Physicians “need to be on the lookout for the possibility that seizures could increase when women start a hormonal contraceptive,” he concluded.
On Twitter @mitchelzoler
PHILADELPHIA – Women with epilepsy often reported having an increased number of seizures when taking a hormonal contraceptive, according to data collected from 1,144 women with epilepsy who completed an online survey.
The data showed that women who used hormonal contraception reported having an increased number of seizures while on the contraceptive about 4.5-fold more often than did women who used nonhormonal contraception. The risk for an increased number of seizures with hormonal contraception seemed greatest for women treated with valproate.
Until now, “valproate was generally accepted as okay to use” by women also taking a hormonal contraceptive, but the new findings suggest that if a woman of childbearing age with epilepsy needs valproate for seizure control she would be better off using a nonhormonal form of contraception such as an intrauterine device, Dr. Andrew G. Herzog said while presenting a poster at the annual meeting of the American Epilepsy Society.
Dr. Herzog highlighted the need for some form of contraception for most younger women on valproate because of the drug’s potential teratogenic effects, but he also stressed that the risk for increased seizures does not appear to affect a majority of women. The survey results showed that overall only 28% of women with epilepsy reported an increased seizure frequency when using a hormonal contraceptive.
“The first goal of a neurologist is to get seizures under control, and you go with the [antiepileptic drugs] that work,” Dr. Herzog said in an interview. Once an effective regimen is found, the physician can then deal with other issues, such as adverse effects as well as the potential for an adverse interaction with a hormonal contraceptive. Valproate can be the antiepileptic drug of choice as it is one of the most effective agents for controlling seizures in patients with primary generalized epilepsy, said Dr. Herzog, professor of neurology at Harvard Medical School, Boston, and director of the neuroendocrine unit of Beth Israel Deaconess Medical Center in Wellesley, Mass.
The new data come from an Internet-based survey, which is subject to biases and appeared to attract a preponderance of responses from women who were better educated and had higher incomes than did the general population. In addition, the researchers collected the data retrospectively. Despite these limitations, the results are notable because they represent the only data set yet reported from a community-based source large enough to allow analysis of the many clinical variables that play into the potential interactions between various contraceptive types, various antiepileptic drug classes, and the diverse number of epilepsy subtypes, he said. Dr. Herzog and his associates are planning a study to collect similar data prospectively, but the results would likely not be available for at least about 5 years, he noted.
The Epilepsy Birth Control Registry enrolled women with epilepsy aged 18-47 years who had a history of using at least one form of contraception while on antiepileptic treatment, and the 1,144 women who completed the survey reported a total of 2,712 contraceptive experiences. The survey asked women, “Do you think this method of birth control changed how often you had seizures?” with the option to reply that their contraceptive method seemed to increase, decrease, or not change their seizure number.
One of the analyses done by Dr. Herzog and his associates compared the responses by women on any form of hormonal contraceptive (combined or progestin pill, hormonal patch, vaginal ring, depot medroxyprogesterone acetate, or implanted hormone) with women on any form of nonhormonal contraception (withdrawal, male or female condom, copper or progestin intrauterine device, or tubal ligation).
The results showed that 72% of women on any hormonal contraceptive and 91% of women on any form of nonhormonal contraceptive reported no change in their seizure frequency. The rates of reporting an increased number of seizures were 19% with hormonal contraceptives and 4% with nonhormonal contraceptives, which computed to a relative risk of about 4.5-fold for an increased number of seizures while on hormonal contraception, compared with nonhormonal contraception, the researchers reported.
Barrier contraception (male or female condoms) had the lowest rate of seizure increase among any of the nonhormonal methods. The risk for greater seizure frequency on hormonal contraceptives of all types was 6.75-fold higher when compared specifically with barrier contraception.
In analyses of specific types of hormonal contraceptives, women using a hormonal patch reported a 68% greater incidence of seizure increases, compared with women using combined oral contraceptive pills (the hormonal method that produced the fewest episodes of seizure increases). Those using a progestin-only pill had a 62% higher rate of seizure increases.
More women on hormonal contraceptives also reported having a decrease in seizures after starting contraception, compared with those starting on a nonhormonal method (9.5% vs. 5.2%, respectively), which calculated to a 85% relative rate increase for decreased seizures. Depot medroxyprogesterone acetate was the only specific hormonal contraceptive that linked with a higher rate of seizure decreases, compared with combined oral pills, a 95% higher rate.
A second analysis of the results by Dr. Herzog and his associates examined the frequencies of seizure outcomes on hormonal and nonhormonal contraceptives stratifying by type of antiepileptic drug women used when starting a particular contraceptive method. This analysis broke down antiepileptic drugs into four types: enzyme inducing (29%), glucuronidated (such as lamotrigine; 27%), nonenzyme inducing (such as levetiracetam; 22%), enzyme inhibiting (valproate; 8%), and a fifth category that included women who were not on any antiepileptic drug (14%).
This analysis showed that the frequency of seizure increases was significantly greater with hormonal contraceptive use, compared with nonhormonal methods, across all five subgroups of antiepileptic drug type. In addition, the frequency of seizure increases with hormonal contraceptives differed significantly, depending on which antiepileptic drug type women used, but these significant differences among the antiepileptic drug types also occurred among women using nonhormonal contraception.
Women receiving a nonenzyme-inducing drug when starting a hormonal contraceptive reported the lowest frequency of seizure increases, a 12% rate. In contrast, women on an enzyme-inhibiting drug, valproate, had the highest rate of increased seizures when starting a hormonal contraceptive, 29%. This calculated out to about a 2.5-fold relative risk increase for having more seizures when starting hormonal contraception while on valproate, compared with women on a nonenzyme-inducing drug, Dr. Herzog reported.
Physicians “need to be on the lookout for the possibility that seizures could increase when women start a hormonal contraceptive,” he concluded.
On Twitter @mitchelzoler
AT AES 2015
Key clinical point: Women with epilepsy often reported having more seizures while taking a hormonal contraceptive, compared with women using nonhormonal contraception.
Major finding: Epileptic women reported a 4.5-fold higher rate of increased seizures when using hormonal contraception, compared with nonhormonal contraception.
Data source: Internet-based survey completed by 1,144 women with epilepsy.
Disclosures: The study received partial support from Lundbeck. Dr. Herzog had no personal disclosures.