User login
Development and Validation of an Administrative Algorithm to Identify Veterans With Epilepsy
Development and Validation of an Administrative Algorithm to Identify Veterans With Epilepsy
Epilepsy affects about 4.5 million people in the United States and 150,000 new individuals are diagnosed each year.1,2 In 2019, epilepsy-attributable health care spending for noninstitutionalized people was around $5.4 billion and total epilepsy-attributable and epilepsy or seizure health care-related costs totaled $54 billion.3
Accurate surveillance of epilepsy in large health care systems can potentially improve health care delivery and resource allocation. A 2012 Institute of Medicine (IOM) report identified 13 recommendations to guide public health action on epilepsy, including validation of standard definitions for case ascertainment, identification of epilepsy through screening programs or protocols, and expansion of surveillance to better understand disease burden.4
A systematic review of validation studies concluded that it is reasonable to use administrative data to identify people with epilepsy in epidemiologic research. Combining The International Classification of Diseases (ICD) codes for epilepsy (ICD-10, G40-41; ICD-9, 345) with antiseizure medications (ASMs) could provide high positive predictive values (PPVs) and combining symptoms codes for convulsions (ICD-10, R56; ICD-9, 780.3, 780.39) with ASMs could lead to high sensitivity.5 However, identifying individuals with epilepsy from administrative data in large managed health care organizations is challenging.6 The IOM report noted that large managed health care organizations presented varying incidence and prevalence estimates due to differing methodology, geographic area, demographics, and definitions of epilepsy.
The Veterans Health Administration (VHA) is the largest integrated US health care system, providing care to > 9.1 million veterans.7 To improve the health and well-being of veterans with epilepsy (VWEs), a network of sites was established in 2008 called the US Department of Veterans Affairs (VA) Epilepsy Centers of Excellence (ECoE). Subsequent to the creation of the ECoE, efforts were made to identify VWEs within VHA databases.8,9 Prior to fiscal year (FY) 2016, the ECoE adopted a modified version of a well-established epilepsy diagnostic algorithm developed by Holden et al for large managed care organizations.10 The original algorithm identified patients by cross-matching ASMs with ICD-9 codes for an index year. But it failed to capture a considerable number of stable patients with epilepsy in the VHA due to incomplete documentation, and had false positives due to inclusion of patients identified from diagnostic clinics. The modified algorithm the ECoE used prior to FY 2016 considered additional prior years and excluded encounters from diagnostic clinics. The result was an improvement in the sensitivity and specificity of the algorithm. Researchers evaluating 500 patients with epilepsy estimated that the modified algorithm had a PPV of 82.0% (95% CI, 78.6%-85.4%).11
After implementation of ICD-10 codes in the VHA in FY 2016, the task of reliably and efficiently identifying VWE led to a 3-tier algorithm. This article presents a validation of the different tiers of this algorithm after the implementation of ICD-10 diagnosis codes and summarizes the surveillance data collected over the years within the VHA showing the trends of epilepsy.
Methods
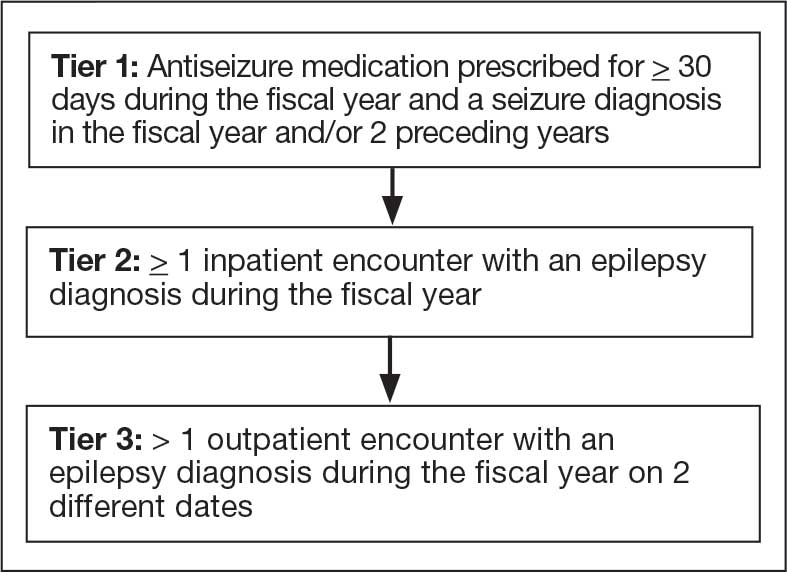
The VHA National Neurology office commissioned a Neurology Cube dashboard in FY 2021 in collaboration with VHA Support Service Center (VSSC) for reporting and surveillance of VWEs as a quality improvement initiative. The Neurology Cube uses a 3-tier system for identifying VWE in the VHA databases. VSSC programmers extract data from the VHA Corporate Data Warehouse (CDW) and utilize Microsoft SQL Server and Microsoft Power BI for Neurology Cube reports. The 3-tier system identifies VWE and divides them into distinct groups. The first tier identifies VWE with the highest degree of confidence; Tiers 2 and 3 represent identification with successively lesser degrees of confidence (Figure 1).
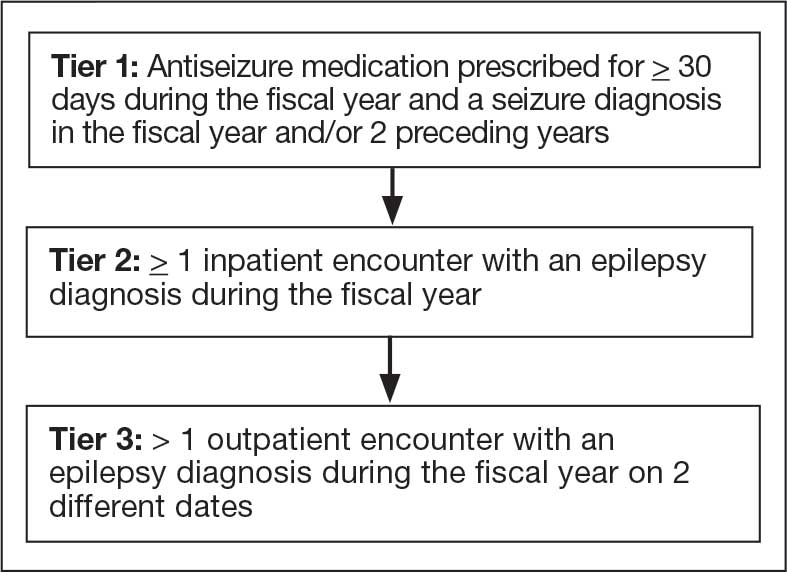
Tier 1
Definition. For a given index year and the preceding 2 years, any of following diagnosis codes on ≥ 1 clinical encounter are considered: 345.xx (epilepsy in ICD-9), 780.3x (other convulsions in ICD-9), G40.xxx (epilepsy in ICD-10), R40.4 (transient alteration of awareness), R56.1 (posttraumatic seizures), or R56.9 (unspecified convulsions). To reduce false positive rates, EEG clinic visits, which may include long-term monitoring, are excluded. Patients identified with ICD codes are then evaluated for an ASM prescription for ≥ 30 days during the index year. ASMs are listed in Appendix 1.
Validation. The development and validation of ICD-9 diagnosis codes crossmatched with an ASM prescription in the VHA has been published elsewhere.11 In FY 2017, after implementation of ICD-10 diagnostic codes, Tier 1 development and validation was performed in 2 phases. Even though Tier 1 study phases were conducted and completed during FY 2017, the patients for Tier 1 were identified from evaluation of FY 2016 data (October 1, 2015, to September 30, 2016). After the pilot analysis, the Tier 1 definition was implemented, and a chart review of 625 randomized patients was conducted at 5 sites for validation. Adequate preliminary data was not available to perform a sample size estimation for this study. Therefore, a practical target of 125 patients was set for Tier 1 from each site to obtain a final sample size of 625 patients. This second phase validated that the crossmatch of ICD-10 diagnosis codes with ASMs had a high PPV for identifying VWE.
Tiers 2 and 3
Definitions. For an index year, Tier 2 includes patients with ≥ 1 inpatient encounter documentation of either ICD-9 345.xx or ICD-10 G40.xxx, excluding EEG clinics. Tier 3 Includes patients who have had ≥ 2 outpatient encounters with diagnosis codes 345.xx or G40.xxx on 2 separate days, excluding EEG clinics. Tiers 2 and 3 do not require ASM prescriptions; this helps to identify VWEs who may be getting their medications outside of VHA or those who have received a new diagnosis.
Validations. Tiers 2 and 3 were included in the epilepsy identification algorithm in FY 2021 after validation was performed on a sample of 8 patients in each tier. Five patients were subsequently identified as having epilepsy in Tier 2 and 6 patients were identified in Tier 3. A more comprehensive validation of Tiers 2 and 3 was performed during FY 2022 that included patients at 5 sites seen during FY 2019 to FY 2022. Since yearly trends showed only about 8% of total patients were identified as having epilepsy through Tiers 2 and 3 we sought ≥ 20 patients per tier for the 5 sites for a total of 200 patients to ensure representation across the VHA. The final count was 126 patients for Tier 2 and 174 patients for Tier 3 (n = 300).
Gold Standard Criteria for Epilepsy Diagnosis
We used the International League Against Epilepsy (ILAE) definition of epilepsy for the validation of the 3 algorithm tiers. ILAE defines epilepsy as ≥ 2 unprovoked (or reflex) seizures occurring > 24 hours apart or 1 unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (≥ 60%) after 2 unprovoked seizures, occurring over the next 10 years.12
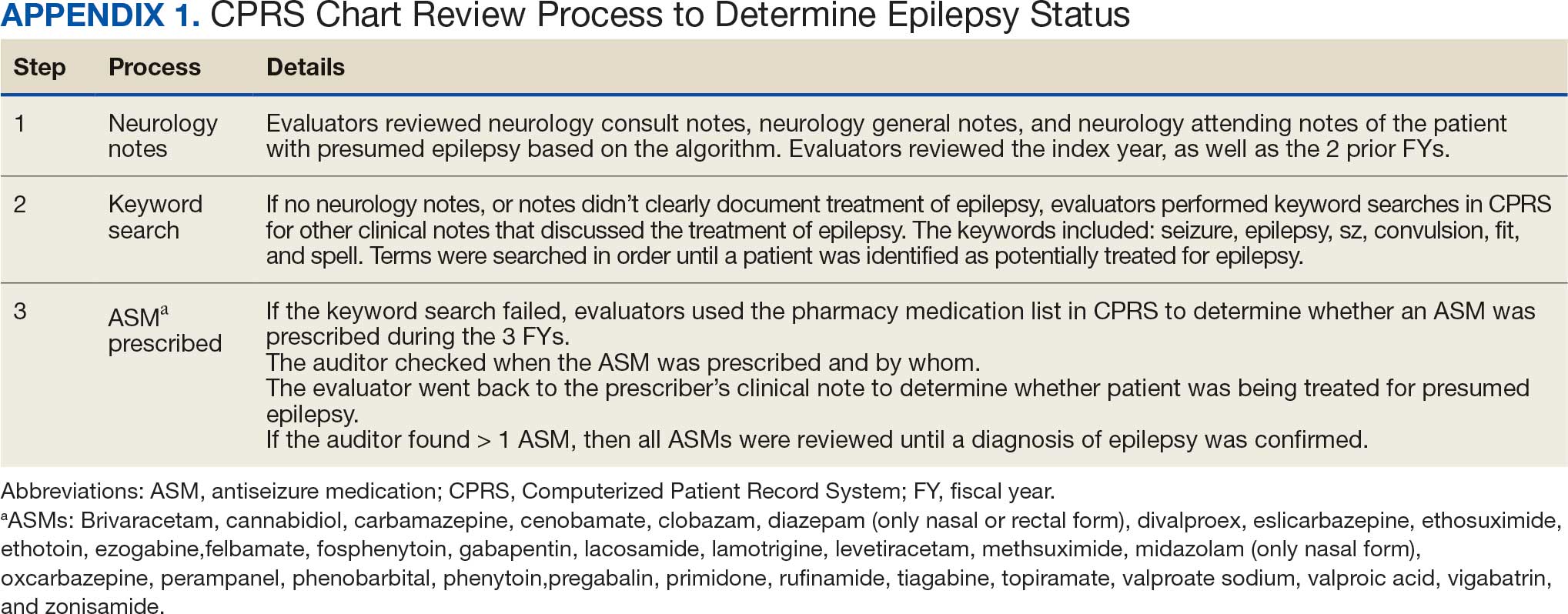
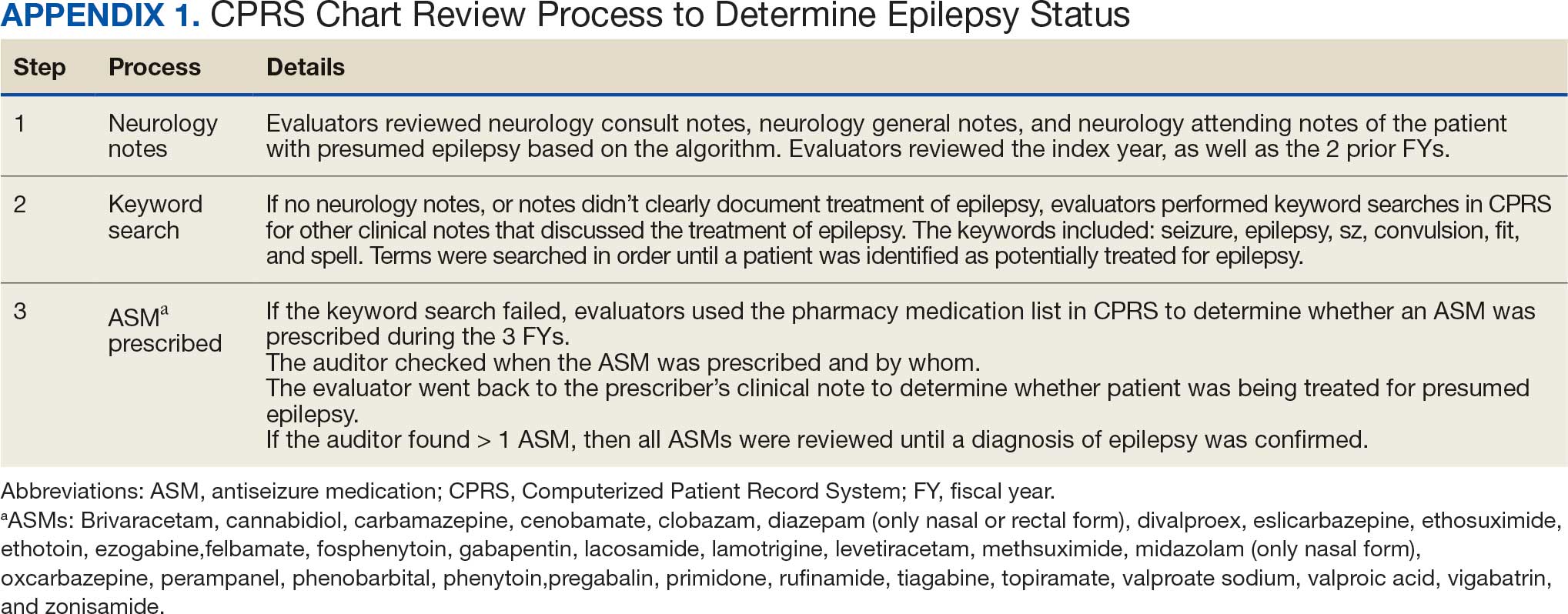
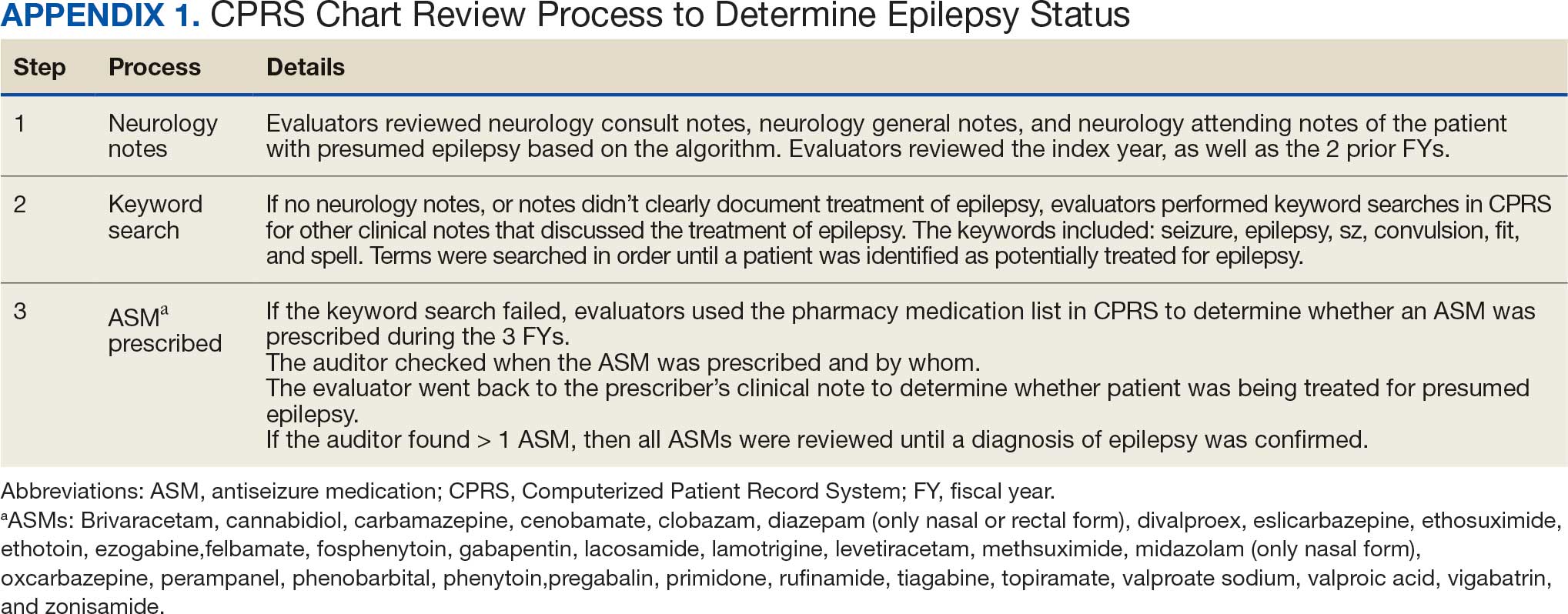
A standard protocol was provided to evaluators to identify patients using the VHA Computerized Patient Record System (Appendix 1). After review, evaluators categorized each patient in 1 of 4 ways: (1) Yes, definite: The patient’s health care practitioner (HCP) believes the patient has epilepsy and is treating with medication; (2) Yes, uncertain: The HCP has enough suspicion of epilepsy that a medication is prescribed, but uncertainty is expressed of the diagnosis; (3) No, definite: The HCP does not believe the patient has epilepsy and is therefore not treating with medication for seizure; (4) No, uncertain: The HCP is not treating with medication for epilepsy, because the diagnostic suspicion is not high enough, but there is suspicion for epilepsy.
As a quality improvement operational project, the Epilepsy National Program Office approved this validation project and determined that institutional review board approval was not required.
Statistical Analysis
Counts and percentages were computed for categories of epilepsy status. PPV of each tier was estimated with asymptotic 95% CIs.
Results
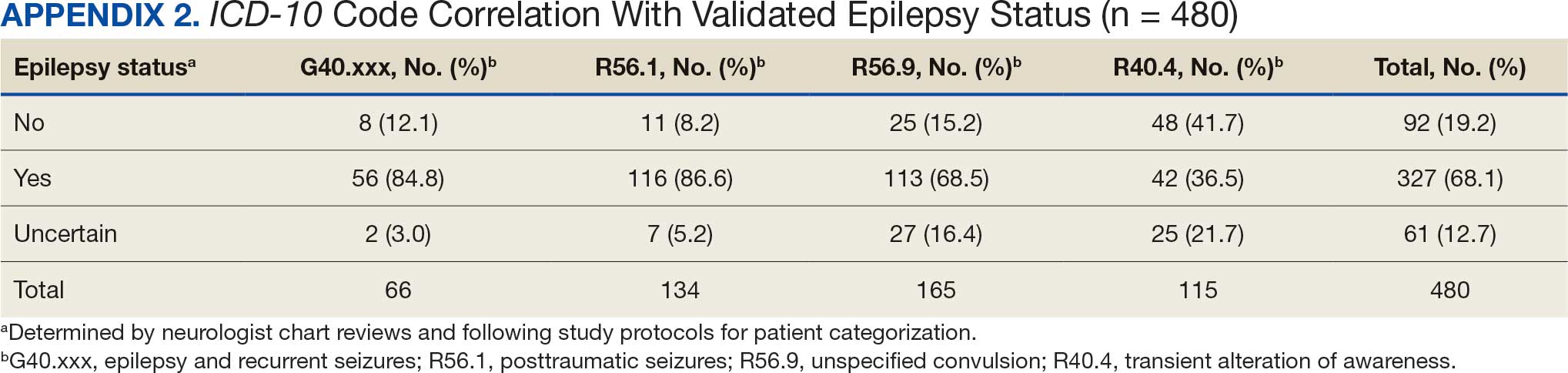
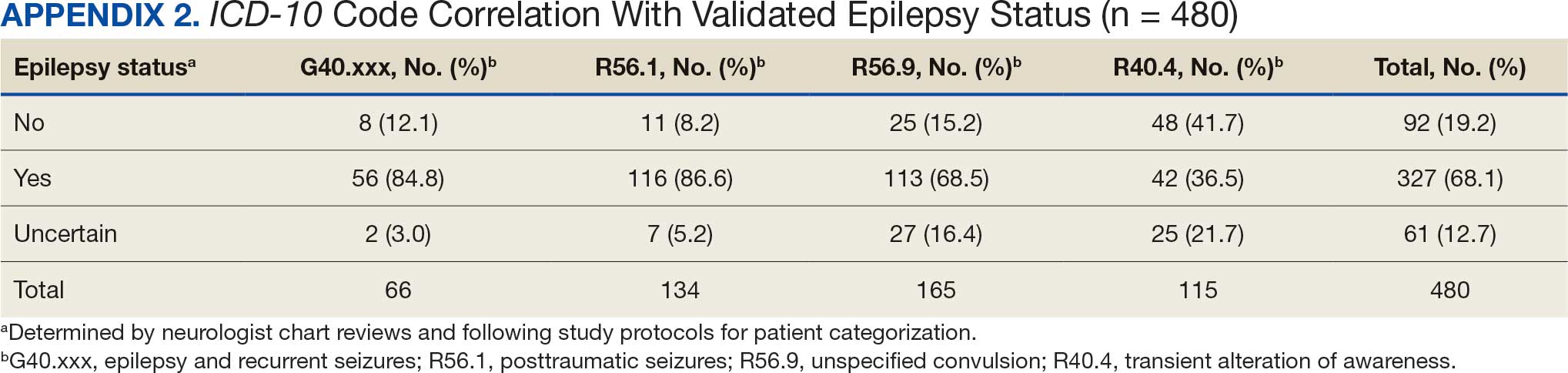
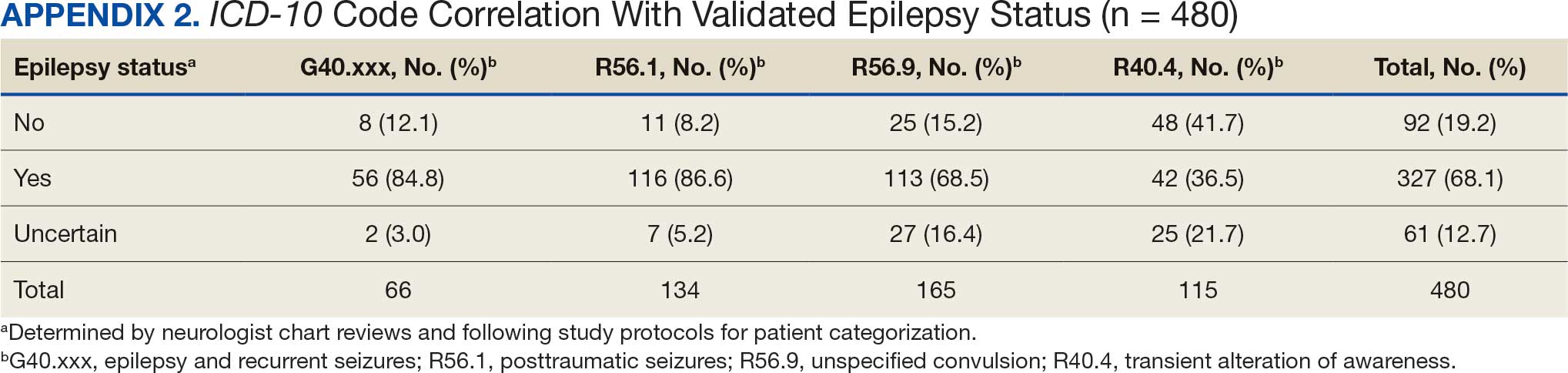
ICD-10 codes for 480 patients were evaluated in Tier 1 phase 1; 13.8% were documented with G40.xxx, 27.9% with R56.1, 34.4% with R56.9, and 24.0% with R40.4 (Appendix 2). In total, 68.1% fulfilled the criteria of epilepsy, 19.2% did not, and 12.7% were uncertain). From the validation of Tier 1 phase 2 (n = 625), the PPV of the algorithm for patients presumed to have epilepsy (definite and uncertain) was 85.1% (95% CI, 82.1%-87.8%) (Table).
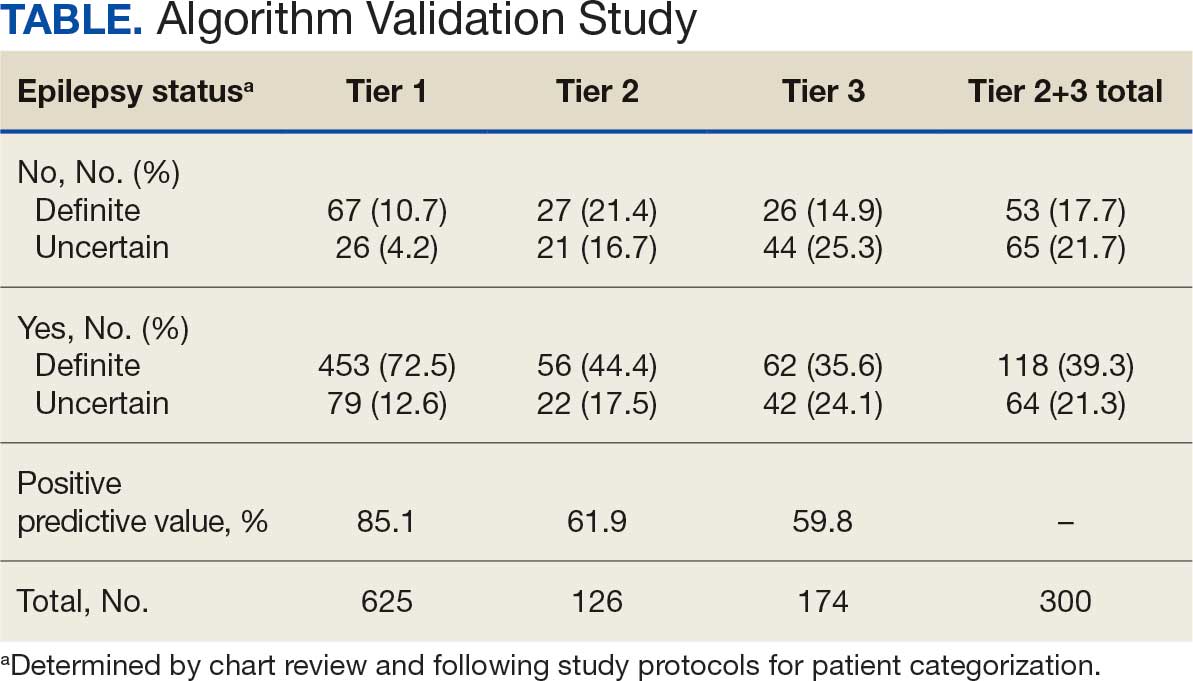
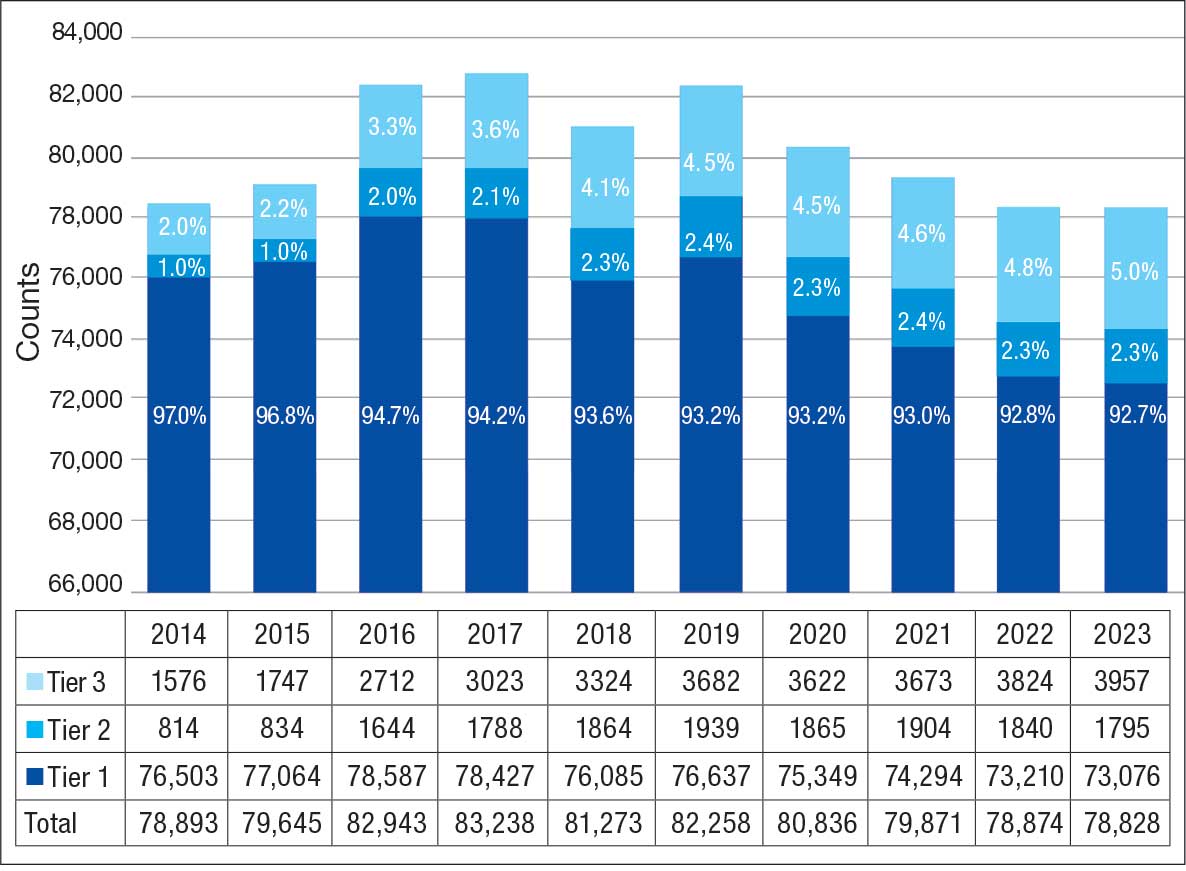
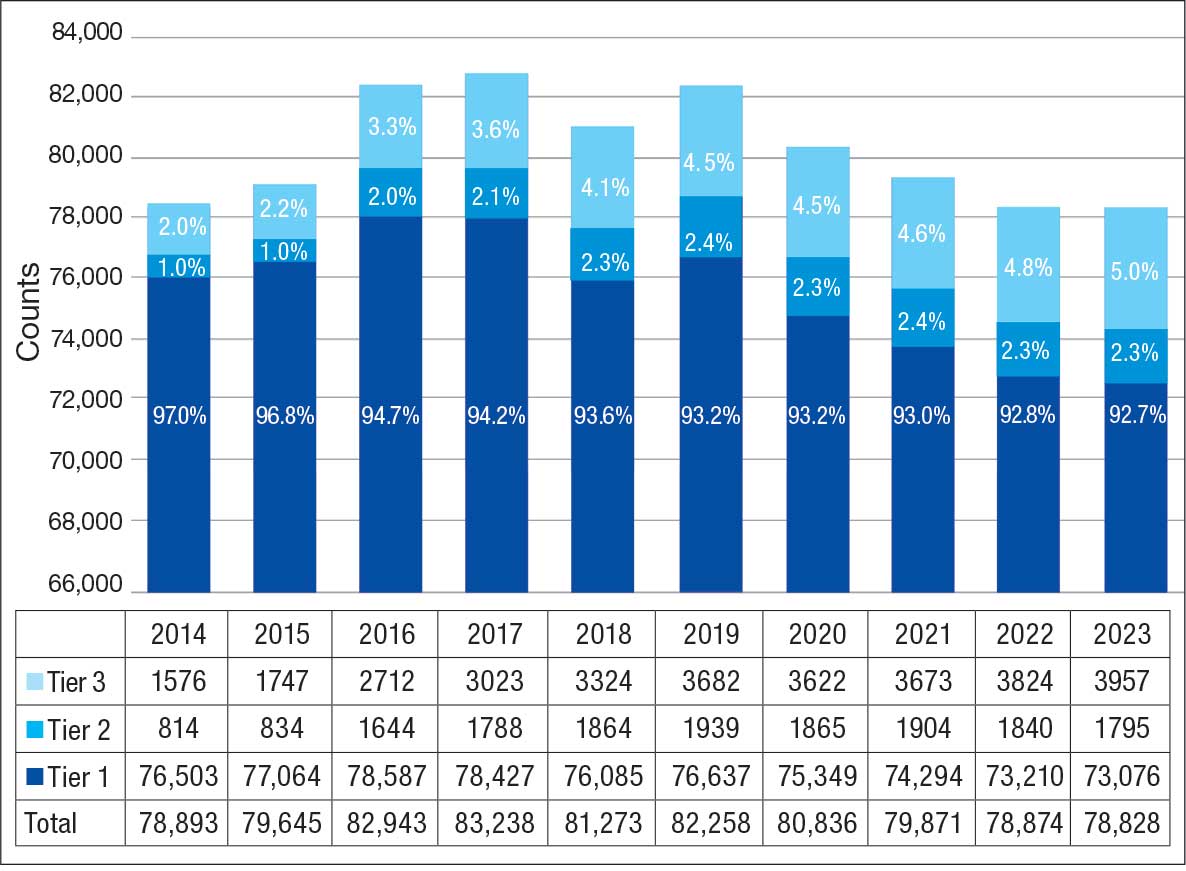
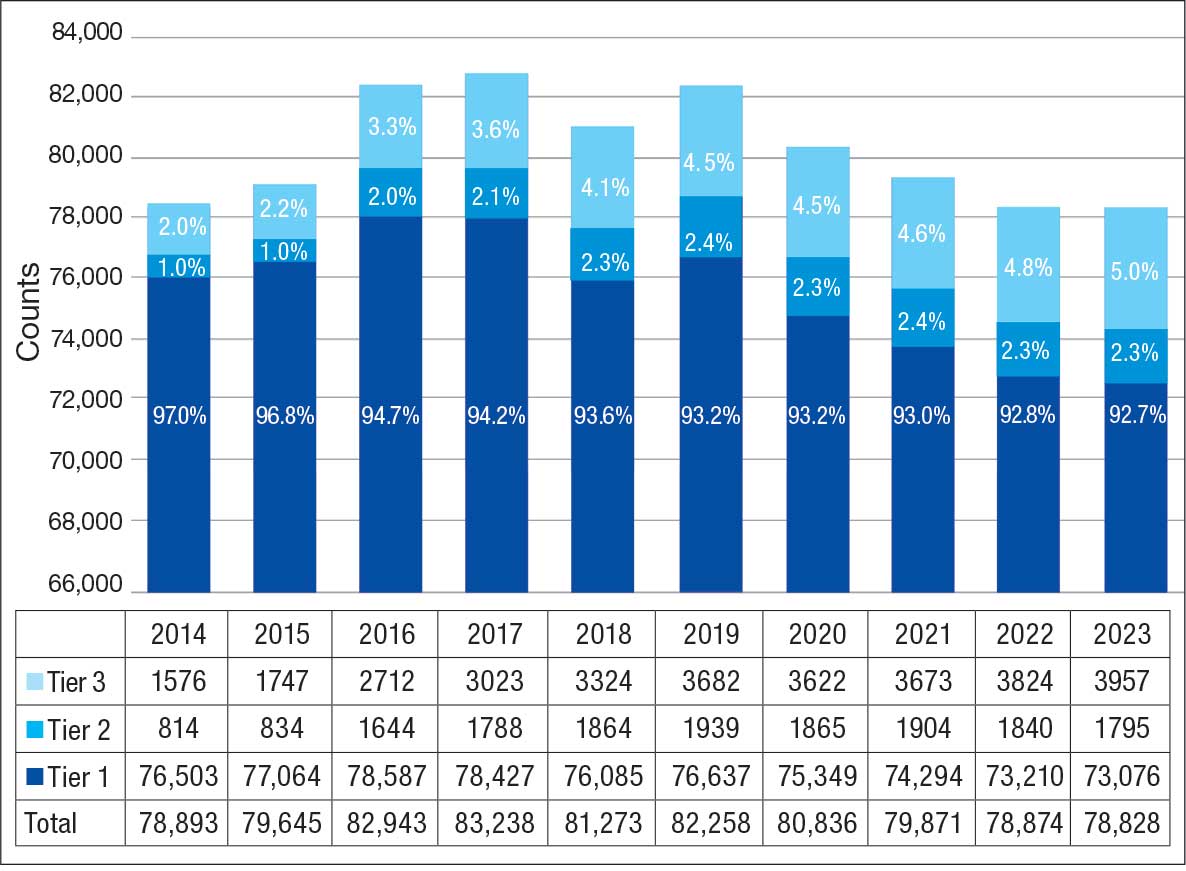
Of 300 patients evaluated, 126 (42.0%) were evaluated for Tier 2 with a PPV of 61.9% (95% CI, 53.4%-70.4%), and 174 (58.0%) patients were evaluated for Tier 3 with a PPV of 59.8% (95% CI, 52.5%-67.1%. The PPV of the algorithm for patients presumed to have epilepsy (definite and uncertain) were combined to calculate the PPV. Estimates of VHA VWE counts were computed for each tier from FY 2014 to FY 2023 using the VSSC Neurology Cube (Figure 2). For all years, > 92% patients were classified using the Tier 1 definition.
Discussion
The development and validation of the 3-tier diagnostic algorithm represents an important advancement in the surveillance and management of epilepsy among veterans within the VHA. The validation of this algorithm also demonstrates its practical utility in a large, integrated health care system.
Specific challenges were encountered when attempting to use pre-existing algorithms; these challenges included differences in the usage patterns of diagnostic codes and the patterns of ASM use within the VHA. These challenges prompted the need for a tailored approach, which led to the development of this algorithm. The inclusion of additional ICD-10 codes led to further revisions and subsequent validation. While many of the basic concepts of the algorithm, including ICD codes and ASMs, could work in other institutions, it would be wise for health care organizations to develop their own algorithms because of certain variables, including organizational size, patient demographics, common comorbidities, and the specific configurations of electronic health records and administrative data systems.
Studies have shown that ICD-10 codes for epilepsy (G40.* and/or R56.9) perform well in identifying epilepsy whether they are assigned by neurologists (sensitivity, 97.7%; specificity, 44.1%; PPV, 96.2%; negative predictive value, 57.7%), or in emergency department or hospital discharges (PPV, 75.5%).13,14 The pilot study of the algorithm’s Tier 1 development (phase 1) evaluated whether the selected ICD-10 diagnostic codes accurately included the VWE population within the VHA and revealed that while most codes (eg, epilepsy [G40.xxx]; posttraumatic seizures [R56.1]; and unspecified convulsions [R56.9]), had a low false positive rate (< 16%), the R40.4 code (transient alteration of awareness) had a higher false positivity of 42%. While this is not surprising given the broad spectrum of conditions that can manifest as transient alteration of awareness, it underscores the inherent challenges in diagnosing epilepsy using diagnosis codes.
In phase 2, the Tier 1 algorithm was validated as effective for identifying VWE in the VHA system, as its PPV was determined to be high (85%). In comparison, Tiers 2 and 3, whose criteria did not require data on VHA prescribed ASM use, had lower tiers of epilepsy predictability (PPV about 60% for both). This was thought to be acceptable because Tiers 2 and 3 represent a smaller population of the identified VWEs (about 8%). These VWEs may otherwise have been missed, partly because veterans are not required to get ASMs from the VHA.
Upon VHA implementation in FY 2021, this diagnostic algorithm exhibited significant clinical utility when integrated within the VSSC Neurology Cube. It facilitated an efficient approach to identifying VWEs using readily available databases. This led to better tracking of real-time epilepsy cases, which facilitated improving current resource allocation and targeted intervention strategies such as identification of drug-resistant epilepsy patients, optimizing strategies for telehealth and patient outreach for awareness of epilepsy care resources within VHA. Meanwhile, data acquired by the algorithm over the decade since its development (FY 2014 to FY 2023) contributed to more accurate epidemiologic information and identification of historic trends. Development of the algorithm represents one of the ways ECoEs have led to improved care for VWEs. ECoEs have been shown to improve health care for veterans in several metrics.15
A strength of this study is the rigorous multitiered validation process to confirm the diagnostic accuracy of ICD-10 codes against the gold standard ILAE definition of epilepsy to identify “definite” epilepsy cases within the VHA. The use of specific ICD codes further enhances the precision of epilepsy diagnoses. The inclusion of ASMs, which are sometimes prescribed for conditions other than epilepsy, could potentially inflate false positive rates.16
This study focused exclusively on the identification and validation of definite epilepsy cases within the VHA VSSC database, employing more stringent diagnostic criteria to ensure the highest level of certainty in ascertaining epilepsy. It is important to note there is a separate category of probable epilepsy, which involves a broader set of diagnostic criteria. While not covered in this study, probable epilepsy would be subject to future research and validation, which could provide insights into a wider spectrum of epilepsy diagnoses. Such future research could help refine the algorithm’s applicability and accuracy and potentially lead to more comprehensive surveillance and management strategies in clinical practice.
This study highlights the inherent challenges in leveraging administrative data for disease identification, particularly for conditions such as epilepsy, where diagnostic clarity can be complex. However, other conditions such as multiple sclerosis have noted similar success with the use of VHA administrative data for categorizing disease.17
Limitations
The algorithm discussed in this article is, in and of itself, generalizable. However, the validation process was unique to the VHA patient population, limiting the generalizability of the findings. Documentation practices and HCP attitudes within the VHA may differ from those in other health care settings. Identifying people with epilepsy can be challenging because of changing definitions of epilepsy over time. In addition to clinical evaluation, EEG and magnetic resonance imaging results, response to ASM treatment, and video-EEG monitoring of habitual events all can help establish the diagnosis. Therefore, studies may vary in how inclusive or exclusive the criteria are. ASMs such as gabapentin, pregabalin, carbamazepine, lamotrigine, topiramate, and valproate are used to treat other conditions, including headaches, generalized pain, and mood disorders. Consequently, including these ASMs in the Tier 1 definition may have increased the false positive rate. Additional research is needed to evaluate whether excluding these ASMs from the algorithm based on specific criteria (eg, dose of ASM used) can further refine the algorithm to identify patients with epilepsy.
Further refinement of this algorithm may also occur as technology changes. Future electronic health records may allow better tracking of different epilepsy factors, the integration of additional diagnostic criteria, and the use of natural language processing or other forms of artificial intelligence.
Conclusions
This study presents a significant step forward in epilepsy surveillance within the VHA. The algorithm offers a robust tool for identifying VWEs with good PPVs, facilitating better resource allocation and targeted care. Despite its limitations, this research lays a foundation for future advancements in the management and understanding of epilepsy within large health care systems. Since this VHA algorithm is based on ASMs and ICD diagnosis codes from patient records, other large managed health care systems also may be able to adapt this algorithm to their data specifications.
- Kobau R, Luncheon C, Greenlund K. Active epilepsy prevalence among U.S. adults is 1.1% and differs by educational level-National Health Interview Survey, United States, 2021. Epilepsy Behav. 2023;142:109180. doi:10.1016/j.yebeh.2023.109180
- GBD 2017 US Neurological Disorders Collaborators, Feigin VL, Vos T, et al. Burden of neurological disorders across the US from 1990-2017: a global burden of disease study. JAMA Neurol. 2021;78:165-176. doi:10.1001/jamaneurol.2020.4152
- Moura LMVR, Karakis I, Zack MM, et al. Drivers of US health care spending for persons with seizures and/or epilepsies, 2010-2018. Epilepsia. 2022;63:2144-2154. doi:10.1111/epi.17305
- Institute of Medicine. Epilepsy Across the Spectrum: Promoting Health and Understanding. The National Academies Press; 2012. Accessed November 11, 2025. www.nap.edu/catalog/13379
- Mbizvo GK, Bennett KH, Schnier C, Simpson CR, Duncan SE, Chin RFM. The accuracy of using administrative healthcare data to identify epilepsy cases: A systematic review of validation studies. Epilepsia. 2020;61:1319-1335. doi:10.1111/epi.16547
- Montouris GD. How will primary care physicians, specialists, and managed care treat epilepsy in the new millennium? Neurology. 2000;55:S42-S44.
- US Department of Veterans Affairs. Veterans Health Administration: About VHA. Accessed November 11, 2025. https://www.va.gov/health/aboutvha.asp
- Veterans’ Mental Health and Other Care Improvements Act of 2008, S 2162, 110th Cong (2008). Accessed November 11, 2025. https://www.congress.gov/bill/110th-congress/senate-bill/2162
- Rehman R, Kelly PR, Husain AM, Tran TT. Characteristics of Veterans diagnosed with seizures within Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762. doi:10.1682/JRRD.2014.10.0241
- Holden EW, Grossman E, Nguyen HT, et al. Developing a computer algorithm to identify epilepsy cases in managed care organizations. Dis Manag. 2005;8:1-14. doi:10.1089/dis.2005.8.1
- Rehman R, Everhart A, Frontera AT, et al. Implementation of an established algorithm and modifications for the identification of epilepsy patients in the Veterans Health Administration. Epilepsy Res. 2016;127:284-290. doi:10.1016/j.eplepsyres.2016.09.012
- Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475-482. doi:10.1111/epi.12550
- Smith JR, Jones FJS, Fureman BE, et al. Accuracy of ICD-10-CM claims-based definitions for epilepsy and seizure type. Epilepsy Res. 2020;166:106414. doi:10.1016/j.eplepsyres.2020.106414
- Jetté N, Reid AY, Quan H, et al. How accurate is ICD coding for epilepsy? Epilepsia. 2010;51:62-69. doi:10.1111/j.1528-1167.2009.02201.x
- Kelly P, Chinta R, Privitera G. Do centers of excellence reduce health care costs? Evidence from the US Veterans Health Administration Centers for Epilepsy. Glob Bus Organ Excell. 2015;34:18-29.
- Haneef Z, Rehman R, Husain AM. Association between standardized mortality ratio and utilization of care in US veterans with drug-resistant epilepsy compared with all US veterans and the US general population. JAMA Neurol. 2022;79:879-887. doi:10.1001/jamaneurol.2022.2290
- Culpepper WJ, Marrie RA, Langer-Gould A, et al. Validation of an algorithm for identifying MS cases in administrative health claims datasets. Neurology. 2019;92:e1016-e1028 doi:10.1212/WNL.0000000000007043
Epilepsy affects about 4.5 million people in the United States and 150,000 new individuals are diagnosed each year.1,2 In 2019, epilepsy-attributable health care spending for noninstitutionalized people was around $5.4 billion and total epilepsy-attributable and epilepsy or seizure health care-related costs totaled $54 billion.3
Accurate surveillance of epilepsy in large health care systems can potentially improve health care delivery and resource allocation. A 2012 Institute of Medicine (IOM) report identified 13 recommendations to guide public health action on epilepsy, including validation of standard definitions for case ascertainment, identification of epilepsy through screening programs or protocols, and expansion of surveillance to better understand disease burden.4
A systematic review of validation studies concluded that it is reasonable to use administrative data to identify people with epilepsy in epidemiologic research. Combining The International Classification of Diseases (ICD) codes for epilepsy (ICD-10, G40-41; ICD-9, 345) with antiseizure medications (ASMs) could provide high positive predictive values (PPVs) and combining symptoms codes for convulsions (ICD-10, R56; ICD-9, 780.3, 780.39) with ASMs could lead to high sensitivity.5 However, identifying individuals with epilepsy from administrative data in large managed health care organizations is challenging.6 The IOM report noted that large managed health care organizations presented varying incidence and prevalence estimates due to differing methodology, geographic area, demographics, and definitions of epilepsy.
The Veterans Health Administration (VHA) is the largest integrated US health care system, providing care to > 9.1 million veterans.7 To improve the health and well-being of veterans with epilepsy (VWEs), a network of sites was established in 2008 called the US Department of Veterans Affairs (VA) Epilepsy Centers of Excellence (ECoE). Subsequent to the creation of the ECoE, efforts were made to identify VWEs within VHA databases.8,9 Prior to fiscal year (FY) 2016, the ECoE adopted a modified version of a well-established epilepsy diagnostic algorithm developed by Holden et al for large managed care organizations.10 The original algorithm identified patients by cross-matching ASMs with ICD-9 codes for an index year. But it failed to capture a considerable number of stable patients with epilepsy in the VHA due to incomplete documentation, and had false positives due to inclusion of patients identified from diagnostic clinics. The modified algorithm the ECoE used prior to FY 2016 considered additional prior years and excluded encounters from diagnostic clinics. The result was an improvement in the sensitivity and specificity of the algorithm. Researchers evaluating 500 patients with epilepsy estimated that the modified algorithm had a PPV of 82.0% (95% CI, 78.6%-85.4%).11
After implementation of ICD-10 codes in the VHA in FY 2016, the task of reliably and efficiently identifying VWE led to a 3-tier algorithm. This article presents a validation of the different tiers of this algorithm after the implementation of ICD-10 diagnosis codes and summarizes the surveillance data collected over the years within the VHA showing the trends of epilepsy.
Methods
The VHA National Neurology office commissioned a Neurology Cube dashboard in FY 2021 in collaboration with VHA Support Service Center (VSSC) for reporting and surveillance of VWEs as a quality improvement initiative. The Neurology Cube uses a 3-tier system for identifying VWE in the VHA databases. VSSC programmers extract data from the VHA Corporate Data Warehouse (CDW) and utilize Microsoft SQL Server and Microsoft Power BI for Neurology Cube reports. The 3-tier system identifies VWE and divides them into distinct groups. The first tier identifies VWE with the highest degree of confidence; Tiers 2 and 3 represent identification with successively lesser degrees of confidence (Figure 1).
Tier 1
Definition. For a given index year and the preceding 2 years, any of following diagnosis codes on ≥ 1 clinical encounter are considered: 345.xx (epilepsy in ICD-9), 780.3x (other convulsions in ICD-9), G40.xxx (epilepsy in ICD-10), R40.4 (transient alteration of awareness), R56.1 (posttraumatic seizures), or R56.9 (unspecified convulsions). To reduce false positive rates, EEG clinic visits, which may include long-term monitoring, are excluded. Patients identified with ICD codes are then evaluated for an ASM prescription for ≥ 30 days during the index year. ASMs are listed in Appendix 1.
Validation. The development and validation of ICD-9 diagnosis codes crossmatched with an ASM prescription in the VHA has been published elsewhere.11 In FY 2017, after implementation of ICD-10 diagnostic codes, Tier 1 development and validation was performed in 2 phases. Even though Tier 1 study phases were conducted and completed during FY 2017, the patients for Tier 1 were identified from evaluation of FY 2016 data (October 1, 2015, to September 30, 2016). After the pilot analysis, the Tier 1 definition was implemented, and a chart review of 625 randomized patients was conducted at 5 sites for validation. Adequate preliminary data was not available to perform a sample size estimation for this study. Therefore, a practical target of 125 patients was set for Tier 1 from each site to obtain a final sample size of 625 patients. This second phase validated that the crossmatch of ICD-10 diagnosis codes with ASMs had a high PPV for identifying VWE.
Tiers 2 and 3
Definitions. For an index year, Tier 2 includes patients with ≥ 1 inpatient encounter documentation of either ICD-9 345.xx or ICD-10 G40.xxx, excluding EEG clinics. Tier 3 Includes patients who have had ≥ 2 outpatient encounters with diagnosis codes 345.xx or G40.xxx on 2 separate days, excluding EEG clinics. Tiers 2 and 3 do not require ASM prescriptions; this helps to identify VWEs who may be getting their medications outside of VHA or those who have received a new diagnosis.
Validations. Tiers 2 and 3 were included in the epilepsy identification algorithm in FY 2021 after validation was performed on a sample of 8 patients in each tier. Five patients were subsequently identified as having epilepsy in Tier 2 and 6 patients were identified in Tier 3. A more comprehensive validation of Tiers 2 and 3 was performed during FY 2022 that included patients at 5 sites seen during FY 2019 to FY 2022. Since yearly trends showed only about 8% of total patients were identified as having epilepsy through Tiers 2 and 3 we sought ≥ 20 patients per tier for the 5 sites for a total of 200 patients to ensure representation across the VHA. The final count was 126 patients for Tier 2 and 174 patients for Tier 3 (n = 300).
Gold Standard Criteria for Epilepsy Diagnosis
We used the International League Against Epilepsy (ILAE) definition of epilepsy for the validation of the 3 algorithm tiers. ILAE defines epilepsy as ≥ 2 unprovoked (or reflex) seizures occurring > 24 hours apart or 1 unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (≥ 60%) after 2 unprovoked seizures, occurring over the next 10 years.12
A standard protocol was provided to evaluators to identify patients using the VHA Computerized Patient Record System (Appendix 1). After review, evaluators categorized each patient in 1 of 4 ways: (1) Yes, definite: The patient’s health care practitioner (HCP) believes the patient has epilepsy and is treating with medication; (2) Yes, uncertain: The HCP has enough suspicion of epilepsy that a medication is prescribed, but uncertainty is expressed of the diagnosis; (3) No, definite: The HCP does not believe the patient has epilepsy and is therefore not treating with medication for seizure; (4) No, uncertain: The HCP is not treating with medication for epilepsy, because the diagnostic suspicion is not high enough, but there is suspicion for epilepsy.
As a quality improvement operational project, the Epilepsy National Program Office approved this validation project and determined that institutional review board approval was not required.
Statistical Analysis
Counts and percentages were computed for categories of epilepsy status. PPV of each tier was estimated with asymptotic 95% CIs.
Results
ICD-10 codes for 480 patients were evaluated in Tier 1 phase 1; 13.8% were documented with G40.xxx, 27.9% with R56.1, 34.4% with R56.9, and 24.0% with R40.4 (Appendix 2). In total, 68.1% fulfilled the criteria of epilepsy, 19.2% did not, and 12.7% were uncertain). From the validation of Tier 1 phase 2 (n = 625), the PPV of the algorithm for patients presumed to have epilepsy (definite and uncertain) was 85.1% (95% CI, 82.1%-87.8%) (Table).
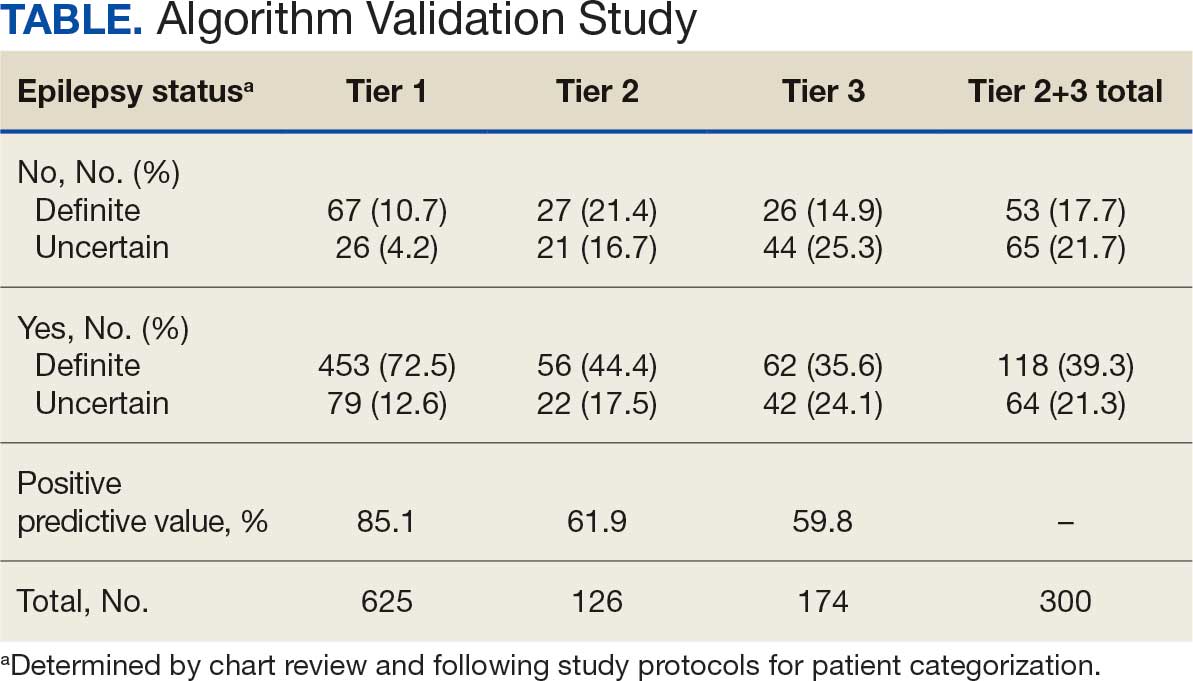
Of 300 patients evaluated, 126 (42.0%) were evaluated for Tier 2 with a PPV of 61.9% (95% CI, 53.4%-70.4%), and 174 (58.0%) patients were evaluated for Tier 3 with a PPV of 59.8% (95% CI, 52.5%-67.1%. The PPV of the algorithm for patients presumed to have epilepsy (definite and uncertain) were combined to calculate the PPV. Estimates of VHA VWE counts were computed for each tier from FY 2014 to FY 2023 using the VSSC Neurology Cube (Figure 2). For all years, > 92% patients were classified using the Tier 1 definition.
Discussion
The development and validation of the 3-tier diagnostic algorithm represents an important advancement in the surveillance and management of epilepsy among veterans within the VHA. The validation of this algorithm also demonstrates its practical utility in a large, integrated health care system.
Specific challenges were encountered when attempting to use pre-existing algorithms; these challenges included differences in the usage patterns of diagnostic codes and the patterns of ASM use within the VHA. These challenges prompted the need for a tailored approach, which led to the development of this algorithm. The inclusion of additional ICD-10 codes led to further revisions and subsequent validation. While many of the basic concepts of the algorithm, including ICD codes and ASMs, could work in other institutions, it would be wise for health care organizations to develop their own algorithms because of certain variables, including organizational size, patient demographics, common comorbidities, and the specific configurations of electronic health records and administrative data systems.
Studies have shown that ICD-10 codes for epilepsy (G40.* and/or R56.9) perform well in identifying epilepsy whether they are assigned by neurologists (sensitivity, 97.7%; specificity, 44.1%; PPV, 96.2%; negative predictive value, 57.7%), or in emergency department or hospital discharges (PPV, 75.5%).13,14 The pilot study of the algorithm’s Tier 1 development (phase 1) evaluated whether the selected ICD-10 diagnostic codes accurately included the VWE population within the VHA and revealed that while most codes (eg, epilepsy [G40.xxx]; posttraumatic seizures [R56.1]; and unspecified convulsions [R56.9]), had a low false positive rate (< 16%), the R40.4 code (transient alteration of awareness) had a higher false positivity of 42%. While this is not surprising given the broad spectrum of conditions that can manifest as transient alteration of awareness, it underscores the inherent challenges in diagnosing epilepsy using diagnosis codes.
In phase 2, the Tier 1 algorithm was validated as effective for identifying VWE in the VHA system, as its PPV was determined to be high (85%). In comparison, Tiers 2 and 3, whose criteria did not require data on VHA prescribed ASM use, had lower tiers of epilepsy predictability (PPV about 60% for both). This was thought to be acceptable because Tiers 2 and 3 represent a smaller population of the identified VWEs (about 8%). These VWEs may otherwise have been missed, partly because veterans are not required to get ASMs from the VHA.
Upon VHA implementation in FY 2021, this diagnostic algorithm exhibited significant clinical utility when integrated within the VSSC Neurology Cube. It facilitated an efficient approach to identifying VWEs using readily available databases. This led to better tracking of real-time epilepsy cases, which facilitated improving current resource allocation and targeted intervention strategies such as identification of drug-resistant epilepsy patients, optimizing strategies for telehealth and patient outreach for awareness of epilepsy care resources within VHA. Meanwhile, data acquired by the algorithm over the decade since its development (FY 2014 to FY 2023) contributed to more accurate epidemiologic information and identification of historic trends. Development of the algorithm represents one of the ways ECoEs have led to improved care for VWEs. ECoEs have been shown to improve health care for veterans in several metrics.15
A strength of this study is the rigorous multitiered validation process to confirm the diagnostic accuracy of ICD-10 codes against the gold standard ILAE definition of epilepsy to identify “definite” epilepsy cases within the VHA. The use of specific ICD codes further enhances the precision of epilepsy diagnoses. The inclusion of ASMs, which are sometimes prescribed for conditions other than epilepsy, could potentially inflate false positive rates.16
This study focused exclusively on the identification and validation of definite epilepsy cases within the VHA VSSC database, employing more stringent diagnostic criteria to ensure the highest level of certainty in ascertaining epilepsy. It is important to note there is a separate category of probable epilepsy, which involves a broader set of diagnostic criteria. While not covered in this study, probable epilepsy would be subject to future research and validation, which could provide insights into a wider spectrum of epilepsy diagnoses. Such future research could help refine the algorithm’s applicability and accuracy and potentially lead to more comprehensive surveillance and management strategies in clinical practice.
This study highlights the inherent challenges in leveraging administrative data for disease identification, particularly for conditions such as epilepsy, where diagnostic clarity can be complex. However, other conditions such as multiple sclerosis have noted similar success with the use of VHA administrative data for categorizing disease.17
Limitations
The algorithm discussed in this article is, in and of itself, generalizable. However, the validation process was unique to the VHA patient population, limiting the generalizability of the findings. Documentation practices and HCP attitudes within the VHA may differ from those in other health care settings. Identifying people with epilepsy can be challenging because of changing definitions of epilepsy over time. In addition to clinical evaluation, EEG and magnetic resonance imaging results, response to ASM treatment, and video-EEG monitoring of habitual events all can help establish the diagnosis. Therefore, studies may vary in how inclusive or exclusive the criteria are. ASMs such as gabapentin, pregabalin, carbamazepine, lamotrigine, topiramate, and valproate are used to treat other conditions, including headaches, generalized pain, and mood disorders. Consequently, including these ASMs in the Tier 1 definition may have increased the false positive rate. Additional research is needed to evaluate whether excluding these ASMs from the algorithm based on specific criteria (eg, dose of ASM used) can further refine the algorithm to identify patients with epilepsy.
Further refinement of this algorithm may also occur as technology changes. Future electronic health records may allow better tracking of different epilepsy factors, the integration of additional diagnostic criteria, and the use of natural language processing or other forms of artificial intelligence.
Conclusions
This study presents a significant step forward in epilepsy surveillance within the VHA. The algorithm offers a robust tool for identifying VWEs with good PPVs, facilitating better resource allocation and targeted care. Despite its limitations, this research lays a foundation for future advancements in the management and understanding of epilepsy within large health care systems. Since this VHA algorithm is based on ASMs and ICD diagnosis codes from patient records, other large managed health care systems also may be able to adapt this algorithm to their data specifications.
Epilepsy affects about 4.5 million people in the United States and 150,000 new individuals are diagnosed each year.1,2 In 2019, epilepsy-attributable health care spending for noninstitutionalized people was around $5.4 billion and total epilepsy-attributable and epilepsy or seizure health care-related costs totaled $54 billion.3
Accurate surveillance of epilepsy in large health care systems can potentially improve health care delivery and resource allocation. A 2012 Institute of Medicine (IOM) report identified 13 recommendations to guide public health action on epilepsy, including validation of standard definitions for case ascertainment, identification of epilepsy through screening programs or protocols, and expansion of surveillance to better understand disease burden.4
A systematic review of validation studies concluded that it is reasonable to use administrative data to identify people with epilepsy in epidemiologic research. Combining The International Classification of Diseases (ICD) codes for epilepsy (ICD-10, G40-41; ICD-9, 345) with antiseizure medications (ASMs) could provide high positive predictive values (PPVs) and combining symptoms codes for convulsions (ICD-10, R56; ICD-9, 780.3, 780.39) with ASMs could lead to high sensitivity.5 However, identifying individuals with epilepsy from administrative data in large managed health care organizations is challenging.6 The IOM report noted that large managed health care organizations presented varying incidence and prevalence estimates due to differing methodology, geographic area, demographics, and definitions of epilepsy.
The Veterans Health Administration (VHA) is the largest integrated US health care system, providing care to > 9.1 million veterans.7 To improve the health and well-being of veterans with epilepsy (VWEs), a network of sites was established in 2008 called the US Department of Veterans Affairs (VA) Epilepsy Centers of Excellence (ECoE). Subsequent to the creation of the ECoE, efforts were made to identify VWEs within VHA databases.8,9 Prior to fiscal year (FY) 2016, the ECoE adopted a modified version of a well-established epilepsy diagnostic algorithm developed by Holden et al for large managed care organizations.10 The original algorithm identified patients by cross-matching ASMs with ICD-9 codes for an index year. But it failed to capture a considerable number of stable patients with epilepsy in the VHA due to incomplete documentation, and had false positives due to inclusion of patients identified from diagnostic clinics. The modified algorithm the ECoE used prior to FY 2016 considered additional prior years and excluded encounters from diagnostic clinics. The result was an improvement in the sensitivity and specificity of the algorithm. Researchers evaluating 500 patients with epilepsy estimated that the modified algorithm had a PPV of 82.0% (95% CI, 78.6%-85.4%).11
After implementation of ICD-10 codes in the VHA in FY 2016, the task of reliably and efficiently identifying VWE led to a 3-tier algorithm. This article presents a validation of the different tiers of this algorithm after the implementation of ICD-10 diagnosis codes and summarizes the surveillance data collected over the years within the VHA showing the trends of epilepsy.
Methods
The VHA National Neurology office commissioned a Neurology Cube dashboard in FY 2021 in collaboration with VHA Support Service Center (VSSC) for reporting and surveillance of VWEs as a quality improvement initiative. The Neurology Cube uses a 3-tier system for identifying VWE in the VHA databases. VSSC programmers extract data from the VHA Corporate Data Warehouse (CDW) and utilize Microsoft SQL Server and Microsoft Power BI for Neurology Cube reports. The 3-tier system identifies VWE and divides them into distinct groups. The first tier identifies VWE with the highest degree of confidence; Tiers 2 and 3 represent identification with successively lesser degrees of confidence (Figure 1).
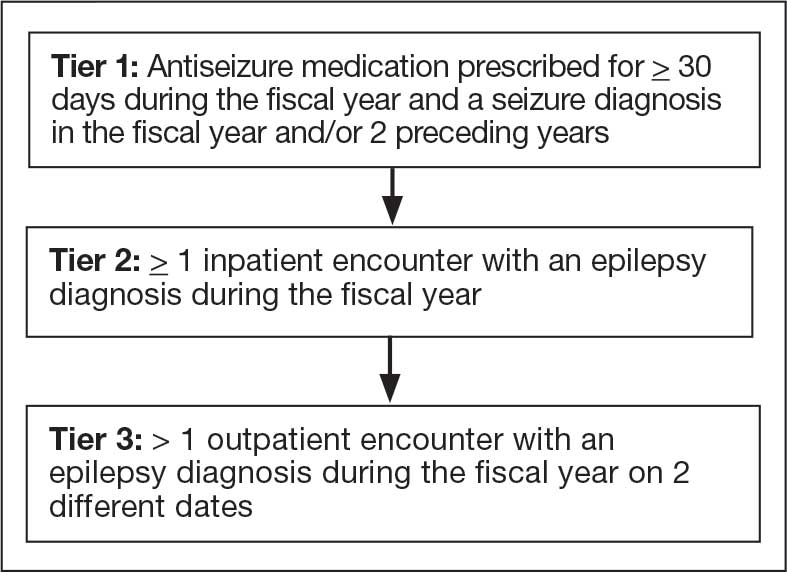
Tier 1
Definition. For a given index year and the preceding 2 years, any of following diagnosis codes on ≥ 1 clinical encounter are considered: 345.xx (epilepsy in ICD-9), 780.3x (other convulsions in ICD-9), G40.xxx (epilepsy in ICD-10), R40.4 (transient alteration of awareness), R56.1 (posttraumatic seizures), or R56.9 (unspecified convulsions). To reduce false positive rates, EEG clinic visits, which may include long-term monitoring, are excluded. Patients identified with ICD codes are then evaluated for an ASM prescription for ≥ 30 days during the index year. ASMs are listed in Appendix 1.
Validation. The development and validation of ICD-9 diagnosis codes crossmatched with an ASM prescription in the VHA has been published elsewhere.11 In FY 2017, after implementation of ICD-10 diagnostic codes, Tier 1 development and validation was performed in 2 phases. Even though Tier 1 study phases were conducted and completed during FY 2017, the patients for Tier 1 were identified from evaluation of FY 2016 data (October 1, 2015, to September 30, 2016). After the pilot analysis, the Tier 1 definition was implemented, and a chart review of 625 randomized patients was conducted at 5 sites for validation. Adequate preliminary data was not available to perform a sample size estimation for this study. Therefore, a practical target of 125 patients was set for Tier 1 from each site to obtain a final sample size of 625 patients. This second phase validated that the crossmatch of ICD-10 diagnosis codes with ASMs had a high PPV for identifying VWE.
Tiers 2 and 3
Definitions. For an index year, Tier 2 includes patients with ≥ 1 inpatient encounter documentation of either ICD-9 345.xx or ICD-10 G40.xxx, excluding EEG clinics. Tier 3 Includes patients who have had ≥ 2 outpatient encounters with diagnosis codes 345.xx or G40.xxx on 2 separate days, excluding EEG clinics. Tiers 2 and 3 do not require ASM prescriptions; this helps to identify VWEs who may be getting their medications outside of VHA or those who have received a new diagnosis.
Validations. Tiers 2 and 3 were included in the epilepsy identification algorithm in FY 2021 after validation was performed on a sample of 8 patients in each tier. Five patients were subsequently identified as having epilepsy in Tier 2 and 6 patients were identified in Tier 3. A more comprehensive validation of Tiers 2 and 3 was performed during FY 2022 that included patients at 5 sites seen during FY 2019 to FY 2022. Since yearly trends showed only about 8% of total patients were identified as having epilepsy through Tiers 2 and 3 we sought ≥ 20 patients per tier for the 5 sites for a total of 200 patients to ensure representation across the VHA. The final count was 126 patients for Tier 2 and 174 patients for Tier 3 (n = 300).
Gold Standard Criteria for Epilepsy Diagnosis
We used the International League Against Epilepsy (ILAE) definition of epilepsy for the validation of the 3 algorithm tiers. ILAE defines epilepsy as ≥ 2 unprovoked (or reflex) seizures occurring > 24 hours apart or 1 unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (≥ 60%) after 2 unprovoked seizures, occurring over the next 10 years.12
A standard protocol was provided to evaluators to identify patients using the VHA Computerized Patient Record System (Appendix 1). After review, evaluators categorized each patient in 1 of 4 ways: (1) Yes, definite: The patient’s health care practitioner (HCP) believes the patient has epilepsy and is treating with medication; (2) Yes, uncertain: The HCP has enough suspicion of epilepsy that a medication is prescribed, but uncertainty is expressed of the diagnosis; (3) No, definite: The HCP does not believe the patient has epilepsy and is therefore not treating with medication for seizure; (4) No, uncertain: The HCP is not treating with medication for epilepsy, because the diagnostic suspicion is not high enough, but there is suspicion for epilepsy.
As a quality improvement operational project, the Epilepsy National Program Office approved this validation project and determined that institutional review board approval was not required.
Statistical Analysis
Counts and percentages were computed for categories of epilepsy status. PPV of each tier was estimated with asymptotic 95% CIs.
Results
ICD-10 codes for 480 patients were evaluated in Tier 1 phase 1; 13.8% were documented with G40.xxx, 27.9% with R56.1, 34.4% with R56.9, and 24.0% with R40.4 (Appendix 2). In total, 68.1% fulfilled the criteria of epilepsy, 19.2% did not, and 12.7% were uncertain). From the validation of Tier 1 phase 2 (n = 625), the PPV of the algorithm for patients presumed to have epilepsy (definite and uncertain) was 85.1% (95% CI, 82.1%-87.8%) (Table).
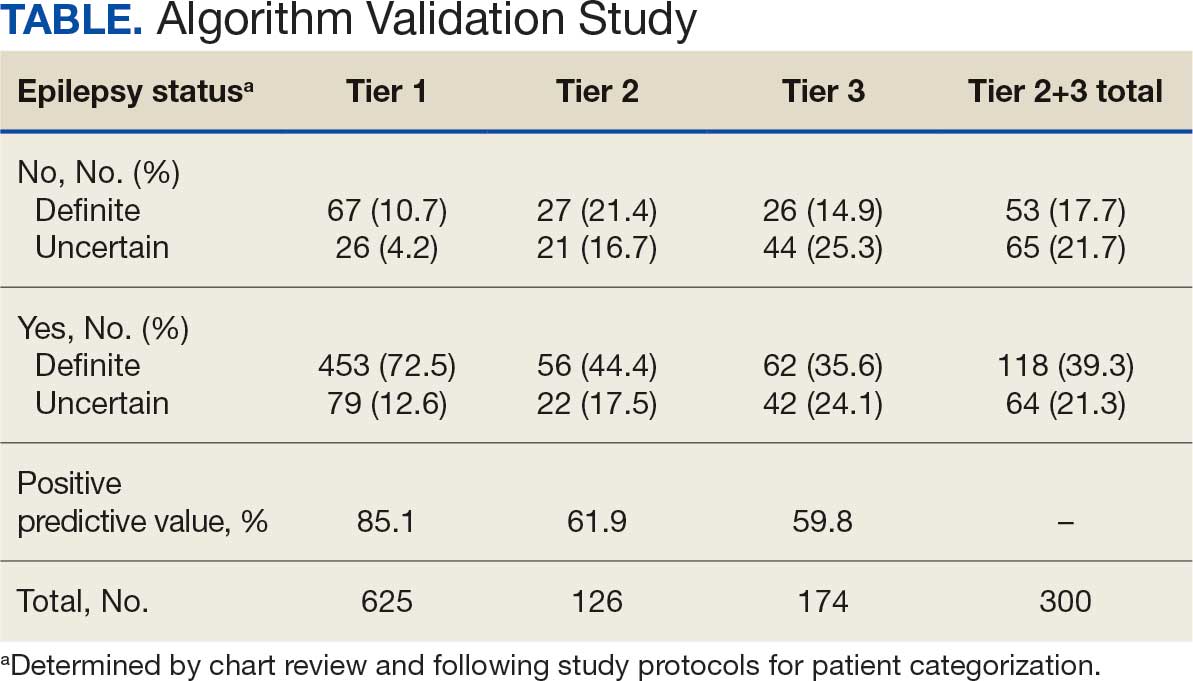
Of 300 patients evaluated, 126 (42.0%) were evaluated for Tier 2 with a PPV of 61.9% (95% CI, 53.4%-70.4%), and 174 (58.0%) patients were evaluated for Tier 3 with a PPV of 59.8% (95% CI, 52.5%-67.1%. The PPV of the algorithm for patients presumed to have epilepsy (definite and uncertain) were combined to calculate the PPV. Estimates of VHA VWE counts were computed for each tier from FY 2014 to FY 2023 using the VSSC Neurology Cube (Figure 2). For all years, > 92% patients were classified using the Tier 1 definition.
Discussion
The development and validation of the 3-tier diagnostic algorithm represents an important advancement in the surveillance and management of epilepsy among veterans within the VHA. The validation of this algorithm also demonstrates its practical utility in a large, integrated health care system.
Specific challenges were encountered when attempting to use pre-existing algorithms; these challenges included differences in the usage patterns of diagnostic codes and the patterns of ASM use within the VHA. These challenges prompted the need for a tailored approach, which led to the development of this algorithm. The inclusion of additional ICD-10 codes led to further revisions and subsequent validation. While many of the basic concepts of the algorithm, including ICD codes and ASMs, could work in other institutions, it would be wise for health care organizations to develop their own algorithms because of certain variables, including organizational size, patient demographics, common comorbidities, and the specific configurations of electronic health records and administrative data systems.
Studies have shown that ICD-10 codes for epilepsy (G40.* and/or R56.9) perform well in identifying epilepsy whether they are assigned by neurologists (sensitivity, 97.7%; specificity, 44.1%; PPV, 96.2%; negative predictive value, 57.7%), or in emergency department or hospital discharges (PPV, 75.5%).13,14 The pilot study of the algorithm’s Tier 1 development (phase 1) evaluated whether the selected ICD-10 diagnostic codes accurately included the VWE population within the VHA and revealed that while most codes (eg, epilepsy [G40.xxx]; posttraumatic seizures [R56.1]; and unspecified convulsions [R56.9]), had a low false positive rate (< 16%), the R40.4 code (transient alteration of awareness) had a higher false positivity of 42%. While this is not surprising given the broad spectrum of conditions that can manifest as transient alteration of awareness, it underscores the inherent challenges in diagnosing epilepsy using diagnosis codes.
In phase 2, the Tier 1 algorithm was validated as effective for identifying VWE in the VHA system, as its PPV was determined to be high (85%). In comparison, Tiers 2 and 3, whose criteria did not require data on VHA prescribed ASM use, had lower tiers of epilepsy predictability (PPV about 60% for both). This was thought to be acceptable because Tiers 2 and 3 represent a smaller population of the identified VWEs (about 8%). These VWEs may otherwise have been missed, partly because veterans are not required to get ASMs from the VHA.
Upon VHA implementation in FY 2021, this diagnostic algorithm exhibited significant clinical utility when integrated within the VSSC Neurology Cube. It facilitated an efficient approach to identifying VWEs using readily available databases. This led to better tracking of real-time epilepsy cases, which facilitated improving current resource allocation and targeted intervention strategies such as identification of drug-resistant epilepsy patients, optimizing strategies for telehealth and patient outreach for awareness of epilepsy care resources within VHA. Meanwhile, data acquired by the algorithm over the decade since its development (FY 2014 to FY 2023) contributed to more accurate epidemiologic information and identification of historic trends. Development of the algorithm represents one of the ways ECoEs have led to improved care for VWEs. ECoEs have been shown to improve health care for veterans in several metrics.15
A strength of this study is the rigorous multitiered validation process to confirm the diagnostic accuracy of ICD-10 codes against the gold standard ILAE definition of epilepsy to identify “definite” epilepsy cases within the VHA. The use of specific ICD codes further enhances the precision of epilepsy diagnoses. The inclusion of ASMs, which are sometimes prescribed for conditions other than epilepsy, could potentially inflate false positive rates.16
This study focused exclusively on the identification and validation of definite epilepsy cases within the VHA VSSC database, employing more stringent diagnostic criteria to ensure the highest level of certainty in ascertaining epilepsy. It is important to note there is a separate category of probable epilepsy, which involves a broader set of diagnostic criteria. While not covered in this study, probable epilepsy would be subject to future research and validation, which could provide insights into a wider spectrum of epilepsy diagnoses. Such future research could help refine the algorithm’s applicability and accuracy and potentially lead to more comprehensive surveillance and management strategies in clinical practice.
This study highlights the inherent challenges in leveraging administrative data for disease identification, particularly for conditions such as epilepsy, where diagnostic clarity can be complex. However, other conditions such as multiple sclerosis have noted similar success with the use of VHA administrative data for categorizing disease.17
Limitations
The algorithm discussed in this article is, in and of itself, generalizable. However, the validation process was unique to the VHA patient population, limiting the generalizability of the findings. Documentation practices and HCP attitudes within the VHA may differ from those in other health care settings. Identifying people with epilepsy can be challenging because of changing definitions of epilepsy over time. In addition to clinical evaluation, EEG and magnetic resonance imaging results, response to ASM treatment, and video-EEG monitoring of habitual events all can help establish the diagnosis. Therefore, studies may vary in how inclusive or exclusive the criteria are. ASMs such as gabapentin, pregabalin, carbamazepine, lamotrigine, topiramate, and valproate are used to treat other conditions, including headaches, generalized pain, and mood disorders. Consequently, including these ASMs in the Tier 1 definition may have increased the false positive rate. Additional research is needed to evaluate whether excluding these ASMs from the algorithm based on specific criteria (eg, dose of ASM used) can further refine the algorithm to identify patients with epilepsy.
Further refinement of this algorithm may also occur as technology changes. Future electronic health records may allow better tracking of different epilepsy factors, the integration of additional diagnostic criteria, and the use of natural language processing or other forms of artificial intelligence.
Conclusions
This study presents a significant step forward in epilepsy surveillance within the VHA. The algorithm offers a robust tool for identifying VWEs with good PPVs, facilitating better resource allocation and targeted care. Despite its limitations, this research lays a foundation for future advancements in the management and understanding of epilepsy within large health care systems. Since this VHA algorithm is based on ASMs and ICD diagnosis codes from patient records, other large managed health care systems also may be able to adapt this algorithm to their data specifications.
- Kobau R, Luncheon C, Greenlund K. Active epilepsy prevalence among U.S. adults is 1.1% and differs by educational level-National Health Interview Survey, United States, 2021. Epilepsy Behav. 2023;142:109180. doi:10.1016/j.yebeh.2023.109180
- GBD 2017 US Neurological Disorders Collaborators, Feigin VL, Vos T, et al. Burden of neurological disorders across the US from 1990-2017: a global burden of disease study. JAMA Neurol. 2021;78:165-176. doi:10.1001/jamaneurol.2020.4152
- Moura LMVR, Karakis I, Zack MM, et al. Drivers of US health care spending for persons with seizures and/or epilepsies, 2010-2018. Epilepsia. 2022;63:2144-2154. doi:10.1111/epi.17305
- Institute of Medicine. Epilepsy Across the Spectrum: Promoting Health and Understanding. The National Academies Press; 2012. Accessed November 11, 2025. www.nap.edu/catalog/13379
- Mbizvo GK, Bennett KH, Schnier C, Simpson CR, Duncan SE, Chin RFM. The accuracy of using administrative healthcare data to identify epilepsy cases: A systematic review of validation studies. Epilepsia. 2020;61:1319-1335. doi:10.1111/epi.16547
- Montouris GD. How will primary care physicians, specialists, and managed care treat epilepsy in the new millennium? Neurology. 2000;55:S42-S44.
- US Department of Veterans Affairs. Veterans Health Administration: About VHA. Accessed November 11, 2025. https://www.va.gov/health/aboutvha.asp
- Veterans’ Mental Health and Other Care Improvements Act of 2008, S 2162, 110th Cong (2008). Accessed November 11, 2025. https://www.congress.gov/bill/110th-congress/senate-bill/2162
- Rehman R, Kelly PR, Husain AM, Tran TT. Characteristics of Veterans diagnosed with seizures within Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762. doi:10.1682/JRRD.2014.10.0241
- Holden EW, Grossman E, Nguyen HT, et al. Developing a computer algorithm to identify epilepsy cases in managed care organizations. Dis Manag. 2005;8:1-14. doi:10.1089/dis.2005.8.1
- Rehman R, Everhart A, Frontera AT, et al. Implementation of an established algorithm and modifications for the identification of epilepsy patients in the Veterans Health Administration. Epilepsy Res. 2016;127:284-290. doi:10.1016/j.eplepsyres.2016.09.012
- Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475-482. doi:10.1111/epi.12550
- Smith JR, Jones FJS, Fureman BE, et al. Accuracy of ICD-10-CM claims-based definitions for epilepsy and seizure type. Epilepsy Res. 2020;166:106414. doi:10.1016/j.eplepsyres.2020.106414
- Jetté N, Reid AY, Quan H, et al. How accurate is ICD coding for epilepsy? Epilepsia. 2010;51:62-69. doi:10.1111/j.1528-1167.2009.02201.x
- Kelly P, Chinta R, Privitera G. Do centers of excellence reduce health care costs? Evidence from the US Veterans Health Administration Centers for Epilepsy. Glob Bus Organ Excell. 2015;34:18-29.
- Haneef Z, Rehman R, Husain AM. Association between standardized mortality ratio and utilization of care in US veterans with drug-resistant epilepsy compared with all US veterans and the US general population. JAMA Neurol. 2022;79:879-887. doi:10.1001/jamaneurol.2022.2290
- Culpepper WJ, Marrie RA, Langer-Gould A, et al. Validation of an algorithm for identifying MS cases in administrative health claims datasets. Neurology. 2019;92:e1016-e1028 doi:10.1212/WNL.0000000000007043
- Kobau R, Luncheon C, Greenlund K. Active epilepsy prevalence among U.S. adults is 1.1% and differs by educational level-National Health Interview Survey, United States, 2021. Epilepsy Behav. 2023;142:109180. doi:10.1016/j.yebeh.2023.109180
- GBD 2017 US Neurological Disorders Collaborators, Feigin VL, Vos T, et al. Burden of neurological disorders across the US from 1990-2017: a global burden of disease study. JAMA Neurol. 2021;78:165-176. doi:10.1001/jamaneurol.2020.4152
- Moura LMVR, Karakis I, Zack MM, et al. Drivers of US health care spending for persons with seizures and/or epilepsies, 2010-2018. Epilepsia. 2022;63:2144-2154. doi:10.1111/epi.17305
- Institute of Medicine. Epilepsy Across the Spectrum: Promoting Health and Understanding. The National Academies Press; 2012. Accessed November 11, 2025. www.nap.edu/catalog/13379
- Mbizvo GK, Bennett KH, Schnier C, Simpson CR, Duncan SE, Chin RFM. The accuracy of using administrative healthcare data to identify epilepsy cases: A systematic review of validation studies. Epilepsia. 2020;61:1319-1335. doi:10.1111/epi.16547
- Montouris GD. How will primary care physicians, specialists, and managed care treat epilepsy in the new millennium? Neurology. 2000;55:S42-S44.
- US Department of Veterans Affairs. Veterans Health Administration: About VHA. Accessed November 11, 2025. https://www.va.gov/health/aboutvha.asp
- Veterans’ Mental Health and Other Care Improvements Act of 2008, S 2162, 110th Cong (2008). Accessed November 11, 2025. https://www.congress.gov/bill/110th-congress/senate-bill/2162
- Rehman R, Kelly PR, Husain AM, Tran TT. Characteristics of Veterans diagnosed with seizures within Veterans Health Administration. J Rehabil Res Dev. 2015;52(7):751-762. doi:10.1682/JRRD.2014.10.0241
- Holden EW, Grossman E, Nguyen HT, et al. Developing a computer algorithm to identify epilepsy cases in managed care organizations. Dis Manag. 2005;8:1-14. doi:10.1089/dis.2005.8.1
- Rehman R, Everhart A, Frontera AT, et al. Implementation of an established algorithm and modifications for the identification of epilepsy patients in the Veterans Health Administration. Epilepsy Res. 2016;127:284-290. doi:10.1016/j.eplepsyres.2016.09.012
- Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475-482. doi:10.1111/epi.12550
- Smith JR, Jones FJS, Fureman BE, et al. Accuracy of ICD-10-CM claims-based definitions for epilepsy and seizure type. Epilepsy Res. 2020;166:106414. doi:10.1016/j.eplepsyres.2020.106414
- Jetté N, Reid AY, Quan H, et al. How accurate is ICD coding for epilepsy? Epilepsia. 2010;51:62-69. doi:10.1111/j.1528-1167.2009.02201.x
- Kelly P, Chinta R, Privitera G. Do centers of excellence reduce health care costs? Evidence from the US Veterans Health Administration Centers for Epilepsy. Glob Bus Organ Excell. 2015;34:18-29.
- Haneef Z, Rehman R, Husain AM. Association between standardized mortality ratio and utilization of care in US veterans with drug-resistant epilepsy compared with all US veterans and the US general population. JAMA Neurol. 2022;79:879-887. doi:10.1001/jamaneurol.2022.2290
- Culpepper WJ, Marrie RA, Langer-Gould A, et al. Validation of an algorithm for identifying MS cases in administrative health claims datasets. Neurology. 2019;92:e1016-e1028 doi:10.1212/WNL.0000000000007043
Development and Validation of an Administrative Algorithm to Identify Veterans With Epilepsy
Development and Validation of an Administrative Algorithm to Identify Veterans With Epilepsy
Higher Epilepsy Mortality in Posttraumatic Cases, VA Study Finds
The risk of death in patients with posttraumatic epilepsy (PTE) varies dramatically by type of brain injury, with some facing twice the mortality rate as those with other forms of epilepsy, according to a new study of Veterans Health Administration data.
Of 210,182 veterans with epilepsy followed for a median of 6 years, those who developed PTE after diffuse cerebral injury, focal cerebral injury, or skull/facial fractures had 16% to 18% higher mortality rates than veterans with nontraumatic epilepsy (NTE) the study found. Published in Neurology, the analysis was completed by Zulfi Haneef, MBBS, MD, of Baylor College of Medicine Medical Center, and colleagues.
Young patients who developed PTE after extracerebral hemorrhage faced the highest risk — double the mortality rate of those with NTE.
“These numbers are striking considering that the group against which these rates are compared — other causes of epilepsy — itself suffers from a high mortality rate,” Haneef said in an interview with Federal Practitioner. “Our findings argue for risk-stratified follow-up in PTE based on the underlying TBI [traumatic brain injury] mechanism and age at epilepsy onset.”
How Common is PTE?
PTE is defined as “long-term predisposition to developing recurrent and unprovoked seizures caused by a traumatic brain injury,” according to neurologist Edilberto Amorim, MD, of University of California at San Francisco Weill Institute for Neurosciences, who was not involved with the study but is familiar with its findings. “We do not fully understand why some people with a traumatic brain injury develop epilepsy and others do not, but the risk is higher with more severe types of TBI.”
PTE accounts for about 5% of all epilepsy cases, Amorim said. The study cites research linking PTE to mortality risk that’s 1.75 to 2.30 higher than in people without epilepsy.
Haneef said the study aimed to shed light on mortality in PTE. “Although epilepsy and TBI are each linked to higher mortality, it had never been conclusively shown that PTE specifically carries higher mortality than nontraumatic epilepsy,” he said. “We set out to answer that question in a large national veterans cohort and to see whether mortality differs by the type of antecedent TBI.”
Methodology and Findings
Researchers tracked 210,182 veterans diagnosed with epilepsy from 2005 to 2022 through the end of 2024: 28,832 with PTE (mean onset age 52.6 years, 7.4% female, 74.2% White, 16.2% Black) and 181,350 with NTE (mean onset age 60.9 years, 8.5% female, 71.0% White, 21.4% Black).
Patients with PTE were defined as having had documentation of TBI within 5 years previous to receiving an epilepsy diagnosis.
Among those with NTE (median follow-up, 6.0 years), 51.1% died. In the PTE group (median follow-up, 6.4 years), 37.3% died.
After adjustment for differences in age, sex, and comorbidities, the risk of mortality in PTE was slightly higher than in NTE (adjusted hazard ratio [aHR], 1.02); the risk was lower for the concussive TBI subtype (aHR, 0.91, both P < .05). “The underlying injury in concussion
is likely to be less severe compared with structural TBI, which may have led to the lower relative mortality observed,” the authors wrote.
However, risk of mortality in PTE was higher than in NTE for cases with underlying TBI subtypes of skull/facial fracture (aHR, 1.18), diffuse cerebral injury (aHR, 1.17), and focal cerebral injury (aHR, 1.16).
“These injuries are associated with greater structural brain damage and sustained neuroinflammation, which are factors linked to harder-to-treat (drug-resistant) epilepsy, which carries higher mortality,” Haneef said. “They may also coexist with extracranial trauma and medical comorbidity that compound long-term risk.”
Among various age groups, there was a notably higher risk of mortality linked to patients aged 18 to 39 years at onset with extracerebral PTE (aHR, 2.02, vs NTE): “In younger patients, extracerebral bleeds (eg, subdural, epidural, and subarachnoid) may reflect higher-energy trauma and more aggressive secondary cascades, amplifying epilepsy severity and longer lifetime exposure to risk. Mechanistic differences in hemorrhage types across ages may also contribute,” Haneef said.
Perspective on Findings
Amorim said the new research is “very useful,” although it has limitations that are common in large database studies. “A key point that this study highlights is the variability in the impact of TBI type on mortality and the differential risk across different age groups,” he said.
As for the higher risk in younger people, Amorim said this may be related to severity of injury: “Older patients often have TBI after falls, while younger patients are more frequently involved in traffic accidents or victims of violence,” he said
In the big picture, Amorim said, “studies like this highlight the importance of moving beyond a one-size-fits-all approach in epilepsy care. Understanding the nuances of posttraumatic epilepsy—how the type of injury, age, and other factors affect outcomes—can help us personalize treatment and counseling and maybe even guide future research into preventing or mitigating epilepsy after brain injury. New methods to automate review of medical records with higher resolution, such as large language models and natural language processing, may make this type of study with large databases even more comprehensive and impactful.”
Haneef said the findings highlight the importance of recognizing PTE as a higher-risk epilepsy and prioritizing early specialty care, especially after focal/diffuse brain injury or fracture. “Screen proactively for drug resistance and fast-track definitive therapies—surgery and device-based therapies—when indicated,” Haneef said. “Management should also include optimized antiseizure therapy, comorbidity control, and safety counseling, since many deaths may be preventable with coordinated multidisciplinary care.”
Haneef added that clinicians should “pay particular attention to younger PTE patients with extracerebral hemorrhage, who showed the greatest relative mortality.”
He also noted that the US Department of Veterans Affairs has comprehensive Epilepsy Centers of Excellence across the country.
The US Department of Defense (DoD) funded the study. Haneef discloses DoD funding, and another author discloses DoD and VA funding. Other authors have no disclosures.
Amorim discloses funding from DoD, NIH, American Heart Association, Regents of the University of California, Cures Within Reach, Zoll Foundation, and Hellman Foundation.
The risk of death in patients with posttraumatic epilepsy (PTE) varies dramatically by type of brain injury, with some facing twice the mortality rate as those with other forms of epilepsy, according to a new study of Veterans Health Administration data.
Of 210,182 veterans with epilepsy followed for a median of 6 years, those who developed PTE after diffuse cerebral injury, focal cerebral injury, or skull/facial fractures had 16% to 18% higher mortality rates than veterans with nontraumatic epilepsy (NTE) the study found. Published in Neurology, the analysis was completed by Zulfi Haneef, MBBS, MD, of Baylor College of Medicine Medical Center, and colleagues.
Young patients who developed PTE after extracerebral hemorrhage faced the highest risk — double the mortality rate of those with NTE.
“These numbers are striking considering that the group against which these rates are compared — other causes of epilepsy — itself suffers from a high mortality rate,” Haneef said in an interview with Federal Practitioner. “Our findings argue for risk-stratified follow-up in PTE based on the underlying TBI [traumatic brain injury] mechanism and age at epilepsy onset.”
How Common is PTE?
PTE is defined as “long-term predisposition to developing recurrent and unprovoked seizures caused by a traumatic brain injury,” according to neurologist Edilberto Amorim, MD, of University of California at San Francisco Weill Institute for Neurosciences, who was not involved with the study but is familiar with its findings. “We do not fully understand why some people with a traumatic brain injury develop epilepsy and others do not, but the risk is higher with more severe types of TBI.”
PTE accounts for about 5% of all epilepsy cases, Amorim said. The study cites research linking PTE to mortality risk that’s 1.75 to 2.30 higher than in people without epilepsy.
Haneef said the study aimed to shed light on mortality in PTE. “Although epilepsy and TBI are each linked to higher mortality, it had never been conclusively shown that PTE specifically carries higher mortality than nontraumatic epilepsy,” he said. “We set out to answer that question in a large national veterans cohort and to see whether mortality differs by the type of antecedent TBI.”
Methodology and Findings
Researchers tracked 210,182 veterans diagnosed with epilepsy from 2005 to 2022 through the end of 2024: 28,832 with PTE (mean onset age 52.6 years, 7.4% female, 74.2% White, 16.2% Black) and 181,350 with NTE (mean onset age 60.9 years, 8.5% female, 71.0% White, 21.4% Black).
Patients with PTE were defined as having had documentation of TBI within 5 years previous to receiving an epilepsy diagnosis.
Among those with NTE (median follow-up, 6.0 years), 51.1% died. In the PTE group (median follow-up, 6.4 years), 37.3% died.
After adjustment for differences in age, sex, and comorbidities, the risk of mortality in PTE was slightly higher than in NTE (adjusted hazard ratio [aHR], 1.02); the risk was lower for the concussive TBI subtype (aHR, 0.91, both P < .05). “The underlying injury in concussion
is likely to be less severe compared with structural TBI, which may have led to the lower relative mortality observed,” the authors wrote.
However, risk of mortality in PTE was higher than in NTE for cases with underlying TBI subtypes of skull/facial fracture (aHR, 1.18), diffuse cerebral injury (aHR, 1.17), and focal cerebral injury (aHR, 1.16).
“These injuries are associated with greater structural brain damage and sustained neuroinflammation, which are factors linked to harder-to-treat (drug-resistant) epilepsy, which carries higher mortality,” Haneef said. “They may also coexist with extracranial trauma and medical comorbidity that compound long-term risk.”
Among various age groups, there was a notably higher risk of mortality linked to patients aged 18 to 39 years at onset with extracerebral PTE (aHR, 2.02, vs NTE): “In younger patients, extracerebral bleeds (eg, subdural, epidural, and subarachnoid) may reflect higher-energy trauma and more aggressive secondary cascades, amplifying epilepsy severity and longer lifetime exposure to risk. Mechanistic differences in hemorrhage types across ages may also contribute,” Haneef said.
Perspective on Findings
Amorim said the new research is “very useful,” although it has limitations that are common in large database studies. “A key point that this study highlights is the variability in the impact of TBI type on mortality and the differential risk across different age groups,” he said.
As for the higher risk in younger people, Amorim said this may be related to severity of injury: “Older patients often have TBI after falls, while younger patients are more frequently involved in traffic accidents or victims of violence,” he said
In the big picture, Amorim said, “studies like this highlight the importance of moving beyond a one-size-fits-all approach in epilepsy care. Understanding the nuances of posttraumatic epilepsy—how the type of injury, age, and other factors affect outcomes—can help us personalize treatment and counseling and maybe even guide future research into preventing or mitigating epilepsy after brain injury. New methods to automate review of medical records with higher resolution, such as large language models and natural language processing, may make this type of study with large databases even more comprehensive and impactful.”
Haneef said the findings highlight the importance of recognizing PTE as a higher-risk epilepsy and prioritizing early specialty care, especially after focal/diffuse brain injury or fracture. “Screen proactively for drug resistance and fast-track definitive therapies—surgery and device-based therapies—when indicated,” Haneef said. “Management should also include optimized antiseizure therapy, comorbidity control, and safety counseling, since many deaths may be preventable with coordinated multidisciplinary care.”
Haneef added that clinicians should “pay particular attention to younger PTE patients with extracerebral hemorrhage, who showed the greatest relative mortality.”
He also noted that the US Department of Veterans Affairs has comprehensive Epilepsy Centers of Excellence across the country.
The US Department of Defense (DoD) funded the study. Haneef discloses DoD funding, and another author discloses DoD and VA funding. Other authors have no disclosures.
Amorim discloses funding from DoD, NIH, American Heart Association, Regents of the University of California, Cures Within Reach, Zoll Foundation, and Hellman Foundation.
The risk of death in patients with posttraumatic epilepsy (PTE) varies dramatically by type of brain injury, with some facing twice the mortality rate as those with other forms of epilepsy, according to a new study of Veterans Health Administration data.
Of 210,182 veterans with epilepsy followed for a median of 6 years, those who developed PTE after diffuse cerebral injury, focal cerebral injury, or skull/facial fractures had 16% to 18% higher mortality rates than veterans with nontraumatic epilepsy (NTE) the study found. Published in Neurology, the analysis was completed by Zulfi Haneef, MBBS, MD, of Baylor College of Medicine Medical Center, and colleagues.
Young patients who developed PTE after extracerebral hemorrhage faced the highest risk — double the mortality rate of those with NTE.
“These numbers are striking considering that the group against which these rates are compared — other causes of epilepsy — itself suffers from a high mortality rate,” Haneef said in an interview with Federal Practitioner. “Our findings argue for risk-stratified follow-up in PTE based on the underlying TBI [traumatic brain injury] mechanism and age at epilepsy onset.”
How Common is PTE?
PTE is defined as “long-term predisposition to developing recurrent and unprovoked seizures caused by a traumatic brain injury,” according to neurologist Edilberto Amorim, MD, of University of California at San Francisco Weill Institute for Neurosciences, who was not involved with the study but is familiar with its findings. “We do not fully understand why some people with a traumatic brain injury develop epilepsy and others do not, but the risk is higher with more severe types of TBI.”
PTE accounts for about 5% of all epilepsy cases, Amorim said. The study cites research linking PTE to mortality risk that’s 1.75 to 2.30 higher than in people without epilepsy.
Haneef said the study aimed to shed light on mortality in PTE. “Although epilepsy and TBI are each linked to higher mortality, it had never been conclusively shown that PTE specifically carries higher mortality than nontraumatic epilepsy,” he said. “We set out to answer that question in a large national veterans cohort and to see whether mortality differs by the type of antecedent TBI.”
Methodology and Findings
Researchers tracked 210,182 veterans diagnosed with epilepsy from 2005 to 2022 through the end of 2024: 28,832 with PTE (mean onset age 52.6 years, 7.4% female, 74.2% White, 16.2% Black) and 181,350 with NTE (mean onset age 60.9 years, 8.5% female, 71.0% White, 21.4% Black).
Patients with PTE were defined as having had documentation of TBI within 5 years previous to receiving an epilepsy diagnosis.
Among those with NTE (median follow-up, 6.0 years), 51.1% died. In the PTE group (median follow-up, 6.4 years), 37.3% died.
After adjustment for differences in age, sex, and comorbidities, the risk of mortality in PTE was slightly higher than in NTE (adjusted hazard ratio [aHR], 1.02); the risk was lower for the concussive TBI subtype (aHR, 0.91, both P < .05). “The underlying injury in concussion
is likely to be less severe compared with structural TBI, which may have led to the lower relative mortality observed,” the authors wrote.
However, risk of mortality in PTE was higher than in NTE for cases with underlying TBI subtypes of skull/facial fracture (aHR, 1.18), diffuse cerebral injury (aHR, 1.17), and focal cerebral injury (aHR, 1.16).
“These injuries are associated with greater structural brain damage and sustained neuroinflammation, which are factors linked to harder-to-treat (drug-resistant) epilepsy, which carries higher mortality,” Haneef said. “They may also coexist with extracranial trauma and medical comorbidity that compound long-term risk.”
Among various age groups, there was a notably higher risk of mortality linked to patients aged 18 to 39 years at onset with extracerebral PTE (aHR, 2.02, vs NTE): “In younger patients, extracerebral bleeds (eg, subdural, epidural, and subarachnoid) may reflect higher-energy trauma and more aggressive secondary cascades, amplifying epilepsy severity and longer lifetime exposure to risk. Mechanistic differences in hemorrhage types across ages may also contribute,” Haneef said.
Perspective on Findings
Amorim said the new research is “very useful,” although it has limitations that are common in large database studies. “A key point that this study highlights is the variability in the impact of TBI type on mortality and the differential risk across different age groups,” he said.
As for the higher risk in younger people, Amorim said this may be related to severity of injury: “Older patients often have TBI after falls, while younger patients are more frequently involved in traffic accidents or victims of violence,” he said
In the big picture, Amorim said, “studies like this highlight the importance of moving beyond a one-size-fits-all approach in epilepsy care. Understanding the nuances of posttraumatic epilepsy—how the type of injury, age, and other factors affect outcomes—can help us personalize treatment and counseling and maybe even guide future research into preventing or mitigating epilepsy after brain injury. New methods to automate review of medical records with higher resolution, such as large language models and natural language processing, may make this type of study with large databases even more comprehensive and impactful.”
Haneef said the findings highlight the importance of recognizing PTE as a higher-risk epilepsy and prioritizing early specialty care, especially after focal/diffuse brain injury or fracture. “Screen proactively for drug resistance and fast-track definitive therapies—surgery and device-based therapies—when indicated,” Haneef said. “Management should also include optimized antiseizure therapy, comorbidity control, and safety counseling, since many deaths may be preventable with coordinated multidisciplinary care.”
Haneef added that clinicians should “pay particular attention to younger PTE patients with extracerebral hemorrhage, who showed the greatest relative mortality.”
He also noted that the US Department of Veterans Affairs has comprehensive Epilepsy Centers of Excellence across the country.
The US Department of Defense (DoD) funded the study. Haneef discloses DoD funding, and another author discloses DoD and VA funding. Other authors have no disclosures.
Amorim discloses funding from DoD, NIH, American Heart Association, Regents of the University of California, Cures Within Reach, Zoll Foundation, and Hellman Foundation.
Can Sea Lions Expand Our Knowledge of Epilepsy?
In 2022, the Journal of Neurosurgery took the unusual step of publishing a case report of a nonhuman subject, in this case an 8-year-old male sea lion named Cronutt, who had severe epilepsy that in many ways mirrored the common form seen in humans.
A 2020 xenotransplantation of interneuron progenitor cells in the sea lion’s hippocampus may have cured him. “He’s doing fantastic,” said Scott Baraban, PhD, a professor of neurological surgery at the University of California San Francisco Weill Institute for Neurosciences. The procedure offered a confirmation of success stories in mice and could serve as a bridge to human studies, although the science remains murky.
Cronutt’s story began the first time he was found stranded along the California coast in San Luis Obispo County, in November 2017, lethargic and disoriented. Nevertheless, he improved quickly under the care of the Marine Mammal Rescue Center in Sausalito, California, and they released him back into the wild 2 weeks later. Unfortunately, his troubles weren’t over. In the next 2 months, he came to the attention of the rehabilitation center two more times, and the resulting habituation to humans meant that he could not be re-released to the wild.
Things only got worse from there. He experienced a convulsive seizure and loss of consciousness in early 2018 and another seizure a year later. Despite anti-seizure medication, the episodes continued, and eventually, he stopped eating for long periods and lost a quarter of his body weight. It looked like euthanasia was the only alternative.
Neurosurgeons Take Notice
Baraban has devoted his career to animal models of epilepsy, focusing mainly on mice. He developed a method to transplant GABAergic interneurons from pigs, which can pick up the inhibitory role of endogenous neurons. In epileptic mice, mouse-derived progenitor cells mature into inhibitory synapses and dampen seizures, and even reverse behavioral problems.
Baraban was intrigued by the potential of the procedure to help sea lions and potentially bridge the gap between murine and human studies, and he was eager to try the approach after he learned of Cronutt’s case through his colleague Paul Buckmaster at Stanford University, California, who had collaborated with the Marine Mammal Rescue Center to demonstrate that sea lions suffer hippocampal damage that is very similar to human temporal lobe epilepsy.
It turns out that surgery on a sea lion is more complicated than on a mouse. The surgeon needs to conduct an MRI scan to locate the lesion and guide the placement of transplanted cells, and the big animals need to be sedated and intubated. Their caretakers are not enthusiastic about invasive procedures, but Cronutt had already been imaged as part of an earlier study of the effects of exposure to domoic acid on the sea lion brain, giving neurosurgeons at UCSF the information they needed.
In 2020, they transplanted GABAergic interneurons into Cronutt’s hippocampus in a last-ditch effort to save his life. He improved rapidly, and his caregivers eventually tapered off his anti-seizure medications. Today, Cronutt is living seizure-free at the Six Flags Discovery Kingdom in Vallejo, California. He even began participating in shows at Six Flags. “He is able to learn things and do things cognitively that he couldn’t do before,” said Baraban.
The researchers have not followed up with more imaging. “We just haven’t had any reason to bother him. It’s very invasive to get him to an MRI center,” said Baraban.
There haven’t been any more procedures on sea lions, in part because sea lions at rescue centers must be returned to the wild within 6-8 months, and animals with pig-based progenitor cells can’t be released. Any sea lion that would undergo such a procedure would have to live permanently in captivity, potentially for 20-30 years. “It’s a huge undertaking and expense,” said Baraban. There are also logistical challenges with the need to have MRI and other facilities close at hand to where the sea lion is kept.
Human Connections
As a veterinarian interested in human epilepsy, Buckmaster sought to find additional animal models for human temporal lobe epilepsy. He later met a veterinarian who worked with the Marine Mammal Center, who told him about temporal lobe epilepsy in sea lions.
Cronutt was just one of hundreds of California sea lions and other mammals rendered helpless by epileptic seizures induced by exposure to domoic acid, a chemical released by toxic algal blooms. Sea otters, whales, and even birds can likewise be affected. Humans, too, though it is rare: A domoic acid poisoning event in mussels from Prince Edward Island led to convulsions and an eventual diagnosis of temporal lobe epilepsy in an 84-year-old Canadian man, and three others died.
Most of Buckmaster’s work had been done in rats, but seizures are different than what are seen in humans. The damage isn’t unilateral, as in human epilepsy. The damage is unilateral in sea lions, and they suffer damage to similar neurons to those injured in humans. “In rats, you don’t see much loss of granule cells, which are the main neuron in the dentate gyrus, a region that’s really affected in temporal lobe epilepsy. In people, there’s a lot of variation, but [on average] you lose about half your granule cells, and that’s similar to sea lions. In rats, they just don’t lose them,” said Buckmaster.
That makes sea lions a useful model, but they hardly crack the case of human epilepsy. “To be humble about it, we don’t really know what’s causing the seizures. We have an idea of what region of the brain the seizures are coming from, but in terms of the cellular mechanisms, it’s still not clear,” said Buckmaster.
He also noted that, unlike sea lions, the vast majority of patients with human epilepsy have no exposure to domoic acid. That said, the case of sea lions and other marine animals makes researchers wonder. “This is speculative, but a lot of people with temporal epilepsy will have a history of some kind of precipitating event. Typically, it’s earlier in life, and a common one is prolonged febrile seizures. That could be a link to the domoic acid exposure in sea lions because the domoic acid exposure in sea lions frequently causes prolonged seizures. If the seizures are severe enough and long enough, they cause permanent brain damage, and that can cause temporal lobe epilepsy. That’s what we strongly believe is causing the temporal lobe epilepsy in sea lions. Prolonged, severe seizures can be caused by many things other than domoic acid, and that could be what causes it in many cases of human temporal lobe epilepsy,” said Buckmaster.
The approach taken with Cronutt makes sense to Buckmaster, who was not directly involved in the procedure. “The ideal treatment would be something that you would administer once, and it would cause cessation of seizures without any side effects. The transplantation of inhibitory cells is a treatment that would last and hopefully wouldn’t have any side effects and hopefully would provide complete control of seizures. It’s unlikely to reach all those goals, but it’s a step in the right direction, hopefully,” said Buckmaster.
He noted that Cronutt is only a single case and not proof that the procedure will work more generally. It’s possible the sea lion would have improved on his own without treatment, and the procedure itself could have influenced the brain. “That’s been the case with other neurological conditions that have attempted to be treated with cell transplantation,” said Buckmaster.
A phase 1/2 clinical trial, sponsored by Neurona Therapeutics, is currently recruiting patients to test transplant of human interneurons created from pluripotent stem cells into both temporal lobes of patients with drug-resistant bilateral mesial temporal lobe epilepsy.
Cronutt’s Course
Although he has improved dramatically, it’s possible that Cronutt continues to experience nonconvulsive seizures, which would not be easy to detect in an animal. “You don’t know if Cronutt’s seizures are controlled or not unless you can look at the electrical activity in Cronutt’s brain, and to my knowledge that has not been done,” said Buckmaster.
Previous studies in rats did repeatedly demonstrate the potential of the treatment approach. Despite the feel-good story of Cronutt, “that’s probably the most compelling evidence in support of that arm of treatment,” said Buckmaster.
Buckmaster and Barbaran had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
In 2022, the Journal of Neurosurgery took the unusual step of publishing a case report of a nonhuman subject, in this case an 8-year-old male sea lion named Cronutt, who had severe epilepsy that in many ways mirrored the common form seen in humans.
A 2020 xenotransplantation of interneuron progenitor cells in the sea lion’s hippocampus may have cured him. “He’s doing fantastic,” said Scott Baraban, PhD, a professor of neurological surgery at the University of California San Francisco Weill Institute for Neurosciences. The procedure offered a confirmation of success stories in mice and could serve as a bridge to human studies, although the science remains murky.
Cronutt’s story began the first time he was found stranded along the California coast in San Luis Obispo County, in November 2017, lethargic and disoriented. Nevertheless, he improved quickly under the care of the Marine Mammal Rescue Center in Sausalito, California, and they released him back into the wild 2 weeks later. Unfortunately, his troubles weren’t over. In the next 2 months, he came to the attention of the rehabilitation center two more times, and the resulting habituation to humans meant that he could not be re-released to the wild.
Things only got worse from there. He experienced a convulsive seizure and loss of consciousness in early 2018 and another seizure a year later. Despite anti-seizure medication, the episodes continued, and eventually, he stopped eating for long periods and lost a quarter of his body weight. It looked like euthanasia was the only alternative.
Neurosurgeons Take Notice
Baraban has devoted his career to animal models of epilepsy, focusing mainly on mice. He developed a method to transplant GABAergic interneurons from pigs, which can pick up the inhibitory role of endogenous neurons. In epileptic mice, mouse-derived progenitor cells mature into inhibitory synapses and dampen seizures, and even reverse behavioral problems.
Baraban was intrigued by the potential of the procedure to help sea lions and potentially bridge the gap between murine and human studies, and he was eager to try the approach after he learned of Cronutt’s case through his colleague Paul Buckmaster at Stanford University, California, who had collaborated with the Marine Mammal Rescue Center to demonstrate that sea lions suffer hippocampal damage that is very similar to human temporal lobe epilepsy.
It turns out that surgery on a sea lion is more complicated than on a mouse. The surgeon needs to conduct an MRI scan to locate the lesion and guide the placement of transplanted cells, and the big animals need to be sedated and intubated. Their caretakers are not enthusiastic about invasive procedures, but Cronutt had already been imaged as part of an earlier study of the effects of exposure to domoic acid on the sea lion brain, giving neurosurgeons at UCSF the information they needed.
In 2020, they transplanted GABAergic interneurons into Cronutt’s hippocampus in a last-ditch effort to save his life. He improved rapidly, and his caregivers eventually tapered off his anti-seizure medications. Today, Cronutt is living seizure-free at the Six Flags Discovery Kingdom in Vallejo, California. He even began participating in shows at Six Flags. “He is able to learn things and do things cognitively that he couldn’t do before,” said Baraban.
The researchers have not followed up with more imaging. “We just haven’t had any reason to bother him. It’s very invasive to get him to an MRI center,” said Baraban.
There haven’t been any more procedures on sea lions, in part because sea lions at rescue centers must be returned to the wild within 6-8 months, and animals with pig-based progenitor cells can’t be released. Any sea lion that would undergo such a procedure would have to live permanently in captivity, potentially for 20-30 years. “It’s a huge undertaking and expense,” said Baraban. There are also logistical challenges with the need to have MRI and other facilities close at hand to where the sea lion is kept.
Human Connections
As a veterinarian interested in human epilepsy, Buckmaster sought to find additional animal models for human temporal lobe epilepsy. He later met a veterinarian who worked with the Marine Mammal Center, who told him about temporal lobe epilepsy in sea lions.
Cronutt was just one of hundreds of California sea lions and other mammals rendered helpless by epileptic seizures induced by exposure to domoic acid, a chemical released by toxic algal blooms. Sea otters, whales, and even birds can likewise be affected. Humans, too, though it is rare: A domoic acid poisoning event in mussels from Prince Edward Island led to convulsions and an eventual diagnosis of temporal lobe epilepsy in an 84-year-old Canadian man, and three others died.
Most of Buckmaster’s work had been done in rats, but seizures are different than what are seen in humans. The damage isn’t unilateral, as in human epilepsy. The damage is unilateral in sea lions, and they suffer damage to similar neurons to those injured in humans. “In rats, you don’t see much loss of granule cells, which are the main neuron in the dentate gyrus, a region that’s really affected in temporal lobe epilepsy. In people, there’s a lot of variation, but [on average] you lose about half your granule cells, and that’s similar to sea lions. In rats, they just don’t lose them,” said Buckmaster.
That makes sea lions a useful model, but they hardly crack the case of human epilepsy. “To be humble about it, we don’t really know what’s causing the seizures. We have an idea of what region of the brain the seizures are coming from, but in terms of the cellular mechanisms, it’s still not clear,” said Buckmaster.
He also noted that, unlike sea lions, the vast majority of patients with human epilepsy have no exposure to domoic acid. That said, the case of sea lions and other marine animals makes researchers wonder. “This is speculative, but a lot of people with temporal epilepsy will have a history of some kind of precipitating event. Typically, it’s earlier in life, and a common one is prolonged febrile seizures. That could be a link to the domoic acid exposure in sea lions because the domoic acid exposure in sea lions frequently causes prolonged seizures. If the seizures are severe enough and long enough, they cause permanent brain damage, and that can cause temporal lobe epilepsy. That’s what we strongly believe is causing the temporal lobe epilepsy in sea lions. Prolonged, severe seizures can be caused by many things other than domoic acid, and that could be what causes it in many cases of human temporal lobe epilepsy,” said Buckmaster.
The approach taken with Cronutt makes sense to Buckmaster, who was not directly involved in the procedure. “The ideal treatment would be something that you would administer once, and it would cause cessation of seizures without any side effects. The transplantation of inhibitory cells is a treatment that would last and hopefully wouldn’t have any side effects and hopefully would provide complete control of seizures. It’s unlikely to reach all those goals, but it’s a step in the right direction, hopefully,” said Buckmaster.
He noted that Cronutt is only a single case and not proof that the procedure will work more generally. It’s possible the sea lion would have improved on his own without treatment, and the procedure itself could have influenced the brain. “That’s been the case with other neurological conditions that have attempted to be treated with cell transplantation,” said Buckmaster.
A phase 1/2 clinical trial, sponsored by Neurona Therapeutics, is currently recruiting patients to test transplant of human interneurons created from pluripotent stem cells into both temporal lobes of patients with drug-resistant bilateral mesial temporal lobe epilepsy.
Cronutt’s Course
Although he has improved dramatically, it’s possible that Cronutt continues to experience nonconvulsive seizures, which would not be easy to detect in an animal. “You don’t know if Cronutt’s seizures are controlled or not unless you can look at the electrical activity in Cronutt’s brain, and to my knowledge that has not been done,” said Buckmaster.
Previous studies in rats did repeatedly demonstrate the potential of the treatment approach. Despite the feel-good story of Cronutt, “that’s probably the most compelling evidence in support of that arm of treatment,” said Buckmaster.
Buckmaster and Barbaran had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
In 2022, the Journal of Neurosurgery took the unusual step of publishing a case report of a nonhuman subject, in this case an 8-year-old male sea lion named Cronutt, who had severe epilepsy that in many ways mirrored the common form seen in humans.
A 2020 xenotransplantation of interneuron progenitor cells in the sea lion’s hippocampus may have cured him. “He’s doing fantastic,” said Scott Baraban, PhD, a professor of neurological surgery at the University of California San Francisco Weill Institute for Neurosciences. The procedure offered a confirmation of success stories in mice and could serve as a bridge to human studies, although the science remains murky.
Cronutt’s story began the first time he was found stranded along the California coast in San Luis Obispo County, in November 2017, lethargic and disoriented. Nevertheless, he improved quickly under the care of the Marine Mammal Rescue Center in Sausalito, California, and they released him back into the wild 2 weeks later. Unfortunately, his troubles weren’t over. In the next 2 months, he came to the attention of the rehabilitation center two more times, and the resulting habituation to humans meant that he could not be re-released to the wild.
Things only got worse from there. He experienced a convulsive seizure and loss of consciousness in early 2018 and another seizure a year later. Despite anti-seizure medication, the episodes continued, and eventually, he stopped eating for long periods and lost a quarter of his body weight. It looked like euthanasia was the only alternative.
Neurosurgeons Take Notice
Baraban has devoted his career to animal models of epilepsy, focusing mainly on mice. He developed a method to transplant GABAergic interneurons from pigs, which can pick up the inhibitory role of endogenous neurons. In epileptic mice, mouse-derived progenitor cells mature into inhibitory synapses and dampen seizures, and even reverse behavioral problems.
Baraban was intrigued by the potential of the procedure to help sea lions and potentially bridge the gap between murine and human studies, and he was eager to try the approach after he learned of Cronutt’s case through his colleague Paul Buckmaster at Stanford University, California, who had collaborated with the Marine Mammal Rescue Center to demonstrate that sea lions suffer hippocampal damage that is very similar to human temporal lobe epilepsy.
It turns out that surgery on a sea lion is more complicated than on a mouse. The surgeon needs to conduct an MRI scan to locate the lesion and guide the placement of transplanted cells, and the big animals need to be sedated and intubated. Their caretakers are not enthusiastic about invasive procedures, but Cronutt had already been imaged as part of an earlier study of the effects of exposure to domoic acid on the sea lion brain, giving neurosurgeons at UCSF the information they needed.
In 2020, they transplanted GABAergic interneurons into Cronutt’s hippocampus in a last-ditch effort to save his life. He improved rapidly, and his caregivers eventually tapered off his anti-seizure medications. Today, Cronutt is living seizure-free at the Six Flags Discovery Kingdom in Vallejo, California. He even began participating in shows at Six Flags. “He is able to learn things and do things cognitively that he couldn’t do before,” said Baraban.
The researchers have not followed up with more imaging. “We just haven’t had any reason to bother him. It’s very invasive to get him to an MRI center,” said Baraban.
There haven’t been any more procedures on sea lions, in part because sea lions at rescue centers must be returned to the wild within 6-8 months, and animals with pig-based progenitor cells can’t be released. Any sea lion that would undergo such a procedure would have to live permanently in captivity, potentially for 20-30 years. “It’s a huge undertaking and expense,” said Baraban. There are also logistical challenges with the need to have MRI and other facilities close at hand to where the sea lion is kept.
Human Connections
As a veterinarian interested in human epilepsy, Buckmaster sought to find additional animal models for human temporal lobe epilepsy. He later met a veterinarian who worked with the Marine Mammal Center, who told him about temporal lobe epilepsy in sea lions.
Cronutt was just one of hundreds of California sea lions and other mammals rendered helpless by epileptic seizures induced by exposure to domoic acid, a chemical released by toxic algal blooms. Sea otters, whales, and even birds can likewise be affected. Humans, too, though it is rare: A domoic acid poisoning event in mussels from Prince Edward Island led to convulsions and an eventual diagnosis of temporal lobe epilepsy in an 84-year-old Canadian man, and three others died.
Most of Buckmaster’s work had been done in rats, but seizures are different than what are seen in humans. The damage isn’t unilateral, as in human epilepsy. The damage is unilateral in sea lions, and they suffer damage to similar neurons to those injured in humans. “In rats, you don’t see much loss of granule cells, which are the main neuron in the dentate gyrus, a region that’s really affected in temporal lobe epilepsy. In people, there’s a lot of variation, but [on average] you lose about half your granule cells, and that’s similar to sea lions. In rats, they just don’t lose them,” said Buckmaster.
That makes sea lions a useful model, but they hardly crack the case of human epilepsy. “To be humble about it, we don’t really know what’s causing the seizures. We have an idea of what region of the brain the seizures are coming from, but in terms of the cellular mechanisms, it’s still not clear,” said Buckmaster.
He also noted that, unlike sea lions, the vast majority of patients with human epilepsy have no exposure to domoic acid. That said, the case of sea lions and other marine animals makes researchers wonder. “This is speculative, but a lot of people with temporal epilepsy will have a history of some kind of precipitating event. Typically, it’s earlier in life, and a common one is prolonged febrile seizures. That could be a link to the domoic acid exposure in sea lions because the domoic acid exposure in sea lions frequently causes prolonged seizures. If the seizures are severe enough and long enough, they cause permanent brain damage, and that can cause temporal lobe epilepsy. That’s what we strongly believe is causing the temporal lobe epilepsy in sea lions. Prolonged, severe seizures can be caused by many things other than domoic acid, and that could be what causes it in many cases of human temporal lobe epilepsy,” said Buckmaster.
The approach taken with Cronutt makes sense to Buckmaster, who was not directly involved in the procedure. “The ideal treatment would be something that you would administer once, and it would cause cessation of seizures without any side effects. The transplantation of inhibitory cells is a treatment that would last and hopefully wouldn’t have any side effects and hopefully would provide complete control of seizures. It’s unlikely to reach all those goals, but it’s a step in the right direction, hopefully,” said Buckmaster.
He noted that Cronutt is only a single case and not proof that the procedure will work more generally. It’s possible the sea lion would have improved on his own without treatment, and the procedure itself could have influenced the brain. “That’s been the case with other neurological conditions that have attempted to be treated with cell transplantation,” said Buckmaster.
A phase 1/2 clinical trial, sponsored by Neurona Therapeutics, is currently recruiting patients to test transplant of human interneurons created from pluripotent stem cells into both temporal lobes of patients with drug-resistant bilateral mesial temporal lobe epilepsy.
Cronutt’s Course
Although he has improved dramatically, it’s possible that Cronutt continues to experience nonconvulsive seizures, which would not be easy to detect in an animal. “You don’t know if Cronutt’s seizures are controlled or not unless you can look at the electrical activity in Cronutt’s brain, and to my knowledge that has not been done,” said Buckmaster.
Previous studies in rats did repeatedly demonstrate the potential of the treatment approach. Despite the feel-good story of Cronutt, “that’s probably the most compelling evidence in support of that arm of treatment,” said Buckmaster.
Buckmaster and Barbaran had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Gestational Eclampsia Linked to Fivefold Epilepsy Risk
Gestational hypertension, preeclampsia, or eclampsia is associated with a significantly higher risk for neurologic disorders such as migraine or epilepsy in the years following a first pregnancy, new research suggests.
The risk was highest in those with gestational eclampsia, who had a 70% increased chance of developing a neurologic disorder, including a fivefold increased risk for epilepsy, investigators found.
“When consulting women with new-onset neurological disorders, it’s important to inquire about their pregnancy history, as pregnancy complications such as gestational hypertension, preeclampsia, and eclampsia have been associated with an increased risk of neurological disorders later in life.” Therese Friis, MD, PhD student, Department of Women’s and Children’s Health, Uppsala University in Sweden, said in an interview.
The findings were published online in JAMA Neurology.
Most studies of maternal outcomes after gestational hypertension, preeclampsia, or eclampsia have focused on long-term risks for cardiovascular disease or neurologic complications such as stroke, dementia, and cognitive impairment. And many of these studies were relatively small and based on interviews or questionnaires.
“We wanted to investigate whether women with a hypertensive disorder of pregnancy also had a risk of other neurological complications, closer in time to the pregnancy,” said Friis.
The new study included 648,385 women (mean age, 28.5 years) whose first pregnancy occurred between 2005 and 2018. Of these, 94% had a normotensive pregnancy, 2% had gestational hypertension, 4% had preeclampsia without eclampsia, and 0.1% had eclampsia.
Gestational hypertension was defined as new-onset systolic blood pressure of ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg; preeclampsia was defined as gestational hypertension accompanied by proteinuria; and eclampsia was defined as tonic-clonic seizures without other etiology accompanied by preeclampsia.
Researchers used linked Swedish national registries that collect data on pregnancies, births, and infant and maternal characteristics. Among other things, they controlled for maternal age, early pregnancy body mass index, education level, and pregestational and gestational diabetes.
The primary outcome was a composite of five new-onset neurologic diagnoses: Migraine, headache, epilepsy, sleep disorder, and mental fatigue (neurasthenia), although one diagnosis was sufficient, from 42 days to 15 years after childbirth. Mean follow-up was 7.7 years.
Fivefold Epilepsy Risk
Compared with normotensive pregnancies, the risk for the primary outcome was 70% greater in those with eclampsia (adjusted hazard ratio [aHR], 1.70; 95% CI, 1.16-2.50), 27% higher for gestational hypertension (aHR, 1.27; 95% CI, 1.12-1.45), and 32% for preeclampsia (aHR, 1.32; 95% CI, 1.22-1.42).
Researchers also looked at the risk for individual neurologic disorders. There were too few neurasthenia events to generate meaningful results, so this diagnosis was omitted from the analysis.
Here, the study found women with eclampsia had five times the risk for epilepsy (aHR, 5.31; 95% CI, 2.85-9.89) compared with women with normotensive pregnancies.
The underlying mechanism for this association is unclear. However, said Friis, eclampsia and epilepsy share common pathways, such as neuroinflammation, and women with epilepsy before pregnancy run an increased risk for eclampsia.
“So common underlying pathways might increase the risk both for eclampsia in cases of a seizure disorder and a future seizure disorder after eclampsia,” she said.
In addition, preeclampsia and, in particular, eclampsia can cause irreversible subclinical cerebral infarcts found in areas of cerebral edema, she added. “These infarcts or scarring of brain tissue could potentially serve as foci for later epileptic activity.”
Researchers separated women with preeclampsia (with or without eclampsia) into those with preterm (less than 37 weeks; 21%) and term (79%) deliveries. As Friis explained, women with preterm preeclampsia have a higher risk for acute complications and long-term cardiovascular outcomes than those with term preeclampsia.
Compared with those with normotensive pregnancies, investigators found an increased risk for the composite neurologic outcome among women with preterm preeclampsia (aHR, 1.54; 95% CI, 1.34-1.79), but also for those with term preeclampsia (aHR, 1.27; 95% CI, 1.17-1.38).
Common Vascular Component
The study also showed gestational hypertension and preeclampsia were associated with a later diagnosis of migraine, suggesting a possible common underlying vascular component.
“The increased risk of migraine following preeclampsia could be linked to endothelial damage at the blood-brain barrier level and alterations in cerebral blood flow and arterial vasospasm found in eclampsia, but this is only speculation,” said Friis.
The analysis also found an association between preeclampsia and a later diagnosis of headache. But this result likely encompasses several headache diagnoses, including migraine, so “it’s challenging to draw conclusions about the underlying mechanisms,” Friis added.
The study didn’t consider diagnoses from primary healthcare, which resulted in relatively few outcomes. The authors explained they could only identify the most severe cases; for example, women referred to specialized care.
Another potential study limitation is that Swedish registers don’t include information on race or ethnicity. Evidence shows there are racial differences in the risk for cardiovascular outcomes after preeclampsia.
This area of research is important as most women will experience at least one pregnancy in their lifetime, and preeclampsia affects 3%-5% of pregnancies. Further research is needed to understand the underlying pathophysiological mechanisms and the long-term consequences of this disorder, said Friis.
She added she hopes more therapeutic options will be available in the future for neuroprotective treatment for women with gestational hypertensive disorders.
Asked to comment, Thomas Vidic, MD, clinical professor of neurology, Indiana University School of Medicine, South Bend, said in an interview that this is an important study that includes robust data.
In his opinion, the most significant study finding is the marked increase in epilepsy risk after gestational eclampsia.
“In women who have new-onset epilepsy of unknown cause, asking about having eclampsia or preeclampsia during pregnancy is definitely a worthwhile question,” he said.
Confirming an etiology paints “a better picture” for patients wondering why they’re experiencing seizures, he added.
As with any registry-based study, this one had some acknowledged limitations, “but at the same time, the authors were able to have such a large database that I think this study is very worthwhile,” said Vidic.
The study received support from the Swedish Research Council. Neither Friis nor Vidic had relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Gestational hypertension, preeclampsia, or eclampsia is associated with a significantly higher risk for neurologic disorders such as migraine or epilepsy in the years following a first pregnancy, new research suggests.
The risk was highest in those with gestational eclampsia, who had a 70% increased chance of developing a neurologic disorder, including a fivefold increased risk for epilepsy, investigators found.
“When consulting women with new-onset neurological disorders, it’s important to inquire about their pregnancy history, as pregnancy complications such as gestational hypertension, preeclampsia, and eclampsia have been associated with an increased risk of neurological disorders later in life.” Therese Friis, MD, PhD student, Department of Women’s and Children’s Health, Uppsala University in Sweden, said in an interview.
The findings were published online in JAMA Neurology.
Most studies of maternal outcomes after gestational hypertension, preeclampsia, or eclampsia have focused on long-term risks for cardiovascular disease or neurologic complications such as stroke, dementia, and cognitive impairment. And many of these studies were relatively small and based on interviews or questionnaires.
“We wanted to investigate whether women with a hypertensive disorder of pregnancy also had a risk of other neurological complications, closer in time to the pregnancy,” said Friis.
The new study included 648,385 women (mean age, 28.5 years) whose first pregnancy occurred between 2005 and 2018. Of these, 94% had a normotensive pregnancy, 2% had gestational hypertension, 4% had preeclampsia without eclampsia, and 0.1% had eclampsia.
Gestational hypertension was defined as new-onset systolic blood pressure of ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg; preeclampsia was defined as gestational hypertension accompanied by proteinuria; and eclampsia was defined as tonic-clonic seizures without other etiology accompanied by preeclampsia.
Researchers used linked Swedish national registries that collect data on pregnancies, births, and infant and maternal characteristics. Among other things, they controlled for maternal age, early pregnancy body mass index, education level, and pregestational and gestational diabetes.
The primary outcome was a composite of five new-onset neurologic diagnoses: Migraine, headache, epilepsy, sleep disorder, and mental fatigue (neurasthenia), although one diagnosis was sufficient, from 42 days to 15 years after childbirth. Mean follow-up was 7.7 years.
Fivefold Epilepsy Risk
Compared with normotensive pregnancies, the risk for the primary outcome was 70% greater in those with eclampsia (adjusted hazard ratio [aHR], 1.70; 95% CI, 1.16-2.50), 27% higher for gestational hypertension (aHR, 1.27; 95% CI, 1.12-1.45), and 32% for preeclampsia (aHR, 1.32; 95% CI, 1.22-1.42).
Researchers also looked at the risk for individual neurologic disorders. There were too few neurasthenia events to generate meaningful results, so this diagnosis was omitted from the analysis.
Here, the study found women with eclampsia had five times the risk for epilepsy (aHR, 5.31; 95% CI, 2.85-9.89) compared with women with normotensive pregnancies.
The underlying mechanism for this association is unclear. However, said Friis, eclampsia and epilepsy share common pathways, such as neuroinflammation, and women with epilepsy before pregnancy run an increased risk for eclampsia.
“So common underlying pathways might increase the risk both for eclampsia in cases of a seizure disorder and a future seizure disorder after eclampsia,” she said.
In addition, preeclampsia and, in particular, eclampsia can cause irreversible subclinical cerebral infarcts found in areas of cerebral edema, she added. “These infarcts or scarring of brain tissue could potentially serve as foci for later epileptic activity.”
Researchers separated women with preeclampsia (with or without eclampsia) into those with preterm (less than 37 weeks; 21%) and term (79%) deliveries. As Friis explained, women with preterm preeclampsia have a higher risk for acute complications and long-term cardiovascular outcomes than those with term preeclampsia.
Compared with those with normotensive pregnancies, investigators found an increased risk for the composite neurologic outcome among women with preterm preeclampsia (aHR, 1.54; 95% CI, 1.34-1.79), but also for those with term preeclampsia (aHR, 1.27; 95% CI, 1.17-1.38).
Common Vascular Component
The study also showed gestational hypertension and preeclampsia were associated with a later diagnosis of migraine, suggesting a possible common underlying vascular component.
“The increased risk of migraine following preeclampsia could be linked to endothelial damage at the blood-brain barrier level and alterations in cerebral blood flow and arterial vasospasm found in eclampsia, but this is only speculation,” said Friis.
The analysis also found an association between preeclampsia and a later diagnosis of headache. But this result likely encompasses several headache diagnoses, including migraine, so “it’s challenging to draw conclusions about the underlying mechanisms,” Friis added.
The study didn’t consider diagnoses from primary healthcare, which resulted in relatively few outcomes. The authors explained they could only identify the most severe cases; for example, women referred to specialized care.
Another potential study limitation is that Swedish registers don’t include information on race or ethnicity. Evidence shows there are racial differences in the risk for cardiovascular outcomes after preeclampsia.
This area of research is important as most women will experience at least one pregnancy in their lifetime, and preeclampsia affects 3%-5% of pregnancies. Further research is needed to understand the underlying pathophysiological mechanisms and the long-term consequences of this disorder, said Friis.
She added she hopes more therapeutic options will be available in the future for neuroprotective treatment for women with gestational hypertensive disorders.
Asked to comment, Thomas Vidic, MD, clinical professor of neurology, Indiana University School of Medicine, South Bend, said in an interview that this is an important study that includes robust data.
In his opinion, the most significant study finding is the marked increase in epilepsy risk after gestational eclampsia.
“In women who have new-onset epilepsy of unknown cause, asking about having eclampsia or preeclampsia during pregnancy is definitely a worthwhile question,” he said.
Confirming an etiology paints “a better picture” for patients wondering why they’re experiencing seizures, he added.
As with any registry-based study, this one had some acknowledged limitations, “but at the same time, the authors were able to have such a large database that I think this study is very worthwhile,” said Vidic.
The study received support from the Swedish Research Council. Neither Friis nor Vidic had relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Gestational hypertension, preeclampsia, or eclampsia is associated with a significantly higher risk for neurologic disorders such as migraine or epilepsy in the years following a first pregnancy, new research suggests.
The risk was highest in those with gestational eclampsia, who had a 70% increased chance of developing a neurologic disorder, including a fivefold increased risk for epilepsy, investigators found.
“When consulting women with new-onset neurological disorders, it’s important to inquire about their pregnancy history, as pregnancy complications such as gestational hypertension, preeclampsia, and eclampsia have been associated with an increased risk of neurological disorders later in life.” Therese Friis, MD, PhD student, Department of Women’s and Children’s Health, Uppsala University in Sweden, said in an interview.
The findings were published online in JAMA Neurology.
Most studies of maternal outcomes after gestational hypertension, preeclampsia, or eclampsia have focused on long-term risks for cardiovascular disease or neurologic complications such as stroke, dementia, and cognitive impairment. And many of these studies were relatively small and based on interviews or questionnaires.
“We wanted to investigate whether women with a hypertensive disorder of pregnancy also had a risk of other neurological complications, closer in time to the pregnancy,” said Friis.
The new study included 648,385 women (mean age, 28.5 years) whose first pregnancy occurred between 2005 and 2018. Of these, 94% had a normotensive pregnancy, 2% had gestational hypertension, 4% had preeclampsia without eclampsia, and 0.1% had eclampsia.
Gestational hypertension was defined as new-onset systolic blood pressure of ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg; preeclampsia was defined as gestational hypertension accompanied by proteinuria; and eclampsia was defined as tonic-clonic seizures without other etiology accompanied by preeclampsia.
Researchers used linked Swedish national registries that collect data on pregnancies, births, and infant and maternal characteristics. Among other things, they controlled for maternal age, early pregnancy body mass index, education level, and pregestational and gestational diabetes.
The primary outcome was a composite of five new-onset neurologic diagnoses: Migraine, headache, epilepsy, sleep disorder, and mental fatigue (neurasthenia), although one diagnosis was sufficient, from 42 days to 15 years after childbirth. Mean follow-up was 7.7 years.
Fivefold Epilepsy Risk
Compared with normotensive pregnancies, the risk for the primary outcome was 70% greater in those with eclampsia (adjusted hazard ratio [aHR], 1.70; 95% CI, 1.16-2.50), 27% higher for gestational hypertension (aHR, 1.27; 95% CI, 1.12-1.45), and 32% for preeclampsia (aHR, 1.32; 95% CI, 1.22-1.42).
Researchers also looked at the risk for individual neurologic disorders. There were too few neurasthenia events to generate meaningful results, so this diagnosis was omitted from the analysis.
Here, the study found women with eclampsia had five times the risk for epilepsy (aHR, 5.31; 95% CI, 2.85-9.89) compared with women with normotensive pregnancies.
The underlying mechanism for this association is unclear. However, said Friis, eclampsia and epilepsy share common pathways, such as neuroinflammation, and women with epilepsy before pregnancy run an increased risk for eclampsia.
“So common underlying pathways might increase the risk both for eclampsia in cases of a seizure disorder and a future seizure disorder after eclampsia,” she said.
In addition, preeclampsia and, in particular, eclampsia can cause irreversible subclinical cerebral infarcts found in areas of cerebral edema, she added. “These infarcts or scarring of brain tissue could potentially serve as foci for later epileptic activity.”
Researchers separated women with preeclampsia (with or without eclampsia) into those with preterm (less than 37 weeks; 21%) and term (79%) deliveries. As Friis explained, women with preterm preeclampsia have a higher risk for acute complications and long-term cardiovascular outcomes than those with term preeclampsia.
Compared with those with normotensive pregnancies, investigators found an increased risk for the composite neurologic outcome among women with preterm preeclampsia (aHR, 1.54; 95% CI, 1.34-1.79), but also for those with term preeclampsia (aHR, 1.27; 95% CI, 1.17-1.38).
Common Vascular Component
The study also showed gestational hypertension and preeclampsia were associated with a later diagnosis of migraine, suggesting a possible common underlying vascular component.
“The increased risk of migraine following preeclampsia could be linked to endothelial damage at the blood-brain barrier level and alterations in cerebral blood flow and arterial vasospasm found in eclampsia, but this is only speculation,” said Friis.
The analysis also found an association between preeclampsia and a later diagnosis of headache. But this result likely encompasses several headache diagnoses, including migraine, so “it’s challenging to draw conclusions about the underlying mechanisms,” Friis added.
The study didn’t consider diagnoses from primary healthcare, which resulted in relatively few outcomes. The authors explained they could only identify the most severe cases; for example, women referred to specialized care.
Another potential study limitation is that Swedish registers don’t include information on race or ethnicity. Evidence shows there are racial differences in the risk for cardiovascular outcomes after preeclampsia.
This area of research is important as most women will experience at least one pregnancy in their lifetime, and preeclampsia affects 3%-5% of pregnancies. Further research is needed to understand the underlying pathophysiological mechanisms and the long-term consequences of this disorder, said Friis.
She added she hopes more therapeutic options will be available in the future for neuroprotective treatment for women with gestational hypertensive disorders.
Asked to comment, Thomas Vidic, MD, clinical professor of neurology, Indiana University School of Medicine, South Bend, said in an interview that this is an important study that includes robust data.
In his opinion, the most significant study finding is the marked increase in epilepsy risk after gestational eclampsia.
“In women who have new-onset epilepsy of unknown cause, asking about having eclampsia or preeclampsia during pregnancy is definitely a worthwhile question,” he said.
Confirming an etiology paints “a better picture” for patients wondering why they’re experiencing seizures, he added.
As with any registry-based study, this one had some acknowledged limitations, “but at the same time, the authors were able to have such a large database that I think this study is very worthwhile,” said Vidic.
The study received support from the Swedish Research Council. Neither Friis nor Vidic had relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM JAMA NEUROLOGY
AI Shows Early Promise in Detecting Infantile Spasms
LOS ANGELES — according to a new study.
Infants with the condition can have poor outcomes with even small delays in diagnosis and ensuing treatment, potentially leading to intellectual disability, autism, and worse epilepsy. “It’s super important to start the treatment early, but oftentimes, these symptoms are just misrecognized by primary care or ER physicians. It takes a long time to diagnose,” said Gadi Miron, MD, who presented the study at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
What Is This? What Should I Do?
Parents who observe unusual behavior often seek advice from friends and family members and receive false reassurance that such behavior isn’t unusual. Even physicians may contribute if they are unaware of infantile spasms, which is a rare disorder. “And then again, they get false reassurance, and because of that false reassurance, you get a diagnostic delay,” said Shaun Hussain, MD, who was asked to comment on the study.
The timing and frequency of infantile spasms create challenges for diagnosis. They only last about 1 second, and they tend to cluster in the morning. By the time a caregiver brings an infant to a healthcare provider, they may have trouble describing the behavior. “Parents are struggling to describe what they saw, and it often just does not resonate, or doesn’t make the healthcare provider think about infantile spasms,” said Hussain.
The idea to employ AI came from looking at videos of infants on YouTube and the realization that many patients upload them in an effort to seek advice. “So many parents upload these videos and ask in the comments, ‘What is this? What should I do? Can somebody help me?’ said Miron, who is a neurologist and researcher at Charité — Universitätsmedizin Berlin in Germany.
AI and Video Can Aid Diagnosis
The researchers built a model that they trained to recognize epileptic spasms using openly available YouTube videos, including 141 infants, 991 recorded seizures, and 597 non-seizure video segments, along with a non-seizure cohort of 127 infants with an accompanying 1385 video segments.
Each video segment was reviewed by two specialists, and they had to agree for it to be counted as an epileptic spasm.
The model detected epileptic seizures with an area under the curve (AUC) of 0.96. It had a sensitivity of 82%, specificity of 90%, and accuracy of 85% when applied to the training set.
The researchers then tested it against three validation sets. In the first, a smartphone-based set retrieved from TikTok of 26 infants with 70 epileptic spasms and 31 non-seizure 5-second video segments, the model had an AUC of 0.98, a sensitivity of 89%, a specificity of 100%, and an accuracy of 92%.
A second smartphone-based set of 67 infants, drawn from YouTube, showed a false detection rate of 0.75% (five detections out of 666 video segments). A third dataset collected from in-hospital EEG monitoring of 21 infants without seizures revealed a false-positive rate of 3.4% (365 of 10,860 video segments).
The group is now developing an app that will allow parents to upload videos that can be analyzed using the model. Physicians can then view the video and determine if there is suspicion of a seizure.
Miron also believes that this approach could find use in other types of seizures and populations, including older children and adults. “We have actually built some models for detection of seizures for videos in adults as well. Looking more towards the future, I’m sure AI will be used to analyze videos of other neurological disorders with motor symptoms [such as] movement disorders and gait,” he said.
Encouraging Early Research
Hussain, who is a professor of pediatrics at UCLA Health, lauded the work generally but emphasized that it is still in the early stage. “Their comparison was a relatively easy one. They’re just comparing normal versus infantile spasms, and they’re looking at the seizure versus normal behavior. Usually, the distinction is much harder in that there are kids who are having behaviors that are maybe other types of seizures, which is much harder to distinguish from infantile spasms, in contrast to just normal behaviors. The other mimic of infantile spasms is things like infant heartburn. Those kids will often have some posturing, and they often will be in pain. They might cry. That’s something that infantile spasms will often generate, so that’s why there’s a lot of confusion between those two,” said Hussain.
He noted that there have been efforts to raise awareness of infantile spasms among physicians and the general public, but that hasn’t reduced the increased detection.
Another Resource
In fact, parents with suspicions often go to social media sites like YouTube and a Facebook group dedicated to infantile spasms. “You can Google infantile spasms, and you’ll see examples of weird behaviors, and then you’ll look in the comments, and you’ll see this commenter said: ‘These could be infantile spasms. You should go to a children’s hospital. Don’t leave until you get an EEG to make sure that these are not seizures. There’s all kinds of great advice there, and it really shouldn’t be the situation where to get the best care, you need to go on YouTube,’ ” said Hussain.
Miron and Hussain had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
LOS ANGELES — according to a new study.
Infants with the condition can have poor outcomes with even small delays in diagnosis and ensuing treatment, potentially leading to intellectual disability, autism, and worse epilepsy. “It’s super important to start the treatment early, but oftentimes, these symptoms are just misrecognized by primary care or ER physicians. It takes a long time to diagnose,” said Gadi Miron, MD, who presented the study at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
What Is This? What Should I Do?
Parents who observe unusual behavior often seek advice from friends and family members and receive false reassurance that such behavior isn’t unusual. Even physicians may contribute if they are unaware of infantile spasms, which is a rare disorder. “And then again, they get false reassurance, and because of that false reassurance, you get a diagnostic delay,” said Shaun Hussain, MD, who was asked to comment on the study.
The timing and frequency of infantile spasms create challenges for diagnosis. They only last about 1 second, and they tend to cluster in the morning. By the time a caregiver brings an infant to a healthcare provider, they may have trouble describing the behavior. “Parents are struggling to describe what they saw, and it often just does not resonate, or doesn’t make the healthcare provider think about infantile spasms,” said Hussain.
The idea to employ AI came from looking at videos of infants on YouTube and the realization that many patients upload them in an effort to seek advice. “So many parents upload these videos and ask in the comments, ‘What is this? What should I do? Can somebody help me?’ said Miron, who is a neurologist and researcher at Charité — Universitätsmedizin Berlin in Germany.
AI and Video Can Aid Diagnosis
The researchers built a model that they trained to recognize epileptic spasms using openly available YouTube videos, including 141 infants, 991 recorded seizures, and 597 non-seizure video segments, along with a non-seizure cohort of 127 infants with an accompanying 1385 video segments.
Each video segment was reviewed by two specialists, and they had to agree for it to be counted as an epileptic spasm.
The model detected epileptic seizures with an area under the curve (AUC) of 0.96. It had a sensitivity of 82%, specificity of 90%, and accuracy of 85% when applied to the training set.
The researchers then tested it against three validation sets. In the first, a smartphone-based set retrieved from TikTok of 26 infants with 70 epileptic spasms and 31 non-seizure 5-second video segments, the model had an AUC of 0.98, a sensitivity of 89%, a specificity of 100%, and an accuracy of 92%.
A second smartphone-based set of 67 infants, drawn from YouTube, showed a false detection rate of 0.75% (five detections out of 666 video segments). A third dataset collected from in-hospital EEG monitoring of 21 infants without seizures revealed a false-positive rate of 3.4% (365 of 10,860 video segments).
The group is now developing an app that will allow parents to upload videos that can be analyzed using the model. Physicians can then view the video and determine if there is suspicion of a seizure.
Miron also believes that this approach could find use in other types of seizures and populations, including older children and adults. “We have actually built some models for detection of seizures for videos in adults as well. Looking more towards the future, I’m sure AI will be used to analyze videos of other neurological disorders with motor symptoms [such as] movement disorders and gait,” he said.
Encouraging Early Research
Hussain, who is a professor of pediatrics at UCLA Health, lauded the work generally but emphasized that it is still in the early stage. “Their comparison was a relatively easy one. They’re just comparing normal versus infantile spasms, and they’re looking at the seizure versus normal behavior. Usually, the distinction is much harder in that there are kids who are having behaviors that are maybe other types of seizures, which is much harder to distinguish from infantile spasms, in contrast to just normal behaviors. The other mimic of infantile spasms is things like infant heartburn. Those kids will often have some posturing, and they often will be in pain. They might cry. That’s something that infantile spasms will often generate, so that’s why there’s a lot of confusion between those two,” said Hussain.
He noted that there have been efforts to raise awareness of infantile spasms among physicians and the general public, but that hasn’t reduced the increased detection.
Another Resource
In fact, parents with suspicions often go to social media sites like YouTube and a Facebook group dedicated to infantile spasms. “You can Google infantile spasms, and you’ll see examples of weird behaviors, and then you’ll look in the comments, and you’ll see this commenter said: ‘These could be infantile spasms. You should go to a children’s hospital. Don’t leave until you get an EEG to make sure that these are not seizures. There’s all kinds of great advice there, and it really shouldn’t be the situation where to get the best care, you need to go on YouTube,’ ” said Hussain.
Miron and Hussain had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
LOS ANGELES — according to a new study.
Infants with the condition can have poor outcomes with even small delays in diagnosis and ensuing treatment, potentially leading to intellectual disability, autism, and worse epilepsy. “It’s super important to start the treatment early, but oftentimes, these symptoms are just misrecognized by primary care or ER physicians. It takes a long time to diagnose,” said Gadi Miron, MD, who presented the study at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
What Is This? What Should I Do?
Parents who observe unusual behavior often seek advice from friends and family members and receive false reassurance that such behavior isn’t unusual. Even physicians may contribute if they are unaware of infantile spasms, which is a rare disorder. “And then again, they get false reassurance, and because of that false reassurance, you get a diagnostic delay,” said Shaun Hussain, MD, who was asked to comment on the study.
The timing and frequency of infantile spasms create challenges for diagnosis. They only last about 1 second, and they tend to cluster in the morning. By the time a caregiver brings an infant to a healthcare provider, they may have trouble describing the behavior. “Parents are struggling to describe what they saw, and it often just does not resonate, or doesn’t make the healthcare provider think about infantile spasms,” said Hussain.
The idea to employ AI came from looking at videos of infants on YouTube and the realization that many patients upload them in an effort to seek advice. “So many parents upload these videos and ask in the comments, ‘What is this? What should I do? Can somebody help me?’ said Miron, who is a neurologist and researcher at Charité — Universitätsmedizin Berlin in Germany.
AI and Video Can Aid Diagnosis
The researchers built a model that they trained to recognize epileptic spasms using openly available YouTube videos, including 141 infants, 991 recorded seizures, and 597 non-seizure video segments, along with a non-seizure cohort of 127 infants with an accompanying 1385 video segments.
Each video segment was reviewed by two specialists, and they had to agree for it to be counted as an epileptic spasm.
The model detected epileptic seizures with an area under the curve (AUC) of 0.96. It had a sensitivity of 82%, specificity of 90%, and accuracy of 85% when applied to the training set.
The researchers then tested it against three validation sets. In the first, a smartphone-based set retrieved from TikTok of 26 infants with 70 epileptic spasms and 31 non-seizure 5-second video segments, the model had an AUC of 0.98, a sensitivity of 89%, a specificity of 100%, and an accuracy of 92%.
A second smartphone-based set of 67 infants, drawn from YouTube, showed a false detection rate of 0.75% (five detections out of 666 video segments). A third dataset collected from in-hospital EEG monitoring of 21 infants without seizures revealed a false-positive rate of 3.4% (365 of 10,860 video segments).
The group is now developing an app that will allow parents to upload videos that can be analyzed using the model. Physicians can then view the video and determine if there is suspicion of a seizure.
Miron also believes that this approach could find use in other types of seizures and populations, including older children and adults. “We have actually built some models for detection of seizures for videos in adults as well. Looking more towards the future, I’m sure AI will be used to analyze videos of other neurological disorders with motor symptoms [such as] movement disorders and gait,” he said.
Encouraging Early Research
Hussain, who is a professor of pediatrics at UCLA Health, lauded the work generally but emphasized that it is still in the early stage. “Their comparison was a relatively easy one. They’re just comparing normal versus infantile spasms, and they’re looking at the seizure versus normal behavior. Usually, the distinction is much harder in that there are kids who are having behaviors that are maybe other types of seizures, which is much harder to distinguish from infantile spasms, in contrast to just normal behaviors. The other mimic of infantile spasms is things like infant heartburn. Those kids will often have some posturing, and they often will be in pain. They might cry. That’s something that infantile spasms will often generate, so that’s why there’s a lot of confusion between those two,” said Hussain.
He noted that there have been efforts to raise awareness of infantile spasms among physicians and the general public, but that hasn’t reduced the increased detection.
Another Resource
In fact, parents with suspicions often go to social media sites like YouTube and a Facebook group dedicated to infantile spasms. “You can Google infantile spasms, and you’ll see examples of weird behaviors, and then you’ll look in the comments, and you’ll see this commenter said: ‘These could be infantile spasms. You should go to a children’s hospital. Don’t leave until you get an EEG to make sure that these are not seizures. There’s all kinds of great advice there, and it really shouldn’t be the situation where to get the best care, you need to go on YouTube,’ ” said Hussain.
Miron and Hussain had no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FROM AES 2024
Angiotensin Receptor Blockers Cut Epilepsy Risk in Patients With Hypertension
LOS ANGELES — (PSE), new research showed.
Investigators found angiotensin receptor blockers are better at cutting the PSE risk in individuals with high blood pressure than angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers, and beta-blockers.
The results suggested angiotensin receptor blockers could be a frontline strategy to proactively forestall development of epilepsy in patients with a history of stroke and hypertension, said the study’s co-lead investigator Giacomo Evangelista, MD, PhD, a resident in neurology at the Epilepsy Center at “G. d’Annunzio” University of Chieti-Pescara, Italy.
The findings were presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Stroke and Seizures Tightly Linked
Stroke is the most common cause of seizures in patients older than 60 years. About 6%-8% of new epilepsy diagnoses in older adult patients are associated with a brain ischemic event.
Hypertension is among the most common risk factors for both epilepsy and stroke. The European Society of Cardiology recommends ACE inhibitors and angiotensin receptor blockers be considered first-line hypertension treatments.
Angiotensin receptor blockers seem to provide a protective effect in terms of seizures in the general population, but their possible preventive role in PSE has not been clear.
The retrospective, observational study included 528 patients (mean age, 71.4 years; 57.19% men) with hypertension and ischemic stroke without a history of epilepsy.
Researchers divided patients into those who developed PSE during the 2-year follow-up and those who didn’t. The main outcome was incidence of PSE associated with angiotensin receptor blocker therapy compared with other antihypertensive drug classes (ACE inhibitors, calcium channel blockers, and beta blockers).
Of the total, 7.2% of patients developed PSE. The study found patients treated with an angiotensin receptor blockers had a lower risk for PSE (P = .009). PSE incidence was higher among patients receiving calcium channel blockers (P = .019) and beta blockers (P = .008), but ACE inhibitors did not appear to affect PSE risk.
Further analysis showed that patients taking a beta blocker were 120% more likely to develop PSE, and those taking a calcium channel blocker were 110% more likely to develop PSE than those taking an angiotensin receptor blocker. The corresponding comparison was 65% for those taking an ACE inhibitor.
Potential Mechanisms
Angiotensin receptor blockers block the angiotensin II type 1 receptor, which may lead to numerous neuroprotective benefits such as improved blood flow to the brain and less neuroinflammation. The blockage may also reduce epilepsy severity and seizure frequency.
ACE inhibitors work in the same system as angiotensin receptor blockers but don’t bind directly to the angiotensin receptor. Experts believe these drugs may lead to inflammation that raises the risk for PSE.
Calcium channel blockers and beta blockers may increase the likelihood of seizures by inducing excessive excitability in the brain, which can trigger seizures.
Other research presented at the meeting found that angiotensin receptor blockers reduce the risk for epilepsy in patients with hypertension even in the absence of stroke.
Using data from an US national administrative database, the retrospective cohort study included 2,261,964 eligible adult beneficiaries diagnosed with hypertension and dispensed at least one angiotensin receptor blocker, ACE inhibitor, beta blocker, or calcium channel blocker from 2010 to 2017.
The study found angiotensin receptor blockers were associated with lower epilepsy incidence than ACE inhibitors (hazard ratio [HR], 0.75; 95% CI, 0.58-0.96), beta blockers (HR, 0.70; 95% CI, 0.54-0.90), and calcium channel blockers (HR, 0.80; 95% CI, 0.61-1.04).
The effect was most robust for the angiotensin receptor blocker losartan and among patients with no preexisting stroke or cardiovascular conditions.
Researchers ran the analysis excluding stroke and the association was still there, said lead study author Kimford Meador, MD, professor of neurology and neurological sciences, Stanford University, Palo Alto, California. “People with hypertension who use angiotensin receptor blockers — even if they don’t have a stroke — are less likely to develop epilepsy than if they use other major anti-hypertensives.”
Exciting and Suggestive
These new studies are “exciting” and “very suggestive,” said Meador. “We don’t have any true antiepileptic drugs; we have antiseizure medications. If we could reduce the incidence of epilepsy, that would be a very big thing.”
But the research to date hasn’t been “definitive” and is subject to bias, he said. “What we really need is a large randomized controlled trial to see if this is real because any observational study in humans has the potential for confounding from unmeasured variables.”
If such a study does show the effect is real, “that would change clinical practice,” said Meador.
As angiotensin receptor blockers have anti-inflammatory effects, researchers are now investigating whether this class of drugs might be useful in other diseases linked to inflammation such as multiple sclerosis, said Meador.
Commenting on the research, Alain Zingraff Looti, MD, assistant professor of neurology and public health sciences, Penn State College of Medicine, Hershey, Pennsylvania, said this new research is “important” although still at a “very preliminary stage.”
As the studies so far have all been observational, “they showed an association, but that doesn’t mean causality,” said Looti. These studies just looked at known potential confounders, “and there may be some unknown confounders that could explain the association,” he added.
But he acknowledged the results make sense from a biological standpoint. He noted that infusing angiotensin receptor blockers into rats causes a “cascade reaction” leading to reduced inflammation in the brain and then to less epilepsy. “Inflammation plays a major role in several models of epilepsy,” he added.
While these new results are important, Looti, too, would like to see a randomized controlled trial to confirm the findings.
Looti and Meador reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
LOS ANGELES — (PSE), new research showed.
Investigators found angiotensin receptor blockers are better at cutting the PSE risk in individuals with high blood pressure than angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers, and beta-blockers.
The results suggested angiotensin receptor blockers could be a frontline strategy to proactively forestall development of epilepsy in patients with a history of stroke and hypertension, said the study’s co-lead investigator Giacomo Evangelista, MD, PhD, a resident in neurology at the Epilepsy Center at “G. d’Annunzio” University of Chieti-Pescara, Italy.
The findings were presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Stroke and Seizures Tightly Linked
Stroke is the most common cause of seizures in patients older than 60 years. About 6%-8% of new epilepsy diagnoses in older adult patients are associated with a brain ischemic event.
Hypertension is among the most common risk factors for both epilepsy and stroke. The European Society of Cardiology recommends ACE inhibitors and angiotensin receptor blockers be considered first-line hypertension treatments.
Angiotensin receptor blockers seem to provide a protective effect in terms of seizures in the general population, but their possible preventive role in PSE has not been clear.
The retrospective, observational study included 528 patients (mean age, 71.4 years; 57.19% men) with hypertension and ischemic stroke without a history of epilepsy.
Researchers divided patients into those who developed PSE during the 2-year follow-up and those who didn’t. The main outcome was incidence of PSE associated with angiotensin receptor blocker therapy compared with other antihypertensive drug classes (ACE inhibitors, calcium channel blockers, and beta blockers).
Of the total, 7.2% of patients developed PSE. The study found patients treated with an angiotensin receptor blockers had a lower risk for PSE (P = .009). PSE incidence was higher among patients receiving calcium channel blockers (P = .019) and beta blockers (P = .008), but ACE inhibitors did not appear to affect PSE risk.
Further analysis showed that patients taking a beta blocker were 120% more likely to develop PSE, and those taking a calcium channel blocker were 110% more likely to develop PSE than those taking an angiotensin receptor blocker. The corresponding comparison was 65% for those taking an ACE inhibitor.
Potential Mechanisms
Angiotensin receptor blockers block the angiotensin II type 1 receptor, which may lead to numerous neuroprotective benefits such as improved blood flow to the brain and less neuroinflammation. The blockage may also reduce epilepsy severity and seizure frequency.
ACE inhibitors work in the same system as angiotensin receptor blockers but don’t bind directly to the angiotensin receptor. Experts believe these drugs may lead to inflammation that raises the risk for PSE.
Calcium channel blockers and beta blockers may increase the likelihood of seizures by inducing excessive excitability in the brain, which can trigger seizures.
Other research presented at the meeting found that angiotensin receptor blockers reduce the risk for epilepsy in patients with hypertension even in the absence of stroke.
Using data from an US national administrative database, the retrospective cohort study included 2,261,964 eligible adult beneficiaries diagnosed with hypertension and dispensed at least one angiotensin receptor blocker, ACE inhibitor, beta blocker, or calcium channel blocker from 2010 to 2017.
The study found angiotensin receptor blockers were associated with lower epilepsy incidence than ACE inhibitors (hazard ratio [HR], 0.75; 95% CI, 0.58-0.96), beta blockers (HR, 0.70; 95% CI, 0.54-0.90), and calcium channel blockers (HR, 0.80; 95% CI, 0.61-1.04).
The effect was most robust for the angiotensin receptor blocker losartan and among patients with no preexisting stroke or cardiovascular conditions.
Researchers ran the analysis excluding stroke and the association was still there, said lead study author Kimford Meador, MD, professor of neurology and neurological sciences, Stanford University, Palo Alto, California. “People with hypertension who use angiotensin receptor blockers — even if they don’t have a stroke — are less likely to develop epilepsy than if they use other major anti-hypertensives.”
Exciting and Suggestive
These new studies are “exciting” and “very suggestive,” said Meador. “We don’t have any true antiepileptic drugs; we have antiseizure medications. If we could reduce the incidence of epilepsy, that would be a very big thing.”
But the research to date hasn’t been “definitive” and is subject to bias, he said. “What we really need is a large randomized controlled trial to see if this is real because any observational study in humans has the potential for confounding from unmeasured variables.”
If such a study does show the effect is real, “that would change clinical practice,” said Meador.
As angiotensin receptor blockers have anti-inflammatory effects, researchers are now investigating whether this class of drugs might be useful in other diseases linked to inflammation such as multiple sclerosis, said Meador.
Commenting on the research, Alain Zingraff Looti, MD, assistant professor of neurology and public health sciences, Penn State College of Medicine, Hershey, Pennsylvania, said this new research is “important” although still at a “very preliminary stage.”
As the studies so far have all been observational, “they showed an association, but that doesn’t mean causality,” said Looti. These studies just looked at known potential confounders, “and there may be some unknown confounders that could explain the association,” he added.
But he acknowledged the results make sense from a biological standpoint. He noted that infusing angiotensin receptor blockers into rats causes a “cascade reaction” leading to reduced inflammation in the brain and then to less epilepsy. “Inflammation plays a major role in several models of epilepsy,” he added.
While these new results are important, Looti, too, would like to see a randomized controlled trial to confirm the findings.
Looti and Meador reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
LOS ANGELES — (PSE), new research showed.
Investigators found angiotensin receptor blockers are better at cutting the PSE risk in individuals with high blood pressure than angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers, and beta-blockers.
The results suggested angiotensin receptor blockers could be a frontline strategy to proactively forestall development of epilepsy in patients with a history of stroke and hypertension, said the study’s co-lead investigator Giacomo Evangelista, MD, PhD, a resident in neurology at the Epilepsy Center at “G. d’Annunzio” University of Chieti-Pescara, Italy.
The findings were presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Stroke and Seizures Tightly Linked
Stroke is the most common cause of seizures in patients older than 60 years. About 6%-8% of new epilepsy diagnoses in older adult patients are associated with a brain ischemic event.
Hypertension is among the most common risk factors for both epilepsy and stroke. The European Society of Cardiology recommends ACE inhibitors and angiotensin receptor blockers be considered first-line hypertension treatments.
Angiotensin receptor blockers seem to provide a protective effect in terms of seizures in the general population, but their possible preventive role in PSE has not been clear.
The retrospective, observational study included 528 patients (mean age, 71.4 years; 57.19% men) with hypertension and ischemic stroke without a history of epilepsy.
Researchers divided patients into those who developed PSE during the 2-year follow-up and those who didn’t. The main outcome was incidence of PSE associated with angiotensin receptor blocker therapy compared with other antihypertensive drug classes (ACE inhibitors, calcium channel blockers, and beta blockers).
Of the total, 7.2% of patients developed PSE. The study found patients treated with an angiotensin receptor blockers had a lower risk for PSE (P = .009). PSE incidence was higher among patients receiving calcium channel blockers (P = .019) and beta blockers (P = .008), but ACE inhibitors did not appear to affect PSE risk.
Further analysis showed that patients taking a beta blocker were 120% more likely to develop PSE, and those taking a calcium channel blocker were 110% more likely to develop PSE than those taking an angiotensin receptor blocker. The corresponding comparison was 65% for those taking an ACE inhibitor.
Potential Mechanisms
Angiotensin receptor blockers block the angiotensin II type 1 receptor, which may lead to numerous neuroprotective benefits such as improved blood flow to the brain and less neuroinflammation. The blockage may also reduce epilepsy severity and seizure frequency.
ACE inhibitors work in the same system as angiotensin receptor blockers but don’t bind directly to the angiotensin receptor. Experts believe these drugs may lead to inflammation that raises the risk for PSE.
Calcium channel blockers and beta blockers may increase the likelihood of seizures by inducing excessive excitability in the brain, which can trigger seizures.
Other research presented at the meeting found that angiotensin receptor blockers reduce the risk for epilepsy in patients with hypertension even in the absence of stroke.
Using data from an US national administrative database, the retrospective cohort study included 2,261,964 eligible adult beneficiaries diagnosed with hypertension and dispensed at least one angiotensin receptor blocker, ACE inhibitor, beta blocker, or calcium channel blocker from 2010 to 2017.
The study found angiotensin receptor blockers were associated with lower epilepsy incidence than ACE inhibitors (hazard ratio [HR], 0.75; 95% CI, 0.58-0.96), beta blockers (HR, 0.70; 95% CI, 0.54-0.90), and calcium channel blockers (HR, 0.80; 95% CI, 0.61-1.04).
The effect was most robust for the angiotensin receptor blocker losartan and among patients with no preexisting stroke or cardiovascular conditions.
Researchers ran the analysis excluding stroke and the association was still there, said lead study author Kimford Meador, MD, professor of neurology and neurological sciences, Stanford University, Palo Alto, California. “People with hypertension who use angiotensin receptor blockers — even if they don’t have a stroke — are less likely to develop epilepsy than if they use other major anti-hypertensives.”
Exciting and Suggestive
These new studies are “exciting” and “very suggestive,” said Meador. “We don’t have any true antiepileptic drugs; we have antiseizure medications. If we could reduce the incidence of epilepsy, that would be a very big thing.”
But the research to date hasn’t been “definitive” and is subject to bias, he said. “What we really need is a large randomized controlled trial to see if this is real because any observational study in humans has the potential for confounding from unmeasured variables.”
If such a study does show the effect is real, “that would change clinical practice,” said Meador.
As angiotensin receptor blockers have anti-inflammatory effects, researchers are now investigating whether this class of drugs might be useful in other diseases linked to inflammation such as multiple sclerosis, said Meador.
Commenting on the research, Alain Zingraff Looti, MD, assistant professor of neurology and public health sciences, Penn State College of Medicine, Hershey, Pennsylvania, said this new research is “important” although still at a “very preliminary stage.”
As the studies so far have all been observational, “they showed an association, but that doesn’t mean causality,” said Looti. These studies just looked at known potential confounders, “and there may be some unknown confounders that could explain the association,” he added.
But he acknowledged the results make sense from a biological standpoint. He noted that infusing angiotensin receptor blockers into rats causes a “cascade reaction” leading to reduced inflammation in the brain and then to less epilepsy. “Inflammation plays a major role in several models of epilepsy,” he added.
While these new results are important, Looti, too, would like to see a randomized controlled trial to confirm the findings.
Looti and Meador reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FROM AES 2024
‘Urgent Need’ to Examine Anti-Seizure Medication Pricing
LOS ANGELES — results of a new study showed.
These findings highlight an “urgent need” to examine ASM pricing, said study investigator Pradeep Javarayee, MD, MBA, assistant professor, Department of Neurology, Medical College of Wisconsin, Milwaukee.
“The price disparity between generic and brand-name anti-seizure medications is growing,” said Javarayee. “Understanding these trends is essential for clinicians to make cost-conscious prescribing decisions and to advocate for policies that ensure equitable access to treatment for patients with epilepsy.”
The findings were presented at American Epilepsy Society (AES) 78th Annual Meeting 2024.
Concerning Trends
Researchers analyzed prices of ASMs using National Average Drug Acquisition Cost (NADAC) data provided by the Centers for Medicare & Medicaid Services from November 2013 to July 2023.
A publicly available resource, NADAC is widely regarded as the most reliable benchmark for drug reimbursement in the United States, said Javarayee. It is based on the price/unit of Medicaid-covered outpatient drugs collected though monthly surveys of retail community pharmacies across the United States.
The database includes medication names, strengths, formulations, and National Drug Codes.
The study examined 23 US Food and Drug Administration–approved ASMs, encompassing 223 oral formulations, which included 112 brand-name and 111 generic products.
To account for inflation, researchers adjusted ASM prices using the Consumer Price Index for Medicinal Drugs–Seasonally Adjusted. They also explored the effects of the COVID-19 pandemic on drug pricing.
The study uncovered trends that Javarayee found concerning. For example, between 2013 and 2023, the average price of brand-name ASMs increased from $8.71 to $15.43, whereas the average price of generic ASMs decreased from $1.39 to $1.26.
Most generic ASMs remained in the low-cost range ($0-$0.25) during the study period, whereas the proportion of higher-priced brand-name ASMs ($10-$50) increased.
The number of brand-name ASMs with a mean price exceeding $15 rose from two (2013-2016) to six (2017-2019) and then to eight (2020-2023).
Unsustainable Price Increases
The study uncovered examples of what Javarayee called “extreme” price differences. For instance, matched brand-name and generic ASMs with price differences of 1000%-9999% increased from 32.88% in 2013-2016 to 41.43% in 2020-2023.
Among brand-name ASMs, cenobamate (Xcopri), which is approved in the United States for partial-onset seizures, had the highest mean price between 2020 and 2023 ($35.59). For generic ASMs, topiramate had the highest mean price in the same time period ($6.64).
Looking at formulation-based cost differences, the study found generic immediate-release formulations were significantly cheaper than extended-release or delayed-release counterparts, with cost differences reaching as high as 7751.20%.
The study also showed the COVID-19 pandemic led to a 24.4% increase in brand-name ASM prices and a 23.1% decrease in generic ASM prices.
The results underscore the need to raise awareness of drug pricing dynamics and call for targeted policy interventions to alleviate the rising cost burden on patients, said Javarayee.
He emphasized that such price increases are unsustainable. “Addressing these disparities is critical not only for improving patient adherence and outcomes but also for reducing the overall economic strain on the healthcare system.”
‘Tip of the Iceberg’
Reached for a comment, Tim Welty, a pharmacist in Des Moines, Iowa, who specializes in epilepsy drugs, agreed that the issue of medication costs needs to be addressed.
“I absolutely think physicians and others need to advocate for transparency in pricing,” he said. It’s not unusual for physician requests to have newer ASMs covered for their patients to be denied, he added.
Welty also noted Congress is currently considering bills that address the lack of transparency in the way medications are reimbursed.
This new study doesn’t reveal what patients are paying for their medications, he said. “These data tell me the national average of the cost to the pharmacy, but don’t tell me what the patient is actually paying, or what the insurance companies are actually paying for these medications.”
A “hot topic” in the industry is the role of pharmacy benefit managers, who are contracted by health insurance companies to manage medication portfolios, in influencing drug prices.
Drug pricing is a complicated topic. “There’s a lot more behind this; this is just like a tip of the iceberg,” said Welty.
Also commenting, Jacqueline French, MD, professor, NYU Comprehensive Epilepsy Center, New York City, said the much higher ASM prices are “very problematic,” particularly for drugs that don’t have a generic.
“I wonder how much the drugs for orphan indications, which are usually higher priced, influenced the numbers.”
The good news, though, is that many people “can safely take generics if they’re available,” said French.
The investigators and Welty reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
LOS ANGELES — results of a new study showed.
These findings highlight an “urgent need” to examine ASM pricing, said study investigator Pradeep Javarayee, MD, MBA, assistant professor, Department of Neurology, Medical College of Wisconsin, Milwaukee.
“The price disparity between generic and brand-name anti-seizure medications is growing,” said Javarayee. “Understanding these trends is essential for clinicians to make cost-conscious prescribing decisions and to advocate for policies that ensure equitable access to treatment for patients with epilepsy.”
The findings were presented at American Epilepsy Society (AES) 78th Annual Meeting 2024.
Concerning Trends
Researchers analyzed prices of ASMs using National Average Drug Acquisition Cost (NADAC) data provided by the Centers for Medicare & Medicaid Services from November 2013 to July 2023.
A publicly available resource, NADAC is widely regarded as the most reliable benchmark for drug reimbursement in the United States, said Javarayee. It is based on the price/unit of Medicaid-covered outpatient drugs collected though monthly surveys of retail community pharmacies across the United States.
The database includes medication names, strengths, formulations, and National Drug Codes.
The study examined 23 US Food and Drug Administration–approved ASMs, encompassing 223 oral formulations, which included 112 brand-name and 111 generic products.
To account for inflation, researchers adjusted ASM prices using the Consumer Price Index for Medicinal Drugs–Seasonally Adjusted. They also explored the effects of the COVID-19 pandemic on drug pricing.
The study uncovered trends that Javarayee found concerning. For example, between 2013 and 2023, the average price of brand-name ASMs increased from $8.71 to $15.43, whereas the average price of generic ASMs decreased from $1.39 to $1.26.
Most generic ASMs remained in the low-cost range ($0-$0.25) during the study period, whereas the proportion of higher-priced brand-name ASMs ($10-$50) increased.
The number of brand-name ASMs with a mean price exceeding $15 rose from two (2013-2016) to six (2017-2019) and then to eight (2020-2023).
Unsustainable Price Increases
The study uncovered examples of what Javarayee called “extreme” price differences. For instance, matched brand-name and generic ASMs with price differences of 1000%-9999% increased from 32.88% in 2013-2016 to 41.43% in 2020-2023.
Among brand-name ASMs, cenobamate (Xcopri), which is approved in the United States for partial-onset seizures, had the highest mean price between 2020 and 2023 ($35.59). For generic ASMs, topiramate had the highest mean price in the same time period ($6.64).
Looking at formulation-based cost differences, the study found generic immediate-release formulations were significantly cheaper than extended-release or delayed-release counterparts, with cost differences reaching as high as 7751.20%.
The study also showed the COVID-19 pandemic led to a 24.4% increase in brand-name ASM prices and a 23.1% decrease in generic ASM prices.
The results underscore the need to raise awareness of drug pricing dynamics and call for targeted policy interventions to alleviate the rising cost burden on patients, said Javarayee.
He emphasized that such price increases are unsustainable. “Addressing these disparities is critical not only for improving patient adherence and outcomes but also for reducing the overall economic strain on the healthcare system.”
‘Tip of the Iceberg’
Reached for a comment, Tim Welty, a pharmacist in Des Moines, Iowa, who specializes in epilepsy drugs, agreed that the issue of medication costs needs to be addressed.
“I absolutely think physicians and others need to advocate for transparency in pricing,” he said. It’s not unusual for physician requests to have newer ASMs covered for their patients to be denied, he added.
Welty also noted Congress is currently considering bills that address the lack of transparency in the way medications are reimbursed.
This new study doesn’t reveal what patients are paying for their medications, he said. “These data tell me the national average of the cost to the pharmacy, but don’t tell me what the patient is actually paying, or what the insurance companies are actually paying for these medications.”
A “hot topic” in the industry is the role of pharmacy benefit managers, who are contracted by health insurance companies to manage medication portfolios, in influencing drug prices.
Drug pricing is a complicated topic. “There’s a lot more behind this; this is just like a tip of the iceberg,” said Welty.
Also commenting, Jacqueline French, MD, professor, NYU Comprehensive Epilepsy Center, New York City, said the much higher ASM prices are “very problematic,” particularly for drugs that don’t have a generic.
“I wonder how much the drugs for orphan indications, which are usually higher priced, influenced the numbers.”
The good news, though, is that many people “can safely take generics if they’re available,” said French.
The investigators and Welty reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
LOS ANGELES — results of a new study showed.
These findings highlight an “urgent need” to examine ASM pricing, said study investigator Pradeep Javarayee, MD, MBA, assistant professor, Department of Neurology, Medical College of Wisconsin, Milwaukee.
“The price disparity between generic and brand-name anti-seizure medications is growing,” said Javarayee. “Understanding these trends is essential for clinicians to make cost-conscious prescribing decisions and to advocate for policies that ensure equitable access to treatment for patients with epilepsy.”
The findings were presented at American Epilepsy Society (AES) 78th Annual Meeting 2024.
Concerning Trends
Researchers analyzed prices of ASMs using National Average Drug Acquisition Cost (NADAC) data provided by the Centers for Medicare & Medicaid Services from November 2013 to July 2023.
A publicly available resource, NADAC is widely regarded as the most reliable benchmark for drug reimbursement in the United States, said Javarayee. It is based on the price/unit of Medicaid-covered outpatient drugs collected though monthly surveys of retail community pharmacies across the United States.
The database includes medication names, strengths, formulations, and National Drug Codes.
The study examined 23 US Food and Drug Administration–approved ASMs, encompassing 223 oral formulations, which included 112 brand-name and 111 generic products.
To account for inflation, researchers adjusted ASM prices using the Consumer Price Index for Medicinal Drugs–Seasonally Adjusted. They also explored the effects of the COVID-19 pandemic on drug pricing.
The study uncovered trends that Javarayee found concerning. For example, between 2013 and 2023, the average price of brand-name ASMs increased from $8.71 to $15.43, whereas the average price of generic ASMs decreased from $1.39 to $1.26.
Most generic ASMs remained in the low-cost range ($0-$0.25) during the study period, whereas the proportion of higher-priced brand-name ASMs ($10-$50) increased.
The number of brand-name ASMs with a mean price exceeding $15 rose from two (2013-2016) to six (2017-2019) and then to eight (2020-2023).
Unsustainable Price Increases
The study uncovered examples of what Javarayee called “extreme” price differences. For instance, matched brand-name and generic ASMs with price differences of 1000%-9999% increased from 32.88% in 2013-2016 to 41.43% in 2020-2023.
Among brand-name ASMs, cenobamate (Xcopri), which is approved in the United States for partial-onset seizures, had the highest mean price between 2020 and 2023 ($35.59). For generic ASMs, topiramate had the highest mean price in the same time period ($6.64).
Looking at formulation-based cost differences, the study found generic immediate-release formulations were significantly cheaper than extended-release or delayed-release counterparts, with cost differences reaching as high as 7751.20%.
The study also showed the COVID-19 pandemic led to a 24.4% increase in brand-name ASM prices and a 23.1% decrease in generic ASM prices.
The results underscore the need to raise awareness of drug pricing dynamics and call for targeted policy interventions to alleviate the rising cost burden on patients, said Javarayee.
He emphasized that such price increases are unsustainable. “Addressing these disparities is critical not only for improving patient adherence and outcomes but also for reducing the overall economic strain on the healthcare system.”
‘Tip of the Iceberg’
Reached for a comment, Tim Welty, a pharmacist in Des Moines, Iowa, who specializes in epilepsy drugs, agreed that the issue of medication costs needs to be addressed.
“I absolutely think physicians and others need to advocate for transparency in pricing,” he said. It’s not unusual for physician requests to have newer ASMs covered for their patients to be denied, he added.
Welty also noted Congress is currently considering bills that address the lack of transparency in the way medications are reimbursed.
This new study doesn’t reveal what patients are paying for their medications, he said. “These data tell me the national average of the cost to the pharmacy, but don’t tell me what the patient is actually paying, or what the insurance companies are actually paying for these medications.”
A “hot topic” in the industry is the role of pharmacy benefit managers, who are contracted by health insurance companies to manage medication portfolios, in influencing drug prices.
Drug pricing is a complicated topic. “There’s a lot more behind this; this is just like a tip of the iceberg,” said Welty.
Also commenting, Jacqueline French, MD, professor, NYU Comprehensive Epilepsy Center, New York City, said the much higher ASM prices are “very problematic,” particularly for drugs that don’t have a generic.
“I wonder how much the drugs for orphan indications, which are usually higher priced, influenced the numbers.”
The good news, though, is that many people “can safely take generics if they’re available,” said French.
The investigators and Welty reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM AES 2024
Women Largely Unaware of Anti-Seizure Med Risks, More Education Needed
LOS ANGELES — The majority of women with epilepsy are inadequately educated about the potential risks associated with anti-seizure medications (ASMs), which include teratogenicity and a reduction in the efficacy of hormonal birth control, early results of a new survey suggested.
In addition, only about a third of survey respondents indicated that they were taking folic acid if pregnant or planning to be or using an effective contraceptive if they wanted to avoid pregnancy.
“Physicians should see it as inside their scope to ask about the family planning aspect of things because it’s relevant to their patients’ neurologic care,” first study author Tori Valachovic, a fourth-year medical student at the University of Rochester School of Medicine, New York, told this news organization.
She noted patients may be taking ASMs not just for seizures but potentially to manage migraines or a mood disorder.
The findings were presented on December 8 at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Unique Survey
Research shows that about half of pregnancies in the United States are unplanned, and the number is even higher among people with epilepsy, said senior author Sarah Betstadt, MD, associate professor of obstetrics and gynecology, University of Rochester. That may be because women aren’t appropriately counseled about ASMs, possibly reducing the effectiveness of their hormonal birth control, she said.
The American Academy of Neurology recommends women with seizure disorders who could become pregnant receive yearly counseling about reproductive health, including ASM teratogenicity and interactions with hormonal contraceptive medications.
The study included 107 women aged 18-49 years at two general neurology outpatient clinics who were taking an ASM and completed a survey between July 2023 and May 2024. Of these, six were pregnant or planning to become pregnant, and 69 were using a barrier, hormonal, or implant form of contraception.
Researchers collected medical histories for each respondent, including how long they had had a seizure disorder, how often they experienced seizures, what anti-seizure drugs they were taking, the type of birth control they used, their pregnancy intentions, and whether they were taking folic acid.
The survey was unique in that questions were personalized. Previous surveys have asked general questions, but for the current survey, patients were required to input their specific ASM and specific birth control, so it was also a test of their knowledge of their specific medications, said Valachovic.
When responding to questions about the safety of their ASMs for pregnancy or whether there were interactions between ASMs and birth control, about two thirds (67.3%) of the participants answered at least one question incorrectly.
The study found 36.2% of those using a barrier, hormonal, or implant contraceptive answered at least one question incorrectly regarding whether their ASM decreased birth control effectiveness.
ASMs such as carbamazepine, phenytoin, phenobarbital, higher doses of topiramate (over 200 mg daily), and oxcarbazepine can make hormonal contraceptives such as pills, patches, and rings less effective, noted Valachovic.
There’s also a bidirectional relationship at play, she added. Hormonal contraceptives can make ASMs such as lamotrigine, valproate, zonisamide, and rufinamide less effective because they decrease the levels of the ASMs.
For questions specifically about the teratogenicity of their medications, about 56.1% of participants did not answer correctly.
ASMs that increase the risk for birth defects include valproic acid (a drug that would be at the top of the list), topiramate, carbamazepine, phenobarbital, and phenytoin, said Valachovic.
However, she added, “It’s a little bit more nuanced” than simply saying, “Don’t take this medication during pregnancy” because the first aim is to control seizures. “Uncontrolled seizures are more dangerous for the fetus and the expectant mother than any ASM,” she explained.
Neurologists and reproductive healthcare providers should work together to better disseminate relevant information to their female patients who could become pregnant, said Betstadt. “We need to have better ways to collaborate. And I think we have to start with educating neurologists,” who care for these women throughout their journey with epilepsy and who during that time may become pregnant.
They “should be talking to their patients annually about whether they plan to be pregnant,” so they can educate them and make them aware of dangers to the fetus with certain medications and the effect of ASMs on birth control, added Betstadt, whose practice focuses on complex family planning.
“Our hope is that patients will have better care that’s in line with their reproductive goals,” she said.
No Trickle-Down Effect
Commenting for this news organization, Alison M. Pack, MD, professor of neurology and Epilepsy Division Chief, Columbia University, New York City, said the study underlines an important quandary: Despite guidelines on risks of combining ASMs and hormonal birth control, this information doesn’t seem to be “trickling down” to women with epilepsy.
“I think part of it is just the state of healthcare delivery these days,” where clinicians are expected to accomplish more and more within a 20-30–minute follow-up visit. It’s tough, too, to keep up with all the potential drug interactions involved with newer ASMs, she said.
“I also think it speaks to the complexity” of healthcare for young women with epilepsy, which involves not just neurologists but obstetricians, gynecologists, and primary care doctors, she added.
Pack doesn’t think epilepsy specialists “integrate” enough with these other specialties. “You need to communicate with the gynecologist; you need to open that line of communication.”
She believes advanced practice providers could play a role in reducing the complexity of treating young women with epilepsy by regularly reviewing how patients are adhering to recommended protocols.
But she pointed out that “in the overall picture, most women with epilepsy do have normal, healthy pregnancies.”
The investigators and Pack reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
LOS ANGELES — The majority of women with epilepsy are inadequately educated about the potential risks associated with anti-seizure medications (ASMs), which include teratogenicity and a reduction in the efficacy of hormonal birth control, early results of a new survey suggested.
In addition, only about a third of survey respondents indicated that they were taking folic acid if pregnant or planning to be or using an effective contraceptive if they wanted to avoid pregnancy.
“Physicians should see it as inside their scope to ask about the family planning aspect of things because it’s relevant to their patients’ neurologic care,” first study author Tori Valachovic, a fourth-year medical student at the University of Rochester School of Medicine, New York, told this news organization.
She noted patients may be taking ASMs not just for seizures but potentially to manage migraines or a mood disorder.
The findings were presented on December 8 at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Unique Survey
Research shows that about half of pregnancies in the United States are unplanned, and the number is even higher among people with epilepsy, said senior author Sarah Betstadt, MD, associate professor of obstetrics and gynecology, University of Rochester. That may be because women aren’t appropriately counseled about ASMs, possibly reducing the effectiveness of their hormonal birth control, she said.
The American Academy of Neurology recommends women with seizure disorders who could become pregnant receive yearly counseling about reproductive health, including ASM teratogenicity and interactions with hormonal contraceptive medications.
The study included 107 women aged 18-49 years at two general neurology outpatient clinics who were taking an ASM and completed a survey between July 2023 and May 2024. Of these, six were pregnant or planning to become pregnant, and 69 were using a barrier, hormonal, or implant form of contraception.
Researchers collected medical histories for each respondent, including how long they had had a seizure disorder, how often they experienced seizures, what anti-seizure drugs they were taking, the type of birth control they used, their pregnancy intentions, and whether they were taking folic acid.
The survey was unique in that questions were personalized. Previous surveys have asked general questions, but for the current survey, patients were required to input their specific ASM and specific birth control, so it was also a test of their knowledge of their specific medications, said Valachovic.
When responding to questions about the safety of their ASMs for pregnancy or whether there were interactions between ASMs and birth control, about two thirds (67.3%) of the participants answered at least one question incorrectly.
The study found 36.2% of those using a barrier, hormonal, or implant contraceptive answered at least one question incorrectly regarding whether their ASM decreased birth control effectiveness.
ASMs such as carbamazepine, phenytoin, phenobarbital, higher doses of topiramate (over 200 mg daily), and oxcarbazepine can make hormonal contraceptives such as pills, patches, and rings less effective, noted Valachovic.
There’s also a bidirectional relationship at play, she added. Hormonal contraceptives can make ASMs such as lamotrigine, valproate, zonisamide, and rufinamide less effective because they decrease the levels of the ASMs.
For questions specifically about the teratogenicity of their medications, about 56.1% of participants did not answer correctly.
ASMs that increase the risk for birth defects include valproic acid (a drug that would be at the top of the list), topiramate, carbamazepine, phenobarbital, and phenytoin, said Valachovic.
However, she added, “It’s a little bit more nuanced” than simply saying, “Don’t take this medication during pregnancy” because the first aim is to control seizures. “Uncontrolled seizures are more dangerous for the fetus and the expectant mother than any ASM,” she explained.
Neurologists and reproductive healthcare providers should work together to better disseminate relevant information to their female patients who could become pregnant, said Betstadt. “We need to have better ways to collaborate. And I think we have to start with educating neurologists,” who care for these women throughout their journey with epilepsy and who during that time may become pregnant.
They “should be talking to their patients annually about whether they plan to be pregnant,” so they can educate them and make them aware of dangers to the fetus with certain medications and the effect of ASMs on birth control, added Betstadt, whose practice focuses on complex family planning.
“Our hope is that patients will have better care that’s in line with their reproductive goals,” she said.
No Trickle-Down Effect
Commenting for this news organization, Alison M. Pack, MD, professor of neurology and Epilepsy Division Chief, Columbia University, New York City, said the study underlines an important quandary: Despite guidelines on risks of combining ASMs and hormonal birth control, this information doesn’t seem to be “trickling down” to women with epilepsy.
“I think part of it is just the state of healthcare delivery these days,” where clinicians are expected to accomplish more and more within a 20-30–minute follow-up visit. It’s tough, too, to keep up with all the potential drug interactions involved with newer ASMs, she said.
“I also think it speaks to the complexity” of healthcare for young women with epilepsy, which involves not just neurologists but obstetricians, gynecologists, and primary care doctors, she added.
Pack doesn’t think epilepsy specialists “integrate” enough with these other specialties. “You need to communicate with the gynecologist; you need to open that line of communication.”
She believes advanced practice providers could play a role in reducing the complexity of treating young women with epilepsy by regularly reviewing how patients are adhering to recommended protocols.
But she pointed out that “in the overall picture, most women with epilepsy do have normal, healthy pregnancies.”
The investigators and Pack reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
LOS ANGELES — The majority of women with epilepsy are inadequately educated about the potential risks associated with anti-seizure medications (ASMs), which include teratogenicity and a reduction in the efficacy of hormonal birth control, early results of a new survey suggested.
In addition, only about a third of survey respondents indicated that they were taking folic acid if pregnant or planning to be or using an effective contraceptive if they wanted to avoid pregnancy.
“Physicians should see it as inside their scope to ask about the family planning aspect of things because it’s relevant to their patients’ neurologic care,” first study author Tori Valachovic, a fourth-year medical student at the University of Rochester School of Medicine, New York, told this news organization.
She noted patients may be taking ASMs not just for seizures but potentially to manage migraines or a mood disorder.
The findings were presented on December 8 at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Unique Survey
Research shows that about half of pregnancies in the United States are unplanned, and the number is even higher among people with epilepsy, said senior author Sarah Betstadt, MD, associate professor of obstetrics and gynecology, University of Rochester. That may be because women aren’t appropriately counseled about ASMs, possibly reducing the effectiveness of their hormonal birth control, she said.
The American Academy of Neurology recommends women with seizure disorders who could become pregnant receive yearly counseling about reproductive health, including ASM teratogenicity and interactions with hormonal contraceptive medications.
The study included 107 women aged 18-49 years at two general neurology outpatient clinics who were taking an ASM and completed a survey between July 2023 and May 2024. Of these, six were pregnant or planning to become pregnant, and 69 were using a barrier, hormonal, or implant form of contraception.
Researchers collected medical histories for each respondent, including how long they had had a seizure disorder, how often they experienced seizures, what anti-seizure drugs they were taking, the type of birth control they used, their pregnancy intentions, and whether they were taking folic acid.
The survey was unique in that questions were personalized. Previous surveys have asked general questions, but for the current survey, patients were required to input their specific ASM and specific birth control, so it was also a test of their knowledge of their specific medications, said Valachovic.
When responding to questions about the safety of their ASMs for pregnancy or whether there were interactions between ASMs and birth control, about two thirds (67.3%) of the participants answered at least one question incorrectly.
The study found 36.2% of those using a barrier, hormonal, or implant contraceptive answered at least one question incorrectly regarding whether their ASM decreased birth control effectiveness.
ASMs such as carbamazepine, phenytoin, phenobarbital, higher doses of topiramate (over 200 mg daily), and oxcarbazepine can make hormonal contraceptives such as pills, patches, and rings less effective, noted Valachovic.
There’s also a bidirectional relationship at play, she added. Hormonal contraceptives can make ASMs such as lamotrigine, valproate, zonisamide, and rufinamide less effective because they decrease the levels of the ASMs.
For questions specifically about the teratogenicity of their medications, about 56.1% of participants did not answer correctly.
ASMs that increase the risk for birth defects include valproic acid (a drug that would be at the top of the list), topiramate, carbamazepine, phenobarbital, and phenytoin, said Valachovic.
However, she added, “It’s a little bit more nuanced” than simply saying, “Don’t take this medication during pregnancy” because the first aim is to control seizures. “Uncontrolled seizures are more dangerous for the fetus and the expectant mother than any ASM,” she explained.
Neurologists and reproductive healthcare providers should work together to better disseminate relevant information to their female patients who could become pregnant, said Betstadt. “We need to have better ways to collaborate. And I think we have to start with educating neurologists,” who care for these women throughout their journey with epilepsy and who during that time may become pregnant.
They “should be talking to their patients annually about whether they plan to be pregnant,” so they can educate them and make them aware of dangers to the fetus with certain medications and the effect of ASMs on birth control, added Betstadt, whose practice focuses on complex family planning.
“Our hope is that patients will have better care that’s in line with their reproductive goals,” she said.
No Trickle-Down Effect
Commenting for this news organization, Alison M. Pack, MD, professor of neurology and Epilepsy Division Chief, Columbia University, New York City, said the study underlines an important quandary: Despite guidelines on risks of combining ASMs and hormonal birth control, this information doesn’t seem to be “trickling down” to women with epilepsy.
“I think part of it is just the state of healthcare delivery these days,” where clinicians are expected to accomplish more and more within a 20-30–minute follow-up visit. It’s tough, too, to keep up with all the potential drug interactions involved with newer ASMs, she said.
“I also think it speaks to the complexity” of healthcare for young women with epilepsy, which involves not just neurologists but obstetricians, gynecologists, and primary care doctors, she added.
Pack doesn’t think epilepsy specialists “integrate” enough with these other specialties. “You need to communicate with the gynecologist; you need to open that line of communication.”
She believes advanced practice providers could play a role in reducing the complexity of treating young women with epilepsy by regularly reviewing how patients are adhering to recommended protocols.
But she pointed out that “in the overall picture, most women with epilepsy do have normal, healthy pregnancies.”
The investigators and Pack reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM AES 2024
Few Focal Epilepsy Cases Controlled by Initial ASM Treatment
LOS ANGELES — Only about 27% of patients newly diagnosed with focal epilepsy are seizure-free on initial anti-seizure medications (ASMs), new research suggested.
This is sobering information to pass on to patients with focal epilepsy who may have high expectations based on prior data. “Patients tend to expect things to happen quickly, said study investigator Sarah Barnard, MD, a research fellow at the School of Translational Medicine, Monash University, Melbourne, Australia.
The study was presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
An International Collaboration
The study is part of the International Human Epilepsy Project (HEP), which focuses on new-onset focal epilepsy, one of the most common forms of the disorder. The researchers are aiming to identify factors that influence treatment response in this population.
For example, they will investigate how specific medications and coexisting conditions affect treatment outcomes. Ultimately, the goal is to enable the development of individualized treatment plans for patients, leading to faster and more effective improvements or potential cures for the condition.
“The investigators wanted to focus in on focal epilepsy and exclude patients with more severe phenotypes, such as those with developmental delays or significant brain injury,” said Barnard. Individuals with focal epilepsy are generally healthy, she added.
In addition, previous studies may have used differing definitions of seizure freedom, said Barnard.
The study included 448 patients, median age about 33 years and 60% women, with focal epilepsy who were enrolled at 34 tertiary epilepsy centers in the United States, Europe, and Australia within 4 months of initiating ASM treatment.
Participants were followed for up to 6 years (the median was 3.13 years). The median age at seizure onset was 29 years, and the median age of treatment initiation was 32 years. The most common first-line ASMs were levetiracetam (56.9%) and lamotrigine (16.5%).
Researchers used updated International League Against Epilepsy definitions. Seizure freedom is defined as no seizures for 12 months or three times the longest pretreatment seizure-free interval, whichever is longer.
Results showed that only 27% of patients were seizure-free in the first year after diagnosis even accounting for a 2-month “medication adjustment” period.
Managing Expectations
Although the study excluded individuals with more severe types of epilepsy, “we still identified a substantial proportion of treatment-resistant cases, suggesting that much more complex factors are at play,” said Jacqueline French, MD, a study coinvestigator and professor at the NYU Langone’s Comprehensive Epilepsy Center in New York City.
“I don’t think we adequately prepare our patients for the challenges of the first year, which can be quite turbulent,” French said.
However, the seizure freedom rate in this study is lower than previous estimates. “It’s much less than what was predicted in other studies, some of which quote around 50%-55% seizure freedom on the first ASM,” said Barnard.
It’s not clear why there’s such a difference, although it may be related to a predominance in the HEP study of patients taking levetiracetam as the first-line ASM. “We didn’t directly look at the rate of treatment response or seizure freedom on levetiracetam,” which is something that will be addressed in a follow-up study, Barnard added.
The difference could be due to the study including only focal epilepsy patients, “who usually have a different treatment regime,” or it could be related to using updated definitions in this study, she said.
Results also showed that patients are at high risk during the first year of treatment, with two thirds experiencing ongoing or worsening seizures during this period. “People have ongoing seizures for the first year, even if they go on to become seizure-free,” Barnard noted.
Experiencing ongoing seizures has potential implications for driving and for employment, she added.
A self-reported history of a psychological disorder was a risk factor for increased treatment resistance. Upon enrollment, each participant completed the Mini International Neuropsychiatric Interview, which Barnard said is a diagnostic, rather than a screening, tool.
One of the team’s next research steps is to look more closely at the role of depression, anxiety, bipolar disorder, and suicidality on treatment response in this patient population, said Barnard.
Important for Patient Counseling
Commenting on the research, Patrick Kwan, MD, PhD, professor, Department of Neuroscience, Monash University, said the research is “very important” in terms of patient counseling.
“For someone newly diagnosed with epilepsy, starting the first medication can be both daunting and confusing, with many uncertainties,” said Kwan. “That’s why it’s valuable to know that nearly a third of patients may not respond to initial treatment.”
He noted that the patients in the study were recruited from major centers, which could attract a specific subset of individuals. “It’s possible that this patient population might represent more severe cases,” he explained.
Kwan also emphasized that the study did not examine the “patterns” of prescription drug choices, adding that he agreed this should be addressed in future analyses.
The researchers and Kwan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
LOS ANGELES — Only about 27% of patients newly diagnosed with focal epilepsy are seizure-free on initial anti-seizure medications (ASMs), new research suggested.
This is sobering information to pass on to patients with focal epilepsy who may have high expectations based on prior data. “Patients tend to expect things to happen quickly, said study investigator Sarah Barnard, MD, a research fellow at the School of Translational Medicine, Monash University, Melbourne, Australia.
The study was presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
An International Collaboration
The study is part of the International Human Epilepsy Project (HEP), which focuses on new-onset focal epilepsy, one of the most common forms of the disorder. The researchers are aiming to identify factors that influence treatment response in this population.
For example, they will investigate how specific medications and coexisting conditions affect treatment outcomes. Ultimately, the goal is to enable the development of individualized treatment plans for patients, leading to faster and more effective improvements or potential cures for the condition.
“The investigators wanted to focus in on focal epilepsy and exclude patients with more severe phenotypes, such as those with developmental delays or significant brain injury,” said Barnard. Individuals with focal epilepsy are generally healthy, she added.
In addition, previous studies may have used differing definitions of seizure freedom, said Barnard.
The study included 448 patients, median age about 33 years and 60% women, with focal epilepsy who were enrolled at 34 tertiary epilepsy centers in the United States, Europe, and Australia within 4 months of initiating ASM treatment.
Participants were followed for up to 6 years (the median was 3.13 years). The median age at seizure onset was 29 years, and the median age of treatment initiation was 32 years. The most common first-line ASMs were levetiracetam (56.9%) and lamotrigine (16.5%).
Researchers used updated International League Against Epilepsy definitions. Seizure freedom is defined as no seizures for 12 months or three times the longest pretreatment seizure-free interval, whichever is longer.
Results showed that only 27% of patients were seizure-free in the first year after diagnosis even accounting for a 2-month “medication adjustment” period.
Managing Expectations
Although the study excluded individuals with more severe types of epilepsy, “we still identified a substantial proportion of treatment-resistant cases, suggesting that much more complex factors are at play,” said Jacqueline French, MD, a study coinvestigator and professor at the NYU Langone’s Comprehensive Epilepsy Center in New York City.
“I don’t think we adequately prepare our patients for the challenges of the first year, which can be quite turbulent,” French said.
However, the seizure freedom rate in this study is lower than previous estimates. “It’s much less than what was predicted in other studies, some of which quote around 50%-55% seizure freedom on the first ASM,” said Barnard.
It’s not clear why there’s such a difference, although it may be related to a predominance in the HEP study of patients taking levetiracetam as the first-line ASM. “We didn’t directly look at the rate of treatment response or seizure freedom on levetiracetam,” which is something that will be addressed in a follow-up study, Barnard added.
The difference could be due to the study including only focal epilepsy patients, “who usually have a different treatment regime,” or it could be related to using updated definitions in this study, she said.
Results also showed that patients are at high risk during the first year of treatment, with two thirds experiencing ongoing or worsening seizures during this period. “People have ongoing seizures for the first year, even if they go on to become seizure-free,” Barnard noted.
Experiencing ongoing seizures has potential implications for driving and for employment, she added.
A self-reported history of a psychological disorder was a risk factor for increased treatment resistance. Upon enrollment, each participant completed the Mini International Neuropsychiatric Interview, which Barnard said is a diagnostic, rather than a screening, tool.
One of the team’s next research steps is to look more closely at the role of depression, anxiety, bipolar disorder, and suicidality on treatment response in this patient population, said Barnard.
Important for Patient Counseling
Commenting on the research, Patrick Kwan, MD, PhD, professor, Department of Neuroscience, Monash University, said the research is “very important” in terms of patient counseling.
“For someone newly diagnosed with epilepsy, starting the first medication can be both daunting and confusing, with many uncertainties,” said Kwan. “That’s why it’s valuable to know that nearly a third of patients may not respond to initial treatment.”
He noted that the patients in the study were recruited from major centers, which could attract a specific subset of individuals. “It’s possible that this patient population might represent more severe cases,” he explained.
Kwan also emphasized that the study did not examine the “patterns” of prescription drug choices, adding that he agreed this should be addressed in future analyses.
The researchers and Kwan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
LOS ANGELES — Only about 27% of patients newly diagnosed with focal epilepsy are seizure-free on initial anti-seizure medications (ASMs), new research suggested.
This is sobering information to pass on to patients with focal epilepsy who may have high expectations based on prior data. “Patients tend to expect things to happen quickly, said study investigator Sarah Barnard, MD, a research fellow at the School of Translational Medicine, Monash University, Melbourne, Australia.
The study was presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
An International Collaboration
The study is part of the International Human Epilepsy Project (HEP), which focuses on new-onset focal epilepsy, one of the most common forms of the disorder. The researchers are aiming to identify factors that influence treatment response in this population.
For example, they will investigate how specific medications and coexisting conditions affect treatment outcomes. Ultimately, the goal is to enable the development of individualized treatment plans for patients, leading to faster and more effective improvements or potential cures for the condition.
“The investigators wanted to focus in on focal epilepsy and exclude patients with more severe phenotypes, such as those with developmental delays or significant brain injury,” said Barnard. Individuals with focal epilepsy are generally healthy, she added.
In addition, previous studies may have used differing definitions of seizure freedom, said Barnard.
The study included 448 patients, median age about 33 years and 60% women, with focal epilepsy who were enrolled at 34 tertiary epilepsy centers in the United States, Europe, and Australia within 4 months of initiating ASM treatment.
Participants were followed for up to 6 years (the median was 3.13 years). The median age at seizure onset was 29 years, and the median age of treatment initiation was 32 years. The most common first-line ASMs were levetiracetam (56.9%) and lamotrigine (16.5%).
Researchers used updated International League Against Epilepsy definitions. Seizure freedom is defined as no seizures for 12 months or three times the longest pretreatment seizure-free interval, whichever is longer.
Results showed that only 27% of patients were seizure-free in the first year after diagnosis even accounting for a 2-month “medication adjustment” period.
Managing Expectations
Although the study excluded individuals with more severe types of epilepsy, “we still identified a substantial proportion of treatment-resistant cases, suggesting that much more complex factors are at play,” said Jacqueline French, MD, a study coinvestigator and professor at the NYU Langone’s Comprehensive Epilepsy Center in New York City.
“I don’t think we adequately prepare our patients for the challenges of the first year, which can be quite turbulent,” French said.
However, the seizure freedom rate in this study is lower than previous estimates. “It’s much less than what was predicted in other studies, some of which quote around 50%-55% seizure freedom on the first ASM,” said Barnard.
It’s not clear why there’s such a difference, although it may be related to a predominance in the HEP study of patients taking levetiracetam as the first-line ASM. “We didn’t directly look at the rate of treatment response or seizure freedom on levetiracetam,” which is something that will be addressed in a follow-up study, Barnard added.
The difference could be due to the study including only focal epilepsy patients, “who usually have a different treatment regime,” or it could be related to using updated definitions in this study, she said.
Results also showed that patients are at high risk during the first year of treatment, with two thirds experiencing ongoing or worsening seizures during this period. “People have ongoing seizures for the first year, even if they go on to become seizure-free,” Barnard noted.
Experiencing ongoing seizures has potential implications for driving and for employment, she added.
A self-reported history of a psychological disorder was a risk factor for increased treatment resistance. Upon enrollment, each participant completed the Mini International Neuropsychiatric Interview, which Barnard said is a diagnostic, rather than a screening, tool.
One of the team’s next research steps is to look more closely at the role of depression, anxiety, bipolar disorder, and suicidality on treatment response in this patient population, said Barnard.
Important for Patient Counseling
Commenting on the research, Patrick Kwan, MD, PhD, professor, Department of Neuroscience, Monash University, said the research is “very important” in terms of patient counseling.
“For someone newly diagnosed with epilepsy, starting the first medication can be both daunting and confusing, with many uncertainties,” said Kwan. “That’s why it’s valuable to know that nearly a third of patients may not respond to initial treatment.”
He noted that the patients in the study were recruited from major centers, which could attract a specific subset of individuals. “It’s possible that this patient population might represent more severe cases,” he explained.
Kwan also emphasized that the study did not examine the “patterns” of prescription drug choices, adding that he agreed this should be addressed in future analyses.
The researchers and Kwan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AES 2024
Smart Mattress to Reduce SUDEP?
LOS ANGELES — says one of the experts involved in its development.
When used along with a seizure detection device, Jong Woo Lee, MD, PhD, associate professor of neurology, Harvard Medical School, and Brigham and Women’s Hospital, both in Boston, Massachusetts, estimates the smart mattress could cut SUDEP by more than 50%.
In addition, early results from an observational study are backing this up, he said.
The findings were presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Most SUDEP Cases Found Face Down
SUDEP is the leading cause of death in children with epilepsy and in otherwise healthy adult patients with epilepsy. When his fifth patient died of SUDEP, Lee decided it was time to try to tackle the high mortality rate associated with these unexpected deaths. “I desperately wanted to help, ” he said.
About 70% of SUDEP occurs during sleep, and victims are found face down, or in the prone position, 90% of the time, said Lee.
“Of course, the best way to prevent SUDEP is not to have a seizure, but once you have a seizure and once you’re face down, your risk for death goes up by somewhere between 30 and 100 times,” he explained.
Lee was convinced SUDEP could be prevented by simple interventions that stimulate the patient and turn them over. He noted the incidence of sudden infant death syndrome, “which has similar characteristics” to SUDEP, has been reduced by up to 75% through campaigns that simply advise placing babies on their backs.
“Most of SUDEP happens because your arousal system is knocked out and you just don’t take the breath that you’re supposed to. Just the act of turning people over and vibrating the bed will stimulate them,” he said.
However, it’s crucial that this be done quickly, said Lee. “When you look at patients who died on video and see the EEGs, everybody took their last breath within 3 minutes.”
Because the window of opportunity is so short, “we think that seizure detection devices alone are not going to really be effective because you just can’t get there or react within those 3 minutes.”
There are currently no products that detect the prone position or have the ability to reposition a patient quickly into the recovery sideways position.
Lee and his colleagues developed a smart system that can be embedded in a mattress that detects when someone is having a seizure, determines if that person is face down, and if so, safely stimulates and repositions them.
The mattress is made up of a series of programmable inflatable blocks or “cells” that have pressure, vibration, temperature, and humidity sensors embedded within. “Based on the pressure readings, we can figure out whether the patient is right side up, on their right side, on their left side, or face down,” said Lee.
If the person is face down, he or she can be repositioned within a matter of seconds. “Each of the cells can lift 1000 pounds,” he said. The mattress is “very comfortable,” said Lee, who has tried it out himself.
Eighteen normative control participants have been enrolled for development and training purposes. To date, 10 of these individuals, aged 18-53 years, weighing 100-182 lb, and with a height of 5 ft 2 in to 6 ft 1 in, underwent extensive formal testing on the prototype bed.
Researchers found the mattress responded quickly to different body positions and weights. “We were able to reposition everybody in around 20 seconds,” said Lee.
The overall accuracy of detecting the prone position was 96.8%. There were no cases of a supine or prone position being mistaken for each other.
Researchers are refining the algorithm to improve the accuracy for detecting the prone position and expect to have a completely functional prototype within a few years.
Big Step Forward
Commenting on the research, Daniel M. Goldenholz, MD, PhD, assistant professor, Division of Epilepsy, Harvard Beth Israel Deaconess Medical Center, Boston, said the study “is a big step forward in the race to provide an actionable tool to prevent SUDEP.”
The technology “appears to mostly be doing what it’s intended to do, with relatively minor technical errors being made,” he said.
However, it is not clear if this technology can truly save lives, said Goldenholz. “The data we have suggests that lying face down in bed after a seizure is correlated with SUDEP, but that does not mean that if we can simply flip people over, they for sure won’t die.”
Even if the new technology “works perfectly,” it’s still an open question, said Goldenholz. If it does save lives, “this will be a major breakthrough, and one that has been needed for a long time.”
However, even if it does not, he congratulates the team for trying to determine if reducing the prone position can help prevent SUDEP. He would like to see more “high-risk, high-reward” studies in the epilepsy field. “We are in so much need of new innovations.”
He said he was “personally very inspired” by this work. “People are dying from this terrible disease, and this team is building what they hope might save lives.”
The study was funded by the National Institutes of Health. The mattress is being developed by Soterya. Lee reported no equity in Soterya. Goldenholz reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
LOS ANGELES — says one of the experts involved in its development.
When used along with a seizure detection device, Jong Woo Lee, MD, PhD, associate professor of neurology, Harvard Medical School, and Brigham and Women’s Hospital, both in Boston, Massachusetts, estimates the smart mattress could cut SUDEP by more than 50%.
In addition, early results from an observational study are backing this up, he said.
The findings were presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Most SUDEP Cases Found Face Down
SUDEP is the leading cause of death in children with epilepsy and in otherwise healthy adult patients with epilepsy. When his fifth patient died of SUDEP, Lee decided it was time to try to tackle the high mortality rate associated with these unexpected deaths. “I desperately wanted to help, ” he said.
About 70% of SUDEP occurs during sleep, and victims are found face down, or in the prone position, 90% of the time, said Lee.
“Of course, the best way to prevent SUDEP is not to have a seizure, but once you have a seizure and once you’re face down, your risk for death goes up by somewhere between 30 and 100 times,” he explained.
Lee was convinced SUDEP could be prevented by simple interventions that stimulate the patient and turn them over. He noted the incidence of sudden infant death syndrome, “which has similar characteristics” to SUDEP, has been reduced by up to 75% through campaigns that simply advise placing babies on their backs.
“Most of SUDEP happens because your arousal system is knocked out and you just don’t take the breath that you’re supposed to. Just the act of turning people over and vibrating the bed will stimulate them,” he said.
However, it’s crucial that this be done quickly, said Lee. “When you look at patients who died on video and see the EEGs, everybody took their last breath within 3 minutes.”
Because the window of opportunity is so short, “we think that seizure detection devices alone are not going to really be effective because you just can’t get there or react within those 3 minutes.”
There are currently no products that detect the prone position or have the ability to reposition a patient quickly into the recovery sideways position.
Lee and his colleagues developed a smart system that can be embedded in a mattress that detects when someone is having a seizure, determines if that person is face down, and if so, safely stimulates and repositions them.
The mattress is made up of a series of programmable inflatable blocks or “cells” that have pressure, vibration, temperature, and humidity sensors embedded within. “Based on the pressure readings, we can figure out whether the patient is right side up, on their right side, on their left side, or face down,” said Lee.
If the person is face down, he or she can be repositioned within a matter of seconds. “Each of the cells can lift 1000 pounds,” he said. The mattress is “very comfortable,” said Lee, who has tried it out himself.
Eighteen normative control participants have been enrolled for development and training purposes. To date, 10 of these individuals, aged 18-53 years, weighing 100-182 lb, and with a height of 5 ft 2 in to 6 ft 1 in, underwent extensive formal testing on the prototype bed.
Researchers found the mattress responded quickly to different body positions and weights. “We were able to reposition everybody in around 20 seconds,” said Lee.
The overall accuracy of detecting the prone position was 96.8%. There were no cases of a supine or prone position being mistaken for each other.
Researchers are refining the algorithm to improve the accuracy for detecting the prone position and expect to have a completely functional prototype within a few years.
Big Step Forward
Commenting on the research, Daniel M. Goldenholz, MD, PhD, assistant professor, Division of Epilepsy, Harvard Beth Israel Deaconess Medical Center, Boston, said the study “is a big step forward in the race to provide an actionable tool to prevent SUDEP.”
The technology “appears to mostly be doing what it’s intended to do, with relatively minor technical errors being made,” he said.
However, it is not clear if this technology can truly save lives, said Goldenholz. “The data we have suggests that lying face down in bed after a seizure is correlated with SUDEP, but that does not mean that if we can simply flip people over, they for sure won’t die.”
Even if the new technology “works perfectly,” it’s still an open question, said Goldenholz. If it does save lives, “this will be a major breakthrough, and one that has been needed for a long time.”
However, even if it does not, he congratulates the team for trying to determine if reducing the prone position can help prevent SUDEP. He would like to see more “high-risk, high-reward” studies in the epilepsy field. “We are in so much need of new innovations.”
He said he was “personally very inspired” by this work. “People are dying from this terrible disease, and this team is building what they hope might save lives.”
The study was funded by the National Institutes of Health. The mattress is being developed by Soterya. Lee reported no equity in Soterya. Goldenholz reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
LOS ANGELES — says one of the experts involved in its development.
When used along with a seizure detection device, Jong Woo Lee, MD, PhD, associate professor of neurology, Harvard Medical School, and Brigham and Women’s Hospital, both in Boston, Massachusetts, estimates the smart mattress could cut SUDEP by more than 50%.
In addition, early results from an observational study are backing this up, he said.
The findings were presented at the American Epilepsy Society (AES) 78th Annual Meeting 2024.
Most SUDEP Cases Found Face Down
SUDEP is the leading cause of death in children with epilepsy and in otherwise healthy adult patients with epilepsy. When his fifth patient died of SUDEP, Lee decided it was time to try to tackle the high mortality rate associated with these unexpected deaths. “I desperately wanted to help, ” he said.
About 70% of SUDEP occurs during sleep, and victims are found face down, or in the prone position, 90% of the time, said Lee.
“Of course, the best way to prevent SUDEP is not to have a seizure, but once you have a seizure and once you’re face down, your risk for death goes up by somewhere between 30 and 100 times,” he explained.
Lee was convinced SUDEP could be prevented by simple interventions that stimulate the patient and turn them over. He noted the incidence of sudden infant death syndrome, “which has similar characteristics” to SUDEP, has been reduced by up to 75% through campaigns that simply advise placing babies on their backs.
“Most of SUDEP happens because your arousal system is knocked out and you just don’t take the breath that you’re supposed to. Just the act of turning people over and vibrating the bed will stimulate them,” he said.
However, it’s crucial that this be done quickly, said Lee. “When you look at patients who died on video and see the EEGs, everybody took their last breath within 3 minutes.”
Because the window of opportunity is so short, “we think that seizure detection devices alone are not going to really be effective because you just can’t get there or react within those 3 minutes.”
There are currently no products that detect the prone position or have the ability to reposition a patient quickly into the recovery sideways position.
Lee and his colleagues developed a smart system that can be embedded in a mattress that detects when someone is having a seizure, determines if that person is face down, and if so, safely stimulates and repositions them.
The mattress is made up of a series of programmable inflatable blocks or “cells” that have pressure, vibration, temperature, and humidity sensors embedded within. “Based on the pressure readings, we can figure out whether the patient is right side up, on their right side, on their left side, or face down,” said Lee.
If the person is face down, he or she can be repositioned within a matter of seconds. “Each of the cells can lift 1000 pounds,” he said. The mattress is “very comfortable,” said Lee, who has tried it out himself.
Eighteen normative control participants have been enrolled for development and training purposes. To date, 10 of these individuals, aged 18-53 years, weighing 100-182 lb, and with a height of 5 ft 2 in to 6 ft 1 in, underwent extensive formal testing on the prototype bed.
Researchers found the mattress responded quickly to different body positions and weights. “We were able to reposition everybody in around 20 seconds,” said Lee.
The overall accuracy of detecting the prone position was 96.8%. There were no cases of a supine or prone position being mistaken for each other.
Researchers are refining the algorithm to improve the accuracy for detecting the prone position and expect to have a completely functional prototype within a few years.
Big Step Forward
Commenting on the research, Daniel M. Goldenholz, MD, PhD, assistant professor, Division of Epilepsy, Harvard Beth Israel Deaconess Medical Center, Boston, said the study “is a big step forward in the race to provide an actionable tool to prevent SUDEP.”
The technology “appears to mostly be doing what it’s intended to do, with relatively minor technical errors being made,” he said.
However, it is not clear if this technology can truly save lives, said Goldenholz. “The data we have suggests that lying face down in bed after a seizure is correlated with SUDEP, but that does not mean that if we can simply flip people over, they for sure won’t die.”
Even if the new technology “works perfectly,” it’s still an open question, said Goldenholz. If it does save lives, “this will be a major breakthrough, and one that has been needed for a long time.”
However, even if it does not, he congratulates the team for trying to determine if reducing the prone position can help prevent SUDEP. He would like to see more “high-risk, high-reward” studies in the epilepsy field. “We are in so much need of new innovations.”
He said he was “personally very inspired” by this work. “People are dying from this terrible disease, and this team is building what they hope might save lives.”
The study was funded by the National Institutes of Health. The mattress is being developed by Soterya. Lee reported no equity in Soterya. Goldenholz reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM AES 2024