User login
ORLANDO – Assessment, education, and a judicious dose of medication can make a big difference to patients who are feeling anxious about undergoing Mohs surgery.
No studies or guidelines lay out a step-by-step management plan for anxious patients. But a little bit of common sense and empathy go a long way in easing the feeling, according to presenters at the annual meeting of the American College of Mohs Surgery.
“We don’t have an algorithm for reducing anxiety,” said Dr. Joseph Sobanko of the University of Pennsylvania, Philadelphia. “But we do have a lot of studies showing that better psychosocial health is related to better surgical outcomes.”
The lack of definitive guidance means that anxious patients might be identified and assessed by gut instinct, he continued. “Those of you who see patients probably have a gestalt technique of identifying the anxious ones. I would suggest this might not be the best way.”
Instead of guessing, he recommends assessing all patients with a validated screening tool, and dealing with anxiety proactively.
Assessing anxiety
Although anxiety assessment may not be part of a typical Mohs surgery intake, it probably should be, Dr. Sobanko said. There are a number of excellent, well-validated tools, and none of them require expertise in psychology to administer.
The Beck Anxiety Inventory is a 21-question index that takes about 10 minutes to complete. It assesses subjective, somatic, and panic-related symptoms of anxiety, and has been validated in a variety of clinical settings. It focuses quite a bit on strong physical symptoms, however, which Dr. Sobanko feels “may not be as relevant for our patients.”
The State-Trait Anxiety Inventory consists of 40 questions and takes about 15 minutes to complete. “I like it because it not only assesses how they generally feel, but how they feel at the moment,” he said. “We think it’s good and we do use it, but it takes a while to complete.”
The Hospital Anxiety and Depression Scale is short, with only 14 questions, and takes only about 5 minutes to complete. “It’s validated for hospital patients, but we are often working with patients who are less sick than that,” Dr. Sobanko said.
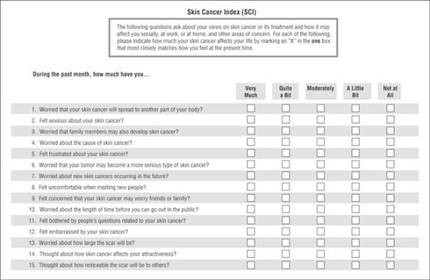
The Skin Cancer Index is his go-to anxiety screen for Mohs patients. It includes 15 questions that “really get to the heart of things that matter to our patients: emotional, social, and appearance issues,” he noted. Created in 2006, it was validated in a large cohort of Mohs surgery patients (Arch Facial Plast Surg. 2006;8[5]:314-318). The questions probe patients’ feelings about the seriousness of their skin cancer, its long-term health effect, and the impact the lesion – and its treatment – will have on appearance.
Tackling anxiety
Dr. Sobanko described his own, soon-to-be-published study of 104 Mohs surgery patients, who were randomized to receive a presurgical phone call to discuss anxiety, or the usual presurgical consultation. It was easy to implement the call, he said, noting that 70% were reached on the first try, and the interaction only took about 7 minutes.
Anxiety was common, with 43% reporting being anxious about the procedure. A frequent worry (25%) was whether their skin cancer would threaten their health over the long term. But both groups reported about the same reduction in anxiety after their discussion with the provider, whether it occurred over the phone or in person. After surgery, they expressed similar levels of satisfaction with the experience.
Clearly, the most effective method of dealing with patient anxiety has yet to be identified, Dr. Sobanko noted. Others are being explored, including music and educational videos.
In 2013, he and colleagues published a small study showing that music significantly reduced anxiety during Mohs surgery (Dermatol Surg. 2013 Feb;39[2]:298-305). It randomized 100 patients to surgery without music, or to listening to a playlist they had selected for themselves. Anxiety was measured using the State-Trait Anxiety Inventory and on a visual analog scale. Subjects in the music group experienced statistically significantly lower scores on both measures, Dr. Sobanko said.
A study presented at the meeting found that a preoperative education video helped as well. Dr. Sidney Smith of the Georgia Skin and Cancer Clinic, Savannah, examined the benefit of a 9-minute video created by the American College of Mohs Surgery. The video interviews patients about their experiences, describes the surgery and overall cure rates, and touches on reconstruction and follow-up.
The study comprised 200 patients; 100 saw the movie, and then completed a 24 question survey about their perception of the procedure. Almost all (94%) of those who viewed it said the video answered their questions; 85% said it relieved their fear about undergoing the surgery.
Treating anxiety
Anxiolytics can be easily employed to help ease day-of-surgery anxiety, Dr. Jerry Brewer said at the meeting. Generally speaking, the medications are safe, well-tolerated, and very effective.
“One thing we should remember, however, is that anxiolytics do not affect pain. They have no effect on pain receptors, although they may affect a patient’s memory of pain. For people who are anxious, though, this can be a really great help,” said Dr. Brewer of the Mayo Clinic, Rochester, Minn.
He favors the short-acting benzodiazepines, particularly midazolam. It has a peak concentration of 17-55 minutes, so it’s particularly well suited for shorter cases. It also has a very rapid metabolization profile, with an elimination half life of 3-7 hours.
Since midazolam has twice the affinity for the benzodiazepine receptors as does diazepam, it can be effective in relatively small doses – usually about 0.25 mg/kg. The dose should be reduced by half for elderly patients and for those with renal or hepatic failure. In those patients, the elimination half-life can be increased up to 13 hours.
The typical dose for both adults and children is 10-20 mg. “We should remember that patients who take narcotics and those who take a benzodiazepine as a sleep aide may be quite tolerant and need a higher dose,” Dr. Brewer said.
Diazepam has a peak concentration of about 2 hours, but a much longer elimination half-life – up to 48 hours in a healthy adult and up to 80 hours in an elderly person. “It’s important that patients know they’re going to have this drug in their system for a couple days. This should be part of the consenting process,” Dr. Brewer pointed out.
Lorazepam has a peak concentration of about 2 hours as well, but a shorter half-life of 12-18 hours. That can be prolonged by 75% in patients with renal problems.
With the right clinical supervision, these medications are very safe, he said. “We treat about 800 patients per year with these and have data on about 12,000. Of those, we have had very few problems. Two have fallen out of bed. One patient wrote and said he was discharged too early, as he was very tired. One person fell and hit his head in the bathroom. One was sedated enough to need a sternal rub to improve responsiveness. And one gentleman enjoyed the medication so much that when the nurse left the room for a moment he grabbed the rest of the dose and drank it.”
Safe discharge is crucial when using anxiolytics, he added. “They absolutely cannot drive themselves home and they cannot go back to work. We make sure there is a reliable person to stay with the patient for at least 4 hours after discharge.”
Dr. Brewer does not discharge any patient until that person displays a zero rating on the Richmond Agitation-Sedation Scale (RASS) sedation scale. “That means he is awake, alert, and calmly interacting with you.”
Neither Dr. Sobanko nor Dr. Brewer had any financial declarations.
ORLANDO – Assessment, education, and a judicious dose of medication can make a big difference to patients who are feeling anxious about undergoing Mohs surgery.
No studies or guidelines lay out a step-by-step management plan for anxious patients. But a little bit of common sense and empathy go a long way in easing the feeling, according to presenters at the annual meeting of the American College of Mohs Surgery.
“We don’t have an algorithm for reducing anxiety,” said Dr. Joseph Sobanko of the University of Pennsylvania, Philadelphia. “But we do have a lot of studies showing that better psychosocial health is related to better surgical outcomes.”
The lack of definitive guidance means that anxious patients might be identified and assessed by gut instinct, he continued. “Those of you who see patients probably have a gestalt technique of identifying the anxious ones. I would suggest this might not be the best way.”
Instead of guessing, he recommends assessing all patients with a validated screening tool, and dealing with anxiety proactively.
Assessing anxiety
Although anxiety assessment may not be part of a typical Mohs surgery intake, it probably should be, Dr. Sobanko said. There are a number of excellent, well-validated tools, and none of them require expertise in psychology to administer.
The Beck Anxiety Inventory is a 21-question index that takes about 10 minutes to complete. It assesses subjective, somatic, and panic-related symptoms of anxiety, and has been validated in a variety of clinical settings. It focuses quite a bit on strong physical symptoms, however, which Dr. Sobanko feels “may not be as relevant for our patients.”
The State-Trait Anxiety Inventory consists of 40 questions and takes about 15 minutes to complete. “I like it because it not only assesses how they generally feel, but how they feel at the moment,” he said. “We think it’s good and we do use it, but it takes a while to complete.”
The Hospital Anxiety and Depression Scale is short, with only 14 questions, and takes only about 5 minutes to complete. “It’s validated for hospital patients, but we are often working with patients who are less sick than that,” Dr. Sobanko said.
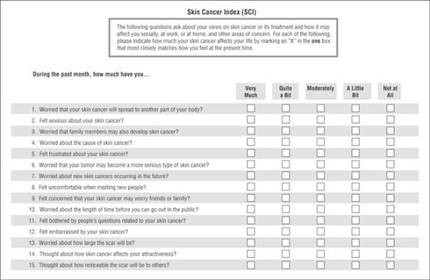
The Skin Cancer Index is his go-to anxiety screen for Mohs patients. It includes 15 questions that “really get to the heart of things that matter to our patients: emotional, social, and appearance issues,” he noted. Created in 2006, it was validated in a large cohort of Mohs surgery patients (Arch Facial Plast Surg. 2006;8[5]:314-318). The questions probe patients’ feelings about the seriousness of their skin cancer, its long-term health effect, and the impact the lesion – and its treatment – will have on appearance.
Tackling anxiety
Dr. Sobanko described his own, soon-to-be-published study of 104 Mohs surgery patients, who were randomized to receive a presurgical phone call to discuss anxiety, or the usual presurgical consultation. It was easy to implement the call, he said, noting that 70% were reached on the first try, and the interaction only took about 7 minutes.
Anxiety was common, with 43% reporting being anxious about the procedure. A frequent worry (25%) was whether their skin cancer would threaten their health over the long term. But both groups reported about the same reduction in anxiety after their discussion with the provider, whether it occurred over the phone or in person. After surgery, they expressed similar levels of satisfaction with the experience.
Clearly, the most effective method of dealing with patient anxiety has yet to be identified, Dr. Sobanko noted. Others are being explored, including music and educational videos.
In 2013, he and colleagues published a small study showing that music significantly reduced anxiety during Mohs surgery (Dermatol Surg. 2013 Feb;39[2]:298-305). It randomized 100 patients to surgery without music, or to listening to a playlist they had selected for themselves. Anxiety was measured using the State-Trait Anxiety Inventory and on a visual analog scale. Subjects in the music group experienced statistically significantly lower scores on both measures, Dr. Sobanko said.
A study presented at the meeting found that a preoperative education video helped as well. Dr. Sidney Smith of the Georgia Skin and Cancer Clinic, Savannah, examined the benefit of a 9-minute video created by the American College of Mohs Surgery. The video interviews patients about their experiences, describes the surgery and overall cure rates, and touches on reconstruction and follow-up.
The study comprised 200 patients; 100 saw the movie, and then completed a 24 question survey about their perception of the procedure. Almost all (94%) of those who viewed it said the video answered their questions; 85% said it relieved their fear about undergoing the surgery.
Treating anxiety
Anxiolytics can be easily employed to help ease day-of-surgery anxiety, Dr. Jerry Brewer said at the meeting. Generally speaking, the medications are safe, well-tolerated, and very effective.
“One thing we should remember, however, is that anxiolytics do not affect pain. They have no effect on pain receptors, although they may affect a patient’s memory of pain. For people who are anxious, though, this can be a really great help,” said Dr. Brewer of the Mayo Clinic, Rochester, Minn.
He favors the short-acting benzodiazepines, particularly midazolam. It has a peak concentration of 17-55 minutes, so it’s particularly well suited for shorter cases. It also has a very rapid metabolization profile, with an elimination half life of 3-7 hours.
Since midazolam has twice the affinity for the benzodiazepine receptors as does diazepam, it can be effective in relatively small doses – usually about 0.25 mg/kg. The dose should be reduced by half for elderly patients and for those with renal or hepatic failure. In those patients, the elimination half-life can be increased up to 13 hours.
The typical dose for both adults and children is 10-20 mg. “We should remember that patients who take narcotics and those who take a benzodiazepine as a sleep aide may be quite tolerant and need a higher dose,” Dr. Brewer said.
Diazepam has a peak concentration of about 2 hours, but a much longer elimination half-life – up to 48 hours in a healthy adult and up to 80 hours in an elderly person. “It’s important that patients know they’re going to have this drug in their system for a couple days. This should be part of the consenting process,” Dr. Brewer pointed out.
Lorazepam has a peak concentration of about 2 hours as well, but a shorter half-life of 12-18 hours. That can be prolonged by 75% in patients with renal problems.
With the right clinical supervision, these medications are very safe, he said. “We treat about 800 patients per year with these and have data on about 12,000. Of those, we have had very few problems. Two have fallen out of bed. One patient wrote and said he was discharged too early, as he was very tired. One person fell and hit his head in the bathroom. One was sedated enough to need a sternal rub to improve responsiveness. And one gentleman enjoyed the medication so much that when the nurse left the room for a moment he grabbed the rest of the dose and drank it.”
Safe discharge is crucial when using anxiolytics, he added. “They absolutely cannot drive themselves home and they cannot go back to work. We make sure there is a reliable person to stay with the patient for at least 4 hours after discharge.”
Dr. Brewer does not discharge any patient until that person displays a zero rating on the Richmond Agitation-Sedation Scale (RASS) sedation scale. “That means he is awake, alert, and calmly interacting with you.”
Neither Dr. Sobanko nor Dr. Brewer had any financial declarations.
ORLANDO – Assessment, education, and a judicious dose of medication can make a big difference to patients who are feeling anxious about undergoing Mohs surgery.
No studies or guidelines lay out a step-by-step management plan for anxious patients. But a little bit of common sense and empathy go a long way in easing the feeling, according to presenters at the annual meeting of the American College of Mohs Surgery.
“We don’t have an algorithm for reducing anxiety,” said Dr. Joseph Sobanko of the University of Pennsylvania, Philadelphia. “But we do have a lot of studies showing that better psychosocial health is related to better surgical outcomes.”
The lack of definitive guidance means that anxious patients might be identified and assessed by gut instinct, he continued. “Those of you who see patients probably have a gestalt technique of identifying the anxious ones. I would suggest this might not be the best way.”
Instead of guessing, he recommends assessing all patients with a validated screening tool, and dealing with anxiety proactively.
Assessing anxiety
Although anxiety assessment may not be part of a typical Mohs surgery intake, it probably should be, Dr. Sobanko said. There are a number of excellent, well-validated tools, and none of them require expertise in psychology to administer.
The Beck Anxiety Inventory is a 21-question index that takes about 10 minutes to complete. It assesses subjective, somatic, and panic-related symptoms of anxiety, and has been validated in a variety of clinical settings. It focuses quite a bit on strong physical symptoms, however, which Dr. Sobanko feels “may not be as relevant for our patients.”
The State-Trait Anxiety Inventory consists of 40 questions and takes about 15 minutes to complete. “I like it because it not only assesses how they generally feel, but how they feel at the moment,” he said. “We think it’s good and we do use it, but it takes a while to complete.”
The Hospital Anxiety and Depression Scale is short, with only 14 questions, and takes only about 5 minutes to complete. “It’s validated for hospital patients, but we are often working with patients who are less sick than that,” Dr. Sobanko said.
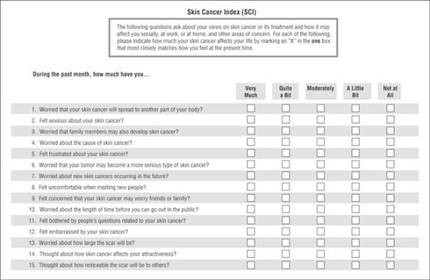
The Skin Cancer Index is his go-to anxiety screen for Mohs patients. It includes 15 questions that “really get to the heart of things that matter to our patients: emotional, social, and appearance issues,” he noted. Created in 2006, it was validated in a large cohort of Mohs surgery patients (Arch Facial Plast Surg. 2006;8[5]:314-318). The questions probe patients’ feelings about the seriousness of their skin cancer, its long-term health effect, and the impact the lesion – and its treatment – will have on appearance.
Tackling anxiety
Dr. Sobanko described his own, soon-to-be-published study of 104 Mohs surgery patients, who were randomized to receive a presurgical phone call to discuss anxiety, or the usual presurgical consultation. It was easy to implement the call, he said, noting that 70% were reached on the first try, and the interaction only took about 7 minutes.
Anxiety was common, with 43% reporting being anxious about the procedure. A frequent worry (25%) was whether their skin cancer would threaten their health over the long term. But both groups reported about the same reduction in anxiety after their discussion with the provider, whether it occurred over the phone or in person. After surgery, they expressed similar levels of satisfaction with the experience.
Clearly, the most effective method of dealing with patient anxiety has yet to be identified, Dr. Sobanko noted. Others are being explored, including music and educational videos.
In 2013, he and colleagues published a small study showing that music significantly reduced anxiety during Mohs surgery (Dermatol Surg. 2013 Feb;39[2]:298-305). It randomized 100 patients to surgery without music, or to listening to a playlist they had selected for themselves. Anxiety was measured using the State-Trait Anxiety Inventory and on a visual analog scale. Subjects in the music group experienced statistically significantly lower scores on both measures, Dr. Sobanko said.
A study presented at the meeting found that a preoperative education video helped as well. Dr. Sidney Smith of the Georgia Skin and Cancer Clinic, Savannah, examined the benefit of a 9-minute video created by the American College of Mohs Surgery. The video interviews patients about their experiences, describes the surgery and overall cure rates, and touches on reconstruction and follow-up.
The study comprised 200 patients; 100 saw the movie, and then completed a 24 question survey about their perception of the procedure. Almost all (94%) of those who viewed it said the video answered their questions; 85% said it relieved their fear about undergoing the surgery.
Treating anxiety
Anxiolytics can be easily employed to help ease day-of-surgery anxiety, Dr. Jerry Brewer said at the meeting. Generally speaking, the medications are safe, well-tolerated, and very effective.
“One thing we should remember, however, is that anxiolytics do not affect pain. They have no effect on pain receptors, although they may affect a patient’s memory of pain. For people who are anxious, though, this can be a really great help,” said Dr. Brewer of the Mayo Clinic, Rochester, Minn.
He favors the short-acting benzodiazepines, particularly midazolam. It has a peak concentration of 17-55 minutes, so it’s particularly well suited for shorter cases. It also has a very rapid metabolization profile, with an elimination half life of 3-7 hours.
Since midazolam has twice the affinity for the benzodiazepine receptors as does diazepam, it can be effective in relatively small doses – usually about 0.25 mg/kg. The dose should be reduced by half for elderly patients and for those with renal or hepatic failure. In those patients, the elimination half-life can be increased up to 13 hours.
The typical dose for both adults and children is 10-20 mg. “We should remember that patients who take narcotics and those who take a benzodiazepine as a sleep aide may be quite tolerant and need a higher dose,” Dr. Brewer said.
Diazepam has a peak concentration of about 2 hours, but a much longer elimination half-life – up to 48 hours in a healthy adult and up to 80 hours in an elderly person. “It’s important that patients know they’re going to have this drug in their system for a couple days. This should be part of the consenting process,” Dr. Brewer pointed out.
Lorazepam has a peak concentration of about 2 hours as well, but a shorter half-life of 12-18 hours. That can be prolonged by 75% in patients with renal problems.
With the right clinical supervision, these medications are very safe, he said. “We treat about 800 patients per year with these and have data on about 12,000. Of those, we have had very few problems. Two have fallen out of bed. One patient wrote and said he was discharged too early, as he was very tired. One person fell and hit his head in the bathroom. One was sedated enough to need a sternal rub to improve responsiveness. And one gentleman enjoyed the medication so much that when the nurse left the room for a moment he grabbed the rest of the dose and drank it.”
Safe discharge is crucial when using anxiolytics, he added. “They absolutely cannot drive themselves home and they cannot go back to work. We make sure there is a reliable person to stay with the patient for at least 4 hours after discharge.”
Dr. Brewer does not discharge any patient until that person displays a zero rating on the Richmond Agitation-Sedation Scale (RASS) sedation scale. “That means he is awake, alert, and calmly interacting with you.”
Neither Dr. Sobanko nor Dr. Brewer had any financial declarations.
EXPERT ANALYSIS FROM THE ACMS ANNUAL MEETING

