User login
› Seek immediate emergency care for patients with chest pain that is exertional, radiating to one or both arms, similar to or worse than prior cardiac chest pain, or associated with nausea, vomiting, or diaphoresis. A
› Be aware that patients with chest pain that is stabbing, pleuritic, positional, or reproducible with palpation are at very low risk for acute coronary syndrome and most likely have chest wall pain. A
› Consider a 2-week course of high-dose proton-pump inhibitor therapy to help identify patients whose chest pain may be from undiagnosed gastroesophageal reflux disease. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Your patient, Amy Z, age 58, was given a diagnosis of hypertension 10 years ago and since then has been maintained on hydrochlorothiazide 50 mg/d and lisinopril 10 mg/d. In the office today, she reports intermittent chest tightness and heaviness. She has no history of coronary artery disease (CAD), cerebrovascular disease, or peripheral vascular disease. She attributes her chest discomfort to emotional stress. She recently started a job after having been unemployed, but still has no health insurance and is concerned about losing her house.
She denies orthopnea and resting or exertional dyspnea, and says she never gets chest pain while climbing stairs. Her blood pressure is elevated at 180/110 mm Hg, but her other vital signs are normal (pulse, 70 beats per minute; respiratory rate, 18 breaths per minute). On physical examination, she has no venous distension in her neck and her lungs are clear. A cardiac exam reveals a regular rate and rhythm, with a normally split S1 and S2 and no murmurs, rubs, or gallops. Palpation of the chest does not reproduce her chest pain.
You are concerned that your patient’s chest pain could be from heart disease, but she wants to defer additional testing because of the cost, stating, “It’s all due to my stress.”
How would you proceed?
Musculoskeletal chest wall pain is the most common cause of chest pain in patients who seek treatment in the office, followed by GI disease and stable heart disease.
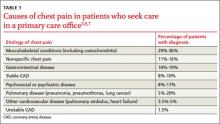
Whether they go to the emergency department (ED) or to their family physician’s office, most patients who seek treatment for chest pain don’t have life-threatening cardiac illness. Of the 8 million patients who visit an ED for chest pain each year, only 13% are diagnosed with acute coronary syndrome (ACS).1,2 Among those seen for chest pain in a primary care office, only a minority (approximately 1.5%) have unstable heart disease.3-5 Cross-sectional studies indicate that musculoskeletal chest wall pain (or “chest wall syndrome [CWS]”) is the most common cause of chest pain in patients who seek treatment in the office, followed by gastrointestinal (GI) disease, stable heart disease, psychosocial or psychiatric conditions, pulmonary disease, and other cardiovascular conditions (TABLE 1).3,6,7
When evaluating patients with chest pain in the office, the challenge is to appropriately evaluate and manage those who are at low risk of ACS, while at the same time identifying and arranging prompt transfer or referral for the minority of patients who are at high cardiac risk. This article describes how to determine which patients require emergency treatment, which tools to use to screen for ACS and other potential causes of chest pain, and how to proceed when initial evaluation and testing do not point to a clear diagnosis.
Start with the ABCs
When a patient presents in primary care with a chief complaint of chest pain, it’s of course critical that you quickly determine if he or she is stable by evaluating the “ABCs” (airway, breathing, and circulation). Any potentially unstable patient should be immediately transferred for emergency care.8 A patient who shows no signs of respiratory distress and whose vital signs are within a normal range is unlikely to be acutely unstable, and can be further evaluated in the office.
If the patient is stable, obtain a history of the onset and evolution of the chest pain, especially its location, quality, duration, and aggravating or alleviating factors. Also ask about a personal or family history of heart disease, hypertension, diabetes, or hypercholesterolemia, and about tobacco use. While the presence of any of these cardiac risk factors may increase suspicion for a cardiac cause for chest pain, the absence of such factors does not eliminate the need for a careful diagnostic evaluation.
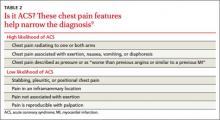
Patients with “typical” chest pain have a higher risk of ACS. In a 2005 review of observational prospective and retrospective studies and systematic reviews, Swap et al9 corroborated the description of “typical” anginal chest pain, indicating that patients whose chest pain is exertional, radiating to one or both arms, similar to or worse than prior cardiac chest pain, or associated with nausea, vomiting, or diaphoresis are at high risk for ACS (TABLE 2).9 These researchers also found that chest pain that is stabbing, pleuritic, positional, or reproducible with palpation suggests that a patient is at low risk for ACS. Pain that is not exertional or that is in a small inframammary area of the chest also suggests a low risk for ACS.9
Marburg Heart Score and other tests can help rule out ACS
As part of your initial physical examination, assess the patient’s overall condition and stability. Be aware, however, that an older literature review found that a physical exam is only minimally helpful in assessing ACS risk in a patient with chest pain. Findings that may increase the risk of ACS are a third heart sound (positive likelihood ratio [LR+] = 3.2; 95% confidence interval [CI], 1.6-6.5), systolic blood pressure <80 mm/Hg (LR+ = 3.1; 95% CI, 1.8-5.2), and pulmonary crackles on auscultation (LR+ = 2.1; 95% CI, 1.4–3.1); however, the absence of these findings does not exclude ACS.10 The most helpful sign or symptom in evaluating a patient with chest pain is chest wall tenderness on palpation, which largely rules out ACS in low-prevalence settings, such as a primary care office.11
Bösner et al12 developed the Marburg Heart Score (MHS) to help primary care physicians evaluate the risk of CAD in patients with chest pain (TABLE 3).12,13 A subsequent validation study found that an MHS ≥3 had a sensitivity of 89.1% (95% CI, 81.1%-94%) and a specificity of 63.5% (95% CI, 60%-66.9%) for CAD.13 The test’s negative predictive value (NPV) of 97.9% (95% CI, 96.2%-98.9%) means that patients with an MHS ≤2 are very unlikely to have CAD; however, the low positive predictive value (PPV) of only 23.3% (95% CI, 19.2%-28.0%) means an MHS ≥3 is not particularly helpful in diagnosing CAD.12,13
Unless it is clear that your patient’s chest pain is unlikely to have a cardiac cause (eg, pain is reproducible on palpation, or an MHS ≤2), order an electrocardiogram (EKG). If the EKG shows ST-segment elevation in 2 or more contiguous leads, presumed new left bundle branch block, ischemic ST-segment depression >.5 mm (.05 mV), or dynamic T-wave inversion with pain or discomfort, the patient needs urgent referral for emergency care.8 If the EKG is nondiagnostic but the chest pain is suspicious for CAD, then further testing with cardiac biomarkers (eg, troponin I or T) is recommended to evaluate for non-ST elevation myocardial infarction. Consider chest radiography if there is evidence of respiratory disease (cough, dyspnea, or a history of pulmonary disease).
Don’t overlook chest wall syndrome, GERD, or panic disorder
There are several conditions to consider in the differential diagnosis of patients whose chest pain does not appear to have a cardiac cause:
CWS is the most common cause of chest pain in primary care patients.14,15 While there are several specific types of chest wall pain—including musculoskeletal pain, parietal or intercostal pain, Tietze’s syndrome, and costochondral pain—all are manifestations of a musculoskeletal disorder and associated with tenderness of the chest wall. CWS is not life threatening, but one study found high rates of anxiety (54%-93%) among patients with moderate to severe CWS.14,15
Few trials have evaluated treatments for chest wall pain or costochondritis, though typical recommendations include nonsteroidal anti-inflammatory medications, use of heat or cold, physical therapy, or injection of local anesthetic.16 One study found that stretching exercises might benefit patients with costochondritis.17
GI disorders. Patients with esophagitis or gastroesophageal reflux disease (GERD) often report heartburn, chronic cough, chronic laryngitis, and asthma.18 However, the sensitivity and specificity of these symptoms are too low to allow diagnosis or exclusion of GERD based on history alone.18
Acid suppression therapy can be used to test for GERD. A 2005 meta-analysis of 6 studies found the sensitivity and specificity of a proton-pump inhibitor (PPI) acid suppression test for the diagnosis of GERD in patients with noncardiac chest pain were 80% (95% CI, 71%-87%) and 74% (95% CI, 64%-83%), respectively.19 One study demonstrated that relief of chest pain after a 14-day course of omeprazole 40 mg/d was more sensitive than endoscopy, manometry, or 24-hour esophageal pH monitoring in diagnosing GERD.20 Another study found that in patients with noncardiac chest pain and normal upper endoscopy, symptomatic relief with lansoprazole 30 mg/d for 4 weeks can be used to diagnose endoscopy-negative GERD.21
It is appropriate to try a high-dose course of a PPI (ie, omeprazole 40 mg twice daily, lansoprazole 30 mg/d, or esomeprazole 40 mg twice daily) to evaluate for GERD as the cause of chest pain in patients who:20-22
• do not initially describe typical reflux symptoms (eg, heartburn, chronic regurgitation, chronic cough, or a sore or burning throat)
• have no history of surgery in the upper GI tract, esophagus, or thorax, and
• have no signs or symptoms that indicate they have a serious or malignant disease (eg, weight loss, anemia, or dysphagia).
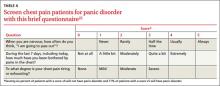
Panic disorder. Several tools have been proposed for screening for panic disorder (PD),23,24 but none have been tested in patients with chest pain. Dammen et al25 developed a 3-item questionnaire to assess for PD among patients with chest pain who were referred for cardiac evaluation (TABLE 4).25 A score ≥5 on the Dammen questionnaire had 55% sensitivity and 86% specificity for PD, with a PPV of 71% and an NPV of 76%.25 Although this instrument has not been subjected to validation studies, using it may help clarify whether further investigation for PD is warranted.
Psychotherapeutic interventions may be effective for patients whose chest pain is caused by PD. A Cochrane review of 15 randomized controlled trials of psychological interventions for chest pain in patients with normal coronary anatomy found that cognitive-behavior therapy, and possibly hypnotherapy, reduced patient reports of chest pain, reduced chest pain frequency, and increased the number of chest pain-free days, at least for 3 months.26
What to do when the diagnosis remains unclear
When your initial evaluation and diagnostic testing yield no clear diagnosis, appropriate follow-up is vital because in the year after primary care patients first develop chest pain, they are 1.5 to 3 times more likely than the general population to be diagnosed with musculoskeletal, GI, psychological, or respiratory problems, nearly 5 times as likely to be diagnosed with heart failure, and nearly 15 times as likely to be diagnosed with coronary heart disease.27,28
Consider ordering exercise or chemical stress testing within 3 to 7 days for a patient with chest pain that suggests ACS but who has normal results on EKG and biomarker testing.8 Interestingly, though, in a study of 4181 patients in an ED chest pain unit who had 2 sets of normal serum troponins during a 6-hour period followed by exercise or chemical stress testing, only 470 patients (11%) had abnormal stress test results and only 37 (.9%) had obstructive CAD that would have potentially benefited from revascularization.29 Thus, testing troponin levels twice over 6 hours is a reasonable alternative to stress testing for a primary care patient with chest pain; stress testing would be unnecessary if both troponin values were normal.
CASE › Based on her current chest pain symptoms, Ms. Z’s MHS is a reassuringly low 1, so CAD is unlikely. However, she scores 5 on the Dammen panic disorder screen. Due to her financial concerns, you decide to forgo stress testing and instead draw a serum troponin now, with plans to repeat later in the afternoon at your clinic lab if the initial result is normal. You encourage her to try a high-dose PPI for 2 weeks to determine whether GERD may be contributing to her symptoms, and offer to help her explore counseling options to address her emotional stressors.
CORRESPONDENCE
William E. Cayley Jr, MD, MDiv, University of Wisconsin, UW Health Augusta Family Medicine Clinic, 207 West Lincoln, Augusta, WI 54722; [email protected]
1. Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122:1756-7176.
2. Bhuiya FA, Pitts SR, McCaig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999-2008. NCHS Data Brief. 2010;43:1-8.
3. Klinkman MS, Stevens D, Gorenflo DW. Episodes of care for chest pain: a preliminary report from MIRNET. Michigan Research Network. J Fam Pract. 1994;38:345-352.
4. McConaghy JR, Oza RS. Outpatient diagnosis of acute chest pain in adults. Am Fam Physician. 2013;87:177-82.
5. Nilsson S, Scheike M, Engblom D, et al. Chest pain and ischaemic heart disease in primary care. Br J Gen Pract. 2003;53:378-382.
6. Buntinx F, Knockaert D, Bruyninckx R, et al. Chest pain in general practice or in the hospital emergency department: is it the same? Fam Pract. 2001;18:586-589.
7. Jonsbu E, Dammen T, Morken G, et al. Cardiac and psychiatric diagnoses among patients referred for chest pain and palpitations. Scand Cardiovasc J. 2009;43:256-259.
8. O’Connor RE, Brady W, Brooks SC, et al. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 suppl 3):S787-S817.
9. Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005;294:2623-2629.
10. Panju AA, Hemmelgarn BR, Guyatt GH, et al. The rational clinical examination. Is this patient having a myocardial infarction? JAMA. 1998;280:1256-1263.
11. Bruyninckx R, Aertgeerts B, Bruyninckx P, et al. Signs and symptoms in diagnosing acute myocardial infarction and acute coronary syndrome: a diagnostic meta-analysis. Br J Gen Pract. 2008;58:105-111.
12. Bösner S, Haasenritter J, Becker A, et al. Ruling out coronary artery disease in primary care: development and validation of a simple prediction rule. CMAJ. 2010;182:1295-1300.
13. Haasenritter J, Bösner S, Vaucher P, et al. Ruling out coronary heart disease in primary care: external validation of a clinical prediction rule. Br J Gen Pract. 2012;62:e415-e421.
14. Bösner S, Becker A, Hani MA, et al. Chest wall syndrome in primary care patients with chest pain: presentation, associated features and diagnosis. Fam Pract. 2010;27:363-369.
15. Verdon F, Burnand B, Herzig L, et al. Chest wall syndrome among primary care patients: a cohort study. BMC Fam Pract. 2007;8:51.
16. Proulx AM, Zryd TW. Costochondritis: diagnosis and treatment. Am Fam Physician. 2009;80:617-620.
17. Rovetta G, Sessarego P, Monteforte P. Stretching exercises for costochondritis pain. G Ital Med Lav Ergon. 2009;31:169-171.
18. Lacy BE, Weiser K, Chertoff J, et al. The diagnosis of gastroesophageal reflux disease. Am J Med. 2010;123: 583-592.
19. Wang WH, Huang JQ, Zheng GF, et al. Is proton pump inhibitor testing an effective approach to diagnose gastroesophageal reflux disease in patients with noncardiac chest pain?: a metaanalysis. Arch Intern Med. 2005;165:1222-1228.
20. Pandak WM, Arezo S, Everett S, et al. Short course of omeprazole: a better first diagnostic approach to noncardiac chest pain than endoscopy, manometry, or 24-hour esophageal pH monitoring. J Clin Gastroenterol. 2002;35:307-314.
21. Xia HH, Lai KC, Lam SK, et al. Symptomatic response to lansoprazole predicts abnormal acid reflux in endoscopy-negative patients with non-cardiac chest pain. Aliment Pharmacol Ther. 2003;17:369-377.
22. Flook NW, Moayyedi P, Dent J, et al. Acid-suppressive therapy with esomeprazole for relief of unexplained chest pain in primary care: a randomized, double-blind, placebo-controlled trial. Am J Gastroenterol. 2013;108:56-64.
23. Stein MB, Roy-Byrne PP, McQuaid JR, et al. Development of a brief diagnostic screen for panic disorder in primary care. Psychosom Med. 1999;61:359-364.
24. Ballenger JC. Treatment of panic disorder in the general medical setting. J Psychosom Res. 1998;44:5-15.
25. Dammen T, Ekeberg O, Arnesen H, et al. The detection of panic disorder in chest pain patients. Gen Hosp Psychiatry. 1999;21:323-332.
26. Kisely SR, Campbell LA, Yelland MJ, et al. Psychological interventions for symptomatic management of non-specific chest pain in patients with normal coronary anatomy. Cochrane Database Syst Rev. 2012;6:CD004101.
27. Ruigómez A, Rodríguez LA, Wallander MA, et al. Chest pain in general practice: incidence, comorbidity and mortality. Fam Pract. 2006;23:167-174.
28. Ruigómez A, Massó-González EL, Johansson S, et al. Chest pain without established ischaemic heart disease in primary care patients: associated comorbidities and mortality. Br J Gen Pract. 2009;59:e78-e86.
29. Hermann LK, Newman DH, Pleasant WA, et al. Yield of routine provocative cardiac testing among patients in an emergency department-based chest pain unit. JAMA Intern Med. 2013;173:1128-1133.
› Seek immediate emergency care for patients with chest pain that is exertional, radiating to one or both arms, similar to or worse than prior cardiac chest pain, or associated with nausea, vomiting, or diaphoresis. A
› Be aware that patients with chest pain that is stabbing, pleuritic, positional, or reproducible with palpation are at very low risk for acute coronary syndrome and most likely have chest wall pain. A
› Consider a 2-week course of high-dose proton-pump inhibitor therapy to help identify patients whose chest pain may be from undiagnosed gastroesophageal reflux disease. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Your patient, Amy Z, age 58, was given a diagnosis of hypertension 10 years ago and since then has been maintained on hydrochlorothiazide 50 mg/d and lisinopril 10 mg/d. In the office today, she reports intermittent chest tightness and heaviness. She has no history of coronary artery disease (CAD), cerebrovascular disease, or peripheral vascular disease. She attributes her chest discomfort to emotional stress. She recently started a job after having been unemployed, but still has no health insurance and is concerned about losing her house.
She denies orthopnea and resting or exertional dyspnea, and says she never gets chest pain while climbing stairs. Her blood pressure is elevated at 180/110 mm Hg, but her other vital signs are normal (pulse, 70 beats per minute; respiratory rate, 18 breaths per minute). On physical examination, she has no venous distension in her neck and her lungs are clear. A cardiac exam reveals a regular rate and rhythm, with a normally split S1 and S2 and no murmurs, rubs, or gallops. Palpation of the chest does not reproduce her chest pain.
You are concerned that your patient’s chest pain could be from heart disease, but she wants to defer additional testing because of the cost, stating, “It’s all due to my stress.”
How would you proceed?
Musculoskeletal chest wall pain is the most common cause of chest pain in patients who seek treatment in the office, followed by GI disease and stable heart disease.
Whether they go to the emergency department (ED) or to their family physician’s office, most patients who seek treatment for chest pain don’t have life-threatening cardiac illness. Of the 8 million patients who visit an ED for chest pain each year, only 13% are diagnosed with acute coronary syndrome (ACS).1,2 Among those seen for chest pain in a primary care office, only a minority (approximately 1.5%) have unstable heart disease.3-5 Cross-sectional studies indicate that musculoskeletal chest wall pain (or “chest wall syndrome [CWS]”) is the most common cause of chest pain in patients who seek treatment in the office, followed by gastrointestinal (GI) disease, stable heart disease, psychosocial or psychiatric conditions, pulmonary disease, and other cardiovascular conditions (TABLE 1).3,6,7
When evaluating patients with chest pain in the office, the challenge is to appropriately evaluate and manage those who are at low risk of ACS, while at the same time identifying and arranging prompt transfer or referral for the minority of patients who are at high cardiac risk. This article describes how to determine which patients require emergency treatment, which tools to use to screen for ACS and other potential causes of chest pain, and how to proceed when initial evaluation and testing do not point to a clear diagnosis.
Start with the ABCs
When a patient presents in primary care with a chief complaint of chest pain, it’s of course critical that you quickly determine if he or she is stable by evaluating the “ABCs” (airway, breathing, and circulation). Any potentially unstable patient should be immediately transferred for emergency care.8 A patient who shows no signs of respiratory distress and whose vital signs are within a normal range is unlikely to be acutely unstable, and can be further evaluated in the office.
If the patient is stable, obtain a history of the onset and evolution of the chest pain, especially its location, quality, duration, and aggravating or alleviating factors. Also ask about a personal or family history of heart disease, hypertension, diabetes, or hypercholesterolemia, and about tobacco use. While the presence of any of these cardiac risk factors may increase suspicion for a cardiac cause for chest pain, the absence of such factors does not eliminate the need for a careful diagnostic evaluation.
Patients with “typical” chest pain have a higher risk of ACS. In a 2005 review of observational prospective and retrospective studies and systematic reviews, Swap et al9 corroborated the description of “typical” anginal chest pain, indicating that patients whose chest pain is exertional, radiating to one or both arms, similar to or worse than prior cardiac chest pain, or associated with nausea, vomiting, or diaphoresis are at high risk for ACS (TABLE 2).9 These researchers also found that chest pain that is stabbing, pleuritic, positional, or reproducible with palpation suggests that a patient is at low risk for ACS. Pain that is not exertional or that is in a small inframammary area of the chest also suggests a low risk for ACS.9
Marburg Heart Score and other tests can help rule out ACS
As part of your initial physical examination, assess the patient’s overall condition and stability. Be aware, however, that an older literature review found that a physical exam is only minimally helpful in assessing ACS risk in a patient with chest pain. Findings that may increase the risk of ACS are a third heart sound (positive likelihood ratio [LR+] = 3.2; 95% confidence interval [CI], 1.6-6.5), systolic blood pressure <80 mm/Hg (LR+ = 3.1; 95% CI, 1.8-5.2), and pulmonary crackles on auscultation (LR+ = 2.1; 95% CI, 1.4–3.1); however, the absence of these findings does not exclude ACS.10 The most helpful sign or symptom in evaluating a patient with chest pain is chest wall tenderness on palpation, which largely rules out ACS in low-prevalence settings, such as a primary care office.11
Bösner et al12 developed the Marburg Heart Score (MHS) to help primary care physicians evaluate the risk of CAD in patients with chest pain (TABLE 3).12,13 A subsequent validation study found that an MHS ≥3 had a sensitivity of 89.1% (95% CI, 81.1%-94%) and a specificity of 63.5% (95% CI, 60%-66.9%) for CAD.13 The test’s negative predictive value (NPV) of 97.9% (95% CI, 96.2%-98.9%) means that patients with an MHS ≤2 are very unlikely to have CAD; however, the low positive predictive value (PPV) of only 23.3% (95% CI, 19.2%-28.0%) means an MHS ≥3 is not particularly helpful in diagnosing CAD.12,13
Unless it is clear that your patient’s chest pain is unlikely to have a cardiac cause (eg, pain is reproducible on palpation, or an MHS ≤2), order an electrocardiogram (EKG). If the EKG shows ST-segment elevation in 2 or more contiguous leads, presumed new left bundle branch block, ischemic ST-segment depression >.5 mm (.05 mV), or dynamic T-wave inversion with pain or discomfort, the patient needs urgent referral for emergency care.8 If the EKG is nondiagnostic but the chest pain is suspicious for CAD, then further testing with cardiac biomarkers (eg, troponin I or T) is recommended to evaluate for non-ST elevation myocardial infarction. Consider chest radiography if there is evidence of respiratory disease (cough, dyspnea, or a history of pulmonary disease).
Don’t overlook chest wall syndrome, GERD, or panic disorder
There are several conditions to consider in the differential diagnosis of patients whose chest pain does not appear to have a cardiac cause:
CWS is the most common cause of chest pain in primary care patients.14,15 While there are several specific types of chest wall pain—including musculoskeletal pain, parietal or intercostal pain, Tietze’s syndrome, and costochondral pain—all are manifestations of a musculoskeletal disorder and associated with tenderness of the chest wall. CWS is not life threatening, but one study found high rates of anxiety (54%-93%) among patients with moderate to severe CWS.14,15
Few trials have evaluated treatments for chest wall pain or costochondritis, though typical recommendations include nonsteroidal anti-inflammatory medications, use of heat or cold, physical therapy, or injection of local anesthetic.16 One study found that stretching exercises might benefit patients with costochondritis.17
GI disorders. Patients with esophagitis or gastroesophageal reflux disease (GERD) often report heartburn, chronic cough, chronic laryngitis, and asthma.18 However, the sensitivity and specificity of these symptoms are too low to allow diagnosis or exclusion of GERD based on history alone.18
Acid suppression therapy can be used to test for GERD. A 2005 meta-analysis of 6 studies found the sensitivity and specificity of a proton-pump inhibitor (PPI) acid suppression test for the diagnosis of GERD in patients with noncardiac chest pain were 80% (95% CI, 71%-87%) and 74% (95% CI, 64%-83%), respectively.19 One study demonstrated that relief of chest pain after a 14-day course of omeprazole 40 mg/d was more sensitive than endoscopy, manometry, or 24-hour esophageal pH monitoring in diagnosing GERD.20 Another study found that in patients with noncardiac chest pain and normal upper endoscopy, symptomatic relief with lansoprazole 30 mg/d for 4 weeks can be used to diagnose endoscopy-negative GERD.21
It is appropriate to try a high-dose course of a PPI (ie, omeprazole 40 mg twice daily, lansoprazole 30 mg/d, or esomeprazole 40 mg twice daily) to evaluate for GERD as the cause of chest pain in patients who:20-22
• do not initially describe typical reflux symptoms (eg, heartburn, chronic regurgitation, chronic cough, or a sore or burning throat)
• have no history of surgery in the upper GI tract, esophagus, or thorax, and
• have no signs or symptoms that indicate they have a serious or malignant disease (eg, weight loss, anemia, or dysphagia).
Panic disorder. Several tools have been proposed for screening for panic disorder (PD),23,24 but none have been tested in patients with chest pain. Dammen et al25 developed a 3-item questionnaire to assess for PD among patients with chest pain who were referred for cardiac evaluation (TABLE 4).25 A score ≥5 on the Dammen questionnaire had 55% sensitivity and 86% specificity for PD, with a PPV of 71% and an NPV of 76%.25 Although this instrument has not been subjected to validation studies, using it may help clarify whether further investigation for PD is warranted.
Psychotherapeutic interventions may be effective for patients whose chest pain is caused by PD. A Cochrane review of 15 randomized controlled trials of psychological interventions for chest pain in patients with normal coronary anatomy found that cognitive-behavior therapy, and possibly hypnotherapy, reduced patient reports of chest pain, reduced chest pain frequency, and increased the number of chest pain-free days, at least for 3 months.26
What to do when the diagnosis remains unclear
When your initial evaluation and diagnostic testing yield no clear diagnosis, appropriate follow-up is vital because in the year after primary care patients first develop chest pain, they are 1.5 to 3 times more likely than the general population to be diagnosed with musculoskeletal, GI, psychological, or respiratory problems, nearly 5 times as likely to be diagnosed with heart failure, and nearly 15 times as likely to be diagnosed with coronary heart disease.27,28
Consider ordering exercise or chemical stress testing within 3 to 7 days for a patient with chest pain that suggests ACS but who has normal results on EKG and biomarker testing.8 Interestingly, though, in a study of 4181 patients in an ED chest pain unit who had 2 sets of normal serum troponins during a 6-hour period followed by exercise or chemical stress testing, only 470 patients (11%) had abnormal stress test results and only 37 (.9%) had obstructive CAD that would have potentially benefited from revascularization.29 Thus, testing troponin levels twice over 6 hours is a reasonable alternative to stress testing for a primary care patient with chest pain; stress testing would be unnecessary if both troponin values were normal.
CASE › Based on her current chest pain symptoms, Ms. Z’s MHS is a reassuringly low 1, so CAD is unlikely. However, she scores 5 on the Dammen panic disorder screen. Due to her financial concerns, you decide to forgo stress testing and instead draw a serum troponin now, with plans to repeat later in the afternoon at your clinic lab if the initial result is normal. You encourage her to try a high-dose PPI for 2 weeks to determine whether GERD may be contributing to her symptoms, and offer to help her explore counseling options to address her emotional stressors.
CORRESPONDENCE
William E. Cayley Jr, MD, MDiv, University of Wisconsin, UW Health Augusta Family Medicine Clinic, 207 West Lincoln, Augusta, WI 54722; [email protected]
› Seek immediate emergency care for patients with chest pain that is exertional, radiating to one or both arms, similar to or worse than prior cardiac chest pain, or associated with nausea, vomiting, or diaphoresis. A
› Be aware that patients with chest pain that is stabbing, pleuritic, positional, or reproducible with palpation are at very low risk for acute coronary syndrome and most likely have chest wall pain. A
› Consider a 2-week course of high-dose proton-pump inhibitor therapy to help identify patients whose chest pain may be from undiagnosed gastroesophageal reflux disease. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Your patient, Amy Z, age 58, was given a diagnosis of hypertension 10 years ago and since then has been maintained on hydrochlorothiazide 50 mg/d and lisinopril 10 mg/d. In the office today, she reports intermittent chest tightness and heaviness. She has no history of coronary artery disease (CAD), cerebrovascular disease, or peripheral vascular disease. She attributes her chest discomfort to emotional stress. She recently started a job after having been unemployed, but still has no health insurance and is concerned about losing her house.
She denies orthopnea and resting or exertional dyspnea, and says she never gets chest pain while climbing stairs. Her blood pressure is elevated at 180/110 mm Hg, but her other vital signs are normal (pulse, 70 beats per minute; respiratory rate, 18 breaths per minute). On physical examination, she has no venous distension in her neck and her lungs are clear. A cardiac exam reveals a regular rate and rhythm, with a normally split S1 and S2 and no murmurs, rubs, or gallops. Palpation of the chest does not reproduce her chest pain.
You are concerned that your patient’s chest pain could be from heart disease, but she wants to defer additional testing because of the cost, stating, “It’s all due to my stress.”
How would you proceed?
Musculoskeletal chest wall pain is the most common cause of chest pain in patients who seek treatment in the office, followed by GI disease and stable heart disease.
Whether they go to the emergency department (ED) or to their family physician’s office, most patients who seek treatment for chest pain don’t have life-threatening cardiac illness. Of the 8 million patients who visit an ED for chest pain each year, only 13% are diagnosed with acute coronary syndrome (ACS).1,2 Among those seen for chest pain in a primary care office, only a minority (approximately 1.5%) have unstable heart disease.3-5 Cross-sectional studies indicate that musculoskeletal chest wall pain (or “chest wall syndrome [CWS]”) is the most common cause of chest pain in patients who seek treatment in the office, followed by gastrointestinal (GI) disease, stable heart disease, psychosocial or psychiatric conditions, pulmonary disease, and other cardiovascular conditions (TABLE 1).3,6,7
When evaluating patients with chest pain in the office, the challenge is to appropriately evaluate and manage those who are at low risk of ACS, while at the same time identifying and arranging prompt transfer or referral for the minority of patients who are at high cardiac risk. This article describes how to determine which patients require emergency treatment, which tools to use to screen for ACS and other potential causes of chest pain, and how to proceed when initial evaluation and testing do not point to a clear diagnosis.
Start with the ABCs
When a patient presents in primary care with a chief complaint of chest pain, it’s of course critical that you quickly determine if he or she is stable by evaluating the “ABCs” (airway, breathing, and circulation). Any potentially unstable patient should be immediately transferred for emergency care.8 A patient who shows no signs of respiratory distress and whose vital signs are within a normal range is unlikely to be acutely unstable, and can be further evaluated in the office.
If the patient is stable, obtain a history of the onset and evolution of the chest pain, especially its location, quality, duration, and aggravating or alleviating factors. Also ask about a personal or family history of heart disease, hypertension, diabetes, or hypercholesterolemia, and about tobacco use. While the presence of any of these cardiac risk factors may increase suspicion for a cardiac cause for chest pain, the absence of such factors does not eliminate the need for a careful diagnostic evaluation.
Patients with “typical” chest pain have a higher risk of ACS. In a 2005 review of observational prospective and retrospective studies and systematic reviews, Swap et al9 corroborated the description of “typical” anginal chest pain, indicating that patients whose chest pain is exertional, radiating to one or both arms, similar to or worse than prior cardiac chest pain, or associated with nausea, vomiting, or diaphoresis are at high risk for ACS (TABLE 2).9 These researchers also found that chest pain that is stabbing, pleuritic, positional, or reproducible with palpation suggests that a patient is at low risk for ACS. Pain that is not exertional or that is in a small inframammary area of the chest also suggests a low risk for ACS.9
Marburg Heart Score and other tests can help rule out ACS
As part of your initial physical examination, assess the patient’s overall condition and stability. Be aware, however, that an older literature review found that a physical exam is only minimally helpful in assessing ACS risk in a patient with chest pain. Findings that may increase the risk of ACS are a third heart sound (positive likelihood ratio [LR+] = 3.2; 95% confidence interval [CI], 1.6-6.5), systolic blood pressure <80 mm/Hg (LR+ = 3.1; 95% CI, 1.8-5.2), and pulmonary crackles on auscultation (LR+ = 2.1; 95% CI, 1.4–3.1); however, the absence of these findings does not exclude ACS.10 The most helpful sign or symptom in evaluating a patient with chest pain is chest wall tenderness on palpation, which largely rules out ACS in low-prevalence settings, such as a primary care office.11
Bösner et al12 developed the Marburg Heart Score (MHS) to help primary care physicians evaluate the risk of CAD in patients with chest pain (TABLE 3).12,13 A subsequent validation study found that an MHS ≥3 had a sensitivity of 89.1% (95% CI, 81.1%-94%) and a specificity of 63.5% (95% CI, 60%-66.9%) for CAD.13 The test’s negative predictive value (NPV) of 97.9% (95% CI, 96.2%-98.9%) means that patients with an MHS ≤2 are very unlikely to have CAD; however, the low positive predictive value (PPV) of only 23.3% (95% CI, 19.2%-28.0%) means an MHS ≥3 is not particularly helpful in diagnosing CAD.12,13
Unless it is clear that your patient’s chest pain is unlikely to have a cardiac cause (eg, pain is reproducible on palpation, or an MHS ≤2), order an electrocardiogram (EKG). If the EKG shows ST-segment elevation in 2 or more contiguous leads, presumed new left bundle branch block, ischemic ST-segment depression >.5 mm (.05 mV), or dynamic T-wave inversion with pain or discomfort, the patient needs urgent referral for emergency care.8 If the EKG is nondiagnostic but the chest pain is suspicious for CAD, then further testing with cardiac biomarkers (eg, troponin I or T) is recommended to evaluate for non-ST elevation myocardial infarction. Consider chest radiography if there is evidence of respiratory disease (cough, dyspnea, or a history of pulmonary disease).
Don’t overlook chest wall syndrome, GERD, or panic disorder
There are several conditions to consider in the differential diagnosis of patients whose chest pain does not appear to have a cardiac cause:
CWS is the most common cause of chest pain in primary care patients.14,15 While there are several specific types of chest wall pain—including musculoskeletal pain, parietal or intercostal pain, Tietze’s syndrome, and costochondral pain—all are manifestations of a musculoskeletal disorder and associated with tenderness of the chest wall. CWS is not life threatening, but one study found high rates of anxiety (54%-93%) among patients with moderate to severe CWS.14,15
Few trials have evaluated treatments for chest wall pain or costochondritis, though typical recommendations include nonsteroidal anti-inflammatory medications, use of heat or cold, physical therapy, or injection of local anesthetic.16 One study found that stretching exercises might benefit patients with costochondritis.17
GI disorders. Patients with esophagitis or gastroesophageal reflux disease (GERD) often report heartburn, chronic cough, chronic laryngitis, and asthma.18 However, the sensitivity and specificity of these symptoms are too low to allow diagnosis or exclusion of GERD based on history alone.18
Acid suppression therapy can be used to test for GERD. A 2005 meta-analysis of 6 studies found the sensitivity and specificity of a proton-pump inhibitor (PPI) acid suppression test for the diagnosis of GERD in patients with noncardiac chest pain were 80% (95% CI, 71%-87%) and 74% (95% CI, 64%-83%), respectively.19 One study demonstrated that relief of chest pain after a 14-day course of omeprazole 40 mg/d was more sensitive than endoscopy, manometry, or 24-hour esophageal pH monitoring in diagnosing GERD.20 Another study found that in patients with noncardiac chest pain and normal upper endoscopy, symptomatic relief with lansoprazole 30 mg/d for 4 weeks can be used to diagnose endoscopy-negative GERD.21
It is appropriate to try a high-dose course of a PPI (ie, omeprazole 40 mg twice daily, lansoprazole 30 mg/d, or esomeprazole 40 mg twice daily) to evaluate for GERD as the cause of chest pain in patients who:20-22
• do not initially describe typical reflux symptoms (eg, heartburn, chronic regurgitation, chronic cough, or a sore or burning throat)
• have no history of surgery in the upper GI tract, esophagus, or thorax, and
• have no signs or symptoms that indicate they have a serious or malignant disease (eg, weight loss, anemia, or dysphagia).
Panic disorder. Several tools have been proposed for screening for panic disorder (PD),23,24 but none have been tested in patients with chest pain. Dammen et al25 developed a 3-item questionnaire to assess for PD among patients with chest pain who were referred for cardiac evaluation (TABLE 4).25 A score ≥5 on the Dammen questionnaire had 55% sensitivity and 86% specificity for PD, with a PPV of 71% and an NPV of 76%.25 Although this instrument has not been subjected to validation studies, using it may help clarify whether further investigation for PD is warranted.
Psychotherapeutic interventions may be effective for patients whose chest pain is caused by PD. A Cochrane review of 15 randomized controlled trials of psychological interventions for chest pain in patients with normal coronary anatomy found that cognitive-behavior therapy, and possibly hypnotherapy, reduced patient reports of chest pain, reduced chest pain frequency, and increased the number of chest pain-free days, at least for 3 months.26
What to do when the diagnosis remains unclear
When your initial evaluation and diagnostic testing yield no clear diagnosis, appropriate follow-up is vital because in the year after primary care patients first develop chest pain, they are 1.5 to 3 times more likely than the general population to be diagnosed with musculoskeletal, GI, psychological, or respiratory problems, nearly 5 times as likely to be diagnosed with heart failure, and nearly 15 times as likely to be diagnosed with coronary heart disease.27,28
Consider ordering exercise or chemical stress testing within 3 to 7 days for a patient with chest pain that suggests ACS but who has normal results on EKG and biomarker testing.8 Interestingly, though, in a study of 4181 patients in an ED chest pain unit who had 2 sets of normal serum troponins during a 6-hour period followed by exercise or chemical stress testing, only 470 patients (11%) had abnormal stress test results and only 37 (.9%) had obstructive CAD that would have potentially benefited from revascularization.29 Thus, testing troponin levels twice over 6 hours is a reasonable alternative to stress testing for a primary care patient with chest pain; stress testing would be unnecessary if both troponin values were normal.
CASE › Based on her current chest pain symptoms, Ms. Z’s MHS is a reassuringly low 1, so CAD is unlikely. However, she scores 5 on the Dammen panic disorder screen. Due to her financial concerns, you decide to forgo stress testing and instead draw a serum troponin now, with plans to repeat later in the afternoon at your clinic lab if the initial result is normal. You encourage her to try a high-dose PPI for 2 weeks to determine whether GERD may be contributing to her symptoms, and offer to help her explore counseling options to address her emotional stressors.
CORRESPONDENCE
William E. Cayley Jr, MD, MDiv, University of Wisconsin, UW Health Augusta Family Medicine Clinic, 207 West Lincoln, Augusta, WI 54722; [email protected]
1. Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122:1756-7176.
2. Bhuiya FA, Pitts SR, McCaig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999-2008. NCHS Data Brief. 2010;43:1-8.
3. Klinkman MS, Stevens D, Gorenflo DW. Episodes of care for chest pain: a preliminary report from MIRNET. Michigan Research Network. J Fam Pract. 1994;38:345-352.
4. McConaghy JR, Oza RS. Outpatient diagnosis of acute chest pain in adults. Am Fam Physician. 2013;87:177-82.
5. Nilsson S, Scheike M, Engblom D, et al. Chest pain and ischaemic heart disease in primary care. Br J Gen Pract. 2003;53:378-382.
6. Buntinx F, Knockaert D, Bruyninckx R, et al. Chest pain in general practice or in the hospital emergency department: is it the same? Fam Pract. 2001;18:586-589.
7. Jonsbu E, Dammen T, Morken G, et al. Cardiac and psychiatric diagnoses among patients referred for chest pain and palpitations. Scand Cardiovasc J. 2009;43:256-259.
8. O’Connor RE, Brady W, Brooks SC, et al. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 suppl 3):S787-S817.
9. Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005;294:2623-2629.
10. Panju AA, Hemmelgarn BR, Guyatt GH, et al. The rational clinical examination. Is this patient having a myocardial infarction? JAMA. 1998;280:1256-1263.
11. Bruyninckx R, Aertgeerts B, Bruyninckx P, et al. Signs and symptoms in diagnosing acute myocardial infarction and acute coronary syndrome: a diagnostic meta-analysis. Br J Gen Pract. 2008;58:105-111.
12. Bösner S, Haasenritter J, Becker A, et al. Ruling out coronary artery disease in primary care: development and validation of a simple prediction rule. CMAJ. 2010;182:1295-1300.
13. Haasenritter J, Bösner S, Vaucher P, et al. Ruling out coronary heart disease in primary care: external validation of a clinical prediction rule. Br J Gen Pract. 2012;62:e415-e421.
14. Bösner S, Becker A, Hani MA, et al. Chest wall syndrome in primary care patients with chest pain: presentation, associated features and diagnosis. Fam Pract. 2010;27:363-369.
15. Verdon F, Burnand B, Herzig L, et al. Chest wall syndrome among primary care patients: a cohort study. BMC Fam Pract. 2007;8:51.
16. Proulx AM, Zryd TW. Costochondritis: diagnosis and treatment. Am Fam Physician. 2009;80:617-620.
17. Rovetta G, Sessarego P, Monteforte P. Stretching exercises for costochondritis pain. G Ital Med Lav Ergon. 2009;31:169-171.
18. Lacy BE, Weiser K, Chertoff J, et al. The diagnosis of gastroesophageal reflux disease. Am J Med. 2010;123: 583-592.
19. Wang WH, Huang JQ, Zheng GF, et al. Is proton pump inhibitor testing an effective approach to diagnose gastroesophageal reflux disease in patients with noncardiac chest pain?: a metaanalysis. Arch Intern Med. 2005;165:1222-1228.
20. Pandak WM, Arezo S, Everett S, et al. Short course of omeprazole: a better first diagnostic approach to noncardiac chest pain than endoscopy, manometry, or 24-hour esophageal pH monitoring. J Clin Gastroenterol. 2002;35:307-314.
21. Xia HH, Lai KC, Lam SK, et al. Symptomatic response to lansoprazole predicts abnormal acid reflux in endoscopy-negative patients with non-cardiac chest pain. Aliment Pharmacol Ther. 2003;17:369-377.
22. Flook NW, Moayyedi P, Dent J, et al. Acid-suppressive therapy with esomeprazole for relief of unexplained chest pain in primary care: a randomized, double-blind, placebo-controlled trial. Am J Gastroenterol. 2013;108:56-64.
23. Stein MB, Roy-Byrne PP, McQuaid JR, et al. Development of a brief diagnostic screen for panic disorder in primary care. Psychosom Med. 1999;61:359-364.
24. Ballenger JC. Treatment of panic disorder in the general medical setting. J Psychosom Res. 1998;44:5-15.
25. Dammen T, Ekeberg O, Arnesen H, et al. The detection of panic disorder in chest pain patients. Gen Hosp Psychiatry. 1999;21:323-332.
26. Kisely SR, Campbell LA, Yelland MJ, et al. Psychological interventions for symptomatic management of non-specific chest pain in patients with normal coronary anatomy. Cochrane Database Syst Rev. 2012;6:CD004101.
27. Ruigómez A, Rodríguez LA, Wallander MA, et al. Chest pain in general practice: incidence, comorbidity and mortality. Fam Pract. 2006;23:167-174.
28. Ruigómez A, Massó-González EL, Johansson S, et al. Chest pain without established ischaemic heart disease in primary care patients: associated comorbidities and mortality. Br J Gen Pract. 2009;59:e78-e86.
29. Hermann LK, Newman DH, Pleasant WA, et al. Yield of routine provocative cardiac testing among patients in an emergency department-based chest pain unit. JAMA Intern Med. 2013;173:1128-1133.
1. Amsterdam EA, Kirk JD, Bluemke DA, et al; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122:1756-7176.
2. Bhuiya FA, Pitts SR, McCaig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999-2008. NCHS Data Brief. 2010;43:1-8.
3. Klinkman MS, Stevens D, Gorenflo DW. Episodes of care for chest pain: a preliminary report from MIRNET. Michigan Research Network. J Fam Pract. 1994;38:345-352.
4. McConaghy JR, Oza RS. Outpatient diagnosis of acute chest pain in adults. Am Fam Physician. 2013;87:177-82.
5. Nilsson S, Scheike M, Engblom D, et al. Chest pain and ischaemic heart disease in primary care. Br J Gen Pract. 2003;53:378-382.
6. Buntinx F, Knockaert D, Bruyninckx R, et al. Chest pain in general practice or in the hospital emergency department: is it the same? Fam Pract. 2001;18:586-589.
7. Jonsbu E, Dammen T, Morken G, et al. Cardiac and psychiatric diagnoses among patients referred for chest pain and palpitations. Scand Cardiovasc J. 2009;43:256-259.
8. O’Connor RE, Brady W, Brooks SC, et al. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 suppl 3):S787-S817.
9. Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005;294:2623-2629.
10. Panju AA, Hemmelgarn BR, Guyatt GH, et al. The rational clinical examination. Is this patient having a myocardial infarction? JAMA. 1998;280:1256-1263.
11. Bruyninckx R, Aertgeerts B, Bruyninckx P, et al. Signs and symptoms in diagnosing acute myocardial infarction and acute coronary syndrome: a diagnostic meta-analysis. Br J Gen Pract. 2008;58:105-111.
12. Bösner S, Haasenritter J, Becker A, et al. Ruling out coronary artery disease in primary care: development and validation of a simple prediction rule. CMAJ. 2010;182:1295-1300.
13. Haasenritter J, Bösner S, Vaucher P, et al. Ruling out coronary heart disease in primary care: external validation of a clinical prediction rule. Br J Gen Pract. 2012;62:e415-e421.
14. Bösner S, Becker A, Hani MA, et al. Chest wall syndrome in primary care patients with chest pain: presentation, associated features and diagnosis. Fam Pract. 2010;27:363-369.
15. Verdon F, Burnand B, Herzig L, et al. Chest wall syndrome among primary care patients: a cohort study. BMC Fam Pract. 2007;8:51.
16. Proulx AM, Zryd TW. Costochondritis: diagnosis and treatment. Am Fam Physician. 2009;80:617-620.
17. Rovetta G, Sessarego P, Monteforte P. Stretching exercises for costochondritis pain. G Ital Med Lav Ergon. 2009;31:169-171.
18. Lacy BE, Weiser K, Chertoff J, et al. The diagnosis of gastroesophageal reflux disease. Am J Med. 2010;123: 583-592.
19. Wang WH, Huang JQ, Zheng GF, et al. Is proton pump inhibitor testing an effective approach to diagnose gastroesophageal reflux disease in patients with noncardiac chest pain?: a metaanalysis. Arch Intern Med. 2005;165:1222-1228.
20. Pandak WM, Arezo S, Everett S, et al. Short course of omeprazole: a better first diagnostic approach to noncardiac chest pain than endoscopy, manometry, or 24-hour esophageal pH monitoring. J Clin Gastroenterol. 2002;35:307-314.
21. Xia HH, Lai KC, Lam SK, et al. Symptomatic response to lansoprazole predicts abnormal acid reflux in endoscopy-negative patients with non-cardiac chest pain. Aliment Pharmacol Ther. 2003;17:369-377.
22. Flook NW, Moayyedi P, Dent J, et al. Acid-suppressive therapy with esomeprazole for relief of unexplained chest pain in primary care: a randomized, double-blind, placebo-controlled trial. Am J Gastroenterol. 2013;108:56-64.
23. Stein MB, Roy-Byrne PP, McQuaid JR, et al. Development of a brief diagnostic screen for panic disorder in primary care. Psychosom Med. 1999;61:359-364.
24. Ballenger JC. Treatment of panic disorder in the general medical setting. J Psychosom Res. 1998;44:5-15.
25. Dammen T, Ekeberg O, Arnesen H, et al. The detection of panic disorder in chest pain patients. Gen Hosp Psychiatry. 1999;21:323-332.
26. Kisely SR, Campbell LA, Yelland MJ, et al. Psychological interventions for symptomatic management of non-specific chest pain in patients with normal coronary anatomy. Cochrane Database Syst Rev. 2012;6:CD004101.
27. Ruigómez A, Rodríguez LA, Wallander MA, et al. Chest pain in general practice: incidence, comorbidity and mortality. Fam Pract. 2006;23:167-174.
28. Ruigómez A, Massó-González EL, Johansson S, et al. Chest pain without established ischaemic heart disease in primary care patients: associated comorbidities and mortality. Br J Gen Pract. 2009;59:e78-e86.
29. Hermann LK, Newman DH, Pleasant WA, et al. Yield of routine provocative cardiac testing among patients in an emergency department-based chest pain unit. JAMA Intern Med. 2013;173:1128-1133.