User login
Amniotic fluid embolism (AFE) occurs in about 1 in 20,000 to 1 in 40,000 deliveries.1,2 Although the condition is rare, the case fatality rate is high, and AFE is a common cause of maternal death in developed countries. AFE cannot be predicted or prevented. Moreover, the condition is difficult to precisely define and is often a diagnosis of exclusion.
AFE should be considered in the differential diagnosis of a pregnant woman with sudden onset of shortness of breath, hypotension, or cardiac arrhythmia or arrest, followed by coagulopathy and hemorrhage. Premonitory symptoms, including restlessness, confusion, disorientation, agitation, chills, nausea, numbness, and tingling, are commonly reported just before the cardiorespiratory collapse. AFE is less likely if the initial obstetric event is hemorrhage in the absence of cardiorespiratory compromise or a preceding coagulopathy.3
Typically, the onset is just before birth, during birth, or within the first few hours after delivery. In the United Kingdom, which has a robust centralized registry for reporting AFE, about 56% of cases occur before birth and 44% after birth.4
Related article: Is the incidence of amniotic fluid embolism rising? John T. Repke, MD (Examining the Evidence, August 2010)
The resources available to obstetric units vary greatly. Each unit needs to assess its resources and develop an AFE treatment protocol that builds on the unique strengths of the unit. Treatment of AFE requires the coordinated actions of anesthesiologists, obstetricians, nurses, the blood bank, pharmacy, and cardiovascular specialists. Coordinated activity among the members of such a large multidisciplinary team requires a written protocol that is practiced on a regular basis.
Six important components of a multidisciplinary response to AFE treatment protocol are:
- high-quality cardiopulmonary resuscitation (CPR)
- a protocol for massive transfusion
- treatment of diffuse bleeding and coagulopathy
- treatment of uterine and pelvic bleeding
- extracorporeal lung and heart support
- post-AFE intensive care.
1. Initiate high-quality CPR
Hypotension and hypoxemia due to cardiac and pulmonary dysfunction are prominent features of AFE. Dysrythmias such as pulseless electrical activity, bradycardia, ventricular fibrillation, and asystole are common. Rapid institution of high-quality CPR is critical to the survival of women with AFE.
Interventions often used in CPR of patients with AFE include initiation of high-quality chest compressions, early defibrillation if indicated, immediate administration of 100% oxygen by mask ventilation followed by early intubation, and rapid establishment of peripheral, arterial, and central venous access. Volume assessment, fluid replacement, and administration of vasopressors and inotropes are also important.
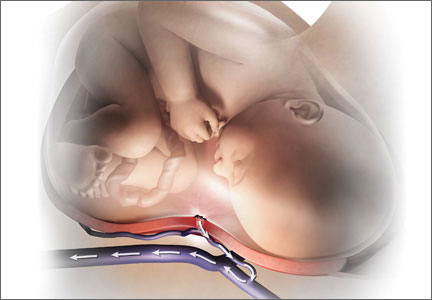
CPR of pregnant women requires special interventions, including maximal left lateral displacement of the uterus to reduce compression of the descending aorta and vena cava. Lateral displacement of the uterus can be accomplished by left lateral tilt or by manual uterine displacement. To optimize the effectiveness of chest compressions, many experts recommend placing the woman in a supine position and using manual uterine displacement rather than a left lateral tilt.5 For chest compressions, the hands should be placed just above the center of the sternum to adjust for the elevation of the diaphragm caused by the gravid uterus.
The gravid uterus can compromise the effectiveness of CPR. Fetal viability and neurologic outcome are best if delivery occurs within 5 minutes of the onset of cardiopulmonary arrest. If the gestational age of the fetus is consistent with extrauterine viability and initial CPR has not restored cardiac function, it is best to initiate fetal delivery within 4 minutes of the onset of cardiopulmonary arrest with the intent to deliver the fetus within 5 minutes.6,7 If the fetus is beyond 20 weeks’ gestational age, delivery early in the course of CPR improves the effectiveness of maternal resuscitation and may increase the probability of maternal survival.
In one study of the response of anesthesiologists, obstetricians, and nurses to a simulated cardiac arrest caused by an AFE, the participants did not routinely use defibrillation when indicated, did not place a firm support under the back for chest compressions, and did not switch the provider of chest compressions every 2 minutes.8 This study indicates that additional training and routinely scheduled multidisciplinary simulation of the response to cardiopulmonary arrest could improve the quality of our CPR.
2. Use a massive transfusion protocol
Severe coagulopathy and diffuse bleeding are commonly encountered in AFE. Target goals for the replacement of blood products include:
- hemoglobin concentration ≥8 g/dL
- fibrinogen ≥150 to 200 mg/dL
- platelets ≥50,000/μL
- prothrombin time international normalized ratio (INR) ≤1.5.
Most massive transfusion protocols provide for the rapid delivery of 4 to 8 units of red blood cells and a similar number of units of fresh frozen plasma to the patient’s bedside. In the management of AFE, 20 to 30 units of red blood cells and a similar quantity of fresh frozen plasma may need to be transfused. Cryoprecipitate takes 20 to 30 minutes to thaw, so preparations to transfuse cryoprecipitate should be initiated as soon as the massive transfusion protocol is triggered. A case of AFE can completely empty the blood bank of all available blood products and necessitate the use of alternative agents.
Lyophilized fibrinogen concentrate (RiaSTAP) is approved by the US Food and Drug Administration for the treatment of congenital hypofibrinogenemia and also may be useful to replace fibrinogen in cases of AFE. In many hospitals, large quantities of fresh frozen plasma are not immediately available; lyophilized fibrinogen concentrate may be especially useful in these settings. Another advantage of fibrinogen concentrate is that large amounts of fibrinogen can be administered in a small volume of intravenous fluid. Fibrinogen concentrate typically is used at a dose of 70 mg/kg of body weight.9,10
Intraoperative red cell salvage occasionally is used in cases of obstetric hemorrhage. In one case report of the use of red cell salvage with leukocyte depletion filtration during treatment of an AFE, acute hypotension developed in the patient after the transfusion of salvaged red cells.11 This case report raises safety concerns about the use of salvaged cells in women with severe AFE.
Related article: 10 practical, evidence-based recommendations for the management of severe postpartum hemorrhage Baha M. Sibai, MD (June 2011)
3. Treat diffuse bleeding and coagulopathy
In addition to the initiation of the massive transfusion protocol, additional treatments that may be helpful in managing the coagulopathy of AFE include tranexamic acid, recombinant factor VIIa (rFVIIa), and exchange transfusion.
AFE is often associated with hyperfibrinolysis, which can cause excessive bleeding.12 Tranexamic acid blocks the lysine binding sites on plasminogen and thereby reduces the lysis of fibrin clots. Clinical trials in patients who have undergone trauma have demonstrated that the administration of tranexamic acid reduces blood loss.13 The dose of tranexamic acid is approximately 10 to 20 mg/kg of body weight, or approximately 1 g.
Controversy exists about the use of rFVIIa to treat the coagulopathy and bleeding caused by AFE. Some authorities believe that rFVIIa is associated with an increased AFE case fatality rate.14 Other authorities believe rFVIIa may be useful in the treatment of AFE coagulopathy, especially when bleeding persists despite aggressive blood and component replacement.”15 The dose of rFVIIa is approximately 90 µg/kg of body weight. rFVIIa is extremely expensive.
Exchange transfusion has been used successfully to treat AFE.16 In women with AFE, exchange transfusion removes circulating cells, cell fragments, and substances that trigger systemic anaphylaxis and coagulopathy, thereby enhancing rapid recovery.
Related article: Act fast when confronted by a coagulopathy postpartum Robert L. Barbieri, MD (Editorial; March 2012)
4. Treat uterine and pelvic bleeding
Obstetrician-gynecologists are experts in the control of uterine and pelvic bleeding. Interventions that commonly are used to control uterine and pelvic bleeding in cases of postpartum hemorrhage, uterine rupture, or placenta accreta also can be applied in cases of AFE with uncontrolled uterine and pelvic bleeding. These techniques include:
- use of uterine compression sutures
- the Bakri balloon
- a uterine tourniquet
- vascular clamps on the ovarian vessels.17,18
In many cases of AFE, total or supracervical hysterectomy is necessary to control uterine bleeding. Uterine artery embolization, if available, has been reported to be helpful in select cases. However, many women with AFE are too unstable to survive transfer to an interventional radiology suite. Additional interventions to control bleeding include hypogastric artery ligation, infrarenal aortic compression, and pelvic packing.
Cross-clamping the aorta below the renal vessels can reduce blood flow to the pelvis and provide time for cardiopulmonary and volume resuscitation. Alternatively, placing pressure on the infrarenal aorta with a sponge or directly by hand can help reduce blood flow to the pelvis.19
In many cases of AFE, pelvic hemorrhage is difficult to control. Even if surgical pedicles are ligated securely, the coagulopathy of AFE may cause persistent oozing from areas of minor tissue trauma. Uncontrolled blood loss can be a proximate cause of death in women with AFE. All written protocols for responding to an AFE should include a plan to use pelvic packing for patients in whom standard operative procedures do not produce adequate control of bleeding. A “mushroom,” “parachute,” or “umbrella” pack has been reported to help stabilize the severely ill patient with pelvic bleeding and permit effective resuscitation and blood product replacement.20
Related articles:
A stitch in time: The B-Lynch, Hayman and Pereira uterine compression sutures Robert L. Barbieri, MD (Editorial, December 2012)
Have you made the best use of the Bakri balloon in PPH? Robert L. Barbieri, MD (Editorial, July 2011)
5. Consider extracorporeal lung and heart support
In many cases of AFE, both lung and cardiac function are severely compromised. Both veno-arterial extracorporeal membrane oxygenation (VA-ECMO) and full cardiopulmonary bypass provide support for the failing lung and heart. Based on a small number of case reports, extracorporeal lung and heart support appear to be useful in the treatment of AFE.21–26 Using the Seldinger technique,27 it is technically feasible to rapidly access a major vein and artery to provide the input and output ports for VA-ECMO. Unlike the cardiopulmonary bypass pump, the VA-ECMO pump does not have a reservoir that needs to be primed with blood and is smaller and more portable. To provide a patient with VA-ECMO or cardiopulmonary bypass, a cardiac interventionist and a perfusionist must be available. Extracorporeal lung and heart support require heparinization of the patient’s blood, which may result in increased bleeding. Both VA-ECMO and cardiopulmonary bypass, along with the diseases for which they are used, may cause renal dysfunction, neurologic injury, and infection.28
Alternative approaches that provide support of the heart—but not lung—are the Impella pump, TandemHeart, and the intra-aortic balloon pump. An alternative that provides lung support—but not cardiac support—is veno-venous ECMO.
In developing a written protocol for responding to an AFE, obstetricians should explore the potential availability of VA-ECMO, cardiopulmonary bypass, or other cardiopulmonary support devices as options for patients who have not responded to standard treatment of AFE and are at high risk of death.
6. Post-AFE intensive care
After stabilization, most women with AFE will require intensive care for 48 to 96 hours. Some experts have proposed that all survivors of cardiopulmonary arrest who are successfully resuscitated and stabilized be transferred to hospitals that specialize in post−cardiac arrest care to improve outcomes.
Assessment of organ injury is important after an AFE. In addition, encephalopathy is a common complication of AFE, and sequential neurologic examination is a priority. Therapeutic hypothermia (TH) may help to preserve neurologic function after AFE.29 However, TH may cause a mild coagulopathy by inhibiting platelet activation and enzyme activity of clotting factors. Because coagulopathy is a prominent feature of AFE, TH may be contraindicated if the patient has a clinically significant baseline coagulopathy.30
DEVELOP AN AFE PROTOCOL AND PRACTICE THE COMPONENTS
Practicing the components of obstetric protocols can improve unit performance and patient outcomes.31 The components of an AFE protocol, as described in this article, include high-quality CPR, a protocol for massive transfusion, treatment of diffuse bleeding and coagulopathy, treatment of uterine and pelvic bleeding, extracorporeal lung and heart support, and post-AFE intensive care. Practicing these components of an AFE protocol will enhance performance across many common obstetric complications including postpartum hemorrhage, uterine rupture, placenta accreta, and pulmonary embolism.
When Chesley “Sully” Sullenberger and his copilot landed Flight 1549 in the Hudson River in New York, he had never practiced that specific response to twin engine failure, but he had practiced many emergency responses involving related scenarios. The combination of exceptional flight experience and years of practicing the response to emergency scenarios in simulation exercises permitted him and his copilot to execute a uniquely clever plan to solve a life-threatening
emergency. In a related way, practicing the components of AFE treatment will help obstetricians, obstetric anesthesiologists, and their multidisciplinary team to improve the responses to all major obstetric emergencies.
INSTANT POLL
Does your obstetric unit have a written protocol for treating an amniotic fluid embolism (AFE)? Has your obstetric unit practiced any of the components of the AFE treatment protocol: 1) high-quality cardiopulmonary resuscitation, 2) a protocol for massive transfusion protocol, 3) treatment of diffuse bleeding and coagulopathy, 4) treatment of uterine and pelvic bleeding, 5) extracorporeal lung and heart support, and 6) post-AFE intensive care?
Tell us—at [email protected]. Please include your name and the city and state in which you practice.
- Kramer MS, Rouleau J, Baskett TF, Joseph KS; Maternal Health Study Group of the Canadian Perinatal Surveillance System. Amniotic-fluid embolism and medical induction of labour: A retrospective, population-based cohort study. Lancet. 2006;368(9545):1444–1448.
- Abenhaim HA, Azoulay L, Kramer MS, Leduc L. Incidence and risk factors of amniotic fluid embolism: A population-based study on 3 million births in the United States. Am J Obstet Gynecol. 2008;199(1):49.e1–49.e8.
- Tuffnell D, Knight M, Plaat F. Amniotic fluid embolism—An update. Anaesthesia. 2011;66(1):3–6.
- Knight M, Tuffnell D, Brocklehurst P, Spark P, Kurinczuk JJ; UK Obstetric Surveillance System. Incidence and risk factors for amniotic-fluid embolism. Obstet Gynecol. 2010;115(5):910–917.
- Kundra P, Khanna S, Habeebullahg S, Ravishankar M. Manual displacement of the uterus during Caesarean section. Anaesthesia. 2007;62(5):460–465.
- Katz VL, Dotters DJ, Droegemueller W. Perimortem cesarean delivery. Obstet Gynecol. 1986;68(4):571–576.
- Katz V, Balderston K, DeFreest M. Perimortem cesarean delivery: Were our assumptions correct? Am J Obstet Gynecol. 2005;192(6):1916–1920.
- Lipman SS, Daniels KI, Carvalho B, et al. Deficits in the provision of cardiopulmonary resuscitation during simulated obstetric crises. Am J Obstet Gynecol. 2010;203(2):179.e1–179.e5.
- Bell SF, Rayment R, Collins PW, Collis RE. The use of fibrinogen concentrate to correct hypofibrinogenaemia rapidly during obstetric haemorrhage. Int J Obstet Anesth. 2010;19(2):218–223.
- Sorensen B, Tang M, Larsen OH, Laursen PN, Fenger-Eriksen C, Rea CJ. The role of fibrinogen: A new paradigm in the treatment of coagulopathic bleeding. Thromb Res. 2011;128(Suppl 1):S13–S16.
- Rogers WK, Wernimont SA, Kumar GC, Bennett E, Chestnut DH. Acute hypotension associated with intraoperative cell salvage using a leukocyte depletion filter during management of obstetric hemorrhage due to amniotic fluid embolism. Anesth Analg. 2013;117(2):449–452.
- Collins NF, Bloor M, McDonnell NJ. Hyperfibrinolysis diagnosed by rotational thromboelastometry in a case of suspected amniotic fluid embolism. Int J Obstet Anesth. 2013;22(1):71–76.
- Ker K, Edwards P, Perel P, Shakur H, Roberts I. Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054.
- Leighton BL, Wall MH, Lockhart EM, Phillips LE, Zatta AJ. Use of recombinant factor VIIa in patients with amniotic fluid embolism: A systematic review of case reports. Anesthesiology. 2011;115(6):1201–1208.
- Huber AW, Raio L, Alberio L, Ghezzi F, Surbek DV. Recombinant human factor VIIa prevents hysterectomy in severe postpartum hemorrhage: single center study. J Perinat Med. 2011;40(1):43–49.
- Dodgson J, Martin J, Boswell J, Goodall HB, Smith R. Probable amniotic fluid embolism precipitated by amniocentesis and treated by exchange transfusion. Brit Med J (Clin Res Ed). 1987;294(6583):1322–1323.
- Barbieri RL. A stitch in time: The B-Lynch, Hayman and Pereira uterine compression sutures. OBG Manage. 2012;24(12):6, 8, 10, 11.
- Barbieri RL. Have you made the best use of the Bakri balloon in PPH? OBG Manage. 2011;23(7):6, 8, 9.
- Belfort MA, Zimmerman J, Schemmer G, Oldroyd R, Smilanich R, Pearce M. Aortic compression and cross clamping in a case of placenta percreta and amniotic fluid embolism: A case report. AJP Rep. 2011;1(1):33–36.
- Dildy GA, Scott JR, Saffer CS, Belfort MA. An
effective pressure pack for severe pelvic hemorrhage. Obstet Gynecol. 2006;108(5):1222–1226. - Stanten RD, Iverson LI, Daugharty TM, Lovett SM, Terry C, Blumenstock E. Amniotic fluid embolism causing catastrophic pulmonary vasoconstriction: Diagnosis by transesophageal echocardiogram and treatment by cardiopulmonary bypass. Obstet Gynecol. 2003;102(3):496–498.
- Ho CH, Chen KB, Liu SK, Liu YF, Cheng HC, Wu RS. Early application of extracorporeal membrane oxygenation in a patient with amniotic fluid embolism. Acta Anaesthesiol Taiwan. 2009;47(2):99–102.
- Shen HP, Chang WC, Yeh LS, Ho M. Amniotic fluid embolism treated with emergency extracorporeal membrane oxygenation: A case report.
J Reprod Med. 2009;54(11–12):706–708. - Lee PH, Shulman MS, Vellayappan U, Symes JF, Olenchock SA Jr. Surgical treatment of amniotic fluid embolism with cardiopulmonary collapse. Ann Thorac Surg. 2010;90(5):1694–1696.
- Firstenberg MS, Abel E, Blais D, et al. Temporary extracorporeal circulatory support and pulmonary embolectomy for catastrophic amniotic fluid embolism. Heart Surg Forum. 2011;14(3):E157–E159.
- Ecker JL, Solt K, Fitzsimons MG, MacGillivray TE. Case records of the Massachusetts General Hospital. Case 40-2012: A 43-year-old woman with cardiorespiratory arrest after a cesarean section. N Engl J Med. 2012;367(26):2528–2536.
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 1953;39(5):368–376.
- Cheng R, Hachamovitch R, Kittelson M, et al. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: A meta-analysis of 1,866 adult patients. Ann Thorac Surg. 2013; epub Nov 8.
- Rittenberger JC, Kelly E, Jang D, Greer K, Heffner A. Successful outcome utilizing hypothermia after cardiac arrest in pregnancy: A case report. Crit Care Med. 2008;36(4):1354–1356.
- Michelson AD, MacGregor H, Barnard MR, Krestin AS, Rohrer MJ, Valeri CR. Reversible inhibition of human platelet activation by hypothermia in vivo and in vitro. Thromb Haemost. 1994;71(5):633–640.
- Rivzi F, Mackey R, Barrett T, McKenna P, Geary M. Successful reduction of massive postpartum haemorrhage by use of guidelines and staff education. BJOG. 2004;111(5):495–498.
Amniotic fluid embolism (AFE) occurs in about 1 in 20,000 to 1 in 40,000 deliveries.1,2 Although the condition is rare, the case fatality rate is high, and AFE is a common cause of maternal death in developed countries. AFE cannot be predicted or prevented. Moreover, the condition is difficult to precisely define and is often a diagnosis of exclusion.
AFE should be considered in the differential diagnosis of a pregnant woman with sudden onset of shortness of breath, hypotension, or cardiac arrhythmia or arrest, followed by coagulopathy and hemorrhage. Premonitory symptoms, including restlessness, confusion, disorientation, agitation, chills, nausea, numbness, and tingling, are commonly reported just before the cardiorespiratory collapse. AFE is less likely if the initial obstetric event is hemorrhage in the absence of cardiorespiratory compromise or a preceding coagulopathy.3
Typically, the onset is just before birth, during birth, or within the first few hours after delivery. In the United Kingdom, which has a robust centralized registry for reporting AFE, about 56% of cases occur before birth and 44% after birth.4
Related article: Is the incidence of amniotic fluid embolism rising? John T. Repke, MD (Examining the Evidence, August 2010)
The resources available to obstetric units vary greatly. Each unit needs to assess its resources and develop an AFE treatment protocol that builds on the unique strengths of the unit. Treatment of AFE requires the coordinated actions of anesthesiologists, obstetricians, nurses, the blood bank, pharmacy, and cardiovascular specialists. Coordinated activity among the members of such a large multidisciplinary team requires a written protocol that is practiced on a regular basis.
Six important components of a multidisciplinary response to AFE treatment protocol are:
- high-quality cardiopulmonary resuscitation (CPR)
- a protocol for massive transfusion
- treatment of diffuse bleeding and coagulopathy
- treatment of uterine and pelvic bleeding
- extracorporeal lung and heart support
- post-AFE intensive care.
1. Initiate high-quality CPR
Hypotension and hypoxemia due to cardiac and pulmonary dysfunction are prominent features of AFE. Dysrythmias such as pulseless electrical activity, bradycardia, ventricular fibrillation, and asystole are common. Rapid institution of high-quality CPR is critical to the survival of women with AFE.
Interventions often used in CPR of patients with AFE include initiation of high-quality chest compressions, early defibrillation if indicated, immediate administration of 100% oxygen by mask ventilation followed by early intubation, and rapid establishment of peripheral, arterial, and central venous access. Volume assessment, fluid replacement, and administration of vasopressors and inotropes are also important.
CPR of pregnant women requires special interventions, including maximal left lateral displacement of the uterus to reduce compression of the descending aorta and vena cava. Lateral displacement of the uterus can be accomplished by left lateral tilt or by manual uterine displacement. To optimize the effectiveness of chest compressions, many experts recommend placing the woman in a supine position and using manual uterine displacement rather than a left lateral tilt.5 For chest compressions, the hands should be placed just above the center of the sternum to adjust for the elevation of the diaphragm caused by the gravid uterus.
The gravid uterus can compromise the effectiveness of CPR. Fetal viability and neurologic outcome are best if delivery occurs within 5 minutes of the onset of cardiopulmonary arrest. If the gestational age of the fetus is consistent with extrauterine viability and initial CPR has not restored cardiac function, it is best to initiate fetal delivery within 4 minutes of the onset of cardiopulmonary arrest with the intent to deliver the fetus within 5 minutes.6,7 If the fetus is beyond 20 weeks’ gestational age, delivery early in the course of CPR improves the effectiveness of maternal resuscitation and may increase the probability of maternal survival.
In one study of the response of anesthesiologists, obstetricians, and nurses to a simulated cardiac arrest caused by an AFE, the participants did not routinely use defibrillation when indicated, did not place a firm support under the back for chest compressions, and did not switch the provider of chest compressions every 2 minutes.8 This study indicates that additional training and routinely scheduled multidisciplinary simulation of the response to cardiopulmonary arrest could improve the quality of our CPR.
2. Use a massive transfusion protocol
Severe coagulopathy and diffuse bleeding are commonly encountered in AFE. Target goals for the replacement of blood products include:
- hemoglobin concentration ≥8 g/dL
- fibrinogen ≥150 to 200 mg/dL
- platelets ≥50,000/μL
- prothrombin time international normalized ratio (INR) ≤1.5.
Most massive transfusion protocols provide for the rapid delivery of 4 to 8 units of red blood cells and a similar number of units of fresh frozen plasma to the patient’s bedside. In the management of AFE, 20 to 30 units of red blood cells and a similar quantity of fresh frozen plasma may need to be transfused. Cryoprecipitate takes 20 to 30 minutes to thaw, so preparations to transfuse cryoprecipitate should be initiated as soon as the massive transfusion protocol is triggered. A case of AFE can completely empty the blood bank of all available blood products and necessitate the use of alternative agents.
Lyophilized fibrinogen concentrate (RiaSTAP) is approved by the US Food and Drug Administration for the treatment of congenital hypofibrinogenemia and also may be useful to replace fibrinogen in cases of AFE. In many hospitals, large quantities of fresh frozen plasma are not immediately available; lyophilized fibrinogen concentrate may be especially useful in these settings. Another advantage of fibrinogen concentrate is that large amounts of fibrinogen can be administered in a small volume of intravenous fluid. Fibrinogen concentrate typically is used at a dose of 70 mg/kg of body weight.9,10
Intraoperative red cell salvage occasionally is used in cases of obstetric hemorrhage. In one case report of the use of red cell salvage with leukocyte depletion filtration during treatment of an AFE, acute hypotension developed in the patient after the transfusion of salvaged red cells.11 This case report raises safety concerns about the use of salvaged cells in women with severe AFE.
Related article: 10 practical, evidence-based recommendations for the management of severe postpartum hemorrhage Baha M. Sibai, MD (June 2011)
3. Treat diffuse bleeding and coagulopathy
In addition to the initiation of the massive transfusion protocol, additional treatments that may be helpful in managing the coagulopathy of AFE include tranexamic acid, recombinant factor VIIa (rFVIIa), and exchange transfusion.
AFE is often associated with hyperfibrinolysis, which can cause excessive bleeding.12 Tranexamic acid blocks the lysine binding sites on plasminogen and thereby reduces the lysis of fibrin clots. Clinical trials in patients who have undergone trauma have demonstrated that the administration of tranexamic acid reduces blood loss.13 The dose of tranexamic acid is approximately 10 to 20 mg/kg of body weight, or approximately 1 g.
Controversy exists about the use of rFVIIa to treat the coagulopathy and bleeding caused by AFE. Some authorities believe that rFVIIa is associated with an increased AFE case fatality rate.14 Other authorities believe rFVIIa may be useful in the treatment of AFE coagulopathy, especially when bleeding persists despite aggressive blood and component replacement.”15 The dose of rFVIIa is approximately 90 µg/kg of body weight. rFVIIa is extremely expensive.
Exchange transfusion has been used successfully to treat AFE.16 In women with AFE, exchange transfusion removes circulating cells, cell fragments, and substances that trigger systemic anaphylaxis and coagulopathy, thereby enhancing rapid recovery.
Related article: Act fast when confronted by a coagulopathy postpartum Robert L. Barbieri, MD (Editorial; March 2012)
4. Treat uterine and pelvic bleeding
Obstetrician-gynecologists are experts in the control of uterine and pelvic bleeding. Interventions that commonly are used to control uterine and pelvic bleeding in cases of postpartum hemorrhage, uterine rupture, or placenta accreta also can be applied in cases of AFE with uncontrolled uterine and pelvic bleeding. These techniques include:
- use of uterine compression sutures
- the Bakri balloon
- a uterine tourniquet
- vascular clamps on the ovarian vessels.17,18
In many cases of AFE, total or supracervical hysterectomy is necessary to control uterine bleeding. Uterine artery embolization, if available, has been reported to be helpful in select cases. However, many women with AFE are too unstable to survive transfer to an interventional radiology suite. Additional interventions to control bleeding include hypogastric artery ligation, infrarenal aortic compression, and pelvic packing.
Cross-clamping the aorta below the renal vessels can reduce blood flow to the pelvis and provide time for cardiopulmonary and volume resuscitation. Alternatively, placing pressure on the infrarenal aorta with a sponge or directly by hand can help reduce blood flow to the pelvis.19
In many cases of AFE, pelvic hemorrhage is difficult to control. Even if surgical pedicles are ligated securely, the coagulopathy of AFE may cause persistent oozing from areas of minor tissue trauma. Uncontrolled blood loss can be a proximate cause of death in women with AFE. All written protocols for responding to an AFE should include a plan to use pelvic packing for patients in whom standard operative procedures do not produce adequate control of bleeding. A “mushroom,” “parachute,” or “umbrella” pack has been reported to help stabilize the severely ill patient with pelvic bleeding and permit effective resuscitation and blood product replacement.20
Related articles:
A stitch in time: The B-Lynch, Hayman and Pereira uterine compression sutures Robert L. Barbieri, MD (Editorial, December 2012)
Have you made the best use of the Bakri balloon in PPH? Robert L. Barbieri, MD (Editorial, July 2011)
5. Consider extracorporeal lung and heart support
In many cases of AFE, both lung and cardiac function are severely compromised. Both veno-arterial extracorporeal membrane oxygenation (VA-ECMO) and full cardiopulmonary bypass provide support for the failing lung and heart. Based on a small number of case reports, extracorporeal lung and heart support appear to be useful in the treatment of AFE.21–26 Using the Seldinger technique,27 it is technically feasible to rapidly access a major vein and artery to provide the input and output ports for VA-ECMO. Unlike the cardiopulmonary bypass pump, the VA-ECMO pump does not have a reservoir that needs to be primed with blood and is smaller and more portable. To provide a patient with VA-ECMO or cardiopulmonary bypass, a cardiac interventionist and a perfusionist must be available. Extracorporeal lung and heart support require heparinization of the patient’s blood, which may result in increased bleeding. Both VA-ECMO and cardiopulmonary bypass, along with the diseases for which they are used, may cause renal dysfunction, neurologic injury, and infection.28
Alternative approaches that provide support of the heart—but not lung—are the Impella pump, TandemHeart, and the intra-aortic balloon pump. An alternative that provides lung support—but not cardiac support—is veno-venous ECMO.
In developing a written protocol for responding to an AFE, obstetricians should explore the potential availability of VA-ECMO, cardiopulmonary bypass, or other cardiopulmonary support devices as options for patients who have not responded to standard treatment of AFE and are at high risk of death.
6. Post-AFE intensive care
After stabilization, most women with AFE will require intensive care for 48 to 96 hours. Some experts have proposed that all survivors of cardiopulmonary arrest who are successfully resuscitated and stabilized be transferred to hospitals that specialize in post−cardiac arrest care to improve outcomes.
Assessment of organ injury is important after an AFE. In addition, encephalopathy is a common complication of AFE, and sequential neurologic examination is a priority. Therapeutic hypothermia (TH) may help to preserve neurologic function after AFE.29 However, TH may cause a mild coagulopathy by inhibiting platelet activation and enzyme activity of clotting factors. Because coagulopathy is a prominent feature of AFE, TH may be contraindicated if the patient has a clinically significant baseline coagulopathy.30
DEVELOP AN AFE PROTOCOL AND PRACTICE THE COMPONENTS
Practicing the components of obstetric protocols can improve unit performance and patient outcomes.31 The components of an AFE protocol, as described in this article, include high-quality CPR, a protocol for massive transfusion, treatment of diffuse bleeding and coagulopathy, treatment of uterine and pelvic bleeding, extracorporeal lung and heart support, and post-AFE intensive care. Practicing these components of an AFE protocol will enhance performance across many common obstetric complications including postpartum hemorrhage, uterine rupture, placenta accreta, and pulmonary embolism.
When Chesley “Sully” Sullenberger and his copilot landed Flight 1549 in the Hudson River in New York, he had never practiced that specific response to twin engine failure, but he had practiced many emergency responses involving related scenarios. The combination of exceptional flight experience and years of practicing the response to emergency scenarios in simulation exercises permitted him and his copilot to execute a uniquely clever plan to solve a life-threatening
emergency. In a related way, practicing the components of AFE treatment will help obstetricians, obstetric anesthesiologists, and their multidisciplinary team to improve the responses to all major obstetric emergencies.
INSTANT POLL
Does your obstetric unit have a written protocol for treating an amniotic fluid embolism (AFE)? Has your obstetric unit practiced any of the components of the AFE treatment protocol: 1) high-quality cardiopulmonary resuscitation, 2) a protocol for massive transfusion protocol, 3) treatment of diffuse bleeding and coagulopathy, 4) treatment of uterine and pelvic bleeding, 5) extracorporeal lung and heart support, and 6) post-AFE intensive care?
Tell us—at [email protected]. Please include your name and the city and state in which you practice.
Amniotic fluid embolism (AFE) occurs in about 1 in 20,000 to 1 in 40,000 deliveries.1,2 Although the condition is rare, the case fatality rate is high, and AFE is a common cause of maternal death in developed countries. AFE cannot be predicted or prevented. Moreover, the condition is difficult to precisely define and is often a diagnosis of exclusion.
AFE should be considered in the differential diagnosis of a pregnant woman with sudden onset of shortness of breath, hypotension, or cardiac arrhythmia or arrest, followed by coagulopathy and hemorrhage. Premonitory symptoms, including restlessness, confusion, disorientation, agitation, chills, nausea, numbness, and tingling, are commonly reported just before the cardiorespiratory collapse. AFE is less likely if the initial obstetric event is hemorrhage in the absence of cardiorespiratory compromise or a preceding coagulopathy.3
Typically, the onset is just before birth, during birth, or within the first few hours after delivery. In the United Kingdom, which has a robust centralized registry for reporting AFE, about 56% of cases occur before birth and 44% after birth.4
Related article: Is the incidence of amniotic fluid embolism rising? John T. Repke, MD (Examining the Evidence, August 2010)
The resources available to obstetric units vary greatly. Each unit needs to assess its resources and develop an AFE treatment protocol that builds on the unique strengths of the unit. Treatment of AFE requires the coordinated actions of anesthesiologists, obstetricians, nurses, the blood bank, pharmacy, and cardiovascular specialists. Coordinated activity among the members of such a large multidisciplinary team requires a written protocol that is practiced on a regular basis.
Six important components of a multidisciplinary response to AFE treatment protocol are:
- high-quality cardiopulmonary resuscitation (CPR)
- a protocol for massive transfusion
- treatment of diffuse bleeding and coagulopathy
- treatment of uterine and pelvic bleeding
- extracorporeal lung and heart support
- post-AFE intensive care.
1. Initiate high-quality CPR
Hypotension and hypoxemia due to cardiac and pulmonary dysfunction are prominent features of AFE. Dysrythmias such as pulseless electrical activity, bradycardia, ventricular fibrillation, and asystole are common. Rapid institution of high-quality CPR is critical to the survival of women with AFE.
Interventions often used in CPR of patients with AFE include initiation of high-quality chest compressions, early defibrillation if indicated, immediate administration of 100% oxygen by mask ventilation followed by early intubation, and rapid establishment of peripheral, arterial, and central venous access. Volume assessment, fluid replacement, and administration of vasopressors and inotropes are also important.
CPR of pregnant women requires special interventions, including maximal left lateral displacement of the uterus to reduce compression of the descending aorta and vena cava. Lateral displacement of the uterus can be accomplished by left lateral tilt or by manual uterine displacement. To optimize the effectiveness of chest compressions, many experts recommend placing the woman in a supine position and using manual uterine displacement rather than a left lateral tilt.5 For chest compressions, the hands should be placed just above the center of the sternum to adjust for the elevation of the diaphragm caused by the gravid uterus.
The gravid uterus can compromise the effectiveness of CPR. Fetal viability and neurologic outcome are best if delivery occurs within 5 minutes of the onset of cardiopulmonary arrest. If the gestational age of the fetus is consistent with extrauterine viability and initial CPR has not restored cardiac function, it is best to initiate fetal delivery within 4 minutes of the onset of cardiopulmonary arrest with the intent to deliver the fetus within 5 minutes.6,7 If the fetus is beyond 20 weeks’ gestational age, delivery early in the course of CPR improves the effectiveness of maternal resuscitation and may increase the probability of maternal survival.
In one study of the response of anesthesiologists, obstetricians, and nurses to a simulated cardiac arrest caused by an AFE, the participants did not routinely use defibrillation when indicated, did not place a firm support under the back for chest compressions, and did not switch the provider of chest compressions every 2 minutes.8 This study indicates that additional training and routinely scheduled multidisciplinary simulation of the response to cardiopulmonary arrest could improve the quality of our CPR.
2. Use a massive transfusion protocol
Severe coagulopathy and diffuse bleeding are commonly encountered in AFE. Target goals for the replacement of blood products include:
- hemoglobin concentration ≥8 g/dL
- fibrinogen ≥150 to 200 mg/dL
- platelets ≥50,000/μL
- prothrombin time international normalized ratio (INR) ≤1.5.
Most massive transfusion protocols provide for the rapid delivery of 4 to 8 units of red blood cells and a similar number of units of fresh frozen plasma to the patient’s bedside. In the management of AFE, 20 to 30 units of red blood cells and a similar quantity of fresh frozen plasma may need to be transfused. Cryoprecipitate takes 20 to 30 minutes to thaw, so preparations to transfuse cryoprecipitate should be initiated as soon as the massive transfusion protocol is triggered. A case of AFE can completely empty the blood bank of all available blood products and necessitate the use of alternative agents.
Lyophilized fibrinogen concentrate (RiaSTAP) is approved by the US Food and Drug Administration for the treatment of congenital hypofibrinogenemia and also may be useful to replace fibrinogen in cases of AFE. In many hospitals, large quantities of fresh frozen plasma are not immediately available; lyophilized fibrinogen concentrate may be especially useful in these settings. Another advantage of fibrinogen concentrate is that large amounts of fibrinogen can be administered in a small volume of intravenous fluid. Fibrinogen concentrate typically is used at a dose of 70 mg/kg of body weight.9,10
Intraoperative red cell salvage occasionally is used in cases of obstetric hemorrhage. In one case report of the use of red cell salvage with leukocyte depletion filtration during treatment of an AFE, acute hypotension developed in the patient after the transfusion of salvaged red cells.11 This case report raises safety concerns about the use of salvaged cells in women with severe AFE.
Related article: 10 practical, evidence-based recommendations for the management of severe postpartum hemorrhage Baha M. Sibai, MD (June 2011)
3. Treat diffuse bleeding and coagulopathy
In addition to the initiation of the massive transfusion protocol, additional treatments that may be helpful in managing the coagulopathy of AFE include tranexamic acid, recombinant factor VIIa (rFVIIa), and exchange transfusion.
AFE is often associated with hyperfibrinolysis, which can cause excessive bleeding.12 Tranexamic acid blocks the lysine binding sites on plasminogen and thereby reduces the lysis of fibrin clots. Clinical trials in patients who have undergone trauma have demonstrated that the administration of tranexamic acid reduces blood loss.13 The dose of tranexamic acid is approximately 10 to 20 mg/kg of body weight, or approximately 1 g.
Controversy exists about the use of rFVIIa to treat the coagulopathy and bleeding caused by AFE. Some authorities believe that rFVIIa is associated with an increased AFE case fatality rate.14 Other authorities believe rFVIIa may be useful in the treatment of AFE coagulopathy, especially when bleeding persists despite aggressive blood and component replacement.”15 The dose of rFVIIa is approximately 90 µg/kg of body weight. rFVIIa is extremely expensive.
Exchange transfusion has been used successfully to treat AFE.16 In women with AFE, exchange transfusion removes circulating cells, cell fragments, and substances that trigger systemic anaphylaxis and coagulopathy, thereby enhancing rapid recovery.
Related article: Act fast when confronted by a coagulopathy postpartum Robert L. Barbieri, MD (Editorial; March 2012)
4. Treat uterine and pelvic bleeding
Obstetrician-gynecologists are experts in the control of uterine and pelvic bleeding. Interventions that commonly are used to control uterine and pelvic bleeding in cases of postpartum hemorrhage, uterine rupture, or placenta accreta also can be applied in cases of AFE with uncontrolled uterine and pelvic bleeding. These techniques include:
- use of uterine compression sutures
- the Bakri balloon
- a uterine tourniquet
- vascular clamps on the ovarian vessels.17,18
In many cases of AFE, total or supracervical hysterectomy is necessary to control uterine bleeding. Uterine artery embolization, if available, has been reported to be helpful in select cases. However, many women with AFE are too unstable to survive transfer to an interventional radiology suite. Additional interventions to control bleeding include hypogastric artery ligation, infrarenal aortic compression, and pelvic packing.
Cross-clamping the aorta below the renal vessels can reduce blood flow to the pelvis and provide time for cardiopulmonary and volume resuscitation. Alternatively, placing pressure on the infrarenal aorta with a sponge or directly by hand can help reduce blood flow to the pelvis.19
In many cases of AFE, pelvic hemorrhage is difficult to control. Even if surgical pedicles are ligated securely, the coagulopathy of AFE may cause persistent oozing from areas of minor tissue trauma. Uncontrolled blood loss can be a proximate cause of death in women with AFE. All written protocols for responding to an AFE should include a plan to use pelvic packing for patients in whom standard operative procedures do not produce adequate control of bleeding. A “mushroom,” “parachute,” or “umbrella” pack has been reported to help stabilize the severely ill patient with pelvic bleeding and permit effective resuscitation and blood product replacement.20
Related articles:
A stitch in time: The B-Lynch, Hayman and Pereira uterine compression sutures Robert L. Barbieri, MD (Editorial, December 2012)
Have you made the best use of the Bakri balloon in PPH? Robert L. Barbieri, MD (Editorial, July 2011)
5. Consider extracorporeal lung and heart support
In many cases of AFE, both lung and cardiac function are severely compromised. Both veno-arterial extracorporeal membrane oxygenation (VA-ECMO) and full cardiopulmonary bypass provide support for the failing lung and heart. Based on a small number of case reports, extracorporeal lung and heart support appear to be useful in the treatment of AFE.21–26 Using the Seldinger technique,27 it is technically feasible to rapidly access a major vein and artery to provide the input and output ports for VA-ECMO. Unlike the cardiopulmonary bypass pump, the VA-ECMO pump does not have a reservoir that needs to be primed with blood and is smaller and more portable. To provide a patient with VA-ECMO or cardiopulmonary bypass, a cardiac interventionist and a perfusionist must be available. Extracorporeal lung and heart support require heparinization of the patient’s blood, which may result in increased bleeding. Both VA-ECMO and cardiopulmonary bypass, along with the diseases for which they are used, may cause renal dysfunction, neurologic injury, and infection.28
Alternative approaches that provide support of the heart—but not lung—are the Impella pump, TandemHeart, and the intra-aortic balloon pump. An alternative that provides lung support—but not cardiac support—is veno-venous ECMO.
In developing a written protocol for responding to an AFE, obstetricians should explore the potential availability of VA-ECMO, cardiopulmonary bypass, or other cardiopulmonary support devices as options for patients who have not responded to standard treatment of AFE and are at high risk of death.
6. Post-AFE intensive care
After stabilization, most women with AFE will require intensive care for 48 to 96 hours. Some experts have proposed that all survivors of cardiopulmonary arrest who are successfully resuscitated and stabilized be transferred to hospitals that specialize in post−cardiac arrest care to improve outcomes.
Assessment of organ injury is important after an AFE. In addition, encephalopathy is a common complication of AFE, and sequential neurologic examination is a priority. Therapeutic hypothermia (TH) may help to preserve neurologic function after AFE.29 However, TH may cause a mild coagulopathy by inhibiting platelet activation and enzyme activity of clotting factors. Because coagulopathy is a prominent feature of AFE, TH may be contraindicated if the patient has a clinically significant baseline coagulopathy.30
DEVELOP AN AFE PROTOCOL AND PRACTICE THE COMPONENTS
Practicing the components of obstetric protocols can improve unit performance and patient outcomes.31 The components of an AFE protocol, as described in this article, include high-quality CPR, a protocol for massive transfusion, treatment of diffuse bleeding and coagulopathy, treatment of uterine and pelvic bleeding, extracorporeal lung and heart support, and post-AFE intensive care. Practicing these components of an AFE protocol will enhance performance across many common obstetric complications including postpartum hemorrhage, uterine rupture, placenta accreta, and pulmonary embolism.
When Chesley “Sully” Sullenberger and his copilot landed Flight 1549 in the Hudson River in New York, he had never practiced that specific response to twin engine failure, but he had practiced many emergency responses involving related scenarios. The combination of exceptional flight experience and years of practicing the response to emergency scenarios in simulation exercises permitted him and his copilot to execute a uniquely clever plan to solve a life-threatening
emergency. In a related way, practicing the components of AFE treatment will help obstetricians, obstetric anesthesiologists, and their multidisciplinary team to improve the responses to all major obstetric emergencies.
INSTANT POLL
Does your obstetric unit have a written protocol for treating an amniotic fluid embolism (AFE)? Has your obstetric unit practiced any of the components of the AFE treatment protocol: 1) high-quality cardiopulmonary resuscitation, 2) a protocol for massive transfusion protocol, 3) treatment of diffuse bleeding and coagulopathy, 4) treatment of uterine and pelvic bleeding, 5) extracorporeal lung and heart support, and 6) post-AFE intensive care?
Tell us—at [email protected]. Please include your name and the city and state in which you practice.
- Kramer MS, Rouleau J, Baskett TF, Joseph KS; Maternal Health Study Group of the Canadian Perinatal Surveillance System. Amniotic-fluid embolism and medical induction of labour: A retrospective, population-based cohort study. Lancet. 2006;368(9545):1444–1448.
- Abenhaim HA, Azoulay L, Kramer MS, Leduc L. Incidence and risk factors of amniotic fluid embolism: A population-based study on 3 million births in the United States. Am J Obstet Gynecol. 2008;199(1):49.e1–49.e8.
- Tuffnell D, Knight M, Plaat F. Amniotic fluid embolism—An update. Anaesthesia. 2011;66(1):3–6.
- Knight M, Tuffnell D, Brocklehurst P, Spark P, Kurinczuk JJ; UK Obstetric Surveillance System. Incidence and risk factors for amniotic-fluid embolism. Obstet Gynecol. 2010;115(5):910–917.
- Kundra P, Khanna S, Habeebullahg S, Ravishankar M. Manual displacement of the uterus during Caesarean section. Anaesthesia. 2007;62(5):460–465.
- Katz VL, Dotters DJ, Droegemueller W. Perimortem cesarean delivery. Obstet Gynecol. 1986;68(4):571–576.
- Katz V, Balderston K, DeFreest M. Perimortem cesarean delivery: Were our assumptions correct? Am J Obstet Gynecol. 2005;192(6):1916–1920.
- Lipman SS, Daniels KI, Carvalho B, et al. Deficits in the provision of cardiopulmonary resuscitation during simulated obstetric crises. Am J Obstet Gynecol. 2010;203(2):179.e1–179.e5.
- Bell SF, Rayment R, Collins PW, Collis RE. The use of fibrinogen concentrate to correct hypofibrinogenaemia rapidly during obstetric haemorrhage. Int J Obstet Anesth. 2010;19(2):218–223.
- Sorensen B, Tang M, Larsen OH, Laursen PN, Fenger-Eriksen C, Rea CJ. The role of fibrinogen: A new paradigm in the treatment of coagulopathic bleeding. Thromb Res. 2011;128(Suppl 1):S13–S16.
- Rogers WK, Wernimont SA, Kumar GC, Bennett E, Chestnut DH. Acute hypotension associated with intraoperative cell salvage using a leukocyte depletion filter during management of obstetric hemorrhage due to amniotic fluid embolism. Anesth Analg. 2013;117(2):449–452.
- Collins NF, Bloor M, McDonnell NJ. Hyperfibrinolysis diagnosed by rotational thromboelastometry in a case of suspected amniotic fluid embolism. Int J Obstet Anesth. 2013;22(1):71–76.
- Ker K, Edwards P, Perel P, Shakur H, Roberts I. Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054.
- Leighton BL, Wall MH, Lockhart EM, Phillips LE, Zatta AJ. Use of recombinant factor VIIa in patients with amniotic fluid embolism: A systematic review of case reports. Anesthesiology. 2011;115(6):1201–1208.
- Huber AW, Raio L, Alberio L, Ghezzi F, Surbek DV. Recombinant human factor VIIa prevents hysterectomy in severe postpartum hemorrhage: single center study. J Perinat Med. 2011;40(1):43–49.
- Dodgson J, Martin J, Boswell J, Goodall HB, Smith R. Probable amniotic fluid embolism precipitated by amniocentesis and treated by exchange transfusion. Brit Med J (Clin Res Ed). 1987;294(6583):1322–1323.
- Barbieri RL. A stitch in time: The B-Lynch, Hayman and Pereira uterine compression sutures. OBG Manage. 2012;24(12):6, 8, 10, 11.
- Barbieri RL. Have you made the best use of the Bakri balloon in PPH? OBG Manage. 2011;23(7):6, 8, 9.
- Belfort MA, Zimmerman J, Schemmer G, Oldroyd R, Smilanich R, Pearce M. Aortic compression and cross clamping in a case of placenta percreta and amniotic fluid embolism: A case report. AJP Rep. 2011;1(1):33–36.
- Dildy GA, Scott JR, Saffer CS, Belfort MA. An
effective pressure pack for severe pelvic hemorrhage. Obstet Gynecol. 2006;108(5):1222–1226. - Stanten RD, Iverson LI, Daugharty TM, Lovett SM, Terry C, Blumenstock E. Amniotic fluid embolism causing catastrophic pulmonary vasoconstriction: Diagnosis by transesophageal echocardiogram and treatment by cardiopulmonary bypass. Obstet Gynecol. 2003;102(3):496–498.
- Ho CH, Chen KB, Liu SK, Liu YF, Cheng HC, Wu RS. Early application of extracorporeal membrane oxygenation in a patient with amniotic fluid embolism. Acta Anaesthesiol Taiwan. 2009;47(2):99–102.
- Shen HP, Chang WC, Yeh LS, Ho M. Amniotic fluid embolism treated with emergency extracorporeal membrane oxygenation: A case report.
J Reprod Med. 2009;54(11–12):706–708. - Lee PH, Shulman MS, Vellayappan U, Symes JF, Olenchock SA Jr. Surgical treatment of amniotic fluid embolism with cardiopulmonary collapse. Ann Thorac Surg. 2010;90(5):1694–1696.
- Firstenberg MS, Abel E, Blais D, et al. Temporary extracorporeal circulatory support and pulmonary embolectomy for catastrophic amniotic fluid embolism. Heart Surg Forum. 2011;14(3):E157–E159.
- Ecker JL, Solt K, Fitzsimons MG, MacGillivray TE. Case records of the Massachusetts General Hospital. Case 40-2012: A 43-year-old woman with cardiorespiratory arrest after a cesarean section. N Engl J Med. 2012;367(26):2528–2536.
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 1953;39(5):368–376.
- Cheng R, Hachamovitch R, Kittelson M, et al. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: A meta-analysis of 1,866 adult patients. Ann Thorac Surg. 2013; epub Nov 8.
- Rittenberger JC, Kelly E, Jang D, Greer K, Heffner A. Successful outcome utilizing hypothermia after cardiac arrest in pregnancy: A case report. Crit Care Med. 2008;36(4):1354–1356.
- Michelson AD, MacGregor H, Barnard MR, Krestin AS, Rohrer MJ, Valeri CR. Reversible inhibition of human platelet activation by hypothermia in vivo and in vitro. Thromb Haemost. 1994;71(5):633–640.
- Rivzi F, Mackey R, Barrett T, McKenna P, Geary M. Successful reduction of massive postpartum haemorrhage by use of guidelines and staff education. BJOG. 2004;111(5):495–498.
- Kramer MS, Rouleau J, Baskett TF, Joseph KS; Maternal Health Study Group of the Canadian Perinatal Surveillance System. Amniotic-fluid embolism and medical induction of labour: A retrospective, population-based cohort study. Lancet. 2006;368(9545):1444–1448.
- Abenhaim HA, Azoulay L, Kramer MS, Leduc L. Incidence and risk factors of amniotic fluid embolism: A population-based study on 3 million births in the United States. Am J Obstet Gynecol. 2008;199(1):49.e1–49.e8.
- Tuffnell D, Knight M, Plaat F. Amniotic fluid embolism—An update. Anaesthesia. 2011;66(1):3–6.
- Knight M, Tuffnell D, Brocklehurst P, Spark P, Kurinczuk JJ; UK Obstetric Surveillance System. Incidence and risk factors for amniotic-fluid embolism. Obstet Gynecol. 2010;115(5):910–917.
- Kundra P, Khanna S, Habeebullahg S, Ravishankar M. Manual displacement of the uterus during Caesarean section. Anaesthesia. 2007;62(5):460–465.
- Katz VL, Dotters DJ, Droegemueller W. Perimortem cesarean delivery. Obstet Gynecol. 1986;68(4):571–576.
- Katz V, Balderston K, DeFreest M. Perimortem cesarean delivery: Were our assumptions correct? Am J Obstet Gynecol. 2005;192(6):1916–1920.
- Lipman SS, Daniels KI, Carvalho B, et al. Deficits in the provision of cardiopulmonary resuscitation during simulated obstetric crises. Am J Obstet Gynecol. 2010;203(2):179.e1–179.e5.
- Bell SF, Rayment R, Collins PW, Collis RE. The use of fibrinogen concentrate to correct hypofibrinogenaemia rapidly during obstetric haemorrhage. Int J Obstet Anesth. 2010;19(2):218–223.
- Sorensen B, Tang M, Larsen OH, Laursen PN, Fenger-Eriksen C, Rea CJ. The role of fibrinogen: A new paradigm in the treatment of coagulopathic bleeding. Thromb Res. 2011;128(Suppl 1):S13–S16.
- Rogers WK, Wernimont SA, Kumar GC, Bennett E, Chestnut DH. Acute hypotension associated with intraoperative cell salvage using a leukocyte depletion filter during management of obstetric hemorrhage due to amniotic fluid embolism. Anesth Analg. 2013;117(2):449–452.
- Collins NF, Bloor M, McDonnell NJ. Hyperfibrinolysis diagnosed by rotational thromboelastometry in a case of suspected amniotic fluid embolism. Int J Obstet Anesth. 2013;22(1):71–76.
- Ker K, Edwards P, Perel P, Shakur H, Roberts I. Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054.
- Leighton BL, Wall MH, Lockhart EM, Phillips LE, Zatta AJ. Use of recombinant factor VIIa in patients with amniotic fluid embolism: A systematic review of case reports. Anesthesiology. 2011;115(6):1201–1208.
- Huber AW, Raio L, Alberio L, Ghezzi F, Surbek DV. Recombinant human factor VIIa prevents hysterectomy in severe postpartum hemorrhage: single center study. J Perinat Med. 2011;40(1):43–49.
- Dodgson J, Martin J, Boswell J, Goodall HB, Smith R. Probable amniotic fluid embolism precipitated by amniocentesis and treated by exchange transfusion. Brit Med J (Clin Res Ed). 1987;294(6583):1322–1323.
- Barbieri RL. A stitch in time: The B-Lynch, Hayman and Pereira uterine compression sutures. OBG Manage. 2012;24(12):6, 8, 10, 11.
- Barbieri RL. Have you made the best use of the Bakri balloon in PPH? OBG Manage. 2011;23(7):6, 8, 9.
- Belfort MA, Zimmerman J, Schemmer G, Oldroyd R, Smilanich R, Pearce M. Aortic compression and cross clamping in a case of placenta percreta and amniotic fluid embolism: A case report. AJP Rep. 2011;1(1):33–36.
- Dildy GA, Scott JR, Saffer CS, Belfort MA. An
effective pressure pack for severe pelvic hemorrhage. Obstet Gynecol. 2006;108(5):1222–1226. - Stanten RD, Iverson LI, Daugharty TM, Lovett SM, Terry C, Blumenstock E. Amniotic fluid embolism causing catastrophic pulmonary vasoconstriction: Diagnosis by transesophageal echocardiogram and treatment by cardiopulmonary bypass. Obstet Gynecol. 2003;102(3):496–498.
- Ho CH, Chen KB, Liu SK, Liu YF, Cheng HC, Wu RS. Early application of extracorporeal membrane oxygenation in a patient with amniotic fluid embolism. Acta Anaesthesiol Taiwan. 2009;47(2):99–102.
- Shen HP, Chang WC, Yeh LS, Ho M. Amniotic fluid embolism treated with emergency extracorporeal membrane oxygenation: A case report.
J Reprod Med. 2009;54(11–12):706–708. - Lee PH, Shulman MS, Vellayappan U, Symes JF, Olenchock SA Jr. Surgical treatment of amniotic fluid embolism with cardiopulmonary collapse. Ann Thorac Surg. 2010;90(5):1694–1696.
- Firstenberg MS, Abel E, Blais D, et al. Temporary extracorporeal circulatory support and pulmonary embolectomy for catastrophic amniotic fluid embolism. Heart Surg Forum. 2011;14(3):E157–E159.
- Ecker JL, Solt K, Fitzsimons MG, MacGillivray TE. Case records of the Massachusetts General Hospital. Case 40-2012: A 43-year-old woman with cardiorespiratory arrest after a cesarean section. N Engl J Med. 2012;367(26):2528–2536.
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 1953;39(5):368–376.
- Cheng R, Hachamovitch R, Kittelson M, et al. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: A meta-analysis of 1,866 adult patients. Ann Thorac Surg. 2013; epub Nov 8.
- Rittenberger JC, Kelly E, Jang D, Greer K, Heffner A. Successful outcome utilizing hypothermia after cardiac arrest in pregnancy: A case report. Crit Care Med. 2008;36(4):1354–1356.
- Michelson AD, MacGregor H, Barnard MR, Krestin AS, Rohrer MJ, Valeri CR. Reversible inhibition of human platelet activation by hypothermia in vivo and in vitro. Thromb Haemost. 1994;71(5):633–640.
- Rivzi F, Mackey R, Barrett T, McKenna P, Geary M. Successful reduction of massive postpartum haemorrhage by use of guidelines and staff education. BJOG. 2004;111(5):495–498.