User login
OBJECTIVES: To investigate the impact of general health screenings and discussions with general practitioners on the cardiovascular risk profile of a random population of patients.
STUDY DESIGN: A population-based, randomized, controlled, 5-year follow-up trial conducted in a primary care setting.
POPULATION: The study group consisted of 2000 patients, randomly selected middle-aged men and women aged 30 to 50 years, from family practices in the district of Ebeltoft, Denmark. Of these patients, 1507 (75.4%) agreed to participate. Patients were randomized into (1) a control group that received no health screenings, (2) an intervention group that received 2 health screenings, (3) an intervention group that received both the 2 screenings and a 45-minute follow-up consultation annually.
OUTCOMES MEASURED: Cardiovascular risk score (CRS), body mass index (BMI), blood pressure, serum cholesterol, carbon monoxide in expiratory air, and tobacco use.
RESULTS: After 5 years, the CRS, BMI, and serum cholesterol levels were lower in the intervention groups compared with the control group. The improved outcome was greater in the baseline risk groups. The number of patients with elevated CRS in the intervention groups was approximately half the number of patients with elevated CRS in the control group. The difference was not a result of medication use. There was no difference between the group that received consultations after the screenings and the group that had health screenings alone.
CONCLUSIONS: Health screenings reduced the CRS in the intervention groups. After 5 years of follow-up, the number of persons at elevated cardiovascular risk was about half that expected, based on the prevalence/proportion in a population not receiving the health checks (the control group). The impact of intervention was higher among at-risk individuals. Consultations about health did not appear to improve the cardiovascular profile of the study population.
- Health screening decreased cardiovascular risk in the general population.
- The mean cardiovascular risk score was modestly reduced, and the proportion of persons at elevated cardiovascular risk was reduced to about half that expected after 5 years.
- The impact was more marked among groups at risk for cardiovascular disease.
- Planned health discussions in relation to the health screening did not seem to increase the impact on cardiovascular risk profile.
Many general practitioners believe their patients benefit from preventive health care and, as a result, many concentrate on identifying and treating risk factors for coronary heart disease (CHD),1,2 as many studies show that intervention can reduce risk.3-6 Other studies have suggested that such intervention results in only modest improvements in the risk profile of the general population,7-12 which raises questions about the efficacy of preventive health care.13,16 As of the early 1990s, few randomized, controlled, long-term trials have documented the effect of health screening as a primary prevention tool in reducing cardiovascular risk in the general population.17,18 In earlier large-scale studies on multiple-riskfactor intervention, interventions were not restricted to the intervention groups (controls received similar interventions to some extent); moreover, the studies contained other methodological problems that may have minimized the outcomes between control and intervention groups.19-21
This study was inspired by a Danish trial22 that focused not only on the prevention of CHD, but on preventing general health problems using lifestyle changes as the primary intervention tool.23 During the 1990s, results from 2 studies using different, though comparable, randomized designs were published.7-10 These studies focused more narrowly on the prevention of CHD8,17,18 and only 1 study had follow-up of more than 1 year. Relevant studies of the impact of intervention, therefore, are still lacking.
This article reports on the impact of general health screenings and health discussions with general practitioners on the cardiovascular risk profile of an unrandomized population. Other aspects of the study have been reported elsewhere.24-32
Methods
Setting and participants
The study took place in the district of Ebeltoft, Aarhus County, Denmark, a rural area with a total population of approximately 13,000. All 9 general practitioners from the district participated. Before the study began, the general practitioners participated in 4 meetings on prevention of heart and lung disease, dietary advice, and engaging in health discussions with patients.
Of 3464 inhabitants aged 30 to 49 years by January 1, 1991, and registered with a local general practitioner, a random sample of 2000 (57.7%) were invited to participate in the study. An employee of Aarhus County who was not otherwise involved in the study selected participants by birth dates. Registration with a general practitioner gives free access to medical services and is available to all Danish citizens. The 3464 persons from whom the participants were drawn constituted 87% of the entire population in the selected age group.
In September 1991, the 2000 persons received an invitation to participate along with a questionnaire about general demographic information and lifestyle, signed by their general practitioner. All who agreed to participate received an extensive supplementary baseline questionnaire with detailed questions that evaluated the participant’s health, lifestyle, psychosocial status, and psychosocial life events. Participants were informed by their general practitioner about which intervention they would be offered.
Randomization
Participants were randomly assigned to 1 of 3 groups by proportional, stratified randomization based on the general practitioner with whom they were registered, their sex, age, cohabitation status, and body mass index (BMI). All 3 groups received questionnaires. Health screenings were offered to 2 of the groups and follow-up health discussions with the general practitioner were offered to participants in only 1 of the 2 intervention groups. An employee of Aarhus County who was not otherwise involved in the study carried out the randomization.
Health screenings
Participants were given a multiphasic, broad-spectrum screening. This included a calculation of cardiovascular risk score (CRS), giving an estimate of the risk of premature cardiovascular disease for each individual. Figure 1 shows the calculation of CRS based on sex, familial inheritance (number of family members with ischemic heart disease before age 55), tobacco use, blood pressure, serum cholesterol (total), and BMI33 and the subsequent division into risk groups. Baseline health screenings were performed by 3 laboratory assistants between December 1991 and June 1992 and took place in the town of Ebeltoft, in the central clinic which 5 of the general practitioners shared. A few weeks after the health screening, all those tested received personal written feedback from their general practitioners. Where values fell outside the normal range, the feedback included advice relating primarily to lifestyle changes. All participants who had been advised that they had an elevated or high CRS were encouraged to see their general practitioner, regardless of their randomization group. All tested participants also received pamphlets on leading a healthy lifestyle from the Danish Heart Foundation.
FIGURE 1
Calculation of cardiovascular risk score
Health discussions
A 45-minute consultation with their own general practitioner was offered to participants from the health screening plus discussion group. Prior to the consultation, the participants completed a short questionnaire about suitable topics for discussion. At the end of the consultation, general practitioners invited participants to set a maximum of 3 health-related lifestyle goals for the following year. In cooperation with the participant, general practitioners then recorded these goals in a separate questionnaire.
Follow-up
Follow-up took place 1 and 5 years after the baseline intervention. Participants received follow-up questionnaires and were offered health screenings and health discussions according to their group of randomization. Participants in the health screening plus discussion group were offered annual consultations. The control group was promised a health screening and a health discussion at the end of the study period. Other details of the design are outlined elsewhere.23
Data analysis and statistics
SPSS version 9.0 for Windows was used to analyze results. Double data entry was used for the laboratory tests. Differences between groups were evaluated by 2- test for categorical data, by t-test for means, and by nonparametric testing for nonparametric data. Ninety-five percent confidence intervals (95% CI) were applied to relative risk (RR) values. Information was used from the baseline questionnaires to identify baseline risk groups among all those randomized. At the 5-year follow-up, randomized groups were compared according to the intention-to-treat rule (ie, regardless of their compliance with the intervention program).
Results
Participation at baseline and follow-up
Seventy-five percent (1507) of the 2000 persons invited to participate agreed to take part in the study. The percentage was higher among women (80.0%) than among men (71.0%).
Table 1shows the distribution of sociodemographic and cardiovascular risk factors at baseline among the randomized groups. No significant differences between groups were found. General practitioners advised 11.4% (103 persons) of the 905 tested in the intervention groups that they had an elevated or high CRS (≥10) at baseline. Of these, 52 belonged to the health screening group and 51 to the health screening plus discussion group. Prior to the test almost all participants were unaware of any existing cardiovascular disease.
Of the 443 persons in the health screening plus discussion group who accepted the offer of a consultation, 307 (69.3%) (95% CI, 64.8%–73.6%) decided to change their lifestyle in 1 or more respects. The number was significantly higher among those who had been advised of an elevated cardiovascular risk and who accepted the offer of a health discussion: 46 of 51 (90.2%) (95% CI, 78.6%–96.7%). In decreasing frequency, the goals set related to weight (63%) (95% CI, 47.5%–76.8%), diet (50.0%) (95% CI, 34.9%–65.1%), physical activity (50.0%) (95% CI, 34.9%–65.1%), smoking (43.5%) (95% CI 28.9%–58.9%), alcohol use (17.4%) (95% CI 7.8%–31.4%), and work (13.0%) (95% CI, 4.9%–26.3%). Emotional well-being, drug treatment, and other subjects (in each case by 2 different participants) were also discussed.
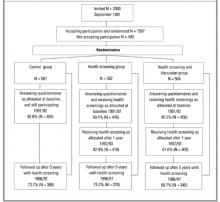
Figure 2 presents the flowchart of the study, focusing on participation in the health screenings. For the health discussions, the participation rate at baseline (1992) was very high. However, interest declined markedly in the follow-up period. Among baseline participants in the health screening plus discussion group, the percentage who agreed to the follow-up consultations was 97.1% in 1992, 35.7% in 1993, 16.9% in 1994, 15.1% in 1995, 8.6% in 1996, and 7.0% in 1997 (87.9% in 1992, 32.3% in 1993, 15.3% in 1994, 13.7% in 1995, 7.7% in 1996, and 6.5% in 1997 of all those randomized into the health screening plus discussion group). In total, 88.9% of those randomized into the health screening plus discussion group had at least 1 health discussion, 45.2% had at least 2 discussions, and 18.1% had at least 3 discussions.
TABLE 1
Baseline demographics and cardiovascular risk factors
| Control | Health screening | Health screening plus discussion | Valid N | |
|---|---|---|---|---|
| All participants | N = 501 | N = 502 | N = 504 | |
| Age in years | 40.4 (5.8) | 40.4 (5.6) | 40.6 (5.7) | 1507 |
| % males | 48.3 | 48.6 | 49.0 | 1507 |
| % cohabitating | 81.7 | 82.3 | 83.8 | 1496 |
| % smokers* | 51.4 | 51.4 | 53.9 | 1501 |
| BMI (kg/m2) | 24.4 (4.0) | 24.1 (3.6) | 24.6 (4.2) | 1463 |
| Screened participants | N = 449 | N = 456 | ||
| CRS | — | 5.69 (3.11) | 5.95 (3.07) | 905 |
| BMI (kg/m2) | — | 24.8 (3.8) | 25.3 (4.7) | 905 |
| Systolic BP (mm Hg) | — | 122.2 (14.5) | 123.0 (16.0) | 905 |
| Diastolic BP (mm Hg) | 77.7 (9.5) | 77.2 (10.0) | 905 | |
| Serum cholesterol (mmol/L)† | — | 5.60 (1.05) | 5.68 (1.06) | 905 |
| CO in exp. air (parts/million)‡ | ||||
| Among all | — | 3 (2–17) | 3 (2–16) | 905 |
| Among smokers | — | 17 (10–24) | 16 (8–24) | 461 |
| Values presented as mean (SD) unless otherwise noted. | ||||
| *Including occasional smokers. | ||||
| †To convert mmol/L to mg/dL, multiply by 38.7. | ||||
| ‡Median (25%–75% percentile). | ||||
| BMI, body mass index; BP, blood pressure; CO, carbon monoxide; CRS, cardiovascular risk score. | ||||
FIGURE 2
Flowchart of participation in The Ebeltoft Health Promotion Study, focusing on participation in the health screenings
Impact on cardiovascular risk
Table 2 shows the mean CRS and other cardiovascular risk factors at the 5-year follow-up. No significant differences were noted in any of the measures between the 2 intervention groups; therefore, data from these 2 groups are presented together. In comparison to the control group, participants in the intervention groups have a significantly lower CRS, BMI, and serum cholesterol level after 5 years. There were no significant differences between the control and intervention groups in terms of blood pressure. Differences between the control and the intervention groups are more pronounced among the baseline risk groups. Smoking and CO concentration were not significantly affected overall or between risk groups.
Table 3 shows a marked difference between the control and the intervention groups in the prevalence of persons with elevated CRS at the 5-year follow-up. The RR is reduced to about half—at the 5-year follow-up the prevalence of those with elevated CRS in the intervention groups is approximately half that in the control group. The absolute risk reduction is 8.6% (number needed to treat = 11.6). The same pattern is evident among baseline risk groups—the RR of having elevated CRS is reduced to about half, but with larger absolute risk reductions.
According to self-reported data at the 5-year follow-up, the positive impact on cardiovascular risk factors was not a result of medication. In the control group, 6.8% were using blood pressure medicine, compared to 4.8% in the intervention groups; 1.0% of the control group and 0.9% of the intervention groups were on heart medication, and 3.9% of the control group and 3.7% of the intervention groups were on diuretic medication.
TABLE 2
Cardiovascular risk score and other cardiovascular risk factors after 5 years of follow-up
| Control | Intervention | |
|---|---|---|
| All participants | N = 369 | N = 724 |
| CRS | 6.25 (3.47) | 5.69 (3.05)* |
| BMI (kg/m2) | 26.5 (4.4) | 25.9 (4.1)† |
| Systolic BP (mm Hg) | 132.6 (19.9) | 130.9 (18.2) |
| Diastolic BP (mm Hg) | 81.0 (11.7) | 79.8 (10.5) |
| Serum cholesterol (mmol/L)‡ | 5.68 (1.06) | 5.54 (1.03)† |
| Smoker participants | N = 181 | N = 345 |
| CRS | 7.47 (3.56) | 6.79 (3.11)† |
| BMI (kg/m2) | 26.2 (4.5) | 25.4 (4.0) |
| Systolic BP (mm Hg) | 132.8 (19.8) | 128.4 (17.4)* |
| Diastolic BP (mm Hg) | 80.9 (11.6) | 78.3 (10.2)* |
| Serum cholesterol (mmol/L)‡ | 5.73 (0.97) | 5.57 (1.07) |
| Overweight participants § | N = 58 | N = 111 |
| CRS | 9.28 (3.29) | 7.50 (2.99)* |
| BMI (kg/m2) | 33.6 (3.9) | 32.2 (3.6)† |
| Systolic BP (mm Hg) | 147.0 (22.3) | 139.0 (20.1)† |
| Diastolic BP (mm Hg) | 89.8 (12.3) | 84.4 (10.7)* |
| Serum cholesterol (mmol/L)‡ | 6.20 (1.12) | 5.81 (0.96)† |
| Values presented as mean (SD) unless otherwise noted. | ||
| *P < .01; | ||
| †P < .05. | ||
| ‡To convert mmol/L to mg/dL, multiply by 38.7. | ||
| §Self-reported BMI ≥ 27.5. | ||
| BMI, body mass index; BP, blood pressure; CO, carbon monoxide; CRS, cardiovascular risk score. | ||
TABLE 3
Prevalence proportion and relative risk of having elevated cardiovascular risk score or other cardiovascular risk factors, after 5 years of follow-up
| Control (%) | Intervention (%) | Intervention/control RR (95% CI) | |
|---|---|---|---|
| All participants | N = 369 | N = 724 | |
| Elevated or high CRS (≥10) | 18.7 | 10.1* | 0.54 (0.40–0.73) |
| BMI (≥27.5 kg/m2) | 35.0 | 30.8 | 0.88 (0.74–1.05) |
| Systolic BP (≥140 mm Hg) | 30.9 | 27.1 | 0.88 (0.72–1.06) |
| Diastolic BP (≥90 mm Hg) | 21.1 | 16.2† | 0.77 (0.59–0.99) |
| Serum cholesterol (≥6 mmol/L)‡ | 39.0 | 31.4† | 0.80 (0.68–0.95) |
| Smoker participants | N = 181 | N = 345 | |
| Elevated or high CRS (≥10) | 28.7 | 16.5* | 0.58 (0.41–0.80) |
| BMI (≥27.5 kg/m2) | 33.7 | 29.3 | 0.87 (0.67–1.13) |
| Systolic BP (≥140 mm Hg) | 31.5 | 23.2† | 0.74 (0.55–0.98) |
| Diastolic BP (≥90 mm Hg) | 22.1 | 12.5* | 0.56 (0.38–0.83) |
| Serum cholesterol (≥6 mmol/L)‡ | 40.3 | 32.5 | 0.81 (0.64–1.02) |
| Overweight participants§ | N = 58 | N = 111 | |
| Elevated or high CRS (≥10) | 46.6 | 21.6* | 0.46 (0.30–0.73) |
| BMI (≥27.5 kg/m2) | 100.0 | 91.9† | 0.92 (0.87–0.97) |
| Systolic BP (≥140 mm Hg) | 63.8 | 36.9* | 0.58 (0.42–0.79) |
| Diastolic BP (≥90 mm Hg) | 46.6 | 26.1* | 0.56 (0.37–0.85) |
| Serum cholesterol (≥6 mmol/L)‡ | 58.6 | 41.4† | 0.71 (0.52–0.96) |
| *P < .01; | |||
| †P < .05. | |||
| ‡ To convert mmol/L to mg/dL, multiply by 38.7. | |||
| §Self-reported BMI ≥ 27.5. | |||
| BMI, body mass index; BP, blood pressure; CRS, cardiovascular risk score; RR, relative risk. | |||
Discussion
This study is the first to present 5-year follow-up results from a randomized controlled trial showing the impact of general health screenings and discussions with general practitioners on the cardiovascular risk profile of a general population. The intervention had a modest impact on mean CRS in the general population, and a marked impact on the prevalence of those who were at cardiovascular risk. The impact was significantly greater for groups at cardiovascular risk; the relative risk reduction was approximately the same in those at risk as those not at risk, but with larger absolute risk reductions. The study does not indicate whether the reduction in CRS factors will result in reduced morbidity or mortality.
At the 5-year follow-up there was no difference between the CRS in the health screening plus discussion group and the screening only group. The discussion alone had no discernible impact. Several factors, however, may obscure the role of the discussions with general practitioners in this study. For ethical reasons, all persons advised of an elevated cardiovascular risk were offered a consultation with their general practitioner, regardless of their intervention group. Although consultations in such cases were probably not as extensive and detailed as those offered as part of the study, they may confound the difference in the degree of intervention between the 2 groups. The Danish Health System ensures that all participants can see their own general practitioner at no cost whenever they wish. Participants who were not offered a health discussion as part of the study may nevertheless have taken advantage of this free system to consult their general practitioner, especially if they were advised to do so. Moreover, the low rate of participation after the primary health discussion weakens the strength of the intervention in the health screening plus discussion group. Although the study thus does not provide evidence that such discussions played an essential role in the intervention, health screenings alone may not achieve the same impact. The psychological impact of the intervention may also be different for those who had personal consultations with their general practitioner after the health screening. The BMI values included a few individuals with unhealthily low BMI (<19). The distribution was not significantly different between the groups, although a tendency for an unhealthily low BMI of a slightly greater number of patients was seen in the intervention groups, highlighting the fact that weight loss is not always a relevant factor. Focusing on lifestyle changes might trigger some individuals to indulge in anorexic attitudes and behavior.
The results indicate that health screenings should be both population-based and individually oriented, and that general practitioners should be involved. The population screening is necessary to identify those at risk, since almost none of those with elevated cardiovascular risk were aware of their condition prior to screening. The fact that the general practitioner personally contacted the participants may have increased the participation rate, which is high in this study. In the written feedback after the screenings, general practitioners adjusted their advice to individual participants according to test results, and where appropriate advised them to come in for a personal consultation.
For several reasons, the impact of the intervention—both health screenings and discussions—may be greater than our findings suggest. We cannot measure the impact of the questionnaires on the control group—a methodological problem which also affected the OXCHECK study.7,8 In the British Family Heart Study,9,10 the control group was apparently unaffected, but the design of that study makes it impossible to assess the impact of subsequent intervention on baseline risk groups. Moreover, the fact that all the participants in the present study live in a small community may reduce the differences in degrees of intervention among the groups, although this is partially addressed by placing cohabiting couples in the same intervention group. Contact among patients within the various clinics involved may also have blurred the differences between the intervention groups.
In the present study, the general practitioners were not trained in any specific psychotherapeutic method for conducting the health discussions. The low rate of participation in follow-up consultations suggests a need to find better methods of motivating participants. Training general practitioners to use motivational discussions to inspire behavioral change, for example, might increase the impact of the intervention.3,4 Counseling to trigger changes in attitude and behavior, particularly when modified to the individual’s readiness to change, might be more effective than a traditional health discussion focusing mainly on various risk factors.
Important findings from this study are that a major part of the population is interested in having health screenings and discussions with their general practitioner, although interest declines rapidly; that individuals with elevated risk of coronary heart disease set relevant goals for themselves for lifestyle changes; and that cardiovascular risk after 5 years of follow-up is reduced. Planned health discussions about the health screening results do not seem to reduce cardiovascular risk.
Acknowledgments
The following general practitioners participated in the study: A. Bøgedal, P. Grønbæk, L. Jørgensen, P.T. Jørgensen, H. Lundberg, J.M. Nielsen, G.S. Pedersen, J.C. Rahbek, and N. Bie. We thank the staff at the general practitioners clinic in Ebeltoft for their extraordinary efforts, including the extensive and brilliant administrative assistance given by A. Hilligsøe and E. Therkildsen. Thanks also to A. Brock, head of the laboratory at Randers Central Hospital for analysis of blood and urine, and Sally Laird for revision of English texts relating to the study.
1. Calnan M, Cant S, Williams S, Killoran A. Involvement of the primary health care team in coronary heart disease prevention. Br J Gen Pract 1994;44:224-8.
2. Christensen B. Effect of general practitioners advice to men with increased risk of ischemic heart disease. Ugeskr Laeger 1995;157:4244-8 (Danish).
3. Hjermann I, Velve Byre K, Holme I, Leren P. Effect of diet and smoking intervention on the incidence of coronary heart disease. Report from the Oslo Study Group of a randomized trial in healthy men. Lancet 1981;2:1303-10.
4. Puska P, Salonen JT, Nissinen A, et al. Change in risk factors for coronary heart disease during 10 years of a community intervention programme (North Karelia project). Br Med J (Clin Res Ed) 1983;287:1840-4.
5. Farquhar JW, Fortmann SP, Flora JA, et al. Effects of community-wide education on cardiovascular disease risk factors. The Stanford Five-City Project. JAMA 1990;264:359-65.
6. Wilhelmsen L, Berglund G, Elmfeldt D, et al. The multifactor primary prevention trial in Goteborg, Sweden. Eur Heart J 1986;4:279-88.
7. Effectiveness of health checks conducted by nurses in primary care: results of the OXCHECK study after one year. Imperial Cancer Research Fund OXCHECK Study Group. BMJ 1994;308:308-12.
8. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. Imperial Cancer Research Fund OXCHECK Study Group. BMJ 1995;310:1099-1104.
9. Randomized controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study. Family Heart Study Group. BMJ 1994;308:313-20.
10. British family heart study: its design and method, and prevalence of cardiovascular risk factors. Family heart study group. Br J Gen Pract 1994;44:62-7.
11. Knutsen SF, Knutsen R. The Tromso Survey: the Family Intervention study the effect of intervention on some coronary risk factors and dietary habits: a 6-year follow-up. Prev Med 1991;20:197-212.
12. Cupples ME, McKnight A. Randomised controlled trial of health promotion in general practice for patients at high cardiovascular risk. BMJ 1994;309:993-6.
13. Stott N. Screening for cardiovascular risk in general practice. BMJ 1994;308:285-6.
14. Stewart-Brown S, Farmer A. Screening could seriously damage your health. BMJ 1997;314:533-4.
15. J, Skrabanek P. Coronary heart disease is not preventable by population interventions. Lancet 1988;2:839-41.
16. Waller D, Agass M, Mant D, Coulter A, Fuller A, Jones L. Health checks in general practice: another example of inverse care? Br Med J 1990;300:1115-8.
17. Ebrahim S, Smith GD. Systematic review of randomised controlled trials of multiple risk factor interventions for preventing coronary heart disease. BMJ 1997;314:1666-74.
18. Ebrahim S, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease (Cohrane Review). In: The Cochrane Library, Issue 3, 2001. Oxford: Update Software.
19. Cutler JL, Ramcharan S, Feldman R, Siegelaub AB, Campbell B, Friedman GD, Dales LG, Collen MF. Multiphasic checkup evaluation study. 1. Methods and population. Prev Med 1973;2:197-206.
20. Dales LG, Friedman GD, Collen MF. Evaluating periodic multiphasic health checkups: a controlled trial. J Chronic Dis 1979;32:385-404.
21. Multiple risk factor intervention trial. Risk factor changes and mortality results. Multiple Risk Factor Intervention Trial Research Group. JAMA 1982;248:1465-77.
22. Bille PE, Freund KC, Frimodt-Møller J. Forebyggende helbred-sundersøgelser/helbreds-samtaler for voksne i Nordjyllands Amt. Denmark: B.J. Grafik; 1990.
23. Lauritzen T, Leboeuf-Yde C, Lunde IM, Nielsen KD. Ebeltoft project: baseline data from a five-year randomized, controlled, prospective health promotion study in a Danish population. Br J Gen Pract 1995;45:542-7.
24. Sorensen HT, Thulstrup AM, Norgdard B, et al. Fetal growth and blood pressure in a Danish population aged 31-51 years. Scand Cardiovasc J 2000;34:390-5.
25. Thulstrup AM, Norgard B, Steffensen FH, Vilstrup H, Sorensen HT, Lauritzen T. Waist circumference and body mass index as predictors of elevated alanine transaminase in Danes aged 30 to 50 years. Dan Med Bull 1999;46:429-31.
26. Thulstrup AM, Sorensen HT, Steffensen FH, Vilstrup H, Lauritzen T. Changes in liver-derived enzymes and self-reported alcohol consumption. A 1-year follow-up study in Denmark. Scand J Gastroenterol 1999;34:189-93.
27. Steffensen FH, Sorensen HT, Brock A, Vilstrup H, Lauritzen T. Alcohol consumption and liver enzymes in persons 30-50 years of age. Cross-sectional study from Ebeltoft. Ugeskr Laeger 1997;159:5945-50.
28. Steffensen FH, Sorensen HT, Brock A, Vilstrup H, Lauritzen T. Alcohol consumption and serum liver-derived enzymes in a Danish population aged 30-50 years. Int J Epidemiol 1997;26:92-9.
29. Leboeuf-Yde C, Klougart N, Lauritzen T. How common is low back pain in the Nordic population? Data from a recent study on a middle-aged general Danish population and four surveys previously conducted in the Nordic countries. Spine 1996;21:1518-25.
30. Lauritzen T, Christiansen JS, Brock A, Mogensen CE. Repeated screening for albumin-creatinine ratio in an unselected population. The Ebeltoft Health Promotion Study, a randomized, population-based intervention trial on health test and health conversations with general practitioners. J Diabetes Complications 1994;8:146-9.
31. Karlsmose B, Lauritzen T, Engberg M, Parving A. A five-year longitudinal study of hearing in a Danish rural population aged 31-50 years. Br J Audiol 2000;34:47-55.
32. Karlsmose B, Lauritzen T, Parving A. Prevalence of hearing impairment and subjective hearing problems in a rural Danish population aged 31-50 years. Br J Audiol 1999;33:395-402.
33. Anggard EE, Land JM, Lenihan CJ, et al. Prevention of cardiovascular disease in general practice: a proposed model. Br Med J (Clin Res Ed) 1986;293:177-80.
34. Roberts A, Roberts P. Intensive cardiovascular risk factor intervention in a rural practice: a glimmer of hope. Br J Gen Pract 1998;48:967-70.
OBJECTIVES: To investigate the impact of general health screenings and discussions with general practitioners on the cardiovascular risk profile of a random population of patients.
STUDY DESIGN: A population-based, randomized, controlled, 5-year follow-up trial conducted in a primary care setting.
POPULATION: The study group consisted of 2000 patients, randomly selected middle-aged men and women aged 30 to 50 years, from family practices in the district of Ebeltoft, Denmark. Of these patients, 1507 (75.4%) agreed to participate. Patients were randomized into (1) a control group that received no health screenings, (2) an intervention group that received 2 health screenings, (3) an intervention group that received both the 2 screenings and a 45-minute follow-up consultation annually.
OUTCOMES MEASURED: Cardiovascular risk score (CRS), body mass index (BMI), blood pressure, serum cholesterol, carbon monoxide in expiratory air, and tobacco use.
RESULTS: After 5 years, the CRS, BMI, and serum cholesterol levels were lower in the intervention groups compared with the control group. The improved outcome was greater in the baseline risk groups. The number of patients with elevated CRS in the intervention groups was approximately half the number of patients with elevated CRS in the control group. The difference was not a result of medication use. There was no difference between the group that received consultations after the screenings and the group that had health screenings alone.
CONCLUSIONS: Health screenings reduced the CRS in the intervention groups. After 5 years of follow-up, the number of persons at elevated cardiovascular risk was about half that expected, based on the prevalence/proportion in a population not receiving the health checks (the control group). The impact of intervention was higher among at-risk individuals. Consultations about health did not appear to improve the cardiovascular profile of the study population.
- Health screening decreased cardiovascular risk in the general population.
- The mean cardiovascular risk score was modestly reduced, and the proportion of persons at elevated cardiovascular risk was reduced to about half that expected after 5 years.
- The impact was more marked among groups at risk for cardiovascular disease.
- Planned health discussions in relation to the health screening did not seem to increase the impact on cardiovascular risk profile.
Many general practitioners believe their patients benefit from preventive health care and, as a result, many concentrate on identifying and treating risk factors for coronary heart disease (CHD),1,2 as many studies show that intervention can reduce risk.3-6 Other studies have suggested that such intervention results in only modest improvements in the risk profile of the general population,7-12 which raises questions about the efficacy of preventive health care.13,16 As of the early 1990s, few randomized, controlled, long-term trials have documented the effect of health screening as a primary prevention tool in reducing cardiovascular risk in the general population.17,18 In earlier large-scale studies on multiple-riskfactor intervention, interventions were not restricted to the intervention groups (controls received similar interventions to some extent); moreover, the studies contained other methodological problems that may have minimized the outcomes between control and intervention groups.19-21
This study was inspired by a Danish trial22 that focused not only on the prevention of CHD, but on preventing general health problems using lifestyle changes as the primary intervention tool.23 During the 1990s, results from 2 studies using different, though comparable, randomized designs were published.7-10 These studies focused more narrowly on the prevention of CHD8,17,18 and only 1 study had follow-up of more than 1 year. Relevant studies of the impact of intervention, therefore, are still lacking.
This article reports on the impact of general health screenings and health discussions with general practitioners on the cardiovascular risk profile of an unrandomized population. Other aspects of the study have been reported elsewhere.24-32
Methods
Setting and participants
The study took place in the district of Ebeltoft, Aarhus County, Denmark, a rural area with a total population of approximately 13,000. All 9 general practitioners from the district participated. Before the study began, the general practitioners participated in 4 meetings on prevention of heart and lung disease, dietary advice, and engaging in health discussions with patients.
Of 3464 inhabitants aged 30 to 49 years by January 1, 1991, and registered with a local general practitioner, a random sample of 2000 (57.7%) were invited to participate in the study. An employee of Aarhus County who was not otherwise involved in the study selected participants by birth dates. Registration with a general practitioner gives free access to medical services and is available to all Danish citizens. The 3464 persons from whom the participants were drawn constituted 87% of the entire population in the selected age group.
In September 1991, the 2000 persons received an invitation to participate along with a questionnaire about general demographic information and lifestyle, signed by their general practitioner. All who agreed to participate received an extensive supplementary baseline questionnaire with detailed questions that evaluated the participant’s health, lifestyle, psychosocial status, and psychosocial life events. Participants were informed by their general practitioner about which intervention they would be offered.
Randomization
Participants were randomly assigned to 1 of 3 groups by proportional, stratified randomization based on the general practitioner with whom they were registered, their sex, age, cohabitation status, and body mass index (BMI). All 3 groups received questionnaires. Health screenings were offered to 2 of the groups and follow-up health discussions with the general practitioner were offered to participants in only 1 of the 2 intervention groups. An employee of Aarhus County who was not otherwise involved in the study carried out the randomization.
Health screenings
Participants were given a multiphasic, broad-spectrum screening. This included a calculation of cardiovascular risk score (CRS), giving an estimate of the risk of premature cardiovascular disease for each individual. Figure 1 shows the calculation of CRS based on sex, familial inheritance (number of family members with ischemic heart disease before age 55), tobacco use, blood pressure, serum cholesterol (total), and BMI33 and the subsequent division into risk groups. Baseline health screenings were performed by 3 laboratory assistants between December 1991 and June 1992 and took place in the town of Ebeltoft, in the central clinic which 5 of the general practitioners shared. A few weeks after the health screening, all those tested received personal written feedback from their general practitioners. Where values fell outside the normal range, the feedback included advice relating primarily to lifestyle changes. All participants who had been advised that they had an elevated or high CRS were encouraged to see their general practitioner, regardless of their randomization group. All tested participants also received pamphlets on leading a healthy lifestyle from the Danish Heart Foundation.
FIGURE 1
Calculation of cardiovascular risk score
Health discussions
A 45-minute consultation with their own general practitioner was offered to participants from the health screening plus discussion group. Prior to the consultation, the participants completed a short questionnaire about suitable topics for discussion. At the end of the consultation, general practitioners invited participants to set a maximum of 3 health-related lifestyle goals for the following year. In cooperation with the participant, general practitioners then recorded these goals in a separate questionnaire.
Follow-up
Follow-up took place 1 and 5 years after the baseline intervention. Participants received follow-up questionnaires and were offered health screenings and health discussions according to their group of randomization. Participants in the health screening plus discussion group were offered annual consultations. The control group was promised a health screening and a health discussion at the end of the study period. Other details of the design are outlined elsewhere.23
Data analysis and statistics
SPSS version 9.0 for Windows was used to analyze results. Double data entry was used for the laboratory tests. Differences between groups were evaluated by 2- test for categorical data, by t-test for means, and by nonparametric testing for nonparametric data. Ninety-five percent confidence intervals (95% CI) were applied to relative risk (RR) values. Information was used from the baseline questionnaires to identify baseline risk groups among all those randomized. At the 5-year follow-up, randomized groups were compared according to the intention-to-treat rule (ie, regardless of their compliance with the intervention program).
Results
Participation at baseline and follow-up
Seventy-five percent (1507) of the 2000 persons invited to participate agreed to take part in the study. The percentage was higher among women (80.0%) than among men (71.0%).
Table 1shows the distribution of sociodemographic and cardiovascular risk factors at baseline among the randomized groups. No significant differences between groups were found. General practitioners advised 11.4% (103 persons) of the 905 tested in the intervention groups that they had an elevated or high CRS (≥10) at baseline. Of these, 52 belonged to the health screening group and 51 to the health screening plus discussion group. Prior to the test almost all participants were unaware of any existing cardiovascular disease.
Of the 443 persons in the health screening plus discussion group who accepted the offer of a consultation, 307 (69.3%) (95% CI, 64.8%–73.6%) decided to change their lifestyle in 1 or more respects. The number was significantly higher among those who had been advised of an elevated cardiovascular risk and who accepted the offer of a health discussion: 46 of 51 (90.2%) (95% CI, 78.6%–96.7%). In decreasing frequency, the goals set related to weight (63%) (95% CI, 47.5%–76.8%), diet (50.0%) (95% CI, 34.9%–65.1%), physical activity (50.0%) (95% CI, 34.9%–65.1%), smoking (43.5%) (95% CI 28.9%–58.9%), alcohol use (17.4%) (95% CI 7.8%–31.4%), and work (13.0%) (95% CI, 4.9%–26.3%). Emotional well-being, drug treatment, and other subjects (in each case by 2 different participants) were also discussed.
Figure 2 presents the flowchart of the study, focusing on participation in the health screenings. For the health discussions, the participation rate at baseline (1992) was very high. However, interest declined markedly in the follow-up period. Among baseline participants in the health screening plus discussion group, the percentage who agreed to the follow-up consultations was 97.1% in 1992, 35.7% in 1993, 16.9% in 1994, 15.1% in 1995, 8.6% in 1996, and 7.0% in 1997 (87.9% in 1992, 32.3% in 1993, 15.3% in 1994, 13.7% in 1995, 7.7% in 1996, and 6.5% in 1997 of all those randomized into the health screening plus discussion group). In total, 88.9% of those randomized into the health screening plus discussion group had at least 1 health discussion, 45.2% had at least 2 discussions, and 18.1% had at least 3 discussions.
TABLE 1
Baseline demographics and cardiovascular risk factors
| Control | Health screening | Health screening plus discussion | Valid N | |
|---|---|---|---|---|
| All participants | N = 501 | N = 502 | N = 504 | |
| Age in years | 40.4 (5.8) | 40.4 (5.6) | 40.6 (5.7) | 1507 |
| % males | 48.3 | 48.6 | 49.0 | 1507 |
| % cohabitating | 81.7 | 82.3 | 83.8 | 1496 |
| % smokers* | 51.4 | 51.4 | 53.9 | 1501 |
| BMI (kg/m2) | 24.4 (4.0) | 24.1 (3.6) | 24.6 (4.2) | 1463 |
| Screened participants | N = 449 | N = 456 | ||
| CRS | — | 5.69 (3.11) | 5.95 (3.07) | 905 |
| BMI (kg/m2) | — | 24.8 (3.8) | 25.3 (4.7) | 905 |
| Systolic BP (mm Hg) | — | 122.2 (14.5) | 123.0 (16.0) | 905 |
| Diastolic BP (mm Hg) | 77.7 (9.5) | 77.2 (10.0) | 905 | |
| Serum cholesterol (mmol/L)† | — | 5.60 (1.05) | 5.68 (1.06) | 905 |
| CO in exp. air (parts/million)‡ | ||||
| Among all | — | 3 (2–17) | 3 (2–16) | 905 |
| Among smokers | — | 17 (10–24) | 16 (8–24) | 461 |
| Values presented as mean (SD) unless otherwise noted. | ||||
| *Including occasional smokers. | ||||
| †To convert mmol/L to mg/dL, multiply by 38.7. | ||||
| ‡Median (25%–75% percentile). | ||||
| BMI, body mass index; BP, blood pressure; CO, carbon monoxide; CRS, cardiovascular risk score. | ||||
FIGURE 2
Flowchart of participation in The Ebeltoft Health Promotion Study, focusing on participation in the health screenings
Impact on cardiovascular risk
Table 2 shows the mean CRS and other cardiovascular risk factors at the 5-year follow-up. No significant differences were noted in any of the measures between the 2 intervention groups; therefore, data from these 2 groups are presented together. In comparison to the control group, participants in the intervention groups have a significantly lower CRS, BMI, and serum cholesterol level after 5 years. There were no significant differences between the control and intervention groups in terms of blood pressure. Differences between the control and the intervention groups are more pronounced among the baseline risk groups. Smoking and CO concentration were not significantly affected overall or between risk groups.
Table 3 shows a marked difference between the control and the intervention groups in the prevalence of persons with elevated CRS at the 5-year follow-up. The RR is reduced to about half—at the 5-year follow-up the prevalence of those with elevated CRS in the intervention groups is approximately half that in the control group. The absolute risk reduction is 8.6% (number needed to treat = 11.6). The same pattern is evident among baseline risk groups—the RR of having elevated CRS is reduced to about half, but with larger absolute risk reductions.
According to self-reported data at the 5-year follow-up, the positive impact on cardiovascular risk factors was not a result of medication. In the control group, 6.8% were using blood pressure medicine, compared to 4.8% in the intervention groups; 1.0% of the control group and 0.9% of the intervention groups were on heart medication, and 3.9% of the control group and 3.7% of the intervention groups were on diuretic medication.
TABLE 2
Cardiovascular risk score and other cardiovascular risk factors after 5 years of follow-up
| Control | Intervention | |
|---|---|---|
| All participants | N = 369 | N = 724 |
| CRS | 6.25 (3.47) | 5.69 (3.05)* |
| BMI (kg/m2) | 26.5 (4.4) | 25.9 (4.1)† |
| Systolic BP (mm Hg) | 132.6 (19.9) | 130.9 (18.2) |
| Diastolic BP (mm Hg) | 81.0 (11.7) | 79.8 (10.5) |
| Serum cholesterol (mmol/L)‡ | 5.68 (1.06) | 5.54 (1.03)† |
| Smoker participants | N = 181 | N = 345 |
| CRS | 7.47 (3.56) | 6.79 (3.11)† |
| BMI (kg/m2) | 26.2 (4.5) | 25.4 (4.0) |
| Systolic BP (mm Hg) | 132.8 (19.8) | 128.4 (17.4)* |
| Diastolic BP (mm Hg) | 80.9 (11.6) | 78.3 (10.2)* |
| Serum cholesterol (mmol/L)‡ | 5.73 (0.97) | 5.57 (1.07) |
| Overweight participants § | N = 58 | N = 111 |
| CRS | 9.28 (3.29) | 7.50 (2.99)* |
| BMI (kg/m2) | 33.6 (3.9) | 32.2 (3.6)† |
| Systolic BP (mm Hg) | 147.0 (22.3) | 139.0 (20.1)† |
| Diastolic BP (mm Hg) | 89.8 (12.3) | 84.4 (10.7)* |
| Serum cholesterol (mmol/L)‡ | 6.20 (1.12) | 5.81 (0.96)† |
| Values presented as mean (SD) unless otherwise noted. | ||
| *P < .01; | ||
| †P < .05. | ||
| ‡To convert mmol/L to mg/dL, multiply by 38.7. | ||
| §Self-reported BMI ≥ 27.5. | ||
| BMI, body mass index; BP, blood pressure; CO, carbon monoxide; CRS, cardiovascular risk score. | ||
TABLE 3
Prevalence proportion and relative risk of having elevated cardiovascular risk score or other cardiovascular risk factors, after 5 years of follow-up
| Control (%) | Intervention (%) | Intervention/control RR (95% CI) | |
|---|---|---|---|
| All participants | N = 369 | N = 724 | |
| Elevated or high CRS (≥10) | 18.7 | 10.1* | 0.54 (0.40–0.73) |
| BMI (≥27.5 kg/m2) | 35.0 | 30.8 | 0.88 (0.74–1.05) |
| Systolic BP (≥140 mm Hg) | 30.9 | 27.1 | 0.88 (0.72–1.06) |
| Diastolic BP (≥90 mm Hg) | 21.1 | 16.2† | 0.77 (0.59–0.99) |
| Serum cholesterol (≥6 mmol/L)‡ | 39.0 | 31.4† | 0.80 (0.68–0.95) |
| Smoker participants | N = 181 | N = 345 | |
| Elevated or high CRS (≥10) | 28.7 | 16.5* | 0.58 (0.41–0.80) |
| BMI (≥27.5 kg/m2) | 33.7 | 29.3 | 0.87 (0.67–1.13) |
| Systolic BP (≥140 mm Hg) | 31.5 | 23.2† | 0.74 (0.55–0.98) |
| Diastolic BP (≥90 mm Hg) | 22.1 | 12.5* | 0.56 (0.38–0.83) |
| Serum cholesterol (≥6 mmol/L)‡ | 40.3 | 32.5 | 0.81 (0.64–1.02) |
| Overweight participants§ | N = 58 | N = 111 | |
| Elevated or high CRS (≥10) | 46.6 | 21.6* | 0.46 (0.30–0.73) |
| BMI (≥27.5 kg/m2) | 100.0 | 91.9† | 0.92 (0.87–0.97) |
| Systolic BP (≥140 mm Hg) | 63.8 | 36.9* | 0.58 (0.42–0.79) |
| Diastolic BP (≥90 mm Hg) | 46.6 | 26.1* | 0.56 (0.37–0.85) |
| Serum cholesterol (≥6 mmol/L)‡ | 58.6 | 41.4† | 0.71 (0.52–0.96) |
| *P < .01; | |||
| †P < .05. | |||
| ‡ To convert mmol/L to mg/dL, multiply by 38.7. | |||
| §Self-reported BMI ≥ 27.5. | |||
| BMI, body mass index; BP, blood pressure; CRS, cardiovascular risk score; RR, relative risk. | |||
Discussion
This study is the first to present 5-year follow-up results from a randomized controlled trial showing the impact of general health screenings and discussions with general practitioners on the cardiovascular risk profile of a general population. The intervention had a modest impact on mean CRS in the general population, and a marked impact on the prevalence of those who were at cardiovascular risk. The impact was significantly greater for groups at cardiovascular risk; the relative risk reduction was approximately the same in those at risk as those not at risk, but with larger absolute risk reductions. The study does not indicate whether the reduction in CRS factors will result in reduced morbidity or mortality.
At the 5-year follow-up there was no difference between the CRS in the health screening plus discussion group and the screening only group. The discussion alone had no discernible impact. Several factors, however, may obscure the role of the discussions with general practitioners in this study. For ethical reasons, all persons advised of an elevated cardiovascular risk were offered a consultation with their general practitioner, regardless of their intervention group. Although consultations in such cases were probably not as extensive and detailed as those offered as part of the study, they may confound the difference in the degree of intervention between the 2 groups. The Danish Health System ensures that all participants can see their own general practitioner at no cost whenever they wish. Participants who were not offered a health discussion as part of the study may nevertheless have taken advantage of this free system to consult their general practitioner, especially if they were advised to do so. Moreover, the low rate of participation after the primary health discussion weakens the strength of the intervention in the health screening plus discussion group. Although the study thus does not provide evidence that such discussions played an essential role in the intervention, health screenings alone may not achieve the same impact. The psychological impact of the intervention may also be different for those who had personal consultations with their general practitioner after the health screening. The BMI values included a few individuals with unhealthily low BMI (<19). The distribution was not significantly different between the groups, although a tendency for an unhealthily low BMI of a slightly greater number of patients was seen in the intervention groups, highlighting the fact that weight loss is not always a relevant factor. Focusing on lifestyle changes might trigger some individuals to indulge in anorexic attitudes and behavior.
The results indicate that health screenings should be both population-based and individually oriented, and that general practitioners should be involved. The population screening is necessary to identify those at risk, since almost none of those with elevated cardiovascular risk were aware of their condition prior to screening. The fact that the general practitioner personally contacted the participants may have increased the participation rate, which is high in this study. In the written feedback after the screenings, general practitioners adjusted their advice to individual participants according to test results, and where appropriate advised them to come in for a personal consultation.
For several reasons, the impact of the intervention—both health screenings and discussions—may be greater than our findings suggest. We cannot measure the impact of the questionnaires on the control group—a methodological problem which also affected the OXCHECK study.7,8 In the British Family Heart Study,9,10 the control group was apparently unaffected, but the design of that study makes it impossible to assess the impact of subsequent intervention on baseline risk groups. Moreover, the fact that all the participants in the present study live in a small community may reduce the differences in degrees of intervention among the groups, although this is partially addressed by placing cohabiting couples in the same intervention group. Contact among patients within the various clinics involved may also have blurred the differences between the intervention groups.
In the present study, the general practitioners were not trained in any specific psychotherapeutic method for conducting the health discussions. The low rate of participation in follow-up consultations suggests a need to find better methods of motivating participants. Training general practitioners to use motivational discussions to inspire behavioral change, for example, might increase the impact of the intervention.3,4 Counseling to trigger changes in attitude and behavior, particularly when modified to the individual’s readiness to change, might be more effective than a traditional health discussion focusing mainly on various risk factors.
Important findings from this study are that a major part of the population is interested in having health screenings and discussions with their general practitioner, although interest declines rapidly; that individuals with elevated risk of coronary heart disease set relevant goals for themselves for lifestyle changes; and that cardiovascular risk after 5 years of follow-up is reduced. Planned health discussions about the health screening results do not seem to reduce cardiovascular risk.
Acknowledgments
The following general practitioners participated in the study: A. Bøgedal, P. Grønbæk, L. Jørgensen, P.T. Jørgensen, H. Lundberg, J.M. Nielsen, G.S. Pedersen, J.C. Rahbek, and N. Bie. We thank the staff at the general practitioners clinic in Ebeltoft for their extraordinary efforts, including the extensive and brilliant administrative assistance given by A. Hilligsøe and E. Therkildsen. Thanks also to A. Brock, head of the laboratory at Randers Central Hospital for analysis of blood and urine, and Sally Laird for revision of English texts relating to the study.
OBJECTIVES: To investigate the impact of general health screenings and discussions with general practitioners on the cardiovascular risk profile of a random population of patients.
STUDY DESIGN: A population-based, randomized, controlled, 5-year follow-up trial conducted in a primary care setting.
POPULATION: The study group consisted of 2000 patients, randomly selected middle-aged men and women aged 30 to 50 years, from family practices in the district of Ebeltoft, Denmark. Of these patients, 1507 (75.4%) agreed to participate. Patients were randomized into (1) a control group that received no health screenings, (2) an intervention group that received 2 health screenings, (3) an intervention group that received both the 2 screenings and a 45-minute follow-up consultation annually.
OUTCOMES MEASURED: Cardiovascular risk score (CRS), body mass index (BMI), blood pressure, serum cholesterol, carbon monoxide in expiratory air, and tobacco use.
RESULTS: After 5 years, the CRS, BMI, and serum cholesterol levels were lower in the intervention groups compared with the control group. The improved outcome was greater in the baseline risk groups. The number of patients with elevated CRS in the intervention groups was approximately half the number of patients with elevated CRS in the control group. The difference was not a result of medication use. There was no difference between the group that received consultations after the screenings and the group that had health screenings alone.
CONCLUSIONS: Health screenings reduced the CRS in the intervention groups. After 5 years of follow-up, the number of persons at elevated cardiovascular risk was about half that expected, based on the prevalence/proportion in a population not receiving the health checks (the control group). The impact of intervention was higher among at-risk individuals. Consultations about health did not appear to improve the cardiovascular profile of the study population.
- Health screening decreased cardiovascular risk in the general population.
- The mean cardiovascular risk score was modestly reduced, and the proportion of persons at elevated cardiovascular risk was reduced to about half that expected after 5 years.
- The impact was more marked among groups at risk for cardiovascular disease.
- Planned health discussions in relation to the health screening did not seem to increase the impact on cardiovascular risk profile.
Many general practitioners believe their patients benefit from preventive health care and, as a result, many concentrate on identifying and treating risk factors for coronary heart disease (CHD),1,2 as many studies show that intervention can reduce risk.3-6 Other studies have suggested that such intervention results in only modest improvements in the risk profile of the general population,7-12 which raises questions about the efficacy of preventive health care.13,16 As of the early 1990s, few randomized, controlled, long-term trials have documented the effect of health screening as a primary prevention tool in reducing cardiovascular risk in the general population.17,18 In earlier large-scale studies on multiple-riskfactor intervention, interventions were not restricted to the intervention groups (controls received similar interventions to some extent); moreover, the studies contained other methodological problems that may have minimized the outcomes between control and intervention groups.19-21
This study was inspired by a Danish trial22 that focused not only on the prevention of CHD, but on preventing general health problems using lifestyle changes as the primary intervention tool.23 During the 1990s, results from 2 studies using different, though comparable, randomized designs were published.7-10 These studies focused more narrowly on the prevention of CHD8,17,18 and only 1 study had follow-up of more than 1 year. Relevant studies of the impact of intervention, therefore, are still lacking.
This article reports on the impact of general health screenings and health discussions with general practitioners on the cardiovascular risk profile of an unrandomized population. Other aspects of the study have been reported elsewhere.24-32
Methods
Setting and participants
The study took place in the district of Ebeltoft, Aarhus County, Denmark, a rural area with a total population of approximately 13,000. All 9 general practitioners from the district participated. Before the study began, the general practitioners participated in 4 meetings on prevention of heart and lung disease, dietary advice, and engaging in health discussions with patients.
Of 3464 inhabitants aged 30 to 49 years by January 1, 1991, and registered with a local general practitioner, a random sample of 2000 (57.7%) were invited to participate in the study. An employee of Aarhus County who was not otherwise involved in the study selected participants by birth dates. Registration with a general practitioner gives free access to medical services and is available to all Danish citizens. The 3464 persons from whom the participants were drawn constituted 87% of the entire population in the selected age group.
In September 1991, the 2000 persons received an invitation to participate along with a questionnaire about general demographic information and lifestyle, signed by their general practitioner. All who agreed to participate received an extensive supplementary baseline questionnaire with detailed questions that evaluated the participant’s health, lifestyle, psychosocial status, and psychosocial life events. Participants were informed by their general practitioner about which intervention they would be offered.
Randomization
Participants were randomly assigned to 1 of 3 groups by proportional, stratified randomization based on the general practitioner with whom they were registered, their sex, age, cohabitation status, and body mass index (BMI). All 3 groups received questionnaires. Health screenings were offered to 2 of the groups and follow-up health discussions with the general practitioner were offered to participants in only 1 of the 2 intervention groups. An employee of Aarhus County who was not otherwise involved in the study carried out the randomization.
Health screenings
Participants were given a multiphasic, broad-spectrum screening. This included a calculation of cardiovascular risk score (CRS), giving an estimate of the risk of premature cardiovascular disease for each individual. Figure 1 shows the calculation of CRS based on sex, familial inheritance (number of family members with ischemic heart disease before age 55), tobacco use, blood pressure, serum cholesterol (total), and BMI33 and the subsequent division into risk groups. Baseline health screenings were performed by 3 laboratory assistants between December 1991 and June 1992 and took place in the town of Ebeltoft, in the central clinic which 5 of the general practitioners shared. A few weeks after the health screening, all those tested received personal written feedback from their general practitioners. Where values fell outside the normal range, the feedback included advice relating primarily to lifestyle changes. All participants who had been advised that they had an elevated or high CRS were encouraged to see their general practitioner, regardless of their randomization group. All tested participants also received pamphlets on leading a healthy lifestyle from the Danish Heart Foundation.
FIGURE 1
Calculation of cardiovascular risk score
Health discussions
A 45-minute consultation with their own general practitioner was offered to participants from the health screening plus discussion group. Prior to the consultation, the participants completed a short questionnaire about suitable topics for discussion. At the end of the consultation, general practitioners invited participants to set a maximum of 3 health-related lifestyle goals for the following year. In cooperation with the participant, general practitioners then recorded these goals in a separate questionnaire.
Follow-up
Follow-up took place 1 and 5 years after the baseline intervention. Participants received follow-up questionnaires and were offered health screenings and health discussions according to their group of randomization. Participants in the health screening plus discussion group were offered annual consultations. The control group was promised a health screening and a health discussion at the end of the study period. Other details of the design are outlined elsewhere.23
Data analysis and statistics
SPSS version 9.0 for Windows was used to analyze results. Double data entry was used for the laboratory tests. Differences between groups were evaluated by 2- test for categorical data, by t-test for means, and by nonparametric testing for nonparametric data. Ninety-five percent confidence intervals (95% CI) were applied to relative risk (RR) values. Information was used from the baseline questionnaires to identify baseline risk groups among all those randomized. At the 5-year follow-up, randomized groups were compared according to the intention-to-treat rule (ie, regardless of their compliance with the intervention program).
Results
Participation at baseline and follow-up
Seventy-five percent (1507) of the 2000 persons invited to participate agreed to take part in the study. The percentage was higher among women (80.0%) than among men (71.0%).
Table 1shows the distribution of sociodemographic and cardiovascular risk factors at baseline among the randomized groups. No significant differences between groups were found. General practitioners advised 11.4% (103 persons) of the 905 tested in the intervention groups that they had an elevated or high CRS (≥10) at baseline. Of these, 52 belonged to the health screening group and 51 to the health screening plus discussion group. Prior to the test almost all participants were unaware of any existing cardiovascular disease.
Of the 443 persons in the health screening plus discussion group who accepted the offer of a consultation, 307 (69.3%) (95% CI, 64.8%–73.6%) decided to change their lifestyle in 1 or more respects. The number was significantly higher among those who had been advised of an elevated cardiovascular risk and who accepted the offer of a health discussion: 46 of 51 (90.2%) (95% CI, 78.6%–96.7%). In decreasing frequency, the goals set related to weight (63%) (95% CI, 47.5%–76.8%), diet (50.0%) (95% CI, 34.9%–65.1%), physical activity (50.0%) (95% CI, 34.9%–65.1%), smoking (43.5%) (95% CI 28.9%–58.9%), alcohol use (17.4%) (95% CI 7.8%–31.4%), and work (13.0%) (95% CI, 4.9%–26.3%). Emotional well-being, drug treatment, and other subjects (in each case by 2 different participants) were also discussed.
Figure 2 presents the flowchart of the study, focusing on participation in the health screenings. For the health discussions, the participation rate at baseline (1992) was very high. However, interest declined markedly in the follow-up period. Among baseline participants in the health screening plus discussion group, the percentage who agreed to the follow-up consultations was 97.1% in 1992, 35.7% in 1993, 16.9% in 1994, 15.1% in 1995, 8.6% in 1996, and 7.0% in 1997 (87.9% in 1992, 32.3% in 1993, 15.3% in 1994, 13.7% in 1995, 7.7% in 1996, and 6.5% in 1997 of all those randomized into the health screening plus discussion group). In total, 88.9% of those randomized into the health screening plus discussion group had at least 1 health discussion, 45.2% had at least 2 discussions, and 18.1% had at least 3 discussions.
TABLE 1
Baseline demographics and cardiovascular risk factors
| Control | Health screening | Health screening plus discussion | Valid N | |
|---|---|---|---|---|
| All participants | N = 501 | N = 502 | N = 504 | |
| Age in years | 40.4 (5.8) | 40.4 (5.6) | 40.6 (5.7) | 1507 |
| % males | 48.3 | 48.6 | 49.0 | 1507 |
| % cohabitating | 81.7 | 82.3 | 83.8 | 1496 |
| % smokers* | 51.4 | 51.4 | 53.9 | 1501 |
| BMI (kg/m2) | 24.4 (4.0) | 24.1 (3.6) | 24.6 (4.2) | 1463 |
| Screened participants | N = 449 | N = 456 | ||
| CRS | — | 5.69 (3.11) | 5.95 (3.07) | 905 |
| BMI (kg/m2) | — | 24.8 (3.8) | 25.3 (4.7) | 905 |
| Systolic BP (mm Hg) | — | 122.2 (14.5) | 123.0 (16.0) | 905 |
| Diastolic BP (mm Hg) | 77.7 (9.5) | 77.2 (10.0) | 905 | |
| Serum cholesterol (mmol/L)† | — | 5.60 (1.05) | 5.68 (1.06) | 905 |
| CO in exp. air (parts/million)‡ | ||||
| Among all | — | 3 (2–17) | 3 (2–16) | 905 |
| Among smokers | — | 17 (10–24) | 16 (8–24) | 461 |
| Values presented as mean (SD) unless otherwise noted. | ||||
| *Including occasional smokers. | ||||
| †To convert mmol/L to mg/dL, multiply by 38.7. | ||||
| ‡Median (25%–75% percentile). | ||||
| BMI, body mass index; BP, blood pressure; CO, carbon monoxide; CRS, cardiovascular risk score. | ||||
FIGURE 2
Flowchart of participation in The Ebeltoft Health Promotion Study, focusing on participation in the health screenings
Impact on cardiovascular risk
Table 2 shows the mean CRS and other cardiovascular risk factors at the 5-year follow-up. No significant differences were noted in any of the measures between the 2 intervention groups; therefore, data from these 2 groups are presented together. In comparison to the control group, participants in the intervention groups have a significantly lower CRS, BMI, and serum cholesterol level after 5 years. There were no significant differences between the control and intervention groups in terms of blood pressure. Differences between the control and the intervention groups are more pronounced among the baseline risk groups. Smoking and CO concentration were not significantly affected overall or between risk groups.
Table 3 shows a marked difference between the control and the intervention groups in the prevalence of persons with elevated CRS at the 5-year follow-up. The RR is reduced to about half—at the 5-year follow-up the prevalence of those with elevated CRS in the intervention groups is approximately half that in the control group. The absolute risk reduction is 8.6% (number needed to treat = 11.6). The same pattern is evident among baseline risk groups—the RR of having elevated CRS is reduced to about half, but with larger absolute risk reductions.
According to self-reported data at the 5-year follow-up, the positive impact on cardiovascular risk factors was not a result of medication. In the control group, 6.8% were using blood pressure medicine, compared to 4.8% in the intervention groups; 1.0% of the control group and 0.9% of the intervention groups were on heart medication, and 3.9% of the control group and 3.7% of the intervention groups were on diuretic medication.
TABLE 2
Cardiovascular risk score and other cardiovascular risk factors after 5 years of follow-up
| Control | Intervention | |
|---|---|---|
| All participants | N = 369 | N = 724 |
| CRS | 6.25 (3.47) | 5.69 (3.05)* |
| BMI (kg/m2) | 26.5 (4.4) | 25.9 (4.1)† |
| Systolic BP (mm Hg) | 132.6 (19.9) | 130.9 (18.2) |
| Diastolic BP (mm Hg) | 81.0 (11.7) | 79.8 (10.5) |
| Serum cholesterol (mmol/L)‡ | 5.68 (1.06) | 5.54 (1.03)† |
| Smoker participants | N = 181 | N = 345 |
| CRS | 7.47 (3.56) | 6.79 (3.11)† |
| BMI (kg/m2) | 26.2 (4.5) | 25.4 (4.0) |
| Systolic BP (mm Hg) | 132.8 (19.8) | 128.4 (17.4)* |
| Diastolic BP (mm Hg) | 80.9 (11.6) | 78.3 (10.2)* |
| Serum cholesterol (mmol/L)‡ | 5.73 (0.97) | 5.57 (1.07) |
| Overweight participants § | N = 58 | N = 111 |
| CRS | 9.28 (3.29) | 7.50 (2.99)* |
| BMI (kg/m2) | 33.6 (3.9) | 32.2 (3.6)† |
| Systolic BP (mm Hg) | 147.0 (22.3) | 139.0 (20.1)† |
| Diastolic BP (mm Hg) | 89.8 (12.3) | 84.4 (10.7)* |
| Serum cholesterol (mmol/L)‡ | 6.20 (1.12) | 5.81 (0.96)† |
| Values presented as mean (SD) unless otherwise noted. | ||
| *P < .01; | ||
| †P < .05. | ||
| ‡To convert mmol/L to mg/dL, multiply by 38.7. | ||
| §Self-reported BMI ≥ 27.5. | ||
| BMI, body mass index; BP, blood pressure; CO, carbon monoxide; CRS, cardiovascular risk score. | ||
TABLE 3
Prevalence proportion and relative risk of having elevated cardiovascular risk score or other cardiovascular risk factors, after 5 years of follow-up
| Control (%) | Intervention (%) | Intervention/control RR (95% CI) | |
|---|---|---|---|
| All participants | N = 369 | N = 724 | |
| Elevated or high CRS (≥10) | 18.7 | 10.1* | 0.54 (0.40–0.73) |
| BMI (≥27.5 kg/m2) | 35.0 | 30.8 | 0.88 (0.74–1.05) |
| Systolic BP (≥140 mm Hg) | 30.9 | 27.1 | 0.88 (0.72–1.06) |
| Diastolic BP (≥90 mm Hg) | 21.1 | 16.2† | 0.77 (0.59–0.99) |
| Serum cholesterol (≥6 mmol/L)‡ | 39.0 | 31.4† | 0.80 (0.68–0.95) |
| Smoker participants | N = 181 | N = 345 | |
| Elevated or high CRS (≥10) | 28.7 | 16.5* | 0.58 (0.41–0.80) |
| BMI (≥27.5 kg/m2) | 33.7 | 29.3 | 0.87 (0.67–1.13) |
| Systolic BP (≥140 mm Hg) | 31.5 | 23.2† | 0.74 (0.55–0.98) |
| Diastolic BP (≥90 mm Hg) | 22.1 | 12.5* | 0.56 (0.38–0.83) |
| Serum cholesterol (≥6 mmol/L)‡ | 40.3 | 32.5 | 0.81 (0.64–1.02) |
| Overweight participants§ | N = 58 | N = 111 | |
| Elevated or high CRS (≥10) | 46.6 | 21.6* | 0.46 (0.30–0.73) |
| BMI (≥27.5 kg/m2) | 100.0 | 91.9† | 0.92 (0.87–0.97) |
| Systolic BP (≥140 mm Hg) | 63.8 | 36.9* | 0.58 (0.42–0.79) |
| Diastolic BP (≥90 mm Hg) | 46.6 | 26.1* | 0.56 (0.37–0.85) |
| Serum cholesterol (≥6 mmol/L)‡ | 58.6 | 41.4† | 0.71 (0.52–0.96) |
| *P < .01; | |||
| †P < .05. | |||
| ‡ To convert mmol/L to mg/dL, multiply by 38.7. | |||
| §Self-reported BMI ≥ 27.5. | |||
| BMI, body mass index; BP, blood pressure; CRS, cardiovascular risk score; RR, relative risk. | |||
Discussion
This study is the first to present 5-year follow-up results from a randomized controlled trial showing the impact of general health screenings and discussions with general practitioners on the cardiovascular risk profile of a general population. The intervention had a modest impact on mean CRS in the general population, and a marked impact on the prevalence of those who were at cardiovascular risk. The impact was significantly greater for groups at cardiovascular risk; the relative risk reduction was approximately the same in those at risk as those not at risk, but with larger absolute risk reductions. The study does not indicate whether the reduction in CRS factors will result in reduced morbidity or mortality.
At the 5-year follow-up there was no difference between the CRS in the health screening plus discussion group and the screening only group. The discussion alone had no discernible impact. Several factors, however, may obscure the role of the discussions with general practitioners in this study. For ethical reasons, all persons advised of an elevated cardiovascular risk were offered a consultation with their general practitioner, regardless of their intervention group. Although consultations in such cases were probably not as extensive and detailed as those offered as part of the study, they may confound the difference in the degree of intervention between the 2 groups. The Danish Health System ensures that all participants can see their own general practitioner at no cost whenever they wish. Participants who were not offered a health discussion as part of the study may nevertheless have taken advantage of this free system to consult their general practitioner, especially if they were advised to do so. Moreover, the low rate of participation after the primary health discussion weakens the strength of the intervention in the health screening plus discussion group. Although the study thus does not provide evidence that such discussions played an essential role in the intervention, health screenings alone may not achieve the same impact. The psychological impact of the intervention may also be different for those who had personal consultations with their general practitioner after the health screening. The BMI values included a few individuals with unhealthily low BMI (<19). The distribution was not significantly different between the groups, although a tendency for an unhealthily low BMI of a slightly greater number of patients was seen in the intervention groups, highlighting the fact that weight loss is not always a relevant factor. Focusing on lifestyle changes might trigger some individuals to indulge in anorexic attitudes and behavior.
The results indicate that health screenings should be both population-based and individually oriented, and that general practitioners should be involved. The population screening is necessary to identify those at risk, since almost none of those with elevated cardiovascular risk were aware of their condition prior to screening. The fact that the general practitioner personally contacted the participants may have increased the participation rate, which is high in this study. In the written feedback after the screenings, general practitioners adjusted their advice to individual participants according to test results, and where appropriate advised them to come in for a personal consultation.
For several reasons, the impact of the intervention—both health screenings and discussions—may be greater than our findings suggest. We cannot measure the impact of the questionnaires on the control group—a methodological problem which also affected the OXCHECK study.7,8 In the British Family Heart Study,9,10 the control group was apparently unaffected, but the design of that study makes it impossible to assess the impact of subsequent intervention on baseline risk groups. Moreover, the fact that all the participants in the present study live in a small community may reduce the differences in degrees of intervention among the groups, although this is partially addressed by placing cohabiting couples in the same intervention group. Contact among patients within the various clinics involved may also have blurred the differences between the intervention groups.
In the present study, the general practitioners were not trained in any specific psychotherapeutic method for conducting the health discussions. The low rate of participation in follow-up consultations suggests a need to find better methods of motivating participants. Training general practitioners to use motivational discussions to inspire behavioral change, for example, might increase the impact of the intervention.3,4 Counseling to trigger changes in attitude and behavior, particularly when modified to the individual’s readiness to change, might be more effective than a traditional health discussion focusing mainly on various risk factors.
Important findings from this study are that a major part of the population is interested in having health screenings and discussions with their general practitioner, although interest declines rapidly; that individuals with elevated risk of coronary heart disease set relevant goals for themselves for lifestyle changes; and that cardiovascular risk after 5 years of follow-up is reduced. Planned health discussions about the health screening results do not seem to reduce cardiovascular risk.
Acknowledgments
The following general practitioners participated in the study: A. Bøgedal, P. Grønbæk, L. Jørgensen, P.T. Jørgensen, H. Lundberg, J.M. Nielsen, G.S. Pedersen, J.C. Rahbek, and N. Bie. We thank the staff at the general practitioners clinic in Ebeltoft for their extraordinary efforts, including the extensive and brilliant administrative assistance given by A. Hilligsøe and E. Therkildsen. Thanks also to A. Brock, head of the laboratory at Randers Central Hospital for analysis of blood and urine, and Sally Laird for revision of English texts relating to the study.
1. Calnan M, Cant S, Williams S, Killoran A. Involvement of the primary health care team in coronary heart disease prevention. Br J Gen Pract 1994;44:224-8.
2. Christensen B. Effect of general practitioners advice to men with increased risk of ischemic heart disease. Ugeskr Laeger 1995;157:4244-8 (Danish).
3. Hjermann I, Velve Byre K, Holme I, Leren P. Effect of diet and smoking intervention on the incidence of coronary heart disease. Report from the Oslo Study Group of a randomized trial in healthy men. Lancet 1981;2:1303-10.
4. Puska P, Salonen JT, Nissinen A, et al. Change in risk factors for coronary heart disease during 10 years of a community intervention programme (North Karelia project). Br Med J (Clin Res Ed) 1983;287:1840-4.
5. Farquhar JW, Fortmann SP, Flora JA, et al. Effects of community-wide education on cardiovascular disease risk factors. The Stanford Five-City Project. JAMA 1990;264:359-65.
6. Wilhelmsen L, Berglund G, Elmfeldt D, et al. The multifactor primary prevention trial in Goteborg, Sweden. Eur Heart J 1986;4:279-88.
7. Effectiveness of health checks conducted by nurses in primary care: results of the OXCHECK study after one year. Imperial Cancer Research Fund OXCHECK Study Group. BMJ 1994;308:308-12.
8. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. Imperial Cancer Research Fund OXCHECK Study Group. BMJ 1995;310:1099-1104.
9. Randomized controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study. Family Heart Study Group. BMJ 1994;308:313-20.
10. British family heart study: its design and method, and prevalence of cardiovascular risk factors. Family heart study group. Br J Gen Pract 1994;44:62-7.
11. Knutsen SF, Knutsen R. The Tromso Survey: the Family Intervention study the effect of intervention on some coronary risk factors and dietary habits: a 6-year follow-up. Prev Med 1991;20:197-212.
12. Cupples ME, McKnight A. Randomised controlled trial of health promotion in general practice for patients at high cardiovascular risk. BMJ 1994;309:993-6.
13. Stott N. Screening for cardiovascular risk in general practice. BMJ 1994;308:285-6.
14. Stewart-Brown S, Farmer A. Screening could seriously damage your health. BMJ 1997;314:533-4.
15. J, Skrabanek P. Coronary heart disease is not preventable by population interventions. Lancet 1988;2:839-41.
16. Waller D, Agass M, Mant D, Coulter A, Fuller A, Jones L. Health checks in general practice: another example of inverse care? Br Med J 1990;300:1115-8.
17. Ebrahim S, Smith GD. Systematic review of randomised controlled trials of multiple risk factor interventions for preventing coronary heart disease. BMJ 1997;314:1666-74.
18. Ebrahim S, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease (Cohrane Review). In: The Cochrane Library, Issue 3, 2001. Oxford: Update Software.
19. Cutler JL, Ramcharan S, Feldman R, Siegelaub AB, Campbell B, Friedman GD, Dales LG, Collen MF. Multiphasic checkup evaluation study. 1. Methods and population. Prev Med 1973;2:197-206.
20. Dales LG, Friedman GD, Collen MF. Evaluating periodic multiphasic health checkups: a controlled trial. J Chronic Dis 1979;32:385-404.
21. Multiple risk factor intervention trial. Risk factor changes and mortality results. Multiple Risk Factor Intervention Trial Research Group. JAMA 1982;248:1465-77.
22. Bille PE, Freund KC, Frimodt-Møller J. Forebyggende helbred-sundersøgelser/helbreds-samtaler for voksne i Nordjyllands Amt. Denmark: B.J. Grafik; 1990.
23. Lauritzen T, Leboeuf-Yde C, Lunde IM, Nielsen KD. Ebeltoft project: baseline data from a five-year randomized, controlled, prospective health promotion study in a Danish population. Br J Gen Pract 1995;45:542-7.
24. Sorensen HT, Thulstrup AM, Norgdard B, et al. Fetal growth and blood pressure in a Danish population aged 31-51 years. Scand Cardiovasc J 2000;34:390-5.
25. Thulstrup AM, Norgard B, Steffensen FH, Vilstrup H, Sorensen HT, Lauritzen T. Waist circumference and body mass index as predictors of elevated alanine transaminase in Danes aged 30 to 50 years. Dan Med Bull 1999;46:429-31.
26. Thulstrup AM, Sorensen HT, Steffensen FH, Vilstrup H, Lauritzen T. Changes in liver-derived enzymes and self-reported alcohol consumption. A 1-year follow-up study in Denmark. Scand J Gastroenterol 1999;34:189-93.
27. Steffensen FH, Sorensen HT, Brock A, Vilstrup H, Lauritzen T. Alcohol consumption and liver enzymes in persons 30-50 years of age. Cross-sectional study from Ebeltoft. Ugeskr Laeger 1997;159:5945-50.
28. Steffensen FH, Sorensen HT, Brock A, Vilstrup H, Lauritzen T. Alcohol consumption and serum liver-derived enzymes in a Danish population aged 30-50 years. Int J Epidemiol 1997;26:92-9.
29. Leboeuf-Yde C, Klougart N, Lauritzen T. How common is low back pain in the Nordic population? Data from a recent study on a middle-aged general Danish population and four surveys previously conducted in the Nordic countries. Spine 1996;21:1518-25.
30. Lauritzen T, Christiansen JS, Brock A, Mogensen CE. Repeated screening for albumin-creatinine ratio in an unselected population. The Ebeltoft Health Promotion Study, a randomized, population-based intervention trial on health test and health conversations with general practitioners. J Diabetes Complications 1994;8:146-9.
31. Karlsmose B, Lauritzen T, Engberg M, Parving A. A five-year longitudinal study of hearing in a Danish rural population aged 31-50 years. Br J Audiol 2000;34:47-55.
32. Karlsmose B, Lauritzen T, Parving A. Prevalence of hearing impairment and subjective hearing problems in a rural Danish population aged 31-50 years. Br J Audiol 1999;33:395-402.
33. Anggard EE, Land JM, Lenihan CJ, et al. Prevention of cardiovascular disease in general practice: a proposed model. Br Med J (Clin Res Ed) 1986;293:177-80.
34. Roberts A, Roberts P. Intensive cardiovascular risk factor intervention in a rural practice: a glimmer of hope. Br J Gen Pract 1998;48:967-70.
1. Calnan M, Cant S, Williams S, Killoran A. Involvement of the primary health care team in coronary heart disease prevention. Br J Gen Pract 1994;44:224-8.
2. Christensen B. Effect of general practitioners advice to men with increased risk of ischemic heart disease. Ugeskr Laeger 1995;157:4244-8 (Danish).
3. Hjermann I, Velve Byre K, Holme I, Leren P. Effect of diet and smoking intervention on the incidence of coronary heart disease. Report from the Oslo Study Group of a randomized trial in healthy men. Lancet 1981;2:1303-10.
4. Puska P, Salonen JT, Nissinen A, et al. Change in risk factors for coronary heart disease during 10 years of a community intervention programme (North Karelia project). Br Med J (Clin Res Ed) 1983;287:1840-4.
5. Farquhar JW, Fortmann SP, Flora JA, et al. Effects of community-wide education on cardiovascular disease risk factors. The Stanford Five-City Project. JAMA 1990;264:359-65.
6. Wilhelmsen L, Berglund G, Elmfeldt D, et al. The multifactor primary prevention trial in Goteborg, Sweden. Eur Heart J 1986;4:279-88.
7. Effectiveness of health checks conducted by nurses in primary care: results of the OXCHECK study after one year. Imperial Cancer Research Fund OXCHECK Study Group. BMJ 1994;308:308-12.
8. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. Imperial Cancer Research Fund OXCHECK Study Group. BMJ 1995;310:1099-1104.
9. Randomized controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study. Family Heart Study Group. BMJ 1994;308:313-20.
10. British family heart study: its design and method, and prevalence of cardiovascular risk factors. Family heart study group. Br J Gen Pract 1994;44:62-7.
11. Knutsen SF, Knutsen R. The Tromso Survey: the Family Intervention study the effect of intervention on some coronary risk factors and dietary habits: a 6-year follow-up. Prev Med 1991;20:197-212.
12. Cupples ME, McKnight A. Randomised controlled trial of health promotion in general practice for patients at high cardiovascular risk. BMJ 1994;309:993-6.
13. Stott N. Screening for cardiovascular risk in general practice. BMJ 1994;308:285-6.
14. Stewart-Brown S, Farmer A. Screening could seriously damage your health. BMJ 1997;314:533-4.
15. J, Skrabanek P. Coronary heart disease is not preventable by population interventions. Lancet 1988;2:839-41.
16. Waller D, Agass M, Mant D, Coulter A, Fuller A, Jones L. Health checks in general practice: another example of inverse care? Br Med J 1990;300:1115-8.
17. Ebrahim S, Smith GD. Systematic review of randomised controlled trials of multiple risk factor interventions for preventing coronary heart disease. BMJ 1997;314:1666-74.
18. Ebrahim S, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease (Cohrane Review). In: The Cochrane Library, Issue 3, 2001. Oxford: Update Software.
19. Cutler JL, Ramcharan S, Feldman R, Siegelaub AB, Campbell B, Friedman GD, Dales LG, Collen MF. Multiphasic checkup evaluation study. 1. Methods and population. Prev Med 1973;2:197-206.
20. Dales LG, Friedman GD, Collen MF. Evaluating periodic multiphasic health checkups: a controlled trial. J Chronic Dis 1979;32:385-404.
21. Multiple risk factor intervention trial. Risk factor changes and mortality results. Multiple Risk Factor Intervention Trial Research Group. JAMA 1982;248:1465-77.
22. Bille PE, Freund KC, Frimodt-Møller J. Forebyggende helbred-sundersøgelser/helbreds-samtaler for voksne i Nordjyllands Amt. Denmark: B.J. Grafik; 1990.
23. Lauritzen T, Leboeuf-Yde C, Lunde IM, Nielsen KD. Ebeltoft project: baseline data from a five-year randomized, controlled, prospective health promotion study in a Danish population. Br J Gen Pract 1995;45:542-7.
24. Sorensen HT, Thulstrup AM, Norgdard B, et al. Fetal growth and blood pressure in a Danish population aged 31-51 years. Scand Cardiovasc J 2000;34:390-5.
25. Thulstrup AM, Norgard B, Steffensen FH, Vilstrup H, Sorensen HT, Lauritzen T. Waist circumference and body mass index as predictors of elevated alanine transaminase in Danes aged 30 to 50 years. Dan Med Bull 1999;46:429-31.
26. Thulstrup AM, Sorensen HT, Steffensen FH, Vilstrup H, Lauritzen T. Changes in liver-derived enzymes and self-reported alcohol consumption. A 1-year follow-up study in Denmark. Scand J Gastroenterol 1999;34:189-93.
27. Steffensen FH, Sorensen HT, Brock A, Vilstrup H, Lauritzen T. Alcohol consumption and liver enzymes in persons 30-50 years of age. Cross-sectional study from Ebeltoft. Ugeskr Laeger 1997;159:5945-50.
28. Steffensen FH, Sorensen HT, Brock A, Vilstrup H, Lauritzen T. Alcohol consumption and serum liver-derived enzymes in a Danish population aged 30-50 years. Int J Epidemiol 1997;26:92-9.
29. Leboeuf-Yde C, Klougart N, Lauritzen T. How common is low back pain in the Nordic population? Data from a recent study on a middle-aged general Danish population and four surveys previously conducted in the Nordic countries. Spine 1996;21:1518-25.
30. Lauritzen T, Christiansen JS, Brock A, Mogensen CE. Repeated screening for albumin-creatinine ratio in an unselected population. The Ebeltoft Health Promotion Study, a randomized, population-based intervention trial on health test and health conversations with general practitioners. J Diabetes Complications 1994;8:146-9.
31. Karlsmose B, Lauritzen T, Engberg M, Parving A. A five-year longitudinal study of hearing in a Danish rural population aged 31-50 years. Br J Audiol 2000;34:47-55.
32. Karlsmose B, Lauritzen T, Parving A. Prevalence of hearing impairment and subjective hearing problems in a rural Danish population aged 31-50 years. Br J Audiol 1999;33:395-402.
33. Anggard EE, Land JM, Lenihan CJ, et al. Prevention of cardiovascular disease in general practice: a proposed model. Br Med J (Clin Res Ed) 1986;293:177-80.
34. Roberts A, Roberts P. Intensive cardiovascular risk factor intervention in a rural practice: a glimmer of hope. Br J Gen Pract 1998;48:967-70.