User login
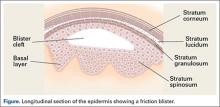
Friction blisters result from repetitive friction and strain forces that develop between the skin and various objects. Blisters form in areas where the stratum corneum and stratum granulosum are sufficiently robust (Figure), such as the palmar and plantar surfaces of the hand and feet. Thus, these layers are capable of transmitting the surface forces to the underlying layer, the stratum spinosum. In areas without strong stratum corneum and stratum granulosum layers, an abrasion forms instead.1
It has been shown that the transmitted frictional forces disrupt the stratum spinosum, with the blister roof being composed of the 2 upper epidermal layers as well as prickle cells of the traumatically disrupted stratum spinosum. The basal cell layer typically shows little damage and the dermal-epidermal junction remains intact.1
Early experimental studies in humans using repeatedly cycled probes demonstrated the pathologic sequence of events in blister formation. First, there is slight exfoliation of the stratum corneum layer, accompanied by a reddened area in the zone of rubbing (erythroderma). This is followed by a pale, narrow demarcation, which forms around the reddened region. Subsequently, this pale area fills in toward the center to occupy the entire affected area, which becomes the blister lesion.1,2
Hydrostatic pressure then causes blister fluid to accumulate within 1 to 2 hours following the trauma. Compared to plasma, the blister fluid has a lower protein level and similar electrolyte content.3,4 Cells in the blister cavity continue to degrade for about 4 hours following the injury, with resumption of cellular activity beginning at 6 hours. Mitotic activity is increased after 24 to 30 hours, and at 48 hours, a new granular layer is present. By 120 hours post-injury, a new stratum corneum is formed.5,6
A number of factors have been found to affect blister formation. Frictional force magnitude and number of cycles play the most obvious role. There is an inverse relationship between the two: as the frictional force increases, fewer cycles are required for blister formation.7 This is likely the reason blisters occur most commonly in areas where the fingertips are in contact with a seam, as opposed to the smoother surface of a baseball.
Many authors have examined moisture’s effect on frictional forces, and found that very dry and very wet skin produce low frictional forces, whereas moist skin produces the highest frictional force.1,2,8-10 In the case of dry skin, this is thought to be due to exfoliation and sloughing of cells from the stratum corneum, which produces a dry lubrication similar to graphite. Very wet skin has a fluid layer that lubricates the 2 surfaces. In the case of moist skin, however, it is hypothesized that surface tension impedes the movement of squamous cells, increasing the frictional forces.2,9 This moist environment is most commonly produced by sweating.
Other factors include skin temperature, which, when elevated, mildly predisposes the skin to blister formation. Some studies have shown temperatures as high as 50°C in rubbing experiments2,7,8,11; however, it should be noted that friction blisters do not resemble second-degree burns, either histologically or clinically.12,13
Blisters in Baseball Pitchers
Blisters in baseball pitchers are a well-known and frequently publicized problem; however, there is a paucity of literature describing the incidence or treatment of such blisters.14,15 The digital pulp experiences frictional forces from the baseball stiches as well as from the distal margin of the nail plate during release of the ball. Forces are transmitted to the ball predominately through the thumb, index, and long fingers. While the thumb acts mainly as a post, the index and long fingers impart the “action” on the ball. Not surprisingly, blisters form most commonly on these 2 fingers. While relatively small in size and significance, the impact of such a blister on a pitcher’s ability to maintain the fine control of his pitches cannot be overlooked. Biomechanical studies have shown that maximum gripping strength is attained when the fingers grasp a dynamometer handle at the level of the distal interphalangeal joint.16 Contact pressure mapping during gripping of a cylindrical object has shown that phalanges 2, 3, and 4 experience the highest forces in gripping and pulling activities.17 No study has specifically addressed phalangeal pressure generation in pitchers, however.
Blister Prevention
Blister prevention and treatment methods in baseball pitchers are steeped in folklore and tradition. Methods for drying out blisters and hardening calluses have included the use of pickle juice, urine, bags of rice, and superglue.14,15 Superglue, surgical glue, or any other foreign substance is not allowed during a game on the finger or hands of pitchers by Major League Baseball rules. Other anecdotal options include the use of compounded medicines that are marketed as creams and sprays designed to toughen skin.
As with other injuries, it is important to recognize any predisposing factors and ways to avoid them. Dampness and temperature (>104°F) have been identified as chief factors that substantially increase the friction coefficient and increase blister incidence.18 While temperature and perspiration are impossible to avoid during competition, steps can be taken to keep the pitcher’s hand dry on the mound as well as between innings, such as a rosin bag, a dry towel, and a rice bucket.
Maintaining fingernail length plays an important role in preventing blister formation. The nail can both protect the adjacent skin by decreasing the frictional force on the skin as well as lead to the development of blisters on the other fingers by repetitive abrasion. Nail length and contour need to be tailored to each pitcher specifically. The length of the nail can protect the finger pulp by minimally “elevating” the ball off of the finger itself. However, too long of a nail may come at the cost of abrading the abutting finger as the spin is imparted onto the ball. The shape of the nail is generally kept well contoured to avoid any sharp edges, which can act as local irritants. In the instance of soft, cracked, or torn nails, some pitchers have used acrylic nails. Maintaining proper fingernail shape and length is an essential preventive measure that requires regular use of clippers and emery boards.
Callus care is also paramount in preventing blister formation. It is believed that development of a callus is inevitable with repetitive throwing and likely protective of the underlying skin. The size and shape of the callus, like that of the nail, needs to be carefully monitored. A callus that becomes overly prominent can lead to increased friction with a baseball seam. This can lead to blister development. A small, smooth callus without edges or loose borders is the goal. The free edges of a callus can be trimmed with clean clippers. Contouring is best performed with careful use of an emery board.
Treatment of Finger Blisters
Blister management is determined by the size of the blister as well as the integrity of the overlying callus. Small blisters with intact skin coverage can be sterilely drained with a needle or a No. 11 blade.6,19-21 This allows apposition of the skin layers and quicker healing. The free edge of the blister can then be repaired with surgical glue. In these instances, a starting pitcher may be required to miss a start to allow further healing. In most cases, there is no need to place the player on the disabled list (DL).
Larger blisters, or those that traumatically open, represent a more concerning issue. The loose layers of skin can be removed, and the raw bed can then be treated with antibiotic ointment for the first 2 to 3 days. Subsequently, benzoin tincture, a commonly used paste of benzoin and alum, can be utilized to toughen the raw skin. Bulky dressings can be applied early in treatment but should then be discouraged, as the underlying skin softens due to the presence of moisture. These instances generally lead to lost time on the field. It is not uncommon that the pitcher requires placement on the 15-day DL.
Summary
Blisters on the fingertips of professional baseball players can lead to significant pain and decreased performance. Prevention of blister formation represents the goal of the player and the medical staff. Skin and nail care requires daily evaluation. When blisters do form, appropriate management can minimize lost time.
1. Sulzberger MB, Cortese TA, Fishman L, Wiley HS. Studies on blisters produced by friction. I. Results of linear rubbing and twisting technics. J Invest Dermatol. 1966;47(5):456-465.
2. Naylor PFD. Experimental friction blisters. Brit J Dermatol. 1955;67(10):327-342.
3. Cortese TA, Mitchell W, Sulzberger MB. Studies on blisters produced by friction. II. The blister fluid. J Invest Dermatol. 1968;50(1):47-53.
4. Schmidt P. Quantification of specific proteins in blister fluid. J Invest Dermatol. 1970;55(4):244-248.
5. Epstein WL, Fukuyama K, Cortese TA. Autographic study of friction blisters. RNA, DNA, and protein synthesis. Arch Dermatol. 1969;99(1):94-106.
6. Cortese TA Jr, Fukuyama K, Epstein W, Sulzberger MB. Treatment of friction blisters. An experimental study. Arch Dermatol. 1968;97(6):717-721.
7. Comaish JS. Epidermal fatigue as a cause of friction blisters. Lancet. 1973;1(7794):81-83.
8. Akers WA, Sulzberger MB. The friction blister. Mil Med. 1972;137(1):l-7.
9. Highley DR, Coomey M, DenBeste M, Wolfman LJ. Frictional properties of skin. J Invest Dermatol. 1977;69(3):303-305.
10. Nacht S, Close J, Yeung D, et al. Skin friction coefficient: changes induced by skin hydration and emollient application and correlation with perceived skin feel. J Soc Cosmet Chern. 1981;32:55-65.
11. Griffin TB, Corqese TA, Layton LL, et al. Inverse time and temperature relationship in experimental friction blisters. J Invest Dermatol. 1969;52:391.
12. Shupp JW, Nazabzadeh TJ, Rosenthal DS, Jordan MH, Fidler P, Jeng JC. A review of the local pathophysiologic bases of burn wound progression. J Burn Care Res. 2010;31(6):849-873.
13. Knapik JJ, Reynolds KL, Duplantis KL, Jones BH. Friction blisters: pathophysiology, prevention and treatment. Sports Med. 1995;20(3):136-147.
14. Sielski M. C.J. Wilson on pitching-hand care. The Wall Street Journal. October 30, 2010. Available at: http://blogs.wsj.com/dailyfix/2010/10/30/cj-wilson-on-caring-for-his-pitching-hand Accessed January 10, 2016.
15. Trezza J. Blisters are normal part of pitching for Lynn. St. Louis Post-Dispatch. July 4, 2014. Available at: http://www.stltoday.com/sports/baseball/professional/blisters-are-normal-part-of-pitching-for-lynn/article_9743c6f9-14b2-5c50-83b4-fa6a3c34cb83.html Accessed January 10, 2016.
16. Kaufmann RA, Kozin SH, Mirarchi A, Holland B, Porter S. Biomechanical analysis of flexor digitorum profundus and superficialis in grip-strenth generation. Am J Orthop. 2007;36(9):E128-E132.
17. Nicholas JW, Corvese RJ, Woolley C, Armstrong TJ. Quantification of hand grasp force using a pressure mapping system. Work. 2012;41(Suppl 1):605-612.
18. Knapik JJ, Reynolds KL. Risk factors for foot blisters during road marching: tobacco use, ethnicity, foot type, previous illness and others. Mil Med. 1999;164(2):92-97.
19. Emer J, Sivek R, Marciniak B. Sports Dermatology: Part 1 of 2. Traumatic or mechanical injuries, inflammatory conditions, and exacerbations of pre-existing conditions. J Clin Aesthet Dermatol. 2015;8(4):31-43.
20. De Luca JF, Adams BB, Yosipovitch G. Skin manifestations of athletes competing in the summer olympics: what a sports medicine physician should know. Sports Med. 2012;42(5):399-413.
21. Helm TN, Bergfeld WF. Sports dermatology. Clin Dermatol. 199;16(1):159-165.
Friction blisters result from repetitive friction and strain forces that develop between the skin and various objects. Blisters form in areas where the stratum corneum and stratum granulosum are sufficiently robust (Figure), such as the palmar and plantar surfaces of the hand and feet. Thus, these layers are capable of transmitting the surface forces to the underlying layer, the stratum spinosum. In areas without strong stratum corneum and stratum granulosum layers, an abrasion forms instead.1
It has been shown that the transmitted frictional forces disrupt the stratum spinosum, with the blister roof being composed of the 2 upper epidermal layers as well as prickle cells of the traumatically disrupted stratum spinosum. The basal cell layer typically shows little damage and the dermal-epidermal junction remains intact.1
Early experimental studies in humans using repeatedly cycled probes demonstrated the pathologic sequence of events in blister formation. First, there is slight exfoliation of the stratum corneum layer, accompanied by a reddened area in the zone of rubbing (erythroderma). This is followed by a pale, narrow demarcation, which forms around the reddened region. Subsequently, this pale area fills in toward the center to occupy the entire affected area, which becomes the blister lesion.1,2
Hydrostatic pressure then causes blister fluid to accumulate within 1 to 2 hours following the trauma. Compared to plasma, the blister fluid has a lower protein level and similar electrolyte content.3,4 Cells in the blister cavity continue to degrade for about 4 hours following the injury, with resumption of cellular activity beginning at 6 hours. Mitotic activity is increased after 24 to 30 hours, and at 48 hours, a new granular layer is present. By 120 hours post-injury, a new stratum corneum is formed.5,6
A number of factors have been found to affect blister formation. Frictional force magnitude and number of cycles play the most obvious role. There is an inverse relationship between the two: as the frictional force increases, fewer cycles are required for blister formation.7 This is likely the reason blisters occur most commonly in areas where the fingertips are in contact with a seam, as opposed to the smoother surface of a baseball.
Many authors have examined moisture’s effect on frictional forces, and found that very dry and very wet skin produce low frictional forces, whereas moist skin produces the highest frictional force.1,2,8-10 In the case of dry skin, this is thought to be due to exfoliation and sloughing of cells from the stratum corneum, which produces a dry lubrication similar to graphite. Very wet skin has a fluid layer that lubricates the 2 surfaces. In the case of moist skin, however, it is hypothesized that surface tension impedes the movement of squamous cells, increasing the frictional forces.2,9 This moist environment is most commonly produced by sweating.
Other factors include skin temperature, which, when elevated, mildly predisposes the skin to blister formation. Some studies have shown temperatures as high as 50°C in rubbing experiments2,7,8,11; however, it should be noted that friction blisters do not resemble second-degree burns, either histologically or clinically.12,13
Blisters in Baseball Pitchers
Blisters in baseball pitchers are a well-known and frequently publicized problem; however, there is a paucity of literature describing the incidence or treatment of such blisters.14,15 The digital pulp experiences frictional forces from the baseball stiches as well as from the distal margin of the nail plate during release of the ball. Forces are transmitted to the ball predominately through the thumb, index, and long fingers. While the thumb acts mainly as a post, the index and long fingers impart the “action” on the ball. Not surprisingly, blisters form most commonly on these 2 fingers. While relatively small in size and significance, the impact of such a blister on a pitcher’s ability to maintain the fine control of his pitches cannot be overlooked. Biomechanical studies have shown that maximum gripping strength is attained when the fingers grasp a dynamometer handle at the level of the distal interphalangeal joint.16 Contact pressure mapping during gripping of a cylindrical object has shown that phalanges 2, 3, and 4 experience the highest forces in gripping and pulling activities.17 No study has specifically addressed phalangeal pressure generation in pitchers, however.
Blister Prevention
Blister prevention and treatment methods in baseball pitchers are steeped in folklore and tradition. Methods for drying out blisters and hardening calluses have included the use of pickle juice, urine, bags of rice, and superglue.14,15 Superglue, surgical glue, or any other foreign substance is not allowed during a game on the finger or hands of pitchers by Major League Baseball rules. Other anecdotal options include the use of compounded medicines that are marketed as creams and sprays designed to toughen skin.
As with other injuries, it is important to recognize any predisposing factors and ways to avoid them. Dampness and temperature (>104°F) have been identified as chief factors that substantially increase the friction coefficient and increase blister incidence.18 While temperature and perspiration are impossible to avoid during competition, steps can be taken to keep the pitcher’s hand dry on the mound as well as between innings, such as a rosin bag, a dry towel, and a rice bucket.
Maintaining fingernail length plays an important role in preventing blister formation. The nail can both protect the adjacent skin by decreasing the frictional force on the skin as well as lead to the development of blisters on the other fingers by repetitive abrasion. Nail length and contour need to be tailored to each pitcher specifically. The length of the nail can protect the finger pulp by minimally “elevating” the ball off of the finger itself. However, too long of a nail may come at the cost of abrading the abutting finger as the spin is imparted onto the ball. The shape of the nail is generally kept well contoured to avoid any sharp edges, which can act as local irritants. In the instance of soft, cracked, or torn nails, some pitchers have used acrylic nails. Maintaining proper fingernail shape and length is an essential preventive measure that requires regular use of clippers and emery boards.
Callus care is also paramount in preventing blister formation. It is believed that development of a callus is inevitable with repetitive throwing and likely protective of the underlying skin. The size and shape of the callus, like that of the nail, needs to be carefully monitored. A callus that becomes overly prominent can lead to increased friction with a baseball seam. This can lead to blister development. A small, smooth callus without edges or loose borders is the goal. The free edges of a callus can be trimmed with clean clippers. Contouring is best performed with careful use of an emery board.
Treatment of Finger Blisters
Blister management is determined by the size of the blister as well as the integrity of the overlying callus. Small blisters with intact skin coverage can be sterilely drained with a needle or a No. 11 blade.6,19-21 This allows apposition of the skin layers and quicker healing. The free edge of the blister can then be repaired with surgical glue. In these instances, a starting pitcher may be required to miss a start to allow further healing. In most cases, there is no need to place the player on the disabled list (DL).
Larger blisters, or those that traumatically open, represent a more concerning issue. The loose layers of skin can be removed, and the raw bed can then be treated with antibiotic ointment for the first 2 to 3 days. Subsequently, benzoin tincture, a commonly used paste of benzoin and alum, can be utilized to toughen the raw skin. Bulky dressings can be applied early in treatment but should then be discouraged, as the underlying skin softens due to the presence of moisture. These instances generally lead to lost time on the field. It is not uncommon that the pitcher requires placement on the 15-day DL.
Summary
Blisters on the fingertips of professional baseball players can lead to significant pain and decreased performance. Prevention of blister formation represents the goal of the player and the medical staff. Skin and nail care requires daily evaluation. When blisters do form, appropriate management can minimize lost time.
Friction blisters result from repetitive friction and strain forces that develop between the skin and various objects. Blisters form in areas where the stratum corneum and stratum granulosum are sufficiently robust (Figure), such as the palmar and plantar surfaces of the hand and feet. Thus, these layers are capable of transmitting the surface forces to the underlying layer, the stratum spinosum. In areas without strong stratum corneum and stratum granulosum layers, an abrasion forms instead.1
It has been shown that the transmitted frictional forces disrupt the stratum spinosum, with the blister roof being composed of the 2 upper epidermal layers as well as prickle cells of the traumatically disrupted stratum spinosum. The basal cell layer typically shows little damage and the dermal-epidermal junction remains intact.1
Early experimental studies in humans using repeatedly cycled probes demonstrated the pathologic sequence of events in blister formation. First, there is slight exfoliation of the stratum corneum layer, accompanied by a reddened area in the zone of rubbing (erythroderma). This is followed by a pale, narrow demarcation, which forms around the reddened region. Subsequently, this pale area fills in toward the center to occupy the entire affected area, which becomes the blister lesion.1,2
Hydrostatic pressure then causes blister fluid to accumulate within 1 to 2 hours following the trauma. Compared to plasma, the blister fluid has a lower protein level and similar electrolyte content.3,4 Cells in the blister cavity continue to degrade for about 4 hours following the injury, with resumption of cellular activity beginning at 6 hours. Mitotic activity is increased after 24 to 30 hours, and at 48 hours, a new granular layer is present. By 120 hours post-injury, a new stratum corneum is formed.5,6
A number of factors have been found to affect blister formation. Frictional force magnitude and number of cycles play the most obvious role. There is an inverse relationship between the two: as the frictional force increases, fewer cycles are required for blister formation.7 This is likely the reason blisters occur most commonly in areas where the fingertips are in contact with a seam, as opposed to the smoother surface of a baseball.
Many authors have examined moisture’s effect on frictional forces, and found that very dry and very wet skin produce low frictional forces, whereas moist skin produces the highest frictional force.1,2,8-10 In the case of dry skin, this is thought to be due to exfoliation and sloughing of cells from the stratum corneum, which produces a dry lubrication similar to graphite. Very wet skin has a fluid layer that lubricates the 2 surfaces. In the case of moist skin, however, it is hypothesized that surface tension impedes the movement of squamous cells, increasing the frictional forces.2,9 This moist environment is most commonly produced by sweating.
Other factors include skin temperature, which, when elevated, mildly predisposes the skin to blister formation. Some studies have shown temperatures as high as 50°C in rubbing experiments2,7,8,11; however, it should be noted that friction blisters do not resemble second-degree burns, either histologically or clinically.12,13
Blisters in Baseball Pitchers
Blisters in baseball pitchers are a well-known and frequently publicized problem; however, there is a paucity of literature describing the incidence or treatment of such blisters.14,15 The digital pulp experiences frictional forces from the baseball stiches as well as from the distal margin of the nail plate during release of the ball. Forces are transmitted to the ball predominately through the thumb, index, and long fingers. While the thumb acts mainly as a post, the index and long fingers impart the “action” on the ball. Not surprisingly, blisters form most commonly on these 2 fingers. While relatively small in size and significance, the impact of such a blister on a pitcher’s ability to maintain the fine control of his pitches cannot be overlooked. Biomechanical studies have shown that maximum gripping strength is attained when the fingers grasp a dynamometer handle at the level of the distal interphalangeal joint.16 Contact pressure mapping during gripping of a cylindrical object has shown that phalanges 2, 3, and 4 experience the highest forces in gripping and pulling activities.17 No study has specifically addressed phalangeal pressure generation in pitchers, however.
Blister Prevention
Blister prevention and treatment methods in baseball pitchers are steeped in folklore and tradition. Methods for drying out blisters and hardening calluses have included the use of pickle juice, urine, bags of rice, and superglue.14,15 Superglue, surgical glue, or any other foreign substance is not allowed during a game on the finger or hands of pitchers by Major League Baseball rules. Other anecdotal options include the use of compounded medicines that are marketed as creams and sprays designed to toughen skin.
As with other injuries, it is important to recognize any predisposing factors and ways to avoid them. Dampness and temperature (>104°F) have been identified as chief factors that substantially increase the friction coefficient and increase blister incidence.18 While temperature and perspiration are impossible to avoid during competition, steps can be taken to keep the pitcher’s hand dry on the mound as well as between innings, such as a rosin bag, a dry towel, and a rice bucket.
Maintaining fingernail length plays an important role in preventing blister formation. The nail can both protect the adjacent skin by decreasing the frictional force on the skin as well as lead to the development of blisters on the other fingers by repetitive abrasion. Nail length and contour need to be tailored to each pitcher specifically. The length of the nail can protect the finger pulp by minimally “elevating” the ball off of the finger itself. However, too long of a nail may come at the cost of abrading the abutting finger as the spin is imparted onto the ball. The shape of the nail is generally kept well contoured to avoid any sharp edges, which can act as local irritants. In the instance of soft, cracked, or torn nails, some pitchers have used acrylic nails. Maintaining proper fingernail shape and length is an essential preventive measure that requires regular use of clippers and emery boards.
Callus care is also paramount in preventing blister formation. It is believed that development of a callus is inevitable with repetitive throwing and likely protective of the underlying skin. The size and shape of the callus, like that of the nail, needs to be carefully monitored. A callus that becomes overly prominent can lead to increased friction with a baseball seam. This can lead to blister development. A small, smooth callus without edges or loose borders is the goal. The free edges of a callus can be trimmed with clean clippers. Contouring is best performed with careful use of an emery board.
Treatment of Finger Blisters
Blister management is determined by the size of the blister as well as the integrity of the overlying callus. Small blisters with intact skin coverage can be sterilely drained with a needle or a No. 11 blade.6,19-21 This allows apposition of the skin layers and quicker healing. The free edge of the blister can then be repaired with surgical glue. In these instances, a starting pitcher may be required to miss a start to allow further healing. In most cases, there is no need to place the player on the disabled list (DL).
Larger blisters, or those that traumatically open, represent a more concerning issue. The loose layers of skin can be removed, and the raw bed can then be treated with antibiotic ointment for the first 2 to 3 days. Subsequently, benzoin tincture, a commonly used paste of benzoin and alum, can be utilized to toughen the raw skin. Bulky dressings can be applied early in treatment but should then be discouraged, as the underlying skin softens due to the presence of moisture. These instances generally lead to lost time on the field. It is not uncommon that the pitcher requires placement on the 15-day DL.
Summary
Blisters on the fingertips of professional baseball players can lead to significant pain and decreased performance. Prevention of blister formation represents the goal of the player and the medical staff. Skin and nail care requires daily evaluation. When blisters do form, appropriate management can minimize lost time.
1. Sulzberger MB, Cortese TA, Fishman L, Wiley HS. Studies on blisters produced by friction. I. Results of linear rubbing and twisting technics. J Invest Dermatol. 1966;47(5):456-465.
2. Naylor PFD. Experimental friction blisters. Brit J Dermatol. 1955;67(10):327-342.
3. Cortese TA, Mitchell W, Sulzberger MB. Studies on blisters produced by friction. II. The blister fluid. J Invest Dermatol. 1968;50(1):47-53.
4. Schmidt P. Quantification of specific proteins in blister fluid. J Invest Dermatol. 1970;55(4):244-248.
5. Epstein WL, Fukuyama K, Cortese TA. Autographic study of friction blisters. RNA, DNA, and protein synthesis. Arch Dermatol. 1969;99(1):94-106.
6. Cortese TA Jr, Fukuyama K, Epstein W, Sulzberger MB. Treatment of friction blisters. An experimental study. Arch Dermatol. 1968;97(6):717-721.
7. Comaish JS. Epidermal fatigue as a cause of friction blisters. Lancet. 1973;1(7794):81-83.
8. Akers WA, Sulzberger MB. The friction blister. Mil Med. 1972;137(1):l-7.
9. Highley DR, Coomey M, DenBeste M, Wolfman LJ. Frictional properties of skin. J Invest Dermatol. 1977;69(3):303-305.
10. Nacht S, Close J, Yeung D, et al. Skin friction coefficient: changes induced by skin hydration and emollient application and correlation with perceived skin feel. J Soc Cosmet Chern. 1981;32:55-65.
11. Griffin TB, Corqese TA, Layton LL, et al. Inverse time and temperature relationship in experimental friction blisters. J Invest Dermatol. 1969;52:391.
12. Shupp JW, Nazabzadeh TJ, Rosenthal DS, Jordan MH, Fidler P, Jeng JC. A review of the local pathophysiologic bases of burn wound progression. J Burn Care Res. 2010;31(6):849-873.
13. Knapik JJ, Reynolds KL, Duplantis KL, Jones BH. Friction blisters: pathophysiology, prevention and treatment. Sports Med. 1995;20(3):136-147.
14. Sielski M. C.J. Wilson on pitching-hand care. The Wall Street Journal. October 30, 2010. Available at: http://blogs.wsj.com/dailyfix/2010/10/30/cj-wilson-on-caring-for-his-pitching-hand Accessed January 10, 2016.
15. Trezza J. Blisters are normal part of pitching for Lynn. St. Louis Post-Dispatch. July 4, 2014. Available at: http://www.stltoday.com/sports/baseball/professional/blisters-are-normal-part-of-pitching-for-lynn/article_9743c6f9-14b2-5c50-83b4-fa6a3c34cb83.html Accessed January 10, 2016.
16. Kaufmann RA, Kozin SH, Mirarchi A, Holland B, Porter S. Biomechanical analysis of flexor digitorum profundus and superficialis in grip-strenth generation. Am J Orthop. 2007;36(9):E128-E132.
17. Nicholas JW, Corvese RJ, Woolley C, Armstrong TJ. Quantification of hand grasp force using a pressure mapping system. Work. 2012;41(Suppl 1):605-612.
18. Knapik JJ, Reynolds KL. Risk factors for foot blisters during road marching: tobacco use, ethnicity, foot type, previous illness and others. Mil Med. 1999;164(2):92-97.
19. Emer J, Sivek R, Marciniak B. Sports Dermatology: Part 1 of 2. Traumatic or mechanical injuries, inflammatory conditions, and exacerbations of pre-existing conditions. J Clin Aesthet Dermatol. 2015;8(4):31-43.
20. De Luca JF, Adams BB, Yosipovitch G. Skin manifestations of athletes competing in the summer olympics: what a sports medicine physician should know. Sports Med. 2012;42(5):399-413.
21. Helm TN, Bergfeld WF. Sports dermatology. Clin Dermatol. 199;16(1):159-165.
1. Sulzberger MB, Cortese TA, Fishman L, Wiley HS. Studies on blisters produced by friction. I. Results of linear rubbing and twisting technics. J Invest Dermatol. 1966;47(5):456-465.
2. Naylor PFD. Experimental friction blisters. Brit J Dermatol. 1955;67(10):327-342.
3. Cortese TA, Mitchell W, Sulzberger MB. Studies on blisters produced by friction. II. The blister fluid. J Invest Dermatol. 1968;50(1):47-53.
4. Schmidt P. Quantification of specific proteins in blister fluid. J Invest Dermatol. 1970;55(4):244-248.
5. Epstein WL, Fukuyama K, Cortese TA. Autographic study of friction blisters. RNA, DNA, and protein synthesis. Arch Dermatol. 1969;99(1):94-106.
6. Cortese TA Jr, Fukuyama K, Epstein W, Sulzberger MB. Treatment of friction blisters. An experimental study. Arch Dermatol. 1968;97(6):717-721.
7. Comaish JS. Epidermal fatigue as a cause of friction blisters. Lancet. 1973;1(7794):81-83.
8. Akers WA, Sulzberger MB. The friction blister. Mil Med. 1972;137(1):l-7.
9. Highley DR, Coomey M, DenBeste M, Wolfman LJ. Frictional properties of skin. J Invest Dermatol. 1977;69(3):303-305.
10. Nacht S, Close J, Yeung D, et al. Skin friction coefficient: changes induced by skin hydration and emollient application and correlation with perceived skin feel. J Soc Cosmet Chern. 1981;32:55-65.
11. Griffin TB, Corqese TA, Layton LL, et al. Inverse time and temperature relationship in experimental friction blisters. J Invest Dermatol. 1969;52:391.
12. Shupp JW, Nazabzadeh TJ, Rosenthal DS, Jordan MH, Fidler P, Jeng JC. A review of the local pathophysiologic bases of burn wound progression. J Burn Care Res. 2010;31(6):849-873.
13. Knapik JJ, Reynolds KL, Duplantis KL, Jones BH. Friction blisters: pathophysiology, prevention and treatment. Sports Med. 1995;20(3):136-147.
14. Sielski M. C.J. Wilson on pitching-hand care. The Wall Street Journal. October 30, 2010. Available at: http://blogs.wsj.com/dailyfix/2010/10/30/cj-wilson-on-caring-for-his-pitching-hand Accessed January 10, 2016.
15. Trezza J. Blisters are normal part of pitching for Lynn. St. Louis Post-Dispatch. July 4, 2014. Available at: http://www.stltoday.com/sports/baseball/professional/blisters-are-normal-part-of-pitching-for-lynn/article_9743c6f9-14b2-5c50-83b4-fa6a3c34cb83.html Accessed January 10, 2016.
16. Kaufmann RA, Kozin SH, Mirarchi A, Holland B, Porter S. Biomechanical analysis of flexor digitorum profundus and superficialis in grip-strenth generation. Am J Orthop. 2007;36(9):E128-E132.
17. Nicholas JW, Corvese RJ, Woolley C, Armstrong TJ. Quantification of hand grasp force using a pressure mapping system. Work. 2012;41(Suppl 1):605-612.
18. Knapik JJ, Reynolds KL. Risk factors for foot blisters during road marching: tobacco use, ethnicity, foot type, previous illness and others. Mil Med. 1999;164(2):92-97.
19. Emer J, Sivek R, Marciniak B. Sports Dermatology: Part 1 of 2. Traumatic or mechanical injuries, inflammatory conditions, and exacerbations of pre-existing conditions. J Clin Aesthet Dermatol. 2015;8(4):31-43.
20. De Luca JF, Adams BB, Yosipovitch G. Skin manifestations of athletes competing in the summer olympics: what a sports medicine physician should know. Sports Med. 2012;42(5):399-413.
21. Helm TN, Bergfeld WF. Sports dermatology. Clin Dermatol. 199;16(1):159-165.