User login
Almost 27% of medical practices are “super-users” of health information technology, but another 39% are “under-users” that may be affecting “the ability of the health system as a whole to provide coordinated and efficient care,” investigators said in the American Journal of Managed Care.
To put it another way, wrote Juliet Rumball-Smith, MBChB, PhD, and her associates, who analyzed data for 30,123 practices from the 2014 Healthcare Information and Management Systems Society (HIMSS) Analytics ambulatory practice survey.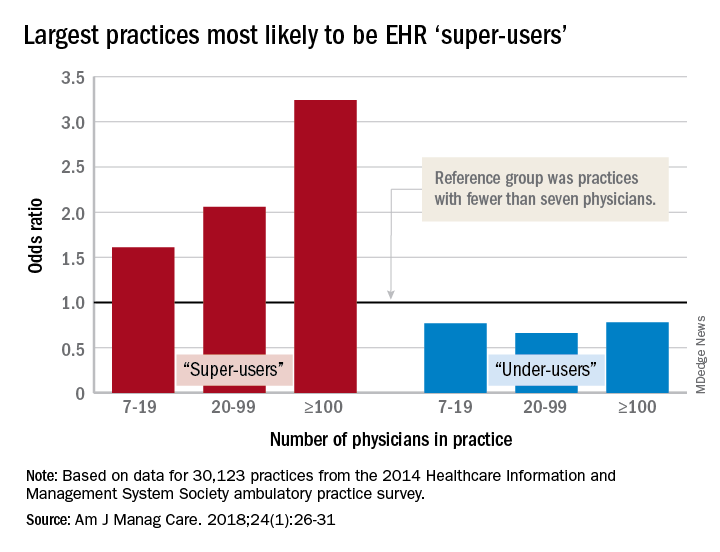
After all the scores were calculated, 8,003 practices (27%) were classified as super-users and 11,706 (39%) as under-users. More specific analysis showed that the smallest practices were least likely to be super-users, and that the likelihood rose with increasing practice size. With practices of fewer than seven physicians as the reference group, odds ratios of being a super-user were 1.61 for practices of 7-19 physicians, 2.06 for those with 20-99 physicians, and 3.24 for those of 100 or more associated physicians, reported Dr. Rumball-Smith and her associates at Rand Health in Santa Monica, Calif.
The situation was not as clear-cut among the technology avoiders, as the odds ratios made practices of 20-99 physicians less likely (0.66) than those of 7-19 (0.77) and 100 or more (0.78) physicians to be under-users, they said.
The super-users also were more likely to located in metropolitan areas (OR, 2.45, compared with rural practices) and in the Midwest (OR, 2.05, compared with the Northeast) or the South (OR, 1.32) and to be primary care/family medicine clinics, which were the reference group for the practice-type comparison (OR, 0.89, for single- or multiple-specialty; 0.64, for specialist services or urgent care), the investigators said.
“It is important that policy makers and health care providers understand the limits of health IT functionality in ambulatory care practices, as strategies aimed at improving the coordination of care or those relying on the EHR as a vehicle for intervention may be hindered by the technological capacity of ambulatory care partners,” they wrote.
The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
SOURCE: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.
Almost 27% of medical practices are “super-users” of health information technology, but another 39% are “under-users” that may be affecting “the ability of the health system as a whole to provide coordinated and efficient care,” investigators said in the American Journal of Managed Care.
To put it another way, wrote Juliet Rumball-Smith, MBChB, PhD, and her associates, who analyzed data for 30,123 practices from the 2014 Healthcare Information and Management Systems Society (HIMSS) Analytics ambulatory practice survey.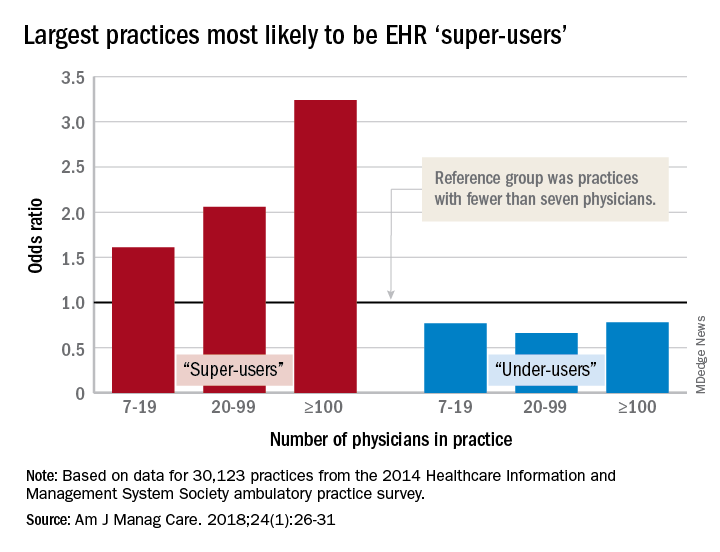
After all the scores were calculated, 8,003 practices (27%) were classified as super-users and 11,706 (39%) as under-users. More specific analysis showed that the smallest practices were least likely to be super-users, and that the likelihood rose with increasing practice size. With practices of fewer than seven physicians as the reference group, odds ratios of being a super-user were 1.61 for practices of 7-19 physicians, 2.06 for those with 20-99 physicians, and 3.24 for those of 100 or more associated physicians, reported Dr. Rumball-Smith and her associates at Rand Health in Santa Monica, Calif.
The situation was not as clear-cut among the technology avoiders, as the odds ratios made practices of 20-99 physicians less likely (0.66) than those of 7-19 (0.77) and 100 or more (0.78) physicians to be under-users, they said.
The super-users also were more likely to located in metropolitan areas (OR, 2.45, compared with rural practices) and in the Midwest (OR, 2.05, compared with the Northeast) or the South (OR, 1.32) and to be primary care/family medicine clinics, which were the reference group for the practice-type comparison (OR, 0.89, for single- or multiple-specialty; 0.64, for specialist services or urgent care), the investigators said.
“It is important that policy makers and health care providers understand the limits of health IT functionality in ambulatory care practices, as strategies aimed at improving the coordination of care or those relying on the EHR as a vehicle for intervention may be hindered by the technological capacity of ambulatory care partners,” they wrote.
The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
SOURCE: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.
Almost 27% of medical practices are “super-users” of health information technology, but another 39% are “under-users” that may be affecting “the ability of the health system as a whole to provide coordinated and efficient care,” investigators said in the American Journal of Managed Care.
To put it another way, wrote Juliet Rumball-Smith, MBChB, PhD, and her associates, who analyzed data for 30,123 practices from the 2014 Healthcare Information and Management Systems Society (HIMSS) Analytics ambulatory practice survey.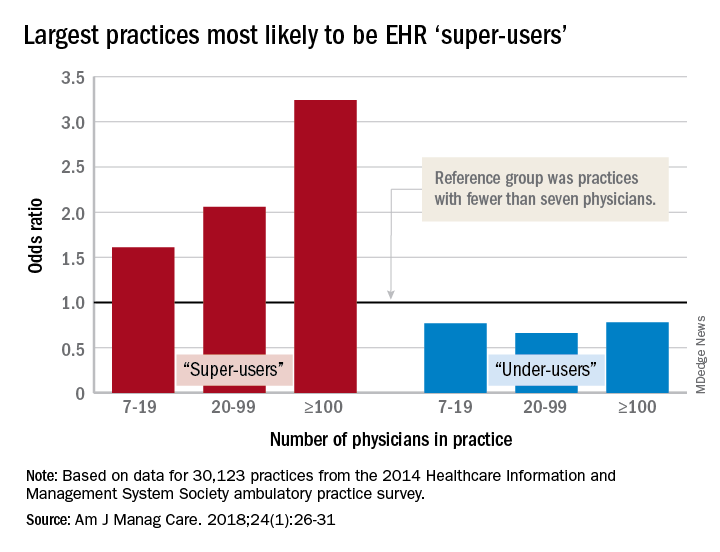
After all the scores were calculated, 8,003 practices (27%) were classified as super-users and 11,706 (39%) as under-users. More specific analysis showed that the smallest practices were least likely to be super-users, and that the likelihood rose with increasing practice size. With practices of fewer than seven physicians as the reference group, odds ratios of being a super-user were 1.61 for practices of 7-19 physicians, 2.06 for those with 20-99 physicians, and 3.24 for those of 100 or more associated physicians, reported Dr. Rumball-Smith and her associates at Rand Health in Santa Monica, Calif.
The situation was not as clear-cut among the technology avoiders, as the odds ratios made practices of 20-99 physicians less likely (0.66) than those of 7-19 (0.77) and 100 or more (0.78) physicians to be under-users, they said.
The super-users also were more likely to located in metropolitan areas (OR, 2.45, compared with rural practices) and in the Midwest (OR, 2.05, compared with the Northeast) or the South (OR, 1.32) and to be primary care/family medicine clinics, which were the reference group for the practice-type comparison (OR, 0.89, for single- or multiple-specialty; 0.64, for specialist services or urgent care), the investigators said.
“It is important that policy makers and health care providers understand the limits of health IT functionality in ambulatory care practices, as strategies aimed at improving the coordination of care or those relying on the EHR as a vehicle for intervention may be hindered by the technological capacity of ambulatory care partners,” they wrote.
The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
SOURCE: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.
FROM AMERICAN JOURNAL OF MANAGED CARE
Key clinical point: Many medical practices are not prepared to take advantage of EHR-based initiatives.
Major finding: 73% of ambulatory practices are not using EHRs “to their full benefit.”
Study details: HIMSS Analytics 2014 ambulatory practice survey for 30,123 practices.
Disclosures: The study was funded by the Commonwealth Fund, Rand, and the Agency for Healthcare Research and Quality. The investigators said that they had no conflicts of interest.
Source: Rumball-Smith J et al. Am J Manag Care. 2018;24(1):26-31.