User login
• Suspect diastolic heart failure in patients who have symptoms of heart failure but a normal ejection fraction, with or without evidence of diastolic abnormalities. B
• Treatment goals for patients who have heart failure with preserved ejection fraction (HFPEF) include normalization of blood pressure, prevention of tachycardia and ischemia, reduction of congestion, and improvement in exercise capacity. B
• Initiate beta-blocker therapy without delay for patients who have acute decompensated HFPEF and tachycardia; consider cardioversion for those with atrial fibrillation. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Most studies of heart failure (HF)—the most common cause of hospitalization in patients older than 65 years1—have focused on patients with reduced ejection fraction (EF). Yet half of those hospitalized for acute decompensated HF have a normal left ventricular EF.2 For these patients, contractility is not the problem—impaired relaxation during diastole is.
Commonly called diastolic HF, heart failure with preserved ejection fraction (HFPEF) is a more precise name for this condition. Patients are usually older than those with a reduced EF.3 Thus, as the US population ages, the prevalence of HFPEF increases, as well.4
Diagnostic criteria have been developed for HFPEF, but there are few large, high-quality studies to guide its treatment. Yet family physicians need to be familiar with HFPEF and know how best to treat it. With extrapolation from studies of patients with reduced EF, as well as expert consensus and our own experience, we offer an evidence-based approach to the management of both stable and acute decompensated HFPEF.
A closer look at diastolic dysfunction
Defined as an abnormality of diastolic compliance, filling, or relaxation of the ventricle, diastolic dysfunction can occur whether EF is normal or abnormal.3 Ventricular diastole includes isovolumic relaxation, early passive filling after mitral valve opening, and active filling during atrial contraction. Transmission of high ventricular pressure to the pulmonary circulation leads to pulmonary edema, dyspnea, and other symptoms of HF. Factors other than abnormal diastolic physiology, such as chronic volume overload, ventricular coupling dyssynchrony, increased autonomic tone leading to reduced venous capacitance, and chronotropic intolerance, may also be involved.5
Patient history: What to look for
A variety of conditions, including ischemia, tachycardia, impaired myocardial relaxation, and age-related loss of myocardial compliance, can contribute to abnormal diastolic function, but the major causes of HFPEF are chronic hypertension, hypertrophic cardiomyopathy, and coronary artery disease (CAD).3 Rarely, infiltrative or restrictive cardiomyopathy (eg, amyloidosis or sarcoidosis) is implicated.6 Noncardiovascular comorbidities such as diabetes, renal impairment, anemia, and chronic lung disease are more prevalent among those with HFPEF, and more women are affected than men.1
Mortality risk. In a study of more than 100,000 hospitalizations for acute decompensated HF, patients with preserved EF had lower in-hospital mortality (3% vs 4% for those with reduced EF).2 Patients with both diabetes and CAD commonly develop HFPEF,7 and the presence of these comorbidities are an independent predictor of 5-year mortality.8
Population studies suggest that 5-year mortality rates for African Americans with HFPEF are higher than for Caucasians with this condition.9 Other predictors of mortality include older age, male sex, lower left ventricular EF, ischemic disease, impaired renal function, and peripheral arterial disease.10-12
Diagnosing HFPEF: What you’ll see, when to test
The presentation of patients with HFPEF is similar to that of individuals with reduced EF. In an outpatient setting, both groups will have reduced exercise capacity; increased neuroendocrine activation, which may cause chronic fluid retention, vasoconstriction, and tachycardia; and a reduced quality of life.5
Neither the American College of Cardiology/American Heart Association (ACC/AHA) nor the Heart Failure Society of America (HFSA)13,14 recommends screening for asymptomatic left ventricular dysfunction. For those with signs and symptoms of HF, however, echocardiography is a key component of the initial evaluation. Echocardiography provides information about left ventricular systolic function, including EF, regional wall motion abnormalities, and wall thickness. Echocardiographic evidence of diastolic abnormalities is found for some patients with HFPEF, while others have no demonstrable diastolic dysfunction.3
While an electrocardiogram (EKG) cannot distinguish between HF with reduced EF and HFPEF, common findings might include signs of ventricular hypertrophy or tachycardia during acute exacerbations. An EKG should be obtained in patients with suspected HF to screen for antecedent causes such as hypertrophy, atrial fibrillation, and ischemia.15
What Doppler echocardiography and the E/A ratio reveal
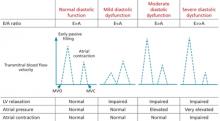
Doppler echocardiography is used to further evaluate the characteristics of blood flow, showing the relationship among left ventricular (LV) relaxation, atrial pressure, atrial contraction, and blood flow velocity across the mitral valve during diastole. The peak velocity of blood flow during early diastole (called the “E wave”) and late diastole (the atrial contraction, or “A wave”) is measured and the E/A ratio (reflecting the transmitral blood flow pattern) is calculated (FIGURE).3
FIGURE
The E/A ratio* and what it reveals
A, atrial contraction; E, early passive filling; MVC, mitral valve closes; MVO, mitral valve opens.
*E/A ratio represents the relationship between the peak velocity of blood flow during early diastole (E wave) and late diastole (A wave).
Adapted from: Aurigemma GP, Gaasch WH. N Engl J Med. 2004.3
Normally, transmitral flow velocity is greater during early diastole than during atrial contraction, and the E/A ratio is approximately 1.5 (E>A). With early diastolic dysfunction, impaired relaxation prevents blood from flowing passively into the LV during early diastole. This causes reversal of the E/A ratio, which drops to <1 (E<A). As diastolic function worsens, atrial contraction is impaired, and left atrial pressure rises. The result: A reduction in the A wave amplitude and proportionally more blood flow during early diastole and a “pseudonormal” (E>A) ratio, with a greater difference between the E and A than is normally observed. This finding is an independent predictor of all-cause mortality in patients with asymptomatic HF.16
Cardiac catheterization. Invasive measurement of LV filling pressures is the gold standard for diagnosing HFPEF. If echocardiography does not lead to a clear diagnosis, cardiac catheterization can provide information about concomitant pulmonary hypertension and mechanical asynchrony that may contribute to symptomatic HF.1 When the diagnosis is uncertain, additional testing—eg, plasma brain natriuretic peptide (BNP), chest x-ray, or exercise testing—may be necessary to establish a diagnosis of symptomatic HF.
The diagnostic criteria developed by HFSA include clinical evidence of HF and:
- echocardiographic evidence of LV hypertrophy or left atrial enlargement (without atrial fibrillation) or
- evidence of diastolic dysfunction on Doppler echocardiography or cardiac catheterization.14
It is important to note that the diagnostic criteria have not been validated, and the sensitivity and specificity of the various clinical findings are not known.
CASE Carrie W, a 76-year-old woman referred to you by a colleague, presents for follow-up after being hospitalized for HF. She recalls feeling fatigue, chest pain, and out of breath with even minimal exertion before being admitted to the hospital.
You obtain her hospital records, which show that echocardiography found impaired LV relaxation based on a reversed E/A ratio and an EF of 65%. In addition, BNP was elevated, and a chest x-ray showed pulmonary vascular congestion. You note that her blood pressure was 175/103 mm Hg on admission and an EKG showed LV hypertrophy and sinus tachycardia, but no ischemia.
Before being hospitalized, Ms. W was taking extended-release metoprolol, aspirin, and lisinopril. The hospitalist added lovastatin and increased the daily dose of extended-release metoprolol from 25 to 100 mg.
What changes, if any, would you make in her medication regimen?
Diastolic dysfunction as chronic disease
Often asymptomatic, diastolic dysfunction should be thought of as a chronic progressive disease characterized by complex physiologic adaptations that vary over time (See “Staging heart failure: The clinical course of HFPEF”.13) Patients with HFPEF have a difficult time tolerating hemodynamic stress and any perturbation of afterload, heart rate, or ventricular function can precipitate an acute exacerbation.2 Clinical factors that precipitate acute decompensation of HFPEF—which we’ll discuss a bit later—include uncontrolled hypertension; atrial fibrillation; and noncardiovascular comorbidities such as lung disease, renal impairment, or sepsis.2
The ACC/AHA staging system for HF can be applied to patients with HFPEF, both to classify disease severity and to track the progression of the disease. Patients at Stage A are at high risk of developing HF, but early and aggressive treatment of hypertension and other cardiovascular risk factors may delay or potentially prevent the onset of overt disease. Stage B refers to patients with known structural disease, such as a history of myocardial infarction or systolic or diastolic dysfunction, but no symptoms of HF.
Patients at Stage C have evidence of structural disease and symptoms of HF, such as fatigue, shortness of breath, or reduced exercise tolerance. This stage represents the spectrum of patients falling into New York Heart Association (NYHA) Class 1 through 3 categories. Finally, patients at Stage D—analogous to NYHA Class 4—have refractory HF, with marked symptoms even at rest despite maximal medical therapy.
The Acute Decompensated HEart failure national REgistry (ADHERE), in which the records of well over 80,000 Medicare patients were reviewed, found that more than 60% of those hospitalized with HFPEF had uncontrolled hypertension, with a systolic pressure >140 mm Hg; 21% had atrial fibrillation.2 These findings emphasize the importance of aggressive blood pressure (BP) and heart rate control.
Management of HFPEF is goal directed
The aim of pharmacologic treatment of HFPEF is to maintain fluid balance, prevent tachycardia, treat and prevent ischemia, and control hypertension (TABLE).14,17-30 While the use of angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and beta-blockers, among other pharmacologic agents, is well studied for patients with reduced EF, there is limited evidence to guide the treatment of those with HFPEF. Although no single agent or drug class has been shown to be superior for such patients, there are a number of pharmacologic treatments to consider.
TABLE
Management of heart failure with preserved ejection fraction—matching treatment and goals14,17-30
| Treatment goal | Modality |
|---|---|
| Reduce congestion | Diuretics Salt restriction |
| Maintain atrial contraction | A-V pacing Cardioversion |
| Prevent tachycardia | A-V pacing Beta-blockers Calcium channel blockers |
| Prevent/treat ischemia | Antiplatelet therapy Beta-blockers Calcium channel blockers Revascularization Statins |
| Control hypertension | Antihypertensive agents:
|
| Promote regression of LV remodeling | ACE inhibitors ARBs |
| Improve exercise capacity | Supervised exercise program |
| ACE, angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; LV, left ventricle. | |
Inhibition of the renin-angiotensin-aldosterone system
Pathologic activation of the renin-angiotensin-aldosterone system (RAAS) contributes to elevated systolic and diastolic pressure, LV hypertrophy, and LV fibrosis. Inhibition of this system is a promising treatment modality for HFPEF.31
ACE inhibitors. Experimental studies suggest that ACE inhibitors benefit the diastolic properties of the heart, in both short- and long-term use. The PEP-CHF trial found that for older patients with diastolic dysfunction, perindopril led to significant improvements in functional class and exercise capacity but failed to show a statistically significant reduction in all-cause mortality or hospitalization for acute decompensated HF.17
ARBs. There is no evidence to show that ARB therapy improves morbidity or mortality in HFPEF. Using surrogate end points, ARBs have been associated with regression of LV hypertrophy, and losartan was found to improve exercise tolerance and quality of life, compared with hydrochlorothiazide.18,19 In the CHARM-Preserved trial, candesartan showed an insignificant reduction in cardiovascular mortality and hospitalization for HF.
These results must be viewed with caution, however, because adverse effects led to high rates of medication discontinuation.32 In the I-PRESERVE trial, irbesartan conferred no benefit with respect to mortality, hospitalization, or quality of life on patients with HFPEF.33
ACE inhibitor or ARB—not both. ACE inhibitors and ARBs are good choices for BP control in patients with HFPEF, especially if LV hypertrophy is present, but periodic testing of renal function and potassium levels is needed. ACE inhibitors and ARBs should not be used concurrently, as the combination increases the risk of acute renal failure and has no benefit in clinical outcomes.34
BP and rate control
In small trials, beta-blockers have been found to improve diastolic function as seen on echocardiography, but data on morbidity and mortality are lacking.20 A secondary analysis of the OPTIMIZE-HF registry found that beta-blocker therapy was associated with reduced mortality and readmission in patients with reduced EF, but not in those with normal EF.21
Findings from the SENIORS trial were more promising: Treatment with nebivolol reduced both mortality and readmission rates for elderly patients with HF, with similar benefits for those with reduced and preserved EF.22 Overall, beta-blockers appear to be a reasonable choice for heart rate and/or BP control in patients who have HFPEF and atrial fibrillation or hypertension. Carvedilol, long-acting metoprolol, and bisoprolol have been shown to reduce mortality in HF with reduced EF, and it is reasonable to choose one of these agents for patients with preserved EF, as well.23
Calcium channel blockers (CCBs) may be useful in treating patients with HFPEF for both BP and heart rate control, as well. Theoretically, CCBs may also improve the process of relaxation by altering intracellular calcium cycling during the contractile cycle in myocytes. This contrasts with the management of HF patients with reduced EF, for whom the use of nonselective CCBs such as diltiazem and verapamil may adversely affect contractility.
In small RCTs, verapamil has been found to improve HF symptoms and exercise tolerance in patients with HFPEF,24 but no evidence of improved outcomes or mortality rates with CCB use has been found.
Other pharmacologic options to consider
Aldosterone antagonist therapy is an important component of treatment for patients with HF with reduced EF. Data supporting the use of spironolactone use from the RALES trial and eplerenone in the EPHESUS and EMPHASIS-HF trials suggest a reduction in mortality in patients with low (<35%) LVEF.25-27 For patients with preserved EF, however, spironolactone is not generally recommended.
A large National Institutes of Health-sponsored trial is underway to determine if the drug is beneficial for patients with preserved LVEF, and will build on a small study in which 30 patients with HFPEF showed improved myocardial function after treatment with spironolactone.35 Until more data become available, the risks of using aldosterone antagonists outweigh the evidence to support their use in this patient population.
Diuretics are an important component of treatment for all patients with HF and fluid overload. The Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial (ALLHAT) showed a reduced incidence of symptomatic HFPEF in patients taking diuretics.28 As is the case with patients with reduced EF, those with preserved EF should be treated with diuretics if they have symptoms of fluid overload.
Statins. Intensive lipid lowering with statin therapy has been shown in observational studies to benefit patients with HFPEF with respect to mortality, independent of baseline low-density lipoprotein cholesterol.29 RCTs are needed to confirm these observations, but statin therapy is recommended for the secondary prevention of cardiovascular disease, independent of the presence of diastolic dysfunction or HFPEF.
Guard against hypotension. Patients with diastolic dysfunction are susceptible to hypotension if there is a rapid reduction in preload with diuretics, nonselective CCBs, or nitrates, so it is important that doses be titrated slowly.
Nonpharmacologic measures are important, too
In addition to optimizing treatment of comorbid conditions, patients with HFPEF should be advised that lifestyle modifications such as weight loss, smoking cessation, and dietary changes can do much to reduce the risk. You can help by providing an exercise “prescription” (with a specified intensity, frequency, and duration) and dietary guidelines, with emphasis on the importance of a low-sodium diet to prevent fluid overload.14,30 Recommend local programs for patients with HF, which many hospitals and health systems offer as part of their efforts to reduce readmission rates.
Consider cardioversion
Tachycardia shortens the time for filling during diastole; thus, it is poorly tolerated in patients with diastolic dysfunction and could trigger acute decompensation. To avoid the risk, restoration of sinus rhythm should be considered for patients with HFPEF and atrial fibrillation. Patients with known paroxysmal or permanent atrial fibrillation and preserved EF should be seen by a cardiologist to determine whether direct current cardioversion or ablation with a permanent pacemaker is appropriate.11 When cardioversion is contraindicated, a beta-blocker is needed to control heart rate and improve hemodynamics.
Patients with stable angina and HFPEF should be evaluated for revascularization when medical therapy alone is not sufficient for symptom relief.10 Here, too, a cardiology consult is indicated for any patient who has HF and an abnormal noninvasive stress test or persistent symptoms despite optimal drug therapy.
Recognizing and responding to acute decompensated HFPEF
The initial response to acute decompensated HFPEF, like that of HF with reduced EF, should be focused on restoring volume status and providing oxygenation, ventilation, and vasodilator therapy in some cases.11 Unlike those with acute decompensated HF with reduced EF, however, patients with HFPEF can safely tolerate the initiation of beta-blockers in the acute phase, especially when rate control is needed.3 Inotropic agents like digoxin and dobutamine, however, are contraindicated.3
Guidelines recommend hospitalization for patients with abnormal vital signs, arrhythmia, and suspected acute coronary syndromes, and consideration of hospitalization for those with associated comorbid conditions, new HF, or progressive fluid overload.13
CASE Because Ms. W has a normal BP and heart rate and is feeling well, you decline to alter her medication regimen. You do, however, recommend that she begin an exercise program, adopt a low-sodium diet, and maintain regular contact with your office so you can evaluate any changes in status.
You introduce Ms. W to the nurse case manager in your office. The nurse works with the patient to develop an action plan that includes daily tracking of her weight and sodium intake; a progressive walking program, starting with 2-minute sessions and progressing to 15 to 30 minutes 3 to 5 times a week; weekly telephone checkins; and immediate calls to report any weight increase or symptoms of HF.
At follow-up 6 months later, Ms. W has improved BP and reports that she enjoys her new exercise routine. She has more energy and denies any edema or breathing difficulties.
1. Lam CSP, Donal E, Kraigher-Krainer E, et al. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13:18-28.
2. Yancy CW, Lopatin M, Stevenson LW, et al. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the acute decompensated heart failure national registry (ADHERE) database. J Am Coll Cardiol. 2006;47:76-84.
3. Aurigemma GP, Gaasch WH. Diastolic heart failure. N Engl J Med. 2004;351:1097-1105.
4. Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251-259.
5. Bench T, Burkhoff D, O’Connell JB, et al. Heart failure with normal ejection fraction: consideration of mechanisms other than diastolic dysfunction. Curr Heart Fail Rep. 2009;6:57-64.
6. Ammash NM, Seward JB, Bailey KR, et al. Clinical profile and outcome of idiopathic restrictive cardiomyopathy. Circulation. 2000;101:2490-2496.
7. Bell DSH. Diabetic cardiomyopathy. Diabetes Care. 2003;26:2949-2951.
8. From AM, Scott CG, Chen HH. The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction: a population-based study. J Am Coll Cardiol. 2010;55:300-305.
9. East MA, Peterson ED, Shaw LK, et al. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J. 2004;148:151-156.
10. Ahmed A, Aronow WS, Fleg JL. Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J. 2006;151:444-450.
11. Hillege HL, Nitsch D, Pfeffer MA, et al. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation. 2006;113:671-678.
12. Somaratne JB, Berry C, McMurray JJ, et al. The prognostic significance of heart failure with preserved left ventricular ejection fraction: a literature-based meta-analysis. Eur J Heart Fail. 2009;11:855-862.
13. 2005 Writing committee members; Hunt SA, Abraham WT, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults. Circulation. 2009;119:e391-e479.
14. Heart Failure Society of America. HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16:e1-e2.
15. Davie AP, Francis CM, Love MP, et al. Value of the electrocardiogram in identifying heart failure due to left ventricular systolic dysfunction. BMJ. 1996;312:222.-
16. Halley CM, Houghtaling PL, Khalil MK, et al. Mortality rate in patients with diastolic dysfunction and normal systolic function. Arch Intern Med. 2011;171:1082-1087.
17. Cleland JGF, Tendera M, Adamus J, et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338-2345.
18. Wachtell K, Bella JN, Rokkedal J, et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment. Circulation. 2002;105:1071-1076.
19. Little WC, Zile MR, Klein A, et al. Effect of losartan and hydrochlorothiazide on exercise tolerance in exertional hypertension and left ventricular diastolic dysfunction. Am J Cardiol. 2006;98:383-385.
20. Bonow RO, Udelson JE. Left ventricular diastolic dysfunction as a cause of congestive heart failure. Mechanisms and management Ann Intern Med. 1992;117:502-510.
21. Hernandez AF, Hammill BG, O’Connor CM, et al. Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (organized program to initiate lifesaving treatment in hospitalized patients with heart failure) registry. J Am Coll Cardiol. 2009;53:184-192.
22. Flather MD, Shibata MC, Coats AJS, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26:215-225.
23. Chavey WE, Bleske BE, Van Harrison R, et al. Pharmacologic management of heart failure caused by systolic dysfunction. Am Fam Physician. 2008;77:957-964.
24. Setaro JF, Zaret BL, Schulman DS, et al. Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol. 1990;66:981-986.
25. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999;341:709-717.
26. Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309-1321.
27. Zannad F, McMurray JJV, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11-21.
28. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA. 2002;288:2981-2997.
29. Fukuta H, Sane DC, Brucks S, et al. Statin therapy may be associated with lower mortality in patients with diastolic heart failure. Circulation. 2005;112:357-363.
30. Arcand JAL, Brazel S, Joliffe C, et al. Education by a dietitian in patients with heart failure results in improved adherence with a sodium-restricted diet: a randomized trial. Am Heart J. 2005;150:716.e1-716.e5.
31. Bernal J, Pitta SR, Thatai D. Role of the renin-angiotensin-aldosterone system in diastolic heart failure: potential for pharmacologic intervention. Am J Cardiovasc Drugs. 2006;6:373-381.
32. Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet. 2003;362:777-781.
33. Massie BM, Carson PE, McMurray JJ, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456-2467.
34. Heran BS, Musini VM, Bassett K, et al. Angiotensin receptor blockers for heart failure. Cochrane Database Syst Rev. 2012;(4):CD003040.-
35. Mottram PM, Haluska B, Leano R, et al. Effect of aldosterone antagonism on myocardial dysfunction in hypertensive patients with diastolic heart failure. Circulation. 2004;0110:558-565.
CORRESPONDENCE Geoffrey D. Mills, MD, PhD, Department of Family and Community Medicine, Jefferson Medical College, 833 Chestnut Street, Suite 301, Philadelphia, PA 19107; [email protected]
• Suspect diastolic heart failure in patients who have symptoms of heart failure but a normal ejection fraction, with or without evidence of diastolic abnormalities. B
• Treatment goals for patients who have heart failure with preserved ejection fraction (HFPEF) include normalization of blood pressure, prevention of tachycardia and ischemia, reduction of congestion, and improvement in exercise capacity. B
• Initiate beta-blocker therapy without delay for patients who have acute decompensated HFPEF and tachycardia; consider cardioversion for those with atrial fibrillation. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Most studies of heart failure (HF)—the most common cause of hospitalization in patients older than 65 years1—have focused on patients with reduced ejection fraction (EF). Yet half of those hospitalized for acute decompensated HF have a normal left ventricular EF.2 For these patients, contractility is not the problem—impaired relaxation during diastole is.
Commonly called diastolic HF, heart failure with preserved ejection fraction (HFPEF) is a more precise name for this condition. Patients are usually older than those with a reduced EF.3 Thus, as the US population ages, the prevalence of HFPEF increases, as well.4
Diagnostic criteria have been developed for HFPEF, but there are few large, high-quality studies to guide its treatment. Yet family physicians need to be familiar with HFPEF and know how best to treat it. With extrapolation from studies of patients with reduced EF, as well as expert consensus and our own experience, we offer an evidence-based approach to the management of both stable and acute decompensated HFPEF.
A closer look at diastolic dysfunction
Defined as an abnormality of diastolic compliance, filling, or relaxation of the ventricle, diastolic dysfunction can occur whether EF is normal or abnormal.3 Ventricular diastole includes isovolumic relaxation, early passive filling after mitral valve opening, and active filling during atrial contraction. Transmission of high ventricular pressure to the pulmonary circulation leads to pulmonary edema, dyspnea, and other symptoms of HF. Factors other than abnormal diastolic physiology, such as chronic volume overload, ventricular coupling dyssynchrony, increased autonomic tone leading to reduced venous capacitance, and chronotropic intolerance, may also be involved.5
Patient history: What to look for
A variety of conditions, including ischemia, tachycardia, impaired myocardial relaxation, and age-related loss of myocardial compliance, can contribute to abnormal diastolic function, but the major causes of HFPEF are chronic hypertension, hypertrophic cardiomyopathy, and coronary artery disease (CAD).3 Rarely, infiltrative or restrictive cardiomyopathy (eg, amyloidosis or sarcoidosis) is implicated.6 Noncardiovascular comorbidities such as diabetes, renal impairment, anemia, and chronic lung disease are more prevalent among those with HFPEF, and more women are affected than men.1
Mortality risk. In a study of more than 100,000 hospitalizations for acute decompensated HF, patients with preserved EF had lower in-hospital mortality (3% vs 4% for those with reduced EF).2 Patients with both diabetes and CAD commonly develop HFPEF,7 and the presence of these comorbidities are an independent predictor of 5-year mortality.8
Population studies suggest that 5-year mortality rates for African Americans with HFPEF are higher than for Caucasians with this condition.9 Other predictors of mortality include older age, male sex, lower left ventricular EF, ischemic disease, impaired renal function, and peripheral arterial disease.10-12
Diagnosing HFPEF: What you’ll see, when to test
The presentation of patients with HFPEF is similar to that of individuals with reduced EF. In an outpatient setting, both groups will have reduced exercise capacity; increased neuroendocrine activation, which may cause chronic fluid retention, vasoconstriction, and tachycardia; and a reduced quality of life.5
Neither the American College of Cardiology/American Heart Association (ACC/AHA) nor the Heart Failure Society of America (HFSA)13,14 recommends screening for asymptomatic left ventricular dysfunction. For those with signs and symptoms of HF, however, echocardiography is a key component of the initial evaluation. Echocardiography provides information about left ventricular systolic function, including EF, regional wall motion abnormalities, and wall thickness. Echocardiographic evidence of diastolic abnormalities is found for some patients with HFPEF, while others have no demonstrable diastolic dysfunction.3
While an electrocardiogram (EKG) cannot distinguish between HF with reduced EF and HFPEF, common findings might include signs of ventricular hypertrophy or tachycardia during acute exacerbations. An EKG should be obtained in patients with suspected HF to screen for antecedent causes such as hypertrophy, atrial fibrillation, and ischemia.15
What Doppler echocardiography and the E/A ratio reveal
Doppler echocardiography is used to further evaluate the characteristics of blood flow, showing the relationship among left ventricular (LV) relaxation, atrial pressure, atrial contraction, and blood flow velocity across the mitral valve during diastole. The peak velocity of blood flow during early diastole (called the “E wave”) and late diastole (the atrial contraction, or “A wave”) is measured and the E/A ratio (reflecting the transmitral blood flow pattern) is calculated (FIGURE).3
FIGURE
The E/A ratio* and what it reveals
A, atrial contraction; E, early passive filling; MVC, mitral valve closes; MVO, mitral valve opens.
*E/A ratio represents the relationship between the peak velocity of blood flow during early diastole (E wave) and late diastole (A wave).
Adapted from: Aurigemma GP, Gaasch WH. N Engl J Med. 2004.3
Normally, transmitral flow velocity is greater during early diastole than during atrial contraction, and the E/A ratio is approximately 1.5 (E>A). With early diastolic dysfunction, impaired relaxation prevents blood from flowing passively into the LV during early diastole. This causes reversal of the E/A ratio, which drops to <1 (E<A). As diastolic function worsens, atrial contraction is impaired, and left atrial pressure rises. The result: A reduction in the A wave amplitude and proportionally more blood flow during early diastole and a “pseudonormal” (E>A) ratio, with a greater difference between the E and A than is normally observed. This finding is an independent predictor of all-cause mortality in patients with asymptomatic HF.16
Cardiac catheterization. Invasive measurement of LV filling pressures is the gold standard for diagnosing HFPEF. If echocardiography does not lead to a clear diagnosis, cardiac catheterization can provide information about concomitant pulmonary hypertension and mechanical asynchrony that may contribute to symptomatic HF.1 When the diagnosis is uncertain, additional testing—eg, plasma brain natriuretic peptide (BNP), chest x-ray, or exercise testing—may be necessary to establish a diagnosis of symptomatic HF.
The diagnostic criteria developed by HFSA include clinical evidence of HF and:
- echocardiographic evidence of LV hypertrophy or left atrial enlargement (without atrial fibrillation) or
- evidence of diastolic dysfunction on Doppler echocardiography or cardiac catheterization.14
It is important to note that the diagnostic criteria have not been validated, and the sensitivity and specificity of the various clinical findings are not known.
CASE Carrie W, a 76-year-old woman referred to you by a colleague, presents for follow-up after being hospitalized for HF. She recalls feeling fatigue, chest pain, and out of breath with even minimal exertion before being admitted to the hospital.
You obtain her hospital records, which show that echocardiography found impaired LV relaxation based on a reversed E/A ratio and an EF of 65%. In addition, BNP was elevated, and a chest x-ray showed pulmonary vascular congestion. You note that her blood pressure was 175/103 mm Hg on admission and an EKG showed LV hypertrophy and sinus tachycardia, but no ischemia.
Before being hospitalized, Ms. W was taking extended-release metoprolol, aspirin, and lisinopril. The hospitalist added lovastatin and increased the daily dose of extended-release metoprolol from 25 to 100 mg.
What changes, if any, would you make in her medication regimen?
Diastolic dysfunction as chronic disease
Often asymptomatic, diastolic dysfunction should be thought of as a chronic progressive disease characterized by complex physiologic adaptations that vary over time (See “Staging heart failure: The clinical course of HFPEF”.13) Patients with HFPEF have a difficult time tolerating hemodynamic stress and any perturbation of afterload, heart rate, or ventricular function can precipitate an acute exacerbation.2 Clinical factors that precipitate acute decompensation of HFPEF—which we’ll discuss a bit later—include uncontrolled hypertension; atrial fibrillation; and noncardiovascular comorbidities such as lung disease, renal impairment, or sepsis.2
The ACC/AHA staging system for HF can be applied to patients with HFPEF, both to classify disease severity and to track the progression of the disease. Patients at Stage A are at high risk of developing HF, but early and aggressive treatment of hypertension and other cardiovascular risk factors may delay or potentially prevent the onset of overt disease. Stage B refers to patients with known structural disease, such as a history of myocardial infarction or systolic or diastolic dysfunction, but no symptoms of HF.
Patients at Stage C have evidence of structural disease and symptoms of HF, such as fatigue, shortness of breath, or reduced exercise tolerance. This stage represents the spectrum of patients falling into New York Heart Association (NYHA) Class 1 through 3 categories. Finally, patients at Stage D—analogous to NYHA Class 4—have refractory HF, with marked symptoms even at rest despite maximal medical therapy.
The Acute Decompensated HEart failure national REgistry (ADHERE), in which the records of well over 80,000 Medicare patients were reviewed, found that more than 60% of those hospitalized with HFPEF had uncontrolled hypertension, with a systolic pressure >140 mm Hg; 21% had atrial fibrillation.2 These findings emphasize the importance of aggressive blood pressure (BP) and heart rate control.
Management of HFPEF is goal directed
The aim of pharmacologic treatment of HFPEF is to maintain fluid balance, prevent tachycardia, treat and prevent ischemia, and control hypertension (TABLE).14,17-30 While the use of angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and beta-blockers, among other pharmacologic agents, is well studied for patients with reduced EF, there is limited evidence to guide the treatment of those with HFPEF. Although no single agent or drug class has been shown to be superior for such patients, there are a number of pharmacologic treatments to consider.
TABLE
Management of heart failure with preserved ejection fraction—matching treatment and goals14,17-30
| Treatment goal | Modality |
|---|---|
| Reduce congestion | Diuretics Salt restriction |
| Maintain atrial contraction | A-V pacing Cardioversion |
| Prevent tachycardia | A-V pacing Beta-blockers Calcium channel blockers |
| Prevent/treat ischemia | Antiplatelet therapy Beta-blockers Calcium channel blockers Revascularization Statins |
| Control hypertension | Antihypertensive agents:
|
| Promote regression of LV remodeling | ACE inhibitors ARBs |
| Improve exercise capacity | Supervised exercise program |
| ACE, angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; LV, left ventricle. | |
Inhibition of the renin-angiotensin-aldosterone system
Pathologic activation of the renin-angiotensin-aldosterone system (RAAS) contributes to elevated systolic and diastolic pressure, LV hypertrophy, and LV fibrosis. Inhibition of this system is a promising treatment modality for HFPEF.31
ACE inhibitors. Experimental studies suggest that ACE inhibitors benefit the diastolic properties of the heart, in both short- and long-term use. The PEP-CHF trial found that for older patients with diastolic dysfunction, perindopril led to significant improvements in functional class and exercise capacity but failed to show a statistically significant reduction in all-cause mortality or hospitalization for acute decompensated HF.17
ARBs. There is no evidence to show that ARB therapy improves morbidity or mortality in HFPEF. Using surrogate end points, ARBs have been associated with regression of LV hypertrophy, and losartan was found to improve exercise tolerance and quality of life, compared with hydrochlorothiazide.18,19 In the CHARM-Preserved trial, candesartan showed an insignificant reduction in cardiovascular mortality and hospitalization for HF.
These results must be viewed with caution, however, because adverse effects led to high rates of medication discontinuation.32 In the I-PRESERVE trial, irbesartan conferred no benefit with respect to mortality, hospitalization, or quality of life on patients with HFPEF.33
ACE inhibitor or ARB—not both. ACE inhibitors and ARBs are good choices for BP control in patients with HFPEF, especially if LV hypertrophy is present, but periodic testing of renal function and potassium levels is needed. ACE inhibitors and ARBs should not be used concurrently, as the combination increases the risk of acute renal failure and has no benefit in clinical outcomes.34
BP and rate control
In small trials, beta-blockers have been found to improve diastolic function as seen on echocardiography, but data on morbidity and mortality are lacking.20 A secondary analysis of the OPTIMIZE-HF registry found that beta-blocker therapy was associated with reduced mortality and readmission in patients with reduced EF, but not in those with normal EF.21
Findings from the SENIORS trial were more promising: Treatment with nebivolol reduced both mortality and readmission rates for elderly patients with HF, with similar benefits for those with reduced and preserved EF.22 Overall, beta-blockers appear to be a reasonable choice for heart rate and/or BP control in patients who have HFPEF and atrial fibrillation or hypertension. Carvedilol, long-acting metoprolol, and bisoprolol have been shown to reduce mortality in HF with reduced EF, and it is reasonable to choose one of these agents for patients with preserved EF, as well.23
Calcium channel blockers (CCBs) may be useful in treating patients with HFPEF for both BP and heart rate control, as well. Theoretically, CCBs may also improve the process of relaxation by altering intracellular calcium cycling during the contractile cycle in myocytes. This contrasts with the management of HF patients with reduced EF, for whom the use of nonselective CCBs such as diltiazem and verapamil may adversely affect contractility.
In small RCTs, verapamil has been found to improve HF symptoms and exercise tolerance in patients with HFPEF,24 but no evidence of improved outcomes or mortality rates with CCB use has been found.
Other pharmacologic options to consider
Aldosterone antagonist therapy is an important component of treatment for patients with HF with reduced EF. Data supporting the use of spironolactone use from the RALES trial and eplerenone in the EPHESUS and EMPHASIS-HF trials suggest a reduction in mortality in patients with low (<35%) LVEF.25-27 For patients with preserved EF, however, spironolactone is not generally recommended.
A large National Institutes of Health-sponsored trial is underway to determine if the drug is beneficial for patients with preserved LVEF, and will build on a small study in which 30 patients with HFPEF showed improved myocardial function after treatment with spironolactone.35 Until more data become available, the risks of using aldosterone antagonists outweigh the evidence to support their use in this patient population.
Diuretics are an important component of treatment for all patients with HF and fluid overload. The Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial (ALLHAT) showed a reduced incidence of symptomatic HFPEF in patients taking diuretics.28 As is the case with patients with reduced EF, those with preserved EF should be treated with diuretics if they have symptoms of fluid overload.
Statins. Intensive lipid lowering with statin therapy has been shown in observational studies to benefit patients with HFPEF with respect to mortality, independent of baseline low-density lipoprotein cholesterol.29 RCTs are needed to confirm these observations, but statin therapy is recommended for the secondary prevention of cardiovascular disease, independent of the presence of diastolic dysfunction or HFPEF.
Guard against hypotension. Patients with diastolic dysfunction are susceptible to hypotension if there is a rapid reduction in preload with diuretics, nonselective CCBs, or nitrates, so it is important that doses be titrated slowly.
Nonpharmacologic measures are important, too
In addition to optimizing treatment of comorbid conditions, patients with HFPEF should be advised that lifestyle modifications such as weight loss, smoking cessation, and dietary changes can do much to reduce the risk. You can help by providing an exercise “prescription” (with a specified intensity, frequency, and duration) and dietary guidelines, with emphasis on the importance of a low-sodium diet to prevent fluid overload.14,30 Recommend local programs for patients with HF, which many hospitals and health systems offer as part of their efforts to reduce readmission rates.
Consider cardioversion
Tachycardia shortens the time for filling during diastole; thus, it is poorly tolerated in patients with diastolic dysfunction and could trigger acute decompensation. To avoid the risk, restoration of sinus rhythm should be considered for patients with HFPEF and atrial fibrillation. Patients with known paroxysmal or permanent atrial fibrillation and preserved EF should be seen by a cardiologist to determine whether direct current cardioversion or ablation with a permanent pacemaker is appropriate.11 When cardioversion is contraindicated, a beta-blocker is needed to control heart rate and improve hemodynamics.
Patients with stable angina and HFPEF should be evaluated for revascularization when medical therapy alone is not sufficient for symptom relief.10 Here, too, a cardiology consult is indicated for any patient who has HF and an abnormal noninvasive stress test or persistent symptoms despite optimal drug therapy.
Recognizing and responding to acute decompensated HFPEF
The initial response to acute decompensated HFPEF, like that of HF with reduced EF, should be focused on restoring volume status and providing oxygenation, ventilation, and vasodilator therapy in some cases.11 Unlike those with acute decompensated HF with reduced EF, however, patients with HFPEF can safely tolerate the initiation of beta-blockers in the acute phase, especially when rate control is needed.3 Inotropic agents like digoxin and dobutamine, however, are contraindicated.3
Guidelines recommend hospitalization for patients with abnormal vital signs, arrhythmia, and suspected acute coronary syndromes, and consideration of hospitalization for those with associated comorbid conditions, new HF, or progressive fluid overload.13
CASE Because Ms. W has a normal BP and heart rate and is feeling well, you decline to alter her medication regimen. You do, however, recommend that she begin an exercise program, adopt a low-sodium diet, and maintain regular contact with your office so you can evaluate any changes in status.
You introduce Ms. W to the nurse case manager in your office. The nurse works with the patient to develop an action plan that includes daily tracking of her weight and sodium intake; a progressive walking program, starting with 2-minute sessions and progressing to 15 to 30 minutes 3 to 5 times a week; weekly telephone checkins; and immediate calls to report any weight increase or symptoms of HF.
At follow-up 6 months later, Ms. W has improved BP and reports that she enjoys her new exercise routine. She has more energy and denies any edema or breathing difficulties.
• Suspect diastolic heart failure in patients who have symptoms of heart failure but a normal ejection fraction, with or without evidence of diastolic abnormalities. B
• Treatment goals for patients who have heart failure with preserved ejection fraction (HFPEF) include normalization of blood pressure, prevention of tachycardia and ischemia, reduction of congestion, and improvement in exercise capacity. B
• Initiate beta-blocker therapy without delay for patients who have acute decompensated HFPEF and tachycardia; consider cardioversion for those with atrial fibrillation. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Most studies of heart failure (HF)—the most common cause of hospitalization in patients older than 65 years1—have focused on patients with reduced ejection fraction (EF). Yet half of those hospitalized for acute decompensated HF have a normal left ventricular EF.2 For these patients, contractility is not the problem—impaired relaxation during diastole is.
Commonly called diastolic HF, heart failure with preserved ejection fraction (HFPEF) is a more precise name for this condition. Patients are usually older than those with a reduced EF.3 Thus, as the US population ages, the prevalence of HFPEF increases, as well.4
Diagnostic criteria have been developed for HFPEF, but there are few large, high-quality studies to guide its treatment. Yet family physicians need to be familiar with HFPEF and know how best to treat it. With extrapolation from studies of patients with reduced EF, as well as expert consensus and our own experience, we offer an evidence-based approach to the management of both stable and acute decompensated HFPEF.
A closer look at diastolic dysfunction
Defined as an abnormality of diastolic compliance, filling, or relaxation of the ventricle, diastolic dysfunction can occur whether EF is normal or abnormal.3 Ventricular diastole includes isovolumic relaxation, early passive filling after mitral valve opening, and active filling during atrial contraction. Transmission of high ventricular pressure to the pulmonary circulation leads to pulmonary edema, dyspnea, and other symptoms of HF. Factors other than abnormal diastolic physiology, such as chronic volume overload, ventricular coupling dyssynchrony, increased autonomic tone leading to reduced venous capacitance, and chronotropic intolerance, may also be involved.5
Patient history: What to look for
A variety of conditions, including ischemia, tachycardia, impaired myocardial relaxation, and age-related loss of myocardial compliance, can contribute to abnormal diastolic function, but the major causes of HFPEF are chronic hypertension, hypertrophic cardiomyopathy, and coronary artery disease (CAD).3 Rarely, infiltrative or restrictive cardiomyopathy (eg, amyloidosis or sarcoidosis) is implicated.6 Noncardiovascular comorbidities such as diabetes, renal impairment, anemia, and chronic lung disease are more prevalent among those with HFPEF, and more women are affected than men.1
Mortality risk. In a study of more than 100,000 hospitalizations for acute decompensated HF, patients with preserved EF had lower in-hospital mortality (3% vs 4% for those with reduced EF).2 Patients with both diabetes and CAD commonly develop HFPEF,7 and the presence of these comorbidities are an independent predictor of 5-year mortality.8
Population studies suggest that 5-year mortality rates for African Americans with HFPEF are higher than for Caucasians with this condition.9 Other predictors of mortality include older age, male sex, lower left ventricular EF, ischemic disease, impaired renal function, and peripheral arterial disease.10-12
Diagnosing HFPEF: What you’ll see, when to test
The presentation of patients with HFPEF is similar to that of individuals with reduced EF. In an outpatient setting, both groups will have reduced exercise capacity; increased neuroendocrine activation, which may cause chronic fluid retention, vasoconstriction, and tachycardia; and a reduced quality of life.5
Neither the American College of Cardiology/American Heart Association (ACC/AHA) nor the Heart Failure Society of America (HFSA)13,14 recommends screening for asymptomatic left ventricular dysfunction. For those with signs and symptoms of HF, however, echocardiography is a key component of the initial evaluation. Echocardiography provides information about left ventricular systolic function, including EF, regional wall motion abnormalities, and wall thickness. Echocardiographic evidence of diastolic abnormalities is found for some patients with HFPEF, while others have no demonstrable diastolic dysfunction.3
While an electrocardiogram (EKG) cannot distinguish between HF with reduced EF and HFPEF, common findings might include signs of ventricular hypertrophy or tachycardia during acute exacerbations. An EKG should be obtained in patients with suspected HF to screen for antecedent causes such as hypertrophy, atrial fibrillation, and ischemia.15
What Doppler echocardiography and the E/A ratio reveal
Doppler echocardiography is used to further evaluate the characteristics of blood flow, showing the relationship among left ventricular (LV) relaxation, atrial pressure, atrial contraction, and blood flow velocity across the mitral valve during diastole. The peak velocity of blood flow during early diastole (called the “E wave”) and late diastole (the atrial contraction, or “A wave”) is measured and the E/A ratio (reflecting the transmitral blood flow pattern) is calculated (FIGURE).3
FIGURE
The E/A ratio* and what it reveals
A, atrial contraction; E, early passive filling; MVC, mitral valve closes; MVO, mitral valve opens.
*E/A ratio represents the relationship between the peak velocity of blood flow during early diastole (E wave) and late diastole (A wave).
Adapted from: Aurigemma GP, Gaasch WH. N Engl J Med. 2004.3
Normally, transmitral flow velocity is greater during early diastole than during atrial contraction, and the E/A ratio is approximately 1.5 (E>A). With early diastolic dysfunction, impaired relaxation prevents blood from flowing passively into the LV during early diastole. This causes reversal of the E/A ratio, which drops to <1 (E<A). As diastolic function worsens, atrial contraction is impaired, and left atrial pressure rises. The result: A reduction in the A wave amplitude and proportionally more blood flow during early diastole and a “pseudonormal” (E>A) ratio, with a greater difference between the E and A than is normally observed. This finding is an independent predictor of all-cause mortality in patients with asymptomatic HF.16
Cardiac catheterization. Invasive measurement of LV filling pressures is the gold standard for diagnosing HFPEF. If echocardiography does not lead to a clear diagnosis, cardiac catheterization can provide information about concomitant pulmonary hypertension and mechanical asynchrony that may contribute to symptomatic HF.1 When the diagnosis is uncertain, additional testing—eg, plasma brain natriuretic peptide (BNP), chest x-ray, or exercise testing—may be necessary to establish a diagnosis of symptomatic HF.
The diagnostic criteria developed by HFSA include clinical evidence of HF and:
- echocardiographic evidence of LV hypertrophy or left atrial enlargement (without atrial fibrillation) or
- evidence of diastolic dysfunction on Doppler echocardiography or cardiac catheterization.14
It is important to note that the diagnostic criteria have not been validated, and the sensitivity and specificity of the various clinical findings are not known.
CASE Carrie W, a 76-year-old woman referred to you by a colleague, presents for follow-up after being hospitalized for HF. She recalls feeling fatigue, chest pain, and out of breath with even minimal exertion before being admitted to the hospital.
You obtain her hospital records, which show that echocardiography found impaired LV relaxation based on a reversed E/A ratio and an EF of 65%. In addition, BNP was elevated, and a chest x-ray showed pulmonary vascular congestion. You note that her blood pressure was 175/103 mm Hg on admission and an EKG showed LV hypertrophy and sinus tachycardia, but no ischemia.
Before being hospitalized, Ms. W was taking extended-release metoprolol, aspirin, and lisinopril. The hospitalist added lovastatin and increased the daily dose of extended-release metoprolol from 25 to 100 mg.
What changes, if any, would you make in her medication regimen?
Diastolic dysfunction as chronic disease
Often asymptomatic, diastolic dysfunction should be thought of as a chronic progressive disease characterized by complex physiologic adaptations that vary over time (See “Staging heart failure: The clinical course of HFPEF”.13) Patients with HFPEF have a difficult time tolerating hemodynamic stress and any perturbation of afterload, heart rate, or ventricular function can precipitate an acute exacerbation.2 Clinical factors that precipitate acute decompensation of HFPEF—which we’ll discuss a bit later—include uncontrolled hypertension; atrial fibrillation; and noncardiovascular comorbidities such as lung disease, renal impairment, or sepsis.2
The ACC/AHA staging system for HF can be applied to patients with HFPEF, both to classify disease severity and to track the progression of the disease. Patients at Stage A are at high risk of developing HF, but early and aggressive treatment of hypertension and other cardiovascular risk factors may delay or potentially prevent the onset of overt disease. Stage B refers to patients with known structural disease, such as a history of myocardial infarction or systolic or diastolic dysfunction, but no symptoms of HF.
Patients at Stage C have evidence of structural disease and symptoms of HF, such as fatigue, shortness of breath, or reduced exercise tolerance. This stage represents the spectrum of patients falling into New York Heart Association (NYHA) Class 1 through 3 categories. Finally, patients at Stage D—analogous to NYHA Class 4—have refractory HF, with marked symptoms even at rest despite maximal medical therapy.
The Acute Decompensated HEart failure national REgistry (ADHERE), in which the records of well over 80,000 Medicare patients were reviewed, found that more than 60% of those hospitalized with HFPEF had uncontrolled hypertension, with a systolic pressure >140 mm Hg; 21% had atrial fibrillation.2 These findings emphasize the importance of aggressive blood pressure (BP) and heart rate control.
Management of HFPEF is goal directed
The aim of pharmacologic treatment of HFPEF is to maintain fluid balance, prevent tachycardia, treat and prevent ischemia, and control hypertension (TABLE).14,17-30 While the use of angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and beta-blockers, among other pharmacologic agents, is well studied for patients with reduced EF, there is limited evidence to guide the treatment of those with HFPEF. Although no single agent or drug class has been shown to be superior for such patients, there are a number of pharmacologic treatments to consider.
TABLE
Management of heart failure with preserved ejection fraction—matching treatment and goals14,17-30
| Treatment goal | Modality |
|---|---|
| Reduce congestion | Diuretics Salt restriction |
| Maintain atrial contraction | A-V pacing Cardioversion |
| Prevent tachycardia | A-V pacing Beta-blockers Calcium channel blockers |
| Prevent/treat ischemia | Antiplatelet therapy Beta-blockers Calcium channel blockers Revascularization Statins |
| Control hypertension | Antihypertensive agents:
|
| Promote regression of LV remodeling | ACE inhibitors ARBs |
| Improve exercise capacity | Supervised exercise program |
| ACE, angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; LV, left ventricle. | |
Inhibition of the renin-angiotensin-aldosterone system
Pathologic activation of the renin-angiotensin-aldosterone system (RAAS) contributes to elevated systolic and diastolic pressure, LV hypertrophy, and LV fibrosis. Inhibition of this system is a promising treatment modality for HFPEF.31
ACE inhibitors. Experimental studies suggest that ACE inhibitors benefit the diastolic properties of the heart, in both short- and long-term use. The PEP-CHF trial found that for older patients with diastolic dysfunction, perindopril led to significant improvements in functional class and exercise capacity but failed to show a statistically significant reduction in all-cause mortality or hospitalization for acute decompensated HF.17
ARBs. There is no evidence to show that ARB therapy improves morbidity or mortality in HFPEF. Using surrogate end points, ARBs have been associated with regression of LV hypertrophy, and losartan was found to improve exercise tolerance and quality of life, compared with hydrochlorothiazide.18,19 In the CHARM-Preserved trial, candesartan showed an insignificant reduction in cardiovascular mortality and hospitalization for HF.
These results must be viewed with caution, however, because adverse effects led to high rates of medication discontinuation.32 In the I-PRESERVE trial, irbesartan conferred no benefit with respect to mortality, hospitalization, or quality of life on patients with HFPEF.33
ACE inhibitor or ARB—not both. ACE inhibitors and ARBs are good choices for BP control in patients with HFPEF, especially if LV hypertrophy is present, but periodic testing of renal function and potassium levels is needed. ACE inhibitors and ARBs should not be used concurrently, as the combination increases the risk of acute renal failure and has no benefit in clinical outcomes.34
BP and rate control
In small trials, beta-blockers have been found to improve diastolic function as seen on echocardiography, but data on morbidity and mortality are lacking.20 A secondary analysis of the OPTIMIZE-HF registry found that beta-blocker therapy was associated with reduced mortality and readmission in patients with reduced EF, but not in those with normal EF.21
Findings from the SENIORS trial were more promising: Treatment with nebivolol reduced both mortality and readmission rates for elderly patients with HF, with similar benefits for those with reduced and preserved EF.22 Overall, beta-blockers appear to be a reasonable choice for heart rate and/or BP control in patients who have HFPEF and atrial fibrillation or hypertension. Carvedilol, long-acting metoprolol, and bisoprolol have been shown to reduce mortality in HF with reduced EF, and it is reasonable to choose one of these agents for patients with preserved EF, as well.23
Calcium channel blockers (CCBs) may be useful in treating patients with HFPEF for both BP and heart rate control, as well. Theoretically, CCBs may also improve the process of relaxation by altering intracellular calcium cycling during the contractile cycle in myocytes. This contrasts with the management of HF patients with reduced EF, for whom the use of nonselective CCBs such as diltiazem and verapamil may adversely affect contractility.
In small RCTs, verapamil has been found to improve HF symptoms and exercise tolerance in patients with HFPEF,24 but no evidence of improved outcomes or mortality rates with CCB use has been found.
Other pharmacologic options to consider
Aldosterone antagonist therapy is an important component of treatment for patients with HF with reduced EF. Data supporting the use of spironolactone use from the RALES trial and eplerenone in the EPHESUS and EMPHASIS-HF trials suggest a reduction in mortality in patients with low (<35%) LVEF.25-27 For patients with preserved EF, however, spironolactone is not generally recommended.
A large National Institutes of Health-sponsored trial is underway to determine if the drug is beneficial for patients with preserved LVEF, and will build on a small study in which 30 patients with HFPEF showed improved myocardial function after treatment with spironolactone.35 Until more data become available, the risks of using aldosterone antagonists outweigh the evidence to support their use in this patient population.
Diuretics are an important component of treatment for all patients with HF and fluid overload. The Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial (ALLHAT) showed a reduced incidence of symptomatic HFPEF in patients taking diuretics.28 As is the case with patients with reduced EF, those with preserved EF should be treated with diuretics if they have symptoms of fluid overload.
Statins. Intensive lipid lowering with statin therapy has been shown in observational studies to benefit patients with HFPEF with respect to mortality, independent of baseline low-density lipoprotein cholesterol.29 RCTs are needed to confirm these observations, but statin therapy is recommended for the secondary prevention of cardiovascular disease, independent of the presence of diastolic dysfunction or HFPEF.
Guard against hypotension. Patients with diastolic dysfunction are susceptible to hypotension if there is a rapid reduction in preload with diuretics, nonselective CCBs, or nitrates, so it is important that doses be titrated slowly.
Nonpharmacologic measures are important, too
In addition to optimizing treatment of comorbid conditions, patients with HFPEF should be advised that lifestyle modifications such as weight loss, smoking cessation, and dietary changes can do much to reduce the risk. You can help by providing an exercise “prescription” (with a specified intensity, frequency, and duration) and dietary guidelines, with emphasis on the importance of a low-sodium diet to prevent fluid overload.14,30 Recommend local programs for patients with HF, which many hospitals and health systems offer as part of their efforts to reduce readmission rates.
Consider cardioversion
Tachycardia shortens the time for filling during diastole; thus, it is poorly tolerated in patients with diastolic dysfunction and could trigger acute decompensation. To avoid the risk, restoration of sinus rhythm should be considered for patients with HFPEF and atrial fibrillation. Patients with known paroxysmal or permanent atrial fibrillation and preserved EF should be seen by a cardiologist to determine whether direct current cardioversion or ablation with a permanent pacemaker is appropriate.11 When cardioversion is contraindicated, a beta-blocker is needed to control heart rate and improve hemodynamics.
Patients with stable angina and HFPEF should be evaluated for revascularization when medical therapy alone is not sufficient for symptom relief.10 Here, too, a cardiology consult is indicated for any patient who has HF and an abnormal noninvasive stress test or persistent symptoms despite optimal drug therapy.
Recognizing and responding to acute decompensated HFPEF
The initial response to acute decompensated HFPEF, like that of HF with reduced EF, should be focused on restoring volume status and providing oxygenation, ventilation, and vasodilator therapy in some cases.11 Unlike those with acute decompensated HF with reduced EF, however, patients with HFPEF can safely tolerate the initiation of beta-blockers in the acute phase, especially when rate control is needed.3 Inotropic agents like digoxin and dobutamine, however, are contraindicated.3
Guidelines recommend hospitalization for patients with abnormal vital signs, arrhythmia, and suspected acute coronary syndromes, and consideration of hospitalization for those with associated comorbid conditions, new HF, or progressive fluid overload.13
CASE Because Ms. W has a normal BP and heart rate and is feeling well, you decline to alter her medication regimen. You do, however, recommend that she begin an exercise program, adopt a low-sodium diet, and maintain regular contact with your office so you can evaluate any changes in status.
You introduce Ms. W to the nurse case manager in your office. The nurse works with the patient to develop an action plan that includes daily tracking of her weight and sodium intake; a progressive walking program, starting with 2-minute sessions and progressing to 15 to 30 minutes 3 to 5 times a week; weekly telephone checkins; and immediate calls to report any weight increase or symptoms of HF.
At follow-up 6 months later, Ms. W has improved BP and reports that she enjoys her new exercise routine. She has more energy and denies any edema or breathing difficulties.
1. Lam CSP, Donal E, Kraigher-Krainer E, et al. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13:18-28.
2. Yancy CW, Lopatin M, Stevenson LW, et al. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the acute decompensated heart failure national registry (ADHERE) database. J Am Coll Cardiol. 2006;47:76-84.
3. Aurigemma GP, Gaasch WH. Diastolic heart failure. N Engl J Med. 2004;351:1097-1105.
4. Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251-259.
5. Bench T, Burkhoff D, O’Connell JB, et al. Heart failure with normal ejection fraction: consideration of mechanisms other than diastolic dysfunction. Curr Heart Fail Rep. 2009;6:57-64.
6. Ammash NM, Seward JB, Bailey KR, et al. Clinical profile and outcome of idiopathic restrictive cardiomyopathy. Circulation. 2000;101:2490-2496.
7. Bell DSH. Diabetic cardiomyopathy. Diabetes Care. 2003;26:2949-2951.
8. From AM, Scott CG, Chen HH. The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction: a population-based study. J Am Coll Cardiol. 2010;55:300-305.
9. East MA, Peterson ED, Shaw LK, et al. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J. 2004;148:151-156.
10. Ahmed A, Aronow WS, Fleg JL. Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J. 2006;151:444-450.
11. Hillege HL, Nitsch D, Pfeffer MA, et al. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation. 2006;113:671-678.
12. Somaratne JB, Berry C, McMurray JJ, et al. The prognostic significance of heart failure with preserved left ventricular ejection fraction: a literature-based meta-analysis. Eur J Heart Fail. 2009;11:855-862.
13. 2005 Writing committee members; Hunt SA, Abraham WT, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults. Circulation. 2009;119:e391-e479.
14. Heart Failure Society of America. HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16:e1-e2.
15. Davie AP, Francis CM, Love MP, et al. Value of the electrocardiogram in identifying heart failure due to left ventricular systolic dysfunction. BMJ. 1996;312:222.-
16. Halley CM, Houghtaling PL, Khalil MK, et al. Mortality rate in patients with diastolic dysfunction and normal systolic function. Arch Intern Med. 2011;171:1082-1087.
17. Cleland JGF, Tendera M, Adamus J, et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338-2345.
18. Wachtell K, Bella JN, Rokkedal J, et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment. Circulation. 2002;105:1071-1076.
19. Little WC, Zile MR, Klein A, et al. Effect of losartan and hydrochlorothiazide on exercise tolerance in exertional hypertension and left ventricular diastolic dysfunction. Am J Cardiol. 2006;98:383-385.
20. Bonow RO, Udelson JE. Left ventricular diastolic dysfunction as a cause of congestive heart failure. Mechanisms and management Ann Intern Med. 1992;117:502-510.
21. Hernandez AF, Hammill BG, O’Connor CM, et al. Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (organized program to initiate lifesaving treatment in hospitalized patients with heart failure) registry. J Am Coll Cardiol. 2009;53:184-192.
22. Flather MD, Shibata MC, Coats AJS, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26:215-225.
23. Chavey WE, Bleske BE, Van Harrison R, et al. Pharmacologic management of heart failure caused by systolic dysfunction. Am Fam Physician. 2008;77:957-964.
24. Setaro JF, Zaret BL, Schulman DS, et al. Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol. 1990;66:981-986.
25. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999;341:709-717.
26. Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309-1321.
27. Zannad F, McMurray JJV, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11-21.
28. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA. 2002;288:2981-2997.
29. Fukuta H, Sane DC, Brucks S, et al. Statin therapy may be associated with lower mortality in patients with diastolic heart failure. Circulation. 2005;112:357-363.
30. Arcand JAL, Brazel S, Joliffe C, et al. Education by a dietitian in patients with heart failure results in improved adherence with a sodium-restricted diet: a randomized trial. Am Heart J. 2005;150:716.e1-716.e5.
31. Bernal J, Pitta SR, Thatai D. Role of the renin-angiotensin-aldosterone system in diastolic heart failure: potential for pharmacologic intervention. Am J Cardiovasc Drugs. 2006;6:373-381.
32. Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet. 2003;362:777-781.
33. Massie BM, Carson PE, McMurray JJ, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456-2467.
34. Heran BS, Musini VM, Bassett K, et al. Angiotensin receptor blockers for heart failure. Cochrane Database Syst Rev. 2012;(4):CD003040.-
35. Mottram PM, Haluska B, Leano R, et al. Effect of aldosterone antagonism on myocardial dysfunction in hypertensive patients with diastolic heart failure. Circulation. 2004;0110:558-565.
CORRESPONDENCE Geoffrey D. Mills, MD, PhD, Department of Family and Community Medicine, Jefferson Medical College, 833 Chestnut Street, Suite 301, Philadelphia, PA 19107; [email protected]
1. Lam CSP, Donal E, Kraigher-Krainer E, et al. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13:18-28.
2. Yancy CW, Lopatin M, Stevenson LW, et al. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the acute decompensated heart failure national registry (ADHERE) database. J Am Coll Cardiol. 2006;47:76-84.
3. Aurigemma GP, Gaasch WH. Diastolic heart failure. N Engl J Med. 2004;351:1097-1105.
4. Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251-259.
5. Bench T, Burkhoff D, O’Connell JB, et al. Heart failure with normal ejection fraction: consideration of mechanisms other than diastolic dysfunction. Curr Heart Fail Rep. 2009;6:57-64.
6. Ammash NM, Seward JB, Bailey KR, et al. Clinical profile and outcome of idiopathic restrictive cardiomyopathy. Circulation. 2000;101:2490-2496.
7. Bell DSH. Diabetic cardiomyopathy. Diabetes Care. 2003;26:2949-2951.
8. From AM, Scott CG, Chen HH. The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction: a population-based study. J Am Coll Cardiol. 2010;55:300-305.
9. East MA, Peterson ED, Shaw LK, et al. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J. 2004;148:151-156.
10. Ahmed A, Aronow WS, Fleg JL. Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J. 2006;151:444-450.
11. Hillege HL, Nitsch D, Pfeffer MA, et al. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation. 2006;113:671-678.
12. Somaratne JB, Berry C, McMurray JJ, et al. The prognostic significance of heart failure with preserved left ventricular ejection fraction: a literature-based meta-analysis. Eur J Heart Fail. 2009;11:855-862.
13. 2005 Writing committee members; Hunt SA, Abraham WT, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults. Circulation. 2009;119:e391-e479.
14. Heart Failure Society of America. HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16:e1-e2.
15. Davie AP, Francis CM, Love MP, et al. Value of the electrocardiogram in identifying heart failure due to left ventricular systolic dysfunction. BMJ. 1996;312:222.-
16. Halley CM, Houghtaling PL, Khalil MK, et al. Mortality rate in patients with diastolic dysfunction and normal systolic function. Arch Intern Med. 2011;171:1082-1087.
17. Cleland JGF, Tendera M, Adamus J, et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338-2345.
18. Wachtell K, Bella JN, Rokkedal J, et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment. Circulation. 2002;105:1071-1076.
19. Little WC, Zile MR, Klein A, et al. Effect of losartan and hydrochlorothiazide on exercise tolerance in exertional hypertension and left ventricular diastolic dysfunction. Am J Cardiol. 2006;98:383-385.
20. Bonow RO, Udelson JE. Left ventricular diastolic dysfunction as a cause of congestive heart failure. Mechanisms and management Ann Intern Med. 1992;117:502-510.
21. Hernandez AF, Hammill BG, O’Connor CM, et al. Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (organized program to initiate lifesaving treatment in hospitalized patients with heart failure) registry. J Am Coll Cardiol. 2009;53:184-192.
22. Flather MD, Shibata MC, Coats AJS, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26:215-225.
23. Chavey WE, Bleske BE, Van Harrison R, et al. Pharmacologic management of heart failure caused by systolic dysfunction. Am Fam Physician. 2008;77:957-964.
24. Setaro JF, Zaret BL, Schulman DS, et al. Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol. 1990;66:981-986.
25. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999;341:709-717.
26. Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309-1321.
27. Zannad F, McMurray JJV, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11-21.
28. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA. 2002;288:2981-2997.
29. Fukuta H, Sane DC, Brucks S, et al. Statin therapy may be associated with lower mortality in patients with diastolic heart failure. Circulation. 2005;112:357-363.
30. Arcand JAL, Brazel S, Joliffe C, et al. Education by a dietitian in patients with heart failure results in improved adherence with a sodium-restricted diet: a randomized trial. Am Heart J. 2005;150:716.e1-716.e5.
31. Bernal J, Pitta SR, Thatai D. Role of the renin-angiotensin-aldosterone system in diastolic heart failure: potential for pharmacologic intervention. Am J Cardiovasc Drugs. 2006;6:373-381.
32. Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet. 2003;362:777-781.
33. Massie BM, Carson PE, McMurray JJ, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456-2467.
34. Heran BS, Musini VM, Bassett K, et al. Angiotensin receptor blockers for heart failure. Cochrane Database Syst Rev. 2012;(4):CD003040.-
35. Mottram PM, Haluska B, Leano R, et al. Effect of aldosterone antagonism on myocardial dysfunction in hypertensive patients with diastolic heart failure. Circulation. 2004;0110:558-565.
CORRESPONDENCE Geoffrey D. Mills, MD, PhD, Department of Family and Community Medicine, Jefferson Medical College, 833 Chestnut Street, Suite 301, Philadelphia, PA 19107; [email protected]