User login
A Danish cohort study provides more evidence of a significant link between HIV infection and two types of skin cancer.
, with incidence rate ratios (IRRs) of 1.79 and 5.40, respectively, when compared with a background population, who were HIV-negative.
“The risk of SCC seemed to increase with increasing level of immunosuppression while the increased risk of BCC was restricted to patients reporting MSM [men who have sex with men] as route of infection,” wrote the authors, led by Silje Haukali Omland, MD, PhD, of the department of dermato-venereology, Copenhagen University Hospital.
The Danish nationwide cohort study, which matched each HIV patient with 5 age- and sex-matched individuals from the background population, was published online March 26 in the Journal of the American Academy of Dermatology.
The results are similar to those published elsewhere, as is the finding that HIV-positive patients do not face a higher risk of malignant melanoma. “The results here confirm prior studies and support heightened vigilance for skin conditions, such as SCC and BCC in HIV patients,” said Michael J. Silverberg, PhD, of Kaiser Permanente Division of Research, in an interview after reviewing the study findings. He was not a study author.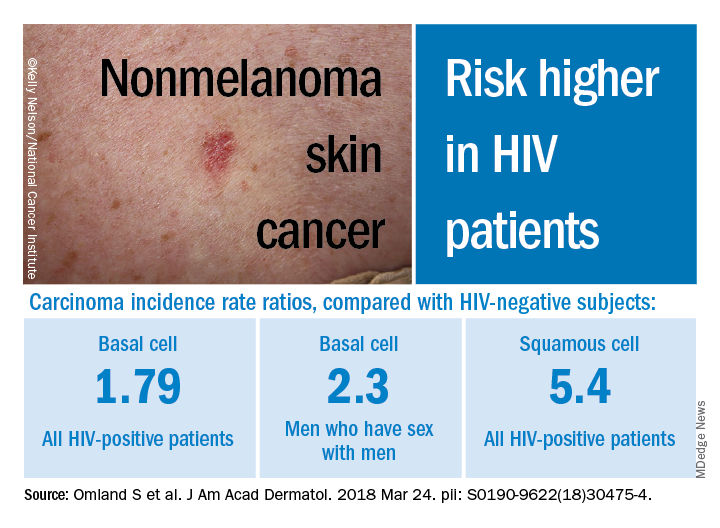
Researchers have long noted a connection between various types of cancer and HIV infection. But, as noted in a 2013 study led by Dr. Silverberg, research into links between HIV and non-melanoma skin cancers has been sparse and inconclusive. That study of white adults found higher adjusted rate ratios for SCC (2.6) and BCC (2.1) among those who were HIV-positive compared with those who were HIV-negative (J Natl Cancer Inst. 2013 Mar 6;105[5]:350-60).
In the Danish study, researchers tracked sex-and age-matched cohorts of HIV-infected (4,280) and non-HIV-infected patients (21,399) aged 16 years or older from study inclusion through as late as 2014. All the HIV-positive subjects had taken antiretroviral medications. The researchers also compared the HIV-positive patients to their non-HIV-infected siblings.
Overall, those who were HIV-positive were more likely to develop BCC (IRR, 1.79, 95% CI, 1.43-2.22), and males who reported sex with men had an even higher risk (IRR, 2.30, 95% CI, 1.76-3.02).
As for SCC, the IRR was 5.40 (95% CI, 3.07-9.52) among those who were HIV-positive, compared with the background population, and the researchers found evidence that risk increased with level of immunosuppression. Those who indicated heterosexual and male homosexual transmission had similar rates of SCC.
The rates of BCC or SCC were not higher among siblings of HIV-positive patients.
In addition, the risk of melanoma was not increased among those who were HIV-positive subjects or their siblings, when compared with the background group. However, the researchers noted that the study turned up a low number of HIV-positive subjects with melanoma, potentially throwing off the results.
The researchers noted that the inclusion of siblings in the study suggests that sun exposure in childhood was not a confounding factor. Presumably, they wrote, the siblings had similar levels of exposure as children, although exposure to sun bed tanning could differ between siblings.
“Study methods appear very strong and consistent with other work done in the area,” Dr. Silverberg said in the interview. As for possible causes of the disparities, he noted that exposure to the sun or to tanning beds could explain the greater risk of BCC among men who have sex with men. “For SCC, there may be a biological link, as studies have suggested a link with human papillomavirus for that particular cancer,” he added.
No study funding was reported. The study authors reported disclosures that included grants, research grants, speaker fees, and/or advisory board honoraria from several drug manufacturers. Dr. Silverberg has no relevant disclosures.
A Danish cohort study provides more evidence of a significant link between HIV infection and two types of skin cancer.
, with incidence rate ratios (IRRs) of 1.79 and 5.40, respectively, when compared with a background population, who were HIV-negative.
“The risk of SCC seemed to increase with increasing level of immunosuppression while the increased risk of BCC was restricted to patients reporting MSM [men who have sex with men] as route of infection,” wrote the authors, led by Silje Haukali Omland, MD, PhD, of the department of dermato-venereology, Copenhagen University Hospital.
The Danish nationwide cohort study, which matched each HIV patient with 5 age- and sex-matched individuals from the background population, was published online March 26 in the Journal of the American Academy of Dermatology.
The results are similar to those published elsewhere, as is the finding that HIV-positive patients do not face a higher risk of malignant melanoma. “The results here confirm prior studies and support heightened vigilance for skin conditions, such as SCC and BCC in HIV patients,” said Michael J. Silverberg, PhD, of Kaiser Permanente Division of Research, in an interview after reviewing the study findings. He was not a study author.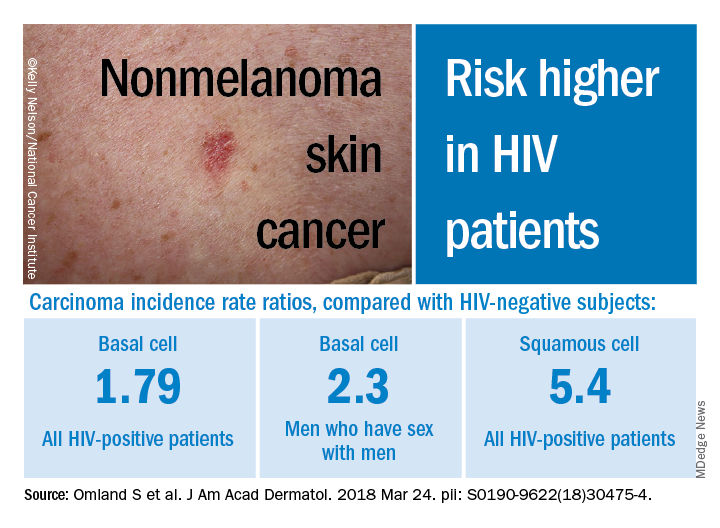
Researchers have long noted a connection between various types of cancer and HIV infection. But, as noted in a 2013 study led by Dr. Silverberg, research into links between HIV and non-melanoma skin cancers has been sparse and inconclusive. That study of white adults found higher adjusted rate ratios for SCC (2.6) and BCC (2.1) among those who were HIV-positive compared with those who were HIV-negative (J Natl Cancer Inst. 2013 Mar 6;105[5]:350-60).
In the Danish study, researchers tracked sex-and age-matched cohorts of HIV-infected (4,280) and non-HIV-infected patients (21,399) aged 16 years or older from study inclusion through as late as 2014. All the HIV-positive subjects had taken antiretroviral medications. The researchers also compared the HIV-positive patients to their non-HIV-infected siblings.
Overall, those who were HIV-positive were more likely to develop BCC (IRR, 1.79, 95% CI, 1.43-2.22), and males who reported sex with men had an even higher risk (IRR, 2.30, 95% CI, 1.76-3.02).
As for SCC, the IRR was 5.40 (95% CI, 3.07-9.52) among those who were HIV-positive, compared with the background population, and the researchers found evidence that risk increased with level of immunosuppression. Those who indicated heterosexual and male homosexual transmission had similar rates of SCC.
The rates of BCC or SCC were not higher among siblings of HIV-positive patients.
In addition, the risk of melanoma was not increased among those who were HIV-positive subjects or their siblings, when compared with the background group. However, the researchers noted that the study turned up a low number of HIV-positive subjects with melanoma, potentially throwing off the results.
The researchers noted that the inclusion of siblings in the study suggests that sun exposure in childhood was not a confounding factor. Presumably, they wrote, the siblings had similar levels of exposure as children, although exposure to sun bed tanning could differ between siblings.
“Study methods appear very strong and consistent with other work done in the area,” Dr. Silverberg said in the interview. As for possible causes of the disparities, he noted that exposure to the sun or to tanning beds could explain the greater risk of BCC among men who have sex with men. “For SCC, there may be a biological link, as studies have suggested a link with human papillomavirus for that particular cancer,” he added.
No study funding was reported. The study authors reported disclosures that included grants, research grants, speaker fees, and/or advisory board honoraria from several drug manufacturers. Dr. Silverberg has no relevant disclosures.
A Danish cohort study provides more evidence of a significant link between HIV infection and two types of skin cancer.
, with incidence rate ratios (IRRs) of 1.79 and 5.40, respectively, when compared with a background population, who were HIV-negative.
“The risk of SCC seemed to increase with increasing level of immunosuppression while the increased risk of BCC was restricted to patients reporting MSM [men who have sex with men] as route of infection,” wrote the authors, led by Silje Haukali Omland, MD, PhD, of the department of dermato-venereology, Copenhagen University Hospital.
The Danish nationwide cohort study, which matched each HIV patient with 5 age- and sex-matched individuals from the background population, was published online March 26 in the Journal of the American Academy of Dermatology.
The results are similar to those published elsewhere, as is the finding that HIV-positive patients do not face a higher risk of malignant melanoma. “The results here confirm prior studies and support heightened vigilance for skin conditions, such as SCC and BCC in HIV patients,” said Michael J. Silverberg, PhD, of Kaiser Permanente Division of Research, in an interview after reviewing the study findings. He was not a study author.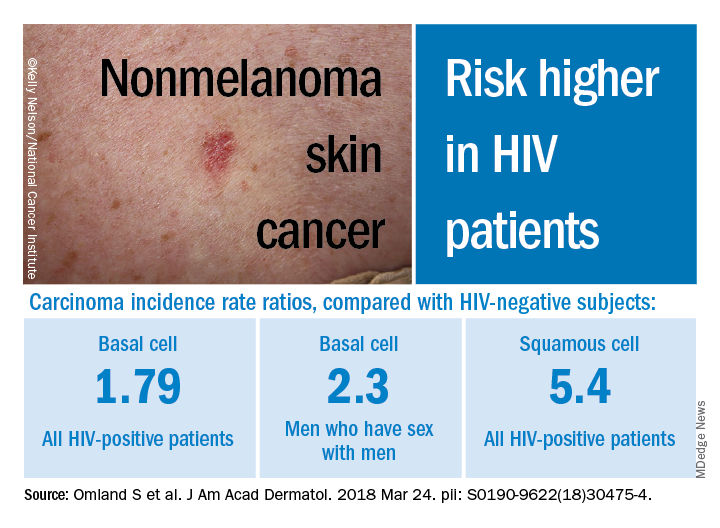
Researchers have long noted a connection between various types of cancer and HIV infection. But, as noted in a 2013 study led by Dr. Silverberg, research into links between HIV and non-melanoma skin cancers has been sparse and inconclusive. That study of white adults found higher adjusted rate ratios for SCC (2.6) and BCC (2.1) among those who were HIV-positive compared with those who were HIV-negative (J Natl Cancer Inst. 2013 Mar 6;105[5]:350-60).
In the Danish study, researchers tracked sex-and age-matched cohorts of HIV-infected (4,280) and non-HIV-infected patients (21,399) aged 16 years or older from study inclusion through as late as 2014. All the HIV-positive subjects had taken antiretroviral medications. The researchers also compared the HIV-positive patients to their non-HIV-infected siblings.
Overall, those who were HIV-positive were more likely to develop BCC (IRR, 1.79, 95% CI, 1.43-2.22), and males who reported sex with men had an even higher risk (IRR, 2.30, 95% CI, 1.76-3.02).
As for SCC, the IRR was 5.40 (95% CI, 3.07-9.52) among those who were HIV-positive, compared with the background population, and the researchers found evidence that risk increased with level of immunosuppression. Those who indicated heterosexual and male homosexual transmission had similar rates of SCC.
The rates of BCC or SCC were not higher among siblings of HIV-positive patients.
In addition, the risk of melanoma was not increased among those who were HIV-positive subjects or their siblings, when compared with the background group. However, the researchers noted that the study turned up a low number of HIV-positive subjects with melanoma, potentially throwing off the results.
The researchers noted that the inclusion of siblings in the study suggests that sun exposure in childhood was not a confounding factor. Presumably, they wrote, the siblings had similar levels of exposure as children, although exposure to sun bed tanning could differ between siblings.
“Study methods appear very strong and consistent with other work done in the area,” Dr. Silverberg said in the interview. As for possible causes of the disparities, he noted that exposure to the sun or to tanning beds could explain the greater risk of BCC among men who have sex with men. “For SCC, there may be a biological link, as studies have suggested a link with human papillomavirus for that particular cancer,” he added.
No study funding was reported. The study authors reported disclosures that included grants, research grants, speaker fees, and/or advisory board honoraria from several drug manufacturers. Dr. Silverberg has no relevant disclosures.
FROM JAAD
Key clinical point: HIV-positive patients are at an increased risk for basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
Major finding: Among HIV-infected patients, the risk of BCC was increased by almost twofold and the risk of BCC was increased by more than fivefold.
Study details: A Danish population-based cohort study of 4,280 HIV-infected patients and 21,399 age-and sex-matched subjects.
Disclosures: No study funding was reported. The authors reported disclosures that included research grants, speaker fees, and/or advisory board honoraria from several drug manufacturers.
Source: Omland S et al. J Am Acad Dermatol. 2018 Mar 24. pii: S0190-9622(18)30475-4. doi: 10.1016/j.jaad.2018.03.024.