User login
• While lithium produces significant remission rates in augmentation efforts for treatment-resistant depression, it is more likely to cause side effects than many other psychotropic agents. A
• Medication and cognitive therapy are equally effective when augmenting antidepressant therapy; cognitive therapy, however, takes longer to achieve remission. B
• Since the efficacy of many agents is similar when augmenting treatment, it’s important to factor the cost of the medication, side effects, and patient preference into the decision process. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The sobering truth about major depression is that too often it goes unrecognized or undertreated.1,2 And even when it is treated correctly, up to 34% of patients fail to respond to treatment.3 In the United States alone, the lifetime prevalence of the disease is 16.2%, and more than 6% of adults experience symptoms of major depression in any given year.2 Obviously, we need to do more for these patients.
Treatment-resistant depression has been defined as the failure to achieve remission after continuous therapy for about 6 to 12 weeks with an adequate dose of a single antidepressant.4 Remission is typically defined as a 50% reduction of scores on depression severity scales, with the 17-item Hamilton Rating Scale of Depression (HRSD17) and the 16-item Quick Inventory of Depressive Symptomatology–Self-Report (QIDS-SR16) being the most often used. An adequate dose is the lowest effective dose that doesn’t cause intolerable side effects.
What are our best options for treatment-resistant depression?
To answer this question, we reviewed all English language studies in PubMed or Medline that were performed among adults using the search terms “augmentation, antidepressants, major depression.” We excluded studies involving patients with comorbid anxiety, bipolar disorder, or other major mental illnesses.
Based on our review of the literature, we found support for several augmentative treatments for patients with treatment-resistant depression (TABLE). Of note, though: Most of these studies were randomized trials dating back nearly 2 decades and had limitations. Most were not blinded, nor did they have consistent placebo controls. The studies were typically small (albeit frequently still showing efficacy for the agent despite lower statistical power) and of relatively short duration (typically 6-14 weeks). There were few studies that looked at treatment approaches over longer periods or that considered indications and timelines for tapering of medications once remission had been achieved. A major exception to the rule was the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, which we’ll discuss below.5
The research points to several viable options: Clinicians can switch antidepressants, augment these agents by adding others—usually nonantidepressants—or completely change the therapeutic approach. Since most of the research discusses augmentation, we’ll focus on that here. Because the decision to use electroconvulsive therapy, vagus nerve stimulators, or other nonpharmaceutical approaches is made in consultation with a psychiatrist, we will not discuss these options.
TABLE
How these agents compare for treatment-resistant depression
| Agent/approach | Remission rate | Starting dose | Titrated to… | Frequency of side effects | SOR rating |
|---|---|---|---|---|---|
| Lithium5-9 | 53%-60% | 300 mg BID-TID | Doses of 800-1500 mg and lithium level of 0.5-1 mmol/L | >25% | A |
| Thyroid supplementation10-13 | 25%-59% | 20-50 mcg | Often not titrated | 11%-25% | A |
| Aripiprazole14-17 | 25%-37% | 2-5 mg | 15-20 mg | 16%-25% | A |
| Olanzapine/fluoxetine18 | 25% | Fixed dose | Fixed dose | 10%-40% | A |
| Risperidone19-21 | 25%-71% | 0.25-1 mg | 0.5-3 mg | 6%-10% | A |
| Quetiapine22,23 | 36%-49% | 25-200 mg | 100-600 mg | >25% | B |
| Mirtazapine24 | 45% | 15 mg | 30 mg | 6%-10% | B |
| Cognitive therapy34 | 23% | NA | NA | 0%-5% | B |
| Folic acid (Leucovorin)26 | 18% | 15 mg | 30 mg | 11%-25% | C |
| SAMe27 | 43% | 800 mg | 1600 mg | 50% | C |
| NA, not applicable; SAMe, S-adenosyl-L-methionine; SOR, strength of recommendation. | |||||
Lithium: Good results, but with side effects
Lithium is one of the oldest and most well studied agents.6-9 Most studies used 900 mg divided into 3 daily doses and titrated to lithium plasma levels of 0.5 to 1 mmol/L. Unfortunately, though, lithium is more likely to cause side effects than many other psychotropic agents (>25%).5-9 And while the research has found that lithium produces significant remission rates, it’s not very effective in patients who have failed multiple antidepressant trials, with only 12.5% to 15.9% of patients in that cohort achieving remission.10,11
Thyroid hormone has only mild side effects
Low-dose thyroid supplementation has been used for decades in euthyroid patients with treatment-resistant depression; remission rates range from 25% to 59%.10-13 Most studies used a low fixed-dose therapy between 25 and 50 mcg daily; side effects were mild and occurred at rates similar to placebo.13
Atypical antipsychotics: Many pluses, but weight gain is an issue
Atypical antipsychotics are an attractive alternative to typical antipsychotics for treatment-resistant depression. They are much less likely to cause extrapyramidal symptoms, tardive dyskinesia, and other motor symptoms, but as a trade-off they often cause weight gain, abnormal glucose metabolism, dyslipidemia, and hyperprolactinemia.
Aripiprazole (Abilify) is 1 of 2 medications approved by the Food and Drug Administration (FDA) for treatment-resistant depression. Studies have shown remission rates of 25% to 37%, with side effects in 16% to 25% of patients.14-16 Akathisia, the major side effect, can be reduced by lowering the starting dose to 2.5 mg.17
Olanzapine, combined with fluoxetine in a fixed-dose pill (Symbyax), is the other FDA-approved agent for treatment-resistant depression. Trivedi and colleagues showed a remission rate of 25.5% and side effects ranging from 10% to 40%.18
Risperidone (Risperdal) rivals the efficacy of the medications previously discussed, but starting doses and titration schedules vary widely, making it difficult to determine which treatment course would be most efficacious.19-21
Quetiapine (Seroquel) has produced mixed results in treatment-resistant patients. That may have been because some studies used lower daily doses—25 to 100 mg—vs 150 to 600 mg in other trials.22 Bauer found higher remission rates compared to placebo (36% vs 24%)23 while Garakani22 did not (49% for quetiapine vs. 63% for placebo when using an intention-to-treat analysis; a similar lack of efficacy was found if those who dropped out of the study were excluded; P<0.29). Garakani also found that dry mouth, sedation, and other side effects occurred in up to 76% of patients. (Of note: Most studies of atypical antipsychotics are industry funded.)
Mirtazapine has not been well studied
Unfortunately, there are very little data on mirtazapine (Remeron). When the drug was added to ongoing antidepressant therapy, a single double-blind, randomized controlled trial found significantly better response rates compared with placebo.24 One advantage of the drug was that it helped relieve the sexual side effects of ongoing selective serotonin reuptake inhibitor (SSRI) therapy.25
Folic acid and SAMe also haven’t been well studied
Up to 50% of Americans have low levels of central nervous system L-methylfolate, which is a key co-factor in monoamine neurotransmitter production. Although lower plasma folate has been linked to depression, folate supplementation as a primary treatment for major depression has not been well studied and its use in treatment-resistant depression is limited to 1 study by Alpert and colleagues.26 Using an open-label, nonplacebo-controlled design in which folinic acid—an activated form of folic acid—was compared with placebo, researchers found remission rates of 18%, which is not significantly higher than the placebo response seen in other studies.
Similarly, there’s limited research on S-adenosyl-L-methionine (SAMe). Using a similar open-label, nonplacebo-controlled design, Alpert found a 43% remission rate in patients with treatment-resistant depression. Side effects occurred in up to half of patients, prompting 6.6% of patients to leave the study.27
Omega-3 fatty acids: The news is mixed
Data are contradictory on the value of omega-3 fatty acid for major depression28,29 and the evidence to support its use in treatment-resistant depression is likewise limited and contradictory.30 Until the data are more consistent and robust, it’s unclear whether omega-3 fatty acid supplementation can benefit patients.
Exercise helps
Some studies suggest that exercise can have a dose-responsive effect on clinical depression.31 As a result, the Treatment with Exercise Augmentation for Depression (TREAD) trial is underway to examine whether it can augment drug therapy. Preliminary evidence suggests that 30 minutes of aerobic exercise most days of the week can be effective.32,33 (For more on exercise, see “Does exercise alleviate symptoms of depression?”)
Cognitive therapy helps patients, and there are no side effects
The STAR*D study showed equivalent efficacy in achieving remission (23% vs. 33%) when comparing augmentation with cognitive therapy and augmentation with medications, with a low rate of side effects seen for cognitive therapy.34 Notably, it took longer to achieve remission (55 vs 40 days) when cognitive therapy was added to antidepressants. (For more on the STAR*D trial, see “What we learned from the STAR*D trial”) It’s also worth mentioning that other researchers did not find similar results for augmentation when they compared cognitive behavioral and brief supportive psychotherapy with medication therapy only.35
The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study is noteworthy because of its size, duration, design, and impact on the treatment of depression.5 This was a multicenter study of 3671 patients with major unipolar depression. Remission was determined by 2 rating scales—HRSD17 and QIDS-SR16*—and side effects were measured at each visit. There was no placebo control, no consideration for atypical antipsychotic medications or other therapies, and randomization was limited.
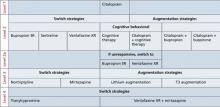
The FIGURE below shows how STAR*D was structured. In Level 1, patients were treated with citalopram (Celexa). If they didn’t go into remission, they were encouraged to proceed to Level 2, which involved 3 arms: switching agents, augmenting agents, or cognitive therapy. Patients chose which arm they wanted and were randomized to the specific medications used in that level. Switch agents included bupropion SR (Wellbutrin SR), sertraline (Zoloft), and venlafaxine XR (Effexor XR). Augmentation was with buspirone (BuSpar) and bupropion. Cognitive therapy was with or without continued citalopram with a second augmentation level of bupropion SR or venlafaxine XR. Level 3 also involved switch and augmentation arms using nortriptyline (Aventyl, Pamelor) or mirtazapine (Remeron) for switch agents and lithium or thyroxine for augmentation. Level 4 involved switching to tranylcypromine (Parnate) or venlafaxine XR plus mirtazapine.
Remission rates were 36.8% for those in Level 1, 30.6% in Level 2, 13.7% in Level 3, and 13% in Level 4. The cumulative remission rate was 67%. While remission rates for switch strategies in Levels 2 and 3 appeared to be lower for pharmacologic agents compared with augmentation strategies (27% vs 35% in Level 2 and 10.7% vs 20.5% in Level 3), the sample sizes were too small for the differences to be statistically significant, and the study was underpowered to establish the superiority of switch vs augmentation strategies.
Finally, it’s important to mention that patients of primary care physicians had similar remission rates, when compared with psychiatrists’ patients.42 Keep in mind, however, that the care provided in the STAR*D trial was structured and protocol-driven. After randomization into 1 medication group or another, dose adjustments were standardized at set intervals and based on inadequate response to validated depression severity assessment tools. Outcomes were patient-based and uniformly applied. This study structure may explain why remission rates were identical regardless of the specialty of the treating physician.
*The 17-item Hamilton Rating Scale of Depression and the 16-item Quick Inventory of Depressive Symptomatology–Self Report.
FIGURE
Structure of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D)
These agents don’t appear helpful in augmentation efforts
Several other agents have been studied with no effect on remission rates. These include pindolol,36 modafinil,37 buspirone, lamotrigine,38 stimulants, and estrogen replacement.
Consider side effects, cost, and patient preference
Because most studies showed that the efficacy of the tested drugs was similar, how do you decide which augmenting agent to prescribe? The usual standard is lithium, which offers rates of remission that are high, but not statistically significantly better when compared with thyroid supplementation and cognitive therapy. Quetiapine, while not more efficacious, may lower scores on depression rating scales more quickly than lithium.39 Additionally, the STAR*D trial suggests that many agents may be used in augmentation with similar results.
In the final analysis, the family physician has to consider factors other than efficacy. You also have to factor in the costs of medicines and lab testing, patient preference, and side effects. Lithium is most likely to cause side effects. Atypical antipsychotics seem to have lower short-term side effect profiles with efficacy similar to cognitive therapy. However, the potential drawbacks of antipsychotics, including aberrations in glucose metabolism, weight, and lipid profiles, are not typically seen in short-term studies. Obviously, more long-term studies are necessary before 1 agent can be deemed superior.
When should you stop therapy?
That question still doesn’t have a definitive answer. The STAR*D trial found that patients who achieved full remission were less likely to relapse/worsen than those who had only a partial response. The time to relapse ranged from 2.5 to 4.5 months and was shorter for those patients requiring 2 or more levels of treatment. As there was no control of the therapeutic interventions used during this time, we can’t be certain about what caused the relapse, but burden of disease, income levels, and ethnicity all played roles in symptom severity, decreasing remission rates, and increasing relapse rates.40,41
While we cannot identify the ideal or even preferred duration of augmentation in patients with treatment-resistant depression, it seems clear that relapse is extremely common and tends to occur relatively early after achieving remission.
CORRESPONDENCE Paul Hicks, MD, Department of Family and Community Medicine, 1450 North Cherry Avenue, Tucson, AZ 85719; [email protected]
1. Kocsis JH, Gelenberg AJ, Rothbaum B, et al. Chronic forms of major depression are still undertreated in the 21st century: systematic assessment of 801 patients presenting for treatment. J Affect Disord. 2008;110:55-61.
2. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095-3105.
3. Fava M, Davidson KG. Definition and epidemiology of treatment-resistant depression. Psychiatr Clin North Am. 1996;19:179-200.
4. Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53:649-659.
5. Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients who required one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905-1917.
6. Cappiello A, McDougle CJ, Delgado PL, et al. Lithium and desipramine versus desipramine alone in the treatment of severe major depression: a preliminary study. Int Clin Psychopharmacol. 1998;13:191-198.
7. Katona CL, Abou-Saleh MT, Harrison DA, et al. Placebo-controlled trial of lithium augmentation of fluoxetine and lofepramine. Br J Psychiatry. 1995;166:80-86.
8. Bauer M, Bschor T, Kunz D, et al. Double-blind, placebo-controlled trial of the use of lithium to augment antidepressant medication in continuation treatment of unipolar major depression. Am J Psychiatry. 2000;157:1429-1435.
9. Joffe RT, Singer W, Levitt AJ, et al. A placebo-controlled comparison of lithium and triiodothyronine augmentation of tricyclic antidepressants in unipolar refractory depression. Arch Gen Psychiatry. 1993;50:387-393.
10. Nierenberg AA, Fava M, Trivedi MH, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. Am J Psychiatry. 2006;163:1519-1530.
11. Nierenberg AA, Papakostas GI, Petersen T, et al. Lithium augmentation of nortriptyline for subjects resistant to multiple antidepressants. J Clin Psychopharmacol. 2003;23:92-95.
12. Aronson R, Offman HJ, Joffe RT, et al. Triiodothyronine augmentation in the treatment of refractory depression. A meta-analysis. Arch Gen Psychiatry. 1996;53:842-848.
13. Joffe RT, Sokolov ST, Levitt AJ. Lithium and triiodothyronine augmentation of antidepressants. Can J Psychiatry. 2006;51:791-793.
14. Berman RM, Fava M, Thase ME, et al. Aripiprazole augmentation in major depressive disorder: a double-blind, placebo-controlled study in patients with inadequate response to antidepressants. CNS Spectr. 2009;14:197-206.
15. Trivedi MH, Thase ME, Fava M, et al. Adjunctive aripiprazole in major depressive disorder: analysis of efficacy and safety in patients with anxious and atypical features. J Clin Psychiatry. 2008;69:1928-1936.
16. Marcus RN, McQuade RD, Carson WH, et al. The efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: a second multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2008;28:156-165.
17. Simon JS, Nemeroff CB. Aripiprazole augmentation of antidepressants for the treatment of partially responding and nonresponding patients with major depressive disorder. J Clin Psychiatry. 2005;66:1216-1220.
18. Trivedi MH, Thase ME, Osuntokun O, et al. An integrated analysis of olanzapine/fluoxetine combination in clinical trials of treatment-resistant depression. J Clin Psychiatry. 2009;70:387-396.
19. Alexopoulos GS, Canuso CM, Gharabawi GM, et al. Placebo-controlled study of relapse prevention with risperidone augmentation in older patients with resistant depression. Am J Geriatr Psychiatry. 2008;16:21-30
20. Mahmoud RA, Pandina GJ, Turkoz I, et al. Risperidone for treatment-refractory major depressive disorder: a randomized trial. Ann Intern Med. 2007;147:593-602
21. Keitner GI, Garlow SJ, Ryan CE, et al. A randomized, placebo-controlled trial of risperidone augmentation for patients with difficult-to-treat unipolar, non-psychotic major depression. J Psychiatr Res. 2009;43:205-214.
22. Garakani A, Martinez JM, Marcus S, et al. A randomized, double-blind, and placebo-controlled trial of quetiapine augmentation of fluoxetine in major depressive disorder. Int Clin Psychopharmacol. 2008;23:269-275.
23. Bauer M, Pretorius HW, Constant EL, et al. Extended-release quetiapine as adjunct to an antidepressant in patients with major depressive disorder: results of a randomized, placebo-controlled, double-blind study. J Clin Psychiatry. 2009;70:540-549.
24. Carpenter LL, Yasmin S, Price LH. Double-blind, placebo-controlled study of antidepressant augmentation with mirtazapine. Biol Psychiatry. 2002;51:183-188.
25. Ozmenler NK, Karlidere T, Bozkurt A, et al. Mirtazapine augmentation in depressed patients with sexual dysfunction due to selective serotonin reuptake inhibitors. Hum Psychopharmacol. 2008;23:321-326.
26. Alpert JE, Mischoulon D, Rubenstein GE, et al. Folinic acid (Leucovorin) as an adjunctive treatment for SSRI-refractory depression. Ann Clin Psychiatry. 2002;14:33-38.
27. Alpert JE, Papakostas G, Mischoulon D, et al. S-adenosyl-Lmethionine (SAMe) as an adjunct for resistant major depressive disorder: an open trial following partial or nonresponse to selective serotonin reuptake inhibitors or venlafaxine. J Clin Psychopharmacol. 2004;24:661-664.
28. Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry. 2002;159:477-479.
29. Carney RM, Freedland KE, Rubin EH, et al. Depression in patients with coronary heart disease: a randomized controlled trial. JAMA. 2009;302:1651-1657.
30. Peet M, Horrobin DE. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry. 2002;59:913-919.
31. Mead GE, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database Syst Rev. 2009;(3):CD004366.-
32. Trivedi MH, Greer TL, Grannemann BD, et al. Exercise as an augmentation strategy for treatment of major depression. J Psychiatr Pract. 2006;12:205-213.
33. Trivedi MH, Greer TL, Grannemann BD, et al. TREAD: Treatment with Exercise Augmentation for Depression: study rationale and design. Clin Trials. 2006;3:291-305.
34. Thase ME, Friedman ES, Biggs MM, et al. Cognitive therapy versus medication in augmentation and switch strategies as second-step treatments: a STAR*D report. Am J Psychiatry. 2007;164:739-752.
35. Kocsis JH, Gelenberg AJ, Rothbaum BO, et al. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: the REVAMP Trial. Arch Gen Psychiatry. 2009;66:1178-1188.
36. Perry EB, Berman RM, Sanacora G, et al. Pindolol augmentation in depressed patients resistant to selective serotonin reuptake inhibitors: a double-blind, randomized, controlled trial. J Clin Psychiatry. 2004;65:238-243.
37. Rasmussen NA, Schrøder P, Olsen LR, et al. Modafi nil augmentation in depressed patients with partial response to antidepressants: a pilot study on self-reported symptoms covered by the Major Depression Inventory (MDI) and the Symptom Checklist (SCL-92). Nord J Psychiatry. 2005;59:173-178.
38. Santos MA, Rocha FL, Hara C. Efficacy and safety of antidepressant augmentation with lamotrigine in patients with treatment-resistant depression: a randomized, placebo-controlled, double-blind study. Prim Care Companion J Clin Psychiatry. 2008;10:187-190.
39. Dorée JP, Des Rosiers J, Lew V, et al. Quetiapine augmentation of treatment-resistant depression: a comparison with lithium. Curr Med Res Opin. 2007;23:333-341.
40. Lesser IM, Castro DB, Gaynes BN, et al. Ethnicity/race and outcome in the treatment of depression: results from STAR*D. Med Care. 2007;45:1043-1051.
41. Lesser IM, Leuchter AF, Trivedi MH, et al. Characteristics of insured and noninsured outpatients with depression in STAR(*) D. Psychiatr Serv. 2005;56:995-1004.
42. Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23:551-560.
• While lithium produces significant remission rates in augmentation efforts for treatment-resistant depression, it is more likely to cause side effects than many other psychotropic agents. A
• Medication and cognitive therapy are equally effective when augmenting antidepressant therapy; cognitive therapy, however, takes longer to achieve remission. B
• Since the efficacy of many agents is similar when augmenting treatment, it’s important to factor the cost of the medication, side effects, and patient preference into the decision process. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The sobering truth about major depression is that too often it goes unrecognized or undertreated.1,2 And even when it is treated correctly, up to 34% of patients fail to respond to treatment.3 In the United States alone, the lifetime prevalence of the disease is 16.2%, and more than 6% of adults experience symptoms of major depression in any given year.2 Obviously, we need to do more for these patients.
Treatment-resistant depression has been defined as the failure to achieve remission after continuous therapy for about 6 to 12 weeks with an adequate dose of a single antidepressant.4 Remission is typically defined as a 50% reduction of scores on depression severity scales, with the 17-item Hamilton Rating Scale of Depression (HRSD17) and the 16-item Quick Inventory of Depressive Symptomatology–Self-Report (QIDS-SR16) being the most often used. An adequate dose is the lowest effective dose that doesn’t cause intolerable side effects.
What are our best options for treatment-resistant depression?
To answer this question, we reviewed all English language studies in PubMed or Medline that were performed among adults using the search terms “augmentation, antidepressants, major depression.” We excluded studies involving patients with comorbid anxiety, bipolar disorder, or other major mental illnesses.
Based on our review of the literature, we found support for several augmentative treatments for patients with treatment-resistant depression (TABLE). Of note, though: Most of these studies were randomized trials dating back nearly 2 decades and had limitations. Most were not blinded, nor did they have consistent placebo controls. The studies were typically small (albeit frequently still showing efficacy for the agent despite lower statistical power) and of relatively short duration (typically 6-14 weeks). There were few studies that looked at treatment approaches over longer periods or that considered indications and timelines for tapering of medications once remission had been achieved. A major exception to the rule was the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, which we’ll discuss below.5
The research points to several viable options: Clinicians can switch antidepressants, augment these agents by adding others—usually nonantidepressants—or completely change the therapeutic approach. Since most of the research discusses augmentation, we’ll focus on that here. Because the decision to use electroconvulsive therapy, vagus nerve stimulators, or other nonpharmaceutical approaches is made in consultation with a psychiatrist, we will not discuss these options.
TABLE
How these agents compare for treatment-resistant depression
| Agent/approach | Remission rate | Starting dose | Titrated to… | Frequency of side effects | SOR rating |
|---|---|---|---|---|---|
| Lithium5-9 | 53%-60% | 300 mg BID-TID | Doses of 800-1500 mg and lithium level of 0.5-1 mmol/L | >25% | A |
| Thyroid supplementation10-13 | 25%-59% | 20-50 mcg | Often not titrated | 11%-25% | A |
| Aripiprazole14-17 | 25%-37% | 2-5 mg | 15-20 mg | 16%-25% | A |
| Olanzapine/fluoxetine18 | 25% | Fixed dose | Fixed dose | 10%-40% | A |
| Risperidone19-21 | 25%-71% | 0.25-1 mg | 0.5-3 mg | 6%-10% | A |
| Quetiapine22,23 | 36%-49% | 25-200 mg | 100-600 mg | >25% | B |
| Mirtazapine24 | 45% | 15 mg | 30 mg | 6%-10% | B |
| Cognitive therapy34 | 23% | NA | NA | 0%-5% | B |
| Folic acid (Leucovorin)26 | 18% | 15 mg | 30 mg | 11%-25% | C |
| SAMe27 | 43% | 800 mg | 1600 mg | 50% | C |
| NA, not applicable; SAMe, S-adenosyl-L-methionine; SOR, strength of recommendation. | |||||
Lithium: Good results, but with side effects
Lithium is one of the oldest and most well studied agents.6-9 Most studies used 900 mg divided into 3 daily doses and titrated to lithium plasma levels of 0.5 to 1 mmol/L. Unfortunately, though, lithium is more likely to cause side effects than many other psychotropic agents (>25%).5-9 And while the research has found that lithium produces significant remission rates, it’s not very effective in patients who have failed multiple antidepressant trials, with only 12.5% to 15.9% of patients in that cohort achieving remission.10,11
Thyroid hormone has only mild side effects
Low-dose thyroid supplementation has been used for decades in euthyroid patients with treatment-resistant depression; remission rates range from 25% to 59%.10-13 Most studies used a low fixed-dose therapy between 25 and 50 mcg daily; side effects were mild and occurred at rates similar to placebo.13
Atypical antipsychotics: Many pluses, but weight gain is an issue
Atypical antipsychotics are an attractive alternative to typical antipsychotics for treatment-resistant depression. They are much less likely to cause extrapyramidal symptoms, tardive dyskinesia, and other motor symptoms, but as a trade-off they often cause weight gain, abnormal glucose metabolism, dyslipidemia, and hyperprolactinemia.
Aripiprazole (Abilify) is 1 of 2 medications approved by the Food and Drug Administration (FDA) for treatment-resistant depression. Studies have shown remission rates of 25% to 37%, with side effects in 16% to 25% of patients.14-16 Akathisia, the major side effect, can be reduced by lowering the starting dose to 2.5 mg.17
Olanzapine, combined with fluoxetine in a fixed-dose pill (Symbyax), is the other FDA-approved agent for treatment-resistant depression. Trivedi and colleagues showed a remission rate of 25.5% and side effects ranging from 10% to 40%.18
Risperidone (Risperdal) rivals the efficacy of the medications previously discussed, but starting doses and titration schedules vary widely, making it difficult to determine which treatment course would be most efficacious.19-21
Quetiapine (Seroquel) has produced mixed results in treatment-resistant patients. That may have been because some studies used lower daily doses—25 to 100 mg—vs 150 to 600 mg in other trials.22 Bauer found higher remission rates compared to placebo (36% vs 24%)23 while Garakani22 did not (49% for quetiapine vs. 63% for placebo when using an intention-to-treat analysis; a similar lack of efficacy was found if those who dropped out of the study were excluded; P<0.29). Garakani also found that dry mouth, sedation, and other side effects occurred in up to 76% of patients. (Of note: Most studies of atypical antipsychotics are industry funded.)
Mirtazapine has not been well studied
Unfortunately, there are very little data on mirtazapine (Remeron). When the drug was added to ongoing antidepressant therapy, a single double-blind, randomized controlled trial found significantly better response rates compared with placebo.24 One advantage of the drug was that it helped relieve the sexual side effects of ongoing selective serotonin reuptake inhibitor (SSRI) therapy.25
Folic acid and SAMe also haven’t been well studied
Up to 50% of Americans have low levels of central nervous system L-methylfolate, which is a key co-factor in monoamine neurotransmitter production. Although lower plasma folate has been linked to depression, folate supplementation as a primary treatment for major depression has not been well studied and its use in treatment-resistant depression is limited to 1 study by Alpert and colleagues.26 Using an open-label, nonplacebo-controlled design in which folinic acid—an activated form of folic acid—was compared with placebo, researchers found remission rates of 18%, which is not significantly higher than the placebo response seen in other studies.
Similarly, there’s limited research on S-adenosyl-L-methionine (SAMe). Using a similar open-label, nonplacebo-controlled design, Alpert found a 43% remission rate in patients with treatment-resistant depression. Side effects occurred in up to half of patients, prompting 6.6% of patients to leave the study.27
Omega-3 fatty acids: The news is mixed
Data are contradictory on the value of omega-3 fatty acid for major depression28,29 and the evidence to support its use in treatment-resistant depression is likewise limited and contradictory.30 Until the data are more consistent and robust, it’s unclear whether omega-3 fatty acid supplementation can benefit patients.
Exercise helps
Some studies suggest that exercise can have a dose-responsive effect on clinical depression.31 As a result, the Treatment with Exercise Augmentation for Depression (TREAD) trial is underway to examine whether it can augment drug therapy. Preliminary evidence suggests that 30 minutes of aerobic exercise most days of the week can be effective.32,33 (For more on exercise, see “Does exercise alleviate symptoms of depression?”)
Cognitive therapy helps patients, and there are no side effects
The STAR*D study showed equivalent efficacy in achieving remission (23% vs. 33%) when comparing augmentation with cognitive therapy and augmentation with medications, with a low rate of side effects seen for cognitive therapy.34 Notably, it took longer to achieve remission (55 vs 40 days) when cognitive therapy was added to antidepressants. (For more on the STAR*D trial, see “What we learned from the STAR*D trial”) It’s also worth mentioning that other researchers did not find similar results for augmentation when they compared cognitive behavioral and brief supportive psychotherapy with medication therapy only.35
The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study is noteworthy because of its size, duration, design, and impact on the treatment of depression.5 This was a multicenter study of 3671 patients with major unipolar depression. Remission was determined by 2 rating scales—HRSD17 and QIDS-SR16*—and side effects were measured at each visit. There was no placebo control, no consideration for atypical antipsychotic medications or other therapies, and randomization was limited.
The FIGURE below shows how STAR*D was structured. In Level 1, patients were treated with citalopram (Celexa). If they didn’t go into remission, they were encouraged to proceed to Level 2, which involved 3 arms: switching agents, augmenting agents, or cognitive therapy. Patients chose which arm they wanted and were randomized to the specific medications used in that level. Switch agents included bupropion SR (Wellbutrin SR), sertraline (Zoloft), and venlafaxine XR (Effexor XR). Augmentation was with buspirone (BuSpar) and bupropion. Cognitive therapy was with or without continued citalopram with a second augmentation level of bupropion SR or venlafaxine XR. Level 3 also involved switch and augmentation arms using nortriptyline (Aventyl, Pamelor) or mirtazapine (Remeron) for switch agents and lithium or thyroxine for augmentation. Level 4 involved switching to tranylcypromine (Parnate) or venlafaxine XR plus mirtazapine.
Remission rates were 36.8% for those in Level 1, 30.6% in Level 2, 13.7% in Level 3, and 13% in Level 4. The cumulative remission rate was 67%. While remission rates for switch strategies in Levels 2 and 3 appeared to be lower for pharmacologic agents compared with augmentation strategies (27% vs 35% in Level 2 and 10.7% vs 20.5% in Level 3), the sample sizes were too small for the differences to be statistically significant, and the study was underpowered to establish the superiority of switch vs augmentation strategies.
Finally, it’s important to mention that patients of primary care physicians had similar remission rates, when compared with psychiatrists’ patients.42 Keep in mind, however, that the care provided in the STAR*D trial was structured and protocol-driven. After randomization into 1 medication group or another, dose adjustments were standardized at set intervals and based on inadequate response to validated depression severity assessment tools. Outcomes were patient-based and uniformly applied. This study structure may explain why remission rates were identical regardless of the specialty of the treating physician.
*The 17-item Hamilton Rating Scale of Depression and the 16-item Quick Inventory of Depressive Symptomatology–Self Report.
FIGURE
Structure of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D)
These agents don’t appear helpful in augmentation efforts
Several other agents have been studied with no effect on remission rates. These include pindolol,36 modafinil,37 buspirone, lamotrigine,38 stimulants, and estrogen replacement.
Consider side effects, cost, and patient preference
Because most studies showed that the efficacy of the tested drugs was similar, how do you decide which augmenting agent to prescribe? The usual standard is lithium, which offers rates of remission that are high, but not statistically significantly better when compared with thyroid supplementation and cognitive therapy. Quetiapine, while not more efficacious, may lower scores on depression rating scales more quickly than lithium.39 Additionally, the STAR*D trial suggests that many agents may be used in augmentation with similar results.
In the final analysis, the family physician has to consider factors other than efficacy. You also have to factor in the costs of medicines and lab testing, patient preference, and side effects. Lithium is most likely to cause side effects. Atypical antipsychotics seem to have lower short-term side effect profiles with efficacy similar to cognitive therapy. However, the potential drawbacks of antipsychotics, including aberrations in glucose metabolism, weight, and lipid profiles, are not typically seen in short-term studies. Obviously, more long-term studies are necessary before 1 agent can be deemed superior.
When should you stop therapy?
That question still doesn’t have a definitive answer. The STAR*D trial found that patients who achieved full remission were less likely to relapse/worsen than those who had only a partial response. The time to relapse ranged from 2.5 to 4.5 months and was shorter for those patients requiring 2 or more levels of treatment. As there was no control of the therapeutic interventions used during this time, we can’t be certain about what caused the relapse, but burden of disease, income levels, and ethnicity all played roles in symptom severity, decreasing remission rates, and increasing relapse rates.40,41
While we cannot identify the ideal or even preferred duration of augmentation in patients with treatment-resistant depression, it seems clear that relapse is extremely common and tends to occur relatively early after achieving remission.
CORRESPONDENCE Paul Hicks, MD, Department of Family and Community Medicine, 1450 North Cherry Avenue, Tucson, AZ 85719; [email protected]
• While lithium produces significant remission rates in augmentation efforts for treatment-resistant depression, it is more likely to cause side effects than many other psychotropic agents. A
• Medication and cognitive therapy are equally effective when augmenting antidepressant therapy; cognitive therapy, however, takes longer to achieve remission. B
• Since the efficacy of many agents is similar when augmenting treatment, it’s important to factor the cost of the medication, side effects, and patient preference into the decision process. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The sobering truth about major depression is that too often it goes unrecognized or undertreated.1,2 And even when it is treated correctly, up to 34% of patients fail to respond to treatment.3 In the United States alone, the lifetime prevalence of the disease is 16.2%, and more than 6% of adults experience symptoms of major depression in any given year.2 Obviously, we need to do more for these patients.
Treatment-resistant depression has been defined as the failure to achieve remission after continuous therapy for about 6 to 12 weeks with an adequate dose of a single antidepressant.4 Remission is typically defined as a 50% reduction of scores on depression severity scales, with the 17-item Hamilton Rating Scale of Depression (HRSD17) and the 16-item Quick Inventory of Depressive Symptomatology–Self-Report (QIDS-SR16) being the most often used. An adequate dose is the lowest effective dose that doesn’t cause intolerable side effects.
What are our best options for treatment-resistant depression?
To answer this question, we reviewed all English language studies in PubMed or Medline that were performed among adults using the search terms “augmentation, antidepressants, major depression.” We excluded studies involving patients with comorbid anxiety, bipolar disorder, or other major mental illnesses.
Based on our review of the literature, we found support for several augmentative treatments for patients with treatment-resistant depression (TABLE). Of note, though: Most of these studies were randomized trials dating back nearly 2 decades and had limitations. Most were not blinded, nor did they have consistent placebo controls. The studies were typically small (albeit frequently still showing efficacy for the agent despite lower statistical power) and of relatively short duration (typically 6-14 weeks). There were few studies that looked at treatment approaches over longer periods or that considered indications and timelines for tapering of medications once remission had been achieved. A major exception to the rule was the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, which we’ll discuss below.5
The research points to several viable options: Clinicians can switch antidepressants, augment these agents by adding others—usually nonantidepressants—or completely change the therapeutic approach. Since most of the research discusses augmentation, we’ll focus on that here. Because the decision to use electroconvulsive therapy, vagus nerve stimulators, or other nonpharmaceutical approaches is made in consultation with a psychiatrist, we will not discuss these options.
TABLE
How these agents compare for treatment-resistant depression
| Agent/approach | Remission rate | Starting dose | Titrated to… | Frequency of side effects | SOR rating |
|---|---|---|---|---|---|
| Lithium5-9 | 53%-60% | 300 mg BID-TID | Doses of 800-1500 mg and lithium level of 0.5-1 mmol/L | >25% | A |
| Thyroid supplementation10-13 | 25%-59% | 20-50 mcg | Often not titrated | 11%-25% | A |
| Aripiprazole14-17 | 25%-37% | 2-5 mg | 15-20 mg | 16%-25% | A |
| Olanzapine/fluoxetine18 | 25% | Fixed dose | Fixed dose | 10%-40% | A |
| Risperidone19-21 | 25%-71% | 0.25-1 mg | 0.5-3 mg | 6%-10% | A |
| Quetiapine22,23 | 36%-49% | 25-200 mg | 100-600 mg | >25% | B |
| Mirtazapine24 | 45% | 15 mg | 30 mg | 6%-10% | B |
| Cognitive therapy34 | 23% | NA | NA | 0%-5% | B |
| Folic acid (Leucovorin)26 | 18% | 15 mg | 30 mg | 11%-25% | C |
| SAMe27 | 43% | 800 mg | 1600 mg | 50% | C |
| NA, not applicable; SAMe, S-adenosyl-L-methionine; SOR, strength of recommendation. | |||||
Lithium: Good results, but with side effects
Lithium is one of the oldest and most well studied agents.6-9 Most studies used 900 mg divided into 3 daily doses and titrated to lithium plasma levels of 0.5 to 1 mmol/L. Unfortunately, though, lithium is more likely to cause side effects than many other psychotropic agents (>25%).5-9 And while the research has found that lithium produces significant remission rates, it’s not very effective in patients who have failed multiple antidepressant trials, with only 12.5% to 15.9% of patients in that cohort achieving remission.10,11
Thyroid hormone has only mild side effects
Low-dose thyroid supplementation has been used for decades in euthyroid patients with treatment-resistant depression; remission rates range from 25% to 59%.10-13 Most studies used a low fixed-dose therapy between 25 and 50 mcg daily; side effects were mild and occurred at rates similar to placebo.13
Atypical antipsychotics: Many pluses, but weight gain is an issue
Atypical antipsychotics are an attractive alternative to typical antipsychotics for treatment-resistant depression. They are much less likely to cause extrapyramidal symptoms, tardive dyskinesia, and other motor symptoms, but as a trade-off they often cause weight gain, abnormal glucose metabolism, dyslipidemia, and hyperprolactinemia.
Aripiprazole (Abilify) is 1 of 2 medications approved by the Food and Drug Administration (FDA) for treatment-resistant depression. Studies have shown remission rates of 25% to 37%, with side effects in 16% to 25% of patients.14-16 Akathisia, the major side effect, can be reduced by lowering the starting dose to 2.5 mg.17
Olanzapine, combined with fluoxetine in a fixed-dose pill (Symbyax), is the other FDA-approved agent for treatment-resistant depression. Trivedi and colleagues showed a remission rate of 25.5% and side effects ranging from 10% to 40%.18
Risperidone (Risperdal) rivals the efficacy of the medications previously discussed, but starting doses and titration schedules vary widely, making it difficult to determine which treatment course would be most efficacious.19-21
Quetiapine (Seroquel) has produced mixed results in treatment-resistant patients. That may have been because some studies used lower daily doses—25 to 100 mg—vs 150 to 600 mg in other trials.22 Bauer found higher remission rates compared to placebo (36% vs 24%)23 while Garakani22 did not (49% for quetiapine vs. 63% for placebo when using an intention-to-treat analysis; a similar lack of efficacy was found if those who dropped out of the study were excluded; P<0.29). Garakani also found that dry mouth, sedation, and other side effects occurred in up to 76% of patients. (Of note: Most studies of atypical antipsychotics are industry funded.)
Mirtazapine has not been well studied
Unfortunately, there are very little data on mirtazapine (Remeron). When the drug was added to ongoing antidepressant therapy, a single double-blind, randomized controlled trial found significantly better response rates compared with placebo.24 One advantage of the drug was that it helped relieve the sexual side effects of ongoing selective serotonin reuptake inhibitor (SSRI) therapy.25
Folic acid and SAMe also haven’t been well studied
Up to 50% of Americans have low levels of central nervous system L-methylfolate, which is a key co-factor in monoamine neurotransmitter production. Although lower plasma folate has been linked to depression, folate supplementation as a primary treatment for major depression has not been well studied and its use in treatment-resistant depression is limited to 1 study by Alpert and colleagues.26 Using an open-label, nonplacebo-controlled design in which folinic acid—an activated form of folic acid—was compared with placebo, researchers found remission rates of 18%, which is not significantly higher than the placebo response seen in other studies.
Similarly, there’s limited research on S-adenosyl-L-methionine (SAMe). Using a similar open-label, nonplacebo-controlled design, Alpert found a 43% remission rate in patients with treatment-resistant depression. Side effects occurred in up to half of patients, prompting 6.6% of patients to leave the study.27
Omega-3 fatty acids: The news is mixed
Data are contradictory on the value of omega-3 fatty acid for major depression28,29 and the evidence to support its use in treatment-resistant depression is likewise limited and contradictory.30 Until the data are more consistent and robust, it’s unclear whether omega-3 fatty acid supplementation can benefit patients.
Exercise helps
Some studies suggest that exercise can have a dose-responsive effect on clinical depression.31 As a result, the Treatment with Exercise Augmentation for Depression (TREAD) trial is underway to examine whether it can augment drug therapy. Preliminary evidence suggests that 30 minutes of aerobic exercise most days of the week can be effective.32,33 (For more on exercise, see “Does exercise alleviate symptoms of depression?”)
Cognitive therapy helps patients, and there are no side effects
The STAR*D study showed equivalent efficacy in achieving remission (23% vs. 33%) when comparing augmentation with cognitive therapy and augmentation with medications, with a low rate of side effects seen for cognitive therapy.34 Notably, it took longer to achieve remission (55 vs 40 days) when cognitive therapy was added to antidepressants. (For more on the STAR*D trial, see “What we learned from the STAR*D trial”) It’s also worth mentioning that other researchers did not find similar results for augmentation when they compared cognitive behavioral and brief supportive psychotherapy with medication therapy only.35
The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study is noteworthy because of its size, duration, design, and impact on the treatment of depression.5 This was a multicenter study of 3671 patients with major unipolar depression. Remission was determined by 2 rating scales—HRSD17 and QIDS-SR16*—and side effects were measured at each visit. There was no placebo control, no consideration for atypical antipsychotic medications or other therapies, and randomization was limited.
The FIGURE below shows how STAR*D was structured. In Level 1, patients were treated with citalopram (Celexa). If they didn’t go into remission, they were encouraged to proceed to Level 2, which involved 3 arms: switching agents, augmenting agents, or cognitive therapy. Patients chose which arm they wanted and were randomized to the specific medications used in that level. Switch agents included bupropion SR (Wellbutrin SR), sertraline (Zoloft), and venlafaxine XR (Effexor XR). Augmentation was with buspirone (BuSpar) and bupropion. Cognitive therapy was with or without continued citalopram with a second augmentation level of bupropion SR or venlafaxine XR. Level 3 also involved switch and augmentation arms using nortriptyline (Aventyl, Pamelor) or mirtazapine (Remeron) for switch agents and lithium or thyroxine for augmentation. Level 4 involved switching to tranylcypromine (Parnate) or venlafaxine XR plus mirtazapine.
Remission rates were 36.8% for those in Level 1, 30.6% in Level 2, 13.7% in Level 3, and 13% in Level 4. The cumulative remission rate was 67%. While remission rates for switch strategies in Levels 2 and 3 appeared to be lower for pharmacologic agents compared with augmentation strategies (27% vs 35% in Level 2 and 10.7% vs 20.5% in Level 3), the sample sizes were too small for the differences to be statistically significant, and the study was underpowered to establish the superiority of switch vs augmentation strategies.
Finally, it’s important to mention that patients of primary care physicians had similar remission rates, when compared with psychiatrists’ patients.42 Keep in mind, however, that the care provided in the STAR*D trial was structured and protocol-driven. After randomization into 1 medication group or another, dose adjustments were standardized at set intervals and based on inadequate response to validated depression severity assessment tools. Outcomes were patient-based and uniformly applied. This study structure may explain why remission rates were identical regardless of the specialty of the treating physician.
*The 17-item Hamilton Rating Scale of Depression and the 16-item Quick Inventory of Depressive Symptomatology–Self Report.
FIGURE
Structure of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D)
These agents don’t appear helpful in augmentation efforts
Several other agents have been studied with no effect on remission rates. These include pindolol,36 modafinil,37 buspirone, lamotrigine,38 stimulants, and estrogen replacement.
Consider side effects, cost, and patient preference
Because most studies showed that the efficacy of the tested drugs was similar, how do you decide which augmenting agent to prescribe? The usual standard is lithium, which offers rates of remission that are high, but not statistically significantly better when compared with thyroid supplementation and cognitive therapy. Quetiapine, while not more efficacious, may lower scores on depression rating scales more quickly than lithium.39 Additionally, the STAR*D trial suggests that many agents may be used in augmentation with similar results.
In the final analysis, the family physician has to consider factors other than efficacy. You also have to factor in the costs of medicines and lab testing, patient preference, and side effects. Lithium is most likely to cause side effects. Atypical antipsychotics seem to have lower short-term side effect profiles with efficacy similar to cognitive therapy. However, the potential drawbacks of antipsychotics, including aberrations in glucose metabolism, weight, and lipid profiles, are not typically seen in short-term studies. Obviously, more long-term studies are necessary before 1 agent can be deemed superior.
When should you stop therapy?
That question still doesn’t have a definitive answer. The STAR*D trial found that patients who achieved full remission were less likely to relapse/worsen than those who had only a partial response. The time to relapse ranged from 2.5 to 4.5 months and was shorter for those patients requiring 2 or more levels of treatment. As there was no control of the therapeutic interventions used during this time, we can’t be certain about what caused the relapse, but burden of disease, income levels, and ethnicity all played roles in symptom severity, decreasing remission rates, and increasing relapse rates.40,41
While we cannot identify the ideal or even preferred duration of augmentation in patients with treatment-resistant depression, it seems clear that relapse is extremely common and tends to occur relatively early after achieving remission.
CORRESPONDENCE Paul Hicks, MD, Department of Family and Community Medicine, 1450 North Cherry Avenue, Tucson, AZ 85719; [email protected]
1. Kocsis JH, Gelenberg AJ, Rothbaum B, et al. Chronic forms of major depression are still undertreated in the 21st century: systematic assessment of 801 patients presenting for treatment. J Affect Disord. 2008;110:55-61.
2. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095-3105.
3. Fava M, Davidson KG. Definition and epidemiology of treatment-resistant depression. Psychiatr Clin North Am. 1996;19:179-200.
4. Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53:649-659.
5. Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients who required one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905-1917.
6. Cappiello A, McDougle CJ, Delgado PL, et al. Lithium and desipramine versus desipramine alone in the treatment of severe major depression: a preliminary study. Int Clin Psychopharmacol. 1998;13:191-198.
7. Katona CL, Abou-Saleh MT, Harrison DA, et al. Placebo-controlled trial of lithium augmentation of fluoxetine and lofepramine. Br J Psychiatry. 1995;166:80-86.
8. Bauer M, Bschor T, Kunz D, et al. Double-blind, placebo-controlled trial of the use of lithium to augment antidepressant medication in continuation treatment of unipolar major depression. Am J Psychiatry. 2000;157:1429-1435.
9. Joffe RT, Singer W, Levitt AJ, et al. A placebo-controlled comparison of lithium and triiodothyronine augmentation of tricyclic antidepressants in unipolar refractory depression. Arch Gen Psychiatry. 1993;50:387-393.
10. Nierenberg AA, Fava M, Trivedi MH, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. Am J Psychiatry. 2006;163:1519-1530.
11. Nierenberg AA, Papakostas GI, Petersen T, et al. Lithium augmentation of nortriptyline for subjects resistant to multiple antidepressants. J Clin Psychopharmacol. 2003;23:92-95.
12. Aronson R, Offman HJ, Joffe RT, et al. Triiodothyronine augmentation in the treatment of refractory depression. A meta-analysis. Arch Gen Psychiatry. 1996;53:842-848.
13. Joffe RT, Sokolov ST, Levitt AJ. Lithium and triiodothyronine augmentation of antidepressants. Can J Psychiatry. 2006;51:791-793.
14. Berman RM, Fava M, Thase ME, et al. Aripiprazole augmentation in major depressive disorder: a double-blind, placebo-controlled study in patients with inadequate response to antidepressants. CNS Spectr. 2009;14:197-206.
15. Trivedi MH, Thase ME, Fava M, et al. Adjunctive aripiprazole in major depressive disorder: analysis of efficacy and safety in patients with anxious and atypical features. J Clin Psychiatry. 2008;69:1928-1936.
16. Marcus RN, McQuade RD, Carson WH, et al. The efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: a second multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2008;28:156-165.
17. Simon JS, Nemeroff CB. Aripiprazole augmentation of antidepressants for the treatment of partially responding and nonresponding patients with major depressive disorder. J Clin Psychiatry. 2005;66:1216-1220.
18. Trivedi MH, Thase ME, Osuntokun O, et al. An integrated analysis of olanzapine/fluoxetine combination in clinical trials of treatment-resistant depression. J Clin Psychiatry. 2009;70:387-396.
19. Alexopoulos GS, Canuso CM, Gharabawi GM, et al. Placebo-controlled study of relapse prevention with risperidone augmentation in older patients with resistant depression. Am J Geriatr Psychiatry. 2008;16:21-30
20. Mahmoud RA, Pandina GJ, Turkoz I, et al. Risperidone for treatment-refractory major depressive disorder: a randomized trial. Ann Intern Med. 2007;147:593-602
21. Keitner GI, Garlow SJ, Ryan CE, et al. A randomized, placebo-controlled trial of risperidone augmentation for patients with difficult-to-treat unipolar, non-psychotic major depression. J Psychiatr Res. 2009;43:205-214.
22. Garakani A, Martinez JM, Marcus S, et al. A randomized, double-blind, and placebo-controlled trial of quetiapine augmentation of fluoxetine in major depressive disorder. Int Clin Psychopharmacol. 2008;23:269-275.
23. Bauer M, Pretorius HW, Constant EL, et al. Extended-release quetiapine as adjunct to an antidepressant in patients with major depressive disorder: results of a randomized, placebo-controlled, double-blind study. J Clin Psychiatry. 2009;70:540-549.
24. Carpenter LL, Yasmin S, Price LH. Double-blind, placebo-controlled study of antidepressant augmentation with mirtazapine. Biol Psychiatry. 2002;51:183-188.
25. Ozmenler NK, Karlidere T, Bozkurt A, et al. Mirtazapine augmentation in depressed patients with sexual dysfunction due to selective serotonin reuptake inhibitors. Hum Psychopharmacol. 2008;23:321-326.
26. Alpert JE, Mischoulon D, Rubenstein GE, et al. Folinic acid (Leucovorin) as an adjunctive treatment for SSRI-refractory depression. Ann Clin Psychiatry. 2002;14:33-38.
27. Alpert JE, Papakostas G, Mischoulon D, et al. S-adenosyl-Lmethionine (SAMe) as an adjunct for resistant major depressive disorder: an open trial following partial or nonresponse to selective serotonin reuptake inhibitors or venlafaxine. J Clin Psychopharmacol. 2004;24:661-664.
28. Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry. 2002;159:477-479.
29. Carney RM, Freedland KE, Rubin EH, et al. Depression in patients with coronary heart disease: a randomized controlled trial. JAMA. 2009;302:1651-1657.
30. Peet M, Horrobin DE. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry. 2002;59:913-919.
31. Mead GE, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database Syst Rev. 2009;(3):CD004366.-
32. Trivedi MH, Greer TL, Grannemann BD, et al. Exercise as an augmentation strategy for treatment of major depression. J Psychiatr Pract. 2006;12:205-213.
33. Trivedi MH, Greer TL, Grannemann BD, et al. TREAD: Treatment with Exercise Augmentation for Depression: study rationale and design. Clin Trials. 2006;3:291-305.
34. Thase ME, Friedman ES, Biggs MM, et al. Cognitive therapy versus medication in augmentation and switch strategies as second-step treatments: a STAR*D report. Am J Psychiatry. 2007;164:739-752.
35. Kocsis JH, Gelenberg AJ, Rothbaum BO, et al. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: the REVAMP Trial. Arch Gen Psychiatry. 2009;66:1178-1188.
36. Perry EB, Berman RM, Sanacora G, et al. Pindolol augmentation in depressed patients resistant to selective serotonin reuptake inhibitors: a double-blind, randomized, controlled trial. J Clin Psychiatry. 2004;65:238-243.
37. Rasmussen NA, Schrøder P, Olsen LR, et al. Modafi nil augmentation in depressed patients with partial response to antidepressants: a pilot study on self-reported symptoms covered by the Major Depression Inventory (MDI) and the Symptom Checklist (SCL-92). Nord J Psychiatry. 2005;59:173-178.
38. Santos MA, Rocha FL, Hara C. Efficacy and safety of antidepressant augmentation with lamotrigine in patients with treatment-resistant depression: a randomized, placebo-controlled, double-blind study. Prim Care Companion J Clin Psychiatry. 2008;10:187-190.
39. Dorée JP, Des Rosiers J, Lew V, et al. Quetiapine augmentation of treatment-resistant depression: a comparison with lithium. Curr Med Res Opin. 2007;23:333-341.
40. Lesser IM, Castro DB, Gaynes BN, et al. Ethnicity/race and outcome in the treatment of depression: results from STAR*D. Med Care. 2007;45:1043-1051.
41. Lesser IM, Leuchter AF, Trivedi MH, et al. Characteristics of insured and noninsured outpatients with depression in STAR(*) D. Psychiatr Serv. 2005;56:995-1004.
42. Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23:551-560.
1. Kocsis JH, Gelenberg AJ, Rothbaum B, et al. Chronic forms of major depression are still undertreated in the 21st century: systematic assessment of 801 patients presenting for treatment. J Affect Disord. 2008;110:55-61.
2. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095-3105.
3. Fava M, Davidson KG. Definition and epidemiology of treatment-resistant depression. Psychiatr Clin North Am. 1996;19:179-200.
4. Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53:649-659.
5. Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients who required one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905-1917.
6. Cappiello A, McDougle CJ, Delgado PL, et al. Lithium and desipramine versus desipramine alone in the treatment of severe major depression: a preliminary study. Int Clin Psychopharmacol. 1998;13:191-198.
7. Katona CL, Abou-Saleh MT, Harrison DA, et al. Placebo-controlled trial of lithium augmentation of fluoxetine and lofepramine. Br J Psychiatry. 1995;166:80-86.
8. Bauer M, Bschor T, Kunz D, et al. Double-blind, placebo-controlled trial of the use of lithium to augment antidepressant medication in continuation treatment of unipolar major depression. Am J Psychiatry. 2000;157:1429-1435.
9. Joffe RT, Singer W, Levitt AJ, et al. A placebo-controlled comparison of lithium and triiodothyronine augmentation of tricyclic antidepressants in unipolar refractory depression. Arch Gen Psychiatry. 1993;50:387-393.
10. Nierenberg AA, Fava M, Trivedi MH, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. Am J Psychiatry. 2006;163:1519-1530.
11. Nierenberg AA, Papakostas GI, Petersen T, et al. Lithium augmentation of nortriptyline for subjects resistant to multiple antidepressants. J Clin Psychopharmacol. 2003;23:92-95.
12. Aronson R, Offman HJ, Joffe RT, et al. Triiodothyronine augmentation in the treatment of refractory depression. A meta-analysis. Arch Gen Psychiatry. 1996;53:842-848.
13. Joffe RT, Sokolov ST, Levitt AJ. Lithium and triiodothyronine augmentation of antidepressants. Can J Psychiatry. 2006;51:791-793.
14. Berman RM, Fava M, Thase ME, et al. Aripiprazole augmentation in major depressive disorder: a double-blind, placebo-controlled study in patients with inadequate response to antidepressants. CNS Spectr. 2009;14:197-206.
15. Trivedi MH, Thase ME, Fava M, et al. Adjunctive aripiprazole in major depressive disorder: analysis of efficacy and safety in patients with anxious and atypical features. J Clin Psychiatry. 2008;69:1928-1936.
16. Marcus RN, McQuade RD, Carson WH, et al. The efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: a second multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2008;28:156-165.
17. Simon JS, Nemeroff CB. Aripiprazole augmentation of antidepressants for the treatment of partially responding and nonresponding patients with major depressive disorder. J Clin Psychiatry. 2005;66:1216-1220.
18. Trivedi MH, Thase ME, Osuntokun O, et al. An integrated analysis of olanzapine/fluoxetine combination in clinical trials of treatment-resistant depression. J Clin Psychiatry. 2009;70:387-396.
19. Alexopoulos GS, Canuso CM, Gharabawi GM, et al. Placebo-controlled study of relapse prevention with risperidone augmentation in older patients with resistant depression. Am J Geriatr Psychiatry. 2008;16:21-30
20. Mahmoud RA, Pandina GJ, Turkoz I, et al. Risperidone for treatment-refractory major depressive disorder: a randomized trial. Ann Intern Med. 2007;147:593-602
21. Keitner GI, Garlow SJ, Ryan CE, et al. A randomized, placebo-controlled trial of risperidone augmentation for patients with difficult-to-treat unipolar, non-psychotic major depression. J Psychiatr Res. 2009;43:205-214.
22. Garakani A, Martinez JM, Marcus S, et al. A randomized, double-blind, and placebo-controlled trial of quetiapine augmentation of fluoxetine in major depressive disorder. Int Clin Psychopharmacol. 2008;23:269-275.
23. Bauer M, Pretorius HW, Constant EL, et al. Extended-release quetiapine as adjunct to an antidepressant in patients with major depressive disorder: results of a randomized, placebo-controlled, double-blind study. J Clin Psychiatry. 2009;70:540-549.
24. Carpenter LL, Yasmin S, Price LH. Double-blind, placebo-controlled study of antidepressant augmentation with mirtazapine. Biol Psychiatry. 2002;51:183-188.
25. Ozmenler NK, Karlidere T, Bozkurt A, et al. Mirtazapine augmentation in depressed patients with sexual dysfunction due to selective serotonin reuptake inhibitors. Hum Psychopharmacol. 2008;23:321-326.
26. Alpert JE, Mischoulon D, Rubenstein GE, et al. Folinic acid (Leucovorin) as an adjunctive treatment for SSRI-refractory depression. Ann Clin Psychiatry. 2002;14:33-38.
27. Alpert JE, Papakostas G, Mischoulon D, et al. S-adenosyl-Lmethionine (SAMe) as an adjunct for resistant major depressive disorder: an open trial following partial or nonresponse to selective serotonin reuptake inhibitors or venlafaxine. J Clin Psychopharmacol. 2004;24:661-664.
28. Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry. 2002;159:477-479.
29. Carney RM, Freedland KE, Rubin EH, et al. Depression in patients with coronary heart disease: a randomized controlled trial. JAMA. 2009;302:1651-1657.
30. Peet M, Horrobin DE. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry. 2002;59:913-919.
31. Mead GE, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database Syst Rev. 2009;(3):CD004366.-
32. Trivedi MH, Greer TL, Grannemann BD, et al. Exercise as an augmentation strategy for treatment of major depression. J Psychiatr Pract. 2006;12:205-213.
33. Trivedi MH, Greer TL, Grannemann BD, et al. TREAD: Treatment with Exercise Augmentation for Depression: study rationale and design. Clin Trials. 2006;3:291-305.
34. Thase ME, Friedman ES, Biggs MM, et al. Cognitive therapy versus medication in augmentation and switch strategies as second-step treatments: a STAR*D report. Am J Psychiatry. 2007;164:739-752.
35. Kocsis JH, Gelenberg AJ, Rothbaum BO, et al. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: the REVAMP Trial. Arch Gen Psychiatry. 2009;66:1178-1188.
36. Perry EB, Berman RM, Sanacora G, et al. Pindolol augmentation in depressed patients resistant to selective serotonin reuptake inhibitors: a double-blind, randomized, controlled trial. J Clin Psychiatry. 2004;65:238-243.
37. Rasmussen NA, Schrøder P, Olsen LR, et al. Modafi nil augmentation in depressed patients with partial response to antidepressants: a pilot study on self-reported symptoms covered by the Major Depression Inventory (MDI) and the Symptom Checklist (SCL-92). Nord J Psychiatry. 2005;59:173-178.
38. Santos MA, Rocha FL, Hara C. Efficacy and safety of antidepressant augmentation with lamotrigine in patients with treatment-resistant depression: a randomized, placebo-controlled, double-blind study. Prim Care Companion J Clin Psychiatry. 2008;10:187-190.
39. Dorée JP, Des Rosiers J, Lew V, et al. Quetiapine augmentation of treatment-resistant depression: a comparison with lithium. Curr Med Res Opin. 2007;23:333-341.
40. Lesser IM, Castro DB, Gaynes BN, et al. Ethnicity/race and outcome in the treatment of depression: results from STAR*D. Med Care. 2007;45:1043-1051.
41. Lesser IM, Leuchter AF, Trivedi MH, et al. Characteristics of insured and noninsured outpatients with depression in STAR(*) D. Psychiatr Serv. 2005;56:995-1004.
42. Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23:551-560.