User login
Telehealth exploded into the public consciousness this year as a way for clinicians and patients to safely connect during the COVID-19 crisis. While telehealth has been part of care delivery at Providence St. Joseph Health (PSJH) for more than a decade, it transitioned almost overnight from an offering most often focused on serving patients in rural areas to a way for any patient to get the care they need virtually whether in a hospital, outpatient facility, or from the comfort and safety of their own home.
Telehealth growth was fueled by changes in regulation and reimbursement during the public health emergency enabling providers to see new and established patients at home across all payer types. To put this growth into perspective, the large PSJH system averaged a few thousand video visits per month in January and February 2020. As COVID transmission spread and lockdowns began, that number climbed to over 15,000 video visits in March to a height of more than 150,000 video visits in May. As of the end of October 2020, PSJH has conducted more than 1.2 million video visits since the beginning of January, steadily accounting for 20%-25% of total visit volume.
Going virtual with gastroenterology
PSJH gastroenterology providers have been a part of this wave, conducting more than 12,000 video visits so far this year (as documented in our Epic EMR), which has been an entirely new method of care delivery for most of these clinicians. We also have many affiliated, private practice gastroenterology providers who practice in our facilities and transitioned quickly to video for outpatient care. Pre- and postprocedure follow-up visits were some of the most common visit types that went virtual, along with new patient visits to establish care and existing patient visits to check in on the status of a health condition, medication, or other concern. Complementary services for gastroenterology patients were transitioned to video over the past 8 months as well. Care management, nutrition services, online support groups, bariatric care information sessions, behavioral health, and more are now available for patients to access virtually.
Remembering it’s not about the tech
New technologies can be challenging to adopt – especially at a pace as rapid as it was this year. Fortunately for PSJH, we had inpatient and outpatient video platforms already in place and an experienced internal telehealth team to scale them quickly to providers and caregivers across system. But even with those advantages, it was still a huge challenge to transition so many providers and caregivers to video visits in such a short time without change management hurdles and bumps along the way.
Too often, there is an overemphasis placed on the technology. It’s a tool, and some technologies are better than others, and they continue to evolve over time. True success or failure lies in the clinical and operational work flows and how well the providers and care teams engage with and adapt them. We found that the providers and staff members willing to venture outside their comfort zone of “how we’ve always done it” and collaborate on the transition to virtual care had the best results. Openness and flexibility to trying new things and using temporary workarounds if existing functionality didn’t meet the need was key to transitioning quickly. Then, by listening to ideas from and sharing feedback among providers, clinics, and geographies, we were able to identify fixes and optimizations that needed to be made to improve the experience for all.
Selecting a video visit platform
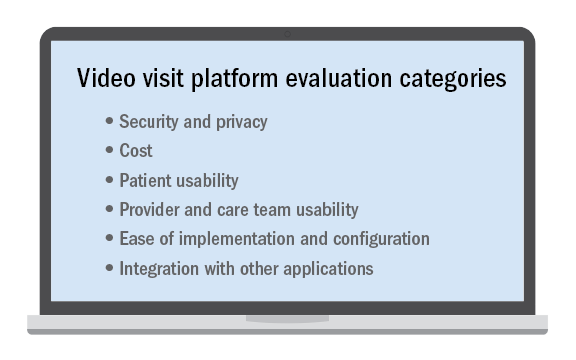
No telehealth platform is perfect and meets every patient, provider, and staff need or request despite what a technology vendor may claim. This is especially true in a large and/or diverse system with many different types of clinical use cases. Determining the “must-have” requirements from among those that may be important or simply nice to have is critical when selecting the video visit platform to use.
It’s not an easy decision and nearly impossible to please everyone. Ensuring that there are clinician, operator, and technical stakeholders all contributing to the requirements and decision-making is essential. While some may prefer a “best-of-breed” solution that does one thing very well, it may have to be paired with a set of other complimentary applications to meet all of the organization’s needs. Alternatively, there may be a platform with an expansive feature set but not all of the features are as strong as desired. Then there are solutions that integrate with your existing applications, which is a compelling option to consider.
Regardless of the tool chosen, best-practice work flows, easy-to-follow documentation, a mix of different training options, and internal technical help that responds quickly is key to implementing it successfully. And once implemented, optimization is an ongoing process to make it easier, faster, and better.
Looking ahead
As we came to the end of 2020, all providers and health systems were paying close attention to the Centers for Medicaid & Medicare Services and state-level regulations and reimbursement changes for 2021 to evaluate the impact on telehealth after the public health emergency and COVID-19 waivers are ended. Advocacy efforts are urging lawmakers to not lose the gains that were made during this time and have enabled millions of patients to access care more easily – changes which we believe they will now expect as an option going forward.
We at Providence believe telehealth’s future is a bright one, especially where value-based/managed care arrangements with payers are in place. In addition to integrating video visits and consults into normal clinical practice, we see further growth in serving patients at home with remote patient monitoring and other home-based programs that leverage connected devices and virtual tools. We also anticipate more providers will acquire licenses in other states to virtually care for patients who lack access to specialty services in their own community, which increases access where it is most needed. After 2020, we hope that telehealth will no longer be a specialized service only some patients can receive but a normal way of delivering care to all.
Ms. Winkelman is the system director of telehealth product development and delivery at Providence St. Joseph Health. Providence is the third-largest nonprofit health system in the United States with 51 hospitals, more than 800 clinics, and a comprehensive range of health and social services across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington.
Telehealth exploded into the public consciousness this year as a way for clinicians and patients to safely connect during the COVID-19 crisis. While telehealth has been part of care delivery at Providence St. Joseph Health (PSJH) for more than a decade, it transitioned almost overnight from an offering most often focused on serving patients in rural areas to a way for any patient to get the care they need virtually whether in a hospital, outpatient facility, or from the comfort and safety of their own home.
Telehealth growth was fueled by changes in regulation and reimbursement during the public health emergency enabling providers to see new and established patients at home across all payer types. To put this growth into perspective, the large PSJH system averaged a few thousand video visits per month in January and February 2020. As COVID transmission spread and lockdowns began, that number climbed to over 15,000 video visits in March to a height of more than 150,000 video visits in May. As of the end of October 2020, PSJH has conducted more than 1.2 million video visits since the beginning of January, steadily accounting for 20%-25% of total visit volume.
Going virtual with gastroenterology
PSJH gastroenterology providers have been a part of this wave, conducting more than 12,000 video visits so far this year (as documented in our Epic EMR), which has been an entirely new method of care delivery for most of these clinicians. We also have many affiliated, private practice gastroenterology providers who practice in our facilities and transitioned quickly to video for outpatient care. Pre- and postprocedure follow-up visits were some of the most common visit types that went virtual, along with new patient visits to establish care and existing patient visits to check in on the status of a health condition, medication, or other concern. Complementary services for gastroenterology patients were transitioned to video over the past 8 months as well. Care management, nutrition services, online support groups, bariatric care information sessions, behavioral health, and more are now available for patients to access virtually.
Remembering it’s not about the tech
New technologies can be challenging to adopt – especially at a pace as rapid as it was this year. Fortunately for PSJH, we had inpatient and outpatient video platforms already in place and an experienced internal telehealth team to scale them quickly to providers and caregivers across system. But even with those advantages, it was still a huge challenge to transition so many providers and caregivers to video visits in such a short time without change management hurdles and bumps along the way.
Too often, there is an overemphasis placed on the technology. It’s a tool, and some technologies are better than others, and they continue to evolve over time. True success or failure lies in the clinical and operational work flows and how well the providers and care teams engage with and adapt them. We found that the providers and staff members willing to venture outside their comfort zone of “how we’ve always done it” and collaborate on the transition to virtual care had the best results. Openness and flexibility to trying new things and using temporary workarounds if existing functionality didn’t meet the need was key to transitioning quickly. Then, by listening to ideas from and sharing feedback among providers, clinics, and geographies, we were able to identify fixes and optimizations that needed to be made to improve the experience for all.
Selecting a video visit platform
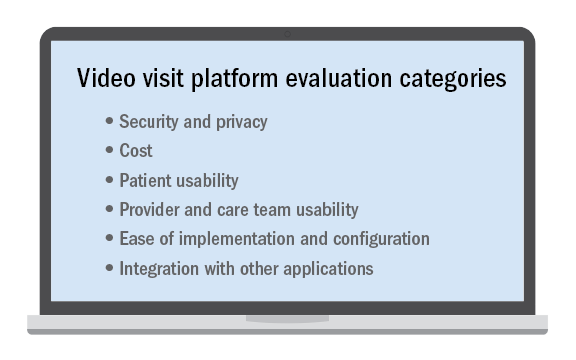
No telehealth platform is perfect and meets every patient, provider, and staff need or request despite what a technology vendor may claim. This is especially true in a large and/or diverse system with many different types of clinical use cases. Determining the “must-have” requirements from among those that may be important or simply nice to have is critical when selecting the video visit platform to use.
It’s not an easy decision and nearly impossible to please everyone. Ensuring that there are clinician, operator, and technical stakeholders all contributing to the requirements and decision-making is essential. While some may prefer a “best-of-breed” solution that does one thing very well, it may have to be paired with a set of other complimentary applications to meet all of the organization’s needs. Alternatively, there may be a platform with an expansive feature set but not all of the features are as strong as desired. Then there are solutions that integrate with your existing applications, which is a compelling option to consider.
Regardless of the tool chosen, best-practice work flows, easy-to-follow documentation, a mix of different training options, and internal technical help that responds quickly is key to implementing it successfully. And once implemented, optimization is an ongoing process to make it easier, faster, and better.
Looking ahead
As we came to the end of 2020, all providers and health systems were paying close attention to the Centers for Medicaid & Medicare Services and state-level regulations and reimbursement changes for 2021 to evaluate the impact on telehealth after the public health emergency and COVID-19 waivers are ended. Advocacy efforts are urging lawmakers to not lose the gains that were made during this time and have enabled millions of patients to access care more easily – changes which we believe they will now expect as an option going forward.
We at Providence believe telehealth’s future is a bright one, especially where value-based/managed care arrangements with payers are in place. In addition to integrating video visits and consults into normal clinical practice, we see further growth in serving patients at home with remote patient monitoring and other home-based programs that leverage connected devices and virtual tools. We also anticipate more providers will acquire licenses in other states to virtually care for patients who lack access to specialty services in their own community, which increases access where it is most needed. After 2020, we hope that telehealth will no longer be a specialized service only some patients can receive but a normal way of delivering care to all.
Ms. Winkelman is the system director of telehealth product development and delivery at Providence St. Joseph Health. Providence is the third-largest nonprofit health system in the United States with 51 hospitals, more than 800 clinics, and a comprehensive range of health and social services across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington.
Telehealth exploded into the public consciousness this year as a way for clinicians and patients to safely connect during the COVID-19 crisis. While telehealth has been part of care delivery at Providence St. Joseph Health (PSJH) for more than a decade, it transitioned almost overnight from an offering most often focused on serving patients in rural areas to a way for any patient to get the care they need virtually whether in a hospital, outpatient facility, or from the comfort and safety of their own home.
Telehealth growth was fueled by changes in regulation and reimbursement during the public health emergency enabling providers to see new and established patients at home across all payer types. To put this growth into perspective, the large PSJH system averaged a few thousand video visits per month in January and February 2020. As COVID transmission spread and lockdowns began, that number climbed to over 15,000 video visits in March to a height of more than 150,000 video visits in May. As of the end of October 2020, PSJH has conducted more than 1.2 million video visits since the beginning of January, steadily accounting for 20%-25% of total visit volume.
Going virtual with gastroenterology
PSJH gastroenterology providers have been a part of this wave, conducting more than 12,000 video visits so far this year (as documented in our Epic EMR), which has been an entirely new method of care delivery for most of these clinicians. We also have many affiliated, private practice gastroenterology providers who practice in our facilities and transitioned quickly to video for outpatient care. Pre- and postprocedure follow-up visits were some of the most common visit types that went virtual, along with new patient visits to establish care and existing patient visits to check in on the status of a health condition, medication, or other concern. Complementary services for gastroenterology patients were transitioned to video over the past 8 months as well. Care management, nutrition services, online support groups, bariatric care information sessions, behavioral health, and more are now available for patients to access virtually.
Remembering it’s not about the tech
New technologies can be challenging to adopt – especially at a pace as rapid as it was this year. Fortunately for PSJH, we had inpatient and outpatient video platforms already in place and an experienced internal telehealth team to scale them quickly to providers and caregivers across system. But even with those advantages, it was still a huge challenge to transition so many providers and caregivers to video visits in such a short time without change management hurdles and bumps along the way.
Too often, there is an overemphasis placed on the technology. It’s a tool, and some technologies are better than others, and they continue to evolve over time. True success or failure lies in the clinical and operational work flows and how well the providers and care teams engage with and adapt them. We found that the providers and staff members willing to venture outside their comfort zone of “how we’ve always done it” and collaborate on the transition to virtual care had the best results. Openness and flexibility to trying new things and using temporary workarounds if existing functionality didn’t meet the need was key to transitioning quickly. Then, by listening to ideas from and sharing feedback among providers, clinics, and geographies, we were able to identify fixes and optimizations that needed to be made to improve the experience for all.
Selecting a video visit platform
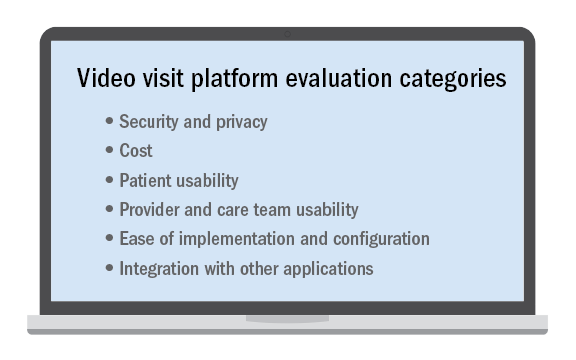
No telehealth platform is perfect and meets every patient, provider, and staff need or request despite what a technology vendor may claim. This is especially true in a large and/or diverse system with many different types of clinical use cases. Determining the “must-have” requirements from among those that may be important or simply nice to have is critical when selecting the video visit platform to use.
It’s not an easy decision and nearly impossible to please everyone. Ensuring that there are clinician, operator, and technical stakeholders all contributing to the requirements and decision-making is essential. While some may prefer a “best-of-breed” solution that does one thing very well, it may have to be paired with a set of other complimentary applications to meet all of the organization’s needs. Alternatively, there may be a platform with an expansive feature set but not all of the features are as strong as desired. Then there are solutions that integrate with your existing applications, which is a compelling option to consider.
Regardless of the tool chosen, best-practice work flows, easy-to-follow documentation, a mix of different training options, and internal technical help that responds quickly is key to implementing it successfully. And once implemented, optimization is an ongoing process to make it easier, faster, and better.
Looking ahead
As we came to the end of 2020, all providers and health systems were paying close attention to the Centers for Medicaid & Medicare Services and state-level regulations and reimbursement changes for 2021 to evaluate the impact on telehealth after the public health emergency and COVID-19 waivers are ended. Advocacy efforts are urging lawmakers to not lose the gains that were made during this time and have enabled millions of patients to access care more easily – changes which we believe they will now expect as an option going forward.
We at Providence believe telehealth’s future is a bright one, especially where value-based/managed care arrangements with payers are in place. In addition to integrating video visits and consults into normal clinical practice, we see further growth in serving patients at home with remote patient monitoring and other home-based programs that leverage connected devices and virtual tools. We also anticipate more providers will acquire licenses in other states to virtually care for patients who lack access to specialty services in their own community, which increases access where it is most needed. After 2020, we hope that telehealth will no longer be a specialized service only some patients can receive but a normal way of delivering care to all.
Ms. Winkelman is the system director of telehealth product development and delivery at Providence St. Joseph Health. Providence is the third-largest nonprofit health system in the United States with 51 hospitals, more than 800 clinics, and a comprehensive range of health and social services across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington.