User login
Removing barriers to high-value IBD care: Challenges and opportunities
Over the last several years, payer policies that dictate and restrict treatments for patients with inflammatory bowel diseases (IBD) have proliferated. The implementation of new coverage restrictions, expansion of services and procedures requiring prior authorization (PA), and dosing and access restriction to covered drugs, and the requirement of repeated treatment reviews including nonmedical switching for stable patients are widespread. The AGA administered a member needs assessment survey in December 2021 to determine the extent to which these policies harm patients and overburden gastroenterologists and their staff.
Survey findings
Most of the 100 surveyed members reported facing administrative burdens that prevented timely access to patient care. Utilization management practices such as PA, step therapy, and nonmedical switching and dosing restrictions create critical barriers to high quality GI care for patients with chronic conditions and jeopardize the physician-patient relationship. At a time when physicians have faced unprecedented challenges because of the public health emergency from the COVID-19 pandemic, these burdens also contribute to increasing physician burnout.
Prior authorization: Among AGA members, 96% of members said that PA is burdensome, with 61% indicating that it is significantly burdensome. Almost 99% of members indicated that PA has a negative impact on patients’ access to clinically appropriate treatments; 89% reported that the burden associated with PA has increased over the last 5 years in their practice.
Step therapy: Among members, 87% described the impact step therapy has on their practice as burdensome. Almost 90% of members said step therapy negatively impacted patients’ access to clinically appropriate treatments. Almost 90% of members felt that there was an overall negative impact on patient clinical outcomes for those patients who were required to follow a step therapy protocol.
Nonmedical switching and dosing restrictions: Out of all members, 86% reported an increase in nonmedical switching and dosing restrictions over the last 5 years; 79% of members noted that these restrictions had a negative impact on patient clinical outcomes.
An increasing number of insurance companies are restricting effective biologic therapy to Food and Drug Administration–labeled doses, in direct conflict with current established best practices. It is most concerning that many patients who had been stable on optimized dosing are suddenly notified that they will no longer be able to receive the dose or treatment frequency prescribed by their physician. The concept of optimizing drug therapy based on disease activity and therapeutic drug monitoring is well established, and artificial restrictions to FDA-labeled doses force unnecessary drug deescalation. This transparent effort to reduce costs lacks evidence for safety. Our sickest patients often require higher doses for induction in order to respond, given drug losses, yet some payers refuse to cover the doses these patients require. This new payer-centered effort prioritizes cost containment over the judgment of the treating physician. It causes direct patient harm risking efficacy or loss of response, and subsequent irreversible disease-related complications.
Medicare drug costs
Medicare patients receiving self-injectable or oral medications are not eligible for co-pay assistance programs through pharmaceutical companies because of federal rules. For non-Medicare patients, these programs reduce the co-pay costs to as low as $5 per month. Medicare patients are able to receive infusions like infliximab and vedolizumab at no cost. However, any self-injectable or oral agent can carry a co-pay of over $1,000. Other than for patients meeting income-based eligibility requirements (e.g., below the poverty line), these treatments become prohibitively expensive. Thousands of patients have had to discontinue their self-injectable and/or oral medications because of this cost or have been denied access to the therapy altogether because of cost.
Need for change
These recent changes in insurance policies have resulted in increased harm to our patients with IBD rather than improving the safety or quality of their care. These changes create barriers to disease treatment and have not improved quality of care, patient outcomes, or quality of life. The AGA and other societies have published multiple guidelines and literature on the management of patients with IBD that should serve as the foundation for insurers’ medication coverage policies. Additionally, insurance companies should seek input from panels of IBD experts when developing their medication coverage policies to ensure they are patient oriented and facilitate high-quality IBD care.
The following are opportunities for insurers to improve the IBD drug approval process:
- Simplify the appeal process.
- Guarantee rapid response/turnaround to appeal processes to avoid additional delays in care.
- Incorporate experienced expert review by a gastroenterologist.
- Ensure coverage of drug and disease monitoring.
- Integrate expert input in policy development.
Conclusion
Effective patient care in IBD, as well as in other chronic gastrointestinal diseases, requires a collaborative approach to maximize clinical outcomes. It is an exciting time in our field, with rapidly expanding therapeutic options to treat IBD that have the potential to modify the disease course and prevent long-term complications for patients. However, optimizing the use of these treatments to achieve disease remission is challenging and requires the ability to individualize the timely choice of medications at the right dose for each patient to capture and monitor response. The ability to provide individualized, data driven care is essential to improving the quality of life of our patients, as well as to reducing health care spending over time.
Achieving high-value care is a goal that benefits everyone involved in the health care system. Policies that interfere with the timely treatment of sick patients with the right therapies, optimized to achieve disease remission, hurt the very patients that our health care system exists to serve. We cannot stand by while impediments to treatment result in harm to our patients and worsen clinical outcomes. Collaboratively developing aligned incentives can lead us to patient-centered policies that fulfill a shared purpose to optimize the health of people with chronic digestive diseases.
The authors reported having no relevant conflicts of interest.
Dr. Feuerstein is with the Center for Inflammatory Bowel Disease at Beth Israel Deaconess Medical Center and is an associate professor of medicine Harvard Medical School, both in Boston. Dr. Sofia is an assistant professor of medicine with the division of gastroenterology and hepatology at Oregon Health and Science University, Portland. Dr. Guha is a professor of medicine at the division of gastroenterology, hepatology and nutrition and is codirector of the Center for Interventional Gastroenterology at UTHealth (iGUT) at UT Health Science Center, Houston. Dr. Streett is a clinical professor of medicine, gastroenterology, and hepatology and director of the IBD Education and Advanced IBD Fellowship at Stanford (Calif.) Medicine.
Over the last several years, payer policies that dictate and restrict treatments for patients with inflammatory bowel diseases (IBD) have proliferated. The implementation of new coverage restrictions, expansion of services and procedures requiring prior authorization (PA), and dosing and access restriction to covered drugs, and the requirement of repeated treatment reviews including nonmedical switching for stable patients are widespread. The AGA administered a member needs assessment survey in December 2021 to determine the extent to which these policies harm patients and overburden gastroenterologists and their staff.
Survey findings
Most of the 100 surveyed members reported facing administrative burdens that prevented timely access to patient care. Utilization management practices such as PA, step therapy, and nonmedical switching and dosing restrictions create critical barriers to high quality GI care for patients with chronic conditions and jeopardize the physician-patient relationship. At a time when physicians have faced unprecedented challenges because of the public health emergency from the COVID-19 pandemic, these burdens also contribute to increasing physician burnout.
Prior authorization: Among AGA members, 96% of members said that PA is burdensome, with 61% indicating that it is significantly burdensome. Almost 99% of members indicated that PA has a negative impact on patients’ access to clinically appropriate treatments; 89% reported that the burden associated with PA has increased over the last 5 years in their practice.
Step therapy: Among members, 87% described the impact step therapy has on their practice as burdensome. Almost 90% of members said step therapy negatively impacted patients’ access to clinically appropriate treatments. Almost 90% of members felt that there was an overall negative impact on patient clinical outcomes for those patients who were required to follow a step therapy protocol.
Nonmedical switching and dosing restrictions: Out of all members, 86% reported an increase in nonmedical switching and dosing restrictions over the last 5 years; 79% of members noted that these restrictions had a negative impact on patient clinical outcomes.
An increasing number of insurance companies are restricting effective biologic therapy to Food and Drug Administration–labeled doses, in direct conflict with current established best practices. It is most concerning that many patients who had been stable on optimized dosing are suddenly notified that they will no longer be able to receive the dose or treatment frequency prescribed by their physician. The concept of optimizing drug therapy based on disease activity and therapeutic drug monitoring is well established, and artificial restrictions to FDA-labeled doses force unnecessary drug deescalation. This transparent effort to reduce costs lacks evidence for safety. Our sickest patients often require higher doses for induction in order to respond, given drug losses, yet some payers refuse to cover the doses these patients require. This new payer-centered effort prioritizes cost containment over the judgment of the treating physician. It causes direct patient harm risking efficacy or loss of response, and subsequent irreversible disease-related complications.
Medicare drug costs
Medicare patients receiving self-injectable or oral medications are not eligible for co-pay assistance programs through pharmaceutical companies because of federal rules. For non-Medicare patients, these programs reduce the co-pay costs to as low as $5 per month. Medicare patients are able to receive infusions like infliximab and vedolizumab at no cost. However, any self-injectable or oral agent can carry a co-pay of over $1,000. Other than for patients meeting income-based eligibility requirements (e.g., below the poverty line), these treatments become prohibitively expensive. Thousands of patients have had to discontinue their self-injectable and/or oral medications because of this cost or have been denied access to the therapy altogether because of cost.
Need for change
These recent changes in insurance policies have resulted in increased harm to our patients with IBD rather than improving the safety or quality of their care. These changes create barriers to disease treatment and have not improved quality of care, patient outcomes, or quality of life. The AGA and other societies have published multiple guidelines and literature on the management of patients with IBD that should serve as the foundation for insurers’ medication coverage policies. Additionally, insurance companies should seek input from panels of IBD experts when developing their medication coverage policies to ensure they are patient oriented and facilitate high-quality IBD care.
The following are opportunities for insurers to improve the IBD drug approval process:
- Simplify the appeal process.
- Guarantee rapid response/turnaround to appeal processes to avoid additional delays in care.
- Incorporate experienced expert review by a gastroenterologist.
- Ensure coverage of drug and disease monitoring.
- Integrate expert input in policy development.
Conclusion
Effective patient care in IBD, as well as in other chronic gastrointestinal diseases, requires a collaborative approach to maximize clinical outcomes. It is an exciting time in our field, with rapidly expanding therapeutic options to treat IBD that have the potential to modify the disease course and prevent long-term complications for patients. However, optimizing the use of these treatments to achieve disease remission is challenging and requires the ability to individualize the timely choice of medications at the right dose for each patient to capture and monitor response. The ability to provide individualized, data driven care is essential to improving the quality of life of our patients, as well as to reducing health care spending over time.
Achieving high-value care is a goal that benefits everyone involved in the health care system. Policies that interfere with the timely treatment of sick patients with the right therapies, optimized to achieve disease remission, hurt the very patients that our health care system exists to serve. We cannot stand by while impediments to treatment result in harm to our patients and worsen clinical outcomes. Collaboratively developing aligned incentives can lead us to patient-centered policies that fulfill a shared purpose to optimize the health of people with chronic digestive diseases.
The authors reported having no relevant conflicts of interest.
Dr. Feuerstein is with the Center for Inflammatory Bowel Disease at Beth Israel Deaconess Medical Center and is an associate professor of medicine Harvard Medical School, both in Boston. Dr. Sofia is an assistant professor of medicine with the division of gastroenterology and hepatology at Oregon Health and Science University, Portland. Dr. Guha is a professor of medicine at the division of gastroenterology, hepatology and nutrition and is codirector of the Center for Interventional Gastroenterology at UTHealth (iGUT) at UT Health Science Center, Houston. Dr. Streett is a clinical professor of medicine, gastroenterology, and hepatology and director of the IBD Education and Advanced IBD Fellowship at Stanford (Calif.) Medicine.
Over the last several years, payer policies that dictate and restrict treatments for patients with inflammatory bowel diseases (IBD) have proliferated. The implementation of new coverage restrictions, expansion of services and procedures requiring prior authorization (PA), and dosing and access restriction to covered drugs, and the requirement of repeated treatment reviews including nonmedical switching for stable patients are widespread. The AGA administered a member needs assessment survey in December 2021 to determine the extent to which these policies harm patients and overburden gastroenterologists and their staff.
Survey findings
Most of the 100 surveyed members reported facing administrative burdens that prevented timely access to patient care. Utilization management practices such as PA, step therapy, and nonmedical switching and dosing restrictions create critical barriers to high quality GI care for patients with chronic conditions and jeopardize the physician-patient relationship. At a time when physicians have faced unprecedented challenges because of the public health emergency from the COVID-19 pandemic, these burdens also contribute to increasing physician burnout.
Prior authorization: Among AGA members, 96% of members said that PA is burdensome, with 61% indicating that it is significantly burdensome. Almost 99% of members indicated that PA has a negative impact on patients’ access to clinically appropriate treatments; 89% reported that the burden associated with PA has increased over the last 5 years in their practice.
Step therapy: Among members, 87% described the impact step therapy has on their practice as burdensome. Almost 90% of members said step therapy negatively impacted patients’ access to clinically appropriate treatments. Almost 90% of members felt that there was an overall negative impact on patient clinical outcomes for those patients who were required to follow a step therapy protocol.
Nonmedical switching and dosing restrictions: Out of all members, 86% reported an increase in nonmedical switching and dosing restrictions over the last 5 years; 79% of members noted that these restrictions had a negative impact on patient clinical outcomes.
An increasing number of insurance companies are restricting effective biologic therapy to Food and Drug Administration–labeled doses, in direct conflict with current established best practices. It is most concerning that many patients who had been stable on optimized dosing are suddenly notified that they will no longer be able to receive the dose or treatment frequency prescribed by their physician. The concept of optimizing drug therapy based on disease activity and therapeutic drug monitoring is well established, and artificial restrictions to FDA-labeled doses force unnecessary drug deescalation. This transparent effort to reduce costs lacks evidence for safety. Our sickest patients often require higher doses for induction in order to respond, given drug losses, yet some payers refuse to cover the doses these patients require. This new payer-centered effort prioritizes cost containment over the judgment of the treating physician. It causes direct patient harm risking efficacy or loss of response, and subsequent irreversible disease-related complications.
Medicare drug costs
Medicare patients receiving self-injectable or oral medications are not eligible for co-pay assistance programs through pharmaceutical companies because of federal rules. For non-Medicare patients, these programs reduce the co-pay costs to as low as $5 per month. Medicare patients are able to receive infusions like infliximab and vedolizumab at no cost. However, any self-injectable or oral agent can carry a co-pay of over $1,000. Other than for patients meeting income-based eligibility requirements (e.g., below the poverty line), these treatments become prohibitively expensive. Thousands of patients have had to discontinue their self-injectable and/or oral medications because of this cost or have been denied access to the therapy altogether because of cost.
Need for change
These recent changes in insurance policies have resulted in increased harm to our patients with IBD rather than improving the safety or quality of their care. These changes create barriers to disease treatment and have not improved quality of care, patient outcomes, or quality of life. The AGA and other societies have published multiple guidelines and literature on the management of patients with IBD that should serve as the foundation for insurers’ medication coverage policies. Additionally, insurance companies should seek input from panels of IBD experts when developing their medication coverage policies to ensure they are patient oriented and facilitate high-quality IBD care.
The following are opportunities for insurers to improve the IBD drug approval process:
- Simplify the appeal process.
- Guarantee rapid response/turnaround to appeal processes to avoid additional delays in care.
- Incorporate experienced expert review by a gastroenterologist.
- Ensure coverage of drug and disease monitoring.
- Integrate expert input in policy development.
Conclusion
Effective patient care in IBD, as well as in other chronic gastrointestinal diseases, requires a collaborative approach to maximize clinical outcomes. It is an exciting time in our field, with rapidly expanding therapeutic options to treat IBD that have the potential to modify the disease course and prevent long-term complications for patients. However, optimizing the use of these treatments to achieve disease remission is challenging and requires the ability to individualize the timely choice of medications at the right dose for each patient to capture and monitor response. The ability to provide individualized, data driven care is essential to improving the quality of life of our patients, as well as to reducing health care spending over time.
Achieving high-value care is a goal that benefits everyone involved in the health care system. Policies that interfere with the timely treatment of sick patients with the right therapies, optimized to achieve disease remission, hurt the very patients that our health care system exists to serve. We cannot stand by while impediments to treatment result in harm to our patients and worsen clinical outcomes. Collaboratively developing aligned incentives can lead us to patient-centered policies that fulfill a shared purpose to optimize the health of people with chronic digestive diseases.
The authors reported having no relevant conflicts of interest.
Dr. Feuerstein is with the Center for Inflammatory Bowel Disease at Beth Israel Deaconess Medical Center and is an associate professor of medicine Harvard Medical School, both in Boston. Dr. Sofia is an assistant professor of medicine with the division of gastroenterology and hepatology at Oregon Health and Science University, Portland. Dr. Guha is a professor of medicine at the division of gastroenterology, hepatology and nutrition and is codirector of the Center for Interventional Gastroenterology at UTHealth (iGUT) at UT Health Science Center, Houston. Dr. Streett is a clinical professor of medicine, gastroenterology, and hepatology and director of the IBD Education and Advanced IBD Fellowship at Stanford (Calif.) Medicine.
AGA helps break down barriers to CRC screening
The new year has already marked major progress for colorectal cancer (CRC) screening with the implementation of the Removing Barriers to Colorectal Cancer Screening Act by the Centers for Medicare & Medicaid Services, which will protect Medicare beneficiaries from an unexpected bill if a polyp is detected and removed during a screening colonoscopy, as well as new guidance from the federal government requiring private insurers to cover colonoscopy as a follow-up to a noninvasive CRC screening test without imposing cost sharing for patients.
The American Gastroenterological Association is strongly committed to reducing the incidence of and mortality from colorectal cancer. There is strong evidence that CRC screening is effective, but only 65% of eligible individuals have been screened. A. Mark Fendrick, MD, and colleagues recently found that cost sharing for CRC screening occurred in 48.2% of patients with commercial insurance and 77.9% of patients with Medicare coverage. The elimination of these barriers to CRC screening should improve adherence and reduce the burden of CRC.
As one of AGA President John M. Inadomi’s initiatives, the AGA created the CRC Screening Continuum Executive Committee in 2021 to develop AGA Position Statements that highlight the continuum of CRC screening and identify barriers, as well as work with stakeholders to eliminate known barriers. Chaired by former AGA President, David Lieberman, MD, AGAF, and with public policy guidance from Kathleen Teixeira, AGA Vice President of Public Policy and Government Affairs at the AGA, the committee identified that, at that time, colonoscopies after positive stool tests had often been considered “diagnostic” and, therefore, were not covered in full the way a preventive screening is required to be covered by the Affordable Care Act (ACA). The committee recognized that copays and deductibles are barriers to CRC screening and contribute to health inequity and socio-economic disparities. Noninvasive screening should be considered a part of programs with multiple steps, all of which – including follow-up colonoscopy if the test is positive – should be covered by payers without cost sharing as part of the screening continuum. Further, screening with high-quality colonoscopy should be covered by payers without cost sharing, consistent with the aims of the ACA. The committee recommended that the full cost of screening, including the bowel prep, facility and professional fees, anesthesia, and pathology, should be covered by payers without cost sharing.
Over the past decade, the AGA and other organizations have spent countless hours advocating for closing the gap. In September 2021, Dr. Inadomi and Dr. Lieberman, along with the American Cancer Society Cancer Action Network and Fight CRC, met with Assistant Secretary of Labor, Ali Khawar, and representatives from the U.S. Department of Health & Human Services and U.S. Department of Treasury to request they direct private health plans to cover colonoscopy after a positive noninvasive CRC screening. In January 2022, guidance from the United States Department of Labor, HHS, and the USDT clarified that private insurance plans must cover follow-up colonoscopies after a positive noninvasive stool test. In the Frequently Asked Questions (FAQs) about the Affordable Care Act Implementation, Part 51, the departments affirmed that a plan or issuer must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive noninvasive stool-based screening test or direct visualization screening test for colorectal cancer for individuals described in a U.S. Preventive Services Task Force (USPSTF) recommendation from May 18, 2021. As stated in that USPSTF recommendation, the follow-up colonoscopy is an integral part of the preventive screening without which the screening would not be complete . The follow-up colonoscopy after a positive noninvasive stool-based screening test or direct visualization screening test is therefore required to be covered without cost sharing in accordance with the requirements of Public Health Service Act section 2713 and its implementing regulations.
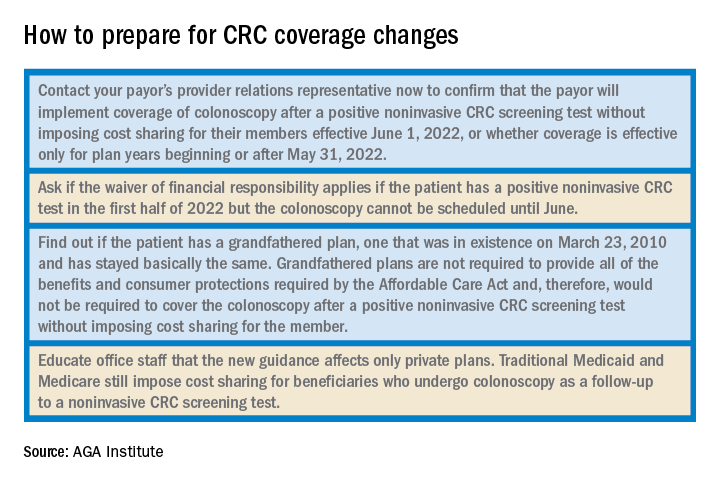
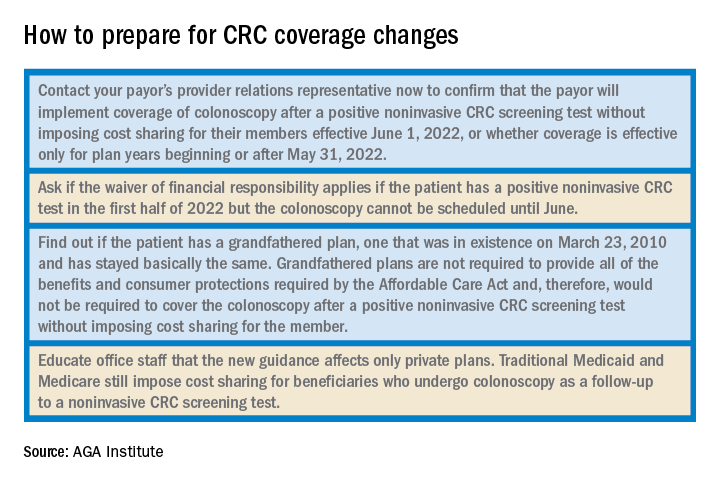
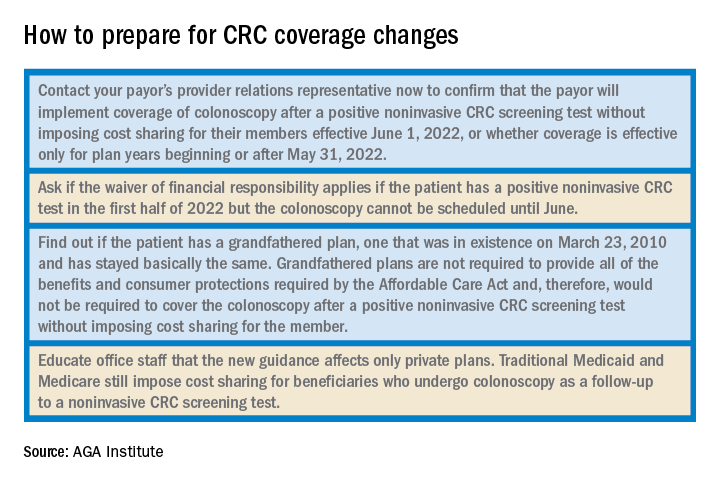
Plans and issuers must provide coverage without cost sharing for plan or policy years beginning on or after May 31, 2022. While this new guidance will expand coverage of follow-up colonoscopies to many more individuals nationwide, including individuals who have coverage through Medicaid expansion, it does not apply to traditional Medicaid and Medicare plans.
The members of the CRC Screening Continuum Executive Committee includes Dr. Brill and Lieberman, as well as Uri Ladabaum, MD; Larry Kim, MD; Folasade May, MD, PhD, MPhil; Caitlin Murphy, MD; and Richard Wender, MD. Disclosures are on file with the AGA National Office.
Dr. Brill is chief medical officer, Predictive Health, Phoenix. Dr. Lieberman is professor of medicine, division of gastroenterology and hepatology, Oregon Health & Science University, Portland, as well as a past president of the AGA. Dr. Brill discloses consulting for Accomplish Health, Alimetry, Allara Health, AnX Robotica, Arch Therapeutics, Biotax, Boomerang Medical, Brightline, Calyx, Capsovision, Check Cap, Clexio, Curology, Docbot, Echosens, Endogastric Solutions, evoEndo, Family First, FDNA, Food Marble, Freespira, Gala Therapeutics, Glaukos, gTech Medical, Gynesonics, Hbox, Hello Heart, HyGIeaCare, Innovative Health Solutions, IronRod Health, Johnson & Johnson, Lantheus, LeMinou, Lumen, Mainstay Medical, MaternaMed, Medtronic, Mightier, Motus GI, OncoSil Medical, Palette Life Sciences, Perry Health, Perspectum, Red Ventures, Reflexion, Respira Labs, Salaso, Smith+Nephew, SonarMD, Stage Zero Life Sciences, Steris, Sword Health, Tabula Rosa Health Care, Ultrasight, Vertos Medical, WL Gore, and holds options/warrants in Accomplish Health, AnX Robotica, Capsovision, Donsini Health, Hbox, Hello Heart, HyGIeaCare, Restech, Perry Health, StageZero Life Sciences, SonarMD. Dr. Lieberman is a consultant to Geneoscopy.
The new year has already marked major progress for colorectal cancer (CRC) screening with the implementation of the Removing Barriers to Colorectal Cancer Screening Act by the Centers for Medicare & Medicaid Services, which will protect Medicare beneficiaries from an unexpected bill if a polyp is detected and removed during a screening colonoscopy, as well as new guidance from the federal government requiring private insurers to cover colonoscopy as a follow-up to a noninvasive CRC screening test without imposing cost sharing for patients.
The American Gastroenterological Association is strongly committed to reducing the incidence of and mortality from colorectal cancer. There is strong evidence that CRC screening is effective, but only 65% of eligible individuals have been screened. A. Mark Fendrick, MD, and colleagues recently found that cost sharing for CRC screening occurred in 48.2% of patients with commercial insurance and 77.9% of patients with Medicare coverage. The elimination of these barriers to CRC screening should improve adherence and reduce the burden of CRC.
As one of AGA President John M. Inadomi’s initiatives, the AGA created the CRC Screening Continuum Executive Committee in 2021 to develop AGA Position Statements that highlight the continuum of CRC screening and identify barriers, as well as work with stakeholders to eliminate known barriers. Chaired by former AGA President, David Lieberman, MD, AGAF, and with public policy guidance from Kathleen Teixeira, AGA Vice President of Public Policy and Government Affairs at the AGA, the committee identified that, at that time, colonoscopies after positive stool tests had often been considered “diagnostic” and, therefore, were not covered in full the way a preventive screening is required to be covered by the Affordable Care Act (ACA). The committee recognized that copays and deductibles are barriers to CRC screening and contribute to health inequity and socio-economic disparities. Noninvasive screening should be considered a part of programs with multiple steps, all of which – including follow-up colonoscopy if the test is positive – should be covered by payers without cost sharing as part of the screening continuum. Further, screening with high-quality colonoscopy should be covered by payers without cost sharing, consistent with the aims of the ACA. The committee recommended that the full cost of screening, including the bowel prep, facility and professional fees, anesthesia, and pathology, should be covered by payers without cost sharing.
Over the past decade, the AGA and other organizations have spent countless hours advocating for closing the gap. In September 2021, Dr. Inadomi and Dr. Lieberman, along with the American Cancer Society Cancer Action Network and Fight CRC, met with Assistant Secretary of Labor, Ali Khawar, and representatives from the U.S. Department of Health & Human Services and U.S. Department of Treasury to request they direct private health plans to cover colonoscopy after a positive noninvasive CRC screening. In January 2022, guidance from the United States Department of Labor, HHS, and the USDT clarified that private insurance plans must cover follow-up colonoscopies after a positive noninvasive stool test. In the Frequently Asked Questions (FAQs) about the Affordable Care Act Implementation, Part 51, the departments affirmed that a plan or issuer must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive noninvasive stool-based screening test or direct visualization screening test for colorectal cancer for individuals described in a U.S. Preventive Services Task Force (USPSTF) recommendation from May 18, 2021. As stated in that USPSTF recommendation, the follow-up colonoscopy is an integral part of the preventive screening without which the screening would not be complete . The follow-up colonoscopy after a positive noninvasive stool-based screening test or direct visualization screening test is therefore required to be covered without cost sharing in accordance with the requirements of Public Health Service Act section 2713 and its implementing regulations.
Plans and issuers must provide coverage without cost sharing for plan or policy years beginning on or after May 31, 2022. While this new guidance will expand coverage of follow-up colonoscopies to many more individuals nationwide, including individuals who have coverage through Medicaid expansion, it does not apply to traditional Medicaid and Medicare plans.
The members of the CRC Screening Continuum Executive Committee includes Dr. Brill and Lieberman, as well as Uri Ladabaum, MD; Larry Kim, MD; Folasade May, MD, PhD, MPhil; Caitlin Murphy, MD; and Richard Wender, MD. Disclosures are on file with the AGA National Office.
Dr. Brill is chief medical officer, Predictive Health, Phoenix. Dr. Lieberman is professor of medicine, division of gastroenterology and hepatology, Oregon Health & Science University, Portland, as well as a past president of the AGA. Dr. Brill discloses consulting for Accomplish Health, Alimetry, Allara Health, AnX Robotica, Arch Therapeutics, Biotax, Boomerang Medical, Brightline, Calyx, Capsovision, Check Cap, Clexio, Curology, Docbot, Echosens, Endogastric Solutions, evoEndo, Family First, FDNA, Food Marble, Freespira, Gala Therapeutics, Glaukos, gTech Medical, Gynesonics, Hbox, Hello Heart, HyGIeaCare, Innovative Health Solutions, IronRod Health, Johnson & Johnson, Lantheus, LeMinou, Lumen, Mainstay Medical, MaternaMed, Medtronic, Mightier, Motus GI, OncoSil Medical, Palette Life Sciences, Perry Health, Perspectum, Red Ventures, Reflexion, Respira Labs, Salaso, Smith+Nephew, SonarMD, Stage Zero Life Sciences, Steris, Sword Health, Tabula Rosa Health Care, Ultrasight, Vertos Medical, WL Gore, and holds options/warrants in Accomplish Health, AnX Robotica, Capsovision, Donsini Health, Hbox, Hello Heart, HyGIeaCare, Restech, Perry Health, StageZero Life Sciences, SonarMD. Dr. Lieberman is a consultant to Geneoscopy.
The new year has already marked major progress for colorectal cancer (CRC) screening with the implementation of the Removing Barriers to Colorectal Cancer Screening Act by the Centers for Medicare & Medicaid Services, which will protect Medicare beneficiaries from an unexpected bill if a polyp is detected and removed during a screening colonoscopy, as well as new guidance from the federal government requiring private insurers to cover colonoscopy as a follow-up to a noninvasive CRC screening test without imposing cost sharing for patients.
The American Gastroenterological Association is strongly committed to reducing the incidence of and mortality from colorectal cancer. There is strong evidence that CRC screening is effective, but only 65% of eligible individuals have been screened. A. Mark Fendrick, MD, and colleagues recently found that cost sharing for CRC screening occurred in 48.2% of patients with commercial insurance and 77.9% of patients with Medicare coverage. The elimination of these barriers to CRC screening should improve adherence and reduce the burden of CRC.
As one of AGA President John M. Inadomi’s initiatives, the AGA created the CRC Screening Continuum Executive Committee in 2021 to develop AGA Position Statements that highlight the continuum of CRC screening and identify barriers, as well as work with stakeholders to eliminate known barriers. Chaired by former AGA President, David Lieberman, MD, AGAF, and with public policy guidance from Kathleen Teixeira, AGA Vice President of Public Policy and Government Affairs at the AGA, the committee identified that, at that time, colonoscopies after positive stool tests had often been considered “diagnostic” and, therefore, were not covered in full the way a preventive screening is required to be covered by the Affordable Care Act (ACA). The committee recognized that copays and deductibles are barriers to CRC screening and contribute to health inequity and socio-economic disparities. Noninvasive screening should be considered a part of programs with multiple steps, all of which – including follow-up colonoscopy if the test is positive – should be covered by payers without cost sharing as part of the screening continuum. Further, screening with high-quality colonoscopy should be covered by payers without cost sharing, consistent with the aims of the ACA. The committee recommended that the full cost of screening, including the bowel prep, facility and professional fees, anesthesia, and pathology, should be covered by payers without cost sharing.
Over the past decade, the AGA and other organizations have spent countless hours advocating for closing the gap. In September 2021, Dr. Inadomi and Dr. Lieberman, along with the American Cancer Society Cancer Action Network and Fight CRC, met with Assistant Secretary of Labor, Ali Khawar, and representatives from the U.S. Department of Health & Human Services and U.S. Department of Treasury to request they direct private health plans to cover colonoscopy after a positive noninvasive CRC screening. In January 2022, guidance from the United States Department of Labor, HHS, and the USDT clarified that private insurance plans must cover follow-up colonoscopies after a positive noninvasive stool test. In the Frequently Asked Questions (FAQs) about the Affordable Care Act Implementation, Part 51, the departments affirmed that a plan or issuer must cover and may not impose cost sharing with respect to a colonoscopy conducted after a positive noninvasive stool-based screening test or direct visualization screening test for colorectal cancer for individuals described in a U.S. Preventive Services Task Force (USPSTF) recommendation from May 18, 2021. As stated in that USPSTF recommendation, the follow-up colonoscopy is an integral part of the preventive screening without which the screening would not be complete . The follow-up colonoscopy after a positive noninvasive stool-based screening test or direct visualization screening test is therefore required to be covered without cost sharing in accordance with the requirements of Public Health Service Act section 2713 and its implementing regulations.
Plans and issuers must provide coverage without cost sharing for plan or policy years beginning on or after May 31, 2022. While this new guidance will expand coverage of follow-up colonoscopies to many more individuals nationwide, including individuals who have coverage through Medicaid expansion, it does not apply to traditional Medicaid and Medicare plans.
The members of the CRC Screening Continuum Executive Committee includes Dr. Brill and Lieberman, as well as Uri Ladabaum, MD; Larry Kim, MD; Folasade May, MD, PhD, MPhil; Caitlin Murphy, MD; and Richard Wender, MD. Disclosures are on file with the AGA National Office.
Dr. Brill is chief medical officer, Predictive Health, Phoenix. Dr. Lieberman is professor of medicine, division of gastroenterology and hepatology, Oregon Health & Science University, Portland, as well as a past president of the AGA. Dr. Brill discloses consulting for Accomplish Health, Alimetry, Allara Health, AnX Robotica, Arch Therapeutics, Biotax, Boomerang Medical, Brightline, Calyx, Capsovision, Check Cap, Clexio, Curology, Docbot, Echosens, Endogastric Solutions, evoEndo, Family First, FDNA, Food Marble, Freespira, Gala Therapeutics, Glaukos, gTech Medical, Gynesonics, Hbox, Hello Heart, HyGIeaCare, Innovative Health Solutions, IronRod Health, Johnson & Johnson, Lantheus, LeMinou, Lumen, Mainstay Medical, MaternaMed, Medtronic, Mightier, Motus GI, OncoSil Medical, Palette Life Sciences, Perry Health, Perspectum, Red Ventures, Reflexion, Respira Labs, Salaso, Smith+Nephew, SonarMD, Stage Zero Life Sciences, Steris, Sword Health, Tabula Rosa Health Care, Ultrasight, Vertos Medical, WL Gore, and holds options/warrants in Accomplish Health, AnX Robotica, Capsovision, Donsini Health, Hbox, Hello Heart, HyGIeaCare, Restech, Perry Health, StageZero Life Sciences, SonarMD. Dr. Lieberman is a consultant to Geneoscopy.
Quality measurement in gastroenterology: A vision for the future
Modern efforts to monitor and improve quality in health care can trace their roots to the early 20th century. At that time, hospitals initiated mechanisms to ensure standard practices for privileging clinicians, reporting medical records and clinical data, and establishing supervised diagnostic facilities. Years later, Avedis Donabedian published “Evaluating the Quality of Medical Care,” which outlined how health care should be measured across three areas – structure, process, and outcome – and became a foundational rubric for assessing quality in medicine.
Over the ensuing decades, with the rise of professional society guidelines and increasing government involvement in the reimbursement of health care, establishing benchmarks and tracking clinical performance has become increasingly important. The passage of the Affordable Care Act subsequently established a formal, legislative mandate for assessing clinical quality tied to reimbursement. Although the context, consequences, and details for reporting have evolved, quality tracking is now firmly entrenched across clinical practice, including gastroenterology. One such mechanism for this is the Merit-Based Incentive Payment System (MIPS), which is a quality payment program (QPP) administered by the Centers for Medicare & Medicaid Services. Today, both government and private payers are assessing measurements and improvements of quality to satisfy the Quintuple Aim of achieving better health outcomes, seeking efficient cost of care, improving patient experience, improving provider experience, and enhancing equity through the reduction health inequalities.
As we transition from a fee-based to a value-based care model, several important developments relevant to the practicing gastroenterologist are likely to occur as the broader landscape of quality reporting will continue shifting. This article will outline a vision of the future in quality measurement for gastroenterology.
Gastroenterologists have relatively few specialty-specific measures on which to report. The widespread use of the adenoma detection rate for screening colonoscopy does represent a success in quality improvement because it is easily calculated, is reproducible, and has been consistently associated with clinical outcomes. But the overall measure set is limited to screening colonoscopy and the management of viral hepatitis, meaning large areas of our practice are not included in this set. Developing new metrics related to broader areas of practice will be necessary to address this current shortcoming and increase the impact of quality programs to clinicians. Indeed, a recent environmental scan performed by the Core Quality Measures Collaborative, a public-private coalition of leaders working to facilitate measure alignment, proposed future areas for development, including gastroesophageal reflux disease, nonalcoholic fatty liver disease, and medication management.
The American Gastroenterological Association, through its defined process of guideline-to-measure development, has responded by creating metrics for the management of acute pancreatitis, Lynch syndrome testing, and eradicating Helicobacter pylori in the context of gastric intestinal metaplasia; additionally, previously defined measures exist for Barrett’s esophagus and inflammatory bowel disease. Therefore, gastroenterologists can expect to report on an expanding collection of measures in the future.
However, recognizing that not all measures may be equally applicable across populations and acknowledging the importance of risk adjustment, incorporating at least an assessment for risk stratification in their future development is vital. Specifically, social risk factors will need to be accounted for during development in ways that might include risk adjustment or stratification by groups. Increasing data demonstrate that clinician performance can vary by population served and that social determinants of health (SDoH) should be incorporated into an assessment of outcomes. Risk stratification may allow clinicians or practices to report outcomes by group without jeopardy of incurring performance-based penalties. However, the ultimate goal should be reducing inequities and closing care gaps rather than inadvertently lowering the bar for clinicians who primarily treat disenfranchised populations. Eventually, any new measures aiming to be included in a QPP require formal validity testing, which can delay their inclusion in such a set. Yet including stratification in their development will provide a more robust and accurate assessment of quality of care delivered according to one’s catchment and help serve to minimize the effects of SDoH.
Another way that quality measurement may account for a more comprehensive assessment of care delivered is by bundling similarly provided services, even those across multiple specialties. Such a future model is the MIPS Value Pathways, currently under development by CMS. While the exact make-up and reporting structure remains to be determined, a group of related metrics – for example, for colonic health – would likely be grouped together. This model might include an evaluation of a practice’s performance in screening colonoscopy, Lynch testing practices, and inflammatory bowel disease management, which could also be relevant to surgeons, pathologists, and oncologists. This paradigm could serve to increase quality alignment across specialties and reinforce a commitment toward improving care delivery and fulfill a value-based mandate.
Within this framework, though, a shared challenge across specialties exists for the capture and reporting of clinical data. The financial and time costs for quality reporting are well documented, therefore any future vision of quality must address means to ease this reporting burden. Accounting for this would be especially impactful to independent as well as small- to moderate-sized practices, which must provide their own resources for collecting and reporting, with the QPP payment adjustments often insufficient to replace lost revenue or expenses. Some administrative relief has been provided by CMS during the current COVID-19 pandemic, but this focused on allowing select clinicians to avoid reporting rather than addressing the fundamental challenges presented by extracting and documenting quality measures. Moving forward, an increasing emphasis will likely be on the use of artificial intelligence (AI), such as natural language processing, combined with discrete code extraction for tracking performance. While AI has the advantage of a more hands-free approach, such a system would itself require monitoring for performance to avoid unintended consequences.
Ultimately, providing high-quality care and improving patient outcomes are universal goals, though demonstrating this aspiration by reporting on quality metrics can be challenging. Quality measurement, though, is now firmly integrated into the fabric of clinical medicine. In the future, more facets of practice will be measured, patient-level factors and cross specialty reporting will increasingly be emphasized, and administrative burdens will be reduced.
Dr. Leiman is assistant professor of medicine at Duke University, Durham, N.C., cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup, and chair of the AGA’s Quality Committee. Dr. Freedman is medical director, SE Territory, Aetna/CVS Health and cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup. Dr. Anjou is a practicing clinical gastroenterologist at Connecticut GI, Torrington, and recent member of the AGA Quality Committee. The authors reported no conflicts related to this article.
Modern efforts to monitor and improve quality in health care can trace their roots to the early 20th century. At that time, hospitals initiated mechanisms to ensure standard practices for privileging clinicians, reporting medical records and clinical data, and establishing supervised diagnostic facilities. Years later, Avedis Donabedian published “Evaluating the Quality of Medical Care,” which outlined how health care should be measured across three areas – structure, process, and outcome – and became a foundational rubric for assessing quality in medicine.
Over the ensuing decades, with the rise of professional society guidelines and increasing government involvement in the reimbursement of health care, establishing benchmarks and tracking clinical performance has become increasingly important. The passage of the Affordable Care Act subsequently established a formal, legislative mandate for assessing clinical quality tied to reimbursement. Although the context, consequences, and details for reporting have evolved, quality tracking is now firmly entrenched across clinical practice, including gastroenterology. One such mechanism for this is the Merit-Based Incentive Payment System (MIPS), which is a quality payment program (QPP) administered by the Centers for Medicare & Medicaid Services. Today, both government and private payers are assessing measurements and improvements of quality to satisfy the Quintuple Aim of achieving better health outcomes, seeking efficient cost of care, improving patient experience, improving provider experience, and enhancing equity through the reduction health inequalities.
As we transition from a fee-based to a value-based care model, several important developments relevant to the practicing gastroenterologist are likely to occur as the broader landscape of quality reporting will continue shifting. This article will outline a vision of the future in quality measurement for gastroenterology.
Gastroenterologists have relatively few specialty-specific measures on which to report. The widespread use of the adenoma detection rate for screening colonoscopy does represent a success in quality improvement because it is easily calculated, is reproducible, and has been consistently associated with clinical outcomes. But the overall measure set is limited to screening colonoscopy and the management of viral hepatitis, meaning large areas of our practice are not included in this set. Developing new metrics related to broader areas of practice will be necessary to address this current shortcoming and increase the impact of quality programs to clinicians. Indeed, a recent environmental scan performed by the Core Quality Measures Collaborative, a public-private coalition of leaders working to facilitate measure alignment, proposed future areas for development, including gastroesophageal reflux disease, nonalcoholic fatty liver disease, and medication management.
The American Gastroenterological Association, through its defined process of guideline-to-measure development, has responded by creating metrics for the management of acute pancreatitis, Lynch syndrome testing, and eradicating Helicobacter pylori in the context of gastric intestinal metaplasia; additionally, previously defined measures exist for Barrett’s esophagus and inflammatory bowel disease. Therefore, gastroenterologists can expect to report on an expanding collection of measures in the future.
However, recognizing that not all measures may be equally applicable across populations and acknowledging the importance of risk adjustment, incorporating at least an assessment for risk stratification in their future development is vital. Specifically, social risk factors will need to be accounted for during development in ways that might include risk adjustment or stratification by groups. Increasing data demonstrate that clinician performance can vary by population served and that social determinants of health (SDoH) should be incorporated into an assessment of outcomes. Risk stratification may allow clinicians or practices to report outcomes by group without jeopardy of incurring performance-based penalties. However, the ultimate goal should be reducing inequities and closing care gaps rather than inadvertently lowering the bar for clinicians who primarily treat disenfranchised populations. Eventually, any new measures aiming to be included in a QPP require formal validity testing, which can delay their inclusion in such a set. Yet including stratification in their development will provide a more robust and accurate assessment of quality of care delivered according to one’s catchment and help serve to minimize the effects of SDoH.
Another way that quality measurement may account for a more comprehensive assessment of care delivered is by bundling similarly provided services, even those across multiple specialties. Such a future model is the MIPS Value Pathways, currently under development by CMS. While the exact make-up and reporting structure remains to be determined, a group of related metrics – for example, for colonic health – would likely be grouped together. This model might include an evaluation of a practice’s performance in screening colonoscopy, Lynch testing practices, and inflammatory bowel disease management, which could also be relevant to surgeons, pathologists, and oncologists. This paradigm could serve to increase quality alignment across specialties and reinforce a commitment toward improving care delivery and fulfill a value-based mandate.
Within this framework, though, a shared challenge across specialties exists for the capture and reporting of clinical data. The financial and time costs for quality reporting are well documented, therefore any future vision of quality must address means to ease this reporting burden. Accounting for this would be especially impactful to independent as well as small- to moderate-sized practices, which must provide their own resources for collecting and reporting, with the QPP payment adjustments often insufficient to replace lost revenue or expenses. Some administrative relief has been provided by CMS during the current COVID-19 pandemic, but this focused on allowing select clinicians to avoid reporting rather than addressing the fundamental challenges presented by extracting and documenting quality measures. Moving forward, an increasing emphasis will likely be on the use of artificial intelligence (AI), such as natural language processing, combined with discrete code extraction for tracking performance. While AI has the advantage of a more hands-free approach, such a system would itself require monitoring for performance to avoid unintended consequences.
Ultimately, providing high-quality care and improving patient outcomes are universal goals, though demonstrating this aspiration by reporting on quality metrics can be challenging. Quality measurement, though, is now firmly integrated into the fabric of clinical medicine. In the future, more facets of practice will be measured, patient-level factors and cross specialty reporting will increasingly be emphasized, and administrative burdens will be reduced.
Dr. Leiman is assistant professor of medicine at Duke University, Durham, N.C., cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup, and chair of the AGA’s Quality Committee. Dr. Freedman is medical director, SE Territory, Aetna/CVS Health and cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup. Dr. Anjou is a practicing clinical gastroenterologist at Connecticut GI, Torrington, and recent member of the AGA Quality Committee. The authors reported no conflicts related to this article.
Modern efforts to monitor and improve quality in health care can trace their roots to the early 20th century. At that time, hospitals initiated mechanisms to ensure standard practices for privileging clinicians, reporting medical records and clinical data, and establishing supervised diagnostic facilities. Years later, Avedis Donabedian published “Evaluating the Quality of Medical Care,” which outlined how health care should be measured across three areas – structure, process, and outcome – and became a foundational rubric for assessing quality in medicine.
Over the ensuing decades, with the rise of professional society guidelines and increasing government involvement in the reimbursement of health care, establishing benchmarks and tracking clinical performance has become increasingly important. The passage of the Affordable Care Act subsequently established a formal, legislative mandate for assessing clinical quality tied to reimbursement. Although the context, consequences, and details for reporting have evolved, quality tracking is now firmly entrenched across clinical practice, including gastroenterology. One such mechanism for this is the Merit-Based Incentive Payment System (MIPS), which is a quality payment program (QPP) administered by the Centers for Medicare & Medicaid Services. Today, both government and private payers are assessing measurements and improvements of quality to satisfy the Quintuple Aim of achieving better health outcomes, seeking efficient cost of care, improving patient experience, improving provider experience, and enhancing equity through the reduction health inequalities.
As we transition from a fee-based to a value-based care model, several important developments relevant to the practicing gastroenterologist are likely to occur as the broader landscape of quality reporting will continue shifting. This article will outline a vision of the future in quality measurement for gastroenterology.
Gastroenterologists have relatively few specialty-specific measures on which to report. The widespread use of the adenoma detection rate for screening colonoscopy does represent a success in quality improvement because it is easily calculated, is reproducible, and has been consistently associated with clinical outcomes. But the overall measure set is limited to screening colonoscopy and the management of viral hepatitis, meaning large areas of our practice are not included in this set. Developing new metrics related to broader areas of practice will be necessary to address this current shortcoming and increase the impact of quality programs to clinicians. Indeed, a recent environmental scan performed by the Core Quality Measures Collaborative, a public-private coalition of leaders working to facilitate measure alignment, proposed future areas for development, including gastroesophageal reflux disease, nonalcoholic fatty liver disease, and medication management.
The American Gastroenterological Association, through its defined process of guideline-to-measure development, has responded by creating metrics for the management of acute pancreatitis, Lynch syndrome testing, and eradicating Helicobacter pylori in the context of gastric intestinal metaplasia; additionally, previously defined measures exist for Barrett’s esophagus and inflammatory bowel disease. Therefore, gastroenterologists can expect to report on an expanding collection of measures in the future.
However, recognizing that not all measures may be equally applicable across populations and acknowledging the importance of risk adjustment, incorporating at least an assessment for risk stratification in their future development is vital. Specifically, social risk factors will need to be accounted for during development in ways that might include risk adjustment or stratification by groups. Increasing data demonstrate that clinician performance can vary by population served and that social determinants of health (SDoH) should be incorporated into an assessment of outcomes. Risk stratification may allow clinicians or practices to report outcomes by group without jeopardy of incurring performance-based penalties. However, the ultimate goal should be reducing inequities and closing care gaps rather than inadvertently lowering the bar for clinicians who primarily treat disenfranchised populations. Eventually, any new measures aiming to be included in a QPP require formal validity testing, which can delay their inclusion in such a set. Yet including stratification in their development will provide a more robust and accurate assessment of quality of care delivered according to one’s catchment and help serve to minimize the effects of SDoH.
Another way that quality measurement may account for a more comprehensive assessment of care delivered is by bundling similarly provided services, even those across multiple specialties. Such a future model is the MIPS Value Pathways, currently under development by CMS. While the exact make-up and reporting structure remains to be determined, a group of related metrics – for example, for colonic health – would likely be grouped together. This model might include an evaluation of a practice’s performance in screening colonoscopy, Lynch testing practices, and inflammatory bowel disease management, which could also be relevant to surgeons, pathologists, and oncologists. This paradigm could serve to increase quality alignment across specialties and reinforce a commitment toward improving care delivery and fulfill a value-based mandate.
Within this framework, though, a shared challenge across specialties exists for the capture and reporting of clinical data. The financial and time costs for quality reporting are well documented, therefore any future vision of quality must address means to ease this reporting burden. Accounting for this would be especially impactful to independent as well as small- to moderate-sized practices, which must provide their own resources for collecting and reporting, with the QPP payment adjustments often insufficient to replace lost revenue or expenses. Some administrative relief has been provided by CMS during the current COVID-19 pandemic, but this focused on allowing select clinicians to avoid reporting rather than addressing the fundamental challenges presented by extracting and documenting quality measures. Moving forward, an increasing emphasis will likely be on the use of artificial intelligence (AI), such as natural language processing, combined with discrete code extraction for tracking performance. While AI has the advantage of a more hands-free approach, such a system would itself require monitoring for performance to avoid unintended consequences.
Ultimately, providing high-quality care and improving patient outcomes are universal goals, though demonstrating this aspiration by reporting on quality metrics can be challenging. Quality measurement, though, is now firmly integrated into the fabric of clinical medicine. In the future, more facets of practice will be measured, patient-level factors and cross specialty reporting will increasingly be emphasized, and administrative burdens will be reduced.
Dr. Leiman is assistant professor of medicine at Duke University, Durham, N.C., cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup, and chair of the AGA’s Quality Committee. Dr. Freedman is medical director, SE Territory, Aetna/CVS Health and cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup. Dr. Anjou is a practicing clinical gastroenterologist at Connecticut GI, Torrington, and recent member of the AGA Quality Committee. The authors reported no conflicts related to this article.
Improving quality and return-on-investment: Provider onboarding
Physician and advanced practice provider (APP) (collectively, “provider”) onboarding into health care delivery settings requires careful planning and systematic integration. Assimilation into health care settings and cultures necessitates more than a 1- or 2-day orientation. Rather, an intentional, longitudinal onboarding program (starting with orientation) needs to be designed to assimilate providers into the unique culture of a medical practice.
Establishing mutual expectations
Communication concerning mutual expectations is a vital component of the agreement between provider and practice. Items that should be included in provider onboarding (likely addressed in either the practice visit or amplified in a contract) include the following:
- Committees: Committee orientation should include a discussion of provider preferences/expectations and why getting the new provider involved in the business of the practice is a priority of the group.
- Operations: Key clinical operations details should be reviewed with the incoming provider and reinforced through follow-up discussions with a physician mentor/coach (for example, call distribution; role of the senior nonclinical leadership team/accountants, fellow practice/group partners, and IT support; role definitions and expectations for duties, transitioning call, and EHR charting; revenue-sharing; supplies/preferences/adaptability to scope type).
- Interests: Specific provider interests (for example, clinical research, infusion, hemorrhoidal banding, weight loss/nutrition, inflammatory bowel disease, irritable bowel disease, pathology) and productivity expectations (for example, number of procedures, number of new and return patient visits per day) should be communicated.
- Miscellaneous: Discussion about marketing the practice, importance of growing satellite programs and nuance of major referral groups to the practice are also key components of the assimilation process.
Leadership self-awareness and cultural alignment
Leadership self-awareness is a key element of provider onboarding. Physicians and APPs are trained to think independently and may be challenged to share decision-making and rely on others. The following are some no-cost self-assessment and awareness resources:
- Myers-Briggs Personality Profile Preferences:
- VIA Strengths:
- VARK Analysis:
Cultural alignment is also a critical consideration to ensure orderly assimilation into the practice/health care setting and with stakeholders. A shared commitment to embed a culture with shared values has relevance to merging cultures – not only when organizations come together – but with individuals as well. Time spent developing a better understanding of the customs, culture and traditions of the practice will be helpful if a practice must change its trajectory based on meeting an unmovable obstruction (for example, market forces requiring practice consolidation).
Improved quality
Transitioning a new provider into an existing practice culture can have a ripple effect on support staff and patient satisfaction and is, therefore, an important consideration in provider onboarding. Written standards, procedures, expectations, and practices are always advisable when possible. Attention to the demographics of the recruited physician is also important with shifts in interests and priorities from a practice. Millennials will constitute most of the workforce by 2025 and arrive with a mindset that the tenure in a role will be shorter than providers before them. Accordingly, the intentionality of the relationship is critical for successful bonding.
If current physician leaders want to achieve simultaneous succession planning and maintain the legacy of a patient-centric and resilient practice, these leaders must consider bridging the “cultural knowledge acumen gap.” James S. Hernandez, MD, MS, FCAP, and colleagues suggest a “connector” role between new and experienced providers. Reverse mentoring/distance/reciprocal mentoring is also mentioned as a two-way learning process between mentor and mentee.
Process structure considerations
Each new hire affects the culture of the practice. Best practices for the onboarding and orientation process should be followed. A written project master list with a timeline for completion of onboarding tasks with responsible and accountable persons, target dates for completion, and measurement should be established. Establishing mutual expectations up front can help practices tailor committee roles and clinical responsibilities to maximize provider engagement and longevity. A robust onboarding process may take up to 2 years depending on the size of the practice and the complexity of its structure and associated duties.
Desired outcomes
The desired outcome of the onboarding process is a satisfied provider whose passion and enthusiasm for quality patient care is demonstrated objectively through excellent performance on clinical quality measures and metrics of patient and referral source satisfaction.
Periodic reviews of how the onboarding process is progressing should be undertaken. These reviews can be modeled after the After-Action Review (AAR) process used in the military for measuring progress. Simply stated, what items went well with onboarding and why? What items did not go well with onboarding and why not? (Consider something like the Center for Medicare & Medicaid Services’ “5 Whys” assessment to determine root cause for items that need correction.) What elements of the onboarding process could be further improved? Using a Delphi method during the AAR session is an excellent way for the group to hear from all participants ranging from senior partners to recently recruited providers.
Conclusion
Medical practices must recognize that assimilating a new provider into the practice through a robust onboarding process is not lost effort but rather a force multiplier. Effective provider onboarding gives the incoming provider a sense of purpose and resolve, which results in optimized clinical productivity and engagement because the new provider is invested in the future of the practice. Once successfully onboarded and integrated into the practice, new providers need to understand that the work effort invested in their onboarding comes with a “pay it forward” obligation for the next provider recruited by the group. Group members also need to realize that the baseline is always changing–the provider onboarding process needs to continually evolve and adapt as the practice changes and new providers are hired.
Mr. Rudnick is a visiting professor and program director healthcare quality, innovation, and strategy at St Thomas University, Miami. Mr. Turner is regional vice president for the Midatlantic market of Covenant Physician Partners.
References
“Best practices for onboarding physicians.” The Rheumatologist. 2019 Sep 17. Accessed 2021 Sep 6. https://www.the-rheumatologist.org/article/best-practices-for-onboarding-new-physicians/
Centers for Medicare & Medicaid Services. Five Whys Tool for Root Cause Analysis: QAPI. 2021. Accessed 2021 Sep 6. https://www.cms.gov/medicare/provider-enrollment-and-certification/qapi/downloads/fivewhys.pdf.
DeIuliis ET, Saylor E. Open J Occup Ther. 2021;9(1):1-13.
Hernandez JS et al. “Discussion: Mentoring millennials for future leadership.” Physician Leadership Journal. 2018 May 14. Accessed 2021 Sep 6. https://www.physicianleaders.org/news/discussion-mentoring-millennials-future-leadership
Moore L et al. J Trauma Acute Care Surg. 2015 Jun;78(6):1168-75..
Klein CJ et al. West J Nurs Res. 2021 Feb;43(2):105-114.
Weinburger T, Gordon J. Health Prog. Nov-Dec 2013;94(6):76-9.
Wentlandt K et al. Healthc Q. 2016;18(4):36-41.
Physician and advanced practice provider (APP) (collectively, “provider”) onboarding into health care delivery settings requires careful planning and systematic integration. Assimilation into health care settings and cultures necessitates more than a 1- or 2-day orientation. Rather, an intentional, longitudinal onboarding program (starting with orientation) needs to be designed to assimilate providers into the unique culture of a medical practice.
Establishing mutual expectations
Communication concerning mutual expectations is a vital component of the agreement between provider and practice. Items that should be included in provider onboarding (likely addressed in either the practice visit or amplified in a contract) include the following:
- Committees: Committee orientation should include a discussion of provider preferences/expectations and why getting the new provider involved in the business of the practice is a priority of the group.
- Operations: Key clinical operations details should be reviewed with the incoming provider and reinforced through follow-up discussions with a physician mentor/coach (for example, call distribution; role of the senior nonclinical leadership team/accountants, fellow practice/group partners, and IT support; role definitions and expectations for duties, transitioning call, and EHR charting; revenue-sharing; supplies/preferences/adaptability to scope type).
- Interests: Specific provider interests (for example, clinical research, infusion, hemorrhoidal banding, weight loss/nutrition, inflammatory bowel disease, irritable bowel disease, pathology) and productivity expectations (for example, number of procedures, number of new and return patient visits per day) should be communicated.
- Miscellaneous: Discussion about marketing the practice, importance of growing satellite programs and nuance of major referral groups to the practice are also key components of the assimilation process.
Leadership self-awareness and cultural alignment
Leadership self-awareness is a key element of provider onboarding. Physicians and APPs are trained to think independently and may be challenged to share decision-making and rely on others. The following are some no-cost self-assessment and awareness resources:
- Myers-Briggs Personality Profile Preferences:
- VIA Strengths:
- VARK Analysis:
Cultural alignment is also a critical consideration to ensure orderly assimilation into the practice/health care setting and with stakeholders. A shared commitment to embed a culture with shared values has relevance to merging cultures – not only when organizations come together – but with individuals as well. Time spent developing a better understanding of the customs, culture and traditions of the practice will be helpful if a practice must change its trajectory based on meeting an unmovable obstruction (for example, market forces requiring practice consolidation).
Improved quality
Transitioning a new provider into an existing practice culture can have a ripple effect on support staff and patient satisfaction and is, therefore, an important consideration in provider onboarding. Written standards, procedures, expectations, and practices are always advisable when possible. Attention to the demographics of the recruited physician is also important with shifts in interests and priorities from a practice. Millennials will constitute most of the workforce by 2025 and arrive with a mindset that the tenure in a role will be shorter than providers before them. Accordingly, the intentionality of the relationship is critical for successful bonding.
If current physician leaders want to achieve simultaneous succession planning and maintain the legacy of a patient-centric and resilient practice, these leaders must consider bridging the “cultural knowledge acumen gap.” James S. Hernandez, MD, MS, FCAP, and colleagues suggest a “connector” role between new and experienced providers. Reverse mentoring/distance/reciprocal mentoring is also mentioned as a two-way learning process between mentor and mentee.
Process structure considerations
Each new hire affects the culture of the practice. Best practices for the onboarding and orientation process should be followed. A written project master list with a timeline for completion of onboarding tasks with responsible and accountable persons, target dates for completion, and measurement should be established. Establishing mutual expectations up front can help practices tailor committee roles and clinical responsibilities to maximize provider engagement and longevity. A robust onboarding process may take up to 2 years depending on the size of the practice and the complexity of its structure and associated duties.
Desired outcomes
The desired outcome of the onboarding process is a satisfied provider whose passion and enthusiasm for quality patient care is demonstrated objectively through excellent performance on clinical quality measures and metrics of patient and referral source satisfaction.
Periodic reviews of how the onboarding process is progressing should be undertaken. These reviews can be modeled after the After-Action Review (AAR) process used in the military for measuring progress. Simply stated, what items went well with onboarding and why? What items did not go well with onboarding and why not? (Consider something like the Center for Medicare & Medicaid Services’ “5 Whys” assessment to determine root cause for items that need correction.) What elements of the onboarding process could be further improved? Using a Delphi method during the AAR session is an excellent way for the group to hear from all participants ranging from senior partners to recently recruited providers.
Conclusion
Medical practices must recognize that assimilating a new provider into the practice through a robust onboarding process is not lost effort but rather a force multiplier. Effective provider onboarding gives the incoming provider a sense of purpose and resolve, which results in optimized clinical productivity and engagement because the new provider is invested in the future of the practice. Once successfully onboarded and integrated into the practice, new providers need to understand that the work effort invested in their onboarding comes with a “pay it forward” obligation for the next provider recruited by the group. Group members also need to realize that the baseline is always changing–the provider onboarding process needs to continually evolve and adapt as the practice changes and new providers are hired.
Mr. Rudnick is a visiting professor and program director healthcare quality, innovation, and strategy at St Thomas University, Miami. Mr. Turner is regional vice president for the Midatlantic market of Covenant Physician Partners.
References
“Best practices for onboarding physicians.” The Rheumatologist. 2019 Sep 17. Accessed 2021 Sep 6. https://www.the-rheumatologist.org/article/best-practices-for-onboarding-new-physicians/
Centers for Medicare & Medicaid Services. Five Whys Tool for Root Cause Analysis: QAPI. 2021. Accessed 2021 Sep 6. https://www.cms.gov/medicare/provider-enrollment-and-certification/qapi/downloads/fivewhys.pdf.
DeIuliis ET, Saylor E. Open J Occup Ther. 2021;9(1):1-13.
Hernandez JS et al. “Discussion: Mentoring millennials for future leadership.” Physician Leadership Journal. 2018 May 14. Accessed 2021 Sep 6. https://www.physicianleaders.org/news/discussion-mentoring-millennials-future-leadership
Moore L et al. J Trauma Acute Care Surg. 2015 Jun;78(6):1168-75..
Klein CJ et al. West J Nurs Res. 2021 Feb;43(2):105-114.
Weinburger T, Gordon J. Health Prog. Nov-Dec 2013;94(6):76-9.
Wentlandt K et al. Healthc Q. 2016;18(4):36-41.
Physician and advanced practice provider (APP) (collectively, “provider”) onboarding into health care delivery settings requires careful planning and systematic integration. Assimilation into health care settings and cultures necessitates more than a 1- or 2-day orientation. Rather, an intentional, longitudinal onboarding program (starting with orientation) needs to be designed to assimilate providers into the unique culture of a medical practice.
Establishing mutual expectations
Communication concerning mutual expectations is a vital component of the agreement between provider and practice. Items that should be included in provider onboarding (likely addressed in either the practice visit or amplified in a contract) include the following:
- Committees: Committee orientation should include a discussion of provider preferences/expectations and why getting the new provider involved in the business of the practice is a priority of the group.
- Operations: Key clinical operations details should be reviewed with the incoming provider and reinforced through follow-up discussions with a physician mentor/coach (for example, call distribution; role of the senior nonclinical leadership team/accountants, fellow practice/group partners, and IT support; role definitions and expectations for duties, transitioning call, and EHR charting; revenue-sharing; supplies/preferences/adaptability to scope type).
- Interests: Specific provider interests (for example, clinical research, infusion, hemorrhoidal banding, weight loss/nutrition, inflammatory bowel disease, irritable bowel disease, pathology) and productivity expectations (for example, number of procedures, number of new and return patient visits per day) should be communicated.
- Miscellaneous: Discussion about marketing the practice, importance of growing satellite programs and nuance of major referral groups to the practice are also key components of the assimilation process.
Leadership self-awareness and cultural alignment
Leadership self-awareness is a key element of provider onboarding. Physicians and APPs are trained to think independently and may be challenged to share decision-making and rely on others. The following are some no-cost self-assessment and awareness resources:
- Myers-Briggs Personality Profile Preferences:
- VIA Strengths:
- VARK Analysis:
Cultural alignment is also a critical consideration to ensure orderly assimilation into the practice/health care setting and with stakeholders. A shared commitment to embed a culture with shared values has relevance to merging cultures – not only when organizations come together – but with individuals as well. Time spent developing a better understanding of the customs, culture and traditions of the practice will be helpful if a practice must change its trajectory based on meeting an unmovable obstruction (for example, market forces requiring practice consolidation).
Improved quality
Transitioning a new provider into an existing practice culture can have a ripple effect on support staff and patient satisfaction and is, therefore, an important consideration in provider onboarding. Written standards, procedures, expectations, and practices are always advisable when possible. Attention to the demographics of the recruited physician is also important with shifts in interests and priorities from a practice. Millennials will constitute most of the workforce by 2025 and arrive with a mindset that the tenure in a role will be shorter than providers before them. Accordingly, the intentionality of the relationship is critical for successful bonding.
If current physician leaders want to achieve simultaneous succession planning and maintain the legacy of a patient-centric and resilient practice, these leaders must consider bridging the “cultural knowledge acumen gap.” James S. Hernandez, MD, MS, FCAP, and colleagues suggest a “connector” role between new and experienced providers. Reverse mentoring/distance/reciprocal mentoring is also mentioned as a two-way learning process between mentor and mentee.
Process structure considerations
Each new hire affects the culture of the practice. Best practices for the onboarding and orientation process should be followed. A written project master list with a timeline for completion of onboarding tasks with responsible and accountable persons, target dates for completion, and measurement should be established. Establishing mutual expectations up front can help practices tailor committee roles and clinical responsibilities to maximize provider engagement and longevity. A robust onboarding process may take up to 2 years depending on the size of the practice and the complexity of its structure and associated duties.
Desired outcomes
The desired outcome of the onboarding process is a satisfied provider whose passion and enthusiasm for quality patient care is demonstrated objectively through excellent performance on clinical quality measures and metrics of patient and referral source satisfaction.
Periodic reviews of how the onboarding process is progressing should be undertaken. These reviews can be modeled after the After-Action Review (AAR) process used in the military for measuring progress. Simply stated, what items went well with onboarding and why? What items did not go well with onboarding and why not? (Consider something like the Center for Medicare & Medicaid Services’ “5 Whys” assessment to determine root cause for items that need correction.) What elements of the onboarding process could be further improved? Using a Delphi method during the AAR session is an excellent way for the group to hear from all participants ranging from senior partners to recently recruited providers.
Conclusion
Medical practices must recognize that assimilating a new provider into the practice through a robust onboarding process is not lost effort but rather a force multiplier. Effective provider onboarding gives the incoming provider a sense of purpose and resolve, which results in optimized clinical productivity and engagement because the new provider is invested in the future of the practice. Once successfully onboarded and integrated into the practice, new providers need to understand that the work effort invested in their onboarding comes with a “pay it forward” obligation for the next provider recruited by the group. Group members also need to realize that the baseline is always changing–the provider onboarding process needs to continually evolve and adapt as the practice changes and new providers are hired.
Mr. Rudnick is a visiting professor and program director healthcare quality, innovation, and strategy at St Thomas University, Miami. Mr. Turner is regional vice president for the Midatlantic market of Covenant Physician Partners.
References
“Best practices for onboarding physicians.” The Rheumatologist. 2019 Sep 17. Accessed 2021 Sep 6. https://www.the-rheumatologist.org/article/best-practices-for-onboarding-new-physicians/
Centers for Medicare & Medicaid Services. Five Whys Tool for Root Cause Analysis: QAPI. 2021. Accessed 2021 Sep 6. https://www.cms.gov/medicare/provider-enrollment-and-certification/qapi/downloads/fivewhys.pdf.
DeIuliis ET, Saylor E. Open J Occup Ther. 2021;9(1):1-13.
Hernandez JS et al. “Discussion: Mentoring millennials for future leadership.” Physician Leadership Journal. 2018 May 14. Accessed 2021 Sep 6. https://www.physicianleaders.org/news/discussion-mentoring-millennials-future-leadership
Moore L et al. J Trauma Acute Care Surg. 2015 Jun;78(6):1168-75..
Klein CJ et al. West J Nurs Res. 2021 Feb;43(2):105-114.
Weinburger T, Gordon J. Health Prog. Nov-Dec 2013;94(6):76-9.
Wentlandt K et al. Healthc Q. 2016;18(4):36-41.
How the 2022 proposed Medicare payment rules impact GI
In July 2021, the Centers for Medicare & Medicaid Services released the Medicare Physician Fee Schedule (PFS) and Hospital Outpatient Prospective Payment System (OPPS)/Ambulatory Surgery Center (ASC) proposed rules for calendar year (CY) 2022. While the OPPS/ASC proposed rule was largely positive for gastroenterology, the PFS proposed rule was more of a mixed bag for practices.
No more colonoscopy coinsurance “loophole”: After nearly a decade of advocacy, the Removing Barriers to Colorectal Cancer Screening Act was finally signed into law this year and will take effect Jan. 1, 2023. The legislation phases out Medicare beneficiary cost-sharing obligations when a polyp or lesion is found and biopsied or removed as part of a screening colonoscopy or flexible sigmoidoscopy. The American Gastroenterological Association is pleased this will finally eliminate a surprise bill for patients and remove a barrier to colorectal cancer screening.
The phase out timeline is as follows:
- 80% payment for services furnished during CY 2022 (coinsurance, 20%).
- 85% payment for services furnished during CY 2023 through CY 2026 (coinsurance, 15%).
- 90% payment for services furnished during CY 2027 through CY 2029 (coinsurance, 10%).
- 100% payment for services furnished from CY 2030 onward (coinsurance, 0%).
Providers must continue to report HCPCS modifier “PT” in the hospital outpatient and ASC during the transition period to indicate that a planned colorectal cancer screening service converted to a diagnostic service.
Proposed 2022 PFS conversion factor could fall 3.75% unless Congress acts: The proposed 2022 PFS conversion factor is $33.58. The decrease reflects the expiration of the 3.75% payment increase provided by the Consolidated Appropriations Act. This congressional intervention averted a significant cut in Medicare physician payment that would have resulted in an almost 10% cut to GI services. The GI societies are working with Congress to avert cuts to physician payments next year as practices continue to recover from the pandemic.
GI procedure payments to increase 3% for hospital outpatient and ASCs: A 2.3% increase has been proposed for the conversion factors, resulting in $84.46 for hospitals and $50.04 for ASCs meeting quality reporting requirements. However, GI endoscopy procedure payments are expected to increase on average 3% in CY 2022.
Colon capsule endoscopy and POEM get new codes and payments: CMS accepted new CPT codes for colon capsule endoscopy (CCE) and peroral endoscopic myotomy (POEM) beginning Jan. 1, 2022.
CMS’s proposed CCE value of 2.41 physician work relative value units (wRVUs) reflects the recommendation of the American Medical Association RVS Update Committee (RUC), which is based on data from physicians who perform the procedure. The proposed national-level physician payments are $116.52 for the professional component and $664.21 for the technical component.
However, CMS did not accept the RUC’s recommendation of 15.50 wRVUs for POEM and, instead, proposed that POEM is similar in work to hemodialysis access CPT code 36819, which has a wRVU of 13.29 and a payment of $792.82. The RUC’s valuation of 15.50 wRVUs was based on data from nearly 120 physicians who perform POEM, and we are disappointed CMS chose to reject the robust survey data. The GI societies will defend the 15.50 wRVU in our comments.
The proposed facility fee for POEM is $3,160.76 in the hospital outpatient setting and $1,848.32 in the ASC. CMS’s proposed facility fee for colon capsule endoscopy is $814.44 in the hospital outpatient setting.
CMS moves physicians to MVPs and plans to phase out MIPS: CMS proposes to revise and phase out the Merit-Based Incentive Payment System (MIPS) and move physicians towards the MIPS Value Pathways (MVPs) system beginning in the 2023 performance year (PY). No GI MVPs were proposed for PY 2023. The GI societies are working with CMS as they develop MVPs to ensure any gastroenterology-related MVPs do not harm gastroenterologists.
CMS is statutorily required to weigh the MIPS Cost and Quality performance categories equally beginning with PY 2022. The proposed PY 2022 MIPS performance categories are:
- Quality: 30%.
- Cost: 30%.
- Promoting Interoperability: 25% (no change from 2021).
- Improvement Activities: 15% (no change from 2021).
CMS is also required by law beginning in 2022 to set the MIPS performance threshold to either the mean or median of the final scores for all MIPS eligible clinicians for a prior period. CMS proposes to use the mean final score from MIPS 2017 performance year/MIPS 2019 payment year, which would result in a performance threshold of 75 points and an additional performance threshold set at 89 points for exceptional performance.
CMS keeps all AGA-stewarded measures in MIPS 2022 program year: CMS has proposed to keep all AGA-stewarded measures in the MIPS program for the 2022 program year and accepted the substantive changes for the one-time screening for hepatitis C virus measure we received last year from the Physician Consortium for Performance Improvement. CMS proposed removal of the claims reporting option of American Society for Gastrointestinal Endoscopy–stewarded measure for photodocumentation of cecal intubation because it is topped-out; however, the registry version is still available in MIPS.
OQR Program includes colonoscopy measure for disparities reporting: CMS has identified six priority measures included in the Hospital Outpatient Quality Reporting (OQR) Program as candidate measures for disparities reporting stratified by dual eligibility, one of which is the Facility 7-Day Risk-Standardized Hospital Visit Rate After Outpatient Colonoscopy (OP-32).
The GI societies will jointly comment on issues in the 2022 PFS and OPPS/ASC proposed rules impacting gastroenterologists. We may also organize members to take action by submitting letters during the comment period, so watch your inbox for invitations to participate. We need your help to influence change.
Shivan Mehta, MD, MBA, is with the division of gastroenterology and hepatology at the University of Pennsylvania, Philadelphia, and is an AGA adviser to the American Medical Association RVS Update Committee. David A. Leiman, MD, MSHP, is with the division of gastroenterology at Duke University, Durham, N.C., and is the chair of the AGA Quality Committee. Neither have conflicts to declare.
In July 2021, the Centers for Medicare & Medicaid Services released the Medicare Physician Fee Schedule (PFS) and Hospital Outpatient Prospective Payment System (OPPS)/Ambulatory Surgery Center (ASC) proposed rules for calendar year (CY) 2022. While the OPPS/ASC proposed rule was largely positive for gastroenterology, the PFS proposed rule was more of a mixed bag for practices.
No more colonoscopy coinsurance “loophole”: After nearly a decade of advocacy, the Removing Barriers to Colorectal Cancer Screening Act was finally signed into law this year and will take effect Jan. 1, 2023. The legislation phases out Medicare beneficiary cost-sharing obligations when a polyp or lesion is found and biopsied or removed as part of a screening colonoscopy or flexible sigmoidoscopy. The American Gastroenterological Association is pleased this will finally eliminate a surprise bill for patients and remove a barrier to colorectal cancer screening.
The phase out timeline is as follows:
- 80% payment for services furnished during CY 2022 (coinsurance, 20%).
- 85% payment for services furnished during CY 2023 through CY 2026 (coinsurance, 15%).
- 90% payment for services furnished during CY 2027 through CY 2029 (coinsurance, 10%).
- 100% payment for services furnished from CY 2030 onward (coinsurance, 0%).
Providers must continue to report HCPCS modifier “PT” in the hospital outpatient and ASC during the transition period to indicate that a planned colorectal cancer screening service converted to a diagnostic service.
Proposed 2022 PFS conversion factor could fall 3.75% unless Congress acts: The proposed 2022 PFS conversion factor is $33.58. The decrease reflects the expiration of the 3.75% payment increase provided by the Consolidated Appropriations Act. This congressional intervention averted a significant cut in Medicare physician payment that would have resulted in an almost 10% cut to GI services. The GI societies are working with Congress to avert cuts to physician payments next year as practices continue to recover from the pandemic.
GI procedure payments to increase 3% for hospital outpatient and ASCs: A 2.3% increase has been proposed for the conversion factors, resulting in $84.46 for hospitals and $50.04 for ASCs meeting quality reporting requirements. However, GI endoscopy procedure payments are expected to increase on average 3% in CY 2022.
Colon capsule endoscopy and POEM get new codes and payments: CMS accepted new CPT codes for colon capsule endoscopy (CCE) and peroral endoscopic myotomy (POEM) beginning Jan. 1, 2022.
CMS’s proposed CCE value of 2.41 physician work relative value units (wRVUs) reflects the recommendation of the American Medical Association RVS Update Committee (RUC), which is based on data from physicians who perform the procedure. The proposed national-level physician payments are $116.52 for the professional component and $664.21 for the technical component.
However, CMS did not accept the RUC’s recommendation of 15.50 wRVUs for POEM and, instead, proposed that POEM is similar in work to hemodialysis access CPT code 36819, which has a wRVU of 13.29 and a payment of $792.82. The RUC’s valuation of 15.50 wRVUs was based on data from nearly 120 physicians who perform POEM, and we are disappointed CMS chose to reject the robust survey data. The GI societies will defend the 15.50 wRVU in our comments.
The proposed facility fee for POEM is $3,160.76 in the hospital outpatient setting and $1,848.32 in the ASC. CMS’s proposed facility fee for colon capsule endoscopy is $814.44 in the hospital outpatient setting.
CMS moves physicians to MVPs and plans to phase out MIPS: CMS proposes to revise and phase out the Merit-Based Incentive Payment System (MIPS) and move physicians towards the MIPS Value Pathways (MVPs) system beginning in the 2023 performance year (PY). No GI MVPs were proposed for PY 2023. The GI societies are working with CMS as they develop MVPs to ensure any gastroenterology-related MVPs do not harm gastroenterologists.
CMS is statutorily required to weigh the MIPS Cost and Quality performance categories equally beginning with PY 2022. The proposed PY 2022 MIPS performance categories are:
- Quality: 30%.
- Cost: 30%.
- Promoting Interoperability: 25% (no change from 2021).
- Improvement Activities: 15% (no change from 2021).
CMS is also required by law beginning in 2022 to set the MIPS performance threshold to either the mean or median of the final scores for all MIPS eligible clinicians for a prior period. CMS proposes to use the mean final score from MIPS 2017 performance year/MIPS 2019 payment year, which would result in a performance threshold of 75 points and an additional performance threshold set at 89 points for exceptional performance.
CMS keeps all AGA-stewarded measures in MIPS 2022 program year: CMS has proposed to keep all AGA-stewarded measures in the MIPS program for the 2022 program year and accepted the substantive changes for the one-time screening for hepatitis C virus measure we received last year from the Physician Consortium for Performance Improvement. CMS proposed removal of the claims reporting option of American Society for Gastrointestinal Endoscopy–stewarded measure for photodocumentation of cecal intubation because it is topped-out; however, the registry version is still available in MIPS.
OQR Program includes colonoscopy measure for disparities reporting: CMS has identified six priority measures included in the Hospital Outpatient Quality Reporting (OQR) Program as candidate measures for disparities reporting stratified by dual eligibility, one of which is the Facility 7-Day Risk-Standardized Hospital Visit Rate After Outpatient Colonoscopy (OP-32).
The GI societies will jointly comment on issues in the 2022 PFS and OPPS/ASC proposed rules impacting gastroenterologists. We may also organize members to take action by submitting letters during the comment period, so watch your inbox for invitations to participate. We need your help to influence change.
Shivan Mehta, MD, MBA, is with the division of gastroenterology and hepatology at the University of Pennsylvania, Philadelphia, and is an AGA adviser to the American Medical Association RVS Update Committee. David A. Leiman, MD, MSHP, is with the division of gastroenterology at Duke University, Durham, N.C., and is the chair of the AGA Quality Committee. Neither have conflicts to declare.
In July 2021, the Centers for Medicare & Medicaid Services released the Medicare Physician Fee Schedule (PFS) and Hospital Outpatient Prospective Payment System (OPPS)/Ambulatory Surgery Center (ASC) proposed rules for calendar year (CY) 2022. While the OPPS/ASC proposed rule was largely positive for gastroenterology, the PFS proposed rule was more of a mixed bag for practices.
No more colonoscopy coinsurance “loophole”: After nearly a decade of advocacy, the Removing Barriers to Colorectal Cancer Screening Act was finally signed into law this year and will take effect Jan. 1, 2023. The legislation phases out Medicare beneficiary cost-sharing obligations when a polyp or lesion is found and biopsied or removed as part of a screening colonoscopy or flexible sigmoidoscopy. The American Gastroenterological Association is pleased this will finally eliminate a surprise bill for patients and remove a barrier to colorectal cancer screening.
The phase out timeline is as follows:
- 80% payment for services furnished during CY 2022 (coinsurance, 20%).
- 85% payment for services furnished during CY 2023 through CY 2026 (coinsurance, 15%).
- 90% payment for services furnished during CY 2027 through CY 2029 (coinsurance, 10%).
- 100% payment for services furnished from CY 2030 onward (coinsurance, 0%).
Providers must continue to report HCPCS modifier “PT” in the hospital outpatient and ASC during the transition period to indicate that a planned colorectal cancer screening service converted to a diagnostic service.
Proposed 2022 PFS conversion factor could fall 3.75% unless Congress acts: The proposed 2022 PFS conversion factor is $33.58. The decrease reflects the expiration of the 3.75% payment increase provided by the Consolidated Appropriations Act. This congressional intervention averted a significant cut in Medicare physician payment that would have resulted in an almost 10% cut to GI services. The GI societies are working with Congress to avert cuts to physician payments next year as practices continue to recover from the pandemic.
GI procedure payments to increase 3% for hospital outpatient and ASCs: A 2.3% increase has been proposed for the conversion factors, resulting in $84.46 for hospitals and $50.04 for ASCs meeting quality reporting requirements. However, GI endoscopy procedure payments are expected to increase on average 3% in CY 2022.
Colon capsule endoscopy and POEM get new codes and payments: CMS accepted new CPT codes for colon capsule endoscopy (CCE) and peroral endoscopic myotomy (POEM) beginning Jan. 1, 2022.
CMS’s proposed CCE value of 2.41 physician work relative value units (wRVUs) reflects the recommendation of the American Medical Association RVS Update Committee (RUC), which is based on data from physicians who perform the procedure. The proposed national-level physician payments are $116.52 for the professional component and $664.21 for the technical component.
However, CMS did not accept the RUC’s recommendation of 15.50 wRVUs for POEM and, instead, proposed that POEM is similar in work to hemodialysis access CPT code 36819, which has a wRVU of 13.29 and a payment of $792.82. The RUC’s valuation of 15.50 wRVUs was based on data from nearly 120 physicians who perform POEM, and we are disappointed CMS chose to reject the robust survey data. The GI societies will defend the 15.50 wRVU in our comments.
The proposed facility fee for POEM is $3,160.76 in the hospital outpatient setting and $1,848.32 in the ASC. CMS’s proposed facility fee for colon capsule endoscopy is $814.44 in the hospital outpatient setting.
CMS moves physicians to MVPs and plans to phase out MIPS: CMS proposes to revise and phase out the Merit-Based Incentive Payment System (MIPS) and move physicians towards the MIPS Value Pathways (MVPs) system beginning in the 2023 performance year (PY). No GI MVPs were proposed for PY 2023. The GI societies are working with CMS as they develop MVPs to ensure any gastroenterology-related MVPs do not harm gastroenterologists.
CMS is statutorily required to weigh the MIPS Cost and Quality performance categories equally beginning with PY 2022. The proposed PY 2022 MIPS performance categories are:
- Quality: 30%.
- Cost: 30%.
- Promoting Interoperability: 25% (no change from 2021).
- Improvement Activities: 15% (no change from 2021).
CMS is also required by law beginning in 2022 to set the MIPS performance threshold to either the mean or median of the final scores for all MIPS eligible clinicians for a prior period. CMS proposes to use the mean final score from MIPS 2017 performance year/MIPS 2019 payment year, which would result in a performance threshold of 75 points and an additional performance threshold set at 89 points for exceptional performance.
CMS keeps all AGA-stewarded measures in MIPS 2022 program year: CMS has proposed to keep all AGA-stewarded measures in the MIPS program for the 2022 program year and accepted the substantive changes for the one-time screening for hepatitis C virus measure we received last year from the Physician Consortium for Performance Improvement. CMS proposed removal of the claims reporting option of American Society for Gastrointestinal Endoscopy–stewarded measure for photodocumentation of cecal intubation because it is topped-out; however, the registry version is still available in MIPS.
OQR Program includes colonoscopy measure for disparities reporting: CMS has identified six priority measures included in the Hospital Outpatient Quality Reporting (OQR) Program as candidate measures for disparities reporting stratified by dual eligibility, one of which is the Facility 7-Day Risk-Standardized Hospital Visit Rate After Outpatient Colonoscopy (OP-32).
The GI societies will jointly comment on issues in the 2022 PFS and OPPS/ASC proposed rules impacting gastroenterologists. We may also organize members to take action by submitting letters during the comment period, so watch your inbox for invitations to participate. We need your help to influence change.
Shivan Mehta, MD, MBA, is with the division of gastroenterology and hepatology at the University of Pennsylvania, Philadelphia, and is an AGA adviser to the American Medical Association RVS Update Committee. David A. Leiman, MD, MSHP, is with the division of gastroenterology at Duke University, Durham, N.C., and is the chair of the AGA Quality Committee. Neither have conflicts to declare.
Fighting back against payer coverage policies
The medical community may have paused during the COVID-19 pandemic, but commercial payers kept pushing forward with new coverage restrictions, expanding the number of services and procedures requiring prior authorization (PA) and restricting covered drugs. As 2020 closed and with 2021 barely underway, the American Gastroenterological Association has been holding discussions with major payers to stop implementation of policies restricting gastroenterologists’ ability to prescribe the most appropriate drugs for their patients’ clinical situations.
The Government Affairs Committee’s Coverage and Reimbursement Subcommittee (CRS) works with commercial payers on issues affecting gastroenterologists and identifies outside experts on the policy subject when necessary. The subcommittee recently worked with UnitedHealthcare on a coverage policy change to make Inflictra (infliximab-dyyb) and Avsola (infliximab-axxq) its preferred products and move Remicade (infliximab) and Renflexis (infliximab-abda) to its nonpreferred list, as announced in UnitedHealthcare’s Medical benefit specialty drug update bulletin. The CRS identified Sundeep Singh, MD, an inflammatory bowel disease specialist from Stanford (Calif.) University, to engage in discussion with UnitedHealthcare on behalf of AGA and lead a multisociety effort with the North American Society For Pediatric Gastroenterology, Hepatology & Nutrition; the American Society for Gastrointestinal Endoscopy; and the American College of Gastroenterology.
After conversations with our physician experts, UnitedHealthcare agreed to notify its medical directors to allow pediatric patients 16 years and younger and currently on a nonpreferred product, such as Remicade, to remain on it if that is the recommendation of the treating physician. Adult patients meeting the following conditions may be allowed to remain on nonpreferred products, but will require the prescribing provider to request a review and a determination will be made on a case-by-case basis:
- Adult patients currently on induction of Remicade for less than 18 months will not be required to switch.
- Adult patients who are having a flare of active disease, who are, therefore, not stable, will not be required to switch.
AGA experts are a vital part of CRS’s work with commercial payers. Dr. Singh and his fellow IBD experts who participated in discussion with UnitedHealthcare helped the payer understand why its original policy implementing nonmedical switching without exceptions was harmful to patients. Dr. Singh had this to say about his experience with the process:
“Thanks to the coordinated efforts between AGA, NASPGHAN, ACG, ASGE, and UnitedHealthcare, we were able to reconcile the policy and knowledge gaps to protect our patients with inflammatory bowel disease. While there are significant cost savings associated with biosimilar use, we wanted to temper the health plan’s initial enthusiasm with the potential costs in patients whose clinical and economic outcomes are not certain yet. As we anticipate other health plans will implement similar policies, this effort may provide a road map for the future.”
The CRS also works with pharmacy benefit management organizations. The AGA joined the ASGE and ACG to ask Express Scripts to not exclude coverage of brand colonoscopy preparations such as Suprep, Clenpiq, and Plenvu. The formulary currently plans to cover only generic products for colon cleansing beginning April 1, 2021, primarily 4-liter polyethylene glycol electrolyte solutions (PEG-ELS).
Clinical representatives and staff from AGA, ACG, and ASGE participated in a fruitful discussion with the leadership of Express Scripts and presented several key discussion points in favor of keeping coverage of brand colonoscopy bowel preparations in addition to PEG-ELS. The multisociety group presented views from practicing gastroenterologists as well as from academicians about the safety and benefits of low-volume preparations for a quality screening colonoscopic exam especially in certain patient populations. Limiting choices of bowel preparations will deter patients from undergoing screening colonoscopies, which have been proven to prevent colorectal cancers. After the multisociety group pointed out the need to individualize the choice of bowel preparation to ensure safety and tolerability, Express Scripts will hopefully agree with the significance of having options for our patients. It was clear that the importance of patient preference and clinical appropriateness for different bowel preparation options was heard by the Express Scripts representatives, so we await their decision with hope.
The AGA is working to address issues with commercial payers, but to be effective we need to hear your experiences. We know commercial payers continue to develop increasingly restrictive PA policies and coverage conditions for procedures and drugs. Reach out to the AGA via the AGA Community, Twitter, or via email to Leslie Narramore, the director of regulatory affairs at AGA, at [email protected] to let us know what’s happening.
Seven options to consider if your PA has been rejected or claim has been denied
- Ask for the credentials of the payer representative who initially denied the request. Even when payer representatives are physicians, they are often not gastroenterologists. Ask to speak with a representative actively practicing gastroenterology.
- Ask to record your conversation with the payer representative for documentation purposes.
- Ask to speak directly to the payer’s medical director.
- Bring the complaint to the payer’s attention on social media. Using social media to bring attention to a denial can sometimes elicit quick, personal outreach from the payer to address the issue.
- Let the AGA know what’s happening. Reach out to the AGA via the AGA Community, via Twitter, or by emailing Leslie Narramore, the director of regulatory affairs at AGA ([email protected]).
- File a complaint with the State Insurance Commissioner. State Insurance Commissioners are responsible for regulating the insurance industry in their state and can investigate to ensure the laws in their state are being followed and providers and patients are being treated fairly. While insurance law and regulation are established at the state level, the insurance commissioners are members of the National Association of Insurance Commissioners (NAIC), which allows them to coordinate insurance regulation among the states and territories. Find out your state’s complaint process because many state insurance commissioners have on online complaint forms. Keep records of all interactions with the insurance company to document that you have attempted to resolve the matter with the payer first.
- File a complaint at the federal level for states without an external review process. If your state doesn’t have an external review process that meets the minimum consumer protection standards, the federal government’s Department of Health & Human Services oversees an external review process for health insurance companies in your state. See www.healthcare.gov/appeal-insurance-company-decision/external-review/ for more information. In states where the federal government oversees the process, insurance companies may choose to participate in an HHS-administered process or contract with independent review organizations. If your plan doesn’t participate in a state or HHS-Administered Federal External Review Process, your health plan must contract with an independent review organization.
Dr. Guha is with the University of Texas Health Science Center in Houston. Dr. Upchurch is with Adena Health System in Chillicothe, Ohio. Both are AGA Coverage and Reimbursement Subcommittee members. The authors have no conflicts to declare.
The medical community may have paused during the COVID-19 pandemic, but commercial payers kept pushing forward with new coverage restrictions, expanding the number of services and procedures requiring prior authorization (PA) and restricting covered drugs. As 2020 closed and with 2021 barely underway, the American Gastroenterological Association has been holding discussions with major payers to stop implementation of policies restricting gastroenterologists’ ability to prescribe the most appropriate drugs for their patients’ clinical situations.
The Government Affairs Committee’s Coverage and Reimbursement Subcommittee (CRS) works with commercial payers on issues affecting gastroenterologists and identifies outside experts on the policy subject when necessary. The subcommittee recently worked with UnitedHealthcare on a coverage policy change to make Inflictra (infliximab-dyyb) and Avsola (infliximab-axxq) its preferred products and move Remicade (infliximab) and Renflexis (infliximab-abda) to its nonpreferred list, as announced in UnitedHealthcare’s Medical benefit specialty drug update bulletin. The CRS identified Sundeep Singh, MD, an inflammatory bowel disease specialist from Stanford (Calif.) University, to engage in discussion with UnitedHealthcare on behalf of AGA and lead a multisociety effort with the North American Society For Pediatric Gastroenterology, Hepatology & Nutrition; the American Society for Gastrointestinal Endoscopy; and the American College of Gastroenterology.
After conversations with our physician experts, UnitedHealthcare agreed to notify its medical directors to allow pediatric patients 16 years and younger and currently on a nonpreferred product, such as Remicade, to remain on it if that is the recommendation of the treating physician. Adult patients meeting the following conditions may be allowed to remain on nonpreferred products, but will require the prescribing provider to request a review and a determination will be made on a case-by-case basis:
- Adult patients currently on induction of Remicade for less than 18 months will not be required to switch.
- Adult patients who are having a flare of active disease, who are, therefore, not stable, will not be required to switch.
AGA experts are a vital part of CRS’s work with commercial payers. Dr. Singh and his fellow IBD experts who participated in discussion with UnitedHealthcare helped the payer understand why its original policy implementing nonmedical switching without exceptions was harmful to patients. Dr. Singh had this to say about his experience with the process:
“Thanks to the coordinated efforts between AGA, NASPGHAN, ACG, ASGE, and UnitedHealthcare, we were able to reconcile the policy and knowledge gaps to protect our patients with inflammatory bowel disease. While there are significant cost savings associated with biosimilar use, we wanted to temper the health plan’s initial enthusiasm with the potential costs in patients whose clinical and economic outcomes are not certain yet. As we anticipate other health plans will implement similar policies, this effort may provide a road map for the future.”
The CRS also works with pharmacy benefit management organizations. The AGA joined the ASGE and ACG to ask Express Scripts to not exclude coverage of brand colonoscopy preparations such as Suprep, Clenpiq, and Plenvu. The formulary currently plans to cover only generic products for colon cleansing beginning April 1, 2021, primarily 4-liter polyethylene glycol electrolyte solutions (PEG-ELS).
Clinical representatives and staff from AGA, ACG, and ASGE participated in a fruitful discussion with the leadership of Express Scripts and presented several key discussion points in favor of keeping coverage of brand colonoscopy bowel preparations in addition to PEG-ELS. The multisociety group presented views from practicing gastroenterologists as well as from academicians about the safety and benefits of low-volume preparations for a quality screening colonoscopic exam especially in certain patient populations. Limiting choices of bowel preparations will deter patients from undergoing screening colonoscopies, which have been proven to prevent colorectal cancers. After the multisociety group pointed out the need to individualize the choice of bowel preparation to ensure safety and tolerability, Express Scripts will hopefully agree with the significance of having options for our patients. It was clear that the importance of patient preference and clinical appropriateness for different bowel preparation options was heard by the Express Scripts representatives, so we await their decision with hope.
The AGA is working to address issues with commercial payers, but to be effective we need to hear your experiences. We know commercial payers continue to develop increasingly restrictive PA policies and coverage conditions for procedures and drugs. Reach out to the AGA via the AGA Community, Twitter, or via email to Leslie Narramore, the director of regulatory affairs at AGA, at [email protected] to let us know what’s happening.
Seven options to consider if your PA has been rejected or claim has been denied
- Ask for the credentials of the payer representative who initially denied the request. Even when payer representatives are physicians, they are often not gastroenterologists. Ask to speak with a representative actively practicing gastroenterology.
- Ask to record your conversation with the payer representative for documentation purposes.
- Ask to speak directly to the payer’s medical director.
- Bring the complaint to the payer’s attention on social media. Using social media to bring attention to a denial can sometimes elicit quick, personal outreach from the payer to address the issue.
- Let the AGA know what’s happening. Reach out to the AGA via the AGA Community, via Twitter, or by emailing Leslie Narramore, the director of regulatory affairs at AGA ([email protected]).
- File a complaint with the State Insurance Commissioner. State Insurance Commissioners are responsible for regulating the insurance industry in their state and can investigate to ensure the laws in their state are being followed and providers and patients are being treated fairly. While insurance law and regulation are established at the state level, the insurance commissioners are members of the National Association of Insurance Commissioners (NAIC), which allows them to coordinate insurance regulation among the states and territories. Find out your state’s complaint process because many state insurance commissioners have on online complaint forms. Keep records of all interactions with the insurance company to document that you have attempted to resolve the matter with the payer first.
- File a complaint at the federal level for states without an external review process. If your state doesn’t have an external review process that meets the minimum consumer protection standards, the federal government’s Department of Health & Human Services oversees an external review process for health insurance companies in your state. See www.healthcare.gov/appeal-insurance-company-decision/external-review/ for more information. In states where the federal government oversees the process, insurance companies may choose to participate in an HHS-administered process or contract with independent review organizations. If your plan doesn’t participate in a state or HHS-Administered Federal External Review Process, your health plan must contract with an independent review organization.
Dr. Guha is with the University of Texas Health Science Center in Houston. Dr. Upchurch is with Adena Health System in Chillicothe, Ohio. Both are AGA Coverage and Reimbursement Subcommittee members. The authors have no conflicts to declare.
The medical community may have paused during the COVID-19 pandemic, but commercial payers kept pushing forward with new coverage restrictions, expanding the number of services and procedures requiring prior authorization (PA) and restricting covered drugs. As 2020 closed and with 2021 barely underway, the American Gastroenterological Association has been holding discussions with major payers to stop implementation of policies restricting gastroenterologists’ ability to prescribe the most appropriate drugs for their patients’ clinical situations.
The Government Affairs Committee’s Coverage and Reimbursement Subcommittee (CRS) works with commercial payers on issues affecting gastroenterologists and identifies outside experts on the policy subject when necessary. The subcommittee recently worked with UnitedHealthcare on a coverage policy change to make Inflictra (infliximab-dyyb) and Avsola (infliximab-axxq) its preferred products and move Remicade (infliximab) and Renflexis (infliximab-abda) to its nonpreferred list, as announced in UnitedHealthcare’s Medical benefit specialty drug update bulletin. The CRS identified Sundeep Singh, MD, an inflammatory bowel disease specialist from Stanford (Calif.) University, to engage in discussion with UnitedHealthcare on behalf of AGA and lead a multisociety effort with the North American Society For Pediatric Gastroenterology, Hepatology & Nutrition; the American Society for Gastrointestinal Endoscopy; and the American College of Gastroenterology.
After conversations with our physician experts, UnitedHealthcare agreed to notify its medical directors to allow pediatric patients 16 years and younger and currently on a nonpreferred product, such as Remicade, to remain on it if that is the recommendation of the treating physician. Adult patients meeting the following conditions may be allowed to remain on nonpreferred products, but will require the prescribing provider to request a review and a determination will be made on a case-by-case basis:
- Adult patients currently on induction of Remicade for less than 18 months will not be required to switch.
- Adult patients who are having a flare of active disease, who are, therefore, not stable, will not be required to switch.
AGA experts are a vital part of CRS’s work with commercial payers. Dr. Singh and his fellow IBD experts who participated in discussion with UnitedHealthcare helped the payer understand why its original policy implementing nonmedical switching without exceptions was harmful to patients. Dr. Singh had this to say about his experience with the process:
“Thanks to the coordinated efforts between AGA, NASPGHAN, ACG, ASGE, and UnitedHealthcare, we were able to reconcile the policy and knowledge gaps to protect our patients with inflammatory bowel disease. While there are significant cost savings associated with biosimilar use, we wanted to temper the health plan’s initial enthusiasm with the potential costs in patients whose clinical and economic outcomes are not certain yet. As we anticipate other health plans will implement similar policies, this effort may provide a road map for the future.”
The CRS also works with pharmacy benefit management organizations. The AGA joined the ASGE and ACG to ask Express Scripts to not exclude coverage of brand colonoscopy preparations such as Suprep, Clenpiq, and Plenvu. The formulary currently plans to cover only generic products for colon cleansing beginning April 1, 2021, primarily 4-liter polyethylene glycol electrolyte solutions (PEG-ELS).
Clinical representatives and staff from AGA, ACG, and ASGE participated in a fruitful discussion with the leadership of Express Scripts and presented several key discussion points in favor of keeping coverage of brand colonoscopy bowel preparations in addition to PEG-ELS. The multisociety group presented views from practicing gastroenterologists as well as from academicians about the safety and benefits of low-volume preparations for a quality screening colonoscopic exam especially in certain patient populations. Limiting choices of bowel preparations will deter patients from undergoing screening colonoscopies, which have been proven to prevent colorectal cancers. After the multisociety group pointed out the need to individualize the choice of bowel preparation to ensure safety and tolerability, Express Scripts will hopefully agree with the significance of having options for our patients. It was clear that the importance of patient preference and clinical appropriateness for different bowel preparation options was heard by the Express Scripts representatives, so we await their decision with hope.
The AGA is working to address issues with commercial payers, but to be effective we need to hear your experiences. We know commercial payers continue to develop increasingly restrictive PA policies and coverage conditions for procedures and drugs. Reach out to the AGA via the AGA Community, Twitter, or via email to Leslie Narramore, the director of regulatory affairs at AGA, at [email protected] to let us know what’s happening.
Seven options to consider if your PA has been rejected or claim has been denied
- Ask for the credentials of the payer representative who initially denied the request. Even when payer representatives are physicians, they are often not gastroenterologists. Ask to speak with a representative actively practicing gastroenterology.
- Ask to record your conversation with the payer representative for documentation purposes.
- Ask to speak directly to the payer’s medical director.
- Bring the complaint to the payer’s attention on social media. Using social media to bring attention to a denial can sometimes elicit quick, personal outreach from the payer to address the issue.
- Let the AGA know what’s happening. Reach out to the AGA via the AGA Community, via Twitter, or by emailing Leslie Narramore, the director of regulatory affairs at AGA ([email protected]).
- File a complaint with the State Insurance Commissioner. State Insurance Commissioners are responsible for regulating the insurance industry in their state and can investigate to ensure the laws in their state are being followed and providers and patients are being treated fairly. While insurance law and regulation are established at the state level, the insurance commissioners are members of the National Association of Insurance Commissioners (NAIC), which allows them to coordinate insurance regulation among the states and territories. Find out your state’s complaint process because many state insurance commissioners have on online complaint forms. Keep records of all interactions with the insurance company to document that you have attempted to resolve the matter with the payer first.
- File a complaint at the federal level for states without an external review process. If your state doesn’t have an external review process that meets the minimum consumer protection standards, the federal government’s Department of Health & Human Services oversees an external review process for health insurance companies in your state. See www.healthcare.gov/appeal-insurance-company-decision/external-review/ for more information. In states where the federal government oversees the process, insurance companies may choose to participate in an HHS-administered process or contract with independent review organizations. If your plan doesn’t participate in a state or HHS-Administered Federal External Review Process, your health plan must contract with an independent review organization.
Dr. Guha is with the University of Texas Health Science Center in Houston. Dr. Upchurch is with Adena Health System in Chillicothe, Ohio. Both are AGA Coverage and Reimbursement Subcommittee members. The authors have no conflicts to declare.
Important lessons about telehealth
Telehealth exploded into the public consciousness this year as a way for clinicians and patients to safely connect during the COVID-19 crisis. While telehealth has been part of care delivery at Providence St. Joseph Health (PSJH) for more than a decade, it transitioned almost overnight from an offering most often focused on serving patients in rural areas to a way for any patient to get the care they need virtually whether in a hospital, outpatient facility, or from the comfort and safety of their own home.
Telehealth growth was fueled by changes in regulation and reimbursement during the public health emergency enabling providers to see new and established patients at home across all payer types. To put this growth into perspective, the large PSJH system averaged a few thousand video visits per month in January and February 2020. As COVID transmission spread and lockdowns began, that number climbed to over 15,000 video visits in March to a height of more than 150,000 video visits in May. As of the end of October 2020, PSJH has conducted more than 1.2 million video visits since the beginning of January, steadily accounting for 20%-25% of total visit volume.
Going virtual with gastroenterology
PSJH gastroenterology providers have been a part of this wave, conducting more than 12,000 video visits so far this year (as documented in our Epic EMR), which has been an entirely new method of care delivery for most of these clinicians. We also have many affiliated, private practice gastroenterology providers who practice in our facilities and transitioned quickly to video for outpatient care. Pre- and postprocedure follow-up visits were some of the most common visit types that went virtual, along with new patient visits to establish care and existing patient visits to check in on the status of a health condition, medication, or other concern. Complementary services for gastroenterology patients were transitioned to video over the past 8 months as well. Care management, nutrition services, online support groups, bariatric care information sessions, behavioral health, and more are now available for patients to access virtually.
Remembering it’s not about the tech
New technologies can be challenging to adopt – especially at a pace as rapid as it was this year. Fortunately for PSJH, we had inpatient and outpatient video platforms already in place and an experienced internal telehealth team to scale them quickly to providers and caregivers across system. But even with those advantages, it was still a huge challenge to transition so many providers and caregivers to video visits in such a short time without change management hurdles and bumps along the way.
Too often, there is an overemphasis placed on the technology. It’s a tool, and some technologies are better than others, and they continue to evolve over time. True success or failure lies in the clinical and operational work flows and how well the providers and care teams engage with and adapt them. We found that the providers and staff members willing to venture outside their comfort zone of “how we’ve always done it” and collaborate on the transition to virtual care had the best results. Openness and flexibility to trying new things and using temporary workarounds if existing functionality didn’t meet the need was key to transitioning quickly. Then, by listening to ideas from and sharing feedback among providers, clinics, and geographies, we were able to identify fixes and optimizations that needed to be made to improve the experience for all.
Selecting a video visit platform
No telehealth platform is perfect and meets every patient, provider, and staff need or request despite what a technology vendor may claim. This is especially true in a large and/or diverse system with many different types of clinical use cases. Determining the “must-have” requirements from among those that may be important or simply nice to have is critical when selecting the video visit platform to use.
It’s not an easy decision and nearly impossible to please everyone. Ensuring that there are clinician, operator, and technical stakeholders all contributing to the requirements and decision-making is essential. While some may prefer a “best-of-breed” solution that does one thing very well, it may have to be paired with a set of other complimentary applications to meet all of the organization’s needs. Alternatively, there may be a platform with an expansive feature set but not all of the features are as strong as desired. Then there are solutions that integrate with your existing applications, which is a compelling option to consider.
Regardless of the tool chosen, best-practice work flows, easy-to-follow documentation, a mix of different training options, and internal technical help that responds quickly is key to implementing it successfully. And once implemented, optimization is an ongoing process to make it easier, faster, and better.
Looking ahead
As we came to the end of 2020, all providers and health systems were paying close attention to the Centers for Medicaid & Medicare Services and state-level regulations and reimbursement changes for 2021 to evaluate the impact on telehealth after the public health emergency and COVID-19 waivers are ended. Advocacy efforts are urging lawmakers to not lose the gains that were made during this time and have enabled millions of patients to access care more easily – changes which we believe they will now expect as an option going forward.
We at Providence believe telehealth’s future is a bright one, especially where value-based/managed care arrangements with payers are in place. In addition to integrating video visits and consults into normal clinical practice, we see further growth in serving patients at home with remote patient monitoring and other home-based programs that leverage connected devices and virtual tools. We also anticipate more providers will acquire licenses in other states to virtually care for patients who lack access to specialty services in their own community, which increases access where it is most needed. After 2020, we hope that telehealth will no longer be a specialized service only some patients can receive but a normal way of delivering care to all.
Ms. Winkelman is the system director of telehealth product development and delivery at Providence St. Joseph Health. Providence is the third-largest nonprofit health system in the United States with 51 hospitals, more than 800 clinics, and a comprehensive range of health and social services across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington.
Telehealth exploded into the public consciousness this year as a way for clinicians and patients to safely connect during the COVID-19 crisis. While telehealth has been part of care delivery at Providence St. Joseph Health (PSJH) for more than a decade, it transitioned almost overnight from an offering most often focused on serving patients in rural areas to a way for any patient to get the care they need virtually whether in a hospital, outpatient facility, or from the comfort and safety of their own home.
Telehealth growth was fueled by changes in regulation and reimbursement during the public health emergency enabling providers to see new and established patients at home across all payer types. To put this growth into perspective, the large PSJH system averaged a few thousand video visits per month in January and February 2020. As COVID transmission spread and lockdowns began, that number climbed to over 15,000 video visits in March to a height of more than 150,000 video visits in May. As of the end of October 2020, PSJH has conducted more than 1.2 million video visits since the beginning of January, steadily accounting for 20%-25% of total visit volume.
Going virtual with gastroenterology
PSJH gastroenterology providers have been a part of this wave, conducting more than 12,000 video visits so far this year (as documented in our Epic EMR), which has been an entirely new method of care delivery for most of these clinicians. We also have many affiliated, private practice gastroenterology providers who practice in our facilities and transitioned quickly to video for outpatient care. Pre- and postprocedure follow-up visits were some of the most common visit types that went virtual, along with new patient visits to establish care and existing patient visits to check in on the status of a health condition, medication, or other concern. Complementary services for gastroenterology patients were transitioned to video over the past 8 months as well. Care management, nutrition services, online support groups, bariatric care information sessions, behavioral health, and more are now available for patients to access virtually.
Remembering it’s not about the tech
New technologies can be challenging to adopt – especially at a pace as rapid as it was this year. Fortunately for PSJH, we had inpatient and outpatient video platforms already in place and an experienced internal telehealth team to scale them quickly to providers and caregivers across system. But even with those advantages, it was still a huge challenge to transition so many providers and caregivers to video visits in such a short time without change management hurdles and bumps along the way.
Too often, there is an overemphasis placed on the technology. It’s a tool, and some technologies are better than others, and they continue to evolve over time. True success or failure lies in the clinical and operational work flows and how well the providers and care teams engage with and adapt them. We found that the providers and staff members willing to venture outside their comfort zone of “how we’ve always done it” and collaborate on the transition to virtual care had the best results. Openness and flexibility to trying new things and using temporary workarounds if existing functionality didn’t meet the need was key to transitioning quickly. Then, by listening to ideas from and sharing feedback among providers, clinics, and geographies, we were able to identify fixes and optimizations that needed to be made to improve the experience for all.
Selecting a video visit platform
No telehealth platform is perfect and meets every patient, provider, and staff need or request despite what a technology vendor may claim. This is especially true in a large and/or diverse system with many different types of clinical use cases. Determining the “must-have” requirements from among those that may be important or simply nice to have is critical when selecting the video visit platform to use.
It’s not an easy decision and nearly impossible to please everyone. Ensuring that there are clinician, operator, and technical stakeholders all contributing to the requirements and decision-making is essential. While some may prefer a “best-of-breed” solution that does one thing very well, it may have to be paired with a set of other complimentary applications to meet all of the organization’s needs. Alternatively, there may be a platform with an expansive feature set but not all of the features are as strong as desired. Then there are solutions that integrate with your existing applications, which is a compelling option to consider.
Regardless of the tool chosen, best-practice work flows, easy-to-follow documentation, a mix of different training options, and internal technical help that responds quickly is key to implementing it successfully. And once implemented, optimization is an ongoing process to make it easier, faster, and better.
Looking ahead
As we came to the end of 2020, all providers and health systems were paying close attention to the Centers for Medicaid & Medicare Services and state-level regulations and reimbursement changes for 2021 to evaluate the impact on telehealth after the public health emergency and COVID-19 waivers are ended. Advocacy efforts are urging lawmakers to not lose the gains that were made during this time and have enabled millions of patients to access care more easily – changes which we believe they will now expect as an option going forward.
We at Providence believe telehealth’s future is a bright one, especially where value-based/managed care arrangements with payers are in place. In addition to integrating video visits and consults into normal clinical practice, we see further growth in serving patients at home with remote patient monitoring and other home-based programs that leverage connected devices and virtual tools. We also anticipate more providers will acquire licenses in other states to virtually care for patients who lack access to specialty services in their own community, which increases access where it is most needed. After 2020, we hope that telehealth will no longer be a specialized service only some patients can receive but a normal way of delivering care to all.
Ms. Winkelman is the system director of telehealth product development and delivery at Providence St. Joseph Health. Providence is the third-largest nonprofit health system in the United States with 51 hospitals, more than 800 clinics, and a comprehensive range of health and social services across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington.
Telehealth exploded into the public consciousness this year as a way for clinicians and patients to safely connect during the COVID-19 crisis. While telehealth has been part of care delivery at Providence St. Joseph Health (PSJH) for more than a decade, it transitioned almost overnight from an offering most often focused on serving patients in rural areas to a way for any patient to get the care they need virtually whether in a hospital, outpatient facility, or from the comfort and safety of their own home.
Telehealth growth was fueled by changes in regulation and reimbursement during the public health emergency enabling providers to see new and established patients at home across all payer types. To put this growth into perspective, the large PSJH system averaged a few thousand video visits per month in January and February 2020. As COVID transmission spread and lockdowns began, that number climbed to over 15,000 video visits in March to a height of more than 150,000 video visits in May. As of the end of October 2020, PSJH has conducted more than 1.2 million video visits since the beginning of January, steadily accounting for 20%-25% of total visit volume.
Going virtual with gastroenterology
PSJH gastroenterology providers have been a part of this wave, conducting more than 12,000 video visits so far this year (as documented in our Epic EMR), which has been an entirely new method of care delivery for most of these clinicians. We also have many affiliated, private practice gastroenterology providers who practice in our facilities and transitioned quickly to video for outpatient care. Pre- and postprocedure follow-up visits were some of the most common visit types that went virtual, along with new patient visits to establish care and existing patient visits to check in on the status of a health condition, medication, or other concern. Complementary services for gastroenterology patients were transitioned to video over the past 8 months as well. Care management, nutrition services, online support groups, bariatric care information sessions, behavioral health, and more are now available for patients to access virtually.
Remembering it’s not about the tech
New technologies can be challenging to adopt – especially at a pace as rapid as it was this year. Fortunately for PSJH, we had inpatient and outpatient video platforms already in place and an experienced internal telehealth team to scale them quickly to providers and caregivers across system. But even with those advantages, it was still a huge challenge to transition so many providers and caregivers to video visits in such a short time without change management hurdles and bumps along the way.
Too often, there is an overemphasis placed on the technology. It’s a tool, and some technologies are better than others, and they continue to evolve over time. True success or failure lies in the clinical and operational work flows and how well the providers and care teams engage with and adapt them. We found that the providers and staff members willing to venture outside their comfort zone of “how we’ve always done it” and collaborate on the transition to virtual care had the best results. Openness and flexibility to trying new things and using temporary workarounds if existing functionality didn’t meet the need was key to transitioning quickly. Then, by listening to ideas from and sharing feedback among providers, clinics, and geographies, we were able to identify fixes and optimizations that needed to be made to improve the experience for all.
Selecting a video visit platform
No telehealth platform is perfect and meets every patient, provider, and staff need or request despite what a technology vendor may claim. This is especially true in a large and/or diverse system with many different types of clinical use cases. Determining the “must-have” requirements from among those that may be important or simply nice to have is critical when selecting the video visit platform to use.
It’s not an easy decision and nearly impossible to please everyone. Ensuring that there are clinician, operator, and technical stakeholders all contributing to the requirements and decision-making is essential. While some may prefer a “best-of-breed” solution that does one thing very well, it may have to be paired with a set of other complimentary applications to meet all of the organization’s needs. Alternatively, there may be a platform with an expansive feature set but not all of the features are as strong as desired. Then there are solutions that integrate with your existing applications, which is a compelling option to consider.
Regardless of the tool chosen, best-practice work flows, easy-to-follow documentation, a mix of different training options, and internal technical help that responds quickly is key to implementing it successfully. And once implemented, optimization is an ongoing process to make it easier, faster, and better.
Looking ahead
As we came to the end of 2020, all providers and health systems were paying close attention to the Centers for Medicaid & Medicare Services and state-level regulations and reimbursement changes for 2021 to evaluate the impact on telehealth after the public health emergency and COVID-19 waivers are ended. Advocacy efforts are urging lawmakers to not lose the gains that were made during this time and have enabled millions of patients to access care more easily – changes which we believe they will now expect as an option going forward.
We at Providence believe telehealth’s future is a bright one, especially where value-based/managed care arrangements with payers are in place. In addition to integrating video visits and consults into normal clinical practice, we see further growth in serving patients at home with remote patient monitoring and other home-based programs that leverage connected devices and virtual tools. We also anticipate more providers will acquire licenses in other states to virtually care for patients who lack access to specialty services in their own community, which increases access where it is most needed. After 2020, we hope that telehealth will no longer be a specialized service only some patients can receive but a normal way of delivering care to all.
Ms. Winkelman is the system director of telehealth product development and delivery at Providence St. Joseph Health. Providence is the third-largest nonprofit health system in the United States with 51 hospitals, more than 800 clinics, and a comprehensive range of health and social services across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington.
Value-based care stunted from delayed Stark and anti-kickback statute reform
Anti-kickback statutes (AKSs) were originally enacted in 1931 to stop Great Depression–era employers from circumventing wage provisions in federal contracts. Since its enactment, AKSs’ main focus has changed and is currently aimed at the health care industry. In addition to AKSs, Stark laws were enacted over 30 years ago to address physician self-referral of Medicare patients. Both laws comprise the government’s main tools for fighting fraud, waste, and abuse.
However, AKSs and Stark laws have not been updated to keep pace with changes in how medical practices do business and care for patients.
Over the years, additional interpretation and clarification has been issued by the Department of Health and Human Services (DHHS) and the Office of Inspector General (OIG). In DHHSs’ June 1, 2012 Advisory Opinion No. 12-06 there is guidance regarding legality of anesthesia services providers’ contract with physician-owned professional corporations or limited liability companies to provide anesthesia services. Specifically, it focused on the “company model” where owners of an ambulatory surgery center (ASC) create a separate company for anesthesia services which directly contracts with anesthesia providers and charges for the anesthesia services while the ASC charges for facility fees. Anyone with specific questions may request an advisory opinion from the OIG about the application of OIG’s fraud and abuse authorities and existing or proposed business arrangements. An OIG advisory opinion is legally binding on the requesting party and DHHS, but not on any other governmental department or agency. While advisory opinions are specific to the entity that requested it and specifically states, “This opinion may not be relied on by any persons other than [name redacted], the requestor of this opinion....” It captured the attention of the medical community. The AGA has argued that this opinion should not be interpreted to mean that all company model frameworks necessarily violate the AKSs and the OIG’s Advisor Opinions FAQ states no person or entity can rely on an advisory opinion issued to someone else. However, Advisory Opinion No. 12-06 has been cited in AKS investigations ever since.
When Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015, it changed how physicians would be paid under Medicare and sought to transition physicians to a more value-based payment system. Physicians were incentivized to develop physician-driven payment models to improve efficiency and patient outcomes. However, existing Stark self-referral laws prohibit physicians from referring patients to an entity in which they have a financial interest. As a result, physician practices are unable to participate in many advanced alternative payment models. Stark laws, which have not been updated since their enactment 30 years ago, pose barriers to care coordination since they prohibit payment arrangements that consider volume or value of referrals or other business generated by the parties. These prohibitions stifle innovations in delivering care by inhibiting practices from incentivizing their physicians to deliver patient care more efficiently, because the practices cannot use resources from designated health services in rewarding or penalizing adherence to new clinical care pathways.
Congress recognized that the Stark law was a barrier to new health care delivery models. Congress, therefore, authorized the HHS Secretary to waive Stark self-referral and anti-kickback laws for accountable care organizations (ACOs). This waiver was not extended to physician-driven alternative payment models (APMs), that also need these exceptions to drive innovation in health care and to implement MACRA law as Congress intended.
AGA and the physician community have long sought to update Stark self-referral and AKSs. Last year, CMS proposed exceptions directed at value-based arrangements that would have allowed providers to participate in value-based arrangements while still protecting the Medicare program from potential abuses. Many of the changes that CMS proposed would have allowed physician practices to engage in value-based arrangements that would improve patient care and AGA provided comments on both the Stark and AKS proposed rules. However, CMS has not yet issued the final rules and has indicated that they will not issue a final rule on Stark which a lost opportunity to improve health care delivery.
On the legislative front, AGA supports S. 2051/H.R. 4206, the Medicare Care Coordination Improvement Act, which would provide CMS with the regulatory authority to create exceptions under the Stark law for APMs and to remove barriers in the current law to the development and operation of such arrangements. The legislation would allow CMS to waive the Stark laws for physicians seeking to develop and operate APMs similar to what Congress allowed for ACOs. The legislation would allow innovative payment models developed by gastroenterologists to be implemented in the Medicare program. Unfortunately, this legislation has received little traction in Congress.
Until meaningful regulatory and legislative reform updating both Stark and AKS occur, innovative payment models must wait and gastroenterologists and other providers will remain vulnerable to these outdated regulations. You can help us advance these issues by sharing how they impact your practice. Tell us what types of value-based arrangements you would participate in and how would they improve patient care and efficacy at [email protected].
Dr. Losurdo is the AGA’s Alternate Advisor to the American Medical Association’s CPT Editorial Panel, a member of the AGA Practice Management and Economics Committee’s Coverage and Reimbursement Subcommittee and is a partner with Elgin Gastro Endoscopy, who owns and ASC, and Managing Partner and Medical Director of Illinois Gastroenterology Group/GI Alliance, Elgin, Ill.
This story was updated on 12/11/2020.
Anti-kickback statutes (AKSs) were originally enacted in 1931 to stop Great Depression–era employers from circumventing wage provisions in federal contracts. Since its enactment, AKSs’ main focus has changed and is currently aimed at the health care industry. In addition to AKSs, Stark laws were enacted over 30 years ago to address physician self-referral of Medicare patients. Both laws comprise the government’s main tools for fighting fraud, waste, and abuse.
However, AKSs and Stark laws have not been updated to keep pace with changes in how medical practices do business and care for patients.
Over the years, additional interpretation and clarification has been issued by the Department of Health and Human Services (DHHS) and the Office of Inspector General (OIG). In DHHSs’ June 1, 2012 Advisory Opinion No. 12-06 there is guidance regarding legality of anesthesia services providers’ contract with physician-owned professional corporations or limited liability companies to provide anesthesia services. Specifically, it focused on the “company model” where owners of an ambulatory surgery center (ASC) create a separate company for anesthesia services which directly contracts with anesthesia providers and charges for the anesthesia services while the ASC charges for facility fees. Anyone with specific questions may request an advisory opinion from the OIG about the application of OIG’s fraud and abuse authorities and existing or proposed business arrangements. An OIG advisory opinion is legally binding on the requesting party and DHHS, but not on any other governmental department or agency. While advisory opinions are specific to the entity that requested it and specifically states, “This opinion may not be relied on by any persons other than [name redacted], the requestor of this opinion....” It captured the attention of the medical community. The AGA has argued that this opinion should not be interpreted to mean that all company model frameworks necessarily violate the AKSs and the OIG’s Advisor Opinions FAQ states no person or entity can rely on an advisory opinion issued to someone else. However, Advisory Opinion No. 12-06 has been cited in AKS investigations ever since.
When Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015, it changed how physicians would be paid under Medicare and sought to transition physicians to a more value-based payment system. Physicians were incentivized to develop physician-driven payment models to improve efficiency and patient outcomes. However, existing Stark self-referral laws prohibit physicians from referring patients to an entity in which they have a financial interest. As a result, physician practices are unable to participate in many advanced alternative payment models. Stark laws, which have not been updated since their enactment 30 years ago, pose barriers to care coordination since they prohibit payment arrangements that consider volume or value of referrals or other business generated by the parties. These prohibitions stifle innovations in delivering care by inhibiting practices from incentivizing their physicians to deliver patient care more efficiently, because the practices cannot use resources from designated health services in rewarding or penalizing adherence to new clinical care pathways.
Congress recognized that the Stark law was a barrier to new health care delivery models. Congress, therefore, authorized the HHS Secretary to waive Stark self-referral and anti-kickback laws for accountable care organizations (ACOs). This waiver was not extended to physician-driven alternative payment models (APMs), that also need these exceptions to drive innovation in health care and to implement MACRA law as Congress intended.
AGA and the physician community have long sought to update Stark self-referral and AKSs. Last year, CMS proposed exceptions directed at value-based arrangements that would have allowed providers to participate in value-based arrangements while still protecting the Medicare program from potential abuses. Many of the changes that CMS proposed would have allowed physician practices to engage in value-based arrangements that would improve patient care and AGA provided comments on both the Stark and AKS proposed rules. However, CMS has not yet issued the final rules and has indicated that they will not issue a final rule on Stark which a lost opportunity to improve health care delivery.
On the legislative front, AGA supports S. 2051/H.R. 4206, the Medicare Care Coordination Improvement Act, which would provide CMS with the regulatory authority to create exceptions under the Stark law for APMs and to remove barriers in the current law to the development and operation of such arrangements. The legislation would allow CMS to waive the Stark laws for physicians seeking to develop and operate APMs similar to what Congress allowed for ACOs. The legislation would allow innovative payment models developed by gastroenterologists to be implemented in the Medicare program. Unfortunately, this legislation has received little traction in Congress.
Until meaningful regulatory and legislative reform updating both Stark and AKS occur, innovative payment models must wait and gastroenterologists and other providers will remain vulnerable to these outdated regulations. You can help us advance these issues by sharing how they impact your practice. Tell us what types of value-based arrangements you would participate in and how would they improve patient care and efficacy at [email protected].
Dr. Losurdo is the AGA’s Alternate Advisor to the American Medical Association’s CPT Editorial Panel, a member of the AGA Practice Management and Economics Committee’s Coverage and Reimbursement Subcommittee and is a partner with Elgin Gastro Endoscopy, who owns and ASC, and Managing Partner and Medical Director of Illinois Gastroenterology Group/GI Alliance, Elgin, Ill.
This story was updated on 12/11/2020.
Anti-kickback statutes (AKSs) were originally enacted in 1931 to stop Great Depression–era employers from circumventing wage provisions in federal contracts. Since its enactment, AKSs’ main focus has changed and is currently aimed at the health care industry. In addition to AKSs, Stark laws were enacted over 30 years ago to address physician self-referral of Medicare patients. Both laws comprise the government’s main tools for fighting fraud, waste, and abuse.
However, AKSs and Stark laws have not been updated to keep pace with changes in how medical practices do business and care for patients.
Over the years, additional interpretation and clarification has been issued by the Department of Health and Human Services (DHHS) and the Office of Inspector General (OIG). In DHHSs’ June 1, 2012 Advisory Opinion No. 12-06 there is guidance regarding legality of anesthesia services providers’ contract with physician-owned professional corporations or limited liability companies to provide anesthesia services. Specifically, it focused on the “company model” where owners of an ambulatory surgery center (ASC) create a separate company for anesthesia services which directly contracts with anesthesia providers and charges for the anesthesia services while the ASC charges for facility fees. Anyone with specific questions may request an advisory opinion from the OIG about the application of OIG’s fraud and abuse authorities and existing or proposed business arrangements. An OIG advisory opinion is legally binding on the requesting party and DHHS, but not on any other governmental department or agency. While advisory opinions are specific to the entity that requested it and specifically states, “This opinion may not be relied on by any persons other than [name redacted], the requestor of this opinion....” It captured the attention of the medical community. The AGA has argued that this opinion should not be interpreted to mean that all company model frameworks necessarily violate the AKSs and the OIG’s Advisor Opinions FAQ states no person or entity can rely on an advisory opinion issued to someone else. However, Advisory Opinion No. 12-06 has been cited in AKS investigations ever since.
When Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) in 2015, it changed how physicians would be paid under Medicare and sought to transition physicians to a more value-based payment system. Physicians were incentivized to develop physician-driven payment models to improve efficiency and patient outcomes. However, existing Stark self-referral laws prohibit physicians from referring patients to an entity in which they have a financial interest. As a result, physician practices are unable to participate in many advanced alternative payment models. Stark laws, which have not been updated since their enactment 30 years ago, pose barriers to care coordination since they prohibit payment arrangements that consider volume or value of referrals or other business generated by the parties. These prohibitions stifle innovations in delivering care by inhibiting practices from incentivizing their physicians to deliver patient care more efficiently, because the practices cannot use resources from designated health services in rewarding or penalizing adherence to new clinical care pathways.
Congress recognized that the Stark law was a barrier to new health care delivery models. Congress, therefore, authorized the HHS Secretary to waive Stark self-referral and anti-kickback laws for accountable care organizations (ACOs). This waiver was not extended to physician-driven alternative payment models (APMs), that also need these exceptions to drive innovation in health care and to implement MACRA law as Congress intended.
AGA and the physician community have long sought to update Stark self-referral and AKSs. Last year, CMS proposed exceptions directed at value-based arrangements that would have allowed providers to participate in value-based arrangements while still protecting the Medicare program from potential abuses. Many of the changes that CMS proposed would have allowed physician practices to engage in value-based arrangements that would improve patient care and AGA provided comments on both the Stark and AKS proposed rules. However, CMS has not yet issued the final rules and has indicated that they will not issue a final rule on Stark which a lost opportunity to improve health care delivery.
On the legislative front, AGA supports S. 2051/H.R. 4206, the Medicare Care Coordination Improvement Act, which would provide CMS with the regulatory authority to create exceptions under the Stark law for APMs and to remove barriers in the current law to the development and operation of such arrangements. The legislation would allow CMS to waive the Stark laws for physicians seeking to develop and operate APMs similar to what Congress allowed for ACOs. The legislation would allow innovative payment models developed by gastroenterologists to be implemented in the Medicare program. Unfortunately, this legislation has received little traction in Congress.
Until meaningful regulatory and legislative reform updating both Stark and AKS occur, innovative payment models must wait and gastroenterologists and other providers will remain vulnerable to these outdated regulations. You can help us advance these issues by sharing how they impact your practice. Tell us what types of value-based arrangements you would participate in and how would they improve patient care and efficacy at [email protected].
Dr. Losurdo is the AGA’s Alternate Advisor to the American Medical Association’s CPT Editorial Panel, a member of the AGA Practice Management and Economics Committee’s Coverage and Reimbursement Subcommittee and is a partner with Elgin Gastro Endoscopy, who owns and ASC, and Managing Partner and Medical Director of Illinois Gastroenterology Group/GI Alliance, Elgin, Ill.
This story was updated on 12/11/2020.
The 2021 proposed Medicare fee schedule: Can the payment cuts be avoided?
Payment cuts to nearly all of medicine, including gastroenterology, could be in store beginning Jan. 1, 2021. Physicians may also face elimination of some services the Centers for Medicare & Medicaid Services granted temporary access to during the coronavirus (COVID-19) pandemic according to CMS’s recently released policy and payment recommendations. These proposals could be implemented as physician practices are still recovering financially from states’ temporary ban on elective surgeries from March through May 2020 in response to the public health emergency (PHE) and continuing to deal with the clinical and financial challenges of the pandemic.
In early August, CMS proposed a number of changes for 2021 that affect physicians. There’s plenty of good, bad, and ugly in this proposed rule.
Let’s start with two positives (The good):
Medicare proposes to maintain the current values for colonoscopy with biopsy (45385) and esophagogastroduodenoscopy (EGD) with biopsy (43239). Despite a recent reevaluation of these codes in 2016 and 2014, respectively, Medicare conceded to Anthem’s suggestion that the procedures were not overvalued and needed another evaluation. The AGA and our sister societies’ data affirmed the current values and Medicare proposed to maintain them in 2021.
Medicare proposes to increase the price for scope video system equipment (ES031) from $36,306 to $70,673.38 and the suction machine (Gomco) (EQ235) from $1,981.66 to $3,195.85, phased in over 2 years. This will provide a small increase in the practice expense value for all GI endoscopy procedures. Since CMS began conducting a review of scope systems in 2017, the AGA and our sister societies have successfully worked to convince the Agency to increase its payment for GI endoscopes and associated equipment by providing invoices. We are pleased Medicare is updating these items to reflect more accurate costs.
Now onto items that could negatively affect the practice of gastroenterology.
The bad
Medicare proposes to stop covering and paying for telephone evaluation and management (E/M) visits as soon as the COVID-19 PHE expires. After originally denying that Medicare beneficiaries had trouble accessing video E/M visits and refusing to cover existing telephone (audio only) E/M codes 99441-99443, the agency responded to enormous pressure from AGA and other specialties and added the codes to its covered telehealth services list, setting the payment equal to office/outpatient established patient E/M codes 99212-99214 during the PHE. Telephone E/M has been a vital lifeline, allowing Medicare beneficiaries who don’t have a smart phone or reliable internet connection to access needed E/M services, while allowing them to stay safe at home during the PHE. There is evidence that our most vulnerable patients have the greatest need for telephone visits to advance their care.1
Medicare’s proposal to stop covering and paying for telephone E/M visits as soon as the COVID-19 PHE expires, while disappointing, is not surprising because of the agency’s reluctance to admit they were needed in the first place. The agency believes that creating a new code for audio-only patient interactions similar to the virtual check-in code G2012 but for a longer unit of time and with an accordingly higher value will suffice. Physicians appreciate that E/M delivered via telephone is not the same as a check-in call to a patient, and the care provided requires similar time, effort, and cognitive load as video visits. The AGA and our sister societies plan to object to Medicare’s proposal to treat these services as “check-ins” with slightly higher payment and will continue to advocate for permanent coverage of the telephone E/M CPT codes and payment parity with in-person E/M visits.
The ugly
The Medicare Physician Fee Schedule (MPFS) conversion factor, the basis of Medicare payments, is proposed to be cut almost 11% percent from $36.09 in 2020 to $32.26 in 2021.
How it happened
Medicare agreed to implement coding and valuation changes to office and outpatient E/M codes (99202-99205, 99211-99215) in 2021 as recommended by the American Medical Association and widely supported by specialty societies. E/M services account for about 40% of all Medicare spending annually, which magnifies the impact of any changes to their relative value units (RVUs). By law, payment increases that occur from new work RVUs must be offset by a reduction, referred to as a budget-neutral adjustment, applied to offset the increase in total spending on the MPFS.2
CMS explained in the 2021 MPFS proposed rule, “If revisions to the RVUs cause expenditures for the year to change by more than $20 million, we make adjustments to ensure that expenditures do not increase or decrease by more than $20 million.” Medicare calculated that the corresponding adjustment to the conversion factor for 2021 needed to fall by nearly 11% to achieve budget neutrality. Because gastroenterologists report a significant portion of E/M in addition to performing procedures, the overall estimated impact is –5% of all reimbursement from Medicare.
What you can do
Visit the AGA Advocacy Action Center at https://gastro.quorum.us/AGAactioncenter/ and select “Fight back against CMS’s cuts to specialty care payments” to tell your lawmakers to stop these cuts and preserve care for patients by waiving Medicare’s budget neutrality requirements for E/M adjustments.
You can also use the AGA’s Medicare Physician Fee Schedule Calculator tool to determine the effect of the proposed cuts.3 By contacting AGA staff, Leslie Narramore, at [email protected] with the overall effect on your practice, you can help AGA use these data as we work with the physician community to urge Congress to prevent these payment cuts.
What AGA is doing
The AGA and our sister societies have joined the AMA and others in urging Congress and CMS to waive budget-neutrality rules for the implementation of the changes in E/M services effective 2021. We also joined with AMA and over 100 specialty societies in a letter asking Secretary of Health & Human Services Alex Azar that the agency use its authority under the public health emergency declaration to waive budget neutrality for the changes, given these difficult times for practices across the country.
What next steps to take
The AGA and our sister societies are developing comment letters in response to the proposals in the 2021 MPFS proposed rule. Medicare plans to publish its final decisions for 2021 in December. Please do your part by visiting the AGA Advocacy Action Center at https://gastro.quorum.us/AGAactioncenter/ to tell your lawmakers to stop the proposed 2021 payment cuts and preserve care for patients by waiving Medicare’s budget-neutrality requirements for E/M adjustments.
References
1. Serper M et al. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic [published online ahead of print, 2020 Jun 18]. Gastroenterology. 2020;S0016-5085(20)34834-4. doi: 10.1053/j.gastro.2020.06.034.
2. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.
3. https://gastro.org/news/prepare-for-and-help-prevent-2021-medicare-cuts-to-gi/.
Dr. Gangarosa is professor of medicine, division of gastroenterology and hepatology, University of North Carolina at Chapel Hill School of Medicine, and chair of the AGA Government Affairs Committee; Dr. Mehta is associate chief innovation officer at Penn Medicine, Philadelphia, a gastroenterologist, assistant professor of medicine at the Perelman School of Medicine, senior fellow at the Leonard Davis Institute of Health Economics, affiliated faculty member at the Center for Health Incentives and Behavioral Economics, and AGA RUC Adviser. They have no conflicts of interest.
Payment cuts to nearly all of medicine, including gastroenterology, could be in store beginning Jan. 1, 2021. Physicians may also face elimination of some services the Centers for Medicare & Medicaid Services granted temporary access to during the coronavirus (COVID-19) pandemic according to CMS’s recently released policy and payment recommendations. These proposals could be implemented as physician practices are still recovering financially from states’ temporary ban on elective surgeries from March through May 2020 in response to the public health emergency (PHE) and continuing to deal with the clinical and financial challenges of the pandemic.
In early August, CMS proposed a number of changes for 2021 that affect physicians. There’s plenty of good, bad, and ugly in this proposed rule.
Let’s start with two positives (The good):
Medicare proposes to maintain the current values for colonoscopy with biopsy (45385) and esophagogastroduodenoscopy (EGD) with biopsy (43239). Despite a recent reevaluation of these codes in 2016 and 2014, respectively, Medicare conceded to Anthem’s suggestion that the procedures were not overvalued and needed another evaluation. The AGA and our sister societies’ data affirmed the current values and Medicare proposed to maintain them in 2021.
Medicare proposes to increase the price for scope video system equipment (ES031) from $36,306 to $70,673.38 and the suction machine (Gomco) (EQ235) from $1,981.66 to $3,195.85, phased in over 2 years. This will provide a small increase in the practice expense value for all GI endoscopy procedures. Since CMS began conducting a review of scope systems in 2017, the AGA and our sister societies have successfully worked to convince the Agency to increase its payment for GI endoscopes and associated equipment by providing invoices. We are pleased Medicare is updating these items to reflect more accurate costs.
Now onto items that could negatively affect the practice of gastroenterology.
The bad
Medicare proposes to stop covering and paying for telephone evaluation and management (E/M) visits as soon as the COVID-19 PHE expires. After originally denying that Medicare beneficiaries had trouble accessing video E/M visits and refusing to cover existing telephone (audio only) E/M codes 99441-99443, the agency responded to enormous pressure from AGA and other specialties and added the codes to its covered telehealth services list, setting the payment equal to office/outpatient established patient E/M codes 99212-99214 during the PHE. Telephone E/M has been a vital lifeline, allowing Medicare beneficiaries who don’t have a smart phone or reliable internet connection to access needed E/M services, while allowing them to stay safe at home during the PHE. There is evidence that our most vulnerable patients have the greatest need for telephone visits to advance their care.1
Medicare’s proposal to stop covering and paying for telephone E/M visits as soon as the COVID-19 PHE expires, while disappointing, is not surprising because of the agency’s reluctance to admit they were needed in the first place. The agency believes that creating a new code for audio-only patient interactions similar to the virtual check-in code G2012 but for a longer unit of time and with an accordingly higher value will suffice. Physicians appreciate that E/M delivered via telephone is not the same as a check-in call to a patient, and the care provided requires similar time, effort, and cognitive load as video visits. The AGA and our sister societies plan to object to Medicare’s proposal to treat these services as “check-ins” with slightly higher payment and will continue to advocate for permanent coverage of the telephone E/M CPT codes and payment parity with in-person E/M visits.
The ugly
The Medicare Physician Fee Schedule (MPFS) conversion factor, the basis of Medicare payments, is proposed to be cut almost 11% percent from $36.09 in 2020 to $32.26 in 2021.
How it happened
Medicare agreed to implement coding and valuation changes to office and outpatient E/M codes (99202-99205, 99211-99215) in 2021 as recommended by the American Medical Association and widely supported by specialty societies. E/M services account for about 40% of all Medicare spending annually, which magnifies the impact of any changes to their relative value units (RVUs). By law, payment increases that occur from new work RVUs must be offset by a reduction, referred to as a budget-neutral adjustment, applied to offset the increase in total spending on the MPFS.2
CMS explained in the 2021 MPFS proposed rule, “If revisions to the RVUs cause expenditures for the year to change by more than $20 million, we make adjustments to ensure that expenditures do not increase or decrease by more than $20 million.” Medicare calculated that the corresponding adjustment to the conversion factor for 2021 needed to fall by nearly 11% to achieve budget neutrality. Because gastroenterologists report a significant portion of E/M in addition to performing procedures, the overall estimated impact is –5% of all reimbursement from Medicare.
What you can do
Visit the AGA Advocacy Action Center at https://gastro.quorum.us/AGAactioncenter/ and select “Fight back against CMS’s cuts to specialty care payments” to tell your lawmakers to stop these cuts and preserve care for patients by waiving Medicare’s budget neutrality requirements for E/M adjustments.
You can also use the AGA’s Medicare Physician Fee Schedule Calculator tool to determine the effect of the proposed cuts.3 By contacting AGA staff, Leslie Narramore, at [email protected] with the overall effect on your practice, you can help AGA use these data as we work with the physician community to urge Congress to prevent these payment cuts.
What AGA is doing
The AGA and our sister societies have joined the AMA and others in urging Congress and CMS to waive budget-neutrality rules for the implementation of the changes in E/M services effective 2021. We also joined with AMA and over 100 specialty societies in a letter asking Secretary of Health & Human Services Alex Azar that the agency use its authority under the public health emergency declaration to waive budget neutrality for the changes, given these difficult times for practices across the country.
What next steps to take
The AGA and our sister societies are developing comment letters in response to the proposals in the 2021 MPFS proposed rule. Medicare plans to publish its final decisions for 2021 in December. Please do your part by visiting the AGA Advocacy Action Center at https://gastro.quorum.us/AGAactioncenter/ to tell your lawmakers to stop the proposed 2021 payment cuts and preserve care for patients by waiving Medicare’s budget-neutrality requirements for E/M adjustments.
References
1. Serper M et al. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic [published online ahead of print, 2020 Jun 18]. Gastroenterology. 2020;S0016-5085(20)34834-4. doi: 10.1053/j.gastro.2020.06.034.
2. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.
3. https://gastro.org/news/prepare-for-and-help-prevent-2021-medicare-cuts-to-gi/.
Dr. Gangarosa is professor of medicine, division of gastroenterology and hepatology, University of North Carolina at Chapel Hill School of Medicine, and chair of the AGA Government Affairs Committee; Dr. Mehta is associate chief innovation officer at Penn Medicine, Philadelphia, a gastroenterologist, assistant professor of medicine at the Perelman School of Medicine, senior fellow at the Leonard Davis Institute of Health Economics, affiliated faculty member at the Center for Health Incentives and Behavioral Economics, and AGA RUC Adviser. They have no conflicts of interest.
Payment cuts to nearly all of medicine, including gastroenterology, could be in store beginning Jan. 1, 2021. Physicians may also face elimination of some services the Centers for Medicare & Medicaid Services granted temporary access to during the coronavirus (COVID-19) pandemic according to CMS’s recently released policy and payment recommendations. These proposals could be implemented as physician practices are still recovering financially from states’ temporary ban on elective surgeries from March through May 2020 in response to the public health emergency (PHE) and continuing to deal with the clinical and financial challenges of the pandemic.
In early August, CMS proposed a number of changes for 2021 that affect physicians. There’s plenty of good, bad, and ugly in this proposed rule.
Let’s start with two positives (The good):
Medicare proposes to maintain the current values for colonoscopy with biopsy (45385) and esophagogastroduodenoscopy (EGD) with biopsy (43239). Despite a recent reevaluation of these codes in 2016 and 2014, respectively, Medicare conceded to Anthem’s suggestion that the procedures were not overvalued and needed another evaluation. The AGA and our sister societies’ data affirmed the current values and Medicare proposed to maintain them in 2021.
Medicare proposes to increase the price for scope video system equipment (ES031) from $36,306 to $70,673.38 and the suction machine (Gomco) (EQ235) from $1,981.66 to $3,195.85, phased in over 2 years. This will provide a small increase in the practice expense value for all GI endoscopy procedures. Since CMS began conducting a review of scope systems in 2017, the AGA and our sister societies have successfully worked to convince the Agency to increase its payment for GI endoscopes and associated equipment by providing invoices. We are pleased Medicare is updating these items to reflect more accurate costs.
Now onto items that could negatively affect the practice of gastroenterology.
The bad
Medicare proposes to stop covering and paying for telephone evaluation and management (E/M) visits as soon as the COVID-19 PHE expires. After originally denying that Medicare beneficiaries had trouble accessing video E/M visits and refusing to cover existing telephone (audio only) E/M codes 99441-99443, the agency responded to enormous pressure from AGA and other specialties and added the codes to its covered telehealth services list, setting the payment equal to office/outpatient established patient E/M codes 99212-99214 during the PHE. Telephone E/M has been a vital lifeline, allowing Medicare beneficiaries who don’t have a smart phone or reliable internet connection to access needed E/M services, while allowing them to stay safe at home during the PHE. There is evidence that our most vulnerable patients have the greatest need for telephone visits to advance their care.1
Medicare’s proposal to stop covering and paying for telephone E/M visits as soon as the COVID-19 PHE expires, while disappointing, is not surprising because of the agency’s reluctance to admit they were needed in the first place. The agency believes that creating a new code for audio-only patient interactions similar to the virtual check-in code G2012 but for a longer unit of time and with an accordingly higher value will suffice. Physicians appreciate that E/M delivered via telephone is not the same as a check-in call to a patient, and the care provided requires similar time, effort, and cognitive load as video visits. The AGA and our sister societies plan to object to Medicare’s proposal to treat these services as “check-ins” with slightly higher payment and will continue to advocate for permanent coverage of the telephone E/M CPT codes and payment parity with in-person E/M visits.
The ugly
The Medicare Physician Fee Schedule (MPFS) conversion factor, the basis of Medicare payments, is proposed to be cut almost 11% percent from $36.09 in 2020 to $32.26 in 2021.
How it happened
Medicare agreed to implement coding and valuation changes to office and outpatient E/M codes (99202-99205, 99211-99215) in 2021 as recommended by the American Medical Association and widely supported by specialty societies. E/M services account for about 40% of all Medicare spending annually, which magnifies the impact of any changes to their relative value units (RVUs). By law, payment increases that occur from new work RVUs must be offset by a reduction, referred to as a budget-neutral adjustment, applied to offset the increase in total spending on the MPFS.2
CMS explained in the 2021 MPFS proposed rule, “If revisions to the RVUs cause expenditures for the year to change by more than $20 million, we make adjustments to ensure that expenditures do not increase or decrease by more than $20 million.” Medicare calculated that the corresponding adjustment to the conversion factor for 2021 needed to fall by nearly 11% to achieve budget neutrality. Because gastroenterologists report a significant portion of E/M in addition to performing procedures, the overall estimated impact is –5% of all reimbursement from Medicare.
What you can do
Visit the AGA Advocacy Action Center at https://gastro.quorum.us/AGAactioncenter/ and select “Fight back against CMS’s cuts to specialty care payments” to tell your lawmakers to stop these cuts and preserve care for patients by waiving Medicare’s budget neutrality requirements for E/M adjustments.
You can also use the AGA’s Medicare Physician Fee Schedule Calculator tool to determine the effect of the proposed cuts.3 By contacting AGA staff, Leslie Narramore, at [email protected] with the overall effect on your practice, you can help AGA use these data as we work with the physician community to urge Congress to prevent these payment cuts.
What AGA is doing
The AGA and our sister societies have joined the AMA and others in urging Congress and CMS to waive budget-neutrality rules for the implementation of the changes in E/M services effective 2021. We also joined with AMA and over 100 specialty societies in a letter asking Secretary of Health & Human Services Alex Azar that the agency use its authority under the public health emergency declaration to waive budget neutrality for the changes, given these difficult times for practices across the country.
What next steps to take
The AGA and our sister societies are developing comment letters in response to the proposals in the 2021 MPFS proposed rule. Medicare plans to publish its final decisions for 2021 in December. Please do your part by visiting the AGA Advocacy Action Center at https://gastro.quorum.us/AGAactioncenter/ to tell your lawmakers to stop the proposed 2021 payment cuts and preserve care for patients by waiving Medicare’s budget-neutrality requirements for E/M adjustments.
References
1. Serper M et al. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic [published online ahead of print, 2020 Jun 18]. Gastroenterology. 2020;S0016-5085(20)34834-4. doi: 10.1053/j.gastro.2020.06.034.
2. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.
3. https://gastro.org/news/prepare-for-and-help-prevent-2021-medicare-cuts-to-gi/.
Dr. Gangarosa is professor of medicine, division of gastroenterology and hepatology, University of North Carolina at Chapel Hill School of Medicine, and chair of the AGA Government Affairs Committee; Dr. Mehta is associate chief innovation officer at Penn Medicine, Philadelphia, a gastroenterologist, assistant professor of medicine at the Perelman School of Medicine, senior fellow at the Leonard Davis Institute of Health Economics, affiliated faculty member at the Center for Health Incentives and Behavioral Economics, and AGA RUC Adviser. They have no conflicts of interest.
Private practice to private equity–backed MSO – Perspectives from the United Digestive team: Part 2
Author’s note: In December 2018, Atlanta Gastroenterology Associates partnered with Frazier Healthcare Partners to form the practice management company United Digestive (UD). Since that time, colleagues across the country have evaluated their own private equity prospects and partnerships, as well as monitored the progress of our transition.
So how are things going? Enjoy part two of this two-part article where we reached out to several team members from all levels within the organization and asked them to share their personal experiences – both highlights and challenges – during UD’s first year.
Did you miss Part 1? Don’t worry, you can read Part 1 here (https://www.mdedge.com/gihepnews/practice-management-toolbox).
There are several private equity–backed GI practice management groups across the country. Why did you and your colleagues decide to partner with UD last year, and, how is the relationship going to date?
Mark Murphy, MD, UD Physician Executive Committee Member Center for Digestive and Liver Health in Savannah, Ga.
- “We previously investigated other partnerships but felt they really did not bring enough value to make our group stronger or more viable. United Digestive was different. The idea of partnering with like-minded gastroenterologists to become a larger, single-specialty entity, with contract negotiation leverage and economies of scale was appealing and would not be possible as a 10-person group. Further, the partnership represented an opportunity to eliminate debt, minimize future risk to younger partners, and yet also embrace an ability to add new services and physicians.
“There were expected hiccups in the beginning: specifically IT and HR issues, which were remedied appropriately and timely. One month after the partnership was completed, reports started coming out of China about a new viral illness – an illness that telescoped our perspective on the consequences of our decision into a timeline of months rather than years.
“UD’s response to the COVID-19 epidemic has been phenomenal. The organization made the tough, but proper clinical calls that limited risks to patients and staff. They came up with a game plan to salvage fiscal viability – rolling out telemedicine in a matter of days and establishing the manner in which patients with high acuity could still be seen and cared for expediently.
“As a solo GI practice, we would have struggled mightily to survive and might have gone bankrupt. Had we been part of a larger non-GI entity (a hospital or multispecialty group), we might have been pressured to engage in unsafe or unethical practices and not consistent with national societal recommendations. Instead, we found ourselves having active discussions with our GI colleagues about the right path forward.”
How do you feel UD has helped improve the quality of patient care and positively impacted patient satisfaction?
Aja McCutchen, MD
- “Prior to UD, we worked diligently to improve our centralized patient service center, phone trees, and optimize the time and communication between patients, providers, and our staff. We now have tools which help identify and track gaps in communication on all levels. We have been able to improve our MA work flow, shorten wait times, and improve the direct dialogue between our practice and our patients. We have also been able to enhance our ancillary service offerings and expand programs that directly benefit our patients.”
Kimberly Orleck, PA-C
- “I think our quality of care has always been top notch and that thankfully has not been altered. UD has concentrated on workflow optimization, enhanced training to our frontline teams, and improved scheduled processes to decrease patient wait time. UD is also paying closer attention to patient ratings, reviews, and calculating net promotor scores. ”
Have there been any initiatives in the first year which improved the management of the organization?
Elizabeth Escalante, Senior Regional Director of Operations, UD
- “Implementation of a business analytics tool was huge this year. It greatly improved visibility into the information we need to have at our fingertips in order to make data-driven decisions for our business. Drilling this down to the frontline manager has increased our understanding of what it truly takes to run a successful practice, and in turn, increased stakeholder buy-in.”
Lakeeta White, Clinical Office Team Lead, and Alexis Sweeney, Medical Assistant
- “The formation of our MA Advisory Committee has been instrumental in helping standardize best practices across the organization. It is comprised of medical assistants across our geographic footprint, and they provide feedback to the management team regarding process improvements, areas for continued training, and more.”
Though many positives may arise out of change, so can some challenges. Have there been any unforeseen hurdles you experience as a result of the new partnership with PE?
Elizabeth Escalante
- “Overall, I believe the changes to the structure of the practice and reorganization of leadership has been positive. As with any organization, one area of improvement is in communication.”
Dr. Patel and Dr. Sonenshine are with Atlanta Gastroenterology Associates, which is part of United Digestive. They have no conflicts.
Author’s note: In December 2018, Atlanta Gastroenterology Associates partnered with Frazier Healthcare Partners to form the practice management company United Digestive (UD). Since that time, colleagues across the country have evaluated their own private equity prospects and partnerships, as well as monitored the progress of our transition.
So how are things going? Enjoy part two of this two-part article where we reached out to several team members from all levels within the organization and asked them to share their personal experiences – both highlights and challenges – during UD’s first year.
Did you miss Part 1? Don’t worry, you can read Part 1 here (https://www.mdedge.com/gihepnews/practice-management-toolbox).
There are several private equity–backed GI practice management groups across the country. Why did you and your colleagues decide to partner with UD last year, and, how is the relationship going to date?
Mark Murphy, MD, UD Physician Executive Committee Member Center for Digestive and Liver Health in Savannah, Ga.
- “We previously investigated other partnerships but felt they really did not bring enough value to make our group stronger or more viable. United Digestive was different. The idea of partnering with like-minded gastroenterologists to become a larger, single-specialty entity, with contract negotiation leverage and economies of scale was appealing and would not be possible as a 10-person group. Further, the partnership represented an opportunity to eliminate debt, minimize future risk to younger partners, and yet also embrace an ability to add new services and physicians.
“There were expected hiccups in the beginning: specifically IT and HR issues, which were remedied appropriately and timely. One month after the partnership was completed, reports started coming out of China about a new viral illness – an illness that telescoped our perspective on the consequences of our decision into a timeline of months rather than years.
“UD’s response to the COVID-19 epidemic has been phenomenal. The organization made the tough, but proper clinical calls that limited risks to patients and staff. They came up with a game plan to salvage fiscal viability – rolling out telemedicine in a matter of days and establishing the manner in which patients with high acuity could still be seen and cared for expediently.
“As a solo GI practice, we would have struggled mightily to survive and might have gone bankrupt. Had we been part of a larger non-GI entity (a hospital or multispecialty group), we might have been pressured to engage in unsafe or unethical practices and not consistent with national societal recommendations. Instead, we found ourselves having active discussions with our GI colleagues about the right path forward.”
How do you feel UD has helped improve the quality of patient care and positively impacted patient satisfaction?
Aja McCutchen, MD
- “Prior to UD, we worked diligently to improve our centralized patient service center, phone trees, and optimize the time and communication between patients, providers, and our staff. We now have tools which help identify and track gaps in communication on all levels. We have been able to improve our MA work flow, shorten wait times, and improve the direct dialogue between our practice and our patients. We have also been able to enhance our ancillary service offerings and expand programs that directly benefit our patients.”
Kimberly Orleck, PA-C
- “I think our quality of care has always been top notch and that thankfully has not been altered. UD has concentrated on workflow optimization, enhanced training to our frontline teams, and improved scheduled processes to decrease patient wait time. UD is also paying closer attention to patient ratings, reviews, and calculating net promotor scores. ”
Have there been any initiatives in the first year which improved the management of the organization?
Elizabeth Escalante, Senior Regional Director of Operations, UD
- “Implementation of a business analytics tool was huge this year. It greatly improved visibility into the information we need to have at our fingertips in order to make data-driven decisions for our business. Drilling this down to the frontline manager has increased our understanding of what it truly takes to run a successful practice, and in turn, increased stakeholder buy-in.”
Lakeeta White, Clinical Office Team Lead, and Alexis Sweeney, Medical Assistant
- “The formation of our MA Advisory Committee has been instrumental in helping standardize best practices across the organization. It is comprised of medical assistants across our geographic footprint, and they provide feedback to the management team regarding process improvements, areas for continued training, and more.”
Though many positives may arise out of change, so can some challenges. Have there been any unforeseen hurdles you experience as a result of the new partnership with PE?
Elizabeth Escalante
- “Overall, I believe the changes to the structure of the practice and reorganization of leadership has been positive. As with any organization, one area of improvement is in communication.”
Dr. Patel and Dr. Sonenshine are with Atlanta Gastroenterology Associates, which is part of United Digestive. They have no conflicts.
Author’s note: In December 2018, Atlanta Gastroenterology Associates partnered with Frazier Healthcare Partners to form the practice management company United Digestive (UD). Since that time, colleagues across the country have evaluated their own private equity prospects and partnerships, as well as monitored the progress of our transition.
So how are things going? Enjoy part two of this two-part article where we reached out to several team members from all levels within the organization and asked them to share their personal experiences – both highlights and challenges – during UD’s first year.
Did you miss Part 1? Don’t worry, you can read Part 1 here (https://www.mdedge.com/gihepnews/practice-management-toolbox).
There are several private equity–backed GI practice management groups across the country. Why did you and your colleagues decide to partner with UD last year, and, how is the relationship going to date?
Mark Murphy, MD, UD Physician Executive Committee Member Center for Digestive and Liver Health in Savannah, Ga.
- “We previously investigated other partnerships but felt they really did not bring enough value to make our group stronger or more viable. United Digestive was different. The idea of partnering with like-minded gastroenterologists to become a larger, single-specialty entity, with contract negotiation leverage and economies of scale was appealing and would not be possible as a 10-person group. Further, the partnership represented an opportunity to eliminate debt, minimize future risk to younger partners, and yet also embrace an ability to add new services and physicians.
“There were expected hiccups in the beginning: specifically IT and HR issues, which were remedied appropriately and timely. One month after the partnership was completed, reports started coming out of China about a new viral illness – an illness that telescoped our perspective on the consequences of our decision into a timeline of months rather than years.
“UD’s response to the COVID-19 epidemic has been phenomenal. The organization made the tough, but proper clinical calls that limited risks to patients and staff. They came up with a game plan to salvage fiscal viability – rolling out telemedicine in a matter of days and establishing the manner in which patients with high acuity could still be seen and cared for expediently.
“As a solo GI practice, we would have struggled mightily to survive and might have gone bankrupt. Had we been part of a larger non-GI entity (a hospital or multispecialty group), we might have been pressured to engage in unsafe or unethical practices and not consistent with national societal recommendations. Instead, we found ourselves having active discussions with our GI colleagues about the right path forward.”
How do you feel UD has helped improve the quality of patient care and positively impacted patient satisfaction?
Aja McCutchen, MD
- “Prior to UD, we worked diligently to improve our centralized patient service center, phone trees, and optimize the time and communication between patients, providers, and our staff. We now have tools which help identify and track gaps in communication on all levels. We have been able to improve our MA work flow, shorten wait times, and improve the direct dialogue between our practice and our patients. We have also been able to enhance our ancillary service offerings and expand programs that directly benefit our patients.”
Kimberly Orleck, PA-C
- “I think our quality of care has always been top notch and that thankfully has not been altered. UD has concentrated on workflow optimization, enhanced training to our frontline teams, and improved scheduled processes to decrease patient wait time. UD is also paying closer attention to patient ratings, reviews, and calculating net promotor scores. ”
Have there been any initiatives in the first year which improved the management of the organization?
Elizabeth Escalante, Senior Regional Director of Operations, UD
- “Implementation of a business analytics tool was huge this year. It greatly improved visibility into the information we need to have at our fingertips in order to make data-driven decisions for our business. Drilling this down to the frontline manager has increased our understanding of what it truly takes to run a successful practice, and in turn, increased stakeholder buy-in.”
Lakeeta White, Clinical Office Team Lead, and Alexis Sweeney, Medical Assistant
- “The formation of our MA Advisory Committee has been instrumental in helping standardize best practices across the organization. It is comprised of medical assistants across our geographic footprint, and they provide feedback to the management team regarding process improvements, areas for continued training, and more.”
Though many positives may arise out of change, so can some challenges. Have there been any unforeseen hurdles you experience as a result of the new partnership with PE?
Elizabeth Escalante
- “Overall, I believe the changes to the structure of the practice and reorganization of leadership has been positive. As with any organization, one area of improvement is in communication.”
Dr. Patel and Dr. Sonenshine are with Atlanta Gastroenterology Associates, which is part of United Digestive. They have no conflicts.