User login
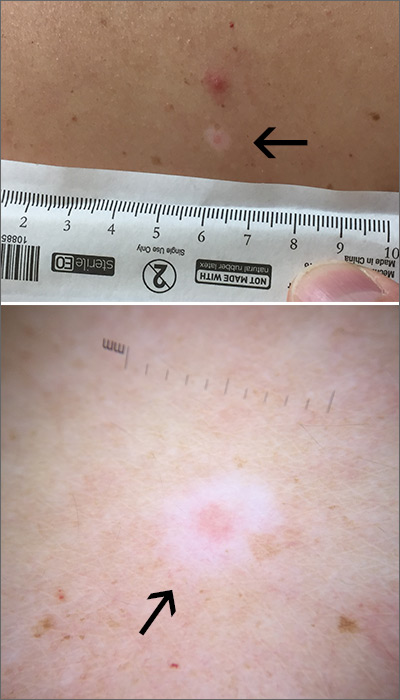
The FP used a dermatoscope to get a better look at the lesion and recognized this as a halo nevus, which is characterized by a central nevus with a halo of depigmentation around it (arrow) and sometimes depigmentation within the nevus itself.
The halo is caused when, occasionally, the body develops an immune reaction to a nevus and its melanocytes. As cytotoxic T cells target those melanocytes, there is loss of pigment to the tissue surrounding the nevus.1
The appearance of the central nevus, rather than the hypopigmentation, determines management strategies. A globular or homogeneous pattern seen on dermoscopy is typically indicative of a benign lesion.2 An atypical pigment network or other melanoma specific structures should raise your suspicions for melanoma or atypical nevus and prompt a deep shave excision sent for pathology to rule out melanoma. A nevus without suspicious features, other than the surrounding hypopigmentation, can be managed conservatively with self-monitoring and re-evaluation.
In this case, the lesion displayed a homogeneous pattern, and the FP advised the patient to self-monitor.
Images and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque, NM.
1. Bayer-Garner IB, Ivan D, Schwartz MR, et al. The immunopathology of regression in benign lichenoid keratosis, keratoacanthoma and halo nevus. Clin Med Res. 2004;2:89-97.
2. Porto AC, Blumetti TP, de Paula Ramos Castro R, et al. Recurrent halo nevus: dermoscopy and confocal microscopy features. JAAD Case Rep. 2017;3:256-258.
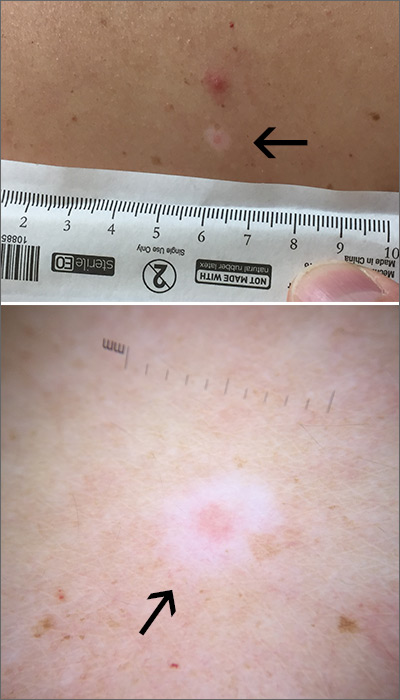
The FP used a dermatoscope to get a better look at the lesion and recognized this as a halo nevus, which is characterized by a central nevus with a halo of depigmentation around it (arrow) and sometimes depigmentation within the nevus itself.
The halo is caused when, occasionally, the body develops an immune reaction to a nevus and its melanocytes. As cytotoxic T cells target those melanocytes, there is loss of pigment to the tissue surrounding the nevus.1
The appearance of the central nevus, rather than the hypopigmentation, determines management strategies. A globular or homogeneous pattern seen on dermoscopy is typically indicative of a benign lesion.2 An atypical pigment network or other melanoma specific structures should raise your suspicions for melanoma or atypical nevus and prompt a deep shave excision sent for pathology to rule out melanoma. A nevus without suspicious features, other than the surrounding hypopigmentation, can be managed conservatively with self-monitoring and re-evaluation.
In this case, the lesion displayed a homogeneous pattern, and the FP advised the patient to self-monitor.
Images and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque, NM.
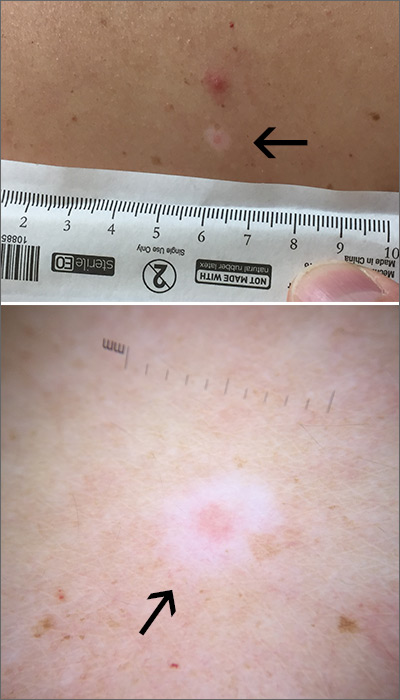
The FP used a dermatoscope to get a better look at the lesion and recognized this as a halo nevus, which is characterized by a central nevus with a halo of depigmentation around it (arrow) and sometimes depigmentation within the nevus itself.
The halo is caused when, occasionally, the body develops an immune reaction to a nevus and its melanocytes. As cytotoxic T cells target those melanocytes, there is loss of pigment to the tissue surrounding the nevus.1
The appearance of the central nevus, rather than the hypopigmentation, determines management strategies. A globular or homogeneous pattern seen on dermoscopy is typically indicative of a benign lesion.2 An atypical pigment network or other melanoma specific structures should raise your suspicions for melanoma or atypical nevus and prompt a deep shave excision sent for pathology to rule out melanoma. A nevus without suspicious features, other than the surrounding hypopigmentation, can be managed conservatively with self-monitoring and re-evaluation.
In this case, the lesion displayed a homogeneous pattern, and the FP advised the patient to self-monitor.
Images and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque, NM.
1. Bayer-Garner IB, Ivan D, Schwartz MR, et al. The immunopathology of regression in benign lichenoid keratosis, keratoacanthoma and halo nevus. Clin Med Res. 2004;2:89-97.
2. Porto AC, Blumetti TP, de Paula Ramos Castro R, et al. Recurrent halo nevus: dermoscopy and confocal microscopy features. JAAD Case Rep. 2017;3:256-258.
1. Bayer-Garner IB, Ivan D, Schwartz MR, et al. The immunopathology of regression in benign lichenoid keratosis, keratoacanthoma and halo nevus. Clin Med Res. 2004;2:89-97.
2. Porto AC, Blumetti TP, de Paula Ramos Castro R, et al. Recurrent halo nevus: dermoscopy and confocal microscopy features. JAAD Case Rep. 2017;3:256-258.
