User login
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
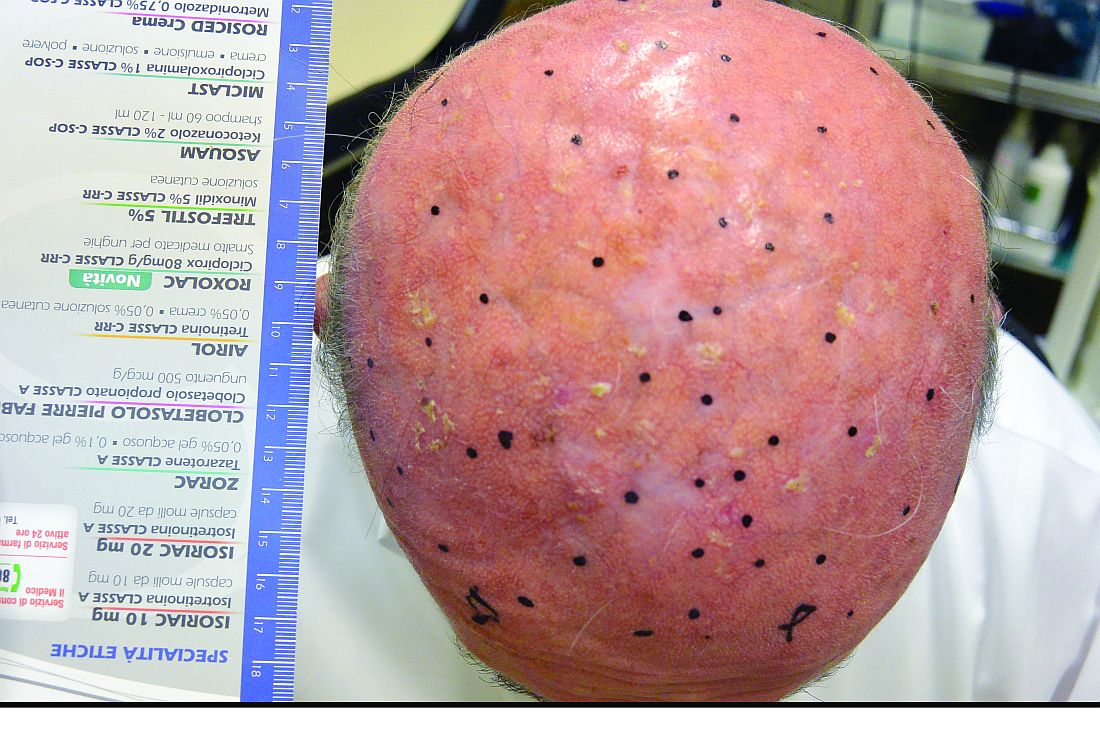
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.