User login
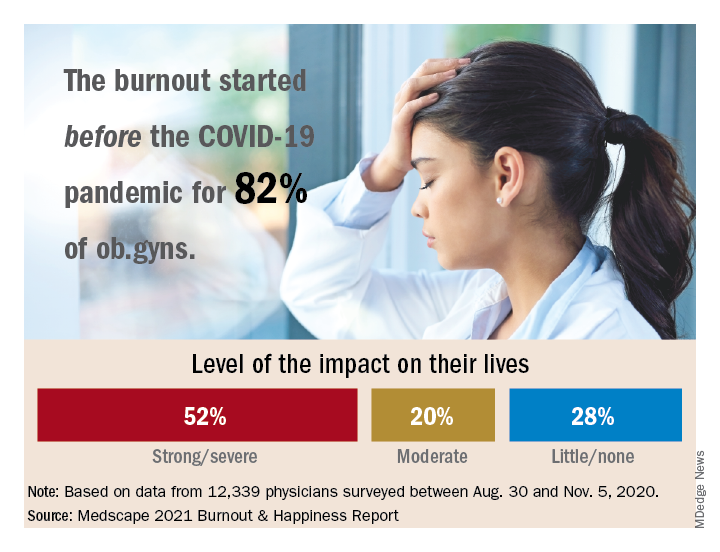
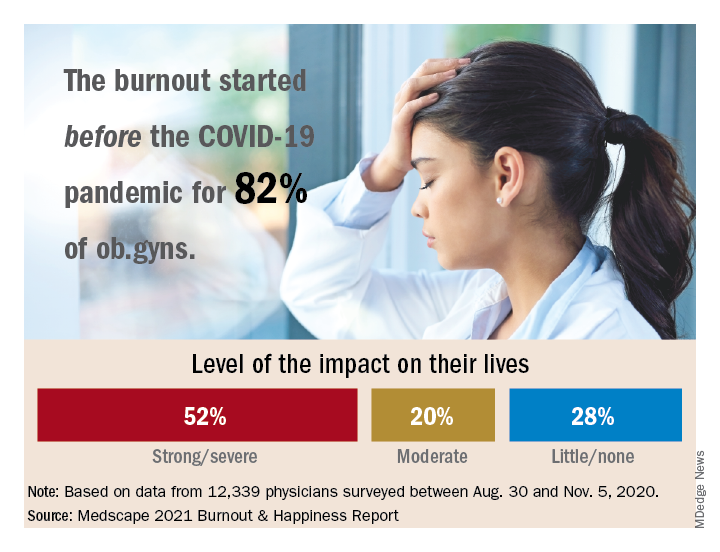
Among ob.gyns. who reported burnout in the past year, 82% say they felt burned out before the advent of the coronavirus pandemic, according the Medscape Obstetrician & Gynecologist Lifestyle, Happiness, & Burnout Report.
The past year brought unusual challenges to physicians in all specialties in different ways.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” wrote Keith L. Martin and Mary Lyn Koval, both of Medscape Business of Medicine, in the introduction to the report.
Although more physicians said their burnout began prior to the pandemic, 81% of ob.gyns. reported that they were happy outside of work prior to the pandemic. However, those reporting happiness outside of work dropped to 57% after the pandemic started.
“One does not have to do a ‘deep dive’ to understand the top reasons reported for burnout,” said Mark P. Trolice, MD, director of Fertility CARE: The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando, in an interview. “Many conversations I have with colleagues are about the frustration of learning and managing electronic health records, insurance reimbursements, and a work-life balance. In addition, more physician practices are being purchased by hospitals or private-equity networks [that are] reducing and/or eliminating the autonomy of physicians.
“While all [respondents] exhibited a dramatic decline in ‘happiness’ prepandemic, compared with our current situation, ob.gyns. were no exception,” he added.
Burnout and suicidal thoughts
Overall, 26% of ob.gyn. survey respondents reported being burned out, 6% reported being depressed, and 18% reported being both burned out and depressed. Of those who reported burnout, 52% said burnout had “a strong or severe impact on my life,” while 20% reported a moderate impact and 28% reported little or no impact.
More than half (56%) of ob.gyns. who reported either depression or burnout said they had not sought professional help, although 17% reported receiving professional care in the past.
The main reason given for not seeking professional help was that burnout and depressive symptoms were not severe enough to merit it, according to 50% of respondents who reported burnout or depression but were not seeking help. In addition, 43% said they were too busy to seek help, 36% said they could deal with their symptoms without professional help, and 24% said they did not want to risk disclosure of their symptoms.
The most common cause of burnout was an overload of bureaucratic tasks, reported by 52% of respondents, followed by “lack of respect from administrators/employers, colleagues, or staff” (43%), and insufficient compensation or reimbursement (39%).
Notably, 19% of ob.gyns. reported suicidal thoughts, and 1% said they had attempted suicide.
“The most concerning statistic from this survey was in reference to suicidal ideation,” said Dr. Trolice. “Approximately one in five ob.gyns. have contemplated suicide, compared with 4.8% of adults age 18 and older in the U.S. reporting in 2019.”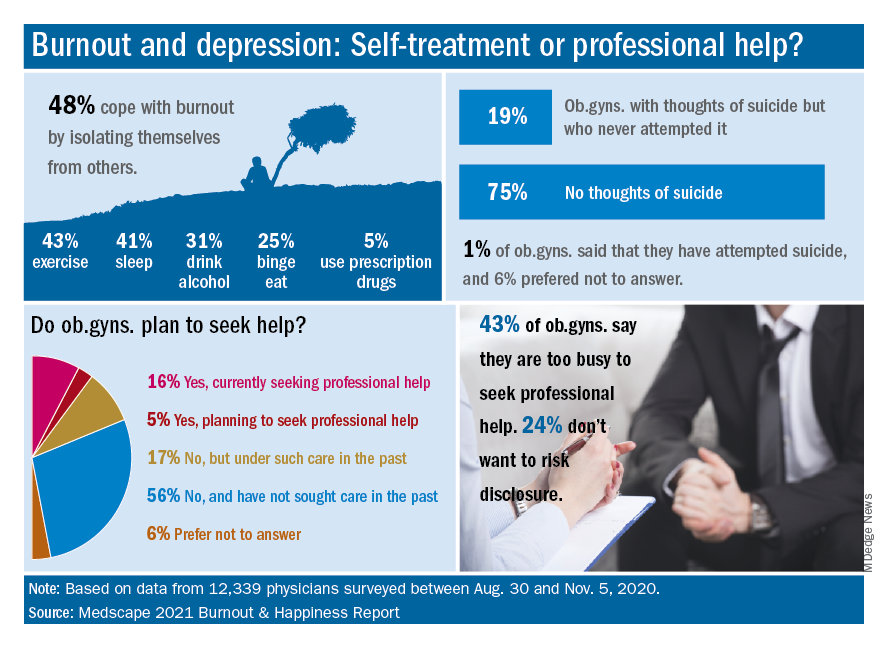
Dr. Trolice said he was not surprised that relatively few ob.gyns. sought help for mental health issues. “Physicians are very private and usually do not seek help from colleagues, presumably from hubris. While this is unfortunate, all hospitals and health care organization should implement regular assessments of physicians’ health to ensure optimal performance from a professional and personal basis.”
Balance and self-care
The top workplace concern, by a large margin, was for work-life balance, reported by 44% of respondents, followed by compensation (19%), combining work and parenting (18%), and relationships with staff and colleagues (8%).
Approximately one-third (36%) of the ob.gyn. respondents said they made time to focus on personal well-being, compared with 35% of physicians overall. Although only 13% reported exercising every day, a total of 69% exercised at least twice a week, similar to the 70% of physicians overall who reported exercising at least twice a week.
“Work-life balance is high on the list of concerns, but physicians are split 50/50 on whether they would accept a salary reduction to improve this aspect of their lives,” Dr. Trolice said.
“Social relationships are a proven value to mental health, yet nearly 50% of ob.gyns. who reported feeling burnout use isolationism as their coping skill, citing a lack of severity to require treatment,” he noted. Nevertheless, more than 80% of responders were married and described their relationship as “good or very good.”
Address burnout at individual and organizational levels
“Sadly, the findings are not surprising,” said Iris Krisha, MD, of Emory University, Atlanta, in an interview. “Burnout rates have been steadily increasing among physicians across all specialties.” Barriers to reducing burnout exist at the organizational and individual level, therefore strategies to reduce burnout should address individual and organizational solutions, Dr. Krishna emphasized. “At the organizational level, solutions may include developing manageable workloads, creating fair productivity targets, encouraging physician engagement in work structure, supporting flexible work schedules, and allowing for protected time for education and exercise. On the individual level, physicians can work to develop stress management strategies, engage in mindfulness and self-care.”
To reduce the burden of bureaucratic tasks, “health care organizations can work toward optimizing electronic medical records and hire staff to offload clerical work, and physicians can seek training in efficiency,” said Dr. Krishna. In addition, “health care organizations can reduce the stigma that may surround burnout or mental health issues, as well as promote a culture of wellness and resilience,” to help reduce and prevent burnout.
Find positivity and purpose
Improving the workplace experience so physicians feel engaged and in control as they navigate their many responsibilities may help reduce burnout, said Dr. Trolice. On the individual level, “finding your purpose to give you more meaning at work, discovering the power of hope to embrace optimism, and building friendships at work for greater engagement with others,” can help as well.
“In the face of adversity and setbacks, people in happier workplaces tend to be better at coping with and recovering from work pressure and at reconciling conflict,” Dr. Trolice emphasized. “The practice of medicine has dramatically changed for many physicians compared with the original expectations when they applied to medical school. Nevertheless, it behooves physician to adapt to 21st century medical care as they remind themselves of their purpose.”
The report included responses from 12,339 physicians across 29 specialties who completed a 10-minute online survey between Aug. 30 and Nov. 5, 2020. Participants were required to be practicing U.S. physicians.
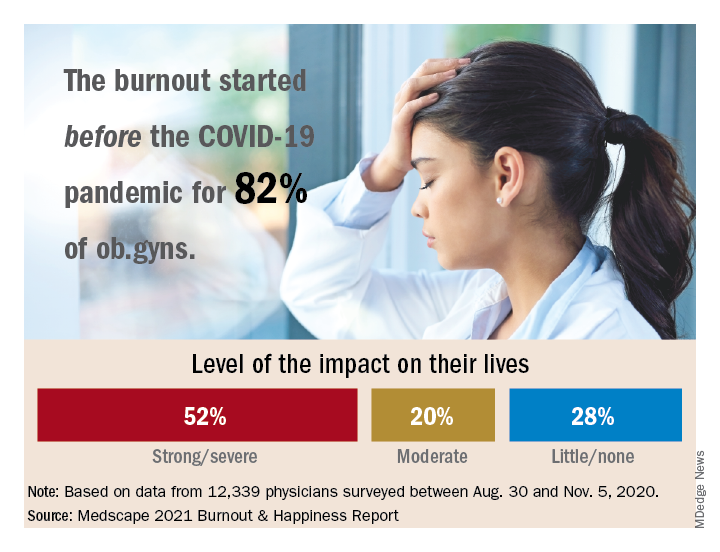
Among ob.gyns. who reported burnout in the past year, 82% say they felt burned out before the advent of the coronavirus pandemic, according the Medscape Obstetrician & Gynecologist Lifestyle, Happiness, & Burnout Report.
The past year brought unusual challenges to physicians in all specialties in different ways.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” wrote Keith L. Martin and Mary Lyn Koval, both of Medscape Business of Medicine, in the introduction to the report.
Although more physicians said their burnout began prior to the pandemic, 81% of ob.gyns. reported that they were happy outside of work prior to the pandemic. However, those reporting happiness outside of work dropped to 57% after the pandemic started.
“One does not have to do a ‘deep dive’ to understand the top reasons reported for burnout,” said Mark P. Trolice, MD, director of Fertility CARE: The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando, in an interview. “Many conversations I have with colleagues are about the frustration of learning and managing electronic health records, insurance reimbursements, and a work-life balance. In addition, more physician practices are being purchased by hospitals or private-equity networks [that are] reducing and/or eliminating the autonomy of physicians.
“While all [respondents] exhibited a dramatic decline in ‘happiness’ prepandemic, compared with our current situation, ob.gyns. were no exception,” he added.
Burnout and suicidal thoughts
Overall, 26% of ob.gyn. survey respondents reported being burned out, 6% reported being depressed, and 18% reported being both burned out and depressed. Of those who reported burnout, 52% said burnout had “a strong or severe impact on my life,” while 20% reported a moderate impact and 28% reported little or no impact.
More than half (56%) of ob.gyns. who reported either depression or burnout said they had not sought professional help, although 17% reported receiving professional care in the past.
The main reason given for not seeking professional help was that burnout and depressive symptoms were not severe enough to merit it, according to 50% of respondents who reported burnout or depression but were not seeking help. In addition, 43% said they were too busy to seek help, 36% said they could deal with their symptoms without professional help, and 24% said they did not want to risk disclosure of their symptoms.
The most common cause of burnout was an overload of bureaucratic tasks, reported by 52% of respondents, followed by “lack of respect from administrators/employers, colleagues, or staff” (43%), and insufficient compensation or reimbursement (39%).
Notably, 19% of ob.gyns. reported suicidal thoughts, and 1% said they had attempted suicide.
“The most concerning statistic from this survey was in reference to suicidal ideation,” said Dr. Trolice. “Approximately one in five ob.gyns. have contemplated suicide, compared with 4.8% of adults age 18 and older in the U.S. reporting in 2019.”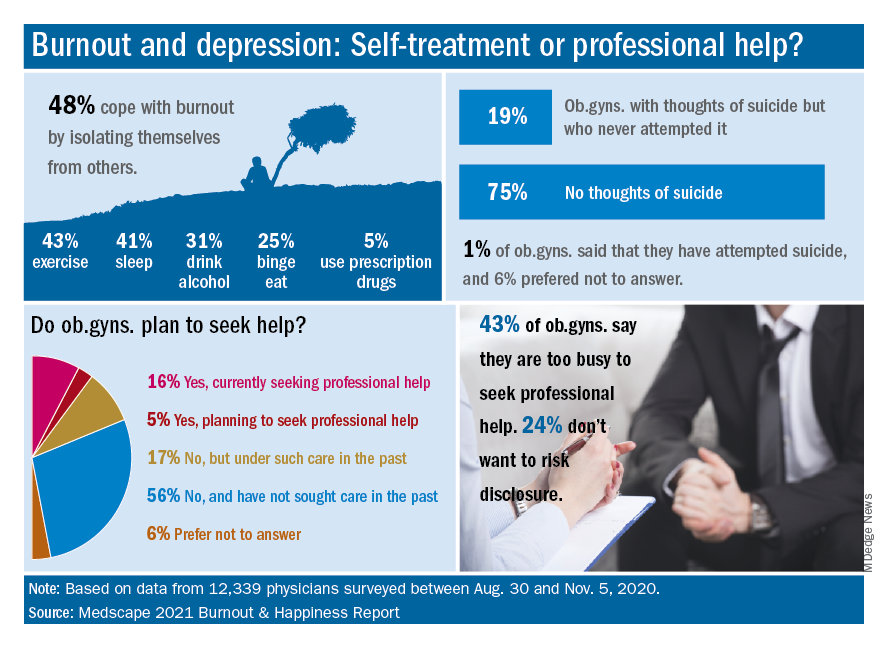
Dr. Trolice said he was not surprised that relatively few ob.gyns. sought help for mental health issues. “Physicians are very private and usually do not seek help from colleagues, presumably from hubris. While this is unfortunate, all hospitals and health care organization should implement regular assessments of physicians’ health to ensure optimal performance from a professional and personal basis.”
Balance and self-care
The top workplace concern, by a large margin, was for work-life balance, reported by 44% of respondents, followed by compensation (19%), combining work and parenting (18%), and relationships with staff and colleagues (8%).
Approximately one-third (36%) of the ob.gyn. respondents said they made time to focus on personal well-being, compared with 35% of physicians overall. Although only 13% reported exercising every day, a total of 69% exercised at least twice a week, similar to the 70% of physicians overall who reported exercising at least twice a week.
“Work-life balance is high on the list of concerns, but physicians are split 50/50 on whether they would accept a salary reduction to improve this aspect of their lives,” Dr. Trolice said.
“Social relationships are a proven value to mental health, yet nearly 50% of ob.gyns. who reported feeling burnout use isolationism as their coping skill, citing a lack of severity to require treatment,” he noted. Nevertheless, more than 80% of responders were married and described their relationship as “good or very good.”
Address burnout at individual and organizational levels
“Sadly, the findings are not surprising,” said Iris Krisha, MD, of Emory University, Atlanta, in an interview. “Burnout rates have been steadily increasing among physicians across all specialties.” Barriers to reducing burnout exist at the organizational and individual level, therefore strategies to reduce burnout should address individual and organizational solutions, Dr. Krishna emphasized. “At the organizational level, solutions may include developing manageable workloads, creating fair productivity targets, encouraging physician engagement in work structure, supporting flexible work schedules, and allowing for protected time for education and exercise. On the individual level, physicians can work to develop stress management strategies, engage in mindfulness and self-care.”
To reduce the burden of bureaucratic tasks, “health care organizations can work toward optimizing electronic medical records and hire staff to offload clerical work, and physicians can seek training in efficiency,” said Dr. Krishna. In addition, “health care organizations can reduce the stigma that may surround burnout or mental health issues, as well as promote a culture of wellness and resilience,” to help reduce and prevent burnout.
Find positivity and purpose
Improving the workplace experience so physicians feel engaged and in control as they navigate their many responsibilities may help reduce burnout, said Dr. Trolice. On the individual level, “finding your purpose to give you more meaning at work, discovering the power of hope to embrace optimism, and building friendships at work for greater engagement with others,” can help as well.
“In the face of adversity and setbacks, people in happier workplaces tend to be better at coping with and recovering from work pressure and at reconciling conflict,” Dr. Trolice emphasized. “The practice of medicine has dramatically changed for many physicians compared with the original expectations when they applied to medical school. Nevertheless, it behooves physician to adapt to 21st century medical care as they remind themselves of their purpose.”
The report included responses from 12,339 physicians across 29 specialties who completed a 10-minute online survey between Aug. 30 and Nov. 5, 2020. Participants were required to be practicing U.S. physicians.
Among ob.gyns. who reported burnout in the past year, 82% say they felt burned out before the advent of the coronavirus pandemic, according the Medscape Obstetrician & Gynecologist Lifestyle, Happiness, & Burnout Report.
The past year brought unusual challenges to physicians in all specialties in different ways.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” wrote Keith L. Martin and Mary Lyn Koval, both of Medscape Business of Medicine, in the introduction to the report.
Although more physicians said their burnout began prior to the pandemic, 81% of ob.gyns. reported that they were happy outside of work prior to the pandemic. However, those reporting happiness outside of work dropped to 57% after the pandemic started.
“One does not have to do a ‘deep dive’ to understand the top reasons reported for burnout,” said Mark P. Trolice, MD, director of Fertility CARE: The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando, in an interview. “Many conversations I have with colleagues are about the frustration of learning and managing electronic health records, insurance reimbursements, and a work-life balance. In addition, more physician practices are being purchased by hospitals or private-equity networks [that are] reducing and/or eliminating the autonomy of physicians.
“While all [respondents] exhibited a dramatic decline in ‘happiness’ prepandemic, compared with our current situation, ob.gyns. were no exception,” he added.
Burnout and suicidal thoughts
Overall, 26% of ob.gyn. survey respondents reported being burned out, 6% reported being depressed, and 18% reported being both burned out and depressed. Of those who reported burnout, 52% said burnout had “a strong or severe impact on my life,” while 20% reported a moderate impact and 28% reported little or no impact.
More than half (56%) of ob.gyns. who reported either depression or burnout said they had not sought professional help, although 17% reported receiving professional care in the past.
The main reason given for not seeking professional help was that burnout and depressive symptoms were not severe enough to merit it, according to 50% of respondents who reported burnout or depression but were not seeking help. In addition, 43% said they were too busy to seek help, 36% said they could deal with their symptoms without professional help, and 24% said they did not want to risk disclosure of their symptoms.
The most common cause of burnout was an overload of bureaucratic tasks, reported by 52% of respondents, followed by “lack of respect from administrators/employers, colleagues, or staff” (43%), and insufficient compensation or reimbursement (39%).
Notably, 19% of ob.gyns. reported suicidal thoughts, and 1% said they had attempted suicide.
“The most concerning statistic from this survey was in reference to suicidal ideation,” said Dr. Trolice. “Approximately one in five ob.gyns. have contemplated suicide, compared with 4.8% of adults age 18 and older in the U.S. reporting in 2019.”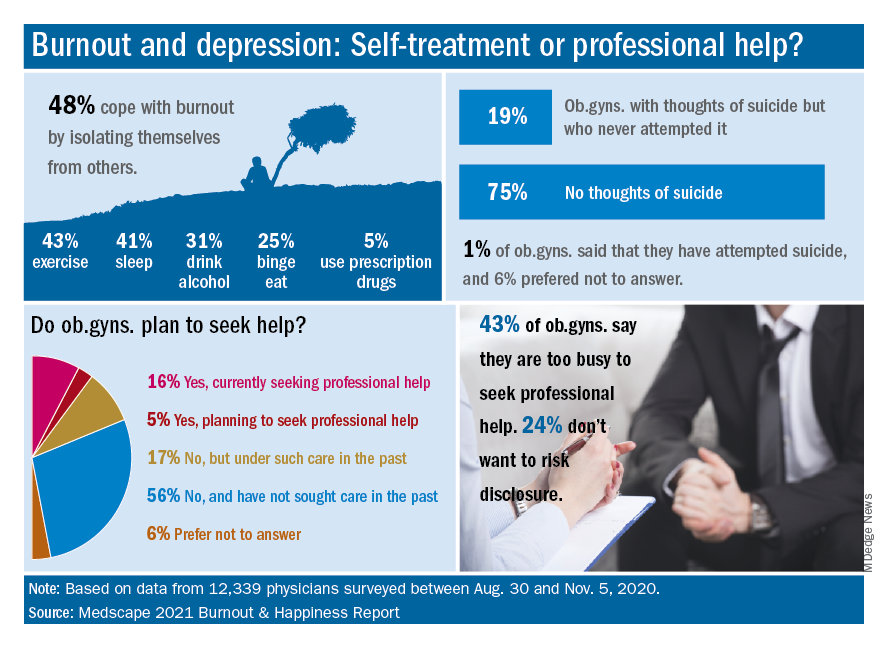
Dr. Trolice said he was not surprised that relatively few ob.gyns. sought help for mental health issues. “Physicians are very private and usually do not seek help from colleagues, presumably from hubris. While this is unfortunate, all hospitals and health care organization should implement regular assessments of physicians’ health to ensure optimal performance from a professional and personal basis.”
Balance and self-care
The top workplace concern, by a large margin, was for work-life balance, reported by 44% of respondents, followed by compensation (19%), combining work and parenting (18%), and relationships with staff and colleagues (8%).
Approximately one-third (36%) of the ob.gyn. respondents said they made time to focus on personal well-being, compared with 35% of physicians overall. Although only 13% reported exercising every day, a total of 69% exercised at least twice a week, similar to the 70% of physicians overall who reported exercising at least twice a week.
“Work-life balance is high on the list of concerns, but physicians are split 50/50 on whether they would accept a salary reduction to improve this aspect of their lives,” Dr. Trolice said.
“Social relationships are a proven value to mental health, yet nearly 50% of ob.gyns. who reported feeling burnout use isolationism as their coping skill, citing a lack of severity to require treatment,” he noted. Nevertheless, more than 80% of responders were married and described their relationship as “good or very good.”
Address burnout at individual and organizational levels
“Sadly, the findings are not surprising,” said Iris Krisha, MD, of Emory University, Atlanta, in an interview. “Burnout rates have been steadily increasing among physicians across all specialties.” Barriers to reducing burnout exist at the organizational and individual level, therefore strategies to reduce burnout should address individual and organizational solutions, Dr. Krishna emphasized. “At the organizational level, solutions may include developing manageable workloads, creating fair productivity targets, encouraging physician engagement in work structure, supporting flexible work schedules, and allowing for protected time for education and exercise. On the individual level, physicians can work to develop stress management strategies, engage in mindfulness and self-care.”
To reduce the burden of bureaucratic tasks, “health care organizations can work toward optimizing electronic medical records and hire staff to offload clerical work, and physicians can seek training in efficiency,” said Dr. Krishna. In addition, “health care organizations can reduce the stigma that may surround burnout or mental health issues, as well as promote a culture of wellness and resilience,” to help reduce and prevent burnout.
Find positivity and purpose
Improving the workplace experience so physicians feel engaged and in control as they navigate their many responsibilities may help reduce burnout, said Dr. Trolice. On the individual level, “finding your purpose to give you more meaning at work, discovering the power of hope to embrace optimism, and building friendships at work for greater engagement with others,” can help as well.
“In the face of adversity and setbacks, people in happier workplaces tend to be better at coping with and recovering from work pressure and at reconciling conflict,” Dr. Trolice emphasized. “The practice of medicine has dramatically changed for many physicians compared with the original expectations when they applied to medical school. Nevertheless, it behooves physician to adapt to 21st century medical care as they remind themselves of their purpose.”
The report included responses from 12,339 physicians across 29 specialties who completed a 10-minute online survey between Aug. 30 and Nov. 5, 2020. Participants were required to be practicing U.S. physicians.