User login
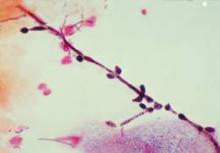
RIO GRANDE, P.R. – In patients with chronic recurrent candida, "the first thing to do is culture," Dr. Ted Rosen said at the Caribbean Dermatology Symposium.
"Make sure that it is really fungal," said Dr. Rosen, a professor of dermatology at Baylor College of Medicine, Houston. About 70%-80% of so-called candida infections aren’t yeast infections at all. Be sure to consider other diagnoses before proceeding with treatment.
If culture confirms the chronic candida diagnosis, fluconazole is the traditional treatment.
In case of vulvovaginal candidiasis, data from several studies now suggest that probiotics also are effective in patients who are not immunocompromised, said Dr. Rosen.
"I’m not really a New Age kind of person, but it turns out that probiotics have shown effectiveness against chronic candida, thrush, and vulvovaginal candida" in otherwise healthy individuals, he said.
Probiotics administered over a fairly long time seem to make those infections stop. As to how this works, "the probiotics secrete a surfactant" that keeps the candida from adhering to tissues. In addition, "the probiotic bacteria act as competition for the yeast forms," Dr. Rosen said. "They [the probiotics] also secrete antibacterial substances because they want to get rid of their competition [the yeast]," he added.
Dr. Rosen cited a recent review of data supporting the impact of probiotics on healthy vaginal flora and their effectiveness for treating and preventing candidiasis. The review was published in the journal Mycoses (2012;55:17-26).
In a randomized, double-blind, placebo-controlled trial of 64 women with vulvovaginal candidiasis, those who took capsules containing Lactobacillus rhamnosus and L. fermentum showed significantly decreased yeast and coliforms after 4 weeks compared with women who took a calcium carbonate placebo. The probiotics group also showed a significant increase in healthy vaginal lactobacilli.
In another randomized, double-blind, placebo controlled trial, women with vulvovaginal candidiasis received a standard dose of fluconazole plus probiotics (L. reuteri and L. rhamnosus) or fluconazole plus placebo once daily for 28 days. At day 28, significantly more women who took probiotics were cured of vulvovaginal candidiasis, based on negative cultures and symptom resolution.
The findings suggest that probiotics may be useful therapeutic interventions for candida, in part because of the nearly nonexistent adverse effects on patients and the lack of resistance developed by the pathogens, the researchers wrote.
Based on the available data, a standard oral probiotic with lactobacillus and bifidobacteria is worth trying in a patient with chronic candida, Dr. Rosen said.
Dr. Rosen had no relevant financial conflicts to disclose. The authors of the study published in Mycoses had no financial conflicts to disclose.
RIO GRANDE, P.R. – In patients with chronic recurrent candida, "the first thing to do is culture," Dr. Ted Rosen said at the Caribbean Dermatology Symposium.
"Make sure that it is really fungal," said Dr. Rosen, a professor of dermatology at Baylor College of Medicine, Houston. About 70%-80% of so-called candida infections aren’t yeast infections at all. Be sure to consider other diagnoses before proceeding with treatment.
If culture confirms the chronic candida diagnosis, fluconazole is the traditional treatment.
In case of vulvovaginal candidiasis, data from several studies now suggest that probiotics also are effective in patients who are not immunocompromised, said Dr. Rosen.
"I’m not really a New Age kind of person, but it turns out that probiotics have shown effectiveness against chronic candida, thrush, and vulvovaginal candida" in otherwise healthy individuals, he said.
Probiotics administered over a fairly long time seem to make those infections stop. As to how this works, "the probiotics secrete a surfactant" that keeps the candida from adhering to tissues. In addition, "the probiotic bacteria act as competition for the yeast forms," Dr. Rosen said. "They [the probiotics] also secrete antibacterial substances because they want to get rid of their competition [the yeast]," he added.
Dr. Rosen cited a recent review of data supporting the impact of probiotics on healthy vaginal flora and their effectiveness for treating and preventing candidiasis. The review was published in the journal Mycoses (2012;55:17-26).
In a randomized, double-blind, placebo-controlled trial of 64 women with vulvovaginal candidiasis, those who took capsules containing Lactobacillus rhamnosus and L. fermentum showed significantly decreased yeast and coliforms after 4 weeks compared with women who took a calcium carbonate placebo. The probiotics group also showed a significant increase in healthy vaginal lactobacilli.
In another randomized, double-blind, placebo controlled trial, women with vulvovaginal candidiasis received a standard dose of fluconazole plus probiotics (L. reuteri and L. rhamnosus) or fluconazole plus placebo once daily for 28 days. At day 28, significantly more women who took probiotics were cured of vulvovaginal candidiasis, based on negative cultures and symptom resolution.
The findings suggest that probiotics may be useful therapeutic interventions for candida, in part because of the nearly nonexistent adverse effects on patients and the lack of resistance developed by the pathogens, the researchers wrote.
Based on the available data, a standard oral probiotic with lactobacillus and bifidobacteria is worth trying in a patient with chronic candida, Dr. Rosen said.
Dr. Rosen had no relevant financial conflicts to disclose. The authors of the study published in Mycoses had no financial conflicts to disclose.
RIO GRANDE, P.R. – In patients with chronic recurrent candida, "the first thing to do is culture," Dr. Ted Rosen said at the Caribbean Dermatology Symposium.
"Make sure that it is really fungal," said Dr. Rosen, a professor of dermatology at Baylor College of Medicine, Houston. About 70%-80% of so-called candida infections aren’t yeast infections at all. Be sure to consider other diagnoses before proceeding with treatment.
If culture confirms the chronic candida diagnosis, fluconazole is the traditional treatment.
In case of vulvovaginal candidiasis, data from several studies now suggest that probiotics also are effective in patients who are not immunocompromised, said Dr. Rosen.
"I’m not really a New Age kind of person, but it turns out that probiotics have shown effectiveness against chronic candida, thrush, and vulvovaginal candida" in otherwise healthy individuals, he said.
Probiotics administered over a fairly long time seem to make those infections stop. As to how this works, "the probiotics secrete a surfactant" that keeps the candida from adhering to tissues. In addition, "the probiotic bacteria act as competition for the yeast forms," Dr. Rosen said. "They [the probiotics] also secrete antibacterial substances because they want to get rid of their competition [the yeast]," he added.
Dr. Rosen cited a recent review of data supporting the impact of probiotics on healthy vaginal flora and their effectiveness for treating and preventing candidiasis. The review was published in the journal Mycoses (2012;55:17-26).
In a randomized, double-blind, placebo-controlled trial of 64 women with vulvovaginal candidiasis, those who took capsules containing Lactobacillus rhamnosus and L. fermentum showed significantly decreased yeast and coliforms after 4 weeks compared with women who took a calcium carbonate placebo. The probiotics group also showed a significant increase in healthy vaginal lactobacilli.
In another randomized, double-blind, placebo controlled trial, women with vulvovaginal candidiasis received a standard dose of fluconazole plus probiotics (L. reuteri and L. rhamnosus) or fluconazole plus placebo once daily for 28 days. At day 28, significantly more women who took probiotics were cured of vulvovaginal candidiasis, based on negative cultures and symptom resolution.
The findings suggest that probiotics may be useful therapeutic interventions for candida, in part because of the nearly nonexistent adverse effects on patients and the lack of resistance developed by the pathogens, the researchers wrote.
Based on the available data, a standard oral probiotic with lactobacillus and bifidobacteria is worth trying in a patient with chronic candida, Dr. Rosen said.
Dr. Rosen had no relevant financial conflicts to disclose. The authors of the study published in Mycoses had no financial conflicts to disclose.
EXPERT ANALYSIS FROM THE CARIBBEAN DERMATOLOGY SYMPOSIUM