User login
Oral Probiotics May Resolve Chronic Vulvovaginal Candidiasis
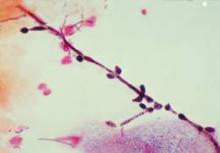
RIO GRANDE, P.R. – In patients with chronic recurrent candida, "the first thing to do is culture," Dr. Ted Rosen said at the Caribbean Dermatology Symposium.
"Make sure that it is really fungal," said Dr. Rosen, a professor of dermatology at Baylor College of Medicine, Houston. About 70%-80% of so-called candida infections aren’t yeast infections at all. Be sure to consider other diagnoses before proceeding with treatment.
If culture confirms the chronic candida diagnosis, fluconazole is the traditional treatment.
In case of vulvovaginal candidiasis, data from several studies now suggest that probiotics also are effective in patients who are not immunocompromised, said Dr. Rosen.
"I’m not really a New Age kind of person, but it turns out that probiotics have shown effectiveness against chronic candida, thrush, and vulvovaginal candida" in otherwise healthy individuals, he said.
Probiotics administered over a fairly long time seem to make those infections stop. As to how this works, "the probiotics secrete a surfactant" that keeps the candida from adhering to tissues. In addition, "the probiotic bacteria act as competition for the yeast forms," Dr. Rosen said. "They [the probiotics] also secrete antibacterial substances because they want to get rid of their competition [the yeast]," he added.
Dr. Rosen cited a recent review of data supporting the impact of probiotics on healthy vaginal flora and their effectiveness for treating and preventing candidiasis. The review was published in the journal Mycoses (2012;55:17-26).
In a randomized, double-blind, placebo-controlled trial of 64 women with vulvovaginal candidiasis, those who took capsules containing Lactobacillus rhamnosus and L. fermentum showed significantly decreased yeast and coliforms after 4 weeks compared with women who took a calcium carbonate placebo. The probiotics group also showed a significant increase in healthy vaginal lactobacilli.
In another randomized, double-blind, placebo controlled trial, women with vulvovaginal candidiasis received a standard dose of fluconazole plus probiotics (L. reuteri and L. rhamnosus) or fluconazole plus placebo once daily for 28 days. At day 28, significantly more women who took probiotics were cured of vulvovaginal candidiasis, based on negative cultures and symptom resolution.
The findings suggest that probiotics may be useful therapeutic interventions for candida, in part because of the nearly nonexistent adverse effects on patients and the lack of resistance developed by the pathogens, the researchers wrote.
Based on the available data, a standard oral probiotic with lactobacillus and bifidobacteria is worth trying in a patient with chronic candida, Dr. Rosen said.
Dr. Rosen had no relevant financial conflicts to disclose. The authors of the study published in Mycoses had no financial conflicts to disclose.
RIO GRANDE, P.R. – In patients with chronic recurrent candida, "the first thing to do is culture," Dr. Ted Rosen said at the Caribbean Dermatology Symposium.
"Make sure that it is really fungal," said Dr. Rosen, a professor of dermatology at Baylor College of Medicine, Houston. About 70%-80% of so-called candida infections aren’t yeast infections at all. Be sure to consider other diagnoses before proceeding with treatment.
If culture confirms the chronic candida diagnosis, fluconazole is the traditional treatment.
In case of vulvovaginal candidiasis, data from several studies now suggest that probiotics also are effective in patients who are not immunocompromised, said Dr. Rosen.
"I’m not really a New Age kind of person, but it turns out that probiotics have shown effectiveness against chronic candida, thrush, and vulvovaginal candida" in otherwise healthy individuals, he said.
Probiotics administered over a fairly long time seem to make those infections stop. As to how this works, "the probiotics secrete a surfactant" that keeps the candida from adhering to tissues. In addition, "the probiotic bacteria act as competition for the yeast forms," Dr. Rosen said. "They [the probiotics] also secrete antibacterial substances because they want to get rid of their competition [the yeast]," he added.
Dr. Rosen cited a recent review of data supporting the impact of probiotics on healthy vaginal flora and their effectiveness for treating and preventing candidiasis. The review was published in the journal Mycoses (2012;55:17-26).
In a randomized, double-blind, placebo-controlled trial of 64 women with vulvovaginal candidiasis, those who took capsules containing Lactobacillus rhamnosus and L. fermentum showed significantly decreased yeast and coliforms after 4 weeks compared with women who took a calcium carbonate placebo. The probiotics group also showed a significant increase in healthy vaginal lactobacilli.
In another randomized, double-blind, placebo controlled trial, women with vulvovaginal candidiasis received a standard dose of fluconazole plus probiotics (L. reuteri and L. rhamnosus) or fluconazole plus placebo once daily for 28 days. At day 28, significantly more women who took probiotics were cured of vulvovaginal candidiasis, based on negative cultures and symptom resolution.
The findings suggest that probiotics may be useful therapeutic interventions for candida, in part because of the nearly nonexistent adverse effects on patients and the lack of resistance developed by the pathogens, the researchers wrote.
Based on the available data, a standard oral probiotic with lactobacillus and bifidobacteria is worth trying in a patient with chronic candida, Dr. Rosen said.
Dr. Rosen had no relevant financial conflicts to disclose. The authors of the study published in Mycoses had no financial conflicts to disclose.
RIO GRANDE, P.R. – In patients with chronic recurrent candida, "the first thing to do is culture," Dr. Ted Rosen said at the Caribbean Dermatology Symposium.
"Make sure that it is really fungal," said Dr. Rosen, a professor of dermatology at Baylor College of Medicine, Houston. About 70%-80% of so-called candida infections aren’t yeast infections at all. Be sure to consider other diagnoses before proceeding with treatment.
If culture confirms the chronic candida diagnosis, fluconazole is the traditional treatment.
In case of vulvovaginal candidiasis, data from several studies now suggest that probiotics also are effective in patients who are not immunocompromised, said Dr. Rosen.
"I’m not really a New Age kind of person, but it turns out that probiotics have shown effectiveness against chronic candida, thrush, and vulvovaginal candida" in otherwise healthy individuals, he said.
Probiotics administered over a fairly long time seem to make those infections stop. As to how this works, "the probiotics secrete a surfactant" that keeps the candida from adhering to tissues. In addition, "the probiotic bacteria act as competition for the yeast forms," Dr. Rosen said. "They [the probiotics] also secrete antibacterial substances because they want to get rid of their competition [the yeast]," he added.
Dr. Rosen cited a recent review of data supporting the impact of probiotics on healthy vaginal flora and their effectiveness for treating and preventing candidiasis. The review was published in the journal Mycoses (2012;55:17-26).
In a randomized, double-blind, placebo-controlled trial of 64 women with vulvovaginal candidiasis, those who took capsules containing Lactobacillus rhamnosus and L. fermentum showed significantly decreased yeast and coliforms after 4 weeks compared with women who took a calcium carbonate placebo. The probiotics group also showed a significant increase in healthy vaginal lactobacilli.
In another randomized, double-blind, placebo controlled trial, women with vulvovaginal candidiasis received a standard dose of fluconazole plus probiotics (L. reuteri and L. rhamnosus) or fluconazole plus placebo once daily for 28 days. At day 28, significantly more women who took probiotics were cured of vulvovaginal candidiasis, based on negative cultures and symptom resolution.
The findings suggest that probiotics may be useful therapeutic interventions for candida, in part because of the nearly nonexistent adverse effects on patients and the lack of resistance developed by the pathogens, the researchers wrote.
Based on the available data, a standard oral probiotic with lactobacillus and bifidobacteria is worth trying in a patient with chronic candida, Dr. Rosen said.
Dr. Rosen had no relevant financial conflicts to disclose. The authors of the study published in Mycoses had no financial conflicts to disclose.
EXPERT ANALYSIS FROM THE CARIBBEAN DERMATOLOGY SYMPOSIUM
Don't Miss These Pediatric Dermatology Diagnoses
RIO GRANDE, P.R. – Langerhans cell histiocytosis can be benign and self-limited, or a disseminated disease with the potential for significant morbidity and death, said Dr. Anthony J. Mancini.
The mortality risk depends on whether high-risk organs such as the liver or spleen are involved, as well as the early response to treatment, said Dr. Mancini, professor of pediatrics and dermatology at Northwestern University and Children’s Memorial Hospital in Chicago.
Langerhans cell histiocytosis (LCH) was one of five pediatric dermatology diagnoses Dr. Mancini urged dermatologists at the annual Caribbean Dermatology Symposium not to miss. Prompt identification of these conditions can improve young patients’ outcomes and reduce the risk for complications later, he said.
The clinical diagnosis of LCH in infants and children includes scaly erythematous seborrheic-like dermatitis, brown or red papules that may be lichenoid, and erythema in skin fold areas including the groin and the anterior neck folds, often with punctate erosions, he noted. Petechiae may be present, and crusted papules on the palms and soles are occasionally seen in young children.
Histopathology of LCH shows a granulomatous infiltrate that is epidermotropic, and the presence of positive CD1a or CD207 staining confirms the diagnosis, he said. An important distinction between LCH and streptococcal intertrigo: The strep responds rapidly to antibiotics and the erosive changes are more diffuse rather than focal.
Kawasaki Disease
"The most feared complication of Kawasaki disease (KD) is that of coronary artery aneurysm," said Dr. Mancini. "So it is very important to think about this disorder and get a rapid diagnosis," he said. The diagnosis is purely clinical, he noted, without the availability of a confirmatory diagnostic test at this time. Therefore, "have a high index of suspicion" for this disorder, he said.
Clinical criteria for KD include oropharyngeal changes, extremity changes, and a polymorphous skin eruption. Common prodromal symptoms may include irritability, vomiting, anorexia, cough, diarrhea, abdominal pain, and joint pain. "These kids appear sick," Dr. Mancini said.
Skin findings in KD may take on several morphologies, including morbilliform, urticarial, serum sickness-like, or even pustular.
One key finding that is suggestive of KD: Accentuation of erythema in skin folds, especially in the form of perineal desquamation, he said. However, blisters and purpura are not typically associated with the disorder.
Congenital Immunodeficiency
"In many patients, skin manifestations may be the presenting finding" of congenital immunodeficiency, Dr. Mancini said. In a recent study of 128 patients with primary immunodeficiency, 48% had skin manifestations, and these were the presenting feature in 39% with total PID and 82% of those with skin lesions (Pediatr. Dermatol. 2011;28;494-501).
Consider congenital immunodeficiency (CID) in cases of severe atopic or seborrheic dermatitis, intertrigo, or erythroderma that are resistant to therapy, said Dr. Mancini. Growth failure, alopecia, and recurrent infections (especially with unusual organisms) also can be signs of CID.
Graft vs. host disease (GVHD) in a skin biopsy increases suspicion for CID, he added.
An initial evaluation for suspected CID should include a complete blood count, quantitative immunoglobulins, mitogen stimulation assay, tetanus titer, T- and B-cell flow cytometry, and nitroblue tetrazolium or chronic granulomatous disease flow assay, said Dr. Mancini.
There are many congenital immunodeficiencies that may present with skin findings, including Wiskott-Aldrich syndrome, chronic mucocutaneous candidiasis, severe combined immunodeficiency, and leukocyte adhesion deficiency.
Drug Hypersensitivity Syndrome (DRESS)
Also known as Drug Reaction With Eosinophilia and Systemic Symptoms (DRESS), drug hypersensitivity tends to occur from 3-8 weeks after starting a particular medication, said Dr. Mancini. A skin rash is one of the most common findings, occurring in 77% to 100% of patients, he said. Facial edema is common, especially in the periorbital area. DRESS also can include fever, lymph node enlargement, and internal organ involvement.
Other clinical symptoms include conjunctivitis, pharyngitis, vomiting, and diarrhea. Telltale hematology findings indicative of DRESS include atypical lymphocytes and eosinophilia; pancytopenia occasionally appears.
The first line of defense is recognition and withdrawal from the drug. Serial monitoring of liver function studies is vital, given the fulminant hepatitis that can ensue, Dr. Mancini said. Treatment with systemic steroids and/or intravenous immunoglobulin is occasionally used, albeit controversially, he noted. Complete resolution of symptoms may take as long as 6 months.
Neonatal Herpes
The risk for neonatal infection with herpes simplex virus (HSV) is highest when the mother has active genital herpes at the time of delivery, Dr. Mancini said. If left untreated, the mortality rate for central nervous system or disseminated neonatal herpes is estimated at 50%-90%, so rapid recognition and diagnosis is vital, he said. The central nervous system, liver, lungs, adrenal glands, and bone marrow are important sites of potential involvement when the process disseminates, he added.
The classic skin presentation of neonatal HSV infection is vesicles and vesiculopustules that may be grouped on a red base or may become hemorrhagic. Bullae, widespread skin erosions, and polycyclic patches occasionally may be seen, and scarring may be present. Prompt evaluation is important, and intravenous acyclovir should be immediately instituted if the diagnosis of neonatal HSV is being considered.
Dr. Mancini said he had no financial conflicts to disclose.
RIO GRANDE, P.R. – Langerhans cell histiocytosis can be benign and self-limited, or a disseminated disease with the potential for significant morbidity and death, said Dr. Anthony J. Mancini.
The mortality risk depends on whether high-risk organs such as the liver or spleen are involved, as well as the early response to treatment, said Dr. Mancini, professor of pediatrics and dermatology at Northwestern University and Children’s Memorial Hospital in Chicago.
Langerhans cell histiocytosis (LCH) was one of five pediatric dermatology diagnoses Dr. Mancini urged dermatologists at the annual Caribbean Dermatology Symposium not to miss. Prompt identification of these conditions can improve young patients’ outcomes and reduce the risk for complications later, he said.
The clinical diagnosis of LCH in infants and children includes scaly erythematous seborrheic-like dermatitis, brown or red papules that may be lichenoid, and erythema in skin fold areas including the groin and the anterior neck folds, often with punctate erosions, he noted. Petechiae may be present, and crusted papules on the palms and soles are occasionally seen in young children.
Histopathology of LCH shows a granulomatous infiltrate that is epidermotropic, and the presence of positive CD1a or CD207 staining confirms the diagnosis, he said. An important distinction between LCH and streptococcal intertrigo: The strep responds rapidly to antibiotics and the erosive changes are more diffuse rather than focal.
Kawasaki Disease
"The most feared complication of Kawasaki disease (KD) is that of coronary artery aneurysm," said Dr. Mancini. "So it is very important to think about this disorder and get a rapid diagnosis," he said. The diagnosis is purely clinical, he noted, without the availability of a confirmatory diagnostic test at this time. Therefore, "have a high index of suspicion" for this disorder, he said.
Clinical criteria for KD include oropharyngeal changes, extremity changes, and a polymorphous skin eruption. Common prodromal symptoms may include irritability, vomiting, anorexia, cough, diarrhea, abdominal pain, and joint pain. "These kids appear sick," Dr. Mancini said.
Skin findings in KD may take on several morphologies, including morbilliform, urticarial, serum sickness-like, or even pustular.
One key finding that is suggestive of KD: Accentuation of erythema in skin folds, especially in the form of perineal desquamation, he said. However, blisters and purpura are not typically associated with the disorder.
Congenital Immunodeficiency
"In many patients, skin manifestations may be the presenting finding" of congenital immunodeficiency, Dr. Mancini said. In a recent study of 128 patients with primary immunodeficiency, 48% had skin manifestations, and these were the presenting feature in 39% with total PID and 82% of those with skin lesions (Pediatr. Dermatol. 2011;28;494-501).
Consider congenital immunodeficiency (CID) in cases of severe atopic or seborrheic dermatitis, intertrigo, or erythroderma that are resistant to therapy, said Dr. Mancini. Growth failure, alopecia, and recurrent infections (especially with unusual organisms) also can be signs of CID.
Graft vs. host disease (GVHD) in a skin biopsy increases suspicion for CID, he added.
An initial evaluation for suspected CID should include a complete blood count, quantitative immunoglobulins, mitogen stimulation assay, tetanus titer, T- and B-cell flow cytometry, and nitroblue tetrazolium or chronic granulomatous disease flow assay, said Dr. Mancini.
There are many congenital immunodeficiencies that may present with skin findings, including Wiskott-Aldrich syndrome, chronic mucocutaneous candidiasis, severe combined immunodeficiency, and leukocyte adhesion deficiency.
Drug Hypersensitivity Syndrome (DRESS)
Also known as Drug Reaction With Eosinophilia and Systemic Symptoms (DRESS), drug hypersensitivity tends to occur from 3-8 weeks after starting a particular medication, said Dr. Mancini. A skin rash is one of the most common findings, occurring in 77% to 100% of patients, he said. Facial edema is common, especially in the periorbital area. DRESS also can include fever, lymph node enlargement, and internal organ involvement.
Other clinical symptoms include conjunctivitis, pharyngitis, vomiting, and diarrhea. Telltale hematology findings indicative of DRESS include atypical lymphocytes and eosinophilia; pancytopenia occasionally appears.
The first line of defense is recognition and withdrawal from the drug. Serial monitoring of liver function studies is vital, given the fulminant hepatitis that can ensue, Dr. Mancini said. Treatment with systemic steroids and/or intravenous immunoglobulin is occasionally used, albeit controversially, he noted. Complete resolution of symptoms may take as long as 6 months.
Neonatal Herpes
The risk for neonatal infection with herpes simplex virus (HSV) is highest when the mother has active genital herpes at the time of delivery, Dr. Mancini said. If left untreated, the mortality rate for central nervous system or disseminated neonatal herpes is estimated at 50%-90%, so rapid recognition and diagnosis is vital, he said. The central nervous system, liver, lungs, adrenal glands, and bone marrow are important sites of potential involvement when the process disseminates, he added.
The classic skin presentation of neonatal HSV infection is vesicles and vesiculopustules that may be grouped on a red base or may become hemorrhagic. Bullae, widespread skin erosions, and polycyclic patches occasionally may be seen, and scarring may be present. Prompt evaluation is important, and intravenous acyclovir should be immediately instituted if the diagnosis of neonatal HSV is being considered.
Dr. Mancini said he had no financial conflicts to disclose.
RIO GRANDE, P.R. – Langerhans cell histiocytosis can be benign and self-limited, or a disseminated disease with the potential for significant morbidity and death, said Dr. Anthony J. Mancini.
The mortality risk depends on whether high-risk organs such as the liver or spleen are involved, as well as the early response to treatment, said Dr. Mancini, professor of pediatrics and dermatology at Northwestern University and Children’s Memorial Hospital in Chicago.
Langerhans cell histiocytosis (LCH) was one of five pediatric dermatology diagnoses Dr. Mancini urged dermatologists at the annual Caribbean Dermatology Symposium not to miss. Prompt identification of these conditions can improve young patients’ outcomes and reduce the risk for complications later, he said.
The clinical diagnosis of LCH in infants and children includes scaly erythematous seborrheic-like dermatitis, brown or red papules that may be lichenoid, and erythema in skin fold areas including the groin and the anterior neck folds, often with punctate erosions, he noted. Petechiae may be present, and crusted papules on the palms and soles are occasionally seen in young children.
Histopathology of LCH shows a granulomatous infiltrate that is epidermotropic, and the presence of positive CD1a or CD207 staining confirms the diagnosis, he said. An important distinction between LCH and streptococcal intertrigo: The strep responds rapidly to antibiotics and the erosive changes are more diffuse rather than focal.
Kawasaki Disease
"The most feared complication of Kawasaki disease (KD) is that of coronary artery aneurysm," said Dr. Mancini. "So it is very important to think about this disorder and get a rapid diagnosis," he said. The diagnosis is purely clinical, he noted, without the availability of a confirmatory diagnostic test at this time. Therefore, "have a high index of suspicion" for this disorder, he said.
Clinical criteria for KD include oropharyngeal changes, extremity changes, and a polymorphous skin eruption. Common prodromal symptoms may include irritability, vomiting, anorexia, cough, diarrhea, abdominal pain, and joint pain. "These kids appear sick," Dr. Mancini said.
Skin findings in KD may take on several morphologies, including morbilliform, urticarial, serum sickness-like, or even pustular.
One key finding that is suggestive of KD: Accentuation of erythema in skin folds, especially in the form of perineal desquamation, he said. However, blisters and purpura are not typically associated with the disorder.
Congenital Immunodeficiency
"In many patients, skin manifestations may be the presenting finding" of congenital immunodeficiency, Dr. Mancini said. In a recent study of 128 patients with primary immunodeficiency, 48% had skin manifestations, and these were the presenting feature in 39% with total PID and 82% of those with skin lesions (Pediatr. Dermatol. 2011;28;494-501).
Consider congenital immunodeficiency (CID) in cases of severe atopic or seborrheic dermatitis, intertrigo, or erythroderma that are resistant to therapy, said Dr. Mancini. Growth failure, alopecia, and recurrent infections (especially with unusual organisms) also can be signs of CID.
Graft vs. host disease (GVHD) in a skin biopsy increases suspicion for CID, he added.
An initial evaluation for suspected CID should include a complete blood count, quantitative immunoglobulins, mitogen stimulation assay, tetanus titer, T- and B-cell flow cytometry, and nitroblue tetrazolium or chronic granulomatous disease flow assay, said Dr. Mancini.
There are many congenital immunodeficiencies that may present with skin findings, including Wiskott-Aldrich syndrome, chronic mucocutaneous candidiasis, severe combined immunodeficiency, and leukocyte adhesion deficiency.
Drug Hypersensitivity Syndrome (DRESS)
Also known as Drug Reaction With Eosinophilia and Systemic Symptoms (DRESS), drug hypersensitivity tends to occur from 3-8 weeks after starting a particular medication, said Dr. Mancini. A skin rash is one of the most common findings, occurring in 77% to 100% of patients, he said. Facial edema is common, especially in the periorbital area. DRESS also can include fever, lymph node enlargement, and internal organ involvement.
Other clinical symptoms include conjunctivitis, pharyngitis, vomiting, and diarrhea. Telltale hematology findings indicative of DRESS include atypical lymphocytes and eosinophilia; pancytopenia occasionally appears.
The first line of defense is recognition and withdrawal from the drug. Serial monitoring of liver function studies is vital, given the fulminant hepatitis that can ensue, Dr. Mancini said. Treatment with systemic steroids and/or intravenous immunoglobulin is occasionally used, albeit controversially, he noted. Complete resolution of symptoms may take as long as 6 months.
Neonatal Herpes
The risk for neonatal infection with herpes simplex virus (HSV) is highest when the mother has active genital herpes at the time of delivery, Dr. Mancini said. If left untreated, the mortality rate for central nervous system or disseminated neonatal herpes is estimated at 50%-90%, so rapid recognition and diagnosis is vital, he said. The central nervous system, liver, lungs, adrenal glands, and bone marrow are important sites of potential involvement when the process disseminates, he added.
The classic skin presentation of neonatal HSV infection is vesicles and vesiculopustules that may be grouped on a red base or may become hemorrhagic. Bullae, widespread skin erosions, and polycyclic patches occasionally may be seen, and scarring may be present. Prompt evaluation is important, and intravenous acyclovir should be immediately instituted if the diagnosis of neonatal HSV is being considered.
Dr. Mancini said he had no financial conflicts to disclose.
EXPERT ANALYSIS FROM THE ANNUAL CARIBBEAN DERMATOLOGY SYMPOSIUM
Vehicle Selection Is Key to Topically Treating Psoriasis
RIO GRANDE, P.R. – When it comes to treating psoriasis patients with topical products, the location of the psoriasis helps determine the best vehicle for delivery, according to Dr. Eric W. Baum.
Some topical therapies work well when used alone, while others are more effective in combination with other products, Dr. Baum said at the annual Caribbean Dermatology Symposium. But the success of any topical psoriasis therapy depends on the vehicle, and the right vehicle varies for each patient.
"The vehicle can greatly influence percutaneous absorption and therefore increase therapeutic efficacy," said Dr. Baum of the University of Alabama at Birmingham.
"Topical psoriasis treatment is quite interesting, because there are so many different choices," said Dr. Baum. "I might use a foam on the hands because it is less sticky; I’ll use sprays with different types of nozzles to penetrate areas that are hard to reach."
Vehicle options for topical psoriasis therapy include cream, ointment, tape, gel, lotion, aerosol spray, foam, solution, shampoo, powder, and oil.
There is no silver bullet when it comes to psoriasis, but topical therapy remains many dermatologists’ first choice for initial treatment, noted Dr. Baum, who shared recent data on three products.
Foam
In a phase III study, clobetasol propionate 0.05% foam (Olux-E, Stiefel) significantly improved erythema, scaling, and plaque thickness in patients with mild to moderate plaque psoriasis after 2 weeks of use, compared with control foam. Based on these findings, the foam is considered to be safe for use in mild to moderate psoriasis patients aged 12 years and older, said Dr. Baum.
In a previous unpublished, company-funded study of Olux-E for moderate to severe atopic dermatitis, patients rated several cosmetic qualities of the foam higher than for other vehicles, including the ability to be easily spread, ease of application, quick absorption, lack of fragrance, and lack of residue, he noted.
Spray
Sprays can be an excellent choice for the scalp or other hairy areas, said Dr. Baum.
In an open-label noncomparator study of triamcinolone acetonide 0.2% spray (Kenalog, Bristol-Myers Squibb) for steroid-responsive dermatoses, 85% of 39 patients reported improvement after 7 days of use. In addition, 95% of patients said they preferred the spray over creams and ointments, 92% said they would request the spray for future use, and more than half reported satisfaction with the cooling effects of the spray (J. Clin. Aesthet. Dermatol. 2010;3:27-31).
The study also found that patients who applied the spray twice daily for scalp or leg psoriasis showed visible improvements after 1 week, suggesting that the long nozzle associated with the spray vehicle allowed for better penetration, said Dr. Baum.
Cream
For large areas of dermatoses, a biphasic cream may be particularly effective, according to Dr. Baum. He and his colleagues studied the effectiveness and patient acceptance of halcinonide 0.1% (Halog, Ranbaxy) for treating large, steroid-responsive dermatoses (J. Clin. Aesthet. Dermatol. 2011;4:29-33).
At baseline, 40 patients aged 23-85 years were diagnosed with moderate to severe dermatoses, and 83% had psoriasis (2 patients were lost to follow-up). After 28 days of treatment with halcinonide cream, 47% of patients were clear or almost clear, said Dr. Baum. And of equal importance, the vehicle was popular with patients; 95% said they "liked the way the product spread on the skin," Dr. Baum said. In addition, 87% said they would ask for the same cream again for another skin problem.
"Halog cream has been around for many years" but physicians may not realize that it is a biphasic cream, said Dr. Baum. "The biphasic cream allows penetration of the medication immediately, and then a delayed response."
When treating psoriasis topically, don’t forget to consider the potency of the product. "If you use a high-potency product in certain areas, you will have a greater risk of some of the adverse side effects of topical corticosteroids that none of us want," said Dr. Baum. It is important to consider these different factors when choosing a topical psoriasis product for a particular location.
Dr. Baum has served as an advisory board member, speaker, investigator, or consultant for Amgen, DUSA, Galderma, GlaxoSmithKline (Stiefel), Intendis (Bayer), Merz, and Ranbaxy.
RIO GRANDE, P.R. – When it comes to treating psoriasis patients with topical products, the location of the psoriasis helps determine the best vehicle for delivery, according to Dr. Eric W. Baum.
Some topical therapies work well when used alone, while others are more effective in combination with other products, Dr. Baum said at the annual Caribbean Dermatology Symposium. But the success of any topical psoriasis therapy depends on the vehicle, and the right vehicle varies for each patient.
"The vehicle can greatly influence percutaneous absorption and therefore increase therapeutic efficacy," said Dr. Baum of the University of Alabama at Birmingham.
"Topical psoriasis treatment is quite interesting, because there are so many different choices," said Dr. Baum. "I might use a foam on the hands because it is less sticky; I’ll use sprays with different types of nozzles to penetrate areas that are hard to reach."
Vehicle options for topical psoriasis therapy include cream, ointment, tape, gel, lotion, aerosol spray, foam, solution, shampoo, powder, and oil.
There is no silver bullet when it comes to psoriasis, but topical therapy remains many dermatologists’ first choice for initial treatment, noted Dr. Baum, who shared recent data on three products.
Foam
In a phase III study, clobetasol propionate 0.05% foam (Olux-E, Stiefel) significantly improved erythema, scaling, and plaque thickness in patients with mild to moderate plaque psoriasis after 2 weeks of use, compared with control foam. Based on these findings, the foam is considered to be safe for use in mild to moderate psoriasis patients aged 12 years and older, said Dr. Baum.
In a previous unpublished, company-funded study of Olux-E for moderate to severe atopic dermatitis, patients rated several cosmetic qualities of the foam higher than for other vehicles, including the ability to be easily spread, ease of application, quick absorption, lack of fragrance, and lack of residue, he noted.
Spray
Sprays can be an excellent choice for the scalp or other hairy areas, said Dr. Baum.
In an open-label noncomparator study of triamcinolone acetonide 0.2% spray (Kenalog, Bristol-Myers Squibb) for steroid-responsive dermatoses, 85% of 39 patients reported improvement after 7 days of use. In addition, 95% of patients said they preferred the spray over creams and ointments, 92% said they would request the spray for future use, and more than half reported satisfaction with the cooling effects of the spray (J. Clin. Aesthet. Dermatol. 2010;3:27-31).
The study also found that patients who applied the spray twice daily for scalp or leg psoriasis showed visible improvements after 1 week, suggesting that the long nozzle associated with the spray vehicle allowed for better penetration, said Dr. Baum.
Cream
For large areas of dermatoses, a biphasic cream may be particularly effective, according to Dr. Baum. He and his colleagues studied the effectiveness and patient acceptance of halcinonide 0.1% (Halog, Ranbaxy) for treating large, steroid-responsive dermatoses (J. Clin. Aesthet. Dermatol. 2011;4:29-33).
At baseline, 40 patients aged 23-85 years were diagnosed with moderate to severe dermatoses, and 83% had psoriasis (2 patients were lost to follow-up). After 28 days of treatment with halcinonide cream, 47% of patients were clear or almost clear, said Dr. Baum. And of equal importance, the vehicle was popular with patients; 95% said they "liked the way the product spread on the skin," Dr. Baum said. In addition, 87% said they would ask for the same cream again for another skin problem.
"Halog cream has been around for many years" but physicians may not realize that it is a biphasic cream, said Dr. Baum. "The biphasic cream allows penetration of the medication immediately, and then a delayed response."
When treating psoriasis topically, don’t forget to consider the potency of the product. "If you use a high-potency product in certain areas, you will have a greater risk of some of the adverse side effects of topical corticosteroids that none of us want," said Dr. Baum. It is important to consider these different factors when choosing a topical psoriasis product for a particular location.
Dr. Baum has served as an advisory board member, speaker, investigator, or consultant for Amgen, DUSA, Galderma, GlaxoSmithKline (Stiefel), Intendis (Bayer), Merz, and Ranbaxy.
RIO GRANDE, P.R. – When it comes to treating psoriasis patients with topical products, the location of the psoriasis helps determine the best vehicle for delivery, according to Dr. Eric W. Baum.
Some topical therapies work well when used alone, while others are more effective in combination with other products, Dr. Baum said at the annual Caribbean Dermatology Symposium. But the success of any topical psoriasis therapy depends on the vehicle, and the right vehicle varies for each patient.
"The vehicle can greatly influence percutaneous absorption and therefore increase therapeutic efficacy," said Dr. Baum of the University of Alabama at Birmingham.
"Topical psoriasis treatment is quite interesting, because there are so many different choices," said Dr. Baum. "I might use a foam on the hands because it is less sticky; I’ll use sprays with different types of nozzles to penetrate areas that are hard to reach."
Vehicle options for topical psoriasis therapy include cream, ointment, tape, gel, lotion, aerosol spray, foam, solution, shampoo, powder, and oil.
There is no silver bullet when it comes to psoriasis, but topical therapy remains many dermatologists’ first choice for initial treatment, noted Dr. Baum, who shared recent data on three products.
Foam
In a phase III study, clobetasol propionate 0.05% foam (Olux-E, Stiefel) significantly improved erythema, scaling, and plaque thickness in patients with mild to moderate plaque psoriasis after 2 weeks of use, compared with control foam. Based on these findings, the foam is considered to be safe for use in mild to moderate psoriasis patients aged 12 years and older, said Dr. Baum.
In a previous unpublished, company-funded study of Olux-E for moderate to severe atopic dermatitis, patients rated several cosmetic qualities of the foam higher than for other vehicles, including the ability to be easily spread, ease of application, quick absorption, lack of fragrance, and lack of residue, he noted.
Spray
Sprays can be an excellent choice for the scalp or other hairy areas, said Dr. Baum.
In an open-label noncomparator study of triamcinolone acetonide 0.2% spray (Kenalog, Bristol-Myers Squibb) for steroid-responsive dermatoses, 85% of 39 patients reported improvement after 7 days of use. In addition, 95% of patients said they preferred the spray over creams and ointments, 92% said they would request the spray for future use, and more than half reported satisfaction with the cooling effects of the spray (J. Clin. Aesthet. Dermatol. 2010;3:27-31).
The study also found that patients who applied the spray twice daily for scalp or leg psoriasis showed visible improvements after 1 week, suggesting that the long nozzle associated with the spray vehicle allowed for better penetration, said Dr. Baum.
Cream
For large areas of dermatoses, a biphasic cream may be particularly effective, according to Dr. Baum. He and his colleagues studied the effectiveness and patient acceptance of halcinonide 0.1% (Halog, Ranbaxy) for treating large, steroid-responsive dermatoses (J. Clin. Aesthet. Dermatol. 2011;4:29-33).
At baseline, 40 patients aged 23-85 years were diagnosed with moderate to severe dermatoses, and 83% had psoriasis (2 patients were lost to follow-up). After 28 days of treatment with halcinonide cream, 47% of patients were clear or almost clear, said Dr. Baum. And of equal importance, the vehicle was popular with patients; 95% said they "liked the way the product spread on the skin," Dr. Baum said. In addition, 87% said they would ask for the same cream again for another skin problem.
"Halog cream has been around for many years" but physicians may not realize that it is a biphasic cream, said Dr. Baum. "The biphasic cream allows penetration of the medication immediately, and then a delayed response."
When treating psoriasis topically, don’t forget to consider the potency of the product. "If you use a high-potency product in certain areas, you will have a greater risk of some of the adverse side effects of topical corticosteroids that none of us want," said Dr. Baum. It is important to consider these different factors when choosing a topical psoriasis product for a particular location.
Dr. Baum has served as an advisory board member, speaker, investigator, or consultant for Amgen, DUSA, Galderma, GlaxoSmithKline (Stiefel), Intendis (Bayer), Merz, and Ranbaxy.
EXPERT ANALYSIS FROM THE ANNUAL CARIBBEAN DERMATOLOGY SYMPOSIUM
Earlier Is Better in Psoriasis Treatment
RIO GRANDE, P.R. – Treating psoriasis patients earlier in life could help prevent later physical and psychological problems, according to Dr. Alexa B. Kimball.
"We used to think that we should save our therapies until our patients really needed them, because we were afraid that toxicity might accumulate," Dr. Kimball said at the annual Caribbean Dermatology Symposium. However, that thinking has changed, thanks in part to the availability of safer treatment options.
But of equal importance, "treating patients early in their disease may have an impact that affects the rest of their lives," including jobs, education, socioeconomic status, and curbing the development of health problems like obesity, cardiovascular disease, and psychiatric disorders, she said.
The quality of life issues associated with psoriasis are well known, but recent data confirm that physical and mental comorbidities start in childhood.
According to recent data from the National Psoriasis Foundation, 38% of children with psoriasis reported being bullied because of their condition, noted Dr. Kimball of Massachusetts General Hospital and Harvard Medical School, both in Boston.
Another study found that approximately one-third of children aged 4-17 years with psoriasis had a body mass index greater than the 95th percentile (N. Engl. J. Med. 2008;358:241-51). Conditions such as childhood obesity are not easily managed, and have significant implications for future health, she said.
In a retrospective study of 7,404 psoriasis patients younger than 18 years and 37,020 healthy controls, children with psoriasis were significantly more likely than controls to develop any psychiatric disorder (5% vs. 4%), depression (3% vs. 2%), and anxiety (2% vs. 1%), Dr. Kimball and her colleagues found (J. Am. Acad. Dermatol. 2012 Jan. 16 [doi:10.1016/j.jaad.2011.11.948]).
And the likelihood of comorbidities in psoriasis patients continues as they grow up, she said. "Chronic disease interacts with psychosocial and health events in a complex and ongoing manner throughout a person’s life."
Comorbidities in psoriasis patients appear to accumulate over time. Dr. Kimball cited data from the Nurses’ Health Study II, a cohort including more than 100,000 women who were aged 27-44 years in 1991. In a subset of 1,813 women with psoriasis, the risk of diabetes was approximately 60% higher, and the risk of hypertension was almost 20% higher, compared with women without psoriasis (Arch. Dermatol. 2009;145:379-82).
In a case-control study conducted by Dr. Kimball and her colleagues, cardiovascular disease, diabetes, depression, hyperlipidemia, hypertension, and obesity all increased significantly in psoriasis patients, compared with healthy controls, over a 4-year follow-up period (J. Am. Acad. Dermatol. 2010;62[suppl. 1]:AB3).
These findings suggest that medical comorbidities associated with psoriasis accumulate over time; therefore, aggressive treatment of psoriasis in younger patients could improve their psychological and physical quality of life, Dr. Kimball said. Although there are no recommendations for additional health screening for psoriasis patients beyond the age-recommended preventive health measures, "younger patients especially need to be monitored for psychiatric issues," she said. And these patients should be kept up to date on vaccinations, particularly the annual flu vaccine and the human papillomavirus vaccine.
Dr. Kimball reported receiving grants, honoraria, consulting fees, and other support from Abbott, Amgen, and Janssen Pharmaceuticals.
RIO GRANDE, P.R. – Treating psoriasis patients earlier in life could help prevent later physical and psychological problems, according to Dr. Alexa B. Kimball.
"We used to think that we should save our therapies until our patients really needed them, because we were afraid that toxicity might accumulate," Dr. Kimball said at the annual Caribbean Dermatology Symposium. However, that thinking has changed, thanks in part to the availability of safer treatment options.
But of equal importance, "treating patients early in their disease may have an impact that affects the rest of their lives," including jobs, education, socioeconomic status, and curbing the development of health problems like obesity, cardiovascular disease, and psychiatric disorders, she said.
The quality of life issues associated with psoriasis are well known, but recent data confirm that physical and mental comorbidities start in childhood.
According to recent data from the National Psoriasis Foundation, 38% of children with psoriasis reported being bullied because of their condition, noted Dr. Kimball of Massachusetts General Hospital and Harvard Medical School, both in Boston.
Another study found that approximately one-third of children aged 4-17 years with psoriasis had a body mass index greater than the 95th percentile (N. Engl. J. Med. 2008;358:241-51). Conditions such as childhood obesity are not easily managed, and have significant implications for future health, she said.
In a retrospective study of 7,404 psoriasis patients younger than 18 years and 37,020 healthy controls, children with psoriasis were significantly more likely than controls to develop any psychiatric disorder (5% vs. 4%), depression (3% vs. 2%), and anxiety (2% vs. 1%), Dr. Kimball and her colleagues found (J. Am. Acad. Dermatol. 2012 Jan. 16 [doi:10.1016/j.jaad.2011.11.948]).
And the likelihood of comorbidities in psoriasis patients continues as they grow up, she said. "Chronic disease interacts with psychosocial and health events in a complex and ongoing manner throughout a person’s life."
Comorbidities in psoriasis patients appear to accumulate over time. Dr. Kimball cited data from the Nurses’ Health Study II, a cohort including more than 100,000 women who were aged 27-44 years in 1991. In a subset of 1,813 women with psoriasis, the risk of diabetes was approximately 60% higher, and the risk of hypertension was almost 20% higher, compared with women without psoriasis (Arch. Dermatol. 2009;145:379-82).
In a case-control study conducted by Dr. Kimball and her colleagues, cardiovascular disease, diabetes, depression, hyperlipidemia, hypertension, and obesity all increased significantly in psoriasis patients, compared with healthy controls, over a 4-year follow-up period (J. Am. Acad. Dermatol. 2010;62[suppl. 1]:AB3).
These findings suggest that medical comorbidities associated with psoriasis accumulate over time; therefore, aggressive treatment of psoriasis in younger patients could improve their psychological and physical quality of life, Dr. Kimball said. Although there are no recommendations for additional health screening for psoriasis patients beyond the age-recommended preventive health measures, "younger patients especially need to be monitored for psychiatric issues," she said. And these patients should be kept up to date on vaccinations, particularly the annual flu vaccine and the human papillomavirus vaccine.
Dr. Kimball reported receiving grants, honoraria, consulting fees, and other support from Abbott, Amgen, and Janssen Pharmaceuticals.
RIO GRANDE, P.R. – Treating psoriasis patients earlier in life could help prevent later physical and psychological problems, according to Dr. Alexa B. Kimball.
"We used to think that we should save our therapies until our patients really needed them, because we were afraid that toxicity might accumulate," Dr. Kimball said at the annual Caribbean Dermatology Symposium. However, that thinking has changed, thanks in part to the availability of safer treatment options.
But of equal importance, "treating patients early in their disease may have an impact that affects the rest of their lives," including jobs, education, socioeconomic status, and curbing the development of health problems like obesity, cardiovascular disease, and psychiatric disorders, she said.
The quality of life issues associated with psoriasis are well known, but recent data confirm that physical and mental comorbidities start in childhood.
According to recent data from the National Psoriasis Foundation, 38% of children with psoriasis reported being bullied because of their condition, noted Dr. Kimball of Massachusetts General Hospital and Harvard Medical School, both in Boston.
Another study found that approximately one-third of children aged 4-17 years with psoriasis had a body mass index greater than the 95th percentile (N. Engl. J. Med. 2008;358:241-51). Conditions such as childhood obesity are not easily managed, and have significant implications for future health, she said.
In a retrospective study of 7,404 psoriasis patients younger than 18 years and 37,020 healthy controls, children with psoriasis were significantly more likely than controls to develop any psychiatric disorder (5% vs. 4%), depression (3% vs. 2%), and anxiety (2% vs. 1%), Dr. Kimball and her colleagues found (J. Am. Acad. Dermatol. 2012 Jan. 16 [doi:10.1016/j.jaad.2011.11.948]).
And the likelihood of comorbidities in psoriasis patients continues as they grow up, she said. "Chronic disease interacts with psychosocial and health events in a complex and ongoing manner throughout a person’s life."
Comorbidities in psoriasis patients appear to accumulate over time. Dr. Kimball cited data from the Nurses’ Health Study II, a cohort including more than 100,000 women who were aged 27-44 years in 1991. In a subset of 1,813 women with psoriasis, the risk of diabetes was approximately 60% higher, and the risk of hypertension was almost 20% higher, compared with women without psoriasis (Arch. Dermatol. 2009;145:379-82).
In a case-control study conducted by Dr. Kimball and her colleagues, cardiovascular disease, diabetes, depression, hyperlipidemia, hypertension, and obesity all increased significantly in psoriasis patients, compared with healthy controls, over a 4-year follow-up period (J. Am. Acad. Dermatol. 2010;62[suppl. 1]:AB3).
These findings suggest that medical comorbidities associated with psoriasis accumulate over time; therefore, aggressive treatment of psoriasis in younger patients could improve their psychological and physical quality of life, Dr. Kimball said. Although there are no recommendations for additional health screening for psoriasis patients beyond the age-recommended preventive health measures, "younger patients especially need to be monitored for psychiatric issues," she said. And these patients should be kept up to date on vaccinations, particularly the annual flu vaccine and the human papillomavirus vaccine.
Dr. Kimball reported receiving grants, honoraria, consulting fees, and other support from Abbott, Amgen, and Janssen Pharmaceuticals.
EXPERT ANALYSIS FROM THE ANNUAL CARIBBEAN DERMATOLOGY SYMPOSIUM
Malignancy Rates Remain Stable in Ustekinumab-Treated Patients
RIO GRANDE, P.R. – Malignancy rates in psoriasis patients treated with ustekinumab did not increase significantly over 4 years of follow-up, based on pooled data from 3,117 patients enrolled in ustekinumab clinical trials.
Ustekinumab has shown effectiveness for treating moderate to severe psoriasis, but due to the potential of increased risk for cancer associated with its use, patients from several clinical trials (including PHOENIX I, PHOENIX II, and ACCEPT) are still being followed, said Dr. Kim A. Papp, director of research at Probity Medical Research, Waterloo, Ont., and colleagues.
The cumulative rates for nonmelanoma skin cancer in patients treated with ustekinumab for psoriasis remained low and stable throughout the follow-up period. A total of 0.57 cancer events per 100 person-years were reported in 2009 and 0.62 cancer events per 100 person-years were reported in 2010. The findings were presented at the annual Caribbean Dermatology Symposium.
In the complete analysis that included 6,791 patient-years of follow-up, 41 patients treated with any dose of ustekinumab developed at least one nonmelanoma skin cancer, and 3 patients developed both basal cell carcinoma and squamous cell carcinoma.
Another 42 patients developed at least one other malignancy, including 4 patients with melanoma in situ. However, no cases of invasive melanoma were observed during the study period. The other most common malignancies were prostate cancer (12 patients), colorectal cancer (4 patients) and breast cancer (3 patients).
By comparison, 39 individuals in the general population (based on the National Cancer Institute’s Surveillance, Epidemiology, and End Results database) developed at least one malignancy.
The findings were limited by the inclusion of several studies of varying lengths and by the inclusion criteria that can make comparison with the general population difficult, the researchers noted. The results suggest that rates of nonmelanoma skin cancer and other malignancies in psoriasis patients taking ustekinumab do not increase over time.
However, "additional long term data from clinical trials, observational registries, and postmarketing reporting databases will continue to define the ustekinumab malignancy risk profile," they wrote.
The study was sponsored by Centocor, which manufactures ustekinmab.
RIO GRANDE, P.R. – Malignancy rates in psoriasis patients treated with ustekinumab did not increase significantly over 4 years of follow-up, based on pooled data from 3,117 patients enrolled in ustekinumab clinical trials.
Ustekinumab has shown effectiveness for treating moderate to severe psoriasis, but due to the potential of increased risk for cancer associated with its use, patients from several clinical trials (including PHOENIX I, PHOENIX II, and ACCEPT) are still being followed, said Dr. Kim A. Papp, director of research at Probity Medical Research, Waterloo, Ont., and colleagues.
The cumulative rates for nonmelanoma skin cancer in patients treated with ustekinumab for psoriasis remained low and stable throughout the follow-up period. A total of 0.57 cancer events per 100 person-years were reported in 2009 and 0.62 cancer events per 100 person-years were reported in 2010. The findings were presented at the annual Caribbean Dermatology Symposium.
In the complete analysis that included 6,791 patient-years of follow-up, 41 patients treated with any dose of ustekinumab developed at least one nonmelanoma skin cancer, and 3 patients developed both basal cell carcinoma and squamous cell carcinoma.
Another 42 patients developed at least one other malignancy, including 4 patients with melanoma in situ. However, no cases of invasive melanoma were observed during the study period. The other most common malignancies were prostate cancer (12 patients), colorectal cancer (4 patients) and breast cancer (3 patients).
By comparison, 39 individuals in the general population (based on the National Cancer Institute’s Surveillance, Epidemiology, and End Results database) developed at least one malignancy.
The findings were limited by the inclusion of several studies of varying lengths and by the inclusion criteria that can make comparison with the general population difficult, the researchers noted. The results suggest that rates of nonmelanoma skin cancer and other malignancies in psoriasis patients taking ustekinumab do not increase over time.
However, "additional long term data from clinical trials, observational registries, and postmarketing reporting databases will continue to define the ustekinumab malignancy risk profile," they wrote.
The study was sponsored by Centocor, which manufactures ustekinmab.
RIO GRANDE, P.R. – Malignancy rates in psoriasis patients treated with ustekinumab did not increase significantly over 4 years of follow-up, based on pooled data from 3,117 patients enrolled in ustekinumab clinical trials.
Ustekinumab has shown effectiveness for treating moderate to severe psoriasis, but due to the potential of increased risk for cancer associated with its use, patients from several clinical trials (including PHOENIX I, PHOENIX II, and ACCEPT) are still being followed, said Dr. Kim A. Papp, director of research at Probity Medical Research, Waterloo, Ont., and colleagues.
The cumulative rates for nonmelanoma skin cancer in patients treated with ustekinumab for psoriasis remained low and stable throughout the follow-up period. A total of 0.57 cancer events per 100 person-years were reported in 2009 and 0.62 cancer events per 100 person-years were reported in 2010. The findings were presented at the annual Caribbean Dermatology Symposium.
In the complete analysis that included 6,791 patient-years of follow-up, 41 patients treated with any dose of ustekinumab developed at least one nonmelanoma skin cancer, and 3 patients developed both basal cell carcinoma and squamous cell carcinoma.
Another 42 patients developed at least one other malignancy, including 4 patients with melanoma in situ. However, no cases of invasive melanoma were observed during the study period. The other most common malignancies were prostate cancer (12 patients), colorectal cancer (4 patients) and breast cancer (3 patients).
By comparison, 39 individuals in the general population (based on the National Cancer Institute’s Surveillance, Epidemiology, and End Results database) developed at least one malignancy.
The findings were limited by the inclusion of several studies of varying lengths and by the inclusion criteria that can make comparison with the general population difficult, the researchers noted. The results suggest that rates of nonmelanoma skin cancer and other malignancies in psoriasis patients taking ustekinumab do not increase over time.
However, "additional long term data from clinical trials, observational registries, and postmarketing reporting databases will continue to define the ustekinumab malignancy risk profile," they wrote.
The study was sponsored by Centocor, which manufactures ustekinmab.
FROM THE ANNUAL CARIBBEAN DERMATOLOGY SYMPOSIUM
Major Finding: A total of 0.57 cancer events per 100 person-years were reported in 2009 and 0.62 cancer events per 100 person-years were reported in 2010.
Data Source: A review of 3,117 adults with psoriasis who were enrolled in ustekinumab clinical trials.
Disclosures: The study was sponsored by Centocor, which manufactures ustekinumab.