User login
› Screen for hypertension in all children over the age of 3 at every visit. C
› Order laboratory evaluation, echocardiography, and renovascular imaging for all children given a diagnosis of hypertension. C
› Advise parents that children with prehypertension and stage 1 hypertension without target-organ damage are eligible to participate in competitive athletics, but those with stage 2 hypertension, target-organ damage, or symptomatic hypertension should not engage in high-static sports (eg, gymnastics, weightlifting, wrestling) until BP is well controlled. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Childhood hypertension is on the rise: Recent data from the National Health and Nutrition Survey suggest 10% of children and adolescents have prehypertension and 4% have hypertension.1-4 Unfortunately, the condition often is missed. In a study of 14,187 children and adolescents who had at least 3 well-child visits at an outpatient academic medical center, 507 patients met the criteria for hypertension, yet only 131 (26%) had this diagnosis documented in their electronic health record.5
In a survey of 89 pediatricians, >50% of respondents said they were not familiar with the most current published recommendations for diagnosing and treating pediatric hypertension.6 Respondents also indicated that the most common reason for not initiating pharmacotherapy for children with hypertension was a lack of familiarity with appropriate antihypertensive agents (54%), followed by concern for adverse medication effects. Delayed diagnosis, evaluation, and treatment of hypertension in young patients can increase the likelihood of serious consequences, including target-organ damage such as left ventricular hypertrophy (LVH). In this review, we’ll describe the factors that put children and adolescents at risk for hypertension, and offer an evidence-based approach to diagnosis and treatment.
Obesity is a key risk factor
An estimated 17% of children aged 2 to 19 are obese.7 Obesity increases a child’s risk for hypertension by approximately 3- to 5-fold, and body mass index (BMI) is greater in children with primary hypertension compared with those with secondary hypertension.8 Hypertension is more common among Hispanic and non-Hispanic black male children and adolescents compared with their white counterparts; these ethnic disparities are not found in females.9,10 Poor diets and physical inactivity further contribute to obesity and hypertension risk. Children who were born preterm or had a very low birth weight also are at increased risk.11
Unchecked hypertension can lead to cardiac, vascular damage
Some children and adolescents with undiagnosed and untreated hypertension have evidence of target-organ damage, including cardiac dysfunction and pathologic vascular abnormalities. LVH is present in 20% to 41% of children and adolescents with hypertension.12,13 Carotid intima-media thickness, an established surrogate marker for atherosclerosis, is abnormally increased in children with hypertension, even after adjusting for BMI.14 Other target organ effects include impaired cognitive function, reduced glomerular filtration rate, microalbuminuria, and retinal arteriolar narrowing.15-17
Pediatric hypertension may persist into adulthood. A meta-analysis of more than 50 studies found that elevated blood pressure (BP) in childhood increases the risk for hypertension as an adult.18
NHLBI recommendations call for a BP check at every visit
The National Heart, Lung, and Blood Institute (NHLBI) Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (“the 4th Report”) recommends measuring BP in all children over age 3 during every health care visit.12 Children under age 3 should have their BP checked in certain circumstances, including preterm delivery, congenital heart disease, recurrent urinary tract infections, renal/urologic disease, organ transplantation, malignancy, and systemic illnesses associated with hypertension.12 The 4th Report is endorsed by the American Academy of Pediatrics (AAP); however, the American Academy of Family Physicians and the US Preventive Services Task Force have concluded that the evidence is insufficient to recommend for or against routine screening for hypertension in children and adolescents to reduce the risk of cardiovascular disease (CVD).19,20
Does the child have hypertension? That depends on several factors
Determining whether a child has hypertension requires that you consult national BP standards to determine if he or she is within the normal range. Normal BP standards for children and adolescents are based on gender, age, and height percentile, and provide a precise classification based on body size.12 These tables are available from the NHLBI Web site at http://www.nhlbi.nih.gov/guidelines/hypertension/child_tbl.htm. Height percentiles in these tables correspond with the Centers for Disease Control and Prevention (CDC) growth charts published in 2000.21 The Baylor College of Medicine Children’s Nutrition Research Center has a web-based calculator to help physicians determine BP percentiles in children and adolescents; it is available at http://www.bcm.edu/bodycomplab/Flashapps/BPVAgeChartpage.html. The International Pediatric Hypertension Association also offers BP charts and calculators at http://www.iphapediatrichypertension.org.
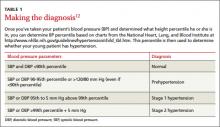
The diagnostic parameters for pediatric hypertension are listed in TABLE 1.12 The higher systolic or diastolic BP percentile value is used to determine a child’s overall BP category. A child is considered normotensive if the BP is <90th percentile. Hypertension is an average systolic or diastolic BP that is ≥95th percentile on at least 3 separate occasions. Stage 1 hypertension is BP levels ranging from the 95th percentile to 5 mm Hg above the 99th percentile, and stage 2 hypertension is BP levels greater than 5 mm Hg above the 99th percentile.
For example, assume you are evaluating a 12-year-old boy who is 61 inches tall and has a BP of 129/87 mm Hg. According to the CDC growth charts, his height puts him in the 75th percentile for his age. Using the NHLBI chart, you determine that he falls in the 95th-99th percentile for BP, and thus, using the categories in TABLE 1, is given a diagnosis of Stage 1 hypertension.
Accurate BP measurement requires using an appropriate cuff size that covers 80% of the child’s upper arm. When the child is between cuff sizes, use the larger cuff because small cuffs overestimate BP readings. BP readings should be taken on the right arm with the arm supported at heart level after the child has been sitting quietly for at least 5 minutes.12 One study showed that the initial BP readings taken in the triage area were significantly higher—often by >10 mm Hg—compared with follow-up measurements in the examination room.22
The preferred method of BP measurement is auscultation; however, oscillometric devices also are acceptable. These devices are easier to use, help eliminate digit bias, and minimize observer variation, but they typically read approximately 6 to 9 mm Hg higher than auscultation.23 For any BP measurement obtained by oscillometry that is >90th percentile, repeat the measurement by auscultation at least twice during the same office visit, and use an average of the repeated measurements.12 Obtain measurements of a lower extremity when you suspect congenital heart disease (eg, aortic coarctation). For any patient in whom you confirm a BP measurement >95th percentile, repeat the measurement within 2 weeks; for BPs >99th percentile, reevaluation should occur within one week.
Ambulatory BP monitoring (ABPM). Because BP measurements have a circadian pattern (higher during the day and reduced by 10% during sleep24) an ABPM device that provides 50 to 60 readings over 24 hours can be useful when evaluating children and adolescents for white-coat hypertension (elevated clinic BP with normal ambulatory BP), masked hypertension (normal clinic BP with elevated ambulatory BP), prehypertension and secondary hypertension (BP generally does not follow circadian patterns).25 ABPM is more accurate than BP self-measurement, but usually is limited to children older than age 5
Steps to take for clinical evaluation
Start by conducting a thorough history and physical examination, looking for information that can help you select the most appropriate tests for the next phase of evaluation.8,12 Calculate the patient’s BMI to screen for obesity, ask about a family history of hypertension or CVD, and determine if the patient is taking any medications that might cause hypertension, such as amphetamines, corticosteroids, or cyclosporine.8 Assess for signs and symptoms that suggest an underlying disease, such as renal disease (hematuria, edema, fatigue) or heart disease (chest pain, exertional dyspnea, palpitations).12
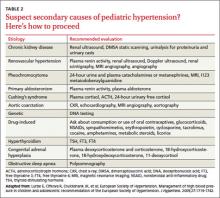
All children diagnosed with hypertension should be screened for secondary causes (TABLE 2). The recommended evaluation is to obtain a renal function panel, electrolytes, urinalysis, urine culture, complete blood count, renovascular imaging, and echocardiogram.12 The most common etiologies for secondary hypertension are renal parenchymal disease (68%), renovascular abnormalities (10%), and endocrinopathies (10%).26 Other causes, such as aortic coarctation, obstructive sleep apnea, iatrogenic factors (eg, toxins, medications, drugs of abuse), and genitourinary abnormalities, account for only a small percentage of cases and should be investigated as clinically indicated.26
Renovascular assessment depends on facility expertise. Imaging options include renal ultrasound (with or without Doppler), computed tomography angiography, renal flow scan, and magnetic resonance angiography. These studies have similar sensitivities and specificities.27 For patients in whom you strongly suspect renovascular disease, renal arteriography (digital subtraction angiography) provides the best images, although it is the most invasive study.27
Refer children and adolescents who are found to have significant abnormalities during the initial evaluation to the appropriate specialist. BP measurements often improve when secondary causes are treated.
Which drugs for which patients?
Pharmacologic management is indicated for pediatric patients with stage 1 or stage 2 hypertension, secondary hypertension, and those with evidence of target-organ damage.12 The goal of therapy is to reduce BP to <95th percentile. In patients with target organ damage, renal disease, or diabetes mellitus, the goal is <90th percentile.12,15,28 Intensive management of BP (≤50th percentile) in children with chronic kidney disease has been shown to delay progression to renal failure,29 but it is uncertain if lower BP goals can slow or prevent additional subclinical target organ damage.
Pharmacotherapy for hypertensive children or adolescents can be challenging because recommendations of which medication to use are based upon expert opinion and extrapolation from randomized trials of adults. The length of therapy (often lifelong), potential adverse effects, and unproven direct mortality benefit complicate this decision. Medication choice usually is based on physician preference or experience.12 The most common antihypertensive drugs prescribed are angiotensin-converting enzyme (ACE) inhibitors (26%), followed by diuretics (20%), and beta-blockers (17%).30,31 The starting doses and other details of medications commonly used to treat pediatric hypertension are listed in TABLE 3.28,32-34
One approach to choosing an antihypertensive drug for children is to measure the patient’s ambulatory plasma renin activity (PRA) level before initiating therapy. Those with high PRA levels (>0.65 ng/mL/h), presumably due to peripheral vasoconstriction, may benefit more from ACE inhibitors, angiotensin receptor blockers (ARBs), or beta-adrenergic antagonists.35 Individuals with low PRA levels (<0.65 ng/mL/h) maintain higher volume/sodium excess and may benefit more from diuretics or calcium channel blockers.35
Ethnicity also may guide medication selection. African American adults do not respond well to ACE inhibitor monotherapy due to decreased PRA and increased salt hypersensitivity.36 One meta-analysis found that African American children and adolescents had inadequate BP response to 6 individual ACE inhibitors, even at higher doses compared with white children and those of other ethnicities, who showed significant improvement in BP.37 ARBs may be a more effective alternative for this population.
Most experts recommend initiating a single agent at a low dose.12 A systematic review found that except for African American children, pediatric patients experienced comparable reductions in BP with ACE inhibitors (10.7/8.1 mm Hg), ARBs (10.5/6.9 mm Hg), and calcium channel blockers (9.3/7.2 mm Hg).38 In addition, ACE inhibitors and ARBs significantly reduced proteinuria by 49% and 59%, respectively.38
Schedule follow-up visits for 2 to 4 weeks (or sooner for patients with stage 2 hypertension) after initiating pharmacotherapy. If BP response is suboptimal, consider increasing the dose before adding a second agent. If the patient experiences significant adverse effects or has an inadequate BP response, changing to a drug from a different class is recommended.39 Patients who do not adequately respond to these approaches may require combination therapy; in such cases, strongly consider consultation with pediatric nephrologist or cardiologist.39 Medication compliance should be verified (eg, by pill counting, parental supervision) in patients who do not respond to therapy. Once BP control has been achieved, visits every 3 to 4 months are appropriate, with periodic laboratory monitoring, especially for children taking diuretics, ACE inhibitors, or ARBs or who have underlying renal disease.
Recommend exercise, but carefully monitor athlete's BP
Encourage obese and overweight children and adolescents to lose weight to maintain a BMI <95th percentile. Current guidelines based on expert opinion recommend that children and adolescents should engage in 60 minutes of daily physical activity.12 A meta-analysis found physical activity led to a 1% and 3% reduction in systolic and diastolic BP, respectively, although these results were not statistically significant.40
Be aware, however, that children and adolescents with hypertension who engage in certain competitive sports can significantly increase their BP and may be at risk for complications.41 According to the AAP guidelines, patients with stage 2 hypertension should not engage in high-static sports (eg, gymnastics, weightlifting, wrestling, boxing, cycling, decathlon, triathlon) until BP is well controlled.41 Patients with target-organ damage, uncontrolled hypertension, or symptomatic hypertension should not participate until BP is well controlled. Patients with prehypertension and stage 1 hypertension without target-organ damage are eligible to participate in competitive athletics. Reassess BP every 6 months in patients who are prehypertensive and every one to 2 weeks for those with stage 1 hypertension. When the patient’s BP remains <90th percentile, routine surveillance every 3 to 6 months is recommended.
What about sodium? Encourage parents of pediatric patients with hypertension to limit their child’s salt intake to 1.2 g/d for those age 4 to 8 and 1.5 g/d for older children.42 A meta-analysis found salt reduction decreased systolic BP by 1.2 mm Hg and diastolic BP by 1.3 mm Hg.43 Though these benefits are small, reducing sodium intake can be one of several lifestyle modifications, such as increased activity and quitting smoking, that can reduce young patients’ risk of hypertension and related cardiovascular sequelae.
CORRESPONDENCE
Robert Gauer, MD, Womack Army Medical Center, 2817 Reilly Road, Fort Bragg NC 28310; [email protected]
1. McNiece KL, Poffenbarger TS, Tuner JL, et al. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr. 2007;150:640-644.e1.
2. Moore WE, Eichner JE, Cohn EM, et al. Blood pressure screening of school children in a multiracial school district: the Healthy Kids Project. Am J Hypertens. 2009;22:351-356.
3. Falkner B. What exactly do the trends mean? Circulation. 2007;116:1437-1439.
4. Feber J, Ahmed M. Hypertension in children: new trends and challenges. Clin Sci (Lond). 2010;119:151-161.
5. Hansen ML, Gunn PW, Kaelber DC. Under diagnosis of hypertension in children and adolescents. JAMA. 2007;298:874-879.
6. Boneparth A, Flynn JT. Evaluation and treatment of hypertension in general pediatric practice. Clin Pediatr (Phila). 2009;48:44-49.
7. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483-490.
8. Feld LG, Corey H. Hypertension in childhood. Pediatr Rev. 2007;28:283-298.
9. Rosner B, Cook N, Portman R, et al. Blood pressure differences by ethnic group among United States children and adolescents. Hypertension. 2009;54:502-508.
10. Din-Dzietham R, Liu Y, Bielo MV, et al. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488-1496.
11. de Jong F, Monuteaux MC, van Elburg RM, et al. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension. 2012;59:226-234.
12. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 suppl 4th report):555-576.
13. Ramaswamy P, Lytrivi ID, Paul C, et al. Regression of left ventricular hypertrophy in children with antihypertensive therapy. Pediatr Nephrol. 2007;22:141-143.
14. Lande MB, Carson NL, Roy J, et al. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40-44.
15. Flynn JT. Pediatric hypertension update. Curr Opin Nephrol Hypertens. 2010;19:292-297.
16. Mitchell P, Cheung N, de Haseth K, et al. Blood pressure and retinal arteriolar narrowing in children. Hypertension. 2007;49:1156-1162.
17. Kupferman JC, Lande MB, Adams HR, et al. Primary hypertension and neurocognitive and executive functioning in school-age children. Pediatr Nephrol. 2013;28:401-408.
18. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review of meta-regression analysis. Circulation. 2008;117:3171-3180.
19. Hypertension. American Academy of Family Physicians Web site. Available at: http://www.aafp.org/patient-care/clinical-recommendations/all/hypertension.html. Accessed February 7, 2014.
20. Screening for high blood pressure: reaffirmation recommendation statement. December 2007. AHRQ publication 08-05105-EF-2. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf07/hbp/hbprs.htm. Accessed October 10, 2012.
21. Growth Charts. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/growthcharts. Accessed July 31, 2012.
22. Podoll A, Grenier M, Croix B, et al. Inaccuracy in pediatric outpatient blood pressure measurement. Pediatrics. 2007;119:e538-e543.
23. Flynn JT, Pierce CB, Miller ER 3rd, et al; Chronic Kidney Disease in Children Study Group. Reliability of resting blood pressure measurement and classification using an oscillometric device in children with chronic kidney disease. J Pediatr. 2012;160:434-440.e.1.
24. Villar VA, Liu T, Jose PA. Recent trends in pediatric hypertension research. J Med Liban. 2010;58:179-184.
25. Swartz SJ, Srivaths PR, Croix B, et al. Cost-effectiveness of ambulatory blood pressure monitoring in the initial evaluation of hypertension in children. Pediatrics. 2008;122:1177-1181.
26. Brady TM, Feld LG. Pediatric approach to hypertension. Semin Nephrol. 2009;29:379-388.
27. Tullus K, Roebuck DJ, McLaren CA, et al. Imaging in the evaluation of renovascular disease. Pediatr Nephrol. 2010;25:1049-1056.
28. Flynn JT. Management of hypertension in the young: role of antihypertensive medications. J Cardiovasc Pharmacol. 2011;58:111-120.
29. ESCAPE Trial Group; Wühl E, Trivelli A, Picca S, et al. Strict blood pressure control and progression of renal failure in children. N Engl J Med. 2009;361:1639-1650.
30. Yoon EY, Cohn L, Rocchini A, et al. Antihypertensive prescribing patterns for adolescents with primary hypertension. Pediatrics. 2012;129:e1-e8.
31. Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. J Clin Hypertens (Greenwich). 2012;14:383-387.
32. Welch WP, Yang W, Taylor-Zapata P, et al. Antihypertensive drug use by children: are the drugs labeled and indicated? J Clin Hypertens. 2012;14:388-395.
33. Lexicomp Pharmaceutical Reference, Version 1.8.3(155). Lexi-Comp Web site. Available at: http://online.lexi.com/crlsql/servlet/crlonline. Accessed July 31, 2012.
34. Robinson RF, Nahata MC, Batisky DL, et al. Pharmacologic treatment of chronic pediatric hypertension. Pediatr Drugs. 2005;7:27-40.
35. Hanevold CD. Concepts guiding therapy for hypertension in children. Expert Rev Cardiovasc Ther. 2009;7:647-657.
36. Brewster LM, van Montfrans GA, Kleijnen J. Systematic review: antihypertensive drug therapy in black patients. Ann Intern Med. 2004;141:614-627.
37. Li JS, Baker-Smith CM, Smith PB, et al. Racial differences in blood pressure response to angiotensin-converting enzyme inhibitors in children a meta-analysis. Clin Pharmacol Ther. 2008;84:315-319.
38. Simonetti GD, Rizzi M, Donadini R, et al. Effects of antihypertensive drugs on blood pressure and proteinuria in childhood. J Hypertens. 2007;25:2370-2376.
39. Lurbe E, Álvarez J, Redon J. Diagnosis and treatment of hypertension in children. Curr Hypertens Rep. 2010;12:480-486.
40. Kelley GA, Kelley KS, Tran ZV. The effects of exercise on resting blood pressure in children and adolescents: a meta-analysis of randomized controlled trials. Prev Cardiol. 2003;6:8-16.
41. McCambridge TM, Benjamin HJ, Breener JS, et al; Council on Sports Medicine and Fitness. Athletic participation by children and adolescents who have systemic hypertension. Pediatrics. 2010;125:1287-1294.
42. 2008 Physical Activity Guidelines for Americans. US Department of Health and Human Services Web site. Available at: http://www.health.gov/PAguidelines/guidelines/default.aspx. Updated March 11, 2013. Accessed February 7, 2014.
43. He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: Meta-analysis of controlled trials. Hypertension. 2006;48:861-869.
› Screen for hypertension in all children over the age of 3 at every visit. C
› Order laboratory evaluation, echocardiography, and renovascular imaging for all children given a diagnosis of hypertension. C
› Advise parents that children with prehypertension and stage 1 hypertension without target-organ damage are eligible to participate in competitive athletics, but those with stage 2 hypertension, target-organ damage, or symptomatic hypertension should not engage in high-static sports (eg, gymnastics, weightlifting, wrestling) until BP is well controlled. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Childhood hypertension is on the rise: Recent data from the National Health and Nutrition Survey suggest 10% of children and adolescents have prehypertension and 4% have hypertension.1-4 Unfortunately, the condition often is missed. In a study of 14,187 children and adolescents who had at least 3 well-child visits at an outpatient academic medical center, 507 patients met the criteria for hypertension, yet only 131 (26%) had this diagnosis documented in their electronic health record.5
In a survey of 89 pediatricians, >50% of respondents said they were not familiar with the most current published recommendations for diagnosing and treating pediatric hypertension.6 Respondents also indicated that the most common reason for not initiating pharmacotherapy for children with hypertension was a lack of familiarity with appropriate antihypertensive agents (54%), followed by concern for adverse medication effects. Delayed diagnosis, evaluation, and treatment of hypertension in young patients can increase the likelihood of serious consequences, including target-organ damage such as left ventricular hypertrophy (LVH). In this review, we’ll describe the factors that put children and adolescents at risk for hypertension, and offer an evidence-based approach to diagnosis and treatment.
Obesity is a key risk factor
An estimated 17% of children aged 2 to 19 are obese.7 Obesity increases a child’s risk for hypertension by approximately 3- to 5-fold, and body mass index (BMI) is greater in children with primary hypertension compared with those with secondary hypertension.8 Hypertension is more common among Hispanic and non-Hispanic black male children and adolescents compared with their white counterparts; these ethnic disparities are not found in females.9,10 Poor diets and physical inactivity further contribute to obesity and hypertension risk. Children who were born preterm or had a very low birth weight also are at increased risk.11
Unchecked hypertension can lead to cardiac, vascular damage
Some children and adolescents with undiagnosed and untreated hypertension have evidence of target-organ damage, including cardiac dysfunction and pathologic vascular abnormalities. LVH is present in 20% to 41% of children and adolescents with hypertension.12,13 Carotid intima-media thickness, an established surrogate marker for atherosclerosis, is abnormally increased in children with hypertension, even after adjusting for BMI.14 Other target organ effects include impaired cognitive function, reduced glomerular filtration rate, microalbuminuria, and retinal arteriolar narrowing.15-17
Pediatric hypertension may persist into adulthood. A meta-analysis of more than 50 studies found that elevated blood pressure (BP) in childhood increases the risk for hypertension as an adult.18
NHLBI recommendations call for a BP check at every visit
The National Heart, Lung, and Blood Institute (NHLBI) Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (“the 4th Report”) recommends measuring BP in all children over age 3 during every health care visit.12 Children under age 3 should have their BP checked in certain circumstances, including preterm delivery, congenital heart disease, recurrent urinary tract infections, renal/urologic disease, organ transplantation, malignancy, and systemic illnesses associated with hypertension.12 The 4th Report is endorsed by the American Academy of Pediatrics (AAP); however, the American Academy of Family Physicians and the US Preventive Services Task Force have concluded that the evidence is insufficient to recommend for or against routine screening for hypertension in children and adolescents to reduce the risk of cardiovascular disease (CVD).19,20
Does the child have hypertension? That depends on several factors
Determining whether a child has hypertension requires that you consult national BP standards to determine if he or she is within the normal range. Normal BP standards for children and adolescents are based on gender, age, and height percentile, and provide a precise classification based on body size.12 These tables are available from the NHLBI Web site at http://www.nhlbi.nih.gov/guidelines/hypertension/child_tbl.htm. Height percentiles in these tables correspond with the Centers for Disease Control and Prevention (CDC) growth charts published in 2000.21 The Baylor College of Medicine Children’s Nutrition Research Center has a web-based calculator to help physicians determine BP percentiles in children and adolescents; it is available at http://www.bcm.edu/bodycomplab/Flashapps/BPVAgeChartpage.html. The International Pediatric Hypertension Association also offers BP charts and calculators at http://www.iphapediatrichypertension.org.
The diagnostic parameters for pediatric hypertension are listed in TABLE 1.12 The higher systolic or diastolic BP percentile value is used to determine a child’s overall BP category. A child is considered normotensive if the BP is <90th percentile. Hypertension is an average systolic or diastolic BP that is ≥95th percentile on at least 3 separate occasions. Stage 1 hypertension is BP levels ranging from the 95th percentile to 5 mm Hg above the 99th percentile, and stage 2 hypertension is BP levels greater than 5 mm Hg above the 99th percentile.
For example, assume you are evaluating a 12-year-old boy who is 61 inches tall and has a BP of 129/87 mm Hg. According to the CDC growth charts, his height puts him in the 75th percentile for his age. Using the NHLBI chart, you determine that he falls in the 95th-99th percentile for BP, and thus, using the categories in TABLE 1, is given a diagnosis of Stage 1 hypertension.
Accurate BP measurement requires using an appropriate cuff size that covers 80% of the child’s upper arm. When the child is between cuff sizes, use the larger cuff because small cuffs overestimate BP readings. BP readings should be taken on the right arm with the arm supported at heart level after the child has been sitting quietly for at least 5 minutes.12 One study showed that the initial BP readings taken in the triage area were significantly higher—often by >10 mm Hg—compared with follow-up measurements in the examination room.22
The preferred method of BP measurement is auscultation; however, oscillometric devices also are acceptable. These devices are easier to use, help eliminate digit bias, and minimize observer variation, but they typically read approximately 6 to 9 mm Hg higher than auscultation.23 For any BP measurement obtained by oscillometry that is >90th percentile, repeat the measurement by auscultation at least twice during the same office visit, and use an average of the repeated measurements.12 Obtain measurements of a lower extremity when you suspect congenital heart disease (eg, aortic coarctation). For any patient in whom you confirm a BP measurement >95th percentile, repeat the measurement within 2 weeks; for BPs >99th percentile, reevaluation should occur within one week.
Ambulatory BP monitoring (ABPM). Because BP measurements have a circadian pattern (higher during the day and reduced by 10% during sleep24) an ABPM device that provides 50 to 60 readings over 24 hours can be useful when evaluating children and adolescents for white-coat hypertension (elevated clinic BP with normal ambulatory BP), masked hypertension (normal clinic BP with elevated ambulatory BP), prehypertension and secondary hypertension (BP generally does not follow circadian patterns).25 ABPM is more accurate than BP self-measurement, but usually is limited to children older than age 5
Steps to take for clinical evaluation
Start by conducting a thorough history and physical examination, looking for information that can help you select the most appropriate tests for the next phase of evaluation.8,12 Calculate the patient’s BMI to screen for obesity, ask about a family history of hypertension or CVD, and determine if the patient is taking any medications that might cause hypertension, such as amphetamines, corticosteroids, or cyclosporine.8 Assess for signs and symptoms that suggest an underlying disease, such as renal disease (hematuria, edema, fatigue) or heart disease (chest pain, exertional dyspnea, palpitations).12
All children diagnosed with hypertension should be screened for secondary causes (TABLE 2). The recommended evaluation is to obtain a renal function panel, electrolytes, urinalysis, urine culture, complete blood count, renovascular imaging, and echocardiogram.12 The most common etiologies for secondary hypertension are renal parenchymal disease (68%), renovascular abnormalities (10%), and endocrinopathies (10%).26 Other causes, such as aortic coarctation, obstructive sleep apnea, iatrogenic factors (eg, toxins, medications, drugs of abuse), and genitourinary abnormalities, account for only a small percentage of cases and should be investigated as clinically indicated.26
Renovascular assessment depends on facility expertise. Imaging options include renal ultrasound (with or without Doppler), computed tomography angiography, renal flow scan, and magnetic resonance angiography. These studies have similar sensitivities and specificities.27 For patients in whom you strongly suspect renovascular disease, renal arteriography (digital subtraction angiography) provides the best images, although it is the most invasive study.27
Refer children and adolescents who are found to have significant abnormalities during the initial evaluation to the appropriate specialist. BP measurements often improve when secondary causes are treated.
Which drugs for which patients?
Pharmacologic management is indicated for pediatric patients with stage 1 or stage 2 hypertension, secondary hypertension, and those with evidence of target-organ damage.12 The goal of therapy is to reduce BP to <95th percentile. In patients with target organ damage, renal disease, or diabetes mellitus, the goal is <90th percentile.12,15,28 Intensive management of BP (≤50th percentile) in children with chronic kidney disease has been shown to delay progression to renal failure,29 but it is uncertain if lower BP goals can slow or prevent additional subclinical target organ damage.
Pharmacotherapy for hypertensive children or adolescents can be challenging because recommendations of which medication to use are based upon expert opinion and extrapolation from randomized trials of adults. The length of therapy (often lifelong), potential adverse effects, and unproven direct mortality benefit complicate this decision. Medication choice usually is based on physician preference or experience.12 The most common antihypertensive drugs prescribed are angiotensin-converting enzyme (ACE) inhibitors (26%), followed by diuretics (20%), and beta-blockers (17%).30,31 The starting doses and other details of medications commonly used to treat pediatric hypertension are listed in TABLE 3.28,32-34
One approach to choosing an antihypertensive drug for children is to measure the patient’s ambulatory plasma renin activity (PRA) level before initiating therapy. Those with high PRA levels (>0.65 ng/mL/h), presumably due to peripheral vasoconstriction, may benefit more from ACE inhibitors, angiotensin receptor blockers (ARBs), or beta-adrenergic antagonists.35 Individuals with low PRA levels (<0.65 ng/mL/h) maintain higher volume/sodium excess and may benefit more from diuretics or calcium channel blockers.35
Ethnicity also may guide medication selection. African American adults do not respond well to ACE inhibitor monotherapy due to decreased PRA and increased salt hypersensitivity.36 One meta-analysis found that African American children and adolescents had inadequate BP response to 6 individual ACE inhibitors, even at higher doses compared with white children and those of other ethnicities, who showed significant improvement in BP.37 ARBs may be a more effective alternative for this population.
Most experts recommend initiating a single agent at a low dose.12 A systematic review found that except for African American children, pediatric patients experienced comparable reductions in BP with ACE inhibitors (10.7/8.1 mm Hg), ARBs (10.5/6.9 mm Hg), and calcium channel blockers (9.3/7.2 mm Hg).38 In addition, ACE inhibitors and ARBs significantly reduced proteinuria by 49% and 59%, respectively.38
Schedule follow-up visits for 2 to 4 weeks (or sooner for patients with stage 2 hypertension) after initiating pharmacotherapy. If BP response is suboptimal, consider increasing the dose before adding a second agent. If the patient experiences significant adverse effects or has an inadequate BP response, changing to a drug from a different class is recommended.39 Patients who do not adequately respond to these approaches may require combination therapy; in such cases, strongly consider consultation with pediatric nephrologist or cardiologist.39 Medication compliance should be verified (eg, by pill counting, parental supervision) in patients who do not respond to therapy. Once BP control has been achieved, visits every 3 to 4 months are appropriate, with periodic laboratory monitoring, especially for children taking diuretics, ACE inhibitors, or ARBs or who have underlying renal disease.
Recommend exercise, but carefully monitor athlete's BP
Encourage obese and overweight children and adolescents to lose weight to maintain a BMI <95th percentile. Current guidelines based on expert opinion recommend that children and adolescents should engage in 60 minutes of daily physical activity.12 A meta-analysis found physical activity led to a 1% and 3% reduction in systolic and diastolic BP, respectively, although these results were not statistically significant.40
Be aware, however, that children and adolescents with hypertension who engage in certain competitive sports can significantly increase their BP and may be at risk for complications.41 According to the AAP guidelines, patients with stage 2 hypertension should not engage in high-static sports (eg, gymnastics, weightlifting, wrestling, boxing, cycling, decathlon, triathlon) until BP is well controlled.41 Patients with target-organ damage, uncontrolled hypertension, or symptomatic hypertension should not participate until BP is well controlled. Patients with prehypertension and stage 1 hypertension without target-organ damage are eligible to participate in competitive athletics. Reassess BP every 6 months in patients who are prehypertensive and every one to 2 weeks for those with stage 1 hypertension. When the patient’s BP remains <90th percentile, routine surveillance every 3 to 6 months is recommended.
What about sodium? Encourage parents of pediatric patients with hypertension to limit their child’s salt intake to 1.2 g/d for those age 4 to 8 and 1.5 g/d for older children.42 A meta-analysis found salt reduction decreased systolic BP by 1.2 mm Hg and diastolic BP by 1.3 mm Hg.43 Though these benefits are small, reducing sodium intake can be one of several lifestyle modifications, such as increased activity and quitting smoking, that can reduce young patients’ risk of hypertension and related cardiovascular sequelae.
CORRESPONDENCE
Robert Gauer, MD, Womack Army Medical Center, 2817 Reilly Road, Fort Bragg NC 28310; [email protected]
› Screen for hypertension in all children over the age of 3 at every visit. C
› Order laboratory evaluation, echocardiography, and renovascular imaging for all children given a diagnosis of hypertension. C
› Advise parents that children with prehypertension and stage 1 hypertension without target-organ damage are eligible to participate in competitive athletics, but those with stage 2 hypertension, target-organ damage, or symptomatic hypertension should not engage in high-static sports (eg, gymnastics, weightlifting, wrestling) until BP is well controlled. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Childhood hypertension is on the rise: Recent data from the National Health and Nutrition Survey suggest 10% of children and adolescents have prehypertension and 4% have hypertension.1-4 Unfortunately, the condition often is missed. In a study of 14,187 children and adolescents who had at least 3 well-child visits at an outpatient academic medical center, 507 patients met the criteria for hypertension, yet only 131 (26%) had this diagnosis documented in their electronic health record.5
In a survey of 89 pediatricians, >50% of respondents said they were not familiar with the most current published recommendations for diagnosing and treating pediatric hypertension.6 Respondents also indicated that the most common reason for not initiating pharmacotherapy for children with hypertension was a lack of familiarity with appropriate antihypertensive agents (54%), followed by concern for adverse medication effects. Delayed diagnosis, evaluation, and treatment of hypertension in young patients can increase the likelihood of serious consequences, including target-organ damage such as left ventricular hypertrophy (LVH). In this review, we’ll describe the factors that put children and adolescents at risk for hypertension, and offer an evidence-based approach to diagnosis and treatment.
Obesity is a key risk factor
An estimated 17% of children aged 2 to 19 are obese.7 Obesity increases a child’s risk for hypertension by approximately 3- to 5-fold, and body mass index (BMI) is greater in children with primary hypertension compared with those with secondary hypertension.8 Hypertension is more common among Hispanic and non-Hispanic black male children and adolescents compared with their white counterparts; these ethnic disparities are not found in females.9,10 Poor diets and physical inactivity further contribute to obesity and hypertension risk. Children who were born preterm or had a very low birth weight also are at increased risk.11
Unchecked hypertension can lead to cardiac, vascular damage
Some children and adolescents with undiagnosed and untreated hypertension have evidence of target-organ damage, including cardiac dysfunction and pathologic vascular abnormalities. LVH is present in 20% to 41% of children and adolescents with hypertension.12,13 Carotid intima-media thickness, an established surrogate marker for atherosclerosis, is abnormally increased in children with hypertension, even after adjusting for BMI.14 Other target organ effects include impaired cognitive function, reduced glomerular filtration rate, microalbuminuria, and retinal arteriolar narrowing.15-17
Pediatric hypertension may persist into adulthood. A meta-analysis of more than 50 studies found that elevated blood pressure (BP) in childhood increases the risk for hypertension as an adult.18
NHLBI recommendations call for a BP check at every visit
The National Heart, Lung, and Blood Institute (NHLBI) Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (“the 4th Report”) recommends measuring BP in all children over age 3 during every health care visit.12 Children under age 3 should have their BP checked in certain circumstances, including preterm delivery, congenital heart disease, recurrent urinary tract infections, renal/urologic disease, organ transplantation, malignancy, and systemic illnesses associated with hypertension.12 The 4th Report is endorsed by the American Academy of Pediatrics (AAP); however, the American Academy of Family Physicians and the US Preventive Services Task Force have concluded that the evidence is insufficient to recommend for or against routine screening for hypertension in children and adolescents to reduce the risk of cardiovascular disease (CVD).19,20
Does the child have hypertension? That depends on several factors
Determining whether a child has hypertension requires that you consult national BP standards to determine if he or she is within the normal range. Normal BP standards for children and adolescents are based on gender, age, and height percentile, and provide a precise classification based on body size.12 These tables are available from the NHLBI Web site at http://www.nhlbi.nih.gov/guidelines/hypertension/child_tbl.htm. Height percentiles in these tables correspond with the Centers for Disease Control and Prevention (CDC) growth charts published in 2000.21 The Baylor College of Medicine Children’s Nutrition Research Center has a web-based calculator to help physicians determine BP percentiles in children and adolescents; it is available at http://www.bcm.edu/bodycomplab/Flashapps/BPVAgeChartpage.html. The International Pediatric Hypertension Association also offers BP charts and calculators at http://www.iphapediatrichypertension.org.
The diagnostic parameters for pediatric hypertension are listed in TABLE 1.12 The higher systolic or diastolic BP percentile value is used to determine a child’s overall BP category. A child is considered normotensive if the BP is <90th percentile. Hypertension is an average systolic or diastolic BP that is ≥95th percentile on at least 3 separate occasions. Stage 1 hypertension is BP levels ranging from the 95th percentile to 5 mm Hg above the 99th percentile, and stage 2 hypertension is BP levels greater than 5 mm Hg above the 99th percentile.
For example, assume you are evaluating a 12-year-old boy who is 61 inches tall and has a BP of 129/87 mm Hg. According to the CDC growth charts, his height puts him in the 75th percentile for his age. Using the NHLBI chart, you determine that he falls in the 95th-99th percentile for BP, and thus, using the categories in TABLE 1, is given a diagnosis of Stage 1 hypertension.
Accurate BP measurement requires using an appropriate cuff size that covers 80% of the child’s upper arm. When the child is between cuff sizes, use the larger cuff because small cuffs overestimate BP readings. BP readings should be taken on the right arm with the arm supported at heart level after the child has been sitting quietly for at least 5 minutes.12 One study showed that the initial BP readings taken in the triage area were significantly higher—often by >10 mm Hg—compared with follow-up measurements in the examination room.22
The preferred method of BP measurement is auscultation; however, oscillometric devices also are acceptable. These devices are easier to use, help eliminate digit bias, and minimize observer variation, but they typically read approximately 6 to 9 mm Hg higher than auscultation.23 For any BP measurement obtained by oscillometry that is >90th percentile, repeat the measurement by auscultation at least twice during the same office visit, and use an average of the repeated measurements.12 Obtain measurements of a lower extremity when you suspect congenital heart disease (eg, aortic coarctation). For any patient in whom you confirm a BP measurement >95th percentile, repeat the measurement within 2 weeks; for BPs >99th percentile, reevaluation should occur within one week.
Ambulatory BP monitoring (ABPM). Because BP measurements have a circadian pattern (higher during the day and reduced by 10% during sleep24) an ABPM device that provides 50 to 60 readings over 24 hours can be useful when evaluating children and adolescents for white-coat hypertension (elevated clinic BP with normal ambulatory BP), masked hypertension (normal clinic BP with elevated ambulatory BP), prehypertension and secondary hypertension (BP generally does not follow circadian patterns).25 ABPM is more accurate than BP self-measurement, but usually is limited to children older than age 5
Steps to take for clinical evaluation
Start by conducting a thorough history and physical examination, looking for information that can help you select the most appropriate tests for the next phase of evaluation.8,12 Calculate the patient’s BMI to screen for obesity, ask about a family history of hypertension or CVD, and determine if the patient is taking any medications that might cause hypertension, such as amphetamines, corticosteroids, or cyclosporine.8 Assess for signs and symptoms that suggest an underlying disease, such as renal disease (hematuria, edema, fatigue) or heart disease (chest pain, exertional dyspnea, palpitations).12
All children diagnosed with hypertension should be screened for secondary causes (TABLE 2). The recommended evaluation is to obtain a renal function panel, electrolytes, urinalysis, urine culture, complete blood count, renovascular imaging, and echocardiogram.12 The most common etiologies for secondary hypertension are renal parenchymal disease (68%), renovascular abnormalities (10%), and endocrinopathies (10%).26 Other causes, such as aortic coarctation, obstructive sleep apnea, iatrogenic factors (eg, toxins, medications, drugs of abuse), and genitourinary abnormalities, account for only a small percentage of cases and should be investigated as clinically indicated.26
Renovascular assessment depends on facility expertise. Imaging options include renal ultrasound (with or without Doppler), computed tomography angiography, renal flow scan, and magnetic resonance angiography. These studies have similar sensitivities and specificities.27 For patients in whom you strongly suspect renovascular disease, renal arteriography (digital subtraction angiography) provides the best images, although it is the most invasive study.27
Refer children and adolescents who are found to have significant abnormalities during the initial evaluation to the appropriate specialist. BP measurements often improve when secondary causes are treated.
Which drugs for which patients?
Pharmacologic management is indicated for pediatric patients with stage 1 or stage 2 hypertension, secondary hypertension, and those with evidence of target-organ damage.12 The goal of therapy is to reduce BP to <95th percentile. In patients with target organ damage, renal disease, or diabetes mellitus, the goal is <90th percentile.12,15,28 Intensive management of BP (≤50th percentile) in children with chronic kidney disease has been shown to delay progression to renal failure,29 but it is uncertain if lower BP goals can slow or prevent additional subclinical target organ damage.
Pharmacotherapy for hypertensive children or adolescents can be challenging because recommendations of which medication to use are based upon expert opinion and extrapolation from randomized trials of adults. The length of therapy (often lifelong), potential adverse effects, and unproven direct mortality benefit complicate this decision. Medication choice usually is based on physician preference or experience.12 The most common antihypertensive drugs prescribed are angiotensin-converting enzyme (ACE) inhibitors (26%), followed by diuretics (20%), and beta-blockers (17%).30,31 The starting doses and other details of medications commonly used to treat pediatric hypertension are listed in TABLE 3.28,32-34
One approach to choosing an antihypertensive drug for children is to measure the patient’s ambulatory plasma renin activity (PRA) level before initiating therapy. Those with high PRA levels (>0.65 ng/mL/h), presumably due to peripheral vasoconstriction, may benefit more from ACE inhibitors, angiotensin receptor blockers (ARBs), or beta-adrenergic antagonists.35 Individuals with low PRA levels (<0.65 ng/mL/h) maintain higher volume/sodium excess and may benefit more from diuretics or calcium channel blockers.35
Ethnicity also may guide medication selection. African American adults do not respond well to ACE inhibitor monotherapy due to decreased PRA and increased salt hypersensitivity.36 One meta-analysis found that African American children and adolescents had inadequate BP response to 6 individual ACE inhibitors, even at higher doses compared with white children and those of other ethnicities, who showed significant improvement in BP.37 ARBs may be a more effective alternative for this population.
Most experts recommend initiating a single agent at a low dose.12 A systematic review found that except for African American children, pediatric patients experienced comparable reductions in BP with ACE inhibitors (10.7/8.1 mm Hg), ARBs (10.5/6.9 mm Hg), and calcium channel blockers (9.3/7.2 mm Hg).38 In addition, ACE inhibitors and ARBs significantly reduced proteinuria by 49% and 59%, respectively.38
Schedule follow-up visits for 2 to 4 weeks (or sooner for patients with stage 2 hypertension) after initiating pharmacotherapy. If BP response is suboptimal, consider increasing the dose before adding a second agent. If the patient experiences significant adverse effects or has an inadequate BP response, changing to a drug from a different class is recommended.39 Patients who do not adequately respond to these approaches may require combination therapy; in such cases, strongly consider consultation with pediatric nephrologist or cardiologist.39 Medication compliance should be verified (eg, by pill counting, parental supervision) in patients who do not respond to therapy. Once BP control has been achieved, visits every 3 to 4 months are appropriate, with periodic laboratory monitoring, especially for children taking diuretics, ACE inhibitors, or ARBs or who have underlying renal disease.
Recommend exercise, but carefully monitor athlete's BP
Encourage obese and overweight children and adolescents to lose weight to maintain a BMI <95th percentile. Current guidelines based on expert opinion recommend that children and adolescents should engage in 60 minutes of daily physical activity.12 A meta-analysis found physical activity led to a 1% and 3% reduction in systolic and diastolic BP, respectively, although these results were not statistically significant.40
Be aware, however, that children and adolescents with hypertension who engage in certain competitive sports can significantly increase their BP and may be at risk for complications.41 According to the AAP guidelines, patients with stage 2 hypertension should not engage in high-static sports (eg, gymnastics, weightlifting, wrestling, boxing, cycling, decathlon, triathlon) until BP is well controlled.41 Patients with target-organ damage, uncontrolled hypertension, or symptomatic hypertension should not participate until BP is well controlled. Patients with prehypertension and stage 1 hypertension without target-organ damage are eligible to participate in competitive athletics. Reassess BP every 6 months in patients who are prehypertensive and every one to 2 weeks for those with stage 1 hypertension. When the patient’s BP remains <90th percentile, routine surveillance every 3 to 6 months is recommended.
What about sodium? Encourage parents of pediatric patients with hypertension to limit their child’s salt intake to 1.2 g/d for those age 4 to 8 and 1.5 g/d for older children.42 A meta-analysis found salt reduction decreased systolic BP by 1.2 mm Hg and diastolic BP by 1.3 mm Hg.43 Though these benefits are small, reducing sodium intake can be one of several lifestyle modifications, such as increased activity and quitting smoking, that can reduce young patients’ risk of hypertension and related cardiovascular sequelae.
CORRESPONDENCE
Robert Gauer, MD, Womack Army Medical Center, 2817 Reilly Road, Fort Bragg NC 28310; [email protected]
1. McNiece KL, Poffenbarger TS, Tuner JL, et al. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr. 2007;150:640-644.e1.
2. Moore WE, Eichner JE, Cohn EM, et al. Blood pressure screening of school children in a multiracial school district: the Healthy Kids Project. Am J Hypertens. 2009;22:351-356.
3. Falkner B. What exactly do the trends mean? Circulation. 2007;116:1437-1439.
4. Feber J, Ahmed M. Hypertension in children: new trends and challenges. Clin Sci (Lond). 2010;119:151-161.
5. Hansen ML, Gunn PW, Kaelber DC. Under diagnosis of hypertension in children and adolescents. JAMA. 2007;298:874-879.
6. Boneparth A, Flynn JT. Evaluation and treatment of hypertension in general pediatric practice. Clin Pediatr (Phila). 2009;48:44-49.
7. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483-490.
8. Feld LG, Corey H. Hypertension in childhood. Pediatr Rev. 2007;28:283-298.
9. Rosner B, Cook N, Portman R, et al. Blood pressure differences by ethnic group among United States children and adolescents. Hypertension. 2009;54:502-508.
10. Din-Dzietham R, Liu Y, Bielo MV, et al. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488-1496.
11. de Jong F, Monuteaux MC, van Elburg RM, et al. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension. 2012;59:226-234.
12. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 suppl 4th report):555-576.
13. Ramaswamy P, Lytrivi ID, Paul C, et al. Regression of left ventricular hypertrophy in children with antihypertensive therapy. Pediatr Nephrol. 2007;22:141-143.
14. Lande MB, Carson NL, Roy J, et al. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40-44.
15. Flynn JT. Pediatric hypertension update. Curr Opin Nephrol Hypertens. 2010;19:292-297.
16. Mitchell P, Cheung N, de Haseth K, et al. Blood pressure and retinal arteriolar narrowing in children. Hypertension. 2007;49:1156-1162.
17. Kupferman JC, Lande MB, Adams HR, et al. Primary hypertension and neurocognitive and executive functioning in school-age children. Pediatr Nephrol. 2013;28:401-408.
18. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review of meta-regression analysis. Circulation. 2008;117:3171-3180.
19. Hypertension. American Academy of Family Physicians Web site. Available at: http://www.aafp.org/patient-care/clinical-recommendations/all/hypertension.html. Accessed February 7, 2014.
20. Screening for high blood pressure: reaffirmation recommendation statement. December 2007. AHRQ publication 08-05105-EF-2. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf07/hbp/hbprs.htm. Accessed October 10, 2012.
21. Growth Charts. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/growthcharts. Accessed July 31, 2012.
22. Podoll A, Grenier M, Croix B, et al. Inaccuracy in pediatric outpatient blood pressure measurement. Pediatrics. 2007;119:e538-e543.
23. Flynn JT, Pierce CB, Miller ER 3rd, et al; Chronic Kidney Disease in Children Study Group. Reliability of resting blood pressure measurement and classification using an oscillometric device in children with chronic kidney disease. J Pediatr. 2012;160:434-440.e.1.
24. Villar VA, Liu T, Jose PA. Recent trends in pediatric hypertension research. J Med Liban. 2010;58:179-184.
25. Swartz SJ, Srivaths PR, Croix B, et al. Cost-effectiveness of ambulatory blood pressure monitoring in the initial evaluation of hypertension in children. Pediatrics. 2008;122:1177-1181.
26. Brady TM, Feld LG. Pediatric approach to hypertension. Semin Nephrol. 2009;29:379-388.
27. Tullus K, Roebuck DJ, McLaren CA, et al. Imaging in the evaluation of renovascular disease. Pediatr Nephrol. 2010;25:1049-1056.
28. Flynn JT. Management of hypertension in the young: role of antihypertensive medications. J Cardiovasc Pharmacol. 2011;58:111-120.
29. ESCAPE Trial Group; Wühl E, Trivelli A, Picca S, et al. Strict blood pressure control and progression of renal failure in children. N Engl J Med. 2009;361:1639-1650.
30. Yoon EY, Cohn L, Rocchini A, et al. Antihypertensive prescribing patterns for adolescents with primary hypertension. Pediatrics. 2012;129:e1-e8.
31. Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. J Clin Hypertens (Greenwich). 2012;14:383-387.
32. Welch WP, Yang W, Taylor-Zapata P, et al. Antihypertensive drug use by children: are the drugs labeled and indicated? J Clin Hypertens. 2012;14:388-395.
33. Lexicomp Pharmaceutical Reference, Version 1.8.3(155). Lexi-Comp Web site. Available at: http://online.lexi.com/crlsql/servlet/crlonline. Accessed July 31, 2012.
34. Robinson RF, Nahata MC, Batisky DL, et al. Pharmacologic treatment of chronic pediatric hypertension. Pediatr Drugs. 2005;7:27-40.
35. Hanevold CD. Concepts guiding therapy for hypertension in children. Expert Rev Cardiovasc Ther. 2009;7:647-657.
36. Brewster LM, van Montfrans GA, Kleijnen J. Systematic review: antihypertensive drug therapy in black patients. Ann Intern Med. 2004;141:614-627.
37. Li JS, Baker-Smith CM, Smith PB, et al. Racial differences in blood pressure response to angiotensin-converting enzyme inhibitors in children a meta-analysis. Clin Pharmacol Ther. 2008;84:315-319.
38. Simonetti GD, Rizzi M, Donadini R, et al. Effects of antihypertensive drugs on blood pressure and proteinuria in childhood. J Hypertens. 2007;25:2370-2376.
39. Lurbe E, Álvarez J, Redon J. Diagnosis and treatment of hypertension in children. Curr Hypertens Rep. 2010;12:480-486.
40. Kelley GA, Kelley KS, Tran ZV. The effects of exercise on resting blood pressure in children and adolescents: a meta-analysis of randomized controlled trials. Prev Cardiol. 2003;6:8-16.
41. McCambridge TM, Benjamin HJ, Breener JS, et al; Council on Sports Medicine and Fitness. Athletic participation by children and adolescents who have systemic hypertension. Pediatrics. 2010;125:1287-1294.
42. 2008 Physical Activity Guidelines for Americans. US Department of Health and Human Services Web site. Available at: http://www.health.gov/PAguidelines/guidelines/default.aspx. Updated March 11, 2013. Accessed February 7, 2014.
43. He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: Meta-analysis of controlled trials. Hypertension. 2006;48:861-869.
1. McNiece KL, Poffenbarger TS, Tuner JL, et al. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr. 2007;150:640-644.e1.
2. Moore WE, Eichner JE, Cohn EM, et al. Blood pressure screening of school children in a multiracial school district: the Healthy Kids Project. Am J Hypertens. 2009;22:351-356.
3. Falkner B. What exactly do the trends mean? Circulation. 2007;116:1437-1439.
4. Feber J, Ahmed M. Hypertension in children: new trends and challenges. Clin Sci (Lond). 2010;119:151-161.
5. Hansen ML, Gunn PW, Kaelber DC. Under diagnosis of hypertension in children and adolescents. JAMA. 2007;298:874-879.
6. Boneparth A, Flynn JT. Evaluation and treatment of hypertension in general pediatric practice. Clin Pediatr (Phila). 2009;48:44-49.
7. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483-490.
8. Feld LG, Corey H. Hypertension in childhood. Pediatr Rev. 2007;28:283-298.
9. Rosner B, Cook N, Portman R, et al. Blood pressure differences by ethnic group among United States children and adolescents. Hypertension. 2009;54:502-508.
10. Din-Dzietham R, Liu Y, Bielo MV, et al. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488-1496.
11. de Jong F, Monuteaux MC, van Elburg RM, et al. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension. 2012;59:226-234.
12. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 suppl 4th report):555-576.
13. Ramaswamy P, Lytrivi ID, Paul C, et al. Regression of left ventricular hypertrophy in children with antihypertensive therapy. Pediatr Nephrol. 2007;22:141-143.
14. Lande MB, Carson NL, Roy J, et al. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40-44.
15. Flynn JT. Pediatric hypertension update. Curr Opin Nephrol Hypertens. 2010;19:292-297.
16. Mitchell P, Cheung N, de Haseth K, et al. Blood pressure and retinal arteriolar narrowing in children. Hypertension. 2007;49:1156-1162.
17. Kupferman JC, Lande MB, Adams HR, et al. Primary hypertension and neurocognitive and executive functioning in school-age children. Pediatr Nephrol. 2013;28:401-408.
18. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review of meta-regression analysis. Circulation. 2008;117:3171-3180.
19. Hypertension. American Academy of Family Physicians Web site. Available at: http://www.aafp.org/patient-care/clinical-recommendations/all/hypertension.html. Accessed February 7, 2014.
20. Screening for high blood pressure: reaffirmation recommendation statement. December 2007. AHRQ publication 08-05105-EF-2. US Preventive Services Task Force Web site. Available at: http://www.uspreventiveservicestaskforce.org/uspstf07/hbp/hbprs.htm. Accessed October 10, 2012.
21. Growth Charts. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/growthcharts. Accessed July 31, 2012.
22. Podoll A, Grenier M, Croix B, et al. Inaccuracy in pediatric outpatient blood pressure measurement. Pediatrics. 2007;119:e538-e543.
23. Flynn JT, Pierce CB, Miller ER 3rd, et al; Chronic Kidney Disease in Children Study Group. Reliability of resting blood pressure measurement and classification using an oscillometric device in children with chronic kidney disease. J Pediatr. 2012;160:434-440.e.1.
24. Villar VA, Liu T, Jose PA. Recent trends in pediatric hypertension research. J Med Liban. 2010;58:179-184.
25. Swartz SJ, Srivaths PR, Croix B, et al. Cost-effectiveness of ambulatory blood pressure monitoring in the initial evaluation of hypertension in children. Pediatrics. 2008;122:1177-1181.
26. Brady TM, Feld LG. Pediatric approach to hypertension. Semin Nephrol. 2009;29:379-388.
27. Tullus K, Roebuck DJ, McLaren CA, et al. Imaging in the evaluation of renovascular disease. Pediatr Nephrol. 2010;25:1049-1056.
28. Flynn JT. Management of hypertension in the young: role of antihypertensive medications. J Cardiovasc Pharmacol. 2011;58:111-120.
29. ESCAPE Trial Group; Wühl E, Trivelli A, Picca S, et al. Strict blood pressure control and progression of renal failure in children. N Engl J Med. 2009;361:1639-1650.
30. Yoon EY, Cohn L, Rocchini A, et al. Antihypertensive prescribing patterns for adolescents with primary hypertension. Pediatrics. 2012;129:e1-e8.
31. Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. J Clin Hypertens (Greenwich). 2012;14:383-387.
32. Welch WP, Yang W, Taylor-Zapata P, et al. Antihypertensive drug use by children: are the drugs labeled and indicated? J Clin Hypertens. 2012;14:388-395.
33. Lexicomp Pharmaceutical Reference, Version 1.8.3(155). Lexi-Comp Web site. Available at: http://online.lexi.com/crlsql/servlet/crlonline. Accessed July 31, 2012.
34. Robinson RF, Nahata MC, Batisky DL, et al. Pharmacologic treatment of chronic pediatric hypertension. Pediatr Drugs. 2005;7:27-40.
35. Hanevold CD. Concepts guiding therapy for hypertension in children. Expert Rev Cardiovasc Ther. 2009;7:647-657.
36. Brewster LM, van Montfrans GA, Kleijnen J. Systematic review: antihypertensive drug therapy in black patients. Ann Intern Med. 2004;141:614-627.
37. Li JS, Baker-Smith CM, Smith PB, et al. Racial differences in blood pressure response to angiotensin-converting enzyme inhibitors in children a meta-analysis. Clin Pharmacol Ther. 2008;84:315-319.
38. Simonetti GD, Rizzi M, Donadini R, et al. Effects of antihypertensive drugs on blood pressure and proteinuria in childhood. J Hypertens. 2007;25:2370-2376.
39. Lurbe E, Álvarez J, Redon J. Diagnosis and treatment of hypertension in children. Curr Hypertens Rep. 2010;12:480-486.
40. Kelley GA, Kelley KS, Tran ZV. The effects of exercise on resting blood pressure in children and adolescents: a meta-analysis of randomized controlled trials. Prev Cardiol. 2003;6:8-16.
41. McCambridge TM, Benjamin HJ, Breener JS, et al; Council on Sports Medicine and Fitness. Athletic participation by children and adolescents who have systemic hypertension. Pediatrics. 2010;125:1287-1294.
42. 2008 Physical Activity Guidelines for Americans. US Department of Health and Human Services Web site. Available at: http://www.health.gov/PAguidelines/guidelines/default.aspx. Updated March 11, 2013. Accessed February 7, 2014.
43. He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: Meta-analysis of controlled trials. Hypertension. 2006;48:861-869.