User login
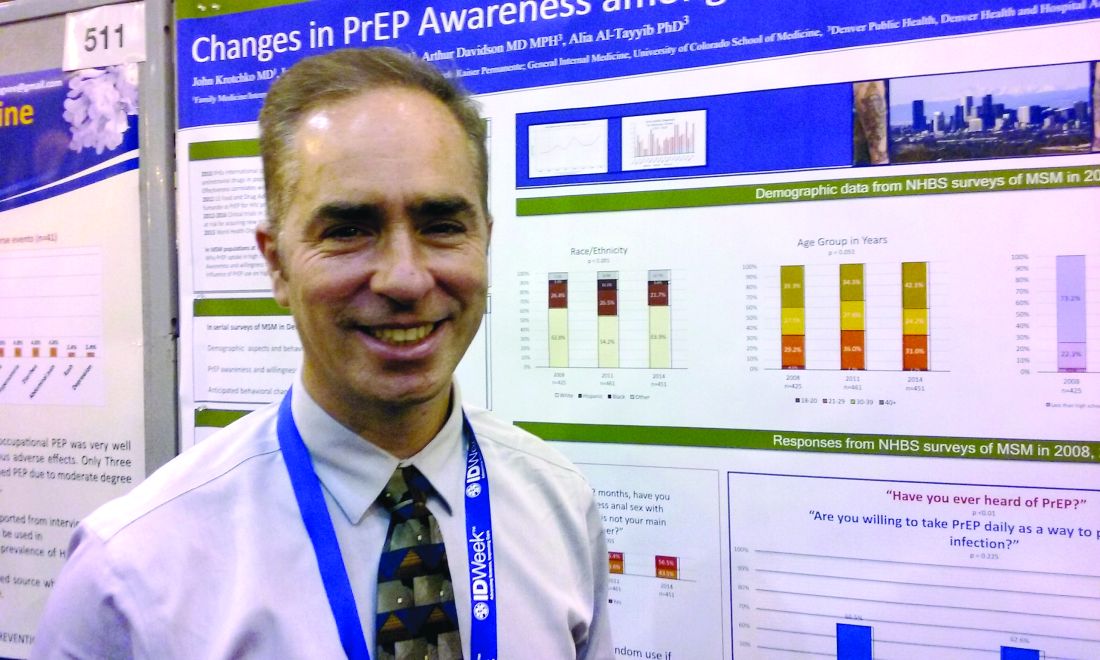
NEW ORLEANS – Awareness about preexposure prophylaxis (PrEP) is steadily increasing among men who have sex with men at high risk for HIV infection, but that increased knowledge did not translate into greater willingness to take the daily pill nor did it increase engagement in high-risk behaviors.
Using questions from the National HIV Behavioral Surveillance System (NHBS), investigators surveyed men who have sex with men in urban settings in 3-year cycles. Awareness about HIV PrEP, once-daily emtricitabine/tenofovir (Truvada) increased from 21% in 2008 to 28% in 2011 to 46% in 2014.
The increase from 2011 to 2014 was statistically significant (P less than .001). The Food and Drug Administration approved the preventive regimen in 2012.
Increased knowledge did not translate to greater willingness to take the daily pill – which has held steady at about 60% of over time.
The number of men who self-reported as HIV negative and sexually active in the previous 12 months included in the survey varied from 421 in 2008, to 461 in 2011, to 451 in 2014.
For people at elevated risk for HIV infection, PrEP also represents an opportunity to take greater control over behavior, according to a recent review (Curr Opin HIV AIDS. 2016;11:3-9). “When you get people in for counseling or condoms, you give them a sense of control,” said Dr. Krotchko of Denver Health Medical Center.
Most survey respondents said they anticipated they would use condoms just as frequently as before if taking PrEP (82%, 78%, and 78%, in 2008, 2011, and 2014, respectively). Similarly, the majority of respondents anticipated having the same number of sexual partners if taking PrEP (92%, 85%, and 89%). These differences were not statistically significant.
The findings indicate availability of HIV PrEP is not increasing unhealthy behaviors, as some may fear. “Riskier behavior while on PrEP has not been borne out by the literature,” Dr. Krotchko said.
Strengths of the study include directly targeting a high-risk population and identifying those with high-risk behaviors who could benefit from use of HIV PrEP. Self-reported anticipated changes may not reflect future behavior in all cases, a potential limitation, Dr. Krotchko pointed out.
The NHBS survey is funded by the Centers for Disease Control and Prevention. IDWeek 2016 comprises the combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
NEW ORLEANS – Awareness about preexposure prophylaxis (PrEP) is steadily increasing among men who have sex with men at high risk for HIV infection, but that increased knowledge did not translate into greater willingness to take the daily pill nor did it increase engagement in high-risk behaviors.
Using questions from the National HIV Behavioral Surveillance System (NHBS), investigators surveyed men who have sex with men in urban settings in 3-year cycles. Awareness about HIV PrEP, once-daily emtricitabine/tenofovir (Truvada) increased from 21% in 2008 to 28% in 2011 to 46% in 2014.
The increase from 2011 to 2014 was statistically significant (P less than .001). The Food and Drug Administration approved the preventive regimen in 2012.
Increased knowledge did not translate to greater willingness to take the daily pill – which has held steady at about 60% of over time.
The number of men who self-reported as HIV negative and sexually active in the previous 12 months included in the survey varied from 421 in 2008, to 461 in 2011, to 451 in 2014.
For people at elevated risk for HIV infection, PrEP also represents an opportunity to take greater control over behavior, according to a recent review (Curr Opin HIV AIDS. 2016;11:3-9). “When you get people in for counseling or condoms, you give them a sense of control,” said Dr. Krotchko of Denver Health Medical Center.
Most survey respondents said they anticipated they would use condoms just as frequently as before if taking PrEP (82%, 78%, and 78%, in 2008, 2011, and 2014, respectively). Similarly, the majority of respondents anticipated having the same number of sexual partners if taking PrEP (92%, 85%, and 89%). These differences were not statistically significant.
The findings indicate availability of HIV PrEP is not increasing unhealthy behaviors, as some may fear. “Riskier behavior while on PrEP has not been borne out by the literature,” Dr. Krotchko said.
Strengths of the study include directly targeting a high-risk population and identifying those with high-risk behaviors who could benefit from use of HIV PrEP. Self-reported anticipated changes may not reflect future behavior in all cases, a potential limitation, Dr. Krotchko pointed out.
The NHBS survey is funded by the Centers for Disease Control and Prevention. IDWeek 2016 comprises the combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
NEW ORLEANS – Awareness about preexposure prophylaxis (PrEP) is steadily increasing among men who have sex with men at high risk for HIV infection, but that increased knowledge did not translate into greater willingness to take the daily pill nor did it increase engagement in high-risk behaviors.
Using questions from the National HIV Behavioral Surveillance System (NHBS), investigators surveyed men who have sex with men in urban settings in 3-year cycles. Awareness about HIV PrEP, once-daily emtricitabine/tenofovir (Truvada) increased from 21% in 2008 to 28% in 2011 to 46% in 2014.
The increase from 2011 to 2014 was statistically significant (P less than .001). The Food and Drug Administration approved the preventive regimen in 2012.
Increased knowledge did not translate to greater willingness to take the daily pill – which has held steady at about 60% of over time.
The number of men who self-reported as HIV negative and sexually active in the previous 12 months included in the survey varied from 421 in 2008, to 461 in 2011, to 451 in 2014.
For people at elevated risk for HIV infection, PrEP also represents an opportunity to take greater control over behavior, according to a recent review (Curr Opin HIV AIDS. 2016;11:3-9). “When you get people in for counseling or condoms, you give them a sense of control,” said Dr. Krotchko of Denver Health Medical Center.
Most survey respondents said they anticipated they would use condoms just as frequently as before if taking PrEP (82%, 78%, and 78%, in 2008, 2011, and 2014, respectively). Similarly, the majority of respondents anticipated having the same number of sexual partners if taking PrEP (92%, 85%, and 89%). These differences were not statistically significant.
The findings indicate availability of HIV PrEP is not increasing unhealthy behaviors, as some may fear. “Riskier behavior while on PrEP has not been borne out by the literature,” Dr. Krotchko said.
Strengths of the study include directly targeting a high-risk population and identifying those with high-risk behaviors who could benefit from use of HIV PrEP. Self-reported anticipated changes may not reflect future behavior in all cases, a potential limitation, Dr. Krotchko pointed out.
The NHBS survey is funded by the Centers for Disease Control and Prevention. IDWeek 2016 comprises the combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
AT IDWEEK 2016
Key clinical point: Adoption and use of HIV PrEP continues to lag behind studies showing its effectiveness in the high-risk population of men who have sex with men.
Major finding: Despite increasing awareness, willingness to use HIV PrEP among MSM remained steady at about 60% over time in a series of national behavioral health surveys.
Data source: The National HIV Behavioral Surveillance System.
Disclosures: Dr. Krotchko had no relevant disclosures.