User login
Clinicians underusing statins, aspirin in HIV patients
NEW ORLEANS – Clinicians may not be prescribing enough statins and/or aspirin therapy for the HIV-infected population at highest risk for atherosclerotic cardiovascular disease, according to the results of a large retrospective study from an HIV clinic in New York.
“We need to shift our paradigm for care – from ‘take antiretrovirals and that’s it’ – to a focus on the whole patient and chronic conditions,” Emma Kaplan-Lewis, MD, said during a poster presentation at an annual scientific meeting on infectious diseases. Risk of cardiovascular events increases 1.5-fold among people with HIV treated with antiretroviral therapy, compared with the uninfected population, she noted.
The investigators examined prescriptions for a statin or aspirin therapy in three high-risk groups, defined by 2013 American College of Cardiology/American Heart Association guidelines and 2011 AHA/American College of Cardiology Foundation guidelines. They classified patients with an ICD-9 code indicating a history of atherosclerotic cardiovascular disease, 40- to 75-year-olds with diabetes and LDL cholesterol greater than 70 mg/dL, and those with an LDL cholesterol level greater than 190 mg/dL.
Almost two-thirds of the higher-risk patients, 141 (61%), had a history of atherosclerotic cardiovascular disease. In this cohort, 56% were prescribed statin therapy, and 100 (71%) were prescribed aspirin.
Of the 85 high-risk patients with diabetes and an LDL greater than 70 mg/dL, 48 (57%) were on statin therapy (aspirin not indicated), and of the 5 high-risk patients with an LDL cholesterol level greater than 190 mg/dL, 3 (60%) were on statin therapy, and 1 (20%) was on aspirin.
The investigators also found 37% of the higher-risk patients were active cigarette smokers. There was a trend toward lower statin use among smokers, 33% versus 44% for nonsmokers. “Smoking was not significantly associated with statin prescription, but this is a modifiable risk factor – after which they may not need a statin,” Dr. Kaplan-Lewis said.
The findings support risk-reduction interventions for people with HIV infection who are at higher risk for cardiovascular disease, Dr. Kaplan-Lewis said. The results support previous reports in the literature, including a study that found 51% of 13,579 veterans infected with HIV had an indication for statin use, but 22% of this group was not prescribed the therapy (Clin Infect Dis. 2016;63:407-13. doi: 10.1093/cid/ciw289).
In 2017, the investigators plan to share the study data with providers. “Each provider will get a list of their patients who should be on a statin. This is about awareness and making it more of a priority,” Dr. Kaplan-Lewis said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The findings of additional research assessing lower thresholds for statin use among people with HIV infection are still pending, Dr. Kaplan-Lewis added.
The study was supported in part by the New York State Department of Health Empire Clinical Research Investigator Program. Dr. Kaplan-Lewis had no relevant disclosures.
NEW ORLEANS – Clinicians may not be prescribing enough statins and/or aspirin therapy for the HIV-infected population at highest risk for atherosclerotic cardiovascular disease, according to the results of a large retrospective study from an HIV clinic in New York.
“We need to shift our paradigm for care – from ‘take antiretrovirals and that’s it’ – to a focus on the whole patient and chronic conditions,” Emma Kaplan-Lewis, MD, said during a poster presentation at an annual scientific meeting on infectious diseases. Risk of cardiovascular events increases 1.5-fold among people with HIV treated with antiretroviral therapy, compared with the uninfected population, she noted.
The investigators examined prescriptions for a statin or aspirin therapy in three high-risk groups, defined by 2013 American College of Cardiology/American Heart Association guidelines and 2011 AHA/American College of Cardiology Foundation guidelines. They classified patients with an ICD-9 code indicating a history of atherosclerotic cardiovascular disease, 40- to 75-year-olds with diabetes and LDL cholesterol greater than 70 mg/dL, and those with an LDL cholesterol level greater than 190 mg/dL.
Almost two-thirds of the higher-risk patients, 141 (61%), had a history of atherosclerotic cardiovascular disease. In this cohort, 56% were prescribed statin therapy, and 100 (71%) were prescribed aspirin.
Of the 85 high-risk patients with diabetes and an LDL greater than 70 mg/dL, 48 (57%) were on statin therapy (aspirin not indicated), and of the 5 high-risk patients with an LDL cholesterol level greater than 190 mg/dL, 3 (60%) were on statin therapy, and 1 (20%) was on aspirin.
The investigators also found 37% of the higher-risk patients were active cigarette smokers. There was a trend toward lower statin use among smokers, 33% versus 44% for nonsmokers. “Smoking was not significantly associated with statin prescription, but this is a modifiable risk factor – after which they may not need a statin,” Dr. Kaplan-Lewis said.
The findings support risk-reduction interventions for people with HIV infection who are at higher risk for cardiovascular disease, Dr. Kaplan-Lewis said. The results support previous reports in the literature, including a study that found 51% of 13,579 veterans infected with HIV had an indication for statin use, but 22% of this group was not prescribed the therapy (Clin Infect Dis. 2016;63:407-13. doi: 10.1093/cid/ciw289).
In 2017, the investigators plan to share the study data with providers. “Each provider will get a list of their patients who should be on a statin. This is about awareness and making it more of a priority,” Dr. Kaplan-Lewis said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The findings of additional research assessing lower thresholds for statin use among people with HIV infection are still pending, Dr. Kaplan-Lewis added.
The study was supported in part by the New York State Department of Health Empire Clinical Research Investigator Program. Dr. Kaplan-Lewis had no relevant disclosures.
NEW ORLEANS – Clinicians may not be prescribing enough statins and/or aspirin therapy for the HIV-infected population at highest risk for atherosclerotic cardiovascular disease, according to the results of a large retrospective study from an HIV clinic in New York.
“We need to shift our paradigm for care – from ‘take antiretrovirals and that’s it’ – to a focus on the whole patient and chronic conditions,” Emma Kaplan-Lewis, MD, said during a poster presentation at an annual scientific meeting on infectious diseases. Risk of cardiovascular events increases 1.5-fold among people with HIV treated with antiretroviral therapy, compared with the uninfected population, she noted.
The investigators examined prescriptions for a statin or aspirin therapy in three high-risk groups, defined by 2013 American College of Cardiology/American Heart Association guidelines and 2011 AHA/American College of Cardiology Foundation guidelines. They classified patients with an ICD-9 code indicating a history of atherosclerotic cardiovascular disease, 40- to 75-year-olds with diabetes and LDL cholesterol greater than 70 mg/dL, and those with an LDL cholesterol level greater than 190 mg/dL.
Almost two-thirds of the higher-risk patients, 141 (61%), had a history of atherosclerotic cardiovascular disease. In this cohort, 56% were prescribed statin therapy, and 100 (71%) were prescribed aspirin.
Of the 85 high-risk patients with diabetes and an LDL greater than 70 mg/dL, 48 (57%) were on statin therapy (aspirin not indicated), and of the 5 high-risk patients with an LDL cholesterol level greater than 190 mg/dL, 3 (60%) were on statin therapy, and 1 (20%) was on aspirin.
The investigators also found 37% of the higher-risk patients were active cigarette smokers. There was a trend toward lower statin use among smokers, 33% versus 44% for nonsmokers. “Smoking was not significantly associated with statin prescription, but this is a modifiable risk factor – after which they may not need a statin,” Dr. Kaplan-Lewis said.
The findings support risk-reduction interventions for people with HIV infection who are at higher risk for cardiovascular disease, Dr. Kaplan-Lewis said. The results support previous reports in the literature, including a study that found 51% of 13,579 veterans infected with HIV had an indication for statin use, but 22% of this group was not prescribed the therapy (Clin Infect Dis. 2016;63:407-13. doi: 10.1093/cid/ciw289).
In 2017, the investigators plan to share the study data with providers. “Each provider will get a list of their patients who should be on a statin. This is about awareness and making it more of a priority,” Dr. Kaplan-Lewis said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The findings of additional research assessing lower thresholds for statin use among people with HIV infection are still pending, Dr. Kaplan-Lewis added.
The study was supported in part by the New York State Department of Health Empire Clinical Research Investigator Program. Dr. Kaplan-Lewis had no relevant disclosures.
AT IDWEEK 2016
Key clinical point: Statins and aspirin therapy are underutilized in a proportion of the HIV positive population at higher risk for cardiovascular disease.
Major finding: Of the 141 high-risk people with HIV infection and a history of atherosclerotic cardiovascular disease, only 56% were prescribed a statin and 71% were prescribed aspirin.
Data source: Poster presentation at IDWeek 2016.
Disclosures: The study was supported in part by the New York State Department of Health Empire Clinical Research Investigator Program. Dr. Kaplan-Lewis had no relevant disclosures.
Surgical discharge data highlight stewardship need at transition
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
AT IDWEEK 2016
Key clinical point:
Major finding: 70% of prescriptions had at least one error in drug choice, dose, indication, or duration.
Data source: A review of discharge data for 150 patients at an academic hospital.
Disclosures: Dr. Scarpato reported having no conflicts of interest.
VIDEO: HIV PrEP effective, but adoption lags among high-risk patients
NEW ORLEANS – The adoption and use of HIV preexposure prophylaxis (PrEP) continues to lag behind studies showing its effectiveness in the high-risk population of men who have sex with men, says a clinician who works with these patients.
John Krotchko, MD, a family practitioner at Denver Health and Hospital Authority, has studied the impact of a community outreach program – targeting HIV-negative men who have sex with men – that educates about HIV PrEP and offers HIV testing. He and his colleagues have examined the effectiveness of this approach, how comfortable participants are discussing their behaviors, and have tried to determine whether availability of HIV PrEP increases high-risk behaviors.
Dr. Krotchko and his colleagues also studied overall trends in awareness about PrEP over time, as well as the acceptability of participants to take a once-daily emtricitabine/tenofovir pill. He explained in a video interview why he believes it’s important to manage these patients in a primary care setting. The interview took place at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Krotchko had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The adoption and use of HIV preexposure prophylaxis (PrEP) continues to lag behind studies showing its effectiveness in the high-risk population of men who have sex with men, says a clinician who works with these patients.
John Krotchko, MD, a family practitioner at Denver Health and Hospital Authority, has studied the impact of a community outreach program – targeting HIV-negative men who have sex with men – that educates about HIV PrEP and offers HIV testing. He and his colleagues have examined the effectiveness of this approach, how comfortable participants are discussing their behaviors, and have tried to determine whether availability of HIV PrEP increases high-risk behaviors.
Dr. Krotchko and his colleagues also studied overall trends in awareness about PrEP over time, as well as the acceptability of participants to take a once-daily emtricitabine/tenofovir pill. He explained in a video interview why he believes it’s important to manage these patients in a primary care setting. The interview took place at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Krotchko had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The adoption and use of HIV preexposure prophylaxis (PrEP) continues to lag behind studies showing its effectiveness in the high-risk population of men who have sex with men, says a clinician who works with these patients.
John Krotchko, MD, a family practitioner at Denver Health and Hospital Authority, has studied the impact of a community outreach program – targeting HIV-negative men who have sex with men – that educates about HIV PrEP and offers HIV testing. He and his colleagues have examined the effectiveness of this approach, how comfortable participants are discussing their behaviors, and have tried to determine whether availability of HIV PrEP increases high-risk behaviors.
Dr. Krotchko and his colleagues also studied overall trends in awareness about PrEP over time, as well as the acceptability of participants to take a once-daily emtricitabine/tenofovir pill. He explained in a video interview why he believes it’s important to manage these patients in a primary care setting. The interview took place at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Krotchko had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT IDWEEK 2016
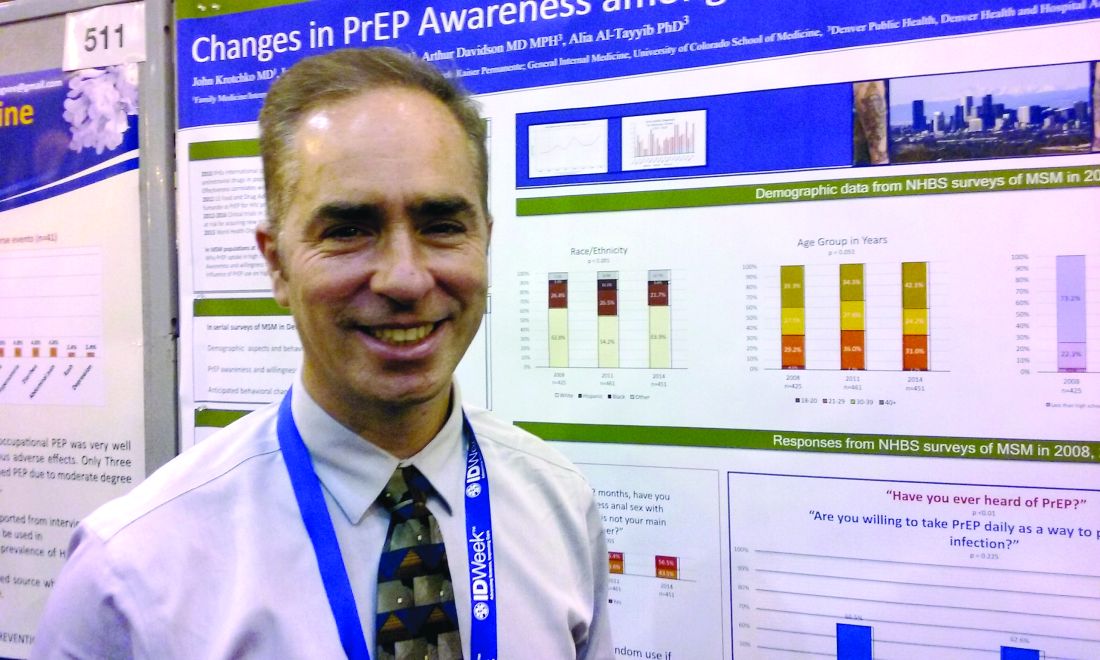
PrEP adoption lagging behind awareness in high-risk population
NEW ORLEANS – Awareness about preexposure prophylaxis (PrEP) is steadily increasing among men who have sex with men at high risk for HIV infection, but that increased knowledge did not translate into greater willingness to take the daily pill nor did it increase engagement in high-risk behaviors.
Using questions from the National HIV Behavioral Surveillance System (NHBS), investigators surveyed men who have sex with men in urban settings in 3-year cycles. Awareness about HIV PrEP, once-daily emtricitabine/tenofovir (Truvada) increased from 21% in 2008 to 28% in 2011 to 46% in 2014.
The increase from 2011 to 2014 was statistically significant (P less than .001). The Food and Drug Administration approved the preventive regimen in 2012.
Increased knowledge did not translate to greater willingness to take the daily pill – which has held steady at about 60% of over time.
The number of men who self-reported as HIV negative and sexually active in the previous 12 months included in the survey varied from 421 in 2008, to 461 in 2011, to 451 in 2014.
For people at elevated risk for HIV infection, PrEP also represents an opportunity to take greater control over behavior, according to a recent review (Curr Opin HIV AIDS. 2016;11:3-9). “When you get people in for counseling or condoms, you give them a sense of control,” said Dr. Krotchko of Denver Health Medical Center.
Most survey respondents said they anticipated they would use condoms just as frequently as before if taking PrEP (82%, 78%, and 78%, in 2008, 2011, and 2014, respectively). Similarly, the majority of respondents anticipated having the same number of sexual partners if taking PrEP (92%, 85%, and 89%). These differences were not statistically significant.
The findings indicate availability of HIV PrEP is not increasing unhealthy behaviors, as some may fear. “Riskier behavior while on PrEP has not been borne out by the literature,” Dr. Krotchko said.
Strengths of the study include directly targeting a high-risk population and identifying those with high-risk behaviors who could benefit from use of HIV PrEP. Self-reported anticipated changes may not reflect future behavior in all cases, a potential limitation, Dr. Krotchko pointed out.
The NHBS survey is funded by the Centers for Disease Control and Prevention. IDWeek 2016 comprises the combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
NEW ORLEANS – Awareness about preexposure prophylaxis (PrEP) is steadily increasing among men who have sex with men at high risk for HIV infection, but that increased knowledge did not translate into greater willingness to take the daily pill nor did it increase engagement in high-risk behaviors.
Using questions from the National HIV Behavioral Surveillance System (NHBS), investigators surveyed men who have sex with men in urban settings in 3-year cycles. Awareness about HIV PrEP, once-daily emtricitabine/tenofovir (Truvada) increased from 21% in 2008 to 28% in 2011 to 46% in 2014.
The increase from 2011 to 2014 was statistically significant (P less than .001). The Food and Drug Administration approved the preventive regimen in 2012.
Increased knowledge did not translate to greater willingness to take the daily pill – which has held steady at about 60% of over time.
The number of men who self-reported as HIV negative and sexually active in the previous 12 months included in the survey varied from 421 in 2008, to 461 in 2011, to 451 in 2014.
For people at elevated risk for HIV infection, PrEP also represents an opportunity to take greater control over behavior, according to a recent review (Curr Opin HIV AIDS. 2016;11:3-9). “When you get people in for counseling or condoms, you give them a sense of control,” said Dr. Krotchko of Denver Health Medical Center.
Most survey respondents said they anticipated they would use condoms just as frequently as before if taking PrEP (82%, 78%, and 78%, in 2008, 2011, and 2014, respectively). Similarly, the majority of respondents anticipated having the same number of sexual partners if taking PrEP (92%, 85%, and 89%). These differences were not statistically significant.
The findings indicate availability of HIV PrEP is not increasing unhealthy behaviors, as some may fear. “Riskier behavior while on PrEP has not been borne out by the literature,” Dr. Krotchko said.
Strengths of the study include directly targeting a high-risk population and identifying those with high-risk behaviors who could benefit from use of HIV PrEP. Self-reported anticipated changes may not reflect future behavior in all cases, a potential limitation, Dr. Krotchko pointed out.
The NHBS survey is funded by the Centers for Disease Control and Prevention. IDWeek 2016 comprises the combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
NEW ORLEANS – Awareness about preexposure prophylaxis (PrEP) is steadily increasing among men who have sex with men at high risk for HIV infection, but that increased knowledge did not translate into greater willingness to take the daily pill nor did it increase engagement in high-risk behaviors.
Using questions from the National HIV Behavioral Surveillance System (NHBS), investigators surveyed men who have sex with men in urban settings in 3-year cycles. Awareness about HIV PrEP, once-daily emtricitabine/tenofovir (Truvada) increased from 21% in 2008 to 28% in 2011 to 46% in 2014.
The increase from 2011 to 2014 was statistically significant (P less than .001). The Food and Drug Administration approved the preventive regimen in 2012.
Increased knowledge did not translate to greater willingness to take the daily pill – which has held steady at about 60% of over time.
The number of men who self-reported as HIV negative and sexually active in the previous 12 months included in the survey varied from 421 in 2008, to 461 in 2011, to 451 in 2014.
For people at elevated risk for HIV infection, PrEP also represents an opportunity to take greater control over behavior, according to a recent review (Curr Opin HIV AIDS. 2016;11:3-9). “When you get people in for counseling or condoms, you give them a sense of control,” said Dr. Krotchko of Denver Health Medical Center.
Most survey respondents said they anticipated they would use condoms just as frequently as before if taking PrEP (82%, 78%, and 78%, in 2008, 2011, and 2014, respectively). Similarly, the majority of respondents anticipated having the same number of sexual partners if taking PrEP (92%, 85%, and 89%). These differences were not statistically significant.
The findings indicate availability of HIV PrEP is not increasing unhealthy behaviors, as some may fear. “Riskier behavior while on PrEP has not been borne out by the literature,” Dr. Krotchko said.
Strengths of the study include directly targeting a high-risk population and identifying those with high-risk behaviors who could benefit from use of HIV PrEP. Self-reported anticipated changes may not reflect future behavior in all cases, a potential limitation, Dr. Krotchko pointed out.
The NHBS survey is funded by the Centers for Disease Control and Prevention. IDWeek 2016 comprises the combined meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
AT IDWEEK 2016
Key clinical point: Adoption and use of HIV PrEP continues to lag behind studies showing its effectiveness in the high-risk population of men who have sex with men.
Major finding: Despite increasing awareness, willingness to use HIV PrEP among MSM remained steady at about 60% over time in a series of national behavioral health surveys.
Data source: The National HIV Behavioral Surveillance System.
Disclosures: Dr. Krotchko had no relevant disclosures.
‘Skip phenomenon’ could explain fluctuating positivity for S. aureus bacteremia
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Inpatient telemedicine could bridge infectious disease specialist gap
NEW ORLEANS – Telemedicine inpatient consultations are a relatively new component in health care, but they could help address the problem of infectious disease physician shortages, particularly in rural communities, according to Lewis McCurdy, MD.
Dr. McCurdy of Carolinas HealthCare System in Charlotte, N.C., shared his experience providing virtual consultations for inpatients at a rural community hospital, noting that the approach was well received by patients, and that uptake by providers doubled during the first year.
Further, the virtual consultations appeared to have important clinical benefits, because very few patients had to be transferred to higher-level acuity facilities. The consultations seemed to help providers with challenging situations that they might not have felt comfortable managing otherwise, such as bloodstream infections, he said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In a video interview, Dr. McCurdy discussed the development of the process for using telemedicine for inpatient consultations, outcomes after about 18 months at one facility, and challenges of providing telemedicine services.
The approach could be very helpful for smaller communities without an infectious disease provider, Dr. McCurdy said.
“This allows us to sort of expand our expertise into those communities on a more efficiently scaled basis,” he explained. “So, it does provide one solution to trying to meet the demand in the community for ID expertise.”
Dr. McCurdy reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Telemedicine inpatient consultations are a relatively new component in health care, but they could help address the problem of infectious disease physician shortages, particularly in rural communities, according to Lewis McCurdy, MD.
Dr. McCurdy of Carolinas HealthCare System in Charlotte, N.C., shared his experience providing virtual consultations for inpatients at a rural community hospital, noting that the approach was well received by patients, and that uptake by providers doubled during the first year.
Further, the virtual consultations appeared to have important clinical benefits, because very few patients had to be transferred to higher-level acuity facilities. The consultations seemed to help providers with challenging situations that they might not have felt comfortable managing otherwise, such as bloodstream infections, he said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In a video interview, Dr. McCurdy discussed the development of the process for using telemedicine for inpatient consultations, outcomes after about 18 months at one facility, and challenges of providing telemedicine services.
The approach could be very helpful for smaller communities without an infectious disease provider, Dr. McCurdy said.
“This allows us to sort of expand our expertise into those communities on a more efficiently scaled basis,” he explained. “So, it does provide one solution to trying to meet the demand in the community for ID expertise.”
Dr. McCurdy reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Telemedicine inpatient consultations are a relatively new component in health care, but they could help address the problem of infectious disease physician shortages, particularly in rural communities, according to Lewis McCurdy, MD.
Dr. McCurdy of Carolinas HealthCare System in Charlotte, N.C., shared his experience providing virtual consultations for inpatients at a rural community hospital, noting that the approach was well received by patients, and that uptake by providers doubled during the first year.
Further, the virtual consultations appeared to have important clinical benefits, because very few patients had to be transferred to higher-level acuity facilities. The consultations seemed to help providers with challenging situations that they might not have felt comfortable managing otherwise, such as bloodstream infections, he said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In a video interview, Dr. McCurdy discussed the development of the process for using telemedicine for inpatient consultations, outcomes after about 18 months at one facility, and challenges of providing telemedicine services.
The approach could be very helpful for smaller communities without an infectious disease provider, Dr. McCurdy said.
“This allows us to sort of expand our expertise into those communities on a more efficiently scaled basis,” he explained. “So, it does provide one solution to trying to meet the demand in the community for ID expertise.”
Dr. McCurdy reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Infectious disease physicians: Antibiotic shortages are the new norm
NEW ORLEANS – Antibiotic shortages reported by the Emerging Infections Network (EIN) in 2011 persist in 2016, according to a web-based follow-up survey of infectious disease physicians.
Of 701 network members who responded to the EIN survey in early 2016, 70% reported needing to modify their antimicrobial choice because of a shortage in the past 2 years. They did so by using broader-spectrum agents (75% of respondents), more costly agents (58%), less effective second-line agents (45%), and more toxic agents (37%), Adi Gundlapalli, MD, PhD, reported at an annual scientific meeting on infectious diseases.
In addition, 73% of respondents reported that the shortages affected patient care or outcomes, reported Dr. Gundlapalli of the University of Utah, Salt Lake City.
The percentage of respondents reporting adverse patient outcomes related to shortages increased from 2011 to 2016 (51% vs.73%), he noted at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The top 10 antimicrobials they reported as being in short supply were piperacillin-tazobactam, ampicillin-sulbactam, meropenem, cefotaxime, cefepime, trimethoprim-sulfamethoxazole (TMP-SMX), doxycycline, imipenem, acyclovir, and amikacin. TMP-SMX and acyclovir were in short supply at both time points.
The most common ways respondents reported learning about drug shortages were from hospital notification (76%), from a colleague (56%), from a pharmacy that contacted them regarding a prescription for the agent (53%), or from the Food and Drug Administration website or another website on shortages (23%). The most common ways of learning about a shortage changed – from notification after trying to prescribe a drug in 2011, to proactive hospital/system (local) notification in 2016; 71% of respondents said that communications in 2016 were sufficient.
Most respondents (83%) reported that guidelines for dealing with shortages had been developed by an antimicrobial stewardship program (ASP) at their institution.
“This, I think, is one of the highlight results,” said Dr. Gundlapalli, who is also a staff physician at the VA Salt Lake City Health System. “In 2011, we had no specific question or comments received about [ASPs], and here in 2016, 83% of respondents’ institutions had developed guidelines related to drug shortages.”
Respondents also had the opportunity to submit free-text responses, and among the themes that emerged was concern regarding toxicity and adverse outcomes associated with increased use of aminoglycosides because of the shortage of piperacillin-tazobactam. Another – described as a blessing in disguise – was the shortage of meropenem, which led one ASP to “institute restrictions on its use, which have continued,” he said.
“Another theme was ‘simpler agents seem more likely to be in shortage,’ ” Dr. Gundlapalli said, noting ampicillin-sulbactam in 2016 and Pen-G as examples.
“And then, of course, the other theme across the board ... was our new asset,” he said, explaining that some respondents commented on the value of ASP pharmacists and programs to help with drug shortage issues.
The overall theme of this follow-up survey, in the context of prior surveys in 2001 and 2011, is that antibiotic shortages are the “new normal – a way of life,” Dr. Gundlapalli said.
“The concerns do persist, and we feel there is further work to be done here,” he said. He specifically noted that there is a need to inform and educate fellows and colleagues in hospitals, increase awareness generally, improve communication strategies, and conduct detailed studies on adverse effects and outcomes.
“And now, since ASPs are very pervasive ... maybe it’s time to formalize and delineate the role of ASPs in antimicrobial shortages,” he said.
The problem of antibiotic shortages “harkens back to the day when penicillin was recycled in the urine [of soldiers in World War II] to save this very scarce resource ... but that’s a very extreme measure to take,” noted Donald Graham, MD, of the Springfield (Ill.) Clinic, one of the study’s coauthors. “It seems like it’s time for the other federal arm – namely, the Food and Drug Administration – to do something about this.”
Dr. Graham said he believes the problem is in part because of economics, and in part because of “the higher standards that the FDA imposes upon these manufacturing concerns.” These drugs often are low-profit items, and it isn’t always in the financial best interest of a pharmaceutical company to upgrade their facilities.
“But they really have to recognize the importance of having availability of these simple agents,” he said, pleading with any FDA representatives in the audience to “maybe think about some of these very high standards.”
Dr. Gundlapalli reported having no disclosures. Dr. Graham disclosed relationships with Astellas and Theravance Biopharma.
NEW ORLEANS – Antibiotic shortages reported by the Emerging Infections Network (EIN) in 2011 persist in 2016, according to a web-based follow-up survey of infectious disease physicians.
Of 701 network members who responded to the EIN survey in early 2016, 70% reported needing to modify their antimicrobial choice because of a shortage in the past 2 years. They did so by using broader-spectrum agents (75% of respondents), more costly agents (58%), less effective second-line agents (45%), and more toxic agents (37%), Adi Gundlapalli, MD, PhD, reported at an annual scientific meeting on infectious diseases.
In addition, 73% of respondents reported that the shortages affected patient care or outcomes, reported Dr. Gundlapalli of the University of Utah, Salt Lake City.
The percentage of respondents reporting adverse patient outcomes related to shortages increased from 2011 to 2016 (51% vs.73%), he noted at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The top 10 antimicrobials they reported as being in short supply were piperacillin-tazobactam, ampicillin-sulbactam, meropenem, cefotaxime, cefepime, trimethoprim-sulfamethoxazole (TMP-SMX), doxycycline, imipenem, acyclovir, and amikacin. TMP-SMX and acyclovir were in short supply at both time points.
The most common ways respondents reported learning about drug shortages were from hospital notification (76%), from a colleague (56%), from a pharmacy that contacted them regarding a prescription for the agent (53%), or from the Food and Drug Administration website or another website on shortages (23%). The most common ways of learning about a shortage changed – from notification after trying to prescribe a drug in 2011, to proactive hospital/system (local) notification in 2016; 71% of respondents said that communications in 2016 were sufficient.
Most respondents (83%) reported that guidelines for dealing with shortages had been developed by an antimicrobial stewardship program (ASP) at their institution.
“This, I think, is one of the highlight results,” said Dr. Gundlapalli, who is also a staff physician at the VA Salt Lake City Health System. “In 2011, we had no specific question or comments received about [ASPs], and here in 2016, 83% of respondents’ institutions had developed guidelines related to drug shortages.”
Respondents also had the opportunity to submit free-text responses, and among the themes that emerged was concern regarding toxicity and adverse outcomes associated with increased use of aminoglycosides because of the shortage of piperacillin-tazobactam. Another – described as a blessing in disguise – was the shortage of meropenem, which led one ASP to “institute restrictions on its use, which have continued,” he said.
“Another theme was ‘simpler agents seem more likely to be in shortage,’ ” Dr. Gundlapalli said, noting ampicillin-sulbactam in 2016 and Pen-G as examples.
“And then, of course, the other theme across the board ... was our new asset,” he said, explaining that some respondents commented on the value of ASP pharmacists and programs to help with drug shortage issues.
The overall theme of this follow-up survey, in the context of prior surveys in 2001 and 2011, is that antibiotic shortages are the “new normal – a way of life,” Dr. Gundlapalli said.
“The concerns do persist, and we feel there is further work to be done here,” he said. He specifically noted that there is a need to inform and educate fellows and colleagues in hospitals, increase awareness generally, improve communication strategies, and conduct detailed studies on adverse effects and outcomes.
“And now, since ASPs are very pervasive ... maybe it’s time to formalize and delineate the role of ASPs in antimicrobial shortages,” he said.
The problem of antibiotic shortages “harkens back to the day when penicillin was recycled in the urine [of soldiers in World War II] to save this very scarce resource ... but that’s a very extreme measure to take,” noted Donald Graham, MD, of the Springfield (Ill.) Clinic, one of the study’s coauthors. “It seems like it’s time for the other federal arm – namely, the Food and Drug Administration – to do something about this.”
Dr. Graham said he believes the problem is in part because of economics, and in part because of “the higher standards that the FDA imposes upon these manufacturing concerns.” These drugs often are low-profit items, and it isn’t always in the financial best interest of a pharmaceutical company to upgrade their facilities.
“But they really have to recognize the importance of having availability of these simple agents,” he said, pleading with any FDA representatives in the audience to “maybe think about some of these very high standards.”
Dr. Gundlapalli reported having no disclosures. Dr. Graham disclosed relationships with Astellas and Theravance Biopharma.
NEW ORLEANS – Antibiotic shortages reported by the Emerging Infections Network (EIN) in 2011 persist in 2016, according to a web-based follow-up survey of infectious disease physicians.
Of 701 network members who responded to the EIN survey in early 2016, 70% reported needing to modify their antimicrobial choice because of a shortage in the past 2 years. They did so by using broader-spectrum agents (75% of respondents), more costly agents (58%), less effective second-line agents (45%), and more toxic agents (37%), Adi Gundlapalli, MD, PhD, reported at an annual scientific meeting on infectious diseases.
In addition, 73% of respondents reported that the shortages affected patient care or outcomes, reported Dr. Gundlapalli of the University of Utah, Salt Lake City.
The percentage of respondents reporting adverse patient outcomes related to shortages increased from 2011 to 2016 (51% vs.73%), he noted at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The top 10 antimicrobials they reported as being in short supply were piperacillin-tazobactam, ampicillin-sulbactam, meropenem, cefotaxime, cefepime, trimethoprim-sulfamethoxazole (TMP-SMX), doxycycline, imipenem, acyclovir, and amikacin. TMP-SMX and acyclovir were in short supply at both time points.
The most common ways respondents reported learning about drug shortages were from hospital notification (76%), from a colleague (56%), from a pharmacy that contacted them regarding a prescription for the agent (53%), or from the Food and Drug Administration website or another website on shortages (23%). The most common ways of learning about a shortage changed – from notification after trying to prescribe a drug in 2011, to proactive hospital/system (local) notification in 2016; 71% of respondents said that communications in 2016 were sufficient.
Most respondents (83%) reported that guidelines for dealing with shortages had been developed by an antimicrobial stewardship program (ASP) at their institution.
“This, I think, is one of the highlight results,” said Dr. Gundlapalli, who is also a staff physician at the VA Salt Lake City Health System. “In 2011, we had no specific question or comments received about [ASPs], and here in 2016, 83% of respondents’ institutions had developed guidelines related to drug shortages.”
Respondents also had the opportunity to submit free-text responses, and among the themes that emerged was concern regarding toxicity and adverse outcomes associated with increased use of aminoglycosides because of the shortage of piperacillin-tazobactam. Another – described as a blessing in disguise – was the shortage of meropenem, which led one ASP to “institute restrictions on its use, which have continued,” he said.
“Another theme was ‘simpler agents seem more likely to be in shortage,’ ” Dr. Gundlapalli said, noting ampicillin-sulbactam in 2016 and Pen-G as examples.
“And then, of course, the other theme across the board ... was our new asset,” he said, explaining that some respondents commented on the value of ASP pharmacists and programs to help with drug shortage issues.
The overall theme of this follow-up survey, in the context of prior surveys in 2001 and 2011, is that antibiotic shortages are the “new normal – a way of life,” Dr. Gundlapalli said.
“The concerns do persist, and we feel there is further work to be done here,” he said. He specifically noted that there is a need to inform and educate fellows and colleagues in hospitals, increase awareness generally, improve communication strategies, and conduct detailed studies on adverse effects and outcomes.
“And now, since ASPs are very pervasive ... maybe it’s time to formalize and delineate the role of ASPs in antimicrobial shortages,” he said.
The problem of antibiotic shortages “harkens back to the day when penicillin was recycled in the urine [of soldiers in World War II] to save this very scarce resource ... but that’s a very extreme measure to take,” noted Donald Graham, MD, of the Springfield (Ill.) Clinic, one of the study’s coauthors. “It seems like it’s time for the other federal arm – namely, the Food and Drug Administration – to do something about this.”
Dr. Graham said he believes the problem is in part because of economics, and in part because of “the higher standards that the FDA imposes upon these manufacturing concerns.” These drugs often are low-profit items, and it isn’t always in the financial best interest of a pharmaceutical company to upgrade their facilities.
“But they really have to recognize the importance of having availability of these simple agents,” he said, pleading with any FDA representatives in the audience to “maybe think about some of these very high standards.”
Dr. Gundlapalli reported having no disclosures. Dr. Graham disclosed relationships with Astellas and Theravance Biopharma.
AT IDWEEK 2016
Key clinical point:
Major finding: 70% of respondents reported needing to modify their antimicrobial choice because of a shortage in the past 2 years, and 73% said shortages affected patient care or outcomes.
Data source: A follow-up survey of 701 physicians.
Disclosures: Dr. Gundlapalli reported having no disclosures. Dr. Graham disclosed relationships with Astellas and Theravance Biopharma.
Phase II data suggest IV zanamivir safe for severe flu in kids
NEW ORLEANS – The investigational intravenous formulation of the neuraminidase inhibitor zanamivir appears to be a safe influenza treatment for hospitalized children and adolescents at high risk of complications who can’t tolerate enteral therapy, according to findings from an open-label, multicenter, phase II study.
In 71 such patients with laboratory-confirmed flu, who presented within 7 days of illness onset and who received intravenous zanamivir (IVZ) for 5-10 days, 72% experienced adverse events (AEs), 21% experienced serious adverse events, and 5 deaths occurred, but none were considered by the investigators to be attributable to IVZ, Jeffrey Blumer, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Rather, the adverse events were “fairly diverse. ... the kinds of things normally seen in critically ill pediatric populations,” he said.
The patients, who had a mean age of 7 years, were treated with IVZ doses selected to provide exposures comparable to 600 mg in adults – a dosage shown in prior studies to be safe and well-tolerated in adults. Patients aged 6 months to under age 6 years received twice-daily doses of 14 mg/kg, and those aged 6 years to less than 18 years received twice-daily doses of 12 mg/kg, not to exceed 600 mg. Doses were adjusted for renal function.
Patients were enrolled from five countries, and most (69%) had received prior treatment with oseltamivir. More than half (56%) had chronic medical conditions.
The median time from symptom onset to IVZ treatment was 4 days, Dr. Blumer of the University of Toledo (Ohio) said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Infiltrate on chest x-ray was seen in 59% of patients, mechanical ventilation was required in 34% of patients, and extracorporeal membrane oxygenation was required in 6% of patients. Treatment in the intensive care unit was required in 65% of patients, and cumulative mortality was 4% at 14 days, and 7% at 28 days.
“Overall, the [IVZ] exposure and then the elimination profiles were consistent across the entire age cohort – unusual for most drugs, but it seemed to hold true, which makes zanamivir a lot easier for us to work with in pediatrics,” Dr. Blumer said.
While the numbers are small, exposure and response delineation didn’t seem to be impacted by mechanical ventilation, by extracorporeal membrane oxygenation, or by continuous renal replacement therapy, which is a good sign, he noted.
“So we generally had good, consistent experience here. ... Overall, 64 of the 71 patients survived, got better, left the ICU, and left the hospital,” Dr. Blumer said.
Of note, a treatment-emergent resistance substitution, E119G, was detected in a day 5 H1N1 isolate from an immunocompetent patient who improved clinically while on IVZ, he said, adding that no phenotype data were available as the sample could not be cultured.
The findings are important, because while zanamivir is currently labeled for patients older than 7 years, and the intravenous formulation currently in development has been shown to be safe for adults, there is a critical unmet need for an effective parenteral treatment for severe flu in children at high risk of complications who cannot tolerate enteral therapy.
“We need a drug that is available for the critically ill. We need a drug available for kids who are unable to take oral therapy, and for treatment of oseltamivir-resistant strains,” he said, adding that the current findings suggest that IVZ – with dose selection based on age, weight, and renal function – is a suitable treatment option for such patients.
“In conclusion, what we saw in this open-label trial was that the dose selection that we utilized gave us the kind of exposure we’d expect, and it seems it was an appropriate way to approach pediatric patients,” he said. “There wasn’t any safety signal attributable to the drug, and the overall pattern was more that of serious influenza, rather than of drug exposure.”
Dr. Blumer reported receiving research support from GlaxoSmithKline, which sponsored the study.
NEW ORLEANS – The investigational intravenous formulation of the neuraminidase inhibitor zanamivir appears to be a safe influenza treatment for hospitalized children and adolescents at high risk of complications who can’t tolerate enteral therapy, according to findings from an open-label, multicenter, phase II study.
In 71 such patients with laboratory-confirmed flu, who presented within 7 days of illness onset and who received intravenous zanamivir (IVZ) for 5-10 days, 72% experienced adverse events (AEs), 21% experienced serious adverse events, and 5 deaths occurred, but none were considered by the investigators to be attributable to IVZ, Jeffrey Blumer, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Rather, the adverse events were “fairly diverse. ... the kinds of things normally seen in critically ill pediatric populations,” he said.
The patients, who had a mean age of 7 years, were treated with IVZ doses selected to provide exposures comparable to 600 mg in adults – a dosage shown in prior studies to be safe and well-tolerated in adults. Patients aged 6 months to under age 6 years received twice-daily doses of 14 mg/kg, and those aged 6 years to less than 18 years received twice-daily doses of 12 mg/kg, not to exceed 600 mg. Doses were adjusted for renal function.
Patients were enrolled from five countries, and most (69%) had received prior treatment with oseltamivir. More than half (56%) had chronic medical conditions.
The median time from symptom onset to IVZ treatment was 4 days, Dr. Blumer of the University of Toledo (Ohio) said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Infiltrate on chest x-ray was seen in 59% of patients, mechanical ventilation was required in 34% of patients, and extracorporeal membrane oxygenation was required in 6% of patients. Treatment in the intensive care unit was required in 65% of patients, and cumulative mortality was 4% at 14 days, and 7% at 28 days.
“Overall, the [IVZ] exposure and then the elimination profiles were consistent across the entire age cohort – unusual for most drugs, but it seemed to hold true, which makes zanamivir a lot easier for us to work with in pediatrics,” Dr. Blumer said.
While the numbers are small, exposure and response delineation didn’t seem to be impacted by mechanical ventilation, by extracorporeal membrane oxygenation, or by continuous renal replacement therapy, which is a good sign, he noted.
“So we generally had good, consistent experience here. ... Overall, 64 of the 71 patients survived, got better, left the ICU, and left the hospital,” Dr. Blumer said.
Of note, a treatment-emergent resistance substitution, E119G, was detected in a day 5 H1N1 isolate from an immunocompetent patient who improved clinically while on IVZ, he said, adding that no phenotype data were available as the sample could not be cultured.
The findings are important, because while zanamivir is currently labeled for patients older than 7 years, and the intravenous formulation currently in development has been shown to be safe for adults, there is a critical unmet need for an effective parenteral treatment for severe flu in children at high risk of complications who cannot tolerate enteral therapy.
“We need a drug that is available for the critically ill. We need a drug available for kids who are unable to take oral therapy, and for treatment of oseltamivir-resistant strains,” he said, adding that the current findings suggest that IVZ – with dose selection based on age, weight, and renal function – is a suitable treatment option for such patients.
“In conclusion, what we saw in this open-label trial was that the dose selection that we utilized gave us the kind of exposure we’d expect, and it seems it was an appropriate way to approach pediatric patients,” he said. “There wasn’t any safety signal attributable to the drug, and the overall pattern was more that of serious influenza, rather than of drug exposure.”
Dr. Blumer reported receiving research support from GlaxoSmithKline, which sponsored the study.
NEW ORLEANS – The investigational intravenous formulation of the neuraminidase inhibitor zanamivir appears to be a safe influenza treatment for hospitalized children and adolescents at high risk of complications who can’t tolerate enteral therapy, according to findings from an open-label, multicenter, phase II study.
In 71 such patients with laboratory-confirmed flu, who presented within 7 days of illness onset and who received intravenous zanamivir (IVZ) for 5-10 days, 72% experienced adverse events (AEs), 21% experienced serious adverse events, and 5 deaths occurred, but none were considered by the investigators to be attributable to IVZ, Jeffrey Blumer, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Rather, the adverse events were “fairly diverse. ... the kinds of things normally seen in critically ill pediatric populations,” he said.
The patients, who had a mean age of 7 years, were treated with IVZ doses selected to provide exposures comparable to 600 mg in adults – a dosage shown in prior studies to be safe and well-tolerated in adults. Patients aged 6 months to under age 6 years received twice-daily doses of 14 mg/kg, and those aged 6 years to less than 18 years received twice-daily doses of 12 mg/kg, not to exceed 600 mg. Doses were adjusted for renal function.
Patients were enrolled from five countries, and most (69%) had received prior treatment with oseltamivir. More than half (56%) had chronic medical conditions.
The median time from symptom onset to IVZ treatment was 4 days, Dr. Blumer of the University of Toledo (Ohio) said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Infiltrate on chest x-ray was seen in 59% of patients, mechanical ventilation was required in 34% of patients, and extracorporeal membrane oxygenation was required in 6% of patients. Treatment in the intensive care unit was required in 65% of patients, and cumulative mortality was 4% at 14 days, and 7% at 28 days.
“Overall, the [IVZ] exposure and then the elimination profiles were consistent across the entire age cohort – unusual for most drugs, but it seemed to hold true, which makes zanamivir a lot easier for us to work with in pediatrics,” Dr. Blumer said.
While the numbers are small, exposure and response delineation didn’t seem to be impacted by mechanical ventilation, by extracorporeal membrane oxygenation, or by continuous renal replacement therapy, which is a good sign, he noted.
“So we generally had good, consistent experience here. ... Overall, 64 of the 71 patients survived, got better, left the ICU, and left the hospital,” Dr. Blumer said.
Of note, a treatment-emergent resistance substitution, E119G, was detected in a day 5 H1N1 isolate from an immunocompetent patient who improved clinically while on IVZ, he said, adding that no phenotype data were available as the sample could not be cultured.
The findings are important, because while zanamivir is currently labeled for patients older than 7 years, and the intravenous formulation currently in development has been shown to be safe for adults, there is a critical unmet need for an effective parenteral treatment for severe flu in children at high risk of complications who cannot tolerate enteral therapy.
“We need a drug that is available for the critically ill. We need a drug available for kids who are unable to take oral therapy, and for treatment of oseltamivir-resistant strains,” he said, adding that the current findings suggest that IVZ – with dose selection based on age, weight, and renal function – is a suitable treatment option for such patients.
“In conclusion, what we saw in this open-label trial was that the dose selection that we utilized gave us the kind of exposure we’d expect, and it seems it was an appropriate way to approach pediatric patients,” he said. “There wasn’t any safety signal attributable to the drug, and the overall pattern was more that of serious influenza, rather than of drug exposure.”
Dr. Blumer reported receiving research support from GlaxoSmithKline, which sponsored the study.
AT ID WEEK 2016
Key clinical point:
Major finding: A total of 72% of patients experienced adverse events and 21% experienced serious adverse events, but none were considered by the investigators to be attributable to intravenous zanamivir.
Data source: An open-label, multicenter, phase II study of 71 children with laboratory-confirmed influenza.
Disclosures: Dr. Blumer reported receiving research support from GlaxoSmithKline, which sponsored the study.
Behavioral interventions durably reduced inappropriate antibiotic prescribing
NEW ORLEANS – The benefits of an 18-month behavioral intervention to reduce inappropriate antibiotic prescribing in the primary care setting were maintained 18 months after the intervention ended, according to follow-up data from a cluster randomized clinical trial.
During the 18-month intervention period, physicians at 47 adult and pediatric practices that participated in the trial, which compared three behavioral interventions and intervention combinations, significantly reduced their inappropriate prescribing.
After 18 months, the results were durable – and particularly so in the groups that received interventions that used “social motivation,” Jeffrey Linder, MD, of Brigham & Women’s Hospital and Harvard Medical School, Boston, reported at an annual scientific meeting on infectious diseases.
A total of 16,959 antibiotic-inappropriate visits (visits for nonspecific upper respiratory tract infections, acute bronchitis, and influenza) were made to 248 clinicians during the 18-month intervention period, and 3,192 such visits were made to 224 clinicians during the postintervention period (JAMA. 2016 Feb 9;315[6]:562-70).
The interventions included “suggested alternatives,” which was an electronic health record-based approach that prompted the prescriber to answer whether a prescription was for an acute respiratory infection. A “yes” answer resulted in the prescriber receiving information about appropriate prescribing, along with a list of “easy nonantibiotic alternatives,” Dr. Linder explained, noting that the interventions involved “trying to make it easy to do the right thing.”
An “accountable justification” intervention used a similar process, but rather than suggesting alternative options, the program asked the prescriber to input a “tweet-length justification” of the prescription. The justification was then entered into the patient’s chart.
The third intervention involved “peer comparison.” Prescribers received monthly e-mail feedback regarding how their prescribing stacked up to that of their peers – specifically noting whether they were or were not “top performers.”
Some of the groups in the trial received combinations of these interventions, but the follow-up analysis showed that the latter two approaches, which involved “social motivation,” had the most durable effects.
For example, the inappropriate antibiotic prescribing rate for those in the “accountable justification” group decreased from 23.2% to 5.2% at the end of the 18-month intervention period (absolute difference, -18.1%) and increased to 9% at the end of follow-up.
The inappropriate prescribing rate decreased from about 20% to about 4% in the “peer comparison” group at the end of the intervention period (absolute difference of -16.3%), then increased to 5% at the end of follow-up, Dr. Linder said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“The statistically best player here – the peer comparison group – went from 20% to 4% to 5%, so it only went back up 1% even after we turned the intervention off for 18 months,” he said.
Antibiotics often are inappropriately prescribed for acute respiratory infections in primary care. Such infections – including colds, sinusitis, strep throat, nonstrep pharyngitis, acute bronchitis, and influenza – make up only 10% of all ambulatory visits in the United States, but they account for 44% of all antibiotic prescribing, Dr. Linder said.
An estimated 50% of antibiotic prescriptions for acute respiratory infections are inappropriate, he added, noting that little success has been achieved with prior antibiotic stewardship efforts that focused largely on clinician education.
“So, we tried to tackle it a bit differently,” he said. “We saw a persistent significant change in antibiotic prescribing in the peer comparison intervention group. ... I would say that interventions that take advantage of social motivation appear to be effective or persistent.”
Dr. Linder reported having no relevant disclosures.
NEW ORLEANS – The benefits of an 18-month behavioral intervention to reduce inappropriate antibiotic prescribing in the primary care setting were maintained 18 months after the intervention ended, according to follow-up data from a cluster randomized clinical trial.
During the 18-month intervention period, physicians at 47 adult and pediatric practices that participated in the trial, which compared three behavioral interventions and intervention combinations, significantly reduced their inappropriate prescribing.
After 18 months, the results were durable – and particularly so in the groups that received interventions that used “social motivation,” Jeffrey Linder, MD, of Brigham & Women’s Hospital and Harvard Medical School, Boston, reported at an annual scientific meeting on infectious diseases.
A total of 16,959 antibiotic-inappropriate visits (visits for nonspecific upper respiratory tract infections, acute bronchitis, and influenza) were made to 248 clinicians during the 18-month intervention period, and 3,192 such visits were made to 224 clinicians during the postintervention period (JAMA. 2016 Feb 9;315[6]:562-70).
The interventions included “suggested alternatives,” which was an electronic health record-based approach that prompted the prescriber to answer whether a prescription was for an acute respiratory infection. A “yes” answer resulted in the prescriber receiving information about appropriate prescribing, along with a list of “easy nonantibiotic alternatives,” Dr. Linder explained, noting that the interventions involved “trying to make it easy to do the right thing.”
An “accountable justification” intervention used a similar process, but rather than suggesting alternative options, the program asked the prescriber to input a “tweet-length justification” of the prescription. The justification was then entered into the patient’s chart.
The third intervention involved “peer comparison.” Prescribers received monthly e-mail feedback regarding how their prescribing stacked up to that of their peers – specifically noting whether they were or were not “top performers.”
Some of the groups in the trial received combinations of these interventions, but the follow-up analysis showed that the latter two approaches, which involved “social motivation,” had the most durable effects.
For example, the inappropriate antibiotic prescribing rate for those in the “accountable justification” group decreased from 23.2% to 5.2% at the end of the 18-month intervention period (absolute difference, -18.1%) and increased to 9% at the end of follow-up.
The inappropriate prescribing rate decreased from about 20% to about 4% in the “peer comparison” group at the end of the intervention period (absolute difference of -16.3%), then increased to 5% at the end of follow-up, Dr. Linder said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“The statistically best player here – the peer comparison group – went from 20% to 4% to 5%, so it only went back up 1% even after we turned the intervention off for 18 months,” he said.
Antibiotics often are inappropriately prescribed for acute respiratory infections in primary care. Such infections – including colds, sinusitis, strep throat, nonstrep pharyngitis, acute bronchitis, and influenza – make up only 10% of all ambulatory visits in the United States, but they account for 44% of all antibiotic prescribing, Dr. Linder said.
An estimated 50% of antibiotic prescriptions for acute respiratory infections are inappropriate, he added, noting that little success has been achieved with prior antibiotic stewardship efforts that focused largely on clinician education.
“So, we tried to tackle it a bit differently,” he said. “We saw a persistent significant change in antibiotic prescribing in the peer comparison intervention group. ... I would say that interventions that take advantage of social motivation appear to be effective or persistent.”
Dr. Linder reported having no relevant disclosures.
NEW ORLEANS – The benefits of an 18-month behavioral intervention to reduce inappropriate antibiotic prescribing in the primary care setting were maintained 18 months after the intervention ended, according to follow-up data from a cluster randomized clinical trial.
During the 18-month intervention period, physicians at 47 adult and pediatric practices that participated in the trial, which compared three behavioral interventions and intervention combinations, significantly reduced their inappropriate prescribing.
After 18 months, the results were durable – and particularly so in the groups that received interventions that used “social motivation,” Jeffrey Linder, MD, of Brigham & Women’s Hospital and Harvard Medical School, Boston, reported at an annual scientific meeting on infectious diseases.
A total of 16,959 antibiotic-inappropriate visits (visits for nonspecific upper respiratory tract infections, acute bronchitis, and influenza) were made to 248 clinicians during the 18-month intervention period, and 3,192 such visits were made to 224 clinicians during the postintervention period (JAMA. 2016 Feb 9;315[6]:562-70).
The interventions included “suggested alternatives,” which was an electronic health record-based approach that prompted the prescriber to answer whether a prescription was for an acute respiratory infection. A “yes” answer resulted in the prescriber receiving information about appropriate prescribing, along with a list of “easy nonantibiotic alternatives,” Dr. Linder explained, noting that the interventions involved “trying to make it easy to do the right thing.”
An “accountable justification” intervention used a similar process, but rather than suggesting alternative options, the program asked the prescriber to input a “tweet-length justification” of the prescription. The justification was then entered into the patient’s chart.
The third intervention involved “peer comparison.” Prescribers received monthly e-mail feedback regarding how their prescribing stacked up to that of their peers – specifically noting whether they were or were not “top performers.”
Some of the groups in the trial received combinations of these interventions, but the follow-up analysis showed that the latter two approaches, which involved “social motivation,” had the most durable effects.
For example, the inappropriate antibiotic prescribing rate for those in the “accountable justification” group decreased from 23.2% to 5.2% at the end of the 18-month intervention period (absolute difference, -18.1%) and increased to 9% at the end of follow-up.
The inappropriate prescribing rate decreased from about 20% to about 4% in the “peer comparison” group at the end of the intervention period (absolute difference of -16.3%), then increased to 5% at the end of follow-up, Dr. Linder said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“The statistically best player here – the peer comparison group – went from 20% to 4% to 5%, so it only went back up 1% even after we turned the intervention off for 18 months,” he said.
Antibiotics often are inappropriately prescribed for acute respiratory infections in primary care. Such infections – including colds, sinusitis, strep throat, nonstrep pharyngitis, acute bronchitis, and influenza – make up only 10% of all ambulatory visits in the United States, but they account for 44% of all antibiotic prescribing, Dr. Linder said.
An estimated 50% of antibiotic prescriptions for acute respiratory infections are inappropriate, he added, noting that little success has been achieved with prior antibiotic stewardship efforts that focused largely on clinician education.
“So, we tried to tackle it a bit differently,” he said. “We saw a persistent significant change in antibiotic prescribing in the peer comparison intervention group. ... I would say that interventions that take advantage of social motivation appear to be effective or persistent.”
Dr. Linder reported having no relevant disclosures.
Key clinical point: The benefits of an 18-month behavioral intervention to reduce inappropriate antibiotic prescribing in the primary care setting were maintained 18 months after the intervention ended, according to follow-up data from a cluster randomized clinical trial.
Major finding: Inappropriate antibiotic prescribing increased only slightly, from 4% to 5%, during 18 months of follow-up in the “peer comparison” group.
Data source: Follow-up of a cluster randomized, controlled clinical trial involving nearly 3,200 patient visits with 224 clinicians.
Disclosures: Dr. Linder reported having no disclosures.
In HIV, omega-3s significantly reduced triglycerides, CRP
NEW ORLEANS – Daily supplementation with high-dose omega-3 fatty acids significantly slashed levels of triglycerides and C-reactive protein (CRP) among people with HIV infection at 2 years, according to a randomized study.
“This is the longest randomized, controlled trial to date of high-dose omega-3 in the HIV infected to evaluate long-term effects on lipids, inflammation, and vascular function,” Gretchen Volpe, MD, said at an annual scientific meeting on infectious diseases. Prior studies were limited to 24 weeks or fewer of omega-3 supplementation, she added.
The trial is part of a bigger trend, one where investigators strive to improve duration and quality of life for people living with HIV/AIDS because of the field’s success in managing HIV infection itself.
“Cardiovascular disease is prevalent in persons with HIV,” said Dr. Volpe of Tufts Medical Center in Boston. “HIV increases cardiovascular disease through several pathways – including dyslipidemia, chronic inflammation, and vascular dysfunction.” Both HIV infection itself as well as antiretroviral therapy can have atherogenic effects on vasculature, she added.
Omega-3 fatty acids have been shown to reduce triglycerides in HIV-infected and non–HIV infected people, and they may reduce inflammation by decreasing the inflammatory mediator arachidonic acid, Dr. Volpe said.
She and her colleagues enrolled HIV-infected adults on stable antiretroviral therapy with fasting triglycerides between 150 mg/dL and 2,500 mg/dL at baseline. They randomized 43 people to 4 g omega-3 (Lovaza) daily, and another 40 people to placebo in an intent-to-treat analysis.
The mean age was 51 years, 21% were women, and there were no significant differences between groups at baseline on lipid parameters or statin use. Most patients (95%) were virologically suppressed, with a mean CD4+ count of 648 cells/mcL. The mean duration of HIV infection was 16 years.
The median decrease in triglycerides at 24 months was 68 mg/dL in the omega-3 group, compared with 22 mg/dL in the placebo group, a significant difference (P = .041). Another primary outcome, change in C-reactive protein as an indication of systemic inflammation, decreased 0.3 mg/L in treated participants, versus an increase of 0.6 mg/L in the placebo group. That difference also was statistically significant (P = .008).
In contrast, there were no significant differences in HDL-C changes, arterial stiffness, or brachial artery reactivity between groups at 2 years. Serious adverse event rates did not differ, either, Dr. Volpe reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society
“Adherence even over a 2-year trial is feasible, and efficacy may increase over time – we noted our 24-month data were more statistically significant than our 12-month data,” Dr. Volpe observed. Omega-3 fatty acid supplementation is well tolerated with limited side effects, she added. “Omega-3 fatty acid supplementation [also] may reduce inflammation as measured by CRP, even for those whose CRP was in the normal range at baseline.”
Total cholesterol did not significantly differ between groups at any time point, Dr. Volpe noted. “But we noticed a trend toward greater reduction in total cholesterol in the treatment group at 12 months and 24 months. There we no differences at any time point between groups in LDL cholesterol, which allays some concerns that fatty acids might increase LDL.”
The use of the prescription formulation of omega-3 fatty acids could be a limitation of the study, Dr. Volpe said, because not all people at risk may be able to access or afford it.
During a question session after the presentation, a meeting attendee asked about over-the-counter formulations that she could recommend to her patients. “We used the high dose, because some previous studies showed a dose-dependent response,” Dr. Volpe responded. “This was a purified formulation, so we could know what we were giving. ... I don’t know how to solve that problem in real life, but maybe use the best preparation that you are most familiar with.”
Another attendee asked about any differences between groups in statin use, alcohol consumption, or smoking. “We had about 30% statin users in either arm,” Dr. Volpe replied. “Some studies have shown that statins reduce or eliminate the effects of omega-3s, whereas other studies have shown that high-dose, high-efficacy statins improve the effects of omega-3s. Whatever the effect was, it was well distributed between groups.” Smoking and drinking rates did not significantly different between groups, she noted.
In a video interview at the meeting, Dr. Volpe discussed the study and its findings.
Dr. Volpe had no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Daily supplementation with high-dose omega-3 fatty acids significantly slashed levels of triglycerides and C-reactive protein (CRP) among people with HIV infection at 2 years, according to a randomized study.
“This is the longest randomized, controlled trial to date of high-dose omega-3 in the HIV infected to evaluate long-term effects on lipids, inflammation, and vascular function,” Gretchen Volpe, MD, said at an annual scientific meeting on infectious diseases. Prior studies were limited to 24 weeks or fewer of omega-3 supplementation, she added.
The trial is part of a bigger trend, one where investigators strive to improve duration and quality of life for people living with HIV/AIDS because of the field’s success in managing HIV infection itself.
“Cardiovascular disease is prevalent in persons with HIV,” said Dr. Volpe of Tufts Medical Center in Boston. “HIV increases cardiovascular disease through several pathways – including dyslipidemia, chronic inflammation, and vascular dysfunction.” Both HIV infection itself as well as antiretroviral therapy can have atherogenic effects on vasculature, she added.
Omega-3 fatty acids have been shown to reduce triglycerides in HIV-infected and non–HIV infected people, and they may reduce inflammation by decreasing the inflammatory mediator arachidonic acid, Dr. Volpe said.
She and her colleagues enrolled HIV-infected adults on stable antiretroviral therapy with fasting triglycerides between 150 mg/dL and 2,500 mg/dL at baseline. They randomized 43 people to 4 g omega-3 (Lovaza) daily, and another 40 people to placebo in an intent-to-treat analysis.
The mean age was 51 years, 21% were women, and there were no significant differences between groups at baseline on lipid parameters or statin use. Most patients (95%) were virologically suppressed, with a mean CD4+ count of 648 cells/mcL. The mean duration of HIV infection was 16 years.
The median decrease in triglycerides at 24 months was 68 mg/dL in the omega-3 group, compared with 22 mg/dL in the placebo group, a significant difference (P = .041). Another primary outcome, change in C-reactive protein as an indication of systemic inflammation, decreased 0.3 mg/L in treated participants, versus an increase of 0.6 mg/L in the placebo group. That difference also was statistically significant (P = .008).
In contrast, there were no significant differences in HDL-C changes, arterial stiffness, or brachial artery reactivity between groups at 2 years. Serious adverse event rates did not differ, either, Dr. Volpe reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society
“Adherence even over a 2-year trial is feasible, and efficacy may increase over time – we noted our 24-month data were more statistically significant than our 12-month data,” Dr. Volpe observed. Omega-3 fatty acid supplementation is well tolerated with limited side effects, she added. “Omega-3 fatty acid supplementation [also] may reduce inflammation as measured by CRP, even for those whose CRP was in the normal range at baseline.”
Total cholesterol did not significantly differ between groups at any time point, Dr. Volpe noted. “But we noticed a trend toward greater reduction in total cholesterol in the treatment group at 12 months and 24 months. There we no differences at any time point between groups in LDL cholesterol, which allays some concerns that fatty acids might increase LDL.”
The use of the prescription formulation of omega-3 fatty acids could be a limitation of the study, Dr. Volpe said, because not all people at risk may be able to access or afford it.
During a question session after the presentation, a meeting attendee asked about over-the-counter formulations that she could recommend to her patients. “We used the high dose, because some previous studies showed a dose-dependent response,” Dr. Volpe responded. “This was a purified formulation, so we could know what we were giving. ... I don’t know how to solve that problem in real life, but maybe use the best preparation that you are most familiar with.”
Another attendee asked about any differences between groups in statin use, alcohol consumption, or smoking. “We had about 30% statin users in either arm,” Dr. Volpe replied. “Some studies have shown that statins reduce or eliminate the effects of omega-3s, whereas other studies have shown that high-dose, high-efficacy statins improve the effects of omega-3s. Whatever the effect was, it was well distributed between groups.” Smoking and drinking rates did not significantly different between groups, she noted.
In a video interview at the meeting, Dr. Volpe discussed the study and its findings.
Dr. Volpe had no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Daily supplementation with high-dose omega-3 fatty acids significantly slashed levels of triglycerides and C-reactive protein (CRP) among people with HIV infection at 2 years, according to a randomized study.
“This is the longest randomized, controlled trial to date of high-dose omega-3 in the HIV infected to evaluate long-term effects on lipids, inflammation, and vascular function,” Gretchen Volpe, MD, said at an annual scientific meeting on infectious diseases. Prior studies were limited to 24 weeks or fewer of omega-3 supplementation, she added.
The trial is part of a bigger trend, one where investigators strive to improve duration and quality of life for people living with HIV/AIDS because of the field’s success in managing HIV infection itself.
“Cardiovascular disease is prevalent in persons with HIV,” said Dr. Volpe of Tufts Medical Center in Boston. “HIV increases cardiovascular disease through several pathways – including dyslipidemia, chronic inflammation, and vascular dysfunction.” Both HIV infection itself as well as antiretroviral therapy can have atherogenic effects on vasculature, she added.
Omega-3 fatty acids have been shown to reduce triglycerides in HIV-infected and non–HIV infected people, and they may reduce inflammation by decreasing the inflammatory mediator arachidonic acid, Dr. Volpe said.
She and her colleagues enrolled HIV-infected adults on stable antiretroviral therapy with fasting triglycerides between 150 mg/dL and 2,500 mg/dL at baseline. They randomized 43 people to 4 g omega-3 (Lovaza) daily, and another 40 people to placebo in an intent-to-treat analysis.
The mean age was 51 years, 21% were women, and there were no significant differences between groups at baseline on lipid parameters or statin use. Most patients (95%) were virologically suppressed, with a mean CD4+ count of 648 cells/mcL. The mean duration of HIV infection was 16 years.
The median decrease in triglycerides at 24 months was 68 mg/dL in the omega-3 group, compared with 22 mg/dL in the placebo group, a significant difference (P = .041). Another primary outcome, change in C-reactive protein as an indication of systemic inflammation, decreased 0.3 mg/L in treated participants, versus an increase of 0.6 mg/L in the placebo group. That difference also was statistically significant (P = .008).
In contrast, there were no significant differences in HDL-C changes, arterial stiffness, or brachial artery reactivity between groups at 2 years. Serious adverse event rates did not differ, either, Dr. Volpe reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society
“Adherence even over a 2-year trial is feasible, and efficacy may increase over time – we noted our 24-month data were more statistically significant than our 12-month data,” Dr. Volpe observed. Omega-3 fatty acid supplementation is well tolerated with limited side effects, she added. “Omega-3 fatty acid supplementation [also] may reduce inflammation as measured by CRP, even for those whose CRP was in the normal range at baseline.”
Total cholesterol did not significantly differ between groups at any time point, Dr. Volpe noted. “But we noticed a trend toward greater reduction in total cholesterol in the treatment group at 12 months and 24 months. There we no differences at any time point between groups in LDL cholesterol, which allays some concerns that fatty acids might increase LDL.”
The use of the prescription formulation of omega-3 fatty acids could be a limitation of the study, Dr. Volpe said, because not all people at risk may be able to access or afford it.
During a question session after the presentation, a meeting attendee asked about over-the-counter formulations that she could recommend to her patients. “We used the high dose, because some previous studies showed a dose-dependent response,” Dr. Volpe responded. “This was a purified formulation, so we could know what we were giving. ... I don’t know how to solve that problem in real life, but maybe use the best preparation that you are most familiar with.”
Another attendee asked about any differences between groups in statin use, alcohol consumption, or smoking. “We had about 30% statin users in either arm,” Dr. Volpe replied. “Some studies have shown that statins reduce or eliminate the effects of omega-3s, whereas other studies have shown that high-dose, high-efficacy statins improve the effects of omega-3s. Whatever the effect was, it was well distributed between groups.” Smoking and drinking rates did not significantly different between groups, she noted.
In a video interview at the meeting, Dr. Volpe discussed the study and its findings.
Dr. Volpe had no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Key clinical point: Two years of high-dose omega-3 supplementation significantly reduced triglycerides and C-reactive protein levels in people with HIV infection.
Major finding: Triglyceride levels over 24 months dropped a median 68 mg/dL with omega-3 treatment, compared with 22 mg/dL with placebo. Similarly, C-reactive protein levels decreased 0.3 mg/L in treated patients, compared with an increase of 0.6 mg/mL in the placebo group.
Data source: A randomized, placebo-controlled trial of 83 patients.
Disclosures: Dr. Volpe had no relevant disclosures.