User login
The dream of family practice began more than 6 decades ago with a movement toward personal physicians who have “… the feeling of warm personal regard and concern of doctor for patient, the feeling that the doctor treats people, not illnesses ….” The personal family physician helps patients “… not because of the interesting medical problems they may present but because they are human beings in need of help.”1 One of the most influential founders of family medicine, Dr. Gayle Stephens, expounded on this idea in a series of essays that tapped into the intellectual, philosophical, historical, and moral underpinnings of our discipline.2
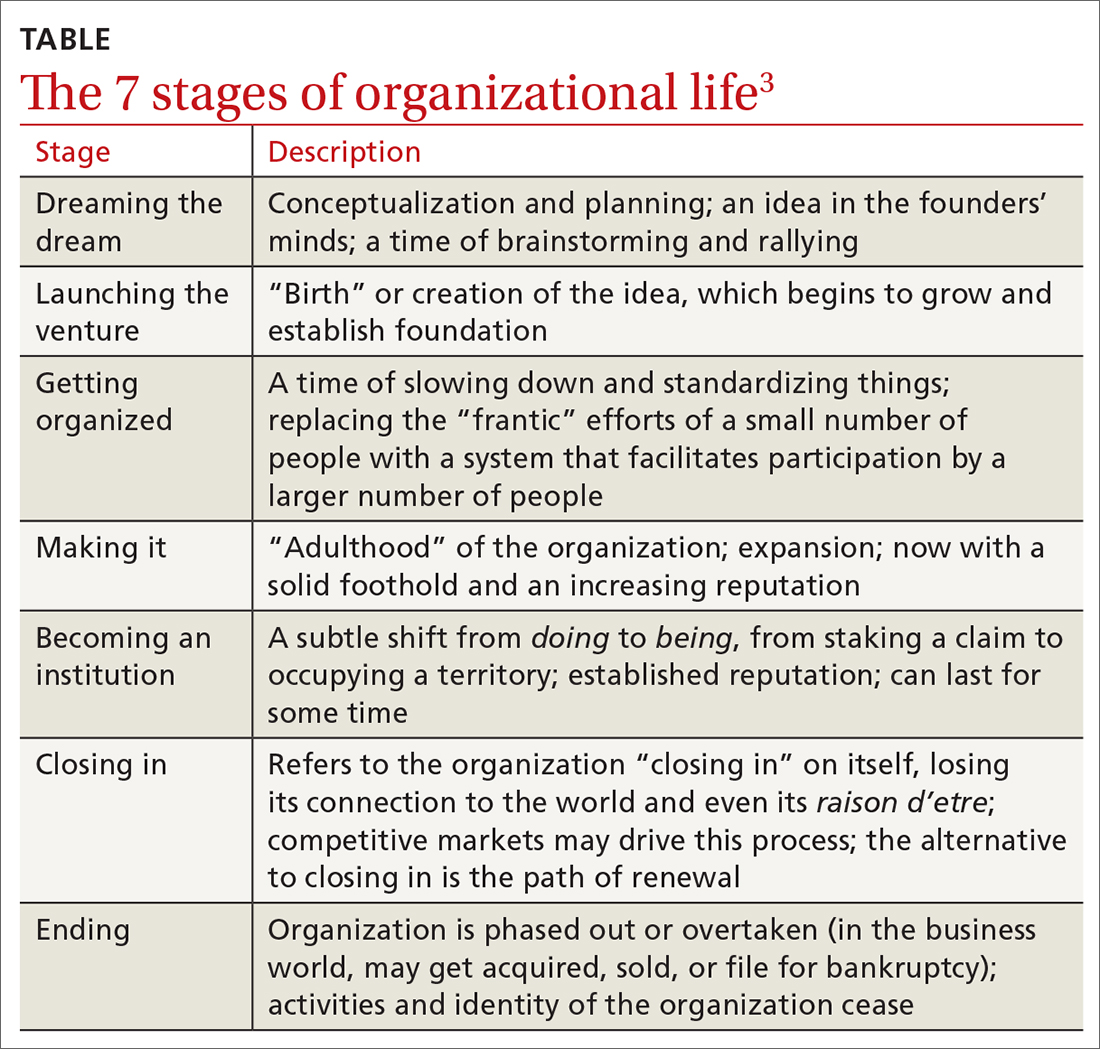
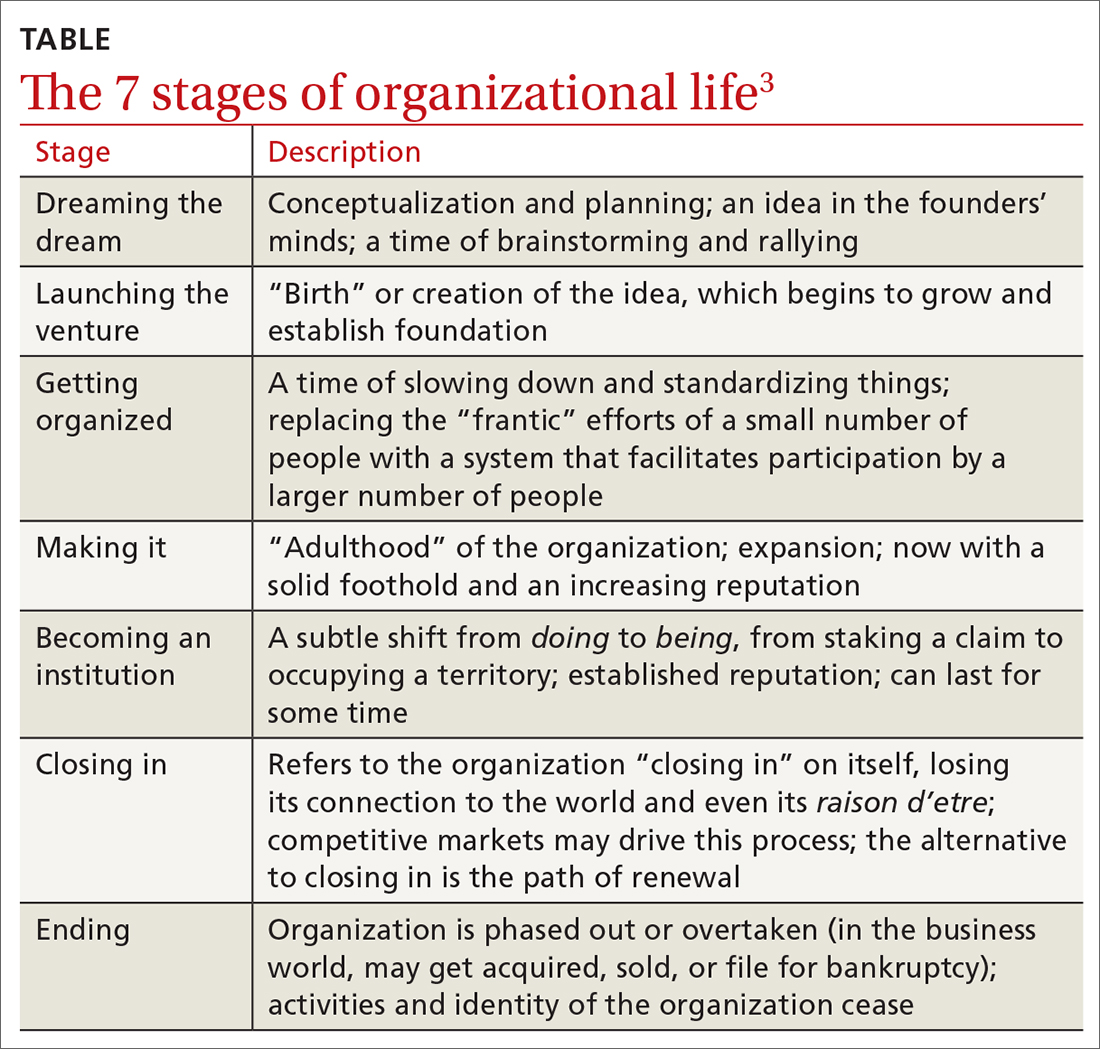
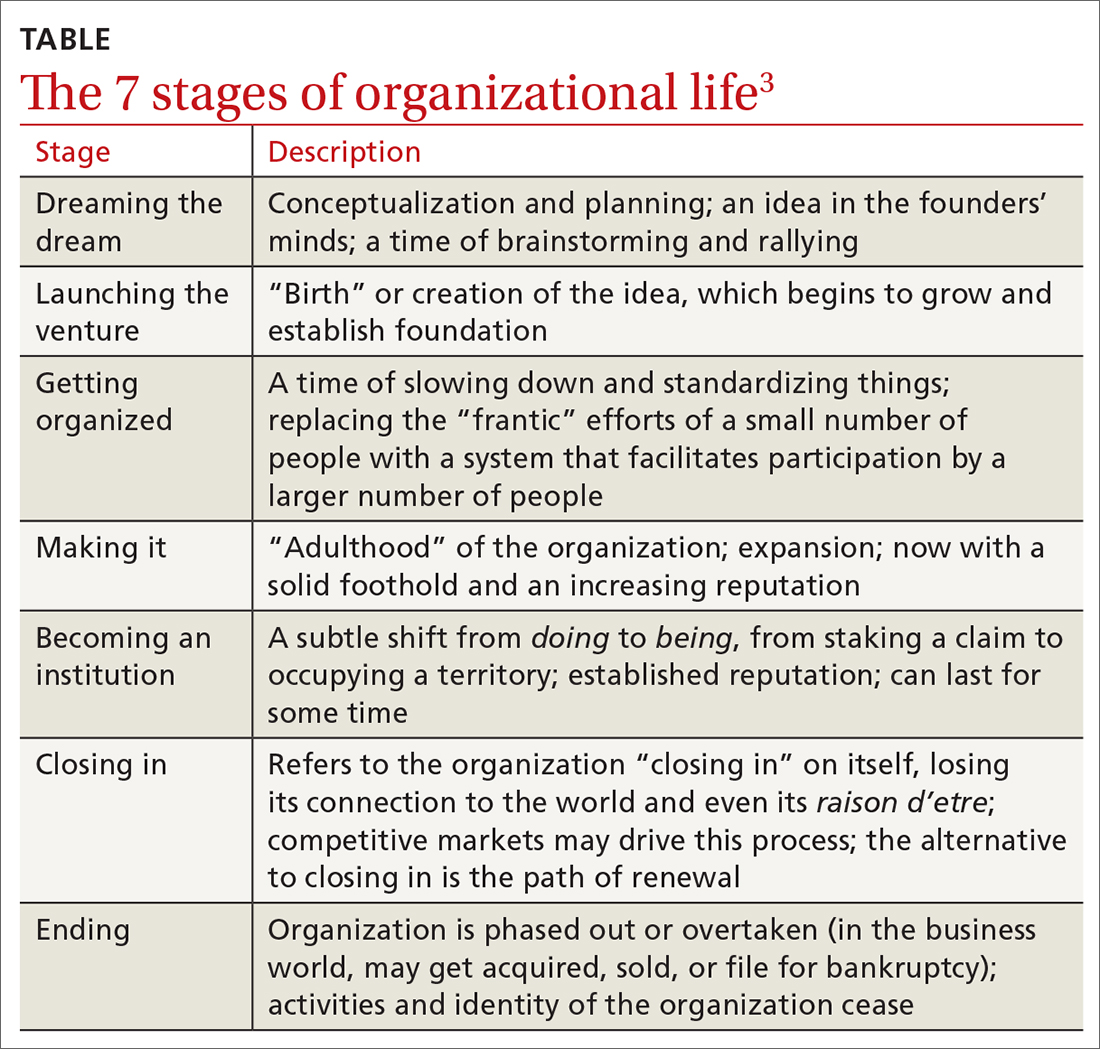
Following the dream and the birth of family medicine—like any organization—its lifecycle can be envisioned as proceeding through the rest of the 7 stages of organizational life (TABLE).3 Now allow me to give you some numbers. There are more than 118,000 family physicians in the United States, 784 family medicine residencies filled by 4530 medical school graduates, more than 150 departments of family medicine, multiple national family medicine organizations, and even a World Organization of Family Doctors.4,5 The American Board of Family Medicine is the second largest medical specialty board in the country. Family doctors make up nearly 40% of our total primary care workforce.6 We launched the venture, got organized, made it. We are an institution.
The threat at the institution stage is that we are on the precipice of “closing in.” Many factors are driving this stage: commoditization in health care, market influences and competition for patients, alternative primary care models, erosion of the patient-physician relationship (partly driven by technology), narrowing scope of care, clinician burnout, and the challenges of implementing value-based care, to name a few. You see what comes next in the TABLE.3 The good news is that there is an alternative to the “natural” progression to the ending stage: the path of renewal.3
In the lifecycle of an organization, the path of renewal starts the cycle anew, with dreaming the dream. I recently had the opportunity to visit Singapore to learn about their health system. Singapore is one of the wealthiest countries in the world. I was impressed with their many innovations, including technological ones, as well as new models of care. However, I was most impressed that the country is betting big on family medicine. Their Ministry of Health has launched an initiative they are calling Healthier SG.7 The goal is for “all Singaporeans to have a trusted and lifelong relationship with [their] family doctor.” Their dream is to bring personal doctoring to everyone in the country to make Singapore healthier.
While their path of renewal is occurring halfway around the world, here at home, our path of renewal has been ignited over the past several years by the work of the Robert Graham Center; the Keystone Conferences; the American Board of Family Medicine; and the National Academies of Science, Engineering, and Medicine, among others.8-11 These organizations are aligning around re-centering on patient-clinician relationships, measuring what is important, care by interprofessional teams, payment reform, professionalism, health equity, improved information technology, and adherence to the best available evidence. We are working toward the solution shop as opposed to the production line.12 We are indeed dreaming a new dream.
While I write about this renewal, I close with an ending. This is the final issue of The Journal of Family Practice. It marks the end of an era of nearly 50 years of publication. The Journal of Family Practice has left a lasting mark, providing generations of clinicians with evidence-based, practical guidance to help care for patients as well as serving as an important venue for scholarly work by the family medicine community. Although I have had the privilege of serving the discipline as an editor-in-chief for only a brief time, I am grateful I had the opportunity. Most of all, I appreciate being on the journey of family medicine with you, renewing the dream together.
The references for this Editorial are available in the online version of the article at www.mdedge.com/familymedicine.
1. Fox TF. The personal doctor and his relation to the hospital. Observations and reflections on some American experiments in general practice by groups. Lancet. 1960;2:743-760.
2. Stephens, GG. The Intellectual Basis of Family Practice. Winter Publishing and Society of Teachers of Family Medicine; 1982.
3. Bridges W, Bridges S. Managing Transitions: Making the Most of Change. 4th ed. Da Capo Press; 2016.
4. Association of American Medical Colleges. Physician specialty data report. Accessed October 25, 2023. www.aamc.org/data-reports/workforce/data/active-physicians-us-doctor-medicine-us-md-degree-specialty-2019
5. American Academy of Family Physicians. 2023 match results for family medicine. Accessed October 25, 2023. www.aafp.org/students-residents/residency-program-directors/national-resident-matching-program-results.html
6. Robert Graham Center. Primary Care in the US: A Chartbook of Facts and Statistics. Accessed October 25, 2023. www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook2021.pdf
7. Ministry of Health Singapore. What is Healthier SG? Accessed October 25, 2023. www.healthiersg.gov.sg/about/what-is-healthier-sg/
8. The Robert Graham Center. Accessed October 25, 2023. www.graham-center.org/home.html
9. Stange KC. Holding on and letting go: a perspective from the Keystone IV Conference. J Am Board Fam Med. 2016;29:S32-S39.
10. American Board of Family Medicine. Family medicine certification. Accessed October 25, 2023. www.theabfm.org/research-articles/family-medicine-certification?page=1
11. National Academies of Sciences, Engineering, and Medicine. Implementing high-quality primary care. Accessed October 25, 2023. www.nationalacademies.org/our-work/implementing-high-quality-primary-care
12. Sinsky CA, Panzer J. The solution shop and the production line—the case for a frameshift for physician practices. N Engl J Med. 2022;386:2452-2453.
The dream of family practice began more than 6 decades ago with a movement toward personal physicians who have “… the feeling of warm personal regard and concern of doctor for patient, the feeling that the doctor treats people, not illnesses ….” The personal family physician helps patients “… not because of the interesting medical problems they may present but because they are human beings in need of help.”1 One of the most influential founders of family medicine, Dr. Gayle Stephens, expounded on this idea in a series of essays that tapped into the intellectual, philosophical, historical, and moral underpinnings of our discipline.2
Following the dream and the birth of family medicine—like any organization—its lifecycle can be envisioned as proceeding through the rest of the 7 stages of organizational life (TABLE).3 Now allow me to give you some numbers. There are more than 118,000 family physicians in the United States, 784 family medicine residencies filled by 4530 medical school graduates, more than 150 departments of family medicine, multiple national family medicine organizations, and even a World Organization of Family Doctors.4,5 The American Board of Family Medicine is the second largest medical specialty board in the country. Family doctors make up nearly 40% of our total primary care workforce.6 We launched the venture, got organized, made it. We are an institution.
The threat at the institution stage is that we are on the precipice of “closing in.” Many factors are driving this stage: commoditization in health care, market influences and competition for patients, alternative primary care models, erosion of the patient-physician relationship (partly driven by technology), narrowing scope of care, clinician burnout, and the challenges of implementing value-based care, to name a few. You see what comes next in the TABLE.3 The good news is that there is an alternative to the “natural” progression to the ending stage: the path of renewal.3
In the lifecycle of an organization, the path of renewal starts the cycle anew, with dreaming the dream. I recently had the opportunity to visit Singapore to learn about their health system. Singapore is one of the wealthiest countries in the world. I was impressed with their many innovations, including technological ones, as well as new models of care. However, I was most impressed that the country is betting big on family medicine. Their Ministry of Health has launched an initiative they are calling Healthier SG.7 The goal is for “all Singaporeans to have a trusted and lifelong relationship with [their] family doctor.” Their dream is to bring personal doctoring to everyone in the country to make Singapore healthier.
While their path of renewal is occurring halfway around the world, here at home, our path of renewal has been ignited over the past several years by the work of the Robert Graham Center; the Keystone Conferences; the American Board of Family Medicine; and the National Academies of Science, Engineering, and Medicine, among others.8-11 These organizations are aligning around re-centering on patient-clinician relationships, measuring what is important, care by interprofessional teams, payment reform, professionalism, health equity, improved information technology, and adherence to the best available evidence. We are working toward the solution shop as opposed to the production line.12 We are indeed dreaming a new dream.
While I write about this renewal, I close with an ending. This is the final issue of The Journal of Family Practice. It marks the end of an era of nearly 50 years of publication. The Journal of Family Practice has left a lasting mark, providing generations of clinicians with evidence-based, practical guidance to help care for patients as well as serving as an important venue for scholarly work by the family medicine community. Although I have had the privilege of serving the discipline as an editor-in-chief for only a brief time, I am grateful I had the opportunity. Most of all, I appreciate being on the journey of family medicine with you, renewing the dream together.
The references for this Editorial are available in the online version of the article at www.mdedge.com/familymedicine.
The dream of family practice began more than 6 decades ago with a movement toward personal physicians who have “… the feeling of warm personal regard and concern of doctor for patient, the feeling that the doctor treats people, not illnesses ….” The personal family physician helps patients “… not because of the interesting medical problems they may present but because they are human beings in need of help.”1 One of the most influential founders of family medicine, Dr. Gayle Stephens, expounded on this idea in a series of essays that tapped into the intellectual, philosophical, historical, and moral underpinnings of our discipline.2
Following the dream and the birth of family medicine—like any organization—its lifecycle can be envisioned as proceeding through the rest of the 7 stages of organizational life (TABLE).3 Now allow me to give you some numbers. There are more than 118,000 family physicians in the United States, 784 family medicine residencies filled by 4530 medical school graduates, more than 150 departments of family medicine, multiple national family medicine organizations, and even a World Organization of Family Doctors.4,5 The American Board of Family Medicine is the second largest medical specialty board in the country. Family doctors make up nearly 40% of our total primary care workforce.6 We launched the venture, got organized, made it. We are an institution.
The threat at the institution stage is that we are on the precipice of “closing in.” Many factors are driving this stage: commoditization in health care, market influences and competition for patients, alternative primary care models, erosion of the patient-physician relationship (partly driven by technology), narrowing scope of care, clinician burnout, and the challenges of implementing value-based care, to name a few. You see what comes next in the TABLE.3 The good news is that there is an alternative to the “natural” progression to the ending stage: the path of renewal.3
In the lifecycle of an organization, the path of renewal starts the cycle anew, with dreaming the dream. I recently had the opportunity to visit Singapore to learn about their health system. Singapore is one of the wealthiest countries in the world. I was impressed with their many innovations, including technological ones, as well as new models of care. However, I was most impressed that the country is betting big on family medicine. Their Ministry of Health has launched an initiative they are calling Healthier SG.7 The goal is for “all Singaporeans to have a trusted and lifelong relationship with [their] family doctor.” Their dream is to bring personal doctoring to everyone in the country to make Singapore healthier.
While their path of renewal is occurring halfway around the world, here at home, our path of renewal has been ignited over the past several years by the work of the Robert Graham Center; the Keystone Conferences; the American Board of Family Medicine; and the National Academies of Science, Engineering, and Medicine, among others.8-11 These organizations are aligning around re-centering on patient-clinician relationships, measuring what is important, care by interprofessional teams, payment reform, professionalism, health equity, improved information technology, and adherence to the best available evidence. We are working toward the solution shop as opposed to the production line.12 We are indeed dreaming a new dream.
While I write about this renewal, I close with an ending. This is the final issue of The Journal of Family Practice. It marks the end of an era of nearly 50 years of publication. The Journal of Family Practice has left a lasting mark, providing generations of clinicians with evidence-based, practical guidance to help care for patients as well as serving as an important venue for scholarly work by the family medicine community. Although I have had the privilege of serving the discipline as an editor-in-chief for only a brief time, I am grateful I had the opportunity. Most of all, I appreciate being on the journey of family medicine with you, renewing the dream together.
The references for this Editorial are available in the online version of the article at www.mdedge.com/familymedicine.
1. Fox TF. The personal doctor and his relation to the hospital. Observations and reflections on some American experiments in general practice by groups. Lancet. 1960;2:743-760.
2. Stephens, GG. The Intellectual Basis of Family Practice. Winter Publishing and Society of Teachers of Family Medicine; 1982.
3. Bridges W, Bridges S. Managing Transitions: Making the Most of Change. 4th ed. Da Capo Press; 2016.
4. Association of American Medical Colleges. Physician specialty data report. Accessed October 25, 2023. www.aamc.org/data-reports/workforce/data/active-physicians-us-doctor-medicine-us-md-degree-specialty-2019
5. American Academy of Family Physicians. 2023 match results for family medicine. Accessed October 25, 2023. www.aafp.org/students-residents/residency-program-directors/national-resident-matching-program-results.html
6. Robert Graham Center. Primary Care in the US: A Chartbook of Facts and Statistics. Accessed October 25, 2023. www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook2021.pdf
7. Ministry of Health Singapore. What is Healthier SG? Accessed October 25, 2023. www.healthiersg.gov.sg/about/what-is-healthier-sg/
8. The Robert Graham Center. Accessed October 25, 2023. www.graham-center.org/home.html
9. Stange KC. Holding on and letting go: a perspective from the Keystone IV Conference. J Am Board Fam Med. 2016;29:S32-S39.
10. American Board of Family Medicine. Family medicine certification. Accessed October 25, 2023. www.theabfm.org/research-articles/family-medicine-certification?page=1
11. National Academies of Sciences, Engineering, and Medicine. Implementing high-quality primary care. Accessed October 25, 2023. www.nationalacademies.org/our-work/implementing-high-quality-primary-care
12. Sinsky CA, Panzer J. The solution shop and the production line—the case for a frameshift for physician practices. N Engl J Med. 2022;386:2452-2453.
1. Fox TF. The personal doctor and his relation to the hospital. Observations and reflections on some American experiments in general practice by groups. Lancet. 1960;2:743-760.
2. Stephens, GG. The Intellectual Basis of Family Practice. Winter Publishing and Society of Teachers of Family Medicine; 1982.
3. Bridges W, Bridges S. Managing Transitions: Making the Most of Change. 4th ed. Da Capo Press; 2016.
4. Association of American Medical Colleges. Physician specialty data report. Accessed October 25, 2023. www.aamc.org/data-reports/workforce/data/active-physicians-us-doctor-medicine-us-md-degree-specialty-2019
5. American Academy of Family Physicians. 2023 match results for family medicine. Accessed October 25, 2023. www.aafp.org/students-residents/residency-program-directors/national-resident-matching-program-results.html
6. Robert Graham Center. Primary Care in the US: A Chartbook of Facts and Statistics. Accessed October 25, 2023. www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook2021.pdf
7. Ministry of Health Singapore. What is Healthier SG? Accessed October 25, 2023. www.healthiersg.gov.sg/about/what-is-healthier-sg/
8. The Robert Graham Center. Accessed October 25, 2023. www.graham-center.org/home.html
9. Stange KC. Holding on and letting go: a perspective from the Keystone IV Conference. J Am Board Fam Med. 2016;29:S32-S39.
10. American Board of Family Medicine. Family medicine certification. Accessed October 25, 2023. www.theabfm.org/research-articles/family-medicine-certification?page=1
11. National Academies of Sciences, Engineering, and Medicine. Implementing high-quality primary care. Accessed October 25, 2023. www.nationalacademies.org/our-work/implementing-high-quality-primary-care
12. Sinsky CA, Panzer J. The solution shop and the production line—the case for a frameshift for physician practices. N Engl J Med. 2022;386:2452-2453.
