User login
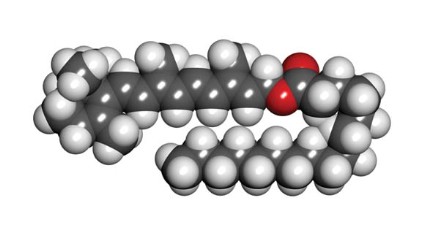
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.