User login
SAN ANTONIO – Current guidelines on community-acquired pneumonia recommend penicillin, amoxicillin, or ampicillin as first-line treatment in children with CAP.
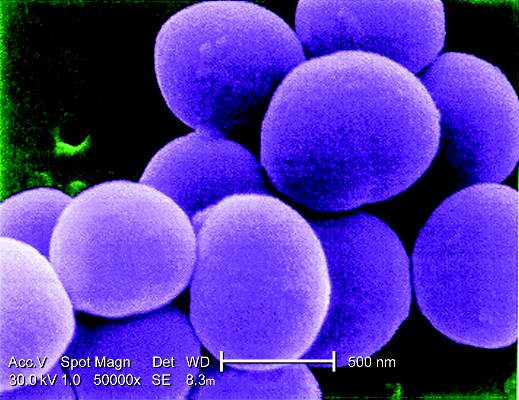
However, a small minority will have Staphylococcus aureus infections not treatable with these antibiotics, raising some concern about how many of these cases might be missed.
At the Pediatric Hospital Medicine 2015 meeting, Dr. Meghan E. Hofto of Children’s of Alabama at the University of Alabama, Birmingham, presented research from a study of 554 patients admitted to the hospital with community acquired pneumonia, including 78 patients with complicated pneumonia.
Seven patients in the cohort (1.3%) had S. aureus infections, Dr. Hofto and her colleagues found. Of those, six were recorded as having complicated pneumonia, characterized by pleural effusion or cavitation.
Six patients with S. aureus had been started on antibiotics in other health care settings prior to admission (amoxicillin n = 4, multiple agents n = 2). One patient positive for flu was first treated with oseltamavir only. However, all staph patients once admitted were started on vancomycin, which is effective against S. aureus, within 24 hours. Five were diagnosed by pleural fluid culture; one case was identified by clinical presentation, and another by sputum culture, Dr. Hofto said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The S. aureus patients were younger than the cohort as a whole (median 18 months vs. 40.5 months). Length of stay was significantly longer for these patients, compared with the rest of the cohort (median 10 vs. 2 days, P less than .01), and S. aureus patients had significantly higher incidence of anemia (P less than .01), a finding that Dr. Hofto said was striking.
Within 24 hours of presentation, six out the seven staph cases had anemia, she said, while of all the 78 patients with complicated disease, 12 had anemia. Community acquired S. aureus pneumonia has been linked in other studies to severe leukopenia, Dr. Hofto noted (BMC Infect Dis. 2013;13:359) and (Paediatric Respiratory Reviews 2011 Sept;12:182-9).In an interview, Dr. Hofto said the findings supported current guidance in favor of first-line penicillin, amoxicillin, or ampicillin. “Part of what we’re looking at with guideline adherence is the barriers to treating with empiric narrow spectrum antibiotics – and obviously, one of the things people are concerned about is that are we going to miss something,” she said.
“I think we can pretty confidently say that if it’s uncomplicated CAP – if there’s no pleural effusion, no necrosis, no cavitation – you can treat with narrow spectrum, and the likelihood of it being staph is slim to none.”
If within 48 hours, patients are not responding to the first-line treatment, “you should start thinking about other causes,” Dr. Hofto said, noting that her review found all staph aureus patients were started on antibiotics effective against S. aureus – mostly vancomycin and ceftriaxone – within 24 hours of presentation.
Dr. Hofto noted as a limitation of her study, which used retrospective chart reviews of more than 3,400 children hospitalized for suspected pneumonia over a 3-year period, that additional S. aureus cases could have been missed because of a lack of proper coding or microbial confirmation. Another limitation was the single-site design and the relatively small number of S. aureus cases.
Dr. Hofto said she is conducting a more in-depth chart review ensure that no further cases of S. aureus CAP were missed in her sample.
The study received no outside funding, and Dr. Hofto disclosed no conflicts of interest.
SAN ANTONIO – Current guidelines on community-acquired pneumonia recommend penicillin, amoxicillin, or ampicillin as first-line treatment in children with CAP.
However, a small minority will have Staphylococcus aureus infections not treatable with these antibiotics, raising some concern about how many of these cases might be missed.
At the Pediatric Hospital Medicine 2015 meeting, Dr. Meghan E. Hofto of Children’s of Alabama at the University of Alabama, Birmingham, presented research from a study of 554 patients admitted to the hospital with community acquired pneumonia, including 78 patients with complicated pneumonia.
Seven patients in the cohort (1.3%) had S. aureus infections, Dr. Hofto and her colleagues found. Of those, six were recorded as having complicated pneumonia, characterized by pleural effusion or cavitation.
Six patients with S. aureus had been started on antibiotics in other health care settings prior to admission (amoxicillin n = 4, multiple agents n = 2). One patient positive for flu was first treated with oseltamavir only. However, all staph patients once admitted were started on vancomycin, which is effective against S. aureus, within 24 hours. Five were diagnosed by pleural fluid culture; one case was identified by clinical presentation, and another by sputum culture, Dr. Hofto said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The S. aureus patients were younger than the cohort as a whole (median 18 months vs. 40.5 months). Length of stay was significantly longer for these patients, compared with the rest of the cohort (median 10 vs. 2 days, P less than .01), and S. aureus patients had significantly higher incidence of anemia (P less than .01), a finding that Dr. Hofto said was striking.
Within 24 hours of presentation, six out the seven staph cases had anemia, she said, while of all the 78 patients with complicated disease, 12 had anemia. Community acquired S. aureus pneumonia has been linked in other studies to severe leukopenia, Dr. Hofto noted (BMC Infect Dis. 2013;13:359) and (Paediatric Respiratory Reviews 2011 Sept;12:182-9).In an interview, Dr. Hofto said the findings supported current guidance in favor of first-line penicillin, amoxicillin, or ampicillin. “Part of what we’re looking at with guideline adherence is the barriers to treating with empiric narrow spectrum antibiotics – and obviously, one of the things people are concerned about is that are we going to miss something,” she said.
“I think we can pretty confidently say that if it’s uncomplicated CAP – if there’s no pleural effusion, no necrosis, no cavitation – you can treat with narrow spectrum, and the likelihood of it being staph is slim to none.”
If within 48 hours, patients are not responding to the first-line treatment, “you should start thinking about other causes,” Dr. Hofto said, noting that her review found all staph aureus patients were started on antibiotics effective against S. aureus – mostly vancomycin and ceftriaxone – within 24 hours of presentation.
Dr. Hofto noted as a limitation of her study, which used retrospective chart reviews of more than 3,400 children hospitalized for suspected pneumonia over a 3-year period, that additional S. aureus cases could have been missed because of a lack of proper coding or microbial confirmation. Another limitation was the single-site design and the relatively small number of S. aureus cases.
Dr. Hofto said she is conducting a more in-depth chart review ensure that no further cases of S. aureus CAP were missed in her sample.
The study received no outside funding, and Dr. Hofto disclosed no conflicts of interest.
SAN ANTONIO – Current guidelines on community-acquired pneumonia recommend penicillin, amoxicillin, or ampicillin as first-line treatment in children with CAP.
However, a small minority will have Staphylococcus aureus infections not treatable with these antibiotics, raising some concern about how many of these cases might be missed.
At the Pediatric Hospital Medicine 2015 meeting, Dr. Meghan E. Hofto of Children’s of Alabama at the University of Alabama, Birmingham, presented research from a study of 554 patients admitted to the hospital with community acquired pneumonia, including 78 patients with complicated pneumonia.
Seven patients in the cohort (1.3%) had S. aureus infections, Dr. Hofto and her colleagues found. Of those, six were recorded as having complicated pneumonia, characterized by pleural effusion or cavitation.
Six patients with S. aureus had been started on antibiotics in other health care settings prior to admission (amoxicillin n = 4, multiple agents n = 2). One patient positive for flu was first treated with oseltamavir only. However, all staph patients once admitted were started on vancomycin, which is effective against S. aureus, within 24 hours. Five were diagnosed by pleural fluid culture; one case was identified by clinical presentation, and another by sputum culture, Dr. Hofto said at the meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
The S. aureus patients were younger than the cohort as a whole (median 18 months vs. 40.5 months). Length of stay was significantly longer for these patients, compared with the rest of the cohort (median 10 vs. 2 days, P less than .01), and S. aureus patients had significantly higher incidence of anemia (P less than .01), a finding that Dr. Hofto said was striking.
Within 24 hours of presentation, six out the seven staph cases had anemia, she said, while of all the 78 patients with complicated disease, 12 had anemia. Community acquired S. aureus pneumonia has been linked in other studies to severe leukopenia, Dr. Hofto noted (BMC Infect Dis. 2013;13:359) and (Paediatric Respiratory Reviews 2011 Sept;12:182-9).In an interview, Dr. Hofto said the findings supported current guidance in favor of first-line penicillin, amoxicillin, or ampicillin. “Part of what we’re looking at with guideline adherence is the barriers to treating with empiric narrow spectrum antibiotics – and obviously, one of the things people are concerned about is that are we going to miss something,” she said.
“I think we can pretty confidently say that if it’s uncomplicated CAP – if there’s no pleural effusion, no necrosis, no cavitation – you can treat with narrow spectrum, and the likelihood of it being staph is slim to none.”
If within 48 hours, patients are not responding to the first-line treatment, “you should start thinking about other causes,” Dr. Hofto said, noting that her review found all staph aureus patients were started on antibiotics effective against S. aureus – mostly vancomycin and ceftriaxone – within 24 hours of presentation.
Dr. Hofto noted as a limitation of her study, which used retrospective chart reviews of more than 3,400 children hospitalized for suspected pneumonia over a 3-year period, that additional S. aureus cases could have been missed because of a lack of proper coding or microbial confirmation. Another limitation was the single-site design and the relatively small number of S. aureus cases.
Dr. Hofto said she is conducting a more in-depth chart review ensure that no further cases of S. aureus CAP were missed in her sample.
The study received no outside funding, and Dr. Hofto disclosed no conflicts of interest.
AT PEDIATRIC HOSPITAL MEDICINE 2015
Key clinical point: About 1% of children presenting to a hospital with community-acquired pneumonia had Staphylococcus aureus infections, which do not respond to recommended first-line narrow spectrum antibiotics for CAP.
Major finding: In a cohort of 554 children admitted with CAP, 7 had S. aureus infections, 6 classed as complicated. All received vancomycin within 24 hours of admission; anemia incidence was significantly higher in S. aureus patients than for the rest of the cohort.
Data source: Retrospective cohort study of more than 3,400 children.
Disclosures: The study received no outside funding, and Dr. Hofto disclosed no conflicts of interest.