User login
A majority of practitioners will at some time encounter scoliosis, the most common spinal deformity seen in pediatric practice.1 This musculoskeletal condition can be found incidentally during routine exams, in the urgent care setting, in the emergency department (ED), or on chest x-rays or other radiographs. In primary care, scoliosis may be overlooked, particularly when the etiology is idiopathic or when well-child visits or routine back exams have been missed.1
The focus of this review will be on early identification of affected patients (most commonly those with adolescent idiopathic scoliosis), with emphasis on evaluation through an excellent physical examination and ordering of appropriate radiographs. Watchful waiting and monitoring are the norm; however, implementing carefully selected treatment options, such as bracing, or making an appropriate referral may make it possible to slow or stop curve progression.1-4
SCOLIOSIS: THE DEFINITION
Scoliosis is a coronal curvature (lateral deviation of the spine) of more than 10°, usually with a rotational component.1,2 A healthy spine is straight in the frontal plane, but curved in the sagittal plane. Normal circumstances include thoracic kyphosis (outward curve of the upper back) and lumbar lordosis (inward curve of the lower back).5 The scoliotic spine deviates away from the midline, and maximal rotation is at the apex of the curve. The apex or point of the curve defines its center, that is, the most laterally deviated vertebra or disc. The first curve to develop is the primary curve; however, when a patient presents with two or three curves, it is difficult to determine which curve is primary.
The secondary curve is a compensatory curve, which develops as a means to balance the head and trunk over the pelvis. A similar compensation may occur in the sagittal plane, exacerbating the normal kyphosis or lordosis or possibly causing rib or scapular prominences.6 Cervical curves can also develop but are more commonly associated with conditions other than idiopathic scoliosis.3 Cervical scoliosis will not be reviewed here.
THE EPIDEMIOLOGY OF SCOLIOSIS TYPES
Eighty percent of all scoliosis patients are diagnosed with idiopathic scoliosis (which may be present in 2% to 3% of the population).1,5 The remaining 20% are diagnosed with congenital, neuromuscular, or syndrome-related spinal deformities.1 The overall prevalence of idiopathic scoliosis (with curves greater than 10°) is 1 to 3 per 100, with a comparable proportion of girls and boys. The prevalence of those with curves greater than 30° is 1 to 3 per 1,000, with a boy-girl ratio of 1:8.7 In the child who is skeletally mature, scoliosis curves measuring less than 30° usually do not progress. However, most curves greater than 50° tend to progress at about 1° per year.7
Idiopathic scoliosis is broken down into age ranges.8Infantile scoliosis is diagnosed from age 0 to 3 years and comprises 0.5% of cases; juvenile scoliosis, with an age range of 4 to 9 years, represents 10.5% of cases; and adolescent scoliosis, diagnosed any time after age 10, accounts for 89% of cases.7 The four main types of scoliosis will be discussed.
Congenital
Congenital scoliosis is defined as a malformed or segmented portion of the spine, a failure of formation of a portion of the spine, or a combination of the two.9 This results in block vertebrae or hemivertebrae, or possibly the fusing of two vertebrae with a bony bridge. Because the associated curves are often rigid, they can be resistant to correction. Worldwide, prevalence of congenital vertebral anomalies is 0.5 to 1.0 per 1,000 live births.10
Congenital scoliosis can be associated with many other congenital abnormalities, as embryonic development of the spine occurs at the same time as that of the heart, kidneys, bowel, and bladder.1 Congenital scoliosis can occur with any of these defects or in the setting of a syndrome, such as VACTERL1,9-11 (ie, vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal defects, and limb abnormalities1; see Table 11,9,11,12). If even one such defect or abnormality is found, associated comorbid conditions should be actively sought.1
In many instances, these abnormalities are noted when children are young; in children younger than 5 years, MRI is warranted, and these patients almost always need sedation during imaging. In the young child who also exhibits urologic issues, an MRI work-up for genitourinary defects can be performed at the same time.1
Patients with abnormal cardiac findings (eg, heart murmur) should be referred for a cardiology work-up.11,13 Chest wall deformities may also be present in children with congenital scoliosis. Multiple congenital rib fusions can cause chest wall constriction, possibly inhibiting growth and lung development. Untreated, this condition can ultimately shorten a child’s lifespan.14
Neuromuscular
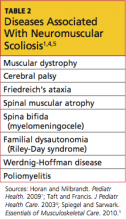
Spinal curvature in a patient with a neuromuscular disease is referred to as neuromuscular scoliosis (see Table 2).1,4,5 Most diagnoses within this category are genetic in nature, although some can result from a traumatic brain injury and/or anoxia (eg, cerebral palsy). Given that this disease state is detected early in most patients’ lives, they are generally followed by an orthopedist (or more specifically, by a pediatric orthopedist) once necessary testing, such as radiography or MRI, has been completed.1,15
Syndrome-related
Patients may have certain genetic conditions or syndromes that put them at high risk for scoliosis.
The two conditions most commonly associated with scoliosis are Marfan syndrome (60%) and neurofibromatosis (10% to 15%).1 Many patients in both groups will require MRI for evaluation; given that they are at high risk for lumbar spondylolisthesis (slippage between two lumbar vertebrae), care should be taken to evaluate for this possible secondary finding.16,17 It should be noted that patients with Marfan syndrome are at high risk for cardiac abnormalities, and those with neurofibromatosis, for dural ectasia and/ or Chiari malformations (which would be detected by MRI).16,18
Patients who have undergone chest wall surgery, such as thoracotomy for congenital heart defect repair, should be evaluated for scoliosis. The incidence of scoliosis is elevated in patients with heart defects, and the association is even greater in those who have had chest wall surgery, especially before age 18 months.19
IDIOPATHIC SCOLIOSIS
Because, by definition, no cause is known, idiopathic scoliosis is considered a diagnosis of exclusion. Affected patients have a normal neurologic exam and usually have no presenting symptoms or evidence of spinal abnormalities.1 Since 1954, idiopathic scoliosis has been divided into three age-groups, as these periods correspond to phases of increased growth velocity that occur during childhood and adolescence.8,20
Infant
A diagnosis of early-onset scoliosis is made when a child presents with scoliosis before age 5; any affected child between 0 and 3 years of age may be included in the infant scoliosis classification.2 All congenital, neuromuscular, and syndrome-related causes will have been excluded. It is felt among many experts that there is always a genetic or familial component to scoliosis. Therefore, when a child's family history is positive for scoliosis, the child should be aggressively screened, and the family should be educated to observe for signs of scoliosis and seek practitioner involvement as soon as any are evident.2
A thorough examination should be completed to rule out organ involvement in the presence of infant scoliosis.1 It is recommended that any infant with scoliotic curves greater than 20° undergo MRI of the head and spine to rule out central nervous system lesions or structural abnormalities. The risk for respiratory failure-related morbidity and mortality is increased in children with untreated early-onset scoliosis who experience curve progression. Rare progressive curves often can be addressed surgically, preserving spine and trunk growth while also achieving curve correction.2
In the majority of cases of infant scoliosis (75% to 90%), curves are left-sided (levoscoliosis)—in contrast to the right-sided curves (dextroscoliosis) more commonly noted in late-onset (juvenile or adolescent) scoliosis3,21 (see Figure 1). Infant scoliosis is slightly more common in boys (60%) than in girls.21
Neither curve lateralization nor gender makes a difference in treatment.2 Approximately 90% of early-onset curves resolve spontaneously, especially in those who are diagnosed before age 1 year. Progression occurring at a rate of 2° to 3° per year is considered gradual, whereas malignant progression often worsens by 10° or more per year, with the condition possibly becoming severe and disabling.2,21
Any infant given a diagnosis of scoliosis by a practitioner other than a pediatric orthopedist should be referred as soon as possible. On referral, copies of previously obtained radiographs and/or MRI should be presented or sent to the orthopedic practitioner, along with the history and physical exam findings, to avoid the need for repeated imaging.
Juvenile
Juvenile idiopathic scoliosis is diagnosed in patients between ages 4 and 9. Presentation in younger members of this age-group tends to resemble that in infantile idiopathic scoliosis, and children in the middle to upper age range tend to present as adolescent patients do.3 Most juvenile patients' curves will resolve without treatment (especially younger children's).
It is recommended that children with juvenile idiopathic scoliosis undergo MRI to rule out brain or spinal abnormalities. In up to 20% of children younger than 10 with curves exceeding 20°, findings on MRI are abnormal.3 Observation with close monitoring of curve progression is key in this population, especially if rapid progression is evident. In children with juvenile idiopathic scoliosis and rapid-onset curve progression, severe trunk deformity or pulmonary and/or cardiac compromise can develop. Curves that reach 30° almost always continue to worsen unless treatment is given.3,7 Timely referral to a pediatric spine orthopedist is warranted for children in this age-group.
Adolescent
It is during adolescence (ages 10 to 18) that idiopathic scoliosis is most common. Approximately 2% to 3% of children ages 10 to 15 have scoliosis with a curve of at least 10°. Among these patients, however, just 5% have scoliosis of clinical significance to warrant treatment (ie, curve progression > 30°).5,22
Each child should be examined initially for nonstructural scoliosis. This includes postural scoliosis, which resolves when a child is recumbent; compensatory scoliosis, which can be the result of a leg-length discrepancy (with no fixed vertebral rotation); sciatic scoliosis, an abnormality that results from avoiding the pain of an irritated sciatic nerve; inflammatory scoliosis, which could result from an infectious process, such as acute appendicitis; and hysterical scoliosis, a very rare form with an underlying psychological factor.4
Structural scoliosis comprises the remaining types of scoliosis, including the idiopathic variety. Patients with adolescent idiopathic scoliosis (AIS) are older than 10 and usually undergoing a rapid growth phase. Thus, some adolescent patients' curves can progress rapidly.4
Adolescents with idiopathic scoliosis rarely complain of pain or neurologic symptoms. Generally, their spinal curves do not cause organ pressure or shortness of breath. Many patients with AIS are involved in extracurricular activities that can trigger low back pain, yet activity-related low back pain is not an uncommon complaint among teens in general. Therefore, it is felt that when a patient with AIS has intermittent low back pain, it is most likely not related to their curve(s). Nevertheless, if a patient with AIS develops continued or unexplained low back pain and/or new neurologic symptoms, MRI is warranted.3
HISTORY, PHYSICAL EXAMINATION, AND DIAGNOSIS
During the exam, elicit any family history of scoliosis, especially in the setting of known diseases, such as Marfan syndrome, neurofibromatosis, muscular dystrophy, or other related diseases. Approximately 30% of AIS patients have a family history of scoliosis, so although the cause may not be clear, some genetic component is possible.3 The examination should stem from the patient's current stage of growth and development (see Table 31,3,4,7,23). The diagnosis of scoliosis is typically made during the examination and confirmed by radiography.
The newborn patient should be kept warm but be wearing only a diaper during the exam. A child or adolescent should be undressed and wearing a patient gown (unless at a school screening).
A general observation should be done initially, including the child's overall shape. The examiner should look for marfanoid features, such as excessive height, long arms, long trunk, and joint laxity.7 In the examination of the feet, an extremely high arch or cavus foot may be indicative of tethered spinal cord, spinal syrinx, or Charcot-Marie-Tooth disease, especially if the cavus is unilateral.1,7,23 MRI would be warranted in these instances.1
The examining clinician should note the child's Tanner stage. Height and weight measurements should be taken, and for a girl, age at menarche should be recorded.4
Next, the skin should be carefully inspected. In the infant, the examiner should look for hairy patches at the base of the spine, cutaneous sinuses, sacral dimpling, or other skin lesions that may suggest spinal dysraphism (ie, failure of the posterior elements to fuse around the spinal cord).4 Examination for café au lait spots and/or freckling in the axilla or groin area should be included, as this could signify neurofibromatosis.1,4,7
Examine the back in a standing child. Note whether the head appears to be centered over the sacrum. Evaluate for shoulder height or truncal asymmetry, scapular or posterior rib prominence, and excessive thoracic kyphosis and/or lumbar lordosis. Examine the pelvic bones, looking for obliquity (ie, one side higher than the other). Look for leg length discrepancy, both while the patient is standing still and during a gait review.1
During an anterior exam, look for shoulder or truncal asymmetry, leg length discrepancy, and anterior rib prominence. If shoulder height asymmetry is apparent, measure from each acromioclavicular joint to the floor and note the difference in centimeters. In the case of pelvic obliquity, measure from each anterior (or posterior) superior iliac spine to the floor and note the difference in centimeters. If the head does not appear to align over the sacrum, lower a plum line from the spinous process of C7 down to the gluteal cleft level. Measure by centimeters the distance from the cleft to the line, noting the side to which the line sways.
View the patient from the side. The sagittal curve can be assessed from the occiput to the sacrum; observe for an increased lordotic or kyphotic curve or abnormal positioning related to abnormal curves.4
The Adams forward bend test should be conducted.24,25 The child who is able to stand faces away from the examiner, then bends forward at the waist with the knees straight and the arms hanging down passively (see Figure 2). The practitioner looks at the spine from behind and notes any rib, thoracic, scapular, or lumbar prominence that could indicate a rotational spine deformity.1,4,7 In some instances, the use of a scoliometer can be helpful to assign a number to the amount of rotation to the spine during the Adams forward bend test. However, primary care offices are not often equipped with this device.26
Motor and Neurologic Examinations
The motor exam includes testing motor strength in all four extremities and noting any asymmetry. The examiner should have the child actively bend in every direction, making note of any deformity, stiffness, or asymmetry. The patient's spine should be palpated, with any tenderness noted, and any available radiographs reviewed.1,4,7
The neurologic exam includes testing cranial nerves, sensation, and reflexes, including the patellar, Achilles, and umbilical reflexes, as well as Babinski's sign. Many patients are areflexic in one or more areas. For instance, a finding of no umbilical (abdominal wink) reflex on either side is not suspicious in itself, but it should alert the practitioner to evaluate carefully for asymmetrical reflexes in one or more areas, especially if they are ipsilateral. Any positive neurologic findings, especially in the setting of scoliosis, warrant an MRI.1,7
Scoliosis Screening in the School Setting
One controversial subject related to scoliosis is school screenings. These screenings were developed in the 1980s for early identification of children with scoliosis curves so that nonsurgical treatment could be initiated promptly, or that surgery, when deemed necessary, could be performed in a timely fashion for optimal results.27
Since then, the effectiveness of screening programs has come under debate; in 2004, the US Preventive Services Task Force28 issued a recommendation (rating, "D Recommendation") against routine screening for idiopathic scoliosis in asymptomatic adolescents, stating that its effectiveness had not been shown in clinical trials. In response, a task force was convened by the American Academy of Orthopaedic Surgeons, the Scoliosis Research Society, the Pediatric Orthopaedic Society of North America, and the American Academy of Pediatrics, with findings published in a 2008 information statement by Richards and Vitale.25 While acknowledging the limitations of support for screening in the literature, the task force concluded:
- Early treatment of the deformities associated with idiopathic scoliosis can result in substantial benefits
- Screening (whether in the school environment or other settings) offers an opportunity for early diagnosis and appropriate referral of otherwise undetected deformities, especially in under-served populations
- In many cases, brace treatment may preclude the need for surgery in children with significant scoliosis
- Identifying deformities that require surgery as early as possible through screening increases the likelihood of good treatment outcomes
- Girls, who reach adolescence two years earlier than boys, should be screened at ages 10 and 12; boys, at age 13 or 14
- School personnel who conduct screening should receive training to detect spinal deformities
- While no screening test is entirely reliable, the forward bend test is considered the most specific test for detection of scoliosis29
- The participating organizations remain committed to preventing inappropriate use of spinal x-rays.25
Despite the ongoing debate, more than half of the US states have screening programs in place.24,27
RADIOGRAPHS/LABORATORY TESTING
Physical examination and a thorough history are most important in evaluation for scoliosis in the primary care setting. When radiographs (x-rays) are considered necessary, posterior-anterior and lateral spine series should be ordered. These are full-length (3-ft)
x-rays of the patient standing with the knees straight (when the child is able to do so).1,4,7 The x-rays are taken in the posterior-anterior direction to minimize breast and organ radiation exposure and to produce an x-ray similar to that of viewing the patient from behind.
If scoliosis is observed on radiography, note the apex of the curve, the location, the direction in which it curves, and any rotational component. Examine for pelvic obliquity, shoulder asymmetry, spondylosis, or spondylolisthesis.7
The Cobb angle is the measurement used to quantify the degree of scoliosis.4,5,7 Using the posterior-anterior radiograph, a line is drawn along the superior endplate of the most curved cephalad vertebra and the inferior endplate of the caudal vertebra. When perpendicular lines are drawn, the intersecting lines form the Cobb angle (see Figure 3, in which "X" indicates the Cobb angle, measured in degrees). An increasing angle reflects the increasing severity of scoliosis.
Other radiographs that may be ordered include supine lateral (bending) x-rays or supine traction radiographs to evaluate curve flexibility before surgery30; recently, hanging total spine x-rays have been investigated to evaluate spine flexibility before brace treatment.31 Additionally, hand/wrist x-rays may be ordered to determine the patient's remaining growth potential. These are most often taken in an orthopedist's office.3
If a diagnosis of scoliosis is made, Risser staging should be completed. Risser sign is a growth marker noted in adolescents by viewing iliac apophyseal ossification on radiograph. The progress of bone fusion over the iliac apophysis reflects remaining skeletal growth and is graded from 0 to 5, with 0 representing no ossification of the iliac apophysis and 5, complete ossification. The lower the grade noted at curve detection, the greater the risk for curve progression.3,4
Other tests may be warranted. If a patient has persistent back or side pain, especially pain that wakens the patient at night, and/ or pain not relieved by aspirin or NSAIDs, then a bone scan should be ordered to rule out discitis, rib or spine osteoid osteoma, spinal or intradural tumors, osteomyelitis, or other abnormalities.7 An MRI is warranted in children younger than 10; those who have left-sided curves, headaches, or neck pain; patients with quickly progressing curves; and those with any abnormality on neurologic exam. This test is generally not necessary in those with AIS if no family history is present and physical exam findings are unremarkable.1,2,5,7 Laboratory tests are generally not ordered for patients with idiopathic scoliosis unless inflammatory or infectious processes are suspected; standard laboratory tests would then follow. The ScoliScoreTM (Axial Biotech, Salt Lake City), a newer genetic screening test, can be used along with clinical and radiographic testing in patients with AIS. It is felt that specific genes are associated with AIS, and this test may help detect them and determine any associated risk for curve progression.1,3
There are several genetic tests for conditions associated with congenital neuromuscular or syndrome-related scoliosis.12,32 These may be ordered by the primary care provider, an orthopedist, or the geneticist.
REFERRAL
According to some researchers, any child with scoliosis greater than 10° should be referred to an orthopedist, preferably a pediatric spine orthopedist, especially when the patient is younger than 10. Referral is also recommended when the curve is left thoracic, or if any abnormal physical findings or a positive family history is present.4,5,7 There is also support for a strategy in which the practitioner closely observes the patient older than 10 with scoliosis but no other abnormalities, then refers the child once the curve reaches 20° to 25°.7 Referral within three months is most likely indicated for those with typical scoliosis and within one month for atypical scoliosis.7
Each practitioner will develop his or her own comfort level in the management of idiopathic scoliosis. Once a referral has been made, the practitioner should follow up to be sure the patient has seen the specialist in a timely fashion, with no appointments missed. Curve progression can develop rapidly, possibly making treatment more difficult once it begins.
TREATMENT
Three main types of treatment are provided for scoliosis: observation, bracing, and surgery.3,5,7 Observation is generally considered sufficient for immature patients whose curves measure less than 25°; usually no treatment will be needed for mature patients with curves less than 25°. Depending on risk stratification, children will initially need serial radiographs every four to six months.2
Most children will be seen by an orthopedist at this point.2,3,22 Oftentimes orthopedists with adult patients will order radiographs every three to five years to be sure the scoliosis has not progressed.3 Treatment of children with neuromuscular or syndrome-related scoliosis is lengthy and will not be addressed in this review.
Orthotic management (bracing or casting) is usually started once the immature patient's curve is between 25° and 45°. Brace treatment is not used to alter or correct scoliosis, but rather to halt its progression until the patient is skeletally mature (more common), a spinal fusion occurs (less common), or both.5 A 20% to 24% risk for eventual surgery has been reported in patients treated with braces.25,33 In infants or young children with congenital (or other) scoliosis, several temporary management options can be used to prevent curve progression while allowing the child's thorax to grow and expand.2
Several surgical interventions are appropriate for scoliosis. For infants or young children, one surgical intervention is the vertical expandable prosthetic titanium rib (VEPTRTM [Synthes, Inc, West Chester, Pennsylvania]). This is a longitudinal rib distraction device that can attach from rib to rib, rib to spine, or rib to pelvis. The device is indicated in the presence of a constrictive chest wall syndrome, which can decrease lung volumes and cause severe deformity if untreated. The device is lengthened every 4 to 6 months, with the goal to delay a final fusion until skeletal maturity.2
The growing rod, a comparable temporary device, is inserted spine to spine and lengthened similarly at various intervals. Growing rods are usually used in older children with scoliosis who await maturity before undergoing a definitive spinal fusion.2
A newer surgical procedure being used at Morgan Stanley Children's Hospital of NewYork-Presbyterian is spinal stapling.34 This involves minimally invasive surgery to implant inch-long staples across the spinal growth plates, which can stop scoliosis from worsening, or even correct the curve.
Spinal fusion with instrumentation, though used in less than 5% of patients with AIS, is considered the definitive surgical treatment for scoliosis.6 Surgical correction is almost always deemed necessary in immature patients with curves greater than 45° and mature patients with curves greater than 50°.3,7,22 The fusion may involve posterior (and sometimes anterior) discectomy and/or bone grafting between the involved vertebrae to help the bones fuse together so that curves cannot progress. The instrumentation (rods, hooks, wires, and/or screws) is used simply to maintain the spine in the best possible position until the actual fusion occurs; this can take months to a year.2,5,7
Risks and benefits of spinal fusion must be thoroughly reviewed with each parent and patient. The reported neurologic injury and mortality rates are less than 1% and less than 0.02%, respectively, in patients with idiopathic scoliosis who undergo the surgery.7 There is an increased incidence of such concerns in patients with other types of scoliosis, given their comorbid issues.35
Alternative treatments such as physical therapy, yoga, massage, acupuncture, and chiropractic medicine do not put patients at risk, and some have found them beneficial.3
EDUCATION
Both patient and parent must be acquainted with the goal of scoliosis diagnosis and treatment: to prevent curve progression, altered body image, and, ultimately, morbidity. Screening, history, examination, and radiographs are important first steps, with the information gained determining when referral to a pediatric spine orthopedist/specialist (if possible) should be made. Once curves reach 25° to 30°, bracing can successfully prevent curve progression; it will not correct the scoliosis.7 Teens who are resistant or reluctant to wear their brace must be made to understand the consequences of not following the treatment regimen, and the clinician's encouragement is essential.
Patients should be encouraged to stay active, with special emphasis on flexibility. Generally, there is no contraindication regarding activities or sports, unless the patient has undergone a surgical procedure; in this case, the practitioner will determine the patient's optimal level of participation in physical activities.
Surgical treatment with fusion and instrumentation is the only proven scoliosis treatment to correct curves (fully or partially) and prevent progression.3,5,7 Curves that reach 50° without treatment in the fully mature individual may continue to worsen into adulthood.
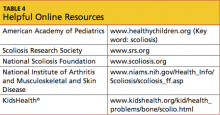
For patients with scoliosis having a possible familial and/or genetic component,2,3,7 there are several Web sites for patients and parents (see Table 4). Some of these address alternative therapy options.
CONCLUSION
Scoliosis is common, but the sequelae of idiopathic scoliosis can be minimized if the condition is diagnosed early and measures to prevent curve progression are initiated in a timely fashion. The key to diagnosing associated comorbid disorders and other related issues is to conduct a thorough patient and family history and complete physical examination. Timely radiographs are warranted in any patient with a positive finding. Ordering appropriate radiographs accurately is essential to facilitate patient care while reducing radiation exposure. Each practitioner must determine his or her level of comfort in managing patients with idiopathic scoliosis or immediately referring the patient once the diagnosis is made. Early referral is best in the primary care practice.
1. Horan MP, Milbrandt TA. Scoliosis in pediatric patients: comorbid disorders and screening. Pediatr Health. 2009;3(5):451-456.
2. Debnath UK. Current concepts in the management of early-onset idiopathic scoliosis. Pediatr Health. 2010;4(3):343-354.
3. Scoliosis Research Society. Idiopathic scoliosis. www.srs.org/patient_and_family/scoliosis/idiopathic. Accessed July 19, 2012.
4. Taft E, Francis R. Evaluation and management of scoliosis. J Pediatr Health Care. 2003;17(1):42- 44.
5. Speigel DA, Sarwark JF. Pediatric orthopaedics. In: Sarwark JF, ed. Essentials of Musculoskeletal Care. 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010:976-1201.
6. Horn PL, Beebe AC. Scoliosis: incidence and current medical and surgical interventions. Heartbeat. 2008;19(3):6-7,17.
7. Janicki JA. Scoliosis. In: Miller MD, Hart JA, MacKnight JM. Essential Orthopaedics. Marietta, GA: Saunders/Elsevier; 2010:881-886.
8. James JIP. Idiopathic scoliosis; the prognosis, diagnosis, and operative indications related to curve patterns and the age at onset. J Bone Joint Surg Br. 1954;36-B(1):36-49.
9. Scoliosis. In: Herring JA. Tachdjian's Pediatric Orthopaedics. Vol I. 4th ed. Philadelphia, PA: Saunders/Elsevier; 2008:265-411.
10. Debnath UK, Goel V, Harshavarfhana N, Webb JK. Congenital scoliosis - Quo vadis? Indian J Orthop. 2010;44(2):137-147.
11. Basu PS, Elsebaie H, Noordeen MH. Congenital spine deformity: a comprehensive assessment at presentation. Spine (Phila Pa 1976). 2002;27(20):2255-2259.
12. Fisher K, Esham RH, Thorneycroft I. Scoliosis associated with typical Mayer-Rokitansky-Küster-Hauser syndrome. South Med J. 2000;93(2):243-246.
13. Hedequist D, Emans J. Congenital scoliosis: a review and update. J Pediatr Orthop. 2007;27(1):106-116.
14. Pehrsson K, Larsson S, Oden A, Nachemson A. Long-term follow-up of patients with untreated scoliosis: a study of mortality, causes of death, and symptoms. Spine (Phila Pa 1976). 1992;17(9):1091-1096.
15. Ferguson RL. Medical and congenital comorbidities associated with spinal deformities in the immature spine. J Bone Joint Surg Am. 2007;89(suppl 1):34-41.
16. Demetracopoulos CA, Sponseller PD. Spinal deformities in Marfan syndrome. Orthop Clin North Am. 2007;38(4):563-572.
17. Crawford AH, Herrera-Soto J. Scoliosis associated with neurofibromatosis. Orthop Clin North Am. 2007;38(4):553-562.
18. Disorders of the spinal cord. In: Herring JA. Tachdjian's Pediatric Orthopaedics. Vol II. 4th ed. Philadelphia, PA: Saunders/Elsevier; 2008:1405-1482.
19. Ruiz-Iban MA, Burgos J, Aguado HJ, et al. Scoliosis after median sternotomy in children with congenital heart disease. Spine (Phila Pa 1976). 2005;30(8):E214-E218.
20. Dimeglio A. Growth of the spine before age 5 years. J Pediatr Orthop B. 1993;1:102-107.
21. Lloyd-Roberts GC, Pilcher MF. Structural idiopathic scoliosis in infancy: a study of natural history of 100 patients. J Bone Joint Surg Br. 1965;47:520-523.
22. Gutknecht S, Lonstein J, Novacheck T. Adolescent idiopathic scoliosis. Pediatric Perspective. 2009;18(4):1-4.
23. Lew SM, Kothbauer KF. Tethered cord syndrome: an updated review. Pediatr Neurosurg. 2007;43(3):236-248.
24. Bunge EM, Juttmann RE, van Biezen FC, et al; Netherlands Evaluation Study on Screening for Scoliosis (NESCIO) Group. Estimating the effectiveness of screening for scoliosis: a case-control study. Pediatrics. 2008;121(1):9-14.
25. Richards BS, Vitale MG. Screening for idiopathic scoliosis in adolescents: an information statement. J Bone Joint Surg. 2008;90(1):195-198.
26. Côté P, Kreitz BG, Cassidy JD, et al. A study of the diagnostic accuracy and reliability of the scoliometer and Adam's forward bend test. Spine. 1998;23(7):796-802.
27. Richards BS, Beaty JH, Thompson GH, Willis RB. Estimating the effectiveness of screening for scoliosis. Pediatrics. 2008:121(6):1297-1298.
28. US Preventive Services Task Force. Screening for idiopathic scoliosis in adolescents: recommendation statement (2004). www.uspreventiveservicestaskforce.org/3rduspstf/scoliosis/scoliors.htm. Accessed July 19, 2012.
29. Karachalios T, Sofianos J, Roidis N, et al. Ten-year follow-up evaluation of a school screening program for scoliosis. Is the forward-bending test an accurate diagnostic criterion for the screening of scoliosis? Spine (Phila Pa 1976). 1999;24(22):2318-2324.
30. Hamzaoglu A, Talu U, Tezer M, et al. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30(14):1627-1642.
31. Kuroki H, Inomata N, Hamanaka H, et al. Significance of hanging total spine x-ray to estimate the indicative correction angle by brace wearing in idiopathic scoliosis patients. Scoliosis. 2012;7:8.
32. Al-Otibi M, Rutka JT. Neurosurgical implications of neurofibromatosis type I in children. Neurosurg Focus. 2006;20(1):E2.
33. Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976). 2007;32(19 suppl):S91-S100.
34. American Academy of Pediatrics. New stapling treatment may help reverse scoliosis: report from the Morgan Stanley Children's Hospital Department of Pediatric Orthopaedics. Section on Orthopaedics Newsletter. Spring 2009. www2.aap.org/sections/ortho/spring2009news.pdf. Accessed July 19, 2012.
35. Reames DL, Smith JS, Fu KG, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis. Spine. 2011;36(18):1484-1491.
A majority of practitioners will at some time encounter scoliosis, the most common spinal deformity seen in pediatric practice.1 This musculoskeletal condition can be found incidentally during routine exams, in the urgent care setting, in the emergency department (ED), or on chest x-rays or other radiographs. In primary care, scoliosis may be overlooked, particularly when the etiology is idiopathic or when well-child visits or routine back exams have been missed.1
The focus of this review will be on early identification of affected patients (most commonly those with adolescent idiopathic scoliosis), with emphasis on evaluation through an excellent physical examination and ordering of appropriate radiographs. Watchful waiting and monitoring are the norm; however, implementing carefully selected treatment options, such as bracing, or making an appropriate referral may make it possible to slow or stop curve progression.1-4
SCOLIOSIS: THE DEFINITION
Scoliosis is a coronal curvature (lateral deviation of the spine) of more than 10°, usually with a rotational component.1,2 A healthy spine is straight in the frontal plane, but curved in the sagittal plane. Normal circumstances include thoracic kyphosis (outward curve of the upper back) and lumbar lordosis (inward curve of the lower back).5 The scoliotic spine deviates away from the midline, and maximal rotation is at the apex of the curve. The apex or point of the curve defines its center, that is, the most laterally deviated vertebra or disc. The first curve to develop is the primary curve; however, when a patient presents with two or three curves, it is difficult to determine which curve is primary.
The secondary curve is a compensatory curve, which develops as a means to balance the head and trunk over the pelvis. A similar compensation may occur in the sagittal plane, exacerbating the normal kyphosis or lordosis or possibly causing rib or scapular prominences.6 Cervical curves can also develop but are more commonly associated with conditions other than idiopathic scoliosis.3 Cervical scoliosis will not be reviewed here.
THE EPIDEMIOLOGY OF SCOLIOSIS TYPES
Eighty percent of all scoliosis patients are diagnosed with idiopathic scoliosis (which may be present in 2% to 3% of the population).1,5 The remaining 20% are diagnosed with congenital, neuromuscular, or syndrome-related spinal deformities.1 The overall prevalence of idiopathic scoliosis (with curves greater than 10°) is 1 to 3 per 100, with a comparable proportion of girls and boys. The prevalence of those with curves greater than 30° is 1 to 3 per 1,000, with a boy-girl ratio of 1:8.7 In the child who is skeletally mature, scoliosis curves measuring less than 30° usually do not progress. However, most curves greater than 50° tend to progress at about 1° per year.7
Idiopathic scoliosis is broken down into age ranges.8Infantile scoliosis is diagnosed from age 0 to 3 years and comprises 0.5% of cases; juvenile scoliosis, with an age range of 4 to 9 years, represents 10.5% of cases; and adolescent scoliosis, diagnosed any time after age 10, accounts for 89% of cases.7 The four main types of scoliosis will be discussed.
Congenital
Congenital scoliosis is defined as a malformed or segmented portion of the spine, a failure of formation of a portion of the spine, or a combination of the two.9 This results in block vertebrae or hemivertebrae, or possibly the fusing of two vertebrae with a bony bridge. Because the associated curves are often rigid, they can be resistant to correction. Worldwide, prevalence of congenital vertebral anomalies is 0.5 to 1.0 per 1,000 live births.10
Congenital scoliosis can be associated with many other congenital abnormalities, as embryonic development of the spine occurs at the same time as that of the heart, kidneys, bowel, and bladder.1 Congenital scoliosis can occur with any of these defects or in the setting of a syndrome, such as VACTERL1,9-11 (ie, vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal defects, and limb abnormalities1; see Table 11,9,11,12). If even one such defect or abnormality is found, associated comorbid conditions should be actively sought.1
In many instances, these abnormalities are noted when children are young; in children younger than 5 years, MRI is warranted, and these patients almost always need sedation during imaging. In the young child who also exhibits urologic issues, an MRI work-up for genitourinary defects can be performed at the same time.1
Patients with abnormal cardiac findings (eg, heart murmur) should be referred for a cardiology work-up.11,13 Chest wall deformities may also be present in children with congenital scoliosis. Multiple congenital rib fusions can cause chest wall constriction, possibly inhibiting growth and lung development. Untreated, this condition can ultimately shorten a child’s lifespan.14
Neuromuscular
Spinal curvature in a patient with a neuromuscular disease is referred to as neuromuscular scoliosis (see Table 2).1,4,5 Most diagnoses within this category are genetic in nature, although some can result from a traumatic brain injury and/or anoxia (eg, cerebral palsy). Given that this disease state is detected early in most patients’ lives, they are generally followed by an orthopedist (or more specifically, by a pediatric orthopedist) once necessary testing, such as radiography or MRI, has been completed.1,15
Syndrome-related
Patients may have certain genetic conditions or syndromes that put them at high risk for scoliosis.
The two conditions most commonly associated with scoliosis are Marfan syndrome (60%) and neurofibromatosis (10% to 15%).1 Many patients in both groups will require MRI for evaluation; given that they are at high risk for lumbar spondylolisthesis (slippage between two lumbar vertebrae), care should be taken to evaluate for this possible secondary finding.16,17 It should be noted that patients with Marfan syndrome are at high risk for cardiac abnormalities, and those with neurofibromatosis, for dural ectasia and/ or Chiari malformations (which would be detected by MRI).16,18
Patients who have undergone chest wall surgery, such as thoracotomy for congenital heart defect repair, should be evaluated for scoliosis. The incidence of scoliosis is elevated in patients with heart defects, and the association is even greater in those who have had chest wall surgery, especially before age 18 months.19
IDIOPATHIC SCOLIOSIS
Because, by definition, no cause is known, idiopathic scoliosis is considered a diagnosis of exclusion. Affected patients have a normal neurologic exam and usually have no presenting symptoms or evidence of spinal abnormalities.1 Since 1954, idiopathic scoliosis has been divided into three age-groups, as these periods correspond to phases of increased growth velocity that occur during childhood and adolescence.8,20
Infant
A diagnosis of early-onset scoliosis is made when a child presents with scoliosis before age 5; any affected child between 0 and 3 years of age may be included in the infant scoliosis classification.2 All congenital, neuromuscular, and syndrome-related causes will have been excluded. It is felt among many experts that there is always a genetic or familial component to scoliosis. Therefore, when a child's family history is positive for scoliosis, the child should be aggressively screened, and the family should be educated to observe for signs of scoliosis and seek practitioner involvement as soon as any are evident.2
A thorough examination should be completed to rule out organ involvement in the presence of infant scoliosis.1 It is recommended that any infant with scoliotic curves greater than 20° undergo MRI of the head and spine to rule out central nervous system lesions or structural abnormalities. The risk for respiratory failure-related morbidity and mortality is increased in children with untreated early-onset scoliosis who experience curve progression. Rare progressive curves often can be addressed surgically, preserving spine and trunk growth while also achieving curve correction.2
In the majority of cases of infant scoliosis (75% to 90%), curves are left-sided (levoscoliosis)—in contrast to the right-sided curves (dextroscoliosis) more commonly noted in late-onset (juvenile or adolescent) scoliosis3,21 (see Figure 1). Infant scoliosis is slightly more common in boys (60%) than in girls.21
Neither curve lateralization nor gender makes a difference in treatment.2 Approximately 90% of early-onset curves resolve spontaneously, especially in those who are diagnosed before age 1 year. Progression occurring at a rate of 2° to 3° per year is considered gradual, whereas malignant progression often worsens by 10° or more per year, with the condition possibly becoming severe and disabling.2,21
Any infant given a diagnosis of scoliosis by a practitioner other than a pediatric orthopedist should be referred as soon as possible. On referral, copies of previously obtained radiographs and/or MRI should be presented or sent to the orthopedic practitioner, along with the history and physical exam findings, to avoid the need for repeated imaging.
Juvenile
Juvenile idiopathic scoliosis is diagnosed in patients between ages 4 and 9. Presentation in younger members of this age-group tends to resemble that in infantile idiopathic scoliosis, and children in the middle to upper age range tend to present as adolescent patients do.3 Most juvenile patients' curves will resolve without treatment (especially younger children's).
It is recommended that children with juvenile idiopathic scoliosis undergo MRI to rule out brain or spinal abnormalities. In up to 20% of children younger than 10 with curves exceeding 20°, findings on MRI are abnormal.3 Observation with close monitoring of curve progression is key in this population, especially if rapid progression is evident. In children with juvenile idiopathic scoliosis and rapid-onset curve progression, severe trunk deformity or pulmonary and/or cardiac compromise can develop. Curves that reach 30° almost always continue to worsen unless treatment is given.3,7 Timely referral to a pediatric spine orthopedist is warranted for children in this age-group.
Adolescent
It is during adolescence (ages 10 to 18) that idiopathic scoliosis is most common. Approximately 2% to 3% of children ages 10 to 15 have scoliosis with a curve of at least 10°. Among these patients, however, just 5% have scoliosis of clinical significance to warrant treatment (ie, curve progression > 30°).5,22
Each child should be examined initially for nonstructural scoliosis. This includes postural scoliosis, which resolves when a child is recumbent; compensatory scoliosis, which can be the result of a leg-length discrepancy (with no fixed vertebral rotation); sciatic scoliosis, an abnormality that results from avoiding the pain of an irritated sciatic nerve; inflammatory scoliosis, which could result from an infectious process, such as acute appendicitis; and hysterical scoliosis, a very rare form with an underlying psychological factor.4
Structural scoliosis comprises the remaining types of scoliosis, including the idiopathic variety. Patients with adolescent idiopathic scoliosis (AIS) are older than 10 and usually undergoing a rapid growth phase. Thus, some adolescent patients' curves can progress rapidly.4
Adolescents with idiopathic scoliosis rarely complain of pain or neurologic symptoms. Generally, their spinal curves do not cause organ pressure or shortness of breath. Many patients with AIS are involved in extracurricular activities that can trigger low back pain, yet activity-related low back pain is not an uncommon complaint among teens in general. Therefore, it is felt that when a patient with AIS has intermittent low back pain, it is most likely not related to their curve(s). Nevertheless, if a patient with AIS develops continued or unexplained low back pain and/or new neurologic symptoms, MRI is warranted.3
HISTORY, PHYSICAL EXAMINATION, AND DIAGNOSIS
During the exam, elicit any family history of scoliosis, especially in the setting of known diseases, such as Marfan syndrome, neurofibromatosis, muscular dystrophy, or other related diseases. Approximately 30% of AIS patients have a family history of scoliosis, so although the cause may not be clear, some genetic component is possible.3 The examination should stem from the patient's current stage of growth and development (see Table 31,3,4,7,23). The diagnosis of scoliosis is typically made during the examination and confirmed by radiography.
The newborn patient should be kept warm but be wearing only a diaper during the exam. A child or adolescent should be undressed and wearing a patient gown (unless at a school screening).
A general observation should be done initially, including the child's overall shape. The examiner should look for marfanoid features, such as excessive height, long arms, long trunk, and joint laxity.7 In the examination of the feet, an extremely high arch or cavus foot may be indicative of tethered spinal cord, spinal syrinx, or Charcot-Marie-Tooth disease, especially if the cavus is unilateral.1,7,23 MRI would be warranted in these instances.1
The examining clinician should note the child's Tanner stage. Height and weight measurements should be taken, and for a girl, age at menarche should be recorded.4
Next, the skin should be carefully inspected. In the infant, the examiner should look for hairy patches at the base of the spine, cutaneous sinuses, sacral dimpling, or other skin lesions that may suggest spinal dysraphism (ie, failure of the posterior elements to fuse around the spinal cord).4 Examination for café au lait spots and/or freckling in the axilla or groin area should be included, as this could signify neurofibromatosis.1,4,7
Examine the back in a standing child. Note whether the head appears to be centered over the sacrum. Evaluate for shoulder height or truncal asymmetry, scapular or posterior rib prominence, and excessive thoracic kyphosis and/or lumbar lordosis. Examine the pelvic bones, looking for obliquity (ie, one side higher than the other). Look for leg length discrepancy, both while the patient is standing still and during a gait review.1
During an anterior exam, look for shoulder or truncal asymmetry, leg length discrepancy, and anterior rib prominence. If shoulder height asymmetry is apparent, measure from each acromioclavicular joint to the floor and note the difference in centimeters. In the case of pelvic obliquity, measure from each anterior (or posterior) superior iliac spine to the floor and note the difference in centimeters. If the head does not appear to align over the sacrum, lower a plum line from the spinous process of C7 down to the gluteal cleft level. Measure by centimeters the distance from the cleft to the line, noting the side to which the line sways.
View the patient from the side. The sagittal curve can be assessed from the occiput to the sacrum; observe for an increased lordotic or kyphotic curve or abnormal positioning related to abnormal curves.4
The Adams forward bend test should be conducted.24,25 The child who is able to stand faces away from the examiner, then bends forward at the waist with the knees straight and the arms hanging down passively (see Figure 2). The practitioner looks at the spine from behind and notes any rib, thoracic, scapular, or lumbar prominence that could indicate a rotational spine deformity.1,4,7 In some instances, the use of a scoliometer can be helpful to assign a number to the amount of rotation to the spine during the Adams forward bend test. However, primary care offices are not often equipped with this device.26
Motor and Neurologic Examinations
The motor exam includes testing motor strength in all four extremities and noting any asymmetry. The examiner should have the child actively bend in every direction, making note of any deformity, stiffness, or asymmetry. The patient's spine should be palpated, with any tenderness noted, and any available radiographs reviewed.1,4,7
The neurologic exam includes testing cranial nerves, sensation, and reflexes, including the patellar, Achilles, and umbilical reflexes, as well as Babinski's sign. Many patients are areflexic in one or more areas. For instance, a finding of no umbilical (abdominal wink) reflex on either side is not suspicious in itself, but it should alert the practitioner to evaluate carefully for asymmetrical reflexes in one or more areas, especially if they are ipsilateral. Any positive neurologic findings, especially in the setting of scoliosis, warrant an MRI.1,7
Scoliosis Screening in the School Setting
One controversial subject related to scoliosis is school screenings. These screenings were developed in the 1980s for early identification of children with scoliosis curves so that nonsurgical treatment could be initiated promptly, or that surgery, when deemed necessary, could be performed in a timely fashion for optimal results.27
Since then, the effectiveness of screening programs has come under debate; in 2004, the US Preventive Services Task Force28 issued a recommendation (rating, "D Recommendation") against routine screening for idiopathic scoliosis in asymptomatic adolescents, stating that its effectiveness had not been shown in clinical trials. In response, a task force was convened by the American Academy of Orthopaedic Surgeons, the Scoliosis Research Society, the Pediatric Orthopaedic Society of North America, and the American Academy of Pediatrics, with findings published in a 2008 information statement by Richards and Vitale.25 While acknowledging the limitations of support for screening in the literature, the task force concluded:
- Early treatment of the deformities associated with idiopathic scoliosis can result in substantial benefits
- Screening (whether in the school environment or other settings) offers an opportunity for early diagnosis and appropriate referral of otherwise undetected deformities, especially in under-served populations
- In many cases, brace treatment may preclude the need for surgery in children with significant scoliosis
- Identifying deformities that require surgery as early as possible through screening increases the likelihood of good treatment outcomes
- Girls, who reach adolescence two years earlier than boys, should be screened at ages 10 and 12; boys, at age 13 or 14
- School personnel who conduct screening should receive training to detect spinal deformities
- While no screening test is entirely reliable, the forward bend test is considered the most specific test for detection of scoliosis29
- The participating organizations remain committed to preventing inappropriate use of spinal x-rays.25
Despite the ongoing debate, more than half of the US states have screening programs in place.24,27
RADIOGRAPHS/LABORATORY TESTING
Physical examination and a thorough history are most important in evaluation for scoliosis in the primary care setting. When radiographs (x-rays) are considered necessary, posterior-anterior and lateral spine series should be ordered. These are full-length (3-ft)
x-rays of the patient standing with the knees straight (when the child is able to do so).1,4,7 The x-rays are taken in the posterior-anterior direction to minimize breast and organ radiation exposure and to produce an x-ray similar to that of viewing the patient from behind.
If scoliosis is observed on radiography, note the apex of the curve, the location, the direction in which it curves, and any rotational component. Examine for pelvic obliquity, shoulder asymmetry, spondylosis, or spondylolisthesis.7
The Cobb angle is the measurement used to quantify the degree of scoliosis.4,5,7 Using the posterior-anterior radiograph, a line is drawn along the superior endplate of the most curved cephalad vertebra and the inferior endplate of the caudal vertebra. When perpendicular lines are drawn, the intersecting lines form the Cobb angle (see Figure 3, in which "X" indicates the Cobb angle, measured in degrees). An increasing angle reflects the increasing severity of scoliosis.
Other radiographs that may be ordered include supine lateral (bending) x-rays or supine traction radiographs to evaluate curve flexibility before surgery30; recently, hanging total spine x-rays have been investigated to evaluate spine flexibility before brace treatment.31 Additionally, hand/wrist x-rays may be ordered to determine the patient's remaining growth potential. These are most often taken in an orthopedist's office.3
If a diagnosis of scoliosis is made, Risser staging should be completed. Risser sign is a growth marker noted in adolescents by viewing iliac apophyseal ossification on radiograph. The progress of bone fusion over the iliac apophysis reflects remaining skeletal growth and is graded from 0 to 5, with 0 representing no ossification of the iliac apophysis and 5, complete ossification. The lower the grade noted at curve detection, the greater the risk for curve progression.3,4
Other tests may be warranted. If a patient has persistent back or side pain, especially pain that wakens the patient at night, and/ or pain not relieved by aspirin or NSAIDs, then a bone scan should be ordered to rule out discitis, rib or spine osteoid osteoma, spinal or intradural tumors, osteomyelitis, or other abnormalities.7 An MRI is warranted in children younger than 10; those who have left-sided curves, headaches, or neck pain; patients with quickly progressing curves; and those with any abnormality on neurologic exam. This test is generally not necessary in those with AIS if no family history is present and physical exam findings are unremarkable.1,2,5,7 Laboratory tests are generally not ordered for patients with idiopathic scoliosis unless inflammatory or infectious processes are suspected; standard laboratory tests would then follow. The ScoliScoreTM (Axial Biotech, Salt Lake City), a newer genetic screening test, can be used along with clinical and radiographic testing in patients with AIS. It is felt that specific genes are associated with AIS, and this test may help detect them and determine any associated risk for curve progression.1,3
There are several genetic tests for conditions associated with congenital neuromuscular or syndrome-related scoliosis.12,32 These may be ordered by the primary care provider, an orthopedist, or the geneticist.
REFERRAL
According to some researchers, any child with scoliosis greater than 10° should be referred to an orthopedist, preferably a pediatric spine orthopedist, especially when the patient is younger than 10. Referral is also recommended when the curve is left thoracic, or if any abnormal physical findings or a positive family history is present.4,5,7 There is also support for a strategy in which the practitioner closely observes the patient older than 10 with scoliosis but no other abnormalities, then refers the child once the curve reaches 20° to 25°.7 Referral within three months is most likely indicated for those with typical scoliosis and within one month for atypical scoliosis.7
Each practitioner will develop his or her own comfort level in the management of idiopathic scoliosis. Once a referral has been made, the practitioner should follow up to be sure the patient has seen the specialist in a timely fashion, with no appointments missed. Curve progression can develop rapidly, possibly making treatment more difficult once it begins.
TREATMENT
Three main types of treatment are provided for scoliosis: observation, bracing, and surgery.3,5,7 Observation is generally considered sufficient for immature patients whose curves measure less than 25°; usually no treatment will be needed for mature patients with curves less than 25°. Depending on risk stratification, children will initially need serial radiographs every four to six months.2
Most children will be seen by an orthopedist at this point.2,3,22 Oftentimes orthopedists with adult patients will order radiographs every three to five years to be sure the scoliosis has not progressed.3 Treatment of children with neuromuscular or syndrome-related scoliosis is lengthy and will not be addressed in this review.
Orthotic management (bracing or casting) is usually started once the immature patient's curve is between 25° and 45°. Brace treatment is not used to alter or correct scoliosis, but rather to halt its progression until the patient is skeletally mature (more common), a spinal fusion occurs (less common), or both.5 A 20% to 24% risk for eventual surgery has been reported in patients treated with braces.25,33 In infants or young children with congenital (or other) scoliosis, several temporary management options can be used to prevent curve progression while allowing the child's thorax to grow and expand.2
Several surgical interventions are appropriate for scoliosis. For infants or young children, one surgical intervention is the vertical expandable prosthetic titanium rib (VEPTRTM [Synthes, Inc, West Chester, Pennsylvania]). This is a longitudinal rib distraction device that can attach from rib to rib, rib to spine, or rib to pelvis. The device is indicated in the presence of a constrictive chest wall syndrome, which can decrease lung volumes and cause severe deformity if untreated. The device is lengthened every 4 to 6 months, with the goal to delay a final fusion until skeletal maturity.2
The growing rod, a comparable temporary device, is inserted spine to spine and lengthened similarly at various intervals. Growing rods are usually used in older children with scoliosis who await maturity before undergoing a definitive spinal fusion.2
A newer surgical procedure being used at Morgan Stanley Children's Hospital of NewYork-Presbyterian is spinal stapling.34 This involves minimally invasive surgery to implant inch-long staples across the spinal growth plates, which can stop scoliosis from worsening, or even correct the curve.
Spinal fusion with instrumentation, though used in less than 5% of patients with AIS, is considered the definitive surgical treatment for scoliosis.6 Surgical correction is almost always deemed necessary in immature patients with curves greater than 45° and mature patients with curves greater than 50°.3,7,22 The fusion may involve posterior (and sometimes anterior) discectomy and/or bone grafting between the involved vertebrae to help the bones fuse together so that curves cannot progress. The instrumentation (rods, hooks, wires, and/or screws) is used simply to maintain the spine in the best possible position until the actual fusion occurs; this can take months to a year.2,5,7
Risks and benefits of spinal fusion must be thoroughly reviewed with each parent and patient. The reported neurologic injury and mortality rates are less than 1% and less than 0.02%, respectively, in patients with idiopathic scoliosis who undergo the surgery.7 There is an increased incidence of such concerns in patients with other types of scoliosis, given their comorbid issues.35
Alternative treatments such as physical therapy, yoga, massage, acupuncture, and chiropractic medicine do not put patients at risk, and some have found them beneficial.3
EDUCATION
Both patient and parent must be acquainted with the goal of scoliosis diagnosis and treatment: to prevent curve progression, altered body image, and, ultimately, morbidity. Screening, history, examination, and radiographs are important first steps, with the information gained determining when referral to a pediatric spine orthopedist/specialist (if possible) should be made. Once curves reach 25° to 30°, bracing can successfully prevent curve progression; it will not correct the scoliosis.7 Teens who are resistant or reluctant to wear their brace must be made to understand the consequences of not following the treatment regimen, and the clinician's encouragement is essential.
Patients should be encouraged to stay active, with special emphasis on flexibility. Generally, there is no contraindication regarding activities or sports, unless the patient has undergone a surgical procedure; in this case, the practitioner will determine the patient's optimal level of participation in physical activities.
Surgical treatment with fusion and instrumentation is the only proven scoliosis treatment to correct curves (fully or partially) and prevent progression.3,5,7 Curves that reach 50° without treatment in the fully mature individual may continue to worsen into adulthood.
For patients with scoliosis having a possible familial and/or genetic component,2,3,7 there are several Web sites for patients and parents (see Table 4). Some of these address alternative therapy options.
CONCLUSION
Scoliosis is common, but the sequelae of idiopathic scoliosis can be minimized if the condition is diagnosed early and measures to prevent curve progression are initiated in a timely fashion. The key to diagnosing associated comorbid disorders and other related issues is to conduct a thorough patient and family history and complete physical examination. Timely radiographs are warranted in any patient with a positive finding. Ordering appropriate radiographs accurately is essential to facilitate patient care while reducing radiation exposure. Each practitioner must determine his or her level of comfort in managing patients with idiopathic scoliosis or immediately referring the patient once the diagnosis is made. Early referral is best in the primary care practice.
A majority of practitioners will at some time encounter scoliosis, the most common spinal deformity seen in pediatric practice.1 This musculoskeletal condition can be found incidentally during routine exams, in the urgent care setting, in the emergency department (ED), or on chest x-rays or other radiographs. In primary care, scoliosis may be overlooked, particularly when the etiology is idiopathic or when well-child visits or routine back exams have been missed.1
The focus of this review will be on early identification of affected patients (most commonly those with adolescent idiopathic scoliosis), with emphasis on evaluation through an excellent physical examination and ordering of appropriate radiographs. Watchful waiting and monitoring are the norm; however, implementing carefully selected treatment options, such as bracing, or making an appropriate referral may make it possible to slow or stop curve progression.1-4
SCOLIOSIS: THE DEFINITION
Scoliosis is a coronal curvature (lateral deviation of the spine) of more than 10°, usually with a rotational component.1,2 A healthy spine is straight in the frontal plane, but curved in the sagittal plane. Normal circumstances include thoracic kyphosis (outward curve of the upper back) and lumbar lordosis (inward curve of the lower back).5 The scoliotic spine deviates away from the midline, and maximal rotation is at the apex of the curve. The apex or point of the curve defines its center, that is, the most laterally deviated vertebra or disc. The first curve to develop is the primary curve; however, when a patient presents with two or three curves, it is difficult to determine which curve is primary.
The secondary curve is a compensatory curve, which develops as a means to balance the head and trunk over the pelvis. A similar compensation may occur in the sagittal plane, exacerbating the normal kyphosis or lordosis or possibly causing rib or scapular prominences.6 Cervical curves can also develop but are more commonly associated with conditions other than idiopathic scoliosis.3 Cervical scoliosis will not be reviewed here.
THE EPIDEMIOLOGY OF SCOLIOSIS TYPES
Eighty percent of all scoliosis patients are diagnosed with idiopathic scoliosis (which may be present in 2% to 3% of the population).1,5 The remaining 20% are diagnosed with congenital, neuromuscular, or syndrome-related spinal deformities.1 The overall prevalence of idiopathic scoliosis (with curves greater than 10°) is 1 to 3 per 100, with a comparable proportion of girls and boys. The prevalence of those with curves greater than 30° is 1 to 3 per 1,000, with a boy-girl ratio of 1:8.7 In the child who is skeletally mature, scoliosis curves measuring less than 30° usually do not progress. However, most curves greater than 50° tend to progress at about 1° per year.7
Idiopathic scoliosis is broken down into age ranges.8Infantile scoliosis is diagnosed from age 0 to 3 years and comprises 0.5% of cases; juvenile scoliosis, with an age range of 4 to 9 years, represents 10.5% of cases; and adolescent scoliosis, diagnosed any time after age 10, accounts for 89% of cases.7 The four main types of scoliosis will be discussed.
Congenital
Congenital scoliosis is defined as a malformed or segmented portion of the spine, a failure of formation of a portion of the spine, or a combination of the two.9 This results in block vertebrae or hemivertebrae, or possibly the fusing of two vertebrae with a bony bridge. Because the associated curves are often rigid, they can be resistant to correction. Worldwide, prevalence of congenital vertebral anomalies is 0.5 to 1.0 per 1,000 live births.10
Congenital scoliosis can be associated with many other congenital abnormalities, as embryonic development of the spine occurs at the same time as that of the heart, kidneys, bowel, and bladder.1 Congenital scoliosis can occur with any of these defects or in the setting of a syndrome, such as VACTERL1,9-11 (ie, vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal defects, and limb abnormalities1; see Table 11,9,11,12). If even one such defect or abnormality is found, associated comorbid conditions should be actively sought.1
In many instances, these abnormalities are noted when children are young; in children younger than 5 years, MRI is warranted, and these patients almost always need sedation during imaging. In the young child who also exhibits urologic issues, an MRI work-up for genitourinary defects can be performed at the same time.1
Patients with abnormal cardiac findings (eg, heart murmur) should be referred for a cardiology work-up.11,13 Chest wall deformities may also be present in children with congenital scoliosis. Multiple congenital rib fusions can cause chest wall constriction, possibly inhibiting growth and lung development. Untreated, this condition can ultimately shorten a child’s lifespan.14
Neuromuscular
Spinal curvature in a patient with a neuromuscular disease is referred to as neuromuscular scoliosis (see Table 2).1,4,5 Most diagnoses within this category are genetic in nature, although some can result from a traumatic brain injury and/or anoxia (eg, cerebral palsy). Given that this disease state is detected early in most patients’ lives, they are generally followed by an orthopedist (or more specifically, by a pediatric orthopedist) once necessary testing, such as radiography or MRI, has been completed.1,15
Syndrome-related
Patients may have certain genetic conditions or syndromes that put them at high risk for scoliosis.
The two conditions most commonly associated with scoliosis are Marfan syndrome (60%) and neurofibromatosis (10% to 15%).1 Many patients in both groups will require MRI for evaluation; given that they are at high risk for lumbar spondylolisthesis (slippage between two lumbar vertebrae), care should be taken to evaluate for this possible secondary finding.16,17 It should be noted that patients with Marfan syndrome are at high risk for cardiac abnormalities, and those with neurofibromatosis, for dural ectasia and/ or Chiari malformations (which would be detected by MRI).16,18
Patients who have undergone chest wall surgery, such as thoracotomy for congenital heart defect repair, should be evaluated for scoliosis. The incidence of scoliosis is elevated in patients with heart defects, and the association is even greater in those who have had chest wall surgery, especially before age 18 months.19
IDIOPATHIC SCOLIOSIS
Because, by definition, no cause is known, idiopathic scoliosis is considered a diagnosis of exclusion. Affected patients have a normal neurologic exam and usually have no presenting symptoms or evidence of spinal abnormalities.1 Since 1954, idiopathic scoliosis has been divided into three age-groups, as these periods correspond to phases of increased growth velocity that occur during childhood and adolescence.8,20
Infant
A diagnosis of early-onset scoliosis is made when a child presents with scoliosis before age 5; any affected child between 0 and 3 years of age may be included in the infant scoliosis classification.2 All congenital, neuromuscular, and syndrome-related causes will have been excluded. It is felt among many experts that there is always a genetic or familial component to scoliosis. Therefore, when a child's family history is positive for scoliosis, the child should be aggressively screened, and the family should be educated to observe for signs of scoliosis and seek practitioner involvement as soon as any are evident.2
A thorough examination should be completed to rule out organ involvement in the presence of infant scoliosis.1 It is recommended that any infant with scoliotic curves greater than 20° undergo MRI of the head and spine to rule out central nervous system lesions or structural abnormalities. The risk for respiratory failure-related morbidity and mortality is increased in children with untreated early-onset scoliosis who experience curve progression. Rare progressive curves often can be addressed surgically, preserving spine and trunk growth while also achieving curve correction.2
In the majority of cases of infant scoliosis (75% to 90%), curves are left-sided (levoscoliosis)—in contrast to the right-sided curves (dextroscoliosis) more commonly noted in late-onset (juvenile or adolescent) scoliosis3,21 (see Figure 1). Infant scoliosis is slightly more common in boys (60%) than in girls.21
Neither curve lateralization nor gender makes a difference in treatment.2 Approximately 90% of early-onset curves resolve spontaneously, especially in those who are diagnosed before age 1 year. Progression occurring at a rate of 2° to 3° per year is considered gradual, whereas malignant progression often worsens by 10° or more per year, with the condition possibly becoming severe and disabling.2,21
Any infant given a diagnosis of scoliosis by a practitioner other than a pediatric orthopedist should be referred as soon as possible. On referral, copies of previously obtained radiographs and/or MRI should be presented or sent to the orthopedic practitioner, along with the history and physical exam findings, to avoid the need for repeated imaging.
Juvenile
Juvenile idiopathic scoliosis is diagnosed in patients between ages 4 and 9. Presentation in younger members of this age-group tends to resemble that in infantile idiopathic scoliosis, and children in the middle to upper age range tend to present as adolescent patients do.3 Most juvenile patients' curves will resolve without treatment (especially younger children's).
It is recommended that children with juvenile idiopathic scoliosis undergo MRI to rule out brain or spinal abnormalities. In up to 20% of children younger than 10 with curves exceeding 20°, findings on MRI are abnormal.3 Observation with close monitoring of curve progression is key in this population, especially if rapid progression is evident. In children with juvenile idiopathic scoliosis and rapid-onset curve progression, severe trunk deformity or pulmonary and/or cardiac compromise can develop. Curves that reach 30° almost always continue to worsen unless treatment is given.3,7 Timely referral to a pediatric spine orthopedist is warranted for children in this age-group.
Adolescent
It is during adolescence (ages 10 to 18) that idiopathic scoliosis is most common. Approximately 2% to 3% of children ages 10 to 15 have scoliosis with a curve of at least 10°. Among these patients, however, just 5% have scoliosis of clinical significance to warrant treatment (ie, curve progression > 30°).5,22
Each child should be examined initially for nonstructural scoliosis. This includes postural scoliosis, which resolves when a child is recumbent; compensatory scoliosis, which can be the result of a leg-length discrepancy (with no fixed vertebral rotation); sciatic scoliosis, an abnormality that results from avoiding the pain of an irritated sciatic nerve; inflammatory scoliosis, which could result from an infectious process, such as acute appendicitis; and hysterical scoliosis, a very rare form with an underlying psychological factor.4
Structural scoliosis comprises the remaining types of scoliosis, including the idiopathic variety. Patients with adolescent idiopathic scoliosis (AIS) are older than 10 and usually undergoing a rapid growth phase. Thus, some adolescent patients' curves can progress rapidly.4
Adolescents with idiopathic scoliosis rarely complain of pain or neurologic symptoms. Generally, their spinal curves do not cause organ pressure or shortness of breath. Many patients with AIS are involved in extracurricular activities that can trigger low back pain, yet activity-related low back pain is not an uncommon complaint among teens in general. Therefore, it is felt that when a patient with AIS has intermittent low back pain, it is most likely not related to their curve(s). Nevertheless, if a patient with AIS develops continued or unexplained low back pain and/or new neurologic symptoms, MRI is warranted.3
HISTORY, PHYSICAL EXAMINATION, AND DIAGNOSIS
During the exam, elicit any family history of scoliosis, especially in the setting of known diseases, such as Marfan syndrome, neurofibromatosis, muscular dystrophy, or other related diseases. Approximately 30% of AIS patients have a family history of scoliosis, so although the cause may not be clear, some genetic component is possible.3 The examination should stem from the patient's current stage of growth and development (see Table 31,3,4,7,23). The diagnosis of scoliosis is typically made during the examination and confirmed by radiography.
The newborn patient should be kept warm but be wearing only a diaper during the exam. A child or adolescent should be undressed and wearing a patient gown (unless at a school screening).
A general observation should be done initially, including the child's overall shape. The examiner should look for marfanoid features, such as excessive height, long arms, long trunk, and joint laxity.7 In the examination of the feet, an extremely high arch or cavus foot may be indicative of tethered spinal cord, spinal syrinx, or Charcot-Marie-Tooth disease, especially if the cavus is unilateral.1,7,23 MRI would be warranted in these instances.1
The examining clinician should note the child's Tanner stage. Height and weight measurements should be taken, and for a girl, age at menarche should be recorded.4
Next, the skin should be carefully inspected. In the infant, the examiner should look for hairy patches at the base of the spine, cutaneous sinuses, sacral dimpling, or other skin lesions that may suggest spinal dysraphism (ie, failure of the posterior elements to fuse around the spinal cord).4 Examination for café au lait spots and/or freckling in the axilla or groin area should be included, as this could signify neurofibromatosis.1,4,7
Examine the back in a standing child. Note whether the head appears to be centered over the sacrum. Evaluate for shoulder height or truncal asymmetry, scapular or posterior rib prominence, and excessive thoracic kyphosis and/or lumbar lordosis. Examine the pelvic bones, looking for obliquity (ie, one side higher than the other). Look for leg length discrepancy, both while the patient is standing still and during a gait review.1
During an anterior exam, look for shoulder or truncal asymmetry, leg length discrepancy, and anterior rib prominence. If shoulder height asymmetry is apparent, measure from each acromioclavicular joint to the floor and note the difference in centimeters. In the case of pelvic obliquity, measure from each anterior (or posterior) superior iliac spine to the floor and note the difference in centimeters. If the head does not appear to align over the sacrum, lower a plum line from the spinous process of C7 down to the gluteal cleft level. Measure by centimeters the distance from the cleft to the line, noting the side to which the line sways.
View the patient from the side. The sagittal curve can be assessed from the occiput to the sacrum; observe for an increased lordotic or kyphotic curve or abnormal positioning related to abnormal curves.4
The Adams forward bend test should be conducted.24,25 The child who is able to stand faces away from the examiner, then bends forward at the waist with the knees straight and the arms hanging down passively (see Figure 2). The practitioner looks at the spine from behind and notes any rib, thoracic, scapular, or lumbar prominence that could indicate a rotational spine deformity.1,4,7 In some instances, the use of a scoliometer can be helpful to assign a number to the amount of rotation to the spine during the Adams forward bend test. However, primary care offices are not often equipped with this device.26
Motor and Neurologic Examinations
The motor exam includes testing motor strength in all four extremities and noting any asymmetry. The examiner should have the child actively bend in every direction, making note of any deformity, stiffness, or asymmetry. The patient's spine should be palpated, with any tenderness noted, and any available radiographs reviewed.1,4,7
The neurologic exam includes testing cranial nerves, sensation, and reflexes, including the patellar, Achilles, and umbilical reflexes, as well as Babinski's sign. Many patients are areflexic in one or more areas. For instance, a finding of no umbilical (abdominal wink) reflex on either side is not suspicious in itself, but it should alert the practitioner to evaluate carefully for asymmetrical reflexes in one or more areas, especially if they are ipsilateral. Any positive neurologic findings, especially in the setting of scoliosis, warrant an MRI.1,7
Scoliosis Screening in the School Setting
One controversial subject related to scoliosis is school screenings. These screenings were developed in the 1980s for early identification of children with scoliosis curves so that nonsurgical treatment could be initiated promptly, or that surgery, when deemed necessary, could be performed in a timely fashion for optimal results.27
Since then, the effectiveness of screening programs has come under debate; in 2004, the US Preventive Services Task Force28 issued a recommendation (rating, "D Recommendation") against routine screening for idiopathic scoliosis in asymptomatic adolescents, stating that its effectiveness had not been shown in clinical trials. In response, a task force was convened by the American Academy of Orthopaedic Surgeons, the Scoliosis Research Society, the Pediatric Orthopaedic Society of North America, and the American Academy of Pediatrics, with findings published in a 2008 information statement by Richards and Vitale.25 While acknowledging the limitations of support for screening in the literature, the task force concluded:
- Early treatment of the deformities associated with idiopathic scoliosis can result in substantial benefits
- Screening (whether in the school environment or other settings) offers an opportunity for early diagnosis and appropriate referral of otherwise undetected deformities, especially in under-served populations
- In many cases, brace treatment may preclude the need for surgery in children with significant scoliosis
- Identifying deformities that require surgery as early as possible through screening increases the likelihood of good treatment outcomes
- Girls, who reach adolescence two years earlier than boys, should be screened at ages 10 and 12; boys, at age 13 or 14
- School personnel who conduct screening should receive training to detect spinal deformities
- While no screening test is entirely reliable, the forward bend test is considered the most specific test for detection of scoliosis29
- The participating organizations remain committed to preventing inappropriate use of spinal x-rays.25
Despite the ongoing debate, more than half of the US states have screening programs in place.24,27
RADIOGRAPHS/LABORATORY TESTING
Physical examination and a thorough history are most important in evaluation for scoliosis in the primary care setting. When radiographs (x-rays) are considered necessary, posterior-anterior and lateral spine series should be ordered. These are full-length (3-ft)
x-rays of the patient standing with the knees straight (when the child is able to do so).1,4,7 The x-rays are taken in the posterior-anterior direction to minimize breast and organ radiation exposure and to produce an x-ray similar to that of viewing the patient from behind.
If scoliosis is observed on radiography, note the apex of the curve, the location, the direction in which it curves, and any rotational component. Examine for pelvic obliquity, shoulder asymmetry, spondylosis, or spondylolisthesis.7
The Cobb angle is the measurement used to quantify the degree of scoliosis.4,5,7 Using the posterior-anterior radiograph, a line is drawn along the superior endplate of the most curved cephalad vertebra and the inferior endplate of the caudal vertebra. When perpendicular lines are drawn, the intersecting lines form the Cobb angle (see Figure 3, in which "X" indicates the Cobb angle, measured in degrees). An increasing angle reflects the increasing severity of scoliosis.
Other radiographs that may be ordered include supine lateral (bending) x-rays or supine traction radiographs to evaluate curve flexibility before surgery30; recently, hanging total spine x-rays have been investigated to evaluate spine flexibility before brace treatment.31 Additionally, hand/wrist x-rays may be ordered to determine the patient's remaining growth potential. These are most often taken in an orthopedist's office.3
If a diagnosis of scoliosis is made, Risser staging should be completed. Risser sign is a growth marker noted in adolescents by viewing iliac apophyseal ossification on radiograph. The progress of bone fusion over the iliac apophysis reflects remaining skeletal growth and is graded from 0 to 5, with 0 representing no ossification of the iliac apophysis and 5, complete ossification. The lower the grade noted at curve detection, the greater the risk for curve progression.3,4
Other tests may be warranted. If a patient has persistent back or side pain, especially pain that wakens the patient at night, and/ or pain not relieved by aspirin or NSAIDs, then a bone scan should be ordered to rule out discitis, rib or spine osteoid osteoma, spinal or intradural tumors, osteomyelitis, or other abnormalities.7 An MRI is warranted in children younger than 10; those who have left-sided curves, headaches, or neck pain; patients with quickly progressing curves; and those with any abnormality on neurologic exam. This test is generally not necessary in those with AIS if no family history is present and physical exam findings are unremarkable.1,2,5,7 Laboratory tests are generally not ordered for patients with idiopathic scoliosis unless inflammatory or infectious processes are suspected; standard laboratory tests would then follow. The ScoliScoreTM (Axial Biotech, Salt Lake City), a newer genetic screening test, can be used along with clinical and radiographic testing in patients with AIS. It is felt that specific genes are associated with AIS, and this test may help detect them and determine any associated risk for curve progression.1,3
There are several genetic tests for conditions associated with congenital neuromuscular or syndrome-related scoliosis.12,32 These may be ordered by the primary care provider, an orthopedist, or the geneticist.
REFERRAL
According to some researchers, any child with scoliosis greater than 10° should be referred to an orthopedist, preferably a pediatric spine orthopedist, especially when the patient is younger than 10. Referral is also recommended when the curve is left thoracic, or if any abnormal physical findings or a positive family history is present.4,5,7 There is also support for a strategy in which the practitioner closely observes the patient older than 10 with scoliosis but no other abnormalities, then refers the child once the curve reaches 20° to 25°.7 Referral within three months is most likely indicated for those with typical scoliosis and within one month for atypical scoliosis.7
Each practitioner will develop his or her own comfort level in the management of idiopathic scoliosis. Once a referral has been made, the practitioner should follow up to be sure the patient has seen the specialist in a timely fashion, with no appointments missed. Curve progression can develop rapidly, possibly making treatment more difficult once it begins.
TREATMENT
Three main types of treatment are provided for scoliosis: observation, bracing, and surgery.3,5,7 Observation is generally considered sufficient for immature patients whose curves measure less than 25°; usually no treatment will be needed for mature patients with curves less than 25°. Depending on risk stratification, children will initially need serial radiographs every four to six months.2
Most children will be seen by an orthopedist at this point.2,3,22 Oftentimes orthopedists with adult patients will order radiographs every three to five years to be sure the scoliosis has not progressed.3 Treatment of children with neuromuscular or syndrome-related scoliosis is lengthy and will not be addressed in this review.
Orthotic management (bracing or casting) is usually started once the immature patient's curve is between 25° and 45°. Brace treatment is not used to alter or correct scoliosis, but rather to halt its progression until the patient is skeletally mature (more common), a spinal fusion occurs (less common), or both.5 A 20% to 24% risk for eventual surgery has been reported in patients treated with braces.25,33 In infants or young children with congenital (or other) scoliosis, several temporary management options can be used to prevent curve progression while allowing the child's thorax to grow and expand.2
Several surgical interventions are appropriate for scoliosis. For infants or young children, one surgical intervention is the vertical expandable prosthetic titanium rib (VEPTRTM [Synthes, Inc, West Chester, Pennsylvania]). This is a longitudinal rib distraction device that can attach from rib to rib, rib to spine, or rib to pelvis. The device is indicated in the presence of a constrictive chest wall syndrome, which can decrease lung volumes and cause severe deformity if untreated. The device is lengthened every 4 to 6 months, with the goal to delay a final fusion until skeletal maturity.2
The growing rod, a comparable temporary device, is inserted spine to spine and lengthened similarly at various intervals. Growing rods are usually used in older children with scoliosis who await maturity before undergoing a definitive spinal fusion.2
A newer surgical procedure being used at Morgan Stanley Children's Hospital of NewYork-Presbyterian is spinal stapling.34 This involves minimally invasive surgery to implant inch-long staples across the spinal growth plates, which can stop scoliosis from worsening, or even correct the curve.
Spinal fusion with instrumentation, though used in less than 5% of patients with AIS, is considered the definitive surgical treatment for scoliosis.6 Surgical correction is almost always deemed necessary in immature patients with curves greater than 45° and mature patients with curves greater than 50°.3,7,22 The fusion may involve posterior (and sometimes anterior) discectomy and/or bone grafting between the involved vertebrae to help the bones fuse together so that curves cannot progress. The instrumentation (rods, hooks, wires, and/or screws) is used simply to maintain the spine in the best possible position until the actual fusion occurs; this can take months to a year.2,5,7
Risks and benefits of spinal fusion must be thoroughly reviewed with each parent and patient. The reported neurologic injury and mortality rates are less than 1% and less than 0.02%, respectively, in patients with idiopathic scoliosis who undergo the surgery.7 There is an increased incidence of such concerns in patients with other types of scoliosis, given their comorbid issues.35
Alternative treatments such as physical therapy, yoga, massage, acupuncture, and chiropractic medicine do not put patients at risk, and some have found them beneficial.3
EDUCATION
Both patient and parent must be acquainted with the goal of scoliosis diagnosis and treatment: to prevent curve progression, altered body image, and, ultimately, morbidity. Screening, history, examination, and radiographs are important first steps, with the information gained determining when referral to a pediatric spine orthopedist/specialist (if possible) should be made. Once curves reach 25° to 30°, bracing can successfully prevent curve progression; it will not correct the scoliosis.7 Teens who are resistant or reluctant to wear their brace must be made to understand the consequences of not following the treatment regimen, and the clinician's encouragement is essential.
Patients should be encouraged to stay active, with special emphasis on flexibility. Generally, there is no contraindication regarding activities or sports, unless the patient has undergone a surgical procedure; in this case, the practitioner will determine the patient's optimal level of participation in physical activities.
Surgical treatment with fusion and instrumentation is the only proven scoliosis treatment to correct curves (fully or partially) and prevent progression.3,5,7 Curves that reach 50° without treatment in the fully mature individual may continue to worsen into adulthood.
For patients with scoliosis having a possible familial and/or genetic component,2,3,7 there are several Web sites for patients and parents (see Table 4). Some of these address alternative therapy options.
CONCLUSION
Scoliosis is common, but the sequelae of idiopathic scoliosis can be minimized if the condition is diagnosed early and measures to prevent curve progression are initiated in a timely fashion. The key to diagnosing associated comorbid disorders and other related issues is to conduct a thorough patient and family history and complete physical examination. Timely radiographs are warranted in any patient with a positive finding. Ordering appropriate radiographs accurately is essential to facilitate patient care while reducing radiation exposure. Each practitioner must determine his or her level of comfort in managing patients with idiopathic scoliosis or immediately referring the patient once the diagnosis is made. Early referral is best in the primary care practice.
1. Horan MP, Milbrandt TA. Scoliosis in pediatric patients: comorbid disorders and screening. Pediatr Health. 2009;3(5):451-456.
2. Debnath UK. Current concepts in the management of early-onset idiopathic scoliosis. Pediatr Health. 2010;4(3):343-354.
3. Scoliosis Research Society. Idiopathic scoliosis. www.srs.org/patient_and_family/scoliosis/idiopathic. Accessed July 19, 2012.
4. Taft E, Francis R. Evaluation and management of scoliosis. J Pediatr Health Care. 2003;17(1):42- 44.
5. Speigel DA, Sarwark JF. Pediatric orthopaedics. In: Sarwark JF, ed. Essentials of Musculoskeletal Care. 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010:976-1201.
6. Horn PL, Beebe AC. Scoliosis: incidence and current medical and surgical interventions. Heartbeat. 2008;19(3):6-7,17.
7. Janicki JA. Scoliosis. In: Miller MD, Hart JA, MacKnight JM. Essential Orthopaedics. Marietta, GA: Saunders/Elsevier; 2010:881-886.
8. James JIP. Idiopathic scoliosis; the prognosis, diagnosis, and operative indications related to curve patterns and the age at onset. J Bone Joint Surg Br. 1954;36-B(1):36-49.
9. Scoliosis. In: Herring JA. Tachdjian's Pediatric Orthopaedics. Vol I. 4th ed. Philadelphia, PA: Saunders/Elsevier; 2008:265-411.
10. Debnath UK, Goel V, Harshavarfhana N, Webb JK. Congenital scoliosis - Quo vadis? Indian J Orthop. 2010;44(2):137-147.
11. Basu PS, Elsebaie H, Noordeen MH. Congenital spine deformity: a comprehensive assessment at presentation. Spine (Phila Pa 1976). 2002;27(20):2255-2259.
12. Fisher K, Esham RH, Thorneycroft I. Scoliosis associated with typical Mayer-Rokitansky-Küster-Hauser syndrome. South Med J. 2000;93(2):243-246.
13. Hedequist D, Emans J. Congenital scoliosis: a review and update. J Pediatr Orthop. 2007;27(1):106-116.
14. Pehrsson K, Larsson S, Oden A, Nachemson A. Long-term follow-up of patients with untreated scoliosis: a study of mortality, causes of death, and symptoms. Spine (Phila Pa 1976). 1992;17(9):1091-1096.
15. Ferguson RL. Medical and congenital comorbidities associated with spinal deformities in the immature spine. J Bone Joint Surg Am. 2007;89(suppl 1):34-41.
16. Demetracopoulos CA, Sponseller PD. Spinal deformities in Marfan syndrome. Orthop Clin North Am. 2007;38(4):563-572.
17. Crawford AH, Herrera-Soto J. Scoliosis associated with neurofibromatosis. Orthop Clin North Am. 2007;38(4):553-562.
18. Disorders of the spinal cord. In: Herring JA. Tachdjian's Pediatric Orthopaedics. Vol II. 4th ed. Philadelphia, PA: Saunders/Elsevier; 2008:1405-1482.
19. Ruiz-Iban MA, Burgos J, Aguado HJ, et al. Scoliosis after median sternotomy in children with congenital heart disease. Spine (Phila Pa 1976). 2005;30(8):E214-E218.
20. Dimeglio A. Growth of the spine before age 5 years. J Pediatr Orthop B. 1993;1:102-107.
21. Lloyd-Roberts GC, Pilcher MF. Structural idiopathic scoliosis in infancy: a study of natural history of 100 patients. J Bone Joint Surg Br. 1965;47:520-523.
22. Gutknecht S, Lonstein J, Novacheck T. Adolescent idiopathic scoliosis. Pediatric Perspective. 2009;18(4):1-4.
23. Lew SM, Kothbauer KF. Tethered cord syndrome: an updated review. Pediatr Neurosurg. 2007;43(3):236-248.
24. Bunge EM, Juttmann RE, van Biezen FC, et al; Netherlands Evaluation Study on Screening for Scoliosis (NESCIO) Group. Estimating the effectiveness of screening for scoliosis: a case-control study. Pediatrics. 2008;121(1):9-14.
25. Richards BS, Vitale MG. Screening for idiopathic scoliosis in adolescents: an information statement. J Bone Joint Surg. 2008;90(1):195-198.
26. Côté P, Kreitz BG, Cassidy JD, et al. A study of the diagnostic accuracy and reliability of the scoliometer and Adam's forward bend test. Spine. 1998;23(7):796-802.
27. Richards BS, Beaty JH, Thompson GH, Willis RB. Estimating the effectiveness of screening for scoliosis. Pediatrics. 2008:121(6):1297-1298.
28. US Preventive Services Task Force. Screening for idiopathic scoliosis in adolescents: recommendation statement (2004). www.uspreventiveservicestaskforce.org/3rduspstf/scoliosis/scoliors.htm. Accessed July 19, 2012.
29. Karachalios T, Sofianos J, Roidis N, et al. Ten-year follow-up evaluation of a school screening program for scoliosis. Is the forward-bending test an accurate diagnostic criterion for the screening of scoliosis? Spine (Phila Pa 1976). 1999;24(22):2318-2324.
30. Hamzaoglu A, Talu U, Tezer M, et al. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30(14):1627-1642.
31. Kuroki H, Inomata N, Hamanaka H, et al. Significance of hanging total spine x-ray to estimate the indicative correction angle by brace wearing in idiopathic scoliosis patients. Scoliosis. 2012;7:8.
32. Al-Otibi M, Rutka JT. Neurosurgical implications of neurofibromatosis type I in children. Neurosurg Focus. 2006;20(1):E2.
33. Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976). 2007;32(19 suppl):S91-S100.
34. American Academy of Pediatrics. New stapling treatment may help reverse scoliosis: report from the Morgan Stanley Children's Hospital Department of Pediatric Orthopaedics. Section on Orthopaedics Newsletter. Spring 2009. www2.aap.org/sections/ortho/spring2009news.pdf. Accessed July 19, 2012.
35. Reames DL, Smith JS, Fu KG, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis. Spine. 2011;36(18):1484-1491.
1. Horan MP, Milbrandt TA. Scoliosis in pediatric patients: comorbid disorders and screening. Pediatr Health. 2009;3(5):451-456.
2. Debnath UK. Current concepts in the management of early-onset idiopathic scoliosis. Pediatr Health. 2010;4(3):343-354.
3. Scoliosis Research Society. Idiopathic scoliosis. www.srs.org/patient_and_family/scoliosis/idiopathic. Accessed July 19, 2012.
4. Taft E, Francis R. Evaluation and management of scoliosis. J Pediatr Health Care. 2003;17(1):42- 44.
5. Speigel DA, Sarwark JF. Pediatric orthopaedics. In: Sarwark JF, ed. Essentials of Musculoskeletal Care. 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010:976-1201.
6. Horn PL, Beebe AC. Scoliosis: incidence and current medical and surgical interventions. Heartbeat. 2008;19(3):6-7,17.
7. Janicki JA. Scoliosis. In: Miller MD, Hart JA, MacKnight JM. Essential Orthopaedics. Marietta, GA: Saunders/Elsevier; 2010:881-886.
8. James JIP. Idiopathic scoliosis; the prognosis, diagnosis, and operative indications related to curve patterns and the age at onset. J Bone Joint Surg Br. 1954;36-B(1):36-49.
9. Scoliosis. In: Herring JA. Tachdjian's Pediatric Orthopaedics. Vol I. 4th ed. Philadelphia, PA: Saunders/Elsevier; 2008:265-411.
10. Debnath UK, Goel V, Harshavarfhana N, Webb JK. Congenital scoliosis - Quo vadis? Indian J Orthop. 2010;44(2):137-147.
11. Basu PS, Elsebaie H, Noordeen MH. Congenital spine deformity: a comprehensive assessment at presentation. Spine (Phila Pa 1976). 2002;27(20):2255-2259.
12. Fisher K, Esham RH, Thorneycroft I. Scoliosis associated with typical Mayer-Rokitansky-Küster-Hauser syndrome. South Med J. 2000;93(2):243-246.
13. Hedequist D, Emans J. Congenital scoliosis: a review and update. J Pediatr Orthop. 2007;27(1):106-116.
14. Pehrsson K, Larsson S, Oden A, Nachemson A. Long-term follow-up of patients with untreated scoliosis: a study of mortality, causes of death, and symptoms. Spine (Phila Pa 1976). 1992;17(9):1091-1096.
15. Ferguson RL. Medical and congenital comorbidities associated with spinal deformities in the immature spine. J Bone Joint Surg Am. 2007;89(suppl 1):34-41.
16. Demetracopoulos CA, Sponseller PD. Spinal deformities in Marfan syndrome. Orthop Clin North Am. 2007;38(4):563-572.
17. Crawford AH, Herrera-Soto J. Scoliosis associated with neurofibromatosis. Orthop Clin North Am. 2007;38(4):553-562.
18. Disorders of the spinal cord. In: Herring JA. Tachdjian's Pediatric Orthopaedics. Vol II. 4th ed. Philadelphia, PA: Saunders/Elsevier; 2008:1405-1482.
19. Ruiz-Iban MA, Burgos J, Aguado HJ, et al. Scoliosis after median sternotomy in children with congenital heart disease. Spine (Phila Pa 1976). 2005;30(8):E214-E218.
20. Dimeglio A. Growth of the spine before age 5 years. J Pediatr Orthop B. 1993;1:102-107.
21. Lloyd-Roberts GC, Pilcher MF. Structural idiopathic scoliosis in infancy: a study of natural history of 100 patients. J Bone Joint Surg Br. 1965;47:520-523.
22. Gutknecht S, Lonstein J, Novacheck T. Adolescent idiopathic scoliosis. Pediatric Perspective. 2009;18(4):1-4.
23. Lew SM, Kothbauer KF. Tethered cord syndrome: an updated review. Pediatr Neurosurg. 2007;43(3):236-248.
24. Bunge EM, Juttmann RE, van Biezen FC, et al; Netherlands Evaluation Study on Screening for Scoliosis (NESCIO) Group. Estimating the effectiveness of screening for scoliosis: a case-control study. Pediatrics. 2008;121(1):9-14.
25. Richards BS, Vitale MG. Screening for idiopathic scoliosis in adolescents: an information statement. J Bone Joint Surg. 2008;90(1):195-198.
26. Côté P, Kreitz BG, Cassidy JD, et al. A study of the diagnostic accuracy and reliability of the scoliometer and Adam's forward bend test. Spine. 1998;23(7):796-802.
27. Richards BS, Beaty JH, Thompson GH, Willis RB. Estimating the effectiveness of screening for scoliosis. Pediatrics. 2008:121(6):1297-1298.
28. US Preventive Services Task Force. Screening for idiopathic scoliosis in adolescents: recommendation statement (2004). www.uspreventiveservicestaskforce.org/3rduspstf/scoliosis/scoliors.htm. Accessed July 19, 2012.
29. Karachalios T, Sofianos J, Roidis N, et al. Ten-year follow-up evaluation of a school screening program for scoliosis. Is the forward-bending test an accurate diagnostic criterion for the screening of scoliosis? Spine (Phila Pa 1976). 1999;24(22):2318-2324.
30. Hamzaoglu A, Talu U, Tezer M, et al. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30(14):1627-1642.
31. Kuroki H, Inomata N, Hamanaka H, et al. Significance of hanging total spine x-ray to estimate the indicative correction angle by brace wearing in idiopathic scoliosis patients. Scoliosis. 2012;7:8.
32. Al-Otibi M, Rutka JT. Neurosurgical implications of neurofibromatosis type I in children. Neurosurg Focus. 2006;20(1):E2.
33. Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976). 2007;32(19 suppl):S91-S100.
34. American Academy of Pediatrics. New stapling treatment may help reverse scoliosis: report from the Morgan Stanley Children's Hospital Department of Pediatric Orthopaedics. Section on Orthopaedics Newsletter. Spring 2009. www2.aap.org/sections/ortho/spring2009news.pdf. Accessed July 19, 2012.
35. Reames DL, Smith JS, Fu KG, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis. Spine. 2011;36(18):1484-1491.