User login
CHICAGO – Preliminary data from a series of multiple sclerosis patients who underwent percutaneous transluminal venoplasty to treat chronic cerebrospinal venous insufficiency suggest that the treatment was safe and offered significant disease-specific and quality of life improvements.
The results of the controversial treatment on 125 patients in the series will need to be validated with future randomized, blinded, controlled trials that evaluate endovascular and surgical options, Dr. Manish Mehta said at the Vascular Annual Meeting.
The patient series follows Dr. Paolo Zamboni’s identification in 2009 of stenoses in the internal jugular veins and azygous vein of patients with MS (J. Neurol. Neurosurg. Psychiatry 2009;80:392-9).
"Dr. Zamboni’s theory has been that stasis of blood can cause reflux, and reflux can cause propagation and [can] break down the blood-brain barrier," Dr. Mehta said. The resulting microbleeds can allow red blood cells to escape into the brain matter, leading to hemosiderin deposits that can act as the inflammatory mediators of an autoimmune response, he said.
Although Dr. Zamboni, a vascular surgeon and professor of surgery at the University of Ferrara (Italy), observed a strong association between chronic cerebrospinal venous insufficiency (CCSVI) and MS, it is unclear if the relationship between CCSVI and MS is causative, or if CCSVI might play a role in the etiology of the disease.
In 2009, Dr. Zamboni also reported on a series of 65 patients who had significant improvements in functional composite scores and quality of life at 1 year (J. Vasc. Surg. 2009;50;1348-58.e1-3).
The preliminary data that Dr. Mehta presented at the meeting came from the LIBERATION study, which is designed to assess the utility of percutaneous transluminal venoplasty for individuals with CCSVI and MS. It’s a prospective, randomized, double-blind study that is currently enrolling 600 patients.
Because there is a learning curve involved with the assessment and technique, the researchers included a prospective longitudinal arm as part of the study. Dr. Mehta of the Albany (N.Y.) Medical College and the director of endovascular services for the Vascular Group PLLC, presented preliminary results on this group of patients.
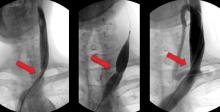
In the study, investigators performed venograms to identify stenoses of 50% or greater in internal jugular and azygous veins in the patients, all of whom underwent venoplasty. Neurologists and other clinicians evaluated the patients at baseline, and then at 1 month, 3 months, and every 6 months thereafter.
The 125 patients included in the study had a mean age of 47 years, and 62% were female. Relapsing-remitting MS accounted for 54% of the patients, followed by secondary-progressive MS in 34% and primary-progressive MS in 12%.
The patients had a total of 230 lesions altogether, 90% of which involved the internal jugular veins; the majority of these were at the origin. The remaining 10% of patients had stenoses in their azygous veins.
The mean degree of occlusion was about 80%, with approximately 1.8 lesions per patient. Immediate success (defined as less than 20% residual stenosis) occurred in 82%. The remaining patients underwent a second venoplasty without stenting.
In all, 79 patients were available for follow-up at a mean of 4.5 years. Restenosis of 50% occurred in eight of these patients, occlusions occurred in two patients, and one patient had new-onset atrial fibrillation.
The investigators reassessed 48 patients with the EDSS (Extended Disability Status Scale) following initial baseline testing. From before to after the procedure, "there was a statistical improvement. Improvements occurred in each of the MS types, except in primary progressive MS," Dr. Mehta said.
Reevaluations of 79 patients who performed a timed 25-foot walk at baseline showed a significant improvement in walking speed. In terms of MS quality of life, from before to after the procedure "there were significant improvements in physical and mental ability. There clearly seems to be a trend. In the modified fatigue impact score, there also seems to be a clear improvement," he said.
Dr. Mehta also said that there was a trend toward improvement in balance, lower-extremity weakness, incontinence, coordination, and vertigo in more than 80% of patients.
Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.
CHICAGO – Preliminary data from a series of multiple sclerosis patients who underwent percutaneous transluminal venoplasty to treat chronic cerebrospinal venous insufficiency suggest that the treatment was safe and offered significant disease-specific and quality of life improvements.
The results of the controversial treatment on 125 patients in the series will need to be validated with future randomized, blinded, controlled trials that evaluate endovascular and surgical options, Dr. Manish Mehta said at the Vascular Annual Meeting.
The patient series follows Dr. Paolo Zamboni’s identification in 2009 of stenoses in the internal jugular veins and azygous vein of patients with MS (J. Neurol. Neurosurg. Psychiatry 2009;80:392-9).
"Dr. Zamboni’s theory has been that stasis of blood can cause reflux, and reflux can cause propagation and [can] break down the blood-brain barrier," Dr. Mehta said. The resulting microbleeds can allow red blood cells to escape into the brain matter, leading to hemosiderin deposits that can act as the inflammatory mediators of an autoimmune response, he said.
Although Dr. Zamboni, a vascular surgeon and professor of surgery at the University of Ferrara (Italy), observed a strong association between chronic cerebrospinal venous insufficiency (CCSVI) and MS, it is unclear if the relationship between CCSVI and MS is causative, or if CCSVI might play a role in the etiology of the disease.
In 2009, Dr. Zamboni also reported on a series of 65 patients who had significant improvements in functional composite scores and quality of life at 1 year (J. Vasc. Surg. 2009;50;1348-58.e1-3).
The preliminary data that Dr. Mehta presented at the meeting came from the LIBERATION study, which is designed to assess the utility of percutaneous transluminal venoplasty for individuals with CCSVI and MS. It’s a prospective, randomized, double-blind study that is currently enrolling 600 patients.
Because there is a learning curve involved with the assessment and technique, the researchers included a prospective longitudinal arm as part of the study. Dr. Mehta of the Albany (N.Y.) Medical College and the director of endovascular services for the Vascular Group PLLC, presented preliminary results on this group of patients.
In the study, investigators performed venograms to identify stenoses of 50% or greater in internal jugular and azygous veins in the patients, all of whom underwent venoplasty. Neurologists and other clinicians evaluated the patients at baseline, and then at 1 month, 3 months, and every 6 months thereafter.
The 125 patients included in the study had a mean age of 47 years, and 62% were female. Relapsing-remitting MS accounted for 54% of the patients, followed by secondary-progressive MS in 34% and primary-progressive MS in 12%.
The patients had a total of 230 lesions altogether, 90% of which involved the internal jugular veins; the majority of these were at the origin. The remaining 10% of patients had stenoses in their azygous veins.
The mean degree of occlusion was about 80%, with approximately 1.8 lesions per patient. Immediate success (defined as less than 20% residual stenosis) occurred in 82%. The remaining patients underwent a second venoplasty without stenting.
In all, 79 patients were available for follow-up at a mean of 4.5 years. Restenosis of 50% occurred in eight of these patients, occlusions occurred in two patients, and one patient had new-onset atrial fibrillation.
The investigators reassessed 48 patients with the EDSS (Extended Disability Status Scale) following initial baseline testing. From before to after the procedure, "there was a statistical improvement. Improvements occurred in each of the MS types, except in primary progressive MS," Dr. Mehta said.
Reevaluations of 79 patients who performed a timed 25-foot walk at baseline showed a significant improvement in walking speed. In terms of MS quality of life, from before to after the procedure "there were significant improvements in physical and mental ability. There clearly seems to be a trend. In the modified fatigue impact score, there also seems to be a clear improvement," he said.
Dr. Mehta also said that there was a trend toward improvement in balance, lower-extremity weakness, incontinence, coordination, and vertigo in more than 80% of patients.
Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.
CHICAGO – Preliminary data from a series of multiple sclerosis patients who underwent percutaneous transluminal venoplasty to treat chronic cerebrospinal venous insufficiency suggest that the treatment was safe and offered significant disease-specific and quality of life improvements.
The results of the controversial treatment on 125 patients in the series will need to be validated with future randomized, blinded, controlled trials that evaluate endovascular and surgical options, Dr. Manish Mehta said at the Vascular Annual Meeting.
The patient series follows Dr. Paolo Zamboni’s identification in 2009 of stenoses in the internal jugular veins and azygous vein of patients with MS (J. Neurol. Neurosurg. Psychiatry 2009;80:392-9).
"Dr. Zamboni’s theory has been that stasis of blood can cause reflux, and reflux can cause propagation and [can] break down the blood-brain barrier," Dr. Mehta said. The resulting microbleeds can allow red blood cells to escape into the brain matter, leading to hemosiderin deposits that can act as the inflammatory mediators of an autoimmune response, he said.
Although Dr. Zamboni, a vascular surgeon and professor of surgery at the University of Ferrara (Italy), observed a strong association between chronic cerebrospinal venous insufficiency (CCSVI) and MS, it is unclear if the relationship between CCSVI and MS is causative, or if CCSVI might play a role in the etiology of the disease.
In 2009, Dr. Zamboni also reported on a series of 65 patients who had significant improvements in functional composite scores and quality of life at 1 year (J. Vasc. Surg. 2009;50;1348-58.e1-3).
The preliminary data that Dr. Mehta presented at the meeting came from the LIBERATION study, which is designed to assess the utility of percutaneous transluminal venoplasty for individuals with CCSVI and MS. It’s a prospective, randomized, double-blind study that is currently enrolling 600 patients.
Because there is a learning curve involved with the assessment and technique, the researchers included a prospective longitudinal arm as part of the study. Dr. Mehta of the Albany (N.Y.) Medical College and the director of endovascular services for the Vascular Group PLLC, presented preliminary results on this group of patients.
In the study, investigators performed venograms to identify stenoses of 50% or greater in internal jugular and azygous veins in the patients, all of whom underwent venoplasty. Neurologists and other clinicians evaluated the patients at baseline, and then at 1 month, 3 months, and every 6 months thereafter.
The 125 patients included in the study had a mean age of 47 years, and 62% were female. Relapsing-remitting MS accounted for 54% of the patients, followed by secondary-progressive MS in 34% and primary-progressive MS in 12%.
The patients had a total of 230 lesions altogether, 90% of which involved the internal jugular veins; the majority of these were at the origin. The remaining 10% of patients had stenoses in their azygous veins.
The mean degree of occlusion was about 80%, with approximately 1.8 lesions per patient. Immediate success (defined as less than 20% residual stenosis) occurred in 82%. The remaining patients underwent a second venoplasty without stenting.
In all, 79 patients were available for follow-up at a mean of 4.5 years. Restenosis of 50% occurred in eight of these patients, occlusions occurred in two patients, and one patient had new-onset atrial fibrillation.
The investigators reassessed 48 patients with the EDSS (Extended Disability Status Scale) following initial baseline testing. From before to after the procedure, "there was a statistical improvement. Improvements occurred in each of the MS types, except in primary progressive MS," Dr. Mehta said.
Reevaluations of 79 patients who performed a timed 25-foot walk at baseline showed a significant improvement in walking speed. In terms of MS quality of life, from before to after the procedure "there were significant improvements in physical and mental ability. There clearly seems to be a trend. In the modified fatigue impact score, there also seems to be a clear improvement," he said.
Dr. Mehta also said that there was a trend toward improvement in balance, lower-extremity weakness, incontinence, coordination, and vertigo in more than 80% of patients.
Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.
FROM THE VASCULAR ANNUAL MEETING
Major Finding: Residual stenosis of less than 20% (defined as immediate success) was observed in 82% of patients.
Data Source: A series of 125 patients with multiple sclerosis who were identified by venogram to have internal jugular and/or azygous veins with stenoses of 50% or greater.
Disclosures: Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.