User login
Symptom Improvement Observed After Venoplasty in MS Patients
CHICAGO – Preliminary data from a series of multiple sclerosis patients who underwent percutaneous transluminal venoplasty to treat chronic cerebrospinal venous insufficiency suggest that the treatment was safe and offered significant disease-specific and quality of life improvements.
The results of the controversial treatment on 125 patients in the series will need to be validated with future randomized, blinded, controlled trials that evaluate endovascular and surgical options, Dr. Manish Mehta said at the Vascular Annual Meeting.
The patient series follows Dr. Paolo Zamboni’s identification in 2009 of stenoses in the internal jugular veins and azygous vein of patients with MS (J. Neurol. Neurosurg. Psychiatry 2009;80:392-9).
"Dr. Zamboni’s theory has been that stasis of blood can cause reflux, and reflux can cause propagation and [can] break down the blood-brain barrier," Dr. Mehta said. The resulting microbleeds can allow red blood cells to escape into the brain matter, leading to hemosiderin deposits that can act as the inflammatory mediators of an autoimmune response, he said.
Although Dr. Zamboni, a vascular surgeon and professor of surgery at the University of Ferrara (Italy), observed a strong association between chronic cerebrospinal venous insufficiency (CCSVI) and MS, it is unclear if the relationship between CCSVI and MS is causative, or if CCSVI might play a role in the etiology of the disease.
In 2009, Dr. Zamboni also reported on a series of 65 patients who had significant improvements in functional composite scores and quality of life at 1 year (J. Vasc. Surg. 2009;50;1348-58.e1-3).
The preliminary data that Dr. Mehta presented at the meeting came from the LIBERATION study, which is designed to assess the utility of percutaneous transluminal venoplasty for individuals with CCSVI and MS. It’s a prospective, randomized, double-blind study that is currently enrolling 600 patients.
Because there is a learning curve involved with the assessment and technique, the researchers included a prospective longitudinal arm as part of the study. Dr. Mehta of the Albany (N.Y.) Medical College and the director of endovascular services for the Vascular Group PLLC, presented preliminary results on this group of patients.
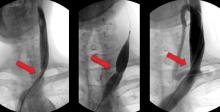
In the study, investigators performed venograms to identify stenoses of 50% or greater in internal jugular and azygous veins in the patients, all of whom underwent venoplasty. Neurologists and other clinicians evaluated the patients at baseline, and then at 1 month, 3 months, and every 6 months thereafter.
The 125 patients included in the study had a mean age of 47 years, and 62% were female. Relapsing-remitting MS accounted for 54% of the patients, followed by secondary-progressive MS in 34% and primary-progressive MS in 12%.
The patients had a total of 230 lesions altogether, 90% of which involved the internal jugular veins; the majority of these were at the origin. The remaining 10% of patients had stenoses in their azygous veins.
The mean degree of occlusion was about 80%, with approximately 1.8 lesions per patient. Immediate success (defined as less than 20% residual stenosis) occurred in 82%. The remaining patients underwent a second venoplasty without stenting.
In all, 79 patients were available for follow-up at a mean of 4.5 years. Restenosis of 50% occurred in eight of these patients, occlusions occurred in two patients, and one patient had new-onset atrial fibrillation.
The investigators reassessed 48 patients with the EDSS (Extended Disability Status Scale) following initial baseline testing. From before to after the procedure, "there was a statistical improvement. Improvements occurred in each of the MS types, except in primary progressive MS," Dr. Mehta said.
Reevaluations of 79 patients who performed a timed 25-foot walk at baseline showed a significant improvement in walking speed. In terms of MS quality of life, from before to after the procedure "there were significant improvements in physical and mental ability. There clearly seems to be a trend. In the modified fatigue impact score, there also seems to be a clear improvement," he said.
Dr. Mehta also said that there was a trend toward improvement in balance, lower-extremity weakness, incontinence, coordination, and vertigo in more than 80% of patients.
Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.
CHICAGO – Preliminary data from a series of multiple sclerosis patients who underwent percutaneous transluminal venoplasty to treat chronic cerebrospinal venous insufficiency suggest that the treatment was safe and offered significant disease-specific and quality of life improvements.
The results of the controversial treatment on 125 patients in the series will need to be validated with future randomized, blinded, controlled trials that evaluate endovascular and surgical options, Dr. Manish Mehta said at the Vascular Annual Meeting.
The patient series follows Dr. Paolo Zamboni’s identification in 2009 of stenoses in the internal jugular veins and azygous vein of patients with MS (J. Neurol. Neurosurg. Psychiatry 2009;80:392-9).
"Dr. Zamboni’s theory has been that stasis of blood can cause reflux, and reflux can cause propagation and [can] break down the blood-brain barrier," Dr. Mehta said. The resulting microbleeds can allow red blood cells to escape into the brain matter, leading to hemosiderin deposits that can act as the inflammatory mediators of an autoimmune response, he said.
Although Dr. Zamboni, a vascular surgeon and professor of surgery at the University of Ferrara (Italy), observed a strong association between chronic cerebrospinal venous insufficiency (CCSVI) and MS, it is unclear if the relationship between CCSVI and MS is causative, or if CCSVI might play a role in the etiology of the disease.
In 2009, Dr. Zamboni also reported on a series of 65 patients who had significant improvements in functional composite scores and quality of life at 1 year (J. Vasc. Surg. 2009;50;1348-58.e1-3).
The preliminary data that Dr. Mehta presented at the meeting came from the LIBERATION study, which is designed to assess the utility of percutaneous transluminal venoplasty for individuals with CCSVI and MS. It’s a prospective, randomized, double-blind study that is currently enrolling 600 patients.
Because there is a learning curve involved with the assessment and technique, the researchers included a prospective longitudinal arm as part of the study. Dr. Mehta of the Albany (N.Y.) Medical College and the director of endovascular services for the Vascular Group PLLC, presented preliminary results on this group of patients.
In the study, investigators performed venograms to identify stenoses of 50% or greater in internal jugular and azygous veins in the patients, all of whom underwent venoplasty. Neurologists and other clinicians evaluated the patients at baseline, and then at 1 month, 3 months, and every 6 months thereafter.
The 125 patients included in the study had a mean age of 47 years, and 62% were female. Relapsing-remitting MS accounted for 54% of the patients, followed by secondary-progressive MS in 34% and primary-progressive MS in 12%.
The patients had a total of 230 lesions altogether, 90% of which involved the internal jugular veins; the majority of these were at the origin. The remaining 10% of patients had stenoses in their azygous veins.
The mean degree of occlusion was about 80%, with approximately 1.8 lesions per patient. Immediate success (defined as less than 20% residual stenosis) occurred in 82%. The remaining patients underwent a second venoplasty without stenting.
In all, 79 patients were available for follow-up at a mean of 4.5 years. Restenosis of 50% occurred in eight of these patients, occlusions occurred in two patients, and one patient had new-onset atrial fibrillation.
The investigators reassessed 48 patients with the EDSS (Extended Disability Status Scale) following initial baseline testing. From before to after the procedure, "there was a statistical improvement. Improvements occurred in each of the MS types, except in primary progressive MS," Dr. Mehta said.
Reevaluations of 79 patients who performed a timed 25-foot walk at baseline showed a significant improvement in walking speed. In terms of MS quality of life, from before to after the procedure "there were significant improvements in physical and mental ability. There clearly seems to be a trend. In the modified fatigue impact score, there also seems to be a clear improvement," he said.
Dr. Mehta also said that there was a trend toward improvement in balance, lower-extremity weakness, incontinence, coordination, and vertigo in more than 80% of patients.
Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.
CHICAGO – Preliminary data from a series of multiple sclerosis patients who underwent percutaneous transluminal venoplasty to treat chronic cerebrospinal venous insufficiency suggest that the treatment was safe and offered significant disease-specific and quality of life improvements.
The results of the controversial treatment on 125 patients in the series will need to be validated with future randomized, blinded, controlled trials that evaluate endovascular and surgical options, Dr. Manish Mehta said at the Vascular Annual Meeting.
The patient series follows Dr. Paolo Zamboni’s identification in 2009 of stenoses in the internal jugular veins and azygous vein of patients with MS (J. Neurol. Neurosurg. Psychiatry 2009;80:392-9).
"Dr. Zamboni’s theory has been that stasis of blood can cause reflux, and reflux can cause propagation and [can] break down the blood-brain barrier," Dr. Mehta said. The resulting microbleeds can allow red blood cells to escape into the brain matter, leading to hemosiderin deposits that can act as the inflammatory mediators of an autoimmune response, he said.
Although Dr. Zamboni, a vascular surgeon and professor of surgery at the University of Ferrara (Italy), observed a strong association between chronic cerebrospinal venous insufficiency (CCSVI) and MS, it is unclear if the relationship between CCSVI and MS is causative, or if CCSVI might play a role in the etiology of the disease.
In 2009, Dr. Zamboni also reported on a series of 65 patients who had significant improvements in functional composite scores and quality of life at 1 year (J. Vasc. Surg. 2009;50;1348-58.e1-3).
The preliminary data that Dr. Mehta presented at the meeting came from the LIBERATION study, which is designed to assess the utility of percutaneous transluminal venoplasty for individuals with CCSVI and MS. It’s a prospective, randomized, double-blind study that is currently enrolling 600 patients.
Because there is a learning curve involved with the assessment and technique, the researchers included a prospective longitudinal arm as part of the study. Dr. Mehta of the Albany (N.Y.) Medical College and the director of endovascular services for the Vascular Group PLLC, presented preliminary results on this group of patients.
In the study, investigators performed venograms to identify stenoses of 50% or greater in internal jugular and azygous veins in the patients, all of whom underwent venoplasty. Neurologists and other clinicians evaluated the patients at baseline, and then at 1 month, 3 months, and every 6 months thereafter.
The 125 patients included in the study had a mean age of 47 years, and 62% were female. Relapsing-remitting MS accounted for 54% of the patients, followed by secondary-progressive MS in 34% and primary-progressive MS in 12%.
The patients had a total of 230 lesions altogether, 90% of which involved the internal jugular veins; the majority of these were at the origin. The remaining 10% of patients had stenoses in their azygous veins.
The mean degree of occlusion was about 80%, with approximately 1.8 lesions per patient. Immediate success (defined as less than 20% residual stenosis) occurred in 82%. The remaining patients underwent a second venoplasty without stenting.
In all, 79 patients were available for follow-up at a mean of 4.5 years. Restenosis of 50% occurred in eight of these patients, occlusions occurred in two patients, and one patient had new-onset atrial fibrillation.
The investigators reassessed 48 patients with the EDSS (Extended Disability Status Scale) following initial baseline testing. From before to after the procedure, "there was a statistical improvement. Improvements occurred in each of the MS types, except in primary progressive MS," Dr. Mehta said.
Reevaluations of 79 patients who performed a timed 25-foot walk at baseline showed a significant improvement in walking speed. In terms of MS quality of life, from before to after the procedure "there were significant improvements in physical and mental ability. There clearly seems to be a trend. In the modified fatigue impact score, there also seems to be a clear improvement," he said.
Dr. Mehta also said that there was a trend toward improvement in balance, lower-extremity weakness, incontinence, coordination, and vertigo in more than 80% of patients.
Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.
FROM THE VASCULAR ANNUAL MEETING
Major Finding: Residual stenosis of less than 20% (defined as immediate success) was observed in 82% of patients.
Data Source: A series of 125 patients with multiple sclerosis who were identified by venogram to have internal jugular and/or azygous veins with stenoses of 50% or greater.
Disclosures: Dr. Mehta and his colleagues reported that they each had several significant financial relationships with device manufacturers.
Risk Assessment Tool Improves VTE Prophylaxis Hospital-Wide
CHICAGO – By implementing an online risk assessment tool, researchers at one institution were able to improve hospital-wide prophylaxis and significantly cut the number of venous thrombotic events, Dr. Nicholas J. Morrissey said at the Vascular Annual Meeting.
"Our overall level of prophylaxis at both campuses was 98%; whereas preimplementation, we had about a 71% level of appropriate prophylaxis," said Dr. Morrissey of the department of surgery at Columbia University in New York.
Starting in June 2010, all patients admitted to New York–Presbyterian Hospital were required to have their venous thromboembolism (VTE) risk assessed as part of their electronic admission orders. Physicians were free to use a specially developed online risk assessment tool or their own judgment regarding prophylaxis.
The VTE risk assessment tool was created by a bicampus committee of clinicians from various specialties, IT support, nursing, and data management staff. This group also reviewed all documented VTE events from June 2010 to the present. Each event was subjected to clinical adjudication for accuracy.
Risk assessment and prophylaxis were monitored using AMALGA (Microsoft) software that allows real-time accumulation of clinical data that goes into the patient’s hospital electronic health record. VTE rates were monitored through chart review by certified coders and were double-checked for accuracy by reviewers with clinical backgrounds.
Patients who were positive for VTE events were further examined and rates were compared before and after implementation of the assessment tool. In addition, a random sampling of patients on several inpatient floors was performed to determine if the adequate level of VTE was being used.
"Through a very recent random sampling of 503 patients in the entire hospital, we looked to see what the adequate prophylaxis level was after the implementation of our tool," said Dr. Morrissey. This was defined as appropriate pharmacologic prophylaxis when indicated.
They also compared pre- and post-implementation periods to assess VTE rates. At New York–Presbyterian’s Columbia University Medical Center campus, the VTE rate prior to assessment implementation was 1.08/1,000 patient-days from January through June 2010. At the same campus, the VTE rate dropped to 0.80/1,000 patient-days from July through December. Similarly, at New York–Presbyterian’s other campus, Weill Cornell Medical Center, the VTE rate was 1.19/1,000 patient-days from January through June 2010; it dropped to 0.84/1,000 patient-days from July through December 2010.
"Interestingly, what we found at both institutions was that our pulmonary embolism rate dropped significantly between the first and second half of 2010," said Dr. Morrissey. At Columbia, the number of pulmonary embolisms dropped from 24 to 15. At Cornell, the number of PEs dropped from 41 to 15.
"We saw that a significant number of patients actually suffered from upper-extremity line-associated clots," he noted. At Columbia, there were 31 upper extremity events from January to June 2010; there were 33 from July to December. At Cornell, there were 38 upper extremity events in the first half of the year and 33 in the second half.
Both institutions used the AMALGA system to provide clinicians with feedback. The software calculates the patient’s risk score in real time as patients are admitted, based on their past medical history. The software also collects all of the information entered into the electronic order set. This allows staff to look and see which patients are listed as high risk or low risk and whether the clinician used the tool appropriately. "So we’re actually able to assess hospital wide how these patients are receiving prophylaxis," said Dr. Morrissey.
The tool also allows the identification of patients that are inappropriately classified based on risk and who are receiving inappropriate prophylaxis. "We can reach out to those clinicians in real time and discuss with them the issues related to prophylaxis."
With further validation, the system could prove a considerable asset in meeting and demonstrating quality goals, he noted.
The authors reported that they have no relevant disclosures.
CHICAGO – By implementing an online risk assessment tool, researchers at one institution were able to improve hospital-wide prophylaxis and significantly cut the number of venous thrombotic events, Dr. Nicholas J. Morrissey said at the Vascular Annual Meeting.
"Our overall level of prophylaxis at both campuses was 98%; whereas preimplementation, we had about a 71% level of appropriate prophylaxis," said Dr. Morrissey of the department of surgery at Columbia University in New York.
Starting in June 2010, all patients admitted to New York–Presbyterian Hospital were required to have their venous thromboembolism (VTE) risk assessed as part of their electronic admission orders. Physicians were free to use a specially developed online risk assessment tool or their own judgment regarding prophylaxis.
The VTE risk assessment tool was created by a bicampus committee of clinicians from various specialties, IT support, nursing, and data management staff. This group also reviewed all documented VTE events from June 2010 to the present. Each event was subjected to clinical adjudication for accuracy.
Risk assessment and prophylaxis were monitored using AMALGA (Microsoft) software that allows real-time accumulation of clinical data that goes into the patient’s hospital electronic health record. VTE rates were monitored through chart review by certified coders and were double-checked for accuracy by reviewers with clinical backgrounds.
Patients who were positive for VTE events were further examined and rates were compared before and after implementation of the assessment tool. In addition, a random sampling of patients on several inpatient floors was performed to determine if the adequate level of VTE was being used.
"Through a very recent random sampling of 503 patients in the entire hospital, we looked to see what the adequate prophylaxis level was after the implementation of our tool," said Dr. Morrissey. This was defined as appropriate pharmacologic prophylaxis when indicated.
They also compared pre- and post-implementation periods to assess VTE rates. At New York–Presbyterian’s Columbia University Medical Center campus, the VTE rate prior to assessment implementation was 1.08/1,000 patient-days from January through June 2010. At the same campus, the VTE rate dropped to 0.80/1,000 patient-days from July through December. Similarly, at New York–Presbyterian’s other campus, Weill Cornell Medical Center, the VTE rate was 1.19/1,000 patient-days from January through June 2010; it dropped to 0.84/1,000 patient-days from July through December 2010.
"Interestingly, what we found at both institutions was that our pulmonary embolism rate dropped significantly between the first and second half of 2010," said Dr. Morrissey. At Columbia, the number of pulmonary embolisms dropped from 24 to 15. At Cornell, the number of PEs dropped from 41 to 15.
"We saw that a significant number of patients actually suffered from upper-extremity line-associated clots," he noted. At Columbia, there were 31 upper extremity events from January to June 2010; there were 33 from July to December. At Cornell, there were 38 upper extremity events in the first half of the year and 33 in the second half.
Both institutions used the AMALGA system to provide clinicians with feedback. The software calculates the patient’s risk score in real time as patients are admitted, based on their past medical history. The software also collects all of the information entered into the electronic order set. This allows staff to look and see which patients are listed as high risk or low risk and whether the clinician used the tool appropriately. "So we’re actually able to assess hospital wide how these patients are receiving prophylaxis," said Dr. Morrissey.
The tool also allows the identification of patients that are inappropriately classified based on risk and who are receiving inappropriate prophylaxis. "We can reach out to those clinicians in real time and discuss with them the issues related to prophylaxis."
With further validation, the system could prove a considerable asset in meeting and demonstrating quality goals, he noted.
The authors reported that they have no relevant disclosures.
CHICAGO – By implementing an online risk assessment tool, researchers at one institution were able to improve hospital-wide prophylaxis and significantly cut the number of venous thrombotic events, Dr. Nicholas J. Morrissey said at the Vascular Annual Meeting.
"Our overall level of prophylaxis at both campuses was 98%; whereas preimplementation, we had about a 71% level of appropriate prophylaxis," said Dr. Morrissey of the department of surgery at Columbia University in New York.
Starting in June 2010, all patients admitted to New York–Presbyterian Hospital were required to have their venous thromboembolism (VTE) risk assessed as part of their electronic admission orders. Physicians were free to use a specially developed online risk assessment tool or their own judgment regarding prophylaxis.
The VTE risk assessment tool was created by a bicampus committee of clinicians from various specialties, IT support, nursing, and data management staff. This group also reviewed all documented VTE events from June 2010 to the present. Each event was subjected to clinical adjudication for accuracy.
Risk assessment and prophylaxis were monitored using AMALGA (Microsoft) software that allows real-time accumulation of clinical data that goes into the patient’s hospital electronic health record. VTE rates were monitored through chart review by certified coders and were double-checked for accuracy by reviewers with clinical backgrounds.
Patients who were positive for VTE events were further examined and rates were compared before and after implementation of the assessment tool. In addition, a random sampling of patients on several inpatient floors was performed to determine if the adequate level of VTE was being used.
"Through a very recent random sampling of 503 patients in the entire hospital, we looked to see what the adequate prophylaxis level was after the implementation of our tool," said Dr. Morrissey. This was defined as appropriate pharmacologic prophylaxis when indicated.
They also compared pre- and post-implementation periods to assess VTE rates. At New York–Presbyterian’s Columbia University Medical Center campus, the VTE rate prior to assessment implementation was 1.08/1,000 patient-days from January through June 2010. At the same campus, the VTE rate dropped to 0.80/1,000 patient-days from July through December. Similarly, at New York–Presbyterian’s other campus, Weill Cornell Medical Center, the VTE rate was 1.19/1,000 patient-days from January through June 2010; it dropped to 0.84/1,000 patient-days from July through December 2010.
"Interestingly, what we found at both institutions was that our pulmonary embolism rate dropped significantly between the first and second half of 2010," said Dr. Morrissey. At Columbia, the number of pulmonary embolisms dropped from 24 to 15. At Cornell, the number of PEs dropped from 41 to 15.
"We saw that a significant number of patients actually suffered from upper-extremity line-associated clots," he noted. At Columbia, there were 31 upper extremity events from January to June 2010; there were 33 from July to December. At Cornell, there were 38 upper extremity events in the first half of the year and 33 in the second half.
Both institutions used the AMALGA system to provide clinicians with feedback. The software calculates the patient’s risk score in real time as patients are admitted, based on their past medical history. The software also collects all of the information entered into the electronic order set. This allows staff to look and see which patients are listed as high risk or low risk and whether the clinician used the tool appropriately. "So we’re actually able to assess hospital wide how these patients are receiving prophylaxis," said Dr. Morrissey.
The tool also allows the identification of patients that are inappropriately classified based on risk and who are receiving inappropriate prophylaxis. "We can reach out to those clinicians in real time and discuss with them the issues related to prophylaxis."
With further validation, the system could prove a considerable asset in meeting and demonstrating quality goals, he noted.
The authors reported that they have no relevant disclosures.
FROM THE VASCULAR ANNUAL MEETING
Risk Assessment Tool Improves VTE Prophylaxis Hospital-Wide
CHICAGO – By implementing an online risk assessment tool, researchers at one institution were able to improve hospital-wide prophylaxis and significantly cut the number of venous thrombotic events, Dr. Nicholas J. Morrissey said at the Vascular Annual Meeting.
"Our overall level of prophylaxis at both campuses was 98%; whereas preimplementation, we had about a 71% level of appropriate prophylaxis," said Dr. Morrissey of the department of surgery at Columbia University in New York.
Starting in June 2010, all patients admitted to New York–Presbyterian Hospital were required to have their venous thromboembolism (VTE) risk assessed as part of their electronic admission orders. Physicians were free to use a specially developed online risk assessment tool or their own judgment regarding prophylaxis.
The VTE risk assessment tool was created by a bicampus committee of clinicians from various specialties, IT support, nursing, and data management staff. This group also reviewed all documented VTE events from June 2010 to the present. Each event was subjected to clinical adjudication for accuracy.
Risk assessment and prophylaxis were monitored using AMALGA (Microsoft) software that allows real-time accumulation of clinical data that goes into the patient’s hospital electronic health record. VTE rates were monitored through chart review by certified coders and were double-checked for accuracy by reviewers with clinical backgrounds.
Patients who were positive for VTE events were further examined and rates were compared before and after implementation of the assessment tool. In addition, a random sampling of patients on several inpatient floors was performed to determine if the adequate level of VTE was being used.
"Through a very recent random sampling of 503 patients in the entire hospital, we looked to see what the adequate prophylaxis level was after the implementation of our tool," said Dr. Morrissey. This was defined as appropriate pharmacologic prophylaxis when indicated.
They also compared pre- and post-implementation periods to assess VTE rates. At New York–Presbyterian’s Columbia University Medical Center campus, the VTE rate prior to assessment implementation was 1.08/1,000 patient-days from January through June 2010. At the same campus, the VTE rate dropped to 0.80/1,000 patient-days from July through December. Similarly, at New York–Presbyterian’s other campus, Weill Cornell Medical Center, the VTE rate was 1.19/1,000 patient-days from January through June 2010; it dropped to 0.84/1,000 patient-days from July through December 2010.
"Interestingly, what we found at both institutions was that our pulmonary embolism rate dropped significantly between the first and second half of 2010," said Dr. Morrissey. At Columbia, the number of pulmonary embolisms dropped from 24 to 15. At Cornell, the number of PEs dropped from 41 to 15.
"We saw that a significant number of patients actually suffered from upper-extremity line-associated clots," he noted. At Columbia, there were 31 upper extremity events from January to June 2010; there were 33 from July to December. At Cornell, there were 38 upper extremity events in the first half of the year and 33 in the second half.
Both institutions used the AMALGA system to provide clinicians with feedback. The software calculates the patient’s risk score in real time as patients are admitted, based on their past medical history. The software also collects all of the information entered into the electronic order set. This allows staff to look and see which patients are listed as high risk or low risk and whether the clinician used the tool appropriately. "So we’re actually able to assess hospital wide how these patients are receiving prophylaxis," said Dr. Morrissey.
The tool also allows the identification of patients that are inappropriately classified based on risk and who are receiving inappropriate prophylaxis. "We can reach out to those clinicians in real time and discuss with them the issues related to prophylaxis."
With further validation, the system could prove a considerable asset in meeting and demonstrating quality goals, he noted.
The authors reported that they have no relevant disclosures.
CHICAGO – By implementing an online risk assessment tool, researchers at one institution were able to improve hospital-wide prophylaxis and significantly cut the number of venous thrombotic events, Dr. Nicholas J. Morrissey said at the Vascular Annual Meeting.
"Our overall level of prophylaxis at both campuses was 98%; whereas preimplementation, we had about a 71% level of appropriate prophylaxis," said Dr. Morrissey of the department of surgery at Columbia University in New York.
Starting in June 2010, all patients admitted to New York–Presbyterian Hospital were required to have their venous thromboembolism (VTE) risk assessed as part of their electronic admission orders. Physicians were free to use a specially developed online risk assessment tool or their own judgment regarding prophylaxis.
The VTE risk assessment tool was created by a bicampus committee of clinicians from various specialties, IT support, nursing, and data management staff. This group also reviewed all documented VTE events from June 2010 to the present. Each event was subjected to clinical adjudication for accuracy.
Risk assessment and prophylaxis were monitored using AMALGA (Microsoft) software that allows real-time accumulation of clinical data that goes into the patient’s hospital electronic health record. VTE rates were monitored through chart review by certified coders and were double-checked for accuracy by reviewers with clinical backgrounds.
Patients who were positive for VTE events were further examined and rates were compared before and after implementation of the assessment tool. In addition, a random sampling of patients on several inpatient floors was performed to determine if the adequate level of VTE was being used.
"Through a very recent random sampling of 503 patients in the entire hospital, we looked to see what the adequate prophylaxis level was after the implementation of our tool," said Dr. Morrissey. This was defined as appropriate pharmacologic prophylaxis when indicated.
They also compared pre- and post-implementation periods to assess VTE rates. At New York–Presbyterian’s Columbia University Medical Center campus, the VTE rate prior to assessment implementation was 1.08/1,000 patient-days from January through June 2010. At the same campus, the VTE rate dropped to 0.80/1,000 patient-days from July through December. Similarly, at New York–Presbyterian’s other campus, Weill Cornell Medical Center, the VTE rate was 1.19/1,000 patient-days from January through June 2010; it dropped to 0.84/1,000 patient-days from July through December 2010.
"Interestingly, what we found at both institutions was that our pulmonary embolism rate dropped significantly between the first and second half of 2010," said Dr. Morrissey. At Columbia, the number of pulmonary embolisms dropped from 24 to 15. At Cornell, the number of PEs dropped from 41 to 15.
"We saw that a significant number of patients actually suffered from upper-extremity line-associated clots," he noted. At Columbia, there were 31 upper extremity events from January to June 2010; there were 33 from July to December. At Cornell, there were 38 upper extremity events in the first half of the year and 33 in the second half.
Both institutions used the AMALGA system to provide clinicians with feedback. The software calculates the patient’s risk score in real time as patients are admitted, based on their past medical history. The software also collects all of the information entered into the electronic order set. This allows staff to look and see which patients are listed as high risk or low risk and whether the clinician used the tool appropriately. "So we’re actually able to assess hospital wide how these patients are receiving prophylaxis," said Dr. Morrissey.
The tool also allows the identification of patients that are inappropriately classified based on risk and who are receiving inappropriate prophylaxis. "We can reach out to those clinicians in real time and discuss with them the issues related to prophylaxis."
With further validation, the system could prove a considerable asset in meeting and demonstrating quality goals, he noted.
The authors reported that they have no relevant disclosures.
CHICAGO – By implementing an online risk assessment tool, researchers at one institution were able to improve hospital-wide prophylaxis and significantly cut the number of venous thrombotic events, Dr. Nicholas J. Morrissey said at the Vascular Annual Meeting.
"Our overall level of prophylaxis at both campuses was 98%; whereas preimplementation, we had about a 71% level of appropriate prophylaxis," said Dr. Morrissey of the department of surgery at Columbia University in New York.
Starting in June 2010, all patients admitted to New York–Presbyterian Hospital were required to have their venous thromboembolism (VTE) risk assessed as part of their electronic admission orders. Physicians were free to use a specially developed online risk assessment tool or their own judgment regarding prophylaxis.
The VTE risk assessment tool was created by a bicampus committee of clinicians from various specialties, IT support, nursing, and data management staff. This group also reviewed all documented VTE events from June 2010 to the present. Each event was subjected to clinical adjudication for accuracy.
Risk assessment and prophylaxis were monitored using AMALGA (Microsoft) software that allows real-time accumulation of clinical data that goes into the patient’s hospital electronic health record. VTE rates were monitored through chart review by certified coders and were double-checked for accuracy by reviewers with clinical backgrounds.
Patients who were positive for VTE events were further examined and rates were compared before and after implementation of the assessment tool. In addition, a random sampling of patients on several inpatient floors was performed to determine if the adequate level of VTE was being used.
"Through a very recent random sampling of 503 patients in the entire hospital, we looked to see what the adequate prophylaxis level was after the implementation of our tool," said Dr. Morrissey. This was defined as appropriate pharmacologic prophylaxis when indicated.
They also compared pre- and post-implementation periods to assess VTE rates. At New York–Presbyterian’s Columbia University Medical Center campus, the VTE rate prior to assessment implementation was 1.08/1,000 patient-days from January through June 2010. At the same campus, the VTE rate dropped to 0.80/1,000 patient-days from July through December. Similarly, at New York–Presbyterian’s other campus, Weill Cornell Medical Center, the VTE rate was 1.19/1,000 patient-days from January through June 2010; it dropped to 0.84/1,000 patient-days from July through December 2010.
"Interestingly, what we found at both institutions was that our pulmonary embolism rate dropped significantly between the first and second half of 2010," said Dr. Morrissey. At Columbia, the number of pulmonary embolisms dropped from 24 to 15. At Cornell, the number of PEs dropped from 41 to 15.
"We saw that a significant number of patients actually suffered from upper-extremity line-associated clots," he noted. At Columbia, there were 31 upper extremity events from January to June 2010; there were 33 from July to December. At Cornell, there were 38 upper extremity events in the first half of the year and 33 in the second half.
Both institutions used the AMALGA system to provide clinicians with feedback. The software calculates the patient’s risk score in real time as patients are admitted, based on their past medical history. The software also collects all of the information entered into the electronic order set. This allows staff to look and see which patients are listed as high risk or low risk and whether the clinician used the tool appropriately. "So we’re actually able to assess hospital wide how these patients are receiving prophylaxis," said Dr. Morrissey.
The tool also allows the identification of patients that are inappropriately classified based on risk and who are receiving inappropriate prophylaxis. "We can reach out to those clinicians in real time and discuss with them the issues related to prophylaxis."
With further validation, the system could prove a considerable asset in meeting and demonstrating quality goals, he noted.
The authors reported that they have no relevant disclosures.
FROM THE VASCULAR ANNUAL MEETING
Major Finding: VTE prophylaxis improved from 71% to 98% with implementation of risk assessment tool.
Data Source: A random sampling of 503 patients in one hospital (two campuses).
Disclosures: The authors reported that they have no relevant disclosures.
Aneurysm Complexity Influences Outcome
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
FROM THE VASCULAR ANNUAL MEETING
Major Finding: Complex abdominal aortic aneurysm repair can be performed with low mortality (1.3%), but an increasing level of aneurysm complexity was significantly associated with higher morbidity and mortality.
Data Source: A review of outcomes of 461 patients undergoing open cAAA repair from 2000 to 2010.
Disclosures: Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
Aneurysm Complexity Influences Outcome
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
FROM THE VASCULAR ANNUAL MEETING
Aneurysm Complexity Influences Outcome
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
CHICAGO – Fenestrated grafts increasingly are being used for endovascular aneurysm repair of complex abdominal aortic aneurysms, but there are few benchmarks for comparing outcomes achieved with open repair and EVAR in these situations.
Dr. Gustavo S. Oderich and his colleagues at the Mayo Clinic, Rochester, Minn., reviewed the outcomes of a series of 461 patients undergoing open complex abdominal aortic aneurysm (cAAA) repair from 2000 to 2010.
They found that open cAAA repair can be done safely, but there is an increasing risk of complications and mortality with more complex anatomies, Dr. Oderich said at the Vascular Annual Meeting.
In their study, available preoperative digital imaging data were analyzed by a blinded investigator. A centerline of flow was used to define aneurysm extent and to predict the expected number of fenestrations that would have been required to provide 2 cm of proximal seal for a fenestrated EVAR procedure, had one been performed. End points examined were mortality, morbidity, renal function (RF) deterioration, reinterventions, and survival.
Among the 354 male and 107 female patients (mean age, 73 years), the overall operative mortality was 1.3% (6/461). Some level of morbidity occurred in 57% (260) of the patients treated, and it was severe in 20% (91) of the overall patients.
The overall 5-year patient survival rate was 72%, with a freedom from reintervention rate of 90% and a freedom from RF deterioration rate of 84%. Dr. Oderich discussed how the increasing level of aneurysm complexity was significantly associated with greater operative mortality, severe morbidity, and dialysis rates – regardless of whether the complexity was classified by anatomic considerations (from juxtarenal to suprarenal to type IV thoracic aortic aneurysm, TAA) or by the expected number of fenestrations (one through four), with more fenestrations equivalent to increasing complexity.
At 5 years, patient survival ranged from 76% in juxtarenal patients to 62% for type IV TAA, with severe morbidity ranging from 13% (juxtarenal) to 43% (type IV TAA). Similarly, severe morbidity in patients with only one expected fenestration was 0%, but reached 42% in patients who would have an expected number of four fenestrations.
"Open cAAA repair can be performed safely with low overall mortality (1.3%), but a high risk of complications, mortality, and complications increasing with worse anatomic classification and a higher expected number of fenestrations. These data can provide a needed benchmark for comparison with results of fenestrated EVAR," said Dr. Oderich.
Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
FROM THE VASCULAR ANNUAL MEETING
Major Finding: Complex abdominal aortic aneurysm repair can be performed with low mortality (1.3%), but an increasing level of aneurysm complexity was significantly associated with higher morbidity and mortality.
Data Source: A review of outcomes of 461 patients undergoing open cAAA repair from 2000 to 2010.
Disclosures: Dr. Oderich stated that he received consulting fees and other remuneration from Medtronic and Cook Medical.
Benefits of Perioperative Statins Borne Out in Trial
CHICAGO – Results from a follow-up analysis of patients in the randomized DECREASE III trial showed that there is an apparent "legacy" effect of perioperative statin therapy, resulting in improved long-term survival, compared with statin initiation after vascular surgery.
Ischemic cardiac events are a major cause of perioperative morbidity and mortality in noncardiac surgery (including vascular surgery), with an estimated 10%-40% of perioperative deaths ascribed to myocardial infarction (MI), according to the original report by Dr. Don Poldermans and the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography) III researchers. Statins, which are associated with improved plaque stability, were plausible candidates to reduce perioperative MI. And in fact, results of the original DECREASE III study showed that in high-risk patients who undergo major vascular surgery, fluvastatin XL reduced myocardial ischemia and the combined end point of cardiovascular death and MI.
Dr. Olaf Schouten from the Erasmus University Medical Center, Rotterdam, the Netherlands, discussed a further analysis of the DECREASE III population at the Vascular Annual Meeting. The investigators examined a total of 497 patients who were randomized to placebo (247 patients) or fluvastatin (250) in the double-blinded trial.
The patients had been started on treatment a median of 34 days prior to surgery. At the end of the DECREASE III study period (30 days after surgery), all patients were prescribed lifelong statins as recommended by current guidelines. The current study relied on all-cause death data obtained from a civil service registry for a median follow-up of 4.8 years, during which time 129 patients died.
Perioperative statin use was associated with a significant reduction of perioperative cardiovascular events (hazard ratio, 0.55), according to Dr. Schouten. In a multivariate analysis that adjusted for possible confounders including cardiovascular risk factors, type and site of vascular surgery, and age, preoperative statin initiation was still significantly associated with an improved long-term outcome (HR, 0.59).
"The randomized DECREASE III trial showed that perioperative statin use is associated with a significant reduction of perioperative cardiovascular events," according to Dr. Schouten. But it appears that statin therapy also results in a long-term survival benefit, compared with postoperative initiation of statin therapy, he added.
"This ‘legacy’ effect might be due to the prevention of perioperative myocardial damage, as patients with myocardial damage had a significantly higher risk of death during follow-up," Dr. Schouten speculated.
"The main message of our study is that all vascular surgery patients eligible for statin therapy [that is, without contraindications] should be prescribed statins at the first, preoperative, and outpatient clinic visit," said Dr. Schouten in an interview. He pointed out that statin therapy is safe in the perioperative period, with no significant side effects; it improves perioperative cardiac outcome; and it is associated with a long-term survival benefit.
"So prescribe statins as soon as possible, keep them on statins in the perioperative period, and keep them on [lifelong statins] after surgery," Dr. Schouten concluded.
Dr. Schouten stated that he had nothing to disclose.
CHICAGO – Results from a follow-up analysis of patients in the randomized DECREASE III trial showed that there is an apparent "legacy" effect of perioperative statin therapy, resulting in improved long-term survival, compared with statin initiation after vascular surgery.
Ischemic cardiac events are a major cause of perioperative morbidity and mortality in noncardiac surgery (including vascular surgery), with an estimated 10%-40% of perioperative deaths ascribed to myocardial infarction (MI), according to the original report by Dr. Don Poldermans and the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography) III researchers. Statins, which are associated with improved plaque stability, were plausible candidates to reduce perioperative MI. And in fact, results of the original DECREASE III study showed that in high-risk patients who undergo major vascular surgery, fluvastatin XL reduced myocardial ischemia and the combined end point of cardiovascular death and MI.
Dr. Olaf Schouten from the Erasmus University Medical Center, Rotterdam, the Netherlands, discussed a further analysis of the DECREASE III population at the Vascular Annual Meeting. The investigators examined a total of 497 patients who were randomized to placebo (247 patients) or fluvastatin (250) in the double-blinded trial.
The patients had been started on treatment a median of 34 days prior to surgery. At the end of the DECREASE III study period (30 days after surgery), all patients were prescribed lifelong statins as recommended by current guidelines. The current study relied on all-cause death data obtained from a civil service registry for a median follow-up of 4.8 years, during which time 129 patients died.
Perioperative statin use was associated with a significant reduction of perioperative cardiovascular events (hazard ratio, 0.55), according to Dr. Schouten. In a multivariate analysis that adjusted for possible confounders including cardiovascular risk factors, type and site of vascular surgery, and age, preoperative statin initiation was still significantly associated with an improved long-term outcome (HR, 0.59).
"The randomized DECREASE III trial showed that perioperative statin use is associated with a significant reduction of perioperative cardiovascular events," according to Dr. Schouten. But it appears that statin therapy also results in a long-term survival benefit, compared with postoperative initiation of statin therapy, he added.
"This ‘legacy’ effect might be due to the prevention of perioperative myocardial damage, as patients with myocardial damage had a significantly higher risk of death during follow-up," Dr. Schouten speculated.
"The main message of our study is that all vascular surgery patients eligible for statin therapy [that is, without contraindications] should be prescribed statins at the first, preoperative, and outpatient clinic visit," said Dr. Schouten in an interview. He pointed out that statin therapy is safe in the perioperative period, with no significant side effects; it improves perioperative cardiac outcome; and it is associated with a long-term survival benefit.
"So prescribe statins as soon as possible, keep them on statins in the perioperative period, and keep them on [lifelong statins] after surgery," Dr. Schouten concluded.
Dr. Schouten stated that he had nothing to disclose.
CHICAGO – Results from a follow-up analysis of patients in the randomized DECREASE III trial showed that there is an apparent "legacy" effect of perioperative statin therapy, resulting in improved long-term survival, compared with statin initiation after vascular surgery.
Ischemic cardiac events are a major cause of perioperative morbidity and mortality in noncardiac surgery (including vascular surgery), with an estimated 10%-40% of perioperative deaths ascribed to myocardial infarction (MI), according to the original report by Dr. Don Poldermans and the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography) III researchers. Statins, which are associated with improved plaque stability, were plausible candidates to reduce perioperative MI. And in fact, results of the original DECREASE III study showed that in high-risk patients who undergo major vascular surgery, fluvastatin XL reduced myocardial ischemia and the combined end point of cardiovascular death and MI.
Dr. Olaf Schouten from the Erasmus University Medical Center, Rotterdam, the Netherlands, discussed a further analysis of the DECREASE III population at the Vascular Annual Meeting. The investigators examined a total of 497 patients who were randomized to placebo (247 patients) or fluvastatin (250) in the double-blinded trial.
The patients had been started on treatment a median of 34 days prior to surgery. At the end of the DECREASE III study period (30 days after surgery), all patients were prescribed lifelong statins as recommended by current guidelines. The current study relied on all-cause death data obtained from a civil service registry for a median follow-up of 4.8 years, during which time 129 patients died.
Perioperative statin use was associated with a significant reduction of perioperative cardiovascular events (hazard ratio, 0.55), according to Dr. Schouten. In a multivariate analysis that adjusted for possible confounders including cardiovascular risk factors, type and site of vascular surgery, and age, preoperative statin initiation was still significantly associated with an improved long-term outcome (HR, 0.59).
"The randomized DECREASE III trial showed that perioperative statin use is associated with a significant reduction of perioperative cardiovascular events," according to Dr. Schouten. But it appears that statin therapy also results in a long-term survival benefit, compared with postoperative initiation of statin therapy, he added.
"This ‘legacy’ effect might be due to the prevention of perioperative myocardial damage, as patients with myocardial damage had a significantly higher risk of death during follow-up," Dr. Schouten speculated.
"The main message of our study is that all vascular surgery patients eligible for statin therapy [that is, without contraindications] should be prescribed statins at the first, preoperative, and outpatient clinic visit," said Dr. Schouten in an interview. He pointed out that statin therapy is safe in the perioperative period, with no significant side effects; it improves perioperative cardiac outcome; and it is associated with a long-term survival benefit.
"So prescribe statins as soon as possible, keep them on statins in the perioperative period, and keep them on [lifelong statins] after surgery," Dr. Schouten concluded.
Dr. Schouten stated that he had nothing to disclose.
FROM THE VASCULAR ANNUAL MEETING
Benefits of Perioperative Statins Borne Out in Trial
CHICAGO – Results from a follow-up analysis of patients in the randomized DECREASE III trial showed that there is an apparent "legacy" effect of perioperative statin therapy, resulting in improved long-term survival, compared with statin initiation after vascular surgery.
Ischemic cardiac events are a major cause of perioperative morbidity and mortality in noncardiac surgery (including vascular surgery), with an estimated 10%-40% of perioperative deaths ascribed to myocardial infarction (MI), according to the original report by Dr. Don Poldermans and the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography) III researchers. Statins, which are associated with improved plaque stability, were plausible candidates to reduce perioperative MI. And in fact, results of the original DECREASE III study showed that in high-risk patients who undergo major vascular surgery, fluvastatin XL reduced myocardial ischemia and the combined end point of cardiovascular death and MI.
Dr. Olaf Schouten from the Erasmus University Medical Center, Rotterdam, the Netherlands, discussed a further analysis of the DECREASE III population at the Vascular Annual Meeting. The investigators examined a total of 497 patients who were randomized to placebo (247 patients) or fluvastatin (250) in the double-blinded trial.
The patients had been started on treatment a median of 34 days prior to surgery. At the end of the DECREASE III study period (30 days after surgery), all patients were prescribed lifelong statins as recommended by current guidelines. The current study relied on all-cause death data obtained from a civil service registry for a median follow-up of 4.8 years, during which time 129 patients died.
Perioperative statin use was associated with a significant reduction of perioperative cardiovascular events (hazard ratio, 0.55), according to Dr. Schouten. In a multivariate analysis that adjusted for possible confounders including cardiovascular risk factors, type and site of vascular surgery, and age, preoperative statin initiation was still significantly associated with an improved long-term outcome (HR, 0.59).
"The randomized DECREASE III trial showed that perioperative statin use is associated with a significant reduction of perioperative cardiovascular events," according to Dr. Schouten. But it appears that statin therapy also results in a long-term survival benefit, compared with postoperative initiation of statin therapy, he added.
"This ‘legacy’ effect might be due to the prevention of perioperative myocardial damage, as patients with myocardial damage had a significantly higher risk of death during follow-up," Dr. Schouten speculated.
"The main message of our study is that all vascular surgery patients eligible for statin therapy [that is, without contraindications] should be prescribed statins at the first, preoperative, and outpatient clinic visit," said Dr. Schouten in an interview. He pointed out that statin therapy is safe in the perioperative period, with no significant side effects; it improves perioperative cardiac outcome; and it is associated with a long-term survival benefit.
"So prescribe statins as soon as possible, keep them on statins in the perioperative period, and keep them on [lifelong statins] after surgery," Dr. Schouten concluded.
Dr. Schouten stated that he had nothing to disclose.
CHICAGO – Results from a follow-up analysis of patients in the randomized DECREASE III trial showed that there is an apparent "legacy" effect of perioperative statin therapy, resulting in improved long-term survival, compared with statin initiation after vascular surgery.
Ischemic cardiac events are a major cause of perioperative morbidity and mortality in noncardiac surgery (including vascular surgery), with an estimated 10%-40% of perioperative deaths ascribed to myocardial infarction (MI), according to the original report by Dr. Don Poldermans and the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography) III researchers. Statins, which are associated with improved plaque stability, were plausible candidates to reduce perioperative MI. And in fact, results of the original DECREASE III study showed that in high-risk patients who undergo major vascular surgery, fluvastatin XL reduced myocardial ischemia and the combined end point of cardiovascular death and MI.
Dr. Olaf Schouten from the Erasmus University Medical Center, Rotterdam, the Netherlands, discussed a further analysis of the DECREASE III population at the Vascular Annual Meeting. The investigators examined a total of 497 patients who were randomized to placebo (247 patients) or fluvastatin (250) in the double-blinded trial.
The patients had been started on treatment a median of 34 days prior to surgery. At the end of the DECREASE III study period (30 days after surgery), all patients were prescribed lifelong statins as recommended by current guidelines. The current study relied on all-cause death data obtained from a civil service registry for a median follow-up of 4.8 years, during which time 129 patients died.
Perioperative statin use was associated with a significant reduction of perioperative cardiovascular events (hazard ratio, 0.55), according to Dr. Schouten. In a multivariate analysis that adjusted for possible confounders including cardiovascular risk factors, type and site of vascular surgery, and age, preoperative statin initiation was still significantly associated with an improved long-term outcome (HR, 0.59).
"The randomized DECREASE III trial showed that perioperative statin use is associated with a significant reduction of perioperative cardiovascular events," according to Dr. Schouten. But it appears that statin therapy also results in a long-term survival benefit, compared with postoperative initiation of statin therapy, he added.
"This ‘legacy’ effect might be due to the prevention of perioperative myocardial damage, as patients with myocardial damage had a significantly higher risk of death during follow-up," Dr. Schouten speculated.
"The main message of our study is that all vascular surgery patients eligible for statin therapy [that is, without contraindications] should be prescribed statins at the first, preoperative, and outpatient clinic visit," said Dr. Schouten in an interview. He pointed out that statin therapy is safe in the perioperative period, with no significant side effects; it improves perioperative cardiac outcome; and it is associated with a long-term survival benefit.
"So prescribe statins as soon as possible, keep them on statins in the perioperative period, and keep them on [lifelong statins] after surgery," Dr. Schouten concluded.
Dr. Schouten stated that he had nothing to disclose.
CHICAGO – Results from a follow-up analysis of patients in the randomized DECREASE III trial showed that there is an apparent "legacy" effect of perioperative statin therapy, resulting in improved long-term survival, compared with statin initiation after vascular surgery.
Ischemic cardiac events are a major cause of perioperative morbidity and mortality in noncardiac surgery (including vascular surgery), with an estimated 10%-40% of perioperative deaths ascribed to myocardial infarction (MI), according to the original report by Dr. Don Poldermans and the DECREASE (Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography) III researchers. Statins, which are associated with improved plaque stability, were plausible candidates to reduce perioperative MI. And in fact, results of the original DECREASE III study showed that in high-risk patients who undergo major vascular surgery, fluvastatin XL reduced myocardial ischemia and the combined end point of cardiovascular death and MI.
Dr. Olaf Schouten from the Erasmus University Medical Center, Rotterdam, the Netherlands, discussed a further analysis of the DECREASE III population at the Vascular Annual Meeting. The investigators examined a total of 497 patients who were randomized to placebo (247 patients) or fluvastatin (250) in the double-blinded trial.
The patients had been started on treatment a median of 34 days prior to surgery. At the end of the DECREASE III study period (30 days after surgery), all patients were prescribed lifelong statins as recommended by current guidelines. The current study relied on all-cause death data obtained from a civil service registry for a median follow-up of 4.8 years, during which time 129 patients died.
Perioperative statin use was associated with a significant reduction of perioperative cardiovascular events (hazard ratio, 0.55), according to Dr. Schouten. In a multivariate analysis that adjusted for possible confounders including cardiovascular risk factors, type and site of vascular surgery, and age, preoperative statin initiation was still significantly associated with an improved long-term outcome (HR, 0.59).
"The randomized DECREASE III trial showed that perioperative statin use is associated with a significant reduction of perioperative cardiovascular events," according to Dr. Schouten. But it appears that statin therapy also results in a long-term survival benefit, compared with postoperative initiation of statin therapy, he added.
"This ‘legacy’ effect might be due to the prevention of perioperative myocardial damage, as patients with myocardial damage had a significantly higher risk of death during follow-up," Dr. Schouten speculated.
"The main message of our study is that all vascular surgery patients eligible for statin therapy [that is, without contraindications] should be prescribed statins at the first, preoperative, and outpatient clinic visit," said Dr. Schouten in an interview. He pointed out that statin therapy is safe in the perioperative period, with no significant side effects; it improves perioperative cardiac outcome; and it is associated with a long-term survival benefit.
"So prescribe statins as soon as possible, keep them on statins in the perioperative period, and keep them on [lifelong statins] after surgery," Dr. Schouten concluded.
Dr. Schouten stated that he had nothing to disclose.
FROM THE VASCULAR ANNUAL MEETING
Major Finding: Perioperative statin use was associated with a significant reduction of perioperative cardiovascular events (HR, 0.55) and improved long-term outcome (HR, 0.59).
Data Source: A further analysis of 497 patients in the randomized, double-blind, DECREASE III trial.
Disclosures: Dr. Schouten stated that he had nothing to disclose.