User login
The “Things We Do for No Reason” series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
CASE PRESENTATION
A 12-month-old female is admitted for acute bronchiolitis with increased work of breathing and decreased oral intake. She is mildly dehydrated upon exam with a sodium level of 139 mEq/L and is given a 20 mL/kg bolus of 0.9% saline. Given the patient’s poor oral intake, the admitting intern orders maintenance intravenous (IV) fluids and asks her senior resident which IV fluid should be used. The medical student on the team wonders if a different IV fluid would be selected for a 2-week-old with a similar presentation.
INTRODUCTION
Maintenance IV fluids are continuously infused to preserve extracellular volume and electrolyte balance when fluids cannot be taken orally. In contrast, resuscitation IV fluids are given as a bolus to patients in states of hypoperfusion to restore extracellular volume. The given IV fluid concentration can be categorized as approximately equal to (isotonic) or less than (hypotonic) the plasma sodium concentration. Refer to Table 1 for the electrolyte composition of commonly used IV fluids. Dextrose is rapidly metabolized upon infusion and does not affect tonicity.
Why You Might Think Hypotonic Maintenance IV Fluids Are The Right Choice
A 1957 publication by Holliday and Segar laid the foundation for maintenance IV fluid and electrolyte requirements in children and was the initial catalyst for the use of hypotonic maintenance IV fluids.1 This manuscript contended that hypotonic IV fluids could supply the water and sodium needed to meet maintenance dietary requirements. This claim led to the predominant use of hypotonic maintenance IV fluids in children. By contrast, isotonic IV fluids have been avoided given the apprehension over electrolytes exceeding maintenance needs.
Concerns about the unintended consequences of fluid overload – edema, hypernatremia, and hypertension secondary to increased sodium load – have led some to avoid isotonic IV fluids.2 When presented with common clinical scenarios of patients at risk for excess antidiuretic hormone (ADH; also known as arginine vasopressin), pediatric residents chose hypotonic (instead of isotonic) IV fluids 78% of the time.3
Why Isotonic Maintenance IV Fluids Are Usually The Right Choice For Children
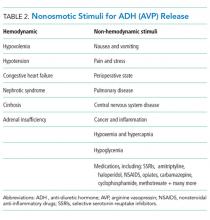
General recommendations for hypotonic IV fluids are primarily based on theoretical calculations from the fluid and electrolyte requirements of healthy individuals, and studies have not validated the use of hypotonic IV fluids in clinical practice.1 Acutely ill patients are at risk for excessive levels of ADH from numerous causes (see Table 2).2 As a result, nearly every hospitalized patient is at risk for excess ADH release, thus making them vulnerable to the development of hyponatremia. The syndrome of inappropriate secretion of ADH (SIADH) occurs when nonosmotic/nonhemodynamic stimuli trigger ADH release, which leads to excessive free-water retention and resultant hyponatremia. Schwartz and Bartter reported the first two cases of SIADH in 1957 when hyponatremia developed in the setting of bronchogenic carcinoma.4 Although the publication by Holliday and Seger did acknowledge the potential for water intoxication, it was written before this report and before the effects of ADH on the sodium levels of hospitalized patients were clearly understood.2 SIADH is now recognized as one of the most common causes of hyponatremia in hospitalized patients.5, 6
Numerous studies have demonstrated that patients who receive hypotonic IV fluids have a significantly higher risk of developing hyponatremia than patients who receive isotonic IV fluids.7,8 An infrequent, yet serious, complication of iatrogenic hyponatremia is hyponatremic encephalopathy, which carries a high rate of morbidity or mortality.9 The prevention of hyponatremia is essential as the early symptoms of hyponatremic encephalopathy are nonspecific and can be easily missed.2
More than 15 prospective randomized controlled trials (RCTs) involving over 2,000 children have demonstrated that isotonic IV fluids are more effective in preventing hospital-acquired hyponatremia than hypotonic IV fluids and are not associated with the development of fluid overload or hypernatremia. A 2014 metaanalysis comprising 10 RCTs and involving over 800 children found that when compared with isotonic IV fluids, hypotonic IV fluids present a relative risk of 2.37 for sodium levels to drop below 135 mEq/L and a relative risk of 6.1 for levels to drop below 130 mEq/L. The numbers needed to treat (NNT) with isotonic IV fluids to prevent hyponatremia in each group were 6 and 17, respectively.7 A Cochrane review published in 2014 presented comparable findings, demonstrating that hypotonic IV fluids had a 34% risk of causing hyponatremia; by comparison, isotonic IV fluids had a 17% risk of causing hyponatremia and a NNT of six to prevent hyponatremia.8 In a large RCT conducted in 2015 with 676 pediatric patients, McNabb et al. found that when compared with patients receiving isotonic IV fluids, those receiving hypotonic IV fluids had a higher incidence of developing hyponatremia (10.9% versus 3.8%) with a NNT of 15 to prevent hyponatremia with the use of isotonic fluids.10 Published trials have likely been underpowered to detect a difference in the infrequent adverse hyponatremia outcomes of seizures and mortality.
On the basis of these data, patient safety alerts have recommended the avoidance of hypotonic IV fluids in the United Kingdom (UK) and Australia, and the 2015 UK guidelines for children now recommend isotonic IV fluids for maintenance needs.11 Although many of the aforementioned studies included predominantly critically ill or surgical pediatric patients, the risk of hyponatremia with hypotonic IV fluids seems similarly increased in nonsurgical and noncritically ill pediatric patients.10
For patients at risk for excess ADH release, some have supported the use of hypotonic IV fluids at a lower than maintenance rate to theoretically decrease the risk of hyponatremia, but this practice has not been effective in preventing hyponatremia.2,12 Unless a patient is in a fluid overload state, such as in congestive heart failure, cirrhosis, or renal failure; isotonic maintenance IV fluids should not result in fluid overload.3 Available evidence for guiding maintenance IV fluid choice in neonates or young infants is limited. Nevertheless, given the aforementioned reasons, we generally recommend the prescription of isotonic IV fluids for most in this population.
Which Isotonic IV Fluid Should Be Used?
The sodium concentration (154 mmol/L) of 0.9% saline, an isotonic IV fluid, is approximately equal to the tonicity of the aqueous phase of plasma. The majority of studies evaluating the risk of hyponatremia with maintenance IV fluids have used 0.9% saline as the studied isotonic IV fluid. Plasma-Lyte and Ringer’s lactate are low-chloride, buffered/balanced solutions. Plasma-Lyte ([Na] = 140 mmol/L) has been demonstrated to be effective in preventing hyponatremia. Ringers’ lactate is slightly hypotonic ([Na] = 130 mmol/L), and its administration is associated with a decrease in serum sodium.13 A resultant dilutional and hyperchloremic metabolic acidosis is more likely to develop with the use of large volumes of 0.9% saline in resuscitation than with the use of balanced solutions.2 Whether the prolonged use of 0.9% saline maintenance IV fluids can lead to this same side effect remains unknown given insufficient evidence.2 Retrospective studies using balanced solutions have shown an association with decreased rates of acute kidney injury (AKI) and mortality when compared with 0.9% saline. However, a RCT with over 2,000 adult ICU patients showed no change in rates of AKI in those that received Plasma-Lyte compared with those who received 0.9% saline.14
Two recent, single-center, prospective studies compared the use of Ringer’s lactate or Plasma-Lyte for resuscitation with that of 0.9% saline. One study was comprised of 15,802 critically ill adults, and the other was comprised of 13,347 noncritically adults. Both studies showed that balanced solutions decreased the rate of major adverse kidney events (defined as a composite of death from any cause, new renal-replacement therapy, or persistent renal injury) within 30 days.15,16 Available published pediatric studies indicate that 0.9% saline is an effective maintenance IV fluid for the prevention of hyponatremia that is not associated with hypernatremia or fluid overload. Further pediatric studies comparing 0.9% saline with balanced solutions are needed.
When Should We Use Hypotonic IV Fluids?
Hypotonic IV fluids may be needed for patients with hypernatremia and a free-water deficit or a renal-concentrating defect with ongoing urinary free-water losses.2 Special care should be taken when choosing maintenance IV fluids for patients with renal disease, liver disease, or heart failure given that these groups have been excluded from some studies.12 These patients may be at risk for increased salt and fluid retention with any IV fluid, and fluid rates need to be restricted. The fluid intake of patients with hyponatremia secondary to SIADH needs close management; these patients benefit from total fluid restriction instead of standard maintenance IV fluid rates.2
What We Should Do Instead?
Maintenance IV fluids should only be used when necessary and should be stopped as soon as they are no longer required, especially in light of the recent shortages in 0.9% saline.17 Similar to all medications, maintenance IV fluids should be individualized to the patient’s needs on the basis of the indication for IV fluids and the patient’s comorbidities.2 Consideration should be given to checking the patient’s electrolyte levels to monitor response to IV fluids, especially during the first 24 hours of admission when risk of hyponatremia is highest. Isotonic IV fluids with 5% dextrose should be used as the maintenance IV fluid in the majority of hospitalized children given its proven benefit in decreasing the rate of hospital-acquired hyponatremia.7,8 Hypotonic IV fluids should be avoided as the default maintenance IV fluid and should only be utilized under specific circumstances.
RECOMMENDATIONS
- When needed, maintenance IV fluids should always be tailored to each individual patient.
- For most acutely ill hospitalized children, isotonic IV fluids should be the maintenance IV fluid of choice.
- Consider monitoring electrolytes to determine the effects of maintenance IV fluids.
CONCLUSION
Enteral maintenance fluids should be used first-line if possible. Although hypotonic IV fluids have historically been the maintenance IV fluid of choice, this class of IV fluids should be avoided for most hospitalized children to decrease the significant risk of iatrogenic hyponatremia, which can be severe and have catastrophic complications. When necessary, isotonic IV fluids should be used for the majority of hospitalized children given that these fluids present a significantly decreased risk for causing hyponatremia. Returning to our case presentation, to decrease the risk of hyponatremia, the senior resident should recommend starting isotonic IV fluids in the 12-month-old and theoretical 2-week-old until oral intake can be maintained.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason”? Let us know what you do in your practice and propose ideas for other “Things We Do for No Reason” topics. Please join in the conversation online at Twitter (#TWDFNR)/Facebook and don’t forget to “Like It” on Facebook or retweet it on Twitter.
Disclosure
The authors have no relevant conflicts of interest to report. No payment or services from a 3rd party were received for any aspect of this submitted work. The authors have no financial relationships with entities in the biomedical arena that could be perceived to influence, or that give the appearance of potentially influencing, what was written in this submitted work.
1. Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics. 1957;19(5):823-832. PubMed
2. Moritz ML, Ayus JC. Maintenance intravenous fluids in acutely Ill patients. N Engl J Med. 2015;373(14):1350-1360. doi: 10.1056/NEJMra1412877. PubMed
3. Freeman MA, Ayus JC, Moritz ML. Maintenance intravenous fluid prescribing practices among paediatric residents. Acta Paediatr. 2012;101(10):e465-e468. doi: 10.1111/j.1651-2227.2012.02780.x. PubMed
4. Schwartz WB BW, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med. 1957;23(4):529-542. doi: 10.1016/0002-9343(57)90224-3. PubMed
5. Wattad A, Chiang ML, Hill LL. Hyponatremia in hospitalized children. Clin Pediatr. 1992;31(3):153-157. doi: 10.1177/000992289203100305. PubMed
6. Greenberg A, Verbalis JG, Amin AN, et al. Current treatment practice and outcomes. Report of the hyponatremia registry. Kidney Int. 2015;88(1):167-177. doi: 10.1038/ki.2015.4. PubMed
7. Foster BA, Tom D, Hill V. Hypotonic versus isotonic fluids in hospitalized children: A systematic review and meta-analysis. J Pediatr. 2014;165(1):163-169.e162. doi: 10.1016/j.jpeds.2014.01.040. PubMed
8. McNab S, Ware RS, Neville KA, et al. Isotonic versus hypotonic solutions for maintenance intravenous fluid administration in children. Cochrane Database Syst Rev. 2014;(12):CD009457. doi: 10.1002/14651858.CD009457.pub2. PubMed
9. Arieff AI, Ayus JC, Fraser CL. Hyponatraemia and death or permanent brain damage in healthy children. BMJ. 1992;304(6836):1218-1222. doi: 10.1136/bmj.304.6836.1218. PubMed
10. McNab S, Duke T, South M, et al. 140 mmol/L of sodium versus 77 mmol/L of sodium in maintenance intravenous fluid therapy for children in hospital (PIMS): A randomised controlled double-blind trial. Lancet. 2015;385(9974):1190-1197. doi: 10.1016/S0140-6736(14)61459-8. PubMed
11. Neilson J, O’Neill F, Dawoud D, Crean P, Guideline Development G. Intravenous fluids in children and young people: summary of NICE guidance. BMJ. 2015;351:h6388. doi: 10.1136/bmj.h6388. PubMed
12. Neville KA, Sandeman DJ, Rubinstein A, Henry GM, McGlynn M, Walker JL. Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective randomized study of fluid type versus fluid rate. J Pediatr. 2010;156(2):313-319. doi: 10.1016/j.jpeds.2009.07.059. PubMed
13. Moritz ML, Ayus JC. Preventing neurological complications from dysnatremias in children. Pediatr Nephrol. 2005;20(12):1687-1700. doi: 10.1007/s00467-005-1933-6. PubMed
14. Young P, Bailey M, Beasley R, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: The SPLIT Randomized Clinical Trial. JAMA. 2015;314(16):1701-1710. doi: 10.1001/jama.2015.12334. PubMed
15. Semler MW, Self WH, Wanderer JP, et al. Balanced crystalloids versus salinein critically Ill adults. N Engl J Med. 2018;378(9):829-839. doi: 10.1056/NEJMoa1711584. PubMed
16. Self WH, Semler MW, Wanderer JP, et al. Balanced crystalloids versus saline in noncritically Ill adults. N Engl J Med. 2018;378(9):819-828. doi: 10.1056/NEJMoa1711586. PubMed
17. Mazer-Amirshahi M, Fox ER. Saline shortages - Many causes, no simple solution. N Engl J Med. 2018;378(16):1472-1474. doi: 10.1056/NEJMp1800347. PubMed
The “Things We Do for No Reason” series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
CASE PRESENTATION
A 12-month-old female is admitted for acute bronchiolitis with increased work of breathing and decreased oral intake. She is mildly dehydrated upon exam with a sodium level of 139 mEq/L and is given a 20 mL/kg bolus of 0.9% saline. Given the patient’s poor oral intake, the admitting intern orders maintenance intravenous (IV) fluids and asks her senior resident which IV fluid should be used. The medical student on the team wonders if a different IV fluid would be selected for a 2-week-old with a similar presentation.
INTRODUCTION
Maintenance IV fluids are continuously infused to preserve extracellular volume and electrolyte balance when fluids cannot be taken orally. In contrast, resuscitation IV fluids are given as a bolus to patients in states of hypoperfusion to restore extracellular volume. The given IV fluid concentration can be categorized as approximately equal to (isotonic) or less than (hypotonic) the plasma sodium concentration. Refer to Table 1 for the electrolyte composition of commonly used IV fluids. Dextrose is rapidly metabolized upon infusion and does not affect tonicity.
Why You Might Think Hypotonic Maintenance IV Fluids Are The Right Choice
A 1957 publication by Holliday and Segar laid the foundation for maintenance IV fluid and electrolyte requirements in children and was the initial catalyst for the use of hypotonic maintenance IV fluids.1 This manuscript contended that hypotonic IV fluids could supply the water and sodium needed to meet maintenance dietary requirements. This claim led to the predominant use of hypotonic maintenance IV fluids in children. By contrast, isotonic IV fluids have been avoided given the apprehension over electrolytes exceeding maintenance needs.
Concerns about the unintended consequences of fluid overload – edema, hypernatremia, and hypertension secondary to increased sodium load – have led some to avoid isotonic IV fluids.2 When presented with common clinical scenarios of patients at risk for excess antidiuretic hormone (ADH; also known as arginine vasopressin), pediatric residents chose hypotonic (instead of isotonic) IV fluids 78% of the time.3
Why Isotonic Maintenance IV Fluids Are Usually The Right Choice For Children
General recommendations for hypotonic IV fluids are primarily based on theoretical calculations from the fluid and electrolyte requirements of healthy individuals, and studies have not validated the use of hypotonic IV fluids in clinical practice.1 Acutely ill patients are at risk for excessive levels of ADH from numerous causes (see Table 2).2 As a result, nearly every hospitalized patient is at risk for excess ADH release, thus making them vulnerable to the development of hyponatremia. The syndrome of inappropriate secretion of ADH (SIADH) occurs when nonosmotic/nonhemodynamic stimuli trigger ADH release, which leads to excessive free-water retention and resultant hyponatremia. Schwartz and Bartter reported the first two cases of SIADH in 1957 when hyponatremia developed in the setting of bronchogenic carcinoma.4 Although the publication by Holliday and Seger did acknowledge the potential for water intoxication, it was written before this report and before the effects of ADH on the sodium levels of hospitalized patients were clearly understood.2 SIADH is now recognized as one of the most common causes of hyponatremia in hospitalized patients.5, 6
Numerous studies have demonstrated that patients who receive hypotonic IV fluids have a significantly higher risk of developing hyponatremia than patients who receive isotonic IV fluids.7,8 An infrequent, yet serious, complication of iatrogenic hyponatremia is hyponatremic encephalopathy, which carries a high rate of morbidity or mortality.9 The prevention of hyponatremia is essential as the early symptoms of hyponatremic encephalopathy are nonspecific and can be easily missed.2
More than 15 prospective randomized controlled trials (RCTs) involving over 2,000 children have demonstrated that isotonic IV fluids are more effective in preventing hospital-acquired hyponatremia than hypotonic IV fluids and are not associated with the development of fluid overload or hypernatremia. A 2014 metaanalysis comprising 10 RCTs and involving over 800 children found that when compared with isotonic IV fluids, hypotonic IV fluids present a relative risk of 2.37 for sodium levels to drop below 135 mEq/L and a relative risk of 6.1 for levels to drop below 130 mEq/L. The numbers needed to treat (NNT) with isotonic IV fluids to prevent hyponatremia in each group were 6 and 17, respectively.7 A Cochrane review published in 2014 presented comparable findings, demonstrating that hypotonic IV fluids had a 34% risk of causing hyponatremia; by comparison, isotonic IV fluids had a 17% risk of causing hyponatremia and a NNT of six to prevent hyponatremia.8 In a large RCT conducted in 2015 with 676 pediatric patients, McNabb et al. found that when compared with patients receiving isotonic IV fluids, those receiving hypotonic IV fluids had a higher incidence of developing hyponatremia (10.9% versus 3.8%) with a NNT of 15 to prevent hyponatremia with the use of isotonic fluids.10 Published trials have likely been underpowered to detect a difference in the infrequent adverse hyponatremia outcomes of seizures and mortality.
On the basis of these data, patient safety alerts have recommended the avoidance of hypotonic IV fluids in the United Kingdom (UK) and Australia, and the 2015 UK guidelines for children now recommend isotonic IV fluids for maintenance needs.11 Although many of the aforementioned studies included predominantly critically ill or surgical pediatric patients, the risk of hyponatremia with hypotonic IV fluids seems similarly increased in nonsurgical and noncritically ill pediatric patients.10
For patients at risk for excess ADH release, some have supported the use of hypotonic IV fluids at a lower than maintenance rate to theoretically decrease the risk of hyponatremia, but this practice has not been effective in preventing hyponatremia.2,12 Unless a patient is in a fluid overload state, such as in congestive heart failure, cirrhosis, or renal failure; isotonic maintenance IV fluids should not result in fluid overload.3 Available evidence for guiding maintenance IV fluid choice in neonates or young infants is limited. Nevertheless, given the aforementioned reasons, we generally recommend the prescription of isotonic IV fluids for most in this population.
Which Isotonic IV Fluid Should Be Used?
The sodium concentration (154 mmol/L) of 0.9% saline, an isotonic IV fluid, is approximately equal to the tonicity of the aqueous phase of plasma. The majority of studies evaluating the risk of hyponatremia with maintenance IV fluids have used 0.9% saline as the studied isotonic IV fluid. Plasma-Lyte and Ringer’s lactate are low-chloride, buffered/balanced solutions. Plasma-Lyte ([Na] = 140 mmol/L) has been demonstrated to be effective in preventing hyponatremia. Ringers’ lactate is slightly hypotonic ([Na] = 130 mmol/L), and its administration is associated with a decrease in serum sodium.13 A resultant dilutional and hyperchloremic metabolic acidosis is more likely to develop with the use of large volumes of 0.9% saline in resuscitation than with the use of balanced solutions.2 Whether the prolonged use of 0.9% saline maintenance IV fluids can lead to this same side effect remains unknown given insufficient evidence.2 Retrospective studies using balanced solutions have shown an association with decreased rates of acute kidney injury (AKI) and mortality when compared with 0.9% saline. However, a RCT with over 2,000 adult ICU patients showed no change in rates of AKI in those that received Plasma-Lyte compared with those who received 0.9% saline.14
Two recent, single-center, prospective studies compared the use of Ringer’s lactate or Plasma-Lyte for resuscitation with that of 0.9% saline. One study was comprised of 15,802 critically ill adults, and the other was comprised of 13,347 noncritically adults. Both studies showed that balanced solutions decreased the rate of major adverse kidney events (defined as a composite of death from any cause, new renal-replacement therapy, or persistent renal injury) within 30 days.15,16 Available published pediatric studies indicate that 0.9% saline is an effective maintenance IV fluid for the prevention of hyponatremia that is not associated with hypernatremia or fluid overload. Further pediatric studies comparing 0.9% saline with balanced solutions are needed.
When Should We Use Hypotonic IV Fluids?
Hypotonic IV fluids may be needed for patients with hypernatremia and a free-water deficit or a renal-concentrating defect with ongoing urinary free-water losses.2 Special care should be taken when choosing maintenance IV fluids for patients with renal disease, liver disease, or heart failure given that these groups have been excluded from some studies.12 These patients may be at risk for increased salt and fluid retention with any IV fluid, and fluid rates need to be restricted. The fluid intake of patients with hyponatremia secondary to SIADH needs close management; these patients benefit from total fluid restriction instead of standard maintenance IV fluid rates.2
What We Should Do Instead?
Maintenance IV fluids should only be used when necessary and should be stopped as soon as they are no longer required, especially in light of the recent shortages in 0.9% saline.17 Similar to all medications, maintenance IV fluids should be individualized to the patient’s needs on the basis of the indication for IV fluids and the patient’s comorbidities.2 Consideration should be given to checking the patient’s electrolyte levels to monitor response to IV fluids, especially during the first 24 hours of admission when risk of hyponatremia is highest. Isotonic IV fluids with 5% dextrose should be used as the maintenance IV fluid in the majority of hospitalized children given its proven benefit in decreasing the rate of hospital-acquired hyponatremia.7,8 Hypotonic IV fluids should be avoided as the default maintenance IV fluid and should only be utilized under specific circumstances.
RECOMMENDATIONS
- When needed, maintenance IV fluids should always be tailored to each individual patient.
- For most acutely ill hospitalized children, isotonic IV fluids should be the maintenance IV fluid of choice.
- Consider monitoring electrolytes to determine the effects of maintenance IV fluids.
CONCLUSION
Enteral maintenance fluids should be used first-line if possible. Although hypotonic IV fluids have historically been the maintenance IV fluid of choice, this class of IV fluids should be avoided for most hospitalized children to decrease the significant risk of iatrogenic hyponatremia, which can be severe and have catastrophic complications. When necessary, isotonic IV fluids should be used for the majority of hospitalized children given that these fluids present a significantly decreased risk for causing hyponatremia. Returning to our case presentation, to decrease the risk of hyponatremia, the senior resident should recommend starting isotonic IV fluids in the 12-month-old and theoretical 2-week-old until oral intake can be maintained.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason”? Let us know what you do in your practice and propose ideas for other “Things We Do for No Reason” topics. Please join in the conversation online at Twitter (#TWDFNR)/Facebook and don’t forget to “Like It” on Facebook or retweet it on Twitter.
Disclosure
The authors have no relevant conflicts of interest to report. No payment or services from a 3rd party were received for any aspect of this submitted work. The authors have no financial relationships with entities in the biomedical arena that could be perceived to influence, or that give the appearance of potentially influencing, what was written in this submitted work.
The “Things We Do for No Reason” series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
CASE PRESENTATION
A 12-month-old female is admitted for acute bronchiolitis with increased work of breathing and decreased oral intake. She is mildly dehydrated upon exam with a sodium level of 139 mEq/L and is given a 20 mL/kg bolus of 0.9% saline. Given the patient’s poor oral intake, the admitting intern orders maintenance intravenous (IV) fluids and asks her senior resident which IV fluid should be used. The medical student on the team wonders if a different IV fluid would be selected for a 2-week-old with a similar presentation.
INTRODUCTION
Maintenance IV fluids are continuously infused to preserve extracellular volume and electrolyte balance when fluids cannot be taken orally. In contrast, resuscitation IV fluids are given as a bolus to patients in states of hypoperfusion to restore extracellular volume. The given IV fluid concentration can be categorized as approximately equal to (isotonic) or less than (hypotonic) the plasma sodium concentration. Refer to Table 1 for the electrolyte composition of commonly used IV fluids. Dextrose is rapidly metabolized upon infusion and does not affect tonicity.
Why You Might Think Hypotonic Maintenance IV Fluids Are The Right Choice
A 1957 publication by Holliday and Segar laid the foundation for maintenance IV fluid and electrolyte requirements in children and was the initial catalyst for the use of hypotonic maintenance IV fluids.1 This manuscript contended that hypotonic IV fluids could supply the water and sodium needed to meet maintenance dietary requirements. This claim led to the predominant use of hypotonic maintenance IV fluids in children. By contrast, isotonic IV fluids have been avoided given the apprehension over electrolytes exceeding maintenance needs.
Concerns about the unintended consequences of fluid overload – edema, hypernatremia, and hypertension secondary to increased sodium load – have led some to avoid isotonic IV fluids.2 When presented with common clinical scenarios of patients at risk for excess antidiuretic hormone (ADH; also known as arginine vasopressin), pediatric residents chose hypotonic (instead of isotonic) IV fluids 78% of the time.3
Why Isotonic Maintenance IV Fluids Are Usually The Right Choice For Children
General recommendations for hypotonic IV fluids are primarily based on theoretical calculations from the fluid and electrolyte requirements of healthy individuals, and studies have not validated the use of hypotonic IV fluids in clinical practice.1 Acutely ill patients are at risk for excessive levels of ADH from numerous causes (see Table 2).2 As a result, nearly every hospitalized patient is at risk for excess ADH release, thus making them vulnerable to the development of hyponatremia. The syndrome of inappropriate secretion of ADH (SIADH) occurs when nonosmotic/nonhemodynamic stimuli trigger ADH release, which leads to excessive free-water retention and resultant hyponatremia. Schwartz and Bartter reported the first two cases of SIADH in 1957 when hyponatremia developed in the setting of bronchogenic carcinoma.4 Although the publication by Holliday and Seger did acknowledge the potential for water intoxication, it was written before this report and before the effects of ADH on the sodium levels of hospitalized patients were clearly understood.2 SIADH is now recognized as one of the most common causes of hyponatremia in hospitalized patients.5, 6
Numerous studies have demonstrated that patients who receive hypotonic IV fluids have a significantly higher risk of developing hyponatremia than patients who receive isotonic IV fluids.7,8 An infrequent, yet serious, complication of iatrogenic hyponatremia is hyponatremic encephalopathy, which carries a high rate of morbidity or mortality.9 The prevention of hyponatremia is essential as the early symptoms of hyponatremic encephalopathy are nonspecific and can be easily missed.2
More than 15 prospective randomized controlled trials (RCTs) involving over 2,000 children have demonstrated that isotonic IV fluids are more effective in preventing hospital-acquired hyponatremia than hypotonic IV fluids and are not associated with the development of fluid overload or hypernatremia. A 2014 metaanalysis comprising 10 RCTs and involving over 800 children found that when compared with isotonic IV fluids, hypotonic IV fluids present a relative risk of 2.37 for sodium levels to drop below 135 mEq/L and a relative risk of 6.1 for levels to drop below 130 mEq/L. The numbers needed to treat (NNT) with isotonic IV fluids to prevent hyponatremia in each group were 6 and 17, respectively.7 A Cochrane review published in 2014 presented comparable findings, demonstrating that hypotonic IV fluids had a 34% risk of causing hyponatremia; by comparison, isotonic IV fluids had a 17% risk of causing hyponatremia and a NNT of six to prevent hyponatremia.8 In a large RCT conducted in 2015 with 676 pediatric patients, McNabb et al. found that when compared with patients receiving isotonic IV fluids, those receiving hypotonic IV fluids had a higher incidence of developing hyponatremia (10.9% versus 3.8%) with a NNT of 15 to prevent hyponatremia with the use of isotonic fluids.10 Published trials have likely been underpowered to detect a difference in the infrequent adverse hyponatremia outcomes of seizures and mortality.
On the basis of these data, patient safety alerts have recommended the avoidance of hypotonic IV fluids in the United Kingdom (UK) and Australia, and the 2015 UK guidelines for children now recommend isotonic IV fluids for maintenance needs.11 Although many of the aforementioned studies included predominantly critically ill or surgical pediatric patients, the risk of hyponatremia with hypotonic IV fluids seems similarly increased in nonsurgical and noncritically ill pediatric patients.10
For patients at risk for excess ADH release, some have supported the use of hypotonic IV fluids at a lower than maintenance rate to theoretically decrease the risk of hyponatremia, but this practice has not been effective in preventing hyponatremia.2,12 Unless a patient is in a fluid overload state, such as in congestive heart failure, cirrhosis, or renal failure; isotonic maintenance IV fluids should not result in fluid overload.3 Available evidence for guiding maintenance IV fluid choice in neonates or young infants is limited. Nevertheless, given the aforementioned reasons, we generally recommend the prescription of isotonic IV fluids for most in this population.
Which Isotonic IV Fluid Should Be Used?
The sodium concentration (154 mmol/L) of 0.9% saline, an isotonic IV fluid, is approximately equal to the tonicity of the aqueous phase of plasma. The majority of studies evaluating the risk of hyponatremia with maintenance IV fluids have used 0.9% saline as the studied isotonic IV fluid. Plasma-Lyte and Ringer’s lactate are low-chloride, buffered/balanced solutions. Plasma-Lyte ([Na] = 140 mmol/L) has been demonstrated to be effective in preventing hyponatremia. Ringers’ lactate is slightly hypotonic ([Na] = 130 mmol/L), and its administration is associated with a decrease in serum sodium.13 A resultant dilutional and hyperchloremic metabolic acidosis is more likely to develop with the use of large volumes of 0.9% saline in resuscitation than with the use of balanced solutions.2 Whether the prolonged use of 0.9% saline maintenance IV fluids can lead to this same side effect remains unknown given insufficient evidence.2 Retrospective studies using balanced solutions have shown an association with decreased rates of acute kidney injury (AKI) and mortality when compared with 0.9% saline. However, a RCT with over 2,000 adult ICU patients showed no change in rates of AKI in those that received Plasma-Lyte compared with those who received 0.9% saline.14
Two recent, single-center, prospective studies compared the use of Ringer’s lactate or Plasma-Lyte for resuscitation with that of 0.9% saline. One study was comprised of 15,802 critically ill adults, and the other was comprised of 13,347 noncritically adults. Both studies showed that balanced solutions decreased the rate of major adverse kidney events (defined as a composite of death from any cause, new renal-replacement therapy, or persistent renal injury) within 30 days.15,16 Available published pediatric studies indicate that 0.9% saline is an effective maintenance IV fluid for the prevention of hyponatremia that is not associated with hypernatremia or fluid overload. Further pediatric studies comparing 0.9% saline with balanced solutions are needed.
When Should We Use Hypotonic IV Fluids?
Hypotonic IV fluids may be needed for patients with hypernatremia and a free-water deficit or a renal-concentrating defect with ongoing urinary free-water losses.2 Special care should be taken when choosing maintenance IV fluids for patients with renal disease, liver disease, or heart failure given that these groups have been excluded from some studies.12 These patients may be at risk for increased salt and fluid retention with any IV fluid, and fluid rates need to be restricted. The fluid intake of patients with hyponatremia secondary to SIADH needs close management; these patients benefit from total fluid restriction instead of standard maintenance IV fluid rates.2
What We Should Do Instead?
Maintenance IV fluids should only be used when necessary and should be stopped as soon as they are no longer required, especially in light of the recent shortages in 0.9% saline.17 Similar to all medications, maintenance IV fluids should be individualized to the patient’s needs on the basis of the indication for IV fluids and the patient’s comorbidities.2 Consideration should be given to checking the patient’s electrolyte levels to monitor response to IV fluids, especially during the first 24 hours of admission when risk of hyponatremia is highest. Isotonic IV fluids with 5% dextrose should be used as the maintenance IV fluid in the majority of hospitalized children given its proven benefit in decreasing the rate of hospital-acquired hyponatremia.7,8 Hypotonic IV fluids should be avoided as the default maintenance IV fluid and should only be utilized under specific circumstances.
RECOMMENDATIONS
- When needed, maintenance IV fluids should always be tailored to each individual patient.
- For most acutely ill hospitalized children, isotonic IV fluids should be the maintenance IV fluid of choice.
- Consider monitoring electrolytes to determine the effects of maintenance IV fluids.
CONCLUSION
Enteral maintenance fluids should be used first-line if possible. Although hypotonic IV fluids have historically been the maintenance IV fluid of choice, this class of IV fluids should be avoided for most hospitalized children to decrease the significant risk of iatrogenic hyponatremia, which can be severe and have catastrophic complications. When necessary, isotonic IV fluids should be used for the majority of hospitalized children given that these fluids present a significantly decreased risk for causing hyponatremia. Returning to our case presentation, to decrease the risk of hyponatremia, the senior resident should recommend starting isotonic IV fluids in the 12-month-old and theoretical 2-week-old until oral intake can be maintained.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason”? Let us know what you do in your practice and propose ideas for other “Things We Do for No Reason” topics. Please join in the conversation online at Twitter (#TWDFNR)/Facebook and don’t forget to “Like It” on Facebook or retweet it on Twitter.
Disclosure
The authors have no relevant conflicts of interest to report. No payment or services from a 3rd party were received for any aspect of this submitted work. The authors have no financial relationships with entities in the biomedical arena that could be perceived to influence, or that give the appearance of potentially influencing, what was written in this submitted work.
1. Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics. 1957;19(5):823-832. PubMed
2. Moritz ML, Ayus JC. Maintenance intravenous fluids in acutely Ill patients. N Engl J Med. 2015;373(14):1350-1360. doi: 10.1056/NEJMra1412877. PubMed
3. Freeman MA, Ayus JC, Moritz ML. Maintenance intravenous fluid prescribing practices among paediatric residents. Acta Paediatr. 2012;101(10):e465-e468. doi: 10.1111/j.1651-2227.2012.02780.x. PubMed
4. Schwartz WB BW, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med. 1957;23(4):529-542. doi: 10.1016/0002-9343(57)90224-3. PubMed
5. Wattad A, Chiang ML, Hill LL. Hyponatremia in hospitalized children. Clin Pediatr. 1992;31(3):153-157. doi: 10.1177/000992289203100305. PubMed
6. Greenberg A, Verbalis JG, Amin AN, et al. Current treatment practice and outcomes. Report of the hyponatremia registry. Kidney Int. 2015;88(1):167-177. doi: 10.1038/ki.2015.4. PubMed
7. Foster BA, Tom D, Hill V. Hypotonic versus isotonic fluids in hospitalized children: A systematic review and meta-analysis. J Pediatr. 2014;165(1):163-169.e162. doi: 10.1016/j.jpeds.2014.01.040. PubMed
8. McNab S, Ware RS, Neville KA, et al. Isotonic versus hypotonic solutions for maintenance intravenous fluid administration in children. Cochrane Database Syst Rev. 2014;(12):CD009457. doi: 10.1002/14651858.CD009457.pub2. PubMed
9. Arieff AI, Ayus JC, Fraser CL. Hyponatraemia and death or permanent brain damage in healthy children. BMJ. 1992;304(6836):1218-1222. doi: 10.1136/bmj.304.6836.1218. PubMed
10. McNab S, Duke T, South M, et al. 140 mmol/L of sodium versus 77 mmol/L of sodium in maintenance intravenous fluid therapy for children in hospital (PIMS): A randomised controlled double-blind trial. Lancet. 2015;385(9974):1190-1197. doi: 10.1016/S0140-6736(14)61459-8. PubMed
11. Neilson J, O’Neill F, Dawoud D, Crean P, Guideline Development G. Intravenous fluids in children and young people: summary of NICE guidance. BMJ. 2015;351:h6388. doi: 10.1136/bmj.h6388. PubMed
12. Neville KA, Sandeman DJ, Rubinstein A, Henry GM, McGlynn M, Walker JL. Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective randomized study of fluid type versus fluid rate. J Pediatr. 2010;156(2):313-319. doi: 10.1016/j.jpeds.2009.07.059. PubMed
13. Moritz ML, Ayus JC. Preventing neurological complications from dysnatremias in children. Pediatr Nephrol. 2005;20(12):1687-1700. doi: 10.1007/s00467-005-1933-6. PubMed
14. Young P, Bailey M, Beasley R, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: The SPLIT Randomized Clinical Trial. JAMA. 2015;314(16):1701-1710. doi: 10.1001/jama.2015.12334. PubMed
15. Semler MW, Self WH, Wanderer JP, et al. Balanced crystalloids versus salinein critically Ill adults. N Engl J Med. 2018;378(9):829-839. doi: 10.1056/NEJMoa1711584. PubMed
16. Self WH, Semler MW, Wanderer JP, et al. Balanced crystalloids versus saline in noncritically Ill adults. N Engl J Med. 2018;378(9):819-828. doi: 10.1056/NEJMoa1711586. PubMed
17. Mazer-Amirshahi M, Fox ER. Saline shortages - Many causes, no simple solution. N Engl J Med. 2018;378(16):1472-1474. doi: 10.1056/NEJMp1800347. PubMed
1. Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics. 1957;19(5):823-832. PubMed
2. Moritz ML, Ayus JC. Maintenance intravenous fluids in acutely Ill patients. N Engl J Med. 2015;373(14):1350-1360. doi: 10.1056/NEJMra1412877. PubMed
3. Freeman MA, Ayus JC, Moritz ML. Maintenance intravenous fluid prescribing practices among paediatric residents. Acta Paediatr. 2012;101(10):e465-e468. doi: 10.1111/j.1651-2227.2012.02780.x. PubMed
4. Schwartz WB BW, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med. 1957;23(4):529-542. doi: 10.1016/0002-9343(57)90224-3. PubMed
5. Wattad A, Chiang ML, Hill LL. Hyponatremia in hospitalized children. Clin Pediatr. 1992;31(3):153-157. doi: 10.1177/000992289203100305. PubMed
6. Greenberg A, Verbalis JG, Amin AN, et al. Current treatment practice and outcomes. Report of the hyponatremia registry. Kidney Int. 2015;88(1):167-177. doi: 10.1038/ki.2015.4. PubMed
7. Foster BA, Tom D, Hill V. Hypotonic versus isotonic fluids in hospitalized children: A systematic review and meta-analysis. J Pediatr. 2014;165(1):163-169.e162. doi: 10.1016/j.jpeds.2014.01.040. PubMed
8. McNab S, Ware RS, Neville KA, et al. Isotonic versus hypotonic solutions for maintenance intravenous fluid administration in children. Cochrane Database Syst Rev. 2014;(12):CD009457. doi: 10.1002/14651858.CD009457.pub2. PubMed
9. Arieff AI, Ayus JC, Fraser CL. Hyponatraemia and death or permanent brain damage in healthy children. BMJ. 1992;304(6836):1218-1222. doi: 10.1136/bmj.304.6836.1218. PubMed
10. McNab S, Duke T, South M, et al. 140 mmol/L of sodium versus 77 mmol/L of sodium in maintenance intravenous fluid therapy for children in hospital (PIMS): A randomised controlled double-blind trial. Lancet. 2015;385(9974):1190-1197. doi: 10.1016/S0140-6736(14)61459-8. PubMed
11. Neilson J, O’Neill F, Dawoud D, Crean P, Guideline Development G. Intravenous fluids in children and young people: summary of NICE guidance. BMJ. 2015;351:h6388. doi: 10.1136/bmj.h6388. PubMed
12. Neville KA, Sandeman DJ, Rubinstein A, Henry GM, McGlynn M, Walker JL. Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective randomized study of fluid type versus fluid rate. J Pediatr. 2010;156(2):313-319. doi: 10.1016/j.jpeds.2009.07.059. PubMed
13. Moritz ML, Ayus JC. Preventing neurological complications from dysnatremias in children. Pediatr Nephrol. 2005;20(12):1687-1700. doi: 10.1007/s00467-005-1933-6. PubMed
14. Young P, Bailey M, Beasley R, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: The SPLIT Randomized Clinical Trial. JAMA. 2015;314(16):1701-1710. doi: 10.1001/jama.2015.12334. PubMed
15. Semler MW, Self WH, Wanderer JP, et al. Balanced crystalloids versus salinein critically Ill adults. N Engl J Med. 2018;378(9):829-839. doi: 10.1056/NEJMoa1711584. PubMed
16. Self WH, Semler MW, Wanderer JP, et al. Balanced crystalloids versus saline in noncritically Ill adults. N Engl J Med. 2018;378(9):819-828. doi: 10.1056/NEJMoa1711586. PubMed
17. Mazer-Amirshahi M, Fox ER. Saline shortages - Many causes, no simple solution. N Engl J Med. 2018;378(16):1472-1474. doi: 10.1056/NEJMp1800347. PubMed
© 2018 Society of Hospital Medicine