User login
› Refer transgender patients to a mental health provider with experience in treating this patient population for diagnosis of gender dysphoria. B
› Confirm patients’ eligibility for hormone therapy and obtain informed consent before initiating it. B
› Treat minor adverse effects of hormone therapy whenever possible, as discontinuing the hormones may be detrimental to the well-being of patients in the process of transitioning. B
› Continue recommended screenings based on the sex the patient was assigned at birth, unless the organ or tissue in question has been surgically removed. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Civil rights for the lesbian, gay, bisexual, and transgender population have advanced markedly in the past decade, and the medical community has gradually begun to address more of their health concerns. More recently, media attention to transgender individuals—although focused primarily on the “appropriate” use of restrooms—has encouraged many more to openly seek care.1,2
It is estimated that anywhere from 0.3% to 5% of the US population identifies as transgender.1-3 While awareness of this population has slowly increased, there is a paucity of research on the hormone treatment that is often essential to patients’ well-being. Studies of surgical options for transgender patients have been minimal, as well.
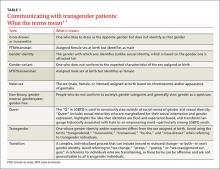
Family physicians are uniquely positioned to coordinate medical services and ensure continuity of care for transgender patients as they strive to become their authentic selves. Our goal in writing this article is to equip you with the tools to provide this patient population with sensitive, high-quality care (TABLE 1).4-7 Our focus is on the diagnosis of gender dysphoria (GD) and its medical and hormonal management—the realm of primary care providers. We briefly discuss surgical management of GD, as well.
Understanding and diagnosing gender dysphoria
Two classification systems are used for diagnoses related to GD: the Diagnostic and Statistical Manual of Mental Disorders, Fifth Ed. (DSM-5)8 and the International Classification of Diseases, 10th Rev. (ICD-10).9
ICD-10 criteria use the term “gender identity disorder;” DSM-5 refers to “gender dysphoria” instead. It is important to emphasize that these classification systems represent an attempt to categorize a group of signs and symptoms that lead to distress for the patient, and are not meant to suggest that being transgender is pathological. In fact, in DSM-5—released in 2013—the American Psychiatric Association revised the terminology to emphasize that such individuals are not “disordered” by the nature of their identity, but rather by the distress that being transgender causes.8
For a diagnosis of GD in children, DSM-5 criteria include characteristics perceived to be incongruent between the child’s sex at birth and the self-identified gender based on preferred activities or dislike of his or her own sexual anatomy. The child must meet 6 or more of the following for at least 6 months:
- a repeatedly stated desire to be, or insistence that he or she is, of the other gender
- in boys, a preference for cross-dressing or simulating female attire; in girls, insistence on wearing only stereotypical masculine clothing
- strong and persistent preferences for cross-gender roles in make-believe play or fantasy
- a strong rejection of toys/games typically associated with the child’s sex
- intense desire to participate in stereotypical games and pastimes of the other gender
- strong preference for playmates of the other gender
- a strong dislike of one’s sexual anatomy
- a strong desire for the primary (eg, penis or vagina) or secondary (eg, menstruation) sex characteristics of the other gender.8
Adolescents and adults must meet 2 or more of the following for at least 6 months:
- a noticeable incongruence between the gender that the patient sees themselves as and their sex characteristics
- an intense need to do away with (or prevent) his or her primary or secondary sex features
- an intense desire to have the primary and/or secondary sex features of the other gender
- a deep desire to transform into another gender
- a profound need for society to treat them as someone of the other gender
- a powerful assurance of having the characteristic feelings and responses of the other gender.8
For children as well as adolescents and adults, the condition should cause the patient significant distress or significantly affect him or her socially, at work or school, and in other important areas of life.8
Is the patient a candidate for hormone therapy?
Two primary sources—Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7, issued by the World Professional Association for Transgender Health (WPATH)10 and Endocrine Treatment of Transsexual Persons11 by the Endocrine Society—offer clinical practice guidance based on evidence and expert opinion.
WPATH recommends that a mental health professional (MHP) experienced in transgender care diagnose GD to ensure that it is not mistaken for a psychiatric condition manifesting as altered gender identity. However, if no one with such experience is available or accessible in the region, it is reasonable for a primary care physician to make the diagnosis and consider initiating hormone therapy without a mental health referral,12 as the expected benefits outweigh the risks of nontreatment.13
Whether or not a MHP confirms a diagnosis of GD, it is still up to the treating physician to confirm the patient’s eligibility and readiness for hormone therapy: He or she should meet DSM-5 or ICD-10 criteria for GD, have no psychiatric comorbidity (eg, schizophrenia, body dysmorphic disorder, or uncontrolled bipolar disorder) likely to interfere with treatment, understand the expected outcomes and the social benefits and risks, and have indicated a willingness to take the hormones responsibly.
Historically, patients were required to have a documented Real-Life Experience (RLE), defined as having fully adopted the new gender role in everyday life for at least 3 months.10,11 This model has fallen out of favor, however, as it is unsupported by evidence and may place transgender individuals at physical and emotional risk.. Instead, readiness is confirmed by obtaining informed consent.12
Puberty may be suppressed with a gonadotropin-releasing hormone (GnRH) agonist in adolescents who have a GD diagnosis and are at Tanner stage 2 to 3 of puberty until age 16. At that point, hormone therapy consistent with their gender identification may be initiated.11 (See “How to help transgender teens.”11,14-20)
How to help transgender teens
Gender exploration is a normal part of childhood. Changes that occur during puberty cause many adolescents to question their ideas of gender and sexuality, but those with persistent gender nonconformity or extreme body dysphoria should receive medical and mental health care as early as possible.
A mental health professional (MHP) can help families create a safe, unconditionally accepting, and supportive environment in which their child can develop into his or her authentic self. A specialist in adolescent gender dysphoria (GD) should be consulted before initiating hormone therapy. Family physicians are well positioned to provide follow-up and ongoing care.
Initiating hormone suppression for adolescents with GD early in puberty can greatly reduce the emotional trauma, as well as the need for surgery related to unwanted secondary sex characteristics. Hormone suppression also gives adolescents more time to explore their gender nonconformity and developmental needs. Treatment with a gonadotropin-releasing hormone agonist such as leuprolide or histrelin can be initiated for adolescents in Tanner Stage 2, assessed by hormone levels, as well as breast, testicle, and pubic hair development (childgrowthfoundation.org/CMS/FILES/Puberty_and_the_Tanner_Stages.pdf), to suppress ongoing puberty.11,14
The effects of puberty blockers are reversible. If preferred, however, medication management can allow teens to progress directly from hormone suppression to the puberty of their self-identified gender once initiation of adult transgender hormone therapy is started—typically around the age of 16.11
Some adolescents may seek medical care well after puberty has begun. It is possible to use hormone suppression therapy after a teen has started to develop unwanted secondary sex characteristics. However, such patients may get less benefit from puberty blockers and often derive more benefit from initiation of cross-gender hormones.
Safety—a broader perspective. Regardless of medical treatment or the age at which treatment is begun, parents and patients need to be reminded that gender transition is about more than hormones. It is crucial that either the MHP or primary care physician, or both, address safety issues and work with the transgender individual to create a comprehensive plan for his or her health, safety, and social well-being.
Psychosocial concerns for transgender youth are vast, often encompassing rejection by peers and potentially, by family and authority figures; harassment; physical, emotional, and sexual abuse; inadequate housing; legal problems; lack of financial support; and educational difficulties.15 School is a particular source of concern. A survey by the Gay, Lesbian and Straight Education Network found, for instance, that nearly 9 in 10 transgender youth had been verbally harassed at school because of their gender expression. More than half also reported being physically harassed (eg, pushed or shoved).15
Bathroom use in schools is a major issue, as well, with transgender youth often prevented from using the restroom or locker room that coincides with their gender identity. In May, 11 states filed a lawsuit against the Obama administration for directing schools to allow such students to do so or risk the loss of federal funds.16
Tools and support. In 2006, the Vancouver Coastal Health, Transcend Transgender Support & Education Society, and the Canadian Rainbow Health Coalition published guidelines for the care of transgender adolescents, including a modification of the HEEADSSS tool (used to assess teens’ psychosocial well-being) specific to transgender youth.17 (See http://www.amsa.org/wp-content/uploads/2015/04/CaringForTransgenderAdolescents.pdf.) The tool can help you identify possible areas of concern and intervene, as needed.
If a patient reports feeling especially vulnerable at school, for example, encourage him or her to identify supportive friends, family members, teachers, or school counselors who can help create safe networks. Suggest that a teen who feels threatened travel in groups whenever possible. Stress to family members that their acceptance is key to nurturing positive feelings in youth with GD. And refer patients and parents to organizations that provide information and support.
Chief among them are Trans Youth Family Allies18 (www.imatyfa.org), which provides resources for parents, educators, and health care practitioners; the Human Rights Campaign, which has created a survival guide for gay and transgender youth who are forced to seek independent living19 (available at hrc-assets.s3-website-us-east-1.amazonaws.com//files/assets/resources/HRC-OnOurOwn-LGBTQYouth.pdf), and the Gay, Lesbian, Bisexual, and Transgender National Help Center, which hosts a GLBT national hotline (888-843-4564) and a weekly Trans Teen Online Talk Group.20 For more information about the online talk group, go to glbthotline.org and click on “transteens.”
Beginning the transition
The transitioning process is a complex and individualized journey that can include inward or outward change, or both.
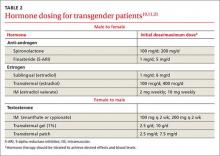
For patients interested in medical interventions, possible therapies include cross-sex hormone administration and gender-affirming surgery. Both are aimed at making the physical and the psychological more congruent. Hormone treatment (TABLE 2)10,11,21 is often essential to reduce the distress of individuals with GD and to help them feel comfortable in their own body. Psychological conditions, such as depression, tend to improve as the transitioning process gets underway.22
Female-to-male transition
CASE 1 ›
Jennie R, a 55-year-old postmenopausal patient, comes to your office for an annual exam. Although you’ve been her primary care physician for several years, she confides for the first time that she has never been comfortable as a woman. “I’ve always felt that my body didn’t belong to me,” the patient admits, and goes on to say that for the last several years she has been living as a man. Jennie R says she is ready to start hormone therapy to assist with the gender transition and asks about the process, the benefits and risks, and how quickly she can expect to achieve the desired results.
If Jennie R were your patient, how would you respond?
Masculinizing hormone treatment
As you would explain to a patient like Jennie R, the goal of hormone therapy is to suppress the effects of the sex assigned at birth and replace them with those of the desired gender. In the case of a female transitioning to a male (known as a transman), masculinizing hormones would promote growth of facial and body hair, cessation of menses, increased muscle mass, deepening of the voice, and clitoral enlargement.11,23,24
Physical changes induced by masculinizing hormone therapy have an expected onset of one to 6 months and achieve maximum effect in approximately 2 to 5 years.10,11 Although there have been no controlled clinical trials evaluating the safety or efficacy of any transitional hormone regimen, WPATH and the Center of Excellence for Transgender Health at the University of California, San Francisco, suggest initiating intramuscular or transdermal testosterone at increasing doses until normal physiologic male testosterone levels between 350 and 700 ng/dL are achieved, or until cessation of menses.13,25-28 The dose at which either, or both, occur should be continued as long-term maintenance therapy. Medroxyprogesterone can be added, if necessary for menstrual cessation, and a GnRH agonist or endometrial ablation can be used for refractory uterine bleeding.29,30
Testosterone is not a contraceptive. It is important to emphasize to transmen like Jennie that they remain at risk of pregnancy if they are having sex with fertile males. Caution patients not to assume that the possibility of pregnancy ends when menses stop.
Treat minor adverse effects. Adverse effects of masculinizing hormones include vaginal atrophy, fat redistribution and weight gain, polycythemia, acne, scalp hair loss, sleep apnea, elevated liver enzymes, hyperlipidemia, cardiovascular disease, diabetes, and bone density loss. Increased risk of cancer of the female organs has not been proven.10,11 It is reasonable to treat minor adverse effects after reviewing the risks vs benefits of doing so, as discontinuing hormone therapy could be detrimental to the well-being of transitioning patients.11
There are absolute contraindications to masculinizing hormone therapy, however, including pregnancy, unstable coronary artery disease, and untreated polycythemia with a hematocrit >55%.10
Monitoring is essential. Patients receiving masculinizing hormone therapy should be monitored every 3 months during the first year and once or twice a year thereafter, with a focused history (including mood symptoms), physical exam (including weight and blood pressure), and labs (including complete blood count, liver function, renal function, and lipids) at each visit.11,23 Some clinicians also check estradiol levels until they fall below 50 pg/mL,23,27 while others take the cessation of uterine bleeding for >6 months as an indicator of estrogen suppression.
Preventive health measures continue. Routine screening should continue, based on the patient’s assigned sex at birth. Thus, a transman who has not had a hysterectomy still needs Pap smears, mammograms if the patient has not had a double mastectomy, and bone mineral density (BMD) testing to screen for osteoporosis.31,32 Some experts recommend starting to test BMD at age 50 for patients receiving masculinizing hormones, given the unknown effect of testosterone on bone density.11,31,32
CASE 1 ›
The first question for a transgender patient is about his or her current gender identity, but Jennie R has already reported living as a man. So you start by asking “What name do you prefer to use?” and “Do you prefer to be referred to with male or female pronouns?”
The patient tells you that he sees himself as a man, he wants to be called Jeff, and he prefers male pronouns. You explain that you believe he has gender dysphoria and would benefit from hormone therapy, but it is important to confirm this diagnosis with a MHP. You explain that testosterone can be prescribed for masculinizing effects, and describe the expected effects—more facial and body hair, a deeper voice and greater muscle mass, among others—and review the likely time frame
You also discuss the risks of masculinizing hormones (hyperlipidemia, cardiovascular disease, diabetes, and loss of bone density) that will need to be monitored. Before he leaves, you give him the name of a MHP who is experienced in transgender care and tell him to make a follow-up appointment with you after he has seen her. At the conclusion of the visit, you make a note of the patient’s name and gender identity in the chart and inform the staff of the changes.
Male-to-female transition
CASE 2 ›
Before heading into your office to talk to a new patient named Carl S, you glance at his chart and see that he is a healthy 21-year-old who has come in for a routine physical. When you enter the room, you find Carl wearing a dress, heels, and make-up. After confirming that you have the right patient, you ask, “What is your current gender identity?” “Female,” says Carl, who indicates that she now goes by Carol. The patient has no medical problems, surgical history, or significant family history, but reports that she has been taking spironolactone and estrogen for the past 3 years. Carol also says she has a new female partner and is having unprotected sexual activity.
Feminizing hormone treatment
The desired effects of feminizing hormones include voice change, decreased hair growth, breast growth, body fat redistribution, decreased muscle mass, skin softening, decreased oiliness of skin and hair, and a decrease in spontaneous erections, testicular volume, and sperm production.10,11 The onset of feminizing effects ranges from one month to one year and the expected maximum effect occurs anywhere between 3 months and 5 years.10,11 Regimens usually include anti-androgen agents and estrogen.13,26-28
The medications that have been most studied with anti-androgenic effects include spironolactone and 5-alpha reductase inhibitors (5-ARIs) such as finasteride. Spironolactone inhibits testosterone secretion and inhibits androgen binding to androgen receptors; 5-ARIs block the conversion of testosterone to 5-alpha-dihydrotestosterone, the more active form.
Estrogen can be administered via oral, sublingual, transdermal, or intramuscular route, but parenteral formulations are preferred to avoid first-pass metabolism. The serum estradiol target is similar to the mean daily level of premenopausal women (<200 pg/mL) and the level of testosterone should be in the normal female range (<55 ng/dL).13,26-28
The selection of medications should be individualized for each patient. Comorbidities must be considered, as well as the risk of adverse effects, which include venous thromboembolism, elevated liver enzymes, breast cancer, cardiovascular disease, diabetes, hyperprolactinemia, weight gain, gallstones, cerebrovascular disease, and severe migraine headaches.10,11 Estrogen therapy is not reported to induce hypertrophy or premalignant changes in the prostate.33 As is the case for masculinizing hormones, feminizing hormone therapy should be continued indefinitely for long-term effects.
Frequent monitoring is recommended. Patients on feminizing hormones (transwomen) should be seen every 2 to 3 months in the first year and monitored once or twice a year thereafter. Serum testosterone and estradiol levels should initially be monitored every 3 months; serum electrolytes, specifically potassium, should be monitored every 2 to 3 months in the first year until stable.
CASE 2 ›
You recommend that Carol S be screened annually for sexually transmitted diseases, as you would for any 21-year-old patient. You point out, too, that while estrogen and androgen-suppressing therapy decrease sperm production, there is a possibility that the patient could impregnate a female partner and recommend that contraception be used if the couple is not trying to conceive.
You also discuss the risks and benefits of hormone therapy and reasonable expectations of continued treatment. You ask Carol to schedule a follow-up visit in 6 months, as her hormone regimen is stable. Finally, if the patient remains on hormone therapy, you mention that the only screening unique to men transitioning to women is for breast cancer, which should begin at 40 to 50 years of age (as it is for all women).
Gender-affirming surgical options
Surgical management of transgender patients is not within the scope of family medicine. But it is essential to know what procedures are available as you may have occasion to advocate for patients during the surgical referral process and possibly to provide postoperative care.
For transmen, surgical options include chest reconstruction, hysterectomy/oophorectomy, metoidioplasty (using the clitoris to surgically approximate a penis), phalloplasty, scrotoplasty, urethroplasty, and vaginectomy.10,34 The surgeries available for transwomen are orchiectomy, vaginoplasty, penectomy, breast augmentation, thyroid chondroplasty and voice surgery, and facial feminization.10,34 Keep in mind that not all transgender individuals desire surgery as part of the transitioning process.
CORRESPONDENCE
Abbas Hyderi, MD, MPH, 1919 West Taylor Street, M/C 663, Chicago, IL 60612; [email protected].
The authors would like to acknowledge the assistance of Michelle Forcier, MD, MPH, and Karen S. Bernstein, MD, MPH, in the preparation of this manuscript.
1. Pew Research Center. A survey of LGBT Americans: attitudes, experiences and values in changing times. Available at: http://www.pewsocialtrends.org/2013/06/13/a-survey-of-lgbt-americans. Accessed June 24, 2015.
2. Gates GJ. How many people are lesbian, gay, bisexual and transgender? Available at: http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf. Accessed May 25, 2016.
3. van Kesteren PJ, Gooren LJ, Megens JA. An epidemiological and demographic study of transsexuals in The Netherlands. Arch Sex Behav. 1996;25:589-600.
4. Bhola S. An ally’s guide to terminology: talking about LGBT people & equality. Available at: http://www.glaad.org/2011/07/28/an-allys-guide-to-terminology-talking-about-lgbt-people-equality. Accessed June 24, 2015.
5. University of California, San Francisco. Transgender terminology. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/tcoe?page=protocol-terminology. Accessed June 24, 2015.
6. Istar A. How queer! the development of gender identity and sexual orientation in LGBTQ-headed families. Fam Process. 2010;49:268-290.
7. Goins ES, Pye D. Check the box that best describes you: reflexively managing theory and praxis in LGBTQ health communication research. Health Commun. 2013;28:397-407.
8. American Psychiatric Association. Gender dysphoria. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association. 2013:451-459.
9. World Health Organization. The International Classification of Diseases, 10th rev. Classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. 1992; Geneva.
10. Coleman E, Bockting W, Botzer M, et al; World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. Int J Transgender. 2011;13:165–232.
11. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine Treatment of transsexual persons: an Endocrine Society Clinical Practice Guideline. J Clin Endo Metabol. 2009;94:3132–3154.
12. University of California, San Francisco. Assessing readiness for hormones. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/tcoe?page=protocol-hormone-ready. Accessed June 24, 2015.
13. Gooren L. Hormone treatment of the adult transsexual patient. Horm Res. 2005;64(suppl 2):S31-S614.
14. Hembree WC. Guidelines for pubertal suspension and gender reassignment for transgender adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20:725-732.
15. Gay, Lesbian, and Straight Education Network (GLSEN). Harsh realities. The experiences of transgender youth in our nation’s schools. Available at: https://www.glsen.org/sites/default/files/Harsh%20Realities.pdf. Accessed May 29, 2016.
16. Berman M, Balingit M. Eleven states sue Obama administration over bathroom guidance for transgender students. May 25, 2016. Washington Post. Available at: https://www.washingtonpost.com/news/post-nation/wp/2016/05/25/texas-governor-says-state-will-sue-obama-administration-over-bathroom-directive/. Accessed May 31, 2016.
17. de Vries AL, Cohen-Kettenis PT, Delemarre-van de Waal H. Clinical management of gender dysphoria in adolescents. 2006. Vancouver Coastal Health - Transgender Health Program. Available at: http://www.amsa.org/wp-content/uploads/2015/04/CaringForTransgenderAdolescents.pdf. Accessed May 26, 2016.
18. TransYouth Family Allies. Empowering transgender youth & families. Available at: http://www.imatyfa.org/. Accessed May 26, 2016.
19. Human Rights Campaign. On our own: a survival guide for independent LGBTQ youth. Available at: https://www.hrc.org/resources/on-our-own-a-survival-guide-for-independent-lgbtq-youth. Accessed May 26, 2016.
20. Gay, Lesbian, Bisexual, and Transgender National Help Center. Available at: www.glbthotline.org. Accessed May 31, 2016.
21. University of California, San Francisco. Hormone administration. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-hormones. Accessed December 12, 2015.
22. Gorin-Lazard A, Baumstarck K, Boyer L, et al. Hormonal therapy is associated with better self-esteem, mood, and quality of life in transsexuals. J Nerv Ment Dis. 2013;201:996-1000.
23. Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in adult men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2006;91:1995-2010.
24. Boloña ER, Uraga MV, Haddad RM, et al. Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc. 2007;82:20-28.
25. Gooren LJ, Giltay EJ. Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of androgens to females. J Sex Med. 2008;5:765-776.
26. Levy A, Crown A, Reid R. Endocrine intervention for transsexuals. Clin Endocrinol (Oxf). 2003;59:409-418.
27. Moore E, Wisniewski A, Dobs A. Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab. 2003;88:3467-3473.
28. Tangpricha V, Ducharme SH, Barber TW, et al. Endocrinologic treatment of gender identity disorders. Endocr Pract. 2003;9:12-21.
29. Dickersin K, Munro MG, Clark M, et al. Hysterectomy compared with endometrial ablation for dysfunctional uterine bleeding: a randomized control trial. Obstet Gynecol. 2007;110:1279-1289.
30. Prasad P, Powell MC. Prospective observational study of thermablate endometrial ablation system as an outpatient procedure. J Minim Invasive Gynecol. 2008;15:476-479.
31. University of California, San Francisco. General prevention and screening. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-screening. Accessed June 24, 2015.
32. Ganly I, Taylor EW. Breast cancer in a trans-sexual man receiving hormone replacement therapy. Br J Surg. 1995;82:341.
33. Meriggiola MC, Gava G. Endocrine care of transpeople part II: a review of cross-sex hormonal treatments, outcomes and adverse effects in transwomen. Clin Endocrinol (Oxf). 2015;83:607-615.
34. University of California, San Francisco. Surgical options. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-surgery. Accessed December 12, 2015.
› Refer transgender patients to a mental health provider with experience in treating this patient population for diagnosis of gender dysphoria. B
› Confirm patients’ eligibility for hormone therapy and obtain informed consent before initiating it. B
› Treat minor adverse effects of hormone therapy whenever possible, as discontinuing the hormones may be detrimental to the well-being of patients in the process of transitioning. B
› Continue recommended screenings based on the sex the patient was assigned at birth, unless the organ or tissue in question has been surgically removed. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Civil rights for the lesbian, gay, bisexual, and transgender population have advanced markedly in the past decade, and the medical community has gradually begun to address more of their health concerns. More recently, media attention to transgender individuals—although focused primarily on the “appropriate” use of restrooms—has encouraged many more to openly seek care.1,2
It is estimated that anywhere from 0.3% to 5% of the US population identifies as transgender.1-3 While awareness of this population has slowly increased, there is a paucity of research on the hormone treatment that is often essential to patients’ well-being. Studies of surgical options for transgender patients have been minimal, as well.
Family physicians are uniquely positioned to coordinate medical services and ensure continuity of care for transgender patients as they strive to become their authentic selves. Our goal in writing this article is to equip you with the tools to provide this patient population with sensitive, high-quality care (TABLE 1).4-7 Our focus is on the diagnosis of gender dysphoria (GD) and its medical and hormonal management—the realm of primary care providers. We briefly discuss surgical management of GD, as well.
Understanding and diagnosing gender dysphoria
Two classification systems are used for diagnoses related to GD: the Diagnostic and Statistical Manual of Mental Disorders, Fifth Ed. (DSM-5)8 and the International Classification of Diseases, 10th Rev. (ICD-10).9
ICD-10 criteria use the term “gender identity disorder;” DSM-5 refers to “gender dysphoria” instead. It is important to emphasize that these classification systems represent an attempt to categorize a group of signs and symptoms that lead to distress for the patient, and are not meant to suggest that being transgender is pathological. In fact, in DSM-5—released in 2013—the American Psychiatric Association revised the terminology to emphasize that such individuals are not “disordered” by the nature of their identity, but rather by the distress that being transgender causes.8
For a diagnosis of GD in children, DSM-5 criteria include characteristics perceived to be incongruent between the child’s sex at birth and the self-identified gender based on preferred activities or dislike of his or her own sexual anatomy. The child must meet 6 or more of the following for at least 6 months:
- a repeatedly stated desire to be, or insistence that he or she is, of the other gender
- in boys, a preference for cross-dressing or simulating female attire; in girls, insistence on wearing only stereotypical masculine clothing
- strong and persistent preferences for cross-gender roles in make-believe play or fantasy
- a strong rejection of toys/games typically associated with the child’s sex
- intense desire to participate in stereotypical games and pastimes of the other gender
- strong preference for playmates of the other gender
- a strong dislike of one’s sexual anatomy
- a strong desire for the primary (eg, penis or vagina) or secondary (eg, menstruation) sex characteristics of the other gender.8
Adolescents and adults must meet 2 or more of the following for at least 6 months:
- a noticeable incongruence between the gender that the patient sees themselves as and their sex characteristics
- an intense need to do away with (or prevent) his or her primary or secondary sex features
- an intense desire to have the primary and/or secondary sex features of the other gender
- a deep desire to transform into another gender
- a profound need for society to treat them as someone of the other gender
- a powerful assurance of having the characteristic feelings and responses of the other gender.8
For children as well as adolescents and adults, the condition should cause the patient significant distress or significantly affect him or her socially, at work or school, and in other important areas of life.8
Is the patient a candidate for hormone therapy?
Two primary sources—Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7, issued by the World Professional Association for Transgender Health (WPATH)10 and Endocrine Treatment of Transsexual Persons11 by the Endocrine Society—offer clinical practice guidance based on evidence and expert opinion.
WPATH recommends that a mental health professional (MHP) experienced in transgender care diagnose GD to ensure that it is not mistaken for a psychiatric condition manifesting as altered gender identity. However, if no one with such experience is available or accessible in the region, it is reasonable for a primary care physician to make the diagnosis and consider initiating hormone therapy without a mental health referral,12 as the expected benefits outweigh the risks of nontreatment.13
Whether or not a MHP confirms a diagnosis of GD, it is still up to the treating physician to confirm the patient’s eligibility and readiness for hormone therapy: He or she should meet DSM-5 or ICD-10 criteria for GD, have no psychiatric comorbidity (eg, schizophrenia, body dysmorphic disorder, or uncontrolled bipolar disorder) likely to interfere with treatment, understand the expected outcomes and the social benefits and risks, and have indicated a willingness to take the hormones responsibly.
Historically, patients were required to have a documented Real-Life Experience (RLE), defined as having fully adopted the new gender role in everyday life for at least 3 months.10,11 This model has fallen out of favor, however, as it is unsupported by evidence and may place transgender individuals at physical and emotional risk.. Instead, readiness is confirmed by obtaining informed consent.12
Puberty may be suppressed with a gonadotropin-releasing hormone (GnRH) agonist in adolescents who have a GD diagnosis and are at Tanner stage 2 to 3 of puberty until age 16. At that point, hormone therapy consistent with their gender identification may be initiated.11 (See “How to help transgender teens.”11,14-20)
How to help transgender teens
Gender exploration is a normal part of childhood. Changes that occur during puberty cause many adolescents to question their ideas of gender and sexuality, but those with persistent gender nonconformity or extreme body dysphoria should receive medical and mental health care as early as possible.
A mental health professional (MHP) can help families create a safe, unconditionally accepting, and supportive environment in which their child can develop into his or her authentic self. A specialist in adolescent gender dysphoria (GD) should be consulted before initiating hormone therapy. Family physicians are well positioned to provide follow-up and ongoing care.
Initiating hormone suppression for adolescents with GD early in puberty can greatly reduce the emotional trauma, as well as the need for surgery related to unwanted secondary sex characteristics. Hormone suppression also gives adolescents more time to explore their gender nonconformity and developmental needs. Treatment with a gonadotropin-releasing hormone agonist such as leuprolide or histrelin can be initiated for adolescents in Tanner Stage 2, assessed by hormone levels, as well as breast, testicle, and pubic hair development (childgrowthfoundation.org/CMS/FILES/Puberty_and_the_Tanner_Stages.pdf), to suppress ongoing puberty.11,14
The effects of puberty blockers are reversible. If preferred, however, medication management can allow teens to progress directly from hormone suppression to the puberty of their self-identified gender once initiation of adult transgender hormone therapy is started—typically around the age of 16.11
Some adolescents may seek medical care well after puberty has begun. It is possible to use hormone suppression therapy after a teen has started to develop unwanted secondary sex characteristics. However, such patients may get less benefit from puberty blockers and often derive more benefit from initiation of cross-gender hormones.
Safety—a broader perspective. Regardless of medical treatment or the age at which treatment is begun, parents and patients need to be reminded that gender transition is about more than hormones. It is crucial that either the MHP or primary care physician, or both, address safety issues and work with the transgender individual to create a comprehensive plan for his or her health, safety, and social well-being.
Psychosocial concerns for transgender youth are vast, often encompassing rejection by peers and potentially, by family and authority figures; harassment; physical, emotional, and sexual abuse; inadequate housing; legal problems; lack of financial support; and educational difficulties.15 School is a particular source of concern. A survey by the Gay, Lesbian and Straight Education Network found, for instance, that nearly 9 in 10 transgender youth had been verbally harassed at school because of their gender expression. More than half also reported being physically harassed (eg, pushed or shoved).15
Bathroom use in schools is a major issue, as well, with transgender youth often prevented from using the restroom or locker room that coincides with their gender identity. In May, 11 states filed a lawsuit against the Obama administration for directing schools to allow such students to do so or risk the loss of federal funds.16
Tools and support. In 2006, the Vancouver Coastal Health, Transcend Transgender Support & Education Society, and the Canadian Rainbow Health Coalition published guidelines for the care of transgender adolescents, including a modification of the HEEADSSS tool (used to assess teens’ psychosocial well-being) specific to transgender youth.17 (See http://www.amsa.org/wp-content/uploads/2015/04/CaringForTransgenderAdolescents.pdf.) The tool can help you identify possible areas of concern and intervene, as needed.
If a patient reports feeling especially vulnerable at school, for example, encourage him or her to identify supportive friends, family members, teachers, or school counselors who can help create safe networks. Suggest that a teen who feels threatened travel in groups whenever possible. Stress to family members that their acceptance is key to nurturing positive feelings in youth with GD. And refer patients and parents to organizations that provide information and support.
Chief among them are Trans Youth Family Allies18 (www.imatyfa.org), which provides resources for parents, educators, and health care practitioners; the Human Rights Campaign, which has created a survival guide for gay and transgender youth who are forced to seek independent living19 (available at hrc-assets.s3-website-us-east-1.amazonaws.com//files/assets/resources/HRC-OnOurOwn-LGBTQYouth.pdf), and the Gay, Lesbian, Bisexual, and Transgender National Help Center, which hosts a GLBT national hotline (888-843-4564) and a weekly Trans Teen Online Talk Group.20 For more information about the online talk group, go to glbthotline.org and click on “transteens.”
Beginning the transition
The transitioning process is a complex and individualized journey that can include inward or outward change, or both.
For patients interested in medical interventions, possible therapies include cross-sex hormone administration and gender-affirming surgery. Both are aimed at making the physical and the psychological more congruent. Hormone treatment (TABLE 2)10,11,21 is often essential to reduce the distress of individuals with GD and to help them feel comfortable in their own body. Psychological conditions, such as depression, tend to improve as the transitioning process gets underway.22
Female-to-male transition
CASE 1 ›
Jennie R, a 55-year-old postmenopausal patient, comes to your office for an annual exam. Although you’ve been her primary care physician for several years, she confides for the first time that she has never been comfortable as a woman. “I’ve always felt that my body didn’t belong to me,” the patient admits, and goes on to say that for the last several years she has been living as a man. Jennie R says she is ready to start hormone therapy to assist with the gender transition and asks about the process, the benefits and risks, and how quickly she can expect to achieve the desired results.
If Jennie R were your patient, how would you respond?
Masculinizing hormone treatment
As you would explain to a patient like Jennie R, the goal of hormone therapy is to suppress the effects of the sex assigned at birth and replace them with those of the desired gender. In the case of a female transitioning to a male (known as a transman), masculinizing hormones would promote growth of facial and body hair, cessation of menses, increased muscle mass, deepening of the voice, and clitoral enlargement.11,23,24
Physical changes induced by masculinizing hormone therapy have an expected onset of one to 6 months and achieve maximum effect in approximately 2 to 5 years.10,11 Although there have been no controlled clinical trials evaluating the safety or efficacy of any transitional hormone regimen, WPATH and the Center of Excellence for Transgender Health at the University of California, San Francisco, suggest initiating intramuscular or transdermal testosterone at increasing doses until normal physiologic male testosterone levels between 350 and 700 ng/dL are achieved, or until cessation of menses.13,25-28 The dose at which either, or both, occur should be continued as long-term maintenance therapy. Medroxyprogesterone can be added, if necessary for menstrual cessation, and a GnRH agonist or endometrial ablation can be used for refractory uterine bleeding.29,30
Testosterone is not a contraceptive. It is important to emphasize to transmen like Jennie that they remain at risk of pregnancy if they are having sex with fertile males. Caution patients not to assume that the possibility of pregnancy ends when menses stop.
Treat minor adverse effects. Adverse effects of masculinizing hormones include vaginal atrophy, fat redistribution and weight gain, polycythemia, acne, scalp hair loss, sleep apnea, elevated liver enzymes, hyperlipidemia, cardiovascular disease, diabetes, and bone density loss. Increased risk of cancer of the female organs has not been proven.10,11 It is reasonable to treat minor adverse effects after reviewing the risks vs benefits of doing so, as discontinuing hormone therapy could be detrimental to the well-being of transitioning patients.11
There are absolute contraindications to masculinizing hormone therapy, however, including pregnancy, unstable coronary artery disease, and untreated polycythemia with a hematocrit >55%.10
Monitoring is essential. Patients receiving masculinizing hormone therapy should be monitored every 3 months during the first year and once or twice a year thereafter, with a focused history (including mood symptoms), physical exam (including weight and blood pressure), and labs (including complete blood count, liver function, renal function, and lipids) at each visit.11,23 Some clinicians also check estradiol levels until they fall below 50 pg/mL,23,27 while others take the cessation of uterine bleeding for >6 months as an indicator of estrogen suppression.
Preventive health measures continue. Routine screening should continue, based on the patient’s assigned sex at birth. Thus, a transman who has not had a hysterectomy still needs Pap smears, mammograms if the patient has not had a double mastectomy, and bone mineral density (BMD) testing to screen for osteoporosis.31,32 Some experts recommend starting to test BMD at age 50 for patients receiving masculinizing hormones, given the unknown effect of testosterone on bone density.11,31,32
CASE 1 ›
The first question for a transgender patient is about his or her current gender identity, but Jennie R has already reported living as a man. So you start by asking “What name do you prefer to use?” and “Do you prefer to be referred to with male or female pronouns?”
The patient tells you that he sees himself as a man, he wants to be called Jeff, and he prefers male pronouns. You explain that you believe he has gender dysphoria and would benefit from hormone therapy, but it is important to confirm this diagnosis with a MHP. You explain that testosterone can be prescribed for masculinizing effects, and describe the expected effects—more facial and body hair, a deeper voice and greater muscle mass, among others—and review the likely time frame
You also discuss the risks of masculinizing hormones (hyperlipidemia, cardiovascular disease, diabetes, and loss of bone density) that will need to be monitored. Before he leaves, you give him the name of a MHP who is experienced in transgender care and tell him to make a follow-up appointment with you after he has seen her. At the conclusion of the visit, you make a note of the patient’s name and gender identity in the chart and inform the staff of the changes.
Male-to-female transition
CASE 2 ›
Before heading into your office to talk to a new patient named Carl S, you glance at his chart and see that he is a healthy 21-year-old who has come in for a routine physical. When you enter the room, you find Carl wearing a dress, heels, and make-up. After confirming that you have the right patient, you ask, “What is your current gender identity?” “Female,” says Carl, who indicates that she now goes by Carol. The patient has no medical problems, surgical history, or significant family history, but reports that she has been taking spironolactone and estrogen for the past 3 years. Carol also says she has a new female partner and is having unprotected sexual activity.
Feminizing hormone treatment
The desired effects of feminizing hormones include voice change, decreased hair growth, breast growth, body fat redistribution, decreased muscle mass, skin softening, decreased oiliness of skin and hair, and a decrease in spontaneous erections, testicular volume, and sperm production.10,11 The onset of feminizing effects ranges from one month to one year and the expected maximum effect occurs anywhere between 3 months and 5 years.10,11 Regimens usually include anti-androgen agents and estrogen.13,26-28
The medications that have been most studied with anti-androgenic effects include spironolactone and 5-alpha reductase inhibitors (5-ARIs) such as finasteride. Spironolactone inhibits testosterone secretion and inhibits androgen binding to androgen receptors; 5-ARIs block the conversion of testosterone to 5-alpha-dihydrotestosterone, the more active form.
Estrogen can be administered via oral, sublingual, transdermal, or intramuscular route, but parenteral formulations are preferred to avoid first-pass metabolism. The serum estradiol target is similar to the mean daily level of premenopausal women (<200 pg/mL) and the level of testosterone should be in the normal female range (<55 ng/dL).13,26-28
The selection of medications should be individualized for each patient. Comorbidities must be considered, as well as the risk of adverse effects, which include venous thromboembolism, elevated liver enzymes, breast cancer, cardiovascular disease, diabetes, hyperprolactinemia, weight gain, gallstones, cerebrovascular disease, and severe migraine headaches.10,11 Estrogen therapy is not reported to induce hypertrophy or premalignant changes in the prostate.33 As is the case for masculinizing hormones, feminizing hormone therapy should be continued indefinitely for long-term effects.
Frequent monitoring is recommended. Patients on feminizing hormones (transwomen) should be seen every 2 to 3 months in the first year and monitored once or twice a year thereafter. Serum testosterone and estradiol levels should initially be monitored every 3 months; serum electrolytes, specifically potassium, should be monitored every 2 to 3 months in the first year until stable.
CASE 2 ›
You recommend that Carol S be screened annually for sexually transmitted diseases, as you would for any 21-year-old patient. You point out, too, that while estrogen and androgen-suppressing therapy decrease sperm production, there is a possibility that the patient could impregnate a female partner and recommend that contraception be used if the couple is not trying to conceive.
You also discuss the risks and benefits of hormone therapy and reasonable expectations of continued treatment. You ask Carol to schedule a follow-up visit in 6 months, as her hormone regimen is stable. Finally, if the patient remains on hormone therapy, you mention that the only screening unique to men transitioning to women is for breast cancer, which should begin at 40 to 50 years of age (as it is for all women).
Gender-affirming surgical options
Surgical management of transgender patients is not within the scope of family medicine. But it is essential to know what procedures are available as you may have occasion to advocate for patients during the surgical referral process and possibly to provide postoperative care.
For transmen, surgical options include chest reconstruction, hysterectomy/oophorectomy, metoidioplasty (using the clitoris to surgically approximate a penis), phalloplasty, scrotoplasty, urethroplasty, and vaginectomy.10,34 The surgeries available for transwomen are orchiectomy, vaginoplasty, penectomy, breast augmentation, thyroid chondroplasty and voice surgery, and facial feminization.10,34 Keep in mind that not all transgender individuals desire surgery as part of the transitioning process.
CORRESPONDENCE
Abbas Hyderi, MD, MPH, 1919 West Taylor Street, M/C 663, Chicago, IL 60612; [email protected].
The authors would like to acknowledge the assistance of Michelle Forcier, MD, MPH, and Karen S. Bernstein, MD, MPH, in the preparation of this manuscript.
› Refer transgender patients to a mental health provider with experience in treating this patient population for diagnosis of gender dysphoria. B
› Confirm patients’ eligibility for hormone therapy and obtain informed consent before initiating it. B
› Treat minor adverse effects of hormone therapy whenever possible, as discontinuing the hormones may be detrimental to the well-being of patients in the process of transitioning. B
› Continue recommended screenings based on the sex the patient was assigned at birth, unless the organ or tissue in question has been surgically removed. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Civil rights for the lesbian, gay, bisexual, and transgender population have advanced markedly in the past decade, and the medical community has gradually begun to address more of their health concerns. More recently, media attention to transgender individuals—although focused primarily on the “appropriate” use of restrooms—has encouraged many more to openly seek care.1,2
It is estimated that anywhere from 0.3% to 5% of the US population identifies as transgender.1-3 While awareness of this population has slowly increased, there is a paucity of research on the hormone treatment that is often essential to patients’ well-being. Studies of surgical options for transgender patients have been minimal, as well.
Family physicians are uniquely positioned to coordinate medical services and ensure continuity of care for transgender patients as they strive to become their authentic selves. Our goal in writing this article is to equip you with the tools to provide this patient population with sensitive, high-quality care (TABLE 1).4-7 Our focus is on the diagnosis of gender dysphoria (GD) and its medical and hormonal management—the realm of primary care providers. We briefly discuss surgical management of GD, as well.
Understanding and diagnosing gender dysphoria
Two classification systems are used for diagnoses related to GD: the Diagnostic and Statistical Manual of Mental Disorders, Fifth Ed. (DSM-5)8 and the International Classification of Diseases, 10th Rev. (ICD-10).9
ICD-10 criteria use the term “gender identity disorder;” DSM-5 refers to “gender dysphoria” instead. It is important to emphasize that these classification systems represent an attempt to categorize a group of signs and symptoms that lead to distress for the patient, and are not meant to suggest that being transgender is pathological. In fact, in DSM-5—released in 2013—the American Psychiatric Association revised the terminology to emphasize that such individuals are not “disordered” by the nature of their identity, but rather by the distress that being transgender causes.8
For a diagnosis of GD in children, DSM-5 criteria include characteristics perceived to be incongruent between the child’s sex at birth and the self-identified gender based on preferred activities or dislike of his or her own sexual anatomy. The child must meet 6 or more of the following for at least 6 months:
- a repeatedly stated desire to be, or insistence that he or she is, of the other gender
- in boys, a preference for cross-dressing or simulating female attire; in girls, insistence on wearing only stereotypical masculine clothing
- strong and persistent preferences for cross-gender roles in make-believe play or fantasy
- a strong rejection of toys/games typically associated with the child’s sex
- intense desire to participate in stereotypical games and pastimes of the other gender
- strong preference for playmates of the other gender
- a strong dislike of one’s sexual anatomy
- a strong desire for the primary (eg, penis or vagina) or secondary (eg, menstruation) sex characteristics of the other gender.8
Adolescents and adults must meet 2 or more of the following for at least 6 months:
- a noticeable incongruence between the gender that the patient sees themselves as and their sex characteristics
- an intense need to do away with (or prevent) his or her primary or secondary sex features
- an intense desire to have the primary and/or secondary sex features of the other gender
- a deep desire to transform into another gender
- a profound need for society to treat them as someone of the other gender
- a powerful assurance of having the characteristic feelings and responses of the other gender.8
For children as well as adolescents and adults, the condition should cause the patient significant distress or significantly affect him or her socially, at work or school, and in other important areas of life.8
Is the patient a candidate for hormone therapy?
Two primary sources—Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7, issued by the World Professional Association for Transgender Health (WPATH)10 and Endocrine Treatment of Transsexual Persons11 by the Endocrine Society—offer clinical practice guidance based on evidence and expert opinion.
WPATH recommends that a mental health professional (MHP) experienced in transgender care diagnose GD to ensure that it is not mistaken for a psychiatric condition manifesting as altered gender identity. However, if no one with such experience is available or accessible in the region, it is reasonable for a primary care physician to make the diagnosis and consider initiating hormone therapy without a mental health referral,12 as the expected benefits outweigh the risks of nontreatment.13
Whether or not a MHP confirms a diagnosis of GD, it is still up to the treating physician to confirm the patient’s eligibility and readiness for hormone therapy: He or she should meet DSM-5 or ICD-10 criteria for GD, have no psychiatric comorbidity (eg, schizophrenia, body dysmorphic disorder, or uncontrolled bipolar disorder) likely to interfere with treatment, understand the expected outcomes and the social benefits and risks, and have indicated a willingness to take the hormones responsibly.
Historically, patients were required to have a documented Real-Life Experience (RLE), defined as having fully adopted the new gender role in everyday life for at least 3 months.10,11 This model has fallen out of favor, however, as it is unsupported by evidence and may place transgender individuals at physical and emotional risk.. Instead, readiness is confirmed by obtaining informed consent.12
Puberty may be suppressed with a gonadotropin-releasing hormone (GnRH) agonist in adolescents who have a GD diagnosis and are at Tanner stage 2 to 3 of puberty until age 16. At that point, hormone therapy consistent with their gender identification may be initiated.11 (See “How to help transgender teens.”11,14-20)
How to help transgender teens
Gender exploration is a normal part of childhood. Changes that occur during puberty cause many adolescents to question their ideas of gender and sexuality, but those with persistent gender nonconformity or extreme body dysphoria should receive medical and mental health care as early as possible.
A mental health professional (MHP) can help families create a safe, unconditionally accepting, and supportive environment in which their child can develop into his or her authentic self. A specialist in adolescent gender dysphoria (GD) should be consulted before initiating hormone therapy. Family physicians are well positioned to provide follow-up and ongoing care.
Initiating hormone suppression for adolescents with GD early in puberty can greatly reduce the emotional trauma, as well as the need for surgery related to unwanted secondary sex characteristics. Hormone suppression also gives adolescents more time to explore their gender nonconformity and developmental needs. Treatment with a gonadotropin-releasing hormone agonist such as leuprolide or histrelin can be initiated for adolescents in Tanner Stage 2, assessed by hormone levels, as well as breast, testicle, and pubic hair development (childgrowthfoundation.org/CMS/FILES/Puberty_and_the_Tanner_Stages.pdf), to suppress ongoing puberty.11,14
The effects of puberty blockers are reversible. If preferred, however, medication management can allow teens to progress directly from hormone suppression to the puberty of their self-identified gender once initiation of adult transgender hormone therapy is started—typically around the age of 16.11
Some adolescents may seek medical care well after puberty has begun. It is possible to use hormone suppression therapy after a teen has started to develop unwanted secondary sex characteristics. However, such patients may get less benefit from puberty blockers and often derive more benefit from initiation of cross-gender hormones.
Safety—a broader perspective. Regardless of medical treatment or the age at which treatment is begun, parents and patients need to be reminded that gender transition is about more than hormones. It is crucial that either the MHP or primary care physician, or both, address safety issues and work with the transgender individual to create a comprehensive plan for his or her health, safety, and social well-being.
Psychosocial concerns for transgender youth are vast, often encompassing rejection by peers and potentially, by family and authority figures; harassment; physical, emotional, and sexual abuse; inadequate housing; legal problems; lack of financial support; and educational difficulties.15 School is a particular source of concern. A survey by the Gay, Lesbian and Straight Education Network found, for instance, that nearly 9 in 10 transgender youth had been verbally harassed at school because of their gender expression. More than half also reported being physically harassed (eg, pushed or shoved).15
Bathroom use in schools is a major issue, as well, with transgender youth often prevented from using the restroom or locker room that coincides with their gender identity. In May, 11 states filed a lawsuit against the Obama administration for directing schools to allow such students to do so or risk the loss of federal funds.16
Tools and support. In 2006, the Vancouver Coastal Health, Transcend Transgender Support & Education Society, and the Canadian Rainbow Health Coalition published guidelines for the care of transgender adolescents, including a modification of the HEEADSSS tool (used to assess teens’ psychosocial well-being) specific to transgender youth.17 (See http://www.amsa.org/wp-content/uploads/2015/04/CaringForTransgenderAdolescents.pdf.) The tool can help you identify possible areas of concern and intervene, as needed.
If a patient reports feeling especially vulnerable at school, for example, encourage him or her to identify supportive friends, family members, teachers, or school counselors who can help create safe networks. Suggest that a teen who feels threatened travel in groups whenever possible. Stress to family members that their acceptance is key to nurturing positive feelings in youth with GD. And refer patients and parents to organizations that provide information and support.
Chief among them are Trans Youth Family Allies18 (www.imatyfa.org), which provides resources for parents, educators, and health care practitioners; the Human Rights Campaign, which has created a survival guide for gay and transgender youth who are forced to seek independent living19 (available at hrc-assets.s3-website-us-east-1.amazonaws.com//files/assets/resources/HRC-OnOurOwn-LGBTQYouth.pdf), and the Gay, Lesbian, Bisexual, and Transgender National Help Center, which hosts a GLBT national hotline (888-843-4564) and a weekly Trans Teen Online Talk Group.20 For more information about the online talk group, go to glbthotline.org and click on “transteens.”
Beginning the transition
The transitioning process is a complex and individualized journey that can include inward or outward change, or both.
For patients interested in medical interventions, possible therapies include cross-sex hormone administration and gender-affirming surgery. Both are aimed at making the physical and the psychological more congruent. Hormone treatment (TABLE 2)10,11,21 is often essential to reduce the distress of individuals with GD and to help them feel comfortable in their own body. Psychological conditions, such as depression, tend to improve as the transitioning process gets underway.22
Female-to-male transition
CASE 1 ›
Jennie R, a 55-year-old postmenopausal patient, comes to your office for an annual exam. Although you’ve been her primary care physician for several years, she confides for the first time that she has never been comfortable as a woman. “I’ve always felt that my body didn’t belong to me,” the patient admits, and goes on to say that for the last several years she has been living as a man. Jennie R says she is ready to start hormone therapy to assist with the gender transition and asks about the process, the benefits and risks, and how quickly she can expect to achieve the desired results.
If Jennie R were your patient, how would you respond?
Masculinizing hormone treatment
As you would explain to a patient like Jennie R, the goal of hormone therapy is to suppress the effects of the sex assigned at birth and replace them with those of the desired gender. In the case of a female transitioning to a male (known as a transman), masculinizing hormones would promote growth of facial and body hair, cessation of menses, increased muscle mass, deepening of the voice, and clitoral enlargement.11,23,24
Physical changes induced by masculinizing hormone therapy have an expected onset of one to 6 months and achieve maximum effect in approximately 2 to 5 years.10,11 Although there have been no controlled clinical trials evaluating the safety or efficacy of any transitional hormone regimen, WPATH and the Center of Excellence for Transgender Health at the University of California, San Francisco, suggest initiating intramuscular or transdermal testosterone at increasing doses until normal physiologic male testosterone levels between 350 and 700 ng/dL are achieved, or until cessation of menses.13,25-28 The dose at which either, or both, occur should be continued as long-term maintenance therapy. Medroxyprogesterone can be added, if necessary for menstrual cessation, and a GnRH agonist or endometrial ablation can be used for refractory uterine bleeding.29,30
Testosterone is not a contraceptive. It is important to emphasize to transmen like Jennie that they remain at risk of pregnancy if they are having sex with fertile males. Caution patients not to assume that the possibility of pregnancy ends when menses stop.
Treat minor adverse effects. Adverse effects of masculinizing hormones include vaginal atrophy, fat redistribution and weight gain, polycythemia, acne, scalp hair loss, sleep apnea, elevated liver enzymes, hyperlipidemia, cardiovascular disease, diabetes, and bone density loss. Increased risk of cancer of the female organs has not been proven.10,11 It is reasonable to treat minor adverse effects after reviewing the risks vs benefits of doing so, as discontinuing hormone therapy could be detrimental to the well-being of transitioning patients.11
There are absolute contraindications to masculinizing hormone therapy, however, including pregnancy, unstable coronary artery disease, and untreated polycythemia with a hematocrit >55%.10
Monitoring is essential. Patients receiving masculinizing hormone therapy should be monitored every 3 months during the first year and once or twice a year thereafter, with a focused history (including mood symptoms), physical exam (including weight and blood pressure), and labs (including complete blood count, liver function, renal function, and lipids) at each visit.11,23 Some clinicians also check estradiol levels until they fall below 50 pg/mL,23,27 while others take the cessation of uterine bleeding for >6 months as an indicator of estrogen suppression.
Preventive health measures continue. Routine screening should continue, based on the patient’s assigned sex at birth. Thus, a transman who has not had a hysterectomy still needs Pap smears, mammograms if the patient has not had a double mastectomy, and bone mineral density (BMD) testing to screen for osteoporosis.31,32 Some experts recommend starting to test BMD at age 50 for patients receiving masculinizing hormones, given the unknown effect of testosterone on bone density.11,31,32
CASE 1 ›
The first question for a transgender patient is about his or her current gender identity, but Jennie R has already reported living as a man. So you start by asking “What name do you prefer to use?” and “Do you prefer to be referred to with male or female pronouns?”
The patient tells you that he sees himself as a man, he wants to be called Jeff, and he prefers male pronouns. You explain that you believe he has gender dysphoria and would benefit from hormone therapy, but it is important to confirm this diagnosis with a MHP. You explain that testosterone can be prescribed for masculinizing effects, and describe the expected effects—more facial and body hair, a deeper voice and greater muscle mass, among others—and review the likely time frame
You also discuss the risks of masculinizing hormones (hyperlipidemia, cardiovascular disease, diabetes, and loss of bone density) that will need to be monitored. Before he leaves, you give him the name of a MHP who is experienced in transgender care and tell him to make a follow-up appointment with you after he has seen her. At the conclusion of the visit, you make a note of the patient’s name and gender identity in the chart and inform the staff of the changes.
Male-to-female transition
CASE 2 ›
Before heading into your office to talk to a new patient named Carl S, you glance at his chart and see that he is a healthy 21-year-old who has come in for a routine physical. When you enter the room, you find Carl wearing a dress, heels, and make-up. After confirming that you have the right patient, you ask, “What is your current gender identity?” “Female,” says Carl, who indicates that she now goes by Carol. The patient has no medical problems, surgical history, or significant family history, but reports that she has been taking spironolactone and estrogen for the past 3 years. Carol also says she has a new female partner and is having unprotected sexual activity.
Feminizing hormone treatment
The desired effects of feminizing hormones include voice change, decreased hair growth, breast growth, body fat redistribution, decreased muscle mass, skin softening, decreased oiliness of skin and hair, and a decrease in spontaneous erections, testicular volume, and sperm production.10,11 The onset of feminizing effects ranges from one month to one year and the expected maximum effect occurs anywhere between 3 months and 5 years.10,11 Regimens usually include anti-androgen agents and estrogen.13,26-28
The medications that have been most studied with anti-androgenic effects include spironolactone and 5-alpha reductase inhibitors (5-ARIs) such as finasteride. Spironolactone inhibits testosterone secretion and inhibits androgen binding to androgen receptors; 5-ARIs block the conversion of testosterone to 5-alpha-dihydrotestosterone, the more active form.
Estrogen can be administered via oral, sublingual, transdermal, or intramuscular route, but parenteral formulations are preferred to avoid first-pass metabolism. The serum estradiol target is similar to the mean daily level of premenopausal women (<200 pg/mL) and the level of testosterone should be in the normal female range (<55 ng/dL).13,26-28
The selection of medications should be individualized for each patient. Comorbidities must be considered, as well as the risk of adverse effects, which include venous thromboembolism, elevated liver enzymes, breast cancer, cardiovascular disease, diabetes, hyperprolactinemia, weight gain, gallstones, cerebrovascular disease, and severe migraine headaches.10,11 Estrogen therapy is not reported to induce hypertrophy or premalignant changes in the prostate.33 As is the case for masculinizing hormones, feminizing hormone therapy should be continued indefinitely for long-term effects.
Frequent monitoring is recommended. Patients on feminizing hormones (transwomen) should be seen every 2 to 3 months in the first year and monitored once or twice a year thereafter. Serum testosterone and estradiol levels should initially be monitored every 3 months; serum electrolytes, specifically potassium, should be monitored every 2 to 3 months in the first year until stable.
CASE 2 ›
You recommend that Carol S be screened annually for sexually transmitted diseases, as you would for any 21-year-old patient. You point out, too, that while estrogen and androgen-suppressing therapy decrease sperm production, there is a possibility that the patient could impregnate a female partner and recommend that contraception be used if the couple is not trying to conceive.
You also discuss the risks and benefits of hormone therapy and reasonable expectations of continued treatment. You ask Carol to schedule a follow-up visit in 6 months, as her hormone regimen is stable. Finally, if the patient remains on hormone therapy, you mention that the only screening unique to men transitioning to women is for breast cancer, which should begin at 40 to 50 years of age (as it is for all women).
Gender-affirming surgical options
Surgical management of transgender patients is not within the scope of family medicine. But it is essential to know what procedures are available as you may have occasion to advocate for patients during the surgical referral process and possibly to provide postoperative care.
For transmen, surgical options include chest reconstruction, hysterectomy/oophorectomy, metoidioplasty (using the clitoris to surgically approximate a penis), phalloplasty, scrotoplasty, urethroplasty, and vaginectomy.10,34 The surgeries available for transwomen are orchiectomy, vaginoplasty, penectomy, breast augmentation, thyroid chondroplasty and voice surgery, and facial feminization.10,34 Keep in mind that not all transgender individuals desire surgery as part of the transitioning process.
CORRESPONDENCE
Abbas Hyderi, MD, MPH, 1919 West Taylor Street, M/C 663, Chicago, IL 60612; [email protected].
The authors would like to acknowledge the assistance of Michelle Forcier, MD, MPH, and Karen S. Bernstein, MD, MPH, in the preparation of this manuscript.
1. Pew Research Center. A survey of LGBT Americans: attitudes, experiences and values in changing times. Available at: http://www.pewsocialtrends.org/2013/06/13/a-survey-of-lgbt-americans. Accessed June 24, 2015.
2. Gates GJ. How many people are lesbian, gay, bisexual and transgender? Available at: http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf. Accessed May 25, 2016.
3. van Kesteren PJ, Gooren LJ, Megens JA. An epidemiological and demographic study of transsexuals in The Netherlands. Arch Sex Behav. 1996;25:589-600.
4. Bhola S. An ally’s guide to terminology: talking about LGBT people & equality. Available at: http://www.glaad.org/2011/07/28/an-allys-guide-to-terminology-talking-about-lgbt-people-equality. Accessed June 24, 2015.
5. University of California, San Francisco. Transgender terminology. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/tcoe?page=protocol-terminology. Accessed June 24, 2015.
6. Istar A. How queer! the development of gender identity and sexual orientation in LGBTQ-headed families. Fam Process. 2010;49:268-290.
7. Goins ES, Pye D. Check the box that best describes you: reflexively managing theory and praxis in LGBTQ health communication research. Health Commun. 2013;28:397-407.
8. American Psychiatric Association. Gender dysphoria. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association. 2013:451-459.
9. World Health Organization. The International Classification of Diseases, 10th rev. Classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. 1992; Geneva.
10. Coleman E, Bockting W, Botzer M, et al; World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. Int J Transgender. 2011;13:165–232.
11. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine Treatment of transsexual persons: an Endocrine Society Clinical Practice Guideline. J Clin Endo Metabol. 2009;94:3132–3154.
12. University of California, San Francisco. Assessing readiness for hormones. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/tcoe?page=protocol-hormone-ready. Accessed June 24, 2015.
13. Gooren L. Hormone treatment of the adult transsexual patient. Horm Res. 2005;64(suppl 2):S31-S614.
14. Hembree WC. Guidelines for pubertal suspension and gender reassignment for transgender adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20:725-732.
15. Gay, Lesbian, and Straight Education Network (GLSEN). Harsh realities. The experiences of transgender youth in our nation’s schools. Available at: https://www.glsen.org/sites/default/files/Harsh%20Realities.pdf. Accessed May 29, 2016.
16. Berman M, Balingit M. Eleven states sue Obama administration over bathroom guidance for transgender students. May 25, 2016. Washington Post. Available at: https://www.washingtonpost.com/news/post-nation/wp/2016/05/25/texas-governor-says-state-will-sue-obama-administration-over-bathroom-directive/. Accessed May 31, 2016.
17. de Vries AL, Cohen-Kettenis PT, Delemarre-van de Waal H. Clinical management of gender dysphoria in adolescents. 2006. Vancouver Coastal Health - Transgender Health Program. Available at: http://www.amsa.org/wp-content/uploads/2015/04/CaringForTransgenderAdolescents.pdf. Accessed May 26, 2016.
18. TransYouth Family Allies. Empowering transgender youth & families. Available at: http://www.imatyfa.org/. Accessed May 26, 2016.
19. Human Rights Campaign. On our own: a survival guide for independent LGBTQ youth. Available at: https://www.hrc.org/resources/on-our-own-a-survival-guide-for-independent-lgbtq-youth. Accessed May 26, 2016.
20. Gay, Lesbian, Bisexual, and Transgender National Help Center. Available at: www.glbthotline.org. Accessed May 31, 2016.
21. University of California, San Francisco. Hormone administration. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-hormones. Accessed December 12, 2015.
22. Gorin-Lazard A, Baumstarck K, Boyer L, et al. Hormonal therapy is associated with better self-esteem, mood, and quality of life in transsexuals. J Nerv Ment Dis. 2013;201:996-1000.
23. Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in adult men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2006;91:1995-2010.
24. Boloña ER, Uraga MV, Haddad RM, et al. Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc. 2007;82:20-28.
25. Gooren LJ, Giltay EJ. Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of androgens to females. J Sex Med. 2008;5:765-776.
26. Levy A, Crown A, Reid R. Endocrine intervention for transsexuals. Clin Endocrinol (Oxf). 2003;59:409-418.
27. Moore E, Wisniewski A, Dobs A. Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab. 2003;88:3467-3473.
28. Tangpricha V, Ducharme SH, Barber TW, et al. Endocrinologic treatment of gender identity disorders. Endocr Pract. 2003;9:12-21.
29. Dickersin K, Munro MG, Clark M, et al. Hysterectomy compared with endometrial ablation for dysfunctional uterine bleeding: a randomized control trial. Obstet Gynecol. 2007;110:1279-1289.
30. Prasad P, Powell MC. Prospective observational study of thermablate endometrial ablation system as an outpatient procedure. J Minim Invasive Gynecol. 2008;15:476-479.
31. University of California, San Francisco. General prevention and screening. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-screening. Accessed June 24, 2015.
32. Ganly I, Taylor EW. Breast cancer in a trans-sexual man receiving hormone replacement therapy. Br J Surg. 1995;82:341.
33. Meriggiola MC, Gava G. Endocrine care of transpeople part II: a review of cross-sex hormonal treatments, outcomes and adverse effects in transwomen. Clin Endocrinol (Oxf). 2015;83:607-615.
34. University of California, San Francisco. Surgical options. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-surgery. Accessed December 12, 2015.
1. Pew Research Center. A survey of LGBT Americans: attitudes, experiences and values in changing times. Available at: http://www.pewsocialtrends.org/2013/06/13/a-survey-of-lgbt-americans. Accessed June 24, 2015.
2. Gates GJ. How many people are lesbian, gay, bisexual and transgender? Available at: http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf. Accessed May 25, 2016.
3. van Kesteren PJ, Gooren LJ, Megens JA. An epidemiological and demographic study of transsexuals in The Netherlands. Arch Sex Behav. 1996;25:589-600.
4. Bhola S. An ally’s guide to terminology: talking about LGBT people & equality. Available at: http://www.glaad.org/2011/07/28/an-allys-guide-to-terminology-talking-about-lgbt-people-equality. Accessed June 24, 2015.
5. University of California, San Francisco. Transgender terminology. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/tcoe?page=protocol-terminology. Accessed June 24, 2015.
6. Istar A. How queer! the development of gender identity and sexual orientation in LGBTQ-headed families. Fam Process. 2010;49:268-290.
7. Goins ES, Pye D. Check the box that best describes you: reflexively managing theory and praxis in LGBTQ health communication research. Health Commun. 2013;28:397-407.
8. American Psychiatric Association. Gender dysphoria. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association. 2013:451-459.
9. World Health Organization. The International Classification of Diseases, 10th rev. Classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. 1992; Geneva.
10. Coleman E, Bockting W, Botzer M, et al; World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. Int J Transgender. 2011;13:165–232.
11. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine Treatment of transsexual persons: an Endocrine Society Clinical Practice Guideline. J Clin Endo Metabol. 2009;94:3132–3154.
12. University of California, San Francisco. Assessing readiness for hormones. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/tcoe?page=protocol-hormone-ready. Accessed June 24, 2015.
13. Gooren L. Hormone treatment of the adult transsexual patient. Horm Res. 2005;64(suppl 2):S31-S614.
14. Hembree WC. Guidelines for pubertal suspension and gender reassignment for transgender adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20:725-732.
15. Gay, Lesbian, and Straight Education Network (GLSEN). Harsh realities. The experiences of transgender youth in our nation’s schools. Available at: https://www.glsen.org/sites/default/files/Harsh%20Realities.pdf. Accessed May 29, 2016.
16. Berman M, Balingit M. Eleven states sue Obama administration over bathroom guidance for transgender students. May 25, 2016. Washington Post. Available at: https://www.washingtonpost.com/news/post-nation/wp/2016/05/25/texas-governor-says-state-will-sue-obama-administration-over-bathroom-directive/. Accessed May 31, 2016.
17. de Vries AL, Cohen-Kettenis PT, Delemarre-van de Waal H. Clinical management of gender dysphoria in adolescents. 2006. Vancouver Coastal Health - Transgender Health Program. Available at: http://www.amsa.org/wp-content/uploads/2015/04/CaringForTransgenderAdolescents.pdf. Accessed May 26, 2016.
18. TransYouth Family Allies. Empowering transgender youth & families. Available at: http://www.imatyfa.org/. Accessed May 26, 2016.
19. Human Rights Campaign. On our own: a survival guide for independent LGBTQ youth. Available at: https://www.hrc.org/resources/on-our-own-a-survival-guide-for-independent-lgbtq-youth. Accessed May 26, 2016.
20. Gay, Lesbian, Bisexual, and Transgender National Help Center. Available at: www.glbthotline.org. Accessed May 31, 2016.
21. University of California, San Francisco. Hormone administration. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-hormones. Accessed December 12, 2015.
22. Gorin-Lazard A, Baumstarck K, Boyer L, et al. Hormonal therapy is associated with better self-esteem, mood, and quality of life in transsexuals. J Nerv Ment Dis. 2013;201:996-1000.
23. Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in adult men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2006;91:1995-2010.
24. Boloña ER, Uraga MV, Haddad RM, et al. Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc. 2007;82:20-28.
25. Gooren LJ, Giltay EJ. Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of androgens to females. J Sex Med. 2008;5:765-776.
26. Levy A, Crown A, Reid R. Endocrine intervention for transsexuals. Clin Endocrinol (Oxf). 2003;59:409-418.
27. Moore E, Wisniewski A, Dobs A. Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab. 2003;88:3467-3473.
28. Tangpricha V, Ducharme SH, Barber TW, et al. Endocrinologic treatment of gender identity disorders. Endocr Pract. 2003;9:12-21.
29. Dickersin K, Munro MG, Clark M, et al. Hysterectomy compared with endometrial ablation for dysfunctional uterine bleeding: a randomized control trial. Obstet Gynecol. 2007;110:1279-1289.
30. Prasad P, Powell MC. Prospective observational study of thermablate endometrial ablation system as an outpatient procedure. J Minim Invasive Gynecol. 2008;15:476-479.
31. University of California, San Francisco. General prevention and screening. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-screening. Accessed June 24, 2015.
32. Ganly I, Taylor EW. Breast cancer in a trans-sexual man receiving hormone replacement therapy. Br J Surg. 1995;82:341.
33. Meriggiola MC, Gava G. Endocrine care of transpeople part II: a review of cross-sex hormonal treatments, outcomes and adverse effects in transwomen. Clin Endocrinol (Oxf). 2015;83:607-615.
34. University of California, San Francisco. Surgical options. UCSF Center of Excellence for Transgender Health. Available at: http://transhealth.ucsf.edu/trans?page=protocol-surgery. Accessed December 12, 2015.