User login
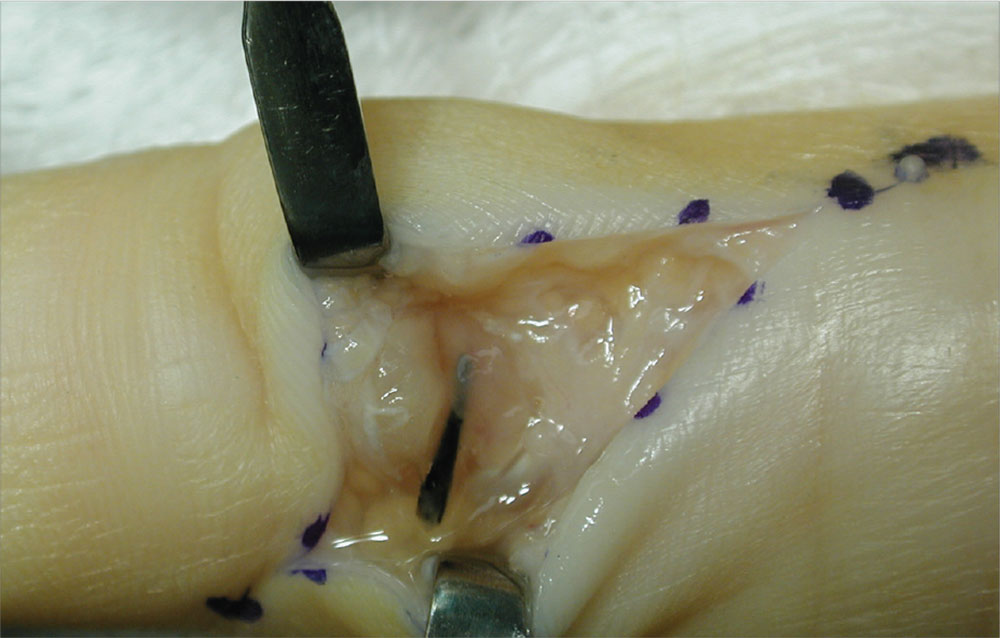
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
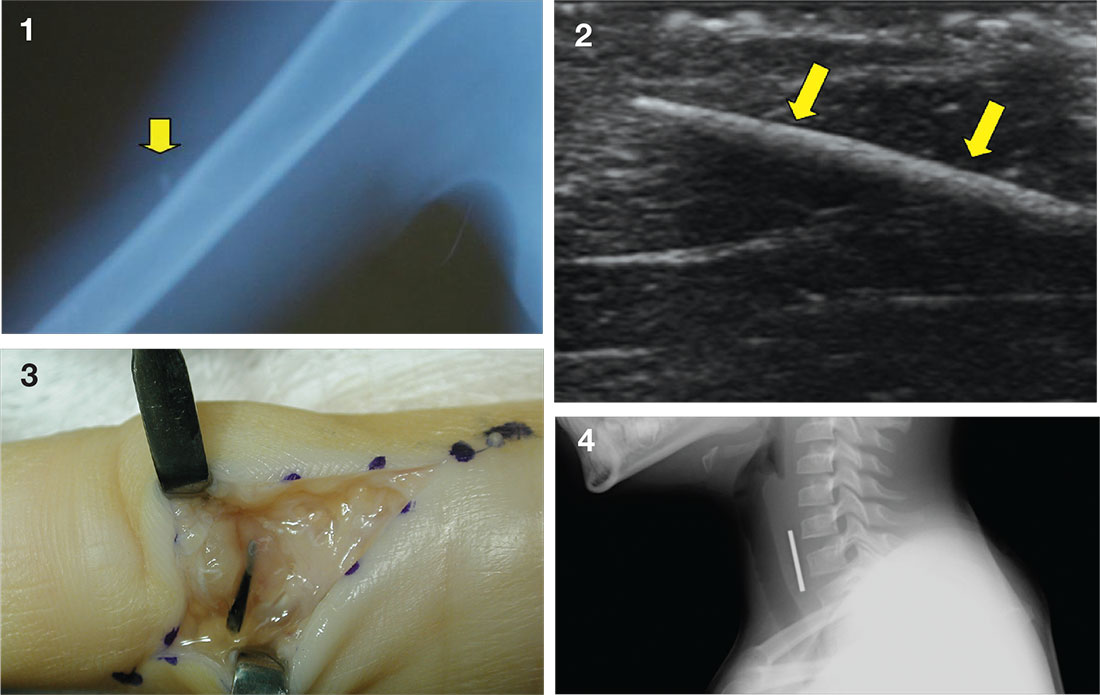
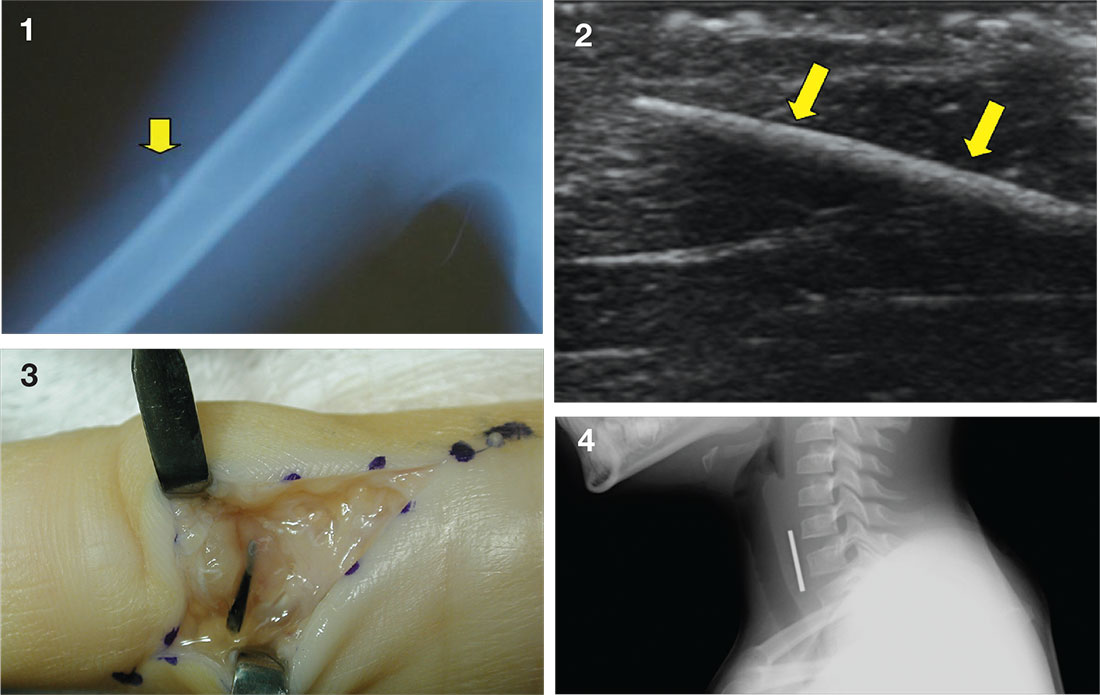
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Complete obstruction should be treated with back blows in a child aged less than 1 year and abdominal thrusts in an older child. In a more stable child, provide supplemental oxygen and consult a physician skilled in laryngoscopy and bronchoscopy for removal of the foreign body. Esophageal foreign bodies may also cause stridor. In these cases the child will often complain of dysphagia or avoid swallowing.
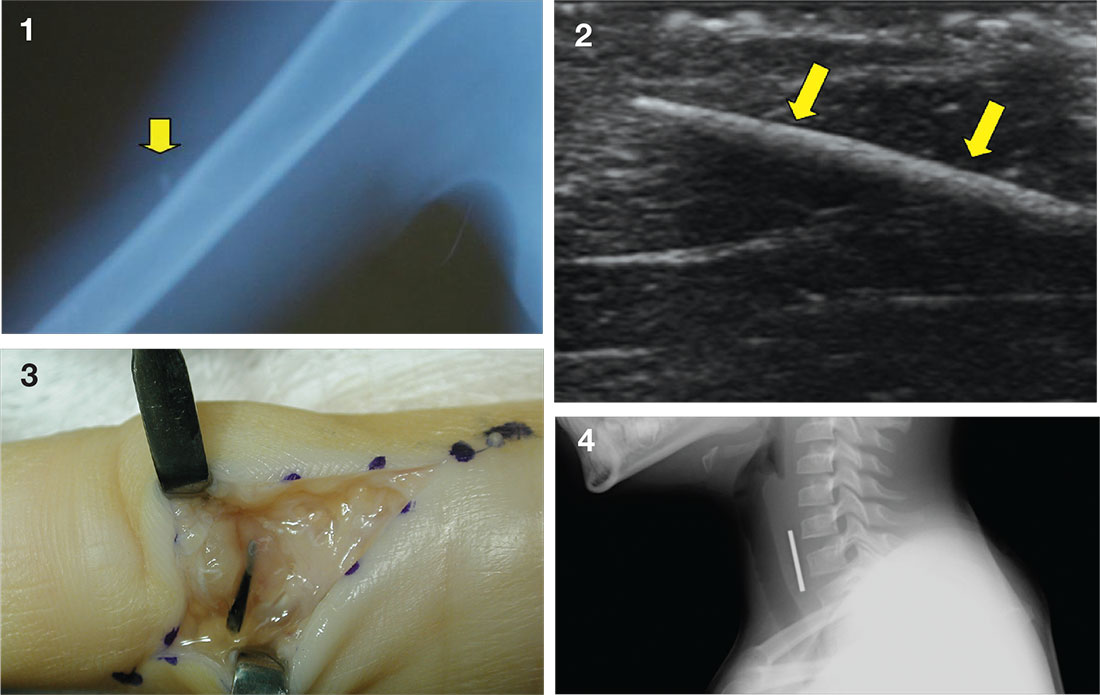
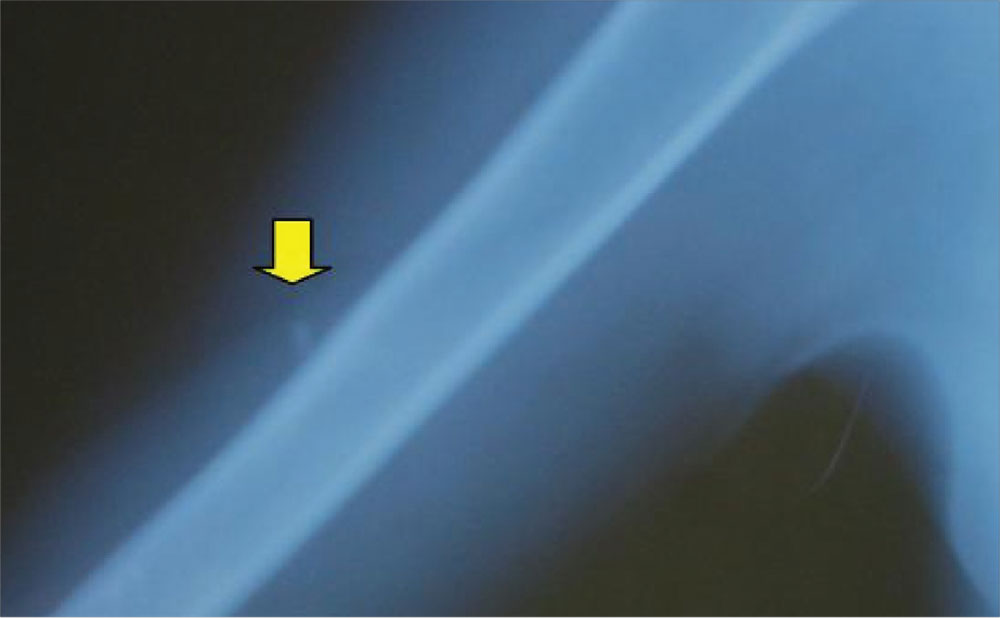
While some objects, such as coins, can be visualized on plain imaging, a negative film does not rule out a foreign body and a specialist should be consulted for endoscopy. A coin in the trachea will be seen on its edge in an anteroposterior view. In the esophagus, it will generally appear as a full circle (en face) in an anteroposterior oblique view. For the lateral view, it is just the opposite, as seen in the case figure.
For more information, see “Differential Diagnosis of Stridor in Children.” Emergency Medicine. 2009 September;41(9):10-11.
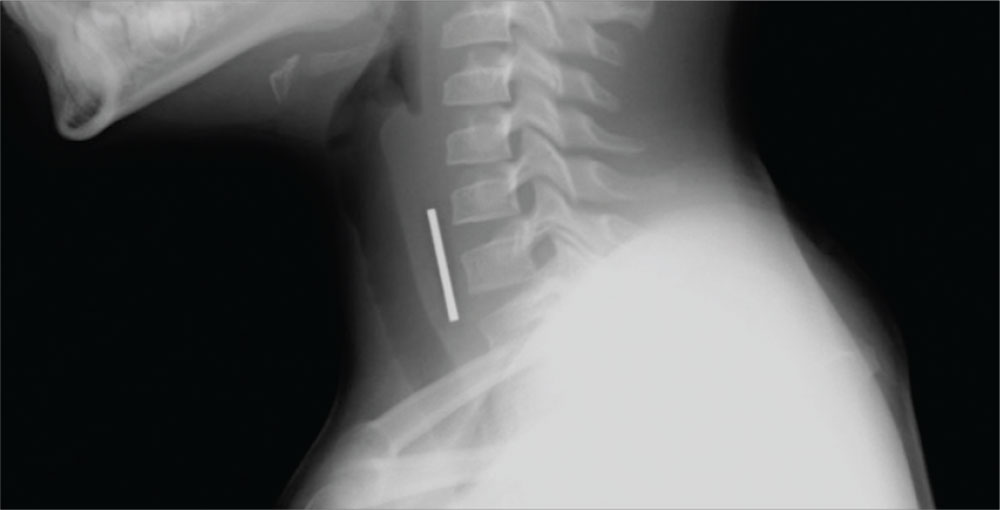
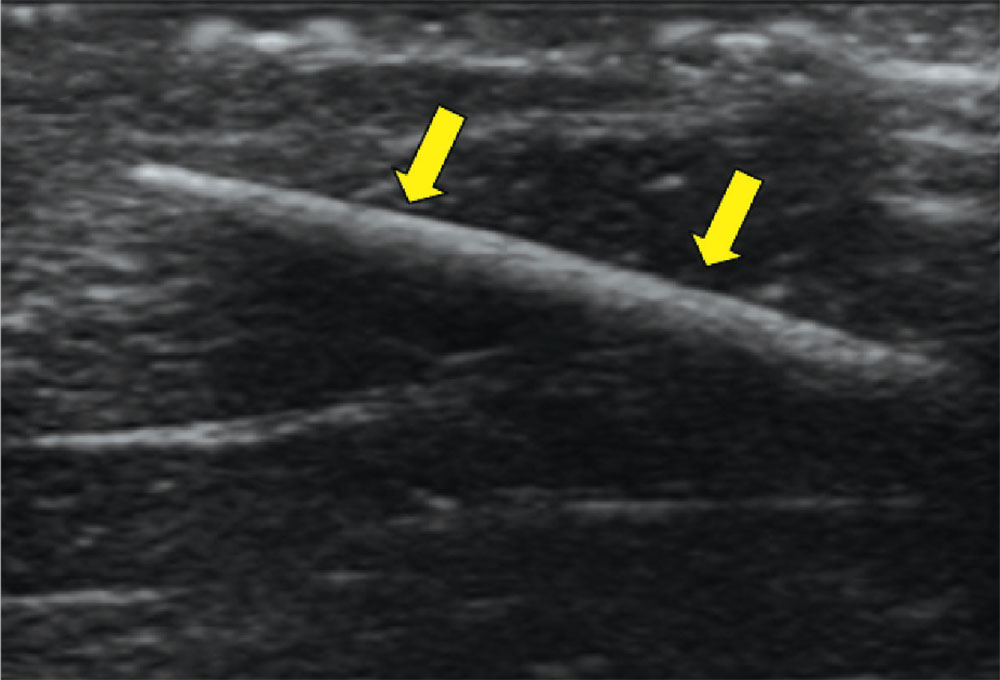
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
You anesthetize the area and begin dissection in an attempt to locate the glass fragment, which goes on for 20 minutes without success. The child and her mother are becoming anxious. You call for the portable ultrasound system, and using its high-frequency transducer, quickly locate the foreign body. After additional anesthesia is applied, the splinter is easily removed under ultrasound guidance and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
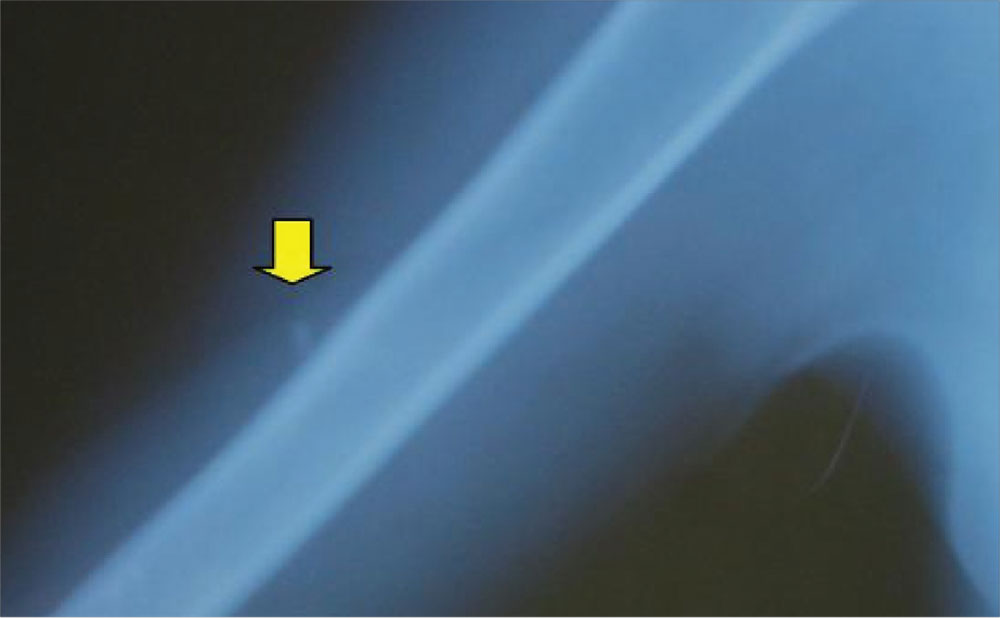
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
The palmar puncture wound site was surgically explored, and no foreign body fragments were found. In addition, the tendons, retracted and delivered through the skin incision, appeared normal.
Histopathology of a specimen intraoperatively biopsied from the flexor tendon sheath showed some refractile foreign material consistent with plant material. After surgery, swelling persisted, and the patient developed limited motion at the extremes of active flexion and extension.
After 2 months, the decision was made to re-explore the palmar puncture site and flexor tendon and obtain tissue specimens for culture, including atypical mycobacterial and fungal cultures. During the second surgery, the palmar site and flexor tendon still appeared unremarkable. As there was some swelling in the long finger, the flexor tendon sheath was explored distally through a separate incision over the middle phalanx. A transversely oriented fragment of the sago palm thorn was found within the flexor tendon sheath. Flexor tendon sheath material was cultured and subsequently found to be negative.
For more information, see “Distal Migration of a Foreign Body (Sago Palm Thorn Fragment) Within the Long-Finger Flexor Tendon Sheath.” Am J Orthop. 2008;37(4):208-209.
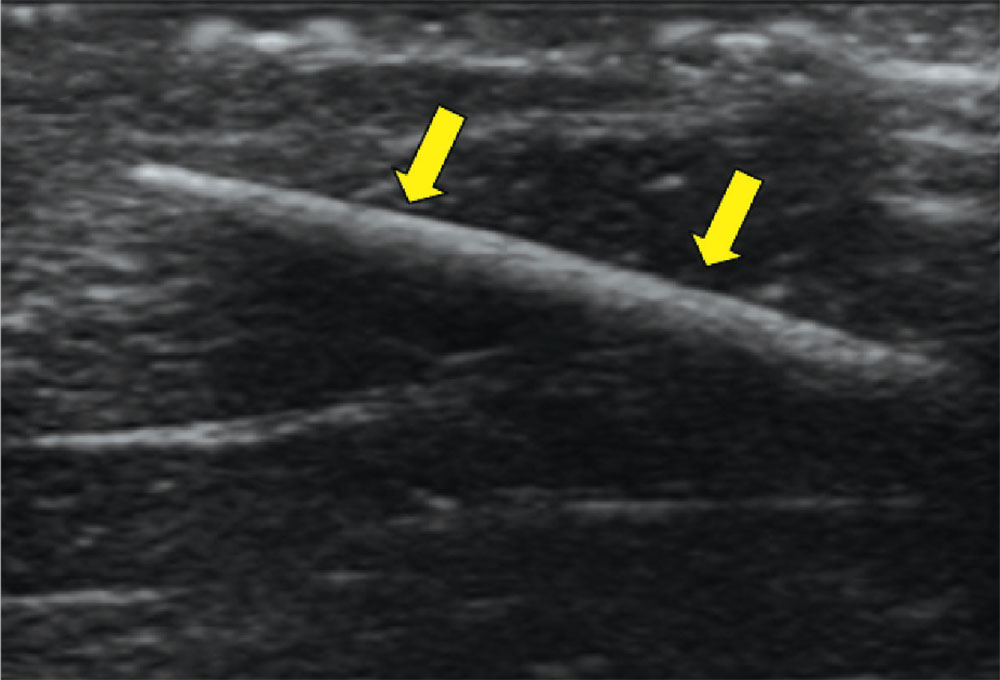
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
With local anesthesia and ultrasound guidance, the splinter is easily removed and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
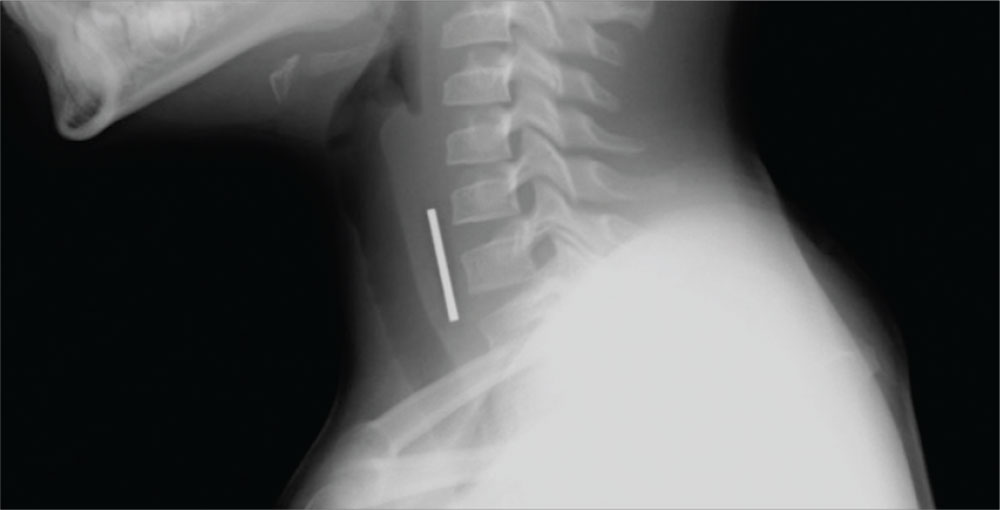
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Complete obstruction should be treated with back blows in a child aged less than 1 year and abdominal thrusts in an older child. In a more stable child, provide supplemental oxygen and consult a physician skilled in laryngoscopy and bronchoscopy for removal of the foreign body. Esophageal foreign bodies may also cause stridor. In these cases the child will often complain of dysphagia or avoid swallowing.
While some objects, such as coins, can be visualized on plain imaging, a negative film does not rule out a foreign body and a specialist should be consulted for endoscopy. A coin in the trachea will be seen on its edge in an anteroposterior view. In the esophagus, it will generally appear as a full circle (en face) in an anteroposterior oblique view. For the lateral view, it is just the opposite, as seen in the case figure.
For more information, see “Differential Diagnosis of Stridor in Children.” Emergency Medicine. 2009 September;41(9):10-11.
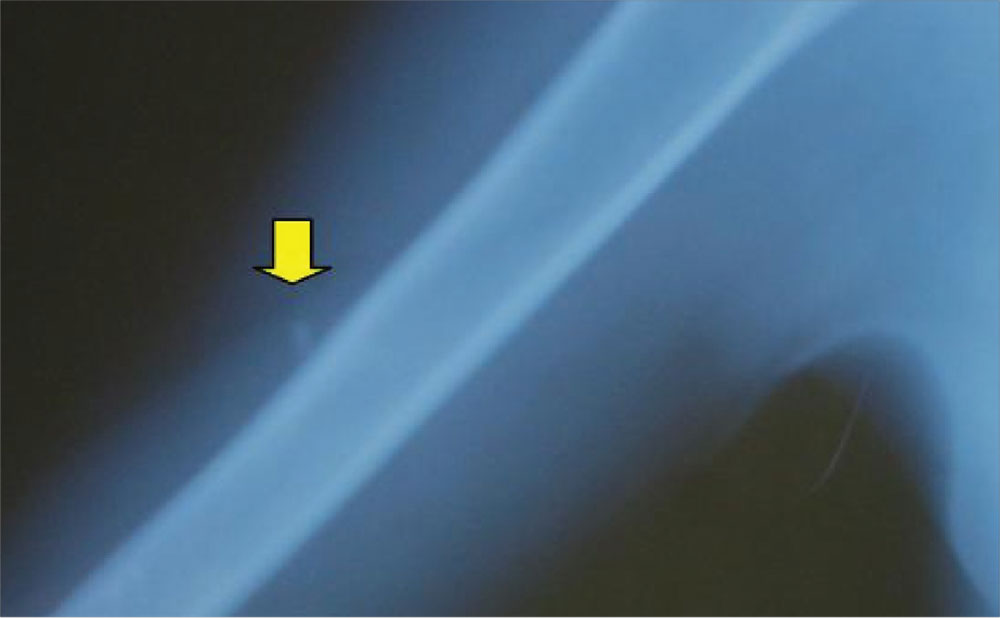
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
You anesthetize the area and begin dissection in an attempt to locate the glass fragment, which goes on for 20 minutes without success. The child and her mother are becoming anxious. You call for the portable ultrasound system, and using its high-frequency transducer, quickly locate the foreign body. After additional anesthesia is applied, the splinter is easily removed under ultrasound guidance and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
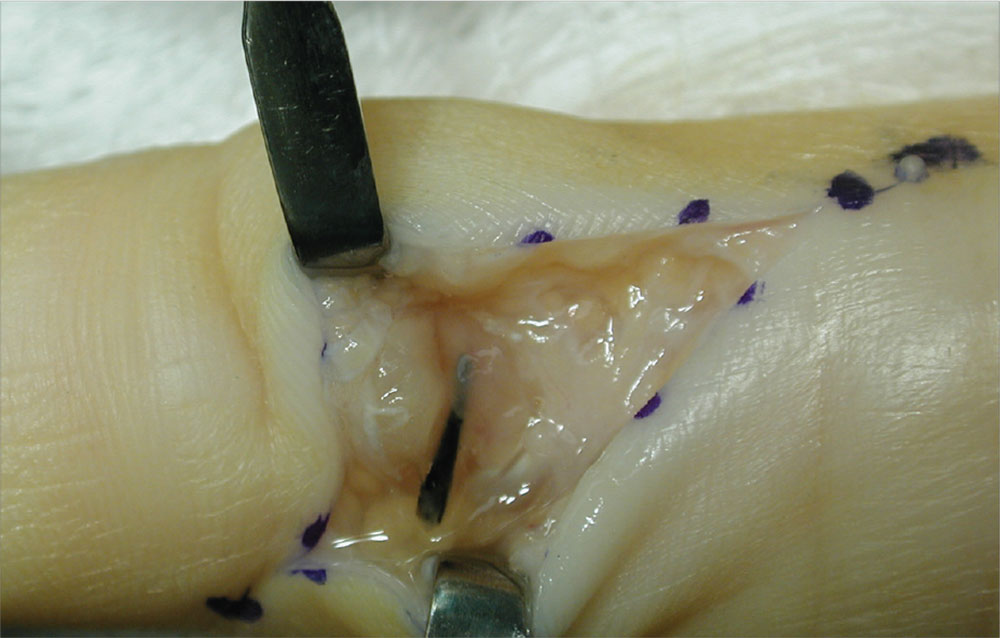
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
The palmar puncture wound site was surgically explored, and no foreign body fragments were found. In addition, the tendons, retracted and delivered through the skin incision, appeared normal.
Histopathology of a specimen intraoperatively biopsied from the flexor tendon sheath showed some refractile foreign material consistent with plant material. After surgery, swelling persisted, and the patient developed limited motion at the extremes of active flexion and extension.
After 2 months, the decision was made to re-explore the palmar puncture site and flexor tendon and obtain tissue specimens for culture, including atypical mycobacterial and fungal cultures. During the second surgery, the palmar site and flexor tendon still appeared unremarkable. As there was some swelling in the long finger, the flexor tendon sheath was explored distally through a separate incision over the middle phalanx. A transversely oriented fragment of the sago palm thorn was found within the flexor tendon sheath. Flexor tendon sheath material was cultured and subsequently found to be negative.
For more information, see “Distal Migration of a Foreign Body (Sago Palm Thorn Fragment) Within the Long-Finger Flexor Tendon Sheath.” Am J Orthop. 2008;37(4):208-209.
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
With local anesthesia and ultrasound guidance, the splinter is easily removed and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
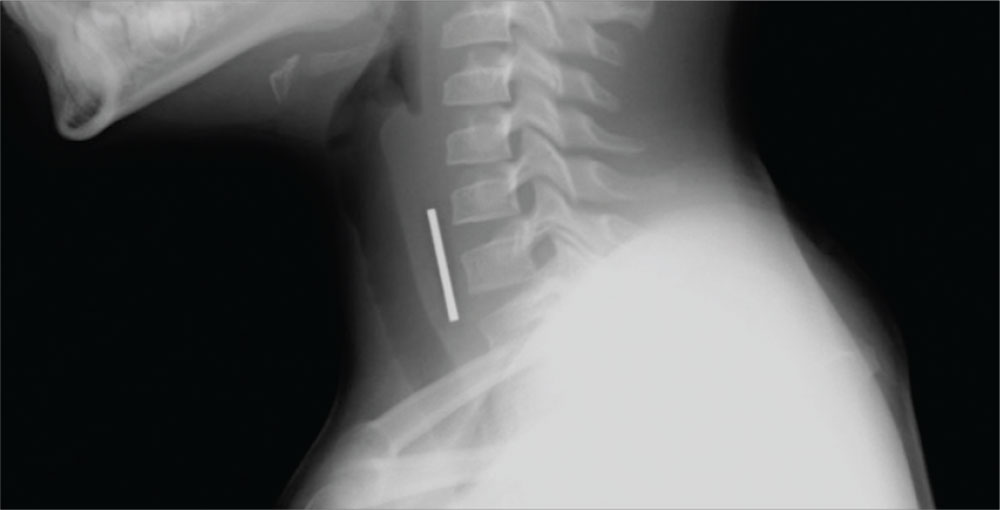
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Complete obstruction should be treated with back blows in a child aged less than 1 year and abdominal thrusts in an older child. In a more stable child, provide supplemental oxygen and consult a physician skilled in laryngoscopy and bronchoscopy for removal of the foreign body. Esophageal foreign bodies may also cause stridor. In these cases the child will often complain of dysphagia or avoid swallowing.
While some objects, such as coins, can be visualized on plain imaging, a negative film does not rule out a foreign body and a specialist should be consulted for endoscopy. A coin in the trachea will be seen on its edge in an anteroposterior view. In the esophagus, it will generally appear as a full circle (en face) in an anteroposterior oblique view. For the lateral view, it is just the opposite, as seen in the case figure.
For more information, see “Differential Diagnosis of Stridor in Children.” Emergency Medicine. 2009 September;41(9):10-11.
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
You anesthetize the area and begin dissection in an attempt to locate the glass fragment, which goes on for 20 minutes without success. The child and her mother are becoming anxious. You call for the portable ultrasound system, and using its high-frequency transducer, quickly locate the foreign body. After additional anesthesia is applied, the splinter is easily removed under ultrasound guidance and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
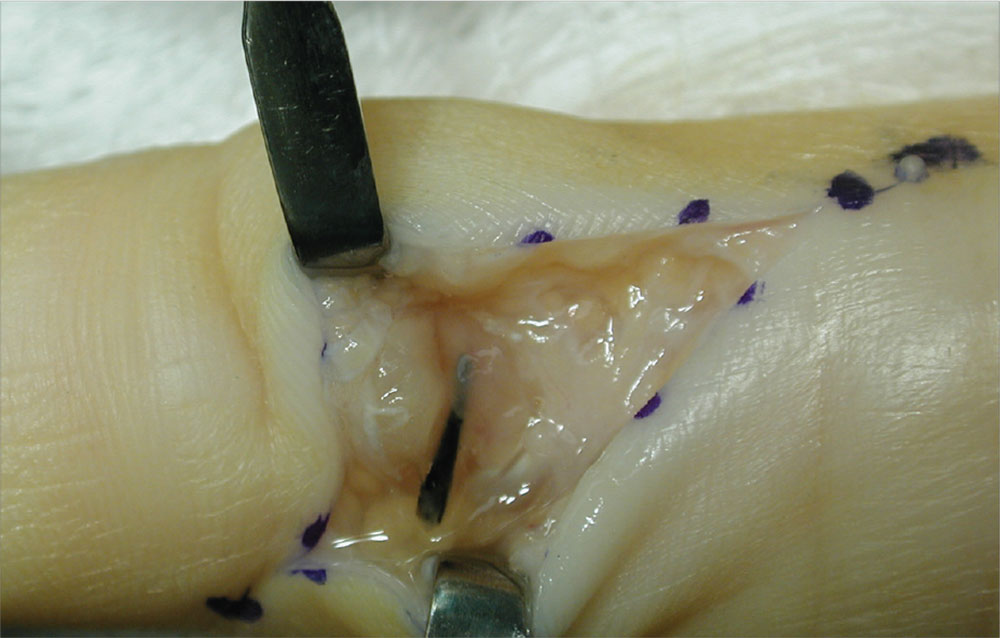
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
The palmar puncture wound site was surgically explored, and no foreign body fragments were found. In addition, the tendons, retracted and delivered through the skin incision, appeared normal.
Histopathology of a specimen intraoperatively biopsied from the flexor tendon sheath showed some refractile foreign material consistent with plant material. After surgery, swelling persisted, and the patient developed limited motion at the extremes of active flexion and extension.
After 2 months, the decision was made to re-explore the palmar puncture site and flexor tendon and obtain tissue specimens for culture, including atypical mycobacterial and fungal cultures. During the second surgery, the palmar site and flexor tendon still appeared unremarkable. As there was some swelling in the long finger, the flexor tendon sheath was explored distally through a separate incision over the middle phalanx. A transversely oriented fragment of the sago palm thorn was found within the flexor tendon sheath. Flexor tendon sheath material was cultured and subsequently found to be negative.
For more information, see “Distal Migration of a Foreign Body (Sago Palm Thorn Fragment) Within the Long-Finger Flexor Tendon Sheath.” Am J Orthop. 2008;37(4):208-209.
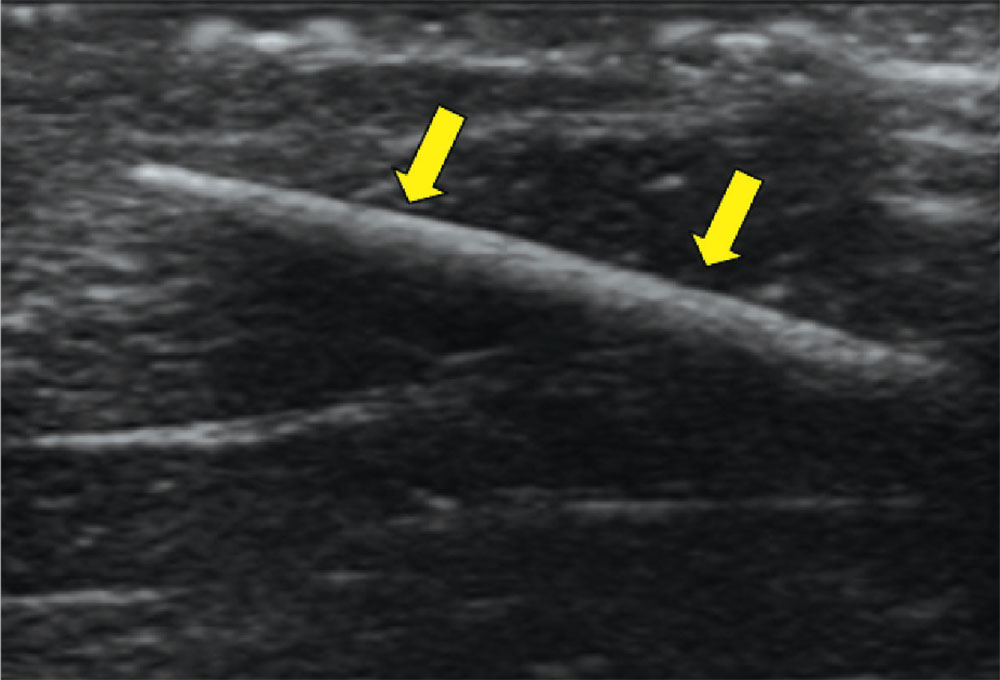
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
With local anesthesia and ultrasound guidance, the splinter is easily removed and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.