User login
Two-Toned Toes
1. A 22-year-old woman dropped an iron on her toe yesterday. Today, the toe is painful at rest and worse with movement.

Diagnosis: The patient was diagnosed with a subungual hematoma and a possible fracture of the distal phalanx. In this case, the clinician offered to drain the hematoma but did not have access to an electrocautery unit. The patient consented to any procedure that would relieve the pain. An open paperclip, held in a hemostat and heated with a torch, was used to pierce the patient’s nail plate and drain the blood, providing immediate relief. Citing lack of insurance, the patient declined an x-ray, despite the possible fracture. The toe was bandaged, and the patient was instructed to keep it elevated and avoid weight-bearing activity. Her toe healed well, and no radiographs were taken.
For more information, see “Painful toe.” J Fam Pract. 2011;60(12).
2. For the past month, a man in his 50s has had a discolored right foot with increasing tenderness, as well as livedo reticularis on the sole and lateral aspect. He has a history of right-arm arterial thrombosis, multiple deep vein thromboses of the legs, ischemic stroke, atrial fibrillation, peripheral arterial disease, and long-term warfarin treatment. Pulses are palpable on exam.

Diagnosis: The patient was diagnosed with antiphospholipid syndrome. He remained on inpatient anticoagulation therapy with fondaparinux and was treated with pulse-dose IV corticosteroids followed by a slow oral taper: daily plasmapheresis for one week, three doses of IV immunoglobulin (0.5 g/kg), and four weekly doses of rituximab (375 mg/m2). His cutaneous findings slowly improved over the next several weeks.
For more information, see “Cyanosis of the Foot.” Cutis. 2017;100(4):206, 209-210.
3. A 35-year-old woman presents in January with purplish toes that are markedly tender to pressure. Recurrent over three successive winters, the initial symptom is an itchy, burning sensation in her toes. The discoloration and other symptoms are constant, not episodic. The condition resolves each year in late spring. Her distal pulses are normal.

Diagnosis: Pernio—also called perniosis or chilblains—is a common dermatologic condition associated with a cold, humid climate. The inflammatory lesions of pernio may be pruritic, painful, erythematous to violaceous plaques, papules, or nodules, which may have overlying blisters or ulcerations. The condition is frequently misdiagnosed; proper diagnosis relies on patient history and clinical picture. Histologic examination is typically not needed or definitive. This patient had moderately disabling pernio, which responded promptly to therapy with a calcium channel blocker.
For more information, see “Erythrocyanotic Discoloration of the Toes.” Cutis. 2000;65(4):223-226.
4. For three days, a 63-year-old man has had severe, sudden-onset pain in the right hallux and fifth toe. The patient has hypertension and hyperlipidemia and has not undergone any vascular procedures. Physical exam reveals cyanotic change with remarkable coldness on the affected toes and livedo reticularis on the underside of the toes. Pulses are palpable. A biopsy of the fifth toe reveals thrombotic arterioles with cholesterol clefts.

Diagnosis: There are a variety of causes for blue toe syndrome, including embolism, thrombosis, vasoconstrictive disorders, infectious and noninfectious inflammation, extensive venous thrombosis, and abnormal blood circulation. Among them, only emboli from atherosclerotic plaques give rise to cholesterol clefts on biopsy. Such atheroemboli are often an iatrogenic complication, especially those caused by invasive percutaneous procedures or damage to the arterial walls from vascular surgery. However, spontaneous plaque hemorrhage or shearing forces of the circulating blood can disrupt atheromatous plaques and cause embolization of cholesterol crystals—which was likely the case with this patient, since no preceding events were noted.
For more information, see “Painful Purple Toes.” Cutis. 2016;98(3):E8-E10.
1. A 22-year-old woman dropped an iron on her toe yesterday. Today, the toe is painful at rest and worse with movement.

Diagnosis: The patient was diagnosed with a subungual hematoma and a possible fracture of the distal phalanx. In this case, the clinician offered to drain the hematoma but did not have access to an electrocautery unit. The patient consented to any procedure that would relieve the pain. An open paperclip, held in a hemostat and heated with a torch, was used to pierce the patient’s nail plate and drain the blood, providing immediate relief. Citing lack of insurance, the patient declined an x-ray, despite the possible fracture. The toe was bandaged, and the patient was instructed to keep it elevated and avoid weight-bearing activity. Her toe healed well, and no radiographs were taken.
For more information, see “Painful toe.” J Fam Pract. 2011;60(12).
2. For the past month, a man in his 50s has had a discolored right foot with increasing tenderness, as well as livedo reticularis on the sole and lateral aspect. He has a history of right-arm arterial thrombosis, multiple deep vein thromboses of the legs, ischemic stroke, atrial fibrillation, peripheral arterial disease, and long-term warfarin treatment. Pulses are palpable on exam.

Diagnosis: The patient was diagnosed with antiphospholipid syndrome. He remained on inpatient anticoagulation therapy with fondaparinux and was treated with pulse-dose IV corticosteroids followed by a slow oral taper: daily plasmapheresis for one week, three doses of IV immunoglobulin (0.5 g/kg), and four weekly doses of rituximab (375 mg/m2). His cutaneous findings slowly improved over the next several weeks.
For more information, see “Cyanosis of the Foot.” Cutis. 2017;100(4):206, 209-210.
3. A 35-year-old woman presents in January with purplish toes that are markedly tender to pressure. Recurrent over three successive winters, the initial symptom is an itchy, burning sensation in her toes. The discoloration and other symptoms are constant, not episodic. The condition resolves each year in late spring. Her distal pulses are normal.

Diagnosis: Pernio—also called perniosis or chilblains—is a common dermatologic condition associated with a cold, humid climate. The inflammatory lesions of pernio may be pruritic, painful, erythematous to violaceous plaques, papules, or nodules, which may have overlying blisters or ulcerations. The condition is frequently misdiagnosed; proper diagnosis relies on patient history and clinical picture. Histologic examination is typically not needed or definitive. This patient had moderately disabling pernio, which responded promptly to therapy with a calcium channel blocker.
For more information, see “Erythrocyanotic Discoloration of the Toes.” Cutis. 2000;65(4):223-226.
4. For three days, a 63-year-old man has had severe, sudden-onset pain in the right hallux and fifth toe. The patient has hypertension and hyperlipidemia and has not undergone any vascular procedures. Physical exam reveals cyanotic change with remarkable coldness on the affected toes and livedo reticularis on the underside of the toes. Pulses are palpable. A biopsy of the fifth toe reveals thrombotic arterioles with cholesterol clefts.

Diagnosis: There are a variety of causes for blue toe syndrome, including embolism, thrombosis, vasoconstrictive disorders, infectious and noninfectious inflammation, extensive venous thrombosis, and abnormal blood circulation. Among them, only emboli from atherosclerotic plaques give rise to cholesterol clefts on biopsy. Such atheroemboli are often an iatrogenic complication, especially those caused by invasive percutaneous procedures or damage to the arterial walls from vascular surgery. However, spontaneous plaque hemorrhage or shearing forces of the circulating blood can disrupt atheromatous plaques and cause embolization of cholesterol crystals—which was likely the case with this patient, since no preceding events were noted.
For more information, see “Painful Purple Toes.” Cutis. 2016;98(3):E8-E10.
1. A 22-year-old woman dropped an iron on her toe yesterday. Today, the toe is painful at rest and worse with movement.

Diagnosis: The patient was diagnosed with a subungual hematoma and a possible fracture of the distal phalanx. In this case, the clinician offered to drain the hematoma but did not have access to an electrocautery unit. The patient consented to any procedure that would relieve the pain. An open paperclip, held in a hemostat and heated with a torch, was used to pierce the patient’s nail plate and drain the blood, providing immediate relief. Citing lack of insurance, the patient declined an x-ray, despite the possible fracture. The toe was bandaged, and the patient was instructed to keep it elevated and avoid weight-bearing activity. Her toe healed well, and no radiographs were taken.
For more information, see “Painful toe.” J Fam Pract. 2011;60(12).
2. For the past month, a man in his 50s has had a discolored right foot with increasing tenderness, as well as livedo reticularis on the sole and lateral aspect. He has a history of right-arm arterial thrombosis, multiple deep vein thromboses of the legs, ischemic stroke, atrial fibrillation, peripheral arterial disease, and long-term warfarin treatment. Pulses are palpable on exam.

Diagnosis: The patient was diagnosed with antiphospholipid syndrome. He remained on inpatient anticoagulation therapy with fondaparinux and was treated with pulse-dose IV corticosteroids followed by a slow oral taper: daily plasmapheresis for one week, three doses of IV immunoglobulin (0.5 g/kg), and four weekly doses of rituximab (375 mg/m2). His cutaneous findings slowly improved over the next several weeks.
For more information, see “Cyanosis of the Foot.” Cutis. 2017;100(4):206, 209-210.
3. A 35-year-old woman presents in January with purplish toes that are markedly tender to pressure. Recurrent over three successive winters, the initial symptom is an itchy, burning sensation in her toes. The discoloration and other symptoms are constant, not episodic. The condition resolves each year in late spring. Her distal pulses are normal.

Diagnosis: Pernio—also called perniosis or chilblains—is a common dermatologic condition associated with a cold, humid climate. The inflammatory lesions of pernio may be pruritic, painful, erythematous to violaceous plaques, papules, or nodules, which may have overlying blisters or ulcerations. The condition is frequently misdiagnosed; proper diagnosis relies on patient history and clinical picture. Histologic examination is typically not needed or definitive. This patient had moderately disabling pernio, which responded promptly to therapy with a calcium channel blocker.
For more information, see “Erythrocyanotic Discoloration of the Toes.” Cutis. 2000;65(4):223-226.
4. For three days, a 63-year-old man has had severe, sudden-onset pain in the right hallux and fifth toe. The patient has hypertension and hyperlipidemia and has not undergone any vascular procedures. Physical exam reveals cyanotic change with remarkable coldness on the affected toes and livedo reticularis on the underside of the toes. Pulses are palpable. A biopsy of the fifth toe reveals thrombotic arterioles with cholesterol clefts.

Diagnosis: There are a variety of causes for blue toe syndrome, including embolism, thrombosis, vasoconstrictive disorders, infectious and noninfectious inflammation, extensive venous thrombosis, and abnormal blood circulation. Among them, only emboli from atherosclerotic plaques give rise to cholesterol clefts on biopsy. Such atheroemboli are often an iatrogenic complication, especially those caused by invasive percutaneous procedures or damage to the arterial walls from vascular surgery. However, spontaneous plaque hemorrhage or shearing forces of the circulating blood can disrupt atheromatous plaques and cause embolization of cholesterol crystals—which was likely the case with this patient, since no preceding events were noted.
For more information, see “Painful Purple Toes.” Cutis. 2016;98(3):E8-E10.
Four Fattened Phalanges
1. A 54-year-old Colombian man presents with nail dystrophy of two years’ duration. Physical exam reveals longitudinally banded thickening of the lateral half of the nail plate with yellowish brown discoloration, transverse overcurvature of the nail, longitudinal white lines, and splinter hemorrhages.

Diagnosis: The lesion, diagnosed as onychomatricoma was surgically removed and sent for histopathologic study. Onychomatricoma is a subungual tumor characterized by banded or diffuse thickening, yellowish discoloration, splinter hemorrhages, and transverse overcurvature of the nail plate. Because the condition is not well known, it is often misdiagnosed.
For more information, see “Onychomatricoma: An Often Misdiagnosed Tumor of the Nails.” Cutis. 2015;96(2):121-124.
2. A 21-year-old woman has a slow-growing, asymptomatic nodule on the great toe. She denies antecedent trauma. A firm, flesh-colored, semimobile, nontender, subungual nodule can be seen in the distal lateral nail bed, extending into the adjacent tissue. Radiographic exam shows focal calcification of the nodule, with direct communication to the underlying distal phalanx.

Diagnosis: Subungual exostosis is a relatively uncommon, benign, osteocartilaginous tumor arising from the distal phalanx beneath the nail. It typically appears on the great toe during the second to third decade of life and has an equal incidence in both sexes. Its similarities to other dermatologic disorders involving the nail bed can lead to misdiagnosis, which may result in inadequate or extreme treatment.
For more information, see “Subungual Exostosis.” Cutis. 2012;90(5):241-243.
3. For the past year, a 30-year-old man’s left great toe has had a 3-cm exophytic, yellowish red, subungual nodule that is obliterating the nail plate. Ten years ago, a similar nodule in the same location was removed via laser by a podiatrist. Plain radiographs demonstrate an inferior cortical lucency of the distal phalanx, as well as a lucency over the nail bed with calcification extending to the soft tissues. MRI reveals bone erosion from the overlying mass.

Diagnosis: Digital fibromyxoma is the term used to describe a distinctive, slow-growing, soft-tissue tumor with a predilection for the periungual or subungual regions of the fingers and toes. This benign growth typically presents as a painless or tender nodule in middle-aged adults, with a slight male predominance. In a case series of 124 patients, 36% who had imaging studies showed bone involvement by an erosive or lytic lesion. Soft-tissue invasion of the bone is demonstrated by scalloping on plain radiographs.
For more information, see “Toe Nodule Obliterating the Nail Bed.” Cutis. 2016;97(4):260, 281-282.
4. A 41-year-old man presents with a slowly growing, tender lesion located on the left great hallux. When it first appeared five months ago, it resembled a blister. On exam today, a firm, 3.5-cm, flesh-colored, pedunculated nodule is seen on the lateral aspect of the toe. No lymphadenopathy is found. The patient reports no history of keloids or trauma to the foot.

Diagnosis: Shave biopsy showed findings consistent with dermatofibrosarcoma protuberans. A chest radiograph was unremarkable. Re-excision was performed with negative margins on frozen section but with positive peripheral and deep margins on permanent sections. The patient subsequently underwent amputation of the left great toe and was lost to follow-up after the initial postoperative period.
For more information, see “Dermatofibrosarcoma Protuberans.” Cutis. 2017;100(1):E6-E7.
1. A 54-year-old Colombian man presents with nail dystrophy of two years’ duration. Physical exam reveals longitudinally banded thickening of the lateral half of the nail plate with yellowish brown discoloration, transverse overcurvature of the nail, longitudinal white lines, and splinter hemorrhages.

Diagnosis: The lesion, diagnosed as onychomatricoma was surgically removed and sent for histopathologic study. Onychomatricoma is a subungual tumor characterized by banded or diffuse thickening, yellowish discoloration, splinter hemorrhages, and transverse overcurvature of the nail plate. Because the condition is not well known, it is often misdiagnosed.
For more information, see “Onychomatricoma: An Often Misdiagnosed Tumor of the Nails.” Cutis. 2015;96(2):121-124.
2. A 21-year-old woman has a slow-growing, asymptomatic nodule on the great toe. She denies antecedent trauma. A firm, flesh-colored, semimobile, nontender, subungual nodule can be seen in the distal lateral nail bed, extending into the adjacent tissue. Radiographic exam shows focal calcification of the nodule, with direct communication to the underlying distal phalanx.

Diagnosis: Subungual exostosis is a relatively uncommon, benign, osteocartilaginous tumor arising from the distal phalanx beneath the nail. It typically appears on the great toe during the second to third decade of life and has an equal incidence in both sexes. Its similarities to other dermatologic disorders involving the nail bed can lead to misdiagnosis, which may result in inadequate or extreme treatment.
For more information, see “Subungual Exostosis.” Cutis. 2012;90(5):241-243.
3. For the past year, a 30-year-old man’s left great toe has had a 3-cm exophytic, yellowish red, subungual nodule that is obliterating the nail plate. Ten years ago, a similar nodule in the same location was removed via laser by a podiatrist. Plain radiographs demonstrate an inferior cortical lucency of the distal phalanx, as well as a lucency over the nail bed with calcification extending to the soft tissues. MRI reveals bone erosion from the overlying mass.

Diagnosis: Digital fibromyxoma is the term used to describe a distinctive, slow-growing, soft-tissue tumor with a predilection for the periungual or subungual regions of the fingers and toes. This benign growth typically presents as a painless or tender nodule in middle-aged adults, with a slight male predominance. In a case series of 124 patients, 36% who had imaging studies showed bone involvement by an erosive or lytic lesion. Soft-tissue invasion of the bone is demonstrated by scalloping on plain radiographs.
For more information, see “Toe Nodule Obliterating the Nail Bed.” Cutis. 2016;97(4):260, 281-282.
4. A 41-year-old man presents with a slowly growing, tender lesion located on the left great hallux. When it first appeared five months ago, it resembled a blister. On exam today, a firm, 3.5-cm, flesh-colored, pedunculated nodule is seen on the lateral aspect of the toe. No lymphadenopathy is found. The patient reports no history of keloids or trauma to the foot.

Diagnosis: Shave biopsy showed findings consistent with dermatofibrosarcoma protuberans. A chest radiograph was unremarkable. Re-excision was performed with negative margins on frozen section but with positive peripheral and deep margins on permanent sections. The patient subsequently underwent amputation of the left great toe and was lost to follow-up after the initial postoperative period.
For more information, see “Dermatofibrosarcoma Protuberans.” Cutis. 2017;100(1):E6-E7.
1. A 54-year-old Colombian man presents with nail dystrophy of two years’ duration. Physical exam reveals longitudinally banded thickening of the lateral half of the nail plate with yellowish brown discoloration, transverse overcurvature of the nail, longitudinal white lines, and splinter hemorrhages.

Diagnosis: The lesion, diagnosed as onychomatricoma was surgically removed and sent for histopathologic study. Onychomatricoma is a subungual tumor characterized by banded or diffuse thickening, yellowish discoloration, splinter hemorrhages, and transverse overcurvature of the nail plate. Because the condition is not well known, it is often misdiagnosed.
For more information, see “Onychomatricoma: An Often Misdiagnosed Tumor of the Nails.” Cutis. 2015;96(2):121-124.
2. A 21-year-old woman has a slow-growing, asymptomatic nodule on the great toe. She denies antecedent trauma. A firm, flesh-colored, semimobile, nontender, subungual nodule can be seen in the distal lateral nail bed, extending into the adjacent tissue. Radiographic exam shows focal calcification of the nodule, with direct communication to the underlying distal phalanx.

Diagnosis: Subungual exostosis is a relatively uncommon, benign, osteocartilaginous tumor arising from the distal phalanx beneath the nail. It typically appears on the great toe during the second to third decade of life and has an equal incidence in both sexes. Its similarities to other dermatologic disorders involving the nail bed can lead to misdiagnosis, which may result in inadequate or extreme treatment.
For more information, see “Subungual Exostosis.” Cutis. 2012;90(5):241-243.
3. For the past year, a 30-year-old man’s left great toe has had a 3-cm exophytic, yellowish red, subungual nodule that is obliterating the nail plate. Ten years ago, a similar nodule in the same location was removed via laser by a podiatrist. Plain radiographs demonstrate an inferior cortical lucency of the distal phalanx, as well as a lucency over the nail bed with calcification extending to the soft tissues. MRI reveals bone erosion from the overlying mass.

Diagnosis: Digital fibromyxoma is the term used to describe a distinctive, slow-growing, soft-tissue tumor with a predilection for the periungual or subungual regions of the fingers and toes. This benign growth typically presents as a painless or tender nodule in middle-aged adults, with a slight male predominance. In a case series of 124 patients, 36% who had imaging studies showed bone involvement by an erosive or lytic lesion. Soft-tissue invasion of the bone is demonstrated by scalloping on plain radiographs.
For more information, see “Toe Nodule Obliterating the Nail Bed.” Cutis. 2016;97(4):260, 281-282.
4. A 41-year-old man presents with a slowly growing, tender lesion located on the left great hallux. When it first appeared five months ago, it resembled a blister. On exam today, a firm, 3.5-cm, flesh-colored, pedunculated nodule is seen on the lateral aspect of the toe. No lymphadenopathy is found. The patient reports no history of keloids or trauma to the foot.

Diagnosis: Shave biopsy showed findings consistent with dermatofibrosarcoma protuberans. A chest radiograph was unremarkable. Re-excision was performed with negative margins on frozen section but with positive peripheral and deep margins on permanent sections. The patient subsequently underwent amputation of the left great toe and was lost to follow-up after the initial postoperative period.
For more information, see “Dermatofibrosarcoma Protuberans.” Cutis. 2017;100(1):E6-E7.
Tick, Tick, Boom
1. A 16-year-old boy presents with a skin ulcer on the dorsum of his hand and swollen glands in the proximal axilla. He works as a camp counselor in South Dakota, leading nature walks and teaching the children to care for animals, including the camp’s rabbits. Several weeks ago, he developed a fever of 103°F, fatigue, and body aches, followed by the appearance of the skin lesion.

Diagnosis: Tularemia—also called rabbit fever or deer fly fever—is caused by the bacterium Francisella tularensis. It is an insect-borne pathogen of rabbits, squirrels, and other rodents, most commonly found in the western United States and Russia. Symptoms vary by mechanism of exposure but include skin ulcers; irritation and inflammation of the eye; sore throat, mouth ulcers, and tonsillitis; lung involvement with cough, chest pain, and difficulty breathing; and swelling of regional lymph nodes. Tularemia can be successfully treated with antibiotics.
For more information, see “Pneumonic Tularemia Presenting With a Vesicular Eruption.” Cutis. 2015;95(4):E17-E18.
2. About 10-12 days after hiking in the Appalachian Mountains, this young woman presents with a 7-in circular rash on her upper back that is slightly warm to the touch. She denies fever, pruritus, and joint pain.

Diagnosis: Lyme disease is the most common tick-borne illness in the United States, with more than 25,000 confirmed cases in 2014. It is concentrated mostly in the northeast and upper Midwest, although in 2014, only five states (Colorado, Hawaii, Louisiana, New Mexico, and Oklahoma) reported no incidence. Lyme disease is caused by Borrelia burgdorferi, which is transmitted to humans by the Ixodes tick.
For more information, see “Beyond the bull's eye: Recognizing Lyme disease.” J Fam Pract. 2016;65(6):373-379.
3. A 42-year-old Native American farmer in Arizona has a reddish purple petechial rash on his ankles and feet. Upon questioning, he reports that about three weeks ago he had a slight fever with headache and malaise. Then, last week, he noticed small, flat, pink, nonitchy macules on his wrists, forearms, and ankles; they are now spreading to the trunk.

Source: CDC
[https://www.cdc.gov/rmsf/symptoms/index.html]
Diagnosis: Rocky Mountain spotted fever, now reported to the CDC as spotted fever rickettsiosis, is a tick-borne illness caused by the gram-negative intracellular bacterium Rickettsia rickettsia. It is endemic in the Southeastern and South Central United States. Most cases occur between April and September, coinciding with the active season of the vector tick species. Early diagnosis is critical because untreated RMSF may progress to fulminant systemic illness.
For more information, see “Fever and Rash in a 3-Year-Old Girl: Rocky Mountain Spotted Fever.” Cutis. 2002;70(3):165-168.
1. A 16-year-old boy presents with a skin ulcer on the dorsum of his hand and swollen glands in the proximal axilla. He works as a camp counselor in South Dakota, leading nature walks and teaching the children to care for animals, including the camp’s rabbits. Several weeks ago, he developed a fever of 103°F, fatigue, and body aches, followed by the appearance of the skin lesion.

Diagnosis: Tularemia—also called rabbit fever or deer fly fever—is caused by the bacterium Francisella tularensis. It is an insect-borne pathogen of rabbits, squirrels, and other rodents, most commonly found in the western United States and Russia. Symptoms vary by mechanism of exposure but include skin ulcers; irritation and inflammation of the eye; sore throat, mouth ulcers, and tonsillitis; lung involvement with cough, chest pain, and difficulty breathing; and swelling of regional lymph nodes. Tularemia can be successfully treated with antibiotics.
For more information, see “Pneumonic Tularemia Presenting With a Vesicular Eruption.” Cutis. 2015;95(4):E17-E18.
2. About 10-12 days after hiking in the Appalachian Mountains, this young woman presents with a 7-in circular rash on her upper back that is slightly warm to the touch. She denies fever, pruritus, and joint pain.

Diagnosis: Lyme disease is the most common tick-borne illness in the United States, with more than 25,000 confirmed cases in 2014. It is concentrated mostly in the northeast and upper Midwest, although in 2014, only five states (Colorado, Hawaii, Louisiana, New Mexico, and Oklahoma) reported no incidence. Lyme disease is caused by Borrelia burgdorferi, which is transmitted to humans by the Ixodes tick.
For more information, see “Beyond the bull's eye: Recognizing Lyme disease.” J Fam Pract. 2016;65(6):373-379.
3. A 42-year-old Native American farmer in Arizona has a reddish purple petechial rash on his ankles and feet. Upon questioning, he reports that about three weeks ago he had a slight fever with headache and malaise. Then, last week, he noticed small, flat, pink, nonitchy macules on his wrists, forearms, and ankles; they are now spreading to the trunk.

Source: CDC
[https://www.cdc.gov/rmsf/symptoms/index.html]
Diagnosis: Rocky Mountain spotted fever, now reported to the CDC as spotted fever rickettsiosis, is a tick-borne illness caused by the gram-negative intracellular bacterium Rickettsia rickettsia. It is endemic in the Southeastern and South Central United States. Most cases occur between April and September, coinciding with the active season of the vector tick species. Early diagnosis is critical because untreated RMSF may progress to fulminant systemic illness.
For more information, see “Fever and Rash in a 3-Year-Old Girl: Rocky Mountain Spotted Fever.” Cutis. 2002;70(3):165-168.
1. A 16-year-old boy presents with a skin ulcer on the dorsum of his hand and swollen glands in the proximal axilla. He works as a camp counselor in South Dakota, leading nature walks and teaching the children to care for animals, including the camp’s rabbits. Several weeks ago, he developed a fever of 103°F, fatigue, and body aches, followed by the appearance of the skin lesion.

Diagnosis: Tularemia—also called rabbit fever or deer fly fever—is caused by the bacterium Francisella tularensis. It is an insect-borne pathogen of rabbits, squirrels, and other rodents, most commonly found in the western United States and Russia. Symptoms vary by mechanism of exposure but include skin ulcers; irritation and inflammation of the eye; sore throat, mouth ulcers, and tonsillitis; lung involvement with cough, chest pain, and difficulty breathing; and swelling of regional lymph nodes. Tularemia can be successfully treated with antibiotics.
For more information, see “Pneumonic Tularemia Presenting With a Vesicular Eruption.” Cutis. 2015;95(4):E17-E18.
2. About 10-12 days after hiking in the Appalachian Mountains, this young woman presents with a 7-in circular rash on her upper back that is slightly warm to the touch. She denies fever, pruritus, and joint pain.

Diagnosis: Lyme disease is the most common tick-borne illness in the United States, with more than 25,000 confirmed cases in 2014. It is concentrated mostly in the northeast and upper Midwest, although in 2014, only five states (Colorado, Hawaii, Louisiana, New Mexico, and Oklahoma) reported no incidence. Lyme disease is caused by Borrelia burgdorferi, which is transmitted to humans by the Ixodes tick.
For more information, see “Beyond the bull's eye: Recognizing Lyme disease.” J Fam Pract. 2016;65(6):373-379.
3. A 42-year-old Native American farmer in Arizona has a reddish purple petechial rash on his ankles and feet. Upon questioning, he reports that about three weeks ago he had a slight fever with headache and malaise. Then, last week, he noticed small, flat, pink, nonitchy macules on his wrists, forearms, and ankles; they are now spreading to the trunk.

Source: CDC
[https://www.cdc.gov/rmsf/symptoms/index.html]
Diagnosis: Rocky Mountain spotted fever, now reported to the CDC as spotted fever rickettsiosis, is a tick-borne illness caused by the gram-negative intracellular bacterium Rickettsia rickettsia. It is endemic in the Southeastern and South Central United States. Most cases occur between April and September, coinciding with the active season of the vector tick species. Early diagnosis is critical because untreated RMSF may progress to fulminant systemic illness.
For more information, see “Fever and Rash in a 3-Year-Old Girl: Rocky Mountain Spotted Fever.” Cutis. 2002;70(3):165-168.
Oral Cues to Disease
1. A 21-year-old man complains of prolonged diarrhea with steady abdominal pain and recent weight loss. He also reports painful knee and hip joints and generalized fatigue. Physical exam reveals fissure-like ulcerations of the mandibular buccal vestibule and localized abdominal pain with fullness in the right lower quadrant.

Diagnosis: Crohn disease can affect the gastrointestinal tract anywhere from the mouth to the anus, and can manifest with oral findings that may not correlate with abdominal symptoms (eg, mucosal cobble stoning, mucosal tags, deep linear ulcerations, gingival hyperplasia, lip fissuring, aphthous ulcers, angular cheilitis). Other features may include diffuse, painless swelling of the lips and mucosal erythema.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
2. Over the past few months, this 43-year-old woman has had multiple severely painful, slow-healing oral ulcers, resulting in the erosion of the lower lip. She reports pain on swallowing and occasional bloody nose after blowing in the morning.

Diagnosis: Vesiculo-bullous lesions in the mouth may be seen with pemphigus vulgaris or bullous pemphigoid. Pemphigus vulgaris, an autoimmune intraepithelial blistering disease, often manifests as flaccid bullae or painful ulcerations in the oral cavity prior to the onset of skin lesions.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
3. A 26-year-old woman presents with fever and fatigue, as well as arthralgia in her hands. Upon examination, she has a malar rash and lichenoid inflammation of the buccal mucosa. She has a family history of autoimmune disorders.

Diagnosis: Oral findings suggestive of systemic or discoid lupus erythematosus may greatly resemble those of oral lichen planus.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
4. This 14-year-old girl is concerned about the multiple ecchymoses and thrombi in her mouth. She feels fatigued and has a fever. Her history includes a tendency to bruise easily, menorrhagia, and a recent infection treated with vancomycin. Physical exam is notable for retinal hemorrhages and jaundice.

Diagnosis: Thrombocytopenia purpura may manifest with oral petechiae, purpura, oral hematomas, or hemorrhagic bullae.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
1. A 21-year-old man complains of prolonged diarrhea with steady abdominal pain and recent weight loss. He also reports painful knee and hip joints and generalized fatigue. Physical exam reveals fissure-like ulcerations of the mandibular buccal vestibule and localized abdominal pain with fullness in the right lower quadrant.

Diagnosis: Crohn disease can affect the gastrointestinal tract anywhere from the mouth to the anus, and can manifest with oral findings that may not correlate with abdominal symptoms (eg, mucosal cobble stoning, mucosal tags, deep linear ulcerations, gingival hyperplasia, lip fissuring, aphthous ulcers, angular cheilitis). Other features may include diffuse, painless swelling of the lips and mucosal erythema.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
2. Over the past few months, this 43-year-old woman has had multiple severely painful, slow-healing oral ulcers, resulting in the erosion of the lower lip. She reports pain on swallowing and occasional bloody nose after blowing in the morning.

Diagnosis: Vesiculo-bullous lesions in the mouth may be seen with pemphigus vulgaris or bullous pemphigoid. Pemphigus vulgaris, an autoimmune intraepithelial blistering disease, often manifests as flaccid bullae or painful ulcerations in the oral cavity prior to the onset of skin lesions.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
3. A 26-year-old woman presents with fever and fatigue, as well as arthralgia in her hands. Upon examination, she has a malar rash and lichenoid inflammation of the buccal mucosa. She has a family history of autoimmune disorders.

Diagnosis: Oral findings suggestive of systemic or discoid lupus erythematosus may greatly resemble those of oral lichen planus.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
4. This 14-year-old girl is concerned about the multiple ecchymoses and thrombi in her mouth. She feels fatigued and has a fever. Her history includes a tendency to bruise easily, menorrhagia, and a recent infection treated with vancomycin. Physical exam is notable for retinal hemorrhages and jaundice.

Diagnosis: Thrombocytopenia purpura may manifest with oral petechiae, purpura, oral hematomas, or hemorrhagic bullae.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
1. A 21-year-old man complains of prolonged diarrhea with steady abdominal pain and recent weight loss. He also reports painful knee and hip joints and generalized fatigue. Physical exam reveals fissure-like ulcerations of the mandibular buccal vestibule and localized abdominal pain with fullness in the right lower quadrant.

Diagnosis: Crohn disease can affect the gastrointestinal tract anywhere from the mouth to the anus, and can manifest with oral findings that may not correlate with abdominal symptoms (eg, mucosal cobble stoning, mucosal tags, deep linear ulcerations, gingival hyperplasia, lip fissuring, aphthous ulcers, angular cheilitis). Other features may include diffuse, painless swelling of the lips and mucosal erythema.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
2. Over the past few months, this 43-year-old woman has had multiple severely painful, slow-healing oral ulcers, resulting in the erosion of the lower lip. She reports pain on swallowing and occasional bloody nose after blowing in the morning.

Diagnosis: Vesiculo-bullous lesions in the mouth may be seen with pemphigus vulgaris or bullous pemphigoid. Pemphigus vulgaris, an autoimmune intraepithelial blistering disease, often manifests as flaccid bullae or painful ulcerations in the oral cavity prior to the onset of skin lesions.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
3. A 26-year-old woman presents with fever and fatigue, as well as arthralgia in her hands. Upon examination, she has a malar rash and lichenoid inflammation of the buccal mucosa. She has a family history of autoimmune disorders.

Diagnosis: Oral findings suggestive of systemic or discoid lupus erythematosus may greatly resemble those of oral lichen planus.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
4. This 14-year-old girl is concerned about the multiple ecchymoses and thrombi in her mouth. She feels fatigued and has a fever. Her history includes a tendency to bruise easily, menorrhagia, and a recent infection treated with vancomycin. Physical exam is notable for retinal hemorrhages and jaundice.

Diagnosis: Thrombocytopenia purpura may manifest with oral petechiae, purpura, oral hematomas, or hemorrhagic bullae.
For more information, see “Oral lesions you can’t afford to miss.” J Fam Pract. 2015;64(7):392-399.
Young & Crusty
1. A 4-year-old boy presents with erythematous, oozing, excoriated plaques on the cheeks and chin (sparing the nose), trunk, and extensor surfaces of the arms and legs. His parents report that the “rash,” which flares on occasion, has been apparent since the boy was 6 months old, and he does anything he can to scratch the itch.

Diagnosis: Diagnosis of atopic dermatitis (AD) is made by age 5 in 85% to 90% of children who develop the disease, and by age 1 in 60% to 65%. AD persists into adulthood in up to one-third of patients. Although the cause is unknown, AD may be triggered by viral infections, food allergens, or weather, and in turn may trigger an inflammatory progression known as atopic march. Other factors affecting AD development include genetics and hygiene.
For more information:
“A Practical Overview of Pediatric Atopic Dermatitis, Part 2: Triggers and Grading.” Cutis. 2016;97(5):326-329.
“A Practical Overview of Pediatric Atopic Dermatitis, Part 3: Differential Diagnosis, Comorbidities, and Measurement of Disease Burden.” Cutis. 2016;97(6):408-412.
2. A child presents with a history of flaccid bullae and encased fluid progressing from clear yellow to turbid and darkish yellow. The pustules have ruptured, resulting in thin, light brown to golden yellow crusts and a collarette of scale at the periphery of the erosion. Itching is mild.

Diagnosis: Bullous impetigo most commonly affects neonates, hence the occasionally used (and inadvisably employed) name pemphigus neonatorum. Bullous impetigo appears to be less contagious than the nonbullous form and is usually sporadic in presentation. Typical areas of occurrence include the trunk and extremities, as well as intertriginous zones (eg, the diaper area, neck folds, and axillae).
For more information, see “Impetigo Update: New Challenges in the Era of Methicillin Resistance.” Cutis. 2010;85(2):65-70.
3. A 16-year-old Hispanic girl seeks consultation for a perioral rash that first appeared two weeks ago, shortly after she used an OTC depilatory agent. The rash has worsened despite application of topical neomycin ointment. The patient reports pruritus and occasional burning. Examination reveals erythema, hyperpigmentation, and excoriation of the skin around the corners of the mouth.

Diagnosis: An allergic contact dermatitis to both the depilatory agent and neomycin was suspected. The patient was advised to discontinue use of both products, and a medium-potency topical steroid was prescribed. She returned for follow-up in 10 days, at which time the condition had improved by about 75%. Therapy was changed to 1% hydrocortisone cream. The patient was instructed to return for patch testing if the dermatitis recurred.
Reprinted with permission from Emergency Medicine. 2010;42(8):19-20. http://www.mdedge.com/emed-journal/article/71585/dermatology/lesion-scrotum
4. The rash on this 5-month-old baby’s hands manifested several weeks ago. It spread to his arms and trunk and is now essentially everywhere except his face. Despite a number of treatment attempts, including oral antibiotics and OTC topical steroid creams, the problem persists.

Diagnosis: The diagnosis of scabies should be confirmed, whenever possible, with microscopic scabetic findings. In addition, treating the whole family and identifying the source of the infestation are crucial. Diagnosis of scabies is difficult in infants, as any part of an infant’s thin, soft, relatively hairless skin is fair game (whereas, in adults, scabies rarely affects skin above the neck). And although infants with scabies undoubtedly itch—probably just as much as adults—they are inept excoriators and even worse historians. In contrast, adults with scabies will scratch and complain continuously while in the exam room.
For more information, see “Baby Has Rash; Parents Feel Itchy.” Clinician Reviews. 2014;24(9):W3.
1. A 4-year-old boy presents with erythematous, oozing, excoriated plaques on the cheeks and chin (sparing the nose), trunk, and extensor surfaces of the arms and legs. His parents report that the “rash,” which flares on occasion, has been apparent since the boy was 6 months old, and he does anything he can to scratch the itch.

Diagnosis: Diagnosis of atopic dermatitis (AD) is made by age 5 in 85% to 90% of children who develop the disease, and by age 1 in 60% to 65%. AD persists into adulthood in up to one-third of patients. Although the cause is unknown, AD may be triggered by viral infections, food allergens, or weather, and in turn may trigger an inflammatory progression known as atopic march. Other factors affecting AD development include genetics and hygiene.
For more information:
“A Practical Overview of Pediatric Atopic Dermatitis, Part 2: Triggers and Grading.” Cutis. 2016;97(5):326-329.
“A Practical Overview of Pediatric Atopic Dermatitis, Part 3: Differential Diagnosis, Comorbidities, and Measurement of Disease Burden.” Cutis. 2016;97(6):408-412.
2. A child presents with a history of flaccid bullae and encased fluid progressing from clear yellow to turbid and darkish yellow. The pustules have ruptured, resulting in thin, light brown to golden yellow crusts and a collarette of scale at the periphery of the erosion. Itching is mild.

Diagnosis: Bullous impetigo most commonly affects neonates, hence the occasionally used (and inadvisably employed) name pemphigus neonatorum. Bullous impetigo appears to be less contagious than the nonbullous form and is usually sporadic in presentation. Typical areas of occurrence include the trunk and extremities, as well as intertriginous zones (eg, the diaper area, neck folds, and axillae).
For more information, see “Impetigo Update: New Challenges in the Era of Methicillin Resistance.” Cutis. 2010;85(2):65-70.
3. A 16-year-old Hispanic girl seeks consultation for a perioral rash that first appeared two weeks ago, shortly after she used an OTC depilatory agent. The rash has worsened despite application of topical neomycin ointment. The patient reports pruritus and occasional burning. Examination reveals erythema, hyperpigmentation, and excoriation of the skin around the corners of the mouth.

Diagnosis: An allergic contact dermatitis to both the depilatory agent and neomycin was suspected. The patient was advised to discontinue use of both products, and a medium-potency topical steroid was prescribed. She returned for follow-up in 10 days, at which time the condition had improved by about 75%. Therapy was changed to 1% hydrocortisone cream. The patient was instructed to return for patch testing if the dermatitis recurred.
Reprinted with permission from Emergency Medicine. 2010;42(8):19-20. http://www.mdedge.com/emed-journal/article/71585/dermatology/lesion-scrotum
4. The rash on this 5-month-old baby’s hands manifested several weeks ago. It spread to his arms and trunk and is now essentially everywhere except his face. Despite a number of treatment attempts, including oral antibiotics and OTC topical steroid creams, the problem persists.

Diagnosis: The diagnosis of scabies should be confirmed, whenever possible, with microscopic scabetic findings. In addition, treating the whole family and identifying the source of the infestation are crucial. Diagnosis of scabies is difficult in infants, as any part of an infant’s thin, soft, relatively hairless skin is fair game (whereas, in adults, scabies rarely affects skin above the neck). And although infants with scabies undoubtedly itch—probably just as much as adults—they are inept excoriators and even worse historians. In contrast, adults with scabies will scratch and complain continuously while in the exam room.
For more information, see “Baby Has Rash; Parents Feel Itchy.” Clinician Reviews. 2014;24(9):W3.
1. A 4-year-old boy presents with erythematous, oozing, excoriated plaques on the cheeks and chin (sparing the nose), trunk, and extensor surfaces of the arms and legs. His parents report that the “rash,” which flares on occasion, has been apparent since the boy was 6 months old, and he does anything he can to scratch the itch.

Diagnosis: Diagnosis of atopic dermatitis (AD) is made by age 5 in 85% to 90% of children who develop the disease, and by age 1 in 60% to 65%. AD persists into adulthood in up to one-third of patients. Although the cause is unknown, AD may be triggered by viral infections, food allergens, or weather, and in turn may trigger an inflammatory progression known as atopic march. Other factors affecting AD development include genetics and hygiene.
For more information:
“A Practical Overview of Pediatric Atopic Dermatitis, Part 2: Triggers and Grading.” Cutis. 2016;97(5):326-329.
“A Practical Overview of Pediatric Atopic Dermatitis, Part 3: Differential Diagnosis, Comorbidities, and Measurement of Disease Burden.” Cutis. 2016;97(6):408-412.
2. A child presents with a history of flaccid bullae and encased fluid progressing from clear yellow to turbid and darkish yellow. The pustules have ruptured, resulting in thin, light brown to golden yellow crusts and a collarette of scale at the periphery of the erosion. Itching is mild.

Diagnosis: Bullous impetigo most commonly affects neonates, hence the occasionally used (and inadvisably employed) name pemphigus neonatorum. Bullous impetigo appears to be less contagious than the nonbullous form and is usually sporadic in presentation. Typical areas of occurrence include the trunk and extremities, as well as intertriginous zones (eg, the diaper area, neck folds, and axillae).
For more information, see “Impetigo Update: New Challenges in the Era of Methicillin Resistance.” Cutis. 2010;85(2):65-70.
3. A 16-year-old Hispanic girl seeks consultation for a perioral rash that first appeared two weeks ago, shortly after she used an OTC depilatory agent. The rash has worsened despite application of topical neomycin ointment. The patient reports pruritus and occasional burning. Examination reveals erythema, hyperpigmentation, and excoriation of the skin around the corners of the mouth.

Diagnosis: An allergic contact dermatitis to both the depilatory agent and neomycin was suspected. The patient was advised to discontinue use of both products, and a medium-potency topical steroid was prescribed. She returned for follow-up in 10 days, at which time the condition had improved by about 75%. Therapy was changed to 1% hydrocortisone cream. The patient was instructed to return for patch testing if the dermatitis recurred.
Reprinted with permission from Emergency Medicine. 2010;42(8):19-20. http://www.mdedge.com/emed-journal/article/71585/dermatology/lesion-scrotum
4. The rash on this 5-month-old baby’s hands manifested several weeks ago. It spread to his arms and trunk and is now essentially everywhere except his face. Despite a number of treatment attempts, including oral antibiotics and OTC topical steroid creams, the problem persists.

Diagnosis: The diagnosis of scabies should be confirmed, whenever possible, with microscopic scabetic findings. In addition, treating the whole family and identifying the source of the infestation are crucial. Diagnosis of scabies is difficult in infants, as any part of an infant’s thin, soft, relatively hairless skin is fair game (whereas, in adults, scabies rarely affects skin above the neck). And although infants with scabies undoubtedly itch—probably just as much as adults—they are inept excoriators and even worse historians. In contrast, adults with scabies will scratch and complain continuously while in the exam room.
For more information, see “Baby Has Rash; Parents Feel Itchy.” Clinician Reviews. 2014;24(9):W3.
Something is Afoot
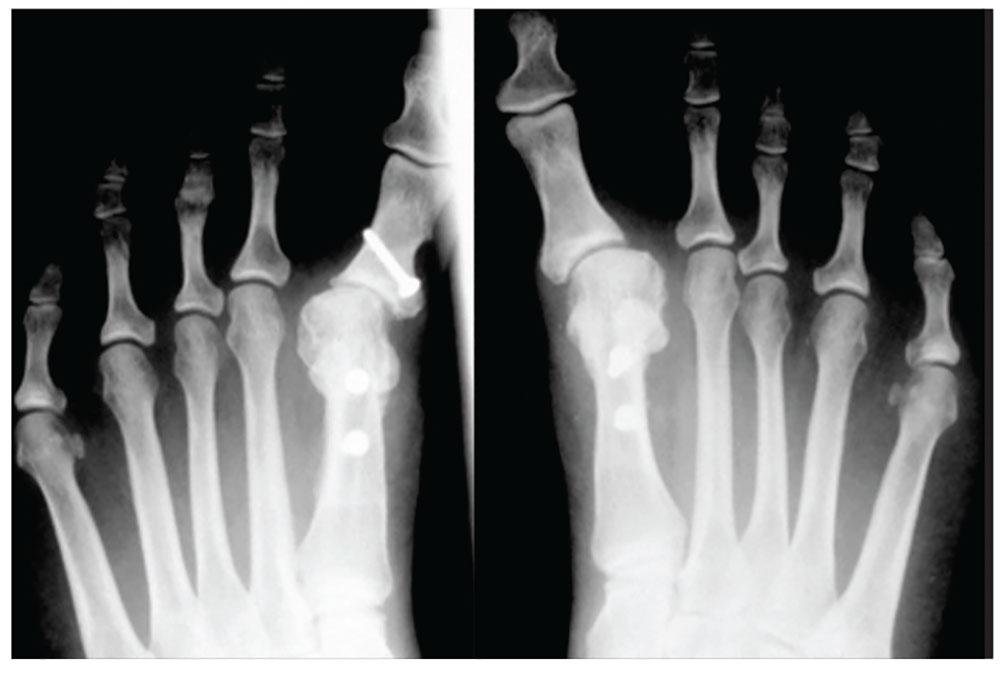
1. A 43-year-old woman presents with progressively worsening bilateral great toe pain that began during pregnancy and increased following the birth of her daughter three years ago. Both of her feet have developed a crescent moon shape, making it painful and difficult to wear normal shoes. This patient has
a) Degenerative arthritis
b) Hallux varus
c) Gout
d) Traumatic sesamoiditis
Diagnosis: Physical exam revealed bilateral hallux varus deformity of the great toe, which was greater on the left foot than on the right (23° and 16°, respectively). The deformities were easily, passively, correctable. Standing radiographs showed evidence of previous proximal osteotomies and well-healed distal first metatarsal osteotomies. Due to unsuccessful nonoperative management, surgical reconstruction was offered.
For further information, see “Bilateral Hallux Varus Deformity Correction With a Suture Button Construct.” Am J Orthop. 2013;42(3):121-124.

2. Following treatment for onychomycosis, this 49-year-old man’s toenails demonstrate inflammation of the medial and lateral nail borders of the hallux and second toes of the left foot. This patient’s diagnosis is
a) Subungual exostosis
b) Primary osteomyelitis of the phalanx
c) Tumors of the nail bed
d) Onychocryptosis
Diagnosis: Onychocryptosis, also known as ingrown toenail, is a rare complication of oral antifungal therapy. As the healthy nail plate advances, it may adhere to the nail bed and cut into the lateral nail folds. In this case, the site of the onychocryptosis corresponded to the proximal clearing of the nail plate. The patient required excision of the nail borders, after which the secondary inflammation resolved. The condition was treated with chemical matrixectomy.
For more information, see “Multiple Onychocryptosis Following Treatment of Onychomycosis With Oral Terbinafine.” Cutis. 2000;66(3):211-212.

3. A 39-year-old man was playing a game of pick-up basketball when he felt a pop, immediately followed by a sharp pain in the back of his ankle and lower leg. He now walks with a limp. The cause is
a) Achilles tendon rupture
b) Medial gastrocnemius tear
c) Calf muscle strain
d) Posterior tibial stress syndrome
Diagnosis: Often diagnosed as an ankle sprain, an Achilles tendon rupture most commonly occurs in middle-aged men from overexertion in sports—usually tennis, racquetball, basketball, or badminton, which involve bursts of jumping, pivoting, and running. Rupture may also occur from a sudden stumble, fall from a significant height, or abrupt step into a hole or off a curb, which causes the tendon to overstretch forcefully.

4. A 60-year-old woman seeks relief for a foot wound of several months’ duration that persists despite use of antibiotics and proper care. The skin over the plantar surface has a full-thickness ulcer, with partial necrosis of the subcutaneous tissue. Her history is significant for diabetes with neuropathy, nephropathy, and retinopathy. The diagnosis is
a) Osteomyelitis
b) Deep venous thrombosis
c) Charcot joint
d) Septic joint
Diagnosis: Charcot joint changes, and an associated stage III pressure ulcer, account for the extensive collapse of the inner arch and “rocker bottom foot” seen on the radiograph. Also known as neurogenic arthropathy, Charcot joint is commonly seen with diabetic neuropathy. In affected patients, secondary degenerative changes to the joints occur with loss of normal muscle tone, proprioception, temperature perception, and pain perception. The joints become loose, enlarged, and boggy. There can be extensive cartilage erosion or osteophyte formation. The normal plantar and heel forces are increased, producing eccentric loading of the foot and leading to microfractures, ligament laxity, and bone destruction.
For more information, see “A disfigured foot with ulcer.” J Fam Pract. 2008;57(5):321-323.
1. A 43-year-old woman presents with progressively worsening bilateral great toe pain that began during pregnancy and increased following the birth of her daughter three years ago. Both of her feet have developed a crescent moon shape, making it painful and difficult to wear normal shoes. This patient has
a) Degenerative arthritis
b) Hallux varus
c) Gout
d) Traumatic sesamoiditis
Diagnosis: Physical exam revealed bilateral hallux varus deformity of the great toe, which was greater on the left foot than on the right (23° and 16°, respectively). The deformities were easily, passively, correctable. Standing radiographs showed evidence of previous proximal osteotomies and well-healed distal first metatarsal osteotomies. Due to unsuccessful nonoperative management, surgical reconstruction was offered.
For further information, see “Bilateral Hallux Varus Deformity Correction With a Suture Button Construct.” Am J Orthop. 2013;42(3):121-124.

2. Following treatment for onychomycosis, this 49-year-old man’s toenails demonstrate inflammation of the medial and lateral nail borders of the hallux and second toes of the left foot. This patient’s diagnosis is
a) Subungual exostosis
b) Primary osteomyelitis of the phalanx
c) Tumors of the nail bed
d) Onychocryptosis
Diagnosis: Onychocryptosis, also known as ingrown toenail, is a rare complication of oral antifungal therapy. As the healthy nail plate advances, it may adhere to the nail bed and cut into the lateral nail folds. In this case, the site of the onychocryptosis corresponded to the proximal clearing of the nail plate. The patient required excision of the nail borders, after which the secondary inflammation resolved. The condition was treated with chemical matrixectomy.
For more information, see “Multiple Onychocryptosis Following Treatment of Onychomycosis With Oral Terbinafine.” Cutis. 2000;66(3):211-212.

3. A 39-year-old man was playing a game of pick-up basketball when he felt a pop, immediately followed by a sharp pain in the back of his ankle and lower leg. He now walks with a limp. The cause is
a) Achilles tendon rupture
b) Medial gastrocnemius tear
c) Calf muscle strain
d) Posterior tibial stress syndrome
Diagnosis: Often diagnosed as an ankle sprain, an Achilles tendon rupture most commonly occurs in middle-aged men from overexertion in sports—usually tennis, racquetball, basketball, or badminton, which involve bursts of jumping, pivoting, and running. Rupture may also occur from a sudden stumble, fall from a significant height, or abrupt step into a hole or off a curb, which causes the tendon to overstretch forcefully.

4. A 60-year-old woman seeks relief for a foot wound of several months’ duration that persists despite use of antibiotics and proper care. The skin over the plantar surface has a full-thickness ulcer, with partial necrosis of the subcutaneous tissue. Her history is significant for diabetes with neuropathy, nephropathy, and retinopathy. The diagnosis is
a) Osteomyelitis
b) Deep venous thrombosis
c) Charcot joint
d) Septic joint
Diagnosis: Charcot joint changes, and an associated stage III pressure ulcer, account for the extensive collapse of the inner arch and “rocker bottom foot” seen on the radiograph. Also known as neurogenic arthropathy, Charcot joint is commonly seen with diabetic neuropathy. In affected patients, secondary degenerative changes to the joints occur with loss of normal muscle tone, proprioception, temperature perception, and pain perception. The joints become loose, enlarged, and boggy. There can be extensive cartilage erosion or osteophyte formation. The normal plantar and heel forces are increased, producing eccentric loading of the foot and leading to microfractures, ligament laxity, and bone destruction.
For more information, see “A disfigured foot with ulcer.” J Fam Pract. 2008;57(5):321-323.
1. A 43-year-old woman presents with progressively worsening bilateral great toe pain that began during pregnancy and increased following the birth of her daughter three years ago. Both of her feet have developed a crescent moon shape, making it painful and difficult to wear normal shoes. This patient has
a) Degenerative arthritis
b) Hallux varus
c) Gout
d) Traumatic sesamoiditis
Diagnosis: Physical exam revealed bilateral hallux varus deformity of the great toe, which was greater on the left foot than on the right (23° and 16°, respectively). The deformities were easily, passively, correctable. Standing radiographs showed evidence of previous proximal osteotomies and well-healed distal first metatarsal osteotomies. Due to unsuccessful nonoperative management, surgical reconstruction was offered.
For further information, see “Bilateral Hallux Varus Deformity Correction With a Suture Button Construct.” Am J Orthop. 2013;42(3):121-124.

2. Following treatment for onychomycosis, this 49-year-old man’s toenails demonstrate inflammation of the medial and lateral nail borders of the hallux and second toes of the left foot. This patient’s diagnosis is
a) Subungual exostosis
b) Primary osteomyelitis of the phalanx
c) Tumors of the nail bed
d) Onychocryptosis
Diagnosis: Onychocryptosis, also known as ingrown toenail, is a rare complication of oral antifungal therapy. As the healthy nail plate advances, it may adhere to the nail bed and cut into the lateral nail folds. In this case, the site of the onychocryptosis corresponded to the proximal clearing of the nail plate. The patient required excision of the nail borders, after which the secondary inflammation resolved. The condition was treated with chemical matrixectomy.
For more information, see “Multiple Onychocryptosis Following Treatment of Onychomycosis With Oral Terbinafine.” Cutis. 2000;66(3):211-212.

3. A 39-year-old man was playing a game of pick-up basketball when he felt a pop, immediately followed by a sharp pain in the back of his ankle and lower leg. He now walks with a limp. The cause is
a) Achilles tendon rupture
b) Medial gastrocnemius tear
c) Calf muscle strain
d) Posterior tibial stress syndrome
Diagnosis: Often diagnosed as an ankle sprain, an Achilles tendon rupture most commonly occurs in middle-aged men from overexertion in sports—usually tennis, racquetball, basketball, or badminton, which involve bursts of jumping, pivoting, and running. Rupture may also occur from a sudden stumble, fall from a significant height, or abrupt step into a hole or off a curb, which causes the tendon to overstretch forcefully.

4. A 60-year-old woman seeks relief for a foot wound of several months’ duration that persists despite use of antibiotics and proper care. The skin over the plantar surface has a full-thickness ulcer, with partial necrosis of the subcutaneous tissue. Her history is significant for diabetes with neuropathy, nephropathy, and retinopathy. The diagnosis is
a) Osteomyelitis
b) Deep venous thrombosis
c) Charcot joint
d) Septic joint
Diagnosis: Charcot joint changes, and an associated stage III pressure ulcer, account for the extensive collapse of the inner arch and “rocker bottom foot” seen on the radiograph. Also known as neurogenic arthropathy, Charcot joint is commonly seen with diabetic neuropathy. In affected patients, secondary degenerative changes to the joints occur with loss of normal muscle tone, proprioception, temperature perception, and pain perception. The joints become loose, enlarged, and boggy. There can be extensive cartilage erosion or osteophyte formation. The normal plantar and heel forces are increased, producing eccentric loading of the foot and leading to microfractures, ligament laxity, and bone destruction.
For more information, see “A disfigured foot with ulcer.” J Fam Pract. 2008;57(5):321-323.
Common Conditions in Persons with Skin of Color
1. This patient is concerned about the numerous long-standing “moles” on her face. Only occasionally pruritic, they are otherwise asymptomatic. Nevertheless, the patient wants them investigated and removed.

Diagnosis: Dermatosis papulosa nigra (DPN) is a benign condition that presents as multiple brown to dark-brown 1- to 5-mm papules on the face, neck, and trunk. The lesions are a sign of aging in darker skinned patients and do not require treatment. They can, however, be safely, easily, and effectively removed. Both electrodesiccation and KTP (532 nm) laser have comparable efficacy in the removal of DPN, according to a 2009 study published in the American Journal of Dermatologic Surgery. Without use of anesthetics, the KTP laser is preferred for patient comfort.
For more information, see “Skin of Color: Dermatosis Papulosa Nigra Removal.” Dermatology News. February 1, 2012.
2. A 17-year-old African-American boy likes to keep his face clean-shaven, but his skin becomes irritated every time he shaves. He states that his father also has this problem, but doesn’t have a solution.

Diagnosis: Pseudofolliculitis is a common skin condition affecting hair-bearing areas of the body that are shaved. It develops when the free end of a tightly coiled hair reenters the skin after shaving, causing a foreign-body–like inflammatory reaction. Tightly curled hair has a greater tendency to pierce the follicle and the surface of the skin, explaining the relative predominance of pseudofolliculitis in patients of African descent; at least half of black men who shave develop the condition.
For more information, see “Bumps in beard area.” J Fam Pract. 2015 November;64(11).
3. A 15-year-old African-American boy presents with a two-month history of hair loss and pruritic papules on the back of his head that developed after a barber shaved the area. There are two dozen 1- to 2-mm papules on his posterior neck and occipital scalp with areas of focal crusting. The patient had a similar episode a year ago after shaving the same area, but those papules cleared after one month of applying rubbing alcohol.

Diagnosis: This patient’s diagnosis is acne keloidalis nuchae (AKN), a chronic folliculitis characterized by smooth, dome-shaped papules on the posterior scalp and neck that become confluent and form firm papules and hairless, keloid-like plaques. Seen almost exclusively in young, postpubescent African-American males, the condition is often asymptomatic, although some patients complain of itching in the affected area.
For more information, see “Scalp papules in a teenage boy.” J Fam Pract. 2017 March;66(3).
4. Several years after a motorcycle accident and resulting road rash, this 23-year-old Hispanic woman is left with complex scars. She experiences pruritus, pain, and hypersensitivity and is seeking relief.

Diagnosis: Often confused with hypertrophic scars, keloids are benign overgrowths of scar tissue that can occur months to years after skin trauma. They are most common in those ages 10 to 30, with a higher incidence among blacks, Hispanics, and Asians. Although the exact etiology of keloids is unknown, they are related to aberrant collagen production and breakdown in wound healing.
For more information, see “Laser treatment of scars and keloids.” Cosmet Dermatol. 2012;25:318-325.
1. This patient is concerned about the numerous long-standing “moles” on her face. Only occasionally pruritic, they are otherwise asymptomatic. Nevertheless, the patient wants them investigated and removed.

Diagnosis: Dermatosis papulosa nigra (DPN) is a benign condition that presents as multiple brown to dark-brown 1- to 5-mm papules on the face, neck, and trunk. The lesions are a sign of aging in darker skinned patients and do not require treatment. They can, however, be safely, easily, and effectively removed. Both electrodesiccation and KTP (532 nm) laser have comparable efficacy in the removal of DPN, according to a 2009 study published in the American Journal of Dermatologic Surgery. Without use of anesthetics, the KTP laser is preferred for patient comfort.
For more information, see “Skin of Color: Dermatosis Papulosa Nigra Removal.” Dermatology News. February 1, 2012.
2. A 17-year-old African-American boy likes to keep his face clean-shaven, but his skin becomes irritated every time he shaves. He states that his father also has this problem, but doesn’t have a solution.

Diagnosis: Pseudofolliculitis is a common skin condition affecting hair-bearing areas of the body that are shaved. It develops when the free end of a tightly coiled hair reenters the skin after shaving, causing a foreign-body–like inflammatory reaction. Tightly curled hair has a greater tendency to pierce the follicle and the surface of the skin, explaining the relative predominance of pseudofolliculitis in patients of African descent; at least half of black men who shave develop the condition.
For more information, see “Bumps in beard area.” J Fam Pract. 2015 November;64(11).
3. A 15-year-old African-American boy presents with a two-month history of hair loss and pruritic papules on the back of his head that developed after a barber shaved the area. There are two dozen 1- to 2-mm papules on his posterior neck and occipital scalp with areas of focal crusting. The patient had a similar episode a year ago after shaving the same area, but those papules cleared after one month of applying rubbing alcohol.

Diagnosis: This patient’s diagnosis is acne keloidalis nuchae (AKN), a chronic folliculitis characterized by smooth, dome-shaped papules on the posterior scalp and neck that become confluent and form firm papules and hairless, keloid-like plaques. Seen almost exclusively in young, postpubescent African-American males, the condition is often asymptomatic, although some patients complain of itching in the affected area.
For more information, see “Scalp papules in a teenage boy.” J Fam Pract. 2017 March;66(3).
4. Several years after a motorcycle accident and resulting road rash, this 23-year-old Hispanic woman is left with complex scars. She experiences pruritus, pain, and hypersensitivity and is seeking relief.

Diagnosis: Often confused with hypertrophic scars, keloids are benign overgrowths of scar tissue that can occur months to years after skin trauma. They are most common in those ages 10 to 30, with a higher incidence among blacks, Hispanics, and Asians. Although the exact etiology of keloids is unknown, they are related to aberrant collagen production and breakdown in wound healing.
For more information, see “Laser treatment of scars and keloids.” Cosmet Dermatol. 2012;25:318-325.
1. This patient is concerned about the numerous long-standing “moles” on her face. Only occasionally pruritic, they are otherwise asymptomatic. Nevertheless, the patient wants them investigated and removed.

Diagnosis: Dermatosis papulosa nigra (DPN) is a benign condition that presents as multiple brown to dark-brown 1- to 5-mm papules on the face, neck, and trunk. The lesions are a sign of aging in darker skinned patients and do not require treatment. They can, however, be safely, easily, and effectively removed. Both electrodesiccation and KTP (532 nm) laser have comparable efficacy in the removal of DPN, according to a 2009 study published in the American Journal of Dermatologic Surgery. Without use of anesthetics, the KTP laser is preferred for patient comfort.
For more information, see “Skin of Color: Dermatosis Papulosa Nigra Removal.” Dermatology News. February 1, 2012.
2. A 17-year-old African-American boy likes to keep his face clean-shaven, but his skin becomes irritated every time he shaves. He states that his father also has this problem, but doesn’t have a solution.

Diagnosis: Pseudofolliculitis is a common skin condition affecting hair-bearing areas of the body that are shaved. It develops when the free end of a tightly coiled hair reenters the skin after shaving, causing a foreign-body–like inflammatory reaction. Tightly curled hair has a greater tendency to pierce the follicle and the surface of the skin, explaining the relative predominance of pseudofolliculitis in patients of African descent; at least half of black men who shave develop the condition.
For more information, see “Bumps in beard area.” J Fam Pract. 2015 November;64(11).
3. A 15-year-old African-American boy presents with a two-month history of hair loss and pruritic papules on the back of his head that developed after a barber shaved the area. There are two dozen 1- to 2-mm papules on his posterior neck and occipital scalp with areas of focal crusting. The patient had a similar episode a year ago after shaving the same area, but those papules cleared after one month of applying rubbing alcohol.

Diagnosis: This patient’s diagnosis is acne keloidalis nuchae (AKN), a chronic folliculitis characterized by smooth, dome-shaped papules on the posterior scalp and neck that become confluent and form firm papules and hairless, keloid-like plaques. Seen almost exclusively in young, postpubescent African-American males, the condition is often asymptomatic, although some patients complain of itching in the affected area.
For more information, see “Scalp papules in a teenage boy.” J Fam Pract. 2017 March;66(3).
4. Several years after a motorcycle accident and resulting road rash, this 23-year-old Hispanic woman is left with complex scars. She experiences pruritus, pain, and hypersensitivity and is seeking relief.

Diagnosis: Often confused with hypertrophic scars, keloids are benign overgrowths of scar tissue that can occur months to years after skin trauma. They are most common in those ages 10 to 30, with a higher incidence among blacks, Hispanics, and Asians. Although the exact etiology of keloids is unknown, they are related to aberrant collagen production and breakdown in wound healing.
For more information, see “Laser treatment of scars and keloids.” Cosmet Dermatol. 2012;25:318-325.
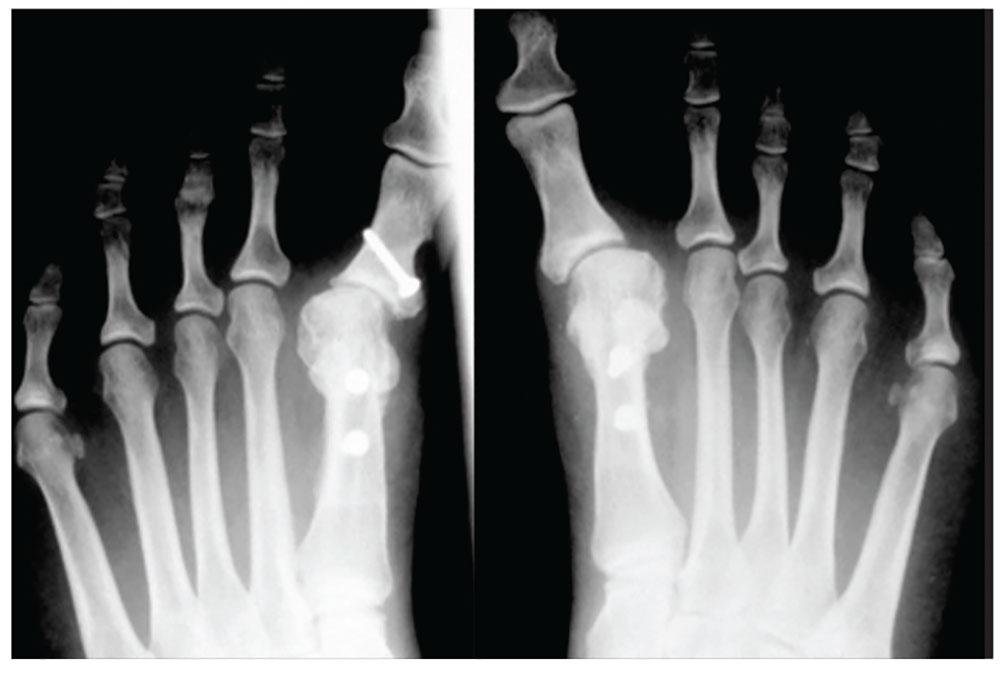
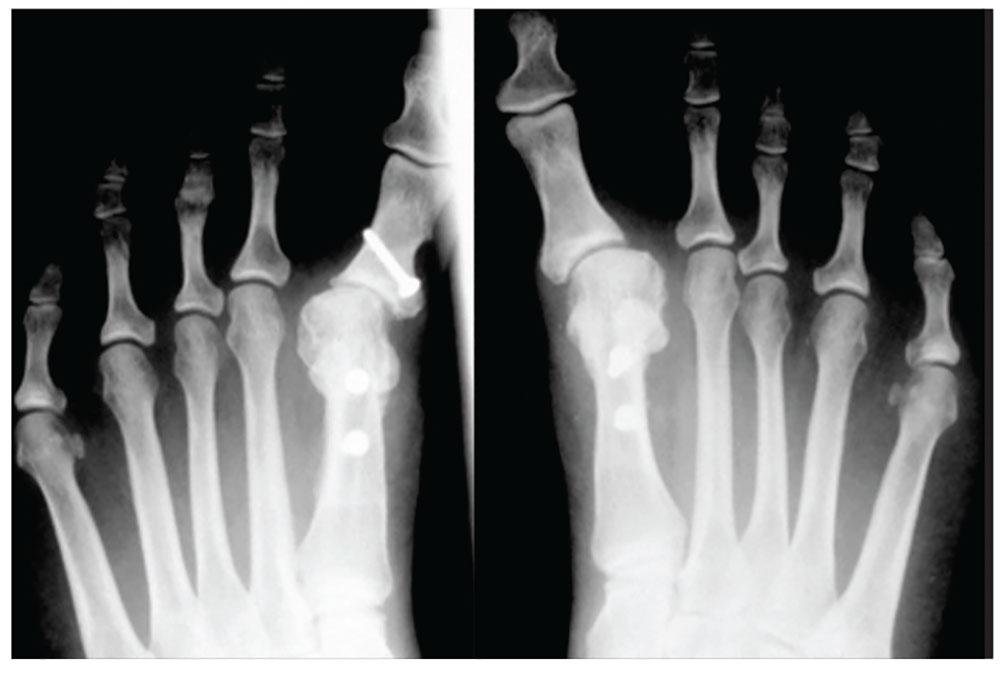
Troublesome Foreign Bodies
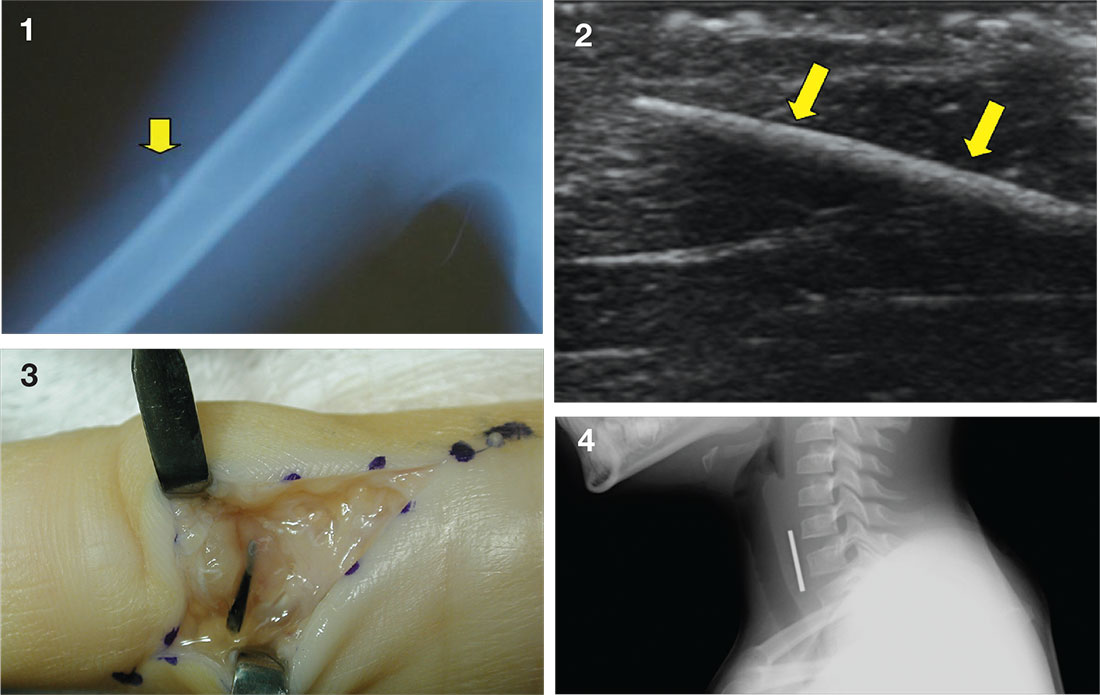
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
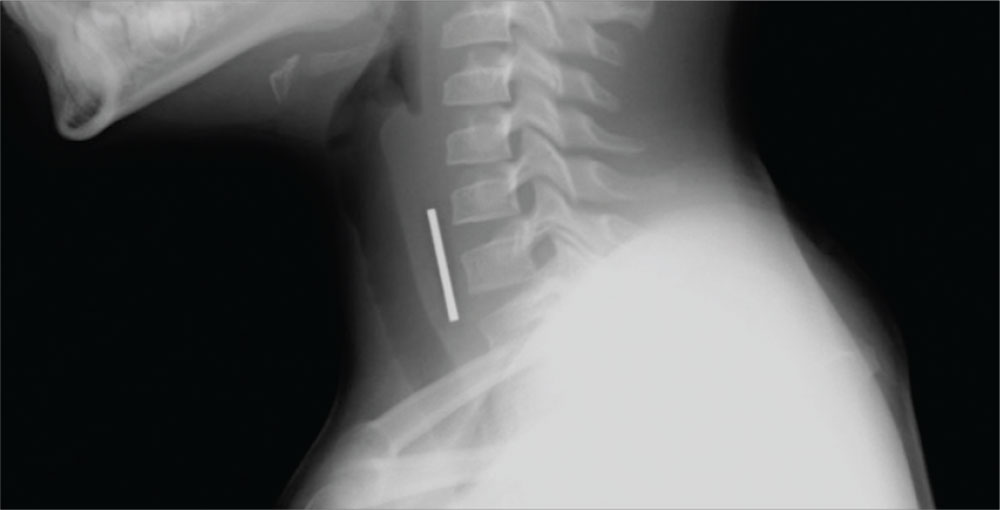
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Complete obstruction should be treated with back blows in a child aged less than 1 year and abdominal thrusts in an older child. In a more stable child, provide supplemental oxygen and consult a physician skilled in laryngoscopy and bronchoscopy for removal of the foreign body. Esophageal foreign bodies may also cause stridor. In these cases the child will often complain of dysphagia or avoid swallowing.
While some objects, such as coins, can be visualized on plain imaging, a negative film does not rule out a foreign body and a specialist should be consulted for endoscopy. A coin in the trachea will be seen on its edge in an anteroposterior view. In the esophagus, it will generally appear as a full circle (en face) in an anteroposterior oblique view. For the lateral view, it is just the opposite, as seen in the case figure.
For more information, see “Differential Diagnosis of Stridor in Children.” Emergency Medicine. 2009 September;41(9):10-11.
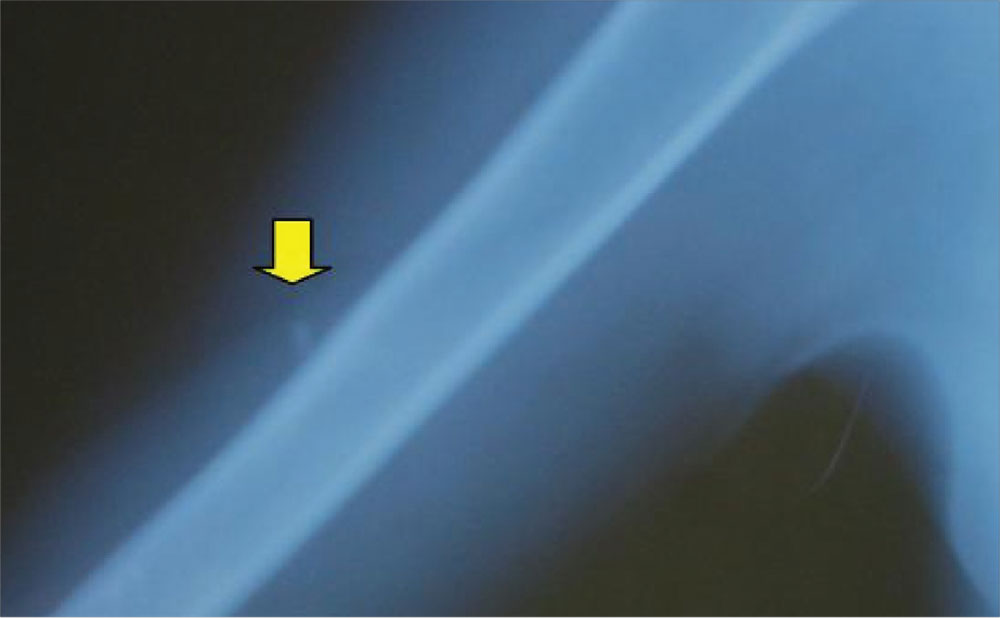
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
You anesthetize the area and begin dissection in an attempt to locate the glass fragment, which goes on for 20 minutes without success. The child and her mother are becoming anxious. You call for the portable ultrasound system, and using its high-frequency transducer, quickly locate the foreign body. After additional anesthesia is applied, the splinter is easily removed under ultrasound guidance and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
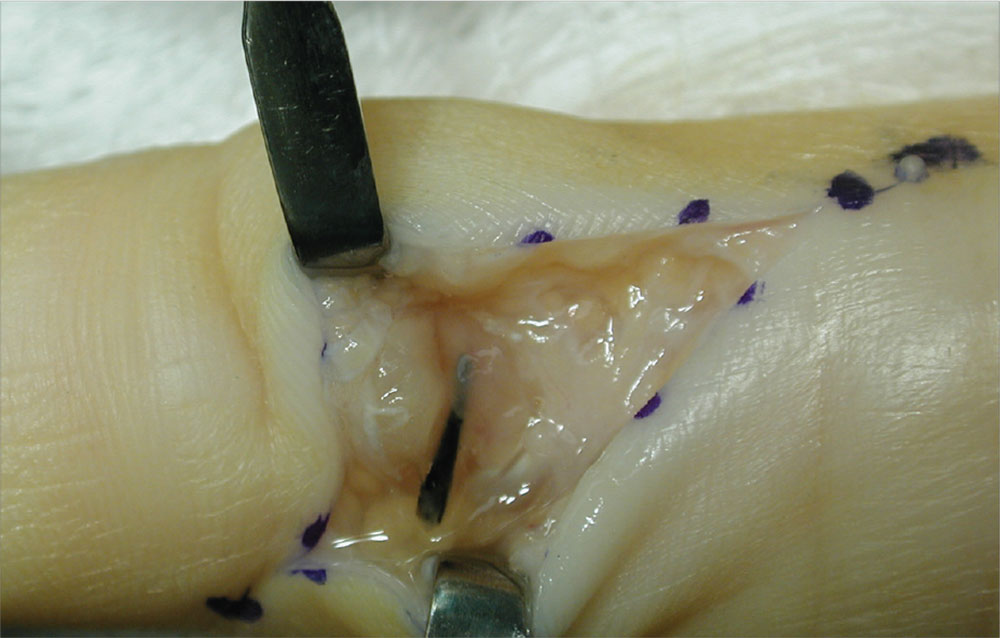
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
The palmar puncture wound site was surgically explored, and no foreign body fragments were found. In addition, the tendons, retracted and delivered through the skin incision, appeared normal.
Histopathology of a specimen intraoperatively biopsied from the flexor tendon sheath showed some refractile foreign material consistent with plant material. After surgery, swelling persisted, and the patient developed limited motion at the extremes of active flexion and extension.
After 2 months, the decision was made to re-explore the palmar puncture site and flexor tendon and obtain tissue specimens for culture, including atypical mycobacterial and fungal cultures. During the second surgery, the palmar site and flexor tendon still appeared unremarkable. As there was some swelling in the long finger, the flexor tendon sheath was explored distally through a separate incision over the middle phalanx. A transversely oriented fragment of the sago palm thorn was found within the flexor tendon sheath. Flexor tendon sheath material was cultured and subsequently found to be negative.
For more information, see “Distal Migration of a Foreign Body (Sago Palm Thorn Fragment) Within the Long-Finger Flexor Tendon Sheath.” Am J Orthop. 2008;37(4):208-209.
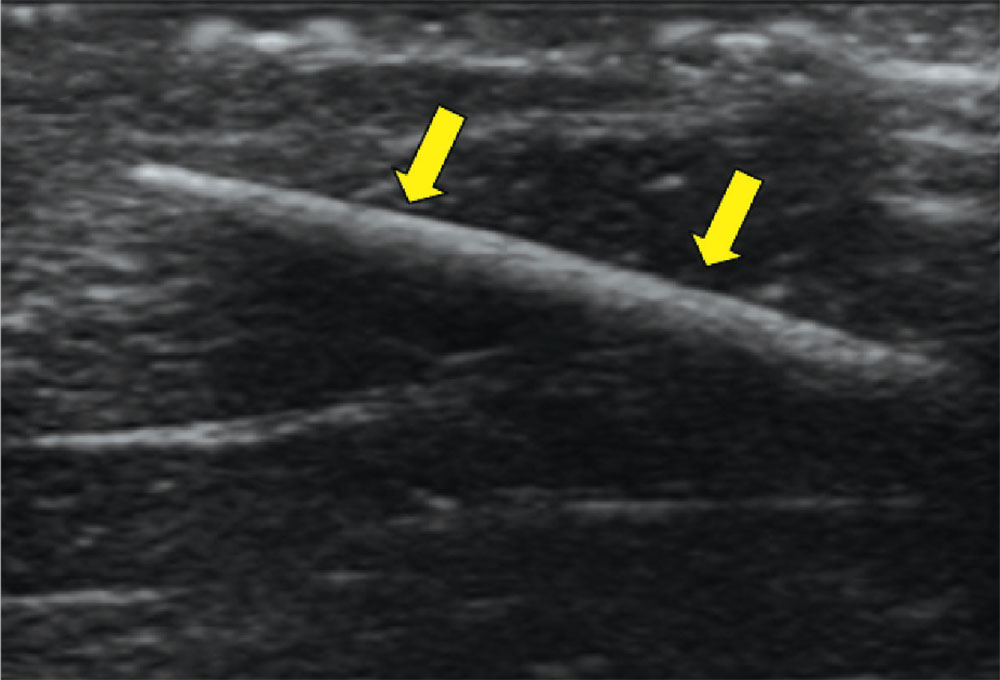
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
With local anesthesia and ultrasound guidance, the splinter is easily removed and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
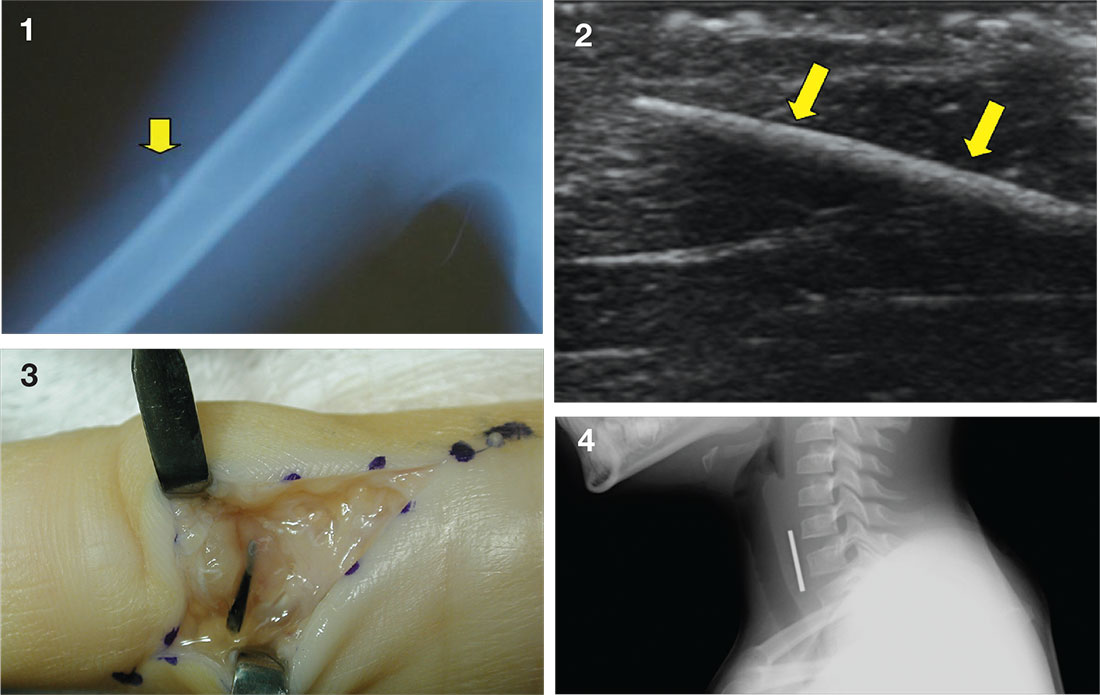
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
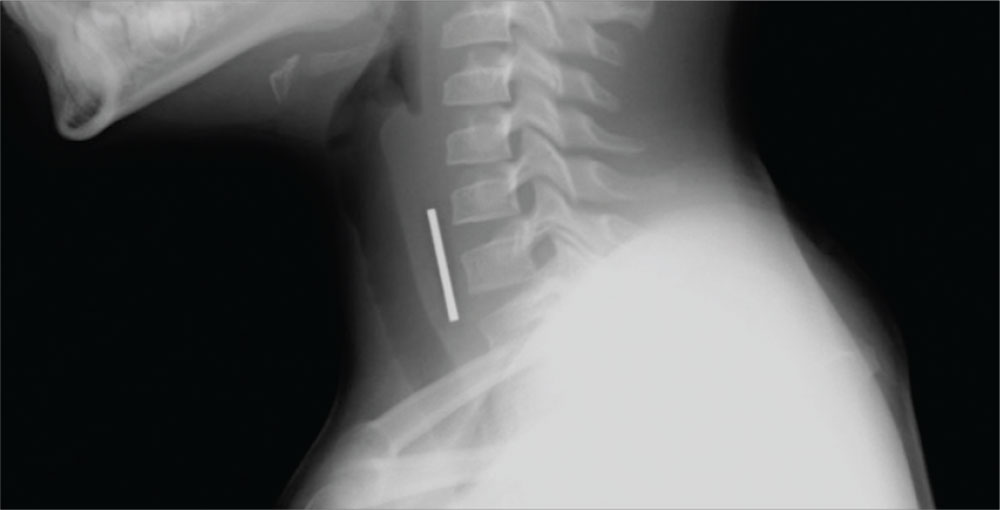
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Complete obstruction should be treated with back blows in a child aged less than 1 year and abdominal thrusts in an older child. In a more stable child, provide supplemental oxygen and consult a physician skilled in laryngoscopy and bronchoscopy for removal of the foreign body. Esophageal foreign bodies may also cause stridor. In these cases the child will often complain of dysphagia or avoid swallowing.
While some objects, such as coins, can be visualized on plain imaging, a negative film does not rule out a foreign body and a specialist should be consulted for endoscopy. A coin in the trachea will be seen on its edge in an anteroposterior view. In the esophagus, it will generally appear as a full circle (en face) in an anteroposterior oblique view. For the lateral view, it is just the opposite, as seen in the case figure.
For more information, see “Differential Diagnosis of Stridor in Children.” Emergency Medicine. 2009 September;41(9):10-11.
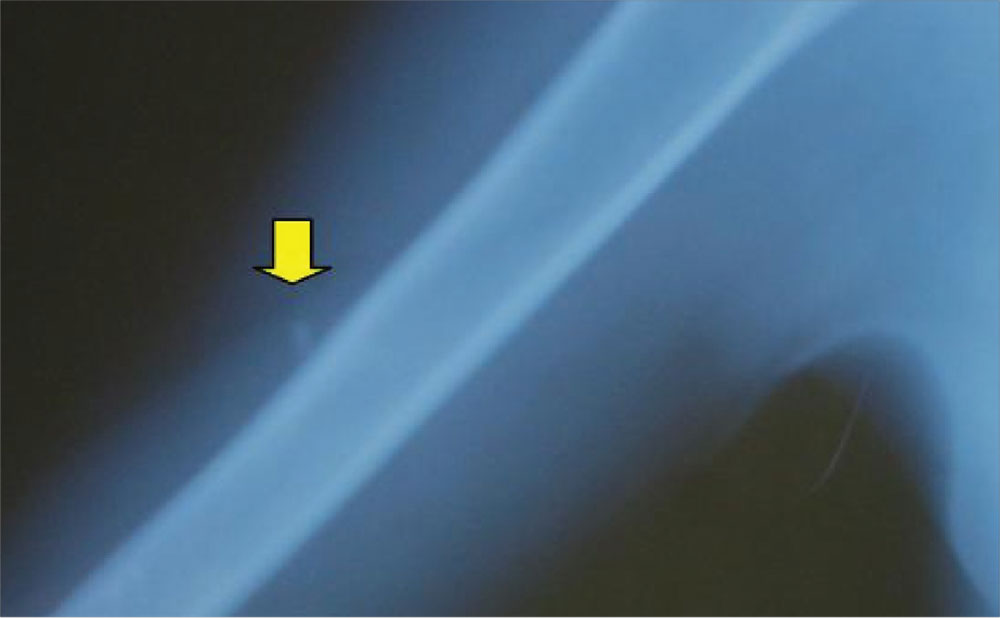
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
You anesthetize the area and begin dissection in an attempt to locate the glass fragment, which goes on for 20 minutes without success. The child and her mother are becoming anxious. You call for the portable ultrasound system, and using its high-frequency transducer, quickly locate the foreign body. After additional anesthesia is applied, the splinter is easily removed under ultrasound guidance and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
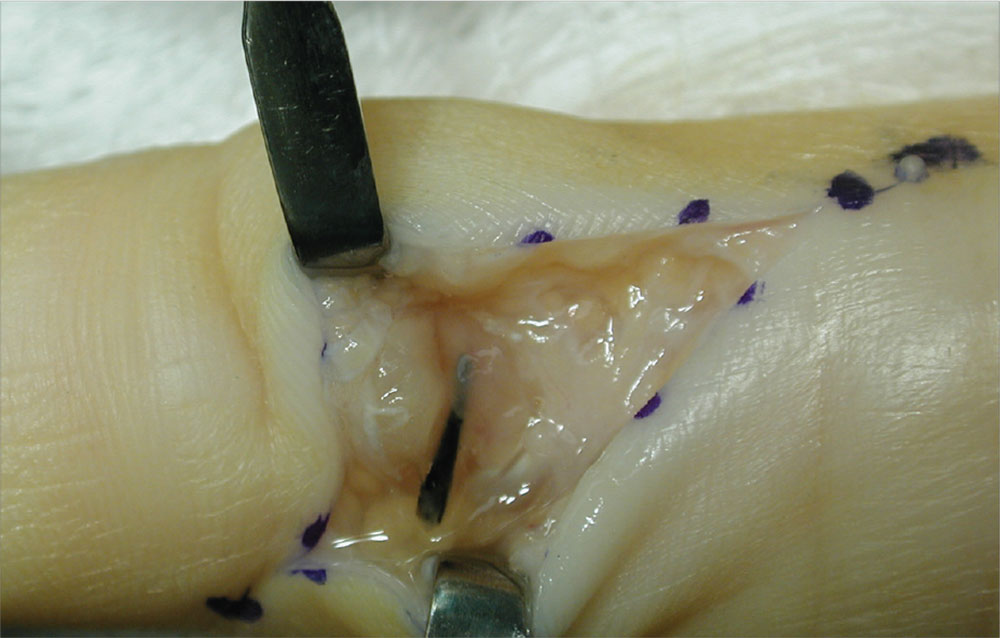
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
The palmar puncture wound site was surgically explored, and no foreign body fragments were found. In addition, the tendons, retracted and delivered through the skin incision, appeared normal.
Histopathology of a specimen intraoperatively biopsied from the flexor tendon sheath showed some refractile foreign material consistent with plant material. After surgery, swelling persisted, and the patient developed limited motion at the extremes of active flexion and extension.
After 2 months, the decision was made to re-explore the palmar puncture site and flexor tendon and obtain tissue specimens for culture, including atypical mycobacterial and fungal cultures. During the second surgery, the palmar site and flexor tendon still appeared unremarkable. As there was some swelling in the long finger, the flexor tendon sheath was explored distally through a separate incision over the middle phalanx. A transversely oriented fragment of the sago palm thorn was found within the flexor tendon sheath. Flexor tendon sheath material was cultured and subsequently found to be negative.
For more information, see “Distal Migration of a Foreign Body (Sago Palm Thorn Fragment) Within the Long-Finger Flexor Tendon Sheath.” Am J Orthop. 2008;37(4):208-209.
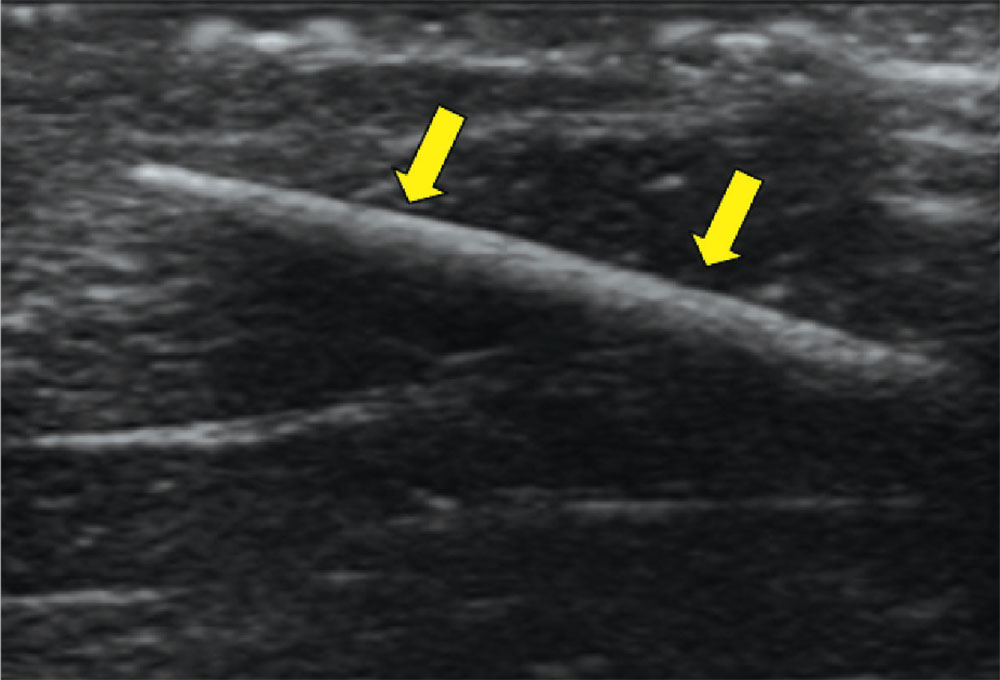
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
With local anesthesia and ultrasound guidance, the splinter is easily removed and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
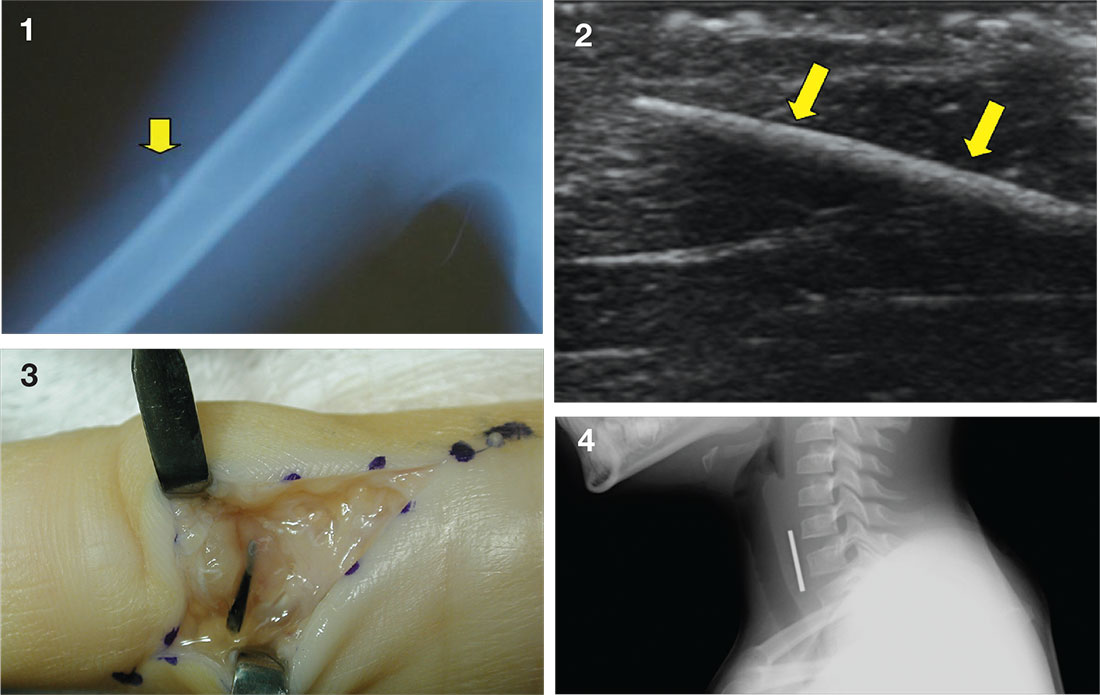
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
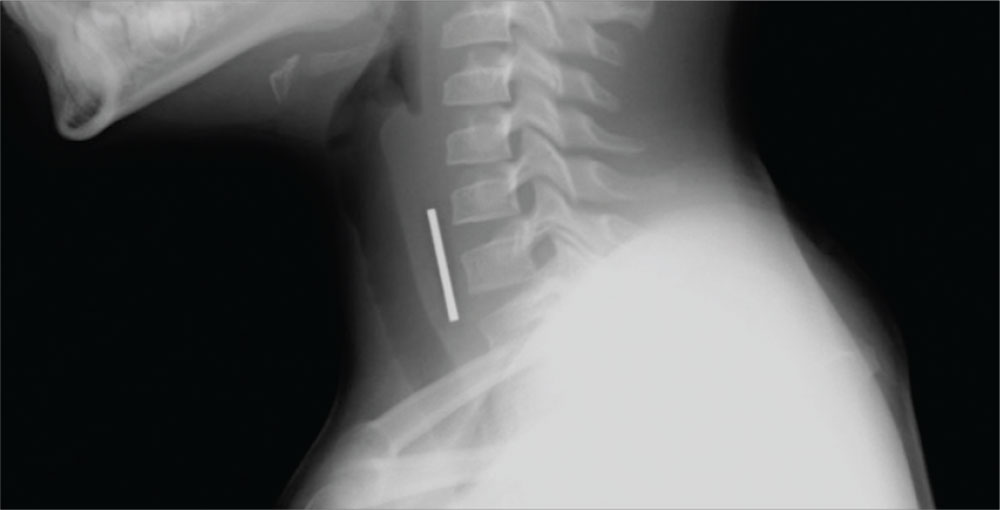
Case a. A 30-month-old boy, who is in obvious distress with a barking cough and croup-like symptoms but no fever, is brought by his mother for examination. History is unremarkable except for a recent choking episode. A radiograph is ordered.
Complete obstruction should be treated with back blows in a child aged less than 1 year and abdominal thrusts in an older child. In a more stable child, provide supplemental oxygen and consult a physician skilled in laryngoscopy and bronchoscopy for removal of the foreign body. Esophageal foreign bodies may also cause stridor. In these cases the child will often complain of dysphagia or avoid swallowing.
While some objects, such as coins, can be visualized on plain imaging, a negative film does not rule out a foreign body and a specialist should be consulted for endoscopy. A coin in the trachea will be seen on its edge in an anteroposterior view. In the esophagus, it will generally appear as a full circle (en face) in an anteroposterior oblique view. For the lateral view, it is just the opposite, as seen in the case figure.
For more information, see “Differential Diagnosis of Stridor in Children.” Emergency Medicine. 2009 September;41(9):10-11.
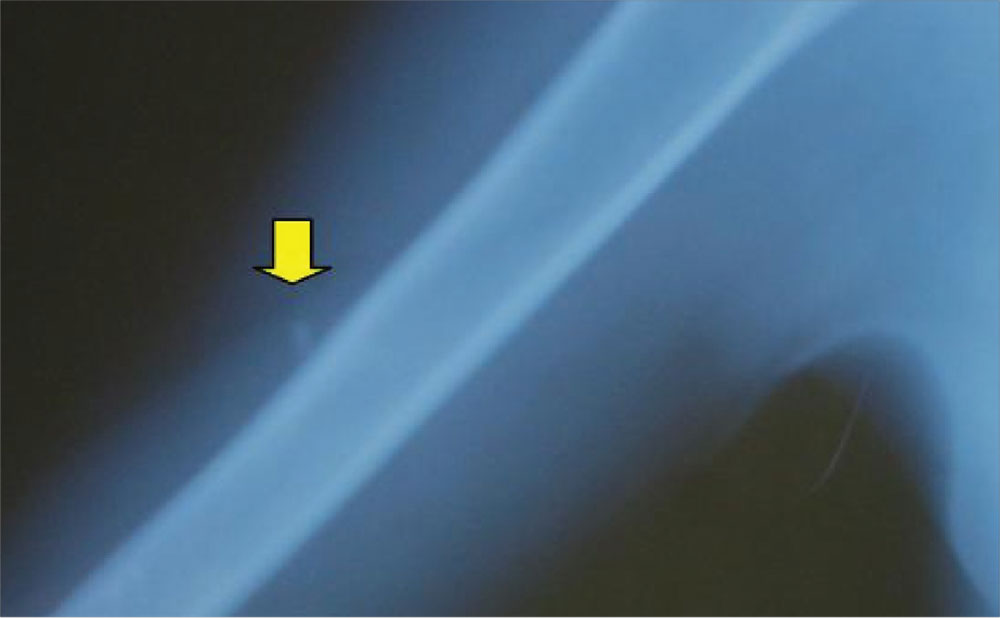
Case b. A 13-year-old girl presents to urgent care with a laceration that occurred when she fell through a glass door. You note a 2-cm linear laceration, and radiography shows what appears to be a residual piece of glass at or near the site of the laceration.
You anesthetize the area and begin dissection in an attempt to locate the glass fragment, which goes on for 20 minutes without success. The child and her mother are becoming anxious. You call for the portable ultrasound system, and using its high-frequency transducer, quickly locate the foreign body. After additional anesthesia is applied, the splinter is easily removed under ultrasound guidance and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
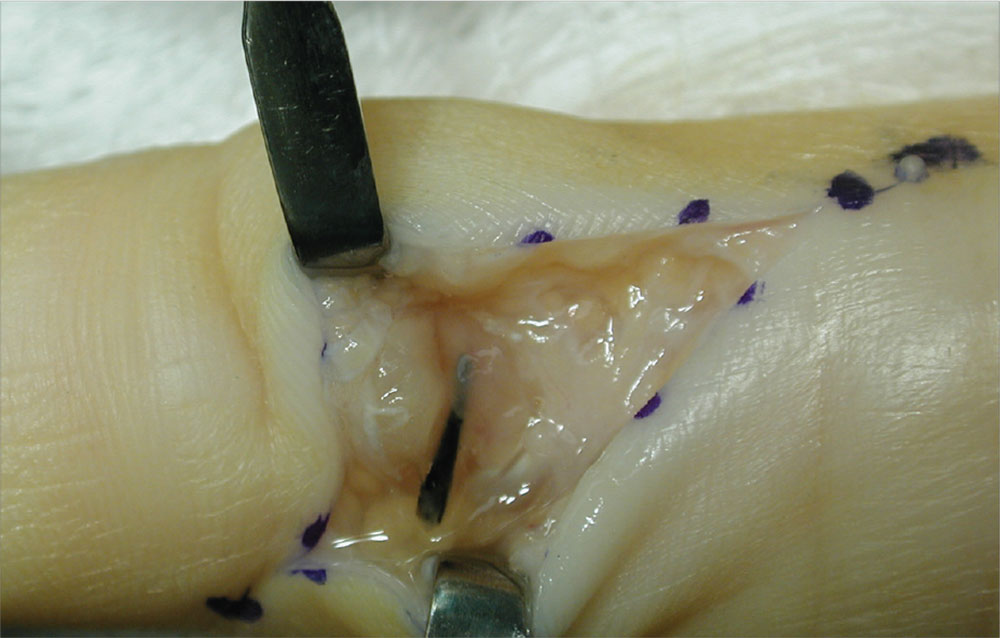
Case c. This patient was punctured by a sago palm thorn, but believes that she removed the entire thorn at the time of injury. A small puncture wound is seen on physical exam, and x-rays are unremarkable. The patient is placed on a 10-day course of oral cephalexin. At follow-up, she has swelling in an adjacent finger.
The palmar puncture wound site was surgically explored, and no foreign body fragments were found. In addition, the tendons, retracted and delivered through the skin incision, appeared normal.
Histopathology of a specimen intraoperatively biopsied from the flexor tendon sheath showed some refractile foreign material consistent with plant material. After surgery, swelling persisted, and the patient developed limited motion at the extremes of active flexion and extension.
After 2 months, the decision was made to re-explore the palmar puncture site and flexor tendon and obtain tissue specimens for culture, including atypical mycobacterial and fungal cultures. During the second surgery, the palmar site and flexor tendon still appeared unremarkable. As there was some swelling in the long finger, the flexor tendon sheath was explored distally through a separate incision over the middle phalanx. A transversely oriented fragment of the sago palm thorn was found within the flexor tendon sheath. Flexor tendon sheath material was cultured and subsequently found to be negative.
For more information, see “Distal Migration of a Foreign Body (Sago Palm Thorn Fragment) Within the Long-Finger Flexor Tendon Sheath.” Am J Orthop. 2008;37(4):208-209.
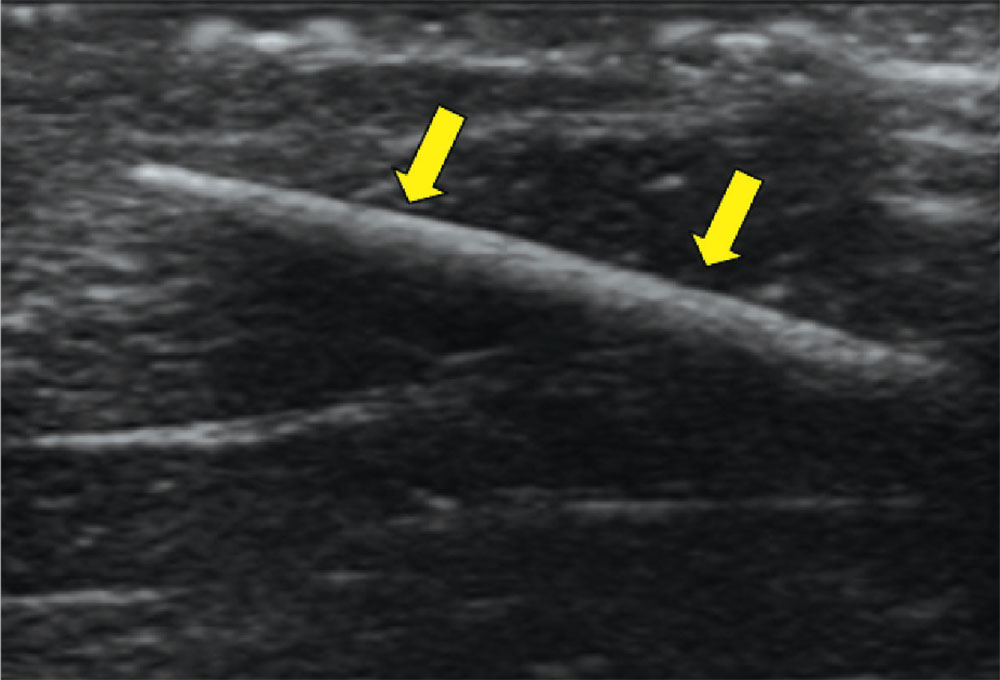
Case d. A 2-year-old boy complains of pain after stepping on a toothpick. His father suspects that part of the toothpick remains embedded. Examination reveals a plantar puncture wound but no sign of a foreign body. Radiography shows no deformity. An ultrasound is ordered and reveals a toothpick segment.
With local anesthesia and ultrasound guidance, the splinter is easily removed and the patient is discharged.
For more information, see “Capturing Elusive Foreign Bodies With Ultrasound.” Emergency Medicine. 2009 June;41(6):36-42.
Clinical Comestibles?
1. This 45-year-old woman’s skin has multiple small, soft, compressible papules, one of which is apt to bleed when scratched. She is concerned that these “cherry red” lesions are precancerous.

Diagnosis: Cherry angiomas, also known as de Morgan spots, are extremely common lesions; though usually asymptomatic, they may bleed with trauma. They occur most commonly as multiple asymptomatic lesions on the trunk and arms. These capillary hemangiomas are dome-shaped, small (0.1 to 0.5 cm in diameter), and bright red to violaceous; they can be flat, raised, or nodular.
Cherry angiomas form as a result of the development of multiple capillaries with narrow lumens and prominent endothelial cells arranged in a lobular pattern in the papillary dermis. Effective treatment options include curettage, laser ablation, and electrodesiccation.
For more information, see Kim, J-H, Park H-Y, Ahn SK. Cherry Angiomas on the Scalp. Case Rep Dermatol. 2009;1(1):82–86.
2. A 60-year-old African-American woman presents with painful swelling of two years’ duration. She delayed care due to lack of insurance. The patient is hypertensive, and her left breast and nipple are retracted, with darkened skin and a peau d’orange texture.

Diagnosis: Palpation of the firm, matted nodes in the left axilla elucidated the diagnosis of breast cancer with lymphedema. Lymphedema causes the skin of the breast to resemble that of an orange.
The patient was referred to the local university’s breast center. Although the prognosis was poor, it was important to make every effort to have the disease staged to determine the most appropriate therapy.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux, EJ. Breast cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:551-556.
For more information, see “Swollen breast and arm.” The Journal of Family Practice. February 6, 2015.
3. This patient presents with her cheeks quite red and covered with hyperkeratotic, rough, pinpoint papules. No other blemishes or lesions are seen on her face, but there are hundreds of hyperkeratotic papules on her bilateral triceps, giving a “chicken skin” appearance.

Diagnosis: Keratosis pilaris (KP) is an extremely common and harmless problem that affects up to 70% of newborns, though it may not fully express until age 1 or 2. Caused by an overproduction of perifollicular keratin, KP is inherited in an autosomal dominant pattern and is often seen in conjunction with atopic dermatitis and related conditions (eg, eczema, xerosis, asthma, icthyosis). KP can manifest anywhere on the body except glabrous skin (palms and soles).
Variants of KP are also common; the one affecting this patient is keratosis pilaris rubra facei. This condition is often confused with acne, but treating it as such worsens irritation—especially in the wintertime, when humidity levels are low.
For more information, see “Acne: Maybe She's Born With It?” Clinician Reviews. 2016 July;26(7):W1.
4. A 5-year-old girl has a fever of 102.4°F and “strawberry tongue.” The posterior pharynx is erythematous with slight exudate visible. The anterior cervical lymph nodes are mildly tender and somewhat enlarged. No rashes are noted.

Diagnosis: The child’s strawberry tongue and scarlet fever were caused by strep pharyngitis. Strawberry tongue, identified by prominent papillae along with erythema (resembling a strawberry), is most commonly seen in children with scarlet fever or Kawasaki disease and usually develops within the first two to three days of illness. A white or yellowish coating typically precedes the distinctive red tongue with white papillae.
In this case, oral penicillin VK was prescribed, along with ibuprofen for the fever and sore throat. Improvement was noted within 24 hours, but the full 10-day course of pencillin was completed to prevent rheumatic fever.
For more information, see “Papillae on tongue.” Journal of Family Practice. January 24, 2014.
1. This 45-year-old woman’s skin has multiple small, soft, compressible papules, one of which is apt to bleed when scratched. She is concerned that these “cherry red” lesions are precancerous.

Diagnosis: Cherry angiomas, also known as de Morgan spots, are extremely common lesions; though usually asymptomatic, they may bleed with trauma. They occur most commonly as multiple asymptomatic lesions on the trunk and arms. These capillary hemangiomas are dome-shaped, small (0.1 to 0.5 cm in diameter), and bright red to violaceous; they can be flat, raised, or nodular.
Cherry angiomas form as a result of the development of multiple capillaries with narrow lumens and prominent endothelial cells arranged in a lobular pattern in the papillary dermis. Effective treatment options include curettage, laser ablation, and electrodesiccation.
For more information, see Kim, J-H, Park H-Y, Ahn SK. Cherry Angiomas on the Scalp. Case Rep Dermatol. 2009;1(1):82–86.
2. A 60-year-old African-American woman presents with painful swelling of two years’ duration. She delayed care due to lack of insurance. The patient is hypertensive, and her left breast and nipple are retracted, with darkened skin and a peau d’orange texture.

Diagnosis: Palpation of the firm, matted nodes in the left axilla elucidated the diagnosis of breast cancer with lymphedema. Lymphedema causes the skin of the breast to resemble that of an orange.
The patient was referred to the local university’s breast center. Although the prognosis was poor, it was important to make every effort to have the disease staged to determine the most appropriate therapy.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux, EJ. Breast cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:551-556.
For more information, see “Swollen breast and arm.” The Journal of Family Practice. February 6, 2015.
3. This patient presents with her cheeks quite red and covered with hyperkeratotic, rough, pinpoint papules. No other blemishes or lesions are seen on her face, but there are hundreds of hyperkeratotic papules on her bilateral triceps, giving a “chicken skin” appearance.

Diagnosis: Keratosis pilaris (KP) is an extremely common and harmless problem that affects up to 70% of newborns, though it may not fully express until age 1 or 2. Caused by an overproduction of perifollicular keratin, KP is inherited in an autosomal dominant pattern and is often seen in conjunction with atopic dermatitis and related conditions (eg, eczema, xerosis, asthma, icthyosis). KP can manifest anywhere on the body except glabrous skin (palms and soles).
Variants of KP are also common; the one affecting this patient is keratosis pilaris rubra facei. This condition is often confused with acne, but treating it as such worsens irritation—especially in the wintertime, when humidity levels are low.
For more information, see “Acne: Maybe She's Born With It?” Clinician Reviews. 2016 July;26(7):W1.
4. A 5-year-old girl has a fever of 102.4°F and “strawberry tongue.” The posterior pharynx is erythematous with slight exudate visible. The anterior cervical lymph nodes are mildly tender and somewhat enlarged. No rashes are noted.

Diagnosis: The child’s strawberry tongue and scarlet fever were caused by strep pharyngitis. Strawberry tongue, identified by prominent papillae along with erythema (resembling a strawberry), is most commonly seen in children with scarlet fever or Kawasaki disease and usually develops within the first two to three days of illness. A white or yellowish coating typically precedes the distinctive red tongue with white papillae.
In this case, oral penicillin VK was prescribed, along with ibuprofen for the fever and sore throat. Improvement was noted within 24 hours, but the full 10-day course of pencillin was completed to prevent rheumatic fever.
For more information, see “Papillae on tongue.” Journal of Family Practice. January 24, 2014.
1. This 45-year-old woman’s skin has multiple small, soft, compressible papules, one of which is apt to bleed when scratched. She is concerned that these “cherry red” lesions are precancerous.

Diagnosis: Cherry angiomas, also known as de Morgan spots, are extremely common lesions; though usually asymptomatic, they may bleed with trauma. They occur most commonly as multiple asymptomatic lesions on the trunk and arms. These capillary hemangiomas are dome-shaped, small (0.1 to 0.5 cm in diameter), and bright red to violaceous; they can be flat, raised, or nodular.
Cherry angiomas form as a result of the development of multiple capillaries with narrow lumens and prominent endothelial cells arranged in a lobular pattern in the papillary dermis. Effective treatment options include curettage, laser ablation, and electrodesiccation.
For more information, see Kim, J-H, Park H-Y, Ahn SK. Cherry Angiomas on the Scalp. Case Rep Dermatol. 2009;1(1):82–86.
2. A 60-year-old African-American woman presents with painful swelling of two years’ duration. She delayed care due to lack of insurance. The patient is hypertensive, and her left breast and nipple are retracted, with darkened skin and a peau d’orange texture.

Diagnosis: Palpation of the firm, matted nodes in the left axilla elucidated the diagnosis of breast cancer with lymphedema. Lymphedema causes the skin of the breast to resemble that of an orange.
The patient was referred to the local university’s breast center. Although the prognosis was poor, it was important to make every effort to have the disease staged to determine the most appropriate therapy.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux, EJ. Breast cancer. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:551-556.
For more information, see “Swollen breast and arm.” The Journal of Family Practice. February 6, 2015.
3. This patient presents with her cheeks quite red and covered with hyperkeratotic, rough, pinpoint papules. No other blemishes or lesions are seen on her face, but there are hundreds of hyperkeratotic papules on her bilateral triceps, giving a “chicken skin” appearance.

Diagnosis: Keratosis pilaris (KP) is an extremely common and harmless problem that affects up to 70% of newborns, though it may not fully express until age 1 or 2. Caused by an overproduction of perifollicular keratin, KP is inherited in an autosomal dominant pattern and is often seen in conjunction with atopic dermatitis and related conditions (eg, eczema, xerosis, asthma, icthyosis). KP can manifest anywhere on the body except glabrous skin (palms and soles).
Variants of KP are also common; the one affecting this patient is keratosis pilaris rubra facei. This condition is often confused with acne, but treating it as such worsens irritation—especially in the wintertime, when humidity levels are low.
For more information, see “Acne: Maybe She's Born With It?” Clinician Reviews. 2016 July;26(7):W1.
4. A 5-year-old girl has a fever of 102.4°F and “strawberry tongue.” The posterior pharynx is erythematous with slight exudate visible. The anterior cervical lymph nodes are mildly tender and somewhat enlarged. No rashes are noted.

Diagnosis: The child’s strawberry tongue and scarlet fever were caused by strep pharyngitis. Strawberry tongue, identified by prominent papillae along with erythema (resembling a strawberry), is most commonly seen in children with scarlet fever or Kawasaki disease and usually develops within the first two to three days of illness. A white or yellowish coating typically precedes the distinctive red tongue with white papillae.
In this case, oral penicillin VK was prescribed, along with ibuprofen for the fever and sore throat. Improvement was noted within 24 hours, but the full 10-day course of pencillin was completed to prevent rheumatic fever.
For more information, see “Papillae on tongue.” Journal of Family Practice. January 24, 2014.
Infectious Penile Lesions
1. A 63-year-old man complains of a mildly painful and tender rash on his penis that has been there for almost two years. The patient is uncircumcised; when the foreskin is retracted, a bright red, erythematous, nonscaly, circumferential plaque is visible on the glans penis, spreading to the foreskin. He denies pain on urination, discharge, fever, malaise, arthralgias, and sexual contact outside of his marriage.

Diagnosis: Zoon balanitis is a benign condition that typically affects uncircumcised middle-aged to elderly men.1,2 Worldwide prevalence among uncircumcised men is approximately 3%.2 The etiology is unknown; it’s thought that this condition may be caused by friction, trauma, heat, lack of hygiene, exogenous or infectious agents, an IgE hypersensitivity, or a chronic infection with Mycobacterium smegmatis.1,2
Typically, the appearance of the lesion precedes diagnosis by about one to 2 years.1 The patient usually complains of mild pruritus and tenderness. Undergarments may be bloodstained.
The lesion associated with Zoon balanitis is a solitary, glistening, shiny, red-to-orange plaque of the glans penis or prepuce of an uncircumcised male. Pinpoint erythematous spots or “cayenne pepper spots” may also be associated with this condition.
For more information on this case, see “Erythematous penile lesion.” J Fam Pract. 2012;61(12):753-755.
2. A 21-year-old man presents with bumps on his penis. He admits to having unprotected sexual intercourse with more than six women in the past year. He is otherwise healthy.

Diagnosis: Genital warts are caused by human papillomavirus infection. The incubation period after exposure ranges from three weeks to eight months. Anogenital warts represent the most common viral sexually transmitted infection in the United States; there are approximately 1 million new cases of genital warts per year. Most infections are transient and clear up within two years, but some infections persist and recur.
The diagnosis is usually clinical; genital warts are typically asymptomatic and present as flesh-colored, exophytic lesions on the genitalia, including the penis, vulva, vagina, scrotum, perineum, and perianal skin. External warts can appear as small bumps, or they may be flat, verrucous, or pedunculated. Treatment options include cryotherapy and prescription imiquimod cream.
For more information on this case, see “Genital bumps.”
3. A 27-year-old man is worried that he may have contracted chlamydia. About five days ago, he experienced pain and a burning feeling with urination. Three days ago, a painful, growing lump near the head of his penis developed. The patient has a purulent urethral discharge and fluctuant, yellowish white, tender swelling on the left side of the frenulum. There are no ulcers, but there is a single 2-cm lymph node in the right inguinal area that is of normal consistency, mobile, nontender, and nonfluctuant.

Diagnosis: The clinical history was consistent with a diagnosis of gonococcal urethritis complicated by a periurethral gland abscess. The location of the swelling was most consistent with an abscess in the Tyson’s gland (also known as tysonitis). The Tyson’s (or preputial) glands of the penis are sebaceous-type glands on either side of the frenulum at the balanopreputial sulcus.1 In women, an abscess of the periurethral Skene’s gland is an analogous gonorrheal complication.
The differential diagnosis of acute swelling on the penile shaft includes syphilis, chancroid, lymphogranuloma venereum, herpes simplex virus, Behçet’s syndrome, a drug reaction, erythema multiforme, Crohn’s disease, lichen planus, amebiasis, scabies, trauma, and cancer.
For more information on this case, see “Returning traveler with painful penile mass.” J Fam Pract. 2011 May;60(5):285-287.
4. A 32-year-old man presents with a week-long history of painful vesicles on the shaft of his penis associated with tender groin adenopathy. Two days ago, the vesicles broke and the pain worsened. The patient had similar lesions a year ago but did not seek medical care. He has had three different female sexual partners over the past two years but has no knowledge of them having any sores or diseases.

Diagnosis: Genital herpes presents with multiple transient, painful vesicles that appear on the penis, vulva, buttocks, perineum, vagina, or cervix. The vesicles break down and become ulcers that develop crusts while healing. Recurrences typically occur 2 to 3 times a year. The duration is shorter and less painful than in primary infections. The lesions often heal completely by 8 to 10 days.
Antiviral therapy is recommended for an initial genital herpes outbreak. Although systemic antiviral drugs can partially control the signs and symptoms of herpes episodes, they do not eradicate the latent virus.
For more information on this case, see “Painful vesicles on penis.”
1. A 63-year-old man complains of a mildly painful and tender rash on his penis that has been there for almost two years. The patient is uncircumcised; when the foreskin is retracted, a bright red, erythematous, nonscaly, circumferential plaque is visible on the glans penis, spreading to the foreskin. He denies pain on urination, discharge, fever, malaise, arthralgias, and sexual contact outside of his marriage.

Diagnosis: Zoon balanitis is a benign condition that typically affects uncircumcised middle-aged to elderly men.1,2 Worldwide prevalence among uncircumcised men is approximately 3%.2 The etiology is unknown; it’s thought that this condition may be caused by friction, trauma, heat, lack of hygiene, exogenous or infectious agents, an IgE hypersensitivity, or a chronic infection with Mycobacterium smegmatis.1,2
Typically, the appearance of the lesion precedes diagnosis by about one to 2 years.1 The patient usually complains of mild pruritus and tenderness. Undergarments may be bloodstained.
The lesion associated with Zoon balanitis is a solitary, glistening, shiny, red-to-orange plaque of the glans penis or prepuce of an uncircumcised male. Pinpoint erythematous spots or “cayenne pepper spots” may also be associated with this condition.
For more information on this case, see “Erythematous penile lesion.” J Fam Pract. 2012;61(12):753-755.
2. A 21-year-old man presents with bumps on his penis. He admits to having unprotected sexual intercourse with more than six women in the past year. He is otherwise healthy.

Diagnosis: Genital warts are caused by human papillomavirus infection. The incubation period after exposure ranges from three weeks to eight months. Anogenital warts represent the most common viral sexually transmitted infection in the United States; there are approximately 1 million new cases of genital warts per year. Most infections are transient and clear up within two years, but some infections persist and recur.
The diagnosis is usually clinical; genital warts are typically asymptomatic and present as flesh-colored, exophytic lesions on the genitalia, including the penis, vulva, vagina, scrotum, perineum, and perianal skin. External warts can appear as small bumps, or they may be flat, verrucous, or pedunculated. Treatment options include cryotherapy and prescription imiquimod cream.
For more information on this case, see “Genital bumps.”
3. A 27-year-old man is worried that he may have contracted chlamydia. About five days ago, he experienced pain and a burning feeling with urination. Three days ago, a painful, growing lump near the head of his penis developed. The patient has a purulent urethral discharge and fluctuant, yellowish white, tender swelling on the left side of the frenulum. There are no ulcers, but there is a single 2-cm lymph node in the right inguinal area that is of normal consistency, mobile, nontender, and nonfluctuant.

Diagnosis: The clinical history was consistent with a diagnosis of gonococcal urethritis complicated by a periurethral gland abscess. The location of the swelling was most consistent with an abscess in the Tyson’s gland (also known as tysonitis). The Tyson’s (or preputial) glands of the penis are sebaceous-type glands on either side of the frenulum at the balanopreputial sulcus.1 In women, an abscess of the periurethral Skene’s gland is an analogous gonorrheal complication.
The differential diagnosis of acute swelling on the penile shaft includes syphilis, chancroid, lymphogranuloma venereum, herpes simplex virus, Behçet’s syndrome, a drug reaction, erythema multiforme, Crohn’s disease, lichen planus, amebiasis, scabies, trauma, and cancer.
For more information on this case, see “Returning traveler with painful penile mass.” J Fam Pract. 2011 May;60(5):285-287.
4. A 32-year-old man presents with a week-long history of painful vesicles on the shaft of his penis associated with tender groin adenopathy. Two days ago, the vesicles broke and the pain worsened. The patient had similar lesions a year ago but did not seek medical care. He has had three different female sexual partners over the past two years but has no knowledge of them having any sores or diseases.

Diagnosis: Genital herpes presents with multiple transient, painful vesicles that appear on the penis, vulva, buttocks, perineum, vagina, or cervix. The vesicles break down and become ulcers that develop crusts while healing. Recurrences typically occur 2 to 3 times a year. The duration is shorter and less painful than in primary infections. The lesions often heal completely by 8 to 10 days.
Antiviral therapy is recommended for an initial genital herpes outbreak. Although systemic antiviral drugs can partially control the signs and symptoms of herpes episodes, they do not eradicate the latent virus.
For more information on this case, see “Painful vesicles on penis.”
1. A 63-year-old man complains of a mildly painful and tender rash on his penis that has been there for almost two years. The patient is uncircumcised; when the foreskin is retracted, a bright red, erythematous, nonscaly, circumferential plaque is visible on the glans penis, spreading to the foreskin. He denies pain on urination, discharge, fever, malaise, arthralgias, and sexual contact outside of his marriage.

Diagnosis: Zoon balanitis is a benign condition that typically affects uncircumcised middle-aged to elderly men.1,2 Worldwide prevalence among uncircumcised men is approximately 3%.2 The etiology is unknown; it’s thought that this condition may be caused by friction, trauma, heat, lack of hygiene, exogenous or infectious agents, an IgE hypersensitivity, or a chronic infection with Mycobacterium smegmatis.1,2
Typically, the appearance of the lesion precedes diagnosis by about one to 2 years.1 The patient usually complains of mild pruritus and tenderness. Undergarments may be bloodstained.
The lesion associated with Zoon balanitis is a solitary, glistening, shiny, red-to-orange plaque of the glans penis or prepuce of an uncircumcised male. Pinpoint erythematous spots or “cayenne pepper spots” may also be associated with this condition.
For more information on this case, see “Erythematous penile lesion.” J Fam Pract. 2012;61(12):753-755.
2. A 21-year-old man presents with bumps on his penis. He admits to having unprotected sexual intercourse with more than six women in the past year. He is otherwise healthy.

Diagnosis: Genital warts are caused by human papillomavirus infection. The incubation period after exposure ranges from three weeks to eight months. Anogenital warts represent the most common viral sexually transmitted infection in the United States; there are approximately 1 million new cases of genital warts per year. Most infections are transient and clear up within two years, but some infections persist and recur.
The diagnosis is usually clinical; genital warts are typically asymptomatic and present as flesh-colored, exophytic lesions on the genitalia, including the penis, vulva, vagina, scrotum, perineum, and perianal skin. External warts can appear as small bumps, or they may be flat, verrucous, or pedunculated. Treatment options include cryotherapy and prescription imiquimod cream.
For more information on this case, see “Genital bumps.”
3. A 27-year-old man is worried that he may have contracted chlamydia. About five days ago, he experienced pain and a burning feeling with urination. Three days ago, a painful, growing lump near the head of his penis developed. The patient has a purulent urethral discharge and fluctuant, yellowish white, tender swelling on the left side of the frenulum. There are no ulcers, but there is a single 2-cm lymph node in the right inguinal area that is of normal consistency, mobile, nontender, and nonfluctuant.

Diagnosis: The clinical history was consistent with a diagnosis of gonococcal urethritis complicated by a periurethral gland abscess. The location of the swelling was most consistent with an abscess in the Tyson’s gland (also known as tysonitis). The Tyson’s (or preputial) glands of the penis are sebaceous-type glands on either side of the frenulum at the balanopreputial sulcus.1 In women, an abscess of the periurethral Skene’s gland is an analogous gonorrheal complication.
The differential diagnosis of acute swelling on the penile shaft includes syphilis, chancroid, lymphogranuloma venereum, herpes simplex virus, Behçet’s syndrome, a drug reaction, erythema multiforme, Crohn’s disease, lichen planus, amebiasis, scabies, trauma, and cancer.
For more information on this case, see “Returning traveler with painful penile mass.” J Fam Pract. 2011 May;60(5):285-287.
4. A 32-year-old man presents with a week-long history of painful vesicles on the shaft of his penis associated with tender groin adenopathy. Two days ago, the vesicles broke and the pain worsened. The patient had similar lesions a year ago but did not seek medical care. He has had three different female sexual partners over the past two years but has no knowledge of them having any sores or diseases.

Diagnosis: Genital herpes presents with multiple transient, painful vesicles that appear on the penis, vulva, buttocks, perineum, vagina, or cervix. The vesicles break down and become ulcers that develop crusts while healing. Recurrences typically occur 2 to 3 times a year. The duration is shorter and less painful than in primary infections. The lesions often heal completely by 8 to 10 days.
Antiviral therapy is recommended for an initial genital herpes outbreak. Although systemic antiviral drugs can partially control the signs and symptoms of herpes episodes, they do not eradicate the latent virus.
For more information on this case, see “Painful vesicles on penis.”



