User login
Keratosis pilaris (KP), also known as lichen planopilaris, is a common inherited disorder characterized by the presence of small folliculocentric keratotic papules that may have surrounding erythema, which gives the skin a stippled appearance resembling gooseflesh.1 Keratosis pilaris has a predilection for the extensor surfaces of the upper arms, thighs, and buttocks; however, a generalized presentation may occur.1-3 Patients usually are asymptomatic with concerns regarding cosmetic appearance. A number of diseases are associated with KP, such as KP atrophicans, erythromelanosis follicularis faciei et colli, and ichthyosis vulgaris. Treatment of KP mainly focuses on avoiding skin dryness and adding keratolytic agents when necessary.1 We report the case of a 29-year-old woman who presented with unilateral generalized KP in the second month of her second pregnancy.
Case Report
A 29-year-old woman presented in the second month of pregnancy with follicular hyperkeratotic papules on the right side of the face, neck, trunk, buttocks, arms, and legs with mild pruritus (Figure 1). According to the patient, when she found out she was pregnant, she discovered several reddish gray papules on the right cheek and dorsal aspect of the right hand that rapidly spread to the neck and trunk but remained restricted to the right side of the body. She occasionally experienced mild pruritus.

| 
|

| 
|
Figure 1. Several reddish gray follicular papules formed red patches on the right side of the face (A). Numerous small hyperpigmented follicular papules were scattered on the right side of the neck; the left side was devoid of lesions, revealing a sharp distinct demarcation line between the involved and uninvolved skin (B). Reddish gray or pigmented lesions were distributed on the hands and thighs but were restricted to the right side (C and D). | |
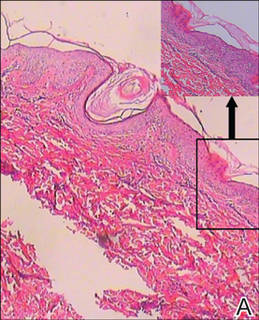
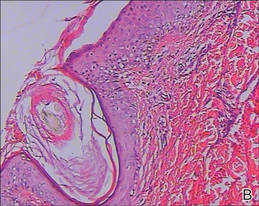
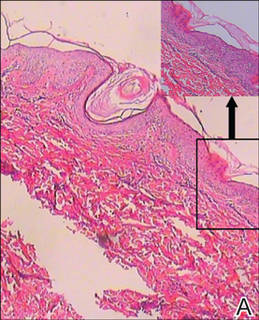
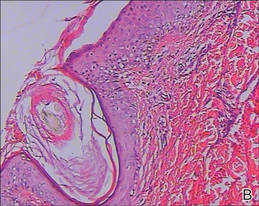
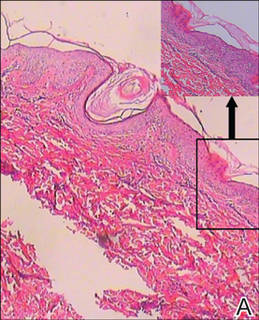
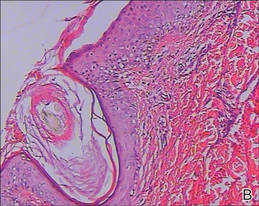
Physical examination revealed numerous small reddish or hyperpigmented follicular papules scattered on the right side of the body, both in the flexor and extensor aspects. The distribution of the lesions did not follow the lines of Blaschko. Strangely, the left side was devoid of lesions, and a sharp distinct line of demarcation separated the involved and uninvolved sides. Physical examination of the scalp, hair, nails, and oral cavity was normal with no atrophy or scarring. The patient’s first pregnancy was aborted in the third month of pregnancy (14 months prior to presentation), but no skin lesions were reported at that time. The patient’s medical history was otherwise unremarkable, and there was no known family history of similar skin lesions. Histopathologic examination of a biopsy taken from a lesion on the right side of the neck showed hyperpigmentation of the basal layer, follicular and interfollicular hyperkeratosis, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration (Figure 2).
Based on the clinical and pathologic findings, a diagnosis of unilateral generalized KP was made. No treatment was administered due to the pregnancy. The patient’s skin condition continued to worsen throughout her pregnancy with more widespread and hyperpigmented lesions, but they remained unilateral. The patient showed no obvious improvement 4 months following delivery, and no treatment was administered because the patient was breastfeeding.
|
|
| Figure 2. Histopathologic examination revealed hyperpigmentation of the basal layer, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration, which suggested typical keratosis pilaris (A and B)(H&E, original magnifications ×40 [inset, original magnification ×100] and ×100). |
Comment
Keratosis pilaris is a common hyperkeratotic condition that typically presents as flesh-colored follicular papules surrounded by varying degrees of perifollicular erythema. Occasionally, inflammatory acneform pustules and papules may appear.1,2 Keratosis pilaris usually presents between the ages of 2 and 3 years, flourishes until 20 years of age, and usually subsides in adulthood.4 Xerotic or atopic individuals are prone to develop KP.2 Other conditions associated with KP include ichthyosis follicularis, atrichia with papular lesions, cardiofasciocutaneous syndrome, ectodermal dysplasia with corkscrew hairs, and keratitis-ichthyosis-deafness syndrome.5 Although its etiology is uncertain, KP is thought to be inherited in an autosomal-dominant fashion.
Histologically, the lesions result from the formation of an orthokeratotic plug, which may contain twisted hairs, that blocks and dilates the orifice and upper portion of the follicular infundibulum. Mild perivascular mononuclear cell infiltrates usually are present in the adjacent dermis.5 Most cases of KP involve lesions that are bilaterally distributed. One report described a 5-year-old girl with lesions that were limited to the right cheek. They were diagnosed as atrophoderma vermiculata, a form of KP atrophicans, which is a less common variant of KP.6 Another report described a 2-year-old girl who developed KP 7 months after birth, which was the only case we found in the English-language literature, according to a PubMed search of articles indexed for MEDLINE using the search terms keratosis pilaris, hemicorporal, and pregnancy, with near-total involvement of one side of the body. The authors believed this peculiar manifestation was probably caused by an inherited segmental anomaly from a postzygotic genetic mutation.7
Our patient’s condition was unusual because the generalized lesions were unilaterally distributed and they occurred early in the pregnancy. Some studies have indicated that hormonal influences may play a role in the development of KP.3,8 Our case also demonstrates KP as a condition in which the onset and severity of the disorder may be associated with the hormonal changes in pregnancy. Additionally, it is worth noting that the lesions presented during the patient’s second pregnancy, but there were no lesions reported during her first pregnancy 14 months prior, which was aborted in the third month. We cannot explain this phenomenon and cannot predict if the lesions will recur in future pregnancies.
Conclusion
We suggest that both a genetic mutation and pregnancy-induced hormonal changes played possible roles in the development and progress of unilateral generalized KP in our patient. Follow-up is necessary in these patients and further work needs to be done to reveal the underlying mechanism.
1. Hwang S, Schwartz RA. Keratosis pilaris: a common follicular hyperkeratosis. Cutis. 2008;82:177-180.
2. Odom RB, James WD, Berger TG. Andrews’ Diseases of the Skin. 9th ed. Philadelphia, PA: WB Saunders; 2000.
3. Jackson JB, Touma SC, Norton AB. Keratosis pilaris in pregnancy: an unrecognized dematosis of pregnancy? W V Med J. 2004;100:26-28.
4. Poskitt L, Wilkinson JD. Natural history of keratosis pilaris. Br J Dermatol. 1994;130:711-713.
5. Griffiths WAD, Judge MR, Leigh IM. Disorders of keratinisation. In: Champion RH, Burton JL, Burns DA, et al, eds. Textbook of Dermatology. 6th ed. Oxford, MA: Blackwell Scientific; 1998.
6. Nico MM, Valente NY, Sotto MN. Folliculitis ulerythematosa reticulata (atrophoderma vermiculata): early detection of a case with unilateral lesions. Pediatr Dermatol. 1998;15:285-286.
7. Ehsani A, Namazi MR, Barikbin B, et al. Unilaterally generalized keratosis pilaris. J Eur Acad Dermatol Venereol. 2003;17:361-362.
8. Barth JH, Wojnarowska F, Dawber RP. Is keratosis pilaris another androgen-dependent dermatosis? Clin Exp Dermatol. 1988;13:240-241.
Keratosis pilaris (KP), also known as lichen planopilaris, is a common inherited disorder characterized by the presence of small folliculocentric keratotic papules that may have surrounding erythema, which gives the skin a stippled appearance resembling gooseflesh.1 Keratosis pilaris has a predilection for the extensor surfaces of the upper arms, thighs, and buttocks; however, a generalized presentation may occur.1-3 Patients usually are asymptomatic with concerns regarding cosmetic appearance. A number of diseases are associated with KP, such as KP atrophicans, erythromelanosis follicularis faciei et colli, and ichthyosis vulgaris. Treatment of KP mainly focuses on avoiding skin dryness and adding keratolytic agents when necessary.1 We report the case of a 29-year-old woman who presented with unilateral generalized KP in the second month of her second pregnancy.
Case Report
A 29-year-old woman presented in the second month of pregnancy with follicular hyperkeratotic papules on the right side of the face, neck, trunk, buttocks, arms, and legs with mild pruritus (Figure 1). According to the patient, when she found out she was pregnant, she discovered several reddish gray papules on the right cheek and dorsal aspect of the right hand that rapidly spread to the neck and trunk but remained restricted to the right side of the body. She occasionally experienced mild pruritus.

| 
|

| 
|
Figure 1. Several reddish gray follicular papules formed red patches on the right side of the face (A). Numerous small hyperpigmented follicular papules were scattered on the right side of the neck; the left side was devoid of lesions, revealing a sharp distinct demarcation line between the involved and uninvolved skin (B). Reddish gray or pigmented lesions were distributed on the hands and thighs but were restricted to the right side (C and D). | |
Physical examination revealed numerous small reddish or hyperpigmented follicular papules scattered on the right side of the body, both in the flexor and extensor aspects. The distribution of the lesions did not follow the lines of Blaschko. Strangely, the left side was devoid of lesions, and a sharp distinct line of demarcation separated the involved and uninvolved sides. Physical examination of the scalp, hair, nails, and oral cavity was normal with no atrophy or scarring. The patient’s first pregnancy was aborted in the third month of pregnancy (14 months prior to presentation), but no skin lesions were reported at that time. The patient’s medical history was otherwise unremarkable, and there was no known family history of similar skin lesions. Histopathologic examination of a biopsy taken from a lesion on the right side of the neck showed hyperpigmentation of the basal layer, follicular and interfollicular hyperkeratosis, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration (Figure 2).
Based on the clinical and pathologic findings, a diagnosis of unilateral generalized KP was made. No treatment was administered due to the pregnancy. The patient’s skin condition continued to worsen throughout her pregnancy with more widespread and hyperpigmented lesions, but they remained unilateral. The patient showed no obvious improvement 4 months following delivery, and no treatment was administered because the patient was breastfeeding.
|
|
| Figure 2. Histopathologic examination revealed hyperpigmentation of the basal layer, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration, which suggested typical keratosis pilaris (A and B)(H&E, original magnifications ×40 [inset, original magnification ×100] and ×100). |
Comment
Keratosis pilaris is a common hyperkeratotic condition that typically presents as flesh-colored follicular papules surrounded by varying degrees of perifollicular erythema. Occasionally, inflammatory acneform pustules and papules may appear.1,2 Keratosis pilaris usually presents between the ages of 2 and 3 years, flourishes until 20 years of age, and usually subsides in adulthood.4 Xerotic or atopic individuals are prone to develop KP.2 Other conditions associated with KP include ichthyosis follicularis, atrichia with papular lesions, cardiofasciocutaneous syndrome, ectodermal dysplasia with corkscrew hairs, and keratitis-ichthyosis-deafness syndrome.5 Although its etiology is uncertain, KP is thought to be inherited in an autosomal-dominant fashion.
Histologically, the lesions result from the formation of an orthokeratotic plug, which may contain twisted hairs, that blocks and dilates the orifice and upper portion of the follicular infundibulum. Mild perivascular mononuclear cell infiltrates usually are present in the adjacent dermis.5 Most cases of KP involve lesions that are bilaterally distributed. One report described a 5-year-old girl with lesions that were limited to the right cheek. They were diagnosed as atrophoderma vermiculata, a form of KP atrophicans, which is a less common variant of KP.6 Another report described a 2-year-old girl who developed KP 7 months after birth, which was the only case we found in the English-language literature, according to a PubMed search of articles indexed for MEDLINE using the search terms keratosis pilaris, hemicorporal, and pregnancy, with near-total involvement of one side of the body. The authors believed this peculiar manifestation was probably caused by an inherited segmental anomaly from a postzygotic genetic mutation.7
Our patient’s condition was unusual because the generalized lesions were unilaterally distributed and they occurred early in the pregnancy. Some studies have indicated that hormonal influences may play a role in the development of KP.3,8 Our case also demonstrates KP as a condition in which the onset and severity of the disorder may be associated with the hormonal changes in pregnancy. Additionally, it is worth noting that the lesions presented during the patient’s second pregnancy, but there were no lesions reported during her first pregnancy 14 months prior, which was aborted in the third month. We cannot explain this phenomenon and cannot predict if the lesions will recur in future pregnancies.
Conclusion
We suggest that both a genetic mutation and pregnancy-induced hormonal changes played possible roles in the development and progress of unilateral generalized KP in our patient. Follow-up is necessary in these patients and further work needs to be done to reveal the underlying mechanism.
Keratosis pilaris (KP), also known as lichen planopilaris, is a common inherited disorder characterized by the presence of small folliculocentric keratotic papules that may have surrounding erythema, which gives the skin a stippled appearance resembling gooseflesh.1 Keratosis pilaris has a predilection for the extensor surfaces of the upper arms, thighs, and buttocks; however, a generalized presentation may occur.1-3 Patients usually are asymptomatic with concerns regarding cosmetic appearance. A number of diseases are associated with KP, such as KP atrophicans, erythromelanosis follicularis faciei et colli, and ichthyosis vulgaris. Treatment of KP mainly focuses on avoiding skin dryness and adding keratolytic agents when necessary.1 We report the case of a 29-year-old woman who presented with unilateral generalized KP in the second month of her second pregnancy.
Case Report
A 29-year-old woman presented in the second month of pregnancy with follicular hyperkeratotic papules on the right side of the face, neck, trunk, buttocks, arms, and legs with mild pruritus (Figure 1). According to the patient, when she found out she was pregnant, she discovered several reddish gray papules on the right cheek and dorsal aspect of the right hand that rapidly spread to the neck and trunk but remained restricted to the right side of the body. She occasionally experienced mild pruritus.

| 
|

| 
|
Figure 1. Several reddish gray follicular papules formed red patches on the right side of the face (A). Numerous small hyperpigmented follicular papules were scattered on the right side of the neck; the left side was devoid of lesions, revealing a sharp distinct demarcation line between the involved and uninvolved skin (B). Reddish gray or pigmented lesions were distributed on the hands and thighs but were restricted to the right side (C and D). | |
Physical examination revealed numerous small reddish or hyperpigmented follicular papules scattered on the right side of the body, both in the flexor and extensor aspects. The distribution of the lesions did not follow the lines of Blaschko. Strangely, the left side was devoid of lesions, and a sharp distinct line of demarcation separated the involved and uninvolved sides. Physical examination of the scalp, hair, nails, and oral cavity was normal with no atrophy or scarring. The patient’s first pregnancy was aborted in the third month of pregnancy (14 months prior to presentation), but no skin lesions were reported at that time. The patient’s medical history was otherwise unremarkable, and there was no known family history of similar skin lesions. Histopathologic examination of a biopsy taken from a lesion on the right side of the neck showed hyperpigmentation of the basal layer, follicular and interfollicular hyperkeratosis, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration (Figure 2).
Based on the clinical and pathologic findings, a diagnosis of unilateral generalized KP was made. No treatment was administered due to the pregnancy. The patient’s skin condition continued to worsen throughout her pregnancy with more widespread and hyperpigmented lesions, but they remained unilateral. The patient showed no obvious improvement 4 months following delivery, and no treatment was administered because the patient was breastfeeding.
|
|
| Figure 2. Histopathologic examination revealed hyperpigmentation of the basal layer, dilated hair follicles containing keratinous plugs, dermal vascular dilatation and congestion, and mild perivascular inflammatory infiltration, which suggested typical keratosis pilaris (A and B)(H&E, original magnifications ×40 [inset, original magnification ×100] and ×100). |
Comment
Keratosis pilaris is a common hyperkeratotic condition that typically presents as flesh-colored follicular papules surrounded by varying degrees of perifollicular erythema. Occasionally, inflammatory acneform pustules and papules may appear.1,2 Keratosis pilaris usually presents between the ages of 2 and 3 years, flourishes until 20 years of age, and usually subsides in adulthood.4 Xerotic or atopic individuals are prone to develop KP.2 Other conditions associated with KP include ichthyosis follicularis, atrichia with papular lesions, cardiofasciocutaneous syndrome, ectodermal dysplasia with corkscrew hairs, and keratitis-ichthyosis-deafness syndrome.5 Although its etiology is uncertain, KP is thought to be inherited in an autosomal-dominant fashion.
Histologically, the lesions result from the formation of an orthokeratotic plug, which may contain twisted hairs, that blocks and dilates the orifice and upper portion of the follicular infundibulum. Mild perivascular mononuclear cell infiltrates usually are present in the adjacent dermis.5 Most cases of KP involve lesions that are bilaterally distributed. One report described a 5-year-old girl with lesions that were limited to the right cheek. They were diagnosed as atrophoderma vermiculata, a form of KP atrophicans, which is a less common variant of KP.6 Another report described a 2-year-old girl who developed KP 7 months after birth, which was the only case we found in the English-language literature, according to a PubMed search of articles indexed for MEDLINE using the search terms keratosis pilaris, hemicorporal, and pregnancy, with near-total involvement of one side of the body. The authors believed this peculiar manifestation was probably caused by an inherited segmental anomaly from a postzygotic genetic mutation.7
Our patient’s condition was unusual because the generalized lesions were unilaterally distributed and they occurred early in the pregnancy. Some studies have indicated that hormonal influences may play a role in the development of KP.3,8 Our case also demonstrates KP as a condition in which the onset and severity of the disorder may be associated with the hormonal changes in pregnancy. Additionally, it is worth noting that the lesions presented during the patient’s second pregnancy, but there were no lesions reported during her first pregnancy 14 months prior, which was aborted in the third month. We cannot explain this phenomenon and cannot predict if the lesions will recur in future pregnancies.
Conclusion
We suggest that both a genetic mutation and pregnancy-induced hormonal changes played possible roles in the development and progress of unilateral generalized KP in our patient. Follow-up is necessary in these patients and further work needs to be done to reveal the underlying mechanism.
1. Hwang S, Schwartz RA. Keratosis pilaris: a common follicular hyperkeratosis. Cutis. 2008;82:177-180.
2. Odom RB, James WD, Berger TG. Andrews’ Diseases of the Skin. 9th ed. Philadelphia, PA: WB Saunders; 2000.
3. Jackson JB, Touma SC, Norton AB. Keratosis pilaris in pregnancy: an unrecognized dematosis of pregnancy? W V Med J. 2004;100:26-28.
4. Poskitt L, Wilkinson JD. Natural history of keratosis pilaris. Br J Dermatol. 1994;130:711-713.
5. Griffiths WAD, Judge MR, Leigh IM. Disorders of keratinisation. In: Champion RH, Burton JL, Burns DA, et al, eds. Textbook of Dermatology. 6th ed. Oxford, MA: Blackwell Scientific; 1998.
6. Nico MM, Valente NY, Sotto MN. Folliculitis ulerythematosa reticulata (atrophoderma vermiculata): early detection of a case with unilateral lesions. Pediatr Dermatol. 1998;15:285-286.
7. Ehsani A, Namazi MR, Barikbin B, et al. Unilaterally generalized keratosis pilaris. J Eur Acad Dermatol Venereol. 2003;17:361-362.
8. Barth JH, Wojnarowska F, Dawber RP. Is keratosis pilaris another androgen-dependent dermatosis? Clin Exp Dermatol. 1988;13:240-241.
1. Hwang S, Schwartz RA. Keratosis pilaris: a common follicular hyperkeratosis. Cutis. 2008;82:177-180.
2. Odom RB, James WD, Berger TG. Andrews’ Diseases of the Skin. 9th ed. Philadelphia, PA: WB Saunders; 2000.
3. Jackson JB, Touma SC, Norton AB. Keratosis pilaris in pregnancy: an unrecognized dematosis of pregnancy? W V Med J. 2004;100:26-28.
4. Poskitt L, Wilkinson JD. Natural history of keratosis pilaris. Br J Dermatol. 1994;130:711-713.
5. Griffiths WAD, Judge MR, Leigh IM. Disorders of keratinisation. In: Champion RH, Burton JL, Burns DA, et al, eds. Textbook of Dermatology. 6th ed. Oxford, MA: Blackwell Scientific; 1998.
6. Nico MM, Valente NY, Sotto MN. Folliculitis ulerythematosa reticulata (atrophoderma vermiculata): early detection of a case with unilateral lesions. Pediatr Dermatol. 1998;15:285-286.
7. Ehsani A, Namazi MR, Barikbin B, et al. Unilaterally generalized keratosis pilaris. J Eur Acad Dermatol Venereol. 2003;17:361-362.
8. Barth JH, Wojnarowska F, Dawber RP. Is keratosis pilaris another androgen-dependent dermatosis? Clin Exp Dermatol. 1988;13:240-241.
Practice Points
- Keratosis pilaris (KP) is a common disorder, with a genetic background and hormonal changes playing possible roles in its development. It also may be associated with a number of diseases.
- The skin lesions of KP usually are bilaterally distributed, either in a generalized or localized distribution. Unilateral lesions are rare. The underlying mechanism of unilateral generalized KP remains unknown.
