User login
ANSWER
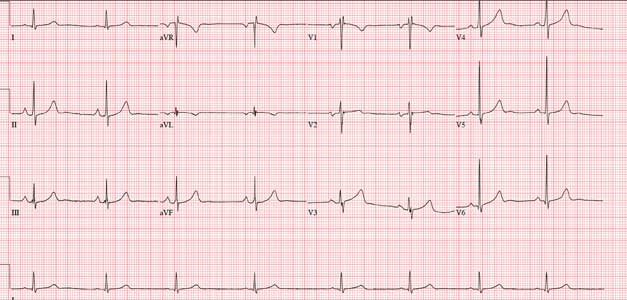
The correct interpretation includes marked sinus bradycardia with sinus arrhythmia, biatrial enlargement, and an RSR’ pattern in lead V1 suggestive of right ventricular conduction delay.
A heart rate below 60 beats/min is considered sinus bradycardia; below 50 beats/min, it may be called marked sinus bradycardia. Sinus arrhythmia is identified by comparing the RR intervals between the third/fourth and fourth/fifth beats on the rhythm strips with the others. This particular variation is most likely respiratory.
Biatrial enlargement is characterized by P waves ≥ 2.5 mm in lead II (right atrial enlargement), P waves > 120 ms in width in lead II, and a biphasic P wave in lead V1 (> 40 ms wide, 1 mm deep). The criteria aren’t crystal clear in this example, but given the large P wave in leads II and aVF and the biphasic P waves in lead V1, the finding is inferred.
Finally, the RSR’ pattern in V1 suggests right ventricular conduction delay but does not meet the criteria (QRS duration > 120 ms) for a right bundle branch block
ANSWER
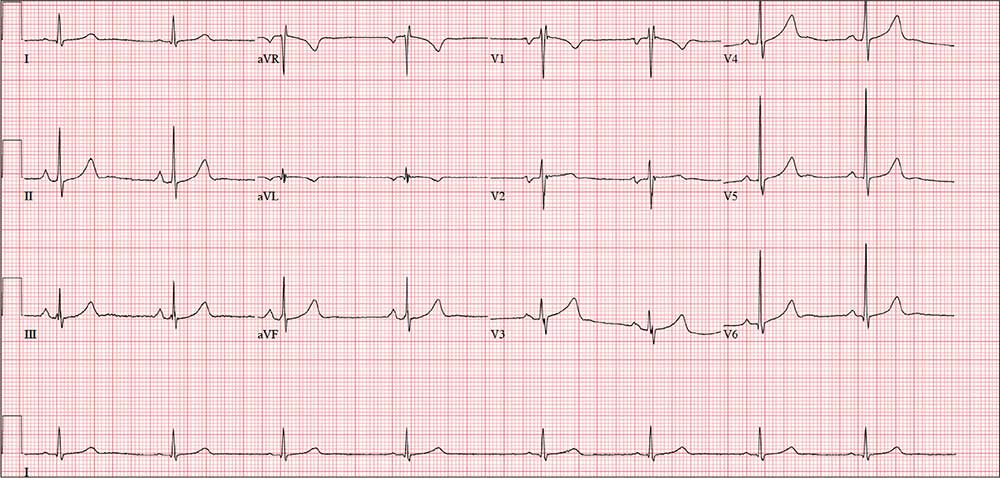
The correct interpretation includes marked sinus bradycardia with sinus arrhythmia, biatrial enlargement, and an RSR’ pattern in lead V1 suggestive of right ventricular conduction delay.
A heart rate below 60 beats/min is considered sinus bradycardia; below 50 beats/min, it may be called marked sinus bradycardia. Sinus arrhythmia is identified by comparing the RR intervals between the third/fourth and fourth/fifth beats on the rhythm strips with the others. This particular variation is most likely respiratory.
Biatrial enlargement is characterized by P waves ≥ 2.5 mm in lead II (right atrial enlargement), P waves > 120 ms in width in lead II, and a biphasic P wave in lead V1 (> 40 ms wide, 1 mm deep). The criteria aren’t crystal clear in this example, but given the large P wave in leads II and aVF and the biphasic P waves in lead V1, the finding is inferred.
Finally, the RSR’ pattern in V1 suggests right ventricular conduction delay but does not meet the criteria (QRS duration > 120 ms) for a right bundle branch block
ANSWER
The correct interpretation includes marked sinus bradycardia with sinus arrhythmia, biatrial enlargement, and an RSR’ pattern in lead V1 suggestive of right ventricular conduction delay.
A heart rate below 60 beats/min is considered sinus bradycardia; below 50 beats/min, it may be called marked sinus bradycardia. Sinus arrhythmia is identified by comparing the RR intervals between the third/fourth and fourth/fifth beats on the rhythm strips with the others. This particular variation is most likely respiratory.
Biatrial enlargement is characterized by P waves ≥ 2.5 mm in lead II (right atrial enlargement), P waves > 120 ms in width in lead II, and a biphasic P wave in lead V1 (> 40 ms wide, 1 mm deep). The criteria aren’t crystal clear in this example, but given the large P wave in leads II and aVF and the biphasic P waves in lead V1, the finding is inferred.
Finally, the RSR’ pattern in V1 suggests right ventricular conduction delay but does not meet the criteria (QRS duration > 120 ms) for a right bundle branch block
For the past 10 years, a 39-year-old man has experienced dyspnea on several occasions—but over the past six months, the severity has increased. The patient says he used to exercise regularly, lifting weights, running up to five miles, and swimming up to a half-mile without difficulty. Now, he can no longer run more than a half-mile without having to stop, and he has given up swimming completely. He denies syncope or near-syncope, palpitations, chest pain, and cough. There is no recent history of upper respiratory infection.
Extensive workup—including an ECG, magnetic resonance angiogram (MRA), transthoracic echocardiogram (TTE), right heart catheterization, and pulmonary function studies—is performed at an outside institution. The ECG demonstrates sinus bradycardia, MRA shows a patent foramen ovale with no shunting, and TTE shows normal left ventricular function and size with a normal ejection fraction and no valvular dysfunction. Right heart catheterization reveals pulmonary artery pressures of 30/10 mm Hg, with a mean pressure of 13 mm Hg. The cardiac output is 9.5 L/min with an arterial saturation of 99%. The Qp:Qs ratio is 1.2:1.
Medical history is positive for childhood asthma, mononucleosis, and two episodes of kidney stones. His current medications include ß-adrenergic and xanthine derivative bronchodilators. He has a true anaphylactic allergy to penicillin.
The patient is recently divorced and lives alone. He has two children, ages 4 and 6, with whom he has weekend visitation rights. He works as a sous chef at a local upscale restaurant. He does not use tobacco products, drinks one to two glasses of wine nightly, and denies recreational drug use. Family history is remarkable for asthma and COPD in both parents (who each smoke 1.5 packs/d of cigarettes).
Review of systems reveals a resolving second-degree thermal burn on the right forearm (work-related) and residual burning with urination from passage of a kidney stone approximately two weeks ago.
Vital signs include a blood pressure of 130/78 mm Hg; pulse, 50 beats/min; respiratory rate, 12 breaths/min-1; O2 saturation, 100% on room air; and temperature, 36.8°C. His weight is 172 lb and his height, 74 in.
Physical exam reveals a healthy-appearing male in no distress. There is no evidence of jugular venous distention or thyromegaly. The lungs are clear bilaterally with no wheezes, crackles, or rales. Cardiac exam reveals a regular rate and rhythm with no extra heart sounds or murmurs. The abdomen is nontender with no organomegaly or bruits. The extremities show no evidence of clubbing, cyanosis, or edema. No rashes on the skin are noted, and the patient is neurologically intact.
A repeat ECG shows a ventricular rate of 49 beats/min; PR interval, 170 ms; QRS duration, 90 ms; QT/QTc interval, 476/429 ms; P axis, 80°; R axis, 58°; and T axis, 72°. What is your interpretation?