User login
› Reassure parents that vaccines are some of the safest and most effective interventions we have to prevent infectious disease. A
› Advise parents that there are multiple systems in place to monitor vaccine safety. C
› Educate parents that lapses in immunization rates can put children at risk of resurgent cases of previously well-controlled diseases, like measles and Haemophilus influenza type b. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When a public health intervention succeeds and achieves long-term suppression of the target problem, an unfortunate irony is that, with time, the intervention can seem less vital. So it is with vaccines. Many patients and physicians today have never experienced the infectious diseases that once caused millions of deaths and much disability each year, and they therefore do not appreciate the impact these diseases had when they were prevalent.
It is estimated that just 9 of the routinely recommended vaccines prevent 42,000 deaths and 20 million cases of disease in every birth cohort.1 With many of these diseases thus held at bay, attention shifted instead to the supposed risks of vaccines. Many people mistakenly believe a vaccine’s potential for harm is more likely than the chance of acquiring the disease it prevents, and they therefore refuse vaccines for themselves and their children, with little chance in the short term of suffering an adverse outcome for their decision.
In this review—which can inform primary care physicians’ discussions with vaccine-hesitant patients—we first highlight 2 preventable diseases, measles and Haemophilus influenzae type b (Hib) infection. Recent residency graduates may never see these diseases thanks to sustained vaccination programs. However, the risk of acquiring these infections has not disappeared entirely. After considering these examples, we examine the totality of the morbidity and mortality prevented by vaccination and describe the safety of current vaccines and the systems in place to assure their continued safety.
Measles: No longer endemic to the United States, but still a risk from importation
In the pre-vaccine era, measles (rubeola) infected more than 500,000 Americans annually and killed roughly 500.2 This highly communicable systemic acute viral infection was once considered universal in childhood. After vaccine licensure in 1963, widespread immunization reduced the incidence by more than 98%, and by 2000 it had eliminated endemic measles from the United States. However, the disease has now reappeared—largely due to international travel and neglect in becoming vaccinated. As of October 31, 2014, the United States had 20 outbreaks and 603 cases of measles reported in 2014—a dramatic increase over recent years.3
Clinical appearance. Acute measles infection is characterized by high fever, cough, coryza, conjunctivitis, and rash. Koplik spots are a 24- to 72-hour pathognomonic exanthem of blue-white spots 1 to 3 mm in diameter on an erythematous base along the buccal mucosa. The resolving exanthem coincides with the eruption of a blanching, maculopapular exanthem originating at the hairline, progressing down the trunk and out to the limbs (sparing the palms and soles), coalescing, and then fading with a fine desquamation in the same order of appearance over 7 days. Additional associated symptoms include anorexia, diarrhea, and generalized lymphadenopathy.2,4
Complications are common with measles. Acute measles infection is rarely fatal. However, serious complications occur in nearly one-third of reported cases.2 During the 1989-1991 measles resurgence in the United States, more than 100 deaths occurred among the 55,000 cases reported.5-7 In early 2011, the United States saw the highest reported number of measles cases since 1996 due to importation. Of the 118 reported cases, 105 (89%) occurred in unvaccinated people, 47 (40%) required hospitalization, and 9 individuals developed pneumonia.8
Complications of measles infection are shown in TABLE 1.2,4 Pneumonia (viral or superimposed bacterial) accounts for 60% of measles-related deaths.2 Neurologic complications, while less frequent, can be severe.
Acute encephalitis occurs in 1 in 1000 to 2000 cases and presents within a week following the exanthem with fever, headache, vomiting, meningismus, change in mental status, convulsions, and coma.2 Encephalitis has a fatality rate of 15%, leaving another 25% with residual neurologic damage.2 Subacute sclerosing panencephalitis (SSPE) occurs in 5 to 10 cases per million (in the United States), on average 7 years after the initial measles infection.9,10 After an insidious onset, behavior and intellect deteriorate, followed by ataxia, myoclonic seizures, and ultimately death. In the United States, the number of reported cases of SSPE has declined with the reduction in measles cases. However, in countries with less robust measles immunization eradication programs, the risk of developing SSPE remains.9,10
Hib: Contained but not eradicated
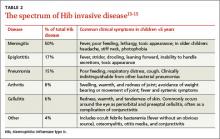
Hib was once the leading cause of meningitis and a major cause of other invasive bacterial diseases, but it has been greatly controlled since the advent of routine Hib vaccination in 1990.11 Hib is an encapsulated, gram-negative coccobacillus. There are 6 major capsular serotypes of Haemophilus influenzae, but serotype b was linked to major invasive disease in humans 95% of the time.12 The spectrum of diseases caused by Hib is seen in TABLE 2.13-15 Hib is transmitted by respiratory droplets from noninfected as well as infected carriers. Asymptomatic nasal carriage in the pre-vaccine era varied from 0.5% to 5%.12
Hib is primarily a disease of young children, with almost all cases occurring in children younger than 5 years of age (66% in those younger than 18 months). Other risk factors for invasive disease are those that increase the spread of respiratory droplets: crowding, lower socioeconomic status, day care attendance, large household size, and school-aged siblings. American Indian and Alaskan Native populations remain at higher risk due to incomplete vaccination rates and the sociodemographic risk factors noted above. Breastfeeding is protective.12
Three percent to 6% of cases of invasive Hib disease are fatal; another 20% can have long-term sequelae such as hearing loss. In the early 1990s, the peak incidence of Hib disease reached 41 cases per 100,000 population.12 The reduction in incidence of Hib disease brought about by universal vaccination has been attributed to individual immunity, decreased asymptomatic nasal carriage, and herd immunity.12
Despite this progress, Hib continues to evade eradication. In Minnesota in 2008, 5 children, ages 5 months to 3 years, contracted invasive Hib disease (3 with meningitis, 1 with pneumonia, 1 with epiglottitis).16 Of the 5, only one was up to date with Hib vaccination; the others had not received vaccine because of shortages or parent refusal. These children were unrelated and had not been in contact with each other.
In a daycare outbreak in the United Kingdom, 2 cases of Hib disease (meningitis and septic arthritis) were identified in fully immunized children younger than 18 months, presumably due to a lack of complete vaccine efficacy.17 A study of nasal carriage (performed just prior to rifampin prophylaxis) among other attendees and caregivers revealed 3 asymptomatic carriers.17 Although Hib is largely well-contained in developed countries due to vaccination policies, the burden of disease in developing countries is estimated to be approximately 8.1 million serious illnesses with 371,000 deaths annually.13
The totality of morbidity and mortality prevented by vaccines
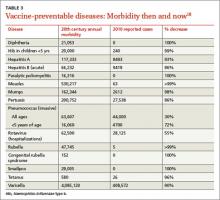
Measles and Hib are 2 examples of vaccine-preventable diseases and the reduction in morbidity and mortality achievable with vaccines. TABLE 318 summarizes the number of pre-vaccine era cases for selected diseases. Routine vaccination against 7 common childhood diseases not only prevents many thousands of deaths, as mentioned earlier,1 but it saves $13.5 billion in direct costs in each birth cohort and saves society $68.8 billion in costs that include disability and lost productivity of both patients and caregivers.1
Put simply, every dollar spent on the vaccination program saves $10 in direct and indirect costs to society.1 Sustaining these successes and averting the resurgence of contained diseases requires a commitment to high immunization rates without delays and lapses—an effort made more challenging in light of misinformation about vaccine safety and resultant parental vaccine hesitancy.
Vaccine safety is ensured by rigorous systems
Despite an impressive record of safety, vaccines still cause anxiety among patients and parents in family practices. A recent survey identified concerns of long-term complications, autism, and thimerosal effects to be foremost on the minds of parents, whereas short-term effects were of much less concern.19 Causation of autism related to vaccines has been dismissed; the initial linkages have been shown to be fraudulent.20 With the exception of some influenza vaccine preparations, thimerosal is no longer present in routinely administered children’s vaccines and has been shown not to be associated with autism.21,22 To address parents’ and patients’ concerns about vaccine safety, and especially those surrounding short- and long-term complications, physicians should have a general understanding of the pre- and post-licensure mechanisms in the United States.
Pre-licensure safety is under the purview of vaccine manufacturers and the Center for Biologics Evaluation and Research at the US Food and Drug Administration (http://www.fda.gov/biologicsbloodvaccines/vaccines/default.htm). For licensure, manufacturers must provide clinical data to demonstrate sufficient safety and efficacy. Accordingly, pre-licensure assessments are conducted in a “closed system” under a research protocol. The vaccine recipients are volitional research subjects selected according to inclusion and exclusion criteria. They are also compensated. However, sample sizes are rarely large enough to exclude rare serious adverse events.
Once licensure has been granted, the focus of safety then shifts to the “open system” of usual clinical practice. Vaccine recipients are unselected members of the general population and may have underlying medical conditions, and sometimes—such as with school entry mandates—are less volitional. In this sphere, the responsible parties for safety include the government, manufacturers, and health care systems.
Three ongoing systems function to assure vaccine safety: the Vaccine Adverse Event Reporting System (VAERS), the Vaccine Safety Datalink (VSD), and the Clinical Immunization Safety Assessment (CISA) Network.23,24
VAERS serves as an early warning system for coincidental safety signals and can generate hypotheses for further investigation.24,25 It is characterized by high sensitivity but low specificity as it relies on voluntary reporting from health care personnel, parents, and others. This system was instrumental in identifying the initial cases of intussusception attributable to the rotavirus vaccine, RotaShield.26
The VSD is a network of 10 large, geographically diverse and linked health maintenance organizations that cover about 3% of the US population. Within this “real time” network, vaccination (exposure) can be compared with outpatient, emergency department, hospital, and laboratory data (health outcomes), while accounting for demographic variables (confounders).27,28 VSD studies linked the measles, mumps, rubella, and varicella vaccine to febrile seizures29 and showed no relationship between cumulative vaccine antigen exposure and autism.30
The CISA was established in 2001 to investigate the pathophysiologic mechanisms and biologic risks of adverse effects following immunization and to provide evidence-based vaccine safety assessments.
Based on all available evidence, routinely recommended vaccines have attained a very high level of safety. As with other preventive services, immunizations are generally provided to healthy individuals to maintain good health; thus, a low tolerance for significant adverse events exists. Well over 100 million doses of vaccines are given each year, yet the VAERS receives, on average, only 28,000 adverse event reports per year.
These reports comprise mild, moderate, and severe reactions to vaccines, but also adverse events that may not be related in any way other than chronologically to the vaccine’s administration. Despite this relatively low number of real safety concerns, it is still more likely that patients will know someone who has had a vaccine-related adverse event than someone who has had some of the diseases the vaccines prevent.31
Final thoughts
Current anti-vaccine sentiments appear to arise from varying perspectives. Some are held by parents of children who have allegedly suffered a severe vaccine related adverse event; others by those opposed to government-mandated school immunization requirements; and some from those who have a dislike of vaccine manufacturers. These sentiments persist in part because of a low level of vaccine preventable diseases: When such illnesses are no longer deemed a threat, those who have concerns about vaccine safety, no matter how invalid, believe their concerns should trump all other considerations.
To appreciate the true benefit of vaccine acceptance, we need only look to Europe, where the anti-vaccine movement has led to high levels of vaccine refusal and a resurgence of vaccine-preventable diseases, such as measles, with their associated morbidity and mortality.32 In advocating for continued acceptance and widespread use of vaccines, family physicians can convey to patients and parents the magnitude of associated health benefits while confidently attesting to the effectiveness and safety of vaccines.
CORRESPONDENCE
John Epling, MD, MSEd, Department of Family Medicine, SUNY Upstate Medical University, 475 Irving Ave, Suite 200, Syracuse, NY 13210; [email protected]
1. Zhou F, Shefer A, Wenger J, et al. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014;133:577-585.
2. Centers for Disease Control and Prevention. Measles. Epidemiology and prevention of vaccine-preventable diseases. The Pink Book: Course Textbook. 12th ed. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/meas.html. Accessed March 4, 2012.
3. Centers for Disease Control and Prevention. Measles (Rubeola). Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/measles/. Accessed November 19, 2014.
4. Measles. In: Pickering LK, Baker CJ, Kimberlin DW, et al, eds. Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009:444-455.
5. Atkinson WL, Orenstein WA, Krugman S. The resurgence of measles in the United States, 1989-1990. Annu Rev Med. 1992;43:451-463.
6. Centers for Disease Control and Prevention (CDC). Measles--United States, 1990. MMWR Morb Mortal Wkly Rep. 1991;40:369-372.
7. Gindler J, Tinker S, Markowitz L, et al. Acute measles mortality in the United States, 1987-2002. J Infect Dis. 2004;189(suppl 1): S69-S77.
8. Centers for Disease Control and Prevention (CDC). Measles: United States, January-May 20, 2011. MMWR Morb Mortal Wkly Rep. 2011;60:666-668.
9. Bernstein DI, Reuman PD, Schiff GM. Rubeola (measles) and subacute sclerosing panencephalitis virus. In: Gorbach SL, Bartlett JG, Blacklow NR (eds). Infectious Diseases. Philadelphia, PA: WB Saunders; 1998:2135.
10. Bellini WJ, Rota JS, Lowe LE, et al. Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. J Infect Dis. 2005;192:1686-1693.
11. Centers for Disease Control and Prevention (CDC). Progress toward elimination of Haemophilus influenza type b invasive disease among infants and children—United States, 1998-2000. MMWR Morb Mortal Wkly Rep. 2002;51:234-237.
12. Centers for Disease Control and Prevention (CDC). Epidemiology and Prevention of Vaccine-Preventable Diseases. The Pink Book, Course Textbook, 12th ed. Haemophilus influenzae type b. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/hib.html. Accessed March 4, 2012.
13. Watt JP, Wolfson LJ, O’Brien KL, et al; Hib and Pneumococcal Global Burden of Disease Study Team. Burden of disease caused by Haemophilus influenzae type b in children younger than 5 years: global estimates. Lancet. 2009;374:903-911.
14. Agrawal A, Murphy TF. Haemophilus influenzae infections in the H. influenzae type b conjugate vaccine era. J Clin Microbiol. 2011;49:3728-3732.
15. Chandran A, Watt JP, Santosham M. Prevention of Haemophilus influenza type b disease: past successes and future challenges. Informa Healthcare. 2005;4:819-827.
16. Centers for Disease Control and Prevention (CDC). Invasive Haemophilus influenza Type B disease in five young children--Minnesota, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:58-60.
17. McVernon J, Morgan P, Mallaghan C, et al. Outbreak of Haemophilus influenzae type b disease among fully vaccinated children in a day-care center. Pediatr Infect Dis J. 2004;23:38-41.
18. Hinman AR, Orenstein WA, Schuchat A; Centers for Disease Control and Prevention (CDC). Vaccine-preventable diseases, immunizations, and MMWR—1961-2011. MMWR Morb Mortal Wkly Rep. 2011;60 suppl 4:49-57.
19. Kempe A, Daley MF, McCauley MM, et al. Prevalence of parental concerns about childhood vaccines: the experience of primary care physicians. Am J Prev Med. 2011;40:548-555.
20. Godlee F, Smith J, Marcovitch H. Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ. 2011;342:c7452.
21. Institute for Vaccine Safety. Thimerosal content in some US Licensed vaccines. Institute for Vaccine Safety Web site. Available at: http://www.vaccinesafety.edu/thi-table.htm. Accessed March 8, 2012.
22. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention: Immunization safety and autism. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccinesafety/00_pdf/CDCStudiesonVaccinesandAutism.pdf. Accessed September 23, 2013.
23. Centers for Disease Control and Prevention. Ensuring the safety of vaccines in the United States. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/hcp/patient-ed/conversations/downloads/vacsafe-ensuring-color-office.pdf. Accessed November 18, 2014.
24. Wharton M. Vaccine safety: current systems and recent findings. Curr Opin Pediatr. 2010;22:88-93.
25. US Food and Drug Administration. Understanding the Vaccine Adverse Event Reporting System (VAERS). US Food and Drug Administration Web site. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/SafetyAvailability/VaccineSafety/UCM298183.pdf. Accessed October 15, 2014.
26. Centers for Disease Control and Prevention (CDC). Suspension of rotavirus vaccine after reports of intussusception--United States, 1999. MMWR Morb Mortal Wkly Rep. 2004;53:786-789.
27. Greene SK, Kulldorff M, Lewis EM, et al. Near real-time surveillance for influenza vaccine safety: proof-of-concept in the Vaccine Safety Datalink Project. Am J Epidemiol. 2010;171:177-188.
28. Iskander J, Broder K. Monitoring the safety of annual and pandemic influenza vaccines: lessons from the US experience. Expert Rev Vaccines. 2008;7:75-82.
29. Klein NP, Fireman B, Yih WK, et al. Measles-mumps-rubella-varicella combination vaccine and the risk of febrile seizures. Pediatrics. 2010;126:e1-e8.
30. DeStefano F, Price CS, Weintraub ES. Increasing exposure to antibody-stimulating proteins and polysaccharides in vaccines is not associated with risk of autism. J Pediatr. 2013;163:561-567.
31. Centers for Disease Control and Prevention (CDC). Epidemiology and prevention of vaccine-preventable diseases. The Pink Book, Course Textbook, 12th ed. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/safety.html. Accessed November 17, 2014.
32. World Health Organization (WHO). Measles outbreak in Europe. Global alert and response. Available at: http://www.who.int/csr/don/2011_04_21/en/index.html. Accessed March 8, 2012.
› Reassure parents that vaccines are some of the safest and most effective interventions we have to prevent infectious disease. A
› Advise parents that there are multiple systems in place to monitor vaccine safety. C
› Educate parents that lapses in immunization rates can put children at risk of resurgent cases of previously well-controlled diseases, like measles and Haemophilus influenza type b. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When a public health intervention succeeds and achieves long-term suppression of the target problem, an unfortunate irony is that, with time, the intervention can seem less vital. So it is with vaccines. Many patients and physicians today have never experienced the infectious diseases that once caused millions of deaths and much disability each year, and they therefore do not appreciate the impact these diseases had when they were prevalent.
It is estimated that just 9 of the routinely recommended vaccines prevent 42,000 deaths and 20 million cases of disease in every birth cohort.1 With many of these diseases thus held at bay, attention shifted instead to the supposed risks of vaccines. Many people mistakenly believe a vaccine’s potential for harm is more likely than the chance of acquiring the disease it prevents, and they therefore refuse vaccines for themselves and their children, with little chance in the short term of suffering an adverse outcome for their decision.
In this review—which can inform primary care physicians’ discussions with vaccine-hesitant patients—we first highlight 2 preventable diseases, measles and Haemophilus influenzae type b (Hib) infection. Recent residency graduates may never see these diseases thanks to sustained vaccination programs. However, the risk of acquiring these infections has not disappeared entirely. After considering these examples, we examine the totality of the morbidity and mortality prevented by vaccination and describe the safety of current vaccines and the systems in place to assure their continued safety.
Measles: No longer endemic to the United States, but still a risk from importation
In the pre-vaccine era, measles (rubeola) infected more than 500,000 Americans annually and killed roughly 500.2 This highly communicable systemic acute viral infection was once considered universal in childhood. After vaccine licensure in 1963, widespread immunization reduced the incidence by more than 98%, and by 2000 it had eliminated endemic measles from the United States. However, the disease has now reappeared—largely due to international travel and neglect in becoming vaccinated. As of October 31, 2014, the United States had 20 outbreaks and 603 cases of measles reported in 2014—a dramatic increase over recent years.3
Clinical appearance. Acute measles infection is characterized by high fever, cough, coryza, conjunctivitis, and rash. Koplik spots are a 24- to 72-hour pathognomonic exanthem of blue-white spots 1 to 3 mm in diameter on an erythematous base along the buccal mucosa. The resolving exanthem coincides with the eruption of a blanching, maculopapular exanthem originating at the hairline, progressing down the trunk and out to the limbs (sparing the palms and soles), coalescing, and then fading with a fine desquamation in the same order of appearance over 7 days. Additional associated symptoms include anorexia, diarrhea, and generalized lymphadenopathy.2,4
Complications are common with measles. Acute measles infection is rarely fatal. However, serious complications occur in nearly one-third of reported cases.2 During the 1989-1991 measles resurgence in the United States, more than 100 deaths occurred among the 55,000 cases reported.5-7 In early 2011, the United States saw the highest reported number of measles cases since 1996 due to importation. Of the 118 reported cases, 105 (89%) occurred in unvaccinated people, 47 (40%) required hospitalization, and 9 individuals developed pneumonia.8
Complications of measles infection are shown in TABLE 1.2,4 Pneumonia (viral or superimposed bacterial) accounts for 60% of measles-related deaths.2 Neurologic complications, while less frequent, can be severe.
Acute encephalitis occurs in 1 in 1000 to 2000 cases and presents within a week following the exanthem with fever, headache, vomiting, meningismus, change in mental status, convulsions, and coma.2 Encephalitis has a fatality rate of 15%, leaving another 25% with residual neurologic damage.2 Subacute sclerosing panencephalitis (SSPE) occurs in 5 to 10 cases per million (in the United States), on average 7 years after the initial measles infection.9,10 After an insidious onset, behavior and intellect deteriorate, followed by ataxia, myoclonic seizures, and ultimately death. In the United States, the number of reported cases of SSPE has declined with the reduction in measles cases. However, in countries with less robust measles immunization eradication programs, the risk of developing SSPE remains.9,10
Hib: Contained but not eradicated
Hib was once the leading cause of meningitis and a major cause of other invasive bacterial diseases, but it has been greatly controlled since the advent of routine Hib vaccination in 1990.11 Hib is an encapsulated, gram-negative coccobacillus. There are 6 major capsular serotypes of Haemophilus influenzae, but serotype b was linked to major invasive disease in humans 95% of the time.12 The spectrum of diseases caused by Hib is seen in TABLE 2.13-15 Hib is transmitted by respiratory droplets from noninfected as well as infected carriers. Asymptomatic nasal carriage in the pre-vaccine era varied from 0.5% to 5%.12
Hib is primarily a disease of young children, with almost all cases occurring in children younger than 5 years of age (66% in those younger than 18 months). Other risk factors for invasive disease are those that increase the spread of respiratory droplets: crowding, lower socioeconomic status, day care attendance, large household size, and school-aged siblings. American Indian and Alaskan Native populations remain at higher risk due to incomplete vaccination rates and the sociodemographic risk factors noted above. Breastfeeding is protective.12
Three percent to 6% of cases of invasive Hib disease are fatal; another 20% can have long-term sequelae such as hearing loss. In the early 1990s, the peak incidence of Hib disease reached 41 cases per 100,000 population.12 The reduction in incidence of Hib disease brought about by universal vaccination has been attributed to individual immunity, decreased asymptomatic nasal carriage, and herd immunity.12
Despite this progress, Hib continues to evade eradication. In Minnesota in 2008, 5 children, ages 5 months to 3 years, contracted invasive Hib disease (3 with meningitis, 1 with pneumonia, 1 with epiglottitis).16 Of the 5, only one was up to date with Hib vaccination; the others had not received vaccine because of shortages or parent refusal. These children were unrelated and had not been in contact with each other.
In a daycare outbreak in the United Kingdom, 2 cases of Hib disease (meningitis and septic arthritis) were identified in fully immunized children younger than 18 months, presumably due to a lack of complete vaccine efficacy.17 A study of nasal carriage (performed just prior to rifampin prophylaxis) among other attendees and caregivers revealed 3 asymptomatic carriers.17 Although Hib is largely well-contained in developed countries due to vaccination policies, the burden of disease in developing countries is estimated to be approximately 8.1 million serious illnesses with 371,000 deaths annually.13
The totality of morbidity and mortality prevented by vaccines
Measles and Hib are 2 examples of vaccine-preventable diseases and the reduction in morbidity and mortality achievable with vaccines. TABLE 318 summarizes the number of pre-vaccine era cases for selected diseases. Routine vaccination against 7 common childhood diseases not only prevents many thousands of deaths, as mentioned earlier,1 but it saves $13.5 billion in direct costs in each birth cohort and saves society $68.8 billion in costs that include disability and lost productivity of both patients and caregivers.1
Put simply, every dollar spent on the vaccination program saves $10 in direct and indirect costs to society.1 Sustaining these successes and averting the resurgence of contained diseases requires a commitment to high immunization rates without delays and lapses—an effort made more challenging in light of misinformation about vaccine safety and resultant parental vaccine hesitancy.
Vaccine safety is ensured by rigorous systems
Despite an impressive record of safety, vaccines still cause anxiety among patients and parents in family practices. A recent survey identified concerns of long-term complications, autism, and thimerosal effects to be foremost on the minds of parents, whereas short-term effects were of much less concern.19 Causation of autism related to vaccines has been dismissed; the initial linkages have been shown to be fraudulent.20 With the exception of some influenza vaccine preparations, thimerosal is no longer present in routinely administered children’s vaccines and has been shown not to be associated with autism.21,22 To address parents’ and patients’ concerns about vaccine safety, and especially those surrounding short- and long-term complications, physicians should have a general understanding of the pre- and post-licensure mechanisms in the United States.
Pre-licensure safety is under the purview of vaccine manufacturers and the Center for Biologics Evaluation and Research at the US Food and Drug Administration (http://www.fda.gov/biologicsbloodvaccines/vaccines/default.htm). For licensure, manufacturers must provide clinical data to demonstrate sufficient safety and efficacy. Accordingly, pre-licensure assessments are conducted in a “closed system” under a research protocol. The vaccine recipients are volitional research subjects selected according to inclusion and exclusion criteria. They are also compensated. However, sample sizes are rarely large enough to exclude rare serious adverse events.
Once licensure has been granted, the focus of safety then shifts to the “open system” of usual clinical practice. Vaccine recipients are unselected members of the general population and may have underlying medical conditions, and sometimes—such as with school entry mandates—are less volitional. In this sphere, the responsible parties for safety include the government, manufacturers, and health care systems.
Three ongoing systems function to assure vaccine safety: the Vaccine Adverse Event Reporting System (VAERS), the Vaccine Safety Datalink (VSD), and the Clinical Immunization Safety Assessment (CISA) Network.23,24
VAERS serves as an early warning system for coincidental safety signals and can generate hypotheses for further investigation.24,25 It is characterized by high sensitivity but low specificity as it relies on voluntary reporting from health care personnel, parents, and others. This system was instrumental in identifying the initial cases of intussusception attributable to the rotavirus vaccine, RotaShield.26
The VSD is a network of 10 large, geographically diverse and linked health maintenance organizations that cover about 3% of the US population. Within this “real time” network, vaccination (exposure) can be compared with outpatient, emergency department, hospital, and laboratory data (health outcomes), while accounting for demographic variables (confounders).27,28 VSD studies linked the measles, mumps, rubella, and varicella vaccine to febrile seizures29 and showed no relationship between cumulative vaccine antigen exposure and autism.30
The CISA was established in 2001 to investigate the pathophysiologic mechanisms and biologic risks of adverse effects following immunization and to provide evidence-based vaccine safety assessments.
Based on all available evidence, routinely recommended vaccines have attained a very high level of safety. As with other preventive services, immunizations are generally provided to healthy individuals to maintain good health; thus, a low tolerance for significant adverse events exists. Well over 100 million doses of vaccines are given each year, yet the VAERS receives, on average, only 28,000 adverse event reports per year.
These reports comprise mild, moderate, and severe reactions to vaccines, but also adverse events that may not be related in any way other than chronologically to the vaccine’s administration. Despite this relatively low number of real safety concerns, it is still more likely that patients will know someone who has had a vaccine-related adverse event than someone who has had some of the diseases the vaccines prevent.31
Final thoughts
Current anti-vaccine sentiments appear to arise from varying perspectives. Some are held by parents of children who have allegedly suffered a severe vaccine related adverse event; others by those opposed to government-mandated school immunization requirements; and some from those who have a dislike of vaccine manufacturers. These sentiments persist in part because of a low level of vaccine preventable diseases: When such illnesses are no longer deemed a threat, those who have concerns about vaccine safety, no matter how invalid, believe their concerns should trump all other considerations.
To appreciate the true benefit of vaccine acceptance, we need only look to Europe, where the anti-vaccine movement has led to high levels of vaccine refusal and a resurgence of vaccine-preventable diseases, such as measles, with their associated morbidity and mortality.32 In advocating for continued acceptance and widespread use of vaccines, family physicians can convey to patients and parents the magnitude of associated health benefits while confidently attesting to the effectiveness and safety of vaccines.
CORRESPONDENCE
John Epling, MD, MSEd, Department of Family Medicine, SUNY Upstate Medical University, 475 Irving Ave, Suite 200, Syracuse, NY 13210; [email protected]
› Reassure parents that vaccines are some of the safest and most effective interventions we have to prevent infectious disease. A
› Advise parents that there are multiple systems in place to monitor vaccine safety. C
› Educate parents that lapses in immunization rates can put children at risk of resurgent cases of previously well-controlled diseases, like measles and Haemophilus influenza type b. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When a public health intervention succeeds and achieves long-term suppression of the target problem, an unfortunate irony is that, with time, the intervention can seem less vital. So it is with vaccines. Many patients and physicians today have never experienced the infectious diseases that once caused millions of deaths and much disability each year, and they therefore do not appreciate the impact these diseases had when they were prevalent.
It is estimated that just 9 of the routinely recommended vaccines prevent 42,000 deaths and 20 million cases of disease in every birth cohort.1 With many of these diseases thus held at bay, attention shifted instead to the supposed risks of vaccines. Many people mistakenly believe a vaccine’s potential for harm is more likely than the chance of acquiring the disease it prevents, and they therefore refuse vaccines for themselves and their children, with little chance in the short term of suffering an adverse outcome for their decision.
In this review—which can inform primary care physicians’ discussions with vaccine-hesitant patients—we first highlight 2 preventable diseases, measles and Haemophilus influenzae type b (Hib) infection. Recent residency graduates may never see these diseases thanks to sustained vaccination programs. However, the risk of acquiring these infections has not disappeared entirely. After considering these examples, we examine the totality of the morbidity and mortality prevented by vaccination and describe the safety of current vaccines and the systems in place to assure their continued safety.
Measles: No longer endemic to the United States, but still a risk from importation
In the pre-vaccine era, measles (rubeola) infected more than 500,000 Americans annually and killed roughly 500.2 This highly communicable systemic acute viral infection was once considered universal in childhood. After vaccine licensure in 1963, widespread immunization reduced the incidence by more than 98%, and by 2000 it had eliminated endemic measles from the United States. However, the disease has now reappeared—largely due to international travel and neglect in becoming vaccinated. As of October 31, 2014, the United States had 20 outbreaks and 603 cases of measles reported in 2014—a dramatic increase over recent years.3
Clinical appearance. Acute measles infection is characterized by high fever, cough, coryza, conjunctivitis, and rash. Koplik spots are a 24- to 72-hour pathognomonic exanthem of blue-white spots 1 to 3 mm in diameter on an erythematous base along the buccal mucosa. The resolving exanthem coincides with the eruption of a blanching, maculopapular exanthem originating at the hairline, progressing down the trunk and out to the limbs (sparing the palms and soles), coalescing, and then fading with a fine desquamation in the same order of appearance over 7 days. Additional associated symptoms include anorexia, diarrhea, and generalized lymphadenopathy.2,4
Complications are common with measles. Acute measles infection is rarely fatal. However, serious complications occur in nearly one-third of reported cases.2 During the 1989-1991 measles resurgence in the United States, more than 100 deaths occurred among the 55,000 cases reported.5-7 In early 2011, the United States saw the highest reported number of measles cases since 1996 due to importation. Of the 118 reported cases, 105 (89%) occurred in unvaccinated people, 47 (40%) required hospitalization, and 9 individuals developed pneumonia.8
Complications of measles infection are shown in TABLE 1.2,4 Pneumonia (viral or superimposed bacterial) accounts for 60% of measles-related deaths.2 Neurologic complications, while less frequent, can be severe.
Acute encephalitis occurs in 1 in 1000 to 2000 cases and presents within a week following the exanthem with fever, headache, vomiting, meningismus, change in mental status, convulsions, and coma.2 Encephalitis has a fatality rate of 15%, leaving another 25% with residual neurologic damage.2 Subacute sclerosing panencephalitis (SSPE) occurs in 5 to 10 cases per million (in the United States), on average 7 years after the initial measles infection.9,10 After an insidious onset, behavior and intellect deteriorate, followed by ataxia, myoclonic seizures, and ultimately death. In the United States, the number of reported cases of SSPE has declined with the reduction in measles cases. However, in countries with less robust measles immunization eradication programs, the risk of developing SSPE remains.9,10
Hib: Contained but not eradicated
Hib was once the leading cause of meningitis and a major cause of other invasive bacterial diseases, but it has been greatly controlled since the advent of routine Hib vaccination in 1990.11 Hib is an encapsulated, gram-negative coccobacillus. There are 6 major capsular serotypes of Haemophilus influenzae, but serotype b was linked to major invasive disease in humans 95% of the time.12 The spectrum of diseases caused by Hib is seen in TABLE 2.13-15 Hib is transmitted by respiratory droplets from noninfected as well as infected carriers. Asymptomatic nasal carriage in the pre-vaccine era varied from 0.5% to 5%.12
Hib is primarily a disease of young children, with almost all cases occurring in children younger than 5 years of age (66% in those younger than 18 months). Other risk factors for invasive disease are those that increase the spread of respiratory droplets: crowding, lower socioeconomic status, day care attendance, large household size, and school-aged siblings. American Indian and Alaskan Native populations remain at higher risk due to incomplete vaccination rates and the sociodemographic risk factors noted above. Breastfeeding is protective.12
Three percent to 6% of cases of invasive Hib disease are fatal; another 20% can have long-term sequelae such as hearing loss. In the early 1990s, the peak incidence of Hib disease reached 41 cases per 100,000 population.12 The reduction in incidence of Hib disease brought about by universal vaccination has been attributed to individual immunity, decreased asymptomatic nasal carriage, and herd immunity.12
Despite this progress, Hib continues to evade eradication. In Minnesota in 2008, 5 children, ages 5 months to 3 years, contracted invasive Hib disease (3 with meningitis, 1 with pneumonia, 1 with epiglottitis).16 Of the 5, only one was up to date with Hib vaccination; the others had not received vaccine because of shortages or parent refusal. These children were unrelated and had not been in contact with each other.
In a daycare outbreak in the United Kingdom, 2 cases of Hib disease (meningitis and septic arthritis) were identified in fully immunized children younger than 18 months, presumably due to a lack of complete vaccine efficacy.17 A study of nasal carriage (performed just prior to rifampin prophylaxis) among other attendees and caregivers revealed 3 asymptomatic carriers.17 Although Hib is largely well-contained in developed countries due to vaccination policies, the burden of disease in developing countries is estimated to be approximately 8.1 million serious illnesses with 371,000 deaths annually.13
The totality of morbidity and mortality prevented by vaccines
Measles and Hib are 2 examples of vaccine-preventable diseases and the reduction in morbidity and mortality achievable with vaccines. TABLE 318 summarizes the number of pre-vaccine era cases for selected diseases. Routine vaccination against 7 common childhood diseases not only prevents many thousands of deaths, as mentioned earlier,1 but it saves $13.5 billion in direct costs in each birth cohort and saves society $68.8 billion in costs that include disability and lost productivity of both patients and caregivers.1
Put simply, every dollar spent on the vaccination program saves $10 in direct and indirect costs to society.1 Sustaining these successes and averting the resurgence of contained diseases requires a commitment to high immunization rates without delays and lapses—an effort made more challenging in light of misinformation about vaccine safety and resultant parental vaccine hesitancy.
Vaccine safety is ensured by rigorous systems
Despite an impressive record of safety, vaccines still cause anxiety among patients and parents in family practices. A recent survey identified concerns of long-term complications, autism, and thimerosal effects to be foremost on the minds of parents, whereas short-term effects were of much less concern.19 Causation of autism related to vaccines has been dismissed; the initial linkages have been shown to be fraudulent.20 With the exception of some influenza vaccine preparations, thimerosal is no longer present in routinely administered children’s vaccines and has been shown not to be associated with autism.21,22 To address parents’ and patients’ concerns about vaccine safety, and especially those surrounding short- and long-term complications, physicians should have a general understanding of the pre- and post-licensure mechanisms in the United States.
Pre-licensure safety is under the purview of vaccine manufacturers and the Center for Biologics Evaluation and Research at the US Food and Drug Administration (http://www.fda.gov/biologicsbloodvaccines/vaccines/default.htm). For licensure, manufacturers must provide clinical data to demonstrate sufficient safety and efficacy. Accordingly, pre-licensure assessments are conducted in a “closed system” under a research protocol. The vaccine recipients are volitional research subjects selected according to inclusion and exclusion criteria. They are also compensated. However, sample sizes are rarely large enough to exclude rare serious adverse events.
Once licensure has been granted, the focus of safety then shifts to the “open system” of usual clinical practice. Vaccine recipients are unselected members of the general population and may have underlying medical conditions, and sometimes—such as with school entry mandates—are less volitional. In this sphere, the responsible parties for safety include the government, manufacturers, and health care systems.
Three ongoing systems function to assure vaccine safety: the Vaccine Adverse Event Reporting System (VAERS), the Vaccine Safety Datalink (VSD), and the Clinical Immunization Safety Assessment (CISA) Network.23,24
VAERS serves as an early warning system for coincidental safety signals and can generate hypotheses for further investigation.24,25 It is characterized by high sensitivity but low specificity as it relies on voluntary reporting from health care personnel, parents, and others. This system was instrumental in identifying the initial cases of intussusception attributable to the rotavirus vaccine, RotaShield.26
The VSD is a network of 10 large, geographically diverse and linked health maintenance organizations that cover about 3% of the US population. Within this “real time” network, vaccination (exposure) can be compared with outpatient, emergency department, hospital, and laboratory data (health outcomes), while accounting for demographic variables (confounders).27,28 VSD studies linked the measles, mumps, rubella, and varicella vaccine to febrile seizures29 and showed no relationship between cumulative vaccine antigen exposure and autism.30
The CISA was established in 2001 to investigate the pathophysiologic mechanisms and biologic risks of adverse effects following immunization and to provide evidence-based vaccine safety assessments.
Based on all available evidence, routinely recommended vaccines have attained a very high level of safety. As with other preventive services, immunizations are generally provided to healthy individuals to maintain good health; thus, a low tolerance for significant adverse events exists. Well over 100 million doses of vaccines are given each year, yet the VAERS receives, on average, only 28,000 adverse event reports per year.
These reports comprise mild, moderate, and severe reactions to vaccines, but also adverse events that may not be related in any way other than chronologically to the vaccine’s administration. Despite this relatively low number of real safety concerns, it is still more likely that patients will know someone who has had a vaccine-related adverse event than someone who has had some of the diseases the vaccines prevent.31
Final thoughts
Current anti-vaccine sentiments appear to arise from varying perspectives. Some are held by parents of children who have allegedly suffered a severe vaccine related adverse event; others by those opposed to government-mandated school immunization requirements; and some from those who have a dislike of vaccine manufacturers. These sentiments persist in part because of a low level of vaccine preventable diseases: When such illnesses are no longer deemed a threat, those who have concerns about vaccine safety, no matter how invalid, believe their concerns should trump all other considerations.
To appreciate the true benefit of vaccine acceptance, we need only look to Europe, where the anti-vaccine movement has led to high levels of vaccine refusal and a resurgence of vaccine-preventable diseases, such as measles, with their associated morbidity and mortality.32 In advocating for continued acceptance and widespread use of vaccines, family physicians can convey to patients and parents the magnitude of associated health benefits while confidently attesting to the effectiveness and safety of vaccines.
CORRESPONDENCE
John Epling, MD, MSEd, Department of Family Medicine, SUNY Upstate Medical University, 475 Irving Ave, Suite 200, Syracuse, NY 13210; [email protected]
1. Zhou F, Shefer A, Wenger J, et al. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014;133:577-585.
2. Centers for Disease Control and Prevention. Measles. Epidemiology and prevention of vaccine-preventable diseases. The Pink Book: Course Textbook. 12th ed. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/meas.html. Accessed March 4, 2012.
3. Centers for Disease Control and Prevention. Measles (Rubeola). Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/measles/. Accessed November 19, 2014.
4. Measles. In: Pickering LK, Baker CJ, Kimberlin DW, et al, eds. Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009:444-455.
5. Atkinson WL, Orenstein WA, Krugman S. The resurgence of measles in the United States, 1989-1990. Annu Rev Med. 1992;43:451-463.
6. Centers for Disease Control and Prevention (CDC). Measles--United States, 1990. MMWR Morb Mortal Wkly Rep. 1991;40:369-372.
7. Gindler J, Tinker S, Markowitz L, et al. Acute measles mortality in the United States, 1987-2002. J Infect Dis. 2004;189(suppl 1): S69-S77.
8. Centers for Disease Control and Prevention (CDC). Measles: United States, January-May 20, 2011. MMWR Morb Mortal Wkly Rep. 2011;60:666-668.
9. Bernstein DI, Reuman PD, Schiff GM. Rubeola (measles) and subacute sclerosing panencephalitis virus. In: Gorbach SL, Bartlett JG, Blacklow NR (eds). Infectious Diseases. Philadelphia, PA: WB Saunders; 1998:2135.
10. Bellini WJ, Rota JS, Lowe LE, et al. Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. J Infect Dis. 2005;192:1686-1693.
11. Centers for Disease Control and Prevention (CDC). Progress toward elimination of Haemophilus influenza type b invasive disease among infants and children—United States, 1998-2000. MMWR Morb Mortal Wkly Rep. 2002;51:234-237.
12. Centers for Disease Control and Prevention (CDC). Epidemiology and Prevention of Vaccine-Preventable Diseases. The Pink Book, Course Textbook, 12th ed. Haemophilus influenzae type b. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/hib.html. Accessed March 4, 2012.
13. Watt JP, Wolfson LJ, O’Brien KL, et al; Hib and Pneumococcal Global Burden of Disease Study Team. Burden of disease caused by Haemophilus influenzae type b in children younger than 5 years: global estimates. Lancet. 2009;374:903-911.
14. Agrawal A, Murphy TF. Haemophilus influenzae infections in the H. influenzae type b conjugate vaccine era. J Clin Microbiol. 2011;49:3728-3732.
15. Chandran A, Watt JP, Santosham M. Prevention of Haemophilus influenza type b disease: past successes and future challenges. Informa Healthcare. 2005;4:819-827.
16. Centers for Disease Control and Prevention (CDC). Invasive Haemophilus influenza Type B disease in five young children--Minnesota, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:58-60.
17. McVernon J, Morgan P, Mallaghan C, et al. Outbreak of Haemophilus influenzae type b disease among fully vaccinated children in a day-care center. Pediatr Infect Dis J. 2004;23:38-41.
18. Hinman AR, Orenstein WA, Schuchat A; Centers for Disease Control and Prevention (CDC). Vaccine-preventable diseases, immunizations, and MMWR—1961-2011. MMWR Morb Mortal Wkly Rep. 2011;60 suppl 4:49-57.
19. Kempe A, Daley MF, McCauley MM, et al. Prevalence of parental concerns about childhood vaccines: the experience of primary care physicians. Am J Prev Med. 2011;40:548-555.
20. Godlee F, Smith J, Marcovitch H. Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ. 2011;342:c7452.
21. Institute for Vaccine Safety. Thimerosal content in some US Licensed vaccines. Institute for Vaccine Safety Web site. Available at: http://www.vaccinesafety.edu/thi-table.htm. Accessed March 8, 2012.
22. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention: Immunization safety and autism. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccinesafety/00_pdf/CDCStudiesonVaccinesandAutism.pdf. Accessed September 23, 2013.
23. Centers for Disease Control and Prevention. Ensuring the safety of vaccines in the United States. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/hcp/patient-ed/conversations/downloads/vacsafe-ensuring-color-office.pdf. Accessed November 18, 2014.
24. Wharton M. Vaccine safety: current systems and recent findings. Curr Opin Pediatr. 2010;22:88-93.
25. US Food and Drug Administration. Understanding the Vaccine Adverse Event Reporting System (VAERS). US Food and Drug Administration Web site. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/SafetyAvailability/VaccineSafety/UCM298183.pdf. Accessed October 15, 2014.
26. Centers for Disease Control and Prevention (CDC). Suspension of rotavirus vaccine after reports of intussusception--United States, 1999. MMWR Morb Mortal Wkly Rep. 2004;53:786-789.
27. Greene SK, Kulldorff M, Lewis EM, et al. Near real-time surveillance for influenza vaccine safety: proof-of-concept in the Vaccine Safety Datalink Project. Am J Epidemiol. 2010;171:177-188.
28. Iskander J, Broder K. Monitoring the safety of annual and pandemic influenza vaccines: lessons from the US experience. Expert Rev Vaccines. 2008;7:75-82.
29. Klein NP, Fireman B, Yih WK, et al. Measles-mumps-rubella-varicella combination vaccine and the risk of febrile seizures. Pediatrics. 2010;126:e1-e8.
30. DeStefano F, Price CS, Weintraub ES. Increasing exposure to antibody-stimulating proteins and polysaccharides in vaccines is not associated with risk of autism. J Pediatr. 2013;163:561-567.
31. Centers for Disease Control and Prevention (CDC). Epidemiology and prevention of vaccine-preventable diseases. The Pink Book, Course Textbook, 12th ed. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/safety.html. Accessed November 17, 2014.
32. World Health Organization (WHO). Measles outbreak in Europe. Global alert and response. Available at: http://www.who.int/csr/don/2011_04_21/en/index.html. Accessed March 8, 2012.
1. Zhou F, Shefer A, Wenger J, et al. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014;133:577-585.
2. Centers for Disease Control and Prevention. Measles. Epidemiology and prevention of vaccine-preventable diseases. The Pink Book: Course Textbook. 12th ed. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/meas.html. Accessed March 4, 2012.
3. Centers for Disease Control and Prevention. Measles (Rubeola). Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/measles/. Accessed November 19, 2014.
4. Measles. In: Pickering LK, Baker CJ, Kimberlin DW, et al, eds. Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009:444-455.
5. Atkinson WL, Orenstein WA, Krugman S. The resurgence of measles in the United States, 1989-1990. Annu Rev Med. 1992;43:451-463.
6. Centers for Disease Control and Prevention (CDC). Measles--United States, 1990. MMWR Morb Mortal Wkly Rep. 1991;40:369-372.
7. Gindler J, Tinker S, Markowitz L, et al. Acute measles mortality in the United States, 1987-2002. J Infect Dis. 2004;189(suppl 1): S69-S77.
8. Centers for Disease Control and Prevention (CDC). Measles: United States, January-May 20, 2011. MMWR Morb Mortal Wkly Rep. 2011;60:666-668.
9. Bernstein DI, Reuman PD, Schiff GM. Rubeola (measles) and subacute sclerosing panencephalitis virus. In: Gorbach SL, Bartlett JG, Blacklow NR (eds). Infectious Diseases. Philadelphia, PA: WB Saunders; 1998:2135.
10. Bellini WJ, Rota JS, Lowe LE, et al. Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. J Infect Dis. 2005;192:1686-1693.
11. Centers for Disease Control and Prevention (CDC). Progress toward elimination of Haemophilus influenza type b invasive disease among infants and children—United States, 1998-2000. MMWR Morb Mortal Wkly Rep. 2002;51:234-237.
12. Centers for Disease Control and Prevention (CDC). Epidemiology and Prevention of Vaccine-Preventable Diseases. The Pink Book, Course Textbook, 12th ed. Haemophilus influenzae type b. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/hib.html. Accessed March 4, 2012.
13. Watt JP, Wolfson LJ, O’Brien KL, et al; Hib and Pneumococcal Global Burden of Disease Study Team. Burden of disease caused by Haemophilus influenzae type b in children younger than 5 years: global estimates. Lancet. 2009;374:903-911.
14. Agrawal A, Murphy TF. Haemophilus influenzae infections in the H. influenzae type b conjugate vaccine era. J Clin Microbiol. 2011;49:3728-3732.
15. Chandran A, Watt JP, Santosham M. Prevention of Haemophilus influenza type b disease: past successes and future challenges. Informa Healthcare. 2005;4:819-827.
16. Centers for Disease Control and Prevention (CDC). Invasive Haemophilus influenza Type B disease in five young children--Minnesota, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:58-60.
17. McVernon J, Morgan P, Mallaghan C, et al. Outbreak of Haemophilus influenzae type b disease among fully vaccinated children in a day-care center. Pediatr Infect Dis J. 2004;23:38-41.
18. Hinman AR, Orenstein WA, Schuchat A; Centers for Disease Control and Prevention (CDC). Vaccine-preventable diseases, immunizations, and MMWR—1961-2011. MMWR Morb Mortal Wkly Rep. 2011;60 suppl 4:49-57.
19. Kempe A, Daley MF, McCauley MM, et al. Prevalence of parental concerns about childhood vaccines: the experience of primary care physicians. Am J Prev Med. 2011;40:548-555.
20. Godlee F, Smith J, Marcovitch H. Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ. 2011;342:c7452.
21. Institute for Vaccine Safety. Thimerosal content in some US Licensed vaccines. Institute for Vaccine Safety Web site. Available at: http://www.vaccinesafety.edu/thi-table.htm. Accessed March 8, 2012.
22. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention: Immunization safety and autism. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccinesafety/00_pdf/CDCStudiesonVaccinesandAutism.pdf. Accessed September 23, 2013.
23. Centers for Disease Control and Prevention. Ensuring the safety of vaccines in the United States. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/hcp/patient-ed/conversations/downloads/vacsafe-ensuring-color-office.pdf. Accessed November 18, 2014.
24. Wharton M. Vaccine safety: current systems and recent findings. Curr Opin Pediatr. 2010;22:88-93.
25. US Food and Drug Administration. Understanding the Vaccine Adverse Event Reporting System (VAERS). US Food and Drug Administration Web site. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/SafetyAvailability/VaccineSafety/UCM298183.pdf. Accessed October 15, 2014.
26. Centers for Disease Control and Prevention (CDC). Suspension of rotavirus vaccine after reports of intussusception--United States, 1999. MMWR Morb Mortal Wkly Rep. 2004;53:786-789.
27. Greene SK, Kulldorff M, Lewis EM, et al. Near real-time surveillance for influenza vaccine safety: proof-of-concept in the Vaccine Safety Datalink Project. Am J Epidemiol. 2010;171:177-188.
28. Iskander J, Broder K. Monitoring the safety of annual and pandemic influenza vaccines: lessons from the US experience. Expert Rev Vaccines. 2008;7:75-82.
29. Klein NP, Fireman B, Yih WK, et al. Measles-mumps-rubella-varicella combination vaccine and the risk of febrile seizures. Pediatrics. 2010;126:e1-e8.
30. DeStefano F, Price CS, Weintraub ES. Increasing exposure to antibody-stimulating proteins and polysaccharides in vaccines is not associated with risk of autism. J Pediatr. 2013;163:561-567.
31. Centers for Disease Control and Prevention (CDC). Epidemiology and prevention of vaccine-preventable diseases. The Pink Book, Course Textbook, 12th ed. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/safety.html. Accessed November 17, 2014.
32. World Health Organization (WHO). Measles outbreak in Europe. Global alert and response. Available at: http://www.who.int/csr/don/2011_04_21/en/index.html. Accessed March 8, 2012.