User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Dr. Judy C. Washington shows URM physicians how to lead
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
Booster shot back-and-forth creates uncertainty, confusion
Many people are confused — patients and healthcare providers alike — in the wake of the U.S. Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) announcements about who is authorized to get a third or ‘booster’ shot of the Pfizer/BioNTech COVID-19 vaccine.
, healthcare providers report. At the same time, the uncertainty from changing federal messages about boosters is causing some chaos, especially in the form of vaccine misinformation.
The confusion started, in part, with the August 13 announcement that immunocompromised Americans were eligible for a booster shot. Next came the initial Biden administration intention to provide most U.S. adults with a third shot starting September 20 — an announcement later rolled back — followed by the Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) limiting boosters to select groups last week.
“It was only 3% of the population that was going to be getting a third dose, then it was back to everyone being able to get the booster, and then it’s back to a select crew,” Louito Edje, MD, a family physician in private practice in Cincinnati, said in an interview with this news organization.
This kind of mixed messaging is generating more questions than answers.
“Even though that is following the science, translating the science into policy, it’s really fraught with confusion for patients, especially,” added Dr. Edje, professor educator in the departments of medical education and family and community medicine at UC Health and a fellow of the American Academy of Family Physicians.
When asked if he’s seeing more uncertainty about boosters, community pharmacist Brian Caswell, RPh, said: “I’m going to have to say yes because I’ve been confused myself at times.”
“Yes, there is a lot of confusion,” added Mr. Caswell, owner or co-owner of four pharmacies in Kansas and Missouri and president of the National Community Pharmacists Association.
Boosting misinformation?
“Unfortunately, confusion leads to an acceleration of misinformation,” Mr. Caswell said.
Dr. Edje shared an example. “The folks who have been hesitant to even get the first vaccine appear now a little less likely to want to go ahead and get vaccinated.”
These patients point to breakthrough COVID-19 cases of the Delta variant, which “reinforces that they don’t need to get vaccinated in the first place,” Dr. Edje said.
“That’s unfortunate because it’s a complete fallacy.”
Clearer communication from the federal government could help alleviate confusion, Mr. Caswell said. “I would like to see an official CDC chart that states who is eligible as of a certain date. Something that is accessible through their webpage or a social media source that can be updated. That would help all of us.”
“For myself, I’ve got patients from Kansas, Oklahoma, and Missouri that might be operating under different guidelines. That makes it even more confusing,” he said.
More clarity is needed for individuals seeking boosters as well. “It would help to be very clear with the general public, who are becoming very knowledgeable within this vaccine realm,” Mr. Caswell said.
‘Gaming the system’
Although most people seeking a booster shot at one of Caswell’s pharmacies are following official recommendations, there are some who remain ineligible but nonetheless come in for an additional vaccine.
“Even before this announcement last Friday, in the latter part of August when the CDC talked about a booster for immunocompromised, we had interest from people who did not meet the criteria,” Mr. Caswell said.
To the ineligible, he and his staff explain the approval process, why certain decisions are made, and point out that the number of eligible Americans is likely to expand in the future.
“The vast majority of them are understanding,” Mr. Caswell said. “But we’ve had some people who really didn’t want to accept the information, and I don’t know what they’ve done.”
“Some people are gaming the system to get their booster or second shot of J&J,” he said.
For example, Mr. Caswell had a patient who crossed over state lines from Missouri seeking a vaccine booster at Wolkar Drug, a pharmacy in Baxter Springs, Kan. “We found out later he had a J&J shot at a facility or provider in Missouri. He came over to Kansas, signed up for it and got a booster with Moderna.”
“We called and asked him if he was aware of it. He said, ‘yes.’ When we questioned him more about it, he hung up.”
Dr. Edje is likewise seeing interest from some ineligible patients, she said.
Crossing a liability line?
Mr. Caswell has asked for advice from lawyers and the State Board of Pharmacy on potential liability if a pharmacist gives a booster to a patient not eligible under the official FDA and CDC guidance.
“We ask patients direct questions about whether they’ve had the COVID vaccine, COVID, and a whole litany of questions they must answer. And we’re assuming they are going to be honest and forthright,” he said. “The pharmacist needs to make sure they make every effort to get that information from the patient.”
Normally, healthcare providers like Mr. Caswell report each COVID-19 vaccination to the state registry after administration. “We have not gone through a police action and checked the registry first,” he said.
But, if people continue to try ‘gaming the system,’ he said, he might have to start checking the state registry before giving someone a booster.
The American Academy of Family Physicians offers advice from the CDC about legal protections for providers.
“As outlined by CDC, any off-label use of the Comirnaty/Pfizer-BioNTech COVID-19 vaccine is not authorized at this time and may not be covered under the PREP Act or the PREP Act declaration. This means that clinicians providing the vaccine outside of the authorized/approved use may not have immunity from claims,” the AAFP website states.
“Per CDC, individuals who receive a third dose may not be eligible for compensation after a possible adverse event. Such use would be in violation of the CDC COVID-19 vaccination program provider agreement and therefore may not be reimbursable and may impact the ability of a provider to remain in the CDC program, in addition to other potential sanctions. Administration fees for off-label doses may not be reimbursed by payers.”
Despite confusion, demand is up
Even amid all the uncertainty, there appears to be a jump in enthusiasm for the booster shots.
“The requests have gone up quite a bit. We’ve seen a number of requests from people in person and over the phone looking to get a booster,” Mr. Caswell said. “Since the discussion at the federal level...there has been a lot of interest in the third shot booster, itself, as well as about a booster for J&J.”
“There is quite a bit of excitement out there,” he said.
Dr. Edje agreed: “I take care of a fair number of folks...including the elderly and healthcare professionals. They are already asking for the booster.”
Interestingly, Dr. Edje would like to get a booster herself but is not eligible for the Pfizer third shot. She is a participant in a Moderna vaccine trial and can only receive additional immunization as part of the study.
‘Walk, don’t run’
To quell any potential early rush to get a third shot, U.S. health officials are reminding booster-ineligible people that they still have some protection against COVID-19.
“If you’re a person who ultimately might get a booster that will make you optimally protected, you don’t necessarily need to get it tomorrow,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases told CNN.
CDC Director Rochelle Walensky, MD, also weighed in. She told ABC that boosters for people who received a Moderna or Johnson & Johnson vaccine will be addressed with urgency.
“I want to reiterate that this is a very slow wane. There is no urgency here to go and get your booster immediately. You know, walk don’t run to your booster appointment,” she said.
“We will come and look at the data for Moderna and J&J in very short order.”
Dr. Edje and Mr. Caswell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Many people are confused — patients and healthcare providers alike — in the wake of the U.S. Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) announcements about who is authorized to get a third or ‘booster’ shot of the Pfizer/BioNTech COVID-19 vaccine.
, healthcare providers report. At the same time, the uncertainty from changing federal messages about boosters is causing some chaos, especially in the form of vaccine misinformation.
The confusion started, in part, with the August 13 announcement that immunocompromised Americans were eligible for a booster shot. Next came the initial Biden administration intention to provide most U.S. adults with a third shot starting September 20 — an announcement later rolled back — followed by the Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) limiting boosters to select groups last week.
“It was only 3% of the population that was going to be getting a third dose, then it was back to everyone being able to get the booster, and then it’s back to a select crew,” Louito Edje, MD, a family physician in private practice in Cincinnati, said in an interview with this news organization.
This kind of mixed messaging is generating more questions than answers.
“Even though that is following the science, translating the science into policy, it’s really fraught with confusion for patients, especially,” added Dr. Edje, professor educator in the departments of medical education and family and community medicine at UC Health and a fellow of the American Academy of Family Physicians.
When asked if he’s seeing more uncertainty about boosters, community pharmacist Brian Caswell, RPh, said: “I’m going to have to say yes because I’ve been confused myself at times.”
“Yes, there is a lot of confusion,” added Mr. Caswell, owner or co-owner of four pharmacies in Kansas and Missouri and president of the National Community Pharmacists Association.
Boosting misinformation?
“Unfortunately, confusion leads to an acceleration of misinformation,” Mr. Caswell said.
Dr. Edje shared an example. “The folks who have been hesitant to even get the first vaccine appear now a little less likely to want to go ahead and get vaccinated.”
These patients point to breakthrough COVID-19 cases of the Delta variant, which “reinforces that they don’t need to get vaccinated in the first place,” Dr. Edje said.
“That’s unfortunate because it’s a complete fallacy.”
Clearer communication from the federal government could help alleviate confusion, Mr. Caswell said. “I would like to see an official CDC chart that states who is eligible as of a certain date. Something that is accessible through their webpage or a social media source that can be updated. That would help all of us.”
“For myself, I’ve got patients from Kansas, Oklahoma, and Missouri that might be operating under different guidelines. That makes it even more confusing,” he said.
More clarity is needed for individuals seeking boosters as well. “It would help to be very clear with the general public, who are becoming very knowledgeable within this vaccine realm,” Mr. Caswell said.
‘Gaming the system’
Although most people seeking a booster shot at one of Caswell’s pharmacies are following official recommendations, there are some who remain ineligible but nonetheless come in for an additional vaccine.
“Even before this announcement last Friday, in the latter part of August when the CDC talked about a booster for immunocompromised, we had interest from people who did not meet the criteria,” Mr. Caswell said.
To the ineligible, he and his staff explain the approval process, why certain decisions are made, and point out that the number of eligible Americans is likely to expand in the future.
“The vast majority of them are understanding,” Mr. Caswell said. “But we’ve had some people who really didn’t want to accept the information, and I don’t know what they’ve done.”
“Some people are gaming the system to get their booster or second shot of J&J,” he said.
For example, Mr. Caswell had a patient who crossed over state lines from Missouri seeking a vaccine booster at Wolkar Drug, a pharmacy in Baxter Springs, Kan. “We found out later he had a J&J shot at a facility or provider in Missouri. He came over to Kansas, signed up for it and got a booster with Moderna.”
“We called and asked him if he was aware of it. He said, ‘yes.’ When we questioned him more about it, he hung up.”
Dr. Edje is likewise seeing interest from some ineligible patients, she said.
Crossing a liability line?
Mr. Caswell has asked for advice from lawyers and the State Board of Pharmacy on potential liability if a pharmacist gives a booster to a patient not eligible under the official FDA and CDC guidance.
“We ask patients direct questions about whether they’ve had the COVID vaccine, COVID, and a whole litany of questions they must answer. And we’re assuming they are going to be honest and forthright,” he said. “The pharmacist needs to make sure they make every effort to get that information from the patient.”
Normally, healthcare providers like Mr. Caswell report each COVID-19 vaccination to the state registry after administration. “We have not gone through a police action and checked the registry first,” he said.
But, if people continue to try ‘gaming the system,’ he said, he might have to start checking the state registry before giving someone a booster.
The American Academy of Family Physicians offers advice from the CDC about legal protections for providers.
“As outlined by CDC, any off-label use of the Comirnaty/Pfizer-BioNTech COVID-19 vaccine is not authorized at this time and may not be covered under the PREP Act or the PREP Act declaration. This means that clinicians providing the vaccine outside of the authorized/approved use may not have immunity from claims,” the AAFP website states.
“Per CDC, individuals who receive a third dose may not be eligible for compensation after a possible adverse event. Such use would be in violation of the CDC COVID-19 vaccination program provider agreement and therefore may not be reimbursable and may impact the ability of a provider to remain in the CDC program, in addition to other potential sanctions. Administration fees for off-label doses may not be reimbursed by payers.”
Despite confusion, demand is up
Even amid all the uncertainty, there appears to be a jump in enthusiasm for the booster shots.
“The requests have gone up quite a bit. We’ve seen a number of requests from people in person and over the phone looking to get a booster,” Mr. Caswell said. “Since the discussion at the federal level...there has been a lot of interest in the third shot booster, itself, as well as about a booster for J&J.”
“There is quite a bit of excitement out there,” he said.
Dr. Edje agreed: “I take care of a fair number of folks...including the elderly and healthcare professionals. They are already asking for the booster.”
Interestingly, Dr. Edje would like to get a booster herself but is not eligible for the Pfizer third shot. She is a participant in a Moderna vaccine trial and can only receive additional immunization as part of the study.
‘Walk, don’t run’
To quell any potential early rush to get a third shot, U.S. health officials are reminding booster-ineligible people that they still have some protection against COVID-19.
“If you’re a person who ultimately might get a booster that will make you optimally protected, you don’t necessarily need to get it tomorrow,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases told CNN.
CDC Director Rochelle Walensky, MD, also weighed in. She told ABC that boosters for people who received a Moderna or Johnson & Johnson vaccine will be addressed with urgency.
“I want to reiterate that this is a very slow wane. There is no urgency here to go and get your booster immediately. You know, walk don’t run to your booster appointment,” she said.
“We will come and look at the data for Moderna and J&J in very short order.”
Dr. Edje and Mr. Caswell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Many people are confused — patients and healthcare providers alike — in the wake of the U.S. Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) announcements about who is authorized to get a third or ‘booster’ shot of the Pfizer/BioNTech COVID-19 vaccine.
, healthcare providers report. At the same time, the uncertainty from changing federal messages about boosters is causing some chaos, especially in the form of vaccine misinformation.
The confusion started, in part, with the August 13 announcement that immunocompromised Americans were eligible for a booster shot. Next came the initial Biden administration intention to provide most U.S. adults with a third shot starting September 20 — an announcement later rolled back — followed by the Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) limiting boosters to select groups last week.
“It was only 3% of the population that was going to be getting a third dose, then it was back to everyone being able to get the booster, and then it’s back to a select crew,” Louito Edje, MD, a family physician in private practice in Cincinnati, said in an interview with this news organization.
This kind of mixed messaging is generating more questions than answers.
“Even though that is following the science, translating the science into policy, it’s really fraught with confusion for patients, especially,” added Dr. Edje, professor educator in the departments of medical education and family and community medicine at UC Health and a fellow of the American Academy of Family Physicians.
When asked if he’s seeing more uncertainty about boosters, community pharmacist Brian Caswell, RPh, said: “I’m going to have to say yes because I’ve been confused myself at times.”
“Yes, there is a lot of confusion,” added Mr. Caswell, owner or co-owner of four pharmacies in Kansas and Missouri and president of the National Community Pharmacists Association.
Boosting misinformation?
“Unfortunately, confusion leads to an acceleration of misinformation,” Mr. Caswell said.
Dr. Edje shared an example. “The folks who have been hesitant to even get the first vaccine appear now a little less likely to want to go ahead and get vaccinated.”
These patients point to breakthrough COVID-19 cases of the Delta variant, which “reinforces that they don’t need to get vaccinated in the first place,” Dr. Edje said.
“That’s unfortunate because it’s a complete fallacy.”
Clearer communication from the federal government could help alleviate confusion, Mr. Caswell said. “I would like to see an official CDC chart that states who is eligible as of a certain date. Something that is accessible through their webpage or a social media source that can be updated. That would help all of us.”
“For myself, I’ve got patients from Kansas, Oklahoma, and Missouri that might be operating under different guidelines. That makes it even more confusing,” he said.
More clarity is needed for individuals seeking boosters as well. “It would help to be very clear with the general public, who are becoming very knowledgeable within this vaccine realm,” Mr. Caswell said.
‘Gaming the system’
Although most people seeking a booster shot at one of Caswell’s pharmacies are following official recommendations, there are some who remain ineligible but nonetheless come in for an additional vaccine.
“Even before this announcement last Friday, in the latter part of August when the CDC talked about a booster for immunocompromised, we had interest from people who did not meet the criteria,” Mr. Caswell said.
To the ineligible, he and his staff explain the approval process, why certain decisions are made, and point out that the number of eligible Americans is likely to expand in the future.
“The vast majority of them are understanding,” Mr. Caswell said. “But we’ve had some people who really didn’t want to accept the information, and I don’t know what they’ve done.”
“Some people are gaming the system to get their booster or second shot of J&J,” he said.
For example, Mr. Caswell had a patient who crossed over state lines from Missouri seeking a vaccine booster at Wolkar Drug, a pharmacy in Baxter Springs, Kan. “We found out later he had a J&J shot at a facility or provider in Missouri. He came over to Kansas, signed up for it and got a booster with Moderna.”
“We called and asked him if he was aware of it. He said, ‘yes.’ When we questioned him more about it, he hung up.”
Dr. Edje is likewise seeing interest from some ineligible patients, she said.
Crossing a liability line?
Mr. Caswell has asked for advice from lawyers and the State Board of Pharmacy on potential liability if a pharmacist gives a booster to a patient not eligible under the official FDA and CDC guidance.
“We ask patients direct questions about whether they’ve had the COVID vaccine, COVID, and a whole litany of questions they must answer. And we’re assuming they are going to be honest and forthright,” he said. “The pharmacist needs to make sure they make every effort to get that information from the patient.”
Normally, healthcare providers like Mr. Caswell report each COVID-19 vaccination to the state registry after administration. “We have not gone through a police action and checked the registry first,” he said.
But, if people continue to try ‘gaming the system,’ he said, he might have to start checking the state registry before giving someone a booster.
The American Academy of Family Physicians offers advice from the CDC about legal protections for providers.
“As outlined by CDC, any off-label use of the Comirnaty/Pfizer-BioNTech COVID-19 vaccine is not authorized at this time and may not be covered under the PREP Act or the PREP Act declaration. This means that clinicians providing the vaccine outside of the authorized/approved use may not have immunity from claims,” the AAFP website states.
“Per CDC, individuals who receive a third dose may not be eligible for compensation after a possible adverse event. Such use would be in violation of the CDC COVID-19 vaccination program provider agreement and therefore may not be reimbursable and may impact the ability of a provider to remain in the CDC program, in addition to other potential sanctions. Administration fees for off-label doses may not be reimbursed by payers.”
Despite confusion, demand is up
Even amid all the uncertainty, there appears to be a jump in enthusiasm for the booster shots.
“The requests have gone up quite a bit. We’ve seen a number of requests from people in person and over the phone looking to get a booster,” Mr. Caswell said. “Since the discussion at the federal level...there has been a lot of interest in the third shot booster, itself, as well as about a booster for J&J.”
“There is quite a bit of excitement out there,” he said.
Dr. Edje agreed: “I take care of a fair number of folks...including the elderly and healthcare professionals. They are already asking for the booster.”
Interestingly, Dr. Edje would like to get a booster herself but is not eligible for the Pfizer third shot. She is a participant in a Moderna vaccine trial and can only receive additional immunization as part of the study.
‘Walk, don’t run’
To quell any potential early rush to get a third shot, U.S. health officials are reminding booster-ineligible people that they still have some protection against COVID-19.
“If you’re a person who ultimately might get a booster that will make you optimally protected, you don’t necessarily need to get it tomorrow,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases told CNN.
CDC Director Rochelle Walensky, MD, also weighed in. She told ABC that boosters for people who received a Moderna or Johnson & Johnson vaccine will be addressed with urgency.
“I want to reiterate that this is a very slow wane. There is no urgency here to go and get your booster immediately. You know, walk don’t run to your booster appointment,” she said.
“We will come and look at the data for Moderna and J&J in very short order.”
Dr. Edje and Mr. Caswell have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cook your amphibians before you eat them
Novel food for thought
When you were growing up, your parents probably told you to brush your teeth before you went to bed, warned you not to run with the scissors or play with matches, and punished you whenever you used the neighbor children to play Schrödinger’s cat.
They did those things for your own good, of course, and now the nation’s mother – the Centers for Disease Control and Prevention – is doing the same by warning us about novel outbreak–associated foods. As in, “Put down that novel outbreak–associated food! You don’t know where it’s been!”
Seriously, you don’t know where it’s been. CDC investigators identified 28 novel foods that were linked to 36 foodborne-disease outbreaks that occurred during 2007-2016, including moringa leaf (herb/spice), tempeh (grain), frog, sprouted nut butter, and skate.
The novel foods implicated in these outbreaks were more likely to be imported, compared with 14,216 outbreaks that occurred from 1973 to 2016, and about half didn’t require refrigeration. Two-thirds did not need to be cooked after purchase. Another thing your parents wouldn’t like: Some can’t be washed, like sheep milk, sugar cane, or the aforementioned nut butter.
We wanted to get a food expert to comment on these novel foods, but our editor said that the assistant manager of our local Burger King wasn’t expert enough, so we’ve commandeered someone else’s expert. Cynthia Sears, MD, of Johns Hopkins University in Baltimore, told Today.com all about the dangers of frogs: “Essentially all amphibians are contaminated, often with salmonella. Eating any amphibian that is not thoroughly cooked is a risk.”
Be sure to cook your amphibians before you eat them. Advice that your parents would be proud to share.
Dieters should stay away from diet drinks
When a drink is labeled “diet” many assume that the calorie-free beverage is the best choice. However, one of the largest studies to date on artificial sweeteners is out to set the record straight.
Artificial sweeteners, or nonnutritive sweeteners (NNS), are used in most if not all diet products to give the illusion of sweetness without the caloric guilt. Some studies say they help with weight loss for that very reason, but others say they can contribute to weight gain. So which is it?
Researchers at the University of Southern California sought to add some clarity to the research already out there.
They looked at an even-gendered split of 74 participants who drank 300 mL of drinks sweetened with NNS, table sugar, or water. The researchers then used functional MRI to see how parts of the brain responsible for appetite and cravings responded to images of high-calorie foods. They also looked at glucose, insulin, and other metabolic hormone levels, as well as how much food the participants ate at their free buffet. (In the participants’ defense, who can say no to a free buffet?)
The researchers made some interesting observations:
- Women who drank the NNS drink ate more than did the table-sugar group, but all men ate the same.
- Images of those calorie-packed goodies increased cravings and appetite for obese men and women in the NNS group, compared with the table-sugar group.
- For all participants who drank the NNS drink, there was a decrease in the hormone that tells the body it’s full.
“By studying different groups we were able to show that females and people with obesity may be more sensitive to artificial sweeteners. For these groups, drinking artificially sweetened drinks may trick the brain into feeling hungry, which may in turn result in more calories being consumed,” Kathleen Page, MD, the study’s corresponding author, said in a separate statement.
Today’s lesson? Don’t believe every label you read.
Instagram vegetables and the triumph of peer pressure
You and your family are sitting down for dinner. You’ve taken the time to prepare a healthy, nutritious meal. Vegetables, rice, seafood – all the right things. But the children around you refuse to partake. What can you do? Why, show them a highly liked photo of broccoli on Instagram!
In reality, kids will probably never like to eat their vegetables, but according to a study published in Appetite, viewing highly liked images on social media can compel adults to eat theirs.
The investigators recruited a group of 169 adults aged 18-28 (average age, 21) and showed them a series of mock Instagram posts of all sorts of food, everything from Brussels sprouts to chocolate cake, as well as nonfood images to act as a baseline. The images had a varying amount of likes. After viewing the images, study participants were offered a snack buffet consisting of grapes and cookies.
The results were a triumph of peer pressure. Those who viewed highly liked images of nutritious foods ate a significantly larger proportion of grapes, compared with those who saw highly liked images of unhealthy food or nonfood.
The authors cautioned that more research is needed, but they said that they’re onto something in the eternal struggle of getting people to eat better. If Mikey liked it, maybe you should, too. Just as long as you don’t try to encourage the eating of peas. That is a dark road none should take, and no one should ever be subjected to that cursed food.
It’s nice to share … hypertension?
You may have heard that, over time, you begin to resemble your spouse. You may have also heard that, as time goes by, your pet might start to resemble you, but that is a story for another time.
A lot of the time, it’s human nature that people partner with someone who is similar to them in physical and environmental status. If you like to go jogging at 5 a.m., you might want a spouse who does the same. A study done using data from couples in Japan and the Netherlands found that couples who had the same lifestyle had similar levels of blood pressure, cholesterol, and triglycerides. They also had similar illnesses such as hypertension and diabetes.
It’s important to note that many of the couples were not very genetically similar but had similar lifestyles. Encourage your partner to have a healthier lifestyle, so you can live on for many years to come!
Novel food for thought
When you were growing up, your parents probably told you to brush your teeth before you went to bed, warned you not to run with the scissors or play with matches, and punished you whenever you used the neighbor children to play Schrödinger’s cat.
They did those things for your own good, of course, and now the nation’s mother – the Centers for Disease Control and Prevention – is doing the same by warning us about novel outbreak–associated foods. As in, “Put down that novel outbreak–associated food! You don’t know where it’s been!”
Seriously, you don’t know where it’s been. CDC investigators identified 28 novel foods that were linked to 36 foodborne-disease outbreaks that occurred during 2007-2016, including moringa leaf (herb/spice), tempeh (grain), frog, sprouted nut butter, and skate.
The novel foods implicated in these outbreaks were more likely to be imported, compared with 14,216 outbreaks that occurred from 1973 to 2016, and about half didn’t require refrigeration. Two-thirds did not need to be cooked after purchase. Another thing your parents wouldn’t like: Some can’t be washed, like sheep milk, sugar cane, or the aforementioned nut butter.
We wanted to get a food expert to comment on these novel foods, but our editor said that the assistant manager of our local Burger King wasn’t expert enough, so we’ve commandeered someone else’s expert. Cynthia Sears, MD, of Johns Hopkins University in Baltimore, told Today.com all about the dangers of frogs: “Essentially all amphibians are contaminated, often with salmonella. Eating any amphibian that is not thoroughly cooked is a risk.”
Be sure to cook your amphibians before you eat them. Advice that your parents would be proud to share.
Dieters should stay away from diet drinks
When a drink is labeled “diet” many assume that the calorie-free beverage is the best choice. However, one of the largest studies to date on artificial sweeteners is out to set the record straight.
Artificial sweeteners, or nonnutritive sweeteners (NNS), are used in most if not all diet products to give the illusion of sweetness without the caloric guilt. Some studies say they help with weight loss for that very reason, but others say they can contribute to weight gain. So which is it?
Researchers at the University of Southern California sought to add some clarity to the research already out there.
They looked at an even-gendered split of 74 participants who drank 300 mL of drinks sweetened with NNS, table sugar, or water. The researchers then used functional MRI to see how parts of the brain responsible for appetite and cravings responded to images of high-calorie foods. They also looked at glucose, insulin, and other metabolic hormone levels, as well as how much food the participants ate at their free buffet. (In the participants’ defense, who can say no to a free buffet?)
The researchers made some interesting observations:
- Women who drank the NNS drink ate more than did the table-sugar group, but all men ate the same.
- Images of those calorie-packed goodies increased cravings and appetite for obese men and women in the NNS group, compared with the table-sugar group.
- For all participants who drank the NNS drink, there was a decrease in the hormone that tells the body it’s full.
“By studying different groups we were able to show that females and people with obesity may be more sensitive to artificial sweeteners. For these groups, drinking artificially sweetened drinks may trick the brain into feeling hungry, which may in turn result in more calories being consumed,” Kathleen Page, MD, the study’s corresponding author, said in a separate statement.
Today’s lesson? Don’t believe every label you read.
Instagram vegetables and the triumph of peer pressure
You and your family are sitting down for dinner. You’ve taken the time to prepare a healthy, nutritious meal. Vegetables, rice, seafood – all the right things. But the children around you refuse to partake. What can you do? Why, show them a highly liked photo of broccoli on Instagram!
In reality, kids will probably never like to eat their vegetables, but according to a study published in Appetite, viewing highly liked images on social media can compel adults to eat theirs.
The investigators recruited a group of 169 adults aged 18-28 (average age, 21) and showed them a series of mock Instagram posts of all sorts of food, everything from Brussels sprouts to chocolate cake, as well as nonfood images to act as a baseline. The images had a varying amount of likes. After viewing the images, study participants were offered a snack buffet consisting of grapes and cookies.
The results were a triumph of peer pressure. Those who viewed highly liked images of nutritious foods ate a significantly larger proportion of grapes, compared with those who saw highly liked images of unhealthy food or nonfood.
The authors cautioned that more research is needed, but they said that they’re onto something in the eternal struggle of getting people to eat better. If Mikey liked it, maybe you should, too. Just as long as you don’t try to encourage the eating of peas. That is a dark road none should take, and no one should ever be subjected to that cursed food.
It’s nice to share … hypertension?
You may have heard that, over time, you begin to resemble your spouse. You may have also heard that, as time goes by, your pet might start to resemble you, but that is a story for another time.
A lot of the time, it’s human nature that people partner with someone who is similar to them in physical and environmental status. If you like to go jogging at 5 a.m., you might want a spouse who does the same. A study done using data from couples in Japan and the Netherlands found that couples who had the same lifestyle had similar levels of blood pressure, cholesterol, and triglycerides. They also had similar illnesses such as hypertension and diabetes.
It’s important to note that many of the couples were not very genetically similar but had similar lifestyles. Encourage your partner to have a healthier lifestyle, so you can live on for many years to come!
Novel food for thought
When you were growing up, your parents probably told you to brush your teeth before you went to bed, warned you not to run with the scissors or play with matches, and punished you whenever you used the neighbor children to play Schrödinger’s cat.
They did those things for your own good, of course, and now the nation’s mother – the Centers for Disease Control and Prevention – is doing the same by warning us about novel outbreak–associated foods. As in, “Put down that novel outbreak–associated food! You don’t know where it’s been!”
Seriously, you don’t know where it’s been. CDC investigators identified 28 novel foods that were linked to 36 foodborne-disease outbreaks that occurred during 2007-2016, including moringa leaf (herb/spice), tempeh (grain), frog, sprouted nut butter, and skate.
The novel foods implicated in these outbreaks were more likely to be imported, compared with 14,216 outbreaks that occurred from 1973 to 2016, and about half didn’t require refrigeration. Two-thirds did not need to be cooked after purchase. Another thing your parents wouldn’t like: Some can’t be washed, like sheep milk, sugar cane, or the aforementioned nut butter.
We wanted to get a food expert to comment on these novel foods, but our editor said that the assistant manager of our local Burger King wasn’t expert enough, so we’ve commandeered someone else’s expert. Cynthia Sears, MD, of Johns Hopkins University in Baltimore, told Today.com all about the dangers of frogs: “Essentially all amphibians are contaminated, often with salmonella. Eating any amphibian that is not thoroughly cooked is a risk.”
Be sure to cook your amphibians before you eat them. Advice that your parents would be proud to share.
Dieters should stay away from diet drinks
When a drink is labeled “diet” many assume that the calorie-free beverage is the best choice. However, one of the largest studies to date on artificial sweeteners is out to set the record straight.
Artificial sweeteners, or nonnutritive sweeteners (NNS), are used in most if not all diet products to give the illusion of sweetness without the caloric guilt. Some studies say they help with weight loss for that very reason, but others say they can contribute to weight gain. So which is it?
Researchers at the University of Southern California sought to add some clarity to the research already out there.
They looked at an even-gendered split of 74 participants who drank 300 mL of drinks sweetened with NNS, table sugar, or water. The researchers then used functional MRI to see how parts of the brain responsible for appetite and cravings responded to images of high-calorie foods. They also looked at glucose, insulin, and other metabolic hormone levels, as well as how much food the participants ate at their free buffet. (In the participants’ defense, who can say no to a free buffet?)
The researchers made some interesting observations:
- Women who drank the NNS drink ate more than did the table-sugar group, but all men ate the same.
- Images of those calorie-packed goodies increased cravings and appetite for obese men and women in the NNS group, compared with the table-sugar group.
- For all participants who drank the NNS drink, there was a decrease in the hormone that tells the body it’s full.
“By studying different groups we were able to show that females and people with obesity may be more sensitive to artificial sweeteners. For these groups, drinking artificially sweetened drinks may trick the brain into feeling hungry, which may in turn result in more calories being consumed,” Kathleen Page, MD, the study’s corresponding author, said in a separate statement.
Today’s lesson? Don’t believe every label you read.
Instagram vegetables and the triumph of peer pressure
You and your family are sitting down for dinner. You’ve taken the time to prepare a healthy, nutritious meal. Vegetables, rice, seafood – all the right things. But the children around you refuse to partake. What can you do? Why, show them a highly liked photo of broccoli on Instagram!
In reality, kids will probably never like to eat their vegetables, but according to a study published in Appetite, viewing highly liked images on social media can compel adults to eat theirs.
The investigators recruited a group of 169 adults aged 18-28 (average age, 21) and showed them a series of mock Instagram posts of all sorts of food, everything from Brussels sprouts to chocolate cake, as well as nonfood images to act as a baseline. The images had a varying amount of likes. After viewing the images, study participants were offered a snack buffet consisting of grapes and cookies.
The results were a triumph of peer pressure. Those who viewed highly liked images of nutritious foods ate a significantly larger proportion of grapes, compared with those who saw highly liked images of unhealthy food or nonfood.
The authors cautioned that more research is needed, but they said that they’re onto something in the eternal struggle of getting people to eat better. If Mikey liked it, maybe you should, too. Just as long as you don’t try to encourage the eating of peas. That is a dark road none should take, and no one should ever be subjected to that cursed food.
It’s nice to share … hypertension?
You may have heard that, over time, you begin to resemble your spouse. You may have also heard that, as time goes by, your pet might start to resemble you, but that is a story for another time.
A lot of the time, it’s human nature that people partner with someone who is similar to them in physical and environmental status. If you like to go jogging at 5 a.m., you might want a spouse who does the same. A study done using data from couples in Japan and the Netherlands found that couples who had the same lifestyle had similar levels of blood pressure, cholesterol, and triglycerides. They also had similar illnesses such as hypertension and diabetes.
It’s important to note that many of the couples were not very genetically similar but had similar lifestyles. Encourage your partner to have a healthier lifestyle, so you can live on for many years to come!
Greater portal use gives patients access, doctors headaches
The use of patient portals that provide access to electronic health records has dramatically increased in the past several years, and patients whose health care practitioner encouraged them to use their online portal accessed them at a higher rate than those who were not encouraged to do so.
These were among the top-line results of a national survey of U.S. adults conducted by the National Institutes of Health from January 2020 to April 2020. Although the COVID-19 pandemic hit the United States in the middle of that period, a report on the survey by the Office of the National Coordinator for Health IT stated, “These findings largely reflect prepandemic rates of individuals being offered and subsequently using their online medical record, also known as a patient portal.”
But with more patient access can come additional work for physicians and other health care practitioners, ranging from an onslaught of patient communications to managing data sent to them by patients.
According to the report, 59% of individuals were offered access to their patient portal, and 38% accessed their record at least once in 2020. By comparison, in 2014, just 42% were offered access to their portal, and 25% used it. But these percentages hardly changed from 2019 to 2020.
The increase in the percentage of people who accessed portals reflects the fact that more people were offered access. In addition, there were signs of rising activity among portal users.
Among patients offered access to their patient portal, 64% accessed it at least once in 2020 – 11 percentage points more than in 2017. Twenty-seven percent of those who had access to a portal used it once or twice; 20% accessed it three to five times; and 18% used it six or more times. The latter two percentages were significantly higher than in 2017.
Of the respondents who were offered access to portals but didn’t use them, 69% said they didn’t access the portal because they preferred to speak with their health care practitioner directly. Sixty-three percent said they didn’t see a need to use their online medical record. This was similar to the percentage 3 years earlier. Other reasons included respondents’ concerns about the privacy/security of online medical records (24%), their lack of comfort with computers (20%), and their lack of Internet access (13%).
The pros and cons of patient portals, greater access
Among portal users who accessed their records through a mobile health app, 51% used the app to facilitate discussions with their health care practitioner in 2020, an 8–percentage point increase from 2017. Fifty-percent of the mobile health app users utilized it to make a decision about how to treat an illness or condition, up from 45% in 2017. And 71% of these individuals used their app to track progress on a health-related goal, just a bit more than in 2017.
Individuals who were encouraged by their health care practitioner to use their patient portal viewed clinical notes and exchanged secure messages with their practitioner at higher rates than those who had not been encouraged. This is not surprising, but it reflects an unintended result of patient portals that many physicians have found burdensome, especially during the pandemic: overflowing electronic in-boxes.
Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, recently tweeted, “We’re seeing huge uptick in in-box messages for MDs during COVID – now seems like biggest driver of MD burnout. The fundamental problem: We turned on 24/7/365 access for patients (who of course like it) with no operational or business model to handle it. Crucial that we fix this.”
Steven Waldren, MD, vice president and chief medical informatics officer at the American Academy of Family Physicians, told this news organization that he agrees that this is a major challenge. “In-box management is a burden on physicians and practices,” he said. “However, it can be done better, either through a team in-box or through better use of technology.”
The team in-box he refers to is a mechanism for triaging patient messages. For example, a triage nurse can look at the messages and decide which ones can be handled by staff and which ones the doctor needs to see. Or physicians and front office staff can see the messages at the same time; a nurse can triage some messages according to protocols, and the physician can respond to any message, depending on what he or she knows about the patient.
Technology can also be enlisted in the effort, he suggested, perhaps by automating the triaging of messages such as prescription refill requests or using artificial intelligence to sort messages by content.
Making patient records portable
Nearly 40% of portal users accessed it using a smartphone app (17%) or with both their smartphone app and their computer (22%). Sixty-one percent of users relied exclusively on computers to access their portals.
About a third of patient portal users downloaded their online medical records in 2020. This proportion has nearly doubled from 17% since 2017, the ONC report noted.
Although the survey didn’t ask about multiple downloads, it appears that most people had to download their records separately from the patient portal of each practitioner who cared for them. Although the Apple Health app allows people to download records to their iPhones from multiple portals using a standard application programming interface, the ONC report says that only 5% of respondents transmitted their records to a service or app, up slightly from 3% in 2017.
Dr. Waldren hopes most patients will have the ability to download and integrate records from multiple practitioners in a few years, but he wouldn’t bet on it.
“A fair amount of work needs to be done on the business side and on figuring out how the data get connected together,” he said. “And there are still privacy concerns with apps.”
Overall, 21% of portal users transmitted their data to at least one outside party in 2020, compared with 14% in 2017. Seventeen percent of them sent their records to another health care practitioner, up from 10% in 2017. Five percent of the users transmitted their records to a caregiver, slightly more than in 2017.
Managing data is a challenge
Asked how physicians feel about portal users adding information to their record or correcting inaccurate information, Dr. Waldren says, “Doctors are already comfortable with patient-generated data. The challenge is managing it. If the patient provides data that’s not easy to put in the EHR, that’s going to add work, and they don’t want to see 100 blood pressure readings.
“You’d be hard-pressed to find a doctor who doesn’t welcome additional information about the patient’s health, but it can be onerous and can take time to enter the data,” Dr. Waldren said.
Overall, he said, “Giving patients the ability to take more ownership of their health and participate in their own care is good and can help us move forward. How this will be integrated into patient care is another question.”
A version of this article first appeared on Medscape.com.
The use of patient portals that provide access to electronic health records has dramatically increased in the past several years, and patients whose health care practitioner encouraged them to use their online portal accessed them at a higher rate than those who were not encouraged to do so.
These were among the top-line results of a national survey of U.S. adults conducted by the National Institutes of Health from January 2020 to April 2020. Although the COVID-19 pandemic hit the United States in the middle of that period, a report on the survey by the Office of the National Coordinator for Health IT stated, “These findings largely reflect prepandemic rates of individuals being offered and subsequently using their online medical record, also known as a patient portal.”
But with more patient access can come additional work for physicians and other health care practitioners, ranging from an onslaught of patient communications to managing data sent to them by patients.
According to the report, 59% of individuals were offered access to their patient portal, and 38% accessed their record at least once in 2020. By comparison, in 2014, just 42% were offered access to their portal, and 25% used it. But these percentages hardly changed from 2019 to 2020.
The increase in the percentage of people who accessed portals reflects the fact that more people were offered access. In addition, there were signs of rising activity among portal users.
Among patients offered access to their patient portal, 64% accessed it at least once in 2020 – 11 percentage points more than in 2017. Twenty-seven percent of those who had access to a portal used it once or twice; 20% accessed it three to five times; and 18% used it six or more times. The latter two percentages were significantly higher than in 2017.
Of the respondents who were offered access to portals but didn’t use them, 69% said they didn’t access the portal because they preferred to speak with their health care practitioner directly. Sixty-three percent said they didn’t see a need to use their online medical record. This was similar to the percentage 3 years earlier. Other reasons included respondents’ concerns about the privacy/security of online medical records (24%), their lack of comfort with computers (20%), and their lack of Internet access (13%).
The pros and cons of patient portals, greater access
Among portal users who accessed their records through a mobile health app, 51% used the app to facilitate discussions with their health care practitioner in 2020, an 8–percentage point increase from 2017. Fifty-percent of the mobile health app users utilized it to make a decision about how to treat an illness or condition, up from 45% in 2017. And 71% of these individuals used their app to track progress on a health-related goal, just a bit more than in 2017.
Individuals who were encouraged by their health care practitioner to use their patient portal viewed clinical notes and exchanged secure messages with their practitioner at higher rates than those who had not been encouraged. This is not surprising, but it reflects an unintended result of patient portals that many physicians have found burdensome, especially during the pandemic: overflowing electronic in-boxes.
Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, recently tweeted, “We’re seeing huge uptick in in-box messages for MDs during COVID – now seems like biggest driver of MD burnout. The fundamental problem: We turned on 24/7/365 access for patients (who of course like it) with no operational or business model to handle it. Crucial that we fix this.”
Steven Waldren, MD, vice president and chief medical informatics officer at the American Academy of Family Physicians, told this news organization that he agrees that this is a major challenge. “In-box management is a burden on physicians and practices,” he said. “However, it can be done better, either through a team in-box or through better use of technology.”
The team in-box he refers to is a mechanism for triaging patient messages. For example, a triage nurse can look at the messages and decide which ones can be handled by staff and which ones the doctor needs to see. Or physicians and front office staff can see the messages at the same time; a nurse can triage some messages according to protocols, and the physician can respond to any message, depending on what he or she knows about the patient.
Technology can also be enlisted in the effort, he suggested, perhaps by automating the triaging of messages such as prescription refill requests or using artificial intelligence to sort messages by content.
Making patient records portable
Nearly 40% of portal users accessed it using a smartphone app (17%) or with both their smartphone app and their computer (22%). Sixty-one percent of users relied exclusively on computers to access their portals.
About a third of patient portal users downloaded their online medical records in 2020. This proportion has nearly doubled from 17% since 2017, the ONC report noted.
Although the survey didn’t ask about multiple downloads, it appears that most people had to download their records separately from the patient portal of each practitioner who cared for them. Although the Apple Health app allows people to download records to their iPhones from multiple portals using a standard application programming interface, the ONC report says that only 5% of respondents transmitted their records to a service or app, up slightly from 3% in 2017.
Dr. Waldren hopes most patients will have the ability to download and integrate records from multiple practitioners in a few years, but he wouldn’t bet on it.
“A fair amount of work needs to be done on the business side and on figuring out how the data get connected together,” he said. “And there are still privacy concerns with apps.”
Overall, 21% of portal users transmitted their data to at least one outside party in 2020, compared with 14% in 2017. Seventeen percent of them sent their records to another health care practitioner, up from 10% in 2017. Five percent of the users transmitted their records to a caregiver, slightly more than in 2017.
Managing data is a challenge
Asked how physicians feel about portal users adding information to their record or correcting inaccurate information, Dr. Waldren says, “Doctors are already comfortable with patient-generated data. The challenge is managing it. If the patient provides data that’s not easy to put in the EHR, that’s going to add work, and they don’t want to see 100 blood pressure readings.
“You’d be hard-pressed to find a doctor who doesn’t welcome additional information about the patient’s health, but it can be onerous and can take time to enter the data,” Dr. Waldren said.
Overall, he said, “Giving patients the ability to take more ownership of their health and participate in their own care is good and can help us move forward. How this will be integrated into patient care is another question.”
A version of this article first appeared on Medscape.com.
The use of patient portals that provide access to electronic health records has dramatically increased in the past several years, and patients whose health care practitioner encouraged them to use their online portal accessed them at a higher rate than those who were not encouraged to do so.
These were among the top-line results of a national survey of U.S. adults conducted by the National Institutes of Health from January 2020 to April 2020. Although the COVID-19 pandemic hit the United States in the middle of that period, a report on the survey by the Office of the National Coordinator for Health IT stated, “These findings largely reflect prepandemic rates of individuals being offered and subsequently using their online medical record, also known as a patient portal.”
But with more patient access can come additional work for physicians and other health care practitioners, ranging from an onslaught of patient communications to managing data sent to them by patients.
According to the report, 59% of individuals were offered access to their patient portal, and 38% accessed their record at least once in 2020. By comparison, in 2014, just 42% were offered access to their portal, and 25% used it. But these percentages hardly changed from 2019 to 2020.
The increase in the percentage of people who accessed portals reflects the fact that more people were offered access. In addition, there were signs of rising activity among portal users.
Among patients offered access to their patient portal, 64% accessed it at least once in 2020 – 11 percentage points more than in 2017. Twenty-seven percent of those who had access to a portal used it once or twice; 20% accessed it three to five times; and 18% used it six or more times. The latter two percentages were significantly higher than in 2017.
Of the respondents who were offered access to portals but didn’t use them, 69% said they didn’t access the portal because they preferred to speak with their health care practitioner directly. Sixty-three percent said they didn’t see a need to use their online medical record. This was similar to the percentage 3 years earlier. Other reasons included respondents’ concerns about the privacy/security of online medical records (24%), their lack of comfort with computers (20%), and their lack of Internet access (13%).
The pros and cons of patient portals, greater access
Among portal users who accessed their records through a mobile health app, 51% used the app to facilitate discussions with their health care practitioner in 2020, an 8–percentage point increase from 2017. Fifty-percent of the mobile health app users utilized it to make a decision about how to treat an illness or condition, up from 45% in 2017. And 71% of these individuals used their app to track progress on a health-related goal, just a bit more than in 2017.
Individuals who were encouraged by their health care practitioner to use their patient portal viewed clinical notes and exchanged secure messages with their practitioner at higher rates than those who had not been encouraged. This is not surprising, but it reflects an unintended result of patient portals that many physicians have found burdensome, especially during the pandemic: overflowing electronic in-boxes.
Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, recently tweeted, “We’re seeing huge uptick in in-box messages for MDs during COVID – now seems like biggest driver of MD burnout. The fundamental problem: We turned on 24/7/365 access for patients (who of course like it) with no operational or business model to handle it. Crucial that we fix this.”
Steven Waldren, MD, vice president and chief medical informatics officer at the American Academy of Family Physicians, told this news organization that he agrees that this is a major challenge. “In-box management is a burden on physicians and practices,” he said. “However, it can be done better, either through a team in-box or through better use of technology.”
The team in-box he refers to is a mechanism for triaging patient messages. For example, a triage nurse can look at the messages and decide which ones can be handled by staff and which ones the doctor needs to see. Or physicians and front office staff can see the messages at the same time; a nurse can triage some messages according to protocols, and the physician can respond to any message, depending on what he or she knows about the patient.
Technology can also be enlisted in the effort, he suggested, perhaps by automating the triaging of messages such as prescription refill requests or using artificial intelligence to sort messages by content.
Making patient records portable
Nearly 40% of portal users accessed it using a smartphone app (17%) or with both their smartphone app and their computer (22%). Sixty-one percent of users relied exclusively on computers to access their portals.
About a third of patient portal users downloaded their online medical records in 2020. This proportion has nearly doubled from 17% since 2017, the ONC report noted.
Although the survey didn’t ask about multiple downloads, it appears that most people had to download their records separately from the patient portal of each practitioner who cared for them. Although the Apple Health app allows people to download records to their iPhones from multiple portals using a standard application programming interface, the ONC report says that only 5% of respondents transmitted their records to a service or app, up slightly from 3% in 2017.
Dr. Waldren hopes most patients will have the ability to download and integrate records from multiple practitioners in a few years, but he wouldn’t bet on it.
“A fair amount of work needs to be done on the business side and on figuring out how the data get connected together,” he said. “And there are still privacy concerns with apps.”
Overall, 21% of portal users transmitted their data to at least one outside party in 2020, compared with 14% in 2017. Seventeen percent of them sent their records to another health care practitioner, up from 10% in 2017. Five percent of the users transmitted their records to a caregiver, slightly more than in 2017.
Managing data is a challenge
Asked how physicians feel about portal users adding information to their record or correcting inaccurate information, Dr. Waldren says, “Doctors are already comfortable with patient-generated data. The challenge is managing it. If the patient provides data that’s not easy to put in the EHR, that’s going to add work, and they don’t want to see 100 blood pressure readings.
“You’d be hard-pressed to find a doctor who doesn’t welcome additional information about the patient’s health, but it can be onerous and can take time to enter the data,” Dr. Waldren said.
Overall, he said, “Giving patients the ability to take more ownership of their health and participate in their own care is good and can help us move forward. How this will be integrated into patient care is another question.”
A version of this article first appeared on Medscape.com.
COVID-19 hospitalization 80% more likely for smokers
Observational data was analyzed alongside hospital coronavirus test data and UK Biobank genetic information for the first time, and the findings are published in Thorax.
The data cover 421,469 people overall. Of these, 3.2% took a polymerase chain reaction swab test, 0.4% of these tested positive, 0.2% of them required hospitalization for COVID-19, and 0.1% of them died because of COVID-19.
When it came to smoking status, 59% had never smoked, 37% were ex-smokers, and 3% were current smokers.
Current smokers were 80% more likely to be admitted to hospital, and significantly more likely to die from COVID-19, than nonsmokers.
Time to quit
Heavy smokers who smoked more than 20 cigarettes a day were 6.11 times more likely to die from COVID-19 than people who had never smoked.
Analysis also showed those with a genetic predisposition to being smokers had a 45% higher infection risk, and 60% higher hospitalization risk.
The authors wrote: “Overall, the congruence of observational analyses indicating associations with recent smoking behaviors and [Mendelian randomization] analyses indicating associations with lifelong predisposition to smoking and smoking heaviness support a causal effect of smoking on COVID-19 severity.”
In a linked podcast, lead researcher Dr. Ashley Clift, said: “Our results strongly suggest that smoking is related to your risk of getting severe COVID, and just as smoking affects your risk of heart disease, different cancers, and all those other conditions we know smoking is linked to, it appears that it’s the same for COVID. So now might be as good a time as any to quit cigarettes and quit smoking.”
These results contrast with previous studies that have suggested a protective effect of smoking against COVID-19. In a linked editorial, Anthony Laverty, PhD, and Christopher Millet, PhD, Imperial College London, wrote: “The idea that tobacco smoking may protect against COVID-19 was always an improbable one.”
A version of this article first appeared on Medscape.com.
Observational data was analyzed alongside hospital coronavirus test data and UK Biobank genetic information for the first time, and the findings are published in Thorax.
The data cover 421,469 people overall. Of these, 3.2% took a polymerase chain reaction swab test, 0.4% of these tested positive, 0.2% of them required hospitalization for COVID-19, and 0.1% of them died because of COVID-19.
When it came to smoking status, 59% had never smoked, 37% were ex-smokers, and 3% were current smokers.
Current smokers were 80% more likely to be admitted to hospital, and significantly more likely to die from COVID-19, than nonsmokers.
Time to quit
Heavy smokers who smoked more than 20 cigarettes a day were 6.11 times more likely to die from COVID-19 than people who had never smoked.
Analysis also showed those with a genetic predisposition to being smokers had a 45% higher infection risk, and 60% higher hospitalization risk.
The authors wrote: “Overall, the congruence of observational analyses indicating associations with recent smoking behaviors and [Mendelian randomization] analyses indicating associations with lifelong predisposition to smoking and smoking heaviness support a causal effect of smoking on COVID-19 severity.”
In a linked podcast, lead researcher Dr. Ashley Clift, said: “Our results strongly suggest that smoking is related to your risk of getting severe COVID, and just as smoking affects your risk of heart disease, different cancers, and all those other conditions we know smoking is linked to, it appears that it’s the same for COVID. So now might be as good a time as any to quit cigarettes and quit smoking.”
These results contrast with previous studies that have suggested a protective effect of smoking against COVID-19. In a linked editorial, Anthony Laverty, PhD, and Christopher Millet, PhD, Imperial College London, wrote: “The idea that tobacco smoking may protect against COVID-19 was always an improbable one.”
A version of this article first appeared on Medscape.com.
Observational data was analyzed alongside hospital coronavirus test data and UK Biobank genetic information for the first time, and the findings are published in Thorax.
The data cover 421,469 people overall. Of these, 3.2% took a polymerase chain reaction swab test, 0.4% of these tested positive, 0.2% of them required hospitalization for COVID-19, and 0.1% of them died because of COVID-19.
When it came to smoking status, 59% had never smoked, 37% were ex-smokers, and 3% were current smokers.
Current smokers were 80% more likely to be admitted to hospital, and significantly more likely to die from COVID-19, than nonsmokers.
Time to quit
Heavy smokers who smoked more than 20 cigarettes a day were 6.11 times more likely to die from COVID-19 than people who had never smoked.
Analysis also showed those with a genetic predisposition to being smokers had a 45% higher infection risk, and 60% higher hospitalization risk.
The authors wrote: “Overall, the congruence of observational analyses indicating associations with recent smoking behaviors and [Mendelian randomization] analyses indicating associations with lifelong predisposition to smoking and smoking heaviness support a causal effect of smoking on COVID-19 severity.”
In a linked podcast, lead researcher Dr. Ashley Clift, said: “Our results strongly suggest that smoking is related to your risk of getting severe COVID, and just as smoking affects your risk of heart disease, different cancers, and all those other conditions we know smoking is linked to, it appears that it’s the same for COVID. So now might be as good a time as any to quit cigarettes and quit smoking.”
These results contrast with previous studies that have suggested a protective effect of smoking against COVID-19. In a linked editorial, Anthony Laverty, PhD, and Christopher Millet, PhD, Imperial College London, wrote: “The idea that tobacco smoking may protect against COVID-19 was always an improbable one.”
A version of this article first appeared on Medscape.com.
Fraudulent misbranding of PPE nets $22 million settlement
Avanos medical to pay $22 million to resolve criminal charge for fraudulent misbranding of PPE
A U.S.-based multinational medical device corporation will pay more than $22 million to resolve a criminal charge regarding fraudulent misbranding of their surgical gowns.
Avanos Medical Inc, which as its U.S. headquarters in Alpharetta, Georgia, is charged with one count of introducing misbranded surgical gowns into interstate commerce with the intent to defraud and mislead.
According to the Department of Justice, the company knowingly falsely labeled its MicroCool surgical gowns as providing AAMI Level 4 protection (the highest level) against fluid and virus penetration. Under the standards set by the American National Standards Institute (ANSI) and the Association for the Advancement of Medical Instrumentation (AAMI), the highest protection level for surgical gowns is reserved for gowns intended to be used in surgeries and other high-risk medical procedures on patients suspected of having infectious diseases.
Avanos admitted to selling hundreds of thousands of MicroCool gowns that were falsely labeled as AAMI Level 4 between late 2014 and early 2015, as well as directly lying to customers about the gowns’ protective capacities. In total, Avanos sold almost $9 million of misbranded MicroCool gowns.
“The last thing health care workers should have to worry about is whether their personal protective equipment lives up to manufacturers’ claims,” said Acting U.S. Attorney Prerak Shah for the Northern District of Texas. “Misbranded PPE can pose serious risks to medical professionals and patients alike.”
Company pays $38.75 million to settle allegations of knowingly selling defective devices
Medical device manufacturers Alere and Alere San Diego (collectively, Alere) have agreed to pay almost $39 million to resolve allegations that they violated the False Claims Act by billing, and causing others to bill, the Medicare program for defective rapid point-of-care testing devices.
From 2008 to 2016, the Department of Justice alleges, Alere knowingly sold defective INRatio blood coagulation monitors used by Medicare beneficiaries who were taking anticoagulants. The software algorithms in the monitors contained a material defect, which Alere had found in their research, to cause inaccurate readings. Blood coagulation monitoring is essential for the safety of these patients, enabling them to maintain a safe dosage of their medications. Taking too much of an anticoagulant can cause major bleeding, while taking too little can cause blood clots that lead to strokes.
While Alere was aware that these devices were linked to over a dozen deaths and hundreds of injuries, the company continued to conceal the defect and billed Medicare for the devices.
In 2016, the product was taken off the market at the request of the FDA.
Mass. doctor, wife charged in international money laundering, fraud scheme
Massachusetts psychiatrist Rahim Shafa, MD, and his wife and office manager, Nahid Tormosi Shafa, are charged in connection to an international money laundering scheme involving importing illegal and misbranded drugs.
Through Shafa’s company, Novel Psychopharmacology, the two allegedly filed false and fraudulent Medicare reimbursement claims from 2016-2019, then deposited the money in their bank accounts, according to federal officials. From 2008-2018, the couple also engaged in an international money laundering scheme to purchase naltrexone pellet implants, disulfiram pellet implants, and injections from Hong Kong that were not approved by the FDA. According to officials, they falsified shipping documents, disguising the naltrexone pellet implants as “plastic beads in plastic tubes” to receive the drugs. They then offered to sell these drugs to patients of Novel Psychopharmacology.
Rahim Shafa was indicted on conspiracies of international money laundering, health care fraud, and defrauding the United States, as well as illegally importing merchandise and purposely delivering misbranded drugs. His wife was indicted on one count each of health care fraud conspiracy and international money laundering conspiracy.
Jury convicts medical equipment company owners of $27 million fraud
A federal jury in Texas convicted the owners of two durable medical equipment (DME) companies linked to a scheme to defraud Medicare.
Leah Hagen, 49, and Michael Hagen, 54, were convicted of one count of conspiracy to defraud the United States and to pay and receive health care kickbacks and one count of conspiracy to commit money laundering. The defendants owned and operated Metro DME Supply and Ortho Pain Solutions.
Ms. Hagen and Mr. Hagen paid a fixed rate per DME item in exchange for prescriptions and paperwork completed by telemedicine doctors that were used to submit false claims to Medicare, which totaled about $59 million. They were paid $27 million, and wired millions to their personal bank accounts. The defendants paid illegal bribes and kickbacks and wired money to their co-conspirator’s call center in the Philippines that provided signed doctor’s orders for orthotic braces.
At trial, evidence showed emails between Leah and Michael Hagen and their co-conspirators outlining a per-product pricing structure for orthotic braces, but not disclosing their agreement as one for marketing and other services.
At sentencing, the Hagens each face a maximum sentence of 25 years in prison.
A version of this article first appeared on Medscape.com.
Avanos medical to pay $22 million to resolve criminal charge for fraudulent misbranding of PPE
A U.S.-based multinational medical device corporation will pay more than $22 million to resolve a criminal charge regarding fraudulent misbranding of their surgical gowns.
Avanos Medical Inc, which as its U.S. headquarters in Alpharetta, Georgia, is charged with one count of introducing misbranded surgical gowns into interstate commerce with the intent to defraud and mislead.
According to the Department of Justice, the company knowingly falsely labeled its MicroCool surgical gowns as providing AAMI Level 4 protection (the highest level) against fluid and virus penetration. Under the standards set by the American National Standards Institute (ANSI) and the Association for the Advancement of Medical Instrumentation (AAMI), the highest protection level for surgical gowns is reserved for gowns intended to be used in surgeries and other high-risk medical procedures on patients suspected of having infectious diseases.
Avanos admitted to selling hundreds of thousands of MicroCool gowns that were falsely labeled as AAMI Level 4 between late 2014 and early 2015, as well as directly lying to customers about the gowns’ protective capacities. In total, Avanos sold almost $9 million of misbranded MicroCool gowns.
“The last thing health care workers should have to worry about is whether their personal protective equipment lives up to manufacturers’ claims,” said Acting U.S. Attorney Prerak Shah for the Northern District of Texas. “Misbranded PPE can pose serious risks to medical professionals and patients alike.”
Company pays $38.75 million to settle allegations of knowingly selling defective devices
Medical device manufacturers Alere and Alere San Diego (collectively, Alere) have agreed to pay almost $39 million to resolve allegations that they violated the False Claims Act by billing, and causing others to bill, the Medicare program for defective rapid point-of-care testing devices.
From 2008 to 2016, the Department of Justice alleges, Alere knowingly sold defective INRatio blood coagulation monitors used by Medicare beneficiaries who were taking anticoagulants. The software algorithms in the monitors contained a material defect, which Alere had found in their research, to cause inaccurate readings. Blood coagulation monitoring is essential for the safety of these patients, enabling them to maintain a safe dosage of their medications. Taking too much of an anticoagulant can cause major bleeding, while taking too little can cause blood clots that lead to strokes.
While Alere was aware that these devices were linked to over a dozen deaths and hundreds of injuries, the company continued to conceal the defect and billed Medicare for the devices.
In 2016, the product was taken off the market at the request of the FDA.
Mass. doctor, wife charged in international money laundering, fraud scheme
Massachusetts psychiatrist Rahim Shafa, MD, and his wife and office manager, Nahid Tormosi Shafa, are charged in connection to an international money laundering scheme involving importing illegal and misbranded drugs.
Through Shafa’s company, Novel Psychopharmacology, the two allegedly filed false and fraudulent Medicare reimbursement claims from 2016-2019, then deposited the money in their bank accounts, according to federal officials. From 2008-2018, the couple also engaged in an international money laundering scheme to purchase naltrexone pellet implants, disulfiram pellet implants, and injections from Hong Kong that were not approved by the FDA. According to officials, they falsified shipping documents, disguising the naltrexone pellet implants as “plastic beads in plastic tubes” to receive the drugs. They then offered to sell these drugs to patients of Novel Psychopharmacology.
Rahim Shafa was indicted on conspiracies of international money laundering, health care fraud, and defrauding the United States, as well as illegally importing merchandise and purposely delivering misbranded drugs. His wife was indicted on one count each of health care fraud conspiracy and international money laundering conspiracy.
Jury convicts medical equipment company owners of $27 million fraud
A federal jury in Texas convicted the owners of two durable medical equipment (DME) companies linked to a scheme to defraud Medicare.
Leah Hagen, 49, and Michael Hagen, 54, were convicted of one count of conspiracy to defraud the United States and to pay and receive health care kickbacks and one count of conspiracy to commit money laundering. The defendants owned and operated Metro DME Supply and Ortho Pain Solutions.
Ms. Hagen and Mr. Hagen paid a fixed rate per DME item in exchange for prescriptions and paperwork completed by telemedicine doctors that were used to submit false claims to Medicare, which totaled about $59 million. They were paid $27 million, and wired millions to their personal bank accounts. The defendants paid illegal bribes and kickbacks and wired money to their co-conspirator’s call center in the Philippines that provided signed doctor’s orders for orthotic braces.
At trial, evidence showed emails between Leah and Michael Hagen and their co-conspirators outlining a per-product pricing structure for orthotic braces, but not disclosing their agreement as one for marketing and other services.
At sentencing, the Hagens each face a maximum sentence of 25 years in prison.
A version of this article first appeared on Medscape.com.
Avanos medical to pay $22 million to resolve criminal charge for fraudulent misbranding of PPE
A U.S.-based multinational medical device corporation will pay more than $22 million to resolve a criminal charge regarding fraudulent misbranding of their surgical gowns.
Avanos Medical Inc, which as its U.S. headquarters in Alpharetta, Georgia, is charged with one count of introducing misbranded surgical gowns into interstate commerce with the intent to defraud and mislead.
According to the Department of Justice, the company knowingly falsely labeled its MicroCool surgical gowns as providing AAMI Level 4 protection (the highest level) against fluid and virus penetration. Under the standards set by the American National Standards Institute (ANSI) and the Association for the Advancement of Medical Instrumentation (AAMI), the highest protection level for surgical gowns is reserved for gowns intended to be used in surgeries and other high-risk medical procedures on patients suspected of having infectious diseases.
Avanos admitted to selling hundreds of thousands of MicroCool gowns that were falsely labeled as AAMI Level 4 between late 2014 and early 2015, as well as directly lying to customers about the gowns’ protective capacities. In total, Avanos sold almost $9 million of misbranded MicroCool gowns.
“The last thing health care workers should have to worry about is whether their personal protective equipment lives up to manufacturers’ claims,” said Acting U.S. Attorney Prerak Shah for the Northern District of Texas. “Misbranded PPE can pose serious risks to medical professionals and patients alike.”
Company pays $38.75 million to settle allegations of knowingly selling defective devices
Medical device manufacturers Alere and Alere San Diego (collectively, Alere) have agreed to pay almost $39 million to resolve allegations that they violated the False Claims Act by billing, and causing others to bill, the Medicare program for defective rapid point-of-care testing devices.
From 2008 to 2016, the Department of Justice alleges, Alere knowingly sold defective INRatio blood coagulation monitors used by Medicare beneficiaries who were taking anticoagulants. The software algorithms in the monitors contained a material defect, which Alere had found in their research, to cause inaccurate readings. Blood coagulation monitoring is essential for the safety of these patients, enabling them to maintain a safe dosage of their medications. Taking too much of an anticoagulant can cause major bleeding, while taking too little can cause blood clots that lead to strokes.
While Alere was aware that these devices were linked to over a dozen deaths and hundreds of injuries, the company continued to conceal the defect and billed Medicare for the devices.
In 2016, the product was taken off the market at the request of the FDA.
Mass. doctor, wife charged in international money laundering, fraud scheme
Massachusetts psychiatrist Rahim Shafa, MD, and his wife and office manager, Nahid Tormosi Shafa, are charged in connection to an international money laundering scheme involving importing illegal and misbranded drugs.
Through Shafa’s company, Novel Psychopharmacology, the two allegedly filed false and fraudulent Medicare reimbursement claims from 2016-2019, then deposited the money in their bank accounts, according to federal officials. From 2008-2018, the couple also engaged in an international money laundering scheme to purchase naltrexone pellet implants, disulfiram pellet implants, and injections from Hong Kong that were not approved by the FDA. According to officials, they falsified shipping documents, disguising the naltrexone pellet implants as “plastic beads in plastic tubes” to receive the drugs. They then offered to sell these drugs to patients of Novel Psychopharmacology.
Rahim Shafa was indicted on conspiracies of international money laundering, health care fraud, and defrauding the United States, as well as illegally importing merchandise and purposely delivering misbranded drugs. His wife was indicted on one count each of health care fraud conspiracy and international money laundering conspiracy.
Jury convicts medical equipment company owners of $27 million fraud
A federal jury in Texas convicted the owners of two durable medical equipment (DME) companies linked to a scheme to defraud Medicare.
Leah Hagen, 49, and Michael Hagen, 54, were convicted of one count of conspiracy to defraud the United States and to pay and receive health care kickbacks and one count of conspiracy to commit money laundering. The defendants owned and operated Metro DME Supply and Ortho Pain Solutions.
Ms. Hagen and Mr. Hagen paid a fixed rate per DME item in exchange for prescriptions and paperwork completed by telemedicine doctors that were used to submit false claims to Medicare, which totaled about $59 million. They were paid $27 million, and wired millions to their personal bank accounts. The defendants paid illegal bribes and kickbacks and wired money to their co-conspirator’s call center in the Philippines that provided signed doctor’s orders for orthotic braces.
At trial, evidence showed emails between Leah and Michael Hagen and their co-conspirators outlining a per-product pricing structure for orthotic braces, but not disclosing their agreement as one for marketing and other services.
At sentencing, the Hagens each face a maximum sentence of 25 years in prison.
A version of this article first appeared on Medscape.com.
Polyethylene glycol linked to rare allergic reactions seen with mRNA COVID-19 vaccines
A common inert ingredient may be the culprit behind the rare allergic reactions reported among individuals who have received mRNA COVID-19 vaccines, according to investigators at a large regional health center that was among the first to administer the shots.
Blood samples from 10 of 11 individuals with suspected allergic reactions reacted to polyethylene glycol (PEG), a component of both the Pfizer and Moderna mRNA vaccines, according to a report in JAMA Network Open.
In total, only 22 individuals had suspected allergic reactions out of nearly 39,000 mRNA COVID-19 vaccine doses administered, the investigators reported, noting that the reactions were generally mild and all fully resolved.
Those findings should be reassuring to individuals who are reticent to sign up for a COVID-19 vaccine because of fear of an allergic reaction, said study senior author Kari Nadeau, MD, PhD, director of the Parker Center for Allergy and Asthma Research at Stanford (Calif.) University.
“We’re hoping that this word will get out and then that the companies could also think about making vaccines that have other products in them that don’t include polyethylene glycol,” Dr. Nadeau said in an interview.
PEG is a compound used in many products, including pharmaceuticals, cosmetics, and food. In the mRNA COVID-19 vaccines, PEG serves to stabilize the lipid nanoparticles that help protect and transport mRNA. However, its use in this setting has been linked to allergic reactions in this and previous studies.
No immunoglobulin E (IgE) antibodies to PEG were detected among the 22 individuals with suspected allergic reactions to mRNA COVID-19 vaccine, but PEG immunoglobulin G (IgG) was present. That suggests non-IgE mediated allergic reactions to PEG may be implicated for the majority of cases, Dr. Nadeau said.
This case series provides interesting new evidence to confirm previous reports that a mechanism other than the classic IgE-mediated allergic response is behind the suspected allergic reactions that are occurring after mRNA COVID-19 vaccine, said Aleena Banerji, MD, associate professor at Harvard Medical School, Boston, and clinical director of the Drug Allergy Program at Massachusetts General Hospital.
“We need to further understand the mechanism of these reactions, but what we know is that IGE mediated allergy to excipients like PEG is probably not the main cause,” Dr. Banerji, who was not involved in the study, said in an interview.
In a recent research letter published in JAMA Internal Medicine, Dr. Banerji and coauthors reported that all individuals with immediate suspected allergic reactions to mRNA COVID-19 vaccine went on to tolerate the second dose, with mild symptoms reported in the minority of patients (32 out of 159, or about 20%).
“Again, that is very consistent with not having an IgE-mediated allergy, so it seems to all be fitting with that picture,” Dr. Banerji said.
The case series by Dr. Nadeau and coauthors was based on review of nearly 39,000 mRNA COVID-19 vaccine doses administered between December 18, 2020 and January 26, 2021. Most mRNA vaccine recipients were Stanford-affiliated health care workers, according to the report.
Among recipients of those doses, they identified 148 individuals who had anaphylaxis-related ICD-10 codes recorded over the same time period. In a review of medical records, investigators pinpointed 22 individuals as having suspected allergy and invited them to participate in follow-up allergy testing.
A total of 11 individuals underwent skin prick testing, but none of them tested positive to PEG or to polysorbate 80, another excipient that has been linked to vaccine-related allergic reactions. One of the patients tested positive to the same mRNA vaccine they had previously received, according to the report.
Those same 11 individuals also underwent basophil activation testing (BAT). In contrast to the skin testing results, BAT results were positive for PEG in 10 of 11 cases (or 91%) and positive for their administered vaccine in all 11 cases, the report shows.
High levels of IgG to PEG were identified in blood samples of individuals with an allergy to the vaccine. Investigators said it’s possible that the BAT results were activated due to IgG via complement activation–related pseudoallergy, or CARPA, as has been hypothesized by some other investigators.
The negative skin prick testing results for PEG, which contrast with the positive BAT results to PEG, suggest that the former may not be appropriate for use as a predictive marker of potential vaccine allergy, according to Dr. Nadeau.
“The take-home message for doctors is to be careful,” she said. “Don’t assume that just because the person skin-tests negative to PEG or to the vaccine itself that you’re out of the woods, because the skin test would be often negative in those scenarios.”
The study was supported by a grants from the Asthma and Allergic Diseases Cooperative Research Centers, a grant from the National Institutes of Health, the National Institute of Allergy and Infectious Disease SARS Vaccine study, the Parker Foundation, the Crown Foundation, and the Sunshine Foundation. Dr. Nadeau reports numerous conflicts with various sources in the industry. Dr. Banerji has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A common inert ingredient may be the culprit behind the rare allergic reactions reported among individuals who have received mRNA COVID-19 vaccines, according to investigators at a large regional health center that was among the first to administer the shots.
Blood samples from 10 of 11 individuals with suspected allergic reactions reacted to polyethylene glycol (PEG), a component of both the Pfizer and Moderna mRNA vaccines, according to a report in JAMA Network Open.
In total, only 22 individuals had suspected allergic reactions out of nearly 39,000 mRNA COVID-19 vaccine doses administered, the investigators reported, noting that the reactions were generally mild and all fully resolved.
Those findings should be reassuring to individuals who are reticent to sign up for a COVID-19 vaccine because of fear of an allergic reaction, said study senior author Kari Nadeau, MD, PhD, director of the Parker Center for Allergy and Asthma Research at Stanford (Calif.) University.
“We’re hoping that this word will get out and then that the companies could also think about making vaccines that have other products in them that don’t include polyethylene glycol,” Dr. Nadeau said in an interview.
PEG is a compound used in many products, including pharmaceuticals, cosmetics, and food. In the mRNA COVID-19 vaccines, PEG serves to stabilize the lipid nanoparticles that help protect and transport mRNA. However, its use in this setting has been linked to allergic reactions in this and previous studies.
No immunoglobulin E (IgE) antibodies to PEG were detected among the 22 individuals with suspected allergic reactions to mRNA COVID-19 vaccine, but PEG immunoglobulin G (IgG) was present. That suggests non-IgE mediated allergic reactions to PEG may be implicated for the majority of cases, Dr. Nadeau said.
This case series provides interesting new evidence to confirm previous reports that a mechanism other than the classic IgE-mediated allergic response is behind the suspected allergic reactions that are occurring after mRNA COVID-19 vaccine, said Aleena Banerji, MD, associate professor at Harvard Medical School, Boston, and clinical director of the Drug Allergy Program at Massachusetts General Hospital.
“We need to further understand the mechanism of these reactions, but what we know is that IGE mediated allergy to excipients like PEG is probably not the main cause,” Dr. Banerji, who was not involved in the study, said in an interview.
In a recent research letter published in JAMA Internal Medicine, Dr. Banerji and coauthors reported that all individuals with immediate suspected allergic reactions to mRNA COVID-19 vaccine went on to tolerate the second dose, with mild symptoms reported in the minority of patients (32 out of 159, or about 20%).
“Again, that is very consistent with not having an IgE-mediated allergy, so it seems to all be fitting with that picture,” Dr. Banerji said.
The case series by Dr. Nadeau and coauthors was based on review of nearly 39,000 mRNA COVID-19 vaccine doses administered between December 18, 2020 and January 26, 2021. Most mRNA vaccine recipients were Stanford-affiliated health care workers, according to the report.
Among recipients of those doses, they identified 148 individuals who had anaphylaxis-related ICD-10 codes recorded over the same time period. In a review of medical records, investigators pinpointed 22 individuals as having suspected allergy and invited them to participate in follow-up allergy testing.
A total of 11 individuals underwent skin prick testing, but none of them tested positive to PEG or to polysorbate 80, another excipient that has been linked to vaccine-related allergic reactions. One of the patients tested positive to the same mRNA vaccine they had previously received, according to the report.
Those same 11 individuals also underwent basophil activation testing (BAT). In contrast to the skin testing results, BAT results were positive for PEG in 10 of 11 cases (or 91%) and positive for their administered vaccine in all 11 cases, the report shows.
High levels of IgG to PEG were identified in blood samples of individuals with an allergy to the vaccine. Investigators said it’s possible that the BAT results were activated due to IgG via complement activation–related pseudoallergy, or CARPA, as has been hypothesized by some other investigators.
The negative skin prick testing results for PEG, which contrast with the positive BAT results to PEG, suggest that the former may not be appropriate for use as a predictive marker of potential vaccine allergy, according to Dr. Nadeau.
“The take-home message for doctors is to be careful,” she said. “Don’t assume that just because the person skin-tests negative to PEG or to the vaccine itself that you’re out of the woods, because the skin test would be often negative in those scenarios.”
The study was supported by a grants from the Asthma and Allergic Diseases Cooperative Research Centers, a grant from the National Institutes of Health, the National Institute of Allergy and Infectious Disease SARS Vaccine study, the Parker Foundation, the Crown Foundation, and the Sunshine Foundation. Dr. Nadeau reports numerous conflicts with various sources in the industry. Dr. Banerji has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A common inert ingredient may be the culprit behind the rare allergic reactions reported among individuals who have received mRNA COVID-19 vaccines, according to investigators at a large regional health center that was among the first to administer the shots.
Blood samples from 10 of 11 individuals with suspected allergic reactions reacted to polyethylene glycol (PEG), a component of both the Pfizer and Moderna mRNA vaccines, according to a report in JAMA Network Open.
In total, only 22 individuals had suspected allergic reactions out of nearly 39,000 mRNA COVID-19 vaccine doses administered, the investigators reported, noting that the reactions were generally mild and all fully resolved.
Those findings should be reassuring to individuals who are reticent to sign up for a COVID-19 vaccine because of fear of an allergic reaction, said study senior author Kari Nadeau, MD, PhD, director of the Parker Center for Allergy and Asthma Research at Stanford (Calif.) University.
“We’re hoping that this word will get out and then that the companies could also think about making vaccines that have other products in them that don’t include polyethylene glycol,” Dr. Nadeau said in an interview.
PEG is a compound used in many products, including pharmaceuticals, cosmetics, and food. In the mRNA COVID-19 vaccines, PEG serves to stabilize the lipid nanoparticles that help protect and transport mRNA. However, its use in this setting has been linked to allergic reactions in this and previous studies.
No immunoglobulin E (IgE) antibodies to PEG were detected among the 22 individuals with suspected allergic reactions to mRNA COVID-19 vaccine, but PEG immunoglobulin G (IgG) was present. That suggests non-IgE mediated allergic reactions to PEG may be implicated for the majority of cases, Dr. Nadeau said.
This case series provides interesting new evidence to confirm previous reports that a mechanism other than the classic IgE-mediated allergic response is behind the suspected allergic reactions that are occurring after mRNA COVID-19 vaccine, said Aleena Banerji, MD, associate professor at Harvard Medical School, Boston, and clinical director of the Drug Allergy Program at Massachusetts General Hospital.
“We need to further understand the mechanism of these reactions, but what we know is that IGE mediated allergy to excipients like PEG is probably not the main cause,” Dr. Banerji, who was not involved in the study, said in an interview.
In a recent research letter published in JAMA Internal Medicine, Dr. Banerji and coauthors reported that all individuals with immediate suspected allergic reactions to mRNA COVID-19 vaccine went on to tolerate the second dose, with mild symptoms reported in the minority of patients (32 out of 159, or about 20%).
“Again, that is very consistent with not having an IgE-mediated allergy, so it seems to all be fitting with that picture,” Dr. Banerji said.
The case series by Dr. Nadeau and coauthors was based on review of nearly 39,000 mRNA COVID-19 vaccine doses administered between December 18, 2020 and January 26, 2021. Most mRNA vaccine recipients were Stanford-affiliated health care workers, according to the report.
Among recipients of those doses, they identified 148 individuals who had anaphylaxis-related ICD-10 codes recorded over the same time period. In a review of medical records, investigators pinpointed 22 individuals as having suspected allergy and invited them to participate in follow-up allergy testing.
A total of 11 individuals underwent skin prick testing, but none of them tested positive to PEG or to polysorbate 80, another excipient that has been linked to vaccine-related allergic reactions. One of the patients tested positive to the same mRNA vaccine they had previously received, according to the report.
Those same 11 individuals also underwent basophil activation testing (BAT). In contrast to the skin testing results, BAT results were positive for PEG in 10 of 11 cases (or 91%) and positive for their administered vaccine in all 11 cases, the report shows.
High levels of IgG to PEG were identified in blood samples of individuals with an allergy to the vaccine. Investigators said it’s possible that the BAT results were activated due to IgG via complement activation–related pseudoallergy, or CARPA, as has been hypothesized by some other investigators.
The negative skin prick testing results for PEG, which contrast with the positive BAT results to PEG, suggest that the former may not be appropriate for use as a predictive marker of potential vaccine allergy, according to Dr. Nadeau.
“The take-home message for doctors is to be careful,” she said. “Don’t assume that just because the person skin-tests negative to PEG or to the vaccine itself that you’re out of the woods, because the skin test would be often negative in those scenarios.”
The study was supported by a grants from the Asthma and Allergic Diseases Cooperative Research Centers, a grant from the National Institutes of Health, the National Institute of Allergy and Infectious Disease SARS Vaccine study, the Parker Foundation, the Crown Foundation, and the Sunshine Foundation. Dr. Nadeau reports numerous conflicts with various sources in the industry. Dr. Banerji has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
More severe psoriasis linked to an increased risk of PsA
Factors that predict the development of psoriasis in patients with psoriasis include nail, inverse, and scalp psoriasis; family history of PsA; as well as severity of skin disease. And like psoriasis, “PsA is associated with a multitude of comorbidities, including cardiovascular disease, metabolic syndrome, Crohn’s disease, obesity, diabetes, uveitis, anxiety, and depression, with correspondingly higher healthcare utilization and direct healthcare costs,” wrote corresponding author Joseph F. Merola, MD, MMSc, and colleagues. The study was published online in the Journal of the American Academy of Dermatology. “Timely and accurate diagnosis of PsA is important for improved patient outcomes and appropriate disease management and may prevent prolonged inflammation that leads to structural joint damage and worsening physical function,” they added.
The mean time of onset of PsA among patients with psoriasis who develop PsA is 10 years after the first signs of psoriasis appear. An estimated 20%-30% of patients with psoriasis have a concurrent diagnosis of PsA, and the annual incidence of PsA has been reported to be 2.7 cases per 100 patients with psoriasis. While previous studies have suggested that a higher incidence of PsA is associated with greater disease severity, there are limited data in the United States on the topic.
For the study, Dr. Merola, a dermatologist and rheumatologist who directs the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston, and his colleagues drew from the Optum EHR database to identify adult patients newly diagnosed with psoriasis between Jan. 1, 2009, and March 31, 2019. Patients diagnosed with psoriasis or PsA prior to the index date were excluded from the analysis for evaluation of incidence but included for evaluation of prevalence. The patients were followed from the index date until the earliest PsA event, death, or end of study or follow-up, whichever came first. The researchers calculated the incidence of PsA among adults with psoriasis as the number of incident PsA events divided by the number of patient-years (PY) at risk, which was reported as the raw incidence per 100 psoriasis PY. They calculated the prevalence of PsA among adults with psoriasis as “the number of prevalent PsA events divided by the number of eligible patients with [psoriasis] and reported by years in the follow-up period,” which was a median of 3.7 years.
A total of 114,868 patients were included in the analysis. At baseline, their mean age was 54 years, 53% were female, 89% were White, and 39% were obese. Most patients (102,553) were on nonsystemic agents during the year after their psoriasis diagnosis, while 6,345 were on nonbiologic systemic therapies (NBSTs) and 5,970 were on biologics. The researchers classified patients as having mild psoriasis if they were taking nonsystemic agents, moderate disease if they were taking NBSTs, or severe disease if they were taking biologics.
The overall incidence rate of PsA was 2.9 events per 100 PY and increased by severity of disease. When calculated by severity, the incidence was 2.1 events per 100 PY for patients with mild psoriasis, 9.9 events per 100 PY for those with moderate psoriasis, and 17.6 events per 100 PY for those with severe psoriasis.
When the researchers excluded patients diagnosed with PsA up to 1 year after being diagnosed with psoriasis, the overall incidence was lower (1.7 events per 100 PY), with similar trends for categories of treatment severity. Specifically, the incidence was 1.5, 3.1, and 4.7 events per 100 PY among those with mild, moderate, and severe psoriasis, based on their treatment groups, respectively.
Among the 120,523 patients with psoriasis who were eligible for the assessment of prevalence of PsA, the overall 5-year prevalence of PsA was 14.2% and rose with severity of disease: 9.9% in patients with mild psoriasis, 35% in patients with moderate psoriasis, and 54.9% in patients with severe psoriasis.
Other predictors of PsA onset for both index-date cohorts included weight of 90 kg or greater, female gender, age group 25-65 years (compared with the age group over 65 years), and rheumatic risk factors such as wrist pain and unspecified rheumatism.
“To ensure timely diagnosis and treatment for management and prevention of PsA, patients with [psoriasis] should be routinely screened, especially those with more severe disease and other PsA risk factors,” the authors advised.
Dr. Merola and colleagues acknowledged certain limitations of their analysis, including the potential for selection bias and its reliance on EHR data which “lacked clinical measures of disease severity such as the PASI, and data on BSA were not available for all study participants; therefore, treatment groups were used as a surrogate for disease severity,” they wrote. “As a result, some patients may have been miscategorized, especially patients with severe disease who were untreated.”
The study was sponsored by Novartis. Dr. Merola disclosed that he is a consultant and/or investigator for Merck, AbbVie, Dermavant, Eli Lilly, Novartis, Janssen, UCB, Celgene, Sanofi, Regeneron, Arena, Sun Pharmaceuticals, Biogen, Pfizer, EMD Serono, Avotres, and LEO Pharma. Four authors are Novartis employees, or employees of a consulting company that provides services to Novartis; and another author disclosed serving as an investigator or consultant for several pharmaceutical companies, including Novartis.
Factors that predict the development of psoriasis in patients with psoriasis include nail, inverse, and scalp psoriasis; family history of PsA; as well as severity of skin disease. And like psoriasis, “PsA is associated with a multitude of comorbidities, including cardiovascular disease, metabolic syndrome, Crohn’s disease, obesity, diabetes, uveitis, anxiety, and depression, with correspondingly higher healthcare utilization and direct healthcare costs,” wrote corresponding author Joseph F. Merola, MD, MMSc, and colleagues. The study was published online in the Journal of the American Academy of Dermatology. “Timely and accurate diagnosis of PsA is important for improved patient outcomes and appropriate disease management and may prevent prolonged inflammation that leads to structural joint damage and worsening physical function,” they added.
The mean time of onset of PsA among patients with psoriasis who develop PsA is 10 years after the first signs of psoriasis appear. An estimated 20%-30% of patients with psoriasis have a concurrent diagnosis of PsA, and the annual incidence of PsA has been reported to be 2.7 cases per 100 patients with psoriasis. While previous studies have suggested that a higher incidence of PsA is associated with greater disease severity, there are limited data in the United States on the topic.
For the study, Dr. Merola, a dermatologist and rheumatologist who directs the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston, and his colleagues drew from the Optum EHR database to identify adult patients newly diagnosed with psoriasis between Jan. 1, 2009, and March 31, 2019. Patients diagnosed with psoriasis or PsA prior to the index date were excluded from the analysis for evaluation of incidence but included for evaluation of prevalence. The patients were followed from the index date until the earliest PsA event, death, or end of study or follow-up, whichever came first. The researchers calculated the incidence of PsA among adults with psoriasis as the number of incident PsA events divided by the number of patient-years (PY) at risk, which was reported as the raw incidence per 100 psoriasis PY. They calculated the prevalence of PsA among adults with psoriasis as “the number of prevalent PsA events divided by the number of eligible patients with [psoriasis] and reported by years in the follow-up period,” which was a median of 3.7 years.
A total of 114,868 patients were included in the analysis. At baseline, their mean age was 54 years, 53% were female, 89% were White, and 39% were obese. Most patients (102,553) were on nonsystemic agents during the year after their psoriasis diagnosis, while 6,345 were on nonbiologic systemic therapies (NBSTs) and 5,970 were on biologics. The researchers classified patients as having mild psoriasis if they were taking nonsystemic agents, moderate disease if they were taking NBSTs, or severe disease if they were taking biologics.
The overall incidence rate of PsA was 2.9 events per 100 PY and increased by severity of disease. When calculated by severity, the incidence was 2.1 events per 100 PY for patients with mild psoriasis, 9.9 events per 100 PY for those with moderate psoriasis, and 17.6 events per 100 PY for those with severe psoriasis.
When the researchers excluded patients diagnosed with PsA up to 1 year after being diagnosed with psoriasis, the overall incidence was lower (1.7 events per 100 PY), with similar trends for categories of treatment severity. Specifically, the incidence was 1.5, 3.1, and 4.7 events per 100 PY among those with mild, moderate, and severe psoriasis, based on their treatment groups, respectively.
Among the 120,523 patients with psoriasis who were eligible for the assessment of prevalence of PsA, the overall 5-year prevalence of PsA was 14.2% and rose with severity of disease: 9.9% in patients with mild psoriasis, 35% in patients with moderate psoriasis, and 54.9% in patients with severe psoriasis.
Other predictors of PsA onset for both index-date cohorts included weight of 90 kg or greater, female gender, age group 25-65 years (compared with the age group over 65 years), and rheumatic risk factors such as wrist pain and unspecified rheumatism.
“To ensure timely diagnosis and treatment for management and prevention of PsA, patients with [psoriasis] should be routinely screened, especially those with more severe disease and other PsA risk factors,” the authors advised.
Dr. Merola and colleagues acknowledged certain limitations of their analysis, including the potential for selection bias and its reliance on EHR data which “lacked clinical measures of disease severity such as the PASI, and data on BSA were not available for all study participants; therefore, treatment groups were used as a surrogate for disease severity,” they wrote. “As a result, some patients may have been miscategorized, especially patients with severe disease who were untreated.”
The study was sponsored by Novartis. Dr. Merola disclosed that he is a consultant and/or investigator for Merck, AbbVie, Dermavant, Eli Lilly, Novartis, Janssen, UCB, Celgene, Sanofi, Regeneron, Arena, Sun Pharmaceuticals, Biogen, Pfizer, EMD Serono, Avotres, and LEO Pharma. Four authors are Novartis employees, or employees of a consulting company that provides services to Novartis; and another author disclosed serving as an investigator or consultant for several pharmaceutical companies, including Novartis.
Factors that predict the development of psoriasis in patients with psoriasis include nail, inverse, and scalp psoriasis; family history of PsA; as well as severity of skin disease. And like psoriasis, “PsA is associated with a multitude of comorbidities, including cardiovascular disease, metabolic syndrome, Crohn’s disease, obesity, diabetes, uveitis, anxiety, and depression, with correspondingly higher healthcare utilization and direct healthcare costs,” wrote corresponding author Joseph F. Merola, MD, MMSc, and colleagues. The study was published online in the Journal of the American Academy of Dermatology. “Timely and accurate diagnosis of PsA is important for improved patient outcomes and appropriate disease management and may prevent prolonged inflammation that leads to structural joint damage and worsening physical function,” they added.
The mean time of onset of PsA among patients with psoriasis who develop PsA is 10 years after the first signs of psoriasis appear. An estimated 20%-30% of patients with psoriasis have a concurrent diagnosis of PsA, and the annual incidence of PsA has been reported to be 2.7 cases per 100 patients with psoriasis. While previous studies have suggested that a higher incidence of PsA is associated with greater disease severity, there are limited data in the United States on the topic.
For the study, Dr. Merola, a dermatologist and rheumatologist who directs the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston, and his colleagues drew from the Optum EHR database to identify adult patients newly diagnosed with psoriasis between Jan. 1, 2009, and March 31, 2019. Patients diagnosed with psoriasis or PsA prior to the index date were excluded from the analysis for evaluation of incidence but included for evaluation of prevalence. The patients were followed from the index date until the earliest PsA event, death, or end of study or follow-up, whichever came first. The researchers calculated the incidence of PsA among adults with psoriasis as the number of incident PsA events divided by the number of patient-years (PY) at risk, which was reported as the raw incidence per 100 psoriasis PY. They calculated the prevalence of PsA among adults with psoriasis as “the number of prevalent PsA events divided by the number of eligible patients with [psoriasis] and reported by years in the follow-up period,” which was a median of 3.7 years.
A total of 114,868 patients were included in the analysis. At baseline, their mean age was 54 years, 53% were female, 89% were White, and 39% were obese. Most patients (102,553) were on nonsystemic agents during the year after their psoriasis diagnosis, while 6,345 were on nonbiologic systemic therapies (NBSTs) and 5,970 were on biologics. The researchers classified patients as having mild psoriasis if they were taking nonsystemic agents, moderate disease if they were taking NBSTs, or severe disease if they were taking biologics.
The overall incidence rate of PsA was 2.9 events per 100 PY and increased by severity of disease. When calculated by severity, the incidence was 2.1 events per 100 PY for patients with mild psoriasis, 9.9 events per 100 PY for those with moderate psoriasis, and 17.6 events per 100 PY for those with severe psoriasis.
When the researchers excluded patients diagnosed with PsA up to 1 year after being diagnosed with psoriasis, the overall incidence was lower (1.7 events per 100 PY), with similar trends for categories of treatment severity. Specifically, the incidence was 1.5, 3.1, and 4.7 events per 100 PY among those with mild, moderate, and severe psoriasis, based on their treatment groups, respectively.
Among the 120,523 patients with psoriasis who were eligible for the assessment of prevalence of PsA, the overall 5-year prevalence of PsA was 14.2% and rose with severity of disease: 9.9% in patients with mild psoriasis, 35% in patients with moderate psoriasis, and 54.9% in patients with severe psoriasis.
Other predictors of PsA onset for both index-date cohorts included weight of 90 kg or greater, female gender, age group 25-65 years (compared with the age group over 65 years), and rheumatic risk factors such as wrist pain and unspecified rheumatism.
“To ensure timely diagnosis and treatment for management and prevention of PsA, patients with [psoriasis] should be routinely screened, especially those with more severe disease and other PsA risk factors,” the authors advised.
Dr. Merola and colleagues acknowledged certain limitations of their analysis, including the potential for selection bias and its reliance on EHR data which “lacked clinical measures of disease severity such as the PASI, and data on BSA were not available for all study participants; therefore, treatment groups were used as a surrogate for disease severity,” they wrote. “As a result, some patients may have been miscategorized, especially patients with severe disease who were untreated.”
The study was sponsored by Novartis. Dr. Merola disclosed that he is a consultant and/or investigator for Merck, AbbVie, Dermavant, Eli Lilly, Novartis, Janssen, UCB, Celgene, Sanofi, Regeneron, Arena, Sun Pharmaceuticals, Biogen, Pfizer, EMD Serono, Avotres, and LEO Pharma. Four authors are Novartis employees, or employees of a consulting company that provides services to Novartis; and another author disclosed serving as an investigator or consultant for several pharmaceutical companies, including Novartis.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Pedunculated Tumor on the Posterior Neck
The Diagnosis: Nodular Hidradenoma
A biopsy of the nodule showed a large, fungating, well-circumscribed, multilobulated neoplasm composed of primarily monotonous eosinophilic cells in a background of keloidal stroma (Figure). There was a minority population of small, monotonous, clear cells within the lobules, and no glandular structures were noted. Neither cytological nor architectural atypia were evident. MART-1/Melan-A and S-100 stains were negative, consistent with a diagnosis of benign nodular hidradenoma.
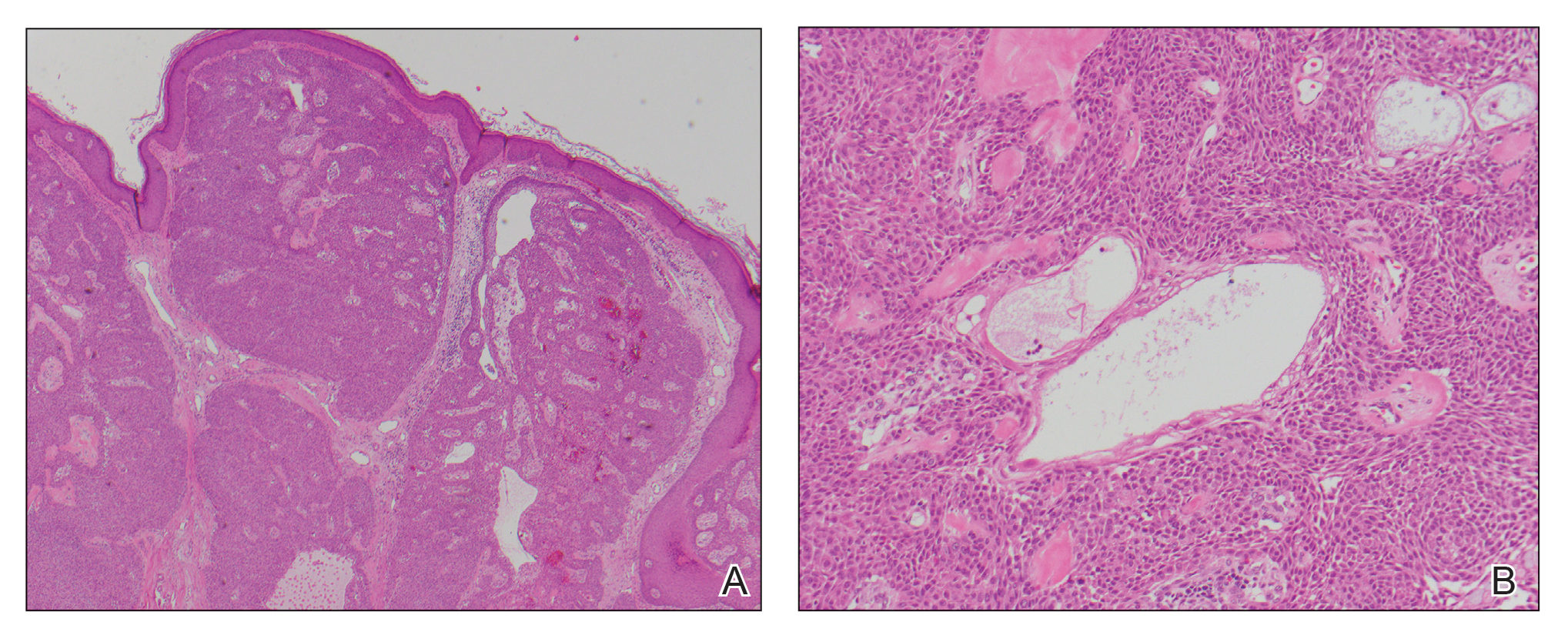
Nodular hidradenoma (also known as acrospiroma, solid-cystic hidradenoma, clear cell hidradenoma, and eccrine sweat gland adenoma) is a benign adnexal tumor of the apocrine or eccrine glands.1,2 Nodular hidradenoma can arise at any cutaneous site but most commonly arises on the head and anterior portion of the trunk and rarely on the extremities.2 It presents as a solitary nodular, cystic, or pedunculated mass that can reach up to several centimeters in diameter.2,3 Nodular hidradenoma more commonly affects women compared to men with a ratio of 1.7 to 1 and commonly presents between the third and fifth decades of life, with an average age at presentation of 37.2 years.2,4 There can be associated skin changes, including smoothening, thickening, ulceration, and bluish discoloration. Dermoscopy commonly shows a pinkish homogenous area that extends throughout the entire lesion. This homogenous area less commonly can be bluish, brownish, or pink-blue. Most nodular hidradenomas also can exhibit vascularization, with arborizing telangiectases, polymorphous atypical vessels, and linear irregular vessels being most common; however, this is not specific to nodular hidradenoma.3 Occasionally, tumors can drain serous or hemorrhagic fluid. Nodular hidradenoma commonly is a slow-growing tumor.5 Rapid increase in tumor size can be indicative of malignant transformation, hemorrhage into the tumor, or trauma to the area.2
Histologically, nodular hidradenoma consists of a circumscribed, nonencapsulated, multilobular tumor commonly found in the dermis and sometimes extending into the subcutaneous tissue. There usually is no epidermal attachment, and the overlying epidermis largely is normal. The tumor consists of large multilobulated areas of epithelial cells, tubular lamina, and large cystic areas filled with homogenous eosinophilic material.1 It notably is composed of 2 epithelial cell types: (1) fusiform cells with elongated vesicular nuclei and basophilic cytoplasm, and (2) large polygonal cells with round eccentric nuclei and eosinophilic, periodic acid–Schiff–positive cytoplasm that washes away during fixation, giving the appearance of clear cells.5 Both types of cells are small, monotonous, and void of mitosis or dyskeratosis. Although there can be ducts with apocrine secretion present within the lobulated tumor, they are not consistently found. Due to the varying features that are neither mandatory nor consistent to arrive at this diagnosis, some dermatopathologists view the term hidradenoma as a catch-all term that includes several different types of benign sweat gland tumors. Some authors divide the terminology into apocrine hidradenoma and eccrine hidradenoma based on whether the tumor is composed of solely clear mucinous cells, or poroid and cuticular cells, respectively.
Although nodular hidradenoma classically is a benign tumor, total surgical excision is recommended due to the rare risk for malignant transformation. Rarely, longstanding hidradenomas can metastasize to lymph nodes, bone, or viscera; in these instances, metastatic hidradenoma has a 5-year survival rate of 30%. Recurrence may occur in tumors that are inadequately excised, and the rate of recurrence is estimated to be approximately 10% of surgically excised tumors.5 However, utilization of Mohs micrographic surgery for excision of nodular hidradenoma is associated with a reduced recurrence rate.6
Keloids present as painful, sometimes pruritic, raised scars that extend beyond the boundary of the initial injury, commonly arising on the shoulder, upper arm, and chest. Histopathology reveals nodules of thick hyalinized collagen bundles, keloidal collagen with mucinous ground substance, and few fibroblasts.7
Metastatic renal cell carcinoma to the skin most commonly presents on the face and scalp as a nodular, rapidly growing, round to oval lesion that is flesh colored to reddish purple in a patient with history of renal cell carcinoma.8 Histopathology shows clusters of atypical, nucleated clear cells surrounded by chicken wire vasculature.8,9
Verruca vulgaris is caused by human papillomavirus and most commonly occurs on the hands and feet. It presents as a pink to white, sessile lesion with a verrucous surface and exophytic growths. Histopathology shows acanthosis; hypergranulosis; exophytic projections with a fibrovascular core; inward cupping of the rete ridges; and koilocytes, which are cells with an eccentric, raisinlike nucleus and vacuolated cytoplasm in the granular layer of the epidermis.10
Similar to nodular hidradenoma, nodular melanoma most commonly presents on the head and neck as a symmetric, elevated, amelanotic nodule, but in contrast to nodular hidradenoma, it typically is confined to a smaller diameter.11 Histologically, it is characterized by sheets of atypical, commonly epithelioid melanocytes with a lack of maturation and brisk mitotic activity extending through the epidermis and dermis with lateral extension limited to less than 3 rete ridges.12
- Patterson JW, Weedon D. Tumors of cutaneous appendages. In: Patterson JW, Weedon D. Weedon’s Skin Pathology. 5th ed. Elsevier; 2020:951-1016.
- Ngo N, Susa M, Nakagawa T, et al. Malignant transformation of nodular hidradenoma in the lower leg. Case Rep Oncol. 2018;11:298-304. doi:10.1159/000489255
- Zaballos P, Gómez-Martín I, Martin JM, et al. Dermoscopy of adnexal tumors. Dermatol Clin. 2018;36:397-412. doi:10.1016/j .det.2018.05.007
- Hernández-Pérez E, Cestoni-Parducci R. Nodular hidradenoma and hidradenocarcinoma: a 10-year review. J Am Acad Dermatol. 1985; 12:15-20. doi:10.1016/s0190-9622(85)70002-3
- Stratigos AJ, Olbricht S, Kwan TH, et al. Nodular hidradenoma. Dermatol Surg. 1998;24:387-391. doi:10.1111/j.1524-4725.1998.tb04173.x
- Yavel R, Hinshaw M, Rao V, et al. Hidradenomas and a hidradenocarcinoma of the scalp managed using Mohs micrographic surgery and a multidisciplinary approach. Dermatol Surg. 2009;35:273-281. doi:10.1111/j.1524-4725.2008.34424.x
- Lee JY-Y, Yang C-C, Chao S-C, et al. Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol. 2004;26:379-384. doi:10.1097/00000372-200410000-00006
- Ferhatoglu MF, Senol K, Filiz AI. Skin metastasis of renal cell carcinoma: a case report. Cureus. 2018;10:E3614. doi:10.7759/cureus.3614
- Jaitly V, Jahan-Tigh R, Belousova T, et al. Case report and literature review of nodular hidradenoma, a rare adnexal tumor that mimics breast carcinoma, in a 20-year-old woman. Lab Med. 2019;50:320-325. doi:10.1093/labmed/lmy084
- Betz SJ. HPV-related papillary lesions of the oral mucosa: a review. Head Neck Pathol. 2019;13:80-90. doi:10.1007/s12105-019-01003-7
- Kalkhoran S, Milne O, Zalaudek I, et al. Historical, clinical, and dermoscopic characteristics of thin nodular melanoma. Arch Dermatol. 2010;146:311-318. doi:10.1001/archdermatol.2009.369
- Smoller BR. Histologic criteria for diagnosing primary cutaneous malignant melanoma. Mod Pathol. 2006;19(suppl 2):S34-S40. doi:10.1038 /modpathol.3800508
The Diagnosis: Nodular Hidradenoma
A biopsy of the nodule showed a large, fungating, well-circumscribed, multilobulated neoplasm composed of primarily monotonous eosinophilic cells in a background of keloidal stroma (Figure). There was a minority population of small, monotonous, clear cells within the lobules, and no glandular structures were noted. Neither cytological nor architectural atypia were evident. MART-1/Melan-A and S-100 stains were negative, consistent with a diagnosis of benign nodular hidradenoma.
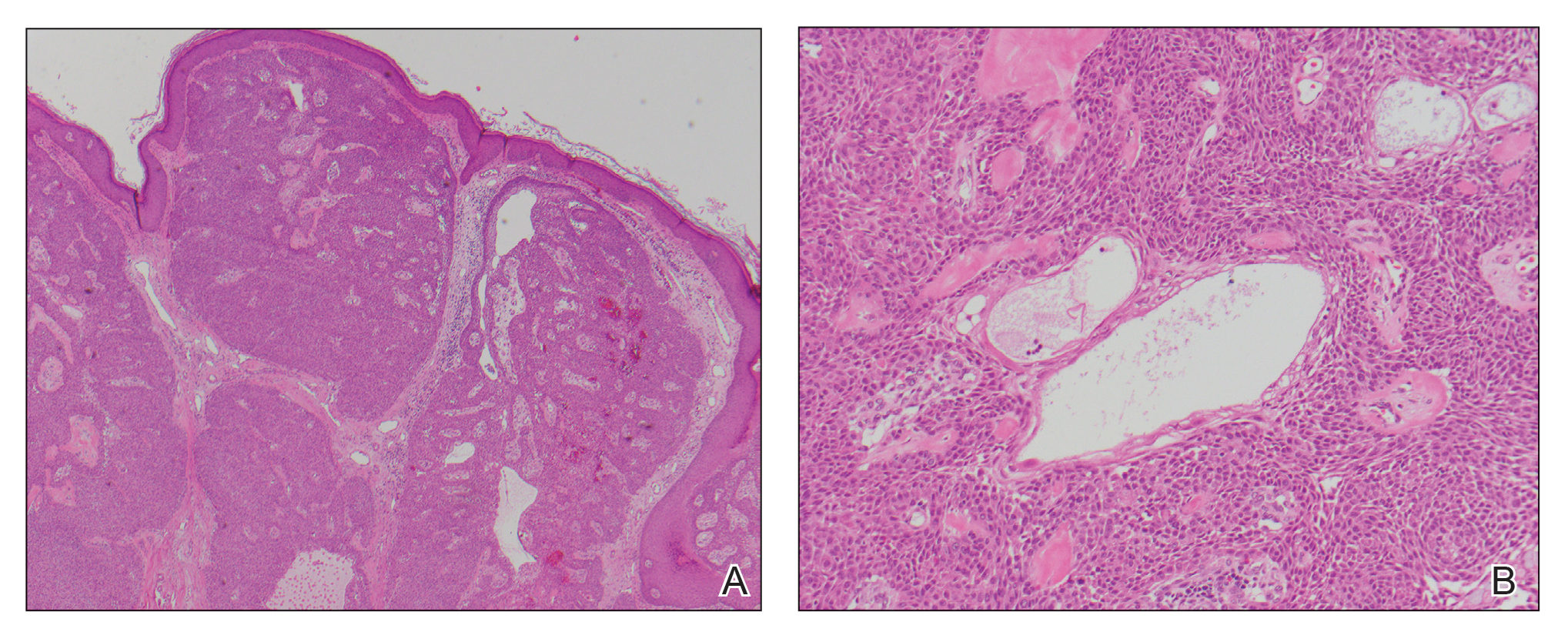
Nodular hidradenoma (also known as acrospiroma, solid-cystic hidradenoma, clear cell hidradenoma, and eccrine sweat gland adenoma) is a benign adnexal tumor of the apocrine or eccrine glands.1,2 Nodular hidradenoma can arise at any cutaneous site but most commonly arises on the head and anterior portion of the trunk and rarely on the extremities.2 It presents as a solitary nodular, cystic, or pedunculated mass that can reach up to several centimeters in diameter.2,3 Nodular hidradenoma more commonly affects women compared to men with a ratio of 1.7 to 1 and commonly presents between the third and fifth decades of life, with an average age at presentation of 37.2 years.2,4 There can be associated skin changes, including smoothening, thickening, ulceration, and bluish discoloration. Dermoscopy commonly shows a pinkish homogenous area that extends throughout the entire lesion. This homogenous area less commonly can be bluish, brownish, or pink-blue. Most nodular hidradenomas also can exhibit vascularization, with arborizing telangiectases, polymorphous atypical vessels, and linear irregular vessels being most common; however, this is not specific to nodular hidradenoma.3 Occasionally, tumors can drain serous or hemorrhagic fluid. Nodular hidradenoma commonly is a slow-growing tumor.5 Rapid increase in tumor size can be indicative of malignant transformation, hemorrhage into the tumor, or trauma to the area.2
Histologically, nodular hidradenoma consists of a circumscribed, nonencapsulated, multilobular tumor commonly found in the dermis and sometimes extending into the subcutaneous tissue. There usually is no epidermal attachment, and the overlying epidermis largely is normal. The tumor consists of large multilobulated areas of epithelial cells, tubular lamina, and large cystic areas filled with homogenous eosinophilic material.1 It notably is composed of 2 epithelial cell types: (1) fusiform cells with elongated vesicular nuclei and basophilic cytoplasm, and (2) large polygonal cells with round eccentric nuclei and eosinophilic, periodic acid–Schiff–positive cytoplasm that washes away during fixation, giving the appearance of clear cells.5 Both types of cells are small, monotonous, and void of mitosis or dyskeratosis. Although there can be ducts with apocrine secretion present within the lobulated tumor, they are not consistently found. Due to the varying features that are neither mandatory nor consistent to arrive at this diagnosis, some dermatopathologists view the term hidradenoma as a catch-all term that includes several different types of benign sweat gland tumors. Some authors divide the terminology into apocrine hidradenoma and eccrine hidradenoma based on whether the tumor is composed of solely clear mucinous cells, or poroid and cuticular cells, respectively.
Although nodular hidradenoma classically is a benign tumor, total surgical excision is recommended due to the rare risk for malignant transformation. Rarely, longstanding hidradenomas can metastasize to lymph nodes, bone, or viscera; in these instances, metastatic hidradenoma has a 5-year survival rate of 30%. Recurrence may occur in tumors that are inadequately excised, and the rate of recurrence is estimated to be approximately 10% of surgically excised tumors.5 However, utilization of Mohs micrographic surgery for excision of nodular hidradenoma is associated with a reduced recurrence rate.6
Keloids present as painful, sometimes pruritic, raised scars that extend beyond the boundary of the initial injury, commonly arising on the shoulder, upper arm, and chest. Histopathology reveals nodules of thick hyalinized collagen bundles, keloidal collagen with mucinous ground substance, and few fibroblasts.7
Metastatic renal cell carcinoma to the skin most commonly presents on the face and scalp as a nodular, rapidly growing, round to oval lesion that is flesh colored to reddish purple in a patient with history of renal cell carcinoma.8 Histopathology shows clusters of atypical, nucleated clear cells surrounded by chicken wire vasculature.8,9
Verruca vulgaris is caused by human papillomavirus and most commonly occurs on the hands and feet. It presents as a pink to white, sessile lesion with a verrucous surface and exophytic growths. Histopathology shows acanthosis; hypergranulosis; exophytic projections with a fibrovascular core; inward cupping of the rete ridges; and koilocytes, which are cells with an eccentric, raisinlike nucleus and vacuolated cytoplasm in the granular layer of the epidermis.10
Similar to nodular hidradenoma, nodular melanoma most commonly presents on the head and neck as a symmetric, elevated, amelanotic nodule, but in contrast to nodular hidradenoma, it typically is confined to a smaller diameter.11 Histologically, it is characterized by sheets of atypical, commonly epithelioid melanocytes with a lack of maturation and brisk mitotic activity extending through the epidermis and dermis with lateral extension limited to less than 3 rete ridges.12
The Diagnosis: Nodular Hidradenoma
A biopsy of the nodule showed a large, fungating, well-circumscribed, multilobulated neoplasm composed of primarily monotonous eosinophilic cells in a background of keloidal stroma (Figure). There was a minority population of small, monotonous, clear cells within the lobules, and no glandular structures were noted. Neither cytological nor architectural atypia were evident. MART-1/Melan-A and S-100 stains were negative, consistent with a diagnosis of benign nodular hidradenoma.
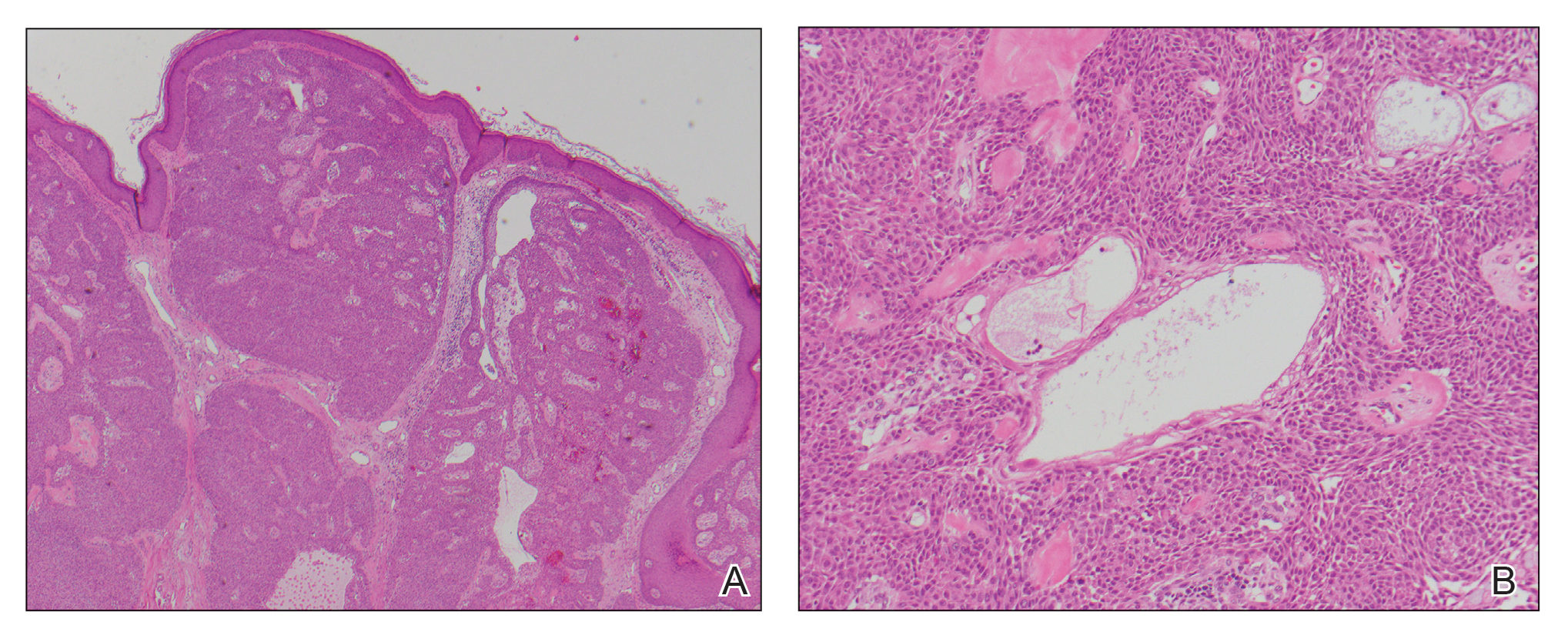
Nodular hidradenoma (also known as acrospiroma, solid-cystic hidradenoma, clear cell hidradenoma, and eccrine sweat gland adenoma) is a benign adnexal tumor of the apocrine or eccrine glands.1,2 Nodular hidradenoma can arise at any cutaneous site but most commonly arises on the head and anterior portion of the trunk and rarely on the extremities.2 It presents as a solitary nodular, cystic, or pedunculated mass that can reach up to several centimeters in diameter.2,3 Nodular hidradenoma more commonly affects women compared to men with a ratio of 1.7 to 1 and commonly presents between the third and fifth decades of life, with an average age at presentation of 37.2 years.2,4 There can be associated skin changes, including smoothening, thickening, ulceration, and bluish discoloration. Dermoscopy commonly shows a pinkish homogenous area that extends throughout the entire lesion. This homogenous area less commonly can be bluish, brownish, or pink-blue. Most nodular hidradenomas also can exhibit vascularization, with arborizing telangiectases, polymorphous atypical vessels, and linear irregular vessels being most common; however, this is not specific to nodular hidradenoma.3 Occasionally, tumors can drain serous or hemorrhagic fluid. Nodular hidradenoma commonly is a slow-growing tumor.5 Rapid increase in tumor size can be indicative of malignant transformation, hemorrhage into the tumor, or trauma to the area.2
Histologically, nodular hidradenoma consists of a circumscribed, nonencapsulated, multilobular tumor commonly found in the dermis and sometimes extending into the subcutaneous tissue. There usually is no epidermal attachment, and the overlying epidermis largely is normal. The tumor consists of large multilobulated areas of epithelial cells, tubular lamina, and large cystic areas filled with homogenous eosinophilic material.1 It notably is composed of 2 epithelial cell types: (1) fusiform cells with elongated vesicular nuclei and basophilic cytoplasm, and (2) large polygonal cells with round eccentric nuclei and eosinophilic, periodic acid–Schiff–positive cytoplasm that washes away during fixation, giving the appearance of clear cells.5 Both types of cells are small, monotonous, and void of mitosis or dyskeratosis. Although there can be ducts with apocrine secretion present within the lobulated tumor, they are not consistently found. Due to the varying features that are neither mandatory nor consistent to arrive at this diagnosis, some dermatopathologists view the term hidradenoma as a catch-all term that includes several different types of benign sweat gland tumors. Some authors divide the terminology into apocrine hidradenoma and eccrine hidradenoma based on whether the tumor is composed of solely clear mucinous cells, or poroid and cuticular cells, respectively.
Although nodular hidradenoma classically is a benign tumor, total surgical excision is recommended due to the rare risk for malignant transformation. Rarely, longstanding hidradenomas can metastasize to lymph nodes, bone, or viscera; in these instances, metastatic hidradenoma has a 5-year survival rate of 30%. Recurrence may occur in tumors that are inadequately excised, and the rate of recurrence is estimated to be approximately 10% of surgically excised tumors.5 However, utilization of Mohs micrographic surgery for excision of nodular hidradenoma is associated with a reduced recurrence rate.6
Keloids present as painful, sometimes pruritic, raised scars that extend beyond the boundary of the initial injury, commonly arising on the shoulder, upper arm, and chest. Histopathology reveals nodules of thick hyalinized collagen bundles, keloidal collagen with mucinous ground substance, and few fibroblasts.7
Metastatic renal cell carcinoma to the skin most commonly presents on the face and scalp as a nodular, rapidly growing, round to oval lesion that is flesh colored to reddish purple in a patient with history of renal cell carcinoma.8 Histopathology shows clusters of atypical, nucleated clear cells surrounded by chicken wire vasculature.8,9
Verruca vulgaris is caused by human papillomavirus and most commonly occurs on the hands and feet. It presents as a pink to white, sessile lesion with a verrucous surface and exophytic growths. Histopathology shows acanthosis; hypergranulosis; exophytic projections with a fibrovascular core; inward cupping of the rete ridges; and koilocytes, which are cells with an eccentric, raisinlike nucleus and vacuolated cytoplasm in the granular layer of the epidermis.10
Similar to nodular hidradenoma, nodular melanoma most commonly presents on the head and neck as a symmetric, elevated, amelanotic nodule, but in contrast to nodular hidradenoma, it typically is confined to a smaller diameter.11 Histologically, it is characterized by sheets of atypical, commonly epithelioid melanocytes with a lack of maturation and brisk mitotic activity extending through the epidermis and dermis with lateral extension limited to less than 3 rete ridges.12
- Patterson JW, Weedon D. Tumors of cutaneous appendages. In: Patterson JW, Weedon D. Weedon’s Skin Pathology. 5th ed. Elsevier; 2020:951-1016.
- Ngo N, Susa M, Nakagawa T, et al. Malignant transformation of nodular hidradenoma in the lower leg. Case Rep Oncol. 2018;11:298-304. doi:10.1159/000489255
- Zaballos P, Gómez-Martín I, Martin JM, et al. Dermoscopy of adnexal tumors. Dermatol Clin. 2018;36:397-412. doi:10.1016/j .det.2018.05.007
- Hernández-Pérez E, Cestoni-Parducci R. Nodular hidradenoma and hidradenocarcinoma: a 10-year review. J Am Acad Dermatol. 1985; 12:15-20. doi:10.1016/s0190-9622(85)70002-3
- Stratigos AJ, Olbricht S, Kwan TH, et al. Nodular hidradenoma. Dermatol Surg. 1998;24:387-391. doi:10.1111/j.1524-4725.1998.tb04173.x
- Yavel R, Hinshaw M, Rao V, et al. Hidradenomas and a hidradenocarcinoma of the scalp managed using Mohs micrographic surgery and a multidisciplinary approach. Dermatol Surg. 2009;35:273-281. doi:10.1111/j.1524-4725.2008.34424.x
- Lee JY-Y, Yang C-C, Chao S-C, et al. Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol. 2004;26:379-384. doi:10.1097/00000372-200410000-00006
- Ferhatoglu MF, Senol K, Filiz AI. Skin metastasis of renal cell carcinoma: a case report. Cureus. 2018;10:E3614. doi:10.7759/cureus.3614
- Jaitly V, Jahan-Tigh R, Belousova T, et al. Case report and literature review of nodular hidradenoma, a rare adnexal tumor that mimics breast carcinoma, in a 20-year-old woman. Lab Med. 2019;50:320-325. doi:10.1093/labmed/lmy084
- Betz SJ. HPV-related papillary lesions of the oral mucosa: a review. Head Neck Pathol. 2019;13:80-90. doi:10.1007/s12105-019-01003-7
- Kalkhoran S, Milne O, Zalaudek I, et al. Historical, clinical, and dermoscopic characteristics of thin nodular melanoma. Arch Dermatol. 2010;146:311-318. doi:10.1001/archdermatol.2009.369
- Smoller BR. Histologic criteria for diagnosing primary cutaneous malignant melanoma. Mod Pathol. 2006;19(suppl 2):S34-S40. doi:10.1038 /modpathol.3800508
- Patterson JW, Weedon D. Tumors of cutaneous appendages. In: Patterson JW, Weedon D. Weedon’s Skin Pathology. 5th ed. Elsevier; 2020:951-1016.
- Ngo N, Susa M, Nakagawa T, et al. Malignant transformation of nodular hidradenoma in the lower leg. Case Rep Oncol. 2018;11:298-304. doi:10.1159/000489255
- Zaballos P, Gómez-Martín I, Martin JM, et al. Dermoscopy of adnexal tumors. Dermatol Clin. 2018;36:397-412. doi:10.1016/j .det.2018.05.007
- Hernández-Pérez E, Cestoni-Parducci R. Nodular hidradenoma and hidradenocarcinoma: a 10-year review. J Am Acad Dermatol. 1985; 12:15-20. doi:10.1016/s0190-9622(85)70002-3
- Stratigos AJ, Olbricht S, Kwan TH, et al. Nodular hidradenoma. Dermatol Surg. 1998;24:387-391. doi:10.1111/j.1524-4725.1998.tb04173.x
- Yavel R, Hinshaw M, Rao V, et al. Hidradenomas and a hidradenocarcinoma of the scalp managed using Mohs micrographic surgery and a multidisciplinary approach. Dermatol Surg. 2009;35:273-281. doi:10.1111/j.1524-4725.2008.34424.x
- Lee JY-Y, Yang C-C, Chao S-C, et al. Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol. 2004;26:379-384. doi:10.1097/00000372-200410000-00006
- Ferhatoglu MF, Senol K, Filiz AI. Skin metastasis of renal cell carcinoma: a case report. Cureus. 2018;10:E3614. doi:10.7759/cureus.3614
- Jaitly V, Jahan-Tigh R, Belousova T, et al. Case report and literature review of nodular hidradenoma, a rare adnexal tumor that mimics breast carcinoma, in a 20-year-old woman. Lab Med. 2019;50:320-325. doi:10.1093/labmed/lmy084
- Betz SJ. HPV-related papillary lesions of the oral mucosa: a review. Head Neck Pathol. 2019;13:80-90. doi:10.1007/s12105-019-01003-7
- Kalkhoran S, Milne O, Zalaudek I, et al. Historical, clinical, and dermoscopic characteristics of thin nodular melanoma. Arch Dermatol. 2010;146:311-318. doi:10.1001/archdermatol.2009.369
- Smoller BR. Histologic criteria for diagnosing primary cutaneous malignant melanoma. Mod Pathol. 2006;19(suppl 2):S34-S40. doi:10.1038 /modpathol.3800508

A 56-year-old man presented with a progressively enlarging lesion on the posterior neck of 8 months’ duration. He reported localized pruritus of the lesion that improved with triamcinolone cream 0.05% and oral hydroxyzine as well as occasional irritation of the mass with oozing of clear fluid and blood. He denied associated pain and constitutional symptoms. Physical examination revealed a 2.5-cm, nodular, pedunculated, rubbery mass with foci of crusting on the central posterior neck. The mass was flesh colored to pink, and no lymphadenopathy was noted on physical examination.
Top questions answered about COVID-19 boosters for your patients
Confusion continues to circulate in the wake of decisions on booster doses of the Pfizer/BioNTech COVID-19 vaccine, all announced within 1 week. Many people – including those now eligible and those who officially have to wait for their shot at a third dose – have questions.
Multiple agencies are involved in the booster decisions, and they have put out multiple – and sometimes conflicting – messages about booster doses, leaving more questions than answers for many people.
On Sept. 22, the Food and Drug Administration granted an emergency use authorization (EUA) for a booster dose of the Pfizer mRNA COVID-19 vaccine for those 65 and older and those at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection – such as frontline health care workers.
The Centers for Disease Control and Prevention Director Rochelle Walensky, MD, then overruled advice from the agency’s Advisory Committee on Immunization Practices (ACIP) to recommend boosters for essential workers such as those working on the front lines during the pandemic.
As it stands now, the CDC recommends that the following groups should get a third dose of the Pfizer vaccine:
- People aged 65 years and older.
- People aged 18 years and older in long-term care settings.
- People aged 50-64 years with underlying medical conditions.
The CDC also recommends that the following groups may receive a booster shot of the Pfizer vaccine, based on their individual benefits and risks:
- People aged 18-49 years with underlying medical conditions.
- People aged 18-64 years at increased risk for COVID-19 exposure and transmission because of occupational or institutional setting.
The CDC currently considers the following groups at increased risk for COVID-19:
- First responders (health care workers, firefighters, police, congregate care staff).
- Education staff (teachers, support staff, day care workers).
- Food and agriculture workers.
- Manufacturing workers.
- Corrections workers.
- U.S. Postal Service workers.
- Public transit workers.
- Grocery store workers.
Health care professionals, among the most trusted sources of COVID-19 information, are likely to encounter a number of patients wondering how all this will work.
“It’s fantastic that boosters will be available for those who the data supports need [them],” Rachael Piltch-Loeb, PhD, said during a media briefing on Sept. 23, held between the FDA and CDC decisions.
“But we’re really in a place where we have a lot more questions and answers about what the next phase of the vaccine availability and updates are going to be in the United States,” added Dr. Piltch-Loeb, preparedness fellow in the division of policy translation and leadership development and a research associate in the department of biostatistics at the Harvard T. H. Chan School of Public Health in Boston.
1. What is the biggest concern you are hearing from patients about getting a booster?
“The biggest concerns are that everyone wants it and they don’t know where to get it. In health care’s defense, the CDC just figured out what to do,” said Janet Englund, MD, professor of pediatric infectious diseases and an infectious disease and virology expert at Seattle Children’s Hospital in Washington.
“Everyone thinks they should be eligible for a booster ... people in their 50s who are not yet 65+, people with young grandchildren, etc.,” she added. “I’m at Seattle Children’s Hospital, so people are asking about booster shots and about getting their children vaccinated.”
Boosters for all COVID-19 vaccines are completely free.
“All COVID-19 vaccines, including booster doses, will be provided free of charge to the U.S. population,” the CDC has said.
2. Will patients need to prove they meet eligibility criteria for a booster shot or will it be the honor system?
“No, patients will only need to attest that they fall into one of the high-risk groups for whom a booster vaccine is authorized,” said Robert Atmar, MD, professor of infectious diseases at Baylor College of Medicine in Houston.
Dr. Piltch-Loeb agreed. “It is likely to be an honor system. It is very unlikely that there will be punishments or other ramifications ... if doses are administered, beyond the approved usage.”
3. If a patient who had the Moderna or the Johnson and Johnson vaccination requests a booster, can health care workers give them Pfizer?
The short answer is no. “This only applies to individuals who have received the Pfizer vaccine,” Dr. Piltch-Loeb said.
More data will be needed before other vaccine boosters are authorized, she added.
“My understanding is the Moderna people have just recently submitted their information, all of their data to the FDA and J&J is in line to do that very shortly,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University in Nashville, Tenn. “I would hope that within the next month to 6 weeks, we will get information about both of those vaccines,” Dr. Schaffner said.
4. When are the “mix-and-match” vaccine study results expected to come out?
“We expect that data from the study will be available in the coming weeks,” said Dr. Atmar, who is the national co-principal investigator of a mix-and-match booster trial launched in June 2021.
5. Are side effects of a booster vaccine expected to be about the same as what people experienced during their first or second immunization?
“I’m expecting the side effects will be similar to the second dose,” Dr. Englund said.
“The data presented ... at ACIP suggests that the side effects from the third shot are either the same or actually less than the first two shots,” said Carlos del Rio, MD, distinguished professor of medicine, epidemiology, and global health, and executive associate dean of Emory University School of Medicine at Grady Health System in Atlanta.
”Everyone reacts very differently to vaccines, regardless of vaccine type,” said Eric Ascher, MD, a family medicine physician at Lenox Hill Hospital in New York City. “I have had patients (as well as personal experience) where there were none to minimal symptoms, and others who felt they had a mild flu for 24 hours.”
“I expect no side effects greater than what was felt with you prior doses,” he said. “The vaccine is very safe and the benefit of vaccination outweighs the risks of any mild side effects.”
6. Is it unethical to give a booster to someone outside the approved groups if there are doses remaining at the end of the day in an open vial?
“Offering a booster shot to someone outside of approved groups if remaining doses will go to waste at the end of the day seems like a prudent decision, and relatively harmless action,” said Faith Fletcher, PhD, assistant professor at the Center for Medical Ethics and Health Policy at Baylor College of Medicine.
“However, if doses continue to fall in the laps of unapproved groups, we must evaluate the vaccine systems and structures that advantage some groups and disadvantage others,” she added. “We know that the distribution of COVID-19 vaccines has not been equitable – and some groups have been left behind.”
“I am not an ethicist and there are many competing concerns that this question addresses,” Dr. Atmar said. For example, “there is not a limitation of vaccine supply in the U.S., so that using leftover vaccine to prevent waste is no longer a major concern in the U.S.”
It could be more of a legal than ethical question, Dr. Atmar said. For an individual outside the authorized groups, legally, the FDA’s EUA for boosting does not allow the vaccine to be administered to this person, he said.
“The rationale for the restricted use in the EUA is that at this time the safety and risks associated with such administration are not known, and the benefits also have not been determined,” Dr. Atmar said. “Members of the ACIP raised concerns about other individuals who may potentially benefit from a booster but are not eligible and the importance of making boosters available to them, but from a legal standpoint – I am also not a lawyer, so this is my understanding – administration of the vaccine is limited to those identified in the EUA.”
7. What is the likelihood that one shot will combine COVID and flu protection in the near future?
It is not likely, Dr. Englund said. “The reason is that the flu vaccine changes so much, and it already has four different antigens. This is assuming we keep the same method of making the flu vaccine – the answer could be different if the flu vaccine becomes an mRNA vaccine in the future.”
Companies such as Moderna and Novavax are testing single-dose shots for COVID-19 and influenza, but they are still far from having anything ready for this flu season in the United States.
8. Is there any chance a booster shot distributed now will need to be redesigned for a future variant?
“Absolutely,” Dr. Englund said. “And a booster dose is the time we may want to consider re-engineering a vaccine.”
9. Do you think the FDA/CDC limitations on who is eligible for a booster was in any way influenced by the World Health Organization call for prioritizing shots for the unvaccinated in lower-resource countries?
“This is absolutely still a global problem,” Dr. Piltch-Loeb said. “We need to get more vaccine to more countries and more people as soon as possible, because if there’s anything we’ve seen about the variants it is that ... they can come from all different places.”
“That being said, I think that it is unlikely to change the course of action in the U.S.,” she added, when it comes to comparing the global need with the domestic policy priorities of the administration.
Dr. Atmar was more direct. “No,” he said. “The WHO recommends against boosting of anyone. The U.S. decisions about boosting those in this country who are eligible are aimed toward addressing perceived needs domestically at the same time that vaccines are being provided to other countries.
“The philosophy is to address both ‘needs’ at the same time,” Dr. Atmar said.
10. What does the future hold for booster shots?
“Predicting the future is really hard, especially when it involves COVID,” Dr. del Rio said.
“Having said that, COVID is not the flu, so I doubt there will be need for annual boosters. I think the population eligible for boosters will be expanded ... and the major population not addressed at this point is the people that received either Moderna or J&J [vaccines].”
Kelly Davis contributed to this feature. A version of this article first appeared on Medscape.com.
Confusion continues to circulate in the wake of decisions on booster doses of the Pfizer/BioNTech COVID-19 vaccine, all announced within 1 week. Many people – including those now eligible and those who officially have to wait for their shot at a third dose – have questions.
Multiple agencies are involved in the booster decisions, and they have put out multiple – and sometimes conflicting – messages about booster doses, leaving more questions than answers for many people.
On Sept. 22, the Food and Drug Administration granted an emergency use authorization (EUA) for a booster dose of the Pfizer mRNA COVID-19 vaccine for those 65 and older and those at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection – such as frontline health care workers.
The Centers for Disease Control and Prevention Director Rochelle Walensky, MD, then overruled advice from the agency’s Advisory Committee on Immunization Practices (ACIP) to recommend boosters for essential workers such as those working on the front lines during the pandemic.
As it stands now, the CDC recommends that the following groups should get a third dose of the Pfizer vaccine:
- People aged 65 years and older.
- People aged 18 years and older in long-term care settings.
- People aged 50-64 years with underlying medical conditions.
The CDC also recommends that the following groups may receive a booster shot of the Pfizer vaccine, based on their individual benefits and risks:
- People aged 18-49 years with underlying medical conditions.
- People aged 18-64 years at increased risk for COVID-19 exposure and transmission because of occupational or institutional setting.
The CDC currently considers the following groups at increased risk for COVID-19:
- First responders (health care workers, firefighters, police, congregate care staff).
- Education staff (teachers, support staff, day care workers).
- Food and agriculture workers.
- Manufacturing workers.
- Corrections workers.
- U.S. Postal Service workers.
- Public transit workers.
- Grocery store workers.
Health care professionals, among the most trusted sources of COVID-19 information, are likely to encounter a number of patients wondering how all this will work.
“It’s fantastic that boosters will be available for those who the data supports need [them],” Rachael Piltch-Loeb, PhD, said during a media briefing on Sept. 23, held between the FDA and CDC decisions.
“But we’re really in a place where we have a lot more questions and answers about what the next phase of the vaccine availability and updates are going to be in the United States,” added Dr. Piltch-Loeb, preparedness fellow in the division of policy translation and leadership development and a research associate in the department of biostatistics at the Harvard T. H. Chan School of Public Health in Boston.
1. What is the biggest concern you are hearing from patients about getting a booster?
“The biggest concerns are that everyone wants it and they don’t know where to get it. In health care’s defense, the CDC just figured out what to do,” said Janet Englund, MD, professor of pediatric infectious diseases and an infectious disease and virology expert at Seattle Children’s Hospital in Washington.
“Everyone thinks they should be eligible for a booster ... people in their 50s who are not yet 65+, people with young grandchildren, etc.,” she added. “I’m at Seattle Children’s Hospital, so people are asking about booster shots and about getting their children vaccinated.”
Boosters for all COVID-19 vaccines are completely free.
“All COVID-19 vaccines, including booster doses, will be provided free of charge to the U.S. population,” the CDC has said.
2. Will patients need to prove they meet eligibility criteria for a booster shot or will it be the honor system?
“No, patients will only need to attest that they fall into one of the high-risk groups for whom a booster vaccine is authorized,” said Robert Atmar, MD, professor of infectious diseases at Baylor College of Medicine in Houston.
Dr. Piltch-Loeb agreed. “It is likely to be an honor system. It is very unlikely that there will be punishments or other ramifications ... if doses are administered, beyond the approved usage.”
3. If a patient who had the Moderna or the Johnson and Johnson vaccination requests a booster, can health care workers give them Pfizer?
The short answer is no. “This only applies to individuals who have received the Pfizer vaccine,” Dr. Piltch-Loeb said.
More data will be needed before other vaccine boosters are authorized, she added.
“My understanding is the Moderna people have just recently submitted their information, all of their data to the FDA and J&J is in line to do that very shortly,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University in Nashville, Tenn. “I would hope that within the next month to 6 weeks, we will get information about both of those vaccines,” Dr. Schaffner said.
4. When are the “mix-and-match” vaccine study results expected to come out?
“We expect that data from the study will be available in the coming weeks,” said Dr. Atmar, who is the national co-principal investigator of a mix-and-match booster trial launched in June 2021.
5. Are side effects of a booster vaccine expected to be about the same as what people experienced during their first or second immunization?
“I’m expecting the side effects will be similar to the second dose,” Dr. Englund said.
“The data presented ... at ACIP suggests that the side effects from the third shot are either the same or actually less than the first two shots,” said Carlos del Rio, MD, distinguished professor of medicine, epidemiology, and global health, and executive associate dean of Emory University School of Medicine at Grady Health System in Atlanta.
”Everyone reacts very differently to vaccines, regardless of vaccine type,” said Eric Ascher, MD, a family medicine physician at Lenox Hill Hospital in New York City. “I have had patients (as well as personal experience) where there were none to minimal symptoms, and others who felt they had a mild flu for 24 hours.”
“I expect no side effects greater than what was felt with you prior doses,” he said. “The vaccine is very safe and the benefit of vaccination outweighs the risks of any mild side effects.”
6. Is it unethical to give a booster to someone outside the approved groups if there are doses remaining at the end of the day in an open vial?
“Offering a booster shot to someone outside of approved groups if remaining doses will go to waste at the end of the day seems like a prudent decision, and relatively harmless action,” said Faith Fletcher, PhD, assistant professor at the Center for Medical Ethics and Health Policy at Baylor College of Medicine.
“However, if doses continue to fall in the laps of unapproved groups, we must evaluate the vaccine systems and structures that advantage some groups and disadvantage others,” she added. “We know that the distribution of COVID-19 vaccines has not been equitable – and some groups have been left behind.”
“I am not an ethicist and there are many competing concerns that this question addresses,” Dr. Atmar said. For example, “there is not a limitation of vaccine supply in the U.S., so that using leftover vaccine to prevent waste is no longer a major concern in the U.S.”
It could be more of a legal than ethical question, Dr. Atmar said. For an individual outside the authorized groups, legally, the FDA’s EUA for boosting does not allow the vaccine to be administered to this person, he said.
“The rationale for the restricted use in the EUA is that at this time the safety and risks associated with such administration are not known, and the benefits also have not been determined,” Dr. Atmar said. “Members of the ACIP raised concerns about other individuals who may potentially benefit from a booster but are not eligible and the importance of making boosters available to them, but from a legal standpoint – I am also not a lawyer, so this is my understanding – administration of the vaccine is limited to those identified in the EUA.”
7. What is the likelihood that one shot will combine COVID and flu protection in the near future?
It is not likely, Dr. Englund said. “The reason is that the flu vaccine changes so much, and it already has four different antigens. This is assuming we keep the same method of making the flu vaccine – the answer could be different if the flu vaccine becomes an mRNA vaccine in the future.”
Companies such as Moderna and Novavax are testing single-dose shots for COVID-19 and influenza, but they are still far from having anything ready for this flu season in the United States.
8. Is there any chance a booster shot distributed now will need to be redesigned for a future variant?
“Absolutely,” Dr. Englund said. “And a booster dose is the time we may want to consider re-engineering a vaccine.”
9. Do you think the FDA/CDC limitations on who is eligible for a booster was in any way influenced by the World Health Organization call for prioritizing shots for the unvaccinated in lower-resource countries?
“This is absolutely still a global problem,” Dr. Piltch-Loeb said. “We need to get more vaccine to more countries and more people as soon as possible, because if there’s anything we’ve seen about the variants it is that ... they can come from all different places.”
“That being said, I think that it is unlikely to change the course of action in the U.S.,” she added, when it comes to comparing the global need with the domestic policy priorities of the administration.
Dr. Atmar was more direct. “No,” he said. “The WHO recommends against boosting of anyone. The U.S. decisions about boosting those in this country who are eligible are aimed toward addressing perceived needs domestically at the same time that vaccines are being provided to other countries.
“The philosophy is to address both ‘needs’ at the same time,” Dr. Atmar said.
10. What does the future hold for booster shots?
“Predicting the future is really hard, especially when it involves COVID,” Dr. del Rio said.
“Having said that, COVID is not the flu, so I doubt there will be need for annual boosters. I think the population eligible for boosters will be expanded ... and the major population not addressed at this point is the people that received either Moderna or J&J [vaccines].”
Kelly Davis contributed to this feature. A version of this article first appeared on Medscape.com.
Confusion continues to circulate in the wake of decisions on booster doses of the Pfizer/BioNTech COVID-19 vaccine, all announced within 1 week. Many people – including those now eligible and those who officially have to wait for their shot at a third dose – have questions.
Multiple agencies are involved in the booster decisions, and they have put out multiple – and sometimes conflicting – messages about booster doses, leaving more questions than answers for many people.
On Sept. 22, the Food and Drug Administration granted an emergency use authorization (EUA) for a booster dose of the Pfizer mRNA COVID-19 vaccine for those 65 and older and those at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection – such as frontline health care workers.
The Centers for Disease Control and Prevention Director Rochelle Walensky, MD, then overruled advice from the agency’s Advisory Committee on Immunization Practices (ACIP) to recommend boosters for essential workers such as those working on the front lines during the pandemic.
As it stands now, the CDC recommends that the following groups should get a third dose of the Pfizer vaccine:
- People aged 65 years and older.
- People aged 18 years and older in long-term care settings.
- People aged 50-64 years with underlying medical conditions.
The CDC also recommends that the following groups may receive a booster shot of the Pfizer vaccine, based on their individual benefits and risks:
- People aged 18-49 years with underlying medical conditions.
- People aged 18-64 years at increased risk for COVID-19 exposure and transmission because of occupational or institutional setting.
The CDC currently considers the following groups at increased risk for COVID-19:
- First responders (health care workers, firefighters, police, congregate care staff).
- Education staff (teachers, support staff, day care workers).
- Food and agriculture workers.
- Manufacturing workers.
- Corrections workers.
- U.S. Postal Service workers.
- Public transit workers.
- Grocery store workers.
Health care professionals, among the most trusted sources of COVID-19 information, are likely to encounter a number of patients wondering how all this will work.
“It’s fantastic that boosters will be available for those who the data supports need [them],” Rachael Piltch-Loeb, PhD, said during a media briefing on Sept. 23, held between the FDA and CDC decisions.
“But we’re really in a place where we have a lot more questions and answers about what the next phase of the vaccine availability and updates are going to be in the United States,” added Dr. Piltch-Loeb, preparedness fellow in the division of policy translation and leadership development and a research associate in the department of biostatistics at the Harvard T. H. Chan School of Public Health in Boston.
1. What is the biggest concern you are hearing from patients about getting a booster?
“The biggest concerns are that everyone wants it and they don’t know where to get it. In health care’s defense, the CDC just figured out what to do,” said Janet Englund, MD, professor of pediatric infectious diseases and an infectious disease and virology expert at Seattle Children’s Hospital in Washington.
“Everyone thinks they should be eligible for a booster ... people in their 50s who are not yet 65+, people with young grandchildren, etc.,” she added. “I’m at Seattle Children’s Hospital, so people are asking about booster shots and about getting their children vaccinated.”
Boosters for all COVID-19 vaccines are completely free.
“All COVID-19 vaccines, including booster doses, will be provided free of charge to the U.S. population,” the CDC has said.
2. Will patients need to prove they meet eligibility criteria for a booster shot or will it be the honor system?
“No, patients will only need to attest that they fall into one of the high-risk groups for whom a booster vaccine is authorized,” said Robert Atmar, MD, professor of infectious diseases at Baylor College of Medicine in Houston.
Dr. Piltch-Loeb agreed. “It is likely to be an honor system. It is very unlikely that there will be punishments or other ramifications ... if doses are administered, beyond the approved usage.”
3. If a patient who had the Moderna or the Johnson and Johnson vaccination requests a booster, can health care workers give them Pfizer?
The short answer is no. “This only applies to individuals who have received the Pfizer vaccine,” Dr. Piltch-Loeb said.
More data will be needed before other vaccine boosters are authorized, she added.
“My understanding is the Moderna people have just recently submitted their information, all of their data to the FDA and J&J is in line to do that very shortly,” said William Schaffner, MD, professor of preventive medicine and infectious diseases at Vanderbilt University in Nashville, Tenn. “I would hope that within the next month to 6 weeks, we will get information about both of those vaccines,” Dr. Schaffner said.
4. When are the “mix-and-match” vaccine study results expected to come out?
“We expect that data from the study will be available in the coming weeks,” said Dr. Atmar, who is the national co-principal investigator of a mix-and-match booster trial launched in June 2021.
5. Are side effects of a booster vaccine expected to be about the same as what people experienced during their first or second immunization?
“I’m expecting the side effects will be similar to the second dose,” Dr. Englund said.
“The data presented ... at ACIP suggests that the side effects from the third shot are either the same or actually less than the first two shots,” said Carlos del Rio, MD, distinguished professor of medicine, epidemiology, and global health, and executive associate dean of Emory University School of Medicine at Grady Health System in Atlanta.
”Everyone reacts very differently to vaccines, regardless of vaccine type,” said Eric Ascher, MD, a family medicine physician at Lenox Hill Hospital in New York City. “I have had patients (as well as personal experience) where there were none to minimal symptoms, and others who felt they had a mild flu for 24 hours.”
“I expect no side effects greater than what was felt with you prior doses,” he said. “The vaccine is very safe and the benefit of vaccination outweighs the risks of any mild side effects.”
6. Is it unethical to give a booster to someone outside the approved groups if there are doses remaining at the end of the day in an open vial?
“Offering a booster shot to someone outside of approved groups if remaining doses will go to waste at the end of the day seems like a prudent decision, and relatively harmless action,” said Faith Fletcher, PhD, assistant professor at the Center for Medical Ethics and Health Policy at Baylor College of Medicine.
“However, if doses continue to fall in the laps of unapproved groups, we must evaluate the vaccine systems and structures that advantage some groups and disadvantage others,” she added. “We know that the distribution of COVID-19 vaccines has not been equitable – and some groups have been left behind.”
“I am not an ethicist and there are many competing concerns that this question addresses,” Dr. Atmar said. For example, “there is not a limitation of vaccine supply in the U.S., so that using leftover vaccine to prevent waste is no longer a major concern in the U.S.”
It could be more of a legal than ethical question, Dr. Atmar said. For an individual outside the authorized groups, legally, the FDA’s EUA for boosting does not allow the vaccine to be administered to this person, he said.
“The rationale for the restricted use in the EUA is that at this time the safety and risks associated with such administration are not known, and the benefits also have not been determined,” Dr. Atmar said. “Members of the ACIP raised concerns about other individuals who may potentially benefit from a booster but are not eligible and the importance of making boosters available to them, but from a legal standpoint – I am also not a lawyer, so this is my understanding – administration of the vaccine is limited to those identified in the EUA.”
7. What is the likelihood that one shot will combine COVID and flu protection in the near future?
It is not likely, Dr. Englund said. “The reason is that the flu vaccine changes so much, and it already has four different antigens. This is assuming we keep the same method of making the flu vaccine – the answer could be different if the flu vaccine becomes an mRNA vaccine in the future.”
Companies such as Moderna and Novavax are testing single-dose shots for COVID-19 and influenza, but they are still far from having anything ready for this flu season in the United States.
8. Is there any chance a booster shot distributed now will need to be redesigned for a future variant?
“Absolutely,” Dr. Englund said. “And a booster dose is the time we may want to consider re-engineering a vaccine.”
9. Do you think the FDA/CDC limitations on who is eligible for a booster was in any way influenced by the World Health Organization call for prioritizing shots for the unvaccinated in lower-resource countries?
“This is absolutely still a global problem,” Dr. Piltch-Loeb said. “We need to get more vaccine to more countries and more people as soon as possible, because if there’s anything we’ve seen about the variants it is that ... they can come from all different places.”
“That being said, I think that it is unlikely to change the course of action in the U.S.,” she added, when it comes to comparing the global need with the domestic policy priorities of the administration.
Dr. Atmar was more direct. “No,” he said. “The WHO recommends against boosting of anyone. The U.S. decisions about boosting those in this country who are eligible are aimed toward addressing perceived needs domestically at the same time that vaccines are being provided to other countries.
“The philosophy is to address both ‘needs’ at the same time,” Dr. Atmar said.
10. What does the future hold for booster shots?
“Predicting the future is really hard, especially when it involves COVID,” Dr. del Rio said.
“Having said that, COVID is not the flu, so I doubt there will be need for annual boosters. I think the population eligible for boosters will be expanded ... and the major population not addressed at this point is the people that received either Moderna or J&J [vaccines].”
Kelly Davis contributed to this feature. A version of this article first appeared on Medscape.com.