User login
News and Views that Matter to Physicians
New Book Chronicles Advances in Understanding NMO and Provides Blueprint for Other Rare Diseases
The Power of Rare: A Blueprint for a Medical Revolution by Victoria Jackson and Michael Yeaman, PhD, provides a model for breaking down silos of medical research to bring together innovative thinkers to advance understanding of rare diseases. Brian Weinshenker, MD, Professor of Neurology at Mayo Clinic, wrote in his review: “In the last decade, neuromyelitis optica has evolved from being unknown to being a Rosetta stone in the understanding of autoimmune disease. In The Power of Rare, Victoria Jackson tells how she catalyzed this transformation by forging a community of medical and scientific allies to change thinking and solve problems.”
The Power of Rare: A Blueprint for a Medical Revolution by Victoria Jackson and Michael Yeaman, PhD, provides a model for breaking down silos of medical research to bring together innovative thinkers to advance understanding of rare diseases. Brian Weinshenker, MD, Professor of Neurology at Mayo Clinic, wrote in his review: “In the last decade, neuromyelitis optica has evolved from being unknown to being a Rosetta stone in the understanding of autoimmune disease. In The Power of Rare, Victoria Jackson tells how she catalyzed this transformation by forging a community of medical and scientific allies to change thinking and solve problems.”
The Power of Rare: A Blueprint for a Medical Revolution by Victoria Jackson and Michael Yeaman, PhD, provides a model for breaking down silos of medical research to bring together innovative thinkers to advance understanding of rare diseases. Brian Weinshenker, MD, Professor of Neurology at Mayo Clinic, wrote in his review: “In the last decade, neuromyelitis optica has evolved from being unknown to being a Rosetta stone in the understanding of autoimmune disease. In The Power of Rare, Victoria Jackson tells how she catalyzed this transformation by forging a community of medical and scientific allies to change thinking and solve problems.”
Guthy-Jackson Charitable Foundation Produces New NMO Podcast
A new podcast series, NMO and the Power of Rare, is now available from the Guthy-Jackson Charitable Foundation. NMO or neuromyelitis optica affects the optic nerves, spinal cord, and brainstem. It can cause blindness and/or paralysis. It is sometimes misdiagnosed as MS.
Episode 1 of the series is titled “The NMO Revolution: The Top 5 NMO Breakthroughs in the Past 5 Years.” Nancy Sicotte, MD, Director of the MS Program at Cedars-Sinai Medical Center, is interviewed for this episode.
A new podcast series, NMO and the Power of Rare, is now available from the Guthy-Jackson Charitable Foundation. NMO or neuromyelitis optica affects the optic nerves, spinal cord, and brainstem. It can cause blindness and/or paralysis. It is sometimes misdiagnosed as MS.
Episode 1 of the series is titled “The NMO Revolution: The Top 5 NMO Breakthroughs in the Past 5 Years.” Nancy Sicotte, MD, Director of the MS Program at Cedars-Sinai Medical Center, is interviewed for this episode.
A new podcast series, NMO and the Power of Rare, is now available from the Guthy-Jackson Charitable Foundation. NMO or neuromyelitis optica affects the optic nerves, spinal cord, and brainstem. It can cause blindness and/or paralysis. It is sometimes misdiagnosed as MS.
Episode 1 of the series is titled “The NMO Revolution: The Top 5 NMO Breakthroughs in the Past 5 Years.” Nancy Sicotte, MD, Director of the MS Program at Cedars-Sinai Medical Center, is interviewed for this episode.
Neuroendocrine Tumor Research Foundation Announces Change of Leadership
After six successful years, Ron Hollander will be stepping down as executive director of the Neuroendocrine Tumor Research Foundation. His successor will be Elyse Gellerman. More.
After six successful years, Ron Hollander will be stepping down as executive director of the Neuroendocrine Tumor Research Foundation. His successor will be Elyse Gellerman. More.
After six successful years, Ron Hollander will be stepping down as executive director of the Neuroendocrine Tumor Research Foundation. His successor will be Elyse Gellerman. More.
Morgan Leary Vaughan Fund Receives Petit Family Foundation Grant
The Morgan Leary Vaughan Fund has received a grant from the Petit Family Foundation in support of the inaugural “Speaking of NEC: Unplugged” event, a one-day regional conference on identifying practical solutions to reduce the devastating effects of necrotizing enterocolitis on premature infants and their families. The event will take place in Hartford, Connecticut, in the spring of 2018.
The Morgan Leary Vaughan Fund has received a grant from the Petit Family Foundation in support of the inaugural “Speaking of NEC: Unplugged” event, a one-day regional conference on identifying practical solutions to reduce the devastating effects of necrotizing enterocolitis on premature infants and their families. The event will take place in Hartford, Connecticut, in the spring of 2018.
The Morgan Leary Vaughan Fund has received a grant from the Petit Family Foundation in support of the inaugural “Speaking of NEC: Unplugged” event, a one-day regional conference on identifying practical solutions to reduce the devastating effects of necrotizing enterocolitis on premature infants and their families. The event will take place in Hartford, Connecticut, in the spring of 2018.
Bridge the Gap – SYNGAP Education and Research Foundation
Register today for the first annual STEP UP for SYNGAP1 Walk at the Houston Zoo. Come walk a 5K among the animals and enjoy a day of family fun on Saturday, December 9, 2017.
Register today for the first annual STEP UP for SYNGAP1 Walk at the Houston Zoo. Come walk a 5K among the animals and enjoy a day of family fun on Saturday, December 9, 2017.
Register today for the first annual STEP UP for SYNGAP1 Walk at the Houston Zoo. Come walk a 5K among the animals and enjoy a day of family fun on Saturday, December 9, 2017.
American Partnership for Eosinophilic Disorders (APFED) Pilot Grants
APFED is now accepting applications for three 2018 HOPE Pilot Grants. This program was established to allow investigators from various disciplines to initiate new projects related to eosinophilic-associated diseases. Find additional information here.
Also, join APFED for an evening of music and fundraising in New York City on November 10, 2017. The event will feature Mike DelGuidice and Big Shot, celebrating the music of Billy Joel. More.
APFED is now accepting applications for three 2018 HOPE Pilot Grants. This program was established to allow investigators from various disciplines to initiate new projects related to eosinophilic-associated diseases. Find additional information here.
Also, join APFED for an evening of music and fundraising in New York City on November 10, 2017. The event will feature Mike DelGuidice and Big Shot, celebrating the music of Billy Joel. More.
APFED is now accepting applications for three 2018 HOPE Pilot Grants. This program was established to allow investigators from various disciplines to initiate new projects related to eosinophilic-associated diseases. Find additional information here.
Also, join APFED for an evening of music and fundraising in New York City on November 10, 2017. The event will feature Mike DelGuidice and Big Shot, celebrating the music of Billy Joel. More.
Adrenal Insufficiency United (AIU) Conference
Registration is now open for AIU’s first-ever conference. The event will take place March 23-25, 2018, in Kansas City. Leading experts will speak on a wide variety of topics important to the AI community. More.
Registration is now open for AIU’s first-ever conference. The event will take place March 23-25, 2018, in Kansas City. Leading experts will speak on a wide variety of topics important to the AI community. More.
Registration is now open for AIU’s first-ever conference. The event will take place March 23-25, 2018, in Kansas City. Leading experts will speak on a wide variety of topics important to the AI community. More.
Making Practice Perfect Download
Please click either of the links below to download your free eBook
Onecount Call To Arms
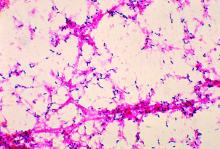
Streptococcal pneumonia’s resistance to macrolides increasing
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
FROM IDWEEK 2016
Key clinical point:
Major finding: S. pneumoniae isolates’ average resistance to the macrolide azithromycin was 48.4% in 2014.
Data source: A prospective collection and investigation of 4,567 non-replicative community-acquired bacterial pneumonia isolates.
Disclosures: The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.