User login
American Society of Clinical Oncology (ASCO): Breast Cancer Symposium
Should ductal carcinoma in situ be treated?
Remarks given during a session of the ASCO Breast Cancer Symposium titled Ductal Carcinoma in Situ Debate: Treatment vs. Observation
Dr. Kuerer comments: There has been a marked increase ductal carcinoma in situ (DCIS) in what is being called overdiagnosis, and this is leading to concerns of overtreatment, which has been in the news now for several years. We have more than 60,000 cases of DCIS diagnosed per year in the United States. We’re trying to prevent invasive breast cancer and distant metastases. The problem is identifying which patients will go on to develop invasive disease. That’s really unknown.
At M.D. Anderson, looking at 10-year follow-up of 2,449 patients, the rate of developing distant metastases was 0.1%. The problem with this is that no prominent variables were associated with the development of invasive metastatic disease. Overall, we are doing a good job at preventing death from breast cancer when we treat DCIS, with less than 1% of patients dying of breast cancer (Ann. Surg. Onc. 2011;18:2873-8).
Dr. Shelley E. Hwang and her group very elegantly started exploring preoperative systemic therapy as a way to get a clue about which patients might be safely observed alone (that is, a core biopsy diagnosis of DCIS and then just follow-up without surgery or other treatments). At M.D. Anderson, we studied whether or not we could eradicate DCIS in patients with human epidermal growth factor receptor 2 (HER2) overexpression by treatment with trastuzumab prior to surgery, under the hypothesis that if we could eradicate the DCIS, we might eventually use this drug potentially to prevent HER2-positive invasive breast cancers. We saw very dramatic responses in their immune response with antibody-dependent cellular cytotoxicity mediated by natural killer cells, which is exciting, but there were no histopathologic changes. The most important finding was that 42% of our patients who we thought only had DCIS actually had occult invasive breast cancer (Cancer 2011;117:39-47). This is concerning because without surgery, we may be missing or leaving untreated invasive breast cancers in some patients.
So, we have an underestimation of invasive breast cancer at DCIS diagnosis. A very elegant meta-analysis of 7,350 patients reported that even if we take patients with non–high-grade, very-small DCIS, we’re still looking at an upgrade to invasive cancer of about 20% (Radiology 2011;260:119-28). The best and most recent studies of MRI and DCIS again found a diagnostic upgrade of about 27%. There were no MRI features correlating with invasive breast cancer, and this resulted in a 31% increase in procedures and more biopsies with the use of MRI.
So where are we? In active surveillance of 14 patients with DCIS at the University of California, San Francisco, 8 went on to surgery at a median follow-up of 28 months, and 5 of the 8 (62%) had invasive breast cancer (The Breast 2011;20:529-33).
What’s the cost to the health care system of surveillance if we biopsy only the DCIS and follow it without surgery or other adjuvant therapies? The psychological cost to our patients? What is the natural history of DCIS if left in place? What will be the result of microcalcifications? How are we going to follow this? What are the criteria that we will use for repeat biopsy? This really is not known.
Which are the patients that we’re going to select for observation alone? There are trials in Europe that have begun or will begin to address the safety of just observing DCIS without surgery and other therapies.
The United Kingdom Low-Risk DCIS Trial is randomizing patients with low and intermediate grade DCIS of any size to biopsy alone without surgical intervention (active monitoring) or standard therapy. Another trial, a joint Dutch Breast Cancer Research Group and European Organization for the Research and Treatment of Cancer trial is randomizing women with low-risk, low-grade DCIS to active surveillance or standard treatment. If we look at M.D. Anderson’s data and our National Cancer Database, only about 10%-15% of patients would be eligible for the latter study. I don’t think with these numbers we’d have a great impact, but it is a start.
I submit that the best U.S. patients to study will be patients with a diagnosis of atypical ductal hyperplasia (generally the smallest lesions and perhaps the earliest form of DCIS) because we have about 100,000 cases each year.
What’s the patient’s perspective? What about the need for continued repeat biopsies, and how this will affect their overall quality of life? Do patients in the United States really want to observe the DCIS in an era when our patients are requesting more and more mastectomy with reconstruction and contralateral mastectomy at diagnosis of DCIS? I seriously doubt that our patients in the United States would agree to be randomized in DCIS trials to no treatment at all. I really don’t know.
Dr. Kuerer is a professor of surgery at the University of Texas M.D. Anderson Cancer Center, Houston. He reported financial associations with Gerson Lehrman Group and McGraw-Hill Publishing.
Dr. Hwang comments: Today, about 1/1,300 screening mammograms result in a diagnosis of DCIS. There are two important considerations when we talk about active surveillance or doing less aggressive treatment. First, what is the rate at which progression to invasive cancer can occur, either with or without treatment? Second, what is the fate of these DCIS lesions? These are issues for which we currently don’t have good answers.
We’re treating all disease detected at an early stage, and for the sake of argument, I’ll include DCIS, as if it likely will cause harm if we did absolutely nothing when, in fact, there could be many cancers that progress so slowly and have such a low propensity for developing metastatic disease that they would not likely cause any symptoms or harm during a patient’s lifetime.
In autopsy series, the disease reservoir of unrecognized DCIS is about 9% and the disease reservoir of invasive cancer is about 1%. It’s not that different from prostate cancer, although at a much lower rate. These data show that there certainly are women who die with DCIS rather than of it.
We really don’t have a very solid understanding of the natural history of DCIS. If we do nothing, but maybe surgically biopsy it, what happens to these patients in the long term? In a meta-analysis, the world’s literature included only 151 cases of women who had surgical biopsy of DCIS that initially was misdiagnosed as a benign lesion and therefore didn’t undergo any further therapy, some with up to 31 years of follow-up. The long-term risk of invasive cancer in this cohort is only 22% (Breast Cancer Res. Treat. 2006;97:135-44). The annual risk of breast cancer in women with atypia is 1% per year, so this ends up looking very similar to the risk of progression that you see for atypical ductal hyperplasia or lobular carcinoma in situ.
The most common treatment for DCIS in the United States is lumpectomy with radiation. A meta-analysis by the European Breast Cancer Trialists’ Group found a 50% proportional reduction in local recurrence risk in women treated with lumpectomy and radiation vs. lumpectomy alone. The absolute magnitude of reduction was dependent on baseline recurrence risk. That’s a really important concept, because if your baseline risk is only 5%, then the 50% proportional reduction only translates into a 2.5% reduction in risk in 10 years.
The prospective, randomized Radiation Therapy Oncologists Group 9804 study randomized low-risk women with DCIS, unlike prior randomized trials that included broad eligibility criteria for DCIS. In 5 years of follow-up, the ipsilateral recurrence risk (which includes both invasive cancer and DCIS) was 3.2% in the lumpectomy-only group vs. 0.4% in the lumpectomy and radiation therapy group. The difference is highly statistically significant, however, given the small absolute difference between groups, the clinical significance certainly can be argued. There was no significant difference between groups in contralateral new primary lesions (Radiat. Oncol. 2012;84:S5).
We just presented a study this year looking at DCIS and competing causes of mortality in different age groups with different types of treatment. Among women with DCIS over 70 years of age, there was a significant difference in overall survival but none of the treatments conferred any benefit in disease-specific survival.
Active surveillance alone may be reasonable to consider in some patients. We can learn a lot from our colleagues who treat prostate cancer. They’re at least 10 years ahead of us in thinking about reducing the harms that have been introduced by screening for prostate cancer. When you look at breast cancer–specific and other-cause mortality in the setting of DCIS, the mortality curves look very similar to those with early-stage prostate cancer. Women with DCIS, regardless of what they are treated with, die of other causes and very rarely die of breast cancer.
When we compare such different options as mastectomy to active surveillance only, it’s really hard for a patient to feel that both of those approaches can offer them the same outcomes. But when you look at the actual data and evidence, the differences in recurrence or progression to invasive cancer don’t translate easily into a large difference in breast cancer mortality provided that patients are diagnosed at stage I or II, with more than a 90% survival from breast cancer.
We have an opportunity to take a big step back and redefine our goals of DCIS “treatment” from “curing” DCIS to trying to reduce breast cancer-specific mortality. This will help us reduce the harms that can result from screening and will reserve our aggressive treatments for those most likely to benefit from them.
Dr. Hwang is a professor of surgery at Duke University, Durham, N.C. She serves as a consultant for Genomic Health.
Remarks given during a session of the ASCO Breast Cancer Symposium titled Ductal Carcinoma in Situ Debate: Treatment vs. Observation
Dr. Kuerer comments: There has been a marked increase ductal carcinoma in situ (DCIS) in what is being called overdiagnosis, and this is leading to concerns of overtreatment, which has been in the news now for several years. We have more than 60,000 cases of DCIS diagnosed per year in the United States. We’re trying to prevent invasive breast cancer and distant metastases. The problem is identifying which patients will go on to develop invasive disease. That’s really unknown.
At M.D. Anderson, looking at 10-year follow-up of 2,449 patients, the rate of developing distant metastases was 0.1%. The problem with this is that no prominent variables were associated with the development of invasive metastatic disease. Overall, we are doing a good job at preventing death from breast cancer when we treat DCIS, with less than 1% of patients dying of breast cancer (Ann. Surg. Onc. 2011;18:2873-8).
Dr. Shelley E. Hwang and her group very elegantly started exploring preoperative systemic therapy as a way to get a clue about which patients might be safely observed alone (that is, a core biopsy diagnosis of DCIS and then just follow-up without surgery or other treatments). At M.D. Anderson, we studied whether or not we could eradicate DCIS in patients with human epidermal growth factor receptor 2 (HER2) overexpression by treatment with trastuzumab prior to surgery, under the hypothesis that if we could eradicate the DCIS, we might eventually use this drug potentially to prevent HER2-positive invasive breast cancers. We saw very dramatic responses in their immune response with antibody-dependent cellular cytotoxicity mediated by natural killer cells, which is exciting, but there were no histopathologic changes. The most important finding was that 42% of our patients who we thought only had DCIS actually had occult invasive breast cancer (Cancer 2011;117:39-47). This is concerning because without surgery, we may be missing or leaving untreated invasive breast cancers in some patients.
So, we have an underestimation of invasive breast cancer at DCIS diagnosis. A very elegant meta-analysis of 7,350 patients reported that even if we take patients with non–high-grade, very-small DCIS, we’re still looking at an upgrade to invasive cancer of about 20% (Radiology 2011;260:119-28). The best and most recent studies of MRI and DCIS again found a diagnostic upgrade of about 27%. There were no MRI features correlating with invasive breast cancer, and this resulted in a 31% increase in procedures and more biopsies with the use of MRI.
So where are we? In active surveillance of 14 patients with DCIS at the University of California, San Francisco, 8 went on to surgery at a median follow-up of 28 months, and 5 of the 8 (62%) had invasive breast cancer (The Breast 2011;20:529-33).
What’s the cost to the health care system of surveillance if we biopsy only the DCIS and follow it without surgery or other adjuvant therapies? The psychological cost to our patients? What is the natural history of DCIS if left in place? What will be the result of microcalcifications? How are we going to follow this? What are the criteria that we will use for repeat biopsy? This really is not known.
Which are the patients that we’re going to select for observation alone? There are trials in Europe that have begun or will begin to address the safety of just observing DCIS without surgery and other therapies.
The United Kingdom Low-Risk DCIS Trial is randomizing patients with low and intermediate grade DCIS of any size to biopsy alone without surgical intervention (active monitoring) or standard therapy. Another trial, a joint Dutch Breast Cancer Research Group and European Organization for the Research and Treatment of Cancer trial is randomizing women with low-risk, low-grade DCIS to active surveillance or standard treatment. If we look at M.D. Anderson’s data and our National Cancer Database, only about 10%-15% of patients would be eligible for the latter study. I don’t think with these numbers we’d have a great impact, but it is a start.
I submit that the best U.S. patients to study will be patients with a diagnosis of atypical ductal hyperplasia (generally the smallest lesions and perhaps the earliest form of DCIS) because we have about 100,000 cases each year.
What’s the patient’s perspective? What about the need for continued repeat biopsies, and how this will affect their overall quality of life? Do patients in the United States really want to observe the DCIS in an era when our patients are requesting more and more mastectomy with reconstruction and contralateral mastectomy at diagnosis of DCIS? I seriously doubt that our patients in the United States would agree to be randomized in DCIS trials to no treatment at all. I really don’t know.
Dr. Kuerer is a professor of surgery at the University of Texas M.D. Anderson Cancer Center, Houston. He reported financial associations with Gerson Lehrman Group and McGraw-Hill Publishing.
Dr. Hwang comments: Today, about 1/1,300 screening mammograms result in a diagnosis of DCIS. There are two important considerations when we talk about active surveillance or doing less aggressive treatment. First, what is the rate at which progression to invasive cancer can occur, either with or without treatment? Second, what is the fate of these DCIS lesions? These are issues for which we currently don’t have good answers.
We’re treating all disease detected at an early stage, and for the sake of argument, I’ll include DCIS, as if it likely will cause harm if we did absolutely nothing when, in fact, there could be many cancers that progress so slowly and have such a low propensity for developing metastatic disease that they would not likely cause any symptoms or harm during a patient’s lifetime.
In autopsy series, the disease reservoir of unrecognized DCIS is about 9% and the disease reservoir of invasive cancer is about 1%. It’s not that different from prostate cancer, although at a much lower rate. These data show that there certainly are women who die with DCIS rather than of it.
We really don’t have a very solid understanding of the natural history of DCIS. If we do nothing, but maybe surgically biopsy it, what happens to these patients in the long term? In a meta-analysis, the world’s literature included only 151 cases of women who had surgical biopsy of DCIS that initially was misdiagnosed as a benign lesion and therefore didn’t undergo any further therapy, some with up to 31 years of follow-up. The long-term risk of invasive cancer in this cohort is only 22% (Breast Cancer Res. Treat. 2006;97:135-44). The annual risk of breast cancer in women with atypia is 1% per year, so this ends up looking very similar to the risk of progression that you see for atypical ductal hyperplasia or lobular carcinoma in situ.
The most common treatment for DCIS in the United States is lumpectomy with radiation. A meta-analysis by the European Breast Cancer Trialists’ Group found a 50% proportional reduction in local recurrence risk in women treated with lumpectomy and radiation vs. lumpectomy alone. The absolute magnitude of reduction was dependent on baseline recurrence risk. That’s a really important concept, because if your baseline risk is only 5%, then the 50% proportional reduction only translates into a 2.5% reduction in risk in 10 years.
The prospective, randomized Radiation Therapy Oncologists Group 9804 study randomized low-risk women with DCIS, unlike prior randomized trials that included broad eligibility criteria for DCIS. In 5 years of follow-up, the ipsilateral recurrence risk (which includes both invasive cancer and DCIS) was 3.2% in the lumpectomy-only group vs. 0.4% in the lumpectomy and radiation therapy group. The difference is highly statistically significant, however, given the small absolute difference between groups, the clinical significance certainly can be argued. There was no significant difference between groups in contralateral new primary lesions (Radiat. Oncol. 2012;84:S5).
We just presented a study this year looking at DCIS and competing causes of mortality in different age groups with different types of treatment. Among women with DCIS over 70 years of age, there was a significant difference in overall survival but none of the treatments conferred any benefit in disease-specific survival.
Active surveillance alone may be reasonable to consider in some patients. We can learn a lot from our colleagues who treat prostate cancer. They’re at least 10 years ahead of us in thinking about reducing the harms that have been introduced by screening for prostate cancer. When you look at breast cancer–specific and other-cause mortality in the setting of DCIS, the mortality curves look very similar to those with early-stage prostate cancer. Women with DCIS, regardless of what they are treated with, die of other causes and very rarely die of breast cancer.
When we compare such different options as mastectomy to active surveillance only, it’s really hard for a patient to feel that both of those approaches can offer them the same outcomes. But when you look at the actual data and evidence, the differences in recurrence or progression to invasive cancer don’t translate easily into a large difference in breast cancer mortality provided that patients are diagnosed at stage I or II, with more than a 90% survival from breast cancer.
We have an opportunity to take a big step back and redefine our goals of DCIS “treatment” from “curing” DCIS to trying to reduce breast cancer-specific mortality. This will help us reduce the harms that can result from screening and will reserve our aggressive treatments for those most likely to benefit from them.
Dr. Hwang is a professor of surgery at Duke University, Durham, N.C. She serves as a consultant for Genomic Health.
Remarks given during a session of the ASCO Breast Cancer Symposium titled Ductal Carcinoma in Situ Debate: Treatment vs. Observation
Dr. Kuerer comments: There has been a marked increase ductal carcinoma in situ (DCIS) in what is being called overdiagnosis, and this is leading to concerns of overtreatment, which has been in the news now for several years. We have more than 60,000 cases of DCIS diagnosed per year in the United States. We’re trying to prevent invasive breast cancer and distant metastases. The problem is identifying which patients will go on to develop invasive disease. That’s really unknown.
At M.D. Anderson, looking at 10-year follow-up of 2,449 patients, the rate of developing distant metastases was 0.1%. The problem with this is that no prominent variables were associated with the development of invasive metastatic disease. Overall, we are doing a good job at preventing death from breast cancer when we treat DCIS, with less than 1% of patients dying of breast cancer (Ann. Surg. Onc. 2011;18:2873-8).
Dr. Shelley E. Hwang and her group very elegantly started exploring preoperative systemic therapy as a way to get a clue about which patients might be safely observed alone (that is, a core biopsy diagnosis of DCIS and then just follow-up without surgery or other treatments). At M.D. Anderson, we studied whether or not we could eradicate DCIS in patients with human epidermal growth factor receptor 2 (HER2) overexpression by treatment with trastuzumab prior to surgery, under the hypothesis that if we could eradicate the DCIS, we might eventually use this drug potentially to prevent HER2-positive invasive breast cancers. We saw very dramatic responses in their immune response with antibody-dependent cellular cytotoxicity mediated by natural killer cells, which is exciting, but there were no histopathologic changes. The most important finding was that 42% of our patients who we thought only had DCIS actually had occult invasive breast cancer (Cancer 2011;117:39-47). This is concerning because without surgery, we may be missing or leaving untreated invasive breast cancers in some patients.
So, we have an underestimation of invasive breast cancer at DCIS diagnosis. A very elegant meta-analysis of 7,350 patients reported that even if we take patients with non–high-grade, very-small DCIS, we’re still looking at an upgrade to invasive cancer of about 20% (Radiology 2011;260:119-28). The best and most recent studies of MRI and DCIS again found a diagnostic upgrade of about 27%. There were no MRI features correlating with invasive breast cancer, and this resulted in a 31% increase in procedures and more biopsies with the use of MRI.
So where are we? In active surveillance of 14 patients with DCIS at the University of California, San Francisco, 8 went on to surgery at a median follow-up of 28 months, and 5 of the 8 (62%) had invasive breast cancer (The Breast 2011;20:529-33).
What’s the cost to the health care system of surveillance if we biopsy only the DCIS and follow it without surgery or other adjuvant therapies? The psychological cost to our patients? What is the natural history of DCIS if left in place? What will be the result of microcalcifications? How are we going to follow this? What are the criteria that we will use for repeat biopsy? This really is not known.
Which are the patients that we’re going to select for observation alone? There are trials in Europe that have begun or will begin to address the safety of just observing DCIS without surgery and other therapies.
The United Kingdom Low-Risk DCIS Trial is randomizing patients with low and intermediate grade DCIS of any size to biopsy alone without surgical intervention (active monitoring) or standard therapy. Another trial, a joint Dutch Breast Cancer Research Group and European Organization for the Research and Treatment of Cancer trial is randomizing women with low-risk, low-grade DCIS to active surveillance or standard treatment. If we look at M.D. Anderson’s data and our National Cancer Database, only about 10%-15% of patients would be eligible for the latter study. I don’t think with these numbers we’d have a great impact, but it is a start.
I submit that the best U.S. patients to study will be patients with a diagnosis of atypical ductal hyperplasia (generally the smallest lesions and perhaps the earliest form of DCIS) because we have about 100,000 cases each year.
What’s the patient’s perspective? What about the need for continued repeat biopsies, and how this will affect their overall quality of life? Do patients in the United States really want to observe the DCIS in an era when our patients are requesting more and more mastectomy with reconstruction and contralateral mastectomy at diagnosis of DCIS? I seriously doubt that our patients in the United States would agree to be randomized in DCIS trials to no treatment at all. I really don’t know.
Dr. Kuerer is a professor of surgery at the University of Texas M.D. Anderson Cancer Center, Houston. He reported financial associations with Gerson Lehrman Group and McGraw-Hill Publishing.
Dr. Hwang comments: Today, about 1/1,300 screening mammograms result in a diagnosis of DCIS. There are two important considerations when we talk about active surveillance or doing less aggressive treatment. First, what is the rate at which progression to invasive cancer can occur, either with or without treatment? Second, what is the fate of these DCIS lesions? These are issues for which we currently don’t have good answers.
We’re treating all disease detected at an early stage, and for the sake of argument, I’ll include DCIS, as if it likely will cause harm if we did absolutely nothing when, in fact, there could be many cancers that progress so slowly and have such a low propensity for developing metastatic disease that they would not likely cause any symptoms or harm during a patient’s lifetime.
In autopsy series, the disease reservoir of unrecognized DCIS is about 9% and the disease reservoir of invasive cancer is about 1%. It’s not that different from prostate cancer, although at a much lower rate. These data show that there certainly are women who die with DCIS rather than of it.
We really don’t have a very solid understanding of the natural history of DCIS. If we do nothing, but maybe surgically biopsy it, what happens to these patients in the long term? In a meta-analysis, the world’s literature included only 151 cases of women who had surgical biopsy of DCIS that initially was misdiagnosed as a benign lesion and therefore didn’t undergo any further therapy, some with up to 31 years of follow-up. The long-term risk of invasive cancer in this cohort is only 22% (Breast Cancer Res. Treat. 2006;97:135-44). The annual risk of breast cancer in women with atypia is 1% per year, so this ends up looking very similar to the risk of progression that you see for atypical ductal hyperplasia or lobular carcinoma in situ.
The most common treatment for DCIS in the United States is lumpectomy with radiation. A meta-analysis by the European Breast Cancer Trialists’ Group found a 50% proportional reduction in local recurrence risk in women treated with lumpectomy and radiation vs. lumpectomy alone. The absolute magnitude of reduction was dependent on baseline recurrence risk. That’s a really important concept, because if your baseline risk is only 5%, then the 50% proportional reduction only translates into a 2.5% reduction in risk in 10 years.
The prospective, randomized Radiation Therapy Oncologists Group 9804 study randomized low-risk women with DCIS, unlike prior randomized trials that included broad eligibility criteria for DCIS. In 5 years of follow-up, the ipsilateral recurrence risk (which includes both invasive cancer and DCIS) was 3.2% in the lumpectomy-only group vs. 0.4% in the lumpectomy and radiation therapy group. The difference is highly statistically significant, however, given the small absolute difference between groups, the clinical significance certainly can be argued. There was no significant difference between groups in contralateral new primary lesions (Radiat. Oncol. 2012;84:S5).
We just presented a study this year looking at DCIS and competing causes of mortality in different age groups with different types of treatment. Among women with DCIS over 70 years of age, there was a significant difference in overall survival but none of the treatments conferred any benefit in disease-specific survival.
Active surveillance alone may be reasonable to consider in some patients. We can learn a lot from our colleagues who treat prostate cancer. They’re at least 10 years ahead of us in thinking about reducing the harms that have been introduced by screening for prostate cancer. When you look at breast cancer–specific and other-cause mortality in the setting of DCIS, the mortality curves look very similar to those with early-stage prostate cancer. Women with DCIS, regardless of what they are treated with, die of other causes and very rarely die of breast cancer.
When we compare such different options as mastectomy to active surveillance only, it’s really hard for a patient to feel that both of those approaches can offer them the same outcomes. But when you look at the actual data and evidence, the differences in recurrence or progression to invasive cancer don’t translate easily into a large difference in breast cancer mortality provided that patients are diagnosed at stage I or II, with more than a 90% survival from breast cancer.
We have an opportunity to take a big step back and redefine our goals of DCIS “treatment” from “curing” DCIS to trying to reduce breast cancer-specific mortality. This will help us reduce the harms that can result from screening and will reserve our aggressive treatments for those most likely to benefit from them.
Dr. Hwang is a professor of surgery at Duke University, Durham, N.C. She serves as a consultant for Genomic Health.
VIDEO: Waiting for long-term data on pCR could be disservice to some breast cancer patients, expert says
SAN FRANCISCO – Only a fraction of patients with breast cancer who are eligible for neoadjuvant therapy are getting it, partly because of confusion around the significance of achieving a pathologic complete response, Dr. William M. Sikov said in an interview at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Dr. Sikov of Brown University, Providence, R.I., explained why it’s been difficult for researchers to show improved outcomes even after a pathologic complete response (pCR) is obtained, but argued that waiting for long-term outcomes data for neoadjuvant therapy could be a disservice to some patients with breast cancer.
Breast cancer surgeons at his own institution have become converts in favor of neoadjuvant therapy, and Dr. Sikov explained why in this video report.
He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Only a fraction of patients with breast cancer who are eligible for neoadjuvant therapy are getting it, partly because of confusion around the significance of achieving a pathologic complete response, Dr. William M. Sikov said in an interview at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Dr. Sikov of Brown University, Providence, R.I., explained why it’s been difficult for researchers to show improved outcomes even after a pathologic complete response (pCR) is obtained, but argued that waiting for long-term outcomes data for neoadjuvant therapy could be a disservice to some patients with breast cancer.
Breast cancer surgeons at his own institution have become converts in favor of neoadjuvant therapy, and Dr. Sikov explained why in this video report.
He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Only a fraction of patients with breast cancer who are eligible for neoadjuvant therapy are getting it, partly because of confusion around the significance of achieving a pathologic complete response, Dr. William M. Sikov said in an interview at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Dr. Sikov of Brown University, Providence, R.I., explained why it’s been difficult for researchers to show improved outcomes even after a pathologic complete response (pCR) is obtained, but argued that waiting for long-term outcomes data for neoadjuvant therapy could be a disservice to some patients with breast cancer.
Breast cancer surgeons at his own institution have become converts in favor of neoadjuvant therapy, and Dr. Sikov explained why in this video report.
He reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM
VIDEO: Unclear if altering lifestyle affects breast cancer
SAN FRANCISCO – Physicians have multiple good reasons to suggest lifestyle changes to many patients with breast cancer, but affecting the cancer itself may not be one of them, Dr. Pamela J. Goodwin said at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
In this video interview, Dr. Goodwin summarizes the ongoing research on how changes in lifestyle such as weight loss, diet, physical activity, and drinking may or may not alter outcomes in patients with breast cancer.
The good news: A drink or two a day probably doesn’t hurt, said Dr. Goodwin, professor of medicine at the University of Toronto’s Mount Sinai Hospital.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Physicians have multiple good reasons to suggest lifestyle changes to many patients with breast cancer, but affecting the cancer itself may not be one of them, Dr. Pamela J. Goodwin said at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
In this video interview, Dr. Goodwin summarizes the ongoing research on how changes in lifestyle such as weight loss, diet, physical activity, and drinking may or may not alter outcomes in patients with breast cancer.
The good news: A drink or two a day probably doesn’t hurt, said Dr. Goodwin, professor of medicine at the University of Toronto’s Mount Sinai Hospital.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Physicians have multiple good reasons to suggest lifestyle changes to many patients with breast cancer, but affecting the cancer itself may not be one of them, Dr. Pamela J. Goodwin said at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
In this video interview, Dr. Goodwin summarizes the ongoing research on how changes in lifestyle such as weight loss, diet, physical activity, and drinking may or may not alter outcomes in patients with breast cancer.
The good news: A drink or two a day probably doesn’t hurt, said Dr. Goodwin, professor of medicine at the University of Toronto’s Mount Sinai Hospital.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE 2014 ASCO BREAST CANCER SYMPOSIUM
VIDEO: Breast cancer symposium take-home messages, Day 1
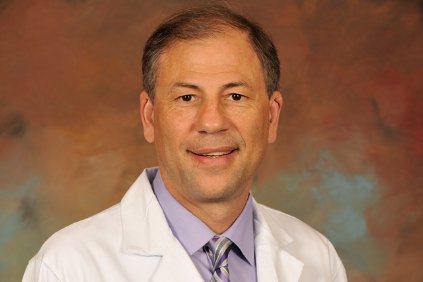
SAN FRANCISCO – Dr. Eleftherios (Terry) Mamounas reviews the first day of the annual breast cancer symposium sponsored by the American Society of Clinical Oncology.
Key sessions covered the increasingly complex topic of genetic risk assessment and stirred up the debate about management of ductal carcinoma in situ (DCIS). Dr. Mamounas, professor of surgery at the University of Central Florida and medical director of the comprehensive breast program at the University of Florida Health Cancer Center, both in Orlando, discusses the significance of atypical hyperplasia, including new data suggesting that the fourfold increased risk of developing breast cancer in women with ductal carcinoma in situ (DCIS) is not further worsened by having a family history of DCIS.
Among the top oral presentations, one study suggested that a nomogram helped predict the risk of locoregional recurrence in patients treated for breast cancer using accelerated partial-breast irradiation. Another study examined the effect of hormone receptor status and local treatment on overall survival for patients with early-stage breast cancer.
Dr. Mamounas also discusses his own study, which he presented at the meeting, showing lower rates of locoregional recurrence in patients who have a pathologic complete response to neoadjuvant therapy. He puts the findings in context with tips on how to incorporate pathologic complete response data into clinical practice.
A separate study reported some of the first data on complication rates after unilateral or bilateral mastectomy and reconstruction. Dr. Mamounas wraps up the day’s review by discussing sessions on the effect of luteinizing hormone-releasing hormone agonists during chemotherapy in preserving ovarian function, and on breast cancer prevention, including the use of aromatase inhibitors.
For more of the meeting’s highlights, see our video interviews with Dr. Hope S. Rugo discussing the events of the second and third days of the Breast Cancer Symposium. Dr. Rugo is director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center.
Dr. Mamounas reported financial associations with Genomic Health, Genentech/Roche, Pfizer, GlaxoSmithKline, Eisai, Celgene, and GE Healthcare.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Dr. Eleftherios (Terry) Mamounas reviews the first day of the annual breast cancer symposium sponsored by the American Society of Clinical Oncology.
Key sessions covered the increasingly complex topic of genetic risk assessment and stirred up the debate about management of ductal carcinoma in situ (DCIS). Dr. Mamounas, professor of surgery at the University of Central Florida and medical director of the comprehensive breast program at the University of Florida Health Cancer Center, both in Orlando, discusses the significance of atypical hyperplasia, including new data suggesting that the fourfold increased risk of developing breast cancer in women with ductal carcinoma in situ (DCIS) is not further worsened by having a family history of DCIS.
Among the top oral presentations, one study suggested that a nomogram helped predict the risk of locoregional recurrence in patients treated for breast cancer using accelerated partial-breast irradiation. Another study examined the effect of hormone receptor status and local treatment on overall survival for patients with early-stage breast cancer.
Dr. Mamounas also discusses his own study, which he presented at the meeting, showing lower rates of locoregional recurrence in patients who have a pathologic complete response to neoadjuvant therapy. He puts the findings in context with tips on how to incorporate pathologic complete response data into clinical practice.
A separate study reported some of the first data on complication rates after unilateral or bilateral mastectomy and reconstruction. Dr. Mamounas wraps up the day’s review by discussing sessions on the effect of luteinizing hormone-releasing hormone agonists during chemotherapy in preserving ovarian function, and on breast cancer prevention, including the use of aromatase inhibitors.
For more of the meeting’s highlights, see our video interviews with Dr. Hope S. Rugo discussing the events of the second and third days of the Breast Cancer Symposium. Dr. Rugo is director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center.
Dr. Mamounas reported financial associations with Genomic Health, Genentech/Roche, Pfizer, GlaxoSmithKline, Eisai, Celgene, and GE Healthcare.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Dr. Eleftherios (Terry) Mamounas reviews the first day of the annual breast cancer symposium sponsored by the American Society of Clinical Oncology.
Key sessions covered the increasingly complex topic of genetic risk assessment and stirred up the debate about management of ductal carcinoma in situ (DCIS). Dr. Mamounas, professor of surgery at the University of Central Florida and medical director of the comprehensive breast program at the University of Florida Health Cancer Center, both in Orlando, discusses the significance of atypical hyperplasia, including new data suggesting that the fourfold increased risk of developing breast cancer in women with ductal carcinoma in situ (DCIS) is not further worsened by having a family history of DCIS.
Among the top oral presentations, one study suggested that a nomogram helped predict the risk of locoregional recurrence in patients treated for breast cancer using accelerated partial-breast irradiation. Another study examined the effect of hormone receptor status and local treatment on overall survival for patients with early-stage breast cancer.
Dr. Mamounas also discusses his own study, which he presented at the meeting, showing lower rates of locoregional recurrence in patients who have a pathologic complete response to neoadjuvant therapy. He puts the findings in context with tips on how to incorporate pathologic complete response data into clinical practice.
A separate study reported some of the first data on complication rates after unilateral or bilateral mastectomy and reconstruction. Dr. Mamounas wraps up the day’s review by discussing sessions on the effect of luteinizing hormone-releasing hormone agonists during chemotherapy in preserving ovarian function, and on breast cancer prevention, including the use of aromatase inhibitors.
For more of the meeting’s highlights, see our video interviews with Dr. Hope S. Rugo discussing the events of the second and third days of the Breast Cancer Symposium. Dr. Rugo is director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center.
Dr. Mamounas reported financial associations with Genomic Health, Genentech/Roche, Pfizer, GlaxoSmithKline, Eisai, Celgene, and GE Healthcare.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM
VIDEO: Dr. Hope S. Rugo on breast cancer symposium hot topics, Day 2
SAN FRANCISCO – Dr. Hope S. Rugo reviews the highlights of Day 2 at the breast cancer symposium sponsored by the American Society of Clinical Oncology, including presentations on new directions in neoadjuvant therapy. Data on pathologic complete response, immune modulation, and postneoadjuvant therapy are modifying oncology, with potential for significant changes in the near future. "I think that we’re seeing a whole new era of drugs in the postneoadjuvant setting," says Dr. Rugo, director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco.
She describes a lively discussion in one session about when to apply data on neoadjuvant therapy to clinical practice.
A "great series of discussions" about managing survivors of breast cancer included a look at when advice on lifestyle modifications goes overboard, she says. For example, survivors do not need to avoid alcohol entirely. "It’s okay for a breast cancer survivor to have a couple of glasses of wine. It’s not the end of the world by any means," Dr. Rugo says.
Clinicians also can go overboard on surveillance after breast cancer treatment, according to Dr. Rugo, and she gives examples from a session debating intensive vs. nonintensive surveillance.
She finishes her recap of the day’s highlights with thoughts on breast reconstruction.
Dr. Rugo disclosed financial associations with Genomic Health, Plexxikon, Merck, and Novartis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Dr. Hope S. Rugo reviews the highlights of Day 2 at the breast cancer symposium sponsored by the American Society of Clinical Oncology, including presentations on new directions in neoadjuvant therapy. Data on pathologic complete response, immune modulation, and postneoadjuvant therapy are modifying oncology, with potential for significant changes in the near future. "I think that we’re seeing a whole new era of drugs in the postneoadjuvant setting," says Dr. Rugo, director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco.
She describes a lively discussion in one session about when to apply data on neoadjuvant therapy to clinical practice.
A "great series of discussions" about managing survivors of breast cancer included a look at when advice on lifestyle modifications goes overboard, she says. For example, survivors do not need to avoid alcohol entirely. "It’s okay for a breast cancer survivor to have a couple of glasses of wine. It’s not the end of the world by any means," Dr. Rugo says.
Clinicians also can go overboard on surveillance after breast cancer treatment, according to Dr. Rugo, and she gives examples from a session debating intensive vs. nonintensive surveillance.
She finishes her recap of the day’s highlights with thoughts on breast reconstruction.
Dr. Rugo disclosed financial associations with Genomic Health, Plexxikon, Merck, and Novartis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Dr. Hope S. Rugo reviews the highlights of Day 2 at the breast cancer symposium sponsored by the American Society of Clinical Oncology, including presentations on new directions in neoadjuvant therapy. Data on pathologic complete response, immune modulation, and postneoadjuvant therapy are modifying oncology, with potential for significant changes in the near future. "I think that we’re seeing a whole new era of drugs in the postneoadjuvant setting," says Dr. Rugo, director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco.
She describes a lively discussion in one session about when to apply data on neoadjuvant therapy to clinical practice.
A "great series of discussions" about managing survivors of breast cancer included a look at when advice on lifestyle modifications goes overboard, she says. For example, survivors do not need to avoid alcohol entirely. "It’s okay for a breast cancer survivor to have a couple of glasses of wine. It’s not the end of the world by any means," Dr. Rugo says.
Clinicians also can go overboard on surveillance after breast cancer treatment, according to Dr. Rugo, and she gives examples from a session debating intensive vs. nonintensive surveillance.
She finishes her recap of the day’s highlights with thoughts on breast reconstruction.
Dr. Rugo disclosed financial associations with Genomic Health, Plexxikon, Merck, and Novartis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM
VIDEO: Complications increase with bilateral mastectomy and reconstruction
SAN FRANCISCO – Women undergoing mastectomy and breast reconstruction for the treatment of breast cancer are more likely to develop perioperative complications if they opt for prophylactic mastectomy of the other breast at the same time, a study of 18,229 cases found.
Compared with women who had a unilateral mastectomy and reconstruction, the 36% of patients who chose bilateral mastectomy and reconstruction were 55% more likely to lose a breast implant (if implants were used for reconstruction), twice as likely to need a transfusion regardless of whether the reconstruction used implants or autologous material, and twice as likely to remain hospitalized for at least 2 days regardless of reconstruction method, Dr. Amanda K. Silva and her associates reported in a poster presentation at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
The reconstruction used implants in 89% of women undergoing bilateral mastectomy and 79% of those getting unilateral mastectomy, Dr. Silva and her colleagues reported.
The overall rate of complications was low, however, averaging 5%, said Dr. Silva, a surgeon at the University of Chicago, and her associates.
In this video interview, Dr. Silva discusses factors that physicians and patients should consider when choosing unilateral or bilateral mastectomy and reconstruction.
Previous studies have compared the risks of unilateral versus bilateral mastectomy without reconstruction, she said, and this study provides some of the first data of risks from either type of mastectomy with reconstruction.
Dr. Silva reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Women undergoing mastectomy and breast reconstruction for the treatment of breast cancer are more likely to develop perioperative complications if they opt for prophylactic mastectomy of the other breast at the same time, a study of 18,229 cases found.
Compared with women who had a unilateral mastectomy and reconstruction, the 36% of patients who chose bilateral mastectomy and reconstruction were 55% more likely to lose a breast implant (if implants were used for reconstruction), twice as likely to need a transfusion regardless of whether the reconstruction used implants or autologous material, and twice as likely to remain hospitalized for at least 2 days regardless of reconstruction method, Dr. Amanda K. Silva and her associates reported in a poster presentation at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
The reconstruction used implants in 89% of women undergoing bilateral mastectomy and 79% of those getting unilateral mastectomy, Dr. Silva and her colleagues reported.
The overall rate of complications was low, however, averaging 5%, said Dr. Silva, a surgeon at the University of Chicago, and her associates.
In this video interview, Dr. Silva discusses factors that physicians and patients should consider when choosing unilateral or bilateral mastectomy and reconstruction.
Previous studies have compared the risks of unilateral versus bilateral mastectomy without reconstruction, she said, and this study provides some of the first data of risks from either type of mastectomy with reconstruction.
Dr. Silva reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Women undergoing mastectomy and breast reconstruction for the treatment of breast cancer are more likely to develop perioperative complications if they opt for prophylactic mastectomy of the other breast at the same time, a study of 18,229 cases found.
Compared with women who had a unilateral mastectomy and reconstruction, the 36% of patients who chose bilateral mastectomy and reconstruction were 55% more likely to lose a breast implant (if implants were used for reconstruction), twice as likely to need a transfusion regardless of whether the reconstruction used implants or autologous material, and twice as likely to remain hospitalized for at least 2 days regardless of reconstruction method, Dr. Amanda K. Silva and her associates reported in a poster presentation at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
The reconstruction used implants in 89% of women undergoing bilateral mastectomy and 79% of those getting unilateral mastectomy, Dr. Silva and her colleagues reported.
The overall rate of complications was low, however, averaging 5%, said Dr. Silva, a surgeon at the University of Chicago, and her associates.
In this video interview, Dr. Silva discusses factors that physicians and patients should consider when choosing unilateral or bilateral mastectomy and reconstruction.
Previous studies have compared the risks of unilateral versus bilateral mastectomy without reconstruction, she said, and this study provides some of the first data of risks from either type of mastectomy with reconstruction.
Dr. Silva reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM
Locoregional recurrence of breast cancer less likely after neoadjuvant complete response
Patients with residual disease after neoadjuvant chemotherapy and surgery for breast cancer had a 60%-280% increased risk for locoregional recurrence, compared with patients with a pathologic complete response, an analysis of data from 12 large clinical trials found.
Investigators analyzed data on 11,955 patients with stage I-III breast cancer who underwent neoadjuvant chemotherapy in studies with long-term follow-up and information on complete pathologic response (no residual cancer in the breast and no cancer in the axillary lymph nodes after surgery). They included 5,252 patients in a multivariate analysis of predictors of locoregional recurrence a median of 5 years after treatment.
Overall, the likelihood of locoregional recurrence was low – less than 10%. Locoregional recurrence was seen in 5.5% of patients with a complete pathologic response to neoadjuvant chemotherapy and in 7.1% of patients without a complete response, a significant 60% increase in risk without a complete response, Dr. Eleftherios Mamounas reported in a press briefing held in advance of the breast cancer symposium sponsored by the American Society of Clinical Oncology.
Patients with residual cancer in the breast after surgery had a 60% higher risk for locoregional recurrence, and patients with residual cancer in the axillary lymph nodes had a 280% increased risk for locoregional recurrence, compared with patients who had a complete pathologic response, reported Dr. Mamounas, professor of surgery at the University of Central Florida, and medical director of the comprehensive breast program at the University of Florida Health Cancer Center, both in Orlando.
Breast cancer subtypes remained independent predictors of locoregional recurrence, regardless of whether patients had a pathologic complete response or not. The cancer recurred locally or regionally in 4% of patients with hormone receptor–positive, human epidermal growth factor receptor 2–negative (HR+/HER2–) grade 1 or 2 cancer, 9% of patients with HR+/HER2– grade 3 cancer, 15% of patients with HR–/HER2+ cancer, 10% of patients with HR+/HER2+ cancer, and 12% of patients with HR–/HER2– cancer (also known as hormone receptor–negative or triple-negative breast cancer).
Those rates would be different today because of more effective treatments for HER2+ breast cancer, he noted.
"For all breast cancer subtypes except for HR+/HER2– grade 1 and 2, there was a progressive increase in the locoregional recurrence rates with decreasing rates of pathologic complete response," he said. In other words, recurrence rates went from highest to lowest in patients "having positive nodes, versus having residual disease in the breast with negative nodes, versus having complete pathologic response," he explained.
Among patients with triple-negative cancer, for example, locoregional recurrence rates went from 6.2% in those with a complete response to 11.9% in patients with residual cancer in the breast but not lymph nodes and 22.1% in those who had positive nodes after treatment.
A pathologic complete response predicted lower locoregional recurrence rates with the various cancer subtypes, regardless of whether the patient underwent lumpectomy or mastectomy, he said.
Based on these results and previously published studies, "we have a lot of evidence that pathologic complete response is predictive of outcome, both in terms of systemic recurrence and also in terms of local recurrence," Dr. Mamounas commented. A previous meta-analysis that reported conflicting results for systemic recurrence "did not quite confirm that an incremental increase in pathologic complete response will improve overall survival, but there are a lot of technical issues if you look at the different studies that were included in the meta-analysis. The bar was very high to prove that concept."
Recurrence is less likely after a pathologic complete response in patients with HER2+ breast cancer, triple-negative cancer, or highly proliferative estrogen receptor–positive breast cancer, he said. That may not be the case for patients with estrogen receptor–positive, HER2– grade 1 disease, who do very well regardless, he added.
"Our findings have clinical implications relative to further tailoring the use of adjuvant radiation therapy after neoadjuvant chemotherapy and support the conduct of ongoing clinical trials attempting to tailor locoregional therapy in this setting," Dr. Mamounas said.
Dr. Mamounas reported financial associations with Genomic Health, GE Healthcare, Celgene, Pfizer, Eisai, and Genentech/Roche. Some of his coinvestigators reported associations with multiple companies.
On Twitter @sherryboschert
This is a group of women who have higher-than-average risk, such that they are being offered up-front chemotherapy to shrink cancers even before they would go for breast surgery.
We’ve known for a long time that this clinical endpoint of complete pathologic response – that is, when you do the breast surgery, there is no evidence of residual cancer – is a powerful predictor of the cancer not recurring somewhere else in the body. These data from Dr. Mamounas show that complete pathologic response also is a predictor for not having the cancer recur within the chest wall or the breast itself. That’s very important information for the clinical team.

|
|
Dr. Mamounas’s data also point to the idea that the breast cancer subtype is very important for predicting the outcomes. In the modern era, so much of what we are thinking about in the way of managing breast cancer is driven by our understanding of these major clinical subtypes, the so-called HER2-positive breast cancers, the so-called triple-negative breast cancers (which lack estrogen receptor, progesterone receptor, and HER2), and finally the spectrum of so-called estrogen receptor–positive, HER2-negative (sometimes called luminal) cancers.
What Dr. Mamounas’s data speak to is a very complicated matrix that helps us understand the risk of local recurrence in a woman who has a greater-than-average risk of breast cancer by factoring in the type of breast cancer, the response that you see with the up-front chemotherapy, and the age of the patient. These multiplex kinds of information set the stage for a variety of trials that are looking at trying to tailor additional therapy for women who are at higher risk and, conversely, sparing women who are at lower risk the need for extra treatment – in this case, possibly the need for radiation therapy.
These are data that really resonate with radiation oncologists, surgeons, and medical oncologists, who are into the nitty-gritty of caring for women with breast cancer and need to determine who is going to need more therapy and who can be spared additional treatment.
Dr. Harold J. Burstein is associate professor of medicine at Harvard Medical School and the Dana-Farber Cancer Institute, both in Boston. He reported having no relevant financial disclosures.
This is a group of women who have higher-than-average risk, such that they are being offered up-front chemotherapy to shrink cancers even before they would go for breast surgery.
We’ve known for a long time that this clinical endpoint of complete pathologic response – that is, when you do the breast surgery, there is no evidence of residual cancer – is a powerful predictor of the cancer not recurring somewhere else in the body. These data from Dr. Mamounas show that complete pathologic response also is a predictor for not having the cancer recur within the chest wall or the breast itself. That’s very important information for the clinical team.

|
|
Dr. Mamounas’s data also point to the idea that the breast cancer subtype is very important for predicting the outcomes. In the modern era, so much of what we are thinking about in the way of managing breast cancer is driven by our understanding of these major clinical subtypes, the so-called HER2-positive breast cancers, the so-called triple-negative breast cancers (which lack estrogen receptor, progesterone receptor, and HER2), and finally the spectrum of so-called estrogen receptor–positive, HER2-negative (sometimes called luminal) cancers.
What Dr. Mamounas’s data speak to is a very complicated matrix that helps us understand the risk of local recurrence in a woman who has a greater-than-average risk of breast cancer by factoring in the type of breast cancer, the response that you see with the up-front chemotherapy, and the age of the patient. These multiplex kinds of information set the stage for a variety of trials that are looking at trying to tailor additional therapy for women who are at higher risk and, conversely, sparing women who are at lower risk the need for extra treatment – in this case, possibly the need for radiation therapy.
These are data that really resonate with radiation oncologists, surgeons, and medical oncologists, who are into the nitty-gritty of caring for women with breast cancer and need to determine who is going to need more therapy and who can be spared additional treatment.
Dr. Harold J. Burstein is associate professor of medicine at Harvard Medical School and the Dana-Farber Cancer Institute, both in Boston. He reported having no relevant financial disclosures.
This is a group of women who have higher-than-average risk, such that they are being offered up-front chemotherapy to shrink cancers even before they would go for breast surgery.
We’ve known for a long time that this clinical endpoint of complete pathologic response – that is, when you do the breast surgery, there is no evidence of residual cancer – is a powerful predictor of the cancer not recurring somewhere else in the body. These data from Dr. Mamounas show that complete pathologic response also is a predictor for not having the cancer recur within the chest wall or the breast itself. That’s very important information for the clinical team.

|
|
Dr. Mamounas’s data also point to the idea that the breast cancer subtype is very important for predicting the outcomes. In the modern era, so much of what we are thinking about in the way of managing breast cancer is driven by our understanding of these major clinical subtypes, the so-called HER2-positive breast cancers, the so-called triple-negative breast cancers (which lack estrogen receptor, progesterone receptor, and HER2), and finally the spectrum of so-called estrogen receptor–positive, HER2-negative (sometimes called luminal) cancers.
What Dr. Mamounas’s data speak to is a very complicated matrix that helps us understand the risk of local recurrence in a woman who has a greater-than-average risk of breast cancer by factoring in the type of breast cancer, the response that you see with the up-front chemotherapy, and the age of the patient. These multiplex kinds of information set the stage for a variety of trials that are looking at trying to tailor additional therapy for women who are at higher risk and, conversely, sparing women who are at lower risk the need for extra treatment – in this case, possibly the need for radiation therapy.
These are data that really resonate with radiation oncologists, surgeons, and medical oncologists, who are into the nitty-gritty of caring for women with breast cancer and need to determine who is going to need more therapy and who can be spared additional treatment.
Dr. Harold J. Burstein is associate professor of medicine at Harvard Medical School and the Dana-Farber Cancer Institute, both in Boston. He reported having no relevant financial disclosures.
Patients with residual disease after neoadjuvant chemotherapy and surgery for breast cancer had a 60%-280% increased risk for locoregional recurrence, compared with patients with a pathologic complete response, an analysis of data from 12 large clinical trials found.
Investigators analyzed data on 11,955 patients with stage I-III breast cancer who underwent neoadjuvant chemotherapy in studies with long-term follow-up and information on complete pathologic response (no residual cancer in the breast and no cancer in the axillary lymph nodes after surgery). They included 5,252 patients in a multivariate analysis of predictors of locoregional recurrence a median of 5 years after treatment.
Overall, the likelihood of locoregional recurrence was low – less than 10%. Locoregional recurrence was seen in 5.5% of patients with a complete pathologic response to neoadjuvant chemotherapy and in 7.1% of patients without a complete response, a significant 60% increase in risk without a complete response, Dr. Eleftherios Mamounas reported in a press briefing held in advance of the breast cancer symposium sponsored by the American Society of Clinical Oncology.
Patients with residual cancer in the breast after surgery had a 60% higher risk for locoregional recurrence, and patients with residual cancer in the axillary lymph nodes had a 280% increased risk for locoregional recurrence, compared with patients who had a complete pathologic response, reported Dr. Mamounas, professor of surgery at the University of Central Florida, and medical director of the comprehensive breast program at the University of Florida Health Cancer Center, both in Orlando.
Breast cancer subtypes remained independent predictors of locoregional recurrence, regardless of whether patients had a pathologic complete response or not. The cancer recurred locally or regionally in 4% of patients with hormone receptor–positive, human epidermal growth factor receptor 2–negative (HR+/HER2–) grade 1 or 2 cancer, 9% of patients with HR+/HER2– grade 3 cancer, 15% of patients with HR–/HER2+ cancer, 10% of patients with HR+/HER2+ cancer, and 12% of patients with HR–/HER2– cancer (also known as hormone receptor–negative or triple-negative breast cancer).
Those rates would be different today because of more effective treatments for HER2+ breast cancer, he noted.
"For all breast cancer subtypes except for HR+/HER2– grade 1 and 2, there was a progressive increase in the locoregional recurrence rates with decreasing rates of pathologic complete response," he said. In other words, recurrence rates went from highest to lowest in patients "having positive nodes, versus having residual disease in the breast with negative nodes, versus having complete pathologic response," he explained.
Among patients with triple-negative cancer, for example, locoregional recurrence rates went from 6.2% in those with a complete response to 11.9% in patients with residual cancer in the breast but not lymph nodes and 22.1% in those who had positive nodes after treatment.
A pathologic complete response predicted lower locoregional recurrence rates with the various cancer subtypes, regardless of whether the patient underwent lumpectomy or mastectomy, he said.
Based on these results and previously published studies, "we have a lot of evidence that pathologic complete response is predictive of outcome, both in terms of systemic recurrence and also in terms of local recurrence," Dr. Mamounas commented. A previous meta-analysis that reported conflicting results for systemic recurrence "did not quite confirm that an incremental increase in pathologic complete response will improve overall survival, but there are a lot of technical issues if you look at the different studies that were included in the meta-analysis. The bar was very high to prove that concept."
Recurrence is less likely after a pathologic complete response in patients with HER2+ breast cancer, triple-negative cancer, or highly proliferative estrogen receptor–positive breast cancer, he said. That may not be the case for patients with estrogen receptor–positive, HER2– grade 1 disease, who do very well regardless, he added.
"Our findings have clinical implications relative to further tailoring the use of adjuvant radiation therapy after neoadjuvant chemotherapy and support the conduct of ongoing clinical trials attempting to tailor locoregional therapy in this setting," Dr. Mamounas said.
Dr. Mamounas reported financial associations with Genomic Health, GE Healthcare, Celgene, Pfizer, Eisai, and Genentech/Roche. Some of his coinvestigators reported associations with multiple companies.
On Twitter @sherryboschert
Patients with residual disease after neoadjuvant chemotherapy and surgery for breast cancer had a 60%-280% increased risk for locoregional recurrence, compared with patients with a pathologic complete response, an analysis of data from 12 large clinical trials found.
Investigators analyzed data on 11,955 patients with stage I-III breast cancer who underwent neoadjuvant chemotherapy in studies with long-term follow-up and information on complete pathologic response (no residual cancer in the breast and no cancer in the axillary lymph nodes after surgery). They included 5,252 patients in a multivariate analysis of predictors of locoregional recurrence a median of 5 years after treatment.
Overall, the likelihood of locoregional recurrence was low – less than 10%. Locoregional recurrence was seen in 5.5% of patients with a complete pathologic response to neoadjuvant chemotherapy and in 7.1% of patients without a complete response, a significant 60% increase in risk without a complete response, Dr. Eleftherios Mamounas reported in a press briefing held in advance of the breast cancer symposium sponsored by the American Society of Clinical Oncology.
Patients with residual cancer in the breast after surgery had a 60% higher risk for locoregional recurrence, and patients with residual cancer in the axillary lymph nodes had a 280% increased risk for locoregional recurrence, compared with patients who had a complete pathologic response, reported Dr. Mamounas, professor of surgery at the University of Central Florida, and medical director of the comprehensive breast program at the University of Florida Health Cancer Center, both in Orlando.
Breast cancer subtypes remained independent predictors of locoregional recurrence, regardless of whether patients had a pathologic complete response or not. The cancer recurred locally or regionally in 4% of patients with hormone receptor–positive, human epidermal growth factor receptor 2–negative (HR+/HER2–) grade 1 or 2 cancer, 9% of patients with HR+/HER2– grade 3 cancer, 15% of patients with HR–/HER2+ cancer, 10% of patients with HR+/HER2+ cancer, and 12% of patients with HR–/HER2– cancer (also known as hormone receptor–negative or triple-negative breast cancer).
Those rates would be different today because of more effective treatments for HER2+ breast cancer, he noted.
"For all breast cancer subtypes except for HR+/HER2– grade 1 and 2, there was a progressive increase in the locoregional recurrence rates with decreasing rates of pathologic complete response," he said. In other words, recurrence rates went from highest to lowest in patients "having positive nodes, versus having residual disease in the breast with negative nodes, versus having complete pathologic response," he explained.
Among patients with triple-negative cancer, for example, locoregional recurrence rates went from 6.2% in those with a complete response to 11.9% in patients with residual cancer in the breast but not lymph nodes and 22.1% in those who had positive nodes after treatment.
A pathologic complete response predicted lower locoregional recurrence rates with the various cancer subtypes, regardless of whether the patient underwent lumpectomy or mastectomy, he said.
Based on these results and previously published studies, "we have a lot of evidence that pathologic complete response is predictive of outcome, both in terms of systemic recurrence and also in terms of local recurrence," Dr. Mamounas commented. A previous meta-analysis that reported conflicting results for systemic recurrence "did not quite confirm that an incremental increase in pathologic complete response will improve overall survival, but there are a lot of technical issues if you look at the different studies that were included in the meta-analysis. The bar was very high to prove that concept."
Recurrence is less likely after a pathologic complete response in patients with HER2+ breast cancer, triple-negative cancer, or highly proliferative estrogen receptor–positive breast cancer, he said. That may not be the case for patients with estrogen receptor–positive, HER2– grade 1 disease, who do very well regardless, he added.
"Our findings have clinical implications relative to further tailoring the use of adjuvant radiation therapy after neoadjuvant chemotherapy and support the conduct of ongoing clinical trials attempting to tailor locoregional therapy in this setting," Dr. Mamounas said.
Dr. Mamounas reported financial associations with Genomic Health, GE Healthcare, Celgene, Pfizer, Eisai, and Genentech/Roche. Some of his coinvestigators reported associations with multiple companies.
On Twitter @sherryboschert
FROM THE ASCO BREAST CANCER SYMPOSIUM
Key clinical point: Response to neoadjuvant chemotherapy for breast cancer predicts the locoregional recurrence risk.
Major finding: Risk for locoregional recurrence was 60%-280% higher in patients without a pathologic complete response.
Data source: A pooled analysis of data on 11,955 patients who got neoadjuvant therapy and surgery for stage I-III breast cancer.
Disclosures: Dr. Mamounas reported financial associations with Genomic Health, GE Healthcare, Celgene, Pfizer, Eisai, and Genentech/Roche. Some of his coinvestigators reported associations with multiple companies.