User login
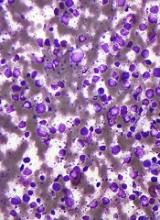
Inhibitor exhibits activity against hematologic malignancies
A dual kinase inhibitor is active against a range of hematologic malignancies, according to preclinical research.
Investigators found that ASN002, a SYK/JAK inhibitor, exhibited “potent” antiproliferative activity in leukemia, lymphoma, and myeloma cell lines.
ASN002 also inhibited tumor growth in mouse models of these malignancies and proved active against ibrutinib-resistant diffuse large B-cell lymphoma (DLBCL).
The investigators presented these results at the AACR Annual Meeting 2017 (abstract 4204).
The work was conducted by employees of Asana BioSciences, the company developing ASN002.
The investigators tested ASN002 in 178 cell lines and found the drug exhibited “strong antiproliferative activity” in a range of hematologic cancer cell lines, including:
- Leukemia—HEL31, HL60, Jurkat, MOLM-13, and MOLM-16
- Lymphoma—KARPAS-299, OCI-LY10, OCI-LY-19, Pfeiffer, Raji, Ramos, SU-DHL-1, SU-DHL-6, and SU-DHL-10
- Myeloma—H929, JJN3, OPM2, and U266.
In addition, ASN002 was active against ibrutinib-resistant clones derived from the DLBCL cell line SU-DHL-6.
In a SU-DHL-6 xenograft model, the combination of ASN002 and ibrutinib was more effective than either compound alone.
The investigators also found that ASN002 alone demonstrated “strong tumor growth inhibition” in mouse models of DLBCL (Pfeiffer and SU-DHL-6), myeloma (H929), and erythroleukemia (HEL).
The team pointed out that ASN002 is currently under investigation in a phase 1/2 study of patients with B-cell lymphomas (DLBCL, mantle cell lymphoma, and follicular lymphoma) as well as solid tumors.
The investigators said that, to date, ASN002 has been well tolerated and has shown encouraging early evidence of clinical activity and symptomatic benefit in the lymphoma patients. ![]()
A dual kinase inhibitor is active against a range of hematologic malignancies, according to preclinical research.
Investigators found that ASN002, a SYK/JAK inhibitor, exhibited “potent” antiproliferative activity in leukemia, lymphoma, and myeloma cell lines.
ASN002 also inhibited tumor growth in mouse models of these malignancies and proved active against ibrutinib-resistant diffuse large B-cell lymphoma (DLBCL).
The investigators presented these results at the AACR Annual Meeting 2017 (abstract 4204).
The work was conducted by employees of Asana BioSciences, the company developing ASN002.
The investigators tested ASN002 in 178 cell lines and found the drug exhibited “strong antiproliferative activity” in a range of hematologic cancer cell lines, including:
- Leukemia—HEL31, HL60, Jurkat, MOLM-13, and MOLM-16
- Lymphoma—KARPAS-299, OCI-LY10, OCI-LY-19, Pfeiffer, Raji, Ramos, SU-DHL-1, SU-DHL-6, and SU-DHL-10
- Myeloma—H929, JJN3, OPM2, and U266.
In addition, ASN002 was active against ibrutinib-resistant clones derived from the DLBCL cell line SU-DHL-6.
In a SU-DHL-6 xenograft model, the combination of ASN002 and ibrutinib was more effective than either compound alone.
The investigators also found that ASN002 alone demonstrated “strong tumor growth inhibition” in mouse models of DLBCL (Pfeiffer and SU-DHL-6), myeloma (H929), and erythroleukemia (HEL).
The team pointed out that ASN002 is currently under investigation in a phase 1/2 study of patients with B-cell lymphomas (DLBCL, mantle cell lymphoma, and follicular lymphoma) as well as solid tumors.
The investigators said that, to date, ASN002 has been well tolerated and has shown encouraging early evidence of clinical activity and symptomatic benefit in the lymphoma patients. ![]()
A dual kinase inhibitor is active against a range of hematologic malignancies, according to preclinical research.
Investigators found that ASN002, a SYK/JAK inhibitor, exhibited “potent” antiproliferative activity in leukemia, lymphoma, and myeloma cell lines.
ASN002 also inhibited tumor growth in mouse models of these malignancies and proved active against ibrutinib-resistant diffuse large B-cell lymphoma (DLBCL).
The investigators presented these results at the AACR Annual Meeting 2017 (abstract 4204).
The work was conducted by employees of Asana BioSciences, the company developing ASN002.
The investigators tested ASN002 in 178 cell lines and found the drug exhibited “strong antiproliferative activity” in a range of hematologic cancer cell lines, including:
- Leukemia—HEL31, HL60, Jurkat, MOLM-13, and MOLM-16
- Lymphoma—KARPAS-299, OCI-LY10, OCI-LY-19, Pfeiffer, Raji, Ramos, SU-DHL-1, SU-DHL-6, and SU-DHL-10
- Myeloma—H929, JJN3, OPM2, and U266.
In addition, ASN002 was active against ibrutinib-resistant clones derived from the DLBCL cell line SU-DHL-6.
In a SU-DHL-6 xenograft model, the combination of ASN002 and ibrutinib was more effective than either compound alone.
The investigators also found that ASN002 alone demonstrated “strong tumor growth inhibition” in mouse models of DLBCL (Pfeiffer and SU-DHL-6), myeloma (H929), and erythroleukemia (HEL).
The team pointed out that ASN002 is currently under investigation in a phase 1/2 study of patients with B-cell lymphomas (DLBCL, mantle cell lymphoma, and follicular lymphoma) as well as solid tumors.
The investigators said that, to date, ASN002 has been well tolerated and has shown encouraging early evidence of clinical activity and symptomatic benefit in the lymphoma patients. ![]()
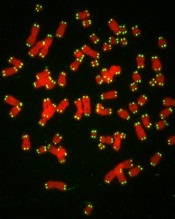
TKI shows promise in preclinical study of AML
WASHINGTON, DC—Preclinical data suggest a novel tyrosine kinase inhibitor (TKI) may be an effective treatment for patients with NTRK-rearranged acute myeloid leukemia (AML).
Entrectinib is a TKI targeting tumors that harbor TRK, ROS1, or ALK fusions.
Researchers found that entrectinib inhibited cell proliferation in NTRK-rearranged AML cell lines.
In mouse models of NTRK-rearranged AML, entrectinib induced tumor regression and eliminated residual AML cells from the bone marrow.
These results were presented at the AACR Annual Meeting 2017 (abstract 5158). The research was conducted by employees of Ignyta, Inc., the company developing entrectinib.
The researchers first tested entrectinib in AML cell lines. They observed “potent” anti-proliferative activity in a pair of NTRK-fusion-positive AML cell lines, IMS-M2 and M0-91.
Entrectinib inhibited TRK signaling and induced cell-cycle arrest in these cell lines. The TKI also induced both caspase 3-dependent apoptosis and PARP cleavage in a dose- and time-dependent manner.
However, entrectinib showed minimal activity against an NTRK-fusion-negative AML cell line, Kasumi-1.
The researchers also tested entrectinib in mouse models of NTRK-fusion-driven AML.
The TKI induced tumor regression in both IMS-M2 and M0-91 models, and the drug eliminated leukemic cells in the bone marrow.
The researchers said these results provide rationale for the clinical development of entrectinib in molecularly defined hematologic malignancies.
Entrectinib is currently being studied in a phase 2 trial of solid tumor malignancies. ![]()
WASHINGTON, DC—Preclinical data suggest a novel tyrosine kinase inhibitor (TKI) may be an effective treatment for patients with NTRK-rearranged acute myeloid leukemia (AML).
Entrectinib is a TKI targeting tumors that harbor TRK, ROS1, or ALK fusions.
Researchers found that entrectinib inhibited cell proliferation in NTRK-rearranged AML cell lines.
In mouse models of NTRK-rearranged AML, entrectinib induced tumor regression and eliminated residual AML cells from the bone marrow.
These results were presented at the AACR Annual Meeting 2017 (abstract 5158). The research was conducted by employees of Ignyta, Inc., the company developing entrectinib.
The researchers first tested entrectinib in AML cell lines. They observed “potent” anti-proliferative activity in a pair of NTRK-fusion-positive AML cell lines, IMS-M2 and M0-91.
Entrectinib inhibited TRK signaling and induced cell-cycle arrest in these cell lines. The TKI also induced both caspase 3-dependent apoptosis and PARP cleavage in a dose- and time-dependent manner.
However, entrectinib showed minimal activity against an NTRK-fusion-negative AML cell line, Kasumi-1.
The researchers also tested entrectinib in mouse models of NTRK-fusion-driven AML.
The TKI induced tumor regression in both IMS-M2 and M0-91 models, and the drug eliminated leukemic cells in the bone marrow.
The researchers said these results provide rationale for the clinical development of entrectinib in molecularly defined hematologic malignancies.
Entrectinib is currently being studied in a phase 2 trial of solid tumor malignancies. ![]()
WASHINGTON, DC—Preclinical data suggest a novel tyrosine kinase inhibitor (TKI) may be an effective treatment for patients with NTRK-rearranged acute myeloid leukemia (AML).
Entrectinib is a TKI targeting tumors that harbor TRK, ROS1, or ALK fusions.
Researchers found that entrectinib inhibited cell proliferation in NTRK-rearranged AML cell lines.
In mouse models of NTRK-rearranged AML, entrectinib induced tumor regression and eliminated residual AML cells from the bone marrow.
These results were presented at the AACR Annual Meeting 2017 (abstract 5158). The research was conducted by employees of Ignyta, Inc., the company developing entrectinib.
The researchers first tested entrectinib in AML cell lines. They observed “potent” anti-proliferative activity in a pair of NTRK-fusion-positive AML cell lines, IMS-M2 and M0-91.
Entrectinib inhibited TRK signaling and induced cell-cycle arrest in these cell lines. The TKI also induced both caspase 3-dependent apoptosis and PARP cleavage in a dose- and time-dependent manner.
However, entrectinib showed minimal activity against an NTRK-fusion-negative AML cell line, Kasumi-1.
The researchers also tested entrectinib in mouse models of NTRK-fusion-driven AML.
The TKI induced tumor regression in both IMS-M2 and M0-91 models, and the drug eliminated leukemic cells in the bone marrow.
The researchers said these results provide rationale for the clinical development of entrectinib in molecularly defined hematologic malignancies.
Entrectinib is currently being studied in a phase 2 trial of solid tumor malignancies. ![]()
CAR T-cell therapy demonstrates efficacy in mice with MM
WASHINGTON, DC—A chimeric antigen receptor (CAR) T-cell therapy is active against multiple myeloma (MM), according to preclinical research.
The therapy, known as P-BCMA-101, demonstrated persistent anti-tumor activity in a mouse model of MM.
Treatment with P-BCMA-101 eliminated tumors after relapse and prolonged survival in the mice, when compared to other CAR-T cell therapies.
These results were presented in a poster at the AACR Annual Meeting 2017 (abstract 3759).
The research was conducted by employees of Poseida Therapeutics Inc., the company developing P-BCMA-101, as well as others.
About P-BCMA-101
The researchers explained that P-BCMA-101 employs a B-cell maturation antigen (BCMA)-specific Centyrin™ rather than a single-chain variable fragment (scFv) for antigen detection.
Centyrins™ are fully human and have similar binding affinities as scFvs. However, Centyrins are smaller, more thermostable, and predicted to be less immunogenic.
P-BCMA-101 is engineered using the PiggyBac™ DNA modification system. PiggyBac eliminates the need to use lentivirus or gamma-retrovirus as a gene delivery mechanism, resulting in improved manufacturing and cost savings.
In addition, the increased cargo capacity of PiggyBac allows for the incorporation of a safety switch and a selectable gene. The safety switch can be “flipped” to enable depletion in case adverse events occur. And the selectable gene allows for enrichment of CARTyrin+ cells using a non-genotoxic drug.
Findings
The researchers found that more than 70% of P-BCMA-101 cells possessed a stem cell memory phenotype, creating a significant population of self-renewing, multipotent progenitors capable of reconstituting the entire spectrum of memory and effector T-cell subsets required to prevent cancer relapse. Similar competitor products typically report 0% to 20% stem cell memory phenotype.
In addition, P-BCMA-101 was enriched with more than 95% of T cells successfully modified, which compares favorably to the roughly 30% to 50% commonly expected with clinical manufacture using lentivirus.
P-BCMA-101 did not exhibit effects of CAR-mediated tonic signaling, a common cause of T-cell exhaustion that leads to poor durability. Tonic signaling is caused by oligomerization of unstable binding domains commonly seen with traditional scFv CARs.
The researchers tested P-BCMA-101 in NSG mice bearing luciferase+ MM.1S cells. The mice received a single administration of either 4 x 106 or 12 x 106 P-BCMA-101 cells.
P-BCMA-101 treatment reduced tumor burden to the limit of detection within 7 days. Conversely, all untreated control mice succumbed to MM within 4 weeks.
P-BCMA-101 expanded and persisted in the treated mice, eliminated tumors following relapse, and prolonged survival.
Most treated mice survived 110 days, and none of them died from tumor burden during the study. This compares favorably to lentivirus-based products that have shown roughly 50-day survival in the same model.
Based on these results, Poseida plans to initiate a phase 1 trial of P-BCMA-101 in patients with relapsed or refractory MM. ![]()
WASHINGTON, DC—A chimeric antigen receptor (CAR) T-cell therapy is active against multiple myeloma (MM), according to preclinical research.
The therapy, known as P-BCMA-101, demonstrated persistent anti-tumor activity in a mouse model of MM.
Treatment with P-BCMA-101 eliminated tumors after relapse and prolonged survival in the mice, when compared to other CAR-T cell therapies.
These results were presented in a poster at the AACR Annual Meeting 2017 (abstract 3759).
The research was conducted by employees of Poseida Therapeutics Inc., the company developing P-BCMA-101, as well as others.
About P-BCMA-101
The researchers explained that P-BCMA-101 employs a B-cell maturation antigen (BCMA)-specific Centyrin™ rather than a single-chain variable fragment (scFv) for antigen detection.
Centyrins™ are fully human and have similar binding affinities as scFvs. However, Centyrins are smaller, more thermostable, and predicted to be less immunogenic.
P-BCMA-101 is engineered using the PiggyBac™ DNA modification system. PiggyBac eliminates the need to use lentivirus or gamma-retrovirus as a gene delivery mechanism, resulting in improved manufacturing and cost savings.
In addition, the increased cargo capacity of PiggyBac allows for the incorporation of a safety switch and a selectable gene. The safety switch can be “flipped” to enable depletion in case adverse events occur. And the selectable gene allows for enrichment of CARTyrin+ cells using a non-genotoxic drug.
Findings
The researchers found that more than 70% of P-BCMA-101 cells possessed a stem cell memory phenotype, creating a significant population of self-renewing, multipotent progenitors capable of reconstituting the entire spectrum of memory and effector T-cell subsets required to prevent cancer relapse. Similar competitor products typically report 0% to 20% stem cell memory phenotype.
In addition, P-BCMA-101 was enriched with more than 95% of T cells successfully modified, which compares favorably to the roughly 30% to 50% commonly expected with clinical manufacture using lentivirus.
P-BCMA-101 did not exhibit effects of CAR-mediated tonic signaling, a common cause of T-cell exhaustion that leads to poor durability. Tonic signaling is caused by oligomerization of unstable binding domains commonly seen with traditional scFv CARs.
The researchers tested P-BCMA-101 in NSG mice bearing luciferase+ MM.1S cells. The mice received a single administration of either 4 x 106 or 12 x 106 P-BCMA-101 cells.
P-BCMA-101 treatment reduced tumor burden to the limit of detection within 7 days. Conversely, all untreated control mice succumbed to MM within 4 weeks.
P-BCMA-101 expanded and persisted in the treated mice, eliminated tumors following relapse, and prolonged survival.
Most treated mice survived 110 days, and none of them died from tumor burden during the study. This compares favorably to lentivirus-based products that have shown roughly 50-day survival in the same model.
Based on these results, Poseida plans to initiate a phase 1 trial of P-BCMA-101 in patients with relapsed or refractory MM. ![]()
WASHINGTON, DC—A chimeric antigen receptor (CAR) T-cell therapy is active against multiple myeloma (MM), according to preclinical research.
The therapy, known as P-BCMA-101, demonstrated persistent anti-tumor activity in a mouse model of MM.
Treatment with P-BCMA-101 eliminated tumors after relapse and prolonged survival in the mice, when compared to other CAR-T cell therapies.
These results were presented in a poster at the AACR Annual Meeting 2017 (abstract 3759).
The research was conducted by employees of Poseida Therapeutics Inc., the company developing P-BCMA-101, as well as others.
About P-BCMA-101
The researchers explained that P-BCMA-101 employs a B-cell maturation antigen (BCMA)-specific Centyrin™ rather than a single-chain variable fragment (scFv) for antigen detection.
Centyrins™ are fully human and have similar binding affinities as scFvs. However, Centyrins are smaller, more thermostable, and predicted to be less immunogenic.
P-BCMA-101 is engineered using the PiggyBac™ DNA modification system. PiggyBac eliminates the need to use lentivirus or gamma-retrovirus as a gene delivery mechanism, resulting in improved manufacturing and cost savings.
In addition, the increased cargo capacity of PiggyBac allows for the incorporation of a safety switch and a selectable gene. The safety switch can be “flipped” to enable depletion in case adverse events occur. And the selectable gene allows for enrichment of CARTyrin+ cells using a non-genotoxic drug.
Findings
The researchers found that more than 70% of P-BCMA-101 cells possessed a stem cell memory phenotype, creating a significant population of self-renewing, multipotent progenitors capable of reconstituting the entire spectrum of memory and effector T-cell subsets required to prevent cancer relapse. Similar competitor products typically report 0% to 20% stem cell memory phenotype.
In addition, P-BCMA-101 was enriched with more than 95% of T cells successfully modified, which compares favorably to the roughly 30% to 50% commonly expected with clinical manufacture using lentivirus.
P-BCMA-101 did not exhibit effects of CAR-mediated tonic signaling, a common cause of T-cell exhaustion that leads to poor durability. Tonic signaling is caused by oligomerization of unstable binding domains commonly seen with traditional scFv CARs.
The researchers tested P-BCMA-101 in NSG mice bearing luciferase+ MM.1S cells. The mice received a single administration of either 4 x 106 or 12 x 106 P-BCMA-101 cells.
P-BCMA-101 treatment reduced tumor burden to the limit of detection within 7 days. Conversely, all untreated control mice succumbed to MM within 4 weeks.
P-BCMA-101 expanded and persisted in the treated mice, eliminated tumors following relapse, and prolonged survival.
Most treated mice survived 110 days, and none of them died from tumor burden during the study. This compares favorably to lentivirus-based products that have shown roughly 50-day survival in the same model.
Based on these results, Poseida plans to initiate a phase 1 trial of P-BCMA-101 in patients with relapsed or refractory MM. ![]()
Cancer risk, burden expected to shift in HIV population
WASHINGTON, DC—New research suggests HIV-positive adults in the US will see a shift in cancer risk and burden in the coming years.
The study indicates that, through 2030, people living with HIV will see a decrease in AIDS-defining cancers, such as non-Hodgkin lymphoma (NHL) and Kaposi sarcoma.
But this group will also see an increase in cancers not linked to AIDS, such as prostate and liver cancers.
Researchers made these projections in a presentation at the AACR Annual Meeting 2017 (abstract 5302).
“Declines in cancer incidence rates, particularly for AIDS-defining cancers, are likely driven by widespread treatment with modern antiretroviral therapies, which reduce immune suppression and decrease risk of some cancers,” said Jessica Y. Islam, a doctoral student at the University of North Carolina Gillings School of Global Public Health in Chapel Hill.
She and her collaborators estimated future cancer risk and burden for HIV-positive people using age-specific cancer incidence data from the National Cancer Institute HIV/AIDS Cancer Match (HACM) Study, and projected HIV prevalence data from the Centers for Disease Control and Prevention.
Cancer incidence
From 2000 to 2012, there were 23,907 cancers reported in 463,300 HIV-infected adults in the HACM Study. Based on trends in this study, the researchers made projections for cancer incidence through 2030.
They projected that HIV-positive adults of all ages will see a significant decrease over time in the incidence of NHL, Kaposi sarcoma, cervical cancer, anal cancer among men who have sex with men (MSM), lung cancer, and Hodgkin lymphoma.
Patients age 65 and older will see a significant decrease in colon cancer incidence over time. However, there will be no significant change for patients younger than 65.
HIV-positive adults of all ages will see no significant change over time in the incidence of liver cancer, oral cavity cancer, anal cancer among non-MSMs, and breast cancer.
The incidence of prostate cancer will increase significantly among patients ages 35 to 44 and among patients ages 45 to 64.
Cancer burden
The researchers said the number of adults living with HIV in the US is projected to increase from 1.06 million in 2006 to 1.17 million in 2018, but it is expected to decline to 1.09 million in 2030.
The team noted that, in 2006, there were an estimated 8241 cancers in patients with HIV—3522 AIDS-defining cancers and 4719 malignancies not associated with AIDS.
In 2030, the total number of cancers in the HIV-positive population is projected to be 6692, with decreases in AIDS-defining cancers (n=716) and increases in other cancers (n=5976) from the 2006 data.
In 2010, the most common cancers among HIV-positive patients were estimated to be NHL (n=1488), Kaposi sarcoma (n=1133), and lung cancer (n=815).
But in 2030, the most common cancers are projected to be prostate (n=1587), lung (n=1027), and liver cancers (n=483).
“It is critical to understand both incidence rates and burden over time, as rates capture changes in cancer risk, and burden quantifies the actual number of cancer cases expected to occur,” said study investigator Meredith S. Shiels, PhD, of the National Cancer Institute in Bethesda, Maryland.
“For example, lung cancer rates are expected to decrease in the future, but the burden is expected to increase due to the growing number of older people living with HIV.” ![]()
WASHINGTON, DC—New research suggests HIV-positive adults in the US will see a shift in cancer risk and burden in the coming years.
The study indicates that, through 2030, people living with HIV will see a decrease in AIDS-defining cancers, such as non-Hodgkin lymphoma (NHL) and Kaposi sarcoma.
But this group will also see an increase in cancers not linked to AIDS, such as prostate and liver cancers.
Researchers made these projections in a presentation at the AACR Annual Meeting 2017 (abstract 5302).
“Declines in cancer incidence rates, particularly for AIDS-defining cancers, are likely driven by widespread treatment with modern antiretroviral therapies, which reduce immune suppression and decrease risk of some cancers,” said Jessica Y. Islam, a doctoral student at the University of North Carolina Gillings School of Global Public Health in Chapel Hill.
She and her collaborators estimated future cancer risk and burden for HIV-positive people using age-specific cancer incidence data from the National Cancer Institute HIV/AIDS Cancer Match (HACM) Study, and projected HIV prevalence data from the Centers for Disease Control and Prevention.
Cancer incidence
From 2000 to 2012, there were 23,907 cancers reported in 463,300 HIV-infected adults in the HACM Study. Based on trends in this study, the researchers made projections for cancer incidence through 2030.
They projected that HIV-positive adults of all ages will see a significant decrease over time in the incidence of NHL, Kaposi sarcoma, cervical cancer, anal cancer among men who have sex with men (MSM), lung cancer, and Hodgkin lymphoma.
Patients age 65 and older will see a significant decrease in colon cancer incidence over time. However, there will be no significant change for patients younger than 65.
HIV-positive adults of all ages will see no significant change over time in the incidence of liver cancer, oral cavity cancer, anal cancer among non-MSMs, and breast cancer.
The incidence of prostate cancer will increase significantly among patients ages 35 to 44 and among patients ages 45 to 64.
Cancer burden
The researchers said the number of adults living with HIV in the US is projected to increase from 1.06 million in 2006 to 1.17 million in 2018, but it is expected to decline to 1.09 million in 2030.
The team noted that, in 2006, there were an estimated 8241 cancers in patients with HIV—3522 AIDS-defining cancers and 4719 malignancies not associated with AIDS.
In 2030, the total number of cancers in the HIV-positive population is projected to be 6692, with decreases in AIDS-defining cancers (n=716) and increases in other cancers (n=5976) from the 2006 data.
In 2010, the most common cancers among HIV-positive patients were estimated to be NHL (n=1488), Kaposi sarcoma (n=1133), and lung cancer (n=815).
But in 2030, the most common cancers are projected to be prostate (n=1587), lung (n=1027), and liver cancers (n=483).
“It is critical to understand both incidence rates and burden over time, as rates capture changes in cancer risk, and burden quantifies the actual number of cancer cases expected to occur,” said study investigator Meredith S. Shiels, PhD, of the National Cancer Institute in Bethesda, Maryland.
“For example, lung cancer rates are expected to decrease in the future, but the burden is expected to increase due to the growing number of older people living with HIV.” ![]()
WASHINGTON, DC—New research suggests HIV-positive adults in the US will see a shift in cancer risk and burden in the coming years.
The study indicates that, through 2030, people living with HIV will see a decrease in AIDS-defining cancers, such as non-Hodgkin lymphoma (NHL) and Kaposi sarcoma.
But this group will also see an increase in cancers not linked to AIDS, such as prostate and liver cancers.
Researchers made these projections in a presentation at the AACR Annual Meeting 2017 (abstract 5302).
“Declines in cancer incidence rates, particularly for AIDS-defining cancers, are likely driven by widespread treatment with modern antiretroviral therapies, which reduce immune suppression and decrease risk of some cancers,” said Jessica Y. Islam, a doctoral student at the University of North Carolina Gillings School of Global Public Health in Chapel Hill.
She and her collaborators estimated future cancer risk and burden for HIV-positive people using age-specific cancer incidence data from the National Cancer Institute HIV/AIDS Cancer Match (HACM) Study, and projected HIV prevalence data from the Centers for Disease Control and Prevention.
Cancer incidence
From 2000 to 2012, there were 23,907 cancers reported in 463,300 HIV-infected adults in the HACM Study. Based on trends in this study, the researchers made projections for cancer incidence through 2030.
They projected that HIV-positive adults of all ages will see a significant decrease over time in the incidence of NHL, Kaposi sarcoma, cervical cancer, anal cancer among men who have sex with men (MSM), lung cancer, and Hodgkin lymphoma.
Patients age 65 and older will see a significant decrease in colon cancer incidence over time. However, there will be no significant change for patients younger than 65.
HIV-positive adults of all ages will see no significant change over time in the incidence of liver cancer, oral cavity cancer, anal cancer among non-MSMs, and breast cancer.
The incidence of prostate cancer will increase significantly among patients ages 35 to 44 and among patients ages 45 to 64.
Cancer burden
The researchers said the number of adults living with HIV in the US is projected to increase from 1.06 million in 2006 to 1.17 million in 2018, but it is expected to decline to 1.09 million in 2030.
The team noted that, in 2006, there were an estimated 8241 cancers in patients with HIV—3522 AIDS-defining cancers and 4719 malignancies not associated with AIDS.
In 2030, the total number of cancers in the HIV-positive population is projected to be 6692, with decreases in AIDS-defining cancers (n=716) and increases in other cancers (n=5976) from the 2006 data.
In 2010, the most common cancers among HIV-positive patients were estimated to be NHL (n=1488), Kaposi sarcoma (n=1133), and lung cancer (n=815).
But in 2030, the most common cancers are projected to be prostate (n=1587), lung (n=1027), and liver cancers (n=483).
“It is critical to understand both incidence rates and burden over time, as rates capture changes in cancer risk, and burden quantifies the actual number of cancer cases expected to occur,” said study investigator Meredith S. Shiels, PhD, of the National Cancer Institute in Bethesda, Maryland.
“For example, lung cancer rates are expected to decrease in the future, but the burden is expected to increase due to the growing number of older people living with HIV.” ![]()
Atezolizumab improved survival in triple-negative breast cancer
Treatment with the anti-PD-L1 cancer immunotherapy atezolizumab produced a durable clinical benefit in patients with metastatic triple-negative breast cancer who responded to treatment, according to results from a phase I study.
Overall survival (OS) rates were 41% at 1 year and 22% at both year 2 and year 3. Patients with PD-L1 on 5% or more of tumor-infiltrating immune cells (IC2/3) achieved even better clinical outcomes: Their OS rates at 1, 2, and 3 years were 45%, 28%, and 28%.
The findings from this early phase I trial, which were presented at the annual meeting of the American Association for Cancer Research, also demonstrated that response rates were higher in the first-line setting, and an exploratory biomarker analysis suggested that higher CD8 T cell and tumor-infiltrating lymphocyte counts also contributed to a better response.
“We have no targeted therapy at the moment for triple-negative breast cancer,” said study lead author Dr. Peter Schmid, director of the St. Bartholomew’s Breast Centre at St. Bartholomew’s Hospital and Barts Cancer Institute in London, during a media briefing. “The treatment we have is chemotherapy, and most patients develop resistance relatively quickly.”
Dr. Schmid noted that the median survival for these patients is still relatively short – about 9-12 months – so, the data from this trial need to be seen in that context.
“On the other hand, triple-negative breast cancer is probably the best subtype of breast cancer in terms of selecting patients for immune therapy,” said Dr. Schmid. “This is based on a high degree of genetic instability, a high rate of mutations, higher levels of PD-L1 expression, and tumor infiltrating lymphocytes inside the tumor.”
Atezolizumab is a humanized monoclonal antibody that disrupts the PD pathway, inhibits the binding of PD-L1 to PD-1 and B7.1, and, in doing so, restores tumor-specific T-cell immunity.
In this study, Dr Schmid and colleagues recruited patients with metastatic triple-negative breast cancer to one of the expansion cohorts of a phase I trial. A total of 112 patients were evaluable for response. Of this group, 19 received atezolizumab as first-line treatment, and 93 had received at least two lines of prior therapy.
Atezolizumab was administered every 3 weeks at 15 mg/kg or 20 mg/kg, and the level of PD-L1 expression on tumor-infiltrating immune cells was evaluated. The primary endpoint of the study was safety, with overall response rate, duration of response, and progression-free survival as key secondary endpoints.
The 1- and 2-year overall survival rates for responders were 100%, but that dropped to 33% and 11%, respectively, for nonresponders. Of the 11 responders, 5 received atezolizumab as first-line therapy, while 9 had high PD-L1 expression (IC2/3).
For patients who received atezolizumab in the first-line setting, 1-year overall survival was 63%, and 2-year overall survival was 47%. The rates were lower for second-line and beyond; 37% and 18%, respectively.
For IC2/3 patients, 1-year overall survival was 45%, compared with 37% for those with low to no PD-L1 expression (IC0/1).
Only 11% of patients experienced treatment-related grade 3 or greater adverse events, and side effects led to treatment discontinuation in 3% of patients.
A key message was that the duration of response had a median of 21 months, and that is significant in this disease setting, explained Dr. Schmid. Another important point was that “overall survival was significantly longer that what we see with chemotherapy.”
Genentech funded the study. Dr Schmid’s spouse is a consultant to Roche/Genentech.
Treatment with the anti-PD-L1 cancer immunotherapy atezolizumab produced a durable clinical benefit in patients with metastatic triple-negative breast cancer who responded to treatment, according to results from a phase I study.
Overall survival (OS) rates were 41% at 1 year and 22% at both year 2 and year 3. Patients with PD-L1 on 5% or more of tumor-infiltrating immune cells (IC2/3) achieved even better clinical outcomes: Their OS rates at 1, 2, and 3 years were 45%, 28%, and 28%.
The findings from this early phase I trial, which were presented at the annual meeting of the American Association for Cancer Research, also demonstrated that response rates were higher in the first-line setting, and an exploratory biomarker analysis suggested that higher CD8 T cell and tumor-infiltrating lymphocyte counts also contributed to a better response.
“We have no targeted therapy at the moment for triple-negative breast cancer,” said study lead author Dr. Peter Schmid, director of the St. Bartholomew’s Breast Centre at St. Bartholomew’s Hospital and Barts Cancer Institute in London, during a media briefing. “The treatment we have is chemotherapy, and most patients develop resistance relatively quickly.”
Dr. Schmid noted that the median survival for these patients is still relatively short – about 9-12 months – so, the data from this trial need to be seen in that context.
“On the other hand, triple-negative breast cancer is probably the best subtype of breast cancer in terms of selecting patients for immune therapy,” said Dr. Schmid. “This is based on a high degree of genetic instability, a high rate of mutations, higher levels of PD-L1 expression, and tumor infiltrating lymphocytes inside the tumor.”
Atezolizumab is a humanized monoclonal antibody that disrupts the PD pathway, inhibits the binding of PD-L1 to PD-1 and B7.1, and, in doing so, restores tumor-specific T-cell immunity.
In this study, Dr Schmid and colleagues recruited patients with metastatic triple-negative breast cancer to one of the expansion cohorts of a phase I trial. A total of 112 patients were evaluable for response. Of this group, 19 received atezolizumab as first-line treatment, and 93 had received at least two lines of prior therapy.
Atezolizumab was administered every 3 weeks at 15 mg/kg or 20 mg/kg, and the level of PD-L1 expression on tumor-infiltrating immune cells was evaluated. The primary endpoint of the study was safety, with overall response rate, duration of response, and progression-free survival as key secondary endpoints.
The 1- and 2-year overall survival rates for responders were 100%, but that dropped to 33% and 11%, respectively, for nonresponders. Of the 11 responders, 5 received atezolizumab as first-line therapy, while 9 had high PD-L1 expression (IC2/3).
For patients who received atezolizumab in the first-line setting, 1-year overall survival was 63%, and 2-year overall survival was 47%. The rates were lower for second-line and beyond; 37% and 18%, respectively.
For IC2/3 patients, 1-year overall survival was 45%, compared with 37% for those with low to no PD-L1 expression (IC0/1).
Only 11% of patients experienced treatment-related grade 3 or greater adverse events, and side effects led to treatment discontinuation in 3% of patients.
A key message was that the duration of response had a median of 21 months, and that is significant in this disease setting, explained Dr. Schmid. Another important point was that “overall survival was significantly longer that what we see with chemotherapy.”
Genentech funded the study. Dr Schmid’s spouse is a consultant to Roche/Genentech.
Treatment with the anti-PD-L1 cancer immunotherapy atezolizumab produced a durable clinical benefit in patients with metastatic triple-negative breast cancer who responded to treatment, according to results from a phase I study.
Overall survival (OS) rates were 41% at 1 year and 22% at both year 2 and year 3. Patients with PD-L1 on 5% or more of tumor-infiltrating immune cells (IC2/3) achieved even better clinical outcomes: Their OS rates at 1, 2, and 3 years were 45%, 28%, and 28%.
The findings from this early phase I trial, which were presented at the annual meeting of the American Association for Cancer Research, also demonstrated that response rates were higher in the first-line setting, and an exploratory biomarker analysis suggested that higher CD8 T cell and tumor-infiltrating lymphocyte counts also contributed to a better response.
“We have no targeted therapy at the moment for triple-negative breast cancer,” said study lead author Dr. Peter Schmid, director of the St. Bartholomew’s Breast Centre at St. Bartholomew’s Hospital and Barts Cancer Institute in London, during a media briefing. “The treatment we have is chemotherapy, and most patients develop resistance relatively quickly.”
Dr. Schmid noted that the median survival for these patients is still relatively short – about 9-12 months – so, the data from this trial need to be seen in that context.
“On the other hand, triple-negative breast cancer is probably the best subtype of breast cancer in terms of selecting patients for immune therapy,” said Dr. Schmid. “This is based on a high degree of genetic instability, a high rate of mutations, higher levels of PD-L1 expression, and tumor infiltrating lymphocytes inside the tumor.”
Atezolizumab is a humanized monoclonal antibody that disrupts the PD pathway, inhibits the binding of PD-L1 to PD-1 and B7.1, and, in doing so, restores tumor-specific T-cell immunity.
In this study, Dr Schmid and colleagues recruited patients with metastatic triple-negative breast cancer to one of the expansion cohorts of a phase I trial. A total of 112 patients were evaluable for response. Of this group, 19 received atezolizumab as first-line treatment, and 93 had received at least two lines of prior therapy.
Atezolizumab was administered every 3 weeks at 15 mg/kg or 20 mg/kg, and the level of PD-L1 expression on tumor-infiltrating immune cells was evaluated. The primary endpoint of the study was safety, with overall response rate, duration of response, and progression-free survival as key secondary endpoints.
The 1- and 2-year overall survival rates for responders were 100%, but that dropped to 33% and 11%, respectively, for nonresponders. Of the 11 responders, 5 received atezolizumab as first-line therapy, while 9 had high PD-L1 expression (IC2/3).
For patients who received atezolizumab in the first-line setting, 1-year overall survival was 63%, and 2-year overall survival was 47%. The rates were lower for second-line and beyond; 37% and 18%, respectively.
For IC2/3 patients, 1-year overall survival was 45%, compared with 37% for those with low to no PD-L1 expression (IC0/1).
Only 11% of patients experienced treatment-related grade 3 or greater adverse events, and side effects led to treatment discontinuation in 3% of patients.
A key message was that the duration of response had a median of 21 months, and that is significant in this disease setting, explained Dr. Schmid. Another important point was that “overall survival was significantly longer that what we see with chemotherapy.”
Genentech funded the study. Dr Schmid’s spouse is a consultant to Roche/Genentech.
FROM THE AACR ANNUAL MEETING
Key clinical point: In a phase I trial, the immunotherapy agent atezolizumab improved survival in triple-negative breast cancer.
Major finding: Overall survival rates were 41% at 1 year and 22% at both year 2 and year 3.
Data source: A phase I trial with a total of 112 patients who were evaluable for response.
Disclosures: Genentech funded the study. Dr Schmid’s spouse is a consultant to Roche/Genentech.
Disease burden impacts outcome of CAR T-cell therapy in B-ALL
WASHINGTON, DC—Results of a retrospective study suggest pretreatment disease burden impacts the outcome of chimeric antigen receptor (CAR) T-cell therapy in patients with relapsed or refractory B-cell acute lymphoblastic leukemia (B-ALL).
Patients who had minimal residual disease (MRD) prior to treatment had superior event-free and overall survival compared to patients who had morphologic disease before treatment.
Patients with MRD were also less likely to experience cytokine release syndrome (CRS) and neurologic toxicity.
Jae Park, MD, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York, New York, presented these results at the AACR Annual Meeting 2017 (abstract CT078).
This study was funded by Juno Therapeutics, the National Cancer Institute, the Terry Fox Foundation, and MSKCC Experimental Therapeutics Center.
“[W]e and other groups have developed and tested CD19-specific [19-28z] CAR T-cell therapy and have reported encouraging results, with high initial complete response rates in patients with B-ALL,” Dr Park said.
“However, relapses are common, even after achieving seemingly deep remission, and severe toxicities have been observed in some patients.”
To gain more insight into these results, Dr Park and his colleagues retrospectively analyzed data from a prospective clinical trial that tested 19-28z CAR T-cell therapy in patients with B-ALL.
All 51 adults in this trial had relapsed after or were refractory to 1 or more conventional multiagent chemotherapy regimens.
The researchers measured disease burden prior to CAR T-cell infusion in all patients and divided them into 2 cohorts:
- 20 patients who had MRD—less than 5% blasts in the bone marrow
- 31 patients who had morphologic disease—5% or more blasts in the bone marrow.
Response and survival
The complete response rate was 95% in the MRD cohort and 77% in the morphologic disease cohort, a difference that was not statistically significant.
At a median follow-up of 18 months, the median event-free survival and overall survival had not been reached for patients in the MRD cohort (because most were still alive and disease-free).
However, for patients in the morphologic disease cohort, the median event-free survival was 6.3 months (P=0.0005), and the median overall survival was 17 months (P=0.0189).
Role of transplant
The researchers found that long-term survival did not improve for patients who proceeded to hematopoietic stem cell transplant (HSCT), regardless of their disease burden at baseline.
“While more patients and longer follow-up will be needed to adequately address the significance of HSCT, the result of this analysis raises a question as to whether 19-28z CAR therapy can be considered as a definitive, curative therapy rather than a bridge to stem cell transplant, at least in a subset of patients,” Dr Park noted.
“Our data suggest that incorporation of 19-28z CAR T cells at the time of MRD following first-line chemotherapy will maximize the durability of CAR T-cell-mediated remissions and survival and can potentially spare these high-risk patients from HSCT, rather than waiting until they relapse morphologically and then trying CAR T-cell therapy when it is less likely to achieve a durable long-term outcome.”
Adverse events and limitations
Patients from the MRD cohort fared better than the morphologic disease cohort in terms of CRS and neurologic toxicity.
Forty-two percent of patients in the morphologic disease cohort developed CRS, compared to 5% of patients in the MRD cohort (P=0.0326).
Neurologic toxicity occurred in 58% of patients in the morphologic disease cohort and 15% of those in the MRD cohort (P=0.0001).
Dr Park noted that a limitation of this study is its retrospective nature, and the findings will need to be validated prospectively.
Furthermore, the analysis on the impact of allogeneic HSCT was limited by a relatively small sample size in each cohort. ![]()
WASHINGTON, DC—Results of a retrospective study suggest pretreatment disease burden impacts the outcome of chimeric antigen receptor (CAR) T-cell therapy in patients with relapsed or refractory B-cell acute lymphoblastic leukemia (B-ALL).
Patients who had minimal residual disease (MRD) prior to treatment had superior event-free and overall survival compared to patients who had morphologic disease before treatment.
Patients with MRD were also less likely to experience cytokine release syndrome (CRS) and neurologic toxicity.
Jae Park, MD, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York, New York, presented these results at the AACR Annual Meeting 2017 (abstract CT078).
This study was funded by Juno Therapeutics, the National Cancer Institute, the Terry Fox Foundation, and MSKCC Experimental Therapeutics Center.
“[W]e and other groups have developed and tested CD19-specific [19-28z] CAR T-cell therapy and have reported encouraging results, with high initial complete response rates in patients with B-ALL,” Dr Park said.
“However, relapses are common, even after achieving seemingly deep remission, and severe toxicities have been observed in some patients.”
To gain more insight into these results, Dr Park and his colleagues retrospectively analyzed data from a prospective clinical trial that tested 19-28z CAR T-cell therapy in patients with B-ALL.
All 51 adults in this trial had relapsed after or were refractory to 1 or more conventional multiagent chemotherapy regimens.
The researchers measured disease burden prior to CAR T-cell infusion in all patients and divided them into 2 cohorts:
- 20 patients who had MRD—less than 5% blasts in the bone marrow
- 31 patients who had morphologic disease—5% or more blasts in the bone marrow.
Response and survival
The complete response rate was 95% in the MRD cohort and 77% in the morphologic disease cohort, a difference that was not statistically significant.
At a median follow-up of 18 months, the median event-free survival and overall survival had not been reached for patients in the MRD cohort (because most were still alive and disease-free).
However, for patients in the morphologic disease cohort, the median event-free survival was 6.3 months (P=0.0005), and the median overall survival was 17 months (P=0.0189).
Role of transplant
The researchers found that long-term survival did not improve for patients who proceeded to hematopoietic stem cell transplant (HSCT), regardless of their disease burden at baseline.
“While more patients and longer follow-up will be needed to adequately address the significance of HSCT, the result of this analysis raises a question as to whether 19-28z CAR therapy can be considered as a definitive, curative therapy rather than a bridge to stem cell transplant, at least in a subset of patients,” Dr Park noted.
“Our data suggest that incorporation of 19-28z CAR T cells at the time of MRD following first-line chemotherapy will maximize the durability of CAR T-cell-mediated remissions and survival and can potentially spare these high-risk patients from HSCT, rather than waiting until they relapse morphologically and then trying CAR T-cell therapy when it is less likely to achieve a durable long-term outcome.”
Adverse events and limitations
Patients from the MRD cohort fared better than the morphologic disease cohort in terms of CRS and neurologic toxicity.
Forty-two percent of patients in the morphologic disease cohort developed CRS, compared to 5% of patients in the MRD cohort (P=0.0326).
Neurologic toxicity occurred in 58% of patients in the morphologic disease cohort and 15% of those in the MRD cohort (P=0.0001).
Dr Park noted that a limitation of this study is its retrospective nature, and the findings will need to be validated prospectively.
Furthermore, the analysis on the impact of allogeneic HSCT was limited by a relatively small sample size in each cohort. ![]()
WASHINGTON, DC—Results of a retrospective study suggest pretreatment disease burden impacts the outcome of chimeric antigen receptor (CAR) T-cell therapy in patients with relapsed or refractory B-cell acute lymphoblastic leukemia (B-ALL).
Patients who had minimal residual disease (MRD) prior to treatment had superior event-free and overall survival compared to patients who had morphologic disease before treatment.
Patients with MRD were also less likely to experience cytokine release syndrome (CRS) and neurologic toxicity.
Jae Park, MD, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York, New York, presented these results at the AACR Annual Meeting 2017 (abstract CT078).
This study was funded by Juno Therapeutics, the National Cancer Institute, the Terry Fox Foundation, and MSKCC Experimental Therapeutics Center.
“[W]e and other groups have developed and tested CD19-specific [19-28z] CAR T-cell therapy and have reported encouraging results, with high initial complete response rates in patients with B-ALL,” Dr Park said.
“However, relapses are common, even after achieving seemingly deep remission, and severe toxicities have been observed in some patients.”
To gain more insight into these results, Dr Park and his colleagues retrospectively analyzed data from a prospective clinical trial that tested 19-28z CAR T-cell therapy in patients with B-ALL.
All 51 adults in this trial had relapsed after or were refractory to 1 or more conventional multiagent chemotherapy regimens.
The researchers measured disease burden prior to CAR T-cell infusion in all patients and divided them into 2 cohorts:
- 20 patients who had MRD—less than 5% blasts in the bone marrow
- 31 patients who had morphologic disease—5% or more blasts in the bone marrow.
Response and survival
The complete response rate was 95% in the MRD cohort and 77% in the morphologic disease cohort, a difference that was not statistically significant.
At a median follow-up of 18 months, the median event-free survival and overall survival had not been reached for patients in the MRD cohort (because most were still alive and disease-free).
However, for patients in the morphologic disease cohort, the median event-free survival was 6.3 months (P=0.0005), and the median overall survival was 17 months (P=0.0189).
Role of transplant
The researchers found that long-term survival did not improve for patients who proceeded to hematopoietic stem cell transplant (HSCT), regardless of their disease burden at baseline.
“While more patients and longer follow-up will be needed to adequately address the significance of HSCT, the result of this analysis raises a question as to whether 19-28z CAR therapy can be considered as a definitive, curative therapy rather than a bridge to stem cell transplant, at least in a subset of patients,” Dr Park noted.
“Our data suggest that incorporation of 19-28z CAR T cells at the time of MRD following first-line chemotherapy will maximize the durability of CAR T-cell-mediated remissions and survival and can potentially spare these high-risk patients from HSCT, rather than waiting until they relapse morphologically and then trying CAR T-cell therapy when it is less likely to achieve a durable long-term outcome.”
Adverse events and limitations
Patients from the MRD cohort fared better than the morphologic disease cohort in terms of CRS and neurologic toxicity.
Forty-two percent of patients in the morphologic disease cohort developed CRS, compared to 5% of patients in the MRD cohort (P=0.0326).
Neurologic toxicity occurred in 58% of patients in the morphologic disease cohort and 15% of those in the MRD cohort (P=0.0001).
Dr Park noted that a limitation of this study is its retrospective nature, and the findings will need to be validated prospectively.
Furthermore, the analysis on the impact of allogeneic HSCT was limited by a relatively small sample size in each cohort. ![]()
Nivolumab boosts 5-year survival in advanced NSCLC
Early data show that treatment with the immune checkpoint inhibitor nivolumab (Opdivo) resulted in a 5-year overall survival rate of 16% among patients with advanced non–small-cell lung cancer (NSCLC).
In comparison, the 5-year survival rate for patients with advanced lung and bronchus cancer, according to SEER data, is 4.3%, and for those with advanced NSCLC, 4.9%.
“This is the first report of the long-term survival rate in patients with metastatic NSCLC treated with an immune checkpoint inhibitor,” said Julie Brahmer, MD, of the Bloomberg Kimmel Institute for Cancer Immunotherapy at Johns Hopkins, Baltimore.
For a small subset of patients, immunotherapy can work for a very long time, explained Dr. Brahmer, who discussed her findings during a presscast at the annual meeting of the American Association for Cancer Research.
The 5-year overall survival rate that was reported in this study was much higher than what has been seen for this patient population who receive the standard of care. Statistics show that the majority of patients with advanced disease will die within a year of their diagnosis, Dr. Brahmer pointed out.
The findings presented at the meeting are updated results from the phase Ib CA209-003 dose-escalation cohort expansion trial that comprised 129 patients with heavily pretreated, advanced NSCLC . The cohort was randomized to receive nivolumab once every 2 weeks for up to 2 years at one of three dose levels: 1 mg/kg, 3 mg/kg, or 10 mg/kg.
A previous analysis of the data showed promising activity, and findings from subsequent clinical trials led to the approval of nivolumab for use in the second line setting of advanced NSCLC.
Dr. Brahmer now reported findings based on 5-year results of this phase Ib trial. “This analysis is based on a minimum follow up of 58 months,” she said.
The overall 5-year survival rates for squamous NSCLC were 16%, and the rates for nonsquamous were 15%.
At 1 year, overall survival was 42%. At 2 years, it was 24%, and at 3 years, 18%.
“After 3 years, the survival curve has plateaued out, which is similar to what has been seen in the past in other diseases treated with immunotherapy,” Dr. Brahmer noted.
Within the cohort, there were 16 patients who had survived for at least 5 years. Of this group, 12 achieved a partial response, 2 patients had stable disease, and 2 had progressive disease.
Dr. Brahmer pointed out that there was nothing different or unusual among the 16 patients who survived for 5 years, compared with the rest of the cohort. Their characteristics were similar to others in the study, most of them were former smokers, and they had very similar rates of different histologies.
One interesting note was that within that group, there were two patients with EGFR mutations. “We usually don’t expect them to do well with immunotherapy,” she said.
Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Early data show that treatment with the immune checkpoint inhibitor nivolumab (Opdivo) resulted in a 5-year overall survival rate of 16% among patients with advanced non–small-cell lung cancer (NSCLC).
In comparison, the 5-year survival rate for patients with advanced lung and bronchus cancer, according to SEER data, is 4.3%, and for those with advanced NSCLC, 4.9%.
“This is the first report of the long-term survival rate in patients with metastatic NSCLC treated with an immune checkpoint inhibitor,” said Julie Brahmer, MD, of the Bloomberg Kimmel Institute for Cancer Immunotherapy at Johns Hopkins, Baltimore.
For a small subset of patients, immunotherapy can work for a very long time, explained Dr. Brahmer, who discussed her findings during a presscast at the annual meeting of the American Association for Cancer Research.
The 5-year overall survival rate that was reported in this study was much higher than what has been seen for this patient population who receive the standard of care. Statistics show that the majority of patients with advanced disease will die within a year of their diagnosis, Dr. Brahmer pointed out.
The findings presented at the meeting are updated results from the phase Ib CA209-003 dose-escalation cohort expansion trial that comprised 129 patients with heavily pretreated, advanced NSCLC . The cohort was randomized to receive nivolumab once every 2 weeks for up to 2 years at one of three dose levels: 1 mg/kg, 3 mg/kg, or 10 mg/kg.
A previous analysis of the data showed promising activity, and findings from subsequent clinical trials led to the approval of nivolumab for use in the second line setting of advanced NSCLC.
Dr. Brahmer now reported findings based on 5-year results of this phase Ib trial. “This analysis is based on a minimum follow up of 58 months,” she said.
The overall 5-year survival rates for squamous NSCLC were 16%, and the rates for nonsquamous were 15%.
At 1 year, overall survival was 42%. At 2 years, it was 24%, and at 3 years, 18%.
“After 3 years, the survival curve has plateaued out, which is similar to what has been seen in the past in other diseases treated with immunotherapy,” Dr. Brahmer noted.
Within the cohort, there were 16 patients who had survived for at least 5 years. Of this group, 12 achieved a partial response, 2 patients had stable disease, and 2 had progressive disease.
Dr. Brahmer pointed out that there was nothing different or unusual among the 16 patients who survived for 5 years, compared with the rest of the cohort. Their characteristics were similar to others in the study, most of them were former smokers, and they had very similar rates of different histologies.
One interesting note was that within that group, there were two patients with EGFR mutations. “We usually don’t expect them to do well with immunotherapy,” she said.
Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Early data show that treatment with the immune checkpoint inhibitor nivolumab (Opdivo) resulted in a 5-year overall survival rate of 16% among patients with advanced non–small-cell lung cancer (NSCLC).
In comparison, the 5-year survival rate for patients with advanced lung and bronchus cancer, according to SEER data, is 4.3%, and for those with advanced NSCLC, 4.9%.
“This is the first report of the long-term survival rate in patients with metastatic NSCLC treated with an immune checkpoint inhibitor,” said Julie Brahmer, MD, of the Bloomberg Kimmel Institute for Cancer Immunotherapy at Johns Hopkins, Baltimore.
For a small subset of patients, immunotherapy can work for a very long time, explained Dr. Brahmer, who discussed her findings during a presscast at the annual meeting of the American Association for Cancer Research.
The 5-year overall survival rate that was reported in this study was much higher than what has been seen for this patient population who receive the standard of care. Statistics show that the majority of patients with advanced disease will die within a year of their diagnosis, Dr. Brahmer pointed out.
The findings presented at the meeting are updated results from the phase Ib CA209-003 dose-escalation cohort expansion trial that comprised 129 patients with heavily pretreated, advanced NSCLC . The cohort was randomized to receive nivolumab once every 2 weeks for up to 2 years at one of three dose levels: 1 mg/kg, 3 mg/kg, or 10 mg/kg.
A previous analysis of the data showed promising activity, and findings from subsequent clinical trials led to the approval of nivolumab for use in the second line setting of advanced NSCLC.
Dr. Brahmer now reported findings based on 5-year results of this phase Ib trial. “This analysis is based on a minimum follow up of 58 months,” she said.
The overall 5-year survival rates for squamous NSCLC were 16%, and the rates for nonsquamous were 15%.
At 1 year, overall survival was 42%. At 2 years, it was 24%, and at 3 years, 18%.
“After 3 years, the survival curve has plateaued out, which is similar to what has been seen in the past in other diseases treated with immunotherapy,” Dr. Brahmer noted.
Within the cohort, there were 16 patients who had survived for at least 5 years. Of this group, 12 achieved a partial response, 2 patients had stable disease, and 2 had progressive disease.
Dr. Brahmer pointed out that there was nothing different or unusual among the 16 patients who survived for 5 years, compared with the rest of the cohort. Their characteristics were similar to others in the study, most of them were former smokers, and they had very similar rates of different histologies.
One interesting note was that within that group, there were two patients with EGFR mutations. “We usually don’t expect them to do well with immunotherapy,” she said.
Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Key clinical point: Treatment with nivolumab resulted in a 5-year overall survival rate that is much higher than what is reported for this patient population receiving standard-of-care treatment.
Major finding: Nivolumab yielded a 5-year survival rate of 16% in a cohort of patients with advanced NSCLC.
Data source: Updated results from a phase Ib study that included 129 patients with advanced NSCLC.
Disclosures: Dr. Brahmer received research funding from, and is an adviser to, Bristol-Myers Squibb, which funded the study.
Drug may be new option for difficult-to-treat DLBCL, doc says
WASHINGTON, DC—Selinexor has demonstrated the potential to become a new oral treatment option for patients with difficult-to-treat diffuse large B-cell lymphoma (DLBCL), according to a presenter at the AACR Annual Meeting 2017.
Interim results from the phase 2b SADAL study showed that selinexor produced a 28.6% overall response rate (ORR), with an 11.1% complete response (CR) rate, in a heavily pretreated, older DLBCL population.
Responses were observed in GCB and non-GCB subtypes, and the median duration of response exceeded 7 months.
The most common adverse events (AEs) were fatigue, thrombocytopenia, nausea, anorexia, and vomiting.
Marie Maerevoet, MD, of the Institute Jules Bordet in Brussels, Belgium, presented data from the SADAL study as abstract CT132/13.*
The trial is sponsored by Karyopharm Therapeutics, the company developing selinexor.
Patients and treatment
The study enrolled 72 patients with relapsed or refractory DLBCL. At least 14 weeks had elapsed since their most recent systemic anti-DLBCL therapy.
The patients received selinexor—an oral selective inhibitor of nuclear export (SINE™) compound—at 60 mg or 100 mg twice weekly (days 1 and 3 each week) of each 28-day cycle.
60 mg arm
There were 37 patients in the 60 mg arm. Their median age was 71 (range, 38-87), and most (n=24) were male. Forty-nine percent of these patients (n=18) had GCB DLBCL.
Fourteen percent of patients had high-risk disease (according to the revised international prognostic index). Forty-three percent had high-intermediate-risk, 30% had low-intermediate-risk, and 14% had low-risk disease.
The patients had received a median of 3 prior treatment regimens (range, 2-5). Twenty-seven percent had received a prior transplant.
100 mg arm
There were 35 patients in the 100 mg arm. Their median age was 68 (range, 32-82), and most (n=23) were male. Fifty-one percent of patients (n=18) had GCB DLBCL.
Eleven percent of patients had high-risk, 40% had high-intermediate-risk, 37% had low-intermediate-risk, and 6% had low-risk disease. For 6% of patients, their risk group was unknown.
The patients had received a median of 3 prior treatment regimens (range, 2-5). Forty-six percent had received a prior transplant.
Safety
All 72 patients were evaluable for safety. The most common AEs across both dosing groups were fatigue (65%), thrombocytopenia (54%), nausea (51%), anorexia (49%), vomiting (35%), and anemia (32%).
These events were primarily grades 1 and 2 and were managed with dose modifications and/or standard supportive care.
The 60 mg dose was better tolerated than the 100 mg dose, with fewer dose interruptions and modifications required in the 60 mg arm.
Grade 3/4 AEs that were more common in the 100 mg arm than the 60 mg arm were fatigue (26% vs 11%), thrombocytopenia (46% vs 32%), and anorexia (11% vs 3%).
Efficacy
Sixty-three patients were analyzed for response. The ORR was 28.6% (18/63), with a CR rate of 11.1% (n=7) and a partial response (PR) rate of 17.5% (n=11).
The rate of stable disease (SD) was 14.3% (n=9), and the rate of progressive disease (PD) was 46% (n=29). Seven patients (11.1%) were not evaluable (NE).
The best responses as of March 1, 2017, according to subtype and selinexor dose, were as follows:
| Category | N | ORR | CR | PR | SD | PD | NE |
| 60 mg | 32 | 9 (28.1%) | 4 (12.5%) | 5 (15.6%) | 3 (9.4%) | 17 (53.1%) | 3 (9.4%) |
| 100 mg | 31 | 9 (29.0%) | 3 (9.7%) | 6 (19.4%) | 6 (19.4%) | 12 (38.7%) | 4 (12.9%) |
| GCB subtype | 32 | 8 (25.0%) | 3 (9.4%) | 5 (15.6%) | 6 (18.8%) | 13 (40.6%) | 5 (15.6%) |
| Non-GCB subtype | 31 | 10 (32.3%) | 4 (12.9%) | 6 (19.4%) | 3 (9.7%) | 16 (51.6%) | 2 (6.5%) |
The median duration of response was greater than 7 months. The median time to response was 2 months.
Among responders, the median time on treatment was 9 months, with a median follow-up of 13 months. As of the data cutoff date, 9 responders remained on treatment, including 6 patients with a CR.
The median overall survival was 8 months for all patients. As of the cutoff date, the median survival for the responders had not been reached.
“With the impressive and durable responses observed to date, including in both the GCB and non-GCB subtypes of DLBCL, single-agent selinexor is demonstrating the potential to become a new oral option for this difficult-to-treat patient population who are not candidates for transplantation and whose disease is unlikely to respond to further chemotherapy or targeted agents,” Dr Maerevoet said.
Trial update
As a result of the interim data from SADAL, and in consultation with the US Food and Drug Administration (FDA), Karyopharm is amending the study protocol.
SADAL will become a single-arm study focusing solely on single-agent selinexor dosed at 60 mg twice weekly.
The study is also being amended to reduce the 14-week treatment-free period to 8 weeks in patients who achieved at least a PR on their most recent therapy. Patients who were refractory to or did not achieve at least a PR on their prior therapy will continue with the 14-week treatment-free period.
Karyopharm plans to enroll up to an additional 90 patients to the new 60 mg single-arm cohort and expects to report top-line results from the SADAL study in mid-2018.
The FDA recently lifted a partial clinical hold placed on the SADAL trial and other trials of selinexor.
The FDA had placed the hold due to a lack of information in the investigator’s brochure, including an incomplete list of serious adverse events associated with selinexor. ![]()
*Data in the abstract differ from the presentation.
WASHINGTON, DC—Selinexor has demonstrated the potential to become a new oral treatment option for patients with difficult-to-treat diffuse large B-cell lymphoma (DLBCL), according to a presenter at the AACR Annual Meeting 2017.
Interim results from the phase 2b SADAL study showed that selinexor produced a 28.6% overall response rate (ORR), with an 11.1% complete response (CR) rate, in a heavily pretreated, older DLBCL population.
Responses were observed in GCB and non-GCB subtypes, and the median duration of response exceeded 7 months.
The most common adverse events (AEs) were fatigue, thrombocytopenia, nausea, anorexia, and vomiting.
Marie Maerevoet, MD, of the Institute Jules Bordet in Brussels, Belgium, presented data from the SADAL study as abstract CT132/13.*
The trial is sponsored by Karyopharm Therapeutics, the company developing selinexor.
Patients and treatment
The study enrolled 72 patients with relapsed or refractory DLBCL. At least 14 weeks had elapsed since their most recent systemic anti-DLBCL therapy.
The patients received selinexor—an oral selective inhibitor of nuclear export (SINE™) compound—at 60 mg or 100 mg twice weekly (days 1 and 3 each week) of each 28-day cycle.
60 mg arm
There were 37 patients in the 60 mg arm. Their median age was 71 (range, 38-87), and most (n=24) were male. Forty-nine percent of these patients (n=18) had GCB DLBCL.
Fourteen percent of patients had high-risk disease (according to the revised international prognostic index). Forty-three percent had high-intermediate-risk, 30% had low-intermediate-risk, and 14% had low-risk disease.
The patients had received a median of 3 prior treatment regimens (range, 2-5). Twenty-seven percent had received a prior transplant.
100 mg arm
There were 35 patients in the 100 mg arm. Their median age was 68 (range, 32-82), and most (n=23) were male. Fifty-one percent of patients (n=18) had GCB DLBCL.
Eleven percent of patients had high-risk, 40% had high-intermediate-risk, 37% had low-intermediate-risk, and 6% had low-risk disease. For 6% of patients, their risk group was unknown.
The patients had received a median of 3 prior treatment regimens (range, 2-5). Forty-six percent had received a prior transplant.
Safety
All 72 patients were evaluable for safety. The most common AEs across both dosing groups were fatigue (65%), thrombocytopenia (54%), nausea (51%), anorexia (49%), vomiting (35%), and anemia (32%).
These events were primarily grades 1 and 2 and were managed with dose modifications and/or standard supportive care.
The 60 mg dose was better tolerated than the 100 mg dose, with fewer dose interruptions and modifications required in the 60 mg arm.
Grade 3/4 AEs that were more common in the 100 mg arm than the 60 mg arm were fatigue (26% vs 11%), thrombocytopenia (46% vs 32%), and anorexia (11% vs 3%).
Efficacy
Sixty-three patients were analyzed for response. The ORR was 28.6% (18/63), with a CR rate of 11.1% (n=7) and a partial response (PR) rate of 17.5% (n=11).
The rate of stable disease (SD) was 14.3% (n=9), and the rate of progressive disease (PD) was 46% (n=29). Seven patients (11.1%) were not evaluable (NE).
The best responses as of March 1, 2017, according to subtype and selinexor dose, were as follows:
| Category | N | ORR | CR | PR | SD | PD | NE |
| 60 mg | 32 | 9 (28.1%) | 4 (12.5%) | 5 (15.6%) | 3 (9.4%) | 17 (53.1%) | 3 (9.4%) |
| 100 mg | 31 | 9 (29.0%) | 3 (9.7%) | 6 (19.4%) | 6 (19.4%) | 12 (38.7%) | 4 (12.9%) |
| GCB subtype | 32 | 8 (25.0%) | 3 (9.4%) | 5 (15.6%) | 6 (18.8%) | 13 (40.6%) | 5 (15.6%) |
| Non-GCB subtype | 31 | 10 (32.3%) | 4 (12.9%) | 6 (19.4%) | 3 (9.7%) | 16 (51.6%) | 2 (6.5%) |
The median duration of response was greater than 7 months. The median time to response was 2 months.
Among responders, the median time on treatment was 9 months, with a median follow-up of 13 months. As of the data cutoff date, 9 responders remained on treatment, including 6 patients with a CR.
The median overall survival was 8 months for all patients. As of the cutoff date, the median survival for the responders had not been reached.
“With the impressive and durable responses observed to date, including in both the GCB and non-GCB subtypes of DLBCL, single-agent selinexor is demonstrating the potential to become a new oral option for this difficult-to-treat patient population who are not candidates for transplantation and whose disease is unlikely to respond to further chemotherapy or targeted agents,” Dr Maerevoet said.
Trial update
As a result of the interim data from SADAL, and in consultation with the US Food and Drug Administration (FDA), Karyopharm is amending the study protocol.
SADAL will become a single-arm study focusing solely on single-agent selinexor dosed at 60 mg twice weekly.
The study is also being amended to reduce the 14-week treatment-free period to 8 weeks in patients who achieved at least a PR on their most recent therapy. Patients who were refractory to or did not achieve at least a PR on their prior therapy will continue with the 14-week treatment-free period.
Karyopharm plans to enroll up to an additional 90 patients to the new 60 mg single-arm cohort and expects to report top-line results from the SADAL study in mid-2018.
The FDA recently lifted a partial clinical hold placed on the SADAL trial and other trials of selinexor.
The FDA had placed the hold due to a lack of information in the investigator’s brochure, including an incomplete list of serious adverse events associated with selinexor. ![]()
*Data in the abstract differ from the presentation.
WASHINGTON, DC—Selinexor has demonstrated the potential to become a new oral treatment option for patients with difficult-to-treat diffuse large B-cell lymphoma (DLBCL), according to a presenter at the AACR Annual Meeting 2017.
Interim results from the phase 2b SADAL study showed that selinexor produced a 28.6% overall response rate (ORR), with an 11.1% complete response (CR) rate, in a heavily pretreated, older DLBCL population.
Responses were observed in GCB and non-GCB subtypes, and the median duration of response exceeded 7 months.
The most common adverse events (AEs) were fatigue, thrombocytopenia, nausea, anorexia, and vomiting.
Marie Maerevoet, MD, of the Institute Jules Bordet in Brussels, Belgium, presented data from the SADAL study as abstract CT132/13.*
The trial is sponsored by Karyopharm Therapeutics, the company developing selinexor.
Patients and treatment
The study enrolled 72 patients with relapsed or refractory DLBCL. At least 14 weeks had elapsed since their most recent systemic anti-DLBCL therapy.
The patients received selinexor—an oral selective inhibitor of nuclear export (SINE™) compound—at 60 mg or 100 mg twice weekly (days 1 and 3 each week) of each 28-day cycle.
60 mg arm
There were 37 patients in the 60 mg arm. Their median age was 71 (range, 38-87), and most (n=24) were male. Forty-nine percent of these patients (n=18) had GCB DLBCL.
Fourteen percent of patients had high-risk disease (according to the revised international prognostic index). Forty-three percent had high-intermediate-risk, 30% had low-intermediate-risk, and 14% had low-risk disease.
The patients had received a median of 3 prior treatment regimens (range, 2-5). Twenty-seven percent had received a prior transplant.
100 mg arm
There were 35 patients in the 100 mg arm. Their median age was 68 (range, 32-82), and most (n=23) were male. Fifty-one percent of patients (n=18) had GCB DLBCL.
Eleven percent of patients had high-risk, 40% had high-intermediate-risk, 37% had low-intermediate-risk, and 6% had low-risk disease. For 6% of patients, their risk group was unknown.
The patients had received a median of 3 prior treatment regimens (range, 2-5). Forty-six percent had received a prior transplant.
Safety
All 72 patients were evaluable for safety. The most common AEs across both dosing groups were fatigue (65%), thrombocytopenia (54%), nausea (51%), anorexia (49%), vomiting (35%), and anemia (32%).
These events were primarily grades 1 and 2 and were managed with dose modifications and/or standard supportive care.
The 60 mg dose was better tolerated than the 100 mg dose, with fewer dose interruptions and modifications required in the 60 mg arm.
Grade 3/4 AEs that were more common in the 100 mg arm than the 60 mg arm were fatigue (26% vs 11%), thrombocytopenia (46% vs 32%), and anorexia (11% vs 3%).
Efficacy
Sixty-three patients were analyzed for response. The ORR was 28.6% (18/63), with a CR rate of 11.1% (n=7) and a partial response (PR) rate of 17.5% (n=11).
The rate of stable disease (SD) was 14.3% (n=9), and the rate of progressive disease (PD) was 46% (n=29). Seven patients (11.1%) were not evaluable (NE).
The best responses as of March 1, 2017, according to subtype and selinexor dose, were as follows:
| Category | N | ORR | CR | PR | SD | PD | NE |
| 60 mg | 32 | 9 (28.1%) | 4 (12.5%) | 5 (15.6%) | 3 (9.4%) | 17 (53.1%) | 3 (9.4%) |
| 100 mg | 31 | 9 (29.0%) | 3 (9.7%) | 6 (19.4%) | 6 (19.4%) | 12 (38.7%) | 4 (12.9%) |
| GCB subtype | 32 | 8 (25.0%) | 3 (9.4%) | 5 (15.6%) | 6 (18.8%) | 13 (40.6%) | 5 (15.6%) |
| Non-GCB subtype | 31 | 10 (32.3%) | 4 (12.9%) | 6 (19.4%) | 3 (9.7%) | 16 (51.6%) | 2 (6.5%) |
The median duration of response was greater than 7 months. The median time to response was 2 months.
Among responders, the median time on treatment was 9 months, with a median follow-up of 13 months. As of the data cutoff date, 9 responders remained on treatment, including 6 patients with a CR.
The median overall survival was 8 months for all patients. As of the cutoff date, the median survival for the responders had not been reached.
“With the impressive and durable responses observed to date, including in both the GCB and non-GCB subtypes of DLBCL, single-agent selinexor is demonstrating the potential to become a new oral option for this difficult-to-treat patient population who are not candidates for transplantation and whose disease is unlikely to respond to further chemotherapy or targeted agents,” Dr Maerevoet said.
Trial update
As a result of the interim data from SADAL, and in consultation with the US Food and Drug Administration (FDA), Karyopharm is amending the study protocol.
SADAL will become a single-arm study focusing solely on single-agent selinexor dosed at 60 mg twice weekly.
The study is also being amended to reduce the 14-week treatment-free period to 8 weeks in patients who achieved at least a PR on their most recent therapy. Patients who were refractory to or did not achieve at least a PR on their prior therapy will continue with the 14-week treatment-free period.
Karyopharm plans to enroll up to an additional 90 patients to the new 60 mg single-arm cohort and expects to report top-line results from the SADAL study in mid-2018.
The FDA recently lifted a partial clinical hold placed on the SADAL trial and other trials of selinexor.
The FDA had placed the hold due to a lack of information in the investigator’s brochure, including an incomplete list of serious adverse events associated with selinexor. ![]()
*Data in the abstract differ from the presentation.
Extremely short and long telomeres linked to risk of leukemia
WASHINGTON, DC—Telomere length may predict cancer risk and could be a target for future therapies, according to research presented at the AACR Annual Meeting 2017.
The study suggests that, overall, longer-than-expected telomeres are associated with an increased risk of cancer.
However, investigators also found an increased risk of certain cancers, including leukemia, among patients who had very short or very long telomeres.
“Telomeres and cancer clearly have a complex relationship,” said study investigator Jian-Min Yuan, MD, PhD, of the University of Pittsburgh Cancer Institute in Pennsylvania.
“Our hope is that by understanding this relationship, we may be able to predict which people are most likely to develop certain cancers so they can take preventive measures and perhaps be screened more often, as well as develop therapies to help our DNA keep or return its telomeres to a healthy length.”
Dr Yuan and his colleagues presented their research as abstract 2267/21.*
The team analyzed blood samples and health data on 26,540 individuals enrolled in the Singapore Chinese Health Study, which has followed the health outcomes of participants since 1993. As of the end of 2015, 4060 participants had developed cancer (77 with leukemia).
The investigators divided participants into 5 groups, based on the length of their telomeres.
The group with the longest telomeres (quartile 5) had a significantly higher risk of developing any cancer than the group with the shortest telomeres (quartile 1), after taking into account the effects of age, sex, education, body mass index, smoking habits, and alcohol consumption. The hazard ratio (HR) was 1.33 (P<0.0001).
In particular, the group with the longest telomeres had a significantly increased risk of colorectal cancer (HR=1.37, P=0.010), breast cancer (HR=1.39, P=0.007), prostate cancer (HR=1.55, P=0.011), and pancreatic cancer (HR=2.58, P=0.009).
On the other hand, the risk of liver cancer decreased as telomere length increased. The HR was 0.72 for patients in quartile 5 compared to those in quartile 1 (Plinear=0.056).
The risk of 3 cancers was greatest for both the groups with extremely short and extremely long telomeres—quartiles 1 and 5, respectively.
For leukemia, the HR was 2.15 for quartile 1 and 1.68 for quartile 5, when compared to quartile 3 (Pnon-linear=0.015).
For bladder cancer, the HRs were 1.72 and 2.17, respectively (Pnon-linear=0.01). And for stomach cancer, the HRs were 1.63 and 1.55, respectively (Pnon-linear=0.020).
“We had the idea for this study more than 7 years ago, but it took the laboratory 3 months to finish quantifying telomere length for just 100 samples, which was not enough to draw any meaningful conclusions,” Dr Yuan said.
“Not even a decade later, we’ve been able to run nearly 30,000 samples in a year and draw these really robust insights, showing how far technology has come. Even more complicated will be linking telomere length to genome-wide analyses, which is on the horizon. We’re on the cusp of gaining a truly remarkable understanding of the complicated biological phenomena that lead to cancer.” ![]()
*The presentation differed from the abstract.
WASHINGTON, DC—Telomere length may predict cancer risk and could be a target for future therapies, according to research presented at the AACR Annual Meeting 2017.
The study suggests that, overall, longer-than-expected telomeres are associated with an increased risk of cancer.
However, investigators also found an increased risk of certain cancers, including leukemia, among patients who had very short or very long telomeres.
“Telomeres and cancer clearly have a complex relationship,” said study investigator Jian-Min Yuan, MD, PhD, of the University of Pittsburgh Cancer Institute in Pennsylvania.
“Our hope is that by understanding this relationship, we may be able to predict which people are most likely to develop certain cancers so they can take preventive measures and perhaps be screened more often, as well as develop therapies to help our DNA keep or return its telomeres to a healthy length.”
Dr Yuan and his colleagues presented their research as abstract 2267/21.*
The team analyzed blood samples and health data on 26,540 individuals enrolled in the Singapore Chinese Health Study, which has followed the health outcomes of participants since 1993. As of the end of 2015, 4060 participants had developed cancer (77 with leukemia).
The investigators divided participants into 5 groups, based on the length of their telomeres.
The group with the longest telomeres (quartile 5) had a significantly higher risk of developing any cancer than the group with the shortest telomeres (quartile 1), after taking into account the effects of age, sex, education, body mass index, smoking habits, and alcohol consumption. The hazard ratio (HR) was 1.33 (P<0.0001).
In particular, the group with the longest telomeres had a significantly increased risk of colorectal cancer (HR=1.37, P=0.010), breast cancer (HR=1.39, P=0.007), prostate cancer (HR=1.55, P=0.011), and pancreatic cancer (HR=2.58, P=0.009).
On the other hand, the risk of liver cancer decreased as telomere length increased. The HR was 0.72 for patients in quartile 5 compared to those in quartile 1 (Plinear=0.056).
The risk of 3 cancers was greatest for both the groups with extremely short and extremely long telomeres—quartiles 1 and 5, respectively.
For leukemia, the HR was 2.15 for quartile 1 and 1.68 for quartile 5, when compared to quartile 3 (Pnon-linear=0.015).
For bladder cancer, the HRs were 1.72 and 2.17, respectively (Pnon-linear=0.01). And for stomach cancer, the HRs were 1.63 and 1.55, respectively (Pnon-linear=0.020).
“We had the idea for this study more than 7 years ago, but it took the laboratory 3 months to finish quantifying telomere length for just 100 samples, which was not enough to draw any meaningful conclusions,” Dr Yuan said.
“Not even a decade later, we’ve been able to run nearly 30,000 samples in a year and draw these really robust insights, showing how far technology has come. Even more complicated will be linking telomere length to genome-wide analyses, which is on the horizon. We’re on the cusp of gaining a truly remarkable understanding of the complicated biological phenomena that lead to cancer.” ![]()
*The presentation differed from the abstract.
WASHINGTON, DC—Telomere length may predict cancer risk and could be a target for future therapies, according to research presented at the AACR Annual Meeting 2017.
The study suggests that, overall, longer-than-expected telomeres are associated with an increased risk of cancer.
However, investigators also found an increased risk of certain cancers, including leukemia, among patients who had very short or very long telomeres.
“Telomeres and cancer clearly have a complex relationship,” said study investigator Jian-Min Yuan, MD, PhD, of the University of Pittsburgh Cancer Institute in Pennsylvania.
“Our hope is that by understanding this relationship, we may be able to predict which people are most likely to develop certain cancers so they can take preventive measures and perhaps be screened more often, as well as develop therapies to help our DNA keep or return its telomeres to a healthy length.”
Dr Yuan and his colleagues presented their research as abstract 2267/21.*
The team analyzed blood samples and health data on 26,540 individuals enrolled in the Singapore Chinese Health Study, which has followed the health outcomes of participants since 1993. As of the end of 2015, 4060 participants had developed cancer (77 with leukemia).
The investigators divided participants into 5 groups, based on the length of their telomeres.
The group with the longest telomeres (quartile 5) had a significantly higher risk of developing any cancer than the group with the shortest telomeres (quartile 1), after taking into account the effects of age, sex, education, body mass index, smoking habits, and alcohol consumption. The hazard ratio (HR) was 1.33 (P<0.0001).
In particular, the group with the longest telomeres had a significantly increased risk of colorectal cancer (HR=1.37, P=0.010), breast cancer (HR=1.39, P=0.007), prostate cancer (HR=1.55, P=0.011), and pancreatic cancer (HR=2.58, P=0.009).
On the other hand, the risk of liver cancer decreased as telomere length increased. The HR was 0.72 for patients in quartile 5 compared to those in quartile 1 (Plinear=0.056).
The risk of 3 cancers was greatest for both the groups with extremely short and extremely long telomeres—quartiles 1 and 5, respectively.
For leukemia, the HR was 2.15 for quartile 1 and 1.68 for quartile 5, when compared to quartile 3 (Pnon-linear=0.015).
For bladder cancer, the HRs were 1.72 and 2.17, respectively (Pnon-linear=0.01). And for stomach cancer, the HRs were 1.63 and 1.55, respectively (Pnon-linear=0.020).
“We had the idea for this study more than 7 years ago, but it took the laboratory 3 months to finish quantifying telomere length for just 100 samples, which was not enough to draw any meaningful conclusions,” Dr Yuan said.
“Not even a decade later, we’ve been able to run nearly 30,000 samples in a year and draw these really robust insights, showing how far technology has come. Even more complicated will be linking telomere length to genome-wide analyses, which is on the horizon. We’re on the cusp of gaining a truly remarkable understanding of the complicated biological phenomena that lead to cancer.”
*The presentation differed from the abstract.
Dual targeting effective in HER2+ metastatic colorectal cancer
The combination of trastuzumab (Herceptin) and lapatinib (Tykerb) resulted in an overall objective response rate of 30% in heavily pretreated patients with HER2-positive metastatic colorectal cancer, according to findings presented at the annual meeting of the American Association for Cancer Research.
Of 33 patients, 2 patients achieved complete responses and 8 had partial responses, while 13 patients achieved stable disease. This brought the total clinical benefit rate to 70% at the time of data cutoff on Feb. 28.
“There is a large unmet need in colorectal cancer,” said study author, Silvia Marsoni, MD, director of the precision medicine unit at the Istituto di Candiolo, Fondazione del Piemonte per l’Oncologia–IRCCS in Turin, Italy.
“The combination of drugs really had a great impact on the tumor,” said Dr. Marsoni, who discussed the findings at a presscast. “One of these complete responders is still alive without evidence of disease at almost 36 months from the beginning of his treatment. This was a very good duration of response.”
HER2 amplification is found in 5% of RAS wild-type metastatic colorectal cancer cases. Dual HER2 blockade with both trastuzumab and lapatinib had inhibited tumor growth in preliminary studies, but that has not been the case for either drug used alone.
The HERACLES trial was conducted at four centers in Italy and enrolled 33 patients with RAS wild-type, HER2-positive tumors that were refractory to standard of care treatments, including the epidermal growth factor receptor (EGFR) inhibitors cetuximab and panitumumab.
“These patients were heavily pretreated and 75% had four or more prior treatments,” explained Dr. Marsoni.
All participants received trastuzumab intravenously with a 4 mg/kg loading dose followed by 2 mg/kg weekly, and lapatinib was given orally at 1,000 mg daily. Treatment continued until disease progression.
The primary endpoint was the objective response rate, and secondary endpoints included progression-free survival and safety.
The two patients who achieved a complete response continue to be disease free, and both had tumors that were refractory to cetuximab and resistant to all standard treatment.
Historically, the response rate in metastatic colorectal cancer after second-line treatment is very low, at less than 5% with chemotherapy and about 10%-20% with anti-EGFR therapy.
“There was really no toxicity,” explained Dr. Marsoni. “We used a lapatinib dose that was about 20% less than what is used in breast cancer to avoid GI toxicity.”
Only six patients (18%) experienced grade 3 side effects, which included fatigue, skin rash, and elevated bilirubin.
“In conclusion, we can say that, even if HER2-positive patients in colon cancer are only 3% of the population, they are still a little and important piece of the cake that can be actively targeted with a new chemotherapy-free regimen,” said Dr. Marsoni. “We have a new potential treatment for this population.”
The combination of trastuzumab (Herceptin) and lapatinib (Tykerb) resulted in an overall objective response rate of 30% in heavily pretreated patients with HER2-positive metastatic colorectal cancer, according to findings presented at the annual meeting of the American Association for Cancer Research.
Of 33 patients, 2 patients achieved complete responses and 8 had partial responses, while 13 patients achieved stable disease. This brought the total clinical benefit rate to 70% at the time of data cutoff on Feb. 28.
“There is a large unmet need in colorectal cancer,” said study author, Silvia Marsoni, MD, director of the precision medicine unit at the Istituto di Candiolo, Fondazione del Piemonte per l’Oncologia–IRCCS in Turin, Italy.
“The combination of drugs really had a great impact on the tumor,” said Dr. Marsoni, who discussed the findings at a presscast. “One of these complete responders is still alive without evidence of disease at almost 36 months from the beginning of his treatment. This was a very good duration of response.”
HER2 amplification is found in 5% of RAS wild-type metastatic colorectal cancer cases. Dual HER2 blockade with both trastuzumab and lapatinib had inhibited tumor growth in preliminary studies, but that has not been the case for either drug used alone.
The HERACLES trial was conducted at four centers in Italy and enrolled 33 patients with RAS wild-type, HER2-positive tumors that were refractory to standard of care treatments, including the epidermal growth factor receptor (EGFR) inhibitors cetuximab and panitumumab.
“These patients were heavily pretreated and 75% had four or more prior treatments,” explained Dr. Marsoni.
All participants received trastuzumab intravenously with a 4 mg/kg loading dose followed by 2 mg/kg weekly, and lapatinib was given orally at 1,000 mg daily. Treatment continued until disease progression.
The primary endpoint was the objective response rate, and secondary endpoints included progression-free survival and safety.
The two patients who achieved a complete response continue to be disease free, and both had tumors that were refractory to cetuximab and resistant to all standard treatment.
Historically, the response rate in metastatic colorectal cancer after second-line treatment is very low, at less than 5% with chemotherapy and about 10%-20% with anti-EGFR therapy.
“There was really no toxicity,” explained Dr. Marsoni. “We used a lapatinib dose that was about 20% less than what is used in breast cancer to avoid GI toxicity.”
Only six patients (18%) experienced grade 3 side effects, which included fatigue, skin rash, and elevated bilirubin.
“In conclusion, we can say that, even if HER2-positive patients in colon cancer are only 3% of the population, they are still a little and important piece of the cake that can be actively targeted with a new chemotherapy-free regimen,” said Dr. Marsoni. “We have a new potential treatment for this population.”
The combination of trastuzumab (Herceptin) and lapatinib (Tykerb) resulted in an overall objective response rate of 30% in heavily pretreated patients with HER2-positive metastatic colorectal cancer, according to findings presented at the annual meeting of the American Association for Cancer Research.
Of 33 patients, 2 patients achieved complete responses and 8 had partial responses, while 13 patients achieved stable disease. This brought the total clinical benefit rate to 70% at the time of data cutoff on Feb. 28.
“There is a large unmet need in colorectal cancer,” said study author, Silvia Marsoni, MD, director of the precision medicine unit at the Istituto di Candiolo, Fondazione del Piemonte per l’Oncologia–IRCCS in Turin, Italy.
“The combination of drugs really had a great impact on the tumor,” said Dr. Marsoni, who discussed the findings at a presscast. “One of these complete responders is still alive without evidence of disease at almost 36 months from the beginning of his treatment. This was a very good duration of response.”
HER2 amplification is found in 5% of RAS wild-type metastatic colorectal cancer cases. Dual HER2 blockade with both trastuzumab and lapatinib had inhibited tumor growth in preliminary studies, but that has not been the case for either drug used alone.
The HERACLES trial was conducted at four centers in Italy and enrolled 33 patients with RAS wild-type, HER2-positive tumors that were refractory to standard of care treatments, including the epidermal growth factor receptor (EGFR) inhibitors cetuximab and panitumumab.
“These patients were heavily pretreated and 75% had four or more prior treatments,” explained Dr. Marsoni.
All participants received trastuzumab intravenously with a 4 mg/kg loading dose followed by 2 mg/kg weekly, and lapatinib was given orally at 1,000 mg daily. Treatment continued until disease progression.
The primary endpoint was the objective response rate, and secondary endpoints included progression-free survival and safety.
The two patients who achieved a complete response continue to be disease free, and both had tumors that were refractory to cetuximab and resistant to all standard treatment.
Historically, the response rate in metastatic colorectal cancer after second-line treatment is very low, at less than 5% with chemotherapy and about 10%-20% with anti-EGFR therapy.
“There was really no toxicity,” explained Dr. Marsoni. “We used a lapatinib dose that was about 20% less than what is used in breast cancer to avoid GI toxicity.”
Only six patients (18%) experienced grade 3 side effects, which included fatigue, skin rash, and elevated bilirubin.
“In conclusion, we can say that, even if HER2-positive patients in colon cancer are only 3% of the population, they are still a little and important piece of the cake that can be actively targeted with a new chemotherapy-free regimen,” said Dr. Marsoni. “We have a new potential treatment for this population.”
FROM THE AACR ANNUAL MEETING
Key clinical point: Dual targeting resulted in a 30% objective response rate in heavily pretreated patients with HER2-positive colorectal cancer.
Major finding: Combination trastuzumab and lapatinib resulted in a 70% clinical benefit in heavily pretreated colorectal cancer patients.
Data source: Multicenter prospective study that included 33 patients with HER2-positive metastatic colorectal cancer who had been heavily pretreated.
Disclosures: The study was funded by the Associazione Italiana per la Ricerca sul Cancro, Fondazione Oncologia Niguarda Onlus, and Roche. The study’s lead investigator, Salvatore Siena, MD, has relationships with Amgen, Bayer, Celgene, Eli Lilly, Merck, Merrimack, Novartis, Roche, and Sanofi.